
Title: Obstetrical Nursing
Author: Carolyn Conant Van Blarcom
Release date: April 9, 2019 [eBook #59234]
Language: English
Credits: Produced by Richard Tonsing and the Online Distributed
Proofreading Team at http://www.pgdp.net (This file was
produced from images generously made available by The
Internet Archive)
Transcriber’s Note:
The cover image was created by the transcriber and is placed in the public domain.

THE CARESS
From the painting by Gari Melchers
In writing this book on obstetrical nursing I have been influenced by certain steadily deepening impressions which have been received in the course of my contact with maternity work in this country, Canada and England during the past twenty years. It has been borne in upon me, in the first place, that very often there is something akin to bewilderment among those nurses who have been trained to care for patients according to the teachings of one group of obstetricians and who later find themselves nursing the patients of other doctors who hold different, or even opposite views. And not infrequently I have found in the nurses a degree of loyalty to their training which made them sceptical, or even intolerant, of nursing methods which differed from those which they had been taught.
I have become convinced, therefore, that a book on obstetrical nursing which would be helpful to and widen the outlook of all nurses, no matter where nor by whom trained, must of necessity describe the underlying principles of obstetrical nursing and offer a survey of the nursing methods which are employed in maternity wards and hospitals of recognized excellence and in the practice of acknowledged authorities upon obstetrics.
This is, I am aware, a unique attitude, for the present text books on obstetrics for nurses reflect, in each instance, the wishes of one doctor, almost entirely, or advocate the methods employed in one hospital. My experience in teaching obstetrical nursing makes me feel that a parallel description of dissimilar nursing procedures serves to broaden the nurse’s attitude toward her work and her grasp of the entire subject, both because she becomes aware of the fact that methods, other than those with which she is familiar, are employed in hospitals of high standing and because she appreciates the fact that these unfamiliar methods may be as efficacious as those in which she has become expert.
xiiAccordingly I have devoted the better part of the past year and a half to a study of the scope and methods of the present training in maternity nursing in several hospitals, in this country and Canada, in which the obstetrical work is of a conspicuously high character, and have presented a composite of this teaching in the succeeding pages.
But that there might not be apparent inconsistencies in the different methods of maternity care described, I have given an explanation of the purposes and general principles of the care, including nursing, which the nurse is likely to find is given to all obstetrical patients, the country over.
For the sake of simplicity and clarity I have divided the book into seven parts, following an introduction which describes the requisites and opportunities of obstetrical nursing and the importance of the nurse’s own attitude toward her work and her patient. The first two parts, dealing with the normal anatomy and physiology of the female generative tract and the development of the fetus, are designed to supply the nurse with enough technical information to make her ministrations intelligent and effective. In this respect, I have doubtless given less than some nurses will wish and possibly more than others will think necessary, but I have given about the average amount of instruction that is found satisfactory in the training schools of high standing. Four of the succeeding parts are devoted respectively to a description of the nurse’s duties during pregnancy, labor, the puerperium and early infancy. In each of these I have explained, first, the normal physiological processes which take place; then, the nurse’s duties under average conditions and finally, her responsibilities in the event of complications or abnormalities. A separate part is devoted to a description of the organized care and instruction of the maternity patient, by public health nurses, both before and after delivery, which have proved to be satisfactory.
While describing various hospital procedures, I have deemed it of practical importance to explain, in each instance, how similar results might be obtained, with improvised appliances, in a patient’s home whether in a city or a rural community. In xiiishort, I have endeavored to make clear the essentials of obstetrical nursing without regard to the status or location of the patient.
Since the patient’s state of nutrition and her frame of mind are of vital importance throughout pregnancy, labor and the puerperium, I have not only dwelt upon them in all descriptions of the nurse’s duties during these periods but have devoted an entire chapter to a simple explanation of the principles of each of these two important subjects.
My varied contact with obstetrical nurses has convinced me that those nurses who appreciate the never ending wonder and beauty of this miracle of the beginning of a new life, derive peculiar satisfaction from the care of the maternity patient. At the same time, in many hospitals, even where the patients are given the most conscientious care, the nurses are often so nearly overwhelmed by the long, irregular hours and the insistent demands of routine duties, that they do not grasp the significance of the event in which they are participants. Accordingly, I have made a sustained effort throughout the following pages to give the young nurse something of a feeling of reverence for this great mystery of birth.
In the course of my survey of the present training in obstetrical nursing, I have met the warmest generosity on the part of the obstetrical and nursing staffs in all of the hospitals which I have visited. Accordingly, I find it very difficult to find adequate expression for my sense of gratitude to the doctors and nurses of the Montreal Maternity Hospital; the Burnside Obstetrical Department of the Toronto General Hospital; The Hospital of the University of Pennsylvania; Bellevue Hospital; The Long Island College Hospital; The Brooklyn Hospital; The Cleveland Maternity Hospital and to Dr. J. Whitridge Williams and Miss Elsie Lawler for making available the entire resources of the wards, clinics, laboratories and class and lecture rooms at Johns Hopkins Hospital.
I wish to offer an expression of deepest possible appreciation to Dr. John W. Harris for the generosity with which he has given of his time, thought and wide experience in an effort to xivprovide accurate and practical information, and to set a high standard of work and ideals for those nurses who would be influenced by this book. Having taught and lectured to nurses, as well as medical students, for years, Dr. Harris is in a position to give counsel and criticism of peculiar value to a book on obstetrical nursing and he has given these throughout the entire preparation of this book.
Because of their concern with any effort to better the state of mothers and babies, I have been given suggestions, assistance and inspiration with the most selfless generosity by The Reverend Father John J. Burke; Dr. J. Clifton Edgar; Dr. Frederic W. Rice; Dr. J. P. Crozer Griffith; Dr. Caroline F. J. Rickards; Dr. Esther Loring Richards; Dr. E. V. McCollum; Miss Nina Simmonds and Dr. John R. Fraser. Among the many nurses with whom I have conferred, I have met a characteristic spirit of helpfulness which has expressed itself in their eager readiness to pass on to other nurses the benefits of their own training and experience. Those to whom I am especially indebted, for aid and suggestions, are Miss Calvin MacDonald; Mrs. Bessie Amerman Haasis; Miss Robina Stewart; Miss Caroline V. Barrett; Miss Katherine de Long; Miss Jean Gunn; Miss Mary E. Robinson; Miss Sara Cooper; Miss Laura F. Keesey; Miss Chelly Wasserberg; Miss Kate Madden; Mrs. Minnie S. Brown; Miss Anne Stevens; Miss Madge Allison and Miss Katherine Tucker.
To Mrs. Elizabeth Porter Wyckoff I am under heavy obligation for most discriminating editorial assistance and for her farsighted criticisms toward increasing the clarity of the text. And I feel sure that the tender little poem on the miracle of motherhood, which Mrs. Elizabeth Newport Hepburn wrote expressly for this book, will be as warmly appreciated by my readers as it is by me.
I wish to express my deep gratitude to Mr. Max Brodel for his invaluable counsel and guidance in planning and assembling the illustrations to elucidate the text. And I am very grateful to Mr. Gari Melchers for the spirit which I believe is infused into this book through the reproduction of two of his lovely paintings of a mother and baby, and to Mr. Russell Drake for xvhis valuable drawings. I wish further to thank Mr. J. Norris Myers, of The Macmillan Company, for unfailing courtesy and helpfulness in facilitating all matters relating to the publication of this book.
For statistical information I am indebted to Dr. Louis I. Dublin and for authority in offering the scientific background of the teaching I have drawn from “The Practice of Obstetrics” by J. Clifton Edgar; “Obstetrics” by J. Whitridge Williams; “The Diseases of Infants and Children” by J. P. Crozer Griffith and “The Prospective Mother” by J. Morris Slemons.
| PAGE | ||
|---|---|---|
| Preface | xi | |
| Introduction | 3 | |
| PART I. | ||
| ANATOMY AND PHYSIOLOGY | ||
| CHAPTER | ||
| I. | Anatomy of the Female Pelvis and Generative Organs | 19 |
| II. | Physiology | 45 |
| PART II. | ||
| THE DEVELOPMENT OF THE BABY | ||
| III. | Development of the Ovum, Embryo, Fetus, Placenta, Cord and Membranes | 61 |
| IV. | Physiology of the Fetus | 84 |
| V. | Signs, Symptoms, and Physiology of Pregnancy | 93 |
| PART III. | ||
| THE EXPECTANT MOTHER | ||
| VI. | Prenatal Care | 111 |
| VII. | Mental Hygiene of the Expectant Mother | 145 |
| VIII. | Preparation of Room, Dressings, and Equipment for Home Delivery | 155 |
| IX. | Complications and Accidents of Pregnancy | 164 |
| PART IV. | ||
| THE BIRTH OF THE BABY | ||
| X. | Presentation and Position of the Fetus | 217 |
| XI. | Symptoms, Course, and Mechanism of Normal Labor | 232 |
| XII. | Nurse’s Duties During Labor | 243 |
| XIII. | Obstetrical Operations and Complicated Labors | 295 |
| xviiiPART V. | ||
| THE YOUNG MOTHER | ||
| XIV. | Physiology of the Puerperium | 317 |
| XV. | Nursing Care During the Normal Puerperium | 323 |
| XVII. | The Nursing Mother | 357 |
| XVII. | Nutrition of the Mother and Her Baby | 368 |
| XVIII. | Complications of the Puerperium | 391 |
| PART VI. | ||
| THE MATERNITY PATIENT IN THE COMMUNITY | ||
| XIX. | Organized Prenatal Work | 405 |
| XX. | Care of the Mother and Baby by Visiting Nurses | 437 |
| PART VII. | ||
| THE CARE OF THE BABY | ||
| XXI. | Characteristics and Development of the Average New-born Baby | 451 |
| XXII. | Nursing Care of the Average New-born Baby | 461 |
| XXIII. | Common Disorders and Abnormalities of Early Infancy | 518 |
| XXIV. | A Final Word | 544 |
| ILLUSTRATIONS | ||
| Anatomy and Physiology. | ||
| FIG. | PAGE | |
|---|---|---|
| 1 a. | Normal female pelvis | 21 |
| b. | Normal male pelvis | 21 |
| 2. | Diagram of pelvic inlet seen from above | 22 |
| 3. | Diagram of pelvic outlet seen from below | 23 |
| 4. | Sagittal section of the pelvis | 24 |
| 5. | Two types of pelvimeters | 25 |
| 6. | Diagram showing method of measuring distance between crests, spines and trochanters | 26 |
| 7. | Diagram showing method of measuring Baudelocque’s diameter | 27 |
| 8. | Diagram showing method of estimating true conjugate | 28 |
| 9. | Diagram showing method of measuring intertuberous diameter | 29 |
| 10. | Anterior view of external and internal female generative organs | 31 |
| 11. | Diagrams of sections of virgin and multiparous uteri | 32 |
| 12. | Sagittal section of female generative tract | 35 |
| 13. | Diagram of external female genitalia | 39 |
| 14. | Sagittal section of breast | 42 |
| 15. | Front view of breast | 43 |
| 16. | Diagram of human ovum | 47 |
| Development of the Baby | ||
| 17. | Diagram of human spermatozoa | 61 |
| 18. | Diagram of segmenting rabbit’s ovum | 65 |
| 19. | Ovum about 13 days old embedded in the decidua | 66 |
| 20. | Diagram of developing fetus, cord, membranes and placenta in utero | 69 |
| 21. | Diagram of structure of placenta | 71 |
| 22. | Photograph of placental vessels | 72 |
| 23. | Maternal surface of the placenta | 74 |
| 24. | Fetal surface of the placenta | 75 |
| 25. | Embryo about 5.5 cm. long in amniotic sac | 77 |
| 26. | Outlines of fetus at different stages | 78 |
| 27. | Full term fetus in utero | 81 |
| xx28. | Diagram of fetal circulation | 85 |
| 29. | Diagram of circulation after birth | 87 |
| 30. | Side and top view of fetal skull | 90 |
| The Expectant Mother. | ||
| 31. | Height of fundus at different stages of pregnancy | 94 |
| 32. | Contour of abdomen at ninth month | 95 |
| 33. | Contour of abdomen at tenth month | 95 |
| 34. | Front view of home-made abdominal binder | 123 |
| 35. | Side view of same | 123 |
| 36. | Back view of same | 123 |
| 37. | Abdominal binder used in above | 124 |
| 38. | Front view of home-made stocking supporters | 124 |
| 39. | Back view of same | 124 |
| 40. | Patient in right-angled position to relieve varicose veins | 138 |
| 41. | Elevated Sims position | 139 |
| 42. | Gloves, ready for dry sterilization | 160 |
| 43. | Delivery pad of newspapers and old muslin | 161 |
| 44. | Diagram of centrally implanted placenta prævia | 174 |
| 45. | Partial placenta prævia | 175 |
| 46. | Diagram of marginal placenta prævia | 176 |
| 47. | Champetier de Ribes’ bag inserted in uterus | 177 |
| 48. | Patient in hot pack given with dry blankets | 197 |
| 49. | Method of giving infusion | 202 |
| The Birth of the Baby. | ||
| 50. | Attitude of fetus in uterus at term | 217 |
| 51. | Illustration from first text-book on obstetrics | 218 |
| 52. | Attitude of fetus in breach presentation | 219 |
| 53. | Attitude of fetus in vertex presentation | 220 |
| 54. | Diagram of six positions in a vertex presentation | 222 |
| 55. | Diagram of six positions in a face presentation | 223 |
| 56. | Diagram of six positions in a breech presentation | 223 |
| 57. | First maneuver in abdominal palpation | 225 |
| 58. | Second maneuver in abdominal palpation | 226 |
| 59. | Third maneuver in abdominal palpation | 227 |
| 60. | Fourth maneuver in abdominal palpation | 228 |
| 61. | Diagrams showing positions of nurse’s hands in four maneuvers of abdominal palpation | 229 |
| 62. | Ascertaining position of fetus by rectal examination | 230 |
| xxi63, 64, 65, 66. | Diagrams showing stages of dilatation and obliteration of cervix | 234 |
| 67. | Characteristic position of patient during first stage pains | 235 |
| 68. | Diagram indicating rotation and pivoting of head during birth | 236 |
| 69. | Anterior shoulder being slipped from under symphysis | 237 |
| 70. | Birth of posterior shoulder | 238 |
| 71. | Diagrams of Duncan and Schultze mechanisms of placental separation | 239 |
| 72. | Section showing thinness of uterine wall before birth of fetus | 240 |
| 73. | Section showing thickness of uterine wall immediately after labor | 241 |
| 74. | Preparing patient for vaginal examination or delivery | 250 |
| 75. | Patient draped for vaginal examination | 251 |
| 76. | Wrong and right methods of boiling gloves | 253 |
| 77. | Powdering hands before putting on dry gloves | 254 |
| 78. | Successive steps in proper method of putting on gloves | 255 |
| 79. | Bed and simple equipment ready for normal delivery | 258 |
| 80. | Instruments shown in Fig. 79 | 260 |
| 81. | Old prints showing early methods of delivery | 261 |
| 82. | Patient draped with sterile dressings for delivery | 262 |
| 83. | Patient pulling on straps while bearing down during second stage | 264 |
| 84. | Palpating baby’s head through perineum | 265 |
| 85. | Baby’s head appearing at vulva | 266 |
| 86. | Head farther advanced | 267 |
| 87. | Holding back head at the height of a pain | 268 |
| 88. | External rotation following birth of head | 269 |
| 89. | Wiping mucus from baby’s mouth | 270 |
| 90. | Stroking baby’s back to stimulate respirations | 271 |
| 91. | Two clamps on cord after pulsation has ceased | 272 |
| 92. | Wrong and right method in tying knot in cord ligature | 272 |
| 93. | Stimulating baby’s respirations | 274 |
| 94, 95. | Stimulating baby’s respirations | 275, 276 |
| 96, 97. | Resuscitating baby by holding under warm water | 277, 278 |
| 98. | Resuscitation by means of direct insufflation | 279 |
| 99. | Delivery of the placenta | 280 |
| 100. | Twisting membranes while withdrawing placenta | 281 |
| 101. | Massaging fundus through abdominal wall | 282 |
| 102. | Showing prolapsed cord between head and pelvic brim | 285 |
| 103. | Giving chloroform for obstetrical anæsthesia | 287 |
| 104, 105. | Giving ether for obstetrical anæsthesia | 289, 290 |
| 106. | Giving ether for complete anæsthesia | 293 |
| xxii107. | a. Tarnier forceps, b. Simpson forceps | 301 |
| 108. | Patient in position and draped for forceps operation | 302 |
| 109. | Forceps sheet used in Fig. 108 | 303 |
| 110. | Two types of leggings for obstetrical use | 304 |
| 111. | Rubber bougie | 311 |
| 112. | Champetier de Ribes’ bag | 311 |
| 113. | Voorhees’ bag | 312 |
| 114. | Bag held in forceps for introduction into uterus | 312 |
| 115. | Syringe for filling above bags after insertion | 312 |
| The Young Mother. | ||
| 116. | Height of fundus on each of first ten days after delivery | 327 |
| 117. | Patient draped for postpartum dressing | 336 |
| 118. | Equipment in rack used in Fig. 117 | 337 |
| 119. | Method of covering nipples with sterile gauze | 339 |
| 120. | Baby nursing through a nipple shield | 341 |
| 121. | Nipple shield used in Fig. 120 | 342 |
| 122. | Supporting heavy breasts by means of folded towels | 343 |
| 123. | Ice caps applied to engorged breasts | 344 |
| 124. | Y binder before application | 345 |
| 125. | Y binder applied | 346 |
| 126. | The same seen from the other side | 347 |
| 127. | Indian binder | 347 |
| 128. | Method of stripping | 348 |
| 129, 130, 131, 132, 133, 134, 135. | Bed exercises taken during the puerperium | 350 to 353 |
| 136. | Knee-chest position | 354 |
| 137. | Exercising by walking on all fours | 354 |
| 138. | Position of mother and baby for nursing in bed | 359 |
| 139. | The Nursing Mother (from a painting by Gari Melchers) | 361 |
| 140. | Baby partially blind as a result of a faulty diet | 378 |
| 141. | Rachitic and normal babies of the same age | 381 |
| 142. | Chest walls of normal and rachitic rats of the same age | 383 |
| 143. | Interior of specimens in Fig. 142 | 384 |
| The Maternity Patient in the Community. | ||
| 144. | Baby’s bed improvised from a market basket | 415 |
| 145. | Layette recommended to expectant mothers by Maternity Centre Association | 416 |
| 146. | Breast tray recommended to expectant mothers by Maternity Centre Association | 417 |
| xxiii147. | Baby’s toilet tray recommended to expectant mothers by Maternity Centre Association | 417 |
| The Baby. | ||
| 148. | Diagram of first teeth | 456 |
| 149. | Umbilical cord immediately after birth | 457 |
| 150. | The same four days later | 457 |
| 151. | Umbilicus immediately after separation of cord | 458 |
| 152. | Well healed umbilicus | 458 |
| 153. | Nursery at Manhattan Maternity Hospital | 465 |
| 154. | Bathing the baby | 467 |
| 155. | Preparation for circumcision | 468 |
| 156. | Baby draped with sterile sheet, in above | 469 |
| 157. | Cord dressed with dry sterile gauze | 470 |
| 158. | Abdominal binder applied over cord dressing | 471 |
| 159. | Satisfactory baby clothes | 473 |
| 160. | Diagonally folded diaper applied | 474 |
| 161. | Longitudinally folded diaper applied | 474 |
| 162. | Sutton poncho to protect baby for outdoor sleeping | 479 |
| 163. | Training the baby to use a chamber | 481 |
| 164. | Stiff cuffs to prevent thumb sucking | 483 |
| 165. | Hammer cap to prevent ruminating | 484 |
| 166. | Ruminating cap applied | 485 |
| 167. | Proper method of carrying baby | 487 |
| 168. | Preparing the baby’s milk | 493 |
| 169. | Giving the baby his bottle | 496 |
| 170. | Holding baby upright after feeding | 497 |
| 171. | Dr. Griffith’s table of fat percentages | 500 |
| 172. | Reverse side of above card | 501 |
| 173. | Baby in a basket ready to travel | 507 |
| 174. | Quilted robe with hood for the premature baby | 509 |
| 175. | Premature baby in lined basket, being fed with Boston feeder | 510 |
| 176. | Bed for premature baby improvised from small clothes basket | 511 |
| 177. | Putting the baby in a wet pack | 521 |
| 178. | Baby in wet pack | 522 |
| 179. | Diagrams showing successive steps in giving the baby a pack | 522 |
| 180. | Baby wrapped in blanket preparatory to gavage | 523 |
| 181. | Gavage | 524 |
| 182. | Obtaining a fresh specimen of urine from the baby | 526 |
| 183. | Obtaining a 24–hour specimen of urine from the baby | 527 |
| xxiv184. | Band to hold baby’s legs while obtaining specimens of urine | 527 |
| 185. | Belt used to hold tube for specimen | 528 |
| 186. | Giving the baby an enema | 530 |
| 187. | Irrigating the eye with a blunt nozzle | 536 |
| 188. | Method of holding baby for treating gonorrhœal ophthalmia | 537 |
| CHARTS. | ||
| No. | ||
| 1. | Showing drop in blood pressure and albumen, after delivery, in eclampsia | 204 |
| 2. | Showing persistence of high blood pressure and albumen in the urine, after delivery, in nephritic toxæmia with convulsions | 206 |
| 3. | Showing temperature curve in streptococcus infection | 397 |
| 4. | Showing temperature curve in gonorrhœal infection | 398 |
| 5. | Showing normal weekly gain in weight during first year of life | 454 |
| 6. | Showing normal daily gain in weight during first two weeks | 520 |
| 7. | Showing loss of weight in inanition fever contrasted with No. 6 | 520 |
| 8. | Showing rise in temperature in inanition fever | 520 |
The avowed purpose of care given to the maternity patient to-day is to minimize the discomforts and perils of her pregnancy, labor, and the puerperium, and so safeguard her and her baby that both will emerge from the lying-in period in a satisfactory condition and with a bright prospect of having permanently good health.
The striking difference between obstetrics as practiced to-day, and that of former times, is that it now lays as much stress upon the future health of the mother and baby as it does upon their immediate safety.
Happily, the present-day obstetrician, who assumes the care of an expectant mother, does so with confidence and optimism because of the available knowledge upon which he may draw for her benefit. Progress in the various branches of medicine and nursing is steadily pointing the way toward greater and more effective safeguards for the maternity patient and her baby.
The value of these safeguards is attested to by the satisfactory results of the care which is given to the patients in well conducted hospitals or in their homes by careful physicians; by various out-patient departments and nursing organizations to patients within their reach. These results are in the form of a large proportion of mothers and babies who are well and continue to be well.
That is one view of the matter. Looking at it from another aspect, we discover that more than seven women still lose their lives for each 1,000 births that occur in this country, the actual number varying in different localities. Childbirth is still second to tuberculosis as a cause of death among women between fifteen and forty-five years of age, and in spite of the proved value of care in making maternity a safe adventure, the larger 4proportion of these women die from infection or toxæmia which are almost entirely preventable.
The incredible fact in this connection is that, while there has been a decline in the deaths from such other controllable conditions as typhoid fever and some of the infectious diseases of childhood, there has been an actual increase in deaths from preventable causes associated with child-bearing.
Dr. Dublin estimates that throughout the United States as a whole, during 1920, the total number of deaths due to childbirth was about 20,000.
In addition to the high death rate among mothers the mortality among babies is even greater. Dr. Dublin estimates that out of every 1,000 babies born during 1920, about 85 died before they were a year old, or about 200,000 in the course of the year, and that the large majority of these died from congenital causes, from infection or nutritional disturbances. Another 100,000 babies perish, yearly, through still births. As all of these conditions are preventable to a greater or lesser degree, we have to acknowledge that many babies die whom we know how to save. There is sound reason, therefore, for the belief that proper care would save the lives of about two-thirds of the mothers and half of the babies who now die and half of the babies who are born dead.
And let it be remembered that conditions which destroy life, also destroy or greatly impair health and resistance to disease. Although we may count the number of mothers and babies who fail to survive the too severe test to which they are put during crucial periods in the lives of both, we cannot count, nor even approximately estimate, the number of those who escape death only to be imprisoned in frail, deformed, or diseased bodies. Therein lies much of the tragedy which follows in the wake of neglect—the lifelong handicaps, suffering, and inefficiency that need not have been.
This lack of care is not due to limitations in medical knowledge, for the efficacy of known methods is being constantly demonstrated. And our instant and generous response, the country over, to appeals for help in relieving various forms of need and disaster does not suggest a national cold-bloodedness, 5or even indifference, to needless suffering. But still a legion of mothers and babies die each year from lack of care, and almost at our very thresholds.
Perhaps the root of the difficulty lies in the fact that childbirth, as well as the attendant suffering and death, are so familiar that they are regarded as being normal incidents in the ordinary course of affairs.
One of the most dramatic of all human events, the birth of a new being, is accepted casually, almost without concern, because it is so frequent—so commonplace.
Moreover, we are all accustomed to hearing stressed the fact that child-bearing is not a disease, but is a normal physiological function.
Not so generally, however, do we hear emphasis made upon the equally important facts that there is extreme danger of infection while these physiological functions are in progress, and that they subject the entire organism to such a strain that there results a dangerously narrow margin between health and disease.
Accordingly, too much is expected, or taken for granted, from the provisions which Nature has made to promote these functions, and not enough assistance is given to protect the mother, while they are in course, or to help the immature baby in adjusting himself to the greatest change which he makes during the entire span of his existence.
When the time comes, and it seems to be approaching, that pregnancy, labor, the puerperium and infancy are regarded as crucial periods in the life history, demanding all the preventives and safeguards that all branches of medicine and nursing can offer, these periods will cease to be so enormously destructive of life and health.
We cannot build a strong race with sickly and maimed mothers and babies, and we can scarcely have other than sickly and maimed mothers and babies without care.
Apparently, then, our national health is in a large measure dependent upon good obstetrics and good obstetrics includes good nursing.
Good nursing implies more than the giving of bed baths and medicines, boiling instruments and serving meals. It is more 6than going on duty at a certain time, carrying out orders for a certain number of hours and going off duty again. It implies care and consideration of the patient as a human being and a determination to nurse her well and happily, no matter what this demands.
In carrying on her work, the maternity nurse may be called upon to aid in prenatal supervision and instruction; to prepare for and assist with a delivery, or to give either exclusive or visiting nursing care to a young mother and her baby. These patients may be in a hospital or at home and the home may be of any kind from a palace to a hut or a tenement. The patients may be in a city, a small town, or a rural community, and in the care of doctors whose methods vary widely.
But in spite of the diversity of conditions and the fact that no two will be quite alike, the general need of all of these patients will be the same.
Their need is care, which includes cleanliness in order to prevent infection; suitable food; fresh air and exercise; regular and sufficient rest and sleep; an equable body temperature; early treatment of complications and correction of physical defects. In short, each patient needs to be watched; needs clean care and to practice the approved principles of personal hygiene from the beginning of pregnancy. This without regard to race, color, creed, occupation, status, or location. It means all maternity patients and their babies the country over.
There was a time when the obstetrician first saw his patient in labor or shortly beforehand, and when the care of the baby began at birth or soon afterward.
We know what this tardy attention has cost in human lives and suffering.
We know, too, that among the mothers, abortion, miscarriages, toxæmias, difficult or impossible labors may be largely prevented through prenatal care; while among babies, the enormously high death rate, during the first month of life from causes which begin to operate before birth, convinces us that we must begin to take care of the baby nine months before he is born, if he is to have the greatest benefits of present available knowledge. Such early care reduces still births and injury during labor; it reduces premature births, which is important, 7because the nearer the baby goes to term the better his chance of survival and of good health, and prenatal care also increases the prospects of satisfactory breast feeding.
Although we know that the ideal is to have all maternity patients supervised and instructed entirely by a physician from the beginning of pregnancy and then delivered in a well conducted hospital, it is scarcely probable that this ideal will ever be realized. There will always be patients who cannot afford to employ a doctor for so long a period; there will always be communities in which hospital provisions do not exist or are inadequate. There will always be expectant mothers whom it would be unwise to remove from home, excepting under pressing conditions, because of the influence exerted by their mere presence in keeping the family group intact. And so on, through a number of deterring conditions which will probably never cease to exist, and which will keep the patient at home.
Since patients who are supervised during pregnancy and delivered in hospitals usually recover, the high rate of death and injury, in this country, is to be found among women who are unsupervised before labor and subsequently delivered at home. Accordingly, if this widespread injury is to be reduced, the essentials of the care which is found to be efficacious must be made available for all patients throughout the length and breadth of the land.
Prenatal care, clean deliveries, and intelligent motherhood will go far toward solving the problem of a high maternal and infant death rate, and these require not widespread care, alone, but widespread teaching as well—impressing upon women and their families the importance of care and precautions in connection with childbirth. Important as it is for men to study and inform themselves in regard to the problems of finance and cattle raising, for example, it is still more important for both men and women to study and appreciate the problems of expectant and actual motherhood.
It is in this teaching that the nurse may be immeasurably helpful, in fact is indispensable, for the carrying of approved care into the home and the general teaching of personal hygiene are inextricably bound up with nursing.
8The details of the care and teaching of patients are, of course, specified by a doctor or a medical board, but the effectiveness of the planning, whether for one or several patients, is very largely dependent upon the nurse’s intelligence, interest and conscientiousness, and her ability to teach.
This is borne out by the almost uniform recommendations, made by official bodies, for provisions looking toward the reduction of maternal and infant deaths including as they do the following:
1. The employment of public health nurses. (To give home care or instruction or both.)
2. The establishment of prenatal clinics and baby health centers. (In both of these the nurse aids in supervising and teaching the mother how to take care of herself and her baby.)
3. Trained attendance during labor. (The nurse aids greatly in preparing for and assisting with clean deliveries.)
4. Improved and increased hospital facilities. (There cannot be good hospital work without good nursing.)
5. Prompt and accurate registration of births. (Here, too, the nurse may be helpful by always making sure that the birth has been reported.)
Here is no light task nor mean privilege which is set before the nurse and in order to meet them fitly she must be prepared. The indispensable requisites for nursing and teaching the maternity patient, whether at home or in a hospital, are training, an exacting conscience, and genuine concern for her patient as an individual.
A certain amount of scientific knowledge is necessary, in this as in any other field, to give the nurse an intelligent background and a kind of definiteness and stability to her work. She should be trained in the essentials of general nursing, of surgical nursing and operating room technique, and in the care of babies. She must of necessity know something of the anatomy and physiology of the female generative organs; the physiological adjustments during pregnancy; the development of the baby within the uterus; the normal process, or mechanism, of labor, and the changes which ordinarily take place during the puerperium. 9Such information will make clear to her the reasons for the care which she gives to her patient, and accordingly her care will be more intelligent. And she will be better able to recognize the difference between evidences of normal physiological changes and the symptoms of complications.
Two of the newer branches of medicine—nutrition and mental hygiene or psychiatry—have a more and more apparent relation to the safety and welfare of the maternity patient, and accordingly are of moment to the maternity nurse. For, it must be remembered, it is the purpose of obstetricians to-day to establish future health for their patients as well as immediate safety. The nurse should endeavor to help with all that the doctor attempts to do toward these ends, and in order to help she must understand.
The maternity nurse can scarcely be expected to specialize in nutrition or in psychiatry, but she may give to her patients the practical benefits of many valuable discoveries in these fields. She may not be able to remember, for example, all of the sources and purposes of lime in the diet, nor of each of the protective substances, often referred to as vitamines, but any nurse can remember and be guided by the fact that her patient will not be satisfactorily nourished either before or after the birth of the baby unless she has a varied diet containing milk, eggs, and green vegetables. She also can explain to her patients that faulty dietaries are responsible for the tradition that each child costs the mother a tooth, as well as the fact there may be undernourishment even among babies who are fed at the breast, if the mother’s diet is inadequate.
And though the mass of nurses cannot be expected to grasp all of the intricacies of psychiatry, they may without exception apply one of its most important principles by adopting a warm and sympathetic attitude toward their patients and by this means win their trust and confidence. The restfulness of this; the relaxation and general state of mind that this will engender in a large proportion of patients will exert a definitely beneficial effect upon the physical well-being of the expectant mother, the woman in labor and the nursing mother.
These simple applications of important scientific discoveries 10that relate to the everyday life of her patient—these are things for the maternity nurse to bear in mind. She is nursing a human being who is passing through crucial periods and anything that affects her as a human being affects her as a patient.
Apparently, then, the work of the obstetrical nurse necessitates a training in general nursing and its various branches, in addition to obstetrics, for there seems to be no aspect of nursing which may not, under some condition, have its place in the care of the mother or her baby. All of this training, however, will prepare her for effective work only if she herself has a spirit of eagerness and enthusiasm. But if she has these and even a little training, she may do much.
Accordingly, let the nurse who has been prepared by a general and special training, and who wants to be of the greatest possible service to the maternity patient start by appreciating a few general principles which will be absolutely indispensable to the success of her work. They may be expressed somewhat as follows:
1. Cleanliness—under all conditions, to protect both mother and baby from infection.
2. Watchfulness—for early symptoms of complications in either mother or baby.
3. Adaptability—to the patient, the doctor, and the surroundings.
4. Sympathy—for every mental and physical stress which the patient may suffer.
If the nurse convinces herself of the import of these requirements and is exacting of herself in giving them broad interpretation, she cannot but nurse her patients well.
She will appreciate the invariable need for cleanliness and watchfulness if she will hark back to the fact that our mothers and babies die in distressingly large numbers from infections, toxæmias, and nutritional disturbances, all of which are usually amenable to preventive or early treatment.
In order to be always clean, always watchful, and always ready to execute, both in letter and spirit, the orders of doctors whose methods of treatment will differ, the nurse will need to be very adaptable. She will need to keep a clear head 11and an open mind and to remember always the ends that are being striven for: the immediate safety and the future wellbeing of the mother and the baby. And she may rest assured that, no matter how they vary as to details, all doctors want all of their patients to be given clean care; watched for symptoms of complications; and given good general nursing.
Considering the need for cleanliness in a very broad and practical sense, the nurse will realize that the test of her ability to protect her maternity patients from infection is not what she is able to do in a hospital where there is every facility for clean work. It is not the ability to maintain asepsis in a tiled operating room that counts, where she is aided by sterilizers, basins, and solutions of various kinds and colors, a wealth of ingenious appliances and a corps of co-workers. It is the understanding and imagination which will enable her, perhaps single-handed, to carry the principles of such work into a patient’s home; to do clean work, from the standpoint of avoiding infection, in a mountain hut or a city tenement where everything is dirty.
The nurse will do well to begin to develop her powers of adaptability while she is still in training. She may greatly increase the value of her hospital experience by trying always to understand the purpose of the care which she is giving and trying at the same time to imagine how, in an average home, she would accomplish the results of this or that procedure which is made easy of execution in the hospital by special equipment. She should never lose sight of the fact that she is not being trained solely to conform to any one hospital routine or to become expert in only one method of nursing care. She is being prepared to go out and give nursing care to any young woman and her baby who need it, no matter where or how they are situated or by what methods they are treated.
If conditions are such that the doctor’s orders and the patient’s requirements seem impossible of fulfillment, then the nurse must attempt the impossible and attempt it with confidence of success.
It is clear that the nurse must cultivate adaptability and resourcefulness if she is to give good care to all her patients 12under all conditions. But even the most efficient and intelligent work will not be wholly satisfactory unless it is infused with a spirit of sympathy for the woman as an individual.
The thing that counts in this connection is what the nurse, herself, means to the woman who is facing a very important and mysterious event, who, after every known aid has been given, must still go through a great deal alone, both mentally and physically. It is not helpful to a woman in such a situation to be told that women have borne children since the dawn of Creation and that they all have had pain; that she will have to go through with it, as they have, and that the less fuss she makes about it the better. But it does help her to have the nurse say that she has been with so many women in labor that she knows they suffer intensely, and because she knows it so well she wants to do all that lies in her power to give even a little relief. The nurse may never know just how she has helped and reassured; how a pain was made a little easier to bear, not only by the hand slipped under an aching back, but also by the sympathy that the act conveyed. But she may be sure that she has helped.
In such a connection, the nurse must guard against the mistake of dividing her patients into well defined groups: those who are poor and those who are more favored. If she unfailingly looks for the human being beyond the patient she will find some of the most sensitive and appreciative of women among the simplest and poorest and they will be warmly responsive to a thoughtful, considerate attitude. And at the same time, the patient in comfortable circumstances who seems to be surrounded by all that one could desire, is often pathetically lonely and isolated. She, too, will be appreciative of encouragement and an attitude of concern for her comfort.
Suffering and anxiety make no class distinctions and have a very leveling effect, for prince and pauper, alike, need sympathy when afflicted.
From the standpoint of the nurse herself, there might be discouragement in this description of what is expected of her, and what are her opportunities in this work of caring for mothers and babies, if she did not go straight to the heart of 13the matter and see that all that is needed, after all, is good nursing. She must realize, of course, that good nursing necessitates training and a spirit of such eager service that she will do for her patient all that lies in her perhaps limited power, and then try to learn of still more that she may offer. And she may rest assured that the value of her work will be quite as dependent upon such a spirit as upon her training.
Obstetrical nursing may be defined, with accuracy, as the nursing care of an obstetrical patient, but its true significance is limited only by the nurse’s ability, resourcefulness, and vision. And the more spirituality which pervades this work the more effective will be the nurse’s skilled ministrations and the more satisfying will it all be to her.
This aspect of maternity nursing—what it means to the nurse herself—should be given full recognition, for although the demands which are made upon her are exacting, she will find more than compensating interest and gratification in her work.
It provides a channel of expression for some of her most elemental and deeply rooted impulses. The desire to create exists within most of us, and surely the nurse tastes of the joys of creation when she watches the beautiful baby body grow and develop under her care. And she has a consciousness of patriotic service, too, for while helping to secure the immediate safety and future health of the baby citizen she is helping to build a strong race.
But this work goes still further and offers even more than these.
The average nurse has a deep maternal instinct. She may not be conscious of it as such, but it is this instinct which prompts her to select nursing from the wide range of occupations and professions which are open to her. And it is entirely natural that she should derive great satisfaction from this vicarious motherhood—this giving of her knowledge and skill in service to the woman with a baby in her arms.
The opportunities for self-expression which are open to the nurse who gives this form of service make us wonder if she should not be included in the enviable group of those others 14whose life work is an expression of themselves—the poets and painters; the architects, musicians, and sculptors—those who create and build because of an urge within them. Surely, the spirit and the results of the work of the nurse who thus gives of herself may be ranged with the efforts of those others whose work is an expression of themselves.
16“The body is the crowning marvel in the world of miracles in which we live. Fearfully and wonderfully made, it claims our respect not only because God fashioned it, but because He fashioned it so well—because it is a thing of beauty, a perfection of mechanism.”
CHAPTER I. ANATOMY OF THE FEMALE PELVIS AND GENERATIVE ORGANS. Normal Female Pelvis. Pelvimetry. Female Organs of Reproduction. Internal Genitalia. Uterus. Fallopian Tubes. Ovaries. Vagina. Bladder. Rectum. External Genitalia. Mons Veneris. Labia Majora. Labia Minora. Vestibule. Vaginal Opening. Fossa Navicularis. Bartholin Glands. Perineum. Breasts.
CHAPTER II. PHYSIOLOGY. Puberty. Ovulation. Menstruation. Modifications of Menstruation. Menopause.
The present broad knowledge of the anatomy of the female pelvis has resulted in an enormous reduction in death and injury among obstetrical patients and their babies.
This knowledge of the pelvic anatomy, relating as it does, to both normal and malformed pelves, has made possible a system of taking measurements, termed pelvimetry, which gives the obstetrician a fair idea of the size and shape of his patient’s pelvis. Such information, coupled with observations upon the size of the child’s head, gives a foundation upon which to base some expectation of the ease or difficulty with which the approaching delivery is likely to be accomplished.
Since each patient’s pelvic measurements are considered from the standpoint of their comparison with normal dimensions, it is manifestly important that the obstetrical nurse have a clear idea of the structure of the normal female pelvis, and also of its commonest variations.
Viewed in its entirety, the pelvis is an irregularly constructed, two-storied, bony cavity, or canal, situated below and supporting the movable parts of the spinal column, and resting upon the femora or thigh bones. (Fig. 1, A. and B.).
Four bones enter into the construction of the pelvis: the two hip bones or ossa innominata, on the sides and in front with the sacrum and coccyx behind.
The innominate bones (ossa innominata), symmetrically placed on each side, are broad, flaring and scoop-shaped. Each bone consists of three main parts, which are separate bones in early life, but firmly welded together in adults: the ilium, ischium and pubis. The ilia are the broad, thin, plate-like sections above, 20their upper, anterior prominences, which may be felt as the hips, are the anterior superior spinous processes used in making pelvic measurements. The margins extending backward from these points are termed the iliac crests.
The ischii are below and it is upon their projections, known as the tuberosities, that the body rests when in the sitting position, and which also serve as landmarks in pelvimetry. The pubes form the front of the pelvic wall, the anterior rami uniting in the median line by means of heavy cartilage and forming the symphysis pubis.
The sacrum and coccyx behind are really the termination of the spinal column, the sacrum consisting, usually, of five rudimentary vertebrae which have fused into one bone. It sometimes consists of four bones, sometimes six, but more often of five. The sacrum completes the pelvic girdle behind by uniting on each side with the ossa innominata by means of strong cartilages, thus forming the sacro-iliac joints. The spinal column rests upon the upper surface of the sacrum. The coccyx, a little wedge-shaped, tail-like appendage, which ordinarily has but slight obstetrical importance, extends in a downward curve from the lower margin of the sacrum, to which it has a cartilaginous attachment, the sacro-coccygeal joint. This joint between the sacrum and coccyx is much more movable in the female than in the male pelvis.
We find, therefore, that although the pelvis constitutes a rigid, bony, ringlike structure, there are four joints: the symphysis pubis, the sacro-coccygeal, and the two sacro-iliac articulations. As the cartilages in these joints become somewhat softened and thickened during pregnancy, because of the increased blood supply, they all permit of a certain, though limited amount of motion at the time of labor. This provision is of considerable obstetrical importance, since the sacro-coccygeal joint allows the child’s head to push back the forward-protruding coccyx, as it passes down the birth canal, thus removing what otherwise might be a serious obstruction. And when, as is sometimes necessary, because of a constricted inlet, the pubic bone is cut through (the operation known as pubiotomy), the hingelike motion of the sacro-iliac joint permits of an appreciable spreading of the two hip bones and a consequent widening of the birth canal.
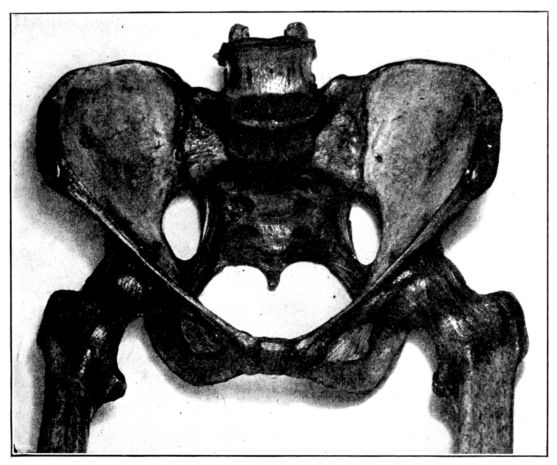
A. Normal female Pelvis.
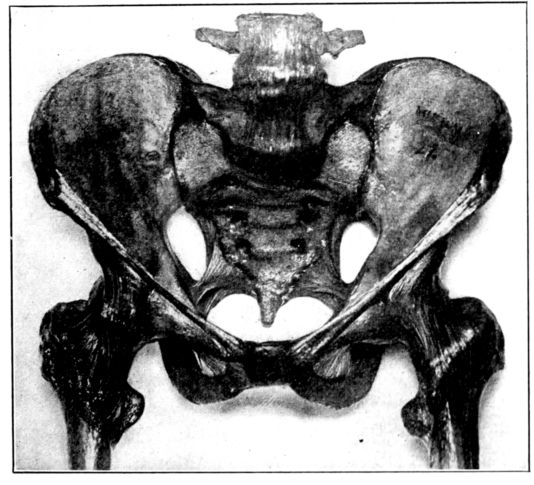
B. Normal male Pelvis.
Fig. 1.—Normal Pelves. Note the broad, shallow, light construction of the female pelvis, A, as compared with the more massive male pelvis, B.
22The pelvic cavity as a whole is divided into the true and false pelves by a constriction of the entire structure known as the brim or inlet. The inlet is not round, its antero-posterior diameter being shortened by the sacro-vertebral joint which protrudes forward and gives the opening something of a blunt, heart-shaped outline. (Fig. 2.)
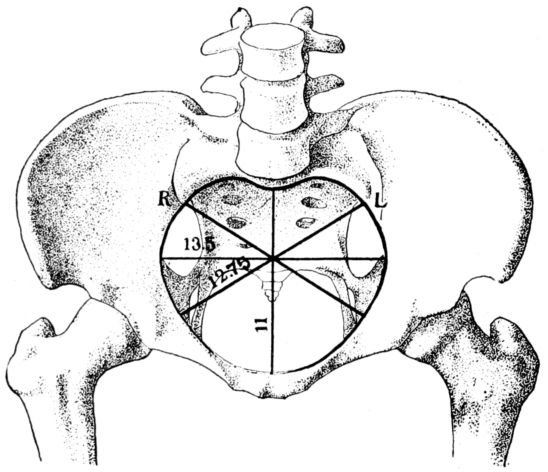
Fig. 2.—Diagram of the pelvic inlet, seen from above, with most important diameters.
As the pelvis occupies an oblique position in the body, the plane of this brim is not horizontal, but slopes up and back from the symphysis-pubis to the promontory of the sacrum. Being swung upon the heads of the femora, the relation of the pelvis to the entire body differs in the sitting and standing positions. When a woman stands upright, her pelvis is so markedly oblique in its position that she would tip backward but for strong tendons attached to the pelvis and running down the front of the thighs. Added strain upon these tendons during pregnancy may account for some of the apparently undue fatigue experienced by the expectant mother.
The shallow, expanded portion of the pelvis above the brim 23is the large, or false pelvis, its walls being formed by the sacrum behind, the fan-like flares of the ilia on each side, with the incompleteness of the bony wall in front made up by abdominal muscles.
The false pelvis ordinarily serves simply as a support for the abdominal viscera, which do not occupy the true pelvis unless forced down by some such pressure as that caused by tight, or poorly fitting corsets. The false pelvis is of little obstetrical importance, its function during pregnancy being to support the enlarged uterus, while at the time of labor it acts as a funnel to direct the child’s body into the true pelvis below.
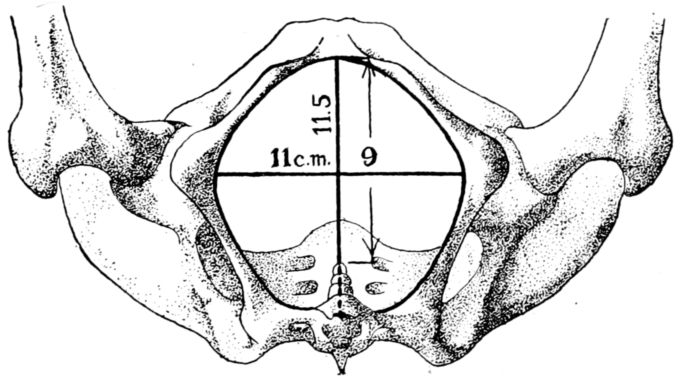
Fig. 3.—Diagram of pelvic outlet, seen from below, with most important diameters.
The true pelvis, on the other hand, is of greatest possible obstetrical importance since the child must pass through its narrow passage during birth. It lies below and somewhat behind the inlet; is an irregularly shaped, bottomless basin, and contains the generative organs, rectum and bladder. Its bony walls are more complete than those of the false pelvis, and are formed by the sacrum, coccyx and innominate bones. Its lower margin constitutes the outlet, or inferior strait, and being longer in its antero-posterior dimension than in its transverse measurement, its long axis is at right angles to the long axis of the inlet. (Fig. 3.) A baby’s head, accordingly, must twist or rotate in making its descent through this bony canal, for the long diameter of the head must first conform to one of the long diameters of the inlet, either transverse or oblique, and then turn so that the length 24of the head is lying antero-posteriorly, in conformity to the long diameter of the outlet, through which it next passes.
The posterior wall of the pelvis, consisting of the sacrum and coccyx, forms a vertical curve and is about three times as deep as the anterior wall formed by the narrow symphysis pubis. The structure as a whole, therefore, curves upon itself, resembling a bent tube with its concavity directed forward. (Fig. 4.)
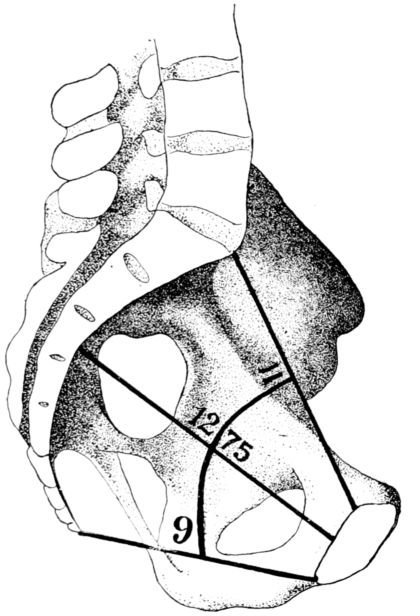
Fig. 4.—Diagram of sagittal section of the pelvis showing curve of the bony canal, with most important diameters.
Thus it becomes apparent that the structure of the pelvis requires the child’s head, not only to rotate in its passage through the birth canal, but also to describe an arc, since the part of the head which passes down the posterior wall travels farther in a given time than the part which passes under the pubis.
This twisting and curving of the birth canal must be appreciated in order to understand the mechanism of labor.
25In considering the question of pelvimetry, we find that there are both external and internal measurements to be taken, all for the purpose of estimating as accurately as possible the shortest diameter of the inlet through which the baby must pass. (Fig. 5.)
According to a common system of mensuration, the first external measurement is the inter-spinous, the distance between the anterior-superior spines, those bony points which are uppermost as the patient lies on her back. This distance is normally 26 centimetres. (Fig. 6.)
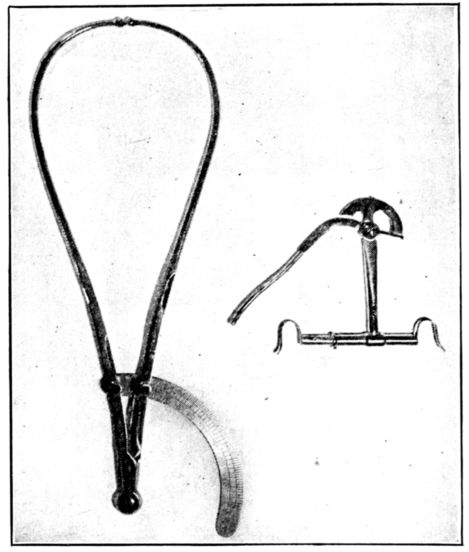
Fig. 5.—Two types of pelvimeters frequently used in taking measurements of the pelvic inlet and outlet.
The second measurement is the inter-crestal, or the distance between the iliac crests, and is normally 28 centimetres.
Baudelocque’s diameter is the third measurement and is taken with the patient lying on her side. (Fig. 7.) It is the distance from the top of the symphysis to a depression just below the last lumbar vertebra. This depression is easily located as it also marks the upper angle of a space just above the buttocks, which in normal pelves is quadrilateral. In malformed pelves this quadrangle may be so misshapen as to become almost a triangle with the apex directed either up or down. This dimension 26is sometimes called the external conjugate and ordinarily measures 21 centimetres.
The fourth measurement is the distance between the great trochanters, or heads of the femora, and normally is 32 centimetres.
All of these measurements, which after all are only approximate, relate to the top of the pelvis and are valuable in that they help in estimating the dimensions of the inlet, which are the important ones, and obviously cannot be measured on a live woman.
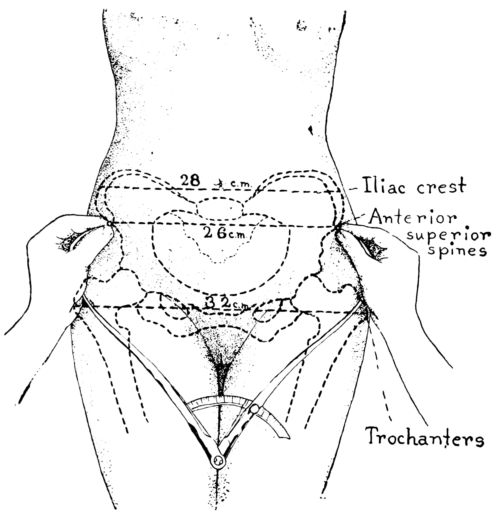
Fig. 6.—Diagram showing method of measuring distances between iliac crests and spines and the trochanters.
The inlet has four measurements of obstetrical importance: the antero-posterior, or true conjugate, which is the distance from the top of the symphysis pubis to the prominence of the sacrum, and is normally 11 centimetres; the transverse diameter, which is at right angles to the true conjugate and is the greatest width of the inlet, measuring from a point on one side of the brim to the corresponding point on the other, is normally 13.5 centimetres, and the two diagonal measurements, known respectively 27as the right and left oblique diameters, which are normally 12.75 centimetres.
Although it is very important to the expectant mother that all of these dimensions be of normal length, the length of the true conjugate, or conjugata vera, is of the gravest importance of all because it is the shortest diameter through which the child’s head must pass. If it is shorter than normal, the channel may be too constricted for the full-term baby’s head to pass through comfortably, thus making a spontaneous delivery extremely difficult, or even impossible.
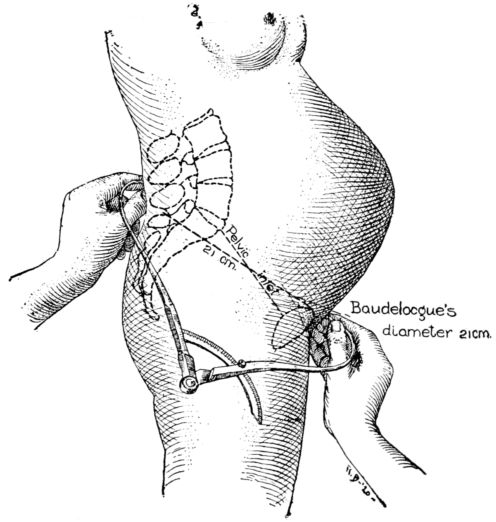
Fig. 7.—Diagram showing method of measuring Baudelocque’s diameter.
The length of the all important, true conjugate is estimated by introducing the first two fingers of one hand into the vagina until the tip of the second finger touches the promontory of the sacrum. (Fig. 8.) The point at which the inner margin of the symphysis then rests upon the forefinger is measured, thus giving the length of the diagonal conjugate. This normally measures 12.5 centimetres or more, and is estimated as being 1.5 centimetres longer than the true conjugate.
28The most important measurement of the outlet is the intertuberous diameter, the distance between the tuberosities of the ischii. This is the shortest diameter through which the child must pass in the inferior strait, and normally measures something more than 8 centimetres, usually about 11 centimetres. (Fig. 9.)
It is possible, by studying such measurements as these, made upon an expectant mother, and comparing them with dimensions which have been accepted as normal, to form a reasonably accurate estimate of the size and shape of her pelvis.
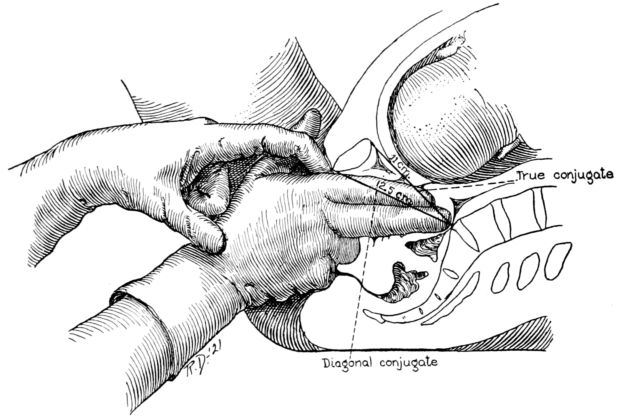
Fig. 8.—Diagram showing method of estimating the true conjugate by measuring the length of the diagonal conjugate.
A delivery may be, and frequently is, accomplished through a pelvis which is not entirely normal in size or shape. But the obstetrician of to-day is closely observant of the patient whose pelvic measurements depart from the normal by more than the accepted margin of safety, and he plans for labor in accordance with the indications in each case.
Disproportion between the measurements of the mother’s pelvis and the size of the child’s head must be considered in this connection. A small pelvis may permit of the spontaneous delivery of a small child, but be too narrow for the passage of a 29full-sized baby, while a woman with a normal pelvis may have an extremely difficult labor because of an unusually large child.
The size and shape of the pelvis is found to vary among different races and in different individuals. And the size and contour of the inlet may be so altered by rickets, lack of proper exercise during early life, or by growths upon the pelvic bones, as to seriously interfere with normal labor.
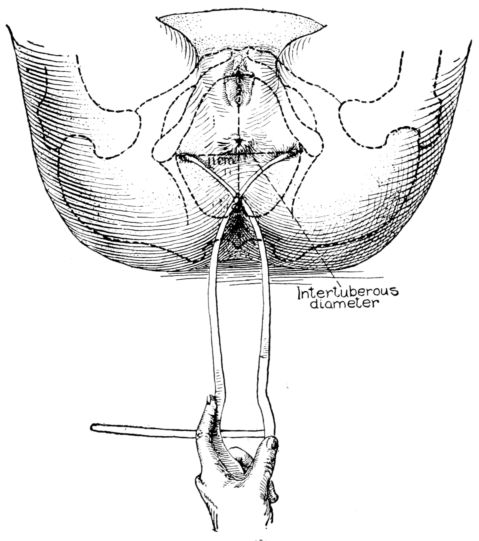
Fig. 9.—Diagram showing method of measuring the inter-tuberous diameter.
The various kinds of malformed pelves may be loosely classified as generally contracted or small; flat; simple funnel; generally contracted funnel; and the rachitic pelves, both flat and generally contracted. There may be a contracted inlet, or a contracted outlet, or both may occur in the same pelvis.[1]
30Rachitic pelves are common among negroes and not altogether rare among white women.
The normal male pelvis is deep, narrow, rough and massive as compared with the female structure (see Fig. 1.), and the angle of the pubic arch, formed by the two pubic bones, is deeper and more acute in the male than in the female skeleton.
The normal female pelvis, on the other hand, is light, broad, shallow, smooth and large, giving evidence of the infinite wisdom and skill that entered into constructing it for the high purpose it was designed to serve.
The female organs of reproduction are divided into two groups, the internal and the external genitals. With them are usually considered certain other structures: the ureters, bladder, urethra, rectum and the perineum, because of their close proximity (Fig. 10.); and the breasts, because of their functional relation to the reproductive organs.
Internal Genitalia. The internal organs of generation are contained in the true pelvic cavity and comprise the uterus and vagina in the centre, an ovary and Fallopian tube on each side, together with their various ligaments, membranes, nerves and blood vessels and a certain amount of fat and connective tissue.
The uterus is the largest of these organs. In its nonpregnant 31state, it is a hollow, flattened, pear-shaped organ about three inches long, one and a quarter inches wide, at its broadest point, three-quarters of an inch thick and weighing about two ounces.
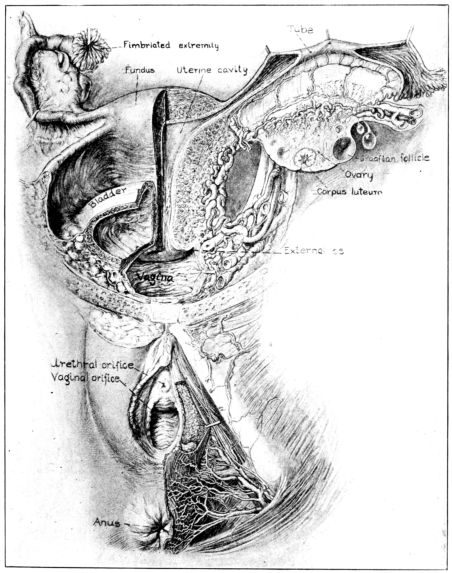
Fig. 10.—Anterior view of female generative tract, showing both external and internal organs. Drawn by Max Brodel. (Used by permission of A. J. Nystrom & Co., Chicago.)
Ordinarily it is a firm, hard mass, consisting of irregularly disposed, involuntary (unstriped or plain) muscle fibres and connective tissue, nerves and blood vessels. The arrangement 32of the uterine muscle fibres is unique, for they run up and down, around and crisscross, forming a veritable network. This strange arrangement of the fibres is favorable to the growth of the uterine musculature during pregnancy, and a factor in preventing hemorrhage after delivery.
The abundant blood supply to the uterus merits a word. It is derived from the uterine arteries, arising from the internal iliacs, and the ovarian artery from the aorta. The arteries from the two sides of the uterus are united by a branch where the neck and body of this organ meet, thus forming an encircling artery. A deep cervical tear during labor may break this vessel and a profuse hemorrhage occur as a result.
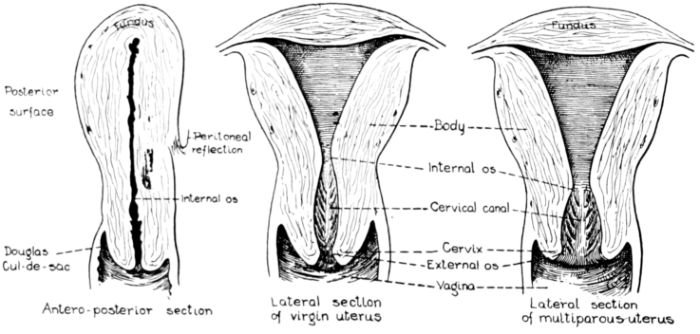
Fig. 11.—Diagrams of sections of virgin and multiparous uteri.
The uterus is covered, front and back, by a fold of the peritoneum, except the lower part of the anterior wall where the peritoneum is reflected up over the bladder. It is lined with a thick, velvety, highly vascular mucous membrane, the endometrium, the surface of which is covered by ciliated, columnar epithelium. Embedded in the endometrium are numerous mucous glands which dip down into the underlying, muscular wall.
The uterus as a whole is comprised of three parts: the fundus, that firm, rounded, head-like part above; the body, or middle portion, and the cervix, or neck, below. It is in the body and cervix that we find the long, narrow uterine cavity, divided by a constriction into two parts. The cavity of the body is little more than a vertical slit, being so flattened from before backward 33that the anterior and posterior surfaces are nearly if not quite in apposition. It is somewhat triangular in shape with an opening at each angle. (Fig. 11.) The lower of these openings leads into the cavity of the cervix through a constriction termed the internal os, while at the cornua, or two upper angles, are the openings into the Fallopian tubes.
The cavity of the cervix is spindle-shaped, being expanded between its two constricted openings, the internal os above and the external os below, which opens into the vagina. The external os in the virgin is a small round hole but has a ragged outline in women who have borne children.
This oblong, muscular body, the uterus, is suspended obliquely in the centre of the pelvic cavity by means of ligaments. In its normal position the entire organ is slightly curved forward, or ante-flexed, the fundus being directed upward and forward and the cervix pointing down and back. This position is affected by a distended bladder or rectum, and also by postural changes in the body as a whole. The cervix protrudes into the anterior wall of the vagina for about one-half inch and almost at right angles, since the vagina slopes down and forward to the outlet.
The upper part of the uterus is held in position by means of ligaments, the lower part being embedded in fat and connective tissue between the bladder and rectum. This more or less of a floating position makes possible the enormous increase in size and upward push or extension of the uterus during pregnancy. The pregnant uterus becomes soft and elastic as it grows. At term it is about a foot long, eight to ten inches wide, and reaches up into the epigastric region. This growth is due in part to the development of new muscle fibres and in part to a growth of the fibres already existing in the uterine wall.
After labor the uterus returns almost, but never entirely, to its former size, shape and general condition.
The Fallopian tubes are two tortuous, muscular tubes, four or five inches long, extending laterally in an upward curve, from the cornua of the uterus and within the folds of the upper margin of the broad ligament, by which they are covered. At their juncture with the uterus, the diameter of these tubes is so small as to admit of the introduction of only a fine bristle, but they 34gradually increase in size toward their termination in wide trumpet-shaped orifices, which open directly into the peritoneal cavity. Finger-like projections called fimbriæ, fringe the margins of these openings.
The mucous lining of the tubes is covered with ciliated epithelium and is continuous with that of the uterus. At the fimbriated extremities of the tubes this lining merges into the peritoneum, the serous lining of the abdominal cavity.
Just here it will be well to say a word about the peritoneum because of the possibility of its becoming infected during labor and the lying-in period, and the very grave consequences of such infection. It is a delicate, highly vascular, serous membrane which both lines the abdominal cavity and covers the abdominal and pelvic organs, which press into its outer surface and are covered much as one’s fingers would be covered by pushing them into the outer surface of a child’s toy balloon. The continuity of this membrane is broken only where it is entered by the Fallopian tubes.
The ovary, the sex gland of the female, is a small, tough ductless gland, about an inch long and three-quarters of an inch wide, or about the size and shape of an almond. It is greyish pink in color and presents a more or less irregular, dimpled surface. An ovary is suspended on either side of the uterus, in the posterior fold of the broad ligament, by which it is partly covered. Its outer end is usually attached to the longest of the fimbriated extremities of the Fallopian tube, the fimbria ovarica, which has the form of a shallow gutter, or groove. The inner end of the ovary is attached to the ovarian ligament, which in turn is attached to the uterus below and behind the tubal entrance.
The ovary consists of two parts, the central part or medulla, composed of connective tissue, nerves, blood and lymph vessels, and the cortex, in which are embedded the vesicular Graafian follicles containing the ova. At birth each ovary contains upwards of 50,000 of these ova, which are the germ cells concerned with reproduction and the process of menstruation.
These ovarian glands perform two vital functions, for in addition to their prime function of producing and maturing the germinal cell of the female, they provide an internal secretion 35which exercises an immeasurably important, though imperfectly understood, influence upon the general well-being of the entire organism.
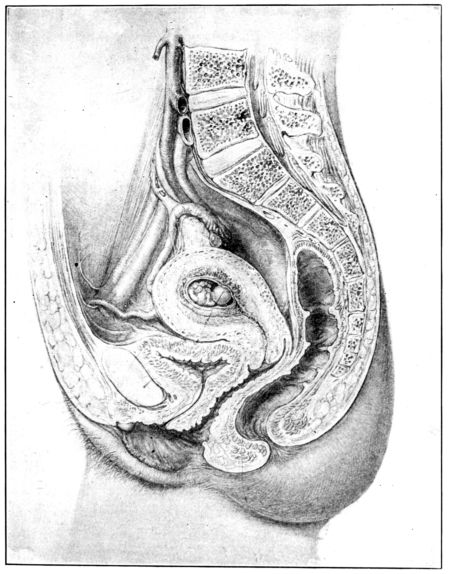
Fig. 12.—Sagittal section of female generative tract. Drawn by Max Brodel. (Used by permission of A. J. Nystrom & Co., Chicago.)
The vagina is an elastic, muscular sheath or tube, about four inches long, lying behind the bladder and urethra and in front of the rectum. It leads interiorly up and backward from the vulva to the cervix, which it encases for about half an inch. The space between the outer surface of the cervix that extends into the vagina, and the surrounding vaginal walls, is called the fornix. 36For convenience of description, this is divided into four sections or fornices: the anterior, posterior and lateral fornices.
Between the posterior fornix and the rectum a fold of the peritoneum drops down and forms a blind pouch known as Douglas’ cul-de-sac. At this point the delicate peritoneum is separated from the vagina by only a thin, easily punctured, muscular wall. This is a fact of grave surgical significance, for unless instruments and nozzles introduced into the vagina are very gently and skillfully directed, they may easily pierce this thin partition. Septic material may thus gain entrance to the peritoneal cavity and peritonitis result.
The bore of the vaginal canal ordinarily permits of the introduction of one or two fingers. It is somewhat flattened from before backward, and on cross section resembles the letter H. During labor this canal becomes enormously dilated, being then four or five inches in diameter, and permits the passage of the full term child.
The vagina is lined with a thick, heavy, mucous membrane which normally lies in transverse folds or corrugations called rugæ. These folds are obliterated and the lining stretched into a smooth surface as the canal dilates during labor.
Attention must be drawn to the fact that the vagina, cervix, uterus and tubes form a continuous canal from the vulva to the easily infected peritoneum, a fact which makes absolute surgical cleanliness in obstetrics virtually a matter of life or death to the patient.
This muscular tube is lined throughout its entire length with mucous membrane, which, though continuous, changes somewhat in character along its course. The epithelial cells of the lining of the tubes and body of the uterus have hair-like projections, cilia, which maintain a constant waving motion from above downward. The effect of this sweeping current is to carry down toward the outlet any object or secretion which may be upon the surface of the lining of the tubes or uterine cavity. The unfertilized ovum is thus swept down to meet the germ cell of the male and become fertilized.
Along this variously constructed canal, at different periods in the life of the individual, pass the matured ovum, the menstrual 37flow, the uterine secretions, the fetus, the placenta and lochia, (the discharge which occurs during the puerperium).
Although the bladder and rectum are not organs of reproduction, they are contained in the pelvic cavity and lie in such close proximity to the internal genitalia that at least a passing word must be devoted to their description.
The bladder is a sac of connective tissue which serves as a reservoir for the urine and is situated behind the symphysis pubis and in front of the uterus and vagina. Urine is conducted into the bladder by the ureters, two slender tubes running down on each side from the basin of the kidney across the pelvic brim to the upper part of the bladder, which they enter somewhat obliquely, at about the level of the cervix. It is thought that pressure of the enlarged pregnant uterus upon the ureters at this point may be one factor in the causation of pyelitis, a frequent complication of pregnancy. The bladder empties itself through the urethra, a short tube which terminates in the meatus urinarius, a tiny opening in the vulva.
The rectum, the lowest segment of the intestinal tract, is situated in the pelvic cavity behind and to the left of the uterus and vagina. It extends downward from the sigmoid flexure of the colon to its termination in the anal opening. The anus is a deeply pigmented, puckered opening situated an inch and a half or two inches behind the vagina. It is guarded by two bands of strong circular muscles, the internal and external sphincter ani. The skin covering the surface of the body extends upward into the anus where it becomes highly vascular and merges into the mucous lining of the rectum. Pressure exerted during pregnancy by the enlarged uterus is felt in both the rectum and bladder, frequently causing a good deal of discomfort and almost painful desire to evacuate their contents.
The blood vessels in the anal lining just within the external sphincter sometimes become engorged and inflamed, even bleeding during pregnancy, as a result of the pressure exerted by the greatly enlarged uterus. The distended blood vessels, which in this condition are called hemorrhoids, not infrequently protrude from the anus and become very painful.
38After having considered the structure and relative positions of the pelvic organs one is able to picture more clearly the arrangement and disposition of the uterine ligaments, all of which are formed by folds of the peritoneum. They are twelve in number, five pairs and two single ligaments, namely: two broad, two round, two utero-sacral, two utero-vesical, two ovarian, one anterior and one posterior ligament.
The broad ligaments are in reality one continuous structure formed by a fold of the peritoneum, which drops down over the uterus, investing the fundus, body, part of the cervix, and part of the posterior wall of the vagina. It unites on each side of the uterus to form a broad, flat membrane which extends laterally to the pelvic wall, dividing the pelvic basin into an anterior and posterior compartment, containing respectively the bladder and rectum. Between the folds of the broad ligament are situated the ovaries and ovarian ligaments, the Fallopian tubes, the round ligaments and a certain amount of muscle and connective tissue, blood vessels, lymphatics and nerves.
The round ligaments, one on each side, are narrow, flat bands of connective tissue derived from the peritoneum and muscle prolonged from the uterus, and containing blood and lymph vessels and nerves. They pass upward and forward from their uterine origin just below and in front of the tubal entrance, finally merging in the mons veneris and labia majora.
The utero-sacral ligaments, of which there is one on each side, arise in the uterus and, extending backward, serve to connect the cervix and vagina with the sacrum.
The utero-vesical ligaments, one on each side, extend forward and connect the uterus and bladder.
The ovarian ligaments, as previously described, are attached to the uterine wall and to the inner end of the ovary, one on each side.
The anterior ligament is a portion of the peritoneum which dips down between the bladder and uterus, forming a pouch. It is known also as the uterine-vesical pouch, or the vesico-uterine excavation.
The posterior ligament is formed in much the same manner by a portion of the peritoneum dipping down behind the uterus, 39in front of the rectum, and forming the recto-vaginal pouch. This is the Douglas’ cul-de-sac previously referred to.
External Genitalia.—The vulva, or external genitalia, are situated in the pudendal crease which lies between the thighs at their junction with the torso, and extends posteriorly from the pubis to a point well up on the sacrum. (Fig. 13.)
The mons veneris is a firm cushion of fat and connective tissue, just over the symphysis pubis. It is covered with skin which contains many sebaceous glands and after puberty is abundantly covered with hair.
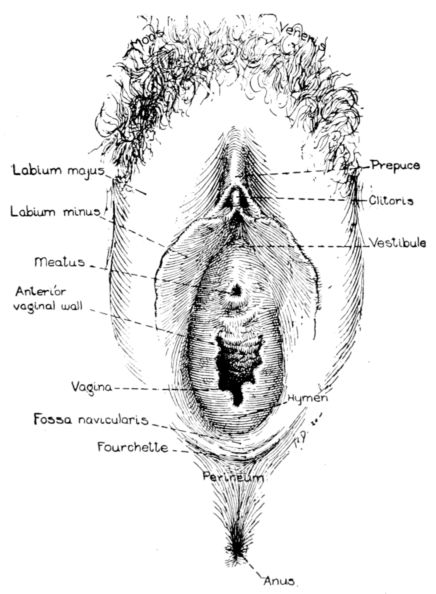
Fig. 13.—Diagram of external female genitalia. (Redrawn from Dickinson.)
The labia majora are heavy ridges of fat and connective tissue, prolonged from the mons veneris and extended down and back almost to the rectum, on each side, forming the lateral boundaries of the groove. They are lined with mucous membrane and covered with skin and hair, the latter growing thinner toward the perineum until it finally disappears.
The labia minora are two small cutaneous folds lying between the labia majora on each side of the vagina. Like the larger 40folds, they taper toward the back and practically disappear in the vaginal wall. Their attenuated posterior ends are joined together behind the vagina by means of a thin, flat fold called the fourchette. The labia minora divide for a short distance before joining at an angle in front, thus forming a double ridge anteriorly. In the depression between these ridges is the clitoris, a small, sensitive projection composed of erectile tissue, nerves and blood vessels and covered with mucous membrane. The meatus urinarius is just below the clitoris and between two small folds of the mucous membrane.
The vestibule is the triangular space between the labia minora, and into it open the meatus urinarius, the vagina and the more important vulvo-vaginal glands.
The vaginal opening is below the vestibule and above the perineum. It is partially closed by the hymen, a fold of mucous membrane disposed irregularly around the outlet, somewhat after the fashion of a circular curtain. The hymen is ragged or more or less scalloped in outline, and varies greatly in size in different women, in some instances extending so far over the opening as nearly or quite to close it.
The fossa navicularis is a depressed space between the hymen and fourchette, so named because of its boat-like shape.
The Bartholin glands, probably the largest and most important of the vulvo-vaginal glands, are situated one on each side of the vagina and open into the groove between the hymen and labia minora. Reference is made to these glands because of the danger of their becoming infected. A gonorrheal infection of these glands is particularly troublesome.
The perineum is a pyramidal structure of connective tissue and muscle which occupies the space between the rectum and vagina, and by forming the floor of the pelvis serves as a support for the pelvic organs. The lower and outer surface of this mass, representing the base of the pyramid, lies between the vaginal opening and the anus and is covered with skin. As the anterior part of the perineum is incorporated in the posterior wall of the vagina, the entire structure becomes stretched and flattened when the vagina is dilated during labor by the passage of the child’s head.
41Unless very carefully guarded at the time of delivery, and often even then, the perineum gives way under the great tension undergone at that time, and a tear is the result. The injury may be only a slight nick in the mucous membrane or it may extend to, or into the levator ani, the most important muscle of the perineal body, or if a “complete tear” will extend all the way through the perineum and completely through the sphincter ani. Such a tear is lamentable, as a break in the ring-shaped sphincter muscle guarding the anal opening robs a woman of control of her bowels, and is repaired with difficulty.
The breasts are large, specially modified skin glands of the compound, racemose or clustering type, embedded in fat and connective tissue and abundantly supplied with nerves and blood vessels. They are situated quite remotely from the pelvic organs, but because of the intimate functional relation between the two, the breasts of the female may be regarded as accessory glands of the generative system. They exist in the male, also, but only in a rudimentary state.
Although the breasts sometimes contain milk during infancy, their true function is to secrete, in the parturient woman, suitable nourishment for the human infant during the first few months of its life.
These glands are symmetrically placed, one on each side of the chest, and occupy the space between the second and sixth ribs extending from the margin of the sternum almost to the mid-axillary line. A bed of connective tissue separates them from the underlying muscles and the ribs. (Fig. 14.)
They vary in size and shape at different ages, and with different individuals, particularly in women who have borne and nursed children, when they tend to become pendulous. But in general they are hemispherical or conical in shape with the nipple protruding from one-quarter to one-half inch from the apex. The nipples are largely composed of sensitive, erectile tissue and become more rigid and prominent during pregnancy and at the menstrual periods. Their surfaces are pierced by the orifices of the milk ducts, which are fifteen or twenty in number. (Fig. 15.)
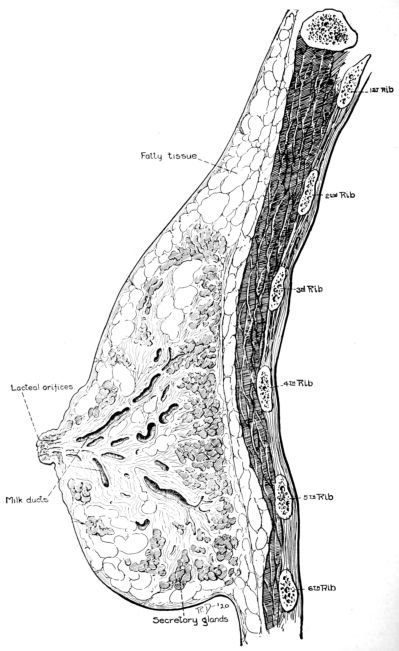
Fig. 14.—Sagittal section of breast showing structure of secretory apparatus.
43The breasts are covered with very delicate, smooth, white skin, excepting for the areolæ, those circular, pigmented areas one to four inches in diameter, which surround the nipples. The areolæ are darker in brunettes than in blonds, and in all women grow darker during pregnancy. The surface of the nipples and of the areolæ is roughened by small, shot-like lumps or papillæ known as the tubercles of Montgomery. This roughness becomes more marked during pregnancy, since the papillæ grow larger and sometimes even contain milk.
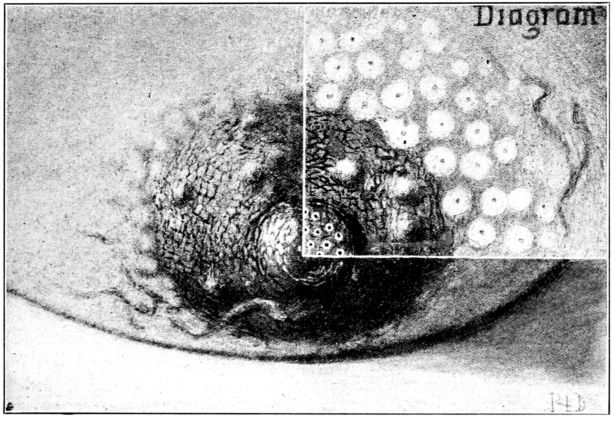
Fig. 15.—Front view of breast showing areola, tubercles of Montgomery and orifices of milk ducts.
The secretory apparatus of the breasts is divided into fifteen or twenty lobes, these in turn being divided into clusters of lobules. The lobules in turn are composed of tiny, secreting cells, called acini, in which the milk is elaborated from the blood. The acini are minute globules lined by a single layer of cells and enveloped by a very delicate membrane. Tiny ducts carry the milk from the acini to the main duct of the lobule, around which the acini cluster. These ducts empty the milk into the larger duct of the lobe, which runs straight to the nipple and opens upon the surface. Just before reaching the surface, each of these lactiferous sinuses expands into an ampulla, a minute reservoir 44for collecting the milk, which is secreted during the periods between nursings.
These clusters of acini uniting to form lobules with tiny ducts leading into the main duct of each lobule, closely resemble a bunch of grapes. The separate grapes correspond to the acini, their small stems correspond to the tiny ducts of the glands which lead to a larger one, and the central stem of the grape cluster, to the milk duct that opens upon the nipple.
The secretory tissue really constitutes a small part of the breasts until they begin to function. But during lactation the acini become enormously developed and enlarged. After lactation ceases, the acini assume a more or less tubal form, many of them undergoing atrophic changes.
Puberty is that period during which childhood develops into sexual maturity, and the individual becomes capable of reproduction.
The age at which puberty occurs varies with climate, race, occupation and with individuals of the same status. But the average age for girls, in temperate climates, is from the twelfth to the sixteenth year; for boys from the fourteenth to the seventeenth year. Girls in southern climates sometimes mature as early as the eighth or ninth year, while in colder regions puberty may be delayed until the eighteenth or twentieth year.
At this time there are many physical and psychical manifestations of the maturing changes in the internal female generative organs. The undeveloped girl grows rapidly at this stage. Her entire body rounds out and assumes a more graceful contour; her breasts increase in size; her hips broaden; the external genitalia enlarge and hair appears over the pubis and on other parts of the body.
As this physical maturity progresses, there is a dawning sex consciousness and the developing girl becomes shy, modest, retiring and introspective. She is very likely to be emotional and hysterical and to display a lack of stability and nervous control, which are not in accord with her usual temperament. A formerly dependable child may become capricious, erratic, and perplexingly inconsistent. One day she may be quite her normal, little-girl self and the next show inexplicably mature qualities. Or she may display a bewildering number of moods and fancies in the span of one short day.
Too much cannot be said of the importance of wise supervision and guidance of the girl’s physical, mental and emotional life at this critical, emotional period. Many gynecological, obstetrical 46and neurological difficulties in her later life may be averted by her observance of sane rules of personal hygiene.
Vigorous and regular out-of-door exercise; a simple, nourishing and well-balanced diet; adequate sleep in a well-ventilated room; regular bathing, and correction of any discoverable physical defects are the essentials.
But of equal, if not greater, importance is an understanding and sympathetic oversight of the girl’s mental and emotional life, a steadying sort of comradeship.
Her extreme sensitiveness and impressionability should be recognized and borne in mind, and every effort made to save her from strain and shock. Her nervous forces should be sedulously conserved by protecting her against experiences and diversions which would be unduly stimulating or irritating. Nor should demands be made upon her uncertain nervous endurance which she is able to meet only by great strain, if at all.
It is important to her future poise and health that her confidence be courted, and when it is won, that all of her outpourings be received with a respect and seriousness commensurate with their great importance to her. Ridicule, and even unresponsiveness or indifference to her interests, may, and often do, result in a hurtful repression of one form or another. The logical consequence of such repression is an increasingly damaging neurosis later on in her life, capable of greatly impairing her health, happiness and usefulness.
In short, all phases of the life of the adolescent girl should be made as wholesome, tranquil and free from stress and strain as is humanly possible.
These comments upon the importance of mental hygiene at puberty may seem irrelevant to a discussion of obstetrical nursing. But the preparation of the entire female organism for its supreme function—that of child-bearing—is of concern to the obstetrical nurse, and should be understood by her. Moreover, every nurse is inevitably a health teacher, either by precept or example, or both. An awareness on her part of the maturing girl’s needs will fit her to help many perplexed mothers whom she meets along the way to a happy solution of this grave and vexing problem.
47The occurrence of puberty marks the establishment of ovulation and menstruation. These two functions are usually performed once a month, ovulation probably occurring about midway during the intermenstrual period.
Ovulation, which is the prime function of the ovary, may be defined as the formation and development of the ovum, and its expulsion, when mature, from the ovary.
The formation of each woman’s full quota of ova is probably complete at birth, though the process may continue until about the second year. At this time it is variously estimated that each of the two ovaries contains from 50,000 to 70,000 ova, but they remain unmatured until puberty, the period at which ovulation is most active.
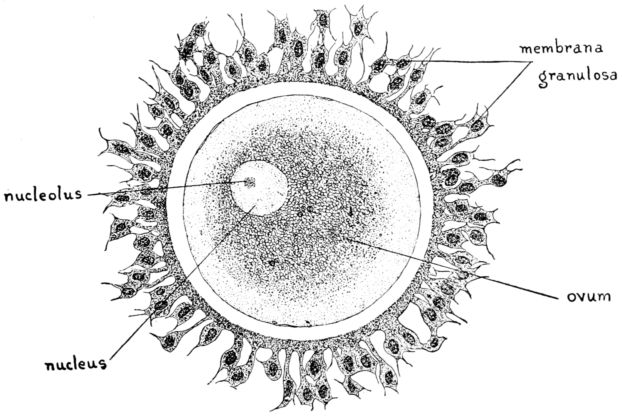
Fig. 16.—Diagram of human ovum.
As the entire complex human body has its origin in this tiny ovum, its course of development is of momentous importance to us, and at the same time it provides a tale of intense interest.
In its unmatured state, the ovum, termed a primordial follicle,
or oöcyte, is a single cell, 1
125 inch in diameter, consisting
of clear protoplasm, the vitellus, and a surrounding vitelline
membrane composed of small, spindle-shaped epithelial cells.
The protoplasm contains a fairly large nucleus, or germinal vesicle,
48within which lies a nucleolus known as the germinal spot.
(Fig. 16.)
The primordial follicle probably lies dormant in this state until puberty, when developmental changes take place, though it is the belief of some authorities that follicles are in the process of development from birth until the end of sexual life, though none fully mature until puberty.
With the advent of puberty the cells composing the vitelline membrane change in character and proliferate rapidly, with the result that the ovum is surrounded by several layers of epithelial cells. Some of the inner cells degenerate and liquify, thus surrounding the ovum with fluid which is contained in a membrane of vascular connective tissue, the theca folliculi; this in turn is lined with epithelial cells, the membrana granulosa. This structure constitutes a Graafian follicle, named for Dr. de Graaf who first described it, and in the course of its maturation is pushed toward the surface of the ovary, where it presents more or less the appearance of a clear blister.
At one point in the enveloping membrana granulosa, the cells proliferate into a mass in which the floating ovum becomes embedded. This mass is termed the discus proligerus and the fluid which surrounds it is the liquor folliculi.
Usually for some strange reason, one, and only one, ovum ripens regularly each month during the years from puberty to the menopause, excepting during pregnancy, when this function is suspended. Occasionally, however, several ova mature at once, a condition which may be one factor in the development of twins. After puberty the ovary contains ova in all stages of development, from the primordial follicle to the Graafian follicle just described.
When a Graafian follicle containing a matured ovum reaches the ovarian surface, its membrane becomes thinner and finally ruptures because of increased tension in the ovary, due to certain circulatory changes. The ovum surrounded by the discus proligerus is thus discharged into the peritoneal cavity near the fimbriated end of the tube. Some ova enter the tube and others float about in the peritoneal cavity, finally disintegrate and are lost.
49The torn envelope of the follicle which remains in the cortex of the ovary becomes filled with blood, which forms into a clot. This clot is first surrounded, and then invaded, by cells containing bright yellow pigment called lutein. The membrane formed from these cells compresses the clot and brings about other changes which speedily transform it into the corpus luteum.
If the discharged ovum becomes fertilized, the corpus luteum remains practically unchanged for months and is termed the corpus verum or corpus luteum of pregnancy. Its secretion is believed to influence the implantation of the ovum and to promote the woman’s general well-being during the period of gestation. It continues to exist throughout pregnancy, and until after delivery, when it is soon absorbed and replaced by normal ovarian tissue, without the formation of scar tissue.
If fertilization does not occur, the body in the ovarian cortex, which is then termed the corpus luteum of menstruation, or false corpus, undergoes rapid degenerative changes and is almost wholly absorbed within a few weeks.
By means of this rather complicated procedure the ovary is saved from becoming a steadily enlarging mass of scar tissue, and consequently devoid of reproductive powers, which would be the case if the wound made by the rupturing of each Graafian follicle were to heal by the usual formation of cicatricial tissue.
Ordinarily the ovum remains unfertilized and is propelled down the Fallopian tube, by the cilia in its lining, to the uterine cavity, where it is lost in the uterine secretions and ultimately carried out in the menstrual flow.
Each time that an ovum matures, however, and is discharged from the ovary the lining of the uterine cavity increases in vascularity and becomes thicker and more velvety; a condition which facilitates an attachment of the ovum in case of fertilization. This preparation of the endometrium is termed “pre-menstrual swelling,” or in popular language, nest-building.
Of the enormous number of ova existing in each woman, relatively few mature and it is apparent that still fewer are fertilized, since each impregnation results in an abortion, a premature labor or a full term child.
Nature’s lavish provision of something more than 100,000 ova 50for each woman, who uses only about 500 in the course of her life, excites no little wonder. But whatever the purpose of this enormous supply, its existence makes possible the removal of all but a small fragment of ovarian tissue in cases of disease, without interference with the process of ovulation, which in turn permits reproduction.
Menstruation, which is the evidence of sexual maturity, is a monthly hemorrhage from the uterus which escapes through the vagina, normally recurring throughout the entire child-bearing period, except during pregnancy and lactation. The duration of this child-bearing period, or sexual activity, is about thirty years and continues from puberty to the menopause.
The frequency of the menstrual periods varies in different women from twenty-one to thirty days, but the normal interval between periods is twenty-eight days, which corresponds in point of time to the menstrual cycle. Thus it is usually four weeks, or a lunar month, from the beginning of one period to the beginning of the period following, making thirteen menstrual periods during each calendar year.
Just why menstruation occurs about every twenty-eight days is not known, but the belief is that, although menstruation is in some way dependent upon ovulation, its periodicity is regulated by the corpus luteum. It is also believed that the corpus luteum of pregnancy holds menstruation in check during the nine months of gestation.
The menstrual cycle is divided into four stages, and though there is not entire unanimity of opinion concerning the changes which take place during these four stages, the preponderance of evidence is in favor of the following processes.
The first or constructive stage lasts about seven days. It is during this stage that the preparative changes, which have been described, are made for the reception of the matured ovum. The uterus becomes engorged with blood and is somewhat enlarged and softened as a result. The endometrium grows deep red, thick and velvety, partly because of the greatly augmented blood supply, and partly because of an actual increase of connective tissue in its structure. There is also an increase in the size and activity of the uterine glands and in the amount of their 51secretions. If the ovum remains unfertilized, which is usually the case, it does not attach itself to this elaborately prepared lining, but passes out with the uterine discharges, and all of this preparation and increased vascularity not only go for naught, but must be undone.
The second stage, therefore, which lasts about five days, is the destructive stage, during which the newly developed tissues are broken down and the menstrual discharge occurs. During this period the greatly increased secretions of the uterine glands mix with the blood that oozes from the engorged endometrium and with the disintegrated uterine tissues, and pour from the vagina as the menstrual flow.
The third, or reparative stage, which follows, occupies about three days. During this stage the destroyed uterine tissues are regenerated by new growth from the deeper, uninjured tissues, and the entire organ returns to its normal state.
The fourth, or quiescent stage, now follows, the damage having been repaired, and lasts twelve or fourteen days. This is the time remaining before Nature with unwearying patience begins all over again to prepare for the reception and attachment of the next matured ovum, in case of its possible fertilization.
It will be seen that the duration of the menstrual period, which is coincident with the destructive stage of the menstrual cycle, is about five days, but it is entirely within normal bounds if it varies in length from two to seven days.
The discharge is usually scant at the beginning of the period, increasing in amount until about the third day, after which it diminishes steadily until its cessation. The normal odor of this discharge, consisting as it does of blood and uterine secretions, has been likened to that of marigolds.
The average amount of blood lost is from six to ten ounces, but it varies greatly among women who are otherwise normal and in good health. Some women regularly lose what seems to be an alarming quantity of blood at each period without suffering any apparent ill effect. Others lose so little that they are scarcely aware of their menses.
As a rule the menstrual flow is more profuse among women in warm climates than in cold regions. English women, for example, 52frequently menstruate profusely while in India, and upon their return to England note a marked decrease in the amount of the discharge. The same is often true of American women who move from Southern to Northern states, while removal from a low to a high altitude usually results in a more profuse flow.
The quantity of the menstrual discharge is affected also by diet, living conditions and by any form of mental or physical excitement or stimulation.
Accordingly, the highly strung, richly nourished women living in luxurious circumstances are likely to menstruate more freely than those less favored who are overworked and poorly nourished.
A shock or great grief, or any great emotional experience; a sea voyage or a long railroad journey may bring on a period before it is due, while the regularity of the periods may be much disturbed, temporarily, by a marked change of climate or altitude, a serious illness or a decided change in one’s daily régime.
The function may be entirely suspended for several months or a year in women who suddenly take up hard work or violent exercise, and persist with it regularly. In such cases the periods gradually recur and finally become normal and regular.
The menstrual period is frequently attended by evidences of marked mental and physical disturbances. While many women are fortunate enough to suffer little or no inconvenience during menstruation, the vast majority are more or less wretched and miserable at this time, although in good health in all other respects. Many are tired, have less endurance than usual and are likely to take cold easily. Headaches with a sense of fullness, dizziness, and heaviness are common accompaniments. Backache is a frequent source of discomfort, while abdominal pain, varying from an uncomfortable sense of dragging heaviness to almost unendurable agony, is the rule rather than the exception. And there may be pain in the hips and thighs as well.
This state of wretchedness is sometimes increased by a loss of appetite, nausea and even vomiting. At the same time there are changes in the breasts which are much the same as, though slighter than, those occurring during pregnancy. They are firmer, may be somewhat increased in size, and many women 53experience a burning, tingling sensation, soreness and even pain. The nipples are turgid and prominent and the pigmented areas grow darker for the time being.
The skin over the rest of the body sometimes changes in appearance and pimples are common; some women are pale and others are flushed during their periods.
These physical disturbances accompanying menstruation vary so widely in different women, and in the same women at different times and under different conditions, that it is not possible to draw a classical picture of the condition. But all of the symptoms above described will persist with more or less severity throughout the entire menstrual life of one woman, while perhaps only one or two of them will occasionally disturb another. Whatever discomfort there may be usually begins from one day to a week before the discharge appears; is at its height during the following day and from that time subsides steadily, until the normally comfortable state is regained. In fact, many women feel better at the end of their periods and during the days immediately following than at any other time during the cycle.
Heat applied to the abdomen and lumbar region during the uncomfortable days; hot baths, rest and quiet, will usually give great relief, as might be expected when there is local congestion and general nervous irritability. In this connection, it is worth mentioning that the discomfort of many women is needlessly increased by their heeding the widespread but fallacious belief that general bathing during menstruation is injurious. While cold plunges and cold showers are not recommended, certainly warm baths are innocuous and immensely satisfying.
In addition to the physical discomfort which is coincident with menstruation, and quite as common, are the evidences of mental and nervous instability. These often show themselves in the form of unwarranted irritability, and in a lack of poise and self-control. Drowsiness and mental sluggishness are not uncommon, and many otherwise cheerful women are almost overwhelmed by depression during menstruation.
All of these departures from what we are accustomed to regard as the normal, or average, mental and physical state of 54women are very baffling, as they may persist after every discoverable defect has been corrected.
But aside from all other considerations it is of obstetrical importance for the sufferer to ascertain the cause of her discomfort if possible. For example, a misplacement of the uterus is a frequent cause of dysmenorrhea and, if it remains uncorrected, may make conception impossible; or if conception perchance does take place, the malposition of the uterus may later be the cause of an interrupted pregnancy.
Endometritis is another cause of menstrual difficulty and if allowed to persist may be one factor in the causation of abnormalities in the attachment of the placenta.
There is evidently an intimate relation between the process of menstruation and the functions of the ductless glands throughout the body; a relation which is far from being understood.
For example, the administration of various preparations of ductless glands for maladies which are apparently unrelated to menstruation, results not alone in an improvement of the condition treated, but frequently in much more comfortable menstrual periods, as well.
It should be borne in mind, also, that the influence exerted by a woman’s mental, or psychic, state upon her menstrual periods is so apparent that it is being given increasingly serious recognition. It is frequently observed that patients who are under treatment for nervous and mental disorders, who are also sufferers from painful menstruation, grow more comfortable during their periods as their neurosis improves.
We have constantly before us examples of painful menstruation being relieved coincidently with an improved mental state among women situated at the two extremes of the social and financial scale. Indolent, self-centred and unoccupied women at one end often become excessively nervous and irritable, and suffer great pain with each period, while the overworked, harassed, poverty-stricken women at the other extreme have similarly trying menstrual experiences. When the self-indulgent sister can be persuaded to engage in some form of physical activity and to interest herself in some work which requires mental effort, and which perhaps makes an emotional appeal as well, she 55frequently finds that her menstrual difficulties become less troublesome.
In the case of the woman in poorer circumstances, an improvement in her mode of living which approaches the normal, and a relief from undue stress and anxiety, will very often be followed by more comfortable menstruation.
A recognition of these rather intangible facts is of consequence to the nurse, as it deepens her appreciation of the necessity for nursing her patient as a complete entity, mentally, physically, spiritually and emotionally. We are insistently reminded at every turn that no one part of the patient, no one aspect of her condition can be separately considered and the remainder overlooked.
The patient can be nursed quite satisfactorily only when she is nursed completely.
Relation Between Ovulation and Menstruation.—Menstruation and ovulation are apparently associated and interdependent, but the exact relation between the two is still obscure and puzzling. It is generally accepted that complete removal of the ovaries stops ovulation and is followed by a cessation of menstruation, and yet cases have been recorded which suggest that these two functions are not invariably correlative.
Evidence of this possible independence is that, although pregnancy must be preceded by ovulation, it has occurred before puberty or after the menopause. And not infrequently pregnancy occurs during lactation, a period when the menstrual function is usually suspended.
It has been claimed by some observers that menstruation has occurred after the complete removal of both ovaries, which would, of course, preclude the possibility of further ovulation. It is possible, however, that in such cases either the ovaries were not entirely removed, though believed to be, or that an accessory ovary existed, since a very small fragment of ovarian tissue will permit the occurrence of ovulation.
As to their chronological relation, information available at present suggests that ovulation occurs about ten or twelve days after the close of the preceding period, and that the corpus luteum 56formed at the site of the rupture reaches its highest development some ten or twelve days later, and that the degenerative changes in the corpus luteum, in case of non-fertilization of the ovum, give rise to menstruation.
Modifications of Menstruation. Dysmenorrhea is painful menstruation.
Menorrhagia is an abnormally copious menstrual flow.
Amenorrhea is irregularity or, to be exact, suppression of the menses. The suppression may be due to an obliteration of the neck of the uterus, or to an occlusion of the vaginal opening.
Vicarious menstruation is an escape of blood from other parts of the body coincident with menstruation. Blood may ooze through the skin covering the breasts; also from hemorrhoids or from the surface of ulcers. Or there may be nose-bleeding, vomiting of blood or pulmonary hemorrhage, particularly among tuberculous patients. Vicarious menstruation usually occurs among nervous, high-strung women and may be regarded as an evidence of ill health. The amount of blood lost in this way is much less than the amount of the menstrual flow.
The menopause, also termed the climacteric and the change of life, marks the permanent cessation of menstruation and of sexual activity. It occurs ordinarily between the ages of forty and fifty; the majority of women stop menstruating at their forty-sixth year. The menopause has occurred as early as the twenty-fifth year, and as late as the eightieth or ninetieth year. But such cases are, of course, extremely rare and their infrequent occurrence is of interest rather than of importance in an effort to ascertain the general average.
As the child-bearing period is normally about thirty years in duration, the prevailing belief is that the menopause comes earlier to women who began menstruating early, than to those who did not reach puberty until later. Some authorities contend, however, that early menstruation indicates extreme vitality, and that this vitality tends to prolong the child-bearing period. According to this theory, then, the menopause would come late to those who matured early and vice-versa.
As the menopause approaches, menstruation occurs irregularly; the discharge sometimes increases slightly but usually diminishes 57in amount and finally disappears altogether, while the generative organs all undergo atrophic changes.
Bearing in mind the disquieting effect of adolescence, and of ovulation, upon the general nervous, mental and physical state, we may reasonably expect that a complete cessation of the ovarian function would be attended by more or less disturbance of the general well-being.
It is true that very many women suffer a certain amount of nervous instability at the menopause; they tire easily; have “hot flashes” and possibly headaches. But under ordinary conditions the discomfort is not great, and after the function has entirely ceased and they become physiologically adjusted to the new order of things, these women often enjoy better health than ever before.
Unfortunately wide currency has been given to exaggerations concerning the symptoms of the menopause. The result is that serious organic diseases which are in no way related to the climacteric are not infrequently attributed to it. For this reason excessive bleeding, heart symptoms and what not are all too often accepted as a matter of course, and accordingly neglected until the patient is beyond medical aid. This is particularly and tragically true of cancer of the uterus.
It is a wise precaution, therefore, to regard with apprehension an increase in the amount of the menstrual flow of any woman past thirty, and not to accept it as a normal forerunner of the menopause.
CHAPTER III. DEVELOPMENT OF THE OVUM, EMBRYO, FETUS, PLACENTA, CORD AND MEMBRANES. The Ovum. The Spermatozoon. Fertilization. Heredity. Sex-determination. Most Favorable Age for Motherhood. The Morula. Growth in the Uterus. The Decidua. Ectoderm. Mesoderm. Entoderm. The Chorion and Placenta. The Amnion. The Umbilical Cord. The Fetus. Growth by Months. Factors Influencing the Size of Child. Multiple Pregnancy. Extra-uterine Pregnancy.
CHAPTER IV. GROWTH AND PHYSIOLOGY OF THE FETUS. Circulation. Kidneys. Bowels. Head. Fontanelles. Occipital Measurements.
CHAPTER V. SIGNS, SYMPTOMS, AND PHYSIOLOGY OF PREGNANCY. Duration of Pregnancy. Date of Labor. Signs of Pregnancy: Presumptive, Probable, and Positive. Physiological Changes in the Maternal Organism: Uterus. Cervix. Vagina. Tubes and Ovaries. Abdomen. Umbilicus. Breasts. Cardio-Vascular System. Respiratory Organs. Digestive Tract. Urinary Apparatus. Bony Structures. Skin. Carriage. Temperature. Mental and Emotional Changes. Ductless Glands.
As we learned in the last chapter, some of the ova which are discharged into the peritoneal cavity enter the fimbriated end of the tube, while very many others perish. As a rule an ovum enters the tubal opening adjacent to the ovary from which it has been discharged, but it is possible for this tiny cell to travel across the body and enter the tube on the opposite side.
This migration of the ovum, as it is termed, has been demonstrated in cases in which pregnancy has followed removal of the ovary on one side and the tube on the other.
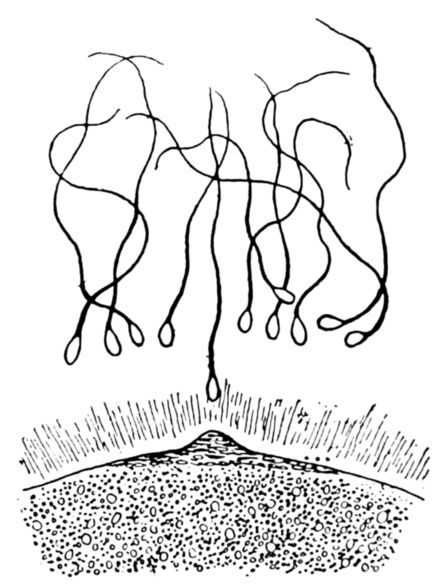
Fig. 17.—Diagram of spermatozoa, the male cells of germination.
There are various theories as to how and why an occasional migrating ovum, floating around in a relatively large cavity, ever enters the tubal opening, which, after all, is not large. The most widely accepted belief is that the motion of the cilia lining the tubes creates a suction which draws the microscopical cell into the opening, the same cilia being the means by which the ovum is later propelled downward through the tube to the uterus.
This journey of the ovum through the tube is of enormous consequence. During its course occur the events which decide whether the ovum shall, like most of its fellows, be simply swept along to no end and lost, or whether by chance it is to receive the mysterious impulse which begins the development of a new human being.
The amazing power which enables this cell to reproduce itself, and to develop with unbelievable complexity, is acquired somewhere 62in the tube by meeting and fusing with a spermatozoon, the germinal cell of the male. (Fig. 17.)
The spermatozoa look very much like microscopic tadpoles, with their flat, oval heads, tapering bodies and long tails. As these tails serve somewhat as propellers, the male cells are capable of very rapid motion. But in spite of their strange appearance, they are cells after all, and resemble the female cells in that each one contains a nucleus, or germinal spot.
An almost inconceivably large number of spermatozoa, floating in the seminal fluid, is deposited in the vagina at the time of intercourse. Nature evidently supplies the male and female cells with equal lavishness, in order to provide for the large number of both kinds which must inevitably be lost, and still have enough survive to accomplish the high purpose of their creation. A very considerable number of spermatozoa enter the uterus, and are enabled through their powers of motility, to travel up into the tubes, in spite of the downward current created by the cilia. And in the tube, usually in the upper end, they meet a recently matured and discharged ovum which is being swept downward, and are attracted to it somewhat as bits of metal are drawn to a magnet. Although the ovum which is destined to be fertilized is surrounded by several spermatozoa, only one actually enters and fuses with it.
This fusion is termed impregnation, fertilization, or, in lay parlance, conception, and the instant at which it occurs marks the beginning of pregnancy. The establishment of this fact is of no little importance, since it does away with any possible controversy concerning the time at which a new life begins. The origin of the child is exactly coincident with the fusion of the male and female germinal cells.
And furthermore, the sex of the child and any inherited traits and characteristics are also established at this decisive instant. No amount of dieting, exercise nor mental effort on the part of the expectant mother can alter or influence them in the smallest degree, for the father has made his complete contribution toward the creation of the new being, and after this event the mother provides nourishment only.
All told, probably more than five hundred theories have been 63advanced to explain what it is that decides of which sex the forthcoming child will be.
In 1907 Dr. Schenck attracted world wide attention by announcing his belief that either sex could be produced in the expected child through the simple expedient of regulating the mother’s diet. Liberal feeding would result in boys, the sturdier sex, and frugality in girls, the smaller, frailer type of baby. But as the results of applying Schenck’s theory have scarcely borne out his claims, it is given but scant attention to-day.
The present belief regarding the causation of sex is that although there is but one kind of ovum, there are two kinds of spermatozoa, one capable of producing a male, and the other a female child. These two kinds are evidently deposited in the vagina in about equal numbers, and the sex-determining form that fertilizes any one ovum is a matter of the merest chance. Statistics show, however, that more male than female babies are born, the usual proportion being about 105 boys to 100 girls among those that reach full term. Among abortions and premature births there is also a larger number of boys than girls, and in elderly primiparæ the ratio increases to about 130 boys to 100 girls. But as more boys die in infancy than girls, the two sexes about even up in the number of those living to adult age.
Apparently, then, there is some factor operating slightly in favor of the purposeful activities of the male-producing spermatozoa. But so far no accurate means has ever been found whereby it was possible to influence the development or discover the sex of a child before its birth.
There is a wide difference of opinion concerning the time of the month when fertilization is most likely to occur. Observations made upon the wives of sailors and under a variety of conditions suggest that the most favorable period is just before or just after menstruation which represents the second stage of the menstrual cycle.
Dr. Williams believes, however, that fertilization is most likely to occur about midway during the intermenstrual period. But since it is probable that spermatozoa are constantly present in the tubes of women who are exposed to the possibility of becoming 64pregnant, it is difficult to do more than speculate about the time of the month at which fertility is greatest.
Another moot question relates to the age of the woman at which it is most desirable that the first child shall be born. Recent observations made by Dr. John W. Harris upon a large number of pregnancies occurring in very young girls indicates that from a standpoint which considers solely the physical welfare of the mother and her infant, sixteen years is the most satisfactory age at which to bear the first child.
However, when motherhood is considered from all standpoints, social, ethical, spiritual as well as physical, the consensus of opinion seems to be that the twenty-third year is the most favorable age for motherhood to begin. Children have been born to little girls nine years old and to women of sixty-two, but the extremes of the reproductive years are not favorable periods for child-bearing.
As soon as a spermatozoon enters an ovum, it disappears and is completely absorbed, and, as the ovum in turn is instantly possessed of new powers, the result of this union is a cell which was previously non-existent.
This new cell is not only capable of reproduction by means of segmentation or cell division, but in the course of its sub-division and proliferation, it forms groups of cells which develop into tissues and structures widely different from each other. The entire complex human body, in addition to the placenta, cord, and membranes, arises from the single, extraordinary cell.
It first divides into two; these two divide into four; the four into eight and thus the process of division and sub-division continues until a solid mass is formed, shaped something like a mulberry and called the morula. (Fig. 18.)
While these developmental changes are taking place, the morula is being carried down the tube toward the uterus, by the sweeping motion of the ciliated membrane. The time consumed by this journey has not been definitely ascertained and though possibly it may be made in a few hours, it probably takes from five days to a week. Since the embryo is constantly moving during this time, it quite evidently has no attachment to the mother and cannot, therefore, derive any great amount 65of nourishment directly from her. The growth and development to this point, then, must be due chiefly to inherent powers within the mass of cells itself.
In all probability, the embryo is still in the morula stage and is about the size of the head of a pin when it reaches the uterus, where it finds that the endometrium has been prepared for its reception by the premenstrual swelling. The mucosa has grown thicker, more velvety and vascular, and its glands have increased in number and activity. The columnar epithelium of the endometrium is replaced by a thick layer of large, vacuolated cells, called decidual cells, and the uterine lining from now on is termed the decidua gravidatis. While the normal uterine mucosa is thin, averaging from 1 to 3 millimetres (0.039 to 0.117 inch) in thickness, it increases to a thickness of about 1 centimetre (⅞ inch) during pregnancy.
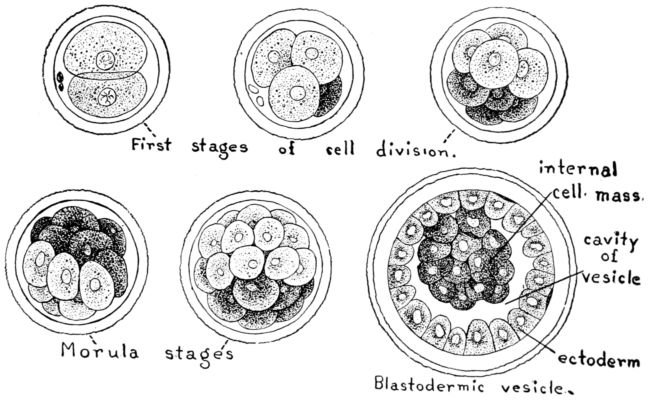
Fig. 18.—Diagram of segmenting rabbit’s ovum.
The point at which the embryo attaches itself to this spongy membrane is entirely a matter of chance. It usually rests somewhere in the upper part of the uterine cavity, promptly destroys the minute underlying area of tissue by digestive action and burrows into the decidua. As the margins of the opening thus made meet and fuse above the ovum, it is completely incapsulated 66in a cavity of its own that has no connection with the uterine cavity. (Fig. 19.)
After this occurrence the decidua consists of three portions: the hypertrophied membrane which lines the uterus as a whole, called the decidua vera, which atrophies during the latter part of pregnancy and is also thrown off in part with the membranes during labor, and later in the uterine discharges; the decidua basalis, or the decidua serotina, is that portion lying directly beneath the embryo which later enters into the formation of the placenta; and the decidua reflexa, which surrounds and covers the buried embryo, consists of the developed and fused margins of the pit in the mucosa, that have grown over the embryo.
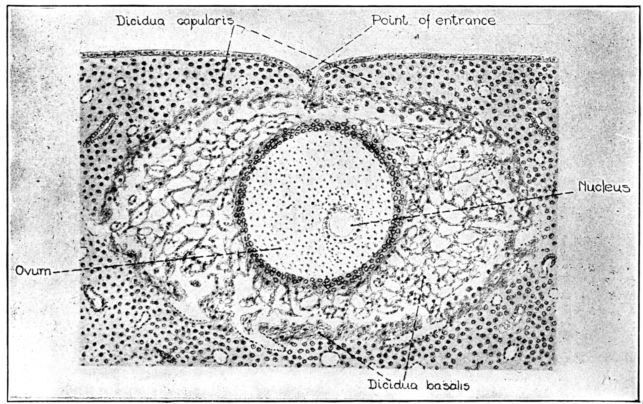
Fig. 19.—Ovum about 13 days old, embedded in the decidua. (The Bryce-Teacher ovum from Human Embryology by Keibel and Mall.)
As the cellular activity continues within the morula, fluid appears in the centre with the result that the cells are rearranged and pushed toward the periphery, thus forming a sac. At this stage the embryo is called the blastodermic vesicle.
At one point on the inner surface of this vesicle the cells proliferate and form a mass which is sometimes called the internal cell mass, or embryonic area, and the single layer of cells comprising the remainder of the vesicular wall, the primitive 67chorion. The cells in the mass are at first disposed in layers, the outer layer being termed the ectoderm; the inner layer the entoderm, while a third layer which appears a little later is called the mesoderm.
Although these three primitive layers of cells have all arisen from the single cell formed by the fused spermatozoon and ovum, they are even now very different in character. The differences steadily increase until finally all of the complex fetal organs and tissues, the membranes, cord and placenta, result from their further specialization and development, as follows:
From the ectoderm arises the skin with its appendages, and the salivary and mammary glands; the nasal passages, upper part of the pharynx and the anus; the crystalline lens, the external ear, the entire nervous system, the sense organs and, in part, the fetal membranes.
From the mesoderm are derived the urinary and reproductive organs; the muscles, bones, and connective tissues and the circulatory systems.
From the entoderm are developed the alimentary canal, the thymus, thyroid, liver, lungs, pancreas, bladder and the various small glands and tubules.
It was formerly believed that the human being existed in miniature in the first cell and that its development during pregnancy was entirely a matter of increase in size. But the microscope has disproved this, and we now know that embryonic development comprises both growth and evolution.
Much of the information accepted to-day is, of course, speculative, having been deduced from observations made upon the reproductive processes of lower mammals, since the youngest human ovum which has been discovered and examined was probably two weeks old. But the evidence points quite convincingly to the belief that the early stages of development consist of proliferation of and alterations in the kinds of cells, their arrangement into groups, and a differentiation of the functional activity of these groups of cells before the mass assumes human form and develops organs.
As to terminology, some authorities call this mass the embryo during this stage of grouping and differentiation, which corresponds 68to the first six weeks of pregnancy, and the fetus from then until the time of delivery. By others it is designated the ovum during the first two weeks of pregnancy, the embryo from the third to the fifth week, after which it is known as the fetus.
From the nurse’s standpoint these distinctions are of no consequence, for the mass may safely be called a fetus from the time that the expectant mother looks to the nurse for guidance and care.
It is scarcely warrantable to take the time and space which would be necessary to trace in detail through its various stages the intricate development of the human body, with its attached membranes. But the whole question is so important and so interesting that we shall at least have a word of description as to its size and characteristics at successive periods.
Although the exact length of time required for the maturation of the fetus is not known, it is estimated that two hundred and eighty days, or ten lunar months, elapse between the beginning of the last menstrual period and the beginning of labor. And in spite of the difference in size among the mothers, it is found that the products of conception develop and grow at a fairly uniform rate of speed.
A new human being is the ultimate result of conception, but the chorion, amnion, placenta and umbilical cord must also be created to serve as aids in building and protecting the developing child during its uterine life. The part played by these accessory structures is so vital, in spite of being temporary, that it will be well for us to look into their origin and functions before considering the fetus itself which they serve.
The Chorion and Placenta. Very early in pregnancy, probably while the fertilized ovum is journeying down the tube, tiny, thread-like projections, called villi, appear over the surface of the primitive chorion, giving it the shaggy appearance of a chestnut burr. Shortly after this shaggy ovum reaches the uterus and is embedded in the lining, the chorion, or the outer fetal membrane, is formed, being partly derived from the ectodermal layer of cells growing within the blastodermal vesicle. The chorion grows rapidly in size and thickness, and the villi upon its surface increase in size, number and complexity by frequent 69branching. In so doing the villi push their way into the maternal tissues surrounding them, and destroy the capillary walls with which they come in contact. Maternal blood escapes through the destroyed walls, forming tiny hemorrhagic areas, or “lakes of blood.” The chorionic villi float freely in these pools of maternal blood, which is constantly being refreshed by an inflow of arterial and an outflow of venous blood through the mother’s vessels.
Blood vessels soon appear in these chorionic villi, and fetal blood then circulates through them. It becomes apparent, therefore, that the maternal and fetal blood streams are in such close relation that they are separated by only the thin membrane which forms the walls of the vessels in the villi. (Fig. 20.)
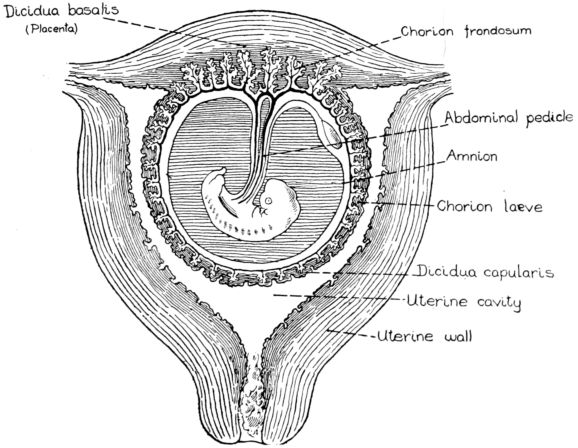
Fig. 20.—Diagram of fetus, cord, membranes and placenta in utero at an early stage of their development.
This arrangement makes it possible for the steadily proliferating villi to discharge one of their functions, which is to receive from the maternal blood nourishment for the embryo, and give up to the parent waste products from the growing body. This exchange of nourishment and waste matter takes place by means 70of osmosis. But freely as the exchange of materials occurs, there is never any contact, or mixing of maternal and fetal blood, nor does maternal blood at any time flow through fetal vessels. It was believed at one time that the fetus was nourished by milk which was in some way secreted by the gravid uterus, but this is disproved by present knowledge of the placental function.
The second function of the villi, particularly after they have developed to the placental stage, is to assist in securely attaching the embryo to the uterine wall.
The villi are equally distributed over the surface of the chorion at first, but as the sac increases in size and pushes out into the uterine cavity, they gradually atrophy and disappear, excepting over the small area beneath the vesicle where the chorion is in contact with the decidua basalis. At this site the villi become much more abundant, and it is here that the placenta eventually develops. This part of the chorion is termed the chorion frondosum, while the remainder, which is in contact with the decidua capsularis, is the chorion læve.
As pregnancy advances and the fetal sac enlarges, the chorion læve covered by the decidua capsularis, or reflexa, is pushed farther out into the uterine cavity, until finally it quite reaches the opposite wall, meets the decidua vera and obliterates the entire space which had existed between the two membranes. This means that instead of a uterine cavity lined with decidua, and a tiny capsule somewhere off to the side lined with chorion, the latter has distended until it completely fills and really becomes the cavity within the uterine walls, thus lining the uterus with chorion and crowding the original lining out of existence. The decidudae capsularis and vera fuse in time and finally the capsularis degenerates and disappears.
The Amnion. Returning for a moment to the blastodermal stage of the ovum, we find that the amnion, or inner membrane, first appears as a tiny vesicle over the dorsal surface of the embryo. Very soon, however, it invests the embryo completely, and the membranous sac is intact, excepting where it is pierced by the umbilical cord. The amnion, too, is derived in part from the ectoderm, but is a stronger, denser membrane than the chorion. At first there is an appreciable space, and some fluid, between 71the two membranes, but as the amnion increases in size with the advance of pregnancy, it comes in contact with and is loosely adherent to the chorion.
Very early in its development the amniotic sac contains a pale yellow fluid known as the amniotic fluid, or liquor amnii, in which the fetus floats. This fluid increases in amount until the end of pregnancy and though the quantity is variable, it usually amounts to about a quart.
The source of the liquor amnii is not definitely known, but it is generally believed to be of maternal origin, secreted from the amniotic membrane, though the possibility of its consisting partly of fetal urine cannot be overlooked. It is about 99% water, containing particles of dead skin and lanugo, a soft downy hair cast off from the body of the fetus, traces of albumen and both organic and inorganic salts.
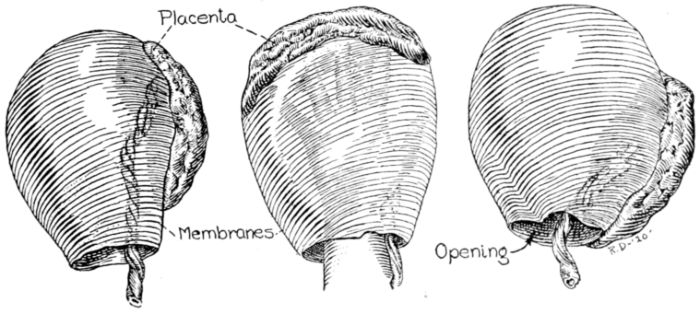
Fig. 21.—Diagram showing general structure and relation of membranes, placenta and cord.
The amniotic fluid serves a variety of purposes. Since the intestines of the fetus contain lanugo and particles of dead skin, it is evident that the child swallows some of this fluid during its uterine life, and possibly obtains in this way much of the fluid necessary for its development.
The increasing bulk of the fluid serves to distend the fetal sac and surrounding uterus, and thus provides the fetus with room for growth and movement. It also prevents adhesions between the child’s skin and the amnion, which are a factor, when by mischance they do occur, in causing monstrosities and intrauterine amputations. The fluid with which it is surrounded 72keeps the fetus at an equable temperature in spite of variations of temperature in the mother’s environment, and minimizes the danger of injury to the fragile little body, from pressure or blows on the mother’s abdomen. And by acting as a water wedge, forced down by uterine contractions at the time of labor, it dilates the cervix sufficiently to permit the expulsion of the full term child.
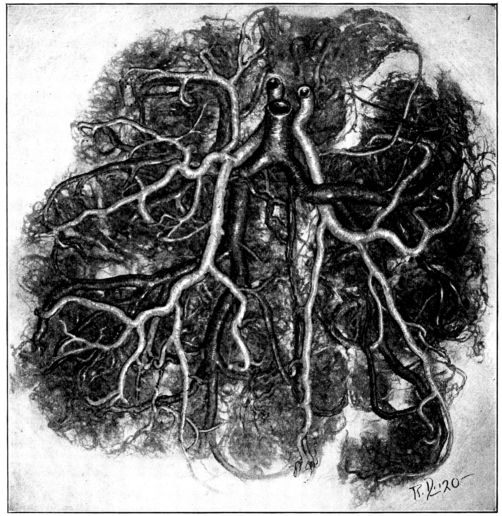
Fig. 22.—Placental blood vessels. Note their branching, tree-like arrangement. (Photographed from an injected specimen in the Obstetrical Laboratory, Johns Hopkins Hospital.)
The placenta. The placenta, in lay parlance the after-birth, is really a thickened, amplified portion of the fetal sac, which has developed at the site of the implantation of the ovum. It is partly fetal and partly maternal in origin, being developed 73jointly from the chorion frondosum with its branching villi, and the underlying decidua basalis.
The chorionic villi already referred to grow and branch in a tree-like fashion (Fig. 22), and push their way farther and farther into the uterine tissues creating the intervillous spaces which fill with maternal blood. From the time that the first fetal blood vessels appear in these floating villi, until the child is born, there is a constant exchange of nutriment and waste matter between the maternal and fetal blood; the arterial maternal blood in the intervillous spaces giving to the fetal blood in the villi the oxygen and other substances necessary to nourish and build the growing young body, and receiving in return the broken-down products of fetal activity. The waste is carried by the maternal blood stream to the mother’s lungs, kidneys and skin, by which it is excreted.
This exchange of substances is accomplished by osmosis and also by selective powers of the cells in the villi. Thus the placenta virtually serves the fetus as lungs, stomach, intestines and kidneys throughout its uterine life.
In addition to the nutritive substances in the mother’s blood, such as albumen, iron and fat which are so altered by cell action as to be absorbable through the villi, certain protective substances as the anti-toxines of diphtheria, tetanus, colon and typhoid bacilli are evidently transmitted from the maternal to the fetal circulation. It is claimed by some authorities that pathogenic organisms, for example, anthrax, pneumonia and tubercle bacilli, may be transmitted from mother to fetus, but the reported cases are so rare that the accepted belief is that organisms are seldom transmitted, if the placenta is healthy and intact. But, according to Dr. Williams, the transmission of typhoid occurs frequently, though malarial parasites cannot pass through the villous membranes.
Only during comparatively recent years has accurate knowledge of the origin and function of the placenta been available. Many varied and interesting beliefs and superstitions gained currency in the past, but all of them were erroneous.
The description of the circulation of the blood by William Harvey in 1628 shed considerable light upon this puzzling question 74concerning the exchange of fuel and ash between the parent and fetal bodies. But a mistaken belief that the maternal blood actually entered and flowed through the fetal vessels resulted from his valuable discovery.
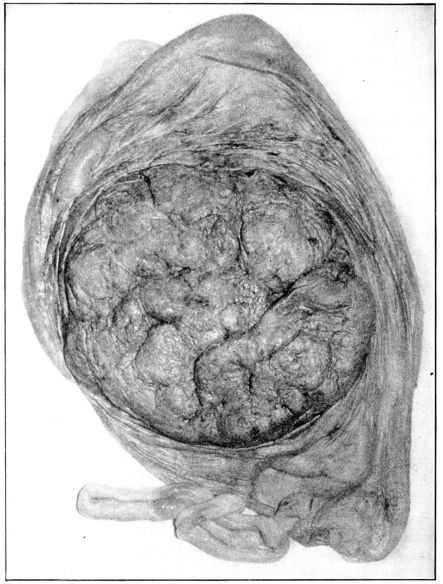
Fig. 23.—Maternal surface of the placenta, surrounded by the membranes and cord. (From a photograph taken at Johns Hopkins Hospital.)
When we examine this interesting structure, the placenta, 75after it is cast off, we find it to be a flattened, fairly round, spongy mass, eight or nine inches in diameter, about an inch thick where the cord arises and thinning out toward the margin. Continued from the margin are the filmy fetal membranes, which together form a ruptured sac. The rupture in these membranes is the opening through which the amniotic fluid escapes, and the child passes during birth.
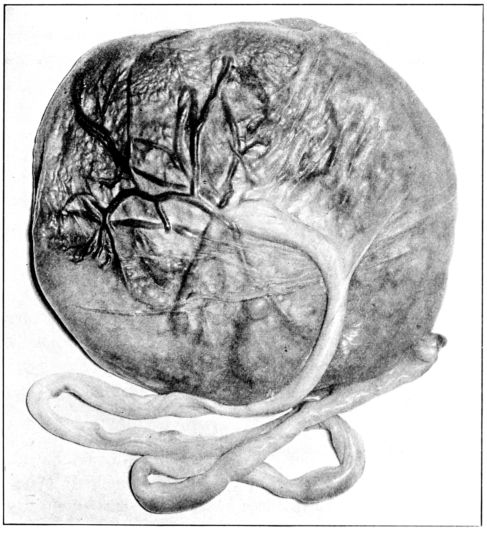
Fig. 24.—Fetal surface of the placenta showing origin of cord. (From photograph taken at Johns Hopkins Hospital.)
The placenta weighs about a pound and a quarter, or ⅙ as much as the child, and accordingly varies in size and weight with the baby. The maternal surface (Fig. 23) having been detached from the uterine wall, is rough and bleeding and is irregularly divided into lobes while the inner, or fetal, surface is smooth 76and glistening and covered with the amnion. The fetal surface (Fig. 24) is traversed by a number of large blood-vessels which converge toward the point of insertion of the umbilical cord, from the vessels of which they really arise. These vessels branch and divide until their termination in the innumerable chorionic villi floating in the lakes of maternal blood.
The Umbilical Cord. The cord, or funis, is a bluish white cord about three-quarters of an inch in diameter, twisted and tortuous throughout its length of about twenty inches. It is the one actual link between the mother and her unborn child, one end being attached to the abdomen of the fetus, about midway between the ensiform and the pubis, and the other to the inner surface of the placenta. The cord is derived from the abdominal pedicle and is merely an extension of the caudal or tail end of the embryo. It is covered with a layer of ectoderm which is continuous with the ectodermal covering of the fetus.
The cord consists of a gelatinous mass known as Wharton’s jelly, in the centre of which are embedded three blood vessels; two arteries through which the vitiated blood flows to the placenta, where it gives up its ash; and one vein which carries oxygenated, nourishment-bearing blood back to the fetus. The life of the fetus, therefore, is absolutely contingent upon an uninterrupted, two-way flow of blood through the cord.
The Fetus. In tracing the development of the ovum after its implantation in the uterine lining, we begin, as previously stated, with a shaggy-looking vesicle, containing fluid, with a clump of cells hanging toward the centre from their point of attachment on the inner surface of the sac. This clump develops into the embryo.
During the first month the mass increases in size, becomes somewhat elongated and curved upon itself with the two extremities almost in contact. The abdominal pedicle, which later becomes the umbilical cord, appears; the alimentary canal exists as a straight tube and the thymus, thyroid, lungs and liver are recognizable. The heart, eyes, nose, ears, and brain appear in rudimentary form and the extremities begin to be evident as tiny, bud-like projections on the surface of the embryo.
By the end of the fourth week the sac is about the size of 77a pigeon’s egg and has two walls. The outer wall, or chorion, as we have already seen, is covered with villi, and the amnion, or inner wall, is smooth; the contained embryo is surrounded by amniotic fluid and measures about 10 millimetres or 4 inches in length.
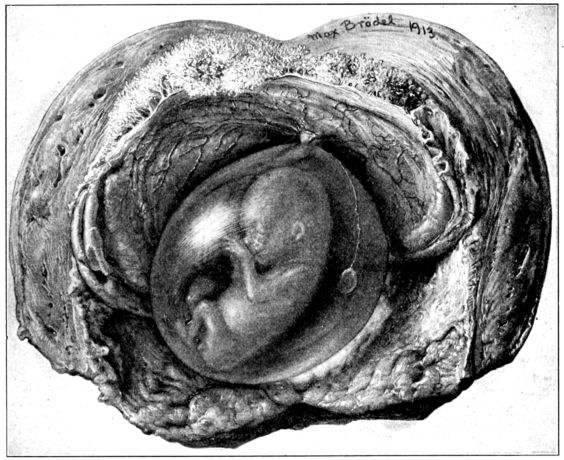
Fig. 25.—Embryo, about 5.5 centimetres long in amniotic sac; uterine wall incised, chorion split and turned back. Drawn by Max Brodel. (From The Umbilicus and Its Diseases, by Thomas R. Cullen, M.D.)
By the end of the second month, or eighth week, the head end of the embryo has greatly increased in size and is about as large as the rest of the body. Bone centres appear in the rudimentary clavicles; the kidneys and supra-renal bodies are formed; the limbs are more developed, webbed hands and feet are formed, the external genitalia are apparent but the sex is not distinguishable. The amnion is distended with fluid, but it is 78not yet in contact with the chorion; the chorionic villi have become more luxuriant on that part of the chorion resting on the decidua basalis, the future site of the placenta. The approximate weight of the embryo is 4 grams and its length 25 millimetres or an inch.
By the end of the third month, or twelfth week, centres of ossification have appeared in most of the bones, the fingers and toes are separated and bear nails in the form of fine membranes; the umbilical cord has definite form, has increased in length and begun to twist. The neck is longer, teeth are forming and the eyes have lids. The amnion and chorion are now in contact, and the villi have disappeared excepting at one point where a small, but complete placenta has developed. The embryo is about 9 centimetres long and weighs about 30 grams.
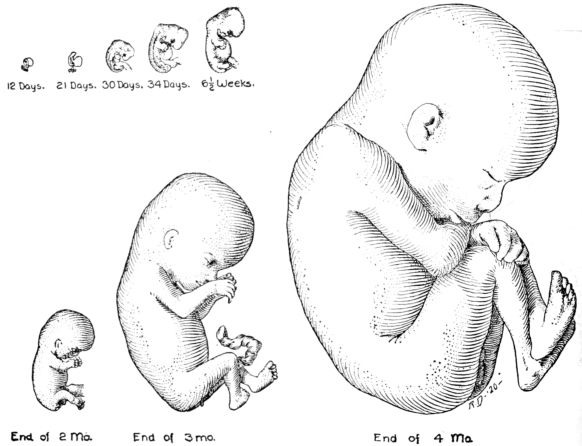
Fig. 26.—Diagram showing appearance of fetus at different stages in its development.
By the end of the fourth month, or sixteenth week, all parts show growth and development; lanugo appears over the body; 79the sex organs are clearly distinguishable and there is tarry fæcal matter, called meconium, in the intestines. The placenta is larger, the cord longer, more spiral and also thicker because of the Whartonian jelly which is beginning to form. The fetus is about 15 centimetres long and weighs about 120 grams.
By the end of the fifth month, or twentieth week, the fetus has both grown and developed markedly. It is now covered with skin on which are occasional patches of vernix caseosa, a greasy, cheesy substance consisting largely of a secretion of the sebaceous glands. There is some fat beneath the skin but the face looks old and wrinkled. Hair has appeared upon the head and the eyelids are opening. It is usually during the fifth month that the expectant mother first feels the fetal movements which are commonly referred to as “quickening.” The body is about 25 centimetres long and weighs about 280 grams.
By the end of the sixth month, or twenty-eighth week, the fetus still looks thin and scrawny, the skin is reddish and is well covered with vernix caseosa and the intestines contain an increased amount of meconium. If born at this time the child will move quite vigorously and cry feebly. Although it is not likely to live for any length of time, every effort should be made to save its life, for it may be that the high rate of mortality at this age is due to the inadequacy of the attempts which are usually made to save the child rather than to the frailty of the child itself. It is about 35 centimetres long and weighs about 1200 grams.
By the end of the eighth month, or thirty-second week, the child has grown to about 42 centimetres in length and 1900 grams in weight, but continues to look thin and old and wrinkled. The nails do not extend beyond the ends of the fingers but are firmer in texture; the lanugo begins to disappear from the face but the hair on the head is more abundant. If born at this stage, the baby will have a fair chance to live, if given painstaking care. This is true in spite of the ancient superstition, still widely current, that a seven months’ baby is more viable than one born at eight months (meaning calendar months). The fact is that after the eighth lunar month, a little more than seven calendar months, 80the probability of the child’s living increases rapidly with the length of its intra-uterine life.
By the end of the ninth month, or thirty-sixth week, the increased deposit of fat under the skin has given a plumper, rounder contour to the entire body; the aged look has passed and the chances for life have greatly increased. The baby now weighs about 2500 grams and is about 46 centimetres long.
The end of the tenth month, or fortieth week, usually marks the end of pregnancy. (Fig. 27.) The average, normally developed baby has attained a length of 50 centimetres (20 inches), and a weight of 3250 grams, or about 7¼ pounds, boys usually being about three ounces heavier than girls.
It must be remembered, however, that these figures merely represent the average drawn from a large number of cases, for there may be a variation in weight among entirely normal healthy babies from a minimum of 2300 grams (5 pounds) to as high as 5000 grams (11 pounds), or more. Babies actually weighing more than 12 pounds are seldom born, in spite of legends and rumors to the contrary.
The length of a normal baby is less variable than the weight. In fact, it is so nearly constant in its increase during the successive months of pregnancy, that the age of a prematurely born fetus may be fairly accurately estimated from its length. This fact is of no little practical importance, since it aids the obstetrician in making a prognosis as to the child’s prospect of living, for he can estimate its intra-uterine age from its body length.
The size of the baby is affected by race, colored babies, for example, averaging a smaller weight than white babies. And, as might be expected, the size of the parents is likely to be reflected in the size of their infants, large parents tending to have large children and vice versa.
The number of children which the mother has previously borne is also a factor, since the first child is usually the smallest, the size of those following showing an increase with the mother’s age up to her twenty-eighth or thirtieth year, provided the successive pregnancies do not occur at too frequent intervals.
The expectant mother’s general state of health, her state of nutrition, the character of her surroundings and her mode of 81living may be expected to influence her baby’s welfare. Hence, women who live in comfortable, or luxurious circumstances usually have more robust babies than those who are run down, poorly nourished or overworked. All of which hints at the great value of prenatal care which will be taken up in detail in a later chapter.
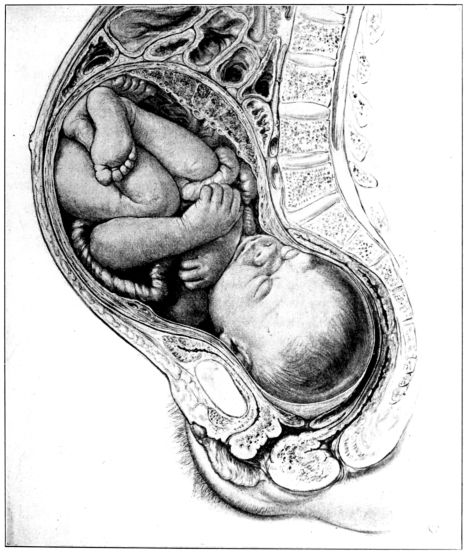
Fig. 27.—Full term fetus in utero. Drawn by Max Brodel. (Used by permission of A. J. Nystrom & Co., Chicago.)
82A multiple pregnancy is one in which the pregnant uterus contains two or more embryos, these being termed twins when there are two and triplets when there are three; quadruplets, quintuplets and sextuplets when there are four, five and six embryos, respectively, six being the largest accredited number on record.
The tendency to multiple pregnancies is apparently inherited, and it sometimes happens that several members of the same family connection have this predisposition, as evidenced by the number of twins and triplets to be found among relatives. It is estimated that twins occur once in 90 pregnancies and triplets once in about 7000 cases.
Twin pregnancies may result from the fertilization of one or of two ova, and are designated as single ovum or double ovum twins respectively. In single ovum twins the egg becomes divided early in its development and two embryos are formed. In such a case there is one placenta, one chorion and two amnions and the babies are of the same sex.
In double ovum twins two ova are fertilized; both may come from the same ovary or there may be one from each side. When double ovum twins occur, there are two placentæ, as a rule, though they may be somewhat fused; two amnions and two chorions and the babies may be of the same sex or each of a different sex.
Twins are often prematurely born and each one is likely to be smaller than a baby resulting from a single pregnancy, but their combined weight is greater than that of one normal baby.
An extra-uterine pregnancy may be defined as a pregnancy which develops outside of the uterus, usually in a tube or ovary. Although in the normal course of events the fertilized ovum travels down the tube and becomes attached to the uterine lining, it is possible for it to stop, and more or less completely develop at any point along the way between the Graafian follicle, from which it has been projected, and the uterus toward which it is traveling. If the fetus develops in the ovary, it is termed an ovarian pregnancy, and a tubal pregnancy if it occurs in the tube, the latter being the most frequent variety of extra-uterine pregnancy.
83In the opinion of Dr. Mall, only about 1 per cent of all extrauterine pregnancies are capable of going to term. There may be an abortion, when the fetus and membranes are partly or completely extruded from the fimbriated end of the tube into the peritoneal cavity; or a rupture of the tube, when the fetus, with or without the membranes, may be expelled into the peritoneal cavity, or between the folds of the broad ligament. If the greater part of the placenta remains attached to the site of its development, in the case of a ruptured tube, it is possible for the fetus to live and grow and even go to term. But if the placenta is nearly, or completely separated, the fetus perishes and may be largely absorbed by the maternal organism, or mummified, or putrefactive changes may take place. It is usually customary to terminate an extra-uterine pregnancy as soon as it is diagnosed, for only a very small number can be expected to go to term, the majority aborting, or rupturing the tube, with serious hemorrhage from the mother as a frequent result.
To sum up the normal pregnancy, we find that in the course of ten lunar months, following the fertilization of an ovum, the uterus grows from a small, flattened, pelvic organ, three inches in length, to a large, globular, muscular sac, constituting an abdominal tumor about fifteen inches long; it increases its weight thirty-two times, that is from two ounces to two pounds, while the capacity of the uterine cavity is multiplied five hundred times. Within the cavity is a child weighing about seven and a quarter pounds, surrounded by a quart or so of amniotic fluid. This fluid is contained in the sac composed of the fetal membranes, the amnion and chorion, which are excessively developed at one point into the placenta. The placenta, in turn, is attached to the child by means of the umbilical cord. The total weight of the uterus and its contents at term is usually about fifteen pounds.
Quite as mysterious and inexplicable as the development of these complex structures from one tiny cell is the fact that when the new human being is ready to begin life as a separate entity, further changes occur within the mother’s body which produce uterine contractions of such a character as to entirely empty the uterus of its contents.
Although the fetus at term is in many respects simply a diminutive, immature man, or woman, its anatomy and physiology present certain characteristics which have adapted it to a protected existence in a sac of fluid. Some of the fetal structures and functions become increasingly active after birth, while others subside and disappear.
We have seen that after the first month of pregnancy the placenta serves the fetus as a combined respiratory and digestive apparatus, not alone in supplying the oxygen and nourishment requisite for life and growth, but also in excreting the broken-down products of fetal life. It apparently acts somewhat as a liver, too, in performing something akin to a glycogenic function.
Obviously, then, the fetus must possess a circulatory mechanism which is peculiar to itself alone, and not found in the independently existing human body, in which the lungs and alimentary tract are functioning as intended. This mechanism is provided by means of certain structures which exist in the fetal circulatory system and which automatically disappear shortly after birth. The nurse must be aware of these anatomical changes that take place, in addition to growth, if she is to have an intelligent grasp of her tiny patient’s possible needs.
The structures which change or disappear after birth are the foramen ovale, a direct opening between the right and left auricles, and four blood vessels: the ductus arteriosus, ductus venosus and the two hypogastric arteries. An understanding of the functions of these vessels involves an understanding of the course followed by the fetal blood currents, as indicated in Fig. 28, page 85.
We see that there are three vessels within the umbilical cord: the umbilical vein and two arteries. In spite of its name, the vein 85conveys arterial blood from the placenta to the fetus. After piercing the baby’s abdominal wall, it divides into two vessels; the larger one, called the ductus venosus, empties into the inferior or ascending vena cava, while the smaller branch joins the portal vein, which enters the liver. The relatively large amount of arterial blood sent directly to the liver may in part account for the large size of this organ in the fetus. Upon its emergence from the liver, this blood stream flows into the inferior vena cava.
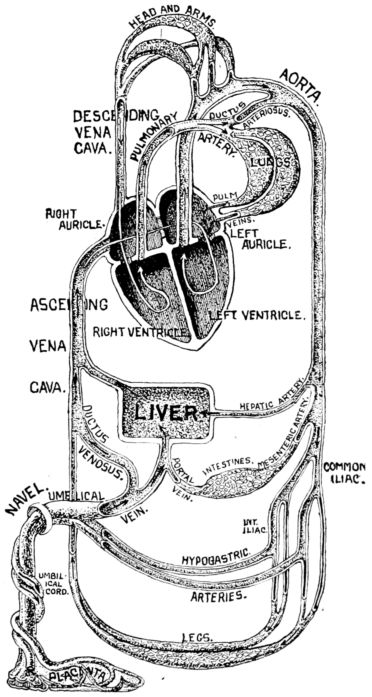
Fig. 28.—Diagram showing course of fetal circulation through hypogastric arteries, ductus venosus, ductus arteriosus and the foramen ovale. (From The American Text Book on Obstetrics.)
86The ascending vena cava, then, pours into the right auricle a mixture of arterial blood, which has come directly from the placenta, and venous blood returned from the liver, intestines and lower extremities. There is a difference of opinion concerning the course of the blood stream after reaching the right auricle. The general teaching, however, is that the eustachian valve, guarding the foramen ovale, deflects the current through this opening from the right into the left auricle. It then pours into the left ventricle, is pumped into the arch of the aorta, from which most of the blood is sent to the head and upper extremities, though a small part carries nourishment to other parts of the body.
The descending, or superior, vena cava, carrying blood returning from the head and arms also empties into the right auricle; this stream presumably crosses the stream which is directed toward the foramen ovale, flows into the right ventricle by which it is pumped into the pulmonary artery. The circulation of blood through the lungs, however, is for their own nourishment, and not for aëration as with the adult. For this reason most of the contents of the fetal pulmonary artery empties into the aorta through the ductus venosus, one of the temporary fetal structures already referred to. From the aorta the stream is directed in part to the lower extremities and the pelvic and abdominal viscera, but most of it flows into the hypogastric arteries. These are also temporary arteries. They lead to the umbilical cord and, as the umbilical arteries, carry the venous or vitiated blood through the cord to the placenta where it is oxygenated, freed of its waste in the chorionic villi and returned to the fetus through the umbilical vein.
As soon as the child is born and it is obliged to obtain its oxygen from the surrounding air, its pulmonary circulation of necessity becomes immediately more important and is greatly increased in volume. In fact, the entire fetal circulation is readjusted to meet the needs of the new and independent functions which the little body now assumes. The temporary structures are obliterated, since they are no longer needed, and the lungs and intestines become more active in compensation.
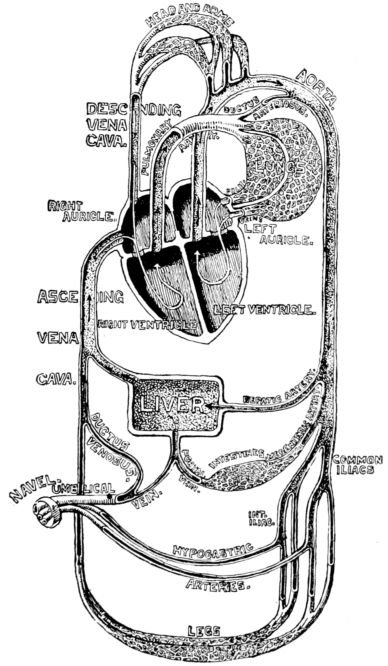
Fig. 29.—Diagram showing circulation of the blood after birth, with hypogastric arteries, ductus venosus, ductus arteriosus and foramen ovale in process of obliteration and pulmonary circulation greatly increased. (From The American Textbook on Obstetrics.)
As the ductus venosus and hypogastric arteries terminate in blind ends and become useless as soon as the umbilical cord is cut, they soon begin to atrophy and are obliterated within a few days after birth. This means that less blood is poured into the right auricle, which naturally results in relatively less tension in the right heart and an increased pressure in the left, which tends to close the foramen ovale. The foramen ovale does not entirely disappear at once, however, but closes gradually, sometimes remaining open for months. Occasionally it remains open permanently, and though some people have gone through life comfortably 88with a patent foramen ovale, its ultimate failure to close usually results in serious circulatory trouble. This is also true of the ductus arteriosus, which sometimes, but not often, fails to close.
The rule is that as the lungs expand and an increased amount of blood is carried to them for aëration, the ductus arteriosus deflects a steadily diminishing stream from the right ventricle to the arch of the aorta. Thus it gradually ceases functioning in most cases and disappears in the course of a few weeks. The abandoned vessels may degenerate and disappear in time or they may persist in the form of small fibrous cords. (Fig. 29.)
Although the circulatory system shows the most elaborate adjustments to the protection afforded by intra-uterine life, there are also other adaptations made by the fetal organism.
The baby acquires about 90 per cent of its weight during the latter half of pregnancy, as well as a steadily increasing proportion of solids and a decrease of fluids in its tissues, for in its early days the embryo consists largely of water. But for all of that, its existence and growth in utero, and the functioning of its heat producing centre require surprisingly little oxygen and nourishment. The amniotic fluid keeps the fetus at an equable temperature, about 1° above that of the mother, and as space within the uterine cavity permits of only limited movement, there is very little combustion for the liberation of heat and energy.
The kidneys assume functional form at a very early fetal age, probably about the seventh week, and the presence of albumen and urea in the amniotic fluid suggest that small amounts of urine may be voided, particularly during the latter part of pregnancy.
The bowels, on the other hand, are normally inactive, this is in spite of the fact that the baby evidently obtains fluid, and possibly some nutriment by swallowing amniotic fluid. But a discharge of meconium may be caused by pressure on the cord or by any condition which interferes with the umbilical circulation. For this reason, meconium stained fluid escaping during labor in a head presentation may be taken as an evidence of imminent asphyxiation, due to an interruption of the umbilical circulation.
The head is the most important part of the fetus, from an 89obstetrical standpoint, since the process of labor is virtually a series of adaptations of the size, shape and position of the fetal skull to the size and shape of the maternal pelvis. And since the pelvis is rigid and inflexible the adjustment must all be made by the fetal head, which is mouldable because of being incompletely ossified at birth. If the head passes through the inlet safely, the rest of the delivery will usually be accomplished with comparative safety. But a marked disproportion between the diameters of the head and pelvis, or limited mouldability of the head, constitutes a serious complication, which will be discussed later in connection with obstetrical operations.
A baby’s head is larger, in proportion to its body, than an adult’s, while the face forms a relatively smaller part of the baby’s than of the adult’s head. The major portion is the dome or vault-like structure forming the top, sides and back of the head, which in turn is made up of separate and as yet ununited bones. They are the two frontal, two parietal, two temporal and the occipital bone, with which the wings of the sphenoid bones, though less important, may be included.
These bones are not joined in the fetal skull, but are separate structures, with soft, membranous spaces between their margins, called sutures; while the irregular spaces formed by the intersection of two or more sutures are called fontanelles, possibly so called by the early observers because the pulsation of the soft tissues beneath these spaces suggests the spurting of a fountain.
The sutures are named and situated as follows: The frontal lies between the two frontal bones; the sagittal extends antero-posteriorly between the parietal bones; the coronal between the frontal bones and the anterior margins of the parietal, while the lambdoidal suture separates the posterior margin of the parietal from the upper margin of the occipital bone. There are also the temporal sutures between the upper margins of the temporal bones and the lower margins of the two parietals, but they are of no obstetrical importance, as they cannot be felt on vaginal examination. (Fig. 30.)
There are two fontanelles of obstetrical significance. The greater, or anterior fontanelle, also called the bregma or sinciput, 90is located at the meeting of the coronal, sagittal and frontal sutures. It is diamond or lozenge shaped, about an inch in diameter and is not obliterated during labor.
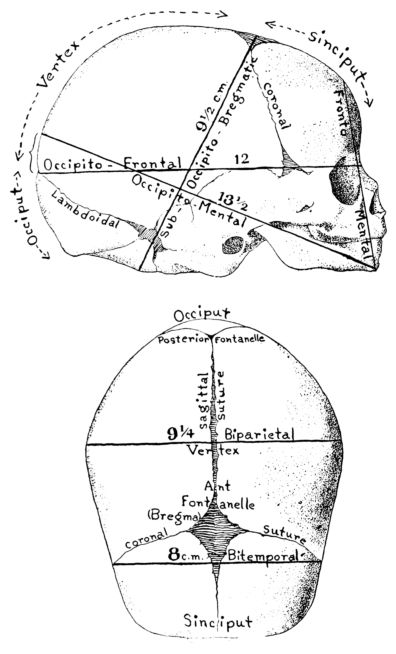
Fig. 30.—Side and top views of fetal skull giving average length of important diameters.
The smaller or posterior fontanelle is the triangular space at the inter-section of the sagittal and lambdoidal sutures, and may be obliterated as the surrounding bony margins approach each other during labor.
The coronal, frontal, lambdoid and sagittal sutures and the anterior and posterior fontanelles are of greatest diagnostic value as they can be felt through the vagina during labor. It is by 91recognizing and locating these sutures and fontanelles at this time that the accoucheur is enabled to determine the exact position and presentation of the fetus.
The fact that the skull is made up of separate bones, with soft membranous spaces interposed between them, permits of its being compressed or moulded to a considerable extent as it passes through the birth canal. Opposing margins may meet, or even overlap, to such a degree that the diameter of the head will be appreciably diminished and permit of its passage through a relatively narrow canal. This mouldability varies greatly, however, and the difference in the degree of compressibility of heads of approximately the same size may spell the difference between an easy and a difficult, or even an impossible labor.
A new-born baby’s head may be so distorted and elongated by the moulding process that it is unsightly and gives the young mother great concern. But the nurse can be quite confident in her assurances that the little head will assume its normal, rounded outline in a very few days.
The five most important diameters of the new-born baby’s head are:
1. The occipito-frontal (abbreviation, O.F.), measured from the root of the nose to the occipital protuberance, is 11.75 centimetres.
2. The biparietal (B.I.P.) is the longest transverse diameter, being the distance between the parietal protuberances, and measures 9.25 centimetres.
3. The bi-temporal (B.T.) is the greatest distance between the temporal bones and measures 8 centimetres.
4. The occipito-mental (O.M.) is the greatest distance from the lower margin of the chin to a point on the posterior extremity of the sagittal suture, and measures 13.5 centimetres.
5. The sub-occipito bregmatic (S.O.B.) is measured from the under surface of the occiput, where it joins the neck, to the centre of the anterior fontanelle, a distance of 9.5 centimetres.
The greatest circumference of the fetal head is at the plane of the occipito-mental and biparietal diameters and measures 38 centimetres. The smallest circumference is at the plane of the sub-occipito-bregmatic and biparietal diameters, and measures 28 centimetres.
92These figures, however, like all of those which it is possible to give, simply represent averages taken from a large number of cases. Individual variations will be found among normal babies, for boys’ heads, for example, are usually larger than girls’ while the head of the first child is likely to be smaller than the heads of those born subsequently.
Signs and Symptoms of Pregnancy. Unfortunately for all parties concerned, the exact duration of pregnancy has never been ascertained, since there is no way of knowing when the ovum is fertilized, the moment which marks the beginning of pregnancy.
It is obviously impossible, therefore, to foretell exactly the date of confinement. But labor usually begins about ten lunar months, forty weeks or from 273 to 280 days after the onset of the last menstrual period.
Thus the approximate date of confinement may be estimated by counting forward 280 days or backward 85 days from the first day of the last period. Or what is perhaps simpler, and amounts to the same thing, one may add seven days to the onset of the last period and count back three months. For example, if the last period began on June third, the addition of seven days gives June tenth, while counting back three months indicates March tenth as the approximate date upon which the confinement may be expected.
This is probably as satisfactory as any known method of computation, but at best it is only approximate, being accurate in about one case in twenty. But it comes within a week of being correct in half the cases, and within two weeks of the date in eighty per cent of all pregnancies.
Another method sometimes employed by obstetricians is to estimate the month to which pregnancy has advanced by measuring the height of the fundus, and thus forecasting the probable date of confinement. It is generally agreed that the ascent of the fundus is fairly uniform and that at the fourth month it is half way between the symphysis and umbilicus; at the sixth month, on a level with the umbilicus; at the seventh month, three fingers’ breadth above; at the eighth month, six fingers 94above the umbilicus and at the ninth month just below the xiphoid. At the tenth month, or term, the fundus sinks downward to about the position it occupied at the eighth month. (Figs. 31, 32 and 33.)
This method, however, is measuring by months, not days, and leaves a wide margin for conjecture as to the exact date.
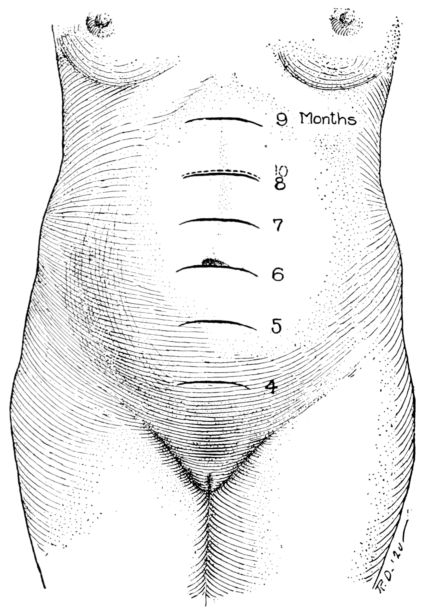
Fig. 31.—Height of fundus at each of the ten lunar months of pregnancy.
Still another method is to count forward 20 or 22 weeks from the day upon which the expectant mother first feels the fetus move. As we shall see presently, this experience, termed “quickening,” usually occurs about the 18th or 20th week, but is so irregular that it is unreliable as a basis for computation.
The possibility of estimating the date of confinement is still further complicated by the fact that there is evidently considerable 95variation in the length of entirely normal pregnancies. Many healthy children are born before ten lunar months have elapsed, while more deliveries occur after than on the expected date. The first pregnancy is usually shorter than subsequent ones, and women who are well nourished and well cared for have longer pregnancies, as a rule, than those less favored.
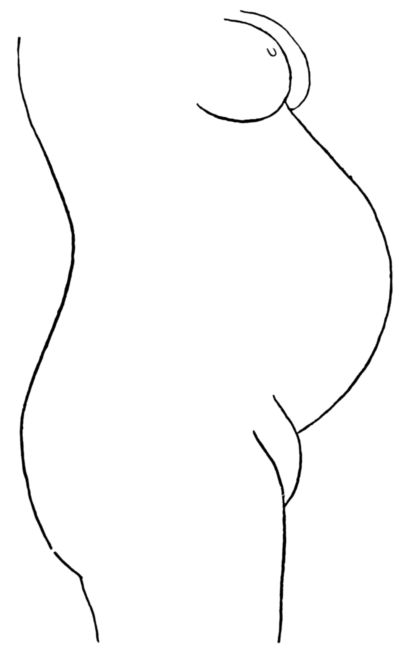
Fig. 32.—Contour of abdomen at ninth month of pregnancy, or before the waistline drops.

Fig. 33.—Contour of abdomen at tenth month of pregnancy, or after the waistline has dropped.
Although the symptoms of pregnancy have been observed throughout the ages by women who have borne children, and accoucheurs of one sort and another who have attended them, a positive diagnosis at an early stage of this condition is sometimes still baffling to the most experienced obstetricians.
So many symptoms of pregnancy are known to women the world over, that an expectant mother frequently recognizes her pregnant state at a very early date. This is particularly true of women who have previously borne children. But as these same symptoms closely resemble those of other conditions, they are not infrequently ascribed to impaired health, with the result that the pregnancy is not discovered until it is well advanced, and then sometimes only by accident. And one even hears of an occasional 96case in which a woman is entirely unaware of her condition until she goes into labor.
The converse is also true, for women sometimes erroneously believe themselves pregnant because of the appearance of well recognized symptoms, which are due to other causes. This condition is known as pseudocyesis, or spurious pregnancy, and is usually found in women approaching the menopause or in young women who intensely desire offspring. It is a pathetic occurrence, and the patient is usually so tenacious of her belief in her approaching motherhood that the obstetrician dispels it only with great difficulty.
For all of these and other reasons it is customary to divide the signs and symptoms of pregnancy into three groups, under self-explanatory headings, namely: presumptive symptoms, and probable and positive signs. Although it is never within the province of a nurse to make a diagnosis, it is important that she be familiar with symptoms. In obstetrics this seems to be particularly true, and especially so if the nurse be engaged in prenatal work or in any branch of public health nursing that brings her in touch with possible or expectant motherhood. The wider her grasp of obstetrical knowledge, the more helpful and reassuring can be her relation to her patient. To this end, therefore, we will take up the most reliable symptoms and signs of pregnancy.
The presumptive signs, which consist largely of subjective symptoms observed by the patient herself, are as follows:
1. Cessation of menstruation. This is usually the first symptom noticed. A period may be omitted from any one of several causes, as has been explained in Chap. II but in a healthy woman of the childbearing age, whose menses have previously been regular, the missing of two successive periods after intercourse is a strong indication of pregnancy.
2. Changes in the breasts. These also occur early. The breasts ordinarily increase in size and firmness, and many women complain of throbbing, tingling or pricking sensations and a feeling of tension and fullness. The breasts may be so tender that even slight pressure is painful. The nipples are larger and more prominent, while both they and the surrounding areolæ grow darker. The veins under the skin are more apparent and the glands of Montgomery larger. If in addition 97to these symptoms it is possible to express a pale yellowish fluid from the nipples of a woman who has not had children, pregnancy may be strongly suspected. But practically all of these symptoms may be due to causes other than pregnancy, and, in the case of a woman who has borne children, milk may be present in the breasts for months, or even years, after the birth of a child.
3. “Morning sickness,” as the name suggests, is nausea, sometimes accompanied by vomiting, from which many pregnant women suffer immediately upon arising in the morning. It varies in severity from a mild attack when the patient first lifts her head to repeated and severe recurrences during the day, and even into the night. More frequently, however, the discomfort passes off in a few hours. When the vomiting persists, it is termed “pernicious vomiting” and is usually accepted as a possible symptom of a reflex, toxic or neurotic condition, all of which will be discussed with the complications of pregnancy. Morning sickness may begin immediately after conception, but sets in as a rule about the sixth week and continues until the third or fourth month. It occurs in about half of all pregnancies and is particularly common among women pregnant for the first time. But on the other hand, it must be borne in mind that many non-pregnant women suffer from nausea in the morning; many women go throughout the entire period of gestation without any such disturbance, while others are entirely comfortable in the morning and nauseated only during the latter part of the day.
4. Frequent micturition. There is usually a desire to void urine frequently during the first three or four months of pregnancy, after which the tendency disappears, but recurs during the later months. The inclination may be due in part to nervousness, but is largely caused by pressure exerted by the enlarging uterus upon the bladder, and not to any functional disturbance of the kidneys, as is sometimes believed. Pressure on the outside of the bladder gives much the same sensation as is experienced when the bladder is distended with urine. After the uterus rises from the pelvic cavity into the abdomen, it no longer crowds the bladder, until it drops during the last month or six weeks, when it again presses upon this organ and cause a desire to void.
5. Increased discoloration of the pigmented areas of the skin, and also of the mucous membranes, is another early symptom of pregnancy. In addition to the deepened tint of the nipples and surrounding areolæ, the so-called linea nigra appears upon the abdomen, extending from the pubis toward the umbilicus. There are also the dark bluish or purplish appearance of the vulval and vaginal linings; the yellowish, irregularly shaped blotches which sometimes appear on the face and neck, known as chloasma: dark circles under the eyes and the striæ on the abdomen.
986. “Quickening” is the widely used term which designates the mother’s first perception of the fetal movements. It occurs about the eighteenth or twentieth week, and is regarded by some obstetricians as a positive and by others as merely a strongly presumptive sign of pregnancy. The sensation is likened to a very slight quivering or tapping, or to the fluttering of a bird’s wings imprisoned in the hand. Beginning very gently, these movements increase in severity as time goes on until they become very troublesome toward the latter part of pregnancy, amounting then to sharp kicks and blows. Women who have had children can usually be relied upon to distinguish between quickening and the somewhat similar sensation caused by the movement of gas in the intestines, but a woman pregnant for the first time may be deceived.
There are many other possible symptoms of pregnancy, but their value is very uncertain. Even the ones described above are not entirely dependable, but if two or more of them occur coincidently, they probably indicate pregnancy. Dr. Slemons sums it up by saying, “If, for example, menstruation has previously been regular and then a period is missed, the patient has good reason to suspect she is pregnant; if the next period is also missed and meanwhile the breasts have enlarged, the nipples darkened, and the secretion of colostrum has begun, it is nearly certain that she is pregnant; whether morning sickness and the desire to pass urine frequently are present is of no importance.”[2]
The probable signs of pregnancy are chiefly discoverable by the physician after careful examination. They also are numerous and uncertain, but there are four which are considered fairly trustworthy.
1. Enlargement of the abdomen, which is first in order of importance, is apparent about the third month. At this stage the growing uterus may be felt through the abdominal wall as a tumor which steadily increases in size as pregnancy advances. Rapid enlargement of the abdomen in a woman of child-bearing age, therefore, may be taken as fair, but not positive, evidence of pregnancy. But too much reliance cannot be placed in this sign, as the abdomen may be enlarged by a tumor, fluid or a rapid increase in fat.
2. Changes in the size, shape and consistency of the uterus which take place during the first three months of pregnancy are very important indications. These are discoverable upon vaginal examination, which shows the uterus to be more ante-flexed than normal, considerably 99enlarged, somewhat globular in shape and of a soft, doughy consistency. About the sixth week the so-called Hegar’s sign is perceptible through bimanual examination, the fingers of one hand being pressed deeply into the abdomen, just above the symphysis and two fingers of the other hand passed through the vagina until they rest in the posterior fornix, behind the cervix. The lower segment of the uterus, which may be felt between the finger tips of the two hands, is extremely soft and compressible. This sign, named for the man who first described it, is one of the most valuable signs in early pregnancy.
3. Softening of the cervix occurs, as a rule, about the beginning of the second month. In some cases, such as certain inflammatory conditions and in carcinoma, this sign may not appear.
4. Painless uterine contractions, called Braxton Hicks from their first observer, begin during the early weeks of pregnancy and recur at intervals of five or ten minutes throughout the entire period of gestation. The patient is not conscious of these contractions, but they may be observed during the early months by bimanual examination, and subsequently by placing the hand on the abdomen. One feels the uterus growing alternately hard and soft as it contracts and relaxes.
But all of the probable signs of pregnancy, like the presumptive symptoms, may be simulated in non-pregnant conditions; hence the appearance of any one of them alone may not be deeply significant. But two or more occurring coincidently constitute strong evidence of pregnancy.
The positive signs of pregnancy, of which there are three, are not apparent until the 18th or 20th week, and all emanate from the fetus.
1. Hearing and counting the fetal heart beat is unmistakable evidence of pregnancy. The sound of the fetal heart beat is usually likened to the ticking of a watch under a pillow. The rate is from 120 to 140 per minute, being about twice as fast as the maternal pulse. So long as its rhythm is regular, however, the rate may drop to 100 or increase to 160 beats per minute without being considered abnormal, or indicative of trouble with the fetus.
2. Ability to palpate the outline of the fetus is also a positive sign of pregnancy, if the head, breech, back and extremities are unmistakably made out through the abdominal wall.
3. Perception of active and passive movements of the fetus is accepted as a third incontrovertible sign of pregnancy. There is some difference of opinion concerning the value of “quickening” alone as a positive sign of pregnancy. But if the fetal movements are also perceptible by the obstetrician through the mother’s abdominal wall or 100by vaginal examination, there can be no doubt about the diagnosis. The movements felt by placing the hand upon the abdomen are termed active movements, while the passive movements result from internal or external ballottement. Ballottement is accomplished by giving a sharp or sudden push to the head or an extremity, and feeling it rebound in a few seconds to its original position. Passive movements may be felt early in the fourth month, and active movements after the 18th or 20th week.
A general understanding of the physiology of pregnancy is indispensable to an appreciation of the importance of observing the present-day teachings about the hygiene of pregnancy. Upon this, in turn, must rest intelligently administered prenatal care, one of the most important branches of obstetrics.
The physiology of pregnancy really represents an adjustment of the various functions of the maternal organism, which are altered to meet the demands made upon the mother’s organs by the body which is developing, growing and functioning within hers. These adjustments are in the nature of an emergency service, since they come into existence and operate only while needed, which is during pregnancy, and promptly disappear when the need for them ceases with the birth of the child. The mother’s body then begins to return to its normal, non-pregnant state, which, with the exception of the breasts, which function for nine or ten months, is accomplished in a few weeks.
But in addition to the normal changes in physiology in the course of pregnancy, there are frequently abnormal changes, too, which may be symptoms of grave complications. The detection of these symptoms, and the employment of treatment which they indicate, constitute one of the most valuable aspects of prenatal care.
Although, as might be expected, the alterations in the structure and functions of the maternal organism are most marked in the generative organs, there are definite changes in other and remote parts of the body as well. And there are adjustments in metabolism, which, though not wholly understood, are now widely recognized as important. It is pretty generally believed that as a direct, result of pregnancy, certain substances are created, 101possibly by the corpus luteum, which circulate in the blood and definitely influence the maternal functions. It is possible that a development of the present imperfect knowledge of these substances will result ultimately in the discovery of a blood reaction which will serve to diagnose pregnancy in an early stage.
At present, we know that, in spite of the creation of an infant body weighing upwards of seven pounds, a placenta weighing more than a pound, together with an increase of about two pounds in the weight of the uterine muscle, all in the short span of nine months, the expectant mother has to eat very little more during this period than she ordinarily does to maintain her own bodily functions. This suggests a highly developed economy in the use of nutritive material by maternal cells.
We also know that the mother excretes waste materials for the fetus and must assume that this requires an increased, or adjusted, functional activity of her excretory organs, the skin, lungs and kidneys. Moreover, the secretory activity of the previously inactive mammary glands, in spite of their remoteness from the pelvis, suggests a nervous or chemical stimulation, or both, which occurs only during pregnancy.
The changes in the uterus itself, however, are unquestionably the most marked that take place during the period of gestation. Those that relate to the lining have been described in a previous chapter. The change and growth in the muscle wall are amazing. New muscle fibres come into existence; those already there increase greatly in size and there is a marked development of connective tissue.
The actual substance of the uterus is so increased that it is converted from an organ weighing two ounces into one weighing two pounds. From a firm, hard, thick walled, somewhat flattened body in its non-pregnant state, the gravid uterus assumes a globular outline and grows so soft that the fetus may be felt through the walls.
During the first few months the uterine walls increase in thickness, but later they grow progressively thinner, until by the end of pregnancy they are only about 5 millimetres thick.
This early growth of the uterus is doubtless brought about by general systemic changes rather than by the presence of the 102contained embryo. Evidence of this is found in the case of tubal pregnancies when there is a definite enlargement of the uterus during the early weeks. After the third month, however, the growth of the uterus is apparently due to pressure which the growing fetus makes on the uterine walls.
The cervix does not enlarge as a result of pregnancy, but it loses its hard cartilaginous consistency, becoming quite soft, and the secretion of the cervical glands is much more profuse.
The changes in the vagina are chiefly due to increased vascularity. The blood vessels are actually larger, the products of the glands are greatly increased and the normal pinkish tint of the mucous lining deepens to red or even purple.
The most important changes in the tubes and ovaries is in their position because of their being carried up from the pelvis by the enlarging uterus into the abdominal cavity. Although they increase in vascularity, ovulation is ordinarily suspended during pregnancy.
The abdomen as a whole changes in contour as it steadily enlarges, and the skin and underlying muscles are somewhat affected as a result. The tension upon the skin is so great that it may rupture the underlying elastic layers which later atrophy and thus produce the familiar striæ of pregnancy, known variously as the striæ gravidarium and the linea albicantes. Fresh striæ are pale pink or bluish in color, but after delivery they take on the silvery, glistening appearance of scar tissue, which they really are.
In a woman who has borne children, therefore, we find both new and old striæ; those resulting from former pregnancies being silvery and shining, while the fresh tears are pink or blue. Striæ may be found also on the breasts, hips and upper part of the thighs, and as they are of purely mechanical origin, are not necessarily associated with pregnancy alone. They may result from a stretching of the skin by ascites, a marked increase in fat or an abdominal tumor.
The same distension that causes striæ sometimes causes a separation of the recti muscles. This separation, known as diastasis, is sometimes slight but frequently very marked, the space between the muscles being easily felt through the thinned abdominal wall.
103The umbilicus is deeply indented during about the first three months of pregnancy. But during the fourth, fifth and sixth months the pit grows steadily shallower, and by the seventh month it is level with the surface. After this it may protrude, in which state it is described as a “pouting umbilicus.”
The increased pigmentation at the umbilicus and in the median line is scarcely to be classified among the abdominal changes, as the skin elsewhere presents the same discolored appearance. The degree of pigmentation varies with the complexion of the individual, as blondes may be but slightly tinted while the discolored areas on a brunette may be dark brown, sometimes almost black.
The changes in the breasts during pregnancy were practically all included in the enumerated signs and symptoms of pregnancy. They increase in size and firmness and become nodular; the nipple is more prominent and together with the surrounding areolæ, grows much darker; the glands of Montgomery are enlarged; the superficial veins grow more prominent, and after the third month a thin, yellowish fluid can be expressed from the nipples. This fluid, called colostrum, consists largely of fat, epithelial cells and colostrum corpuscles and differs from milk, in its yellowish color, and in the fact that it coagulates like the white of an egg when boiled. The previously quiescent mammary glands develop very early in pregnancy an ability to select from the blood stream the necessary materials to produce a secretion. Colostrum is the product of their activity until about the third day after delivery, when milk appears.
Changes in the cardio-vascular system are among those which are not altogether understood, and it is still a moot question as to whether or not there is an actual increase in the amount of maternal blood during pregnancy. But results of the most recent investigations suggest that there is a definite increase in both the cells and the plasma. This increased amount circulating through the heart subjects it to a certain amount of strain, with the result that the organ is slightly hypertrophied and the pulse pressure is higher.
The respiratory organs do not show any marked alterations. The upward pressure of the enlarging uterus gradually shortens the height of the thoracic cavity, but if it grows sufficiently wide 104in compensation, there is no decrease in the capacity of the lungs. If this does not occur, the patient may suffer from shortness of breath. The larynx is sometimes reddened and edematous, a fact which explains the damaging effects which child-bearing may have upon the voice of singers.
Changes in the digestive tract during pregnancy are the morning sickness already described, and constipation. The latter is suffered by at least one half of all pregnant women, and is due chiefly to pressure of the uterus on the intestines, though impaired tone of the stretched abdominal muscles may be a factor. This condition is most troublesome during the latter part of pregnancy. There also may be gastric indigestion causing acidity, flatulence and heartburn, and intestinal indigestion giving rise to diarrhea and cramp-like pains. The appetite may be very capricious during the early weeks, and become almost ravenous later on.
Changes in the urinary apparatus include frequency of micturition mentioned among the symptoms of pregnancy.
The changes in the bony structures of the pregnant woman are characterized by partial decalcification. This is accounted for by the fact that the developing fetus requires a definite amount of calcium in the formation of its osseous structures, and unless the expectant mother absorbs an adequate quantity from her food, it must be extracted from the bones and similar structures, such as the teeth. Her bones and teeth accordingly grow softer, and we have the well-known adage, “for every child a tooth,” as well as the fact that fractures during pregnancy unite very slowly. There are also the softened cartilages which were referred to in connection with the anatomy of the pelvis. A part of the softening of the pelvic cartilages, however, is due to a temporarily increased blood supply. As will be explained in the chapter on nutrition, this partial decalcification of the mother is entirely unnecessary, and the newer knowledge of nutrition points the way to its prevention.
The skin changes consist chiefly in the appearance of striæ and the increased pigmentation to which reference has already been made. There is also an increased activity of the sebaceous and sweat glands and the hair follicles, the latter sometimes resulting 105in the hair becoming much more abundant during the period of gestation. Although the pigmented areas on the breasts and abdomen never quite return to their original hue, the chloasmata, sometimes called the “masque des femmes enceintes,” practically always disappear and leave no trace, a fact that is frequently a comfort to an expectant mother.
The carriage is somewhat affected during pregnancy because the increased size and weight of the abdominal tumor shifts the centre of gravity. In an effort to preserve an upright position the woman throws back her head and shoulders and finally assumes a gait that may be described as a waddle, particularly noticeable in short women.
Temperature changes are probably not caused by pregnancy per se, though some authorities believe that there is normally a slight elevation during the latter part of the day.
Mental and emotional changes are usually included among the alterations which occur during pregnancy, but the present status of psychiatry suggests that this may not be altogether true. It is a fact that many pregnant women show marked mental and emotional unbalance, but as yet there seems to be no evidence that these states are inherently due to pregnancy, though the same condition may recur in the same woman each time that she is pregnant.
We shall consider this important subject more at length in the chapter on mental hygiene, so it may be enough simply to say at this juncture that, in a sensitively strung or uncertainly poised woman, the state of being pregnant may be merely the last straw, so to speak, that upsets her equilibrium; and that some other experience, which would be an equal strain upon her slender ability to make adjustments, would result in exactly the same mental or emotional distortion, just as certain physical signs in pregnancy may be produced also in the non-pregnant state, and are not, therefore, necessarily inherent to the gravid state.
Changes in the ductless glands are in much the same category. Functional disturbances of these glands occurring at any time may give rise to great irritability, excitability or to other mental symptoms. A non-pregnant woman with even a very 106slight degree of hyperthyroidism, for example, may be noticeably unstable mentally or emotionally. Since there is evidently an inter-relation and inter-dependence of the functions of the ductless glands, and since ovulation, the function of one of these glands, is suspended during pregnancy, we can readily believe that other glands would undergo changes as a result. Alterations in the thyroid are particularly apparent as it becomes enlarged and more active in the majority of pregnant women, as does also the anterior lobe of the pituitary body. This increased activity may tend to compensate for the suspended function of the ovaries. But the alterations in the functions of the other glands, compensatory though they be in part, apparently produce much the same sort of nervous symptoms that they are capable of producing in a non-pregnant woman.
Taking the condition as a whole, pregnancy is usually characterized by an improved state of health. During the first few months there may be lassitude and loss of weight, but the latter part of the period is notable for an unusual degree of general well being and for an increase in flesh over the entire body, which may amount to as much as twenty-five or thirty pounds.
About fifteen pounds of the increased weight is lost at the time of labor and a still further reduction occurs during the succeeding weeks when the mother’s body returns approximately to its original condition. But it sometimes happens that the improved state of nutrition acquired during pregnancy becomes permanent.
CHAPTER VI. PRENATAL CARE. Instruction of the Mother, Examinations, and Observations. Importance of Prenatal Care. The Nurse’s Part. Personal Hygiene of Pregnancy. Excretions. Kidneys. Urine Tests. Skin. Bowels. Clothes: corsets, binders, shoes. Diet. Fresh Air and Exercise. Rest and Sleep. Care of the Breasts. Teeth. Travelling. Marital Relation. Common Discomforts during Pregnancy. Nausea and Vomiting. Heartburn. Distress. Flatulence. Diarrhea. Pressure Symptoms. Swelling of the Feet. Varicose Veins. Hemorrhoids. Cramps in the Legs. Shortness of Breath. Vaginal Discharge. Itching. Early Symptoms of Complications of Pregnancy: Toxemias, Premature Terminations, Hemorrhage.
CHAPTER VII. MENTAL HYGIENE OF THE EXPECTANT MOTHER. Common Causes of Mental and Nervous Breakdown during Pregnancy. Nurse’s Attitude.
CHAPTER VIII. PREPARATION OF ROOM, DRESSINGS AND EQUIPMENT FOR HOME DELIVERY.
CHAPTER IX. COMPLICATIONS AND ACCIDENTS OF PREGNANCY. Premature Terminations of Pregnancy. Definition of Terms. Abortions. Causes: Abnormalities of Fetus; Abnormalities in the Generative Tract; Acute Infectious Diseases; Mental or Emotional Stress; Physical Shocks. Premonitory Symptoms. Prevention, Treatment, and Nursing Care of Threatened, Incomplete, and Complete Abortions. Missed Abortion. Therapeutic Abortion. Clerical and Legal Aspects of Abortion. Criminal Abortion. Premature Labor: Causes, Treatment and Nursing Care. Ante-partum Hemorrhage. Placenta Prævia: Cause, Symptoms, Treatment and Nursing Care. Premature Separation of a Normally Implanted Placenta: Cause, Symptoms, Treatment and Nursing Care. Toxemias of Pregnancy. Pernicious Vomiting of Pregnancy. Symptoms, Treatment and Nursing Care of Reflex Vomiting, Neurotic Vomiting, Toxemic Vomiting. Pre-eclamptic Toxemia: Symptoms, Prevention, Treatment and Nursing Care. Eclampsia: Symptoms, Treatment and Nursing Care. Nephritic Toxemia: Cause, Symptoms, Treatment and Nursing Care. Acute Yellow Atrophy of the Liver: Cause, Symptoms, Treatment and Nursing Care. Other Important Complications of Pregnancy: Syphilis. Heart Lesions. Pulmonary Tuberculosis. Thyroidism. Pyelitis. Gonorrhea.
The day is long since past when the obstetrician’s concern for his patient began when she went into labor. The obstetrician of to-day watches and cares for his patient throughout pregnancy, for he knows that by so doing he greatly increases her chances of surviving the ordeal of childbirth, and the baby’s prospect of living through that perilous first year.
Although many conditions that result in invalidism or death occur during labor or the puerperium, they have their beginnings during pregnancy. Their prevention, then, or early recognition, followed by prompt and efficient treatment, will avert many of the dreaded complications and emergencies associated with childbearing.
In order to prevent these disasters it is necessary to supervise the expectant mother and care for her from early in pregnancy—from the time of conception if possible—until the onset of labor, and this is prenatal care. It may be divided into instruction, examinations and observations, as follows:
1. a. Teaching the expectant mother the principles of personal hygiene, as especially adapted to meet her needs, and helping her to adopt them;
b. Describing to her the more apparent, normal changes of pregnancy which she is likely to notice and perhaps not understand, and also the common symptoms of complications which she may detect and should report;
2. The doctor’s preliminary examination, early in pregnancy, comprising a study of the size, shape and proportions of the pelvis, and later their relation to the size and mouldability of the baby’s head; a Wassermann test for syphilis; urinalysis and measuring the blood pressure. In addition to these, a complete physical survey is made, consisting of examinations of the heart, lungs, breasts, abdomen, a vaginal smear for gonorrhea, and the patient’s height, weight and temperature;
3. Constant watching for early symptoms of the complications 112of pregnancy, with speedy treatment of such symptoms when they appear, and relieving the common discomforts of pregnancy; making observations upon the presentation and size of the fetus, later in pregnancy, in order to plan ahead of time for the delivery, if the patient’s condition makes this advisable.
Prenatal care of this character is essentially preventive for both the mother and the new-born baby.
We gain a faint impression of what it may prevent when we learn that year after year, about 17,000 young women die in the United States from causes associated with childbirth, which are known to be largely preventable (during 1918 the number was 23,000); and that each year about 112,000 babies are born dead, and 100,000 of those born alive perish during the first month of life, also from causes which are largely controllable.
But 17,000 dead mothers and 200,000 dead babies, most of whom might have lived, are not all that enter into the annual erection of this national monument to neglect. There are also the unrecorded and uncounted victims of little or no obstetrical care who have had too much vigor to succumb completely and die, and who, therefore, live on through years of wretched invalidism. Sometimes, it is true, their disability is slight, so slight as to be uninteresting, and of no statistical importance. But to the woman herself, who must resume the functions of mother, homemaker, wife and general utility person, the disability may be enough to make life endlessly dreary and discouraging. And yet, she is perhaps only just below the physical level upon which she could live her life with joy and eagerness; and proper care when the baby came would have left her upon that level.
The effect of the mother’s impairment reaches far beyond her own invalidism, for such women are not as well able to rear and care for their children satisfactorily as are fresh, buoyant mothers. Whatever makes for good obstetrics, therefore, makes for a better race, and, as we shall see later, measures that tend to improve the health of the race tend to lessen the hazards of childbearing.
Ideal prenatal care, then, would really begin during the expectant mother’s own infancy, but we must be content here with 113a description of the care that is advisable, and desired, for expectant mothers from the beginning of pregnancy.
There is considerable difference of opinion among physicians concerning the stage of pregnancy at which it is desirable to see the expectant mother for the first time, and the frequency of subsequent observations. But the growing tendency is for the doctor to see his patient as early as possible, for the preliminary examination, and to follow a fairly uniform routine in the kind and frequency of subsequent observations, and in the personal hygiene which the patient is advised to adopt.
Thus, it has become generally customary to see the patient, take her temperature, pulse and blood pressure and make a urinalysis once a month during the first half of pregnancy, and then every two weeks until the onset of labor, or possibly once a week toward the end. These periodic examinations keep the physician constantly informed about his patient’s condition, and frequently disclose very early symptoms of a complication which is easily amenable to treatment at that stage, but which might prove serious if allowed to progress unchecked. Albumen in the urine, for example, or an increase in the blood pressure, in a woman who had no other symptoms, would suggest the advisability of watching for further symptoms of toxemia; while an elevation of temperature, even though the patient was not uncomfortable, might lead to the early discovery of tuberculosis, pyelitis or some other infection not otherwise apparent.
It is this stitch in time that means so much to the pregnant woman and her expected baby.
But the most painstaking obstetrician requires the co-operation of his patient in innumerable little ways, if she is to have the fullest benefits of his skill; for it is not so much what the doctor advises that counts as how the patient lives.
It is at this point that nurses are more and more being given opportunity for immensely gratifying service. A private patient who is in the care of an obstetrician is, of course, supervised and instructed by her doctor. But there are other patients—women who cannot afford this individual care, but who need care none the less. And it is these expectant mothers that nurses are helping the doctors to instruct in the principles of right living, 114and are watching for danger signs, through visiting nurse societies, out-patient departments of hospitals and through prenatal clinics.
The character and extent of the instruction and supervision given by the nurses is, of course, decided by the medical board of her organization, and is often affected by the conditions under which the work is conducted. The nurses in a rural community, for example, may take blood pressures and test urine for albumen, while in cities, rich in doctors and medical institutions, these observations might not be among their duties.
In addition to this definite relation to expectant mothers, nurses are meeting them, unofficially and informally, at every turn; women who are needing, but not receiving, care from a doctor or an organization; women who are puzzled or troubled over their condition, but do not know where nor how to obtain advice; women who could employ a physician but do not appreciate the importance of his care.
Every nurse should recognize it as her duty to advise an unsupervised, pregnant woman to place herself under medical care, no matter under what conditions she meets her.
In the discharge of her duties, the nurse will sometimes need no little ingenuity to adapt the routines of prenatal care, as prescribed by her organization, to the mentality, traditions and varied demands of the daily lives of her patients. But this will have to be done, for though in a general way the needs of all expectant mothers are the same, their circumstances and personalities are infinitely varied.
It may require undreamed-of tact and resourcefulness to convince a patient that details of care, which seem wholly unrelated to her or her baby’s welfare, will actually increase their chances for life and health. For this reason, it is of almost prime importance that the nurse win her patient’s friendship and confidence. She will then scarcely realize that she is being taught, but will do and continue to do as she is advised, because of an almost insensible reliance upon the judgment and sincerity of her counsellors.
It is not the single examination of a specimen of urine that counts, nor the exercise taken with pleasure and enthusiasm 115during the first few days of its novelty. It is not the rest, fresh air nor proper food, taken according to rule for a week or two, that will keep her fit. It is the aggregate and repetition of the infinite number of details that make up the expectant mother’s mental and physical life during twenty-four hours in each day, seven days a week, throughout forty long weeks, that grow longer and more monotonous as pregnancy advances; it is the mosaic that she makes out of the minutiae of her daily life that counts. And paradoxical as it seems, she must shape her days to meet her own and her baby’s needs with such steady persistence that she finally lives them almost unconsciously of what she is doing, and also without introspection.
Obviously, then, the expectant mother’s mental attitude is of considerable importance.
She should in general continue the diversions, work and amusements that she is accustomed to and enjoys, if they are not contra-indicated; cultivate a cheerful, hopeful frame of mind; guard against being self-centred and over watchful of symptoms, and at the same time not adopt the dangerous habit of uncomplainingly ascribing to pregnancy all of the discomforts and unfamiliar conditions which may arise. In short, to forget that she is pregnant in so far as that is consistent with the care that she should take of herself.
She should understand that childbearing is a normal function, but, like other normal functions, may become abnormal if neglected; and that a sick pregnancy is not a normal one.
In connection with the patient’s mental attitude and her anxieties, the nurse may be of great comfort in helping to dispel superstitions and the widely credited and depressing beliefs concerning maternal impressions.
After one has traced the development of the human body in the uterus, and even faintly understood its growth and method of nourishment, it is impossible to believe that the mother’s thoughts or experiences could in any way deform or mark her child, or alter its sex. That the mother’s “reaching up,” for example, could slip the cord around the unborn baby’s neck is manifestly absurd, as well as the previously mentioned superstitions about the eight-month baby’s slender chances for survival.
116But superstitions are always fondly cherished, for, as Gibbon tells us, “the practise of superstition is so congenial to the multitude, that if they are forcibly awakened, they still regret the loss of their pleasing vision.” We can scarcely wonder however that even intelligent and educated people hold utterly improbable beliefs about pregnancy, for the most fanciful of them are quite as easy to believe as the thing that we know actually occurs—the development of a human body from a single cell.
These fanciful beliefs, however, are sometimes serious matters to the young woman who is traveling, day by day, toward a great and mysterious event, and they should not be laughed to scorn, but explained away seriously and with sympathy. She may be told quite simply, that after conception she gives her baby only nourishment; that the baby’s connection with her body is through the cord and placenta, in neither of which are there nerves; and that even if the blood could carry mental and nervous impulses, which it cannot, the maternal and fetal blood never come in actual contact with each other. A tale which she has heard about a woman who saw something distressing and later gave birth to a marked child may cease to worry her if she is reminded of the innumerable babies, beautiful and unmarked, which are born to women who have had equally shocking experiences. It is scarcely probable that any woman lives through the ten months of pregnancy without seeing, hearing or thinking things that would disfigure a baby if maternal impressions could produce such results, and yet newborn babies are very rarely blemished. Although the ultimate causes of marks and deformities of the fetus are not definitely known, they are probably to be found in faulty development very early in the embryonic life, and, therefore, are not preventable.
In coming to the expectant mother’s personal hygiene, we find that an understanding of the physiology of pregnancy almost of itself indicates what this hygiene should include. We shall take it up in detail, however, and describe what is at present considered a reasonable outline of the routine desired for the average pregnant woman, who is found by careful examination 117to be normal and free from complications, and needing only to keep well. But, as has been said, and must be oft repeated, the ideal routine cannot be deposited en bloc upon all expectant mothers. It must be adjusted to the individual and to her circumstances.
Excretions. Although, as has been explained previously, the pregnant woman does not have to eat for two, she does have to eliminate the waste and broken-down products from two bodies, through her own excretory organs: the kidneys, skin, lungs and bowels. True, the amount of the baby’s ash is not great, but is of such a character that its elimination is important and increases the strain upon the maternal excretory apparatus.
Kidneys. One of the most important factors in prenatal care is promoting the function of the kidneys and watching their output. It is probably more true of the kidneys than of any other organs that a slight abnormality which would not give trouble at other times may, if neglected during pregnancy, produce very grave results. The amount of urine passed in twenty-four hours should be measured, and a specimen prepared, once a month during the first half of pregnancy and every two weeks afterward. If less than three pints are passed the patient should know, without further instruction, that she is not taking enough water and must take more. And so it is the nurse’s duty, in this connection, to convince her patient of the importance of drinking an abundance of water, and periodically measuring her urine and sending specimens to the doctor for examination.
She is very likely to follow such advice if she is told that by so doing she will help to prevent convulsions, for most women know of this complication and dread it.
In preparing a specimen, a covered or corked receptacle which is large enough to hold the voidings for twenty-four hours, must be thoroughly washed and scalded; in it should be collected the total amount of urine voided during twenty-four hours and kept in a place that is cool enough to prevent putrefactive changes. The additional precaution of putting a teaspoonful of chloroform into the receptacle is wise and does not injure the specimen. The patient should be instructed to empty her bladder at any designated hour, and then keep all urine voided from that time 118until the corresponding hour on the following day. The urine should be shaken so as to mix thoroughly the different voidings, and six or eight ounces poured into a bottle which has been washed and scalded, carefully corked and labelled with the date, patient’s name, address and the total amount for twenty-four hours.
If the nurse is called upon to test for albumen, either of the following will serve, unless the doctor specifies a test which he prefers:
Heat and acetic acid test: Fill a test tube about half full of urine and gently boil the upper part in a flame; add five drops of 2% to 5% acetic acid and again boil gently. The presence of albumen is shown by a white cloud in the upper part of the urine.
Esbach’s test: Fill a test tube half full of urine; add eight or ten drops of Esbach’s Solution. The presence of albumen is shown by a white flocculent precipitate in the upper part of the urine.
Skin. Under ordinary conditions, the skin serves as a protective covering for the body, helps to regulate the body temperature and acts constantly as an excretory organ. This last function is performed by the sweat glands which open upon the surface of the body, and we are told that there are some twenty-eight miles of these minute, tube-like structures in the skin. These glands should be, and usually are, constantly active and they daily pour upon the surface of the body an oily substance that lubricates the skin and something over a pint of water containing waste matter, that is inimical to health if retained in the body. We are not aware of this constant excretion of fluids, which, therefore, is termed “insensible perspiration,” but it continues even in cold weather and must not be interrupted if health is to be preserved. If the oil, dust, particles of dead skin and the waste material left by dried perspiration are allowed to remain upon the surface of the body, they will clog the pores and gland openings and thus interfere with their functions. The removal of this material, then, is an imperative health measure. This is done automatically, in part, for the fluid evaporates, and much of the solid matter is rubbed off on the clothing. But the most important aids to the skin’s activity are the drinking of 119plenty of water, deep breathing, exercise and warm baths; baths serving the double purpose of removing waste matter already on the surface, and stimulating the glands to increased activity in giving off still more.
This explains the importance to the expectant mother of thorough and regular bathing, and of keeping her body evenly warm. Most doctors advise a warm, not hot, shower or tub bath every day, with soap used freely over the entire body, followed by a brisk rub. The best time for this warm, cleansing bath, as a rule, is just before retiring, as it is soothing and restful and tends to induce sleep. Very hot baths are fatiguing, particularly during pregnancy, and should never be taken except with the doctor’s permission; but cold baths usually may be continued throughout pregnancy if the patient is accustomed to them and reacts well afterwards. Under these conditions the morning cold plunge, shower or sponge is beneficial, as it stimulates the circulation and thus promotes the activity of the skin. Some doctors forbid tub bathing of any kind after the seventh month, on the ground that as the patient sits in the tub her vagina is filled with water, which may contain infective material. Should labor occur shortly afterward an infection might result. As the patient is heavy and somewhat uncertain on her feet, there is also the danger of her slipping and falling while getting in or out of the tub.
Other doctors permit tub baths throughout pregnancy, up until the onset of labor; while as to hot foot baths, there seems to be no reason for or against them at any time during the nine months.
Bathing in a quiet stream or lake is apparently harmless, but sea bathing, if the surf is rough, is inadvisable because of the impact of the waves upon the abdomen and the general violence of the exercise.
The importance of keeping the body evenly warm throughout pregnancy cannot be overemphasized, for a sudden chilling or wetting may so check the excretory function of the skin as to throw a greater burden upon the kidneys than they can meet, in their effort to eliminate the skin’s share of the body waste. Accordingly, a single chilling will sometimes be enough to precipitate 120an eclamptic seizure. This may be one reason why we see eclampsia more frequently during cold weather or after a sudden drop in the temperature after warm or mild days.
Bowels. The bowels, also, eliminate a certain amount of toxic material and if they do not move thoroughly at least once a day, deleterious substances are absorbed into the system and an extra tax is placed upon the kidneys in an attempt to excrete them.
Unhappily, a large proportion of pregnant women suffer from constipation, particularly during the later weeks, though women who have always had a tendency of this kind may have trouble from the very beginning of pregnancy. Sluggish peristalsis, due to pressure by the enlarged uterus upon the intestines, is probably the prime cause, though impaired tone of the stretched abdominal muscles also may be a factor.
The bowels should move regularly every day, and to this end the patient should regularly attempt to empty them, immediately after breakfast usually being the best time. The importance of regularity in making the attempt cannot be overemphasized, even though the bowels do not always move.
Exercise, the intake of an abundance of fluids, eating fresh fruit, coarse vegetables and bulky cereals, such as bran, to stimulate peristalsis, and drinking a glass of hot or cold water upon retiring and arising are all laxative in their effect. As the regular use of enemata only tends to lessen intestinal tone, they should not be employed unless ordered by the doctor; nor should the patient take cathartics without the doctor’s order. But she may safely increase the amount of her fluids and the bulk of her food, in order to regulate her bowels, and may also take senna and prunes cooked together. A simple way of preparing prunes for this purpose is to pour a quart of boiling water over an ounce of senna leaves and allow it to stand for about two hours. A pound of well washed prunes should soak over-night in this infusion, which has been strained, and the combination cooked until tender. They may be sweetened with two tablespoons of brown sugar, and the flavor improved by adding a stick of cinnamon or slice of lemon while they are cooking. Half a dozen of these prunes, with some of the syrup, may be taken at the evening 121meal to start with, and increased or decreased in number as necessary.
Clothes. The chief purpose of clothes under all conditions is to aid in keeping the body warm, thus helping to preserve an even circulation and the activity of the sweat glands. As has been pointed out, this is of especial importance during pregnancy. The expectant mother’s clothes should be not only sufficiently warm, but they should be equally warm over the entire body. They should be light and porous, and fairly loose, so as not to interfere with the circulation or other body functions. There must be no pressure on chest or abdomen; no tight garters, belts, collars or shoes.
The patient’s clothes, like every other detail in her care, will have to be adapted to her environment and mode of living. If her house is well and evenly heated during the cold months, she may quite safely dress lightly while indoors; if it is not, she should be advised to wear underwear with high neck, long sleeves and drawers, both indoors and out, except when the weather is warm enough to induce free perspiration. At all times, however, the warmth of her clothing must be adjusted to the temperature of the home, the climate and to the state of the weather.
Bearing in mind the importance of diversion and amusements, it becomes apparent that in addition to the hygienic qualities mentioned, the expectant mother’s clothes should be as pretty and becoming as is consistent with her circumstances. She is much more likely to go about and mingle with her friends if she is fortified with the consciousness that she is becomingly and well dressed. Which, of course, is not peculiar to pregnant women.
The expectant mother’s clothes should be so made that their weight will hang from the shoulders instead of from the waistband.
And that brings us to the question of corsets, one of the most discussed garments in her wardrobe. Women who have not been accustomed to wearing corsets will scarcely feel the need of adopting them during pregnancy, except perhaps during the later weeks when the heavy, pendulous abdomen needs to be supported for the sake of comfort. This is particularly true of 122women who have borne children and whose flaccid abdominal walls give but poor support to the uterus.
Women who have been wearing comfortable, well-fitting corsets probably will not feel the need of making a change until the third or fourth month. By this time the uterus has pushed up out of the pelvis into the abdomen and accordingly the corsets must be so constructed that they will accommodate themselves to an abdomen that is steadily increasing in size and also changing in shape; will provide support for both abdomen and breasts and still not compress nor disguise the figure. To be entirely satisfactory in their adjustability, the maternity corsets must be made of very soft material and have elastic inserts and side, as well as front or back lacings. They should extend well down in front and fit snugly over the hips. The upper part may be fitted with adjustable shoulder-straps that will support the breasts and help to suspend some of the abdominal weight from the shoulders; but at the same time will not interfere with the development of the breasts nor compress the nipples. Many women find great comfort in wearing a short-waisted maternity corset and a brassiere.
The front-lace corset is usually found to be the most satisfactory, for the patient may lace it from below upward while lying on her back. This enables her to draw it in snugly about the hips, below the abdomen, and adjust the garment to the abdominal curve so as to really support, without compressing the uterus. Other excellent corsets lace both front and back and are capable of very comfortable adjustments. If the nurse clearly understands the purpose of a maternity corset, she will be able to explain to her patient why the same style as she ordinarily wears, no matter how large, will not be satisfactory during pregnancy, and may be even harmful.
Even a properly fitting maternity corset may become uncomfortable during the last few weeks of pregnancy, and have to be replaced by an abdominal supporter of linen or rubber. And when this stage is reached, even the woman who has worn no corsets may be made more comfortable by adopting such a support, particularly at night. There are many admirable binders on the market, or the nurse and patient may fashion some such an one as is shown in Figs. 34, 35, 36 and 37. Comfortable and inexpensive stocking supporters, which meet all practical requirements, may be made by the patient from tapes or strips of muslin. (Figs. 38 and 39.)
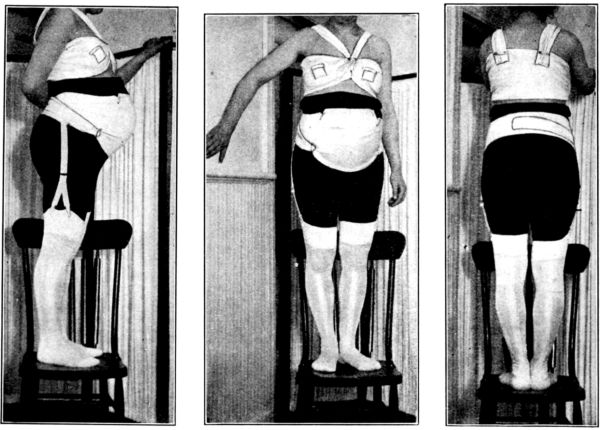
Figs. 34, 35, and 36.—Front, side and back views of home-made binder for supporting heavy, pendulous abdomen during later weeks of pregnancy. It is adjusted as the patient lies down, the ends being crossed in the back and pinned to the lower margin of the front, thus giving additional support.
Also breast-binder made of a straight strip of soft cotton material, 10 or 12 inches wide and 2 yards long. This is crossed in front and held with safety pins, the ends being carried over the shoulders and pinned to the back of the binder. It should be snug below the breasts but loose over the nipples. The openings over the nipples show how this binder may be used to support the breasts of the nursing mother. (From photographs taken at the Maternity Centre Association, New York.)
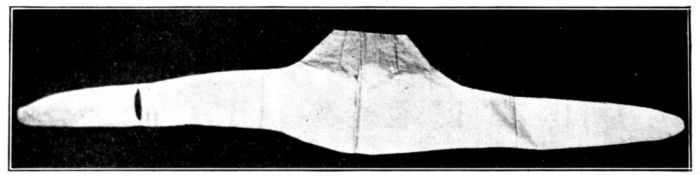
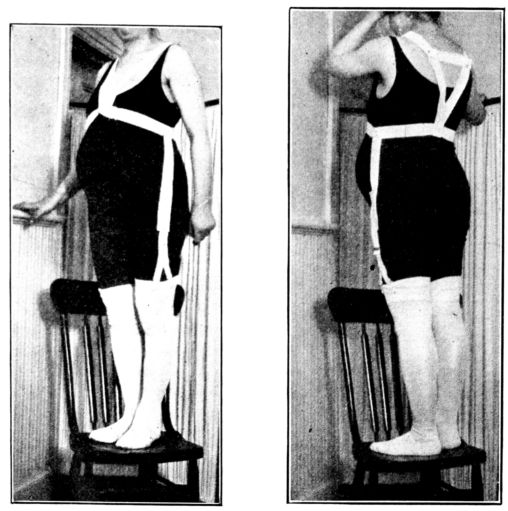
Figs. 38 and 39.—Front and back view of home-made stocking supporters made of webbing or 1–inch strips of muslin and a pair of child’s side garters. The straps are sewed together in the back, but pinned in front to permit adjustment as the abdomen enlarges. (By courtesy of the Maternity Centre Association, New York.)
The expectant mother’s shoes also merit considerable attention 125and thought. Her feet are larger than usual because they are likely to be somewhat swollen during the latter part of pregnancy, and the increased weight of her body tends to spread them. This added weight also increases the strain put upon the arch and flat foot is a not infrequent result, unless the arch is well supported. Another reason for the need of proper shoes is that, as pregnancy advances, the body’s centre of gravity changes. The pregnant woman becomes unstable on her feet and needs low, broad, firm heels. They need not necessarily be flat at first, if the patient has been accustomed to wearing moderately high ones, for the sudden lowering of the heels may injure her arches. High French heels, of course, should be avoided because they not only increase the difficulty and discomfort of walking but cause backache, as well, by forcing a posture that adds to the pressure on the lower part of the abdomen. They also increase the risk of turning the ankles, tripping and falling.
The patient’s shoes should be an inch longer than those she ordinarily wears; they should have broad toes and fit snugly over the instep, in spite of being large. If her shoes are not comfortable the expectant mother will tire easily and tend to take less exercise than she should.
Diet.—It is advisable for both nurse and patient to understand, and keep clearly in mind, the purposes which are served by the food intake of the expectant mother, and what foods and practices will defeat, and what will accomplish these purposes. Her food should provide nourishment, as under ordinary conditions; it should promote the functions of her skin, kidneys and bowels, because of the waste from her own and her baby’s body which she must excrete; it should be adequate to build and nourish the baby’s body without drawing materials from the mother’s own tissues. Moreover, proper food during pregnancy is an essential factor in preparing the mother to nurse her baby, which is as important as nourishing the fetus in utero.
In order to accomplish these various ends the patient must not only eat suitable food, but she must digest and assimilate it. This requires that she sedulously guard against overeating, constipation and indigestion of any kind. Indigestion may be 126avoided during pregnancy exactly as it is at other times, by eating proper food; by cultivating a happy frame of mind; by exercise, fresh air, adequate rest and sleep.
If accustomed to a fairly simple, well-balanced, mixed diet, the average expectant mother will need to make little or no change, excepting to make her evening meal light if it has been a hearty one; for she uses her nutritive material with surprising economy and does not have to “eat for two,” as is so commonly believed. It is a safe general principle that an amount and kind of food that keeps the expectant mother, herself, in a state of health and good nutrition, is favorable to satisfactory development of the fetus until the latter part of pregnancy.
She will probably be able to understand why this is true if it is explained that her baby gains nine-tenths of his weight after the fifth month, and one-half of his weight during the last eight weeks of pregnancy; also that if she takes too much food, the excess is stored up in both her own and the baby’s tissues; if too little, the fetus is nourished and her body deprived.
It is very unwise for the mother to diet with the idea of keeping the child small, and thus make labor easy, unless she is so ordered by her physician. In general, it is the size of the fetal skull that makes labor easy or difficult, and not the amount of fat distributed over the child’s body. And if the patient cuts down the minerals in her diet to make the fetal bones soft, and thus increase the compressibility of the skull, the fetus will extract lime from her bones and teeth, so that the only effect is upon herself.
The expectant mother’s meals should be taken with clock-like regularity, eaten slowly and masticated thoroughly. Three meals a day will usually suffice during at least the first half of pregnancy. The possible need for slight additional food after that may be supplied more satisfactorily by lunches of milk, cocoa or broth and crackers or toast, between meals and upon retiring, than by taking larger meals. But if the patient has a tendency to nausea, early in pregnancy, she will often be able to control it by taking a little food regularly five or six times daily, instead of the usual three meals.
127In general the expectant mother should eat an abundance of fruit and vegetables, taking at least some uncooked fruit and a green salad, daily, and making sure that her food contains a good deal of residue, such as is provided by fruit and coarse vegetables. This residue increases the bulk of the intestinal contents, which stimulates peristaltic action and thus helps to overcome the tendency toward constipation. As fat is less easily digested, and more likely to cause nausea during pregnancy, than carbohydrates, it is better for the patient to eat no more fat than usual, but to supply the additional energy needed after about the sixth month, by taking a little more starch. But after all, only a slight increase is needed, and this chiefly during the last three or four weeks.
It is of the greatest importance that every pregnant woman drink an abundance of fluid, to act as solvent for her food and waste material, and stimulate the activity of her kidneys, skin and bowels. She needs about three quarts daily, and most of this should be water, the remainder consisting of milk, cocoa, soup, and other liquids.
Alcohol should not be taken under any circumstances, except upon a doctor’s order, while tea and coffee, if taken at all, should be used with moderation. The patient should be advised to avoid fried food, pastry, rich desserts, rich salad-dressings and any other food which would ordinarily disagree with her. In fact any article of food that disagrees with her in a non-pregnant state should be avoided during pregnancy, no matter how valuable it may be as nourishment to the majority of people.
On the other hand, it sometimes happens that an article of food which is likely to disagree with other people will be easily digested by the pregnant woman, and if it adds to the pleasure of her meals should not be taboo, for the enjoyment of one’s meals promotes digestion. So-called “cravings” are not as common in fact as they are in rumor, but the expectant mother may have a capricious appetite and display strange likes and dislikes for certain dishes, possibly because of her tendency to be nauseated.
The average pregnant woman with no symptoms of complications will be able to supply her needs, and at the same time 128keep within the bounds of safety if she selects her diet from such groups as the following:
Animal Foods.—Milk and eggs are the most satisfactory, but for the sake of variety, and to tempt her appetite, she will usually be allowed to have fish, the various kinds of shell fish, beef, lamb, chicken or game rather sparingly, preferably only once a day. Pork, veal, and goose should be avoided as a rule, and particularly by women with whom they ordinarily disagree.
Soups.—Thin soups and broths have little food value, but, because of their appetizing flavor and aroma, are an aid to digestion, and frequently will stimulate a flagging appetite and prompt the patient to eat and assimilate more than she would without them. Cream soups and purées obviously have a high food value, and, like thin soups and broths, also supply a definite amount of fluid which the patient must have.
Vegetables.—The group of vegetables usually designated as “leafy” are of even greater importance to the expectant mother than they are to the average person. Of these, she may safely eat onions, asparagus, celery, string beans, spinach, and make a point of taking a green salad, such as lettuce, cress, or romaine, at least once daily. Sweet potatoes, white potatoes, rice, peas, Lima beans, tomatoes, beets and carrots may also be eaten with safety as a rule, but cabbage, cauliflower, corn, egg-plant, Brussels sprouts, parsnips, cucumbers, and radishes should be taken with great caution and avoided altogether if they cause flatulence or any kind of distress.
Fresh Fruits.—A necessary part of the diet is fresh fruit, and among those fruits which are both beneficial and harmless are apples, peaches, apricots, pears, oranges, figs, cherries, pineapple, grapes, plums, strawberries, raspberries, blackberries, and grapefruit. These are more likely to be laxative if eaten alone, as before breakfast and at bedtime. Cooked fruits are also valuable articles of diet, but are probably less laxative than raw fruit. Some of the citrus fruits, oranges, grapefruit and lemons, should be taken daily because of their antiscorbutic properties.
Cereals.—For their nourishing and laxative qualities, cereals are important, and their food value is increased by the milk and cream which are usually taken with them. Cooked cereals should invariably be cooked longer than the usual directions suggest. Bran, eaten alone, as a cereal or in combination with other grains, is an excellent laxative.
Breads.—Graham, cornmeal, whole wheat and bran bread are all good. In general the expectant mother will be on the safe side if she eats sparingly, if at all, of very fresh or hot breads and hot cakes.
Desserts.—Desserts are very important for they add to the attractiveness of most people’s meals, and if wisely chosen and properly 129made, may supply a good deal of easily digested nourishment. They may include, in addition to fresh and cooked fruits and preserves, ice-cream, a wide variety of custards, creams and puddings made largely of milk, eggs, and some ingredient to give substance and firmness, such as gelatine, cornstarch, rice, tapioca, farina, arrow-root and similar materials.
Fresh Air and Exercise. If the nurse has become aware of the value of promoting all of the normal physiological processes of the pregnant woman, she already realizes how important are fresh air and exercise to the patient and her expected baby.
The average individual uses every minute the oxygen contained in four bushels of air, and since the pregnant woman takes in through her lungs the oxygen for both herself and the baby, she must have an adequate quantity of constantly changing air to supply at least this amount. She should spend at least two hours of each day in the open air. If the weather is so stormy or severe as to make it undesirable for her to go out from under cover, because of the danger of getting wet or chilled, she may wrap up well and take her airing on a protected porch or in a room with all of the windows wide open. But this is only a part of it, for the air in her house, or rooms, must be kept fresh all day by being constantly changed; this requires a steady inpouring of fresh air and outpouring of stale, vitiated air.
A very good way to accomplish this is to have one or more windows open slightly, top and bottom, all the time. But there must be no sudden changes of temperature, nor drafts, for fear of chilling the patient’s skin. At night she should sleep in a room with the windows open, taking care to be well protected by light, warm coverings.
Each detail of the expectant mother’s daily routine seems to be more important than the last. And so when we come to the question of regular outdoor exercise we almost think that whatever else may be neglected, this is indispensable, since it promotes digestion, stimulates the functions of the skin and lungs; steadies the nerves, quiets the mind and promotes sleep. And more than that, walking, which is probably the most satisfactory form of exercise, also strengthens some of the muscles that are used during labor. But exercise is downright injurious if continued to the point of fatigue, no matter how little has been 130taken. Each woman must be a law unto herself in this matter, therefore, and must be impressed with the importance of stopping before she is tired. She should start by walking only a short distance, increasing gradually until she is able to walk possibly as much as an hour in the morning and an hour in the afternoon, if she can do so without fatigue.
All violent exercises and sports are of course to be avoided, particularly swimming, horseback riding, and tennis. While motoring and carriage riding are pleasant diversions, they cannot be classed as exercise. They should be taken only in comfortable vehicles and over smooth roads, so that there will be no jarring nor jolting, and the patient should not do the driving herself.
A certain amount of exercise, in the shape of light housework, may be taken indoors. It is distinctly beneficial, if not continued to the point of fatigue, both because of the exercise which it provides, and also the diversion and interest, for these promote mental and physical health. But this indoor exercise must not interfere with, nor to any degree replace, the daily exercise out of doors; nor must it include heavy work, such as washing, sweeping, heavy lifting, running a sewing machine by foot nor much running up and down stairs. However, the amount and kind of work which a woman may comfortably and safely do are so related to what she has been accustomed to, that it is not possible to offer more than general suggestions, which will help in the planning for each individual. All patients will do well to moderate their activities at the time when they would ordinarily menstruate.
There are patients to whom massage and gymnastics are beneficial during pregnancy, when for some reason the out-of-door activities are contra-indicated. This might be true of a patient with heart trouble, for example, or one who is being kept in bed to avert an abortion, and accordingly is a matter which must be entirely in the doctor’s hands.
Rest and Sleep. When we studied the bony structures of the female body, we found that as the abdominal tumor of pregnancy increased in size and weight, the body’s centre of gravity 131changed and the pregnant woman was required to make a constant, though unconscious effort to stand upright. This is probably one reason for the fatigue which expectant mothers so often feel without apparent cause, and for the fact that they are likely to tire rather more easily than usual.
Accordingly, the patient may have to rest frequently during the day, in order to avoid the ill effects of fatigue. She should work and exercise in short periods rather than long, always lying down when tired, and for an hour or two after the noon meal. She must be particularly careful not to be over-active, nor to overexert herself at the time when menstruation would occur were she not pregnant, for fear of bringing on an abortion. This precaution is particularly important during the first four months, the period when abortions occur most frequently.
Since eight hours’ sleep is usually considered necessary to keep the average person in good condition, the pregnant woman cannot expect to progress satisfactorily with less. In fact, it is so important to her general well-being that she should be taught and persuaded to do everything in her power to secure it.
Fresh air during the day and open windows at night; prudent eating; a comfortable bed furnished with warm but light bedding; warm baths; a hot water bag to the feet and a hot drink upon retiring are all conducive to sleep.
But in addition to these, and perhaps of even more import, are cheerfulness and a tranquil, untroubled state of mind. It is well for the nurse to make a mental note of that intangible but influential fact, for she can usually exert a great deal of influence in shaping her patient’s or patients’ moods.
Breasts.—Breast feeding is the most urgent single need of the baby, for whose coming we are making preparation, and practically every mother, excepting those with definite physical disability, can supply this need of her baby’s, if she gives herself proper care both before and after its birth. It is true, that everything that promotes her general health helps to prepare her to nurse the baby, but there is need also for care of the breasts and nipples themselves, to make the nursing satisfactory, and to prevent sore nipples and possibly even breast abscesses.
132Briefly, this local care consists of supporting heavy breasts, but avoiding pressure; bringing out flat or retracted nipples and toughening the skin which covers the nipples.
After they become heavy and uncomfortable the breasts may be supported by brassieres, which are snug below the breasts, loose over the breasts themselves and suspended from shoulder straps; or by some such binder as is shown in Figs. 34, 35, and 36, which answers the same purpose.
If the patient’s nipples are flat or retracted, she should begin about the fifth month to make them more prominent in order that the baby may grasp them easily. There are several ways of accomplishing this, all of them in the nature of massage, but whatever is done must be done regularly and persistently. One simple and effective method is to grasp the nipple between the thumb and forefinger, draw it out, hold it for a moment, then release it and allow it to retract. This should be done over and over, two or three times daily. Or the unstoppered opening of a warm bottle may be placed over a flat nipple and held in place until the nipple is drawn up into the neck of the bottle as it cools and forms a vacuum.
The toughening of the nipples should be begun eight weeks before the baby is expected. There are two general methods which seem to give about equally satisfactory results; one is to harden the skin with astringents and the other is to soften it with ointments. In either case, the nipples should first be scrubbed gently with a soft brush or cloth, warm water and soap, for about five minutes night and morning. They may then be rubbed with lanoline, cocoa-butter or vaseline and covered with a piece of clean soft cloth or gauze, to protect the clothing; or they may be bathed with a wash consisting of equal parts of a saturated solution of boracic acid and 95% grain alcohol. Tannin, benzoin and a great variety of astringents are also used, and with satisfactory results. But the essential is to decide upon some method of preparation, of proved value, and then persuade the patient to employ it with faithful regularity.
Care of the Teeth. It is important that the pregnant woman give her teeth excellent care, for in addition to the conditions with which we all have to cope, she must combat the effect 133of her tendency to have an acid stomach. And her teeth are prone to decay and crumble, since the fetus extracts lime salts from her bones and teeth, unless she is careful to take in through her food a supply which is adequate to meet the fetal needs. It is therefore advisable for her to place herself under the care of a dentist, as soon as she knows of her pregnancy, and have any necessary work done at that time, as delay may be serious.
Some physicians think it advisable to have an X-ray examination of the teeth made as a routine, in order to discover any existing pockets of pus at the apices of devitalized teeth. They feel, that because of the somewhat unstable condition of the pregnant organism, these localized infections are more of a menace to the expectant mother than to the ordinary individual, and that in some cases they should be drained.
As to daily care of the teeth, the patient should use dental floss and brush her teeth after each meal, and use an alkaline mouth wash several times daily, particularly after vomiting and before retiring. Much damage may be done by the acid secretions in the mouth if they are allowed to bathe the teeth through the long night stretches. Common cooking-soda, lime-water or milk of magnesia make excellent mouth washes.
Traveling. In this day, when people travel so much and so easily, it is common to hear discussions as to its advisability for the prospective mother. Like many other details of prenatal care, this point cannot be settled once for all women, nor for all stages of pregnancy. Each patient’s general condition must be considered; her tendency to nausea; the length of the journey and the ease with which it may be made, and whether or not she has ever had, or been threatened with an abortion. In general, traveling is less hazardous for the expectant mother to-day than it was formerly, to just the extent that it causes less strain, discomfort and fatigue. But as a rule it is considered wise for her to avoid traveling during the first sixteen and the last four weeks of pregnancy, and at the times when menstruation would ordinarily occur. Obviously, then, in the interests of prevention, a journey should not be undertaken at any time without a physician’s approval.
The marital relation is usually considered inadvisable in all 134cases after the eighth month of pregnancy, and among women who have had abortions or miscarriages it is best omitted throughout the entire period of gestation. This is particularly true of elderly primiparæ.
There are many minor disturbances which overtake the pregnant woman, and though not serious in themselves, her comfort is greatly increased by having them relieved, and this promotes her general welfare. The relief of these discomforts, when they are slight or only temporary, sometimes resolves itself into little more than a question of nursing. When long continued or severe, however, they constitute complications which the doctor treats accordingly.
Nausea and vomiting are probably the commonest disturbances of pregnancy and vary from the slightest feeling of nausea when the patient first raises her head in the morning, to persistent and frequent vomiting which then assumes grave proportions and is termed “pernicious vomiting.” Although it is possible that even the slightest nausea is due to a mild toxemia, there can be no doubt that in many instances the patient’s mental attitude is an important factor.
Dr. Slemons makes the interesting observation, that women who are unaware of their pregnancy for several months are seldom troubled with nausea, while those who erroneously believe themselves to be pregnant will suffer from this well-known symptom of pregnancy, until convinced of their mistake. The nausea then subsides.
As there is a marked tendency toward nausea during early pregnancy, it may be brought on by slight causes which would not produce it under ordinary conditions. Anxiety, grief, fright, shock, incessant worrying, fits of rage, introspection, brooding, or any great emotional stress may cause nausea when the diet is entirely satisfactory. But indiscretions in diet, rapid or over-eating also may cause nausea and vomiting in the expectant mother.
We seem to get back to the principles of personal hygiene as 135preventives of nausea during pregnancy, for simple, light food, taken in small quantities five or six times daily, eaten slowly and masticated thoroughly; the cultivation of a happy frame of mind; exercise and fresh air all tend to avert this very uncomfortable condition. Its prevention is of great importance, as the habit of vomiting is easily acquired but broken with difficulty. The common causes of nausea, and their prevention, should therefore be explained to the average patient, for she will then be able to help herself in warding it off.
Should “morning sickness” occur, however, it may be relieved in many cases, by eating two or three hard, unsweetened crackers or pieces of toast, with nothing to drink, immediately upon awakening and then lying still afterwards for half or three quarters of an hour. The sufferer should then dress slowly, sitting down as much as possible while doing so, and eat her regular breakfast. Lying flat, without a pillow, and keeping very quiet for a little while after meals, or whenever feeling the slightest premonitory symptom, will frequently prevent, and also relieve nausea, and sometimes comfort is derived from the use of either hot or cold applications to the abdomen. Some patients are relieved by having hot coffee or even a full breakfast before arising.
Heartburn, so called, which is experienced by many pregnant women, has nothing to do with the heart. It is caused solely by an excess of hydrochloric acid in the stomach, and is usually described as a burning sensation first in the stomach, then rising into the throat. It may be prevented, as a rule, by taking a tablespoonful of olive oil, or a cupful of cream or rich milk, fifteen or twenty minutes before meals, and avoiding fat and fried food at the meals immediately following.
This apparent inconsistency in treatment is due to the facts that fat taken into the empty stomach tends to inhibit the secretion of acid, while fat and fatty foods taken with meals tend to prolong their stay in the stomach and this in turn stimulates the secretion of hydrochloric acid, the thing to be avoided.
A patient with a tendency to heartburn will be wise, therefore, if she generally eliminates oils, fats and fatty foods from 136her meals, and definitely avoids them when the burning occurs. Since the painful, burning sensation is directly due to an excess of acid in the stomach, the obvious step toward relief is to take an alkali at once. A tablespoonful of lime-water is often satisfactory; a teaspoonful of sodium bicarbonate in water; a small piece of magnesium carbonate may be nibbled by itself, or any alkaline water that the patient fancies may be taken.
Distress. There is another form of discomfort, often vague and ill-defined, commonly called “distress” and occurring after eating. It may be neither heartburn nor pain, but resemble both and make the patient very miserable. It is usually seen in women who eat rapidly, do not chew their food thoroughly or eat more at one time than the stomach can hold comfortably. The prevention, naturally, lies in taking small amounts of food slowly and masticating thoroughly.
Flatulence may or may not be associated with heartburn, but it is fairly common and rather uncomfortable. It is usually due to bacterial action in the intestines, which results in the formation of gas. As has been previously explained, the pressure of the enlarged uterus upon the intestines and absence of pressure by the abdominal muscles, retards normal peristalsis, with the result that gas sometimes accumulates to a very uncomfortable extent. It is clear, therefore, that a daily bowel movement is of prime importance in preventing and relieving flatulence, and also that foods which form gas should be carefully excluded from the diet. The chief offenders are parsnips, beans, corn, fried foods, sweets of all kinds, pastry and very sweet desserts. Various intestinal disinfectants are employed, as in non-pregnant states, and also yeast cakes, cultures of Bulgarian bacilli and artificially fermented milk containing bacteria that are antagonistic to the gas-producing forms.
In the opinion of some doctors, flatulence is sometimes an early symptom of toxemia.
Diarrhea. Although diarrhea is not one of the commonest disturbances of pregnancy, neither is it infrequent, and must be borne in mind in connection with digestive troubles. Of course, a pregnant woman may have an attack of diarrhea from the same causes that produce it in any one else, and its relief would 137be obtained by the usual methods, chiefly the correction of dietetic errors. But on the other hand, it may be due entirely to the uterine pressure on irritable intestines. Like flatulence, it is regarded by some doctors as a possible symptom of toxemia.
Pressure Symptoms. Under the general heading of pressure symptoms are several forms of discomfort resulting from pressure of the enlarged uterus on the veins returning from the lower part of the body, thus interfering with the flow of blood back to the heart. As both the cause and relief of these symptoms are associated with the force of gravity, the nurse will usually know what to do in mild cases without further explanation. In general the heavy abdomen should be supported by a binder or properly fitting corset, the patient should keep off her feet as much as possible and elevate the swollen part.
The commonest pressure symptoms are swollen feet, varicose veins, hemorrhoids, cramps in the legs and shortness of breath, and though they may appear at any time during the last half, of pregnancy, they grow progressively worse as pregnancy advances.
Swelling of the feet is very common, and when very slight may not be serious nor particularly uncomfortable. The edema may be confined to the back of the ankle, which grows white and shining, or it may extend all the way up the legs to the thighs and include the vulva. Sitting down, with the feet resting on a chair, or lying down with the feet elevated on a pillow will naturally give a certain amount of relief. If the swelling and discomfort are extreme the patient may have to go to bed until they subside, but very often she will secure adequate relief by elevating her feet for even a little while, several times a day. But while employing these harmless, and clearly indicated measures, to make her patient comfortable, the nurse must be keenly alive to the fact that while edema of the feet, legs and vulva may be of solely mechanical origin, they are also symptoms of toxemia, about the most dreaded complication of pregnancy. And as recognition of the earliest signs of toxemia is among the triumphs of prenatal nursing, even the slightest swelling must be reported to the doctor and immediate steps taken to have the urine measured and examined.
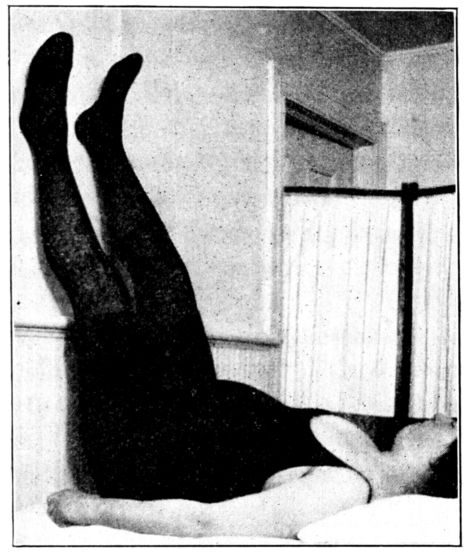
Fig. 40.—Right angled position, to relieve edema or varicose veins of feet and legs. (By courtesy of The Maternity Centre Association.)
Varicose veins are not peculiar to pregnancy, but are among the pressure symptoms which frequently accompany this condition during the later months, particularly among women who have borne children. The superficial veins in the legs will often be equal to the tension put upon them the first time, but will give way as the strain is repeated during subsequent pregnancies. The distension of the veins is not serious as a rule, but may be very uncomfortable; this, coupled with the unsightly appearance, sometimes has a bad mental effect. Varicose veins may occur in the vulva, but they are usually confined to the legs, and both legs are about equally affected. But as the position of the child in utero may exert greater pressure on the right than on the left side, the veins on that side may be more distended; or the right side alone may be affected.
Relief is obtained by keeping off the feet, and particularly by elevating them and also by the use of elastic bandages. When a woman finds it difficult or nearly impossible to sit or lie down for any length of time, she may accomplish a great deal in a few moments by lying flat on the bed with her legs extended straight 139into the air, at right angles to her body, resting against the wall or head board, as shown in Fig. 40. This right-angled position for five minutes, three or four times a day will accomplish wonders in reducing varicose veins.
In addition to posture, a spiral elastic bandage will give relief and help to prevent the veins from growing larger, if applied freshly after each time that the leg is elevated. The most satisfactory bandages, from the standpoint of expense, comfort and cleanliness, are of stockinette or of flannel cut on the bias, measuring three or four inches wide and eight or nine yards long. If made of flannel, the selvedges should be whipped together smoothly so that there is neither ridge nor pucker at the seam. The bandage should be applied spirally with firm, even pressure, starting with a few turns over the foot to secure it, and leaving the heel uncovered, carried up the leg to a point above the highest swollen vessels. As a rule, it may be left off at night.
There are satisfactory elastic stockings on the market, but they are expensive, often cannot be washed and seem to offer no advantage over the bandages.
Engorged veins in the vulva may be relieved by lying flat and elevating the hips, or by adopting the elevated Sims’ position for a few moments, several times a day. (Fig. 41).
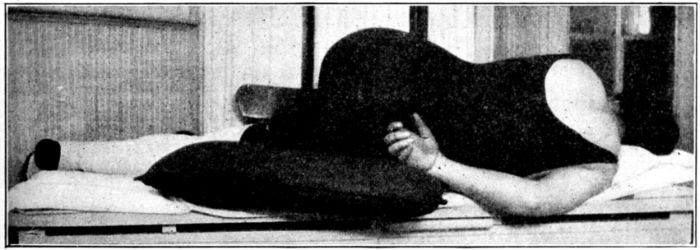
Fig. 41.—Elevated Sims’ position to relieve varicose veins of the vulva. (By courtesy of The Maternity Centre Association.)
Hemorrhoids are virtually varicose veins which protrude from the rectum, but, unlike those in the legs, are extremely painful. As it is the straining incident to constipation that causes these engorged veins to prolapse, this condition constitutes 140one more reason for preventing constipation. A pregnant woman whose bowels move freely every day rarely has hemorrhoids.
Should hemorrhoids appear, the first step is to have them gently pushed back into the rectum. The patient can usually do this for herself, quite satisfactorily, after lubricating her fingers with vaseline or cold cream. Lying down, with the hips elevated on a pillow; the application of an ice bag, cold cloths or witch-hazel compresses to the anus will almost always give relief. When the condition is severe, the physician may prescribe medicated ointments, lotions or suppositories, but operation is seldom resorted to during pregnancy, for fear of bringing on labor prematurely. Sometimes the hemorrhoids are worse during the first few days after labor, but as a rule they disappear with the removal of the cause, which in this case is pressure made by the enlarged uterus.
Cramps in the legs, numbness or tingling may be caused by the pressure of the large, heavy uterus upon nerve trunks supplying the lower extremities. The recumbent position; applying heat and rubbing the painful areas will often give comfort.
Shortness of breath is sometimes very troublesome toward the end of pregnancy, and, as may be easily seen, is due to the upward, and not downward pressure of the uterus. For this reason it is aggravated by the patient’s lying down and relieved by her sitting up or being well propped up on pillows, or a back rest.
Vaginal discharge. The normal vaginal discharge is greatly increased during the latter months of pregnancy, as was pointed out in Chapter V, so that ordinarily the moderately profuse yellowish or white discharge at this time has no particular significance. Its existence should be noted, however, and brought to the doctor’s attention, for a very profuse discharge is likely to be regarded as a possible evidence of gonorrhea. For this reason a smear is usually made, when the discharge is excessive, to establish or eliminate this diagnosis; if it is positive, it indicates the necessity for treatment to safeguard both mother and baby.
As the normal vaginal discharge has antiseptic properties, it should not be removed by douches, which many patients are 141eager to take; but if it is irritating and causes itching or burning the patient may be made entirely comfortable by avoiding the use of soap and by bathing the vulva with a solution of sodium bicarbonate or with olive oil.
Itching of the skin is a fairly common discomfort, and is possibly a result of irritating material being excreted by the skin glands and deposited upon the surface of the body. The local irritation usually may be allayed, if not very severe, by bathing the uncomfortable areas with a solution of sodium bicarbonate, or a lotion consisting of a pint of lime-water, half an ounce of glycerine and thirty drops of carbolic acid. It is a good plan, also, for the patient to increase the amount of fluids which she is taking, in order to promote the activity of the skin, kidneys and bowels, and thus dilute the material that may be responsible for the itching and increase its elimination through all channels. In other words the itching may be due to a mild toxemia.
Some women complain of discomfort caused by the stretching of the skin over the enlarged abdomen, which becomes so tense it feels as though it might tear apart. There is a very old and widely current belief that this sensation may be relieved by rubbing the abdomen with some kind of an oil or ointment. And, moreover, that such oiling will not only increase the elasticity of the superficial layers of the skin, but the deeper layers as well, and that by this means striæ may be prevented. There seems to be little foundation for the fear that the skin will tear, or belief in the efficacy of the oiling, but if a woman fancies that she is safer and more comfortable after oiling her abdomen, there is certainly no reason why she should not do so.
It is evident that by teaching the principles of personal hygiene to the expectant mother so convincingly that she will adopt them, and sometimes, by employing simple nursing procedures to relieve the various discomforts of pregnancy, much will be accomplished toward promoting the welfare of both the patient 142and the expected baby. But this is not enough. The nurse must also be on the alert to detect and report the early symptoms of complications, for there may be times when she will be the first one to see the patient after a symptom has developed.
The principal complications of pregnancy which are amenable to preventive or early treatment are the toxemias, premature terminations of pregnancy and hemorrhage.
The causes of these conditions and the details of treatment and nursing care are so inextricably associated with each other that they are discussed together and at some length in another chapter. But their most conspicuous, early signs are briefly noted here, since watching for them constitutes a part of routine prenatal care.
The toxemias are apparently caused by disturbed metabolism and impaired or inadequate excretory processes. Their prevention is to be accomplished largely by observing the principles of personal hygiene previously described, and in quickly treating early symptoms. One of the commonest of these symptoms is headache, sometimes persistent and very severe. Others are disturbed vision, dizziness and more persistent or severe vomiting than could reasonably be called “morning sickness”; puffiness under the eyes, or elsewhere about the face, or of the hands; anything more than very slight swelling of the feet and ankles; high or increasing blood pressure; mental depression; albumen in the urine, amounting to more than a trace, and epigastric pain, are all possible symptoms of toxemia. A patient in whom even one of these symptoms appears is usually placed under close observation; frequently put to bed and her diet restricted to milk, or even water, until the symptoms subside.
The common symptoms of premature termination of pregnancy, (an abortion, miscarriage or premature labor) are bleeding, with or without pain in the small of the back, followed by cramp-like pains in the abdomen. Bleeding or a bloody discharge, therefore, irrespective of pain should be regarded as a symptom of pending labor and the patient should be put to bed promptly, and kept quiet. Preventive treatment, after pregnancy has begun, consists largely of rest, particularly at the time when menstruation would ordinarily occur; avoidance of physical 143shocks and of overwork during the later weeks. Prolonged failure on the part of the patient to feel fetal movements or of the nurse or doctor to hear the fetal heartbeat after they have once been manifest usually indicates the death of the child and precedes its expulsion.
Bleeding, or a sudden increase in the size of the uterus with a rapid pulse or general symptoms of shock, may be the symptoms of hemorrhage caused by placenta prævia or premature separation of a normally implanted placenta; upon the appearance of any one of these signs the patient should be put to bed and kept absolutely quiet.
To sum up, we find that the following symptoms may be forerunners of serious complications, and therefore should be watched for and reported to the doctor immediately upon their discovery:
These are generally accepted as the cardinal danger signs of pregnancy, any one of which, alone or in combination with one or more of the others, is of significance and should be reported to the doctor at once.
When all is said and done, our wish for the expectant mother is for little more than that she shall live a normal, wholesome life; that she shall be willing, and also be able to weave into her every day life the principles of personal hygiene which every one 144should adopt; that she shall be carefully watched for complications throughout the entire period of pregnancy, and that these complications shall be speedily treated.
Adoption of personal hygiene, then, and prevention of complications by their early detection and treatment—these we want for every woman who is looking forward to motherhood.
For lack of these things there are sick and blind and maimed babies and invalid women; there are lonely, motherless children and bereaved mothers in every corner of our land.
It is only once in a long time that the obstetrical nurse has a patient who is suffering from such a marked mental disturbance that her condition is diagnosed and treated as a psychosis. But more often than not she has a patient who is secretly suffering a good deal of mental stress and pain, which is not recognized and not treated.
In fact, by virtue of the deep significance of the states of pregnancy and motherhood, and the long period of time through which they continue, it is scarcely possible for them not to produce a mental effect of some sort upon the average woman. Sometimes this effect is a very happy one; but all too often it is quite the reverse. It is safe to say that the majority of maternity patients are passing through deep waters, and the nurse’s usefulness to these charges will be greatly broadened if she has at least some understanding of the cause and character of these mental sufferings.
In the ordinary course of events, from birth to death, we all of us are being called upon continuously to adjust ourselves to all sorts of experiences, situations and emotional strains peculiar first to early childhood, then the school epoch, the period of emancipation from home and finally to the life work. And as we take our way, we develop habits of meeting the sorrow and disappointments that come; the anxiety, criticism, success, failure, illness, poverty and what not.
Some individuals habitually face the issues of life, whether large or small, and habitually overcome difficulties for themselves and for other people. They are described by the psychiatrists as being grown up, or psychologically evolved.
Others follow the course of least resistance; never face their problems; are thoughtless and inconsiderate in their demands; 146are unable to make decisions and accordingly live upon the mental and moral strength of others. Such people are referred to as being infantile, or psychologically undeveloped. They are not unlike the baby who gets “what he wants when he wants it” by the unreasoning method of screaming and pounding upon his high chair with a spoon. He is scarcely more irresponsible than the hysterical adult who gains her point by developing a headache or fainting, flying into a rage or tearing her clothes and smashing china. Such people make little or no adjustment to unsatisfactory conditions and have poor capacity for endurance or sacrifice.
With not a few women this poor capacity is a result of lifelong indulgence or protection by unwise parents, and they never reason out the question of obligation or responsibility because they never have to. Everything is done for them. All rough places are so consistently smoothed out that they never entertain the idea that effort or adaptation on their part could possibly be in order.
There are others who cherish trouble, make difficulty where there need be none and steadfastly refuse to acknowledge good fortune or see the silver lining. This is their method of securing attention, much as the baby cries or screams to the same end.
Between these extreme types are ranged people who display innumerable shadings and degrees of psychological development. Some cope satisfactorily with their life situation because that situation is neither difficult nor beyond their capacity for adjustment. Others need a little bolstering up now and then to bridge over the gap between the demands made upon them and their ability to meet these demands. Still others have to be literally carried when disaster overtakes them, or they break down.
As might be expected, our ability to stand the big tests or strains that may come to us; our manner of meeting them and their effect upon us depend very largely upon how we have habitually met the lesser trials that have come to us previously, how we have habitually adjusted ourselves to the experiences of life. For after all the test of life is a measure of one’s capacity for adaptation to these experiences and to surroundings.
The strain that measures our ability to adapt ourselves may 147be one big stroke or it may be a long drawn out trial which would be of small consequence were it of short duration. It is the persistency and the monotony of a lesser care that so often wears away the rock of our endurance.
If a strain proves to be too much for our adaptive capacity, and we break down under it, our manner of breaking will be characteristic of us, or an accentuation of what might have been called our bendings under lesser difficulties in the past.
The expectant mother is no exception to these general principles. She does not develop nervous breakdowns either more or less frequently than the non-pregnant woman who is under an equal strain. She is merely a human being whose adaptive capacity is being tested. But the test is severe for there is, perhaps, no greater strain upon the adaptive capacity of a human being than that to which a woman is subjected during pregnancy, confinement and the months directly following the birth of a child. She may be expected to meet this strain just as she would meet another equally great demand upon her adaptive capacity.
Otherwise, pregnancy of itself does not affect the brain or the mind, any more than it affects the kidneys, for example. But like the kidneys, the brain or the mentality may have difficulty in coping with the additional strain that is put upon it during pregnancy, and if the strain is greater than the ability to function in either case there is likely to be a breakdown.
It is now generally believed, therefore, that there is no psychosis which is typical of pregnancy. But that during pregnancy one may see all types of neuroses and psychoses which are frequently associated with other severe strains upon the individual. We see depressions, excitement, paranoid trends, delusional and hallucination states, hypochondriasis, obsessive fears, anxiety attacks, hysterical manifestations as well as the so-called “neurotic vomiting.”
Aside from the delirium-like experiences often associated with the toxemias of pregnancy, none of the above mentioned conditions are referable to any disturbance of the physiologic or metabolic functioning of the patient, so far as science can demonstrate. They are merely accentuations of poor habits of adjustment 148to difficulties, which the patient has betrayed all her life.
The psychoses of pregnancy and the puerperium require skilful handling and the nurse is not called upon to care for them except under the constant supervision of a physician.
She is, however, constantly brought face to face with facts of fear and worry and conflicting desires which play a tremendous rôle in the well-being of the patient during the months of pregnancy and confinement. The chief source of happiness and of unrest is the mother’s attitude toward the coming of the baby.
Just here it may be helpful to have a word about what is meant by “conflict” and the “mechanism” which produces it. As a starting point there must be a recognition of the fact that the deepest and most influential feminine instinct is maternal—the desire to have and care for a child. It is primal. It has been in women since the dawn of Creation and although in many women it is put down, stifled or complicated by other desires, it cannot be destroyed. Not a few women deny this instinct, but back of their denial is some reason, conscious or unconscious, which is not harmonious with the idea of motherhood. The woman may be selfish, for example; she may be vain and not want to lose her grace and charm through pregnancy.
When some such feeling is strong it conflicts with the deeper one of maternalism and there is a lack of harmony or a “conflict.” It is just that—a conflict or struggle between two emotions and the result is a state of mental unrest. A homely comparison might be found in the digestive disturbance which may follow an effort to cope with two incompatible articles of food at the same time. The patient may have nausea, vomiting, pain or even more severe symptoms. The severity of the symptoms and their effect upon the patient depend somewhat upon the average vigor or stability ordinarily displayed by the digestive tract under a lesser strain. People with so-called delicate digestions may be greatly upset by combinations of food which others are able to cope with and suffer little or no inconvenience.
When a well evolved individual has a desire which results from our culture or civilization (a wish to preserve her grace or her luxuries, for example), that is in conflict with a deeper 149primal instinct, she will often be able to reason out the situation, and in the case of approaching motherhood, decide that the baby is worth any sacrifice, any inconvenience, and go joyfully through her period of expectancy. She will glory in the consciousness of her ability to realize the supreme purpose of a woman’s creation. In other words she adjusts herself to the situation, harmonizes the discordant desires and is mentally undisturbed.
A less well evolved woman, like a person with a delicate, easily upset digestive tract, will have difficulty in making an adjustment—in harmonizing her instinctive desire for motherhood and her acquired desire for comfort, attention and the things demanded by convention. The conflict may be violent enough to greatly upset her. This is particularly true if the demands of our cultural state make it necessary for the patient to keep this turmoil below the surface with no safety valve to relieve the pressure.
This problem of the mother’s attitude toward the coming of the baby is very general and varied as well. The mothers of families already large and poverty stricken are usually quite frank in expressing their dismay over the expected birth and lament the prospect of this extra burden, but at the same time they decide to make the best of it and they succeed in making a pretty satisfactory adjustment. Moreover, they do not feel the necessity for concealing their feelings or do not “repress” them, and accordingly find some relief in being candid.
The mothers of the middle and upper classes, however, are often surrounded by an atmosphere of conventional codes that are stifling to mental honesty. Accordingly they are less genuine in expressing their true attitude toward the coming child. To many of them—the selfish, self-centered type—the new baby will bring inconvenience rather than hardship. The importance of their ego will be dimmed. There will be a cutting down of luxuries and of freedom for social activities, and increased responsibility with closer confinement to the home. And while they give utterance to joy and pleasure over the prospect of having a baby, this does not quite reflect their inmost feelings.
Not a few women find an outlet for the tension caused by 150their conflict by being fretful and irritable or through conduct which they would have displayed if annoyed or chagrined about something other than the approaching birth of a child. Because of this outlet they are not so likely to break down.
It is by no means the rôle of the nurse to pry into the affairs of her patients, but she can often become the avenue of ventilation for a patient suffering from a mental conflict, and with very happy results. For one of the most helpful things that such a person can do is to talk, and little by little bring out and put into words the buried thoughts, dreads or shame that may be causing the conflict. Very often the listener will say surprisingly little and will express no definite opinions, but by a sympathetic, responsive attitude encourage the worried person to pour out the content of her mind.
Another source of unrest in the mind of the expectant mother, especially during her first pregnancy, is the fear of death during labor, or the development of complications. She is reluctant to speak of these things to her husband, family or friends, lest they laugh at her or regard her as a coward at the prospect of pain. Or she may be unwilling to distress those who love her by admitting her fear.
Fear of death and disease are very common traits and equally common is the hesitancy we all have in acknowledging them. And so the patient keeps these things to herself and turns them over and over in her mind; buries them and tries to put them out of her thoughts. But they stick. Her fear and her dread color everything that she hears, and very often and unwittingly her friends and relatives make matters worse by recounting the unhappy experiences of other mothers that they have known. At the same time these communicative friends do not tell of the immeasurably greater number of women who have come through safely, nor does the patient dwell upon these in her mind. She remembers the women who had convulsions or fever or a hemorrhage, or the one who died.
The nurse who sees the human being beyond the obstetrical case will appreciate the pain which such a conflict causes and by being sympathetic and responsive will try to make it easy for her patient to talk it over. The patient should invariably find 151her nurse ready to listen and to give assurances of the proved value of the precautions that are being taken to safeguard her and her baby. For not a few women are torn, not alone by the fear that things will go wrong with themselves, but with the fear that harm may come to the baby that they long to take into their arms and keep.
Other women are upset because of a habitual inability to make decisions that will bring about a marked change in their lives. They find it difficult to accept pregnancy because its consummation will definitely alter their state. Life may prove to be more satisfactory because of the baby, or it may be less so. But in any event it cannot be the same and they dread making an irrevokable change.
Still another cause of distress is the current belief as to hereditary influence, and the possible effect upon the unborn child of unsuccessful attempts at abortion which the patient has made early in her pregnancy. Every family has its skeleton of a relative who is “queer,” feeble-minded, epileptic or who has died in a sanitarium or state hospital for the insane. The fear that the child may “strike back” to one of these individuals, and suffer retardation in his mental development, often amounts to little less than an obsession.
The nurse may often dispel such an anxiety by drawing upon even her slender knowledge of embryology and reassure her patient that we know very little about inheritance, but that the evidence is that environment and early training are such important determining factors, that a child is more likely to be affected by the example and guidance of his parents during his first few years than through transmission from their blood.
Attempted abortions during the early months of pregnancy are more common than is generally supposed. Of their effect upon the offspring we know very little. We do know, however, that an attempt to produce an abortion often gives rise to a good deal of secret worry on the part of the expectant mother. It is the nucleus of many a vague depression during pregnancy, not only because of remorse over wrong-doing, but also because of fear that the child who is coming, in spite of the attempt to destroy him, may suffer the consequences. This is another of 152the anxieties which the patient can seldom bring herself to discuss with her family or even with her physician. But it so occupies her mind that she may allude to it, in a roundabout way, to the nurse who becomes her constant companion, as though describing the act of a friend. The nurse who reads between the lines may often relieve a serious tension caused in this way by discussing the matter casually and impersonally. Above all she must not assume an attitude of disapproval, for it is not within her province to go into the ethics or morality of the act. Her function at this time is solely to give the patient an opportunity to ventilate her thoughts.
Another real cause of worry during pregnancy is the patient’s fear of her own inadequacy to care for and to rear a child in the best possible manner. The idea of assuming the physical care and the moral guidance of another human being is often little less than terrifying to a young woman whose responsibilities in the past have been shared or carried by some one else. Or to the one who has gone through life hunting for, and exaggerating, the difficulties in a situation, before attempting to meet it; and perhaps to the one who is habitually conscientious in all of her relations with other people.
Still another type, and one which presents a much simpler situation, is the expectant or young mother who is scarcely suffering from a mental strain, but has a little let-down in her customary poise and self-control, such as we so often see in convalescents and chronic invalids.
Pregnancy, labor, and the puerperium are normal physiological processes, it is true, but they impose a physical tax and the patient is sometimes physically tired and after labor may suffer something akin to surgical shock.
The physical weariness may be due to an insufficiency on the part of some one of the internal secretions. But in any event the patient feels tired and may show the same sensitiveness or irritability that any of us show when tired and exhausted and she will merit considerable forbearance on the part of those who surround her.
But when we understand, even faintly, the conflicts which are possible in the mental life of the expectant mother—the 153incompatibility of her age-old maternal instinct and the desires born of our culture and civilization, it is not difficult to see that her adaptive capacity may be sorely tested.
The cause of her trouble is not apparent to the patient’s associates but they are aware of its manifestations in the shape of moods, temper tantrums, strange conduct and all sorts of nervous and mental symptoms. If such a patient does not get relief through talking things over, but continues to brood and worry alone—to repress the cause of the conflict—she may not be sufficiently adaptive to endure its ravaging effects, and have a nervous or mental breakdown as a result.
It is hoped that the nurse may understand from this discussion that the conflicting thoughts which her patient does not discuss, but buries and keeps below the surface of her mind, are the factor that works harm in her mental life. If the nurse can get her patient to ventilate these thoughts, they will be robbed of much of their power to injure. But this patient, like any one else, will talk freely only when she talks spontaneously and she will do this only when she senses in her nurse a sympathy and a sincere concern over her troubles.
Accordingly, the nurse should try to so attune herself as to be receptive to evidences of the patient’s moods and impulses, and possibly from a chance remark get a clue to the repressed desires which are working harm. She will then be able to meet the patient on that ground.
It is not that the relief of the patient by means of mental catharsis is necessarily a nurse’s function. It is simply that a patient suffering from a conflict should talk freely to some one, it does not matter who, and by virtue of the long hours which they spend together, the nurse very often happens to be that some one. People do not ordinarily find it easy to lay bare their inmost thoughts before the members of their family and the patient may not discuss her conflict with her physician, which of course is the ideal, because his visits are relatively short and do not favor the ambling, desultory conversation into which the nurse and patient may so easily drift.
On the other hand, the nurse must not look for trouble, in order to be useful, nor by the slightest intimation give her patient 154an idea that it is a common practice among expectant mothers to worry, be fearful or alarmed. If the patient displays these emotions the nurse must be ready, but she must not be suggestive. Her attitude must be entirely passive for she is simply a receptacle into which the patient may pour her conflicting thoughts. But the receptacle must be always available.
The positive course which the nurse may take is to be unfailingly hopeful and courageous and take it for granted that her patient is filled with joy and pride over her pregnancy. The gratification is there by instinct, but it may be so buried and complicated by other emotions that the patient is not wholly aware of it. It may be surprisingly clarifying for the nurse to say quite simply, “But, after all, it is a wonderful thing to have a baby and you are proud and glad that he is coming. He will be worth any sacrifice.”
If the nurse will so far put herself in the patient’s place that she is glad, sincerely glad, that the baby is coming, this attitude will communicate itself to the expectant mother. Happiness and enthusiasm are very infectious.
To sum it all up: The expectant mother who habitually has not made satisfactory adjustments during her life may be bending under a mental burden that is a little heavier than her slender, unevolved powers can bear. The nurse’s part is to recognize this possibility and realize that while she cannot attempt to correct the difficulty she can be a prop by simply being optimistic and reassuring. A patient who may be suffering from a mental conflict is often saved from a breakdown by little more than a ready sympathy which is born of understanding.
It sometimes devolves upon the nurse to give advice in selecting and preparing the room to be used for a home confinement, and very often to help the prospective mother in preparing and assembling adequate equipments for the delivery and for the care of herself and the baby afterwards.
Under such circumstances the nurse must feel under compulsion to do all in her power to make the home delivery satisfactory, from the standpoint of the patient’s happiness and contentment and from the standpoint of surgical cleanliness and efficiency as well, so that normal cases, at least, may be attended with reasonable safety at home.
We know that the deaths, incident to childbirth, throughout this country at large, have not declined during the past decade, in spite of improved obstetrical methods and skill and the large percentage of recoveries in hospitals where they are applied. In the homes, in general, young mothers continue to die in distressingly large numbers, chiefly from infection, which we know is largely preventable. Apparently, then, in some important particulars the conditions surrounding the majority of home deliveries are still such as to be almost a menace to life and health. And as it is manifestly impossible for all obstetrical patients to be cared for in hospitals, home deliveries need to be made safer, which virtually means, made cleaner.
This grave need cannot be dismissed by the nurse as something outside of her province. She may aid greatly, and therefore is under obligation to do so, in making home confinements surgically clean, by being conscientious and thoughtful and thorough in her preparations and assistance.
A relatively small percentage of obstetrical patients require operative assistance, but without a single exception they all require 156cleanliness; cleanliness of appliances and cleanliness of methods.
As the first labor is usually longer and more difficult than later ones, and the percentage of lacerations and operative interference is higher, primiparæ should be delivered in hospitals when possible, as well as all cases presenting any complication or abnormality. But women who are normal, particularly multiparæ, and these constitute the vast majority of obstetrical patients, should be able to remain at home in safety.
In most instances the patient who is to be delivered at home will have to occupy her accustomed room and there is no alternative. Should there be a choice of rooms, however, one should be selected that is cool and shady, if the confinement takes place during the summer, but bright and sunny for occupancy during most of the year; it should be conveniently near a bathroom if possible, and have an adjoining room for the nurse and baby to occupy.
The arrangement and furnishings of the room will not of necessity vary greatly from those of a room which is to be occupied by any patient. Carpets, upholstered furniture, heavy draperies and curtains are no more suitable in this than in any patient’s room.
The ideal is: A room with a washable floor with small, light rugs; freshly laundered curtains at the windows; a single, brass or iron bedstead, about 30 inches high, with a firm mattress, and so placed as to be accessible from both sides and with the foot in a good light, either by day or by night; a bedside table and two others (folding card tables are a great convenience); a bureau; a washstand, unless there is a bathroom on the same floor; one or two comfortable chairs, two or three straight chairs and a couch or chaise longue, all of which should be of wood or wicker or covered with freshly laundered chintzes.
Barrenness is not only unnecessary but is to be avoided, for the room should be as cheerful and pretty as is compatible with cleanliness. There is usually no objection to pictures on the wall, but the room should be free from useless, small articles which are dust catchers, give the nurse unnecessary work, and occupy space needed for other things. Between such a room as this and 157the one which the nurse finds must be used, there may be a dismaying difference, and so once more she must exercise her ingenuity and resourcefulness; change and improve where it is possible and make the best of conditions that cannot be altered, for the baby is coming and the mother must be safeguarded from infection and other disaster, no matter what the room is like.
Much as we should like ideally to equip and prepare every room to be used for a home confinement, we cannot overlook the importance of having preparations made with as little disturbance as possible to the patient and her household. Preparations made with bustle and ostentation are suggestive of inefficiency; are bad for the patient, frequently causing her great alarm, and in the main had better be omitted. The nurse who is able to go into a home quietly and unobtrusively and accept what she finds, even carpets and draperies, and still do clean work, is doing better nursing than the one who arranges a faultless room but upsets her patient and disrupts the household in the process.
Common sense, judgment and tact, then, will sometimes be as important in preparing a room for home delivery as are washable floors, curtains and furniture.
While we do not advise nor elect to have carpets, draperies and upholstery in a delivery room, we know that they need not menace the patient’s welfare if all details of the work about the patient, herself, are scrupulously clean. That is the one point which the nurse must bear constantly in mind, the paramount importance of clean work about the patient.
The room should be given a thorough housecleaning about two weeks before the expected date of delivery. If there is carpet on the floor, there should be a large canvas or rubber, or an abundance of newspapers available to protect it, about, and under the bed; and if the bed is of wood, the sideboards and foot should be covered to protect them from injury by soap, water and solutions which may be spattered or spilled during labor. If the bed is low, there should be four solid blocks of wood prepared, upon which to elevate it, after removing the casters, and it is also a good plan to have a large board, or table 158leaves, in readiness to slip under the mattress to make it firm, particularly if the bed is soft or sinks in the middle.
So much for the room.
In preparing the dressings and assembling the various articles to be used the nurse will do well to remember that, although it is possible to use a number of things during labor, it is also possible to do excellent work with a meagre equipment supplemented with a cool head and ingenuity and training and above all, an exacting conscience. The average nurse will wish, usually, to follow a median course in her preparations, having everything at hand that will facilitate the work; be adequately equipped for emergencies but not burdened with non-essentials.
As the wishes and methods of different doctors vary, the articles needed in assisting them must of necessity vary also. But in addition to the instruments which will be used, the following articles will meet the ordinary requirements during a home confinement, and many of them, or adequate substitutes, are to be found in the average household.
For the Mother and the Delivery:
In addition to these, a certain supply of sterile dressings will be needed. Complete outfits of such dressings, sterilized and ready for use, may be obtained from any one of a number of firms, or the following may be prepared by the nurse or by the patient, under the nurse’s direction:
Dressings:
These may be put up into packages in the usual manner, using muslin for wrapping, and sterilized in the patient’s home as follows: Fill a wash boiler about ¼ full of water and fashion a hammock from a towel or strong piece of muslin, tied securely with strings at each end and hung from the handles so that the bottom of the hammock in about half way down in the boiler. As the weight of the dressings makes the hammock sag low, in the middle, it is usually necessary to place a rack, or support of some kind, in the bottom of the boiler to hold the dressings well above the bubbling water, at the point where they hang lowest. Pile the dressings into the hammock, cover the boiler tightly and keep the water boiling vigorously for one hour; dry the packages in the sun or by placing them in the oven for a few moments, and at the end of twenty-four hours repeat the steaming and drying process, wrap the packages in a clean sheet or paper and put them away in a drawer or covered box where they should remain until time to prepare for the delivery. The brushes, douche pan, irrigation-bag, and other articles which must be surgically clean 160may be sterilized in the same way. The gloves may be sterilized in this way or boiled immediately before delivery. If sterilized by steam, the gloves should be thoroughly dried, dusted with talcum inside and out to prevent them from sticking together, and may be wrapped in packages or placed in individual cases (Fig. 42). A small towel or piece of soft muslin and a ball of gauze containing talcum powder, if placed in the case and sterilized with the gloves, are often a convenience to the doctor in putting on the gloves.
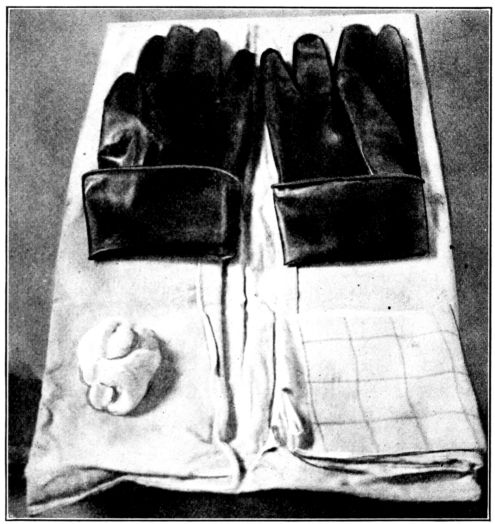
Fig. 42.—Gloves with cuffs turned up, lying with small towel and powder puff of gauze and talcum, on double envelope case in which they may be dry-sterilized. (From photograph taken at the Brooklyn Hospital.)
The newspaper delivery pads offer excellent protection and are made of six thicknesses of paper covered with a piece of freshly laundered muslin, which is folded over the edges and basted in place. (Fig. 43). These pads may be made virtually sterile by ironing them on the muslin side with a very hot iron, folding the ironed surface inside without touching it; again ironing on the outside and wrapping in a clean muslin or sheet, 161also recently ironed, and putting away in a place protected from dust.
The nurse herself should have:
Fig. 43.—Reverse side of pad made of newspapers and old muslin to protect bed during a home confinement. If muslin is held in place with safety pins it may be removed easily, washed and used for another pad. (Courtesy of The Maternity Centre Association.)
The doctor will usually supply himself with any articles needed beyond those which have been enumerated, but the nurse should be sure about the following in order that she may prepare whatever he may lack:
162In planning the baby clothes, there are a few important factors to bear in mind. The clothes should be simple; not more than twenty-seven inches long; warm, but light in weight, and large enough to fit loosely. Like the dressings, complete layettes may be bought outright, but if the mother wishes to make the little garments herself, the following list will be found to provide an adequate supply of clothing for the new baby. (See also Fig. 159.)
For the Baby, Layette:
Additional Articles Which Are Needed or Useful in the Care of the Baby:
The above lists of dressings and articles for the baby can be considerably modified and still be satisfactory. The leaflet of “Advice for Mothers” issued by the Maternity Centre Association, New York City (see p. 429), gives a somewhat curtailed list of equipment which proves to be adequate and within the means of most of the patients with whom the Association works.
It is usually a good plan for the nurse to advise the patient to have her dressings ready by about the end of the seventh calendar month, and the layette by the end of the eighth month. A baby born before this time would probably be so frail that it would be wrapped in cotton and not require the clothes ordinarily prepared for a full-term baby.
The prenatal care which was outlined in an earlier chapter becomes more impressive when one considers the disasters which it is designed to prevent. And the nurse will be more eager and able to watch her patient intelligently, and instruct her convincingly, if she appreciates and understands something of the conditions which she is helping to avert. She will give more effective nursing care, too, when complications do occur, if she gives it understandingly. In the toxemias, particularly, the importance of the nursing care looms large, for it is painstaking attention to details that makes this care so nearly a matter of life or death to the patient.
In considering the complications of pregnancy, the nurse in training needs a reminder that hospital experience is likely to give her an exaggerated idea of the relative frequency with which they occur. This is due to the fact that most maternity patients in hospitals are there because they are known to be abnormal in some way, or because they are pregnant for the first time, and first pregnancies are more likely to end in difficult and complicated labors than later ones. The vast majority of cases run practically uncomplicated courses, for pregnancy, labor and the puerperium are normal physiological processes. It is extremely serious, however, to allow them to become abnormal.
Watchfulness throughout pregnancy, then, in the interest of preventing disaster, cannot be too insistently advocated.
Some complications that are watched for during pregnancy are peculiar to that condition alone, and these may be divided into three general groups:
1. The premature terminations of pregnancy, which are designated as abortions, miscarriages and premature labors.
2. Ante-partum hemorrhages, due to either a placenta prævia 165or a premature separation of a normally implanted placenta, the latter being termed “accidental hemorrhage.”
3. The toxemias, including pernicious vomiting, pre-eclamptic toxemia, eclampsia and possibly nephritic toxemia, though this condition is not invariably associated with pregnancy.
There are other conditions, not necessarily inherent to the state of pregnancy, but which should be detected and treated early, since their development coincidently with expectant motherhood may threaten the safety of the patient or the child, or both. Probably the most serious of these is syphilis, though gonorrhea, impaired kidneys, heart lesions, tuberculosis or a general state of poor nutrition also may prove to be grave.
Any chronic, organic disease is likely to be increased in severity by the strain which pregnancy puts upon the impaired organs, in common with the rest of the maternal body. But acute diseases usually run about the same course in pregnant, as in non-pregnant women, except when an infection causes an abortion, the shock of which, in turn, reduces the patient’s resistance against the complicating disease.
As we consider these various, dreaded complications which may arise during pregnancy, infrequent though they be, we feel that no amount of effort is too much to make, if we can, thereby, save one mother or one baby from their destructive effects. We are stirred by the urgency of preventing a premature ending of pregnancy, for example, when we see it, not so much as simply another obstetrical emergency, but in its true, tragic light as the loss of an infant life and the bereavement of an expectant mother.
The termination of pregnancy before the expected time is termed an abortion, miscarriage, or a premature labor or birth, according to the stage to which the pregnancy has advanced, but there are wide variations in the accepted meanings of these terms, among both lay and medical people.
In the lay mind, abortions are usually associated with criminal practice and the term is seldom used, while miscarriage is a term which is loosely applied to all deliveries occurring before the child is viable, or before the seventh month. It is not uncommon, 166however, to hear the term abortion used to designate the termination of a pregnancy before the end of the fourth month; miscarriage, one which occurs between the end of the fourth and seventh months, and premature labor as one which takes place any time after the seventh month, but before the expected date of confinement.
Medical people, on the other hand, seldom use the term miscarriage, but designate as abortions all terminations of pregnancy which occur before the end of the seventh month; and premature labor, those occurring from that time until the estimated date of confinement. It is these meanings which will be intended when the terms abortion and premature labor are used in the following pages.
Abortions. In the nature of things, it is impossible to say how often abortions occur. They sometimes happen so early in pregnancy that the patient is unaware of the accident; or, if she does know of it, she may take no notice of it or regard it of so little consequence that she does not consult a doctor; while in many cases it is intentionally concealed because of having been criminally induced. But such information as is available suggests that at least one out of every five pregnancies ends in an abortion.
Since the ovum is insecurely attached to the uterus until the sixteenth or eighteenth week, an abortion is more likely to occur during this time than later, while of this period, the second and third months seem to be the most perilous.
Abortions are less likely to happen during first pregnancies than succeeding ones; they occur more often among women over thirty-five years old than in younger ones, and in all cases are most likely to take place at the time when the menstrual period would fall due were the woman not pregnant. Their frequency probably increases with the number of pregnancies, because of the tendency of multiparous women to have endometritis, which, as we shall see later, is a causative factor.
Causes. There is a variety of causes of abortions and miscarriages, some entirely unavoidable, but many which are preventable, and it is well for the nurse to be familiar with those which operate most frequently, as follows:
1671. Certain abnormalities of the developing fetus are inconsistent with life, and are, therefore, a frequent cause of abortion. Dr. Mall, of Johns Hopkins University, showed after years of investigation that at least one-third of the embryos obtained from abortions were malformed and would have developed into monstrosities had they lived to term. It is often a great comfort to the expectant mother who loses her baby early in pregnancy to realize that had she carried her baby to term it might have been a monster, and that, therefore, she has not lost a beautiful, normal child. Just why these abnormalities occur is not known, nor is there any known method of preventing or correcting them. There also may be such defects in the placental development, that the fetus does not derive sufficient nourishment to continue its development, and dies very early as a result.
2. Abnormalities in the generative tract may cause abortions, the most common of these being inflammation of the uterine lining and a malposition of the uterus itself. Gonorrheal infection is a frequent cause of such an inflammation, which so alters the decidua that a satisfactory implantation of the ovum is impossible, and it perishes from lack of nourishment. Uterine misplacements, particularly retroflexion and prolapse, are important causative factors in abortions. This is because the malposition interferes with the blood supply and lesions in the endometrium result. This also presents an unsatisfactory lodgement for the ovum and it cannot survive for long.
3. Acute infectious diseases all tend to cause the death of the fetus and thus cause abortions. Fetal death in these cases is believed to be due to the transmission of toxic material from mother to child, as may occur also in such poisoning as phosphorus, lead and illuminating gas.
4. Mental or emotional stress may be the cause of an abortion, but less importance is attached to these factors to-day than formerly. There is an occasional case, however, which can be explained on no other grounds.
5. Physical shocks, such as falls, blows upon the abdomen, jumping, tripping over carpets, jars, jolting or overexertion, may be the exciting cause of an abortion where there is a marked irritability of the uterine muscles. This factor is largely influenced by individual stability, however, as a slight jar will cause an abortion in one woman, and violent experiences will have no effect upon another, at the same stage of pregnancy.
Symptoms. For purposes of differentiation in treatment, abortions are usually divided into three groups and designated as threatened, complete and incomplete, but the premonitory symptoms of all of the varieties are the same. They are bleeding, 168with pain that is usually intermittent, beginning in the small of the back and finally felt as cramps in the lower part of the abdomen. Since menstruation is suspended during pregnancy, it is a safe precaution to regard any bleeding during this period, with or without pain, as a symptom of pending delivery.
Prevention of abortions is of course more satisfactory than remedial treatment, and a nurse may be very helpful in this respect, by explaining the underlying causes to the patients in her care, and winning their cooperation in preventing a deplorable accident.
Preventive treatment really begins very early. In the chapter on menstruation we referred to the importance of a young woman’s ascertaining the cause of painful menses, in the interest of good obstetrics, since inflammation of the uterine lining or a uterine misplacement might be responsible not only for the dysmenorrhea, but if neglected might, later, be factors in causing interrupted pregnancies. The correction of such physical defects, then, no matter when they are discovered, is an important step in preventing abortions.
A misplacement may be corrected, frequently, by means of a pessary, though suspension is done in some cases; an inflamed lining, which provides unsatisfactory lodgement for the ovum, may be removed by curettage. The new lining which replaces the old one is sometimes capable of receiving and holding the ovum.
There are also some more immediate preventive measures. A woman who is pregnant for the first time, and who, therefore, does not know whether or not she is likely to abort, should avoid such risks as fatigue, sweeping, lifting or moving heavy objects, running a sewing machine by foot, running, jumping, dancing, traveling or any action which might jar or jolt her during the first sixteen or eighteen weeks of pregnancy.
On the other hand, there are many groundless beliefs concerning the causes of abortions which the nurse may well dispel. Purgatives and other drugs have much less effect in causing abortions under normal conditions than is generally believed. But with a patient who has very irritable uterine muscles, such a drug as quinine, for example, may act as the last straw in producing 169an abortion which would almost certainly have been brought on by some other slight stimulation had the drug not been taken. Nor can reaching up, or sleeping with the arms over the head, possibly separate the embryo from the uterine lining, yet many women believe that they can.
In the case of an expectant mother who has had an abortion, even more precautions than I have suggested will have to be taken, for she is in greater danger of aborting than is a woman who has not had this experience. It is of prime importance that she have the cause of her previous abortion discovered, and if possible, corrected. In addition to this, she should be particularly careful to observe precautionary measures as she approaches the stage of her pregnancy at which the previous abortion occurred. The accident is most likely to be repeated at about the same time, or a little earlier, in each succeeding pregnancy. The patient should remain quietly in bed for at least a week before and after the time when an abortion is feared.
Complete rest and physical relaxation are such effective preventive measures that patients with a tendency to have abortions, who have been willing to stay in bed throughout practically the entire period of gestation, have gone through pregnancy without interruption, and been delivered of normal babies at term. As out-of-door exercise is clearly impossible in such cases, it is imperative that the patient keep her room particularly well-ventilated all of the time, and, under the doctor’s direction, have massage or bed exercises.
Since abortion seems to be due, so often, to excessively irritable uterine muscle fibres that respond to even slight stimulation, a patient who is known to have difficulty in carrying a child to term is usually advised to avoid the marital relation throughout pregnancy.
Some patients with defective uterine lining will have slight bleeding for a long time, possibly throughout the entire period of pregnancy, because a small area of the placenta has separated, leaving, however, a sufficiently large attached area to nourish the fetus. Such women should, of course, be under a doctor’s care and sedulously avoid all shocks to the uterine musculature, for the separated area may very easily be increased to such a size 170that the fetus will be unable to secure adequate nourishment, and die as a result. And the mother’s life, too, may be endangered by hemorrhage from the separated surfaces.
To sum up in a word, we may almost say that, after pregnancy has begun, preventive treatment consists of rest and avoiding physical shocks, particularly during the first sixteen or eighteen weeks and at the time when menstruation would occur were the woman not pregnant.
Treatment, in the different degrees of abortion, employed by most physicians, is usually along some such lines as the following:
1. Threatened. A threatened abortion is one in which there is some loss of blood, associated with pain in the back and lower abdomen, but without expulsion of the products of conception. The treatment, as a rule, is absolute rest in bed and the administration of powerful sedatives.
2. Incomplete. An incomplete abortion is one in which the fetus is expelled but the placenta and membranes remain in the uterine cavity. The treatment is removal of the retained tissues, followed by the same care that is given during the normal puerperium. Prompt action in completing the delivery is important because of the hemorrhage that usually persists until the uterus is entirely emptied of its contents. Since the pregnant uterus is very soft, the retained membranes are more often removed manually than instrumentally, for a curette may be very easily pushed through the uterine wall, and peritonitis would be likely to follow.
3. Complete. A complete abortion, as the term suggests, is one in which all the products of conception are expelled. The treatment and care are exactly the same as are given after a normal delivery. This point cannot be stressed too strongly, for it is because so many women fail to appreciate the necessity for adequate post-partum care, that abortions are so often followed by ill health and invalidism.
Many doctors follow these various remedial measures with a search for the cause of the abortion just past, in order that it may be corrected if possible and recurrent abortions prevented.
A missed abortion occurs but rarely, and is one in which the embryo, or fetus dies, and is retained within the uterine cavity for months, or even years, sometimes without any unfavorable results to the mother. In these cases, symptoms of abortion sometimes appear and then subside without any part of the uterine 171contents being expelled. In other cases there are no signs except that the abdomen stops growing. There are cases on record in which the fetus has become mummified and others in which it has been partly absorbed by the maternal organism.
In addition to abortions which occur spontaneously there are also induced abortions, and these are designated as therapeutic or criminal, according to the motive for the induction.
Therapeutic abortions are resorted to when the patient’s condition is so grave that it is apparently necessary to empty the uterus in order to save her life. Such a condition may exist, for example, when pregnancy is complicated by pulmonary tuberculosis, heart disease, toxemia, hemorrhage or some condition which is inherent to pregnancy. An abortion induced under these circumstances is countenanced by law, as it is performed to prevent the loss of life from disease; but an abortion is not legal if brought on to save the woman from suicide, because of her unwillingness to become a mother.
The Catholic Church, however, teaches that it is never permissible to take the life of the child in order to save the life of the mother. It teaches that, even according to natural law, the child is not an unjust aggressor: and that both child and mother have an equal right to life.
There is apparently no reason why a therapeutic abortion should be followed by ill health, for, since it is performed openly, it is done under clean, and otherwise favorable conditions, and the patient is given adequate after-care. It is only because the reverse conditions frequently prevail: the unclean delivery and subsequent neglect which go hand in hand with the secrecy of illegal performance that abortions are followed so often by disaster.
As to the legal aspect of the matter, the laws relating to therapeutic abortion vary in the different states. But they are fairly uniform in their intent, and make quite clear the difference between this procedure and the induction of abortion for any reason other than medical necessity.
Dr. Slemons writes of the seriousness of criminal abortion in no uncertain terms, in “The Prospective Mother.” “At Common Law” (an inheritance from England) he tells us, “abortion 172is punishable as homicide when the woman dies or when the operation results fatally to the infant, after it has been born alive. If performed for the purpose of killing the child, the crime is murder; in the absence of such intent, it is manslaughter. The woman who commits an abortion upon herself is likewise guilty of the crime.”
Premature Labor is the termination of pregnancy after the seventh month, but before term. Premature births are much less frequent than abortions or miscarriages. They usually occur spontaneously, but are sometimes induced for therapeutic purposes, or from criminal motives.
The premature baby’s chances of living are directly proportionate to the length of its uterine life. This has already been stated, but will bear repetition in view of the widely current fallacy that a seven-months’ baby is more likely to live than one born after eight months of pregnancy. The facts are that as a rule, the nearer pregnancy approaches term, the more likely is the baby to survive, provided it weighs four pounds or more, and is forty centimeters or more in length. A smaller baby than this has but a slender chance to live.
We ordinarily designate as premature any baby that weighs between 1500 and 2500 grams, or measures between thirty-six and forty-five centimeters in length, and consider such a baby has a favorable outlook if given special care. This special care of premature babies will be described in connection with the care of the baby.
Causes. Syphilis was formerly thought to be a common cause of abortion, but although this has been disproved by recent investigations, the disease is still regarded as a frequent cause of spontaneous premature labor. In fact, Dr. Williams considers syphilis the most frequent single cause of premature births, and regards the birth of a dead, macerated fetus, or a history of repeated premature labors, or stillbirths, as strongly suggestive of syphilis.
“In my experience,” he says, “the recognition and treatment of this disease is the most important matter in connection with the prophylaxis of premature labor.... Some idea of the importance may be gained from the fact that in a series of 334 premature 173labors, I found that syphilis was the etiological factor in over 40 per cent., while toxemia, placenta prævia and fetal deformity were concerned in 8.6 and 3.3 per cent., respectively. Sentex, who studied 485 cases in Pinard’s clinic arrived at similar conclusions and found the underlying cause to be syphilis in 42.7 per cent., albuminuria in 10.8 per cent., and abnormalities of the fetus in 11.1 per cent.”[3]
Other causes of premature births are the toxemias of pregnancy, chronic nephritis, diabetes, pneumonia, typhoid fever, organic heart disease, continuous overwork during the latter part of pregnancy, and such poisoning as lead and illuminating gas, while of alcoholism, Dr. Ballantyne says, “prematurity of birth is an undoubted result.”
Another important cause of premature births, of comparatively recent recognition, is previous operation upon the cervix, particularly high amputations; while placenta prævia and malformations of the fetus, or monsters, are also reckoned with as causative factors. Hydramnios sometimes brings on a premature labor by so distending the uterus as to stimulate contractions.
Labor is sometimes induced prematurely when this procedure may be expected to relieve an abnormality or complication which threatens the life of the mother or baby, or both. Some of the indications for this course are: seriously overtaxed heart or kidneys; a marked disproportion between the size of the child’s head and the mother’s pelvis, or a fetus that has been dead for two weeks or more. However, the reasons for it and the methods employed in inducing labor will be discussed more at length in the chapter on obstetric operations.
A therapeutic induction of premature labor, like a therapeutic abortion, is not of itself usually considered any more serious for the mother than a normal delivery, since it can be performed with care and cleanliness, qualities not usually associated with the work of practitioners who are willing to do criminal operations.
Treatment. The nursing care of the patient after a premature labor is the same as that given after a normal delivery. Much invalidism would be avoided if all women could be convinced 174of the importance of staying in bed just as long, and having just as good care after a premature as after a full-term labor. The difficulty of so convincing her is perhaps due to the fact that the small, premature child is expelled more quickly and less painfully than a baby at term and there is comparatively little blood lost in the course of its birth.
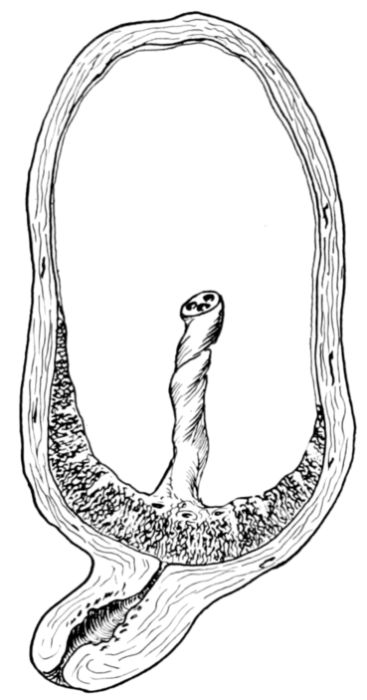
Fig. 44.—Diagram of centrally implanted placenta prævia.
Ante-partum hemorrhage, which is a hemorrhage occurring before delivery, is another serious complication of pregnancy. During the early months, hemorrhages are usually due to abortion, menstruation or lesions of the cervix and are not severe as a rule. But during the last three months hemorrhages are almost invariably due to placenta prævia or premature separation of a normally implanted placenta, and are often profuse.
Placenta Prævia is one of the most serious conditions met with in obstetrics, the maternal mortality being about 40 per cent. and the baby death rate about 66 per cent. The frequency with which it occurs is variously estimated as from one in 250 cases to one in every 1000.
In order to understand what is happening to the patient in this condition, we must go back to the question of the implantation of the ovum. We learned that, as a rule, after the ovum entered the uterus it attached itself to a point in the uterine lining high up on the anterior or posterior wall. Unhappily, the position of this point of attachment is a mere matter of chance, and the ovum sometimes, but not often, is implanted so far down toward the cervix that as the placenta develops at that site it partially or completely overlaps the internal os. It is the extent to which the placenta grows over the cervical opening that determines whether it is of the central, partial or marginal variety.

Fig. 45.—Partial placenta prævia. Section of uterine wall and cervix showing that part of the maternal surface of the placenta which extends over the cervical opening and is exposed by dilation of the internal os, with an escape of blood from the open vessels as a result. Drawn by Max Brodel. (From “The Treatment of Placenta Praevia,” by William B. Thompson, M.D.—Johns Hopkins Hospital Bulletin, July, 1921.)
176A centrally implanted placenta prævia (Fig. 44) is one which entirely covers the os; a partial placenta prævia (Fig. 45), as the name suggests, only partially covers the opening, while if it is implanted so high up that only its margin overlaps the os, it is designated as marginal placenta prævia. (Fig. 46.)
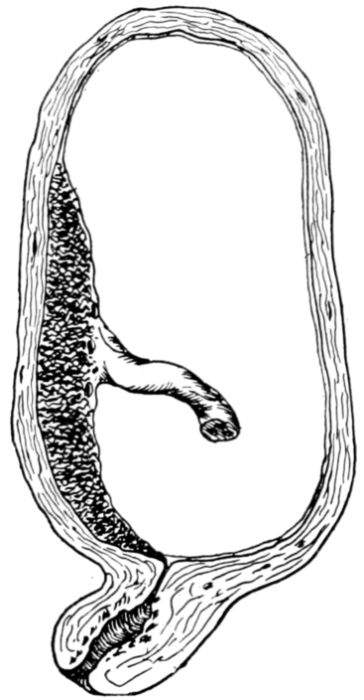
Fig. 46.—Diagram of marginal placenta prævia.
Another classification groups all placenta prævia as complete or incomplete, the latter comprising the partial and marginal varieties, as well as the lateral which is so attached that it does not quite reach the edge of the internal os. However, as these terms do not differ widely and are clearly descriptive, the differences are of no great moment to the nurse, as the treatment is practically the same and the nurse’s duties quite the same for all varieties.
Cause. Not much is definitely known about the cause of placenta prævia, but it is evident that multiparity is a factor, since the condition is found about six times as frequently among women who have borne children, as it is among those who are pregnant for the first time. A diseased uterine lining is probably the fundamental cause, and this may explain why the trouble is found more frequently among the poorer classes, since such women as a class have less skilled medical attention than those in better circumstance.
One theory is that an old endometritis results in a very unfertile soil for the implantation of the ovum and as a result the ovum migrates to other parts of the uterine cavity in its search for a more favorable site, and comes to lodge near the lower segment.
Symptoms. The symptom of placenta prævia is hemorrhage, 177occurring during the latter part of pregnancy or at the onset of labor. The cause of the hemorrhage is the separation of that part of the placenta covering the internal os, when the latter dilates, thus presenting an exposed, bleeding surface. The hemorrhage is usually so profuse that unless it is controlled, both mother and child may bleed to death.
Treatment. Unhappily there is no preventive treatment for placenta prævia, beyond that which is included in treatment for endometritis, and good care during the preceding puerperium.
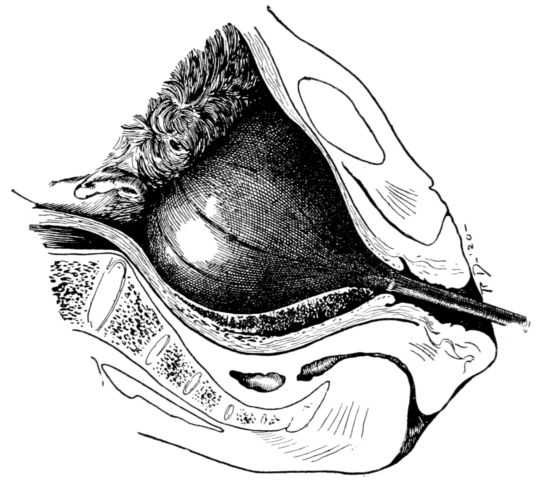
Fig. 47.—Position of Champetier de Ribes’ bag to stop hemorrhage, from placenta prævia, by pressure.
Since the great danger in this complication is from hemorrhage the doctor’s principal effort is directed toward its control. Infection and shock are also feared but the first step is to stop the bleeding. A common method is to stimulate the uterus to contract; that necessitates the removal of its contents, or the induction of labor.
The separation of the placenta leaves open, bleeding vessels in the uterine wall and placenta, which can only be closed by pressure, until the uterus contracts on its own vessels. The doctor sometimes makes pressure with tampons of gauze, by rupturing the membranes and bringing down the presenting part of the child to press against the bleeding surface, or by introducing a 178rubber bag into the cervix and pumping it full of sterile water. (Fig. 47.) By means of its weight and downward traction, this bag presses against the bleeding areas and thus checks the hemorrhage. It also tends to dilate the cervix, after which the baby is sometimes born spontaneously and sometimes delivered artificially.
Premature Separation of a Normally Implanted Placenta. A placenta prævia, as has been explained, is abnormally situated. But it sometimes happens that a placenta that is normally placed will separate prematurely, with hemorrhage as the inevitable result. Such a hemorrhage is termed “accidental” to distinguish it from the unavoidable bleeding caused by a placenta prævia. If the blood escapes from the vagina, the hemorrhage is called “frank,” but if it is retained within the uterine cavity it is called a “concealed” hemorrhage.
Causes. Endometritis is probably an underlying cause, though very little is definitely known on the subject. Previous pregnancies are believed to be a factor, as this accident occurs less often among women who are pregnant for the first time than among those who have borne children, and also as the frequency of the hemorrhages apparently increases with the number of previous pregnancies. Nephritis is believed to be a possible cause, as well as anemia, general ill-health, toxemia, physical shocks, and frequently recurring pregnancies.
Symptoms. In a frank hemorrhage, the chief symptom is an escape of blood from the vagina, occasionally accompanied by pain. A frank accidental hemorrhage occurs once in about every two hundred cases, according to Dr. Edgar’s estimate, but, although more frequent than placenta prævia, it is much less serious.
A concealed accidental hemorrhage, on the other hand, is an extremely grave complication for both mother and child, for according to observations made by Dr. Goodell, the death rate is 51 per cent. among mothers and 94 per cent. among babies.[4] The symptoms are acute anemia, abdominal pain, a general state of shock, and usually an increased enlargement of the uterus. The blood may be retained between the uterine wall 179and the placenta or membranes, or its escape from the vagina may be prevented by the child’s presenting part fitting tightly into the outlet and acting as a plug.
Treatment. The treatment of a frank hemorrhage depends upon its severity. If the bleeding is only moderate, labor is ordinarily allowed to proceed normally and unassisted. If the bleeding is profuse, however, the patient is usually delivered promptly.
The treatment for a concealed hemorrhage consists of emptying the uterus speedily in order that the muscles may contract and stop the bleeding by closing the uterine vessels; and of treating the accompanying shock which may be almost, if not quite, as serious as the hemorrhage itself.
It is very disappointing to have to realize that there is very little that a nurse may do, before the arrival of the doctor, for a patient who is having an ante-partum hemorrhage. As has been explained, it is often necessary to pack the cervix or introduce a bag, for the purpose of stopping the bleeding by pressure, and of stimulating the uterine contractions which will expel the child and empty the uterus. These measures are surgical operations and quite evidently the nurse cannot attempt to perform them. She can, however, put the patient to bed and have her lie flat, without a pillow, and, partly for the mental effect upon the patient, apply ice-bags or compresses to her abdomen. As nervousness and excitement only tend to increase the bleeding, the nurse has an excellent opportunity to try to soothe and quiet a frightened woman, and convince her that she can help herself, in this emergency, by quieting her mind and body.
Pending the doctor’s arrival, the nurse should have a large receptacle of water, boiling, to sterilize the instruments and bags that he may want to use; clean towels and sheets, a nail brush, hot water, soap, and a basin of an antiseptic solution for his hands.
There is probably no group of complications which prove to be more baffling to the obstetrician than the toxemias of pregnancy. 180Certainly they are challenging the best efforts of many earnest investigators, for it is known that the toxemias cause some of the gravest conditions that arise during pregnancy, and they are suspected of being the underlying cause of still others which are as yet unaccounted for.
Comparatively little is known of the origin of the toxemias, except that they are due to pregnancy. But happily, a good deal is known about preventing them, and also about relieving them, particularly in the early stages; accordingly many mothers and babies are saved who otherwise would perish.
The entire subject of the prevention and treatment of these disorders will be somewhat simplified for the nurse if she will recall the general question of the adaptations of the mother’s physiology during pregnancy. She will then remember that there were certain alterations of function which were necessary to keep the maternal organism normal, while it bore the strain of supplying nourishment to the fetus from its own blood stream, and received in turn the broken-down products of fetal activity. If these adaptations are insufficient to meet the demands made upon the maternal organism, a serious toxic condition may result.
To put the matter briefly, there is in the toxemias of pregnancy a disturbance of the mother’s metabolism, involving the liver and kidneys, and a resulting retention within her body of something which should be excreted. The retention of this material, which may be of fetal or maternal origin, or both, may give rise to symptoms which range anywhere from slight headache or nausea to coma, convulsions and death.
Beyond these general facts, there seems to be deep obscurity concerning the cause of this group of complications, of which pernicious vomiting, pre-eclamptic toxemia and eclampsia are the most widely and generally recognized.
While nephritic toxemia and acute yellow atrophy of the liver cannot be designated, quite accurately, as toxemias due to pregnancy, they are usually included in this group. This may be because they are toxemias which have many features in common with those of pregnancy, as to symptoms and treatment, and 181because of the frequency with which they appear coincidently with pregnancy, although not always due primarily to that state.
From the nurse’s standpoint, it will perhaps be as well to regard all of the toxemias of pregnancy as manifestations of the same general disturbance, which vary according to the stage of pregnancy at which they appear, and which differ from each other chiefly in severity, or degree, rather than in kind.
In all cases the patients need to have their toxicity lessened by dilution, and this is accomplished by giving fluids, copiously, and by increasing elimination by promoting the activity of the skin, kidneys and bowels. And since the nervous system is irritated by the toxins, sometimes slightly and sometimes profoundly, the patient must be protected from outside irritation and stimulation. This means quiet; a soft light, or even darkness in the room; gentle handling; and with mildly toxic, conscious patients, a pleasant, reassuring and encouraging manner. With those who are unconscious, each touch must be the lightest and gentlest possible.
These are the main features of the nursing care: forcing fluids and keeping the patient warm and quiet. They offer the nurse wide scope in adjustment and adaptation to each patient, according to her immediate condition and to the methods of the physician in charge. There is a difference of opinion among doctors as to details of treatment, but the fundamentals of the care are the same. In taking up, in turn, these manifestations of disturbed metabolism during pregnancy, we find that vomiting is the first to appear.
Pernicious Vomiting of Pregnancy usually occurs during the first three months. We learned in the preceding chapter that a milder form of the malady, known as “morning sickness,” is present in about half of all pregnancies. This mild type ordinarily consists of a feeling of nausea, possibly accompanied by vomiting, immediately upon raising the head in the morning, and a capricious appetite. It appears at about the fourth or sixth week and subsides in the course of a few weeks, sometimes after no more care than the nursing which was described, leaving the patient none the worse as a result of the attack.
182With some women, however, the distress does not disappear in this prompt and satisfactory manner, in which case it is described as “pernicious vomiting.” The nausea in the morning may then persist for hours; it may occur later in the day, or even at night; it may come on during a meal and consist of a single attack of vomiting, after which food is taken and retained; or it may be so persistent that the patient will be unable to retain anything taken by mouth at any time of the day or night. Such a condition, is, of course, serious, and may terminate fatally. The patient may become exhausted from lack of food or because of the toxic condition which is responsible for the vomiting, or both.
There seem to be three possible classifications of pernicious vomiting: (1) One of reflex origin, (2) one of neurotic origin, and (3) one due to a toxemia, resulting from disturbed metabolism. Not all physicians accept the possibility of all of these factors, however, for while some recognize both toxemia and neuroses as causes, they question the possibility of a reflex cause. Others believe that all nausea of pregnancy, from the mildest to the most severe form, is of toxic origin, while still others contend that even the severest pernicious vomiting is always neurotic. However, as toxicity under any conditions is very likely to give rise to nervous symptoms, and as a nervous, unstable woman may be made very ill by a slight degree of toxicity, it may be that both factors sometimes enter into the causation of this disorder.
Reflex vomiting. Those who subscribe to the theory of reflex vomiting believe that it may result from the irritation caused by a retroverted uterus, or occasionally by an ovarian cyst, an erosion on the cervix or by adhesions.
The treatment for reflex vomiting, quite obviously, consists of correcting the disturbing condition, whatever it may be, after which the nausea usually subsides in a short time. The nurse should take care that her patient resumes a regular diet very gradually, even after the cause of the nausea has been removed, for the stomach has become irritable and the vomiting habit, both mental and physical, though easily established, is usually broken up with considerable difficulty. Breakfast in 183bed; concentrated liquid foods or easily digested solids, particularly carbohydrates; aerated waters; cold fruit juices and cracked ice are easy to retain and tend to allay nausea.
Neurotic vomiting. Severe vomiting which is due to some kind of mental stress or suffering, and commonly called “neurotic vomiting,” is not always so easily relieved. In the opinion of many psychiatrists the vomiting frequently constitutes a protection, or possibly a protest, which the patient has developed subconsciously, because of some reason for fearing, or not wanting, to become a mother.
It is difficult to outline the nursing care of such patients with any degree of precision, as no two can be cared for in quite the same way. While in some cases the patient is a selfish, overindulged woman who objects to motherhood because of its inconveniences, in others, she is tortured by fear of inability to go through her pregnancy successfully, though sincerely wanting to; or she may be bewildered and overwhelmed by the prospect of the dangers of childbirth and responsibilities of motherhood, a truly pathetic figure whose distress may often be greatly relieved by the nurse who has enough insight to grasp the situation. As I have discussed this subject more at length in the chapter on mental hygiene, I shall say only a word here, as a reminder that the nurse will need all of the tact, resourcefulness, sympathy and understanding which she is capable of offering, if she is to give real help to some of her patients who suffer from neurotic vomiting.
In addition to the mental nursing, which will be necessary, the patient also needs physical care, for though her trouble may be of emotional origin, she is, nevertheless, physically ill. As a rule, the best results are obtained by putting the patient to bed and separating her from her family as completely as possible. A daily routine should be adopted and rigidly observed, and the patient repeatedly assured that the course being followed will end in recovery.
It is usually considered advisable not to offer food by mouth, in the beginning, but instead to give nourishment, as well as large amounts of saline and sugar solutions by enemata, during the first few days. One routine is to give 500 cubic centimetres 184very slowly, every six hours at first, gradually decreasing the treatments to one a day as the patient improves. The rectum is irrigated with a simple enema, once daily, immediately preceding one of the injections, consisting of an ounce of dextrose or glucose and one dram of salt to a pint of water.
Small amounts of liquid nourishment are finally given by mouth, and given frequently, the quantity being increased gradually as the patient improves. Very light and easily digestible solid foods, chiefly carbohydrates, are added by degrees, and in the end, five or six small meals, rather than three full ones, are given in the course of the day.
In some cases the patient is induced to drink, daily, two or three quarts of sugar solution (an ounce of lactose to a pint of water), and to nibble at will on olives, walnuts, crisp crackers, or some such articles of food, which are kept within reach on her bedside table. These are usually retained, excepting in very severe cases, to the patient’s great encouragement.
The duration and severity of the attacks vary widely. Some patients are very ill and for a long time, even requiring an abortion before showing signs of improvement, while others recover in a few days if wisely managed. If a patient once suffers from neurotic vomiting, she is very likely to have it in subsequent pregnancies, particularly if the circumstances of her life remain unaltered.
Toxemic vomiting is regarded by some doctors as a very grave and very rare complication of pregnancy, which is usually fatal; by others as simply a severe form of the very common “morning sickness,” which they believe is always toxic, no matter how mild; while still others, as already stated, doubt the occurrence of such a condition as toxemic vomiting of pregnancy. I mention these differences of opinion in order that the nurse may be aware of their existence and be prepared to adjust herself whole-heartedly to the different methods of treatment for which they are responsible. For no matter what else may vary, the earnestness and sincerity of the nurse’s attitude must be a veritable Gibralter of reliability.
The chief symptoms of toxemic vomiting, in addition to persistent vomiting, as described by those who recognize its 185occurrence, are coffee-ground vomitus; a diminished amount of urine, possibly containing albumen, acetone bodies and casts; coma and sometimes convulsions. The disease may run its course swiftly and the patient die in a week or ten days, or it may persist less acutely for weeks, in which case there is extreme emaciation and prostration. In those cases which come to autopsy there is a definite and characteristic, central necrosis of the liver lobule.
The treatment and nursing care vary widely because so little is definitely known about the cause, and because of the varieties of theories concerning it which are held by different obstetricians. Some believe that prompt emptying of the uterus is about the only course which is effective, while others feel that because of the probable toxicity of the patient it is advisable also to stimulate all of the excretory organs. Accordingly, they give free purges, colonic irrigations, hot packs and copious amounts of sugar and saline solution by mouth, rectum, intravenously and by infusion.
Corpus luteum, too, is sometimes given hypodermically two or three times weekly. Although this treatment is not in universal use or favor, some patients seem to be given absolute relief by its administration.
A fairly typical method of treating toxemic vomiting, and of which the nursing care forms a large part is somewhat as follows: When the vomiting is only moderately severe, the patient is put to bed and isolated from relatives and friends, because of her nervousness resulting from the toxemia. She is given an abundance of very cold, 5 per cent. lactose solution by mouth in water or lemonade; from four to six ounces being given every half hour if she is able to retain it. If she is unable to take, by mouth, a total of about three litres of this solution, in the course of twenty-four hours, she is sometimes given one or two litres (of a 10 per cent. solution) by rectum by means of the drip method. At least three hours are devoted to giving this amount of fluid, the rectum being first washed out with a simple enema.
It is usually considered important to persist in giving small amounts of practically any article of food that the patient 186fancies, in order to encourage her in the belief that she can take nourishment and also to accustom her stomach to receive and retain food. Olives and nuts are particularly valuable for this purpose and are often kept on the patient’s bedside table where she can reach them and nibble on them at will. Ice cold fruits and fruit juices are useful, while strained apple sauce, ice cold, is very valuable as a starting point from which a more generous diet may be gradually developed. All foods should be very cold except broths, which should be very hot. The dietary is gradually increased to six small meals daily from which fats and proteids are omitted.
In more severe cases, or if the patient does not improve, an injection of 300 cubic centimetres of fresh 5 per cent. solution of glucose is given under each breast daily, and sometimes a mild sweat-bath, given with blankets and lasting twenty minutes. (See page 197 for sweat-bath.)
In very severe cases when the patient is unable to retain anything taken by mouth; loses weight and strength; when possibly the urine decreases in amount and contains acetone bodies and ammonia, the situation is serious and the treatment is more drastic. All effort to give fluid by mouth is abandoned and in addition to the sub-mammary injection of glucose solution, a colonic irrigation of one and a half to two gallons of sodium bicarbonate solution (from 2% to 5%) at 110° F., is given once daily by the drip method. The daily hot pack is continued; a mustard leaf is applied to the abdomen if necessary to relieve the pain and nausea; glucose solution may be given intravenously and also a nutritive enema, three times daily, consisting of a raw egg, four ounces of peptonized milk and one-half ounce of whiskey.
The method employed at the Toronto General Hospital in treating patients suffering from toxemic vomiting is outlined as follows by Dr. J. G. Gallie: “The patient is given as much as she is able to drink. A nutrient enema is given three or four times daily, consisting of six ounces of a 10 per cent. solution of glucose in saline. Bromide and chloral may have to be added to the last nutrient in the evening. A simple enema is given each morning. Nutrients are discontinued when the urine becomes 187free of acetone bodies. In more severe cases, where fluid cannot be taken by mouth, it may be supplied interstitially or intravenously, a 5 per cent. solution of glucose being used. When vomiting ceases, and solid food can be taken, the feeding is begun very carefully with small quantities of carbohydrates. Lactose is added where possible to any fluid taken. Frequent small meals are then instituted—six between 7 a.m. and 10.30 p.m., thus reducing to the smallest space of time the period of starvation during the twenty-four hours. Protein may be added to the diet when nausea is under control, but fat should be left out for some time.”
Such a course of treatment, quite evidently, is designed to relieve a toxic condition, in which increased elimination is important, and to quiet an irritable nervous system.
As the patient with toxemic vomiting is often very uncomfortable because of a bad taste and dryness of her mouth, some kind of a mouth wash which she finds refreshing should be used frequently. And since a degree of toxicity which is capable of producing such a condition as is described above will almost inevitably produce nervous symptoms, as well, the nurse’s attitude toward her patient must always be one of sympathy, encouragement and optimism.
When the patient’s condition is so desperate that pregnancy is terminated, with the hope of saving her life, ether or nitrous oxide gas, or both, is used as an anesthetic rather than chloroform, which of itself tends to produce a liver necrosis.
Pre-eclamptic Toxemia is the most common of all the toxemias of pregnancy, occurring several times in every hundred pregnancies. It develops more frequently among women who are pregnant for the first time than among those who have borne children, and one attack usually confers an immunity against a recurrence.
As pre-eclamptic toxemia usually responds to treatment, but if neglected, frequently ends in the much more serious disease of eclampsia, the imperative need of supervision and care during pregnancy are once more borne in upon us.
Symptoms. Pre-eclamptic toxemia seldom appears before the second half of pregnancy, usually not until after the sixth 188or seventh month, and the symptoms vary widely in severity. They may range from headache and nausea, so slight as to cause the patient little or no inconvenience, to coma and death.
The patient may be entirely normal for six or seven months and then notice that her rings and shoes are a little tight, because of the slight swelling of her hands and feet. Puffiness of the eyelids may appear, and other parts of the body may also be slightly swollen. Headache, dizziness, lassitude, drowsiness, depression, apprehension, nausea and vomiting are all symptoms, as also are high blood pressure and a diminished amount of urine, containing albumen. The patient frequently complains of visual disturbance, which may be only a slight blurring, but in severe cases may amount to total blindness.
Other symptoms, when the condition is grave, are epigastric pain; rapid pulse; extreme nervousness and excitement, which may amount almost to insanity; or drowsiness, which grows deeper and deeper until the patient sinks into a coma. Under such conditions, she may die without recovering consciousness, but more frequently, eclampsia ensues. The child may perish as a result of the toxemia and a dead, premature baby be born.
Prevention is of course, the most important aspect of the treatment and is accomplished by means of the pre-natal care and supervision which were described in the last chapter. In this connection must be mentioned again the danger, during pregnancy, of overeating. It is more and more frequently observed that toxemic seizures follow in the wake of a single, large, heavy meal, such as one is so likely to take at Thanksgiving or Christmas time. This is particularly true of patients who have had nausea or who have even slightly disabled kidneys, which, though able to meet the ordinary demands made by pregnancy, are inadequate to cope with the sudden strain imposed by a large meal. In such a case, toxic materials which should be excreted are retained within the body, and the familiar symptoms of toxemia are the result.
Much the same condition is produced by the patient’s getting wet or chilled. The excretory function of the skin is interfered with, under such circumstances, and the kidneys are unable to 189do enough extra work to make up for the skin’s failure, and again toxic material is retained, instead of being excreted.
Treatment and Nursing Care. As might be expected, the details of treatment and nursing care of a pre-eclamptic patient vary with different doctors and with the severity of the attack. But the essentials of treatment, the country over, may be summed up as rest and elimination, coupled with close watching for unfavorable symptoms.
The surest way to have the patient really rest is to put her to bed, even in mild cases, and recovery is so hastened, thereby, that she is well paid for the temporary inconvenience.
Since it is widely believed that the metabolic disturbance, in toxemia, is related to the nitrogenous part of the diet, the course usually followed in this particular is a reduction of the nitrogen intake. This is accomplished by putting the patient on a very low protein diet or a milk diet, consisting of two quarts of milk daily. This amount of milk provides adequate nourishment, for the time being, and also supplies a large part of the fluid which is needed to promote elimination. In addition to this, however, the patient is given one, or better still, two quarts of water every day, and free saline purges.
Very frequently this treatment is all that is necessary. The blood pressure falls in a few days, the albumen in the urine gradually disappears, the patient completely recovers and in due time has a normal labor.
But in more severe and less amenable cases it is necessary to increase the eliminative treatment and give copious colonic irrigations; sweat baths, in the form of hot packs or hot air baths, and even venesection and saline infusions, in order to relieve the symptoms. Sometimes, even these are not enough and the high blood pressure and albumen, which are probably the most significant symptoms, will continue. If so, and the patient grows worse, or if she simply fails to respond to the treatment, the usual practice is to induce labor. A daily output of five grams of albumen to a litre of urine, and a blood pressure of 200 millimetres are usually regarded as insistent indications that pregnancy should be terminated. Otherwise, eclampsia, always so 190dreaded, is practically sure to follow and endanger the life of both mother and child.
It may be mentioned here that the normal blood pressure, during the latter part of pregnancy, is about 120 millimetres. A gradual increase to 130, or even 140 millimetres, may not be serious, but a sudden rise or a pressure of 150 millimetres should be regarded with alarm, even though all other symptoms be absent. The reason for this is that eclampsia may, and sometimes does, occur with little or no warning except the high, or suddenly increasing blood pressure.
Eclampsia. Pre-eclamptic toxemia, as the name suggests, is a condition that frequently precedes eclampsia, and the importance of the prevention, early recognition and prompt treatment of this forerunner is due to the seriousness of eclampsia which threatens to ensue. This disease, which may be defined as a toxemia occurring before, during or after labor, is one of the gravest complications which arise in obstetrics. It is usually associated with both tonic and clonic convulsions, unconsciousness and coma.
Patients who have a tendency to kidney trouble and to digestive disturbances, such as so-called “biliousness,” are evidently likely to have eclampsia; and in eclampsia there is a peripheral necrosis of the liver which occurs in no other condition. These facts suggest that possibly when metabolism is proceeding normally, the liver converts certain material, whose retention within the body is inimical to health, into a form which the kidneys can excrete without great effort; that if the liver fails in this function, the kidneys are unable to stand the increased strain put upon them, as is evidenced by casts and albumen which appear in the urine, and the retained material gives rise to toxemia. It is possible that disturbed functions of other glandular organs, such as the thyroid, may play a part in causing eclampsia, but this, too, is only conjecture.
The frequency with which the disease occurs has been variously estimated at from one in 500 to one in 100 cases, apparently being more common in first pregnancies than subsequent ones, but more serious when occurring among women who have had children before. One attack is believed to confer an immunity, 191or, as Dr. Chipman puts it, “the woman with eclampsia vaccinates herself.” The average death rate from eclampsia is from 20 to 35 per cent. of the mothers and about 50 per cent. of the babies, except where the desired care can be given, either at home or in a hospital, when the mortality is greatly reduced. These figures vary, somewhat, according to the time of the onset, as the disease is usually more fatal if the convulsions occur before or during labor, than afterward.
Some authorities feel, however, that eclampsia is quite as fatal after, as before, labor.
Symptoms. The symptoms, as a rule, are those of pre-eclamptic toxemia which have persisted and grown more severe, accompanied by convulsions and coma. The blood pressure may be from 150 to 250 millimetres and the urine, in addition to showing many and varied casts, contains albumen, which varies in amount from a few grams per litre to more than a hundred in severe cases. In those cases which prove fatal and come to autopsy, there is always found a characteristic, peripheral necrosis of the liver, and since it is found in no other disease it definitely establishes the diagnosis. It is true that this is of no help to the poor woman who died, but it is of help to those investigators who are so earnestly studying the disease with the hope of finding its cause and cure.
Although there are frequently pre-eclamptic symptoms which have grown worse, with or without treatment, it sometimes happens that the patient has no warning discomfort and the first sign of the disease is a convulsion; or a patient who has been treated for pre-eclamptic toxemia may apparently recover, even to the extent of having the albumen disappear from her urine, and suddenly have a convulsion.
Convulsions, which are both tonic and clonic in character, occur in about 99.5 per cent. of all eclamptic cases and are very distressing to watch. They are sometimes preceded by an aura, but often are so unheralded that they may even occur while the patient is asleep. They ordinarily begin with a twitching of the eyelids; the eyes are wide open and staring and the pupils are first contracted and then dilated. The twitching extends to the muscles about the nose and mouth, then to the neck and arms, 192and so on until the entire body is convulsive. The patient’s face is usually cyanotic and badly distorted, the mouth being drawn to one side; she clenches her fists, rolls her head from side to side and tosses violently about the bed. She is totally unconscious and insensible to light, and during the seizure may not breathe beyond giving one or two struggling gasps. Her head is frequently bent backward, her neck forming a continuous curve with her stiffened, arched back. Another distressing feature is the protruding tongue and the frothy saliva, which is blood stained if the patient is not prevented from biting her tongue by the introduction of some sort of a mouth gag between her teeth.
Such is the typical eclamptic convulsion.
The attacks vary greatly in their intensity and duration. There may be only a few twitches, lasting ten or fifteen seconds or violent convulsions lasting as long as two minutes, their number and severity increasing with the seriousness of the patient’s condition. In mild cases there may be but one or two convulsions, particularly if the onset is either late in labor or postpartum. But as a rule, there are several convulsions; ten, twenty or thirty, and sometimes, though rarely, as many as a hundred.
The patient always goes into a coma after a convulsion and this also varies in length and profundity, her condition during the intervals being very suggestive of the probable outcome of the disease. If the attacks recur frequently, as they usually do in extreme cases, the patient is likely to remain unconscious during the entire interval; but she will usually awaken between attacks that are far apart, and this is regarded as a hopeful sign. The respirations are labored and noisy as a rule, and the pulse full and bounding, in which case the outlook is good. The temperature is often normal, but may go as high as 104° F. or 105° F., dropping rapidly as the attacks subside. But a weak, rapid pulse together with a high temperature, and above all, a persistently high blood pressure, no matter what the other symptoms may be, are always unfavorable.
Concerning the varied results of eclampsia, the opinion seems to be growing that if it develops during late pregnancy, labor 193is likely to set in and a premature child be born spontaneously; in some cases, however, for reasons already given, labor is induced, while in others the mother dies undelivered. The fetus may die, after which the convulsions practically always cease and the infant is often born later in a macerated state; or the patient may recover, go to term and give birth to a normal, healthy baby.
When eclampsia occurs during labor the pains usually increase in force and frequency, thus hastening delivery, after which the convulsions usually cease. It will be noted that death or expulsion of the fetus is in almost all cases followed by immediate cessation of the symptoms and by ultimate recovery.
Treatment and Nursing Care. There is so little definite information about the cause of eclampsia that there is quite naturally some difference of opinion as to the best methods of curative treatment. Unquestionably, prevention is of first importance and this is accomplished through the watchfulness and care during the antenatal period as described.
Dr. Edgar characterizes eclampsia as a preventable disease, and though an occasional case will develop in spite of preventive treatment the general results achieved tend to bear out his definition. For example, in a series of 1200 maternity cases at Bellevue Hospital during 1920, prenatal care was given to 900 women and not one case of eclampsia occurred among them, while among the remaining 300 women who had not been seen during pregnancy, there were ten eclamptics. It is but fair to bear in mind that as some of these patients were taken into the hospital because of their having eclampsia, the proportion is abnormally high. The Henry Street Settlement reports through its maternity service that there was but one case of eclampsia among 7600 women who were given prenatal care by its nurses in 1920. These figures, contrasted with the average of one case in about every 500 pregnancies, furnish astounding evidence of what can be done through prenatal care in the prevention of this one disease alone.
As to curative treatment, the variations of opinion are after all of little consequence to the nurse, for there is almost entire unanimity concerning the general principles, and it is these that shape the nursing care. Broadly speaking, they comprise effort 194to dilute the toxic material in the system, promote its elimination through the various excretory channels and quiet the patient’s nervous excitability.
Since eclampsia occurs only in connection with pregnancy, and the convulsions usually cease if the fetus dies or is born, one line of reasoning is that the most effective way to treat the disease is to terminate pregnancy. Formerly this was almost always done, and is still practised by some obstetricians. Those who do not agree with this theory contend that the eclamptic woman is a very ill woman whose nervous system is so irritated that the slightest stimulation or irritation works harm. In view of this they feel that manual or instrumental dilation of the cervix, preparatory to delivering the child through that channel, or delivery through an incision in either the abdominal wall or cervix, constitutes a shock that outweighs the advantages of emptying the uterus; therefore, that as a rule, less harm is done by noninterference, quieting the patient and increasing her eliminative functions, than by terminating pregnancy. This line of reasoning also takes into consideration the fact that from 15 per cent. to 20 per cent. of the cases of eclampsia are postpartum, indicating that convulsions may occur even after the uterus has been emptied.
The growing tendency is to adopt a middle course and treat each individual case according to the conditions and indications which it presents. Thus the same doctor will hastily induce labor in a case where the blood pressure and albumen remain alarmingly high, or increase, in spite of all efforts to reduce them, and in another case will go to the extreme of conservatism, doing nothing but quiet the patient with morphia or chloral, or both, and stimulate all of her excretory organs with abundant fluids.
But the nurse’s duties, and I may say her opportunities, for she is privileged to do much, are virtually the same no matter which course is followed, except, of course, the preparation for delivery, if this is performed.
The nurse is concerned with helping to reduce the intake of nitrogenous food, or proteids; diluting the toxines retained in the body; promoting the activity of the kidneys, bowels, liver, lungs and skin; guarding the patient against all avoidable stimulation 195from without, such as noise, light, ungentle handling and undue resistance to the patient’s convulsive movements; and protecting her from injuring herself by biting her tongue, falling out of bed or striking the wall or head of the bed during convulsions.
By striving to accomplish these general results for her eclamptic patient the nurse will aid immeasurably in saving her life.
A milk diet is the means of reducing the nitrogen intake; or in some cases even that small amount of proteid is deemed too much, and only water is given until 24 to 48 hours after the convulsive seizures have ceased. From three to five litres of these fluids should be given in the course of twenty-four hours, in order to increase elimination by way of both kidneys and skin, and it usually taxes the nurse’s patience and ingenuity to give this amount, for the patient will seldom take large quantities of fluids willingly, even when quite conscious. A surprising amount of water may be given to the sleeping or unconscious patient by dropping it into her mouth from the point of a teaspoon, taking care to give it only at those moments when she is lying quite still. If the nurse attempts to hold the restless patient’s head, or so much as places her hand upon the chin to steady it in order to give water, the irritation, though slight, may be enough to cause a return of the tossing and struggling.
Lithia water and cream-of-tartar lemonade (a teaspoonful of cream of tartar to a pint of water), are frequently given because of their diuretic and diaphoretic action; but whatever the fluid, it must be given persistently, with greatest gentleness and with care that the patient does not choke nor aspirate it into her lungs and thus possibly cause pneumonia. Food even in liquid form is not given while the patient is unconscious, because of this danger of aspiration and subsequent pneumonia.
The bowels are stimulated to greater activity by powerful purges, such as croton oil, in olive oil, dropped on the back of the tongue, or salts or castor oil given by stomach tube.
Copious colonic irrigations, alternating with hot packs so that one or the other is given every six, eight or twelve hours, according to the seriousness of the case, are frequently given and with excellent results. A colonic irrigation may be given by 196means of the Murphy drip method or through a rectal tube so contrived that a two-way flow of fluid is possible. Water, normal saline (2 drams of salt to a quart of water), or a weak solution of sodium bicarbonate (an ounce of soda to a quart of water), are all used for colonic irrigations, which are given at a temperature of 110° F., very slowly, with the receptacle for the solution placed so low that the flow is under very slight pressure. The patient should lie on her left side, in a comfortable position and be warmly covered. The tube should be introduced from 12 to 18 inches, and the stop cock arranged so that it will take from twenty to thirty minutes for each gallon of fluid to run in and out. About two gallons are usually used for the first irrigation, the amount being increased until five gallons are used each time. The beneficial effects of the colonic irrigations are two-fold, for in addition to removing the toxic material that may be in the colon and rectum, a good deal of fluid is absorbed through the intestinal wall.
The function of the lungs may be promoted by using oxygen and by keeping the air in the patient’s room fresh and constantly moving, but moving so gently that there is no perceptible draft. The nurse must remember that the skin also is an excretory organ whose function is being stimulated, and this necessitates its being kept warm.
Some obstetricians feel that it is as important to increase the excretions of the skin as of the kidneys, and that inability to induce perspiration is an unfavorable sign. Others, who disagree on this point, believe that the skin is of minor importance but that the bowels are of equal consequence with the kidneys. However, the nurse will do no harm, and will err on the safe side if she takes care to keep her patient warm and constantly protects her from being chilled, that is from exposure or changes in the temperature of her surroundings. A flannel nightgown or dressing gown will help to this end, or if neither is available, at least the patient’s chest and arms may be protected by warm bed jacket, or sweater, put on backwards and fastened at the back of the neck. This protection, together with a number of blankets, with or without hot water bags between them, will often induce a slight but constant perspiration, particularly if fluids 197by mouth are being forced at the same time. This may be all of the stimulation that the skin needs, and has the advantage of not greatly disturbing the patient, a point that cannot be too constantly borne in mind.
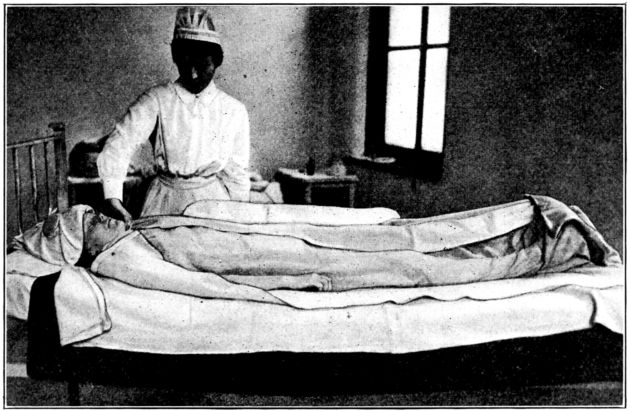
Fig. 48.—Patient in hot pack given with dry blankets and hot-water bags. The blankets are turned back in this picture to show their arrangement. (From photograph taken at Johns Hopkins Hospital.)
If something more is needed, the hot dry pack is a widely used and usually efficacious method of producing a sweat and can be given easily in the patient’s home with no more equipment than the average family possesses or can obtain. The articles needed are two rubber sheets or two heavy quilts; four blankets; three, four or five hot water bags; an ice cap or a basin with ice and two cloths for the patient’s head; a pitcher of the fluid that she is taking, and a feeding cup, drinking tube, small pitcher or a spoon with which to give it. One rubber sheet (or one of the quilts), and two blankets should be slipped under the patient, after the regular bedclothes have been loosened at the foot. If the patient is having convulsions it is better to leave on her a warm garment with sleeves to insure against her arms and chest being uncovered, otherwise the nightgown may be removed.
The patient is covered with one blanket which is tucked between 198her legs and around her body with her arms out, so that no two surfaces of the skin come in contact. The blanket on which she lies is brought up about her; another blanket should be laid over this and tucked in well about the neck, shoulders and entire body, while the fourth blanket is next wrapped around her from below. One long or two short hot water bottles should be placed on each side of the patient and one at her feet, all being placed outside the four blankets. The second rubber sheet, or quilt, is thrown over the whole and the ice cap, or cold compresses (changed every four or five minutes) placed on her forehead. (Fig. 48.)
A patient may usually be left in such a pack as this from half an hour to an hour, but since any sweat bath is more or less depressing, she must be watched constantly for evidence of exhaustion, such as a weak, rapid, irregular pulse and increased weakness, or the sudden relaxation of an active eclamptic patient.
In some instances the hot-water bags may be inadvisable, because of supplying more heat than the condition of the patient warrants; but if they are used, the nurse must remember how easily an unconscious or ill person is burned. She must watch the bags, move them frequently and take care that one of them does not slip under the patient. And while the pack is in progress, an even greater effort than ever should be made to force the fluids.
If the blankets are wrapped snugly about the patient, alternately from below and above as described, they will frequently provide all of the restraint that is necessary should she have a convulsion while in the pack. The importance of protecting her against exposure and chilling while in the pack cannot be too insistently stressed.
If I have seemed to dwell at surprising length upon rudimentary nursing details, in this connection, it is because the patient’s life literally depends upon the nurse’s conscientious and painstaking attention to these same details. The doctor may study the case ever so earnestly and order the treatment ever so wisely, but if every detail of that treatment is not thoughtfully and skilfully carried out, it may do the patient more harm than good. And on the other hand, I can think of no circumstance 199that gives the nurse deeper gratification than the almost miraculous improvement in an eclamptic patient, sometimes only overnight, after she has taxed to the utmost all of her ingenuity to make her ministrations effective.
Appliances for giving hot packs and hot-air baths are usually found in all hospitals, and the nurse will use them as directed, which obviates any necessity for describing them here. But in addition to correctly adjusting and using the appliance itself, she must watch her patient for evidence of exhaustion or shock; protect her from burns; keep cold applications on her head and give her as much fluid as possible. And when the hot pack is over, the patient must be taken from it gradually; one blanket at a time, or the heat slowly reduced, and then the greatest care taken that she is not chilled while being put into dry clothing, for she must be kept warm and perspire slightly even after the sweat is finished.
Restraint during convulsions should be as mild as possible, for resistance only increases the patient’s excitement, and sustained effort should be made to reduce it instead. To this end there are innumerable details to be considered. Every act must be performed as quietly as possible. The nurse must walk lightly and if her tread will be made softer by wearing bedroom slippers, she should wear them. She should consciously guard against kicking or striking the bed. All talking should be in low tones; doors opened and closed quietly; papers should not be rustled nor furniture scraped on the floor. The room should be as dark as is feasible and the source of light screened from the patient’s eyes.
She should be saved from biting her tongue by having placed between her teeth something that will serve as a mouth gag and still not cut nor bruise the mucous membranes. In a private home, one will find that a cork answers admirably; or the handle of a wooden spoon well wrapped with gauze or a clean handkerchief; or a small roll of bandage or clean cloth tightly rolled. Another method is to take a fresh handkerchief, or napkin, in the fingers by opposite corners, twist it slightly into a roll and force it between the teeth and tie the two corners firmly together at the back of the neck.
200Venesection. The large intake of fluids tends to dilute and eliminate the toxins which are giving so much trouble, but another very prompt and efficacious measure is to withdraw from 500 cubic centimetres to 1000 cubic centimetres of blood by venesection, according to the condition of the pulse. In preparing for a venesection the nurse will slip a small rubber, covered with a towel, under the arm that is to be opened, and scrub the inner surface of the elbow with soap and solutions according to the wishes of the doctor in charge, and cover the cleaned area with a dry sterile towel or one wet with a disinfecting solution. A sterile towel should be slipped under the patient’s arm, one laid over the arm above and one below the cleaned area so that the entire surrounding field is protected by sterile towels.
For the puncture there will be needed a sterile canula, or infusion needle, with a piece of rubber tubing attached; a sterile receptacle for the blood, usually a 1000 cubic centimetre, graduated measuring-glass; both dry and alcohol sponges or cotton pledgets; adhesive plaster, or a bandage to hold in place the small dressing which is applied after the needle is withdrawn; and a tourniquet for tight application to the upper arm to impede the return of the venous blood and thus distend the large vein to be seen near the surface of the inner curve of the arm. This vein usually may be easily pierced, without incising the skin, the canula pointed toward the hand to meet the blood stream, after which the tourniquet is removed. Sometimes it is necessary to incise the skin in order that the vein may be exposed and the needle inserted into it directly. In this case the doctor will need, in addition to the articles already mentioned, a scalpel, a pair of tissue forceps, three or four artery clamps, a needle holder, skin needles and sutures.
A venesection is practically always followed by a drop in the blood pressure and a marked improvement in the general condition.
Infusions, or subcutaneous injections of saline solutions, are also frequently given to eclamptic patients with beneficial results. About 1000 cubic centimetres at 105° F. is introduced slowly into the tissues, and the solution may be normal saline, consisting of two drams of common salt to a litre of distilled water, filtered 201and sterilized; or possibly one containing five grains each of sodium bicarbonate and sodium chloride to the litre.
The articles necessary, in addition to the soap and solutions for cleaning up the skin, are a small rubber to protect the bed; three or four sterile towels; a flask of the solution at 105° F.; sterile infusion bottle, or can, with rubber tubing fitted with a piece of glass tubing at some point in its length, through which the flow of the solution may be watched, a stopcock, and an infusion needle (I cannot refrain from cautioning the nurse to be sure that the tubing does not leak; is not collapsed and stuck together at any point along its length, and that the needle is sharp, free from rust and contains a wire as evidence of not being clogged); two hot water bottles about half full, with air expelled; a pole or stand upon which to hang the bottle; a package of gauze sponges, or squares, and narrow strips of adhesive.
The fluid is usually introduced between the breast tissues and underlying muscles; the area to scrub up in preparation being just below the breast, where the curve begins, and toward the axilla. The bottle which contains the solution should be stoppered with sterile cotton, or, if a can, covered with a sterile towel, and hung between the hot water bottles, to keep the fluid warm, and held in place with a towel pinned around them, top and bottom. (Fig. 49.)
If the nurse is to give the infusion, she should grasp the end of the needle, to which the tubing is attached, with her right hand, pierce a piece of sterile gauze; open the stop cock and allow the air and cold fluid to escape, leaving a drop on the point of the needle; lift the patient’s breast with her left hand and quickly plunge the needle in just under it. The direction of the needle should be parallel to the chest wall to insure its running below the breast tissue, and above, not between the ribs. The needle, and the gauze through which it runs, may be held in place by means of narrow strips of adhesive plaster. The stop cock should be so adjusted that the warm fluid will flow into the tissues very slowly, about an hour being required to introduce 1000 cubic centimetres. During this time the patient must be kept well covered and the solution kept at about 105° F. as some of the heat is lost in its course through the tubing. A hot water bag placed upon the bed, over a coil of the tubing, is another means of maintaining the desired temperature, but it must be watched and moved from time to time, to guard against burning the patient. In hospitals where the infusion apparatus is equipped with a heater, hot water bags are, of course not needed, but they are of practical service in a patient’s home.
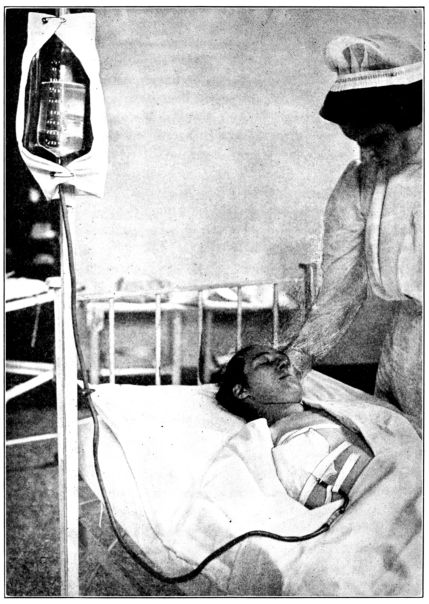
Fig. 49.—Infusion being given under breast; needle held in place by strips of adhesive and the solution kept warm by hot-water bottles suspended on each side of the infusion bottle.
203Termination of pregnancy is resorted to much less frequently than formerly, because it is believed that an eclamptic patient is particularly susceptible to infection and also that the shock of an induced labor is serious to so ill a woman.
The method of terminating pregnancy, when this is finally deemed necessary, depends upon the condition of the cervix; the size of the child; and upon the patient’s general condition. The method may be simple induction of labor, by the introduction of a bougie, if haste is not imperative; introduction of a bag; manual dilation of the cervix, if it is soft and partly obliterated; vaginal hysterectomy, or even cesarean section.
Chloroform is not used as an anesthetic, in eclampsia, nor to relieve the labor pains nor control the convulsions because of its tendency to increase the liver necrosis which is incidental to the disease.
Recovery is comparatively rapid, when it occurs. The blood pressure drops to normal; the albumen and casts disappear from the urine and all symptoms subside in from two to four weeks. (Chart 1.) And, happily, since one attack confers an immunity, the patient who recovers from eclampsia need not fear a recurrence of the disease.
Nephritic Toxemia is a serious toxemia, sometimes complicating pregnancy, and though it may occur at any time during the period of gestation, it usually develops during the latter months. As a rule, it is simply an exacerbation and accentuation of a previously existing, chronic nephritis, of which the patient may, or may not, have been aware; though in some instances the disability of the kidneys may arise during pregnancy. In many cases, so far as the kidneys are concerned, the patient is entirely normal in the non-pregnant state, and even during pregnancy, up to a certain point; then her kidneys prove to be unequal to the 204added metabolic strain of pregnancy, and signs of renal insufficiency appear.
Such a patient will suffer from toxemia, with each recurring pregnancy, the symptoms almost always appearing earlier, and with increased severity, with each pregnancy, as the permanent damage to the kidneys is increased by each successive attack.
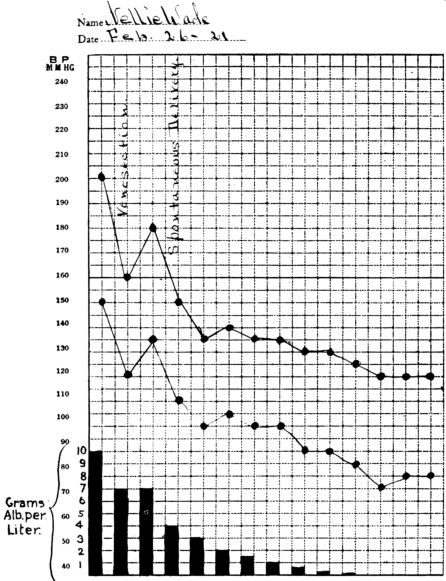
Chart 1.—Chart showing relatively rapid disappearance of albumen from the urine and return of blood pressure to normal, after delivery in eclampsia.
Symptoms. The symptoms in nephritic toxemia are practically 205the same as those in chronic nephritis: lassitude, headache, visual disturbances, edema, high blood pressure and casts and large amounts of albumen in the urine. In some instances, the patient suffers such slight discomfort that the increased blood pressure and urinary symptoms are the only precursors of coma, and possibly convulsions which cannot be distinguished from an eclamptic seizure.
As the patient may die in the coma, no matter how suddenly it develops, the value of regular urinalyses and observations upon the blood pressure, which are included in prenatal care, must once more be mentioned.
In severe, chronic cases infarcts (hemorrhagic or necrotic areas) appear in the placenta. These may be extensive enough to interfere with the nourishment of the fetus, which, being already weakened by the toxic effects of the disease, is unable to survive. As a result, nephritic toxemia is second only to syphilis in causing premature deaths. When the child dies, the symptoms usually begin to subside in a week, or possibly two, and the dead fetus is expelled.
Treatment and Nursing Care. The treatment and nursing care are virtually the same as for pre-eclamptic toxemia; rest in bed, milk diet, forced fluids, purges, and in addition, observations upon the intake and output of fluids. The output of urine will not equal the amount of fluid which the patient takes in, at first, but in those patients who improve, the amount of urine gradually increases until it equals the amount of fluid ingested. The edema and other symptoms improve, except the high blood pressure and the albumen in the urine, which sometimes persist for months. (Chart 2.)
If the patient has coma or convulsions, the treatment is the same as in eclampsia.
A patient with inadequate kidneys who has never been able to carry a child to term may sometimes achieve this coveted end by going to bed a few weeks before the period in her pregnancy when the toxic symptoms have usually appeared, taking only milk for food, drinking large amounts of water, and keeping her bowels moving freely.
It is impossible to distinguish between eclampsia and nephritic 206toxemia during an attack, but this is of no importance at the time, as the treatment of the two diseases is the same.
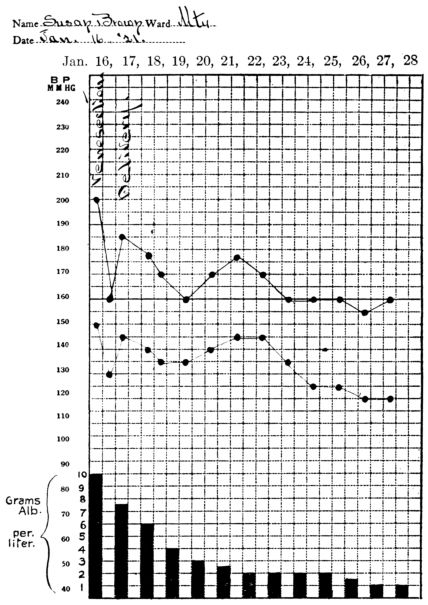
Chart 2.—Chart showing persistence of high blood pressure and of albumen in the urine, after delivery, in nephritic toxemia with convulsions.
But during the puerperium, the differential diagnosis may be made, for in eclampsia the blood pressure falls rapidly to normal and the casts and albumen disappear from the urine in from two to four weeks. In nephritic toxemia, on the other hand, although the blood pressure falls somewhat, and the albumen decreases 207in amount as the patient’s general condition improves, by the end of the puerperium the blood pressure is still elevated and casts and albumen are still present in the urine.
In eclamptic cases that come to autopsy, there is a typical, peripheral necrosis of the liver, but in nephritic toxemia there is no liver lesion.
Acute Yellow Atrophy of the Liver is one of the grave but very rare toxemias of pregnancy and though it may occur at any stage it usually appears during the latter part of pregnancy or during the puerperium. This complicating condition is not peculiar to pregnancy alone, although from forty to sixty per cent. of the cases which occur are in pregnant women.
The symptoms, which sometimes come on suddenly in a woman who previously has been entirely well, may suggest phosphorus poisoning. They are abdominal pain, headache, vomiting, and diarrhea followed in some cases by coma and convulsions, and in others by violent delirium. With these symptoms are jaundice and a diminished amount of urine, which contains albumen, casts, and usually a good deal of blood. The picture is practically that of pernicious vomiting plus jaundice and pain.
Little is known of the ultimate cause of the disease, but it produces rapid atrophic and degenerative changes in the liver, and though mild cases sometimes recover, the outcome is usually fatal. It was formerly thought that the termination of pregnancy virtually cured the condition, but the present belief is that delivery produces little or no effect. The tendency now, therefore, is simply to employ the same kind of eliminative treatment that is used in eclampsia.
Among the more serious complications of pregnancy, which are not due to that condition, but which it is important to recognize and treat early, may be included syphilis, heart lesions, pulmonary tuberculosis, thyroidism, gonorrhea and pyelitis.
“Syphilis is one of the most important complications of pregnancy,” in the opinion of Dr. Williams, “as it is the most important single cause of fetal death.”
In support of this contention, Dr. Williams reports upon a series of 10,000 consecutive deliveries which took place under his observation, and in which syphilis caused 26.4 per cent. of the 208deaths among 705 babies who died after the seventh month of pregnancy or during the first two weeks after birth. Furthermore, nearly as many more babies who were discharged alive, at the age of two weeks, died in a short time or gave evidence of having syphilis later on in life.
Believing in the importance of diagnosing and treating this disease during pregnancy, Dr. Williams subsequently made observations upon 4,000 cases in which Wassermann tests were given, and to which 421 women gave positive reactions. In this series of 4,000 deliveries, 302 babies died during the last two months of uterine life, or the first two weeks of extra-uterine existence. The relative frequency of the various causes which worked destruction in these 302 little lives is given by Dr. Williams in the following table:—
| Syphilis | 104 | cases | 34.44% |
| Dystocia | 46 | cases | 15.20% |
| Toxemia | 35 | cases | 11.55% |
| Prematurity | 32 | cases | 10.59% |
| Cause unknown | 26 | cases | 8.61% |
| Placenta prævia and premature separation | 16 | cases | 5.28% |
| Deformity | 11 | cases | 3.64% |
| Eleven other causes | 32 | cases | 10.69% |
| Total | 302 | 100.00% |
It will be seen from these figures that syphilis caused almost as many deaths as the three causes, next in order, combined.
The effect upon the child’s chances for life, of treating the expectant mother for syphilis, is suggested by comparing the results among the 421 syphilitic women who were not treated at all; those treated insufficiently by receiving but two or three doses of salvarsan and no after-treatment of mercury (because of the patient’s lack of cooperation or because treatment was instituted too late in pregnancy); and those treated satisfactorily, which meant the administration of from four to six doses of salvarsan followed by mercurial treatment continued sufficiently long to result in a Wassermann reaction that was negative, and remained so.
Among those mothers who were not treated, 52 per cent. of the babies were born dead or had syphilis; among those treated 209incompletely, 37 per cent. and among those treated until cured, syphilis caused the death of or was demonstrable in but 6.7 per cent. of the babies.[5]
The deductions to be made from these dramatic figures is, that although syphilis seems to have about the same effect upon the pregnant, as the non-pregnant woman, it constitutes a serious menace to infant life and health.
Accordingly, it is very important that every pregnant woman be given the Wassermann test as early as the third or fourth month, and any woman who gives a positive reaction should be urged to submit to intensive treatment until cured. Her compliance will apparently multiply by seven or eight her expected baby’s chances for life.
Heart Lesions sometimes present grave complications during pregnancy, or at the time of labor, because the damaged or weakened heart is unable to meet the greatly added strain put upon it at these times. Spontaneous, premature labor sometimes results from serious heart trouble, while in some cases labor is artificially induced to relieve the overworked organ of the strain that is evidently exhausting it. Quite obviously it is an important step toward the prevention of both these deplorable occurrences to have the difficulty recognized early. Rest in bed and the same kind of medical treatment that would ordinarily be given for a poorly compensating heart will sometimes enable the disabled organ to carry its load throughout pregnancy. But care is necessary.
Pulmonary Tuberculosis is so common under all conditions that it is not surprising to find it fairly often among pregnant women. Since the treatment for this disease consists largely of effort to conserve the patient’s forces and build up the bodily resistance, the drain which pregnancy makes upon the system is likely to be inimical to the tuberculous patient’s improvement. It is the general opinion, therefore, that the tuberculous 210patient grows worse during pregnancy, and is still further weakened by the ordeal of labor and the drain of nursing her baby.
Some women with tuberculosis improve during the period of pregnancy, but decline after delivery. The disease may advance rapidly in such cases and the patient succumb very early.
There is great reluctance to terminate pregnancy in tuberculous patients, except in extreme cases as a last resort, to save the mother’s life, or when, after the child is viable, its chances for life would seem to be better if it were brought into the world, because of the mother’s possible death.
Certain it is that the care which is given to the non-pregnant tuberculous person is needed to an even greater degree by the expectant mother who is suffering from this disease. And under such care, it not infrequently happens that the patient will go through pregnancy safely, and if the care is continued after delivery, and her baby not allowed to nurse, her ultimate recovery does not seem to be retarded by the experience.
Tuberculosis is sometimes, though not frequently, transmitted from the mother to the fetus; but babies born of these mothers are not likely to be robust, particularly as they must be deprived of that bulwark of early infancy—maternal nursing.
Thyroidism in pregnancy has been, and still is, so widely discussed and studied that the nurse will do well to at least take cognizance of that fact, even though no definite conclusions seem to have been generally accepted.
The toxemias of pregnancy are so shrouded in mystery, and knowledge of the functions and inter-relations of the ductless glands is still so meagre, though it is known that one, the ovary, is inevitably concerned with pregnancy, that one is not surprised to find certain investigators considering these two problems together. Nor is it surprising that directly opposite views are held concerning the relation of thyroidism to toxemia.
Since the nurse will sometimes care for toxemic patients who are treated for thyroidism, either by means of gland therapy or operative procedure, she should understand the rationale of such treatment when she meets it.
Dr. Williams says, for example, “A considerable amount of work has been done in this direction, but the consensus of opinion 211is that abnormalities of the thyroid secretion play no part in the causation of eclampsia.”
On the other hand, it will be remembered that the thyroid gland is usually somewhat enlarged during pregnancy, and in this connection Dr. Edgar observes that “The normal enlargement of this organ in the gravida has been wanting in certain cases of eclampsia.”
Dr. Edward P. Davis summarizes his opinions on the subject as follows: “Hyper-thyroidism in pregnancy produces a toxic condition in the mother, which exposes her to the danger of the toxemia of pregnancy and her child to the dangers which accompany that condition. During pregnancy, the patient has a rapid pulse, often with high tension, and attacks of breathlessness and syncope, and intense nervousness. When uterine contractions begin, the action of the heart becomes exceedingly rapid; there is difficulty in breathing and the patient is brought into great distress. It is often necessary to give prompt assistance in labor, and this may require the performance of cesarean section. The child is exposed to the risks of rapid delivery, although, if section be performed, the risk to the child is reduced to the lowest point. When the placenta is examined, it is found that certain changes have taken place in its structure which interfere with the circulation of the blood through the placenta, and may indirectly bring about the death of the fetus. The child is also subject to the same toxic conditions which the mother has had and may die from failure of the liver and kidneys or in convalescence.
“A minute discussion of the subject would be occupied largely by the question of exactly what are the poisons which cause this condition, and this question has not yet been definitely answered.
“So far as neutralizing the results of excessive action of the thyroid, it is best accomplished by rest, a diet from which meat and other heavy proteins are excluded, regulation in the action of the bowels and the avoidance of nervous excitement or undue exertion. If the action of the heart is excessively disturbed, those drugs which control cardiac action must be used. In extreme cases, morphine and atropine are given.”
212Pyelitis is a fairly common, and sometimes a very painful and serious complication arising during the latter half of pregnancy. It is an inflammation of the pelvis of the kidney, most frequently the right, caused by a damming back of urine, because of pressure of the enlarged uterus on the ureter where it crosses the pelvic brim; and by infection, which may travel up from the bladder or be conveyed by the lymph and blood streams, frequently from the intestines. The colon bacillus is the commonest offender, though the streptococcus, gonococcus or even the tubercle bacillus may be the cause.
Frequently the patient will be entirely well, aside from a slight irritability of the bladder causing frequent micturition, and suddenly have paroxysms of acute pain in the region of the kidney, which may be swollen and very painful on palpation. She will have fever and sometimes chills and a catheterized specimen of urine will contain pus and bacteria. The kidney may suddenly empty itself of pus after which the pain and swelling will subside, only to recur when the pus accumulates again.
The treatment is rest in bed, a bland diet and an abundance of milk and water to drink. As the infection is often of intestinal origin, drugs are usually given to prevent intestinal fermentation and keep the bowels moving freely. Sometimes, though rarely, when the patient does not improve under treatment, pregnancy is terminated to relieve the pressure on the ureter and thus drain the diseased kidney by permitting an unobstructed flow of urine.
The tendency of the disease is to subside spontaneously, but sometimes it is necessary to incise and drain the kidney, or even to remove it; while in others the infection is so virulent that the patient dies of septicemia.
Gonorrhea during pregnancy may cause great discomfort in the shape of irritation and itching of the vulva, or even excoriation of the mucous membrane, and sometimes abscesses of the vulvovaginal glands. Occasionally the infection reaches the decidua and causes an abortion. But the chief danger in gonorrhea is that, after delivery, if the disease has remained uncured, the organisms may travel up from the vagina to the uterine cavity and tubes, and there set up an inflammation, or possibly cause 213a general postpartum infection. The greatest danger to the child is that its eyes may become infected during the passage of the head through the birth canal. This is the reason for the very great care that is taken of the eyes of the newborn, which will be described in a later chapter.
It is very important, therefore, for the sake of both mother and child, that gonorrhea be discovered early, for treatment started at this stage is often attended by very gratifying results, as the disease may be entirely cured before it is able to invade the uterus and tubes. This is because the closure of the internal os, by the membranes, converts the vagina and cervix into more or less of a cul-de-sac, to which the infection is restricted. Being thus localized, it may often be eradicated with relatively little trouble.
The yellow vaginal discharge, characteristic of gonorrhea, may become profuse and purulent. It is removed by means of low, very gently given douches. Tampons and vaginal suppositories are sometimes used, while abscesses and abrasions are given appropriate surgical treatment.
The nurse must observe the strictest technique while caring for these patients because of the danger of infecting herself and others with the discharges. She should wear a gown and rubber gloves when giving douches or dressing diseased vulva, and because of the possibility of contamination by splashing fluids, she should hold her head well to one side in addition to protecting her eyes with goggles. All utensils for each patient should be isolated and they should also be washed and boiled after each time that they are used.
214“Lying-in is neither a disease nor an accident, and any fatality attending it is not to be counted as so much per cent. of inevitable loss. On the contrary, a death in child-bed is almost a subject for an inquest. It is nothing short of a calamity which it is right that we should know all about, to avoid it in future.”
CHAPTER X. PRESENTATION AND POSITION OF THE FETUS. Breech, Head, Face, and Vertex Presentations. Longitudinal and Transverse Presentations. Position of Fetus. Time of Engagement. Methods of Ascertaining Position and Presentation of Fetus. Abdominal Palpation. Vaginal Examination. Rectal Examination. Auscultation of the Fetal Heart.
CHAPTER XI. SYMPTOMS, COURSE, AND MECHANISM OF NORMAL LABOR. Onset of Labor. Three Stages of Labor.
CHAPTER XII. NURSE’S DUTIES DURING LABOR. General Principles of Treatment and Nursing Care. Psychology of the Patient. Preparation for Vaginal Examination or Delivery. Nurse’s Duties during First Stage. Second Stage. Maintaining of Surgical Cleanliness. Immediate Care of the Child. Resuscitation of New-born Child. Third Stage. Immediate Aftercare of the Patient. Nurse’s Duties if the Doctor Is Delayed. Prolapsed Cord. Post-partum Hemorrhage. Obstetrical Anesthesia: Chloroform. Ether. Nitrous Oxide Gas Analgesia. Twilight Sleep. Complete Anesthesia.
CHAPTER XIII. OBSTETRICAL OPERATIONS AND COMPLICATED LABORS. Conditions Giving Rise to Operations. Preparation for Operation in the Home. Perineal Lacerations. Episiotomy. Breech Extraction. Version. The Use of Forceps. Symphysiotomy. Vaginal Hysterotomy. Cesarean Section. Ruptured Uterus. Destructive Operations. Induced Abortions and Premature Labors. Accouchement Forcé.
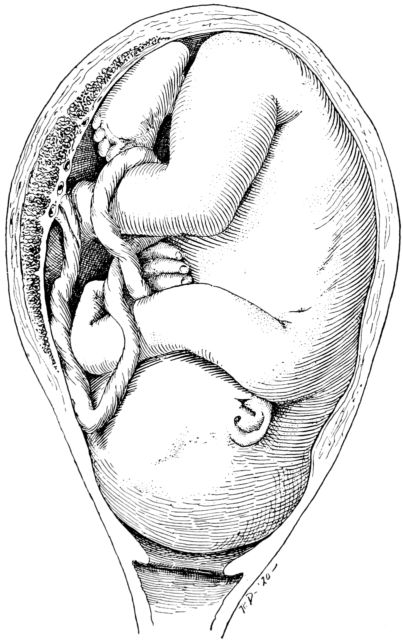
Fig. 50.—Most frequent attitude of fetus in uterine cavity, at term.
Returning for a moment to the pregnant uterus at term, we find it to be a thin-walled, muscular sac containing the mature fetus, attached by means of the umbilical cord to the placenta 218and floating in the amniotic fluid, which is contained within a sac formed by the amniotic and chorionic membranes.
The average fetus at term is about 50 centimetres long, weighs about 3250 grams and is curved and folded upon itself into an ovoid mass, occupying the smallest possible space. (Fig. 50.) Its most frequent attitude is with the back arched; the head bent forward, with chin resting upon chest; arms crossed upon chest below chin; thighs flexed upon abdomen and knees bent.
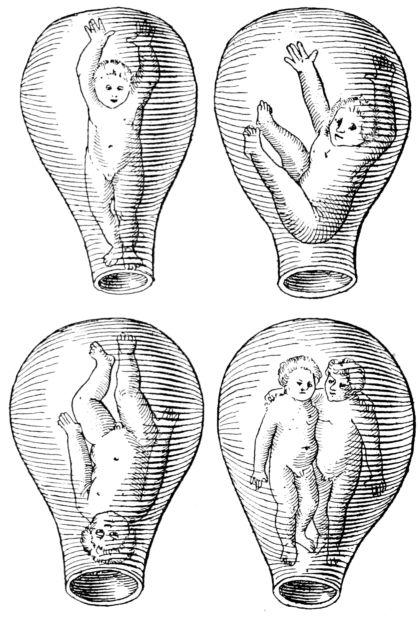
Fig. 51.—Illustrations from the first textbook on obstetrics, Roesslin’s “Rosengarten,” 1513, which gives an amusing impression of early ideas of the position of the fetus in utero.
With a few exceptions the long axis of the fetus is parallel to the long axis of the mother, and most frequently the head is 219downward. It was formerly believed that the child stood upright in the uterus until toward the end of pregnancy and then somersaulted to the position it occupied immediately before birth. (Fig. 51.) But it is now known that though the fetus may move about and change its position during the early part of pregnancy, it is not likely greatly to alter its relation to the mother’s body during the tenth lunar month.

Fig. 52.—Attitude of fetus in breech presentation.
It seems advisable to define here certain terms which are in common use in discussing patients in labor, and which will be employed in the following pages.
A nullipara (0–para) is a woman who has not had children.
A primigravida is a woman who is pregnant for the first time.
A primipara (1–para) applies to a woman during her first labor and until the beginning of her second labor.
2–para, 3–para and 4–para apply to women in succeeding labors which correspond to the numerals used.
A multipara is a woman who has had more than one child.
220There is also a terminology, with abbreviations, which is fairly generally used in this country and England to designate the position which the child, about to be born, occupies in relation to its mother’s body. A diagnosis of this position is, of course, absolutely necessary to a skilful management of labor, and the nurse should understand the meanings of the terms used, and also their distinctions and subdivisions.
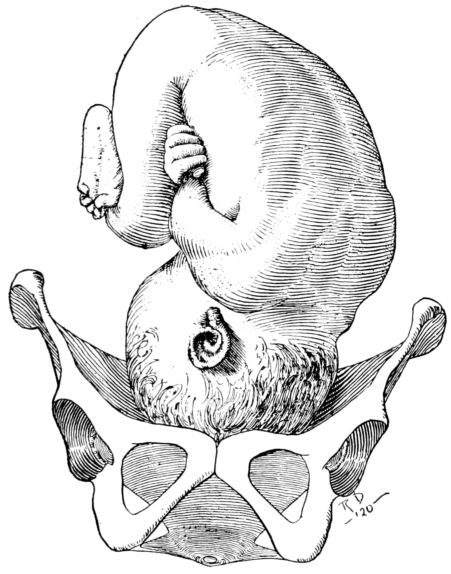
Fig. 53.—Attitude of fetus in vertex presentation.
The presentation of the fetus is the term which is employed to indicate the part of the baby’s body which is at the brim of the mother’s pelvis. Thus the part of the fetus which is lowermost is designated as the presenting part and gives the presentation its name. If the breech is downward, therefore, it is a breech presentation (Fig. 52), and if the head is the lower pole it is termed a head, or cephalic presentation. (Fig. 53.) The head presentations are divided into two main groups, which are designated, respectively, as face and vertex presentations. For 221example, if the baby’s neck is so arched that the chin rests upon the chest, the crown of its head, or the vertex, is the part that is lowest in the birth canal and is the part that will be seen first at the vaginal outlet. Therefore, this is called a vertex, or occipital presentation. But if the neck is bent sharply backward, the face becomes the presenting part and we have a face presentation.
The breech, face and vertex presentations are sometimes referred to as longitudinal presentations since in these instances the long axes of the bodies of mother and child are parallel. In transverse presentations, however, the child lies across the uterus, with one side or the other at the pelvic brim.
The transverse presentations are infrequent, occurring once in about 250 cases, and are regarded as abnormal because spontaneous delivery under such circumstances is extremely rare. They are more likely to be seen, when they do occur, among multiparæ and women who have contracted pelves.
The longitudinal presentations, however, constitute something over 99 per cent. of all cases and are regarded as normal, since the child occupying this relationship may be born spontaneously. In about 3 per cent. of the longitudinal presentation the breech is the presenting part and in about 97 per cent. it is the head. Of these, the vertex presentation is the one most commonly seen and is the one in which the child is most easily delivered. Face presentations are very rare, occurring in only a fraction of 1 per cent. of all cases.
In addition to the child’s presentation, there is also its position, which is an entirely different matter, for in each longitudinal presentation the presenting part may occupy any one of six positions.
By position is meant the relation of some arbitrarily chosen point on the presenting part of the fetus, to the right or left side of the mother, and to the front (anterior), side (transverse) or back (posterior) segment of that side.
Taking these up in turn, we find, that in transverse presentations the shoulder, acromion process, is the point on the baby’s body which is chosen, to give the four possible positions their names.
222In breech presentations the sacrum is the arbitrarily chosen point.
In face presentations it is the chin, or mentum, while in vertex presentations the occiput is the point chosen.
Presentation, then, describes the relation of the long axis of the entire fetal body to the mother’s body, while position describes the relation between the baby’s shoulder, sacrum, face or occiput to the mother’s pelvis.
If the child is so placed in the uterus that the head is the presenting part; the neck arched with chin on chest, and the occiput directed toward the mother’s left side, and more to the front than to the side, the presentation would be longitudinal, of the vertex variety, and the position would be a left-occipito-anterior. The arbitrarily chosen point on the child’s body (the occiput) would be directed toward the left, anterior segment of the mother’s pelvis. This is the situation most commonly seen and the description of this presentation and position are abbreviated, by taking the first letter of each word, into L. O. A.
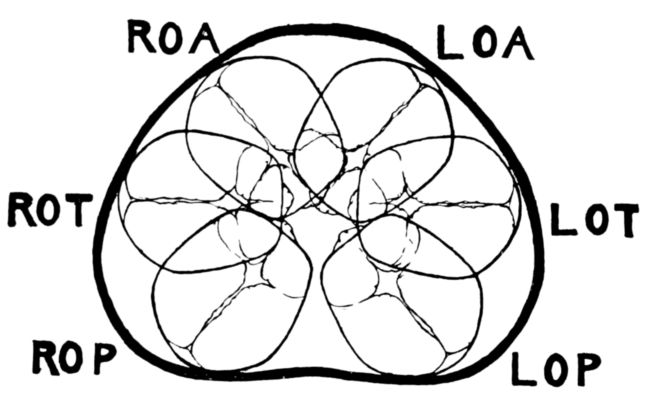
Fig. 54.—Diagram showing the six possible positions in a vertex presentation.
If the occiput were turned directly toward the mother’s left side, neither to the front nor the back, we should have a left-occipito-transverse, L. O. T., and if it were directed toward the left posterior segment of the pelvis the position would be left-occipito-posterior, or L. O. P. As there are three corresponding positions on the right side, anterior, transverse and posterior, there are six possible positions for the child to occupy in the vertex, or occipital presentations, as follows:
Similarly there are six face (Fig. 55) and six breech (Fig. 56) presentations. Thus, if the chin (mentum) is resting in the left anterior segment of the mother’s pelvis, the position would be left-mento-anterior, or L. M. A. If the breech presents and the sacrum is in that relation the position is left-sacro-anterior, or L. S. A.
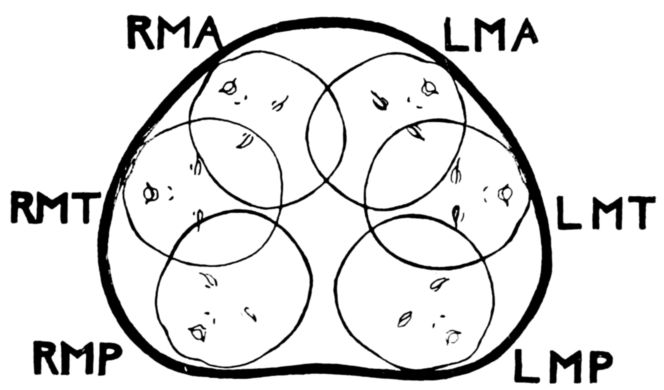
Fig. 55.—Diagram showing the six possible positions in a face presentation.
In describing the transverse presentations, four words, instead of three are used; thus, left-acromio-dorso-anterior, or L. A. D. A.
There are but four varieties of transverse presentations, since the shoulder is either anterior or posterior: thus left-acromio-dorso-anterior, left-acromio-dorso-posterior and the two corresponding positions on the right side.
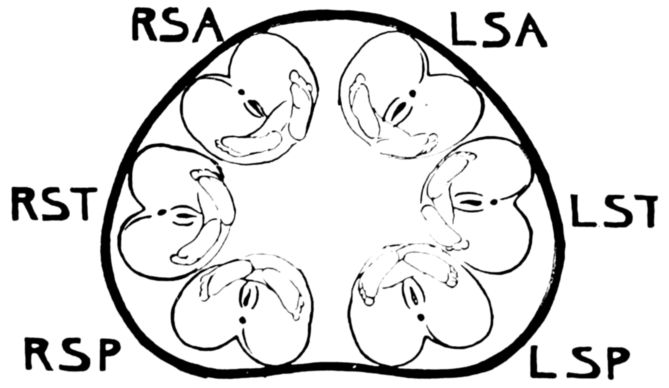
Fig. 56.—Diagram showing the six possible positions in a breech presentation.
224During the last two to four weeks of pregnancy, particularly among the primiparæ, the top of the fundus settles to the level which it reached at about the eighth month, and the lower part of the abdomen becomes more pendulous than formerly. The patient usually breathes much more comfortably after this change in contour takes place, but, at the same time, she may have cramps in her legs as a result of the increased pressure; more difficulty in walking; frequent micturition and desire to empty her bowels, while the vaginal discharge may be considerably increased. It is at this time that the presenting part enters the superior strait and is spoken of as being “engaged.”
The time at which engagement takes place depends upon three factors: Whether the patient is a multipara or a primipara; the size and normality of the pelvis; the size and position of the fetus. It is often helpful to the obstetrician in planning for the delivery to know whether or not the presenting part is engaged, particularly in primiparæ.
Although in primiparæ engagement usually occurs about four weeks before labor begins, it does not normally take place in multiparæ until immediately before labor. This difference is accounted for in the increased tonicity of the uterine and abdominal muscles of primiparous women. In certain abnormalities, or marked disproportion between the diameters of the child’s head and mother’s pelvis, engagement may not take place until labor is well advanced, or possibly not at all.
The presentation and position of the fetus are ascertained by means of abdominal palpation, vaginal examination, rectal examination and auscultation of the fetal heart.
Palpation of the child’s body through the mother’s abdominal wall is possible under ordinary conditions, because the uterine and abdominal muscles are so stretched and thinned that the various parts may be made out through them. But it is sometimes difficult in hydramnios and is practically impossible in very fat patients or in the case of a ruptured uterus when the fetal outline is obscured by hemorrhage. This procedure has been practiced only during comparatively recent years, and is regarded by many obstetricians as one of the most important factors in reducing the frequency of puerperal infections and 225thus in decreasing maternal deaths. The explanation is that in general the dangers of puerperal infection are believed to increase in direct proportion to the number of times a patient is examined vaginally; and since it has been known how to diagnose the child’s position by means of abdominal palpation, the necessity for vaginal examinations is not so great and they are accordingly made less frequently.
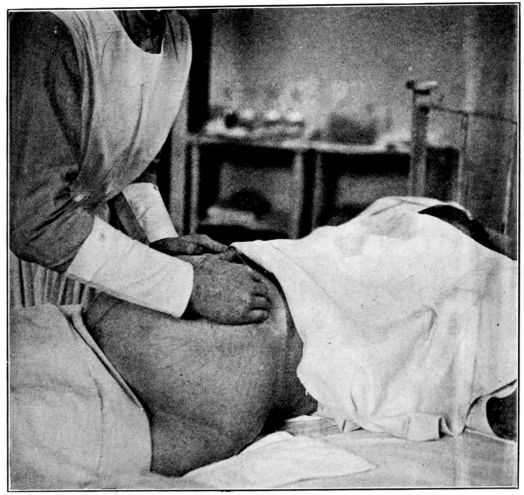
Fig. 57.—First maneuver in abdominal palpation to discover position of fetus.
Rectal examinations may also be regarded as a factor in preventing infection, for, since much the same information may be obtained by means of them as by vaginal examinations, after the onset of labor, they often replace direct exploration of the easily infected birth canal.
226Abdominal palpation, as usually practiced, consists of four maneuvers, with the patient lying flat and squarely on her back with the abdomen exposed. The nurse should bear in mind that successful palpation requires even pressure. Cold hands applied to the abdomen or quick, jabbing motions with the fingers will usually stimulate the muscles lying beneath them to contract, thus somewhat obscuring the outline of the child. Such palpation is also very uncomfortable for the patient; but firm, even pressure, started gently, with warm hands, does not hurt.
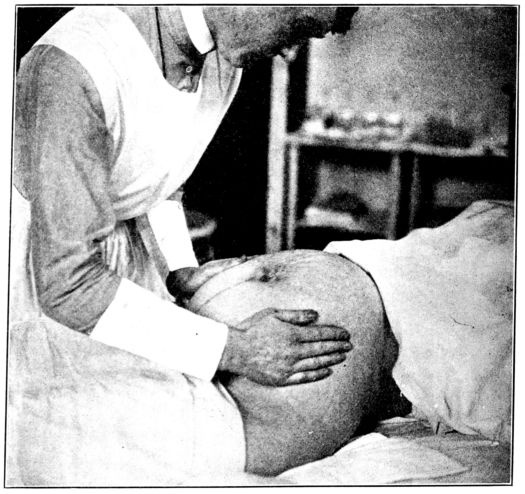
Fig. 58.—Second maneuver in abdominal palpation.
First Maneuver. The purpose of the first maneuver is to ascertain what is in the fundus; this is usually either the head or the breech. The nurse should stand facing the patient and gently 227apply the entire tactile surface of the fingers of both hands to the upper part of the abdomen, on opposite sides and somewhat curved about the fundus. (Fig. 57.) In this way the outline of the pole of the fetus which occupies the fundus may be made out. If the head is uppermost, it will be felt as a hard, round object which is movable or ballottable between the two hands, and if the breech, it will be felt as a softer, less movable, less regularly shaped body.
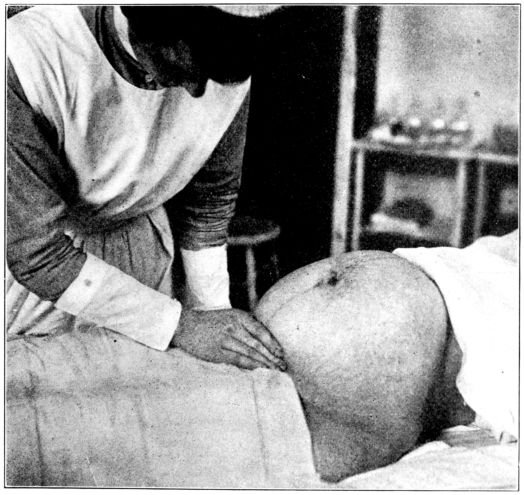
Fig. 59.—Third maneuver in abdominal palpation.
Second Maneuver. Having determined whether the head or the breech is in the fundus, the next step is to locate the child’s back and the small parts in their relation to the right and left sides of the mother. This is accomplished by slipping the hands 228down to a slightly lower position on the sides of the abdomen than they occupy in the first maneuver, and making firm, even pressure with the entire palmar surface of both hands. The back is felt as a smooth, hard surface under the palm and fingers of one hand, and the small parts, or hands, feet and knees, as irregular knobs or lumps, under the hand on the opposite side. (Fig. 58.)
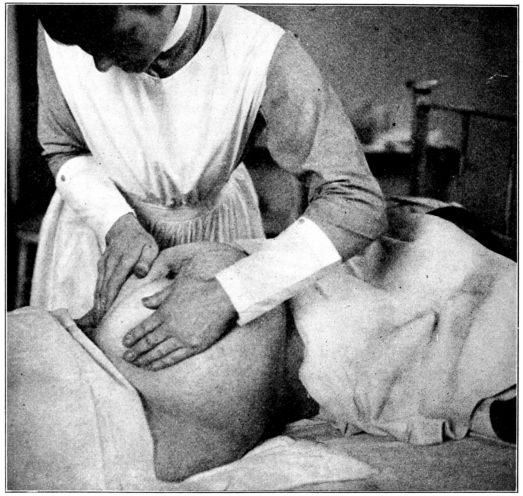
Fig. 60.—Fourth maneuver in abdominal palpation. (This series of pictures is from photographs taken at Johns Hopkins Hospital.)
Third Maneuver. Unless the presenting part is engaged, the third maneuver virtually amounts to a confirmation of the impression gained by the first maneuver, by showing which pole is directed toward the pelvis. The thumb and fingers of one hand 229are spread as widely apart as possible, applied to the abdomen just above the symphysis and then brought together to grasp the part of the fetus which lies between them. If not engaged, the head will be felt as hard, round and movable, while the breech will be less clearly defined. (Fig. 59.)
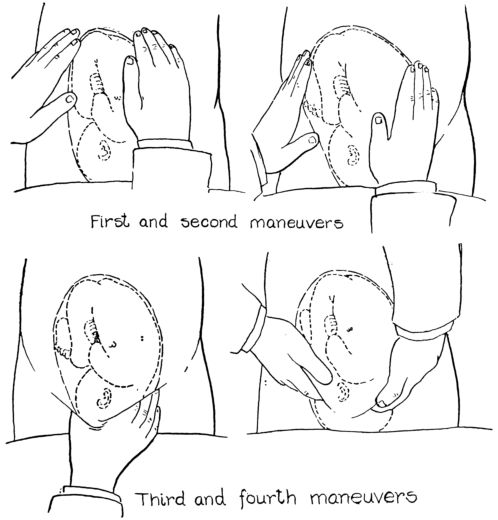
Fig. 61.—Diagrams showing relation of nurse’s hands to fetus in the four maneuvers of abdominal palpation.
Fourth Maneuver. The fourth maneuver is of particular value after the presenting part has become engaged. The nurse faces the patient’s feet in this position, and directs the first three fingers of each hand down into the pelvis, on either side of the fetus, to ascertain whether it is a face or vertex presentation, by discovering whether chin or occiput is the higher cephalic prominence in the mother’s pelvis. (Fig. 60.) If it is a vertex presentation, 230the neck will be flexed, with the chin on the chest and consequently higher in the pelvis than the occiput. The nurse’s fingers of one hand will accordingly come in contact with the chin on the side opposite to the child’s back, before the fingers of the other hand reach the occiput. If, however, it is a face presentation, the neck will be bent sharply backward and the nurse’s fingers will feel the occiput first, and on the same side as the baby’s back. This maneuver tells, also, how far into the pelvis the presenting part has descended.
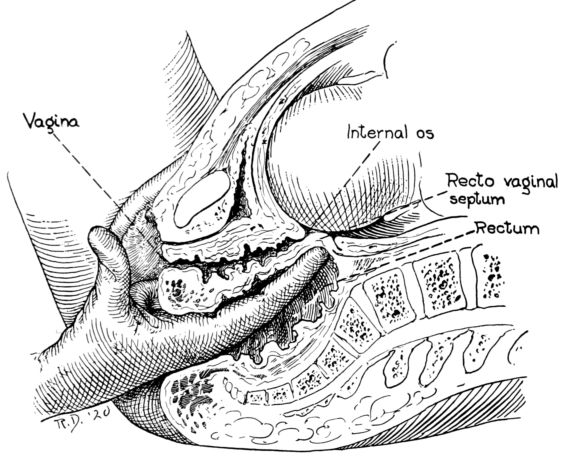
Fig. 62.—Diagram showing method of ascertaining position of fetus by means of rectal examination. Examining finger palpates head through recto-vaginal septum.
Vaginal Examination. The information obtained by vaginal examination, before the cervix is dilated, is rather uncertain since the child’s presenting part must be palpated through the fornix. But after complete, or even partial dilatation, the exploring finger is able to feel the sagittal suture and one fontanelle, in a vertex presentation, and diagnose the position by discovering the direction of the suture and whether it is the anterior or posterior fontanelle that is felt. The anterior fontanelle, it 231will be remembered, is relatively large and four-sided, while the posterior is small and more nearly triangular in shape. In a face presentation, the features may be felt; in a breech the examining finger can palpate the buttocks and genital crease.
Because of the possible danger of introducing infective material into the birth canal, the tendency is to make fewer and fewer vaginal examinations, and then only after the most painstaking preparation which will be described presently. Needless to state, vaginal examinations are not within the province of the nurse.
Rectal Examinations. More and more frequently rectal examinations are being employed to obtain information about the child’s position, as the examining finger is able to feel the surface of the presenting part through the recto-vaginal septum, after the cervix is dilated, and there is no danger of infecting the birth canal while so doing. For this reason nurses are frequently taught to make rectal examinations, thereby increasing the value of their assistance to the doctor in watching the progress of labor. (Fig. 62.)
Auscultation of the fetal heart is valuable in confirming the diagnosis of presentation and position which has been made by palpation. In vertex and breech presentations the heartbeat is best heard through the baby’s back and in face presentations it is transmitted through the chest, which presents a convex surface in this case and fits into the curve of the uterine wall. In anterior vertex presentations the heart is heard a little to the side and below the umbilicus; in transverse, further to the side, and in posterior, well toward the back.
Labor may be defined as the process by means of which the product of conception is separated and expelled from the mother’s body. It ordinarily occurs about 280 days from the beginning of the last menstrual period. (See p. 93.)
The cause of labor is not known. Many theories have been advanced to explain why the uterine contractions, which have occurred painlessly throughout pregnancy, and without expulsive force, finally become painful at the end of the tenth month and so changed in character as to extrude the uterine contents; but as yet, none is wholly satisfactory nor generally accepted. Nor is it known why some labors are premature and some delayed.
The onset of labor is usually marked by the patient’s becoming conscious of the uterine contractions through dragging pains which may be felt first in the back and then in the lower part of the abdomen and the thighs. At first the pains are feeble and infrequent, but they gradually grow more severe and more frequent. Intestinal colic is sometimes mistaken for labor pains, but when the paroxysms are rhythmical and the uterus is felt, through the abdominal wall, to grow hard as the pain increases and soft as it subsides, there can be no doubt but that the patient is in labor. The first signs of labor may be a gush of amniotic fluid, caused by the rupture of the membranes, or of blood, but these are not typical.
For purposes of convenience, labor is usually described as consisting of three periods or stages. The first stage begins with the onset of labor and lasts until the cervix is completely dilated; the second stage begins with the complete dilatation of the cervix and lasts until the child is born; the third stage begins with the birth of the child and lasts until the placenta is expelled.
233The entire duration of labor may vary from a few moments, comprising a few pains, to several days of severe and exhausting pain, but the average length of the first labor is 18 hours and of subsequent labors about 12 hours, divided respectively into the three periods as follows:
| 1st stage. | 2nd stage. | 3rd stage. | Total. | |
|---|---|---|---|---|
| Primipara | 16 hours | 1¾ hours | 15 minutes | 18 hours. |
| Multipara | 11 hours | 45 minutes | 15 minutes | 12 hours. |
The longer labor in primiparous women is due to the greater tone, and thus the greater resistance offered by the muscles of the cervix and perineum. Elderly primiparæ are likely to have longer labors than young primiparæ.
First Stage. This is frequently called the stage of dilatation. During this period the contractions of the uterine muscles make pressure upon the amniotic sac of fluid, forcing it gradually down and into the cervix as a water wedge, widening the internal os first, then the external os, until the entire canal is fully dilated (thinned out); shortened to about one-half inch in length and finally obliterated so that it is uninterruptedly continuous with the lower uterine segment. (Figs. 63, 64, 65, 66.)
The first stage pains begin by being mild and occurring at intervals of from 15 to 30 minutes, but they gradually increase in frequency and intensity until at the end of 14 to 16 hours they are very severe and recur every three or four minutes, each pain lasting about one minute. The pains begin in the back, pass slowly forward to the abdomen and down into the thighs.
The patient is entirely comfortable, as a rule, between pains and until they become very frequent will usually feel able, in fact prefer, to be up and about, but if she is on her feet when a contraction begins she will usually seek relief by assuming a characteristic leaning position (Fig. 67) or by sitting down, until the pain subsides. As dilatation advances, the patient has an increasing, sometimes persistent, desire to empty the bowels and bladder because of encroachment upon these two organs by the descending head. She may vomit, also, when the cervix becomes nearly or quite dilated.
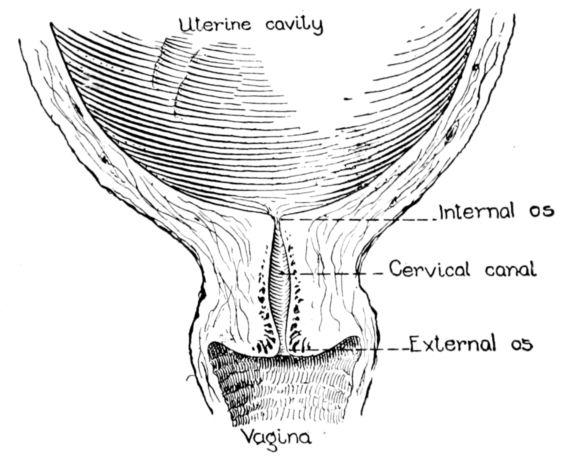
Fig. 63.
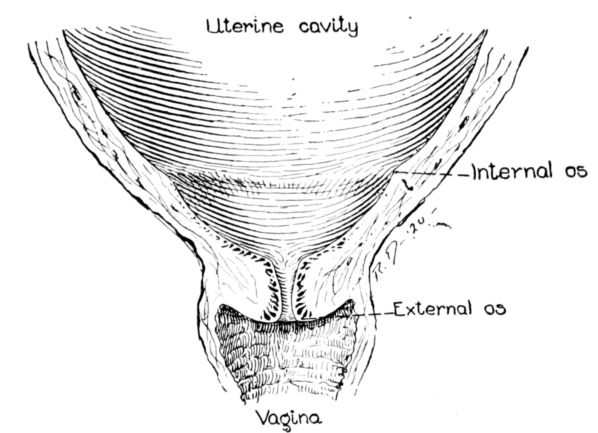
Fig. 64.
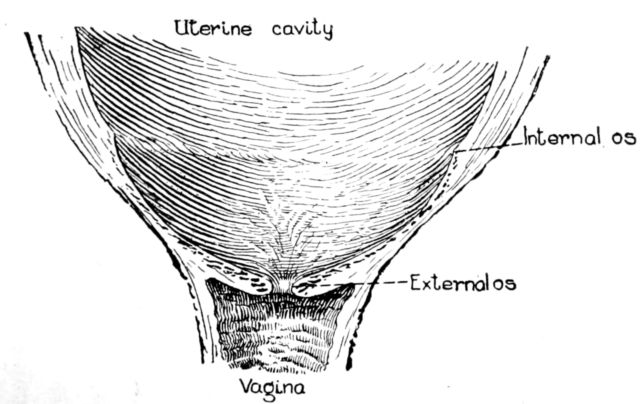
Fig. 65.
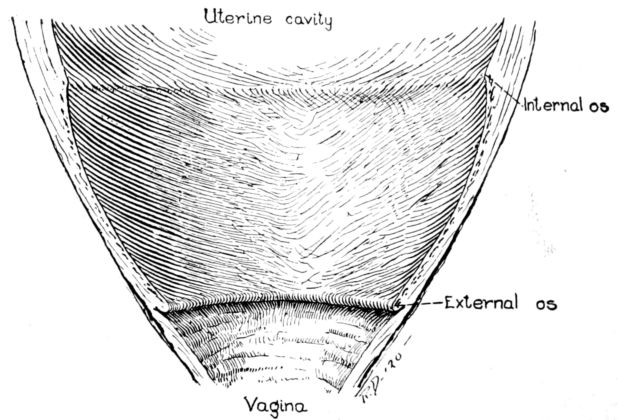
Fig. 66.
235In the course of this stretching process, the cervix sustains many tiny lesions, from which blood oozes and tinges the vaginal discharge. This blood-stained secretion is often called the “show” and usually appears toward the end of the first stage.
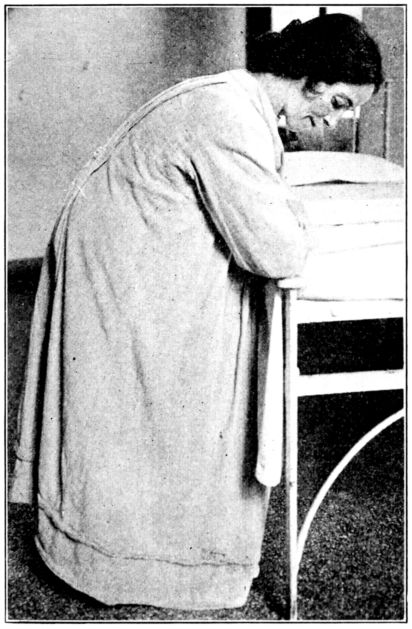
Fig. 67.—Characteristic position which patient often assumes during pains in first stage.
As a rule, when the cervix is fully dilated the membranes rupture and there is a sudden gush of that part of the fluid which was below the fetus in the amniotic sac, but the rupture of the membranes does not necessarily mark the end of the first stage. In some instances they rupture before the cervix is fully dilated; in others, though not often, before the patient goes into labor, thus producing what is known as a “dry” labor.
The abdominal muscles do not contract very forcibly during the first stage, the expulsive force in this period coming almost entirely from the uterine contractions. The patient’s cries at this time are sharp and complaining in contrast to the groans and grunts which accompany the second stage.
236Complete dilatation of the cervix marks the termination of the first stage.

Fig. 68.—Diagram indicating the rotation and pivoting of baby’s head during birth.
Second Stage. The second stage is sometimes called the stage of descent, or expulsion, of the fetus. The patient should and is usually quite willing to be in bed throughout the second stage, during which she should not be left alone. The pains are now regular, occurring at intervals of about two minutes from the beginning of one to the beginning of the pain following, and as the contractions last about one minute and are excruciatingly painful, the patient has very little respite from her suffering. Her face is flushed and she may perspire freely.
The abdominal and respiratory muscles are brought into active use during the second stage, contracting simultaneously with the uterine muscles and increasing their expulsive force. These are apparently controlled by the patient’s will at first, and she is able somewhat to increase their power by taking a deep breath, closing her lips, bracing her feet, pulling against something with her hands, straining with all her might and “bearing down.” Finally, however, the whole bearing down process becomes involuntary, is accompanied by intense pain and the 237deep grunting sound, which is characteristic of the well-advanced second stage. Under normal conditions, the child descends a little farther into the pelvis with each contraction, and finally the presenting part begins to distend the perineum and to separate the labia advancing at the height of each pain and slipping back a little as it subsides.
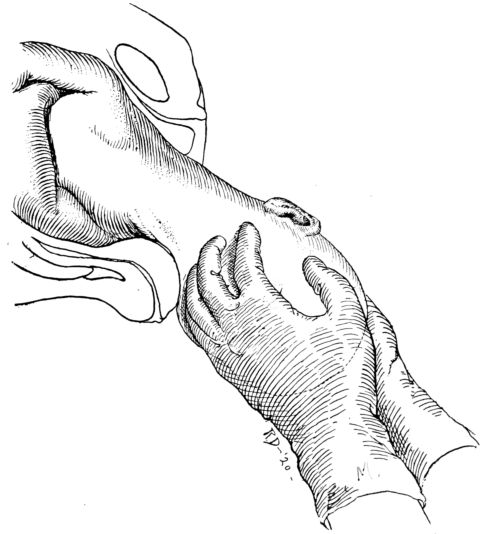
Fig. 69.—Anterior shoulder being slipped from under symphysis to facilitate birth of posterior shoulder.
The baby descends into and through the mother’s pelvis by means of a series of twisting and curving motions, accommodating the long axes of its head to the long diameters of the pelvis. The head being somewhat compressible and mouldable, because of imperfect ossification, is capable of a good deal of accommodation to the mother’s pelvis.
238The mechanism of labor, therefore, is virtually a series of adaptations of the size, shape and mouldability of the baby’s head to the size and shape of the mother’s pelvis. If the head passes through the inlet satisfactorily, the rest of the labor will usually be accomplished with comparative safety. But a marked disproportion between the diameters of the head and pelvis may interfere with the engagement or descent of the head and produce a serious complication.
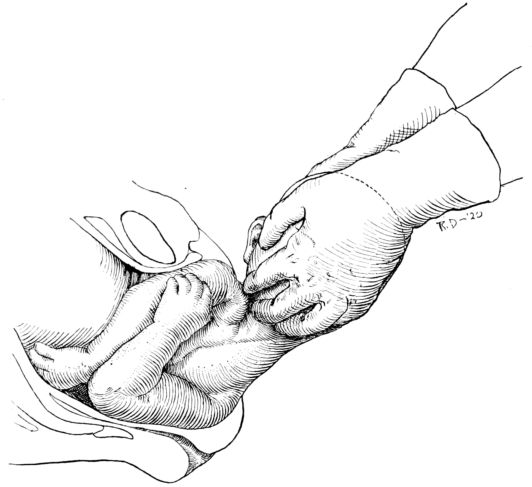
Fig. 70.—Delivery of posterior shoulder.
The long diameter of the head must first conform to one of the long diameters of the inlet, usually oblique, and then turn so that the length of the head is lying antero-posterior in conformity to the long diameter of the outlet through which it next passes. As the head descends and rotates it also describes an arc because the posterior wall of the pelvis, consisting of the sacrum and coccyx, is about three times as deep as the anterior 239wall formed by the symphysis. That part of the baby’s head which passes down the posterior wall of the pelvis must therefore travel three times as far in a given time as the part which simply slips under the short symphysis pubis.
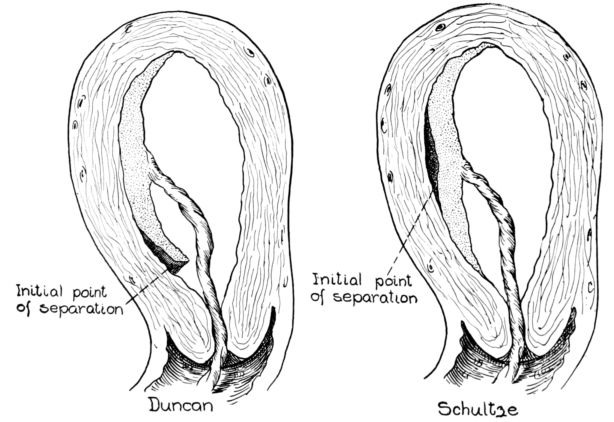
Fig. 71.—Diagrams showing Duncan and Schultze mechanisms of placental separation.
In a vertex presentation, left-occipito-anterior position, while the occiput passes under the symphysis and appears at the distending vaginal outlet, the face passes down the posterior wall and along the floor of the pelvis. As pressure is exerted by the rapidly succeeding contractions, the head pivots about the pubis, thus extending the neck and pushing the face farther downward and forward. After emergence of the back and top of the head below the symphysis, the forehead appears over the posterior margin of the vagina, then the brow, eyes, nose, mouth and chin in turn, and the entire head is born. (Fig. 68.) The baby’s head then drops forward, in relation to its own body, with its face toward the mother’s rectum and the occiput in front of the pubis, but soon the occiput rotates toward the mother’s left side, resuming the relation that it bore to the inner aspect of her pelvis before expulsion. The undelivered shoulders are now antero-posterior, 240one under the pubis and the other resting on the perineum. (Fig. 69.) The lower, or posterior shoulder is born first (Fig. 70), followed quickly by the anterior shoulder and the rest of the body, and the amniotic fluid which was behind the child’s body. Thus is the second stage completed.
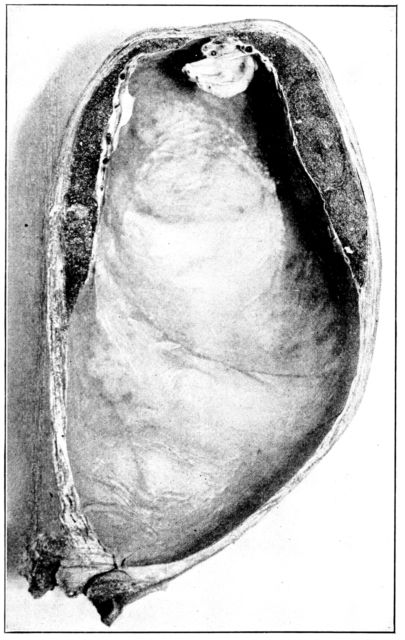
Fig. 72.—Longitudinal section through uterus showing thinness of uterine wall before expulsion of fetus, contrasting sharply with thickened wall in Fig. 73. (From photograph of specimen, to which twin placentæ are still adherent in upper segment, in the obstetrical laboratory, Johns Hopkins Hospital.)
Third Stage. The third stage, sometimes termed the placental stage, is that period following the birth of the child, during which the placenta is delivered. For a few moments after the baby is born the tired mother lies quietly and free from pain, as there is a temporary cessation of the uterine contractions, 241and she often sleeps as a result of the anesthetic given during the second stage.
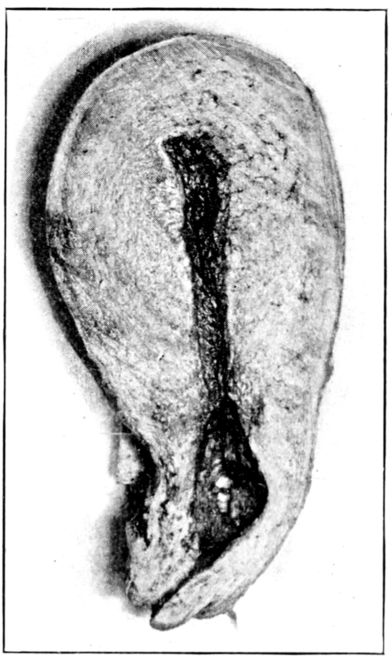
Fig. 73.—Longitudinal section through uterus, immediately after labor, showing marked thickening of wall as a result of muscular contraction. (From photograph of specimen in the obstetrical laboratory, Johns Hopkins Hospital.)
The uterus has greatly decreased in size, the fundus now lying below the umbilicus where it may be felt as a firm, solid mass. The uterine contractions are resumed in the course of a few moments and as they persist, the uterus grows smaller, thereby greatly decreasing the area of placental attachment. As the placenta is non-contractile it cannot accommodate itself to this decreased area of attachment, and so is literally squeezed from its moorings. It is then gradually forced down into the lower uterine segment where it may be located by the distension of the abdominal wall which it produces just above the symphysis. After the separation of the placenta is complete the uterus rises in the abdominal cavity until the fundus is felt above the umbilicus. The placenta, finally, may be completely expelled spontaneously, or expressed by slight pressure made upon the fundus by the accoucheur.
The placental detachment may begin at the centre, the area of separation spreading to the margin, or the detachment may start at the margin of the placenta and extend toward the centre. Either is normal. These two modes of placental separation are named the Schultze and the Duncan, respectively, from the men who first described them. (Fig. 71.)
In the Schultze mechanism, which occurs most frequently, the separating process begins at the centre of the placenta and the glistening fetal surface appears at the vaginal outlet. In this case there is practically no bleeding during the third stage 242as the inverted placenta blocks the vagina and holds back the blood.
In Duncan’s mechanism the detachment begins at the margin, the placenta rolls upon itself and presents at the outlet by its roughened maternal surface and there is usually slight but continuous bleeding from the time the separation begins. When the placenta is delivered, the collapsed membranes trail after it like a tapering cord. A good deal of blood is lost at the time of the placental expulsion and immediately afterwards, but this profuse bleeding usually subsides in a few moments. Although the loss of blood may be as much as 500 cubic centimetres without its being regarded as serious, the average amount is about 350 cubic centimetres.
The patient has been through a severe ordeal and at the end of the third stage of labor she is usually tired out and cold.
The extent of the nurse’s helpfulness during labor, both to the patient and to the doctor, will depend very largely upon the intelligence with which she grasps what is taking place and upon her own attitude, as an individual, toward the patient and the miraculous event which approaches. Important as is the preparation of the room and dressings, this other factor is almost equally influential.
It will be wiser, therefore, for the nurse to try to picture the process of labor in each instance, and to be guided by a few broad principles that apply to all cases under all conditions, rather than to try to memorize the details of her duties and of the desirable equipment and preparation.
The process of labor we have just described.
As to the general principles: If there is any time in a nurse’s career when she should give scrupulous attention to establishing and maintaining asepsis, it is during labor, for the patient’s life may, and often does depend upon it. If there is any time when she should be watchful for developments and for symptoms of complications, it is during labor, for again the patient’s life may depend upon this.
Her powers of adaptability to doctor, patient and surroundings may be severely tried, for though they all may be infinitely varied, the nurse must invariably be clear-headed and efficient and the adequacy of her service must never fail.
The sympathetic insight, which should constantly underlie the work of the obstetrical nurse, will be needed at this crucial time of labor in the fullest and finest and completest sense. This is almost her test as a nurse and as a womanly woman, for she needs to be both, supremely.
Perhaps she had better imagine for a moment what this occurrence, that we baldly term labor, may mean to the patient 244and look at it as nearly as possible from the standpoint of the patient herself. It is one of the most stirring and momentous experiences of her life, particularly if the expected baby is her first child. She is about to realize the sweetest and tenderest of dreams—that of motherhood—cherished throughout nine long months. She is also approaching a period of excruciating pain, and knows it, with her eyes wide open to the possibility of not surviving it; and an event so amazing in its mystery and wonder that to only the most stolid can it fail to be a deeply emotional experience.
And so, the young woman, to whom we refer so impersonally as “the patient,” is an intensely personal being at this time, experiencing a number of the most poignant of the human emotions: awe, expectancy, doubt, uncertainty, dread and in some cases fear amounting almost to terror. And through it all her body is being racked and exhausted with pain that grows harder and harder to bear.
It is known that the ravaging effects of pain, coupled with great emotional stress, such as fear, worry, doubt, anger or apprehension, upon the physical well-being of surgical patients, is such that death itself may be caused by excessive fear and suffering. Accordingly, many careful surgeons take elaborate precautions to tranquillize a patient who is about to be operated upon, if for no other reason than to increase his chance for recovery.
There can be no doubt that nervous and emotional disturbances are detrimental to the physical well-being of the patient in labor, also, and this fact alone is enough to warrant an effort to avert them. If the nurse appreciates the significance of the emotional influence and shapes her attitude and conduct accordingly, she will thereby help to increase the ease and safety of the actual delivery. Just what that attitude shall be, no one can say, for it must be developed, in each case, in such a way as to win the confidence and meet the needs of that particular patient.
But in all cases the nurse should impress her patient with her sincere sympathy and appreciation of the fact that she, the patient, is going through a difficult time. Through it all the 245nurse must be cheerful, encouraging and optimistic; very gentle; very calm and reassuring in all that she does in preparing for the delivery. She must steadily increase the patient’s realization of the part which she herself must play in the effort which is being made to carry the event through to a happy issue.
The occasion need not, should not, be a mournful one but it is often a very sacred one to the patient, and the nurse should be dignified, almost reverential in her bearing.
If the patient feels secure in the belief that her ordeal is not being taken lightly; that it is being regarded seriously, as it merits, and that every known precaution is being taken, and taken confidently, to safeguard her and her baby’s welfare, her actual physical condition will be favorably affected by the condition of mind thus produced. And her patience and courage will often be strengthened if the nurse will explain, from time to time, the cause of certain conditions that normally arise, and which otherwise might give her alarm. It is the mysterious events, the unexpected and unexplained that so often terrify.
This giving of comfort and strength to the variety of temperaments and mentalities which the nurse meets among her patients will involve a very sensitive adjustment of manner on her part, but it is one aspect of her duty, none the less, and one which will give her great satisfaction.
Happily, the onset of labor is usually gradual, as has been described, and there is accordingly ample time during the first stage for deliberate and unhurried preparation for the birth of the baby. The character of the preparation and of the nurse’s assistance will vary greatly according to the wishes of the attending doctor; the duration of labor; the circumstances and condition of the patient, and whether she is at home or in a hospital.
It is a fairly general routine, at present, both in hospitals and in the home, to give the patient a soap-suds enema and a shower or sponge bath, at the onset of labor; to braid her hair in two braids and dress her in freshly laundered stockings and nightgown and a dressing gown. The enema is given to empty the rectum of material which might be expelled during labor 246and contaminate the field. For this reason, enemata are often given until the fluid returns clear, virtually irrigating the rectum, and are repeated every six or eight hours during the first stage. The enema should be given to the patient in bed and expelled into a bed-pan, as it is not wise for her to use the toilet after labor has begun. Sometimes the vulva and perineal region are shaved and scrubbed at the onset of labor, either before or immediately after the bath and enema. But the time and sequence of the different steps in the preparation for labor are governed entirely by the wishes of the individual doctor, to which the nurse may very easily adjust herself.
The patient should be given a bed-pan and encouraged to void every four hours. If she is unable to do so, and the bladder becomes distended, the doctor will usually wish to have her catheterized, and with a rubber catheter. This distension is not uncommon, and in extreme cases the bladder may reach to the umbilicus. The nurse should therefore observe the amount of urine which the patient voids and also watch the lower abdomen for bladder distension, which may be observed easily, excepting in very fat patients.
The seriousness of a distended bladder lies in the fact that it may markedly retard labor, partly by interfering with the descent of the baby’s head and partly through reflex inhibition of the uterine contractions. The prevention of a distended bladder during labor, therefore, is of considerable importance.
As the pains are infrequent and not severe at first, the patient will usually prefer to be up and about, most of the time during the first stage, when it occurs in the daytime, and many doctors think it important that she should be. They feel that patients tend to stay in bed too much during the first stage, since being on their feet would really promote their comfort and also have a tendency to make the pains more regular and efficient. But, on the other hand, the patient must be cautioned against tiring herself, and should, therefore, lie down often enough and long enough to avert fatigue. When labor begins at night, it is well to advise the patient to stay in bed and to sleep as much as possible until morning. Even though her sleep be disturbed and broken by the labor pains, she will be much less tired in the morning than if she had gotten up and had no sleep at all.
247The patient should also be advised against trying to hasten labor by bearing down during first stage pains, since the only result at this time will be to waste her strength which will be needed later. This is one of the points that the nurse will do well to explain; that no voluntary effort on the patient’s part, during the first stage, will advance labor and if she tires herself by making such efforts before the second stage pains begin she will not be able to use them as effectively as she would were she in a rested condition.
Bearing in mind the importance of conserving all of her forces, it is usually advisable for a patient in labor to have no visitors, particularly the type of person who would be likely to offer advice and gratuitous information.
She should drink water freely and take some kind of light nourishment about every four hours. As pain of any kind tends to retard digestion, the diet during labor is usually restricted to fluids, such as broths, weak tea or coffee and sometimes milk or cocoa; while occasionally crackers and crisp toast are allowed. Whatever nourishment is given must be very light because of the probability of the patient’s vomiting and the possibility of her having to be given complete anesthesia before the termination of labor.
The maternal temperature, pulse and respirations should be taken every two or four hours and the fetal heart rate from every hour to every two hours, according to the wishes of the doctor.
The time at which the nurse should call the doctor is the subject of considerable discussion. Doctors never want to be called too late, neither do they wish to be called unnecessarily early, though they prefer to have the nurse err on that side, if at all. On general principles the doctor should be notified as soon as the patient goes into labor, in order that he may make his various plans with the pending delivery in mind. But if the nurse remembers that in primiparæ the first stage of labor usually lasts about sixteen hours and in multiparæ about eleven hours, she will realize that if the pains begin between the hours of eleven p.m. and seven a.m., and are of average character, mild and infrequent, she is not warranted in disturbing the doctor’s much needed sleep, unless he has explicitly requested her to do 248so. But under average conditions he should be notified by seven o’clock in the morning that the patient is in labor; at what hour the pains began; their character and frequency at the time of the report; the patient’s temperature, pulse and respirations and general condition and the fetal heart rate.
During the early hours of the first stage the nurse should begin to arrange the room and bed for delivery. She will need two, or preferably, three tables, though the top of a bureau may be used in place of one table. A washstand or the bathroom should be equipped for the doctor with soap; two sterile brushes; nail scissors or clippers and file or orange stick; hot water; alcohol and a solution of bichlorid 1–1000, biniodid 1–5000, lysol 2 per cent. or any solution that he may wish; sterile gloves and sterile vaseline or albolene to lubricate his hands. In short, an equipment which will enable him to prepare his hands exactly as he would for performing a major operation.
A large receptacle of water may be boiled, covered and set aside to cool; a boiler or large kettle placed in readiness for boiling instruments or other appliances that the doctor may bring; the room may be given a final cleaning: floor wiped up, furniture and all small articles wiped with a damp cloth; the unopened packages of dressings, sterile douche pan, irrigation-bag and basins may be placed on the tables, ready to be opened when needed, together with the other articles which have been prepared.
In preparing the bed in a patient’s home, it is practically always advisable to make it firm by slipping a board, or the leaves from a dining-table, between the mattress and springs. The bed should be made up with three freshly laundered sheets, the entire mattress being protected by means of a rubber placed under the lower sheet; next a rubber draw sheet, covered by one of muslin, while the top sheet, light blanket and counterpane should be left free at the foot. A flat hair pillow is better than one of feathers.
If the doctor wishes to make a vaginal examination, it devolves upon the nurse to prepare the patient with the most scrupulous care, as it is by means of vaginal examinations, made without careful preparation, that so many parturient women 249are infected. In fact, even the most conscientious preparation sometimes seems to be an inadequate safeguard, for infection has been known to follow in its wake. For this reason, some obstetricians prefer to make no vaginal examination during labor, when previous inspection has indicated that the case is normal, depending rather upon rectal examinations for guiding information.
The patient should be placed in bed, on a douche pan, with knees flexed and well separated; gown tucked up under her arms; draped with a sheet or the bedding folded down to her knees according to the extent of the area to be prepared; and the articles needed for the preparation arranged on a table at the bedside. The nurse should trim her nails, scrub her hands with soap and hot water; shave the vulva, supra-pubic region and inner surface of the thighs and rinse with sterile water. In shaving the vulva, the strokes should be from above downward, greatest care being taken not to allow hair, soap or water to enter the vaginal opening. She should then scrub her hands vigorously for three minutes, scrubbing about the nails with especial thoroughness. Some obstetricians have the entire area from the umbilicus to the knees prepared as for an operation, while others prepare only the supra-pubic region, inner surface of the thighs and the vulva. The number and kind of solutions which are used in this preparation also vary greatly, but in general the shaving is followed by a thorough scrubbing, by clean hands, with green soap and sterile water, then iodin, lysol or alcohol and bichlorid or biniodid solution, according to the custom of the doctor. (Fig. 74.)
But the kind and number of the solutions are probably not so important as the nurse’s technique. Throughout the entire course of the preparation she must apply the principles of what she was taught about the technique of preparing the skin for an operation and regard the perineal region in the same light as she would the field which was being prepared for a major operation; scrubbing from the centre toward the periphery, always, in order not to carry infective material from an unclean to a clean area, which in this case is the vaginal outlet.
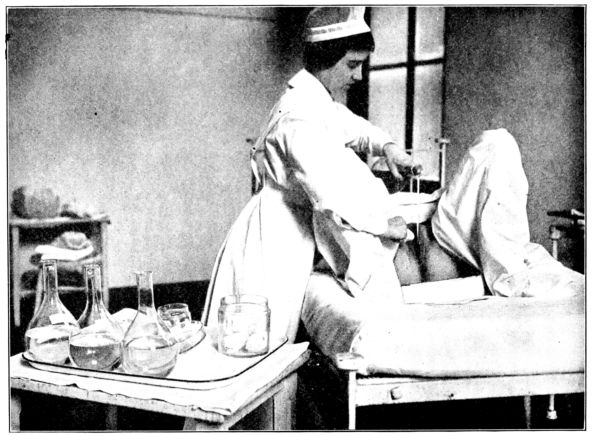
Fig. 74.—Bathing the vulva preparatory to vaginal examination or delivery. (From photograph taken at Johns Hopkins Hospital.)
251The supra-pubic region and abdomen are scrubbed across, back and forth, working up from the symphysis; the strokes on the thighs are up and down; in the groin, down toward the rectum, and away from the vagina, never toward it, and fluids poured upon the vulval region must never run into the vagina from over surrounding skin. A sponge or scrub ball must be discarded after approaching the rectum, or stroking away from the vagina in any direction. Some obstetricians instruct the nurse to place a firm, sterile cotton pad or scrub ball between the labia, against the vaginal opening while scrubbing and flushing the adjacent areas, to preclude the possibility of introducing fluids. But with a painstaking nurse this is scarcely necessary.
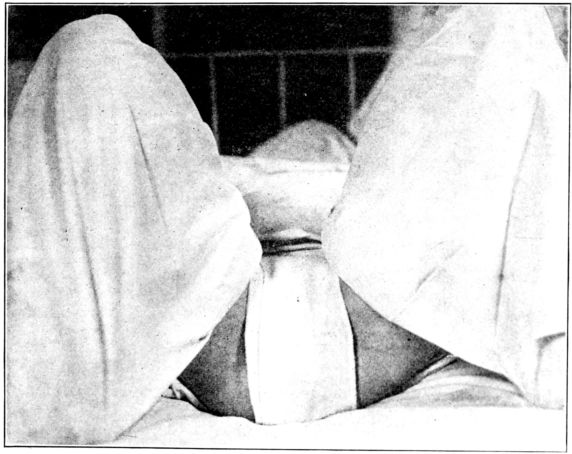
Fig. 75.—Patient draped for vaginal examination; vulva covered with sterile towel. (From photograph taken at Johns Hopkins Hospital.)
After the surrounding areas have been prepared, the labia are separated and the inner surfaces scrubbed, first across, then from above downward, and flushed by pouring the solution directly between the folds. After the patient has been given this preparation, a dry sterile towel or pad is placed over the vulva; the douche pan is removed, the back and hips are dried, 252after which the patient is so draped with a clean sheet that only the perineal region is exposed, and a sterile towel is slipped under the buttocks. (Fig. 75.)
To summarize the preparation for vaginal examination or delivery:
This may be taken as a description of a fairly typical method of preparing a patient for vaginal examination or for delivery, which is widely employed and with satisfactory results. But it is by no means the only satisfactory procedure, for many other and different methods of preparation also are followed by excellent results, as measured by the patient’s temperature during the puerperium.
The details of preparation vary so greatly, even among different doctors in the same hospital, that the nurse will simply have to bear in mind the general principles of asepsis and antisepsis, and adjust herself to the practices of the individual doctor. And she must remember that in spite of the best planning, there will be emergencies and precipitate labors, when the preparation will necessarily be modified, and sometimes so curtailed that even the bath and enema are omitted.
But in all cases the nurse can, and must, bear in mind that on one point there is virtually no difference of opinion among obstetricians of to-day; and that is the imperative necessity of having everything sterile that is brought to the perineal region or used in any way in connection with the delivery, or as nearly sterile as is possible under the circumstances.
By many doctors this is considered the most important factor, as to surgical cleanliness, in the entire preparation. In their opinion the local preparation of the patient may, with safety, be restricted to clipping the pubic hairs (instead of shaving), 253and scrubbing the vulva with only soap and water. But these doctors believe at the same time that the patient is dangerously susceptible to infection which may be conveyed to her from without, and accordingly they do not permit vaginal examinations to be made during labor, and make the most exacting demands concerning the maintenance of perfect surgical technique, by all who assist with the delivery.
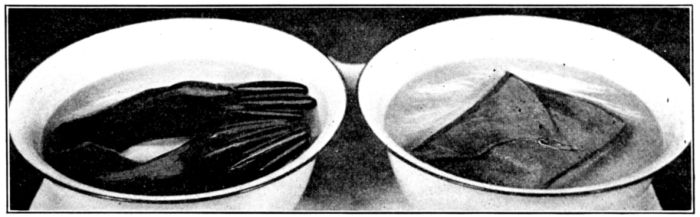
Fig. 76.—Wrong and right methods of boiling gloves. Note that gloves in basin at the left are partly above the surface of the water and therefore will not be sterilized. Those in basin at the right are kept below the surface by the weight of the towel and will be sterilized by the boiling water.
In this connection, much depends upon the actual sterilization of the rubber gloves, either by boiling or by steam under pressure; and the method of putting on the gloves, in order that once having been sterilized, they may be kept so. It is useless to attempt to sterilize gloves by boiling, if they are thrown loosely into a kettle of water. There will practically always be enough air in the fingers to keep at least a part of the gloves out of the water, and consequently unaffected by its heat. They should be put into a covered wire basket that will be entirely submerged, or they may be wrapped in a towel, the weight of which will carry them below the surface of the water (Fig. 76), and insure their being completely covered while boiling, which should continue for ten to fifteen minutes. The doctor will usually want boiled gloves placed in a large basin of bichlorid solution, 1–1,000, or lysol 2 per cent., from which he may remove them after scrubbing his hands. If dry gloves are used, there should be in readiness a sterile towel and powder with which to 254dry and powder the hands before putting on the gloves. (Fig. 77.)
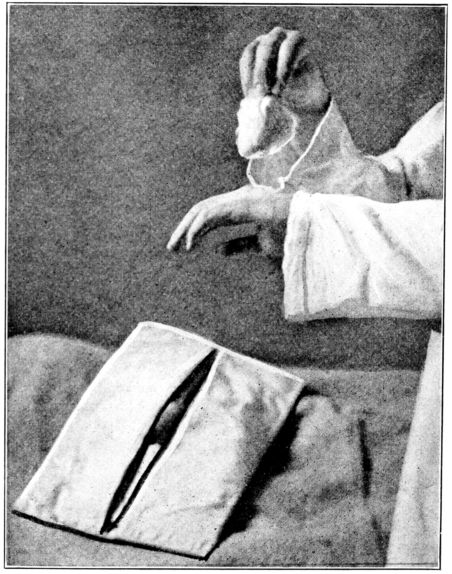
Fig. 77.—Powdering hands before putting on dry gloves. (From photograph taken at the Brooklyn Hospital.)
Whether boiled or steamed, the cuffs of the gloves should first be turned up toward the hand, to make it possible to put them on without touching the glove fingers with ungloved hands. (Fig. 78.) For no matter how long and carefully the hands are scrubbed and soaked, they cannot be made absolutely sterile, and therefore, in relation to the gloves which are sterile, the bare hands must always be regarded as unclean. Too much thought and attention cannot be given to the sterilization and handling of the gloves, for the patient’s very life may depend upon their aseptic condition.
After the doctor has seen the patient, the nurse will make observations and communicate with him in accordance with instructions 255which she must make sure to obtain from him at that time. Many doctors wish to be with a primipara continuously from the time the cervix is completely dilated, and with multiparæ after it is half dilated. But that, of course, is a matter which each doctor decides for himself. The nurse’s responsibility is to learn his wishes.
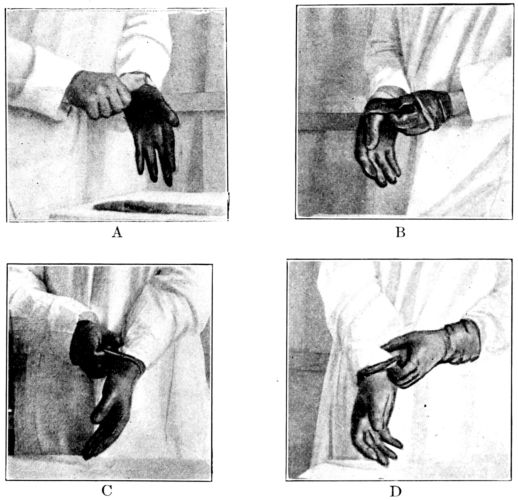
Fig. 78.—Successive steps in proper method of putting on sterile gloves to avoid contaminating outside of gloves with bare fingers. (From photographs taken at the Long Island College Hospital.)
Watchfulness, then, is of extreme importance; watching for symptoms of complications or change in the patient’s condition, and watching the progress of labor in order to keep the doctor fully informed about his patient’s condition. Nurses are very frequently taught to make rectal examinations for the sake of increasing the value of their assistance in this respect.
Although unexpected symptoms do not, as a rule, develop 256suddenly during the first stage, the nurse must be none the less vigilant for them. The doctor should be notified if the pains suddenly grow either more or less frequent, or more or less severe; if there is any bulging of the perineum; if the membranes rupture; if there is any bleeding or a prolapsed cord; if there is extreme restlessness or any evidence of unusual distress; a rising temperature or pulse; a temperature of 100° F. or a pulse of more than 100 or less than 60; a fetal heart rate of more than 150 or less than 116, or any marked change of any kind in the patient’s condition.
During the latter part of the first stage, and during the second stage, the patient has an almost continuous desire to empty her bowels, because of pressure made upon the rectum by the descending head. This is another point which the nurse explain to her patient, in assuring her that frequent attempts to use the bed-pan will give no relief.
The end of the first stage is reached when the cervix is fully dilated, at which time the pains occur about every two minutes, are stronger and more severe, and the patient begins to feel like bearing down. The membranes frequently rupture at this point and the vaginal discharge is blood tinged. The patient should remain in bed and not be left alone from this time on.
To sum up the nurse’s duties during the first stage of labor, when the patient is almost entirely in the nurse’s care:
The second stage is shorter, harder and more perilous than the first. The uterine contractions are stronger; more frequent and more expulsive, and the baby steadily curves and rotates its way down through the birth canal.
257With the onset of the second stage the nurse should complete the preparations for the baby’s birth, bearing in mind that with a primipara the baby probably will not come for an hour and a half or two hours, but may come in half an hour or less if the patient is a multipara. Everything which is to be used should be conveniently placed, but the packages are not necessarily opened at this time.
In addition to the sterile dressings, basins, gloves, instruments and various other articles which have been enumerated, the nurse must remember that there should be for the baby a box or basket lined with a blanket and containing one, or preferably two, hot-water bottles at 125° F.; in hospitals, an adhesive strip for the baby’s name or a name necklace; a binder of flannel or sterile gauze, according to the custom of the doctor; sterile olive oil or albolene for the first oiling and one or two tubs, in case the baby needs to be resuscitated.
There will be needed, also, a covered basin for the placenta; chloroform and an inhaler; Wassermann tubes, for those doctors who make this test as a routine; hypodermic syringe and needles, with pituitrin, ergotole and drugs for stimulation which the doctor may specify. (Figs. 79, 80.)
In the meantime, the force and frequency of the pains should be noted, and some doctors require a record of both the fetal and maternal pulse rate every half hour, and notification if the baby’s is over 150 or below 116, or the mother’s over 100 or below 60. Extreme restlessness, distress, vaginal bleeding, prolapsed cord, a temperature of 100° F., or any marked change must be communicated to the doctor immediately, if it occurs before he has started for his patient.
The patient may complain of intense pain in her back and cramps in her legs during the second stage. Pressure made by the nurse’s hand, or a small pillow slipped under the small of the back will frequently relieve the backache, while cramps in the legs may be relieved by straightening, and slightly elevating the leg, and rubbing it while in that position. As these pains are usually due to pressure they have no serious significance and subside as soon as the child is born.
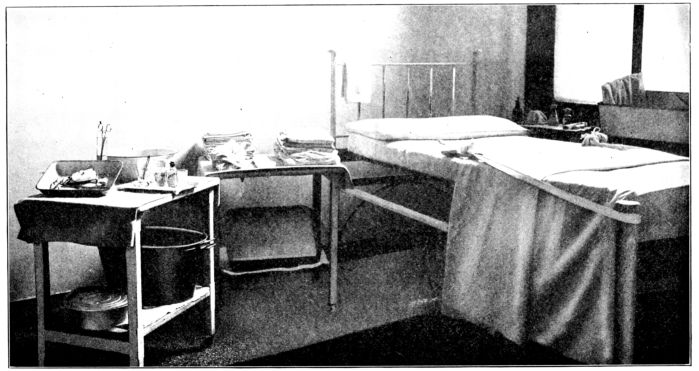
Fig. 79.—Bed and simple equipment in readiness for normal delivery. (From photograph taken at Johns Hopkins Hospital.)
260The nurse may find herself in any one of three situations during the second stage. The doctor may arrive in ample time to conduct the delivery; he may be slightly delayed and the nurse endeavor to retard labor, according to instructions; or the baby may be born, with or without the expulsion of the placenta, before his arrival.
When the doctor arrives at the onset of, or during the second stage of labor, the nurse acts solely under his direction, the nature of her offices depending somewhat upon the condition and surroundings of the patient, and whether or not the nurse is the only person at hand to give assistance. In any case, the gloves, and instruments for repairing a tear should be boiled and in readiness; the dressings and other articles to be used are to be conveniently arranged upon the tables and opened at the proper time.
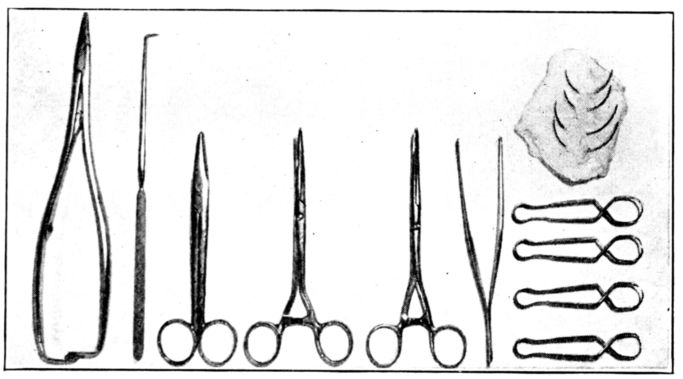
Fig. 80.—Instruments for normal delivery shown in boiling basin on table in Fig. 79: Needle holder. Blunt hook. Blunt scissors. 2 small Kelly clamps. Mouse tooth forceps. 4 towel clips. 2 large perineal needles and 2 cervical needles in gauze sponge.
After having everything ready and at hand for the delivery, the nurse may be called upon to clean up and act as an assistant, or to give the anesthetic. If she cleans up, she should wear a sterile gown and gloves, and if it is the doctor’s custom, a cap and mask as well, having prepared her hands somewhat as follows:[6]
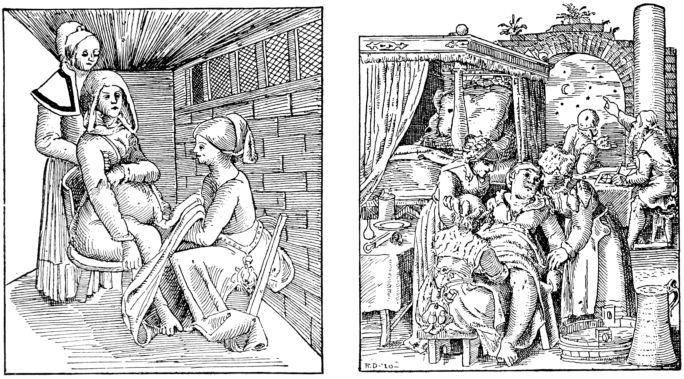
Fig. 81.—Old prints illustrating early ideas of suitable methods of making examinations and conducting deliveries, furnishing interesting contrast with present-day methods. Concern seems to be divided between the patient and the signs of the Zodiac in the picture at the right.
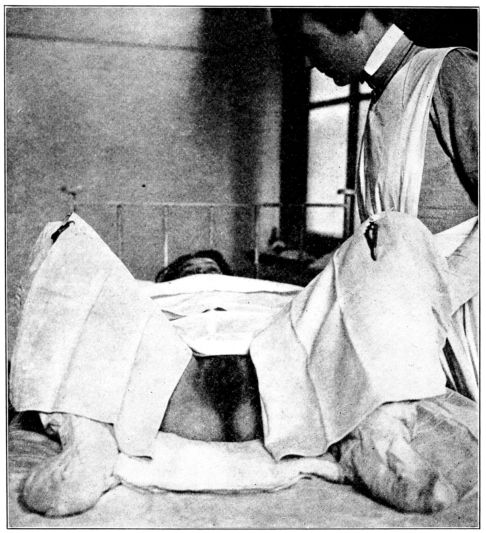
Fig. 82.—Patient draped with sterile towels, leggings, sheet and delivery pad for delivery. (From photograph taken at Johns Hopkins Hospital.)
The patient is given a final scrubbing with green soap and sterile water and an antiseptic solution, by some one with clean hands, and is further protected by means of sterile leggings, a sterile towel across the abdomen and one covering the inner surface of each thigh, held in place by sterile clips or safety pins. 263The lower half of the bed is covered with a sterile sheet while a sterile delivery pad is slipped under the patient’s hips. (Fig. 82.)
If the delivery is made with the patient lying on her side, the sterile dressings are so arranged as to cover all but the perineal region after she is placed in the desired position.
This brings up the question of the nurse’s obligation to protect her patient from the embarrassment of unnecessary exposure at any time during labor. The field which is prepared must be uncovered temporarily, and while the patient is being draped for examination or delivery a certain amount of exposure is unavoidable; but there are many little ways in which the nurse may show her consideration for the patient in this connection and the patient always appreciates the protection.
During the second stage, the preservation of asepsis, watching the progress of labor and watching for unfavorable symptoms, are of even greater importance than during the first stage. After the patient has been prepared and draped with sterile dressings, neither they nor the perineal region should be touched with anything unsterile.
If for any reason it has not been possible to sterilize sheets and towels, or more are needed after the prepared supply has been exhausted, the inner surfaces of towels and sheets that have been ironed either by hand or machinery, and folded with the ironed surfaces inside without being touched, may be regarded as practically sterile.
As the second stage advances, the patient may greatly aid the progress of labor by voluntarily bearing down during pains, and the nurse in turn may be called upon to help by encouraging her and explaining just what she should do. At the beginning of a pain the patient should take a deep breath, close her lips, brace her feet and strain with all her strength. If she opens her mouth and cries out, she fails to use her pains to the best advantage. The effect of this bearing down may be increased by providing the patient with straps, attached to the foot of the bed, upon which she may pull during the contractions, as she bears down. (Fig. 83.) Or, what is often a great comfort to her, she may pull upon the nurse’s hands as the latter braces 264herself so as to offer strong resistance. If the nurse can be spared from other duties to give this kind of assistance, it is indeed a comfort to the patient, who appears to derive from it both a moral and physical sense of being helped in her struggle. It is also important to assure the patient, between pains, that she is doing well, and that her efforts are advancing the baby, if this is true; and if not, she may under ordinary conditions be urged to make greater effort.
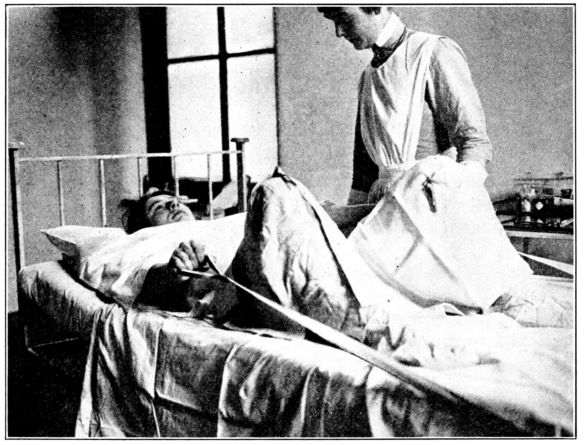
Fig. 83.—Patient pulling on straps while bearing down during second stage pains. (From photograph taken at Johns Hopkins Hospital.)
Before the head can be seen at the outlet or its advance noted by perineal bulging, the stage of its descent is often ascertained by palpating through the perineum, the fingers of a gloved hand pressing upward, on one side of the vulva. (Fig. 84. See Figs. 85, 86, 87, and 88 for appearance, advance and birth of head during normal delivery.)
Immediately after the birth of the head, and before the birth of the body, the nurse is frequently asked to wipe the baby’s mouth and eyes and sometimes to drop nitrate of silver into the eyes. In such a case she should wipe out the mouth very gently 265with a bit of sterile gauze, wet with boric, wrapped about her little finger, reaching well back into the throat; the eyes should be wiped from the nose outward, a separate wipe being used for each eye. The purpose of these maneuvers, when they are employed, is to favor respiration from the beginning by removing mucus that might impede it and to remove possible infective material from the lashes before it is spread to the conjunctivæ by the baby’s winking. The silver solution is to destroy germs that may have gotten into the eye.
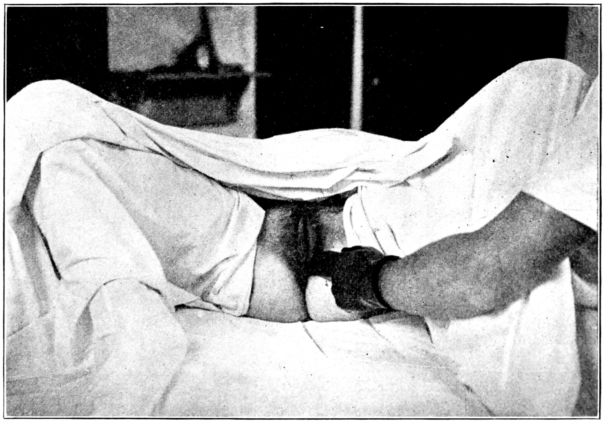
Fig. 84.—Palpating through the perineum to ascertain the stage of descent of the baby’s head. (From photograph taken at Johns Hopkins Hospital.)
As soon as the baby is completely born a sterile douche pan should be slipped under the patient or a small sterile basin placed close to the perineum, to receive the blood which escapes during the third stage. This is partly to protect the bed, but chiefly that the blood may be measured, as in no other way can it be ascertained how much the patient loses. A loss of 600 cubic centimetres or more is regarded as a hemorrhage.
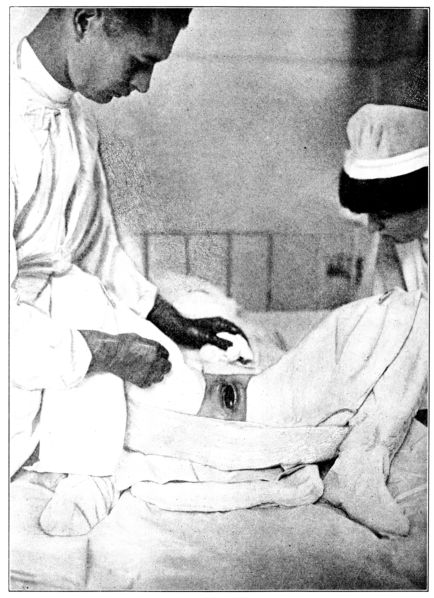
Fig. 85.—Baby’s head appearing at the vulva at the height of a pain. (This and succeeding pictures of a normal delivery are from photographs taken at Johns Hopkins Hospital.)
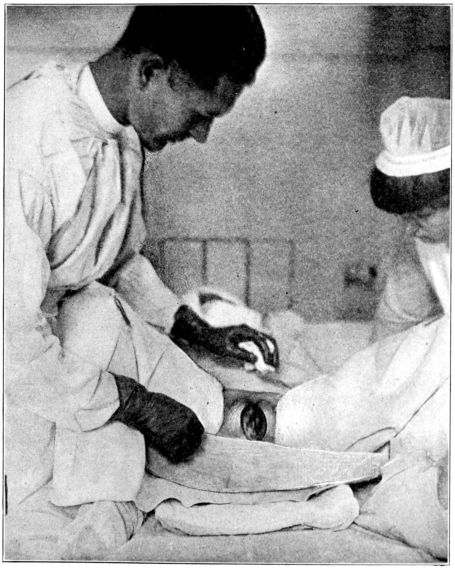
Fig. 86.—Advance of the head indicated by stretching of the vulva and perineum.
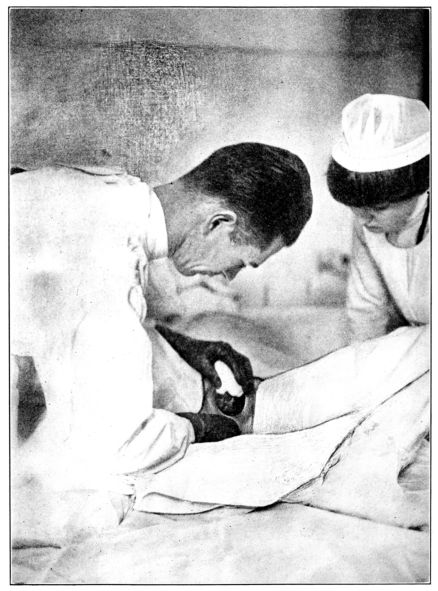
Fig. 87.—Holding back the head at the height of a pain to prevent a perineal tear.
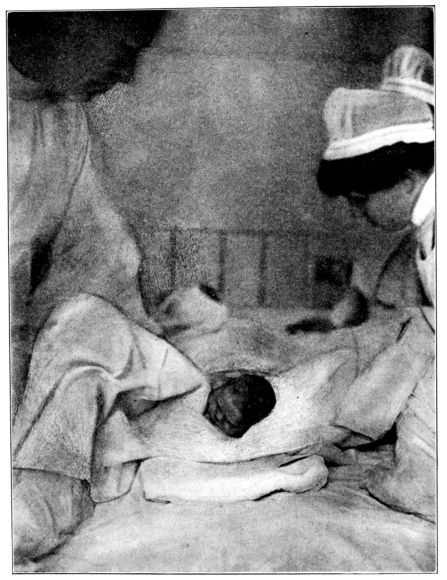
Fig. 88.—Birth of the head immediately followed by external rotation.
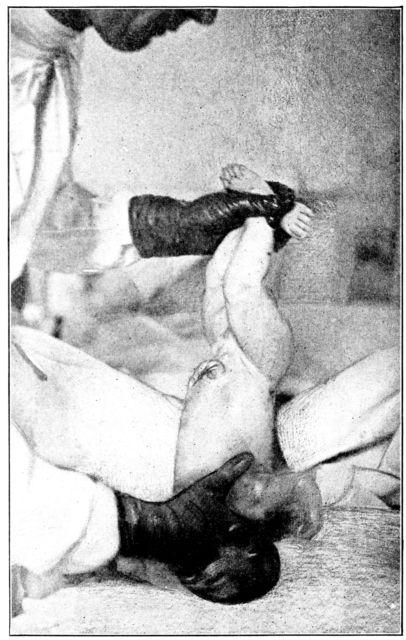
Fig. 89.—Wiping mucus from baby’s mouth with gauze wrapped about little finger.
Immediate Care of the Child. After the baby has been brought safely into the world, it is of greatest possible importance to make sure that it begins its separate existence by crying lustily, in order fully to expand its lungs. This provides for oxygenation of its blood, which has taken place, until now, through the placental circulation. In many cases the baby cries satisfactorily without aid, but not infrequently must be stimulated to do so. In all instances the first step is to clear the air passages of the mucus lodged in the mouth and throat, by some one of the many approved methods. One is by means of a piece of wet sterile gauze wrapped about the little finger, and wiped gently about in the back part of the baby’s mouth (Fig. 89), though many doctors object to this procedure for fear of abrading the very delicate mucous membrane, no matter how lightly it is done. They prefer to hold the baby by its feet, with the head hanging down and the neck sharply curved backward, when by gravity the mucus will drop out of the mouth; or, holding the baby by the feet, to run the thumb and forefinger along the 271neck on either side of the trachea, toward the mouth, and force out the mucus in that way. If the baby does not cry well after the mucus is removed, it may usually be stimulated to do so if held by the feet, head downward, and the back gently rubbed (Fig. 90) or the face stroked or the buttocks spanked two or three times. When holding the baby in this position the nurse should slip one finger between the ankles and grasp them firmly.
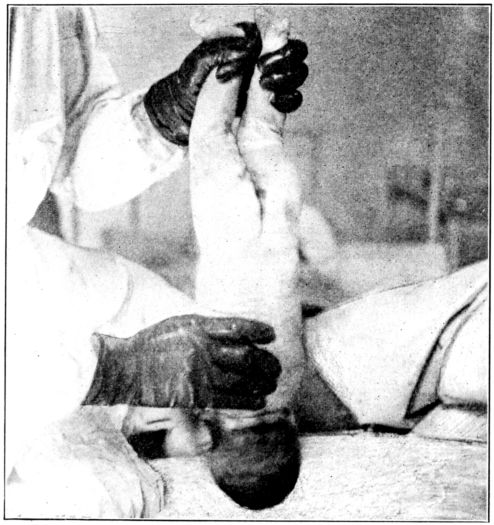
Fig. 90.—Stroking baby’s back to stimulate respirations.
After the baby has cried well it may be laid on the foot of its mother’s bed. At this juncture it seems pertinent to stress two points which must be remembered throughout the entire routine of the baby’s care, namely: the importance of protecting it from infection and from being chilled. As the baby lies on the mother’s bed, before the cord is cut, it finds itself in a room which is many degrees cooler than the very warm habitat from which it has just emerged; it is struggling to establish its functions, which are suddenly deprived of the mother’s help, chief 272of which at the moment are respiration and the circulation. Body warmth is one of the most valuable aids in promoting an even circulation, and accordingly the baby should be kept warm from the beginning. For this purpose there should be a small sterile blanket, or piece of flannel, in readiness to protect the little body as it lies on the bed, awaiting further developments. The hands and feet of the newborn baby that lies uncovered for even a quarter of an hour, or more, are nearly always cold, and as this must be guarded against in an older, more securely established baby, it cannot be desirable for the newly born.
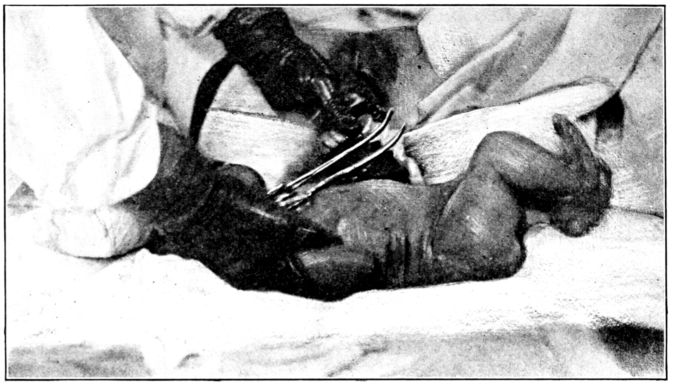
Fig. 91.—Showing two clamps on cord after pulsation has ceased.
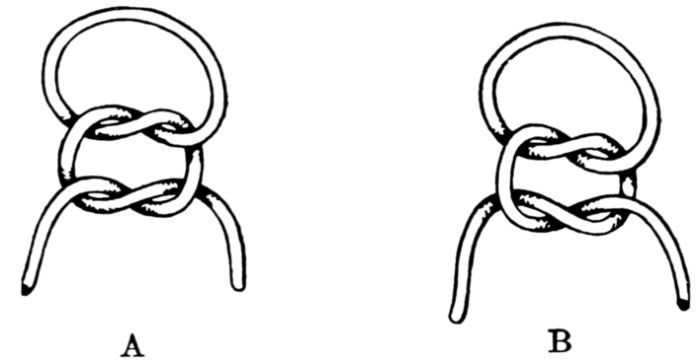
Fig. 92.—Wrong and right method of tying knot in cord ligature. A will slip. B will not.
As soon as the cord ceases to pulsate, it is usually clamped with two clamps about two inches apart (Fig. 91) and cut between the clamps. The scissors should have blunt points, in order not to scratch or cut the baby, who may be wriggling vigorously by this time. The cord is tied tightly with a sterile 273cord ligature, in a square knot that will not slip (Fig. 92), about an inch from the abdominal wall. It is considered a safe precaution, after removing the clamp, to bend the cord back upon itself and tie it a second time with the same ligature, as the danger of hemorrhage from a loosely tied cord is serious when the baby is kept sufficiently warm. The placental end of the cord is also tied, or it remains clamped until the placenta is expelled, because of the possibility of there being another child in the uterus and the danger of its bleeding to death through the open cord.
Some doctors do not tie the cord, but crush the vessels with a clamp which is left on the cord for about half an hour and then permanently removed, but this should not be done by a nurse upon her own responsibility.
Very often the person who performs the delivery removes the blood, mucus and vernix from the baby’s body, as soon as the cord is tied, by sponging it thoroughly with albolene or olive oil; wraps the cord stump with a sterile, dry or alcohol sponge and applies the abdominal binder while an assistant holds the baby by the feet, head down. It is also very common simply to oil the baby with unsterile lard, oil or vaseline, cover the cord with sterile gauze and leave the bath, cord-dressing and binder to be attended to later.
If the delivery takes place in a hospital the baby must be marked before it is taken from the delivery room, with adhesive plaster, upon which its mother’s name is plainly printed, or with the name necklace, now so frequently used.
The baby is once more wrapped in a warm blanket and placed, with a hot-water bottle, at 125° F., in the basket or box, which was prepared for it. Although the baby should be well covered, care must be taken to leave the face fully exposed as a young baby is easily suffocated. It was formerly customary to lay the new baby on its right side, but with the present fuller knowledge of the fetal circulation and the changes which take place after birth, this practice has been largely done away with.
Resuscitation of the Newborn Baby. If the baby breathes feebly, or even if it does not cry vigorously, the effort to stimulate the respirations may have to be continued for an hour or 274more after the cord is tied. In addition to the simple methods, previously described, which are very commonly employed at the time of labor, such as stroking the baby’s back or holding him by the feet and spanking him (Fig. 93), the following measures are sometimes resorted to if the baby’s condition demands it:
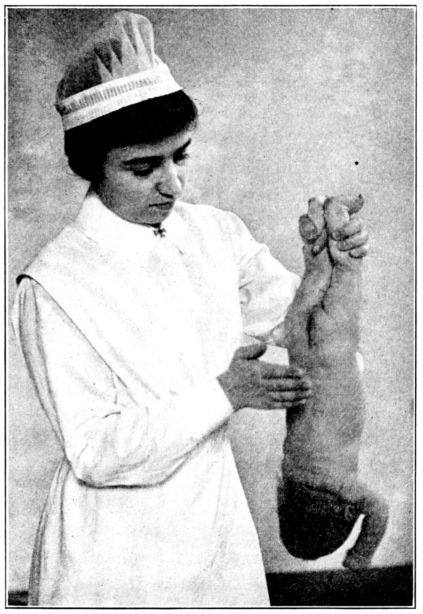
Fig. 93.—Stimulating respirations by holding the baby head downward and sharply spanking him. Note the method of grasping the baby’s ankles with one finger between them to prevent his slipping from the nurse’s hand.
One method is to hold the baby with its chest resting on the palm of one hand, with head, legs and arms hanging forward, thus compressing the chest wall and favoring expiration (Fig. 94), and then turning it over on its back, in the other hand, in which position the head, legs and arms hang backward, thus expanding the chest and favoring an inspiratory movement. 275(See Fig. 95.) Alternate repetitions of these positions, about twelve times a minute, will often stimulate the child to breathe satisfactorily.
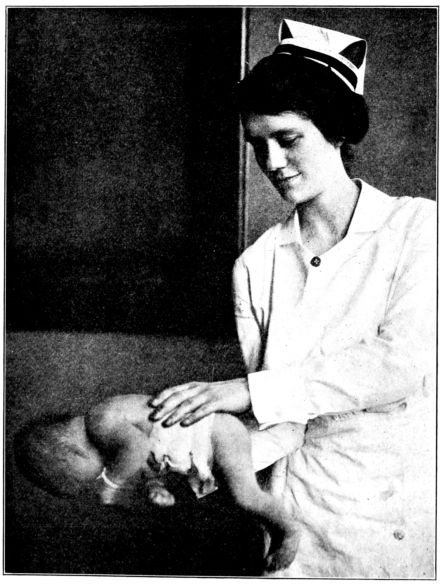
Fig. 94. (See also Fig. 95.)
Figs. 94 and 95 show method of stimulating respirations by resting the baby alternately on his chest and back on the nurse’s hands. (From photographs taken at Bellevue Hospital.)
Another method is alternately to plunge the baby into tubs of hot and cold water. But as there is doubt about the wisdom 276of chilling the entire surface of the baby’s body, the cold plunge is forbidden by many doctors, who, instead, dash a little cold water upon the face and chest, while the body is immersed in water at about 110° F.
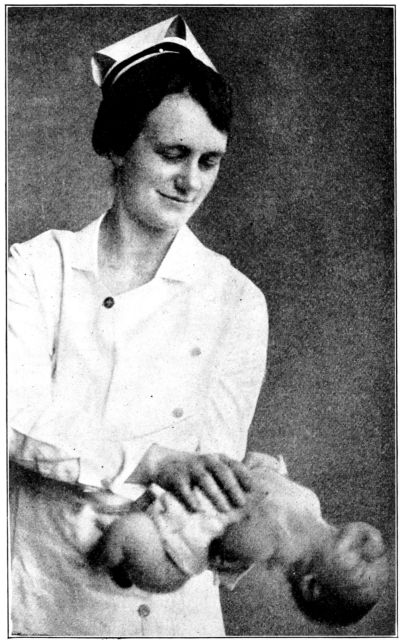
Fig. 95.—Resuscitating the baby. (See also Fig. 94.)
A widely used and efficacious method is to hold the baby continuously in a tub of water at about 110° F., and alternately extend and fold its body, thus keeping it warm while stimulating inspiration and expiration. (Figs. 96, 97.)
277Direct insufflation may be employed while the baby is in the warm water, by protecting its face with clean dry gauze and blowing directly into its mouth at intervals corresponding to those of normal inspiration. (Fig. 98.)
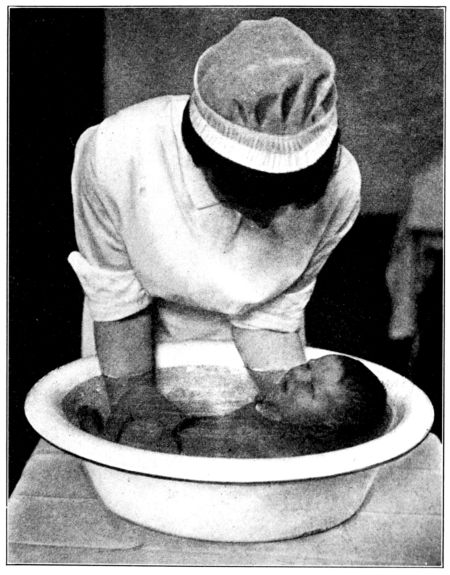
Fig. 96. (See also Fig. 97.)
Figs. 96 and 97 show method of resuscitating the baby by alternately
extending and folding his body under warm water. (From photographs
taken at Johns Hopkins Hospital.)
Another procedure is to hold the baby by the shoulders, with its body hanging down, thus expanding the chest, and then to toss it quickly upwards, folding the legs upon the chest to compress it. This method is objected to by many obstetricians on the ground that it both exhausts and chills the baby.
The outstanding requirements in resuscitating a baby are to stimulate its respiratory movements, by alternately expanding and contracting the chest; to promote its circulation by keeping it warm, and to avoid exhausting the very frail little body. Gentle handling, therefore, is important.
After the birth of the baby, some doctors request the nurse to rest one hand on the mother’s abdomen in order to feel the 279fundus as it rises while expelling the placenta, and to keep him informed concerning its consistency. Others regard this as a dangerous practice and forbid it.
As a rule, there is little bleeding until the placenta has separated. If bleeding does occur, it is the practice of some doctors to have the uterus gently massaged through the abdominal wall, to stimulate contractions, while others consider this inadvisable.
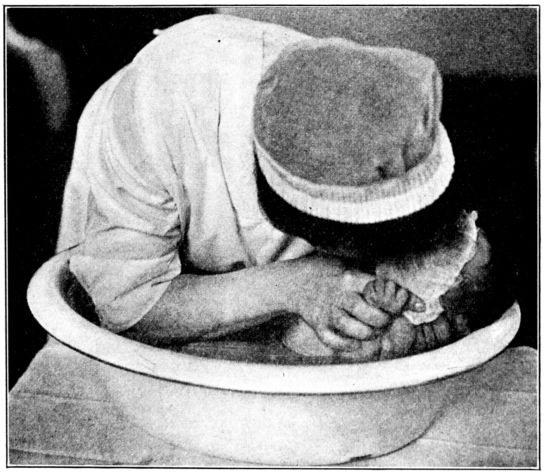
Fig. 98.—Stimulating respiration by means of direct insufflation, the baby’s face being covered with clean gauze. (From photograph taken at Johns Hopkins Hospital.)
After the placenta separates and descends into the lower uterine segment, it produces a bulging just above the symphysis, while the fundus may be felt as a firm, hard mass above the umbilicus. Since the placenta is entirely separated from the uterus at this time, its complete expulsion is usually aided, when it does not occur spontaneously, by gentle pressure upon the fundus. The accoucheur holds his hand just below the vaginal outlet, to receive the placenta (Fig. 99), which he turns over and over in his hands, thus twisting the membranes, and gradually draws it away from the mother, the membranes trailing 280after in the form of a tapering cord. (Fig. 100.) It is important that the placenta and membranes be carefully examined to make sure that they are intact, for if fragments of either are retained within the uterus they will prevent its firm contraction and thus may be a cause of post-partum hemorrhage. For this reason, only very gentle pressure and traction are used in expressing the placenta and withdrawing the membranes, for the use of force might leave small particles adhering to the uterine lining, which would otherwise separate with the rest, in due time, as a result of the uterine contractions.
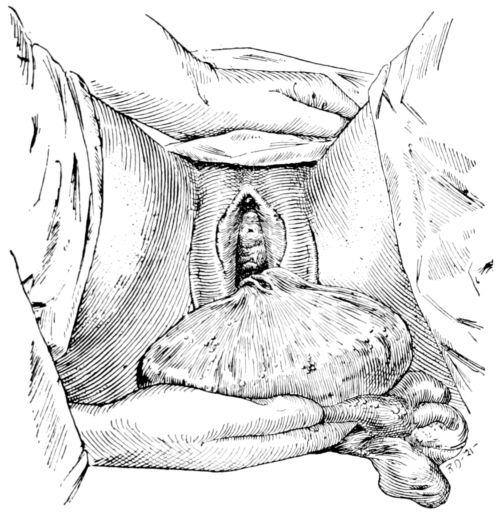
Fig. 99.—Delivery of the placenta.
Having been inspected, the placenta should be placed in a covered receptacle to be disposed of as the doctor directs, as many physicians make a routine laboratory examination of the placenta and wish to have it kept for this purpose.
With the birth of the placenta comes a gush of blood, as the uterine vessels, some of which are as large as a lead pencil at this time, are left wide and gaping. The bleeding usually subsides very shortly, however, as the blood vessels are closed by involuntary contraction of the network of uterine muscle fibres in which they are enmeshed, and which are sometimes referred 281to as “living ligatures.” If the bleeding continues, these contractions should be stimulated by massage. This is done by grasping the uterus through the abdominal wall firmly with one hand and kneading vigorously. Rubbing the top of the fundus with the fingers usually is not enough. The fundus should be grasped by the entire hand; the thumb curved across the anterior surface and the fingers, directed deep into the abdomen, behind it. (Fig. 101.)
Pituitrin or ergot, or both, are frequently given to further stimulate contractions of the uterine muscles. Since the action of pituitrin is quick, but evanescent, and the effect of ergot is slower and more lasting, both a quick and lasting effect is obtained by giving them together.
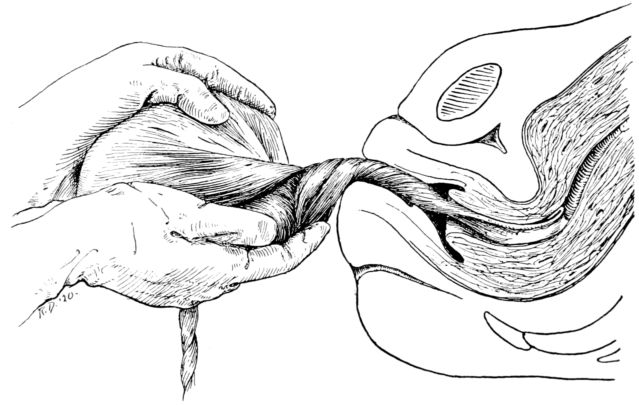
Fig. 100.—Twisting the membranes while withdrawing them from uterus.
The expulsion of the placenta ends the third stage and completes the process of labor.
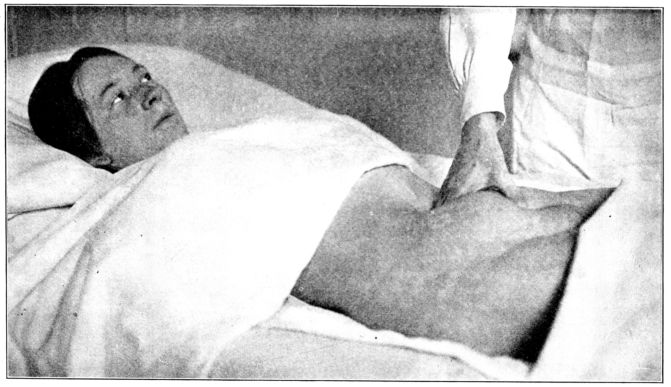
Fig. 101.—Grasping fundus through abdominal wall in giving massage to stimulate uterine contractions.
283Immediate After-care of the Patient. The patient should be bathed and dried about the thighs and buttocks, the vulva being bathed with alcohol or an antiseptic solution, and a sterile perineal pad applied. The douche-pan, wet towels, delivery pad and draw sheet are replaced by a dry draw-sheet and a towel or pad slipped under the patient’s hips, while a fresh nightgown is put on if the one worn during labor is wet or soiled. The perineal pad is very commonly held in place by a T. binder, with which all nurses are familiar, but some doctors prefer an abdominal binder to which a perineal strap is attached. This abdominal support may be a straight swathe or a Scultetus bandage, varying with the wishes of the doctor, and it may or may not be used in conjunction with a pad, so applied as to make pressure over the fundus. Other doctors forbid the application of any kind of a perineal dressing from the time of delivery, but instead, have a large, sterile pad slipped under the patient to receive the discharge.
The patient is usually tired and cold at the conclusion of labor, and may even have a nervous chill. Although this chill is not serious, the patient is none the less uncomfortable, and she should be warmly covered, be given something hot to drink, and a hot-water bag placed at her feet.
All possible effort must now be made to secure for her rest, quiet, and an opportunity to sleep. Every one but the doctor and the nurse had better be excluded from the room, which should be absolutely quiet, somewhat darkened and well ventilated. In addition to this, the majority of doctors now require that either they or the nurse shall stay with the patient and keep one hand resting on the fundus for at least an hour after delivery as a safeguard against post-partum hemorrhage. As long as the fundus is felt through the abdominal wall as a firm, hard mass, its irregularly arranged muscle fibres are contracted upon the blood vessels, and will prevent an escape of blood. But if the fundus feels soft and boggy, its muscles are relaxed, the constrictions are somewhat released from the open vessels, and serious bleeding may occur unless they are stimulated to contract again.
If the Doctor Is Delayed. It sometimes happens that labor progresses with unexpected rapidity, or that the doctor is delayed in his arrival and the nurse is accordingly confronted with the emergency of being alone with the patient during part or all of the delivery.
When the baby is making such rapid descent that the nurse fears it may be born before the doctor’s arrival, she may somewhat 284retard labor by covering her hand with a folded, sterile towel, if she has not had time enough to put on gloves, and hold back the head by pressing against the perineum during pains, at the same time instructing the patient to open her mouth, breathe deeply and try not to bear down. It is sometimes easier for the patient not to bear down if she lies on her side.
If by mischance, or in spite of her efforts, the baby so far descends that the brow appears before the doctor’s arrival, the nurse cannot safely hold it back longer because of the danger of the baby becoming asphyxiated. She should, up to this point, hold the head back during pains in order that the perineum may be stretched slowly, with the hope of preventing a tear. (See Fig. 87.) It is the sudden distension of the perineum and expulsion of the baby’s head at the height of a pain that frequently causes lacerations. If fecal matter is expressed during pains, the field should be wiped, downward, with sterile sponges and bathed with the antiseptic solution at hand.
After the brow is born, the nurse may gradually release the pressure and allow the head to emerge, and remembering the position of the child and the mechanism of its birth, assist Nature in its complete delivery. After the head is born, it drops down toward the mother’s rectum, after which external rotation, or restitution, takes place. (See Fig. 88.) A finger should be slipped around the neck in search of coils of cord, which, if felt, should be slipped over the baby’s head. Otherwise, pressure upon the cord in that unnatural position might so interfere with the circulation as to asphyxiate the baby.
The shoulders may be born spontaneously or the nurse may grasp the head with both hands, curving the fingers of one hand under the baby’s chin, and of the other, under the occiput, and make gentle, downward traction (See Fig. 69.) in order to slip the anterior shoulder from under the symphysis; and then pull gently upward, to deliver the lower or posterior shoulder (see Fig. 70.), after which the rest of the body follows easily.
This description of how a nurse may conduct a normal delivery by fairly typical and generally approved methods is only intended to guide her in an emergency, when there has been no understanding between her and the doctor about what she should 285do in event of his absence; or when he has authorized her to use her best judgment in safeguarding the lives of mother and baby.
It is obviously of extreme importance for the nurse to ascertain definitely the doctor’s wishes in this connection, as he sometimes will be unwilling to have the nurse give any attention to either mother or baby, even to tie the cord, before his arrival.
Prolapsed Cord. If the umbilical cord should prolapse at any time during labor, in the absence of the doctor, or lacking instructions, the nurse should elevate the patient’s hips, in order that gravity may lessen the pressure on the cord as it lies between the presenting part and the pelvic brim. Otherwise, the interference with the placental circulation may result in asphyxiation of the baby. (Fig. 102.)
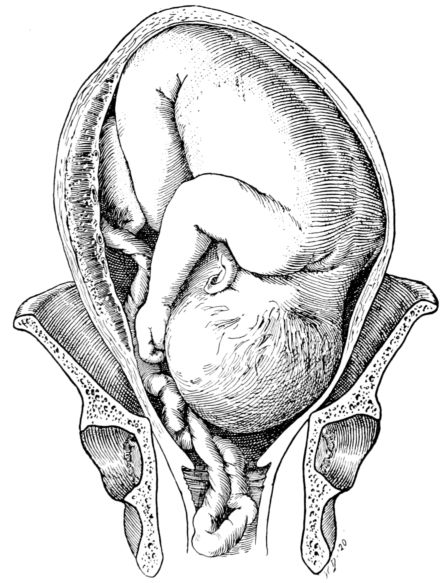
Fig. 102.—Drawing showing how prolapsed cord may be pressed between baby’s head and pelvic brim, thus cutting off placental circulation.
The elevated Sims position is often effective. Or, a straight chair may be upturned and pushed under the mattress, from 286the foot toward the head, in such a way that the patient will be lying on an incline which slopes upward from the head of the bed toward the foot. Or the chair may be placed in the same position on top of the mattress, with the top of the chair-back under the patient’s shoulders. The chair should be padded with pillows in order to minimize the patient’s discomfort as she lies in this trying position.
Post-partum Hemorrhage. Should a post-partum hemorrhage occur, in the absence of the doctor, the nurse should massage the fundus, unless she has been instructed not to, and have some one elevate the foot of the bed on blocks or the seat of a firm, straight chair. The use of ice bags or cold compresses on the abdomen is sometimes helpful and some physicians advise placing the baby at the mother’s breast immediately, since the suckling stimulates the uterine muscles to contract.
In anticipation of a post-partum hemorrhage, the nurse must have a clear understanding of the doctor’s wishes, particularly in regard to the administration of pituitrin and ergot which are so widely and efficaciously used to check post-partum bleeding.
Those of us who are accustomed to seeing anesthetics used to relieve patients of the worst of their pain, during labor, find it hard to realize that until comparatively recent years women went through this suffering without mitigation.
The use of anesthesia was introduced into obstetrical practice, in 1847, by Sir James Y. Simpson of Scotland, who first used ether but later adopted chloroform when he learned that it also had anesthetic properties. Its use in America was subsequently introduced by Dr. Channing of Boston.
In the early days, the idea of using anesthesia during labor was greeted with a storm of protest, both from the clergy and the laity, because of their belief that the relief of women in childbirth was contrary to the teachings of the Bible, as set forth in God’s curse on Eve, when He said, “In sorrow thou shalt bring forth children.”
There is to-day practical unanimity of opinion concerning the advantages which are derived from the use of anesthesia 287when any operative procedures are employed; but there is still some objection to its use in spontaneous deliveries. This is partly on medical grounds because of the possible ill effects of anesthetics and is partly a persistence of the early religious protest. However, in the vast majority of cases, some kind of an anesthetic, or analgesic, is administered to the woman in labor because the advantages of its use are generally conceded.
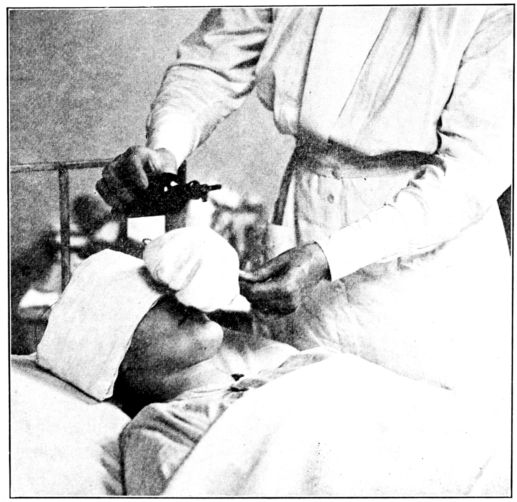
Fig. 103.—Method of giving chloroform for obstetrical anæsthesia.
The agents used are chloroform, ether and nitrous oxid gas, while what is popularly called “twilight sleep” is produced, completely or in a modified degree, by the hypodermic administration of scopolamin and morphine.
Chloroform. Of these various drugs chloroform is apparently the anesthetic most widely used in normal obstetrics. Its advantages are that it is easy to give; quick in its action and is followed by little or no nausea or other ill effects. For some reason, as yet not explained, the woman in labor enjoys a certain amount of immunity against chloroform poisoning, but this tolerance 288exists only during labor as the puerperal woman is subject to the same dangers as any other individual.
Chloroform is not usually administered until the patient is well along in the second stage, or until the head may be felt through the perineum, or is in sight. The patient’s face should be oiled and protected with a towel or gauze folded across her brow, mouth and chin to prevent burns that might follow the inadvertent dropping of chloroform on her face. With the beginning of a pain, a few drops are poured on the inhaler which is held about an inch from the face to give a free admixture of air, and the patient is told to breathe in deeply. (Fig. 103.) The inhaler is removed as soon as the pain subsides, but reapplied as soon as another pain begins. The patient retains consciousness and is able to talk under this degree of anesthesia, but her suffering is greatly relieved. It has the advantage, also, of lessening the danger of perineal tears, as the accoucheur has better control of the delivery when the patient lies quietly than when she tosses violently about the bed, and a tear resulting from the sudden delivery of the head at the height of a pain may in this way be averted.
This light, intermittent anesthesia, now so widely used, is called obstetrical anesthesia or anesthesia à la reine, after Queen Victoria, upon whom it was first employed at the birth of her seventh child, in 1853.
When the perineum is distended to its maximum, obstetrical anesthesia is not always sufficient, and complete anesthesia may be employed; but even this requires very little chloroform. Under ordinary conditions, the anesthesia is discontinued as soon as the child is born, for unless there is an extensive tear, the patient is sufficiently anesthetized to permit of a perineal repair and the delivery of the placenta.
Chloroform is not often given early in labor because of the general belief that its free or prolonged use lessens the force and frequency of uterine contractions, thus prolonging labor, and also may unfavorably affect the child. But small doses seem to stimulate rather than retard contractions, and by having her pain relieved, the patient is prompted to make greater effort to use her abdominal muscles, an end greatly to be desired.
289If complete anesthesia is needed for more than a few moments, after the child is born, ether usually replaces the chloroform, being considered more satisfactory for prolonged anesthesia, but many obstetricians prefer not to give it until after delivery because of its possible effect upon the child.

Fig. 104.—Giving ether for obstetrical anæsthesia. Ether is poured into cone which is covered with nurse’s hand to prevent evaporation. When the beginning of a contraction is felt by hand on abdomen, the cone is placed about an inch from the patient’s face. (From photograph taken at the Maternity Hospital, Cleveland.)
As chloroform poisoning is likely to produce degenerative changes in the liver, and eclampsia also causes a liver necrosis, chloroform is not used for an eclamptic patient.

Fig. 105.—As pain increases and patient becomes accustomed to ether, the cone is lowered and held close to her face until pain subsides. Sufficient ether to control the next pain is then poured into cone. (From photograph taken at the Maternity Hospital, Cleveland.)
Ether, also, is used widely in normal obstetrics and is almost always preferred for continuous anesthesia, because of its being safer than chloroform. Unlike chloroform, ether is sometimes given in the first stage after the pains have become severe and frequent. About a dram of ether is poured into the cone which is held just off the patient’s face (Fig. 104.) until the beginning of a contraction, at which time it is lowered and held close to her face (Fig. 105.) As the action of ether is slower than chloroform, it should be poured into the cone in advance of a pain, which the nurse anticipates by feeling the uterus begin to grow hard under the hand which she keeps upon the patient’s abdomen. If the ether is not poured into the cone 291until a pain begins, its anesthetic effect may be lost because of the delay in its administration.
At the Cleveland Maternity Hospital, where ether is used during normal labor, the nurses are taught to give it as has just been described, with further instructions from Miss MacDonald, as follows: “A patient will vaporize about one dram of ether per pain during the early first stage, gradually vaporizing a greater amount until she will vaporize two or three drams per pain near the end of the second stage. Should the patient reach the excitement stage of ether before she is in the second stage of labor, discontinue the ether for from five to fifteen minutes, then give a lessened amount.
“Should it be necessary to control the descent of the presenting part, light anesthesia may be given. This may be managed by putting about two drams of ether in the cone at intervals frequent enough to sufficiently retard the descent of the presenting part. This procedure almost obliterates contractions. Lift the cone from the face for a few moments at frequent intervals to admit air. Keep the ether vapor of such concentration as avoids choking, coughing or vomiting. This may be done by administering a small amount frequently, rather than a large amount at longer intervals. When the desired stage is reached, try to keep the patient at this degree of anesthesia by giving a few drams of anesthetic at regular intervals.”
Nitrous Oxid Gas Analgesia. The effect of this drug is termed analgesia rather than anesthesia, because the patient does not lose consciousness but is unconscious of pain. From a medical standpoint it is considered practically ideal for use in obstetrics. If given skillfully it seems to have no bad effects upon the child; it tends to stimulate, rather than diminish uterine contractions; it may be started, with safety; as soon as the patient begins to suffer severely, and continued for several hours if necessary.
Its disadvantages are that it is very expensive; it can be given safely only by a skillful, trained person; the apparatus necessary for its administration is expensive, heavy and difficult to transport. But when these difficulties can be overcome, its use is attended with very satisfactory results.
292“Twilight Sleep,” so called, or Dämmerschlaf, as it is termed in Germany, has been and still is discussed so widely, that the nurse should know something of it, whether or not she aids in its administration. It may be described as a state of amnesia, or forgetfulness, produced by the hypodermic injection of morphin and scopolamin. The patient, therefore, is conscious of pain at the time but speedily forgets it.
This treatment was first used widely in Freiburg. Following an enthusiastic report from there upon a large number of cases in which it had been used, there was such a clamor for it by American women, that its temporary use was practically forced upon obstetricians in this country. It was given what appears to have been a fair trial, but its continued use in this country has not been widespread. Those obstetricians who object to its use describe its disadvantages as follows: It cannot be used outside of a well-conducted hospital; it requires the constant attendance of a well-trained obstetrician or obstetrical nurse throughout the entire course of labor; it is suitable for use in certain selected normal cases only; it prolongs the second stage and increases the percentage of cases in which operative interference is necessary; it has an asphyxiating effect upon the child and increases the percentage of fetal deaths.
On the other hand, the use of scopolamin and morphin is a routine in certain excellent maternity hospitals, and by many obstetricians of the first rank, who maintain that with a nurse in attendance and the observance of ordinary precautionary measures, the advantages far outweigh the disadvantages of a modified “twilight sleep.” An anesthetic is usually administered during the second stage, after the use of the scopolamin-morphin treatment.
Complete Anesthesia. If an emergency should arise and the nurse be required to change from the light anesthesia à la reine, and to give complete anesthesia, her responsibilities increase, for she must watch carefully the patient’s pulse, respirations, color and pupils. The flat pillow which is ordinarily left under the patient’s head during normal labor, should be removed and the inhaler should be held closely over her face with the 293nurse’s fingers so placed as to hold it in position and also to hold the patient’s jaw forward and up. (Fig. 106.)
The ether should be dropped in clean drops, not poured, upon the inhaler. The dripping should be steady, but slow at first, gradually increased as the patient becomes accustomed to the fumes.
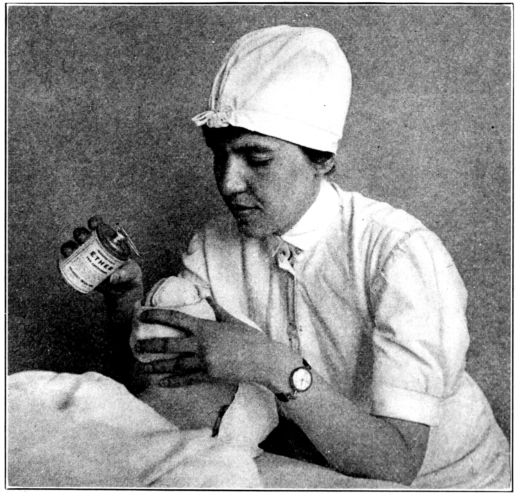
Fig. 106.—Method of holding inhaler and supporting patient’s jaw in giving ether for complete anesthesia. (From photograph taken at Johns Hopkins Hospital.)
With the average, normal patient who is taking ether well the respirations become somewhat stertorous and more rapid, increasing to possibly 36 or 40 per minute; the pulse starts at a little above the normal rate and increases to 116 or 120 and then drops to normal, which is slightly below the rate at which it started; the color is normal at first and then may become crimson, or it may change very little; the pupils first dilate, and then contract almost to a pin point.
294Unfavorable signs are: respirations that are rapid and shallow, then possibly slow, but still shallow; increasing pulse rate, this being so serious that the ether is usually stopped if the pulse approaches 140, and stimulation is promptly given; cyanosis which is slight at first and then extreme, and dilated pupils.
It is obviously not wise nor possible to attempt, by means of a few paragraphs and illustrations to teach a nurse so technical and important a procedure as the administration of an anesthetic, but it is hoped that these general suggestions may be helpful, particularly to the nurse who is unexpectedly confronted by an emergency.
Under all conditions the nurse must remember that no matter what anesthetic is given, nor by whom it is administered, she must guard against the very prevalent tendency to talk freely while the patient is going under, in the belief that she is unaware of what is going on about her. Many patients suffer great mental distress because of hearing, or partly hearing conversation not intended for their ears, which takes place in their hearing while they are incompletely anesthetized.
Unhappily, not all labors run the smooth and uncomplicated course which was described in the last chapter. Certain abnormalities sometimes arise to complicate delivery, occasionally necessitating operative interference or relief.
There is little that a nurse can do alone, in the presence of complicated labor, but her preparations and assistance will be more effective if she understands the purpose of the operations, and she will better appreciate the gravity of certain symptoms, which she is required to watch for and report, if she realizes the extreme seriousness of their import.
The principal conditions which give rise to, or follow complications, prevent spontaneous delivery or necessitate operations at the time of labor are perineal lacerations; contracted or malformed pelves; marked disproportion between the diameters of the child’s head and mother’s pelvis; ruptured uterus; exhaustion of the mother; poor muscle tone or certain chronic and acute diseases of the mother; death of the fetus; prolapsed cord; certain presentations of the fetus in which spontaneous delivery is doubtful or impossible.
The preparations for operations in hospitals are all so carefully planned and systematized that in the presence of such emergencies the nurse will merely have to carry out the customary routine, but in a patient’s home she may have to exercise a good deal of originality in attempting to meet the needs of the occasion and imitate hospital provisions.
A satisfactory operating table may be fashioned in any one of a number of ways. If the bed is high enough, it may sometimes be made fairly satisfactory by slipping a board, such as a table leaf, under the mattress to make it firm. The use of a 296kitchen table is time-honored, but it is an unsafe practice unless the available table is very secure and firm, which is usually not the case with present-day kitchen tables. A flat-topped chest of drawers, with the casters removed, makes an excellent operating table, for it is firm, a good height and about the right size. Or an ordinary bureau may be pressed into service after taking out the casters and removing the mirror by unscrewing its supports. The front and sides of a bureau, or chest of drawers so used should be protected from the damaging effects of fluids and solutions by being covered with a bed-rubber or newspapers. A pad for the top of the improvised operating table may be arranged by folding a blanket or quilt to the proper size and folding over that the rubber draw-sheet and a clean muslin sheet.
If the operation requires that the patient be held in the lithotomy position (on her back with thighs and knees flexed and knees well separated), and the doctor’s equipment does not include a strap to hold the legs, one may be improvised from a sheet. It should be folded diagonally, over and over, into a strip possibly a foot wide, passed over one shoulder and the tapering ends used to tie around the legs, above the knees, to hold them in the desired position. Bandages or tapes are not always satisfactory, for the support is subject to a good deal of strain, and narrow strips sometimes cut painfully into the legs and shoulders. Certainly if tapes or bandages are used, cotton pads or folded towels should be interposed between them and the patient’s skin.
In general, the nurse will prepare as for a normal delivery, in each instance adding such details of equipment, or preparation as the contemplated operation requires. Rigid asepsis must be observed throughout the preparations and the operations. When large instruments or appliances are to be used, a wash boiler is probably the safest thing in which to boil them, for it is scarcely possible entirely to cover them with water in a smaller receptacle; and they must be well covered while boiling, or they will not be sterile.
Perineal Lacerations. A large proportion of women during the birth of the first baby sustain some degree of perineal laceration, 297which may amount to nothing more than a nick in the mucous membrane, or it may extend entirely across the perineal body and tear through the rectal sphincter. The causes of these tears are generally conceded to be rigidity of the perineal muscles; disproportion between the size of the child’s head and the vulval opening; a sudden expulsion of the child’s head, before the perineum is fully distended, and certain abnormalities in the mechanism of labor. Lacerations may, therefore, be prevented, or limited, in many cases by holding back the baby’s head and allowing it to dilate the perineum slowly. But in spite of the most skillful and careful efforts, tears of some degree occur in most primiparæ, and probably in half of all multiparæ. These injuries are usually described as being of the first, second or third degree, according to their extent.
A first degree tear is one that extends only through the mucous membrane, usually at the margin of the perineum, without involving any of the muscles.
A second degree tear is one that extends down into the perineal body and may involve the levator ani, or even extend down to, but not through the rectal sphincter. Such a tear usually extends upward on one or both sides of the vagina making a triangular injury.
A third degree tear extends entirely across the perineal body and through the rectal sphincter and sometimes up the anterior wall of the rectum. This variety is often called a complete tear, in contradistinction to those of first and second degree, which are incomplete.
It is a fairly general custom to repair these lacerations at the time of labor, no matter what their extent, the sutures being introduced but not tied, during the third stage. The patient is usually sufficiently anesthetized to permit of this, without further anesthesia, in all but complete tears, and as there is usually but very slight bleeding before the expulsion of the placenta, the field is comparatively clear and the stitches are easily put into place. They are not tied, as a rule, until after delivery of the placenta because of the strain which its expulsion would put upon the fresh stitches. In all but very slight tears, the doctor will usually want the patient turned across the 298bed, with her hips brought to the edge, and her legs supported in the lithotomy position. As the few instruments necessary for perineal repairs should be boiled and placed in readiness before labor, there is usually no further preparation for the nurse to make, and the perineal dressing, after the stitches have been taken, is ordinarily the same as that following a normal delivery. (See Fig. 80 for necessary instruments.)
Some physicians prefer not to repair perineal tears until some days after labor, contending that the congestion of the soft parts immediately after delivery is not favorable to a satisfactory union. When the repair is made subsequently, therefore, the nurse prepares as she would for any perineal operation, performed independently of labor. Repairs are not often postponed for more than a few days, since long delayed or neglected attention frequently gives rise to gynecological disorders, such as descensus or prolapse of the uterus.
Episiotomy. Some obstetricians prefer to anticipate a perineal tear by making an oblique incision, usually on one or both sides, extending downward and outward from the margin of the vaginal outlet down into the perineum. This operation is termed episiotomy, and the incision is sutured after labor just as a tear would be. It is the belief of those who perform this operation that the clean-cut incision heals more satisfactorily than an irregular tear, and that by directing the incision to the side, away from the median line, the integrity of the rectal sphincter is preserved, even though the perineum tears beyond the end of the incision, when distended during the birth of the head.
Breech Extraction. In some cases of breech presentation, particularly among primiparæ, it is necessary to assist nature in the delivery of the child in order to save its life. Complete anesthesia is usually necessary at such times and the patient is preferably on a table or at the edge of the bed in a lithotomy position.
In the majority of cases, no effort is made toward assistance until the body is born as far as the umbilicus, partly because of the difficulty of taking hold of the child securely before that time, and partly because the perineum is not likely to be fully 299distended, in which case a serious tear would probably result. But after the body has been extruded as far as the umbilicus, it is usually considered imperative to complete the delivery within eight minutes to save the child from asphyxiation, due either to pressure on the cord between the head and pelvic brim, or to premature separation of the placenta. The baby’s feet or legs are grasped by a towel to prevent slipping, and downward traction is made on the body until the tips of the scapulæ appear at the outlet. During this procedure the nurse may be called upon to make pressure on the uterus with the idea of keeping the baby’s head flexed forward; preventing the arms from becoming extended upward above the head and also to help in expelling the child.
After the scapulæ appear, the arm lying posteriorly is brought down over the chest and delivered. The body is then rotated until the other arm lies posteriorly and that is delivered. After delivery of the arms and shoulders the head is usually delivered by what is known as Mauriceau’s maneuver as follows: The accoucheur slips the index finger of one hand into the vaginal outlet and into the child’s mouth, and supports the body of the child upon his hand and forearm; two fingers of the other hand are slipped around the back of the neck and curved forward like hooks over the shoulders and strong downward traction is made by these fingers; not by the one in the baby’s mouth. The occiput emerges from beneath the symphysis, after which the body is lifted upward and the chin, nose, forehead and entire head are born.
Version. By version is meant the turning of the child within the uterus so that the part which was presenting at the superior strait is replaced by another part, in order to hasten or facilitate delivery. It is usually performed as the patient lies flat on her back, completely anesthetized, and with great gentleness, for fear of rupturing the uterus.
Common indications for a version are a transverse presentation; a prolapsed cord, when the head has just begun to enter the superior strait; and in some cases of placenta prævia. When the fetus is so turned that the head becomes the presenting part, the procedure is termed a cephalic version; if so turned that 300the breech presents, it is termed a podalic version. The methods of accomplishing these ends are described as external version, if the turning is done entirely with the hands working through the abdominal wall; internal version if one entire hand is introduced into the uterine cavity, and combined version when one hand is outside on the abdomen and two fingers of the other are introduced through the cervix into the uterus.
External cephalic version is often performed late in pregnancy, or early in labor, in transverse and also in breech presentations, to secure a vertex presentation because of the high fetal death rate in breech extractions. Podalic version, or making the breech the presenting part, is often performed in transverse presentations, in placenta prævia and when the cord or extremities are prolapsed. Having converted the presentation into a breech, the usual breech extraction is performed.
Forceps are instruments which are used to extract the child when presenting by the head in certain conditions which endanger the life of mother or child. The value of forceps in obstetrics can scarcely be overestimated, as before their invention the only operative method of delivering a live baby was by means of version and extraction, and in these the fetal death rate was high. The obstetrical instruments in use up to that time, therefore, were all for the destruction of the child in utero.
Forceps were devised, and first used, in great secrecy, early in the 17th century, by a Dr. Chamberlen, in England, who jealously guarded all information relating to his invention from every one but members of his own family.
There were several doctors in the Chamberlen family who practiced obstetrics and who used these forceps, but knowledge concerning the nature of the instruments and methods of using them was not shared with members of the medical profession outside of that family, until the beginning of the 18th century. Since that time the use of forceps has been widely extended and the original Chamberlen instruments have been so modified and altered and improved by different obstetricians, that there is now a bewildering number and variety in existence and in use. Probably the most widely used are those which were devised by Dr. Tarnier of France and Dr. Simpson of England, respectively. (Fig. 107.) The Tarnier instrument is known as an axis traction 301forceps, and can be used in all kinds of forceps operations, while Dr. Simpson’s are suitable for use only in low forceps cases.
There are two groups of indications for the use of forceps; those relating to the condition of the child and those relating to the mother.
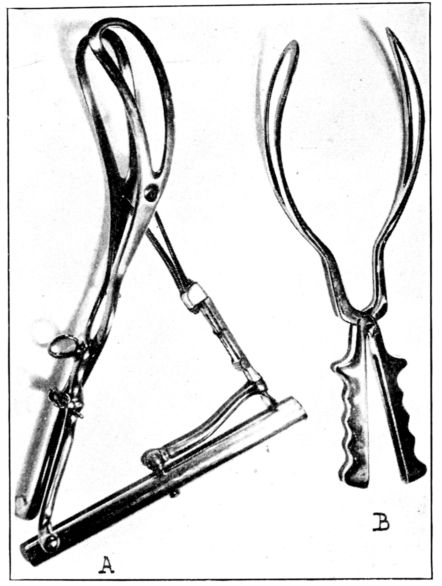
Fig. 107.—Two widely used forceps. A, Tarnier axis-traction forceps. B, Simpson forceps.
Indications for their use in the interests of the child are symptoms of asphyxia, and these are the passage of meconium, in head presentations, and a change in the rate or rhythm of the fetal heartbeat. As pressure on the abdomen of the fetus during labor, in breech presentations, is very likely to express meconium, this is not of special significance in these cases. But in head presentations, the escape of meconium suggests paralysis of the rectal sphincter muscles, due to imperfect oxygenation, which, in turn, is caused by interference with the placental circulation by pressure on the cord or premature separation of the placenta.
Conditions which menace the life of the mother, and indicate 302the use of forceps, are inadequate contractions of the uterine and abdominal muscles; exhaustion, as indicated by an increase in the maternal pulse rate or elevation of temperature, and in certain chronic and infectious diseases, when the patient may be unable to stand the strain of the second stage.
Forceps are usually employed when the head fails to make satisfactory advancement after two hours of good, second-stage pains, or when it remains in one place on the perineum for an hour, in spite of good, second-stage pains.
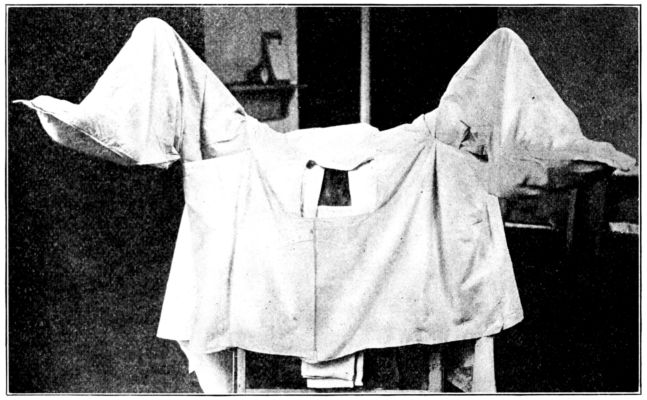
Fig. 108.—Patient in position and draped for forceps operation. (From photograph taken at Johns Hopkins Hospital.)
Otherwise, there is danger of necrosis or sloughing of the soft parts as a result of pressure, with a subsequent recto-vaginal or vesico-vaginal fistula.
Among the acute conditions in which forceps are indicated are typhoid fever; pneumonia; acute edema of the lungs, hemorrhage from premature separation of the placenta; intra-partum infection and eclampsia, while they are sometimes used in such chronic conditions as pulmonary tuberculosis; various heart lesions, particularly when there is broken compensation.
Before applying forceps the operator will usually wish to satisfy himself that the following conditions exist: Complete dilatation of the cervix, otherwise severe lacerations with hemorrhage 303may result; the head must have entered the pelvis, otherwise an imperfect application of the forceps may result in death of the fetus and serious injury to the mother; the position of the child’s head must be known in order that the forceps may be properly applied over the ears; the membranes must have ruptured or the forceps may slip.
Forceps operations are usually designated as being high, mid or low, depending upon the level to which the head has descended into the pelvis. If the head is at the superior strait, a high forceps operation is necessary; mid forceps if the head is half way down and on a level with the ischial spines and low forceps when the head is on or just above the perineum.
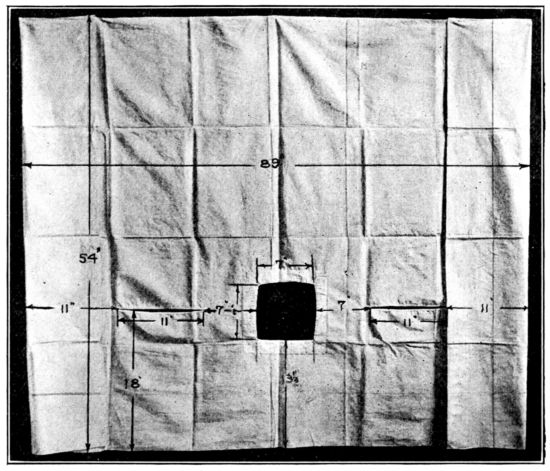
Fig. 109.—Forceps sheet used in Fig. 108.
The application of low forceps is a simple operation and attended by little danger to mother or child; mid forceps is more serious and high forceps is very serious for the child and sometimes for the mother.
When forceps are applied, the patient must be at the edge of the bed or preferably on a table, in the lithotomy position (Fig. 108), and completely anesthetized. She should be shaved and scrubbed as for a normal delivery, after which a sterile 304towel soaked in bichlorid 1–1,000 or lysol 2 per cent., is placed over the vulva and allowed to remain until the operation is performed. She should be draped with sterile leggings and towels, one of which is folded over the centre of a wide strip of adhesive about twenty inches long, and hung curtain-like over the rectum by strapping the free ends to the buttocks on each side, while over all is placed a sheet with three openings; two slits for the legs to pass through and one rectangle which exposes the field of operation. (Figs. 109, 110.)
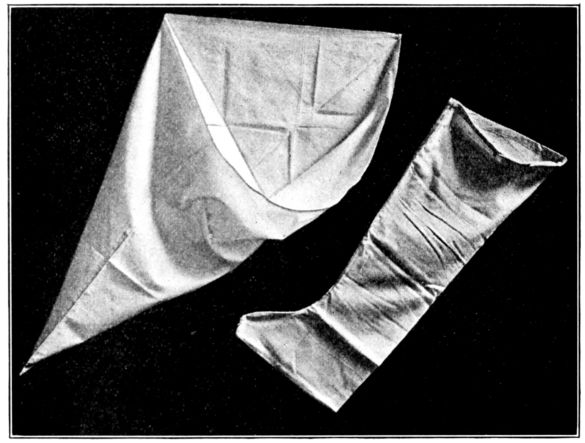
Fig. 110.—Two types of easily made leggings suitable for use during delivery or obstetrical operations.
Pubiotomy, or hebotomy, consists in sawing through the pubic bone on one side of the symphysis with a string or Gigli saw. This operation is performed in some cases of moderately contracted and funnel pelves, through which the normal expulsive forces of labor are unable to force the child. The separation of the bone allows it to gape, because of the hingelike movement of the sacro-iliac joint, and thus the superior strait is appreciably widened and the child may be delivered by high forceps or version. As the bone heals by fibrous union, there is sometimes permanent enlargement of the 305pelvis and there are seldom any unsatisfactory after-effects, such as impairment of locomotion. Pubiotomy is sometimes the operation decided upon when a patient is seen for the first time after labor is well advanced, and a conservative Cæsarean section is thought inadvisable because of the risk of infection. But the operation is becoming more and more rare, for the general practice of measuring the pelvis and supervising patients during pregnancy discloses serious disproportions early enough to make a Cæsarean section the elective operation.
Symphysiotomy. This operation is a cutting through the cartilage of the symphysis pubis, instead of through the pubic bone, as in pubiotomy. It was formerly performed for much the same reasons that pubiotomy is now used, but has been practically abandoned since the development of the latter operation. The reasons for giving it up were that the close proximity of the bladder to the symphysis resulted in frequent injuries to that organ, and as the cartilage of the symphysis does not heal as well as the pubic bone, the patients frequently experienced difficulty in walking and showed a tendency to tire more easily after the operation than before it was performed.
Vaginal Hysterotomy, or vaginal Cæsarean section, as it is sometimes called, consists of incising the cervix anteriorly and posteriorly, delivering the child and placenta and suturing the wounds. It is sometimes performed in cases which for some reason require immediate delivery, as in severe cases of eclampsia. It is only possible when the relation between the pelvis and the child’s head is such as to permit the child to pass through the inlet. It is rarely done in primiparæ, because rigidity of the outlet prevents proper exposure; or in multiparæ at term as the incisions have to be extended so high to deliver a term baby, that there is danger of tearing the lower uterine segment.
Cæsarean Section is the operation by means of which the child is delivered through an incision in the abdominal and uterine walls. It is believed by some that the operation was named for Julius Cæsar, who was presumably delivered by this method, but this seems scarcely probable. The operation was frequently fatal in those days and, moreover, as the uterine wall was not sutured after the child was extracted, a woman was not 306likely to have other children afterward even if she did live, and Cæsar’s mother had several children after he was born. Another explanation for the name is that during Cæsar’s reign a law was passed which required that the abdomen be opened and the child extracted in every case in which a woman died late in pregnancy, as one means of increasing the population.
Thus it will be seen that the operation itself is very ancient, but as performed to-day it embodies the most modern and scientific knowledge and methods. The usual indications for it are cases of contracted or deformed pelves; cases of tumors which block the birth canal or when very speedy delivery is imperative as in some cases of eclampsia.
The anatomical indications for Cæsarean section are dependent upon the degree and character of the pelvic contractions and upon the size and mouldability of the child’s head in relation to the pelvis. This explains why in two women with pelves of the same size and shape, one will have a spontaneous delivery and one will require a section. The former has a relatively small child which can pass through her pelvis; while the second woman’s baby is too large, or the head not sufficiently mouldable, to pass through hers.
This is one exemplification of the great importance of pelvimetry and of constant watching during pregnancy, for the best results from Cæsarean section are obtained when it is recognized that spontaneous delivery is unlikely or impossible; the operation accordingly is performed at a time which is deliberately selected by the obstetrician. The elected time is often about two weeks before the expected date of confinement in order that the baby may have the longest possible intra-uterine life and that the operation may be performed before the patient goes into labor. In these cases in which it is known that a section is to be performed vaginal examinations are omitted after the pelvic measurements are taken, in order to minimize the possibilities of infection, this being one of the great risks of the operation.
Until recent years the operation was usually delayed until after the patient had been vaginally examined, had been in labor long enough to be exhausted and the only other courses open were high forceps or a destructive operation upon the child. The 307results of the operation undertaken under such circumstances were not good, and the maternal deaths from infection were so frequent that the operation on the whole was very hazardous. But improved surgical technique and extended knowledge of the pelvis have so revolutionized Cæsarean section that it is now successful in the majority of cases.
There are three main types of Cæsarean section: conservative, radical and extraperitoneal.
The conservative operation consists of opening the abdomen in the mid-line; incising the uterus; extracting the child and placenta, and suturing both uterine and abdominal walls. This is the usual operation when there is a choice, but because of the danger of infection, it is ordinarily performed only before the onset of labor or in the early part of the first stage, and many obstetricians are loath to undertake it then if the patient has been examined vaginally, particularly if the technique of the examination was open to question.
In the radical operation the abdomen and uterus are incised; the child and placenta extracted and the uterus is amputated just above the cervix. This operation is usually performed when labor is well advanced and there is fear of infection.
In the extraperitoneal operation the incision in the abdomen is made low down on one side, the peritoneum is not incised but is peeled back from the bladder and lower part of the uterus. The uterus may thus be opened and the child and placenta extracted, without entering the peritoneal cavity, thereby greatly reducing the risk of infection, and also without necessitating the removal of the uterus as a safeguard against infection. This operation, also, is performed late in labor when infection is feared, but is considered very difficult and therefore is not common.
The nurse’s duties in connection with a Cæsarean section are the same as those in any abdominal operation plus preparations for receiving and reviving the baby.
A Ruptured Uterus is a splitting of the uterine wall at some point, usually in the lower uterine segment, that has become thinned or weakened and unable to stand the strain of further stretching incident to uterine contractions, and is accompanied by an extrusion of all or a part of the uterine contents 308into the abdominal cavity. The rupture of a uterus during labor is a very rare accident, occurring but once in from 500 to 1,000 cases and usually only in prolonged labors, obstructed labors or certain faulty presentations. It is also a very grave accident, since the baby nearly always dies and sometimes the mother as well.
The cause of a ruptured uterus may be found in scar tissue, following a Cæsarean section or an injury; inherent defects in the tissues comprising the uterine wall; contracted pelves; neglected transverse presentations and the accident may occur during a version. It is usually preceded by extreme tenderness in the lower uterine segment, the part that is being abnormally stretched. The common symptoms, after the rupture has occurred, are sudden and acute abdominal pain during a contraction, which the patient describes as being unlike anything she has ever felt and as though “something had given way” inside of her. There is immediate and complete cessation of labor pains because the torn uterus no longer contracts. Sooner or later the patient has symptoms of shock because of the hemorrhage, which is usually internal, though there may be vaginal bleeding as well. Her face becomes pale and drawn and covered with perspiration; her pulse is weak and rapid; she appears exhausted and collapsed and may complain of chilly sensations and air hunger.
Abdominal palpation shows that the lower uterine segment is even more sensitive than formerly and that the presenting part has slipped away from the superior strait while at the side of the fetus the contracted uterus, partly or entirely empty, may be felt as a hard mass. The symptoms of shock may be delayed for some time when they will be accompanied, as a rule, by abdominal distension, due to hemorrhage, and a slight elevation of temperature.
The prevention of this disaster lies in performing version and prompt extraction in transverse presentations, as soon as the cervix is dilated, and in interference if the presenting part does not engage after an hour of strong, second-stage pains.
The treatment of a ruptured uterus is influenced by many factors. Possibly the most frequent course followed is to open 309the abdominal cavity and repair or remove the uterus, after extracting the fetus and placenta, according to existing conditions and the judgment of the operator. Sometimes the fetus is removed through the vagina and the uterus repaired through that channel.
Destructive Operations have as their purpose the crushing or dismembering of the child in utero so that it may pass through the pelvis. In the early days such operations were resorted to fairly often in the presence of conditions that threatened the mother’s life and which apparently could not be met in any other way. They are performed less and less frequently to-day because of the success attending the performance of Cæsarean section, version, pubiotomy and forceps operations. They are never sanctioned by the Catholic Church in cases where the child is alive.
Induced Abortions and Premature Labors. As was explained in the chapter on complications and accidents of pregnancy, it is sometimes deemed advisable, or necessary to terminate pregnancy by artificial means, in the interests of the mother or child or both.
The procedures are termed induced abortion, induced premature labor and accouchement forcé. The effects of these operations, per se, when skillfully performed, for therapeutic purposes, are not usually considered more serious for the mother than a normal delivery, since they can be performed with deliberate care and cleanliness and can be followed by adequate aftercare. When the reverse conditions prevail, as in criminal abortions, the patient’s subsequent suffering or ill health are more likely to be due to the poor obstetrics and unclean work which is characteristic of practitioners who are willing to do illegal operations, than to the termination of pregnancy itself. It is important that the nurse fully appreciate this and be as scrupulously careful in her preparations for, and assistance with these operations as for a major operation or a normal delivery.
Induced abortion applies to the termination of pregnancy before the child is viable, or before the end of the twenty-eighth week, and is performed solely in the interests of the mother, as the fetus is always lost. It is resorted to in those cases where 310the mother is suffering from some condition, which may or may not be inherent to pregnancy, which threatens her life or health but which it is believed may be cured or arrested if uncomplicated by pregnancy. Such conditions may be toxemic vomiting; nephritis, particularly with evidences of increasing renal insufficiency; bleeding, due to an incomplete abortion; a dead fetus; infection following an attempt at criminal abortion. Contracted pelves and pulmonary tuberculosis are sometimes taken as indications for inducing abortions, but with the development and improvement of obstetrical operations, more and more women are able to go nearly, or quite, to term and be delivered of live babies; while increasing medical knowledge concerning the care of patients with tuberculosis, and also with some heart lesions, is applied so successfully during the prenatal period that some pregnancies which formerly would have been terminated, are now allowed to continue, and with happy results.
The methods of induction depend upon the stage to which pregnancy has advanced and also upon the importance of haste. In the very early stages, one method is for the operator to dilate the cervix with a dilator; insert one finger into the cervix and up into the uterus and separate the placenta from its uterine attachment, while making pressure on the uterus from above with the other hand on the abdomen. Another method is to introduce a gauze pack into the cervix, packing it and the vagina firmly and leaving the packing for twenty-four hours. When it is removed the ovum frequently follows. Sometimes the membranes are ruptured, after which the amniotic fluid drains off and the ovum is expelled; or vaginal hysterotomy is sometimes performed when the patient’s condition is such that haste is imperative. The termination of pregnancy before viability is never sanctioned by the Catholic Church, because of the almost certain loss of the child.
Induction of premature labor. This procedure is the termination of pregnancy after the twenty-eighth week, or after the child is viable, and may be performed to save either the mother or the child or both, from conditions which would evidently work destruction if allowed to persist. The indications for inducing labor prematurely may be a seriously overtaxed 311heart or kidneys; pulmonary tuberculosis; preëclamptic toxemia or nephritic toxemia; chorea, neuritis; pyelitis; placenta prævia; a fetus that has been dead for two weeks, with no signs of labor; in some cases of nephritis when the fetus during previous pregnancies has died, and it is believed that the child may be saved by inducing labor before the stage in pregnancy at which the others perished.
Labor is sometimes induced when the mother’s pelvis is normal, but the child has grown as large as is safe in anticipation of a spontaneous labor, and particularly if the expected date of confinement has passed.
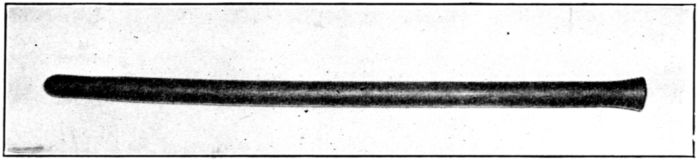
Fig. 111.—Rubber bougie used in inducing labor.
A common method of inducing labor when haste is not important, is to introduce one or more bougies (Fig. 111) through the cervix into the uterine cavity between the membranes and the uterine wall. The presence of the bougies will often stimulate the uterine contractions and bring on labor, with expulsion of the fetus, in from six to twenty-four hours.
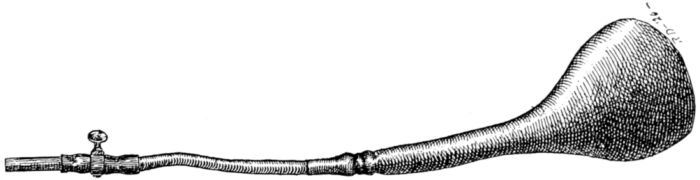
Fig. 112.—Champetier de Ribes’ bag.
More speedy results are obtained by the use of rubber bags, which may be collapsed before introduction and expanded afterward by filling them with sterile salt solution. There is a great variety of bags for this purpose, two of which that are frequently used are the Champetier de Ribes (Fig. 112) and the Voorhees 312bags. (Fig. 113.) They come in graduated sizes, the largest holding about 500 cubic centimetres.

Fig. 113.—Voorhees’ bag, collapsed.

Fig. 114.—Rubber bag rolled and held in forceps for introduction into uterus.
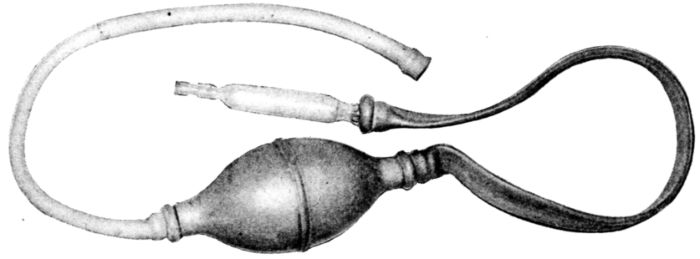
Fig. 115.—Syringe for introducing sterile water into bag after its insertion into the uterus.
The operation is performed with the patient in the dorsal position. The cervix is drawn down into sight, with forceps, and if intact, is slightly dilated. The bag is rolled tightly, held in suitable forceps (Fig. 114), and after being well lubricated is introduced through the slightly dilated cervix into the lower uterine segment, and pumped full of sterile salt solution. The solution is first measured in order to be sure that the bag is filled to its desired capacity, and is then introduced by means 313of a syringe, (Fig. 115), through the rubber tubing which is attached to the lower end of the bag, and which is then closed off by the stop cock, to prevent escape of the fluid. It is very important that the solution be sterile in view of the possibility of any rubber bag rupturing, particularly when pressed upon by the contracting uterus. (See Fig. 47 for position of bag after introduction into uterus.)
The presence of this bag stimulates uterine contractions, the cervix dilates, the bag is expelled and in some instances the child is delivered spontaneously and in others by means of forceps. The effect of this bag in producing labor may be hastened by tying a weight to the end of the tubing and allowing it to hang over the side of the bed. This traction and pressure help to dilate the cervix and seem to increase the irritation of the uterine muscles, thus increasing the force of their contractions.
Accouchement forcé is a speedy, forced delivery requiring the forcible widening of an intact, or partly dilated cervix, manually, or instrumentally. It is sometimes performed when existing conditions require extreme haste, as in certain heart lesions; eclampsia; concealed or accidental hemorrhage or in any condition which suddenly arises to threaten the life of the patient or her expected baby. But as the shock of this operation is great and the condition which threatens the patient can usually be better relieved by means of some one of the operations already described, it is less and less frequently performed.
CHAPTER XIV. THE PUERPERIUM. Physiology. Involution. After-pains. Lochia. Loss of Weight. Menstruation. Lactation. Abdominal Wall. Digestive Tract. Temperature. Pulse. Skin. Urine.
CHAPTER XV. ROUTINE NURSING CARE DURING THE PUERPERIUM. Complications to be Guarded against. General Treatment of the Patient. Nursing Care. Position in Bed. Sitting up. The Daily Bath. Diet. The Bowels. The Bladder. Catheterization. Temperature, Pulse, and Respiration. Care of the Perineum. Care of the Breasts. Lactation. Stripping. Abdominal Binders and Bed Exercises.
CHAPTER XVI. THE NURSING MOTHER. Normal Routine. The Establishment of Breast Feeding. The Mother’s Frame of Mind and State of Nutrition. Method of Nursing. The Nursing Schedule. Personal Hygiene of the Nursing Mother. Diet. Bowels. Rest and Exercise. Recreation. Weaning. Drying up the Breasts.
CHAPTER XVII. NUTRITION OF THE MOTHER AND HER BABY. Importance of Adequate Nutrition in First Weeks of Life. Necessary Elements of an Adequate Dietary. “Vitamines.” Danger of Deficiency Diseases. Danger of Conditions Approaching Recognizable Disease. The Deficiency Diseases. Scurvy. Infantile Scurvy. Corrective Diet. Beriberi. Xerophthalmia. Pellagra. Rickets. Corrective Diet. Application of Principles of Nutrition to the Diet of the Nursing Mother.
CHAPTER XVIII. COMPLICATIONS OF THE PUERPERIUM. Postpartum Hemorrhage. Causes, Treatment and Nursing Care. Puerperal Infection. History of Disease. Prevention. Symptoms, Treatment and Nursing Care. Phlegmasia alba dolens, or “Milk leg.” Puerperal Mania.
The puerperium[8] is ordinarily regarded as comprising the five or six weeks immediately following delivery. During this period the mother’s body undergoes various changes which restore it very nearly to its pre-pregnant state, leaving the patient in a normal, healthy condition. The most important of these changes are involution of the uterus, loss of weight and improvement in tone of the abdominal and perineal muscles. The alterations which produce this restoration are normal physiological processes, but mismanagement or lack of care while they are taking place may result in serious complications; these may be immediate or remote, such as hemorrhage and infection or chronic invalidism.
Recognition of these dangers, and the possibility of preventing them, is responsible for the present custom of obstetricians to watch over their patients during the puerperium. This is in sharp contrast to the old practice of the doctor’s visiting the puerperal woman only when there was a complication so apparent that he was summoned.
The precautions and the care which the doctor takes of his patient after delivery involve intelligent and watchful nursing. In order to give this the nurse must understand something of the normal physiology of the puerperium, just as she did in pregnancy and labor. Otherwise she may not be able to distinguish evidences of normal changes from symptoms of complications.
Involution. Considerable attention is centred in the remarkable atrophic changes that take place in the uterus during the puerperium, for it is upon their being normal that the patient’s recovery and future well-being so largely depend. Immediately 318after delivery the uterus weighs about two pounds; is from seven to eight inches high; about five inches across and four inches thick. The top of the fundus may be felt above the umbilicus, and the inner surface, where the placenta was attached, is raw and bleeding. At the end of six or eight weeks the uterus has descended into the pelvic cavity and resumed approximately its original position and size, and its former weight of two ounces; a new lining has developed from the few glands which have not been cast off in the discharges.
This rapid diminution in the size of the uterus is termed involution and is accomplished by means of a process of self-digestion or autolysis. The protein material in the uterine walls is broken down into simpler components which are absorbed and eventually cast off largely through the urine. This change and absorption of uterine tissues is similar to the resolution that takes place in a consolidated lung in pneumonia.
Since satisfactory involution is necessary to the patient’s future health, its progress should be watched with deep concern and interest, and all possible effort made to promote it; firm consistency of the uterus and a steady descent into the pelvis and normal lochia being the chief evidences of satisfactory involution. There is evidently a close relation between the functions of the breasts and of the uterus during the puerperium, and as a rule involution accordingly progresses more normally in women who nurse their babies than in those who do not.
The so-called “after-pains” are also affected by nursing, being more severe as a rule when the baby is at the breast than at other times. These pains are caused by the alternate contractions and relaxations of the uterine muscles and are more common in multiparæ, than in primiparæ, because the muscles of the former have somewhat less tone than the latter and therefore tend to relax, and then contract, whereas the better muscle tone of the primipara tends to keep the uterus steadily contracted.
These after pains usually subside after the first twenty-four hours, though they may persist for three or four days. They may amount to little more than discomfort, but not infrequently are so severe as to require the administration of sedatives. Persistent after pains may be due to retained clots.
The cervix, vagina and perineum which have become stretched 319and swollen during labor, gradually regain their tone during the puerperium, and the stretched uterine ligaments become shorter as they recover their tone, finally regaining their former state. Until the ligaments and the pelvic floor and abdominal wall are restored to normal tonicity the uterus is not adequately supported and therefore may be easily displaced.
The lochia consists of the uterine and vaginal secretions and the blood and uterine lining which are cast off during the puerperium. During the first three or four days this discharge is bright red, consisting almost entirely of blood, and is termed the lochia rubra. As the color gradually fades and becomes brownish it is called the lochia serosa. After about the tenth day, if involution is normal, the discharge is whitish or yellowish and is designated as the lochia alba. The total amount of the lochial discharge has been variously estimated at from one to three pints, being more profuse in multiparæ than primiparæ, and in women who do not nurse their babies. Under normal conditions the discharge is profuse at first, gradually diminishing until it entirely disappears by the end of the puerperium. There may be small amounts of blood retained during the first day or two and expelled later as clots, without any serious significance, and there may be a pinkish discharge after the patient gets up for the first time, but if the lochia is persistently blood-tinged it may be taken as an indication that the uterus is not involuting as it should.
The normal characteristic odor is flat and stale. A foul odor, no odor at all or a marked decrease in the amount of the discharge is suggestive of infection.
Loss of Weight. One of the striking changes during the puerperium is the loss in weight, due largely to three factors: the elimination of fluids from the edematous tissues; the decrease in the size of the uterus and the escape of vaginal and uterine secretions, termed the lochia. The smaller amount of food taken during the first few days post-partum also may be a factor.
This loss in weight is extremely variable, fat women naturally losing more than thin women and those who nurse their babies losing more than those who do not.
Dr. Edgar estimates that the loss through the lochia amounts 320to something over three pounds, and the loss through fluids from the tissues, from nine to ten pounds. According to Dr. Slemons, the loss in fluids equals about 1/10th of the patient’s weight at the beginning of the puerperium, while all agree that the uterus decreases about two pounds in weight. All told, then, the patient may normally lose from twelve to fifteen pounds during the puerperium. This loss may be somewhat controlled, however, by a suitable diet, and under most conditions the patient should return to not less than her pre-pregnant weight by the end of the sixth or eighth week.
Menstruation. Although in the ideal course of events, the mother does not menstruate while nursing her baby, that is, for eight to ten months, Dr. Slemons estimates that about one-third of all nursing mothers begin to menstruate about two months after delivery, while according to Dr. Edgar one-half of those who do not nurse their babies begin to menstruate in six weeks after delivery.
Menstruation is more likely to return early in primiparæ than in multiparæ. Patients sometimes wonder whether this early discharge is menstrual or lochial, and though they can not tell, a physician can easily decide by examination, and it is important that he be given the opportunity to do so. A nursing mother may menstruate once and then not again for several months or a year; or she may menstruate regularly and nurse her baby satisfactorily at the same time, though menstruation is usually regarded as unfavorable to lactation.
Lactation. During the first two or three days after the baby is born, the breasts secrete a small amount of yellowish fluid called colostrum, which differs from milk chiefly in that it contains less fat and more salts and serum-albumen than milk and in the fact that it coagulates upon boiling. About the third day after delivery, the meagre amount of colostrum is replaced by milk and as it increases rapidly in amount, the breasts usually become tense and swollen at this juncture, and sometimes very painful; but this turgidity usually subsides after a day or two.
The function of the breasts, that of secreting milk, is definitely stimulated by the baby’s suckling and will not continue for more than a few days without this stimulation, a fact to be remembered if it is desirable for any reason to dry up the breasts.
321The ideal condition is for the breasts to secrete a quantity and quality of milk which will adequately nourish the baby for eight or ten months. The reverse of this condition is sometimes found in very young or in elderly women, or in very fat or frail, undernourished women.
Ovulation is usually suspended during lactation, but a mother may become pregnant a few weeks after delivery even while nursing her baby, though the quality of her milk is likely to be unfavorably affected by the pregnancy. But, as has been explained, the return of menstruation does not necessarily exert as unfavorable an influence upon lactation as was formerly believed.
Abdominal Wall. The abdominal wall is usually overstretched during pregnancy, and immediately after labor when the tension is removed, the skin lies in folds and the entire wall is soft and flabby. The normal and desirable course is for the muscles gradually to regain their tone; for the excess of fat to be absorbed and the walls to approach their original state in the course of a few weeks. The striæ usually remain, and the muscles sometimes fail to regain their tone, as for example when pregnancies follow each other in rapid succession or when there has been excessive distension. In such cases there is likely to be the pendulous abdomen so often seen in multiparæ, and a diastasis, or separation of the rectus muscles.
Digestive Tract. During the first day or two after delivery the mother may have very little appetite but she is usually very thirsty. She will almost inevitably be constipated, because of the loss of intra-abdominal pressure; the sluggishness of the intestines acquired during pregnancy; her recumbent position, lack of exercise and the fact that she is taking relatively less food than usual and that her bowels were freely evacuated at the onset of labor.
Temperature. The temperature often rises to about 99° F. immediately after labor but it should drop to normal in a few hours and practically remain so. For various causes, some of which are unexplained, the temperature will not infrequently be slightly above normal at times during the first few days of the puerperium, without the patient’s seeming to suffer any ill effects. But the fairly general agreement among obstetricians 322seems to be that a temperature of 100.4° F. is the upper limit of normality and that infection is to be suspected if it reaches that point and remains there for twenty-four hours.
Pulse. The normal pulse rate is usually slower during the puerperium, being about 60 or 70 beats to the minute, and is referred to as puerperal bradycardia. It is thought that this is due to the absolute rest in bed and the decreased strain upon the heart after the birth of the baby.
Skin. There is usually profuse perspiration during the first few days, while the elimination of fluids is most active, but it gradually subsides and becomes normal by the end of a week. The perspiration sometimes has a strong odor and there is not infrequently an appreciable amount of desquamation.
Urine. Many patients find it difficult, even impossible, to void urine during the first several hours after delivery because of the removal of intra-abdominal pressure; the recumbent position and the swelling and bruised state of the tissues about the urethra. The bladder is likely to be less sensitive than usual and the patient will be able to retain an abnormally large amount of urine for several hours without discomfort, or desire to void.
The output of urine during the first few days is greater than normal, and there is also a considerable increase in the amount of nitrogen excreted, beginning two or three days after delivery. This is evidently derived from the broken down proteins in the uterine wall, and the excess gradually subsides as involution progresses, and disappears by the time the uterus descends into the pelvis.
When one considers the severe ordeal that the young mother has just passed through, her recovery and return to a normal state are surprisingly rapid, when she is given good care.
In general, the nursing care during the puerperium is much the same as that which is given to a surgical patient, with special attention to the breasts and perineum and a sustained effort to prevent complications and restore the mother to a normal state of health in due time.
As the nurse doubtless realizes by this time, the principal complications to guard against during the puerperium are hemorrhage from the still raw area, where the placenta was attached to the inner surface of the uterus; infection of the birth canal; breast abscesses; displacement of the uterus and subinvolution, or failure of the uterus to return to its normal size and condition in the usual length of time.
In addition to guarding against these definite complications, the nurse must help to save her patient from the less tangible, but perhaps equally injurious effects of fatigue of mind and body. As many young mothers are in a more or less unstable, excitable condition after the baby’s birth, the beneficial effect of promoting a tranquil and contented state of mind can scarcely be overestimated.
The doctor may be ever so tactful and cheering and sustaining, but his contacts with the patient are short and infrequent as compared with the nurse’s constant companionship. She can, therefore, by her attitude, manner and conduct practically create or destroy the atmosphere that is necessary to her patient’s welfare.
In order to give the best and most helpful service the nurse must try from the very beginning to understand her patient as an individual and adapt herself to the patient’s temperament. Some women are rested and soothed by being talked with, read to, diverted and amused in one way or another, during most of 324the time, and will grow nervous and depressed if left to their own devices. Others, who have greater resources within themselves are happier and better off when left to themselves a good deal, and given an opportunity to think things over. Some women are much subdued as the consciousness of their motherhood grows upon them, and they feel a kind of awe and wonder about this baby that they begin to realize is their own. It is a big experience, this one of motherhood, full of promise and responsibilities, and the young mother herself very often wants to think it out. She will enjoy talking when she wants to talk, but may be irritated and exhausted by a nurse who tries to entertain her all of the time.
For this reason, the most conscientious and painstaking nurse imaginable may destroy her usefulness, by adopting the wrong attitude toward her patient during this period of enforced intimacy. Some women want, and even need to be indulged and petted; but, on the other hand, a certain type of reserved and dignified woman is affronted by such attention or by the easy air of familiarity that another courts; one patient is exhausted by the unvarying punctuality and precision of a conscientious, but unadaptable nurse, while that very punctuality and precision is satisfying and restful to another.
It is not a simple matter to sound the depths of a patient’s personality, for they are all complex and each one is peculiar to herself. That fact must not be overlooked for each patient is an entirely new and different problem and not like any other that the nurse has had before. But the nurse who is sincere and sympathetic and who earnestly tries to put herself in her patient’s place and see things from her standpoint, will, by virtue of that very attitude, accomplish much toward sensing the patient’s temperament and establishing harmonious relations. Moreover, the patient, herself, will all unconsciously make something of an adjustment to the nurse when she feels the nurse’s sincerity and her eagerness to be of service.
One factor in shaping the young mother’s state of mind, which the nurse must take into account is that the entire scheme and purpose of her patient’s life have been changed. She has been plunged very suddenly into a wholly new condition and 325her reaction to this change will depend upon her temperament, disposition and habits of adjustment.
She has spent nine months looking forward to an event that has been consummated; she has spent nine months in a state of more or less apprehension and suspense that have been abruptly ended, and we know that it is quite natural for any one to experience a letting down, or something akin to collapse, when long-continued uncertainty is ended, even though it ends happily.
And as recovery progresses the patient becomes aware, perhaps only vaguely, of another change which is not always a welcome one. For nine months she has been the centre of interest in her immediate circle; she has been the object of unremitting concern and solicitude, and much as she and her family may have tried to keep her life normal, she and her needs have constantly been given the first consideration. The very mystery of the child developing within her has created an attitude of respect, almost of reverence, which was never her portion before. In every way she has been shielded, protected and cared for, and all eyes, including her own, have steadily looked forward to the event for which this care has been preparing her—her ordeal of childbirth and the coming of her baby.
And now her ordeal is over. Her baby is here. Every one may be said to be breathing easily at last and they are no longer apprehensive and absorbingly interested in her. As a result the young mother will soon become simply one of the family and the community, and will cease to be the centre of reverential interest and solicitude.
It is scarcely human to welcome such a change in one’s state, and though in all probability very few mothers are conscious of resenting it, very many actually do. And for this reason very many unwittingly cling to a rôle of semi-invalidism. It is entirely unconscious on their part and it is also very human and natural.
To aid in the process of bracing up such a young woman to resume her former life and to meet the demands which it imposes; or to protect another patient of the eager, buoyant type from exposing herself too early to the onslaughts made by 326everyday life, is far from being a simple task, and to meet it no one rule can be laid down. There are all of the variations and degrees between the timid or self-indulgent woman, who must be encouraged and spurred on, and the too active, ambitious patient, who must be steadied and held back for a time.
But here, again, this is simply a part of the nurse’s duty; one aspect which makes nursing the gratifying service that it is.
Fortunately the majority of young mothers are happy and normal in their outlook and may be kept so by the exercise of an average amount of tact and amiability on the part of the nurse. The actual physical care of the patient during the puerperium is a fairly simple matter for the well trained nurse. She will find, however, that in hospitals, private practice and public-health work alike there will be wide differences in the treatment given by different doctors, during this period, just as there were during pregnancy and labor, and she will have to carry out the prescribed directions enthusiastically and loyally no matter how they vary from those of the doctors who helped in her training.
The details of the care will be indicated by the individual doctor, but the general, underlying principles—cleanliness, watchfulness, adaptability and sympathetic understanding will apply to the nursing of all patients. The most notable differences of opinion relate to the care of the breasts, the perineum and the use of abdominal binders, the accepted routine for the general nursing of average, normal cases being fairly uniform the country over.
As has been stated, the general nursing care of the puerperal patient is much the same as that given to any surgical patient, with such adaptations as are indicated by the condition and needs of the young mother.
Position in Bed. The question of the patient’s position in bed is probably the first one that presents itself to the nurse after that first hour when the patient must be kept flat on her back and the fundus closely watched. She should continue to lie quietly on her back for a few hours, with only a small pillow 327under her head, as moving about may cause hemorrhage. Some doctors permit the patient to turn from side to side at will after a few hours of quiet, while others do not allow this for two or three days particularly if the patient has perineal stitches, unless her knees are tightly bound together. Their reason for this precaution is fear that the stitches may be torn out if the thighs are separated and also that air may gain access to the uterine vessels, through the relaxed and gaping birth canal, and produce air embolism. It is a routine in some hospitals to keep the head of the patient’s bed elevated during the first week, to promote drainage, but as a rule it is in the usual position.
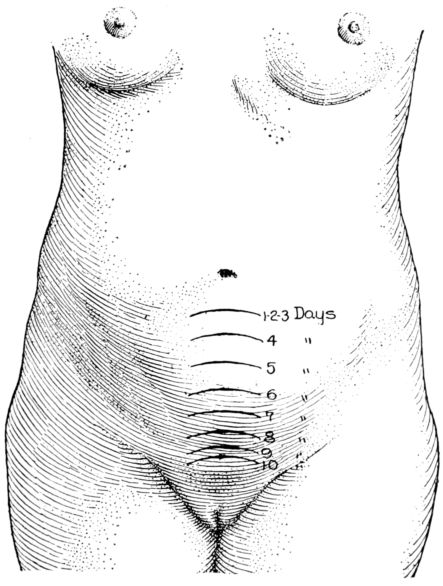
Fig. 116.—Height of fundus on each of the first ten days after delivery.
Quite commonly the patient is encouraged to lie first on one side and then on the other, after she begins to move about in bed unassisted, and then face downward at intervals, in order to change the position of the uterus and thus tend to prevent backward displacement.
328In many hospitals, it is part of the daily routine to measure and record the height of the fundus (Fig. 116) above the symphysis, in addition to noting the character, amount and odor of the lochia, in order to judge if involution is progressing normally. A uterus that does not remain firm and does not steadily shrink in size and descend into the pelvis is not involuting properly, and the usual remedy is more rest and a longer stay in bed, with an icecap over the fundus.
Sitting Up. Except when there are perineal stitches or the temperature has been elevated at some time following delivery, the patient is ordinarily allowed to sit up in bed about the sixth or eighth day. If the lochia is normal, the uterus firm and in the proper position in the abdomen and her general condition satisfactory, she is allowed to sit up in a chair for a little while about the ninth or tenth day. Some patients are able to sit up for an hour the first time without being tired, but it is often better for them to sit up for a few moments morning and afternoon on the first day, than for a longer time at one stretch. The patient is usually allowed to sit up an hour longer on each successive day and to walk a few steps on the third or fourth day after getting up.
A patient with stitches does not usually sit up in bed until the ninth or tenth day, when the stitches are removed, sitting up in a chair for an hour, two or three days later. If she has had fever, the time at which she may sit up will of necessity depend upon her condition.
The return to normal life must be very gradual and this also must be regulated by the patient’s general condition and her recuperative powers. A pinkish or red discharge or backache should be taken as warnings against standing or walking or working. The possible consequences of ignoring these warnings and being up and about too soon, may be displacement, even prolapse of the uterus; hemorrhage, from dislodgment of clots in the uterine vessels; metritis or endometritis.
It is not a good plan, as a rule, for the patient to go up and down stairs until the baby is about four weeks old, nor wholly to resume her normal activities within six or eight weeks after delivery.
329In addition to this sustained, general care, it is a customary preventive measure for the doctor to make a thorough pelvic examination from four to six weeks after delivery. A slight abnormality, if detected at this time may usually be corrected with little difficulty, but if allowed to persist may result in chronic invalidism or necessitate an operation. If the uterus is not properly involuted, for example, or the perineum is found to be flabby, more rest in bed is indicated; while a uterine displacement, which seems to be present in about a third of all cases, usually may be corrected by the adjustment of a pessary.
The time of sitting up, of getting up and of walking about varies so with the individual, therefore, that it is not possible to describe a definite routine, for some patients recover slowly and would be injured by getting up and about at a period which would be entirely safe and normal for the majority. It must be determined in each case by the condition of the uterus, the appearance and amount of the lochia and the patient’s general condition.
Quite evidently, then, much ill health and many gynecological operations may be prevented by caution, prudence and good care during the first few days and weeks after the baby’s birth, while the patient returns to a normal mode of living.
The Daily Bath. During the first week or two the patient’s skin must aid in excreting fluids from the edematous tissues throughout the body and broken down products from the involuting uterus. Therefore she should have a bath of warm water and soap every day, to remove material already on the surface and stimulate the skin to further activity, and an alcohol rub at night, if possible. It is important for the nurse to remember, while bathing her patient, that she is perspiring freely and therefore may be easily chilled if not well protected.
It is often a good plan to have the patient, without stitches, begin to bathe herself in bed, after the third or fourth day, for the sake of the exercise, and also the encouragement that it offers. When all is going well, tub-bathing is usually resumed by the third or fourth week.
Diet. Opinions as to diet vary slightly with different doctors and in different hospitals, but in general, a patient in good 330condition is given liquid food during the first twelve to twenty-four hours after delivery; then a soft diet for a day or two, a nourishing, light diet being resumed by the third or fourth day, or after the bowels have moved freely.
The patient will usually have little appetite, at first, and will have to be tempted by small amounts of invitingly served food. The factors which the nurse must bear in mind when arranging the patient’s dietary are the general nutrition of the mother; the desirability of minimizing her loss of weight during the puerperium; increasing her strength and, particularly, of promoting the function of her breasts, in order to produce milk of a quality and quantity adequate to nourish the baby.
The best producer of such milk is a diet consisting largely of milk, eggs, leafy vegetables and fresh fruits, taken with an appetite that is made keen by constant fresh air. The nurse will do well to convince her patient of this, in addition to bearing it in mind herself, and to place little reliance on so-called milk producing foods.
The young mother’s dietary may well be made up from the groups of foods that are suitable for the expectant mother. (See Chapter VI). At this time, as during pregnancy, she must avoid all food which may produce any form of indigestion, but for the baby’s sake, now, as well as her own. While it is not generally believed, to-day, that there are many, if any articles of diet which in themselves affect the mother’s milk unfavorably, it is generally conceded that a derangement of her digestion may, and usually does, have a deleterious effect upon her milk, and therefore upon the baby.
The old, and widespread, belief that certain substances from such highly flavored vegetables as onions, cabbage, turnips and garlic are excreted through the milk, to the baby’s detriment, is not given general credence to-day. On the other hand, it is known, however, that certain protective substances in certain foods are excreted through the milk, to the baby’s distinct advantage, and it is therefore, important that the mother’s diet should regularly contain those articles of food which contain them. These foods are milk; egg yolk; glandular organs, such as sweet-breads, kidneys and liver; the green salads, such as 331lettuce, romaine, endive and cress and the citrus fruits, or oranges, grapefruit and lemons.
These are called “protective foods” because they protect the body against the so-called deficiency diseases known as scurvy, beri-beri, xerophthalmia, which with rickets and pellagra are discussed in the chapter on Nutrition. It is possible for a baby who nurses at the breast of a woman whose diet is poor in protective foods, to be so insufficiently nourished, in some particular, as to be on the border line of one of these diseases, or even to develop the disease itself. This is one reason for the statement that the nursing mother must “eat for two.”
Certain drugs are excreted through the milk and may affect the baby in the same way as though they were administered directly, for example: salicylic acid, potassium iodid, lead, mercury, iron, arsenic, atropine, chloral, alcohol and opium.[9]
In addition to her food the nursing mother should have an abundance of water to drink, and to facilitate this it is a good plan to keep a pitcher or thermos bottle of water on the bedside table, and replenish it regularly, every four hours.
In general, the young mother should have light, nourishing, easily digestible food, with little, if any meat; an abundance of cereals, creamed dishes, creamed soups, eggs, salads and the fresh fruits and vegetables which ordinarily agree with her; at least a quart of milk, daily, in addition to that which is used in preparing her meals, and an abundance of water to drink.
The Bowels. The puerperal patient is almost always constipated, and needs assistance in regaining regularity in the movements of her bowels.
The routine use of cathartics and enemata varies, but it is very common to give an enema on the second morning after delivery or castor oil or Rochelle salts, followed by an enema if necessary. After this, a mild cathartic or a low enema is given often enough to produce a daily movement when this is not accomplished by means of the diet.
Some doctors, however, prefer that the bowels shall not move for four or five days after delivery, believing that this delay reduces 332the danger of infection from the intestinal contents, which are swarming with organisms, particularly the colon bacillus.
In cases of third degree tears, catharsis is practically always delayed for four to six days in order that the torn edges of the rectal sphincter may become well united before being strained by a bowel movement. In these cases an enema of six or eight ounces of warm olive oil is often given and the patient encouraged to retain it over night, in order to soften the contents of the rectum and lessen the strain and irritation of evacuation.
The Bladder. The question of helping the patient to void after delivery is one of extreme importance, because she will almost certainly have difficulty in emptying her bladder, and yet catheterization is not to be resorted to unless absolutely necessary. As a rule the patient should be encouraged to try to void from four to eight hours after delivery. If she is unable to do so at first there are several aids which the nurse should employ before admitting the patient’s inability to empty her bladder. Inducing her to drink copious amounts of hot fluids is the first step. Very often she will then void if placed upon a bedpan containing water hot enough to give off steam, and more warm, sterile water is poured directly upon the urethral outlet; or hot and cold sterile water may be dashed, alternately, upon the meatus.
The sound of running water is often helpful as well as the application of hot stupes over the supra-pubic region. When everything else fails, success frequently follows the application of a partly filled hot-water bottle over the bladder, held in place by a tight binder, particularly if the patient rests upon a pan of steaming water at the same time.
The danger of infecting the bladder, by carrying lochia into it upon the catheter, is so great that some doctors choose what they regard as the lesser of two evils, and allow the patient to be assisted to the sitting position, if she has not a serious tear. Not infrequently the patient’s inability to void is due to the fact that she is unaccustomed to using a bedpan, and would have difficulty in using one under any conditions, but is able to void while sitting up. As the danger of infection is greater two or three days after delivery than at first, because of the beginning 333decomposition of the lochia, it is very evidently important to help the patient to establish the habit of voiding from the beginning, for if she is catheterized once there is great likelihood that she will need to have it continued for some days.
If the first attempts are unsuccessful, therefore, but the patient thinks that she may be able to void later, if the efforts are repeated, catheterization is sometimes delayed for as long as sixteen to eighteen hours after delivery in the hope that it may be avoided altogether.
When the most persistent and painstaking efforts fail, and catheterization is necessary, the nurse must remember the extreme gravity of her responsibility and preserve asepsis throughout the procedure. Although there is extreme danger of infection, it can be prevented as a rule, and its occurrence is therefore regarded as almost inexcusable.
In preparing for catheterization, the nurse should drape the patient as for a vaginal examination, making sure that she is warmly covered, and place her on a sterile douche- or bedpan. If it is done at night she should place the light in a position at once safe and advantageous. She should have at hand on a tray: sterile forceps; cotton pledgets; two glass catheters (in case one should be broken or become contaminated); a disinfecting solution such as bichlorid, 1–4,000 or lysol 1 per cent.; a sterile receptacle in which to receive the urine; sterile towels and a dressing basin or paper bag for the used pledgets.
The preparation of the nurse’s hands, at this point, varies in different hospitals, but always the greatest care is taken to bring nothing unsterile in contact with the vulva and meatus.
According to one method, the nurse scrubs her hands for three minutes and prepares the patient as for a vaginal examination, removes the douche pan and places a sterile towel over the vulva. She then scrubs and soaks her hands as described in Chapter XII, puts on sterile gloves, places a sterile towel over the patient’s abdomen and slips one under her hips. She should then separate the labia with the gloved fingers of the left hand, drawing the fingers upward a little to make the meatus more prominent. The inner surface of the labia is then bathed with pledgets soaked with the disinfecting solution, with downward 334strokes, each pledget being used but once. Five or six pledgets should be used, one after the other, to sponge the meatus, each pledget being placed squarely against the orifice, without touching the adjacent tissues, and given a slight, downward twisting motion and discarded. The bowl may then be placed in position to receive the urine, and the catheter picked up with the fingers, by its open end. The rounded end must be carefully inspected to insure against using one that is cracked or broken, after which it is slowly and gently introduced into the urethra for two or three inches. If the urine does not flow freely the catheter may be slightly withdrawn and light pressure made upon the bladder.
Before removing the catheter the nurse must locate the fundus and assure herself that it is in a proper position. If it is pushed up or to one side she will know that the bladder is still distended, and that more urine must be withdrawn. After the bladder has been emptied the nurse should place one finger over the open end of the catheter and remove it slowly.
Another method of catheterization differs from the one just described, in the preparation of the nurse’s hands. In this instance she simply washes her hands well with soap and hot water and wears neither gloves nor finger cots.
She bathes the vulva with pledgets and an antiseptic solution, using forceps, and then separates the labia with two dry pledgets, one each under forefinger and thumb of the left hand, and proceeds as above. It will be observed that the nurse avoids touching the inner surface of the labia or the meatus with anything but sterile pledgets and the sterile catheter. The advantage of this procedure is that it is accomplished quickly and with the minimum of disturbance to the patient.
A distended bladder may so easily occur unless the patient is carefully observed during the puerperium that the nurse should charge herself to watch for this complication. She should give the patient a bedpan every four hours, note the contour of the abdomen and measure the urine during the first week, remembering that the patient should void considerably more than the average amount, both because of the amount of milk and water that she is taking, and the fluid which she is eliminating from her tissues. The importance of measuring the urine lies 335in the fact that though the patient may void fairly regularly she may not empty her bladder, and thus enough urine may accumulate to distend it.
The temperature, pulse and respirations are usually taken and recorded every four hours for the first five or six days and then two or three times daily, if normal. If the temperature is above normal at any time, the nurse should take it every two hours until it becomes normal and notify the doctor immediately if it goes as high as 100.4° F., or if the pulse reaches 100.
Care of the Perineum. The best way of caring for the perineum, during the first week or ten days after delivery, is a moot question, and the nurse may find herself sorely perplexed by the widely divergent instructions of different doctors who have excellent results, unless she goes back of the details themselves and recognizes their purpose. She will then see that there is entire agreement about the importance of protecting the patient against infection, at this time, when infection may so easily occur. And so far as the nurse is concerned, this means cleanliness as to methods and appliances, when making perineal dressings, and extreme precaution against conveying infection to her patient. The minimum requisites for this are that the bedpan shall be sterilized, by steam or boiling, at least once a day, and well scrubbed and scalded after each time that it is used, and that the nurse shall at least scrub her hands with soap and hot water before making each perineal dressing, and apply only sterile pads.
After the perineum is bathed, immediately following delivery, the usual practice is to apply a sterile pad, after which a fresh one is applied as often as necessary at first, every four hours during the first week and subsequently every eight hours. When the dressing is changed, and after each voiding and defecation, the perineum is bathed with sterile pledgets and some such antiseptic solution as bichlorid 1–2,000 or lysol ½ per cent. or 1 per cent. (Figs. 117 and 118.) The soiled pad must always be removed from above downward and the bathing also directed toward the rectum, each pledget being used for one stroke only. The rectum is bathed last, a fresh sterile pad applied and the patient’s hips and back thoroughly dried.
336The nurse may be required to scrub and soak her hands, wear sterile gloves and hold the pledgets in forceps when bathing the perineum, the object of such precautions being, quite clearly, to avoid infecting the patient from without, for the inner surface of the uterus is still regarded as an open wound.
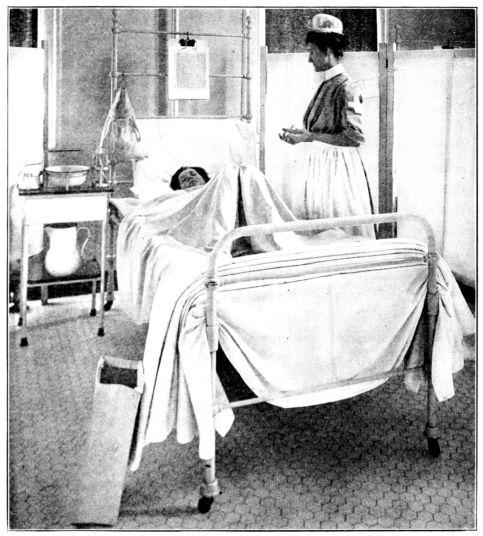
Fig. 117.—Preparation and draping of patient for post-partum dressing. Note rack of equipment on table; bag of dry, sterile pledgets at head of bed; paper bag on floor for used pledgets. The nurse has scrubbed her hands. (From photograph taken at The Manhattan Maternity Hospital.)
Some obstetricians believe that the perineal pad is a menace, since it slips and moves about, and thus may transfer infective material from the anus to the vagina. Accordingly, they forbid 337the use of all perineal dressings and instead have large, sterile, absorbent pads slipped under the patient’s hips to receive the lochia, the pads being changed as often as necessary. This is the practice at the Brooklyn Hospital, for example, where the nurse bathes the vulva with lysol 1 per cent., placing the patient on a sterile bedpan, using sterile forceps and cotton swabs and wearing sterile gloves while making the dressing.
Another method is to place the patient on a sterile bedpan, remove the pad and with gloved hands pour from a sterile pitcher a warm antiseptic solution over the groin and outside of the vulva; then to separate the labia and pour the solution between them, in some instances pressing a dry, sterile pledgets to the vaginal orifice during the irrigation.
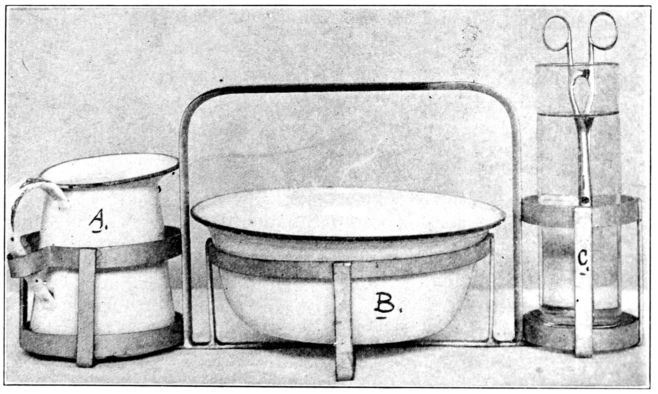
Fig. 118.—Equipment, in rack, used at The Manhattan Maternity Hospital in bathing perineum. A, pitcher of lysol, 1%. B, basin of pledgets in lysol. C, sponge-sticks in alcohol.
When the urine is being measured, as it frequently is during the first week, the solution which is used for irrigating the vulva should be measured beforehand and the contents of the bedpan measured after the dressing, in order that the amount of urine passed, if any, may be ascertained.
Another method of bathing the perineum, that employed at Johns Hopkins Hospital, is simply to bathe the perineum with 338soap and warm water, without separating the labia, using a clean wash cloth and afterwards applying a sterile pad, the pads being changed every four hours, or oftener if necessary. The theory upon which this procedure is based is that the steady outward flow of the lochia constantly carries material, infective and otherwise, away from the generative tract, and that if nothing is introduced between the labia or into the vagina the patient will not be infected.
In caring for the perineum, the nurse must remember also the real danger of the patient infecting herself with her own fingers and should caution her against taking this risk. The patient should be told that if she feels uncomfortable, or thinks she is bleeding, she must lie quietly and summon a nurse, but on no account to try to find out for herself what is wrong. There is little doubt that cases of severe infection have been caused by the introduction of organisms into the vagina by means of the patient’s own fingers, after the most scrupulous precautions had been taken by doctors and nurses to avoid that very disaster.
In most instances the care of the perineum is the same whether or not there are stitches, and in any case the method employed will be specified by the doctor. The nurse’s responsibility is to appreciate the object of the care, whatever form it may take, and bring intelligence to bear in giving it.
When there are perineal stitches, it is a wise and harmless precaution to fasten a towel or bandage about the patient’s knees for a few days, to prevent her pulling apart the uniting edges of the tear as she moves about in bed.
Douches. In connection with perineal dressings, it may be well to caution the nurse against giving douches without explicit orders. Douches are seldom given early in the puerperium, for fear of carrying infective material up into the uterus, except occasionally in cases of hemorrhage, in which case they are given by the doctor.
Sometimes, however, a low vaginal douche is given daily for some time after the patient gets up, with the idea of increasing her comfort and promoting involution. About two quarts of some weak antiseptic solution at 110° F. is given with the nozzle introduced just within the vaginal outlet, and the container of 339the solution placed only slightly above the level of the patient’s hips, in order that the stream may be very gentle.
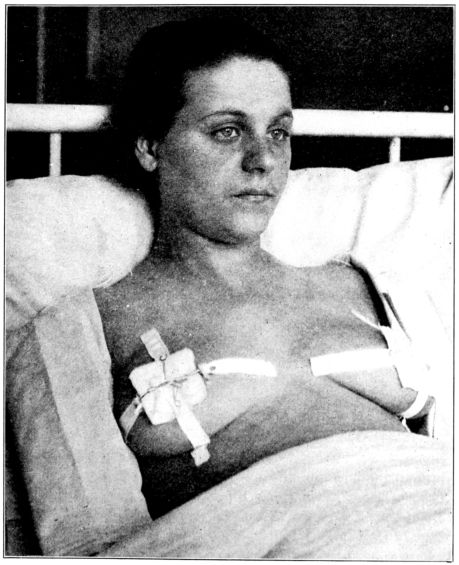
Fig. 119.—Sterile gauze held in place over nipples by means of adhesive strips and tapes. (From photograph taken at Bellevue Hospital.)
The Care of the Breasts. There is a wide difference of opinion about the proper care of the breasts, also, but here again, although the details vary, the ultimate objects of the care are always the same, namely: to facilitate the baby’s nursing, promote the mother’s comfort and prevent breast abscesses. These 340ends are usually accomplished by keeping the nipples clean and intact and by giving support and rest to heavy, painful breasts.
The patient who has cared for her nipples during the latter part of pregnancy will usually have little or no trouble with them during the period of lactation, if the care is continued. But this attention is imperative.
It is very generally customary to have the nipples bathed before and after each nursing with a saturated solution of boracic acid, in either water or alcohol, using sterile pledgets and forceps, and to keep them clean between nursings by applying sterile gauze. This gauze may be held in place by means of a breast binder or by tapes tied through the ends of narrow strips of adhesive plaster, four being applied to each breast. (Fig. 119.) Strips of adhesive plaster about five inches long are folded over at one end, two adhesive surfaces being in contact for about an inch. Through a hole in the folded end a narrow tape or bobbin is tied and the strips applied to the breast, beginning at the margin of the areola and extending outward. The free ends of the tapes are tied over squares of sterile gauze, between nursings, and untied to expose the nipple at nursing time.
Lead shields are sometimes used to protect the healthy nipple and not infrequently are applied to cracked nipples, being held in place by means of a breast binder. The secretion of milk which escapes into the shield is acted upon by the metal and the result is a lead wash which continuously bathes the nipple. The shields should be scrubbed with sapolio and boiled once daily.
Another method, and one widely employed, is to anoint the nipple after nursing with sterile albolene or a paste of sterile bismuth and castor oil, and apply squares of sterile paraffin paper. These bits of paper are pressed into place and held for a moment by the nurse’s hand, the warmth of which softens and moulds them to the breast after which they remain in place. In some instances the bismuth and castor oil paste is wiped off, with a sterile pledget, before nursing and in others it is not.
In some hospitals, neither gauze nor paper is used, the nipples being protected by putting sterile night-gowns on the patients.
The purpose of all of these methods is to keep the nipples 341clean, and here again the patient must be cautioned against infecting herself. No amount of care on the nurse’s part will protect the patient if she touches her nipples with her fingers.
The nurse will appreciate the reason for all of this painstaking care if she calls to mind the fact that the breast tissues are highly vascular and excessively active at this time and therefore very susceptible to infection, and also that the baby’s suckling is often very vigorous and accompanied by a good deal of chewing and gnawing of the nipples. Unless the nipples have been toughened, and sometimes even when they have, the skin becomes abraded or cracked as a result of the baby’s suckling, thus creating a portal of entry for infecting organisms, in addition to the milk ducts which lead back into the breast tissues. Unless the nipples are kept clean, constantly, they may become infected by organisms from the baby’s mouth or on the patient’s hands, bedding or gown with a breast abscess as a result. The important thing, then, is to keep the nipples clean and not allow anything unsterile, excepting the baby’s mouth, to come in contact with them at any time.
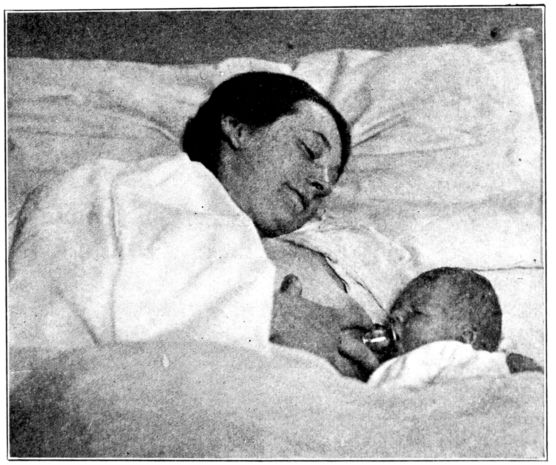
Fig. 120.—Protecting cracked nipples by having the baby nurse through a shield. (From photograph taken at Johns Hopkins Hospital.)
It is sometimes the practice to swab the baby’s mouth with 342boric soaked cotton or gauze before each nursing, but many doctors hold that this is injurious to the delicate mucous lining of the baby’s mouth. The opinions for and against this routine seem to be about equally prevalent.

Fig. 121.—Nipple shield used in Fig. 120.
If the nipples become painful or cracked, one can easily understand that continued suckling would only aggravate the condition and increase the danger of infection. But the baby must nurse, if possible, and so in the majority of cases a nipple shield is used (Figs. 120–121) as a protection, and after nursing the fissures or abraded areas are painted with bismuth and castor oil paste; compound tincture of benzoin; balsam of Peru; argyrol, silver nitrate or sometimes only alcohol. The application is made with sterile swabs prepared by twisting a wisp of cotton about the end of a toothpick. If the crack or abrasion is extensive enough to cause bleeding, even nursing through a shield is sometimes, but not necessarily discontinued, while the other treatment is the same as for a nipple that does not bleed.
Sound, uninjured nipples, then, are to be kept clean and protected from infection and those which are abraded or cracked are to be kept clean and also protected against further injury.
Lactation. About the third or fourth day after delivery, when milk replaces colostrum, the breasts become swollen, engorged and often very painful, and not infrequently, a hard, sensitive lump or “cake” may be felt. The growing tendency, now, is merely to support these heavy breasts by means of a binder which has straps passing over the shoulders, in order to hold them up without making pressure (Fig. 122) and to apply ice caps or hot compresses to the painful areas. It used to be customary to massage and pump caked breasts, to apply pressure and various kinds of lotions or ointments. Though one, or all of these measures are still employed, in some cases, the general practice is to avoid manipulating the breasts but to empty them regularly by the baby’s nursing; support them and allow Nature to make an adjustment between the amount secreted and the amount withdrawn.
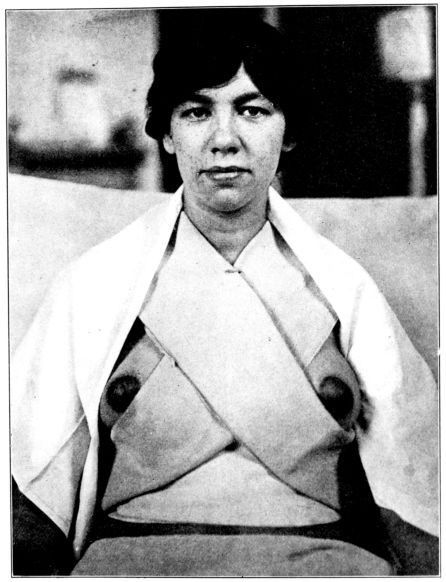
Fig. 122.—A simple method of supporting heavy breasts by means of three folded towels; one fastened about the waist, one over each shoulder, crossing front and back.
Free purging is sometimes employed and the amount of fluids reduced until the engorgement and discomfort subside. This happy issue is practically always reached if the baby nurses regularly and satisfactorily, as there is a spontaneous adjustment between the amount secreted by the mother and that withdrawn 344by the baby. But as abscesses may follow in the wake of caked breasts, particularly if the nipples are sore, it is of great importance that the nurse watch closely for the first evidence of painful lumps. The prompt application of a supporting bandage and ice bags (Fig. 123) or hot compresses will, in the majority of cases, give speedy and complete relief. So widely is this believed that many doctors regard the care of the breasts, including the prevention of breast abscesses, as a nursing question, entirely, and conversely are likely to regard the occurrence of a breast abscess as an evidence of careless nursing.

Fig. 123.—Ice caps held in place on painful breasts by straight binder with darts pinned in under breasts and supported by shoulder straps of muslin bandage.
Certain it is that breast abscesses are almost never seen where 345the nurses have this sense of responsibility, and habitually watch the breasts closely and promptly use support and either heat or cold when the breasts become heavy and sensitive.
There are innumerable bandages and methods for supporting heavy breasts, any one of which is efficacious so long as it meets the two chief requirements: to lift the breasts, suspending their weight from the shoulders, and, while fitting snugly below to avoid making pressure at any point, particularly over the nipples. One of the most satisfactory and widely used supports is the Y-bandage, (Figs. 124, 125, 126), another, the Indian binder (Fig. 127.)
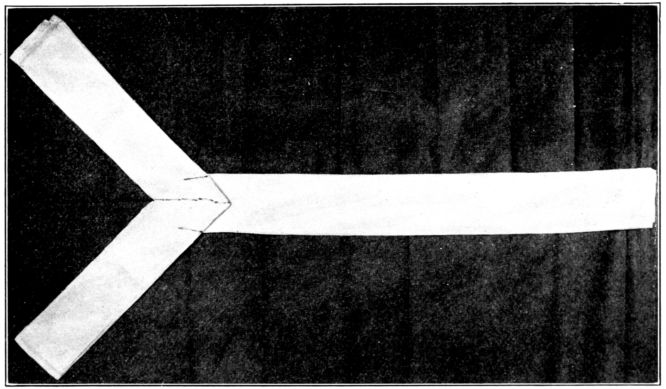
Fig. 124.—Modified Richardson “Y” binder made of two strips of soft muslin, full width of material and 44 inches long, folded into strips of same width as distance from margin of patient’s breast to outer part of areola. One strip is folded in the middle at right angles and pinned to one end of the other strip as indicated. (Figs. 124, 125, 126, with captions, are from The Maternity Hospital, Cleveland, by courtesy of Miss Calvin MacDonald.)
The nurse must on no account massage or pump engorged breasts on her own responsibility, for there is a good deal of evidence to show that any such manipulation tends to increase the amount of the secretion and this in turn increases the engorgement and pain. It is possible, too, that massage may bruise the breasts and thus make them more susceptible to infection.
Mastitis. When infection occurs, the swollen, painful 346breasts may grow hot and red, the patient may complain of chilliness and have a slight fever, with or without there being an abscess. Even then the general treatment is most frequently found to consist of support; ice or heat; catharsis and restricted fluids, though in some cases the breasts are pumped and nursing is discontinued.
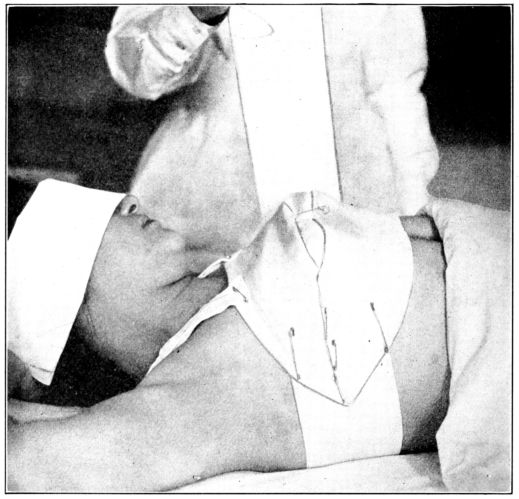
Fig. 125.—Bandage in Fig. 124 applied. The long arm of binder is placed under patient’s shoulders, one end of the Y being brought around the top of the breasts and the other around the lower part, toward the nurse, crossed at right angles under the arm and pinned to long arm of bandage as indicated in Fig. 126. The nipples are covered with sterile gauze and the upper and lower parts of the Y fastened with a safety pin between the breasts. The remaining length of the long arm is brought across the breasts and fastened with a safety-pin to the opposite side. When the baby nurses this pin is removed as well as the one between the breasts. The entire binder should be snug and held in place by means of shoulder straps, pinned front and back.
When the inflammation so far progresses as to require that 347the breast be opened and drained, the subsequent nursing care will be outlined by the doctor to meet the needs of each case. It is a painful operation and often a serious one, for the destruction of breast tissue may be extensive enough to render the breasts valueless as milk-producing organs. The healing is slow and altogether the occurrence is a most lamentable one.
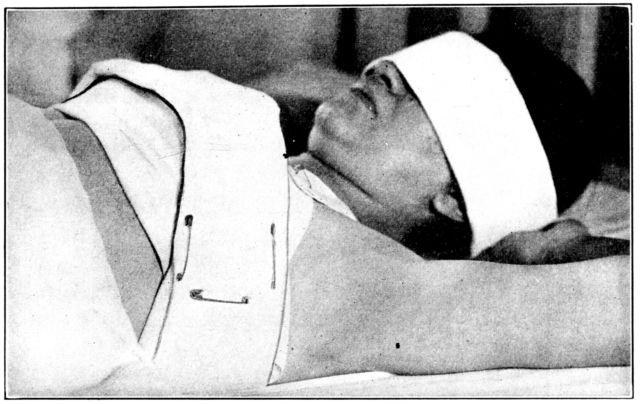
Fig. 126.—Y bandage in Fig. 125 seen from the opposite side.
The nurse’s part in preventing this complication is cleanliness and gentleness in her attentions; unremitting watchfulness; immediate application of a suspensory bandage and either heat or cold, upon the first sign of engorgement and prompt reporting to the doctor.
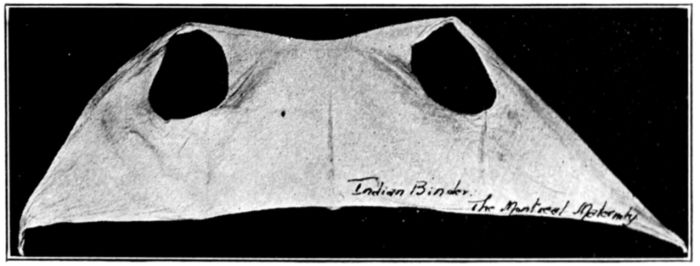
Fig. 127.—Indian Binder used at The Montreal Maternity Hospital for supporting heavy breasts. The tapering ends tie in a knot in front.
If the patient’s nipples have not been toughened during pregnancy 348or if flat or retracted nipples have not been satisfactorily brought out, it may be necessary for the nurse to employ the treatment to these ends which were described in the chapter on pre-natal care. In the meantime the baby may have to nurse through a shield until the nipple is brought out prominently enough for him to grasp it well.
Stripping. Sometimes in cases of depressed nipples, which the baby cannot grasp, or when the baby is too feeble, to nurse at the breast, milk is withdrawn from the breast by means of so-called “stripping.” The nurse should scrub her hands thoroughly with hot water and soap and dry them on a sterile towel before beginning. The breast is grasped by placing the thumb and forefinger of the right hand on the areola on opposite sides of the nipple but well below it. The nipple is then raised from the breast by a quick, lifting and rolling motion of the thumb and finger, accompanied by slight pressure. A sterile medicine glass should be held in position to receive the milk which spurts from the nipple, but the glass should not touch the breast. (Fig. 128.)
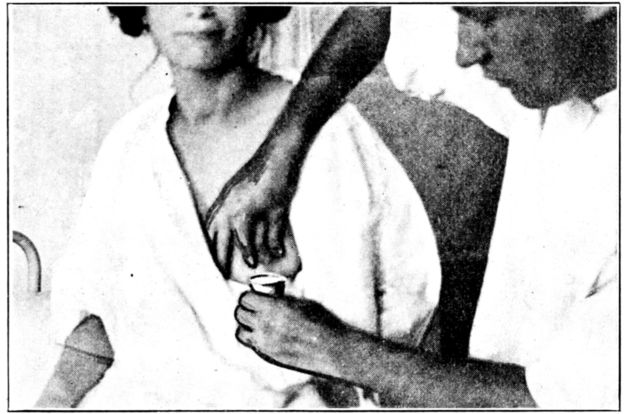
Fig. 128.—Position of thumb and finger below nipple on areola, in stripping breasts. (From photograph taken at The Long Island College Hospital.)
There is a knack about stripping and it requires practice, but those doctors who advocate it feel that it empties the breast, when this is necessary, with less disturbance than that caused by pumping, and as the milk is projected directly from the nipple 349into the sterile glass, without any of it running over the nipple or breast as may happen in pumping, it has the additional advantage of always being sterile.
Extreme gentleness must be used; the openings of the milk ducts must not be touched by the fingers, and the thumb and finger must not press deeply enough to reach the glandular tissue itself. If done properly stripping neither stimulates nor bruises the breast tissue nor does it cause the patient even temporary discomfort.
Abdominal Binders and Bed Exercises. There is considerable difference of opinion about the advantage of using abdominal binders upon the puerperal patient while she is in bed, and the nurse will accordingly care for the patients of some doctors who use them and for those of others who do not.
The application of a moderately snug binder for the first day or two is a fairly common practice, for multiparæ, particularly, are often made very uncomfortable by the sudden release of tension on their flabby abdominal walls; a discomfort which a binder will relieve. And during the first few days after the patient gets up and walks about, she is sometimes given great comfort by a binder that is put on as she lies on her back, and is adjusted snugly about her hips and the lower part of her abdomen.
But the continued use of a binder after the first day or two, while the patient is still in bed, is not as general as it formerly was. Many women ask for binders in the belief that they help to “get the figure back” to its original outline, and some doctors feel that the use of the binder is helpful in restoring the tone to the abdominal muscles, which amounts to about the same thing. Both the straight swathe and the Scultetus binder are used for this purpose and they are put on in the usual manner; snugly and with even pressure, but not tight enough to bind.
Those doctors who disapprove of the binder believe that it interferes with involution and, by making pressure, tends to push the uterus back and cause a retro-position, in addition to retarding instead of promoting a return of normal tone to the abdominal muscles.
Accordingly, they instruct their patients to take exercises, instead of wearing binders, and they have these exercises started 350while the patient is still in bed. Their adoption, and the rate at which they are increased, are entirely dependent upon the individual patient’s condition, for they must never be continued to the point of fatigue. There are, therefore, no definite rules laid down, concerning these exercises, beyond a description of the positions and movements themselves, and their sequence.
Those which are taught to the patients at the Long Island College Hospital are so simple, and evidently productive of such happy results that they offer excellent examples of this form of treatment. They are, of course, taken only by the doctor’s order, but the nurse’s intelligent supervision increases their effectiveness.
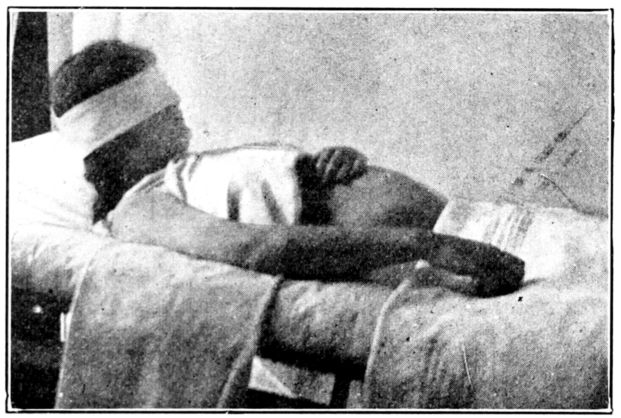
The general purpose of these exercises is to strengthen the abdominal muscles, thus helping to prevent a large, pendulous abdomen; to increase the patient’s general strength and tone, just as exercise benefits the average person; to promote involution; to prevent retro-version and in a measure, increase intestinal tone and thus relieve constipation. To accomplish these much to be desired ends the exercises must be taken with moderation and judgment; started slowly; increased very gradually and constantly adapted to the strength of the individual patient. Otherwise they may do more harm than good. In the average, uncomplicated case in which the patient is doing well, she usually 351starts the chin-to-chest exercise from twelve to twenty-four hours after delivery. She should lie flat on her back and raise her head until her chin rests upon her chest. (Fig. 129.) If she rests her hand upon her abdomen, she will feel for herself that the abdominal muscles contract, and accordingly will be disposed to continue the exercises with more interest and confidence than she otherwise might. The movement is repeated twenty-five times, morning and evening, every day, and continued as long as the patient is in bed.
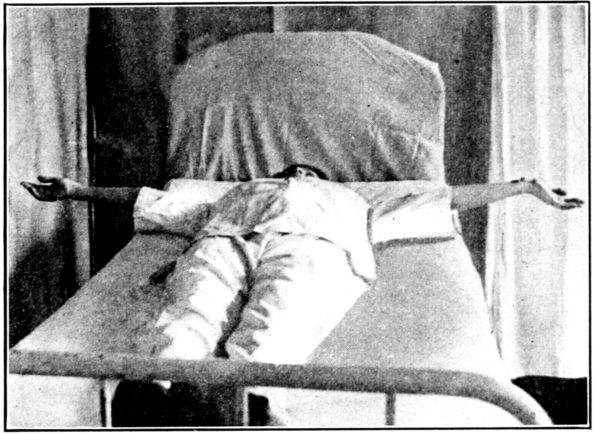
Fig. 130.
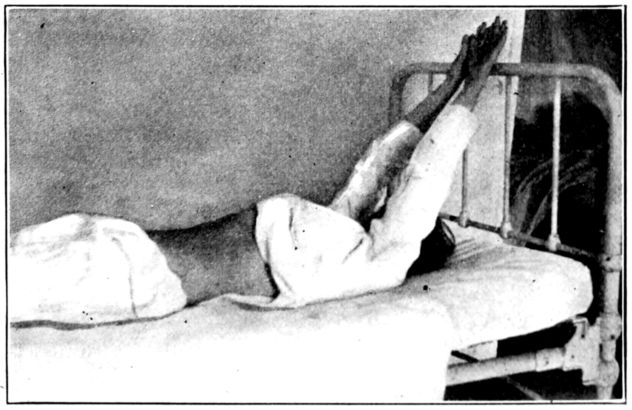
Fig. 131.
The familiar, deep-breathing exercise is ordinarily started 352on the third or fourth day. The patient should lie flat, with her arms at her sides, then extend them straight out from the shoulders (Fig. 130), raise them above her head (Fig. 131) and return them to the original position. This is repeated ten times morning and evening, daily, as long as the patient is in bed.
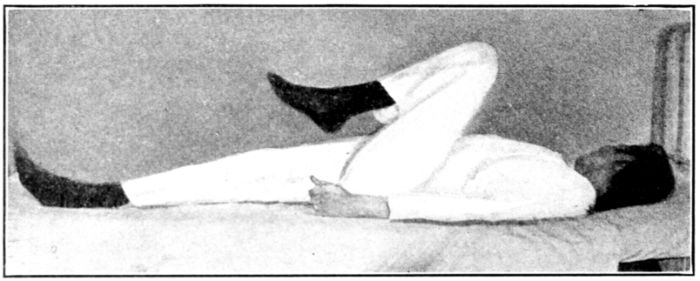
Fig. 132.
The one-leg-flexion exercises are not done by patients with perineal stitches, but in other cases they are usually started about the fifth day. The thigh is flexed sharply on the abdomen and leg on thigh (Fig. 132), then extended and lowered to the bed. This is repeated ten times, with each leg, morning and evening for one, or possibly two days.
The next exercise replaces the one-leg-flexion and is started after the latter has been done for one or two days, according to the strength of the patient, and it in turn is continued for only one or two days. Both thighs are sharply flexed on abdomen and legs on thighs (Fig. 133), then extended and lowered but not far enough for the heels to rest upon the bed before being flexed again. This is repeated ten times morning and evening.
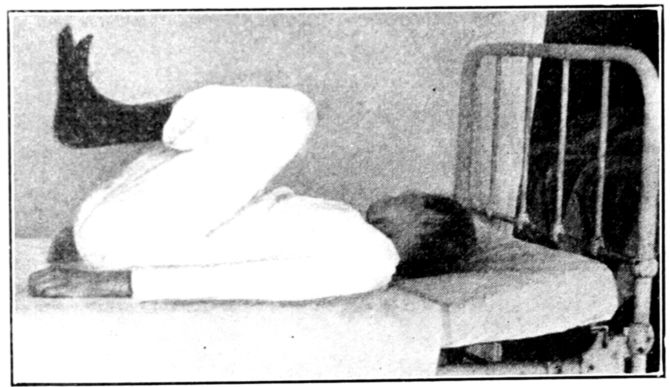
Fig. 133.
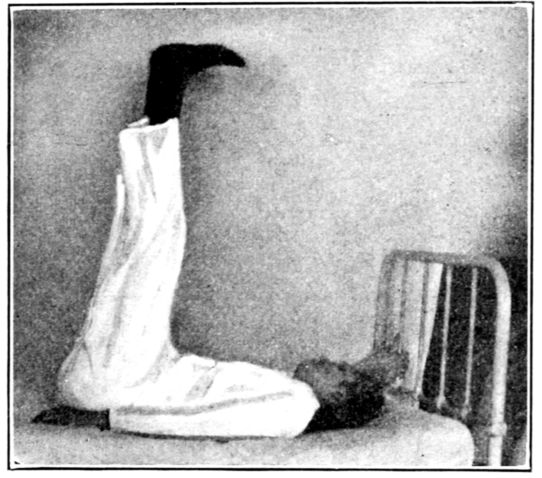
Fig. 134.
Next is the exercise for which the leg-flexion exercises prepare the patient, and which are discontinued when this one is adopted. It is started, as a rule, about the seventh day, or three or four days before the patient gets up. Both legs are slowly lifted to a position at right angles to the body (Fig. 134) and slowly lowered, but not far enough for the heels to touch the bed (Fig. 135), and the movement repeated. As this exercise requires a good deal of effort, it must be taken up very gradually, as follows: The legs should be raised on the first day, once in the morning and twice in the evening; second day, three times in the morning and four times in the evening; third day, five times in the morning and six times in the evening and so on, if the patient is not fatigued, until the exercise is repeated ten times each morning and evening. It is continued for several months.
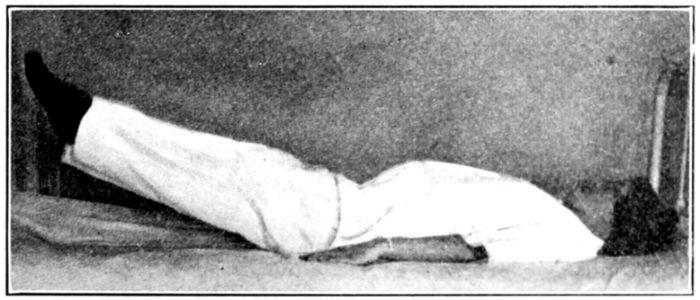
Fig. 135.
The knee chest position (Fig. 136) is intended to counteract 354the tendency toward retroversion, from which so many women suffer after childbirth. It is usually started about the seventh day and the patient begins by remaining in that position for a moment or two, gradually lengthening the time to about five minutes each morning and evening for about two months.
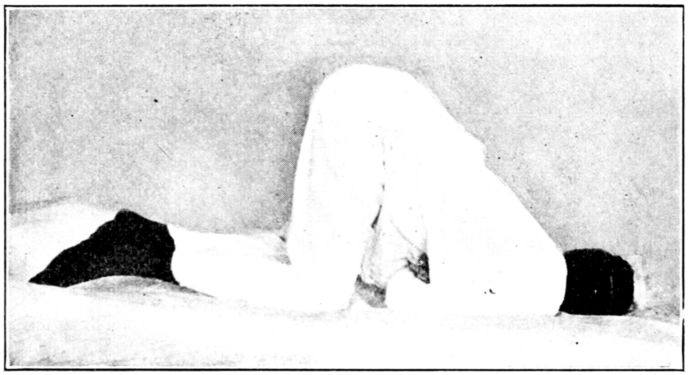
Fig. 136.—Knee chest position.
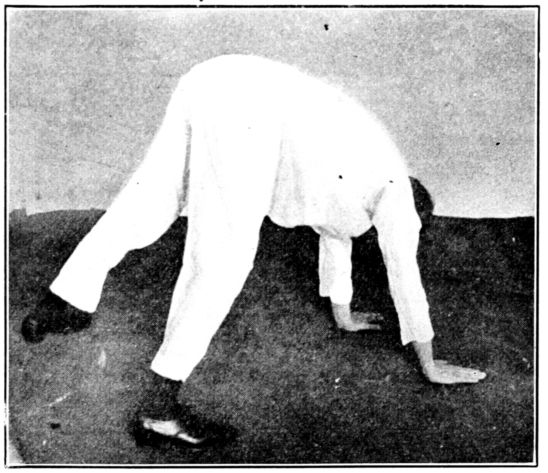
Fig. 137.—Walking on all fours. (From a photograph taken at the Long Island College Hospital.)
Walking on all fours is violent exercise and has to be taken up very gradually. Some patients are able to attempt it on the first day out of bed, if they have been taking the other exercises, but as a rule it is not started until the second or third day. The patient’s clothes should be free from all constrictions; the knees should be held stiff and straight with the feet widely 355separated, to allow a rush of air into the vagina, and the entire palmar surface of the hands should rest flat on the floor. (Fig. 137.) The patient should start by taking only a few steps each morning and evening, gradually lengthening the walk to five minutes twice daily and continuing it for about two months.
It is believed that as the patient walks in this position the uterus and rectum rub against each other producing something the same result as would be obtained by massage. The effect of the exercise is to promote involution and diminish the tendency toward constipation and retroversion, apparently preventing malposition entirely in a large percentage of cases. Though not widely used, its beneficial effects are unquestioned by those doctors who employ it.
In taking a general survey of the young mother and her needs, we realize that in a broad sense she is not ill, in so far as no pathological condition exists. But she is in a transitional state and may become acutely or chronically ill if not carefully watched and nursed. In general her mental, physical and nervous forces must be conserved and increased, and this requires thoughtful and devoted attention from the nurse. She must be scrupulously clean in her care of the nipples and perineum, and in order to be able promptly to inform the doctor of any departure from the normal in the patient’s condition, the nurse’s watchfulness should embrace regular observations upon the following:
If all goes well and there are no complications, the patient will usually be able to assume full charge of her baby by the sixth or eighth week, and practically return to her customary mode of living, with the difference that she now has the care of a baby which she did not have before. The care of that baby 356requires certain, definite care of herself, as a nursing mother, which will be described in detail in the next chapter.
To sum up the general principles of nursing the young mother during the puerperium, we find that just as during pregnancy and labor, the nurse must first be familiar with the normal changes that occur in order that she may recognize the abnormal. Then, as before, the nurse’s care of the individual patient must rest unfailingly upon a foundation of cleanliness in order to prevent infection; watchfulness, which implies ability to recognize normal changes and unfavorable symptoms; adjustment to the methods of the attending physician and to all of the circumstances surrounding the patient, and the wisest and tenderest consideration for her patient as an individual.
Not infrequently the nurse remains with her patient after the end of the puerperium, and therefore she may have the care of the mother and baby for several weeks, or even months. The most valuable single service which she can perform in this capacity is to help in making it possible for the mother to nurse her baby at the breast. For both the nurse and the mother must realize that the breast-fed baby is much more likely to live through the difficult first year, and is markedly less susceptible to disease and infection than is the bottle-fed baby.
The first step is to convince the young mother of what it means to her baby and her obligation to try to nurse him, since, excepting under very rare and unusual conditions, she can nurse him if she wants to enough to make the necessary effort and sacrifice.
The important contra-indications for attempting breast-feeding are retracted nipples, tuberculosis, eclampsia, severe heart or kidney disease and certain acute infectious diseases such as typhoid fever.
It seldom happens that the mother who has had average prenatal care, followed by good care during and after delivery, is unable to nurse her baby if she orders her life in the way that is known to be necessary to promote and maintain lactation. The first essential is her real desire to nurse her baby; next, her appreciation of the continuous care of herself that is necessary and third, her whole-hearted willingness to take this care for her baby’s sake.
It is safe to say that if the doctor and the nurse and the patient all want the baby to nurse at the breast, and all do everything in their power to make this possible, they will almost invariably succeed. This assertion can scarcely be made too positively, 358and the nurse should never lose sight of the fact that if the baby is not breast-fed he is being defrauded, and in the vast majority of cases, because of insufficient effort on the part of the doctor, nurse or patient, or all three.
A favorable frame of mind and state of good nutrition in the mother are the two indispensable factors in establishing breast-feeding and in maintaining the secretion of an adequate supply of breast-milk. These conditions, in turn, are both affected by her general mode of living, as long as the baby nurses.
Women with happy, cheerful dispositions usually nurse their babies satisfactorily, while those who worry and fret are likely to have an insufficient supply of milk, or milk of a poor quality. And in addition to this sustained influence, the temporary effect of a fit of temper; of fright; grief; anxiety or any marked emotional disturbance is frequently injurious to the quality of milk that previously has been satisfactory. Actual poisons are created by such emotions and may affect the baby so unfavorably as to make it advisable to give him artificial food, for the time being, and empty the breasts by stripping or pumping, before he resumes breast feeding.
A mother’s lack of faith in her ability to nurse is so detrimental in its effect that she must be assured over and over, that she can nurse her baby if she will persevere. If the nursing does not go well at first she must not give up, but must continue to put the baby to the breasts regularly, as this is the best means of stimulating them to activity. His feeding should be supplemented with modified cow’s milk, if the breast milk is inadequate, either in amount or quality.
Method of Nursing. The baby should be put to the breast for the first time between eight and twelve hours after he is born. This gives the tired mother an opportunity to rest and sleep, and the baby, too, is benefited by being kept warm and quiet during this interval. His need for food is not great as yet, nor is there much if any nourishment available for him.
In preparing to nurse her baby, the mother should turn slightly to one side, and hold the baby in the curve of her arm so that he may easily grasp the nipple on that side. She should hold her breast from the baby’s face with her free hand by placing 359the thumb above and fingers below the nipple, thus leaving his nose uncovered, to permit his breathing freely. (Fig. 138.) The mother and baby should lie in such positions that both will be comfortable and relaxed, and the baby will be able to take into his mouth, not only the nipple but the areola as well, so as to compress the base of the nipple with his jaws as he extracts the milk by suction.
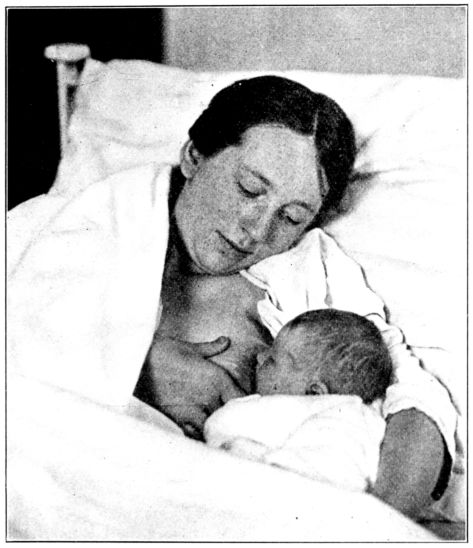
Fig. 138.—Position of mother and baby for nursing in bed.
The nurse may have to resort to a number of expedients in persuading the baby to begin to nurse, for he does not always take the breast eagerly at first. He must be kept awake and sometimes suckling will be encouraged by patting or stroking his cheek. Or if his head is drawn away from the breast, a little, he will sometimes take a firmer hold and begin to nurse. Moistening the nipple by expressing a few drops of colostrum or with 360sweetened water may stimulate the baby’s appetite and thus prompt him to nurse.
The young mother must be prepared to find very discouraging the early attempts to induce the baby to nurse, but if the nurse will help her to persevere in making regular attempts she will almost certainly succeed.
During the first two or three days the baby obtains only colostrum, while nursing, but the regular suckling is extremely important, not alone for the sake of getting him into the habit of nursing but for the sake of stimulating the breasts to secrete milk.
Moreover, the irritation of the nipples so definitely promotes involution of the uterus that this process goes on more rapidly in women who nurse their babies than in those who do not. If the nipples are not sufficiently prominent for the baby to grasp them, a shield will have to be used while they are being brought out. But the shield should be discarded as soon as possible for it is the baby’s suckling that produces the physiological effects. If a shield is used, it should be washed and boiled after each use and kept, between nursings, in a sterile jar or a solution of boracic acid.
The length of the nursing periods and the intervals between them have to be adjusted to the needs and condition of each baby; his weight, vigor, the rapidity with which he nurses, the character of his stools and his general condition, all of which will be considered in connection with the care of the baby. The intervals between nursings are measured from the beginning of one feeding to the beginning of the next, and are fairly uniform for babies of the same age and weight. The length of the nursing period itself is usually from ten to twenty minutes.
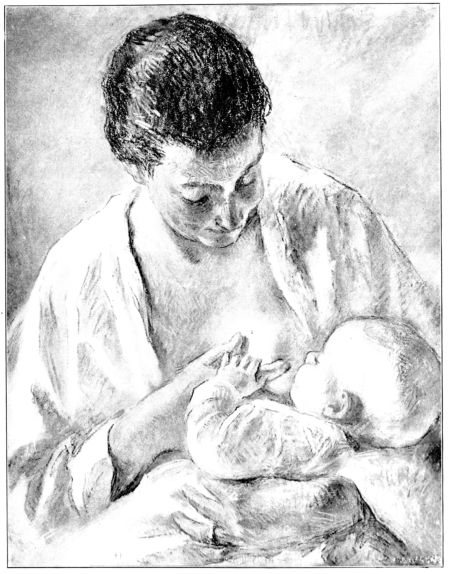
Fig. 139.—The Nursing Mother. (By permission from a pastel by Gari Melchers.)
362The average baby nurses about every six hours during the first two days, or four times in twenty-four hours. According to one schedule he will nurse every three hours during the day for about three months, beginning with the third day, and at 10 p.m. and 2 a.m., or seven times in twenty four hours. From the third to the sixth month he nurses every three hours during the day and at ten o’clock at night, or six times in twenty-four hours, and from that time until he is weaned he should nurse at four hour intervals during the day and at ten o’clock at night, or five times daily, as follows:
| Day | Night | ||||||
|---|---|---|---|---|---|---|---|
| First and second days | 6 | 12 | 6 | 12 | |||
| First three months | 6 | 9 | 12 | 3 | 6 | 10 | 2 a. m. |
| Third to sixth month | 6 | 9 | 12 | 3 | 6 | 10 | |
| After the sixth month | 6 | 10 | 2 | 6 | 10 | ||
It is becoming more and more common to omit night feedings after 10 p.m., even during the first three months, with the average baby who is in good condition. When this practice is adopted the baby not only seems to do as well as he normally should, but to benefit by the long digestive rest during the night. Certainly the mother profits by the unbroken sleep which this makes possible.
As a rule the baby should nurse from one side, only, at each nursing, emptying the breasts alternately, but if there is not enough milk in one breast for a complete feeding both breasts may be used at one nursing. Neither the mother nor the baby should be permitted to sleep while he is at the breast, but he should pause every four or five minutes to keep from feeding too rapidly.
After the mother sits up, she may occupy a low, comfortable chair while nursing the baby. She should lean slightly forward and raise the knee upon which the baby rests by placing her foot on a stool, supporting his head in the curve of her arm, and holding her breast from his face, just as she did while in bed. (Fig. 139.) She should nurse him in a quiet room where she will not be disturbed nor interrupted and where the baby and her breasts will be protected from drafts or from being chilled. Many women prefer always to lie down when nursing the baby.
Before the nurse leaves her patient she should teach her how to care for her nipples, including the preparation of boric solution; the importance of washing her hands before bathing her nipples, and of keeping the breasts covered with clean gauze between nursings.
The personal hygiene of the nursing mother should be virtually a continuation of that which is advisable during the latter part of the puerperium; a normal, tranquil kind of life which is unfailingly regular in its daily routine.
But this is not quite as easy as it sounds, for during the puerperium the young mother is still something of a patient and is regarded as such, while during the months that follow she is simply a nursing mother, who must live sanely and moderately for her baby’s sake, and at the same time take her place among people who are not under compulsion to place any special restrictions upon their daily lives. It is much easier to take precautions and follow directions for a few days or weeks, while the situation is novel, than it is to persist month after month without help or encouragement. The young mother’s family often fails to appreciate the difficulty of her problem and for this reason she is sometimes unable to care for herself, as she should, with the result that she cannot nurse her baby successfully.
As long as the nurse remains with her patient, therefore, she must try to impress upon both the patient and the members of her household that the most important single factor in the care of the new baby is the sustained and regular care which the nursing mother should take of herself. For it must be remembered constantly that it is not alone breast feeding, but satisfactory breast feeding that nourishes and builds and protects the baby. Unsatisfactory breast milk may be positively injurious, and irregularity and thoughtlessness in the mother’s mode of living will usually produce milk of this character.
Therefore, for ten or twelve months after the baby is born, the mother should discharge her responsibility and obligation to him by regulating her own life to meet his needs.
Diet. Throughout the entire nursing period the mother’s diet must be such that it will nourish her and also aid in producing milk which will meet the baby’s needs. His needs are that the daily demands of his growing body shall be supplied and that he shall be given those materials which will build a sound body, with resistance against disease and infection.
364So important is this matter of nutrition, and the principles upon which it rests, that it is discussed at considerable length in the succeeding chapter. At this point, however, it may be stated briefly that the most valuable article in the nursing mother’s dietary is milk, and that to this should be added eggs and the vegetables which are designated as “leafy,” and fresh fruits, particularly oranges. These foods are rich in the materials which are essential to the baby’s nutrition, good health, and resistance.
She should have a generous, simple, nourishing mixed diet, then, consisting largely of milk, eggs, and leafy vegetables. She must steadily guard against indigestion for if her digestion is deranged the baby is almost sure to suffer. Rich and highly seasoned foods must be avoided, as well as alcohol, strong tea and coffee or any articles of food or drink that might upset her.
It becomes apparent that although the expectant mother does not have to “eat for two,” the nursing mother does, in certain respects. She should augment the nourishment provided by her three regular meals, by taking a glass of milk, cocoa or some beverage made of milk, during the morning, afternoon and before retiring.
The morning and afternoon lunches had better be taken about an hour and a half after breakfast and luncheon, respectively, in order not to impair the appetite for the meals which follow.
It is very important that the nursing mother shall take her meals with clock-like regularity and enjoy them, but at the same time she must guard against overeating, for fear of deranging her digestion. She must drink water freely, partly for the sake of promoting intestinal activity.
Bowels. The nursing mother’s bowels must move freely and regularly every day, but she should not take cathartics nor even enemata without a doctor’s order.
She will usually be able to establish the habit of a daily movement by taking exercise, eating bulky fruit and vegetables, drinking an abundance of water and regularly attempting to empty her bowels, every day, preferably immediately after breakfast.
Rest and Exercise. The nursing mother will not thrive, 365nor will the baby, unless she has adequate rest and sleep and takes at least a moderate amount of daily exercise in the open air. She should have eight hours sleep, out of the twenty-four, in a room with open windows, and as fatigue has an injurious effect upon the character of the milk, the average mother should lie down for a while every afternoon.
Her exercise will have to be adjusted to her tastes, customary habits, circumstances and physical endurance, for it must always be stopped before she is tired. Walking is often the best form of exercise that the nursing mother can take, though she may engage in any mild sports that she enjoys. Violent exercise is inadvisable because of the exhaustion that may follow.
Recreation. Part of the value of exercise lies in the pleasure and diversion which it gives, for a happy, contented frame of mind is practically indispensable to the production of good milk. In addition to some regular and enjoyable exercise, therefore, the mother needs a certain amount of recreation and change of thought and environment. If her life is monotonous and colorless, the average woman is likely to become irritable and depressed; to lose her poise and perspective; to worry and fret, and then, no matter what she eats nor how much she sleeps, her digestion will suffer, her milk will be affected and the baby will pay. This, of course, goes back to the question of her mental state and the condition of her nerves as being determining factors in the young mother’s ability to nurse her baby successfully.
For the sake of giving her an opportunity to go out, mingle with her friends or enjoy some music or a play, it is often a very good plan to replace one breast feeding, some time in the course of each day, with a bottle feeding. The freedom which this long interval between two nursings gives the mother for diversion and amusement, will usually affect her general condition so favorably that the quality of her milk is better than it otherwise would be, and the baby is benefited as a result. This single supplementary feeding cannot be regarded lightly, however, for it must be prepared with the same cleanliness and accuracy as an artificial diet.
Weaning. One advantage in giving the baby a supplementary 366bottle, once a day, is that it paves the way for weaning, when the time comes to make this change. Under ordinary conditions, the mother begins to wean her baby about the eighth or tenth month. Having started by replacing one breast feeding, daily, with a bottle feeding, she should gradually increase the number of daily artificial feedings until all of the breast feedings are discontinued by the time the baby is eleven or twelve months old. There are exceptions to this general rule, of course, and under any conditions the weaning should always be directed by a doctor, for the baby will suffer unless it is skillfully done.
If the mother’s milk is satisfactory and the baby is doing well, it is often considered wiser not to discontinue the breast feeding entirely, during the hot summer months, even though the weaning falls due at this time.
It was formerly deemed advisable to wean the baby for any one of several reasons, but at present the only indications for this step which are generally accepted by the medical profession, are: pulmonary tuberculosis, acute infectious diseases in the mother, and pregnancy. Menstruation, which is normally suspended during lactation, was long regarded as incompatible with satisfactory nursing, but it is now known that if the mother is taking proper care of herself and is in generally good condition, the effect of menstruation upon the milk is usually for the duration of the periods only. It may be necessary to supplement the breast feeding with suitably modified cow’s milk during menstruation, but the baby should be put to the breast regularly, just the same, for if the stimulation of the baby’s suckling is discontinued, the temporary reduction in the amount of milk secreted will probably be permanent.
The state of pregnancy, however, is different, for though some women nurse the baby satisfactorily for some months after becoming pregnant, it is not considered advisable to subject a woman to the combined strain of pregnancy and nursing. Moreover, the mother’s milk is usually impoverished during pregnancy and the nursing baby suffers in consequence.
Drying up the Breasts used to be a great bugbear. Lotions, ointments and binders were employed and often a breast pump as well. Various drugs were given by mouth and the patient 367was more or less rigidly dieted. It is true that some of these measures are still employed and are followed by a disappearance of the milk. But at the same time, the breasts dry up quite as satisfactorily when none of these things is done, provided the baby does not nurse. It is not known what starts the secretion of milk in the mother’s breasts but certain it is that absence of the baby’s suckling prevents it.
If the drying up of the breasts is left to the nurse, as it so frequently is, her wisest course will be to do nothing beyond applying a supporting bandage if the breasts are heavy enough to be uncomfortable. She may rely absolutely upon the fact that the baby’s suckling is the most important stimulation in promoting the activity of the breasts and if this stimulation is not given, or is removed, the secretion of milk will invariably subside in the course of a few days. It is true, that the breasts may be engorged and very uncomfortable for a day or two, and in addition to a supporting bandage the doctor may order sedatives, but the discomfort subsides as the secretion disappears. This is true whether the reason for drying up the breasts is that the baby is still born or has died, or a live baby’s nursing is discontinued.
Naturally, the nurse will not press her patient to drink an extra amount of milk if it is not desirable to promote the activity of the breasts, but, unless otherwise ordered, there is no necessity for placing any other restrictions upon her patient’s diet.
In thinking over the period of lactation, as a whole, it is apparent that the most valuable service which the nurse can offer to the nursing mother, is assistance in planning and living a simple, normal, tranquil life; helping her to eat, sleep, bathe, and exercise and to nurse her baby with unfailing regularity—all for the sake of providing her baby with adequate nourishment. This must be the chief end and aim of her existence.
Normal breast-milk is the ideal baby food and there is no entirely satisfactory substitute. It greatly increases the baby’s chances of living through the first year, and protects him from many diseases.
Quite evidently, breast-feeding is every baby’s right and the nurse can and should help him to secure it.
The importance of providing the expectant and nursing mother with suitable food has been stressed so insistently in the preceding pages, that it is advisable to explain to the nurse the reason for these recommendations, in regard to certain groups of foods, and thus make clear why a young mother may eat a large amount of food and have an adequate amount of breast milk, and yet fail to nourish her baby satisfactorily.
The following material is available in these pages through the interest and generosity of Dr. E. V. McCollum and Miss Nina Simmonds, Professor and Assistant Professor of Chemical Hygiene, School of Hygiene and Public Health, Johns Hopkins University. This information is the result of many years of research and experimentation on many thousands of laboratory animals and of observations upon human beings as well. Dr. McCollum and Miss Simmonds offer the fruits of their labors to obstetrical nurses, in the belief that they are in a peculiarly favorable position to aid in improving the nutritional state of the coming generation.
In order that such a discussion may not seem irrelevant to obstetrical nursing, the nurse must remind herself anew, that the object of obstetrics to-day is not only to carry a woman safely through childbirth, but to give her such care from the beginning of pregnancy that she and the baby shall emerge from this experience, not merely alive, but well and vigorous and with every prospect of continuing to be so.
It is the acknowledged obligation of those engaged in obstetrical work to strive toward improving the health of the race at its source—the health of the mothers and babies. Malnourished mothers and malnourished babies do not develop a hardy race.
369It is probably safe to say that the two most influential factors in creating and maintaining a satisfactory state of health are suitable nutrition and prevention of infection; and although we shall concern ourselves solely with nutrition in this chapter, it should be stated in passing that a state of good nutrition goes far toward protecting the individual from infection.
It will help in clarifying the subject to explain in the beginning that a state of good nutrition is not necessarily evidenced by one’s being tall nor by being fat. But it is evidenced by normal size and development; sound teeth and bones; hair and skin of normal color and texture; blood of the normal composition; stable nerves; vigor both mental and physical; normally functioning organs and resistance to disease, and above all that indescribable condition which is summed up as a state of general well-being.
That this degree of nutritional stability is not as prevalent in this country as might be desired is disclosed by reports upon findings of the examining boards for army service, over a period of three years and physical examinations of various groups of school children throughout the country. It was found in the first case, that about sixteen per cent. of the apparently normal young men who were inspected for military service, were undernourished in some degree, and according to Dr. Thomas W. Wood, Professor of Physical Education, Columbia University, “Five million children in the United States are suffering from malnutrition.” This army of undernourished children, which represents about one-third of the children of the country, is on the broad highway to ill health, invalidism of various kinds and degrees, instability and inefficiency. They are certainly not developing into the clear-eyed, alert, buoyant individuals that go to make up good citizenry.
The tragic aspect of this state of undernourishment is that though a great deal can be done to nourish and build up the malnourished child or adult, a certain amount of damage that results from inadequate nourishment during the early, formative weeks and months cannot be entirely repaired later on in life.
As the baby grows and develops, certain substances are 370needed at the various stages of its progress, and if these are not supplied at these stages, there will always be some degree of inadequacy in the adult make up. It is much like the futility, when building a house, of using bricks without straw for the foundation instead of firm, durable rock, and then trying to make it substantial and secure later on by using good materials when constructing the upper stories.
The solid foundation and substantial beams and girders for men and women are put in during infancy and early childhood in the shape of good material that forms good nerves, muscles, bones, teeth and general physical stability. It is practically impossible to make up to the older child or adult for damage caused by failure to supply sufficient nourishment to the growing, developing, infant body.
We see all about us the results of this form of neglect of babies, in the bow-legged, knock-kneed, undersized, misshapen, chicken-breasted adults and in those who are nervous and below par in endurance; are susceptible to colds and other infections and may be summed up as being “not strong.”
The reasons for much of the undernourishment among people in this country to-day are to be found in certain widespread misconceptions of long standing as to what constitutes a state of good nutrition or malnutrition and the value and purposes of different foodstuffs. For malnutrition does not necessarily describe a simple condition due to an insufficient amount of food, but to any one of several complex conditions due to a lack in the food of one or more essential substances.
One may eat a large amount of food and even have a well-padded body and yet be seriously in need of certain food factors—in other words, be incompletely nourished in some particular.
That was possibly the first misconception—the belief that one simply needed enough food, and accordingly was well nourished if three large meals were eaten daily, irrespective of the composition of those meals. A step forward was taken when housewives 371and people generally accepted the fact that quantity alone was not enough to consider in providing food, but that the dietary should consist of balanced amounts of the five food materials: fats, carbohydrates, proteins, minerals and water, in order to build and maintain the body in a state of health.
But this, too, was found to be an error, in so far as it was only a part of the truth, for it was next ascertained that even provision for a suitable balance of the five food groups was not enough to nourish us, but that we must consider the heat and energy producing properties of these component parts, as measured by the caloric unit, and each must daily take in the requisite number of calories if we would keep our engines going.
It is now known that even this is not enough, for we may eat food in ample quantities, consisting of the properly balanced fats, proteids, carbohydrates, minerals and water, and it may daily yield the required number of calories, and still we may suffer from seriously faulty nutrition.
Hess and Unger state in this connection, that, “in framing dietaries for children and adults, our minds are still focused on insuring a sufficient supply of calories in the food, and we have not yet reacted in practice to the newer knowledge that ample carbohydrates, fats and proteins may constitute a dangerously deficient diet.”[10]
We find an explanation for this fact in the comparatively recent recognition of three substances, as yet not clearly understood, which are contained in a certain few articles of food, each one of which is essential to growth and normal health and well-being, though not necessarily concerned in the production of heat or energy. Various terms have been applied to these mysterious, but necessary substances, such as vitamines, accessory food substances as applied to all, or fat-soluble A, water-soluble B and water-soluble C to designate them separately.
A surprisingly small amount of each of these substances is sufficient to meet the needs of an individual, but no one of these, even in this small amount, can be safely dispensed with, for if the diet is deficient, or lacking in one or more of them some 372form of nutritional disturbance will result. It may be severe enough to be diagnosed as a disease, or it may be only enough to keep the individual below a normal state of health.
When the disturbance is profound enough to produce a definite, recognizable condition, it is designated as a deficiency disease, of which there are three: scurvy, beri-beri and xerophthalmia. With these are sometimes included rickets and pellagra. The exact cause of the two latter disorders is not definitely known but both are associated with faulty nutrition. Poor hygienic conditions may enter into the causation of rickets, and infection may be a factor in the occurrence of pellagra, but neither disease appears among those who are suitably fed while both diseases may be produced by faulty diet and both may be cured with suitable food.
But probably of graver importance to the public welfare than the well defined nutritional disturbances, themselves, is the fact that between a state of good health and the level upon which a disease is recognizable is a long scale, along which are ranged an uncounted army of under-par, half-sick people. These are the ones who are tired, nervous, susceptible to infections, with feeble recuperative powers, and in general are more or less ineffective in the business of life.
It is this borderline state, or as Dr. Goldberger terms it, “the twilight zone,” which cannot quite be called disease but is not health, that is serious to the masses, for diagnosed disease is given treatment, but nervousness, lack of energy and endurance, weakness and inefficiency are not treated; they are merely tolerated, as a rule. The sufferers fail to reach their highest possible development and they fail to be of highest value to society.
This is the condition which can be so largely prevented by giving the baby a good nutritional foundation; this must be started during its prenatal life, carried through the nursing period and then continued throughout the rest of his life. Since the nurse is very likely to be entrusted with the arrangement of the patient’s dietary, being told merely to give a liquid, soft or light diet and possibly to avoid certain articles, it will mean much to the coming generation if nurses at large are able so to 373compose the various diets for the expectant and nursing mother, that they will provide not only the requisite fats, proteids, carbohydrates, minerals and water and yield the necessary calories, but also contain all three protective substances: fat-soluble A, water-soluble B and water-soluble C. It can be demonstrated that when these food factors are not present in the mother’s diet, they will not appear in her milk, and accordingly will not be supplied to her baby.
This is the crux of the whole matter. If the mother’s diet is faulty, her milk will be faulty in the same respect and the baby will start life with tissues which contain an inadequate amount of the substances that are necessary to make them sound and promote health.
That is what we have in mind when we say that the mother’s milk must be satisfactory not alone in quantity but in quality as well.
In order to make quite clear how damaging are the results of diets which are deficient or lacking in these protective substances, we shall take up, briefly, the deficiency diseases in turn.
Scurvy (scorbutus) is caused by a lack or deficiency of the substance called water-soluble C, the most unstable of all the protective substances, being easily impaired or destroyed by heating, drying or aging. This anti-scorbutic substance is present in fresh milk, potatoes, oranges, lemons, onions, and such fresh vegetables as lettuce, raw cabbage and celery and in apples, pears, peaches, bananas and cantaloupe. Tomatoes are rich in the anti-scorbutic substance and, moreover, this form is but slightly injured by heating or aging, for which reason canned tomatoes are frequently used both to prevent and to cure scurvy.
Scurvy is a disease which develops slowly. The patient loses weight, is anemic, pale, weak and short of breath. The gums become swollen, bleed easily and frequently ulcerate; the teeth loosen and often drop out. Necrotic areas in the bones may result. Hemorrhages into the mucous membranes and the skin are characteristic. Large black and blue spots develop in the skin, after trivial injury, or even spontaneously. The ankles become edematous and in severe cases a hard, board-like condition of the skin and subcutaneous tissues develops. There is 374sometimes severe headache and in the later stages there may be convulsions and delirium.
Although scurvy has been known to exist for centuries, well developed cases are not often seen among adults to-day, because experience has taught the importance of including some fresh food in the dietary, and present transportation facilities make this a fairly simple matter for most people. The disease was doubtless limited almost entirely to soldiers and pioneers until after the discovery of America. This event marked the beginning of long sailing voyages, with diets of dried and otherwise preserved foods, and scurvy began to take a heavy toll of life among the mariners. It became known as “the calamity of sailors” because of its frequency on shipboard. A notable instance in the history of the disease was the voyage of Jacques Cartier, in 1536, when he lost twenty-six of his party from scurvy, and only saved the remainder by the use of an infusion of pine needles. The efficacy of fresh fruits and vegetables in the prevention and cure of scurvy was discovered by common experience; when it became customary to administer lime- or lemon-juice to all sailors, scurvy practically disappeared from the service.
Although we seldom see actual cases of the disease among adults to-day, it is believed that there are large numbers of border-line cases among people who subsist largely on meats, canned and dried vegetables and canned fruits, the meat-bread-and-potato type of diet, for several months at a time, as during the winter season.
“Every individual requires a certain amount of anti-scorbutic substance in his dietary, or to put this statement in a broader way, every nation has need for a per capita quota of foodstuffs containing this necessary food factor, if scurvy is to be avoided.”[11]
Infantile scurvy is seen among babies who are fed solely on milk that has been heated, boiled, pasteurized or canned, since the anti-scorbutic substance in milk is practically destroyed by heating or aging. The disease is characterized by malnutrition, 375pain, typical changes in the structure of the bones and hemorrhage in various parts of the body, most frequently in the gums and beneath the periosteum. The disease develops slowly, the first symptoms appearing between the seventh and tenth months. Tenderness or pain in the legs is perhaps the most common symptom and may be detected first by the baby’s crying when its diaper is changed or its stockings are put on. And a baby that previously has been cheerful, playful and active will prefer to lie quietly and will cry whenever it is touched. He grows pale, listless and weak and fails to gain in weight or length. The large joints are likely to be swollen and tender; the swollen gums may bleed; the urine may be diminished in amount and contain blood and there also may be edema. But it is quite possible for a baby to be in serious need of an anti-scorbutic and still not present well defined symptoms of scurvy, or it may suffer from the latent or subacute type of the disease. In the latter case there may be stationary weight; fretfulness; a muddy complexion; rapid pulse and respirations; edema over the tibiæ with perhaps tenderness of the bones and tiny hemorrhagic areas over the body.
Scurvy may be both prevented and cured by giving orange juice, potato water, or tomato juice to a baby whose diet consists of milk that has been heated and is therefore lacking in water-soluble C. Many doctors believe that an anti-scorbutic should be started as early as the end of the first month, with babies fed on pasteurized milk, for the disease develops so slowly that severe damage may be done if the administration of this material is delayed until symptoms appear.
Scurvy, itself, does not often cause death among babies, but its occurrence is serious since it renders the infants very susceptible to infection, particularly nasal diphtheria and “grip.” Recovery from even severe attacks is amazingly rapid, sometimes being complete in a week or ten days as a sole result of giving orange juice.
It is sometimes recommended that modified milk, for infant feeding, be made up with potato water, instead of barley water, since the latter has no anti-scorbutic properties, while potatoes are somewhat protective even after being cooked.
376Spinach water is sometimes given, but there is doubt in some minds about its anti-scorbutic value, which seems to be more damaged by heat than that of potatoes and tomatoes.
Canned tomatoes are valuable because of being inexpensive and preserving their anti-scorbutic properties, even after heating. It is the opinion of many pediatricians that babies tolerate canned tomatoes very well, and in some cases may be given as much as four, six, or even eight ounces daily, without causing trouble.
Infusion of orange peel also is used in the prevention and treatment of scurvy and has the advantage of being inexpensive since the orange itself may be used for other purposes.
But orange juice and lemon juice are generally accepted as being the most valuable of all anti-scorbutics. Orange juice may be started early, and to be of value as a preventive, must be started early or scurvy will have started to develop. The common practice is to give a dram, daily, at three months, increase it to an ounce by the sixth month and two ounces when the baby is a year old. It should be diluted with water and given in two doses, midway between two morning and afternoon feedings.
To sum up: Scurvy in infants or adults is the result of a diet which is deficient or lacking in the anti-scorbutic substance, called water-soluble C, and may be prevented or cured by adding to the faulty diet those articles of food which contain this substance, namely, fresh milk, oranges, leafy, green vegetables, cabbage, onions, potatoes or tomatoes. Although scurvy is seldom seen in breast-fed babies it is believed that an infant nursing at the breast of a woman whose diet is poor or lacking in the anti-scorbutic substance may suffer a certain degree of starvation for this food factor.
Recent work at the University of Minnesota has shown that milk from cows on dry feeds is very much lower in anti-scorbutic properties than milk from cows on green pasture. This provides a strong argument for giving orange juice to all artificially fed babies, for one cannot always know how the cows, from which the milk is obtained, are fed.
Beri-beri is a deficiency disease, chiefly characterized by 377paralysis and caused by a diet which is lacking or poor in water-soluble B. The foods which entirely lack this substance are polished rice, starch, sugar, glucose, and the fats and oils from both animal and vegetable sources, while those which are poor in it are the products of degerminated cereal grains, such as tapioca, hominy, cornmeal, macaroni, spaghetti and the muscle cuts of meat, such as steak, roast, chops, ham and fish and fowl muscle. Foods which are rich in water-soluble B are beans, peas, the root vegetables as beets, carrots, white and sweet potatoes, leafy vegetables, fruits, milks, eggs and the glandular organs such as liver, kidneys and sweet breads.
The early symptoms of beri-beri are fatigue and depression; numbness and stiffness in the legs; more or less edema of the ankles and face, followed by tenderness of the calf muscles, and tingling or burning sensations in the feet, legs and arms. There are two types of the disease, the dry and the wet. In the dry type, wasting anesthesia and paralysis are the chief symptoms, while the most marked evidences of the wet type are the edema, which may be excessive, affecting the entire body. The death rate from beri-beri is usually high.
We are accustomed to thinking of this disease as occurring chiefly among the Orientals, for it was long confined to Southern China, Japan, the Dutch East Indies and the Malay Peninsula. But it may occur among any people whose diet is poor in those foods containing the particular substance which protects against it. It is common in Newfoundland and Labrador and certain parts of South America and among people who eat little aside from staple, non-perishable, cereal products, wheat bread made from bolted flour, fish and salt meats. An evidence of this near at home was an outbreak of typical beri-beri, in the jail at Elizabeth, N. J., in 1914, caused by the faulty diet of the inmates.
The disease may be prevented or cured only by including in the diet such food as milk, eggs, fresh fruit and vegetables.
Xerophthalmia is a deficiency disease characterized by eye lesions and due to a lack of, or deficiency in the diet of the protective substance which has been designated as fat-soluble A. This substance is absent in polished rice, and present in but small amounts in barley and other cereals; in muscle cuts of meat; in 378peas, beans and other vegetables excepting those described as “leafy.” It is contained in cod-liver oil, butter, cream, egg yolk, liver, kidneys and the leafy vegetables.
In the early stages of the disease the eyes are inflamed and the lids badly swollen. If the diet is wholly lacking in fat-soluble A, the disease progresses rapidly, the eye balls frequently rupture and the lens and vitreous humor are expelled, with total and permanent blindness as the tragic result. On the other hand, the malady clears up in a very spectacular manner if, in the early stages, the patient is fed those foods which contain the mysterious, but indispensable fat-soluble A.
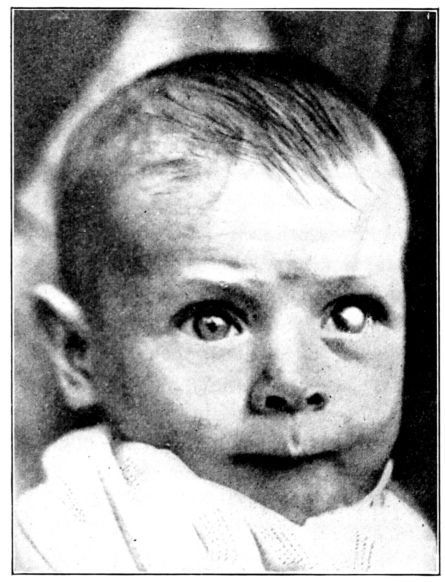
Fig. 140.—This baby is totally blind in the left eye as a result of ulcers, due to a long continued diet of cereals with a little skimmed milk; in other words, a diet poor in fat-soluble A. The right eye became involved but administration of cod-liver oil was followed by speedy recovery and partial vision was saved. There is little doubt but that the baby would have been totally blind had the faulty diet been continued. (From the Newer Knowledge of Nutrition, by E. V. McCollum.)
Well developed xerophthalmia is not common in this country 379but one sees inflamed eyes and corneal ulcers in young children which clear up with little local treatment after a mother has been persuaded to give the patient more fresh milk, butter and green vegetables.
Mori reports upon about 1500 cases occurring in Japan, in 1905, among children between the ages of two and five years. He states that the disease does not occur among the fisher folk but among people whose diet is largely composed of rice, barley, cereals, beans and “other vegetables,” but he does not state what the other vegetables are. Prompt relief of the eye symptoms was observed when cod-liver oil, chicken livers and eel fat were administered.
Bloch describes cases of xerophthalmia among infants under one year of age, in the vicinity of Copenhagen, during the years of 1912 and 1916. (Fig. 140.) The babies were also suffering from malnutrition and the skin was dry, shrivelled and scaly. Their diet consisted largely of separator skimmed milk, which was, therefore, practically fat-free, oatmeal gruel and barley soup. The milk was pasteurized and then cooked in the home before being fed to the babies. Such a diet was so faulty that the infants in question may well have been border-line cases of scurvy and beri-beri, as well as developed cases of xerophthalmia. It is also evident that the children were unquestionably suffering from rickets.
It is believed that the condition known as night-blindness is related to, or a mild or early form of xerophthalmia. It occurs in Newfoundland and Labrador, among men in lumber camps and elsewhere, whose diet consists chiefly of wheat flour, beans, meat, fish, molasses, raisins and coffee. Such a diet is made up of those parts of the plant or animal which have good keeping qualities, but these qualities do not compensate for the poverty of the protective substance.
Dr. Anna Strong, who has had experience as a medical missionary in India, observes that night-blindness is common in the vicinity of Calcutta, and it is said to occur frequently in Russia during the Lenten fasts. The popular treatment for this condition consists of poulticing the eyes with fresh goat’s liver and giving the liver as a food as well; while in Japan the efficacy 380of eating liver to cure night-blindness has been recognized from early times.
Pellagra is a disease of obscure origin, associated with faulty nutrition, which involves the nervous and digestive systems and the skin. Usually one of the first symptoms is soreness and inflammation of the mouth, then a remarkable, symmetrical eruption appears on parts of the body, which, with weakness, nervousness and indigestion form the most characteristic picture of the disease.
There are some indications that infection may be the immediate cause, but the strong evidence is that a faulty diet is the chief predisposing cause of the disease. Certain it is that pellagra is both prevented and cured by a diet containing liberal amounts of milk, eggs and leafy vegetables. On the other hand, those who live during the winter months on a diet chiefly derived from bolted white flour, degerminated cornmeal, polished rice, starch, sugar, molasses and fat pork, furnish the victims of this dreaded disease in the spring.
Pellagra was discovered in Northern Spain, by Cassal, in 1735, but for many years it had been of common occurrence in parts of Italy, and during the last century has been prevalent in parts of France, the Balkans, especially Roumania, and for a lesser time, in Egypt. In America the disease was not recognized with certainty until 1908, but from that year its incidence apparently increased, until by 1917 there were 170,000 cases of pellagra recorded in the United States, principally located in the Southern States.
In 1914, Dr. Joseph Goldberger, of the United States Public Health Service, began an investigation of the factors concerned in causing pellagra. After he had studied its prevalence in various orphanages in the South, and had relieved the situation by improving the diet with milk, fresh vegetables and meat, he was anxious to know whether the disease could be produced by a faulty dietary, of the type common among pellagrins. He planned an experiment to this end, which would restrict men to a diet similar to that which had been supplied in the institutions where pellagra had been endemic, and where it had been relieved by the improvements in the food supply which have been mentioned. 381This type of diet was also very characteristic of that used in the homes of the cotton mill workers throughout the South, where pellagra was so common. The Governor of Mississippi offered pardon to any of the healthy white men in the state prison who would submit themselves as subjects for the experiment, and eleven actually underwent the test.
The men were put upon a diet consisting of articles made from white, wheat flour, degerminated cornmeal (maize), polished rice, starch, sugar, molasses, pork fat, sweet potatoes, coffee and very small quantities of collards and turnip greens—so small as to furnish inadequate protection against a certain degree of undernourishment. At the end of five and a half months six of the eleven men developed the skin lesions characteristic of incipient pellagra.
As a result of his investigations, Dr. Goldberger points out the important fact that when milk, eggs, meat, fresh fruit and vegetables are included in the diet, pellagra does not develop, also that the disease may be cured by giving these articles of food to the afflicted person.
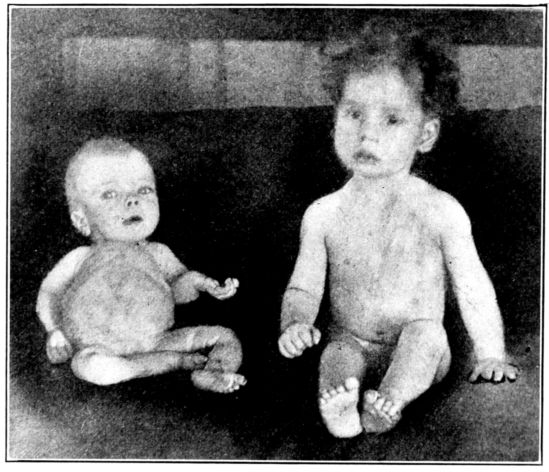
Fig. 141.—Rachitic baby and normal baby of the same age, showing dwarfism and deformities caused by rickets. (By courtesy of Dr. Leonard Findlay, Glasgow, Scotland.)
Rickets. The actual cause of rickets is not definitely known, 382but the disease apparently results from wrong proportions between calcium and phosphorus, and to unfavorable amounts of these two substances in the food. Accordingly, it may be said to be due to a faulty diet—one which is rich in carbohydrates and poor in fats and possibly some substance as yet unrecognized—and it may be both prevented and cured by what is now regarded as suitable feeding.
The chief characteristics of the disease are arrested growth and softening of the bones, with dwarfism and deformities as a result. (Fig. 141.) It is essentially a disease of infancy, occurring as a rule, between the fourth and eighteenth months but some of its unfavorable effects, such as bone deformities and poor resistance to disease, may persist throughout life.
Although babies rarely die of rickets alone, it is one of the most serious of all health problems and obstacles to normal development and stability, since it predisposes to such diseases as bronchitis, pneumonia, tuberculosis, measles, and whooping cough and in general greatly enfeebles the powers of resistance and recuperation.
It is common among babies who are fed solely or continuously on heated milk, either boiled or canned, and on proprietary foods and sweetened condensed milk. There has been some speculation about the possible relation between rickets and fat-soluble A, but no definite conclusions have yet been reached. It is known, however, that rickets may develop among nursing babies whose mothers are on faulty diets, and that the disease may be prevented and cured by the administration of cod-liver oil, which is rich in fat-soluble A. Sunshine, also, seems to have a pronounced effect in preventing and in curing the disease.
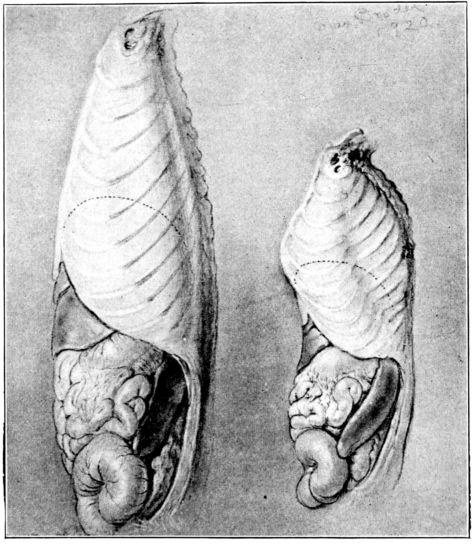
Fig. 142.—Exterior of thorax of normal rat and rachitic rat of same age. The latter shows dwarfism and deformities resembling pigeon breast so frequently seen in human beings suffering from rickets. (From The Newer Knowledge of Nutrition, by E. V. McCollum.)
Symptoms. The common symptoms of rickets which appear early are irritability; restlessness particularly at night; a tendency toward convulsions from very slight cause; digestive disturbances and profuse perspiration about the head. The baby may be fat, but is likely to be flabby and to have a characteristically white, “pasty” color. The fontanelles are large and late in closing; the abdomen is large and the chest narrow; dentition is usually delayed and the teeth may be soft and decay early. But the most conspicuous effect of rickets is upon the entire bony skeleton, due to the inadequacy of the lime deposit. The bones are soft, easily bent and broken and often misshapen. Their growth is likely to be retarded and the ends of the long bones may be enlarged, giving the familiar swollen wrists and ankles, while the nodules which form at the junction of the ribs and sternum, produce the beaded appearance so commonly called a “rickety rosary.” The bones in the arms and legs may become curved as the baby lies or sits in its crib, making him either bow-legged or knock-kneed. The deformity is increased by walking because the soft bones are easily bent by the weight of the body. The spinal column may be curved or too weak to permit the baby to sit straight or stand alone. The entire chest wall is often 384deformed (Figs. 142, 143) producing the familiar “chicken breast,” as well as a serious decrease in the size of the thoracic cavity, and through loss of rigidity of the bony wall, the respiratory movements may be seriously impaired. The forehead is prominent and the whole head looks square and larger than normal, while the pelvic deformities in girl babies often give rise to very serious obstetrical complications later in life, as has been previously explained.
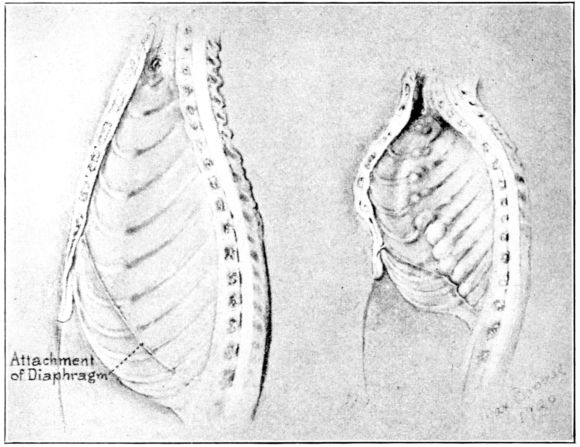
Fig. 143.—Interior of specimens in Fig. 142 showing nodules, due to rickets, protruding into thoracic cavity and encroaching upon space occupied by heart and lungs. This is a factor in the respiratory diseases which frequently complicate rickets.
Although lack of fresh air and sunshine seem to be factors in producing rickets, it has been observed that the disease does not develop in poor surroundings if the diet is suitable or if cod-liver oil is given to babies fed artificially, or on unsatisfactory breast milk; but that it may occur in the presence of satisfactory hygienic conditions if the diet is faulty in certain respects. For children under a year old, the desirable food is good breast milk, or, lacking that, fresh, certified cows’ milk, with fruit juices, scraped beef, eggs and strained vegetable purées, started as early and increased as rapidly as the baby can digest them.
385Treatment. Cod-liver oil and sunshine, together with proper food, are the essentials in treating rickets. When cod-liver oil is given to a baby whose diet is faulty, it exerts a marked tendency toward enabling the bones to develop satisfactorily even when the mineral content of the food is unfavorable. The use of sunshine, either by moving the baby from a dark to a light house, or by exposing his body to the direct rays of the sun is found to be of pronounced therapeutic value. These factors, in addition to general good care constitute the treatment, but it is a long slow process, taking from three to fifteen months, and it is doubtful if the damage which the disease works can ever be entirely repaired.
Rickets is more common during the cold months of the year, winter and spring, than during the milder summer and autumn seasons. A possible explanation for this lies in the higher value of the cows’ food during the warm months when green things form the diets of animals. Since it is now recognized that milk is not a constant product, but that its properties vary with the food of the animals that produce it, cows’ milk would be favorably influenced by their being put to pasture.
Similar evidence of such an influence is seen in the fact that although rickets is not seen among breast-fed babies whose mothers are on satisfactory diets, it may and does occur in breast-fed babies who are nourished by mothers who are, themselves, on dietaries which are poor in milk and fresh fruit and vegetables.
Drs. Hess and Unger made a study of the occurrence of rickets among colored babies in a section of New York City and the value of cod-liver oil as a preventive of this disease. In commenting upon their findings, they state, “This tendency is so marked that it may be safely stated that over ninety per cent. of the colored babies have rickets, and that even a majority of those that are breast-fed show some signs of this disorder.” They ascertained that the average diet of the mothers of these rickety babies was largely made up of carbohydrates and proteins, being poor in fats, although the diets yielded a daily quota of calories which represented almost the requisite amount for 386their individual weights. But they took little fresh milk or fresh fruit or vegetables, using canned and dried products freely.
It is important to note here that it is a diet of heated milk, rich in carbohydrates but poor in fats, that produces rickets in a bottle-fed baby—almost the same type of diet which in a nursing mother results in rickets in a breast-fed baby.
In an endeavor to prevent rickets among these incompletely nourished babies, Drs. Hess and Unger carried on a definitely organized experiment. “Our plan,” they report, “was to give infants under six-months one-half teaspoonful of oil three times daily and older infants twice this amount. It was found that almost all babies can take cod-liver oil, although it may disagree temporarily and may have to be discontinued for short intervals when there is digestive disturbance. Infants of from two to three months tolerate the oil in half-teaspoonful doses, and younger ones may be given still smaller amounts.” In commenting upon the tabulated results of this interesting study they say: “It is seen that we were able to prevent the development of rickets in more than four-fifths of the infants who received the oil for six months, and in more than half of those who were given it for four months. This result must be considered satisfactory when we note that, of the sixteen infants who did not receive the oil, fifteen showed signs of rickets, though all of them lived under the same conditions and many in the very same families. No other treatment was given, nor was a change of diet or mode of life attempted which could account for the difference in the results between the two groups of cases.” The poor quality of the breast milk of these inadequately nourished mothers is suggested by the further statement: “Table two shows that the cod-liver oil proved to be a more potent factor than breast feeding in warding off rickets, and that almost all the colored babies developed rickets even though nursed.”
It may seem like a far cry from scurvy among sailors, on shipboard, xerophthalmia among lumbermen in Labrador, and beri-beri among the Orientals to the nursing mother and her baby in our care.
But when we gather all of these apparently unrelated threads together and consider them in their possible relation to this same 387nursing mother and her baby, right here at hand, the following facts stand out as being of insistent importance to their well-being:
We must see to it, therefore, that our selection of food for 388the expectant and nursing mother provides those substances which are necessary to promote growth and development and preserve health, if we are to live up to our claim that the aim of obstetrical nursing is to aid in building a strong, vigorous and buoyant race.
The nurse may find herself feeling a bit dismayed at the prospect of trying to remember at all times which foods contain fat-soluble A, for example, and which are poor in water-soluble C, but she can remember in general, that milk and leafy vegetables are the great protective foods and that any diet which is poor in these is incapable of nourishing satisfactorily; and by calling to mind the deficiency diseases, previously described, she will be impressed anew by the seriousness of faulty nutrition.
By milk we mean, in addition to fresh milk, cream, butter, butter-milk, cream-soups and sauces, custards, ice-cream and all dishes and beverages made of milk.
By leafy vegetables we mean lettuce, romaine, endive, cress, celery, cabbage, spinach, onions, string beans, asparagus, cauliflower, Brussels sprouts, artichokes, beet greens, dandelions, turnip tops and the like.
Other foods which are rich in protective substances are fresh fruit, egg-yolks and glandular organs.
Nearly all of the common foods are deficient in some respect, but as the shortcomings of the various groups are different, we can arrange entirely satisfactory diets by combining foods which supplement each other’s deficiencies. This explains to us why the meat-potato-peas-beans-bread-and-pie type of meals fails to supply adequate nourishment. These foods belong in the same general group and are deficient in about the same kind of food factors, thus tending to duplicate, rather than supplement each other.
If such a fare is enriched by the addition of the protective foods, milk and leafy vegetables, we have a well rounded diet in which the deficiencies of one group of foods are supplied by the properties of the other groups. In fact, it is only by such a supplementing combination that an entirely satisfactory diet can be secured.
Dr. McCollum points out that the mother on a faulty diet 389cannot nurse her baby to his advantage. “The mammary gland,” he says, “picks up from the blood both of the chemically unidentified food essentials, fat-soluble A and water-soluble B, and passes these into the milk, but it is unable to produce either of these substances anew. When one or the other of these is absent from the mother’s diet it is not found in the milk. We have shown the possibility of producing milk, poor or lacking in each of these substances and therefore not capable of inducing growth.”[12]
Dr. W. E. Musgrave gives dramatic accounts of the effect upon nursing babies of faulty nutrition among mothers in the Philippines, as follows: “Infant mortality in Manila,” he writes, “is greater than it is in any other city from which we have records. The underdeveloped and undernourished condition of the great masses of the Filipino people is due to a number of causes, the principal one being insufficient quantity and injudicious variety of foodstuffs employed. The cause of the enormous influence of the faulty nutrition of the mothers upon infant mortality directly and indirectly is one of the most important subjects within the scope of any investigation of this character. The mortality in breast-fed children is higher than it is among children artificially fed. This condition so far as we know is peculiar to the Philippines. The logical, and we believe, the correct explanation of this is the deficiency in quality and quantity of the mother’s milk. There are not in history more pathetic examples of unavailing self-sacrifice than are daily seen in our large clinics of poor, half-starved, undernourished mothers attempting to supply from their breasts food enough for one or more children, when their own metabolisms are in a starved condition. When asked the direct question as to the supply of foodstuffs these mothers almost invariably state that they have plenty to eat and the pathetic part of the story is that they believe that they are stating facts. These abnormal premises are the result of a peculiar unexplainable psychology that is of very wide application in this country that the administration 390of food is more to satisfy hunger than to produce flesh and blood, and that the cheapest way in which hunger may be satisfied produces a satisfactory form of existence.”
It is generally agreed that the two big problems of babyhood are proper nutrition and the prevention of infection, but nutrition is perhaps the greater problem, since any form or degree of malnutrition lessens the baby’s powers to resist and to recover from infection. Whether breast-fed or bottle-fed, therefore, it is imperative that the baby be nourished in the complete sense of being given all of the food materials which are essential to normal growth, development and protection against disease.
If the baby is artificially fed on milk that has been heated, his diet needs to be augmented by such protectives as cod-liver oil and orange juice, since the protective properties of milk are impaired by heating. If he is breast-fed, the mother will be able to supply to her baby the requisite nourishment and protective substances only if she, herself, is adequately nourished and in good condition.
That is the point of this entire discussion: The nursing mother must be on a satisfactory diet or she cannot satisfactorily nurse her baby. And by satisfactorily nursing her baby we mean, to give him from the beginning, through her milk, the materials necessary to build well and firmly that temple, in the shape of his body, which he will occupy throughout life; a structure so securely built, from the foundation up through each stage, that it will be able to withstand the attacks of disease and weather the inevitable storm and stress of life.
McCollum. The Newer Knowledge of Nutrition, 2nd edition. New York, 1918.
McCollum and Simmonds. The American Home Diet, Detroit, 1919.
McCollum. Newer Aspects of Nutrition, Proceedings of the Institute of Medicine of Chicago, 1920, iii, 13.
Musgrave, W. E. The Philippine Jour. of Science, Series B, vol. 8, 1913, 459.
Goldberger, J. Jour. Amer. Med. Assoc., 1916, lxvi, 471.
Hess, A. F. and Unger, L. J. Prophylactic Therapy for Rickets in a Negro Community.
The most important of the complications of the puerperium are subinvolution and malpositions of the uterus; breast abscesses; hemorrhage and infection.
The importance of these to the nurse lies in their preventability, by means of the clean and efficient care which she helps to give during pregnancy, labor and the early weeks after the baby is born.
The nurse’s part in prevention and treatment of subinvolution, malpositions of the uterus and breast abscesses is so bound up in the daily care of the young mother that it was described in the preceding chapter.
Hemorrhage. Under ordinary conditions, a patient may lose as much as 500 cubic centimetres of blood during or immediately after labor, without serious results, but a loss of 600 cubic centimetres or more is regarded as a hemorrhage and as requiring speedy attention.
According to Dr. Williams, severe hemorrhage occurs only once in every few hundred labors, and with proper treatment, should not result fatally in more than one out of every 2000 or 2500 cases.
The severe hemorrhage due to a partially separated placenta occurs during the third stage of labor and was discussed in that connection. As the danger of hemorrhage, after labor is completed, is greatest during that critical hour immediately following, it is practically routine the country over to watch the patient closely during this period, both for the sake of preventing bleeding and detecting its early evidence, should hemorrhage occur, thus making prompt treatment possible.
The causes of post-partum hemorrhage are: Deep cervical tears, retained portions of the placenta, and atony of the uterus.
392The treatment of hemorrhage due to tears of the generative tract is suturing the torn edges.
Since the retention of even a small piece of placental tissue will prevent the uterus from contracting firmly, the treatment of hemorrhage from this cause is immediate removal of the retained fragment. It is to obviate this occurrence that the placenta is carefully inspected after its expulsion. If it is not intact, the obstetrician may introduce his finger and remove the retained portion, thus making it possible for the uterus to contract properly and close off the open blood vessels.
Atony, or impaired tone of the uterine muscles, may result in hemorrhage because of failure of the muscle fibres to constrict the vessels. Quite evidently, the first step toward controlling hemorrhage from this cause is to stimulate the muscles to contract; this is done by means of massage and the administration of pituitrin and ergot. Elevation of the foot of the bed and application of ice-bag to the abdomen are also employed.
In severe cases, the doctor may give an intra-uterine douche of hot, sterile salt solution and if this fails he may pack the uterus tightly with sterile gauze. The douche and pack represent operative maneuvers and, therefore, are never to be undertaken by the nurse. Her assistance is important, however, as strictest asepsis is imperative and she will have to prepare the patient and the necessary articles with the greatest care.
Should bleeding become profuse during the doctor’s absence the nurse must stay with the patient and massage the fundus and have some one else elevate the foot of the bed on the seat of a straight chair or upon firm blocks and summon the doctor. In anticipation of such an emergency the nurse must always have an understanding with the doctor about the administration of pituitrin and ergot. If there has been no understanding, and the doctor is delayed or the bleeding becomes alarmingly profuse, the nurse will usually be upheld if she gives 1 cubic centimetre of pituitrin, hypodermically and a dram of ergot by mouth.
It is, of course, definitely understood that nurses do not give medicines without orders, but a single dose of pituitrin and ergot upon the occurrence of a profuse hemorrhage can scarcely do harm and may actually save the patient’s life. Such 393a situation is an emergency fortunately a rare one, and the nurse will have to be quick-witted and use the best judgment she is capable of.
The patient is usually more or less shocked by the time the bleeding has been controlled and needs the rest, quiet and stimulation that are ordinarily employed in such cases. She should be well wrapped in blankets and surrounded with hot water bottles placed outside the blankets, watched constantly and moved frequently; salt solution or strong coffee are sometimes given by enema, or saline infusions or intra-venous injections may be given. The patient must be kept warm and quiet and pressed to drink large amounts of fluids.
But above all the nurse must remember that severe hemorrhage from a relaxed uterus can almost always be prevented if the fundus is kept hard, by massage when necessary, during the first hour or so after delivery.
Puerperal infection is usually regarded as a condition which results from the entrance of infective bacteria into the female generative tract during labor or the puerperium, to distinguish it from other infections which may occur coincidently with the puerperal state, but not necessarily be related to it.
Puerperal infection is one of the most destructive and most dreaded of the complications which may overtake the obstetrical patient, and has evidently been so considered since the days of Hippocrates. Until recent years this veritable scourge was so utterly baffling that it was regarded as more or less of a dispensation of a Divine Providence and therefore to be accepted with the same philosophical resignation as earthquakes and cyclones.
In dramatic contrast to this unresisting attitude is the present knowledge concerning the cause and prevention of this disease, and the general belief that it is a wound infection and therefore practically preventive; that it is to be ascribed to the carelessness of mankind rather than to the indifference of Providence.
This change is due very largely to the devoted work of three men who were deeply stirred by the tragic frequency with which young women laid down their lives in so-called “child bed fever.” 394These men were Ignaz Semmelweiss, Oliver Wendell Holmes, better known to Americans as poet and humorist, and Louis Pasteur, each contributing his own special observations to the sum of knowledge which was to mean so much to mothers of the future. Also the theories of Lister concerning antisepsis and the inauguration of the use of sterile rubber gloves by Dr. Halsted, of Johns Hopkins Hospital, has had the same life-saving effect upon obstetrical patients as upon all surgical patients.
In 1843, Oliver Wendell Holmes read a paper before the Boston Society for Medical Improvement, entitled “The Contagiousness of Puerperal Fever.” In this paper he presented striking evidence that in many instances, something was conveyed by doctor or nurse, from an ill person to a maternity patient with puerperal fever as a result. He was attacked and ridiculed for his theories and some of the leading obstetricians declared that it was an insult to their intelligence to expect them to believe that creatures too small to be seen by the naked eye could work such havoc.
In 1847 Ignaz Semmelweiss, of the Vienna Lying-in Hospital, decided as a result of some of his investigations that puerperal infection was a wound infection, and that the infecting organisms were introduced into the birth canal on the examining finger of the doctor or nurse, after contact with an infected patient or cadaver. Accordingly he required that all vaginal examinations be preceded by washing the hands in chloride of lime, after which precautions the mortality from infection dropped from 10 per cent. to less than 1 per cent. In 1867 Semmelweiss offered his theories and conclusions in a masterly work on this subject, the title of which may be translated as “The Etiology, Conception and Prophylaxis of Child-Bed Fever,” but the actual cause of the disease was still unknown.
But about 1879 Pasteur demonstrated what is now known as the streptococcus, in certain patients suffering from puerperal fever.
“Pasteur,” wrote M. Roux, “does not hesitate to declare that that microscopic organism (a microbe in the shape of a chain or chaplet) is the most frequent cause of infection in recently delivered women. One day, in a discussion on puerperal fever at the Academy, one of 395his most weighty colleagues was eloquently enlarging upon the causes of epidemics in lying-in hospitals; Pasteur interrupted him from his place. ‘None of those things cause the epidemic; it is the nursing and medical staff who carry the microbe from an infected woman to a healthy one.’ And as the orator replied that he feared that microbe would never be found, Pasteur went to the blackboard and drew a diagram of the chain-like organism, saying: ‘There, that is what it is like!’ His conviction was so deep that he could not help expressing it forcibly. It would be impossible now to picture the state of surprise and stupefaction into which he would send the students and doctors in hospitals, when, with an assurance and simplicity almost disconcerting in a man who was entering a lying-in ward for the first time, he criticised the appliances, and declared that the linen should be put into a sterilizing stove.”[13]
Slowly, but very slowly, the teachings of these earnest men were adopted by the medical profession, with the result that in well-conducted, modern hospitals the precautions which have been described in preceding chapters are rigidly observed. And to-day, one woman in about 1,000 in such hospitals dies of puerperal infection, instead of one in ten, as in the early days. In the year 1864, 23 per cent. of the patients at the Maternité, in Paris, died of puerperal infection.
But unhappily, the decline in the occurrence of puerperal infection, in this country is largely confined to the hospitals, for in the homes throughout the land the disease is almost as common as it was in the days of our fathers, or even grandfathers. Of approximately 20,000 deaths from childbirth in this country during 1920, about one-half, or possibly 10,000 were from puerperal infection.
To the nurse there is considerable significance in Pasteur’s characterization of the infected young mother as an “invaded patient,” for the nurse’s preparation for labor and her care of the patient during the puerperium should be enormously influential in preventing this “invasion.” In this connection she may well ponder Miss Nightingale’s assertion that “The fear of dirt is the beginning of good nursing.” Certainly the obstetrical patient cannot be well cared for unless the nurse has this fear in her heart.
396Puerperal infection, then, in the light of present information, is regarded as a wound infection caused by the streptococcus, gonococcus, colon bacillus, gas bacillus or any other pus producing organism. Of these, the streptococcus infection is the most frequently seen and is also the most serious, about 10 per cent. of such infections resulting fatally; while the gonorrheal infection, though seldom ending in death, usually causes sterility.
Infection during the puerperium occurs most often in the uterus, and, if mild, may amount to nothing more than endometritis, or inflammation of the uterine lining. In more serious cases, the inflammation may spread to the tubes and ovaries; may cause abscesses in the broad ligament and general peritonitis. A streptococcus infection may spread through the lymphatics and cause general septicemia.
Infection of the raw and bleeding placental site may occur at any time during labor or the ten days following, though the danger of infection decreases steadily after the first day postpartum.
Symptoms. The symptoms vary greatly according to the infecting organism and according to the site and extent of the inflammation. In mild types of infection, the patient may be entirely normal for the first three or four days and then complain of chilliness or even have a chill; her temperature will be slightly above normal, finally reaching about 101° F., where it hovers for ten days or two weeks, after which it drops again to normal and the patient recovers.
The severe type, which is so dreaded, is the one in which the patient is normal until the third or fourth day when she complains of tenderness, chilliness, weariness, and of being generally wretched. She may complain of chilliness but more often has a chill.
The pulse is usually rapid and the temperature goes up somewhat abruptly. (Chart 3.) The condition of the lochia depends upon the infecting organism. In streptococcal infection the lochia is often greatly decreased in amount and almost odorless, while in colon bacillus infections the lochia is profuse and foul-smelling. The attack may be very acute and result 397fatally in a few days, or it may gradually subside and the patient recover.
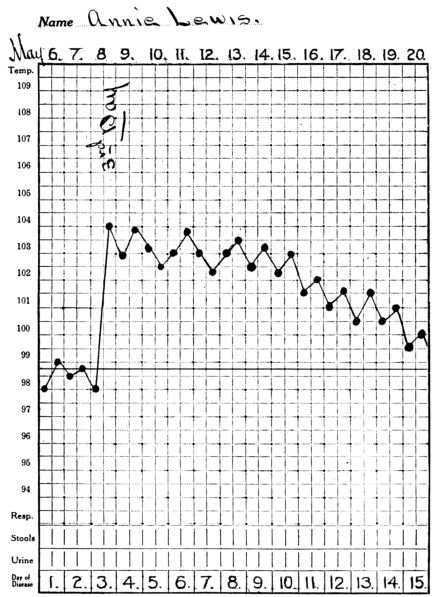
Chart 3.—Chart showing rise in temperature about 3rd day after delivery in a streptococcus infection.
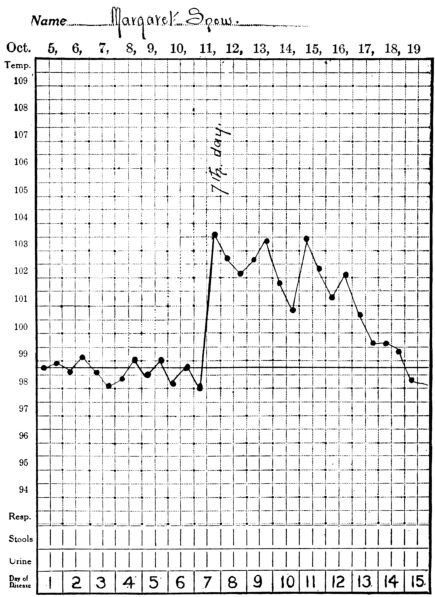
Chart 4.—Chart showing rise in temperature about 7th day after delivery in gonorrheal infection.
In gonorrheal infections the temperature does not go up until later, from the sixth or to the tenth day, as a rule. (Chart 4.) The patient is not usually very ill and generally recovers. But the gonococcus is very likely to produce an inflammation of the tubes and to close up the fimbriated opening. Thus it is impossible for ova thereafter to enter the tube and gain access to the uterus and accordingly the patient cannot again become pregnant. Unlike other infections, gonorrhea is not conveyed to the patient during or soon after labor on instruments or examining fingers, but is already present in the vulvo-vaginal 399glands and from them may travel to the uterine cavity and to the tubes.
Treatment and Nursing Care. Preventive. There is so little that can be done toward curing a patient suffering from puerperal infection that the greatest effort should be made to prevent the disease. The nurse’s part in preventing this complication is an important one and consists of making such preparation for labor that it may be conducted with absolute cleanliness; maintaining the same asepsis during delivery as she would throughout a major surgical operation and protecting the perineum from infection after delivery.
Curative. The curative treatment for puerperal infection resolves itself largely into good nursing care. The patient should be kept warm and quiet and as comfortable as possible; elimination is promoted, her strength is saved and her general resistance increased in every way possible. The head of the bed is frequently elevated, to promote drainage; the windows are kept open to provide plenty of fresh air; the diet is light and nourishing and the patient is encouraged to drink an abundance of water. Ice caps to the head and abdomen are frequently used to make the patient more comfortable; also cold sponge baths when the temperature is high.
A patient suffering from puerperal infection should be conscientiously isolated. If the nurse who cares for her is forced to come in contact with other patients, she should wear gloves and a gown while attending the infected woman and thoroughly scrub and soak her hands after each attention.
It was formerly the practice to curette the patient suffering from puerperal infection, and give intra-uterine douches, but it is now pretty generally believed that neither of these procedures does any appreciable good, but on the other hand may do harm. The objection to curettage is on the ground that by this means the protective wall which Nature has developed to prevent the further invasion of bacteria into the uterine tissues, is removed and a new bleeding area is provided for further and easy development of the inflammation.
Antiseptic douches seem to be useless, for if they are strong enough to be germicidal they are likely to injure the tissues and 400also do harm by being absorbed into the system; while weaker solutions will not destroy the organisms but are likely to carry more infective material up into the uterus. In cases of putrid endometritis, however, if the doctor cleans out the uterus with his finger, a douche of sterile salt solution is often given for the purpose of removing any putrefactive material which may have been left behind.
Phlegmasia alba dolens or “milk leg.” In some cases of puerperal infection, thrombi are formed in the veins of the pelvis, from which particles may be broken off and carried to various parts of the body and cause phlebitis or even abscesses. If thrombi lodge in the large vessels of the thigh, the interference of the venous circulation results in swelling and tenderness of the leg which is often referred to as “milk leg.” This condition is rather rare and does not usually appear until the second or third week after delivery.
The swelling ordinarily starts at the foot and gradually extends up to the thigh. The patient complains of pain in the calf of her leg and she may have an elevated temperature, rapid pulse and the general wretchedness associated with an infection.
The main feature of the treatment is rest in bed; the patient should be kept there for at least a week after her temperature becomes normal; her leg should be elevated, wrapped in cotton batting and the bedclothes held from it by means of a bed cradle or some sort of a light frame. The nurse should never rub the affected leg, and the patient should also be cautioned against this for fear of dislodging a particle of the thrombus and causing an embolism elsewhere, possibly in the lungs. For the same reason, the patient must be warned not to make sudden or violent movements for some time after she is allowed to be up and about, but to walk and move rather slowly. The swelling and discomfort may subside in a few weeks or they may persist for months.
Puerperal Mania. A word about extreme mental unbalance during the puerperium is worth while at this point because the nurse will frequently hear of this distressing condition, and will almost inevitably come in contact with it at some time. It was formerly believed that there were certain mental disorders 401which were peculiar to pregnancy and the puerperium, but this belief has given way before the present knowledge of psychiatry.
The puerperal patient is sometimes delirious and violent for longer or shorter periods of time, but apparently these conditions are due to toxemia or fever, or a mental unbalance has resulted from her reaction to the idea of motherhood, just as it would have resulted from an equal strain of some other character.
In other words, the young mother may suffer mental derangement from the same causes that would produce this state in any other person, but not from causes or conditions which are peculiar to the puerperium.
If the excitement or delirium are due to a toxemia, they are relieved by treating the cause, while from the nurse’s standpoint the care would be the same as for any delirious patient. The patient should not be left alone and she should be protected against doing herself any injury.
A mental disturbance which is due to the patient’s inability to adjust herself to the state of motherhood, and all that that implies to her, is a different matter, and is discussed in the chapter on mental hygiene.
402“Sympathy with, interest in the poor so as to help them, can only be got by long and close intercourse in their own houses—not patronizing—not ‘talking down’ to them—not ‘prying about’—sympathy which will grow in insight and love with every visit.”—Florence Nightingale.
CHAPTER XIX. ORGANIZED PRENATAL WORK. Mortality in Childbearing. Aims of Prenatal Care. Difficulties: Educational, Economic, Social, Professional. Prenatal Work in Other Countries. Progress of Prenatal Work in this Country. The Women’s Municipal League of Boston. Maternity Centre Association of New York. Routine and Methods. Results. The Situation in the Country as a Whole. Prenatal Care in Rural Communities. Forms and Routines used by Maternity Centre Association, New York City.
CHAPTER XX. HOME DELIVERIES AND CARE OF THE YOUNG MOTHER BY VISITING NURSES. Forms and Routines of the Philadelphia Visiting Nurse Society.
The foregoing discussions of prenatal care and the principal complications of pregnancy, and the dangers to which expectant mothers, young mothers and their babies are exposed, bring us sharply face to face with the questions, “What can be done about it?” “What is being done about it?” and, “Is anything more possible?”
We have considered the problem, and the remedy, at very close range; that is, from the standpoint of the individual patient. We are now concerned to know whether or not the remedy, in the shape of care and supervision during pregnancy, may be extended in proportion to the enormous multiplication of the problem, when instead of one patient we must think of millions. In other words, is country-wide prenatal care, with all that it implies, practicable? And if so, by what means or method?
Let us review the problem for a moment, and acknowledge the pathos and tragedy of it.
Child-bearing is so dangerous, under present conditions in this country, that it stands second only to tuberculosis as a cause of death among women between the ages of 15 and 44. The discharge of woman’s supreme function is apparently very hazardous.
Dr. Dublin summarizes as follows the rate at which mothers die throughout the country at large:
406And then, as though in answer to our question, “What can be done about it?” he states that, “among women who receive prenatal and maternal care under skilled direction:
Obviously, then, only a few—too few—American women are receiving the minimum of care that makes child-bearing a reasonably safe adventure.
Perhaps it will be well for the nurse to pause just here for a fresh reminder that the end really to be desired through prenatal care is not so much the mere prevention of death among mothers and infants, as the promotion of health, as well; our charges must be not only saved but saved to mental and physical health, vigor and well-being, capable of being useful, productive citizens. Happily, both life and health are conserved by the same measures, and effort toward either end helps to accomplish both.
Although the inhabitants of a prosperous country like the United States should be a hardy people, the results of medical examinations by the draft boards, during the war, gave us a rude awakening to the fact that they are not.
An appallingly large number of young men who were passing in every day life as normal were found to be physically unfit for military service. And we know that a large part of this unfitness resulted from inadequate care, of some kind, during the weeks and months that comprise the beginning of life.
It can scarcely be doubted that the most critical period in the life history of the individual is the first ten months—the nine months of intra-uterine life and the first month after birth. Good care, then, during this critical period is indispensable in the building of a healthy race. The difficulty in the way of giving this care, at present, seems to be fourfold: educational, economic, social and professional, and may be summed up somewhat as follows:
In many of the large cities women have access to excellent obstetrical and prenatal care; both those who can pay for it and also the poor woman who cannot, though very many in both groups still fail to take advantage of the opportunities that are open to them.
But the city women of moderate means, and those in small towns and rural communities are in general unprovided for. And it is their babies who grow up and later constitute the backbone, weak or strong, of the nation.
Certain foreign countries which have evinced more concern for the welfare of mothers and babies than has the United States have demonstrated that widespread prenatal care is entirely possible and practicable, and they regard it also as an imperative measure toward promoting the national welfare.
The actual origin of this prenatal care is somewhat difficult to locate. There are the consultations for pregnant women instituted in Paris several years ago by Dr. Budin. But Dr. Ballantyne, of Edinburgh, is generally regarded as the father of the prenatal work because of his work on abnormalities of pregnancy and his insistence upon the importance of what might be accomplished through intelligent care and supervision of all women, not alone abnormal cases, throughout pregnancy.
In England for nearly twenty years the supervision and instruction of expectant mothers has been an integral part of the work of midwives who are trained, registered and controlled by government authority. Of late the work among mothers and babies has been so extended that during the war, always a destructive period for babies, the infant death rate was reduced to the lowest figure in the country’s history. This was accomplished partly through a maternity benefit which helped the 408mother to pay for obstetrical care, and partly through indirect government aid, in the form of: compulsory notification of births; a great increase in the number of “health visitors” and welfare centres, and government grants to local authorities which defrayed half the expense of giving prenatal, natal and postnatal care and of instructing mothers in the care of themselves and their babies. Especial effort has been made to help the mothers in rural sections; more small hospitals being maintained, more physicians being provided and assistance given in caring for older children, during the mother’s absence, if she was obliged to go to a hospital at the time of delivery.
New Zealand also has made marked progress in its work of saving the lives and promoting the health of its mothers and babies, having at present the lowest infant death rate in the world. This has been brought about largely through the efforts of the “Society for the Health of Mothers and Children,” an organization employing visiting nurses, called Plunkett Nurses, in honor of the family by that name which has greatly aided the work.
The outstanding features of this work are educational and preventive; the mothers being instructed from early in pregnancy about the care of themselves and the preparation for, and subsequent care of their babies. Prenatal clinics are maintained and the facilities for hospital care are being steadily increased and improved.
One is impressed by the spirit animating this organization, as expressed in a statement of its “functions,” one of which is as follows: “To uphold the sacredness of the body and the duty of health, to inculcate a lofty view of the responsibilities of maternity and the duty of every mother to fit herself for the perfect fulfillment of the natural calls of motherhood, both before and after childbirth, and especially to advocate and promote the breast feeding of infants.” Work based upon such idealism could not but be effective.
The New Zealand undertaking is regarded as patriotic, rather than philanthropic, and mothers who are visited and cared for are accordingly encouraged to pay for this service, if financially able to do so. The Government supervises and warmly supports 409the work of this Society and also aids by enforcing the most perfect system of birth registration in the world, without which the results of the work could not be accurately gauged.
England and New Zealand, as countries, have pointed the way toward accomplishing a nation-wide reduction of maternal and infant mortality and morbidity by making provision for widely organized prenatal care. They recognize the problem as one of public concern. They get at the heart of it: ignorance on one hand and poor or inadequate care on the other. They apply a practical solution, comprising a system of preventive, instructive prenatal care, together with improved and increased facilities for medical and nursing care at the time of delivery and afterward.
This country has been strangely laggard in making widespread, organized effort along these lines, to safeguard its mothers and babies, through prenatal care. But sporadic, volunteer effort has been made in certain cities, and has been crowned with brilliant success.
The first of these attempts in this country was made in Boston, in 1909, with a maternity nurse working under the auspices of the Women’s Municipal League. The work, which was established by Mrs. William Lowell Putnam, was designed to show what could be accomplished by intensive work in a small group of city mothers, and suggest the feasibility of its extension to larger numbers.
“The routine, which has been evolved through a five-year experiment by the Prenatal Committee of the Women’s Municipal League,” says Mrs. Putnam, “has reduced the infant deaths, among those cared for by a third to one-half, as compared with cases not receiving this care. Still-births have been cut in half. Premature births have been reduced to seven-tenths of one per cent. These results were obtained by supervision during pregnancy only, and at a cost of less than $3.00 per patient; an expense which the patients were always encouraged to meet if possible.
“The success of this venture proved to be so satisfactory that the Boston workers have gone still further toward supplying the needs of mothers and babies by adding to the prenatal care, 410care at the time of birth and afterwards until the mother is again on her feet. Through the courtesy of one of the largest Boston hospitals, a clinic is held weekly in its Out-Patient Department. The hospital is in no way responsible for the clinic, simply lending the room in which the clinics are held. The medical care at the clinic and in the patients’ homes is given by obstetricians from the staff of the Boston Lying-in Hospital. Medical examinations are made during pregnancy at the clinic, and a nurse visits and instructs the patient during the period of expectancy, always under the direction of a physician. The delivery is performed in the home by a physician connected with the clinic, at which the nurse also is in attendance. She visits the mother and baby twice daily for three days subsequent to the delivery, gradually making her visits less frequent thereafter. The doctor pays from two to four postnatal visits, as may be needed. For this prenatal, natal and postnatal, medical and nursing care, $40.00 is the entire amount charged, and the work is self-supporting with the nurse’s time filled. Prenatal care, alone, is given if desired by a physician and with visits at the clinic included; the charge for this service is $10.00.”
I refer to the work in Boston, particularly, as its inauguration by Mrs. Putnam marked the beginning of this branch of public-health work in this country, though to-day the same kind of service is available to expectant mothers in many of the large, and some of the smaller cities. Visiting nurse associations, the country over are giving postnatal and infant care (in some instances, excellent prenatal care, too), often providing for or assisting with the deliveries, and effecting an enormous saving of life and health by so doing. But the number of patients who are cared for by each organization is relatively so small that even the aggregate of the work done reaches a pathetically small proportion of the mothers and babies in the country as a whole who need care.
The first comprehensive effort, in the United States, to meet the need of all expectant mothers in an entire community, was inaugurated in New York City, in 1918, by the Maternity Centre Association, the chief function of the organization being to coordinate the work of agencies already in existence.
411This Association was formed as a result of the work of the Maternity Protective Committee of the Women’s City Club and the Maternity Service Association of Physicians and Hospital Superintendents.
The form of organization, purpose and methods of work of this association may be studied with profit, for having been started on a small scale as an experiment, it now constitutes a demonstration of how, through co-ordinated effort, prenatal and obstetrical care may be extended almost indefinitely to expectant mothers in urban districts, and at a low cost.
The purpose and scope of the work are described by Miss Anne Stevens, its former Director, who tells us “that it is the aim of the Association to cover completely the need for maternity care, prenatal, delivery and postnatal, in a given community, by providing for every woman in that community, medical supervision and nursing care from the beginning of her pregnancy until her baby is one month old. This is being attempted, not by establishing another medical and nursing agency, but by establishing a centre through which the maternity work of every hospital, private physician, midwife and nursing agency in the community may be co-ordinated and developed to its fullest extent; a centre at which there will be a complete record of every pregnancy in that district; a centre from which the whole community may be educated to realize the need of and to demand adequate medical supervision and nursing care for every woman and her baby before and after birth.”
It is not, then, an experiment in prenatal clinics, many of which have been conducted, both in New York and elsewhere; but it is an experiment in its attempt to provide adequate care for every pregnant woman in the community from the beginning of her pregnancy until her baby is a month old.
Standards for adequate prenatal care, upon which to base the work, were formulated by the Maternity Service Association of Physicians. The nurses worked with these standards as a guide and gradually developed detailed routines, as a result of frequent conferences over the difficulties and problems arising in the course of their daily work among the patients.
These various adaptations were, of course, approved and 412authorized by the Medical Board of the Association. Because these routines meet the doctor’s requirements so satisfactorily, and have been evolved out of the experience of many nurses, concentrating their best efforts upon this work, they are copied on pages 423 to 436 with the belief that they will be suggestive, and perhaps save time and effort for those who may wish to inaugurate similar work.
Every effort is made by the Association to reach all of the expectant mothers in the ten zones into which, for the purposes of the work, the Borough of Manhattan was divided by the preliminary committee[14] called by Dr. Haven Emerson, who at that time was Commissioner of Health for New York City. This Committee was called for the purpose of surveying the obstetrical facilities of Manhattan, and offering suggestions as to how they might be utilized in an effort to decrease the persistently high infant mortality.
Patients are reported for care by hospitals, dispensaries, clinics, relief agencies, church clubs, settlements and the like and are discovered in various ways by the nurses on their rounds.
The nurse’s first visit to a patient is little more than a friendly one. In fact, she may have to make several such calls before she is able to so far win the patient’s confidence and friendship that she will consent to place herself under supervision. For in addition to obtaining her verbal consent, the establishment of this sympathetic relationship is found to be necessary before the nurse can feel sure that the patient will freely tell of her symptoms and follow the advice given.
Before making plans, or talking to the patient about prenatal care, the nurse ascertains what arrangements, if any, the patient herself has made for care at the expected confinement. She finds that the expectant mothers fall into four groups:
The nurse’s relation to a patient registered with a hospital 413for delivery depends upon the scope of the work of that particular institution. Some hospitals will register patients early in pregnancy, and assume the entire medical and nursing care and supervision from that time until after the baby is born. The Maternity Centre nurse, obviously, has no responsibility for these patients. But she does give nursing care and instruction to patients registered with hospitals which have not facilities for prenatal clinics or visiting nurses to send into the patients’ homes. The hospital resident, in these cases, assumes responsibility for medical supervision of the patients and receives a report from the Maternity Centre upon each nursing visit; and the nurse in turn urges the patient to return to the hospital, periodically, to see the doctor, in accordance with instructions received from the hospital.
This form of co-operation has proved to be so satisfactory that many hospitals now do not wait for the Maternity Centre nurses to discover patients registered with them, but each day notify the nurses of newly registered patients and ask that they be given the routine nursing care and supervision by a Maternity Centre nurse.
When a nurse finds, upon her first visit to a patient, that she has engaged a physician to attend her at the time of confinement, she gives no advice, but sends to the doctor a form letter, prepared by the Medical Board, offering to nurse that patient according to the routine of the Maternity Centre Association if he wishes, and to report to him upon each nursing visit. A very small percentage of physicians refuse this offer of assistance, the majority accepting it with eagerness. Patients who have engaged their own physician for delivery, naturally, are not asked to go to the Maternity Centre clinics for medical examination or advice, but are invited to go for the nurse’s instructions, and to attend the group conferences that will be described later.
If the patient belongs to the third group, having engaged a midwife, the nurse goes in person to see the midwife, as letters are usually of little avail. She asks the midwife to bring her patient to the clinic, explaining that, though midwives are taught to conduct deliveries, they are not taught to make the examinations 414that are now known to be so important to the future welfare of mothers and babies, but that such examinations can be made at the clinic by the doctor. If the initial examination discloses any abnormality, this fact is explained to the midwife and also that the rules governing her practice forbid her caring for such a patient. The nurse, midwife and patient then plan for adequate care at the time of delivery. In this way the nurses win and retain the confidence and good will of the midwives; and since these women exert a powerful influence over their patients and their families, their co-operation is of considerable value in persuading the patients to accept more skilled care than midwives can offer.
If, on the other hand, the initial examination does not disclose any abnormality, the midwife is simply asked to allow the nurse to visit the patient at regular intervals, in a supervisory way, and to have the patient report to the clinic doctor for his periodic observations and advice. The intelligent midwives, who speak English, are usually co-operative, but the others are sometimes suspicious and persuade their patients to refuse the nurse’s supervision.
For the patients in the fourth group, those who have made no arrangement for care at the time of delivery, the nurse is even more responsible. The plans for these patients include three fundamental requirements: a complete physical examination; the correction of physical defects, so far as is possible, and a study of the environment and social status of the patient; this in order to adapt the care during pregnancy and at the time of delivery to each individual’s condition and circumstances.
From time to time the nurse explains to the patient, as much as she can, about pregnancy and the changes that accompany it and the reasons for the advice that is given, in order to secure her intelligent co-operation. Experience has taught that it is not enough to advise the patient to do thus-and-so because the doctor thinks best. But if she understands that examination of her urine, for example, may disclose conditions that can be cured, but which if neglected may cause headaches, or convulsions, she is much more likely to provide a specimen for examination than if she is asked for one without explanation.
415The care of each patient is a tactful adjustment of the prescribed routine to the condition, habits and temperament of that patient. It is carried on through a combination of visits which the nurse makes to the patient’s home and visits which the patient makes to the nurse at the Maternity Centre in her district. The advantages of this combination of visits are, that the nurse first knows the patient in her own home, and can help to plan for the desired care with the conditions of this home in mind, and perhaps evolve from the patient’s simple belongings the equipment needed for her care; also that at the Centre it is possible to assemble the patients and give them a certain amount of informal group instruction. There is at each Centre a doll model of a baby; a model of a baby’s bed (Fig. 144), showing that a box or a basket may be used with entire satisfaction; a model of the mother’s bed, prepared for delivery at home and protected with newspaper pads; a complete layette (Fig. 145) to show the mothers how simple such an outfit can and should be; patterns for making each garment and some one to help the women to make them; a breast tray (Fig. 146) and a baby’s toilet tray (Fig. 147), so complete and yet so simple that no woman with a few chipped or cracked cups to spare need be dismayed.
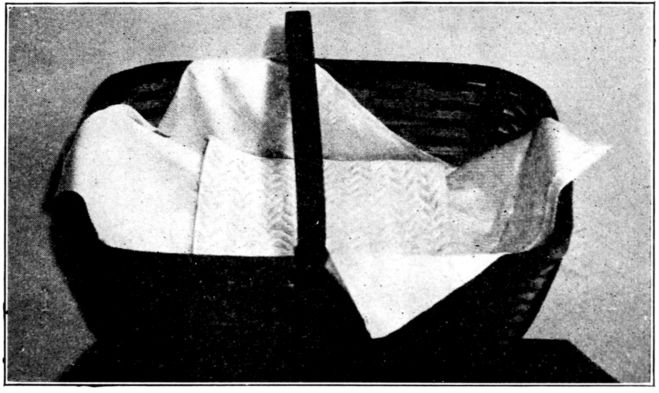
Fig. 144.—Separate bed for the baby improvised from a market basket. (By courtesy of the Maternity Centre Association.)
In the course of this group instruction the women are taught how to prepare for, and later care for their babies. One week, 416the nurse demonstrates to the group how to handle the baby, dressing and undressing or bathing it; or explains the reason for making each article in the model layette, or the purpose and use of each article on the toilet tray, and shows them how to make boric acid solution and swabs. In short, each detail in the care of the baby is gone over. Every alternate week the mothers demonstrate to the nurse. They dress and undress the doll model; explain and demonstrate how to make boric acid solution; how to prepare sterile water and give it to the baby. Many of the mothers attend the classes for several weeks in succession, and frequently a mother returns with her three-week-old baby to make sure that she has not forgotten any of the details of infant care which the nurse tried to teach her before the baby came.
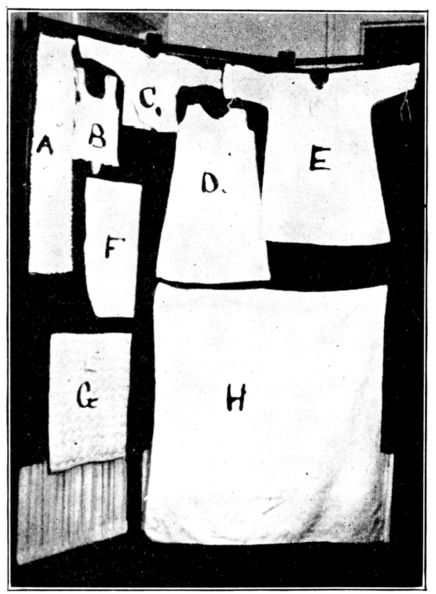
Fig. 145.—Layette recommended to patients by Maternity Centre Association:
A. Flannel binder.
B. Knitted band with straps.
C. Shirt.
D. Petticoat.
E. Dress or nightgown.
F. Diaper.
G. Pad for basket-bed.
H. Flannel square.
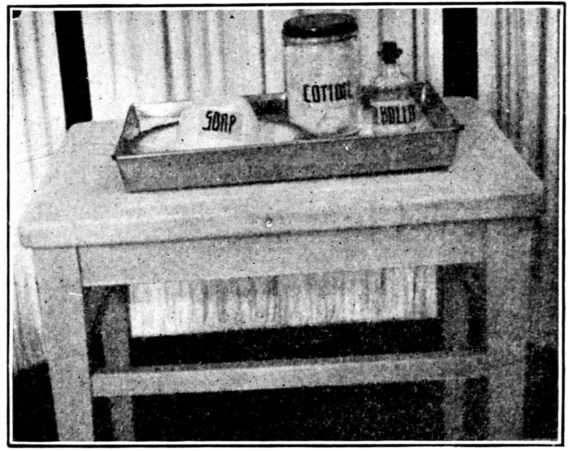
Fig. 146.—Breast tray improvised from articles to be found in any home, contains: Jar of cotton pledgets; bottle of liquid petrolatum; soap on saucer, covered with cup for water to bathe nipples. (By courtesy of the Maternity Centre Association.)
A patient is not asked to go to the Centre for any reason if she seems very reluctant to go; or if her going is inadvisable for physical reasons or if it would entail great hardship, because of young children who would have to be taken with her, or left at home alone. But when they can go, it simplifies the work and enables each nurse to supervise a larger number of patients than if she did all of the traveling and visiting.
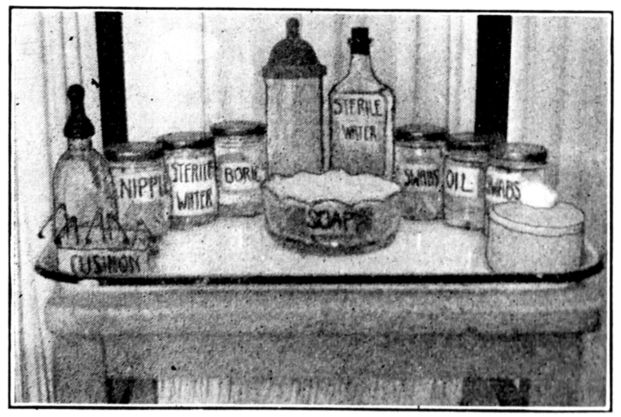
Fig. 147.—Baby’s toilet tray equipped with jelly glasses, bottles, celluloid hair receiver for cotton, and a soap dish, containing:
1. Safety pins sticking in cake of soap.
2. Jar for sterile nipples.
3. Jar of sterile water.
4. Jar of boracic acid solution.
5. Nursing bottle.
6. Sterile water to drink.
7. Nursing bottle for water.
8. Small tooth pick swabs.
9. Liquid petrolatum.
10. Gauze mouth swabs.
11. Absorbent cotton.
12. Soap.
(By courtesy of the Maternity Centre Association.)
418Each patient is seen by a doctor or a nurse every two weeks until the seventh month of pregnancy, and once a week after the seventh month. At each visit the nurse follows as much of the prescribed routine as is possible; this routine consists of testing for albumen in the urine; taking the systolic blood pressure; listening to the fetal heart; questioning the patient and looking for the objective symptoms of complications. During these visits to the homes the nurses are able also to help their patients assemble entirely satisfactory outfits for the care of their nipples, consisting perhaps of jelly glasses, cheese jars, or handleless cups. And they help to find a place on the shelf where this little equipment may be kept undisturbed and always ready for use. When it comes to the measuring of urine, they explain that the regular size tomato can holds just a quart, and is therefore quite as satisfactory for that purpose as a costly graduated glass measure.
No patient is dismissed for failure to follow advice; the nurse continues her visits, unless the patient positively refuses to admit her, and she continues to advise, adjusting and modifying the ideal routine and persuading the patient to do as much as she can, or will.
If abnormalities develop during pregnancy, the nurse arranges for immediate medical care, either at the patient’s home or in a hospital. If the clinic doctor feels that the patient should have hospital care, but she will not or cannot go to a hospital, she is persuaded to engage a doctor, and a nurse from the Centre helps, as a visiting nurse, to take care of the patient in her own home.
The next responsibility of the nurse is to advise the patient in arranging for care at the time of delivery, this advice being based upon the patient’s physical condition, the circumstances of her home life and the available facilities for care. Although hospital care may be the ideal for all patients, from an obstetrical standpoint, the mother cannot always be removed from her home with safety to the family circle. Her physical and social conditions therefore are considered together; if there is no complicating home problem, it is usual to advise hospital care for primiparæ and for all patients who have, or develop 419abnormalities, or have a history of previous difficult labors, complications or abnormalities.
Patients who, the doctors think, give promise of having complicated labors and who prefer to remain at home are advised to engage a doctor, and to arrange with the Henry Street Settlement for nursing care at the time of delivery and during the puerperium, as the Maternity Centre nurses do not perform this service.
At one time, however, the Centre provided assistance to patients delivered at home, in the shape of a working housekeeper to discharge the mother’s household duties while she remained in bed the necessary length of time after the baby was born, or in some cases, while she took much needed rest during the latter part of pregnancy. For this purpose the nurses had a list of women who were good housekeepers and clean workers and whose own children were partly grown. These women were glad of an opportunity to do part time work and earn a little extra money. They were paid thirty cents an hour, twenty-five cents for lunch and whatever their carfare amounted to, the patient paying whatever she could afford toward the fund, provided by the Women’s City Club, from which these working housekeepers were paid. This service, which in no wise replaced the nurse’s care, has been temporarily discontinued because of lack of funds, but proved to be so valuable that it will be resumed as soon as possible.
Supervisory postnatal visits are paid to patients, not under the care of the visiting nurse service, who have been under Maternity Centre Association care during pregnancy, as well as to those who have not had this care but are referred to the Centre, by hospitals, upon their discharge. The nurse first visits to satisfy herself that the mother is able to care for her baby and to give any instructions that seem to be necessary. She then visits the patient, or the patient visits the nurse, when she is able, until the baby is a month old, when she is urged to register the baby at a baby health station.
The importance and value of birth-registration is explained to the mother and the nurse endeavors to have a copy of a birth certificate in the mother’s hands before the case is dismissed.
420The importance of post-partum examinations, not later than six weeks after delivery, is also impressed upon the patient. Patients who are not to be examined by the doctors who delivered them are given a post-partum examination by a doctor at the Maternity Centre, to make sure that they are dismissed in good condition, or are referred to the proper agency for further care, this being the first step in prenatal care for the next baby.
Is all of this elaborate organization and detailed care worth while?
A recent statement issued by the Maternity Centre Association replies convincingly that it is. It says that during 1920 among women in the Borough of Manhattan not under Maternity Centre supervision:
Whereas, among women in Manhattan who were supervised by the Association, during the same period:
The Association does not usurp nor supplant, but endeavors to give impulse to public and private agencies alike in affording the best possible supervision and care for expectant and parturient mothers and their babies.
Thus has the stupendous problem in New York been attacked with courage and with gratifying results. Much might be accomplished in smaller and less complex communities with proportionately less difficulty.
But all of the foregoing relates to city dwellers. What about the expectant mothers in isolated and rural communities?
I wish we did not have to say.
Prenatal care is practically unknown among them and there is scarcely any provision for obstetrical care, either. The nearest physician may live miles away and even though one were near, 421country women and their husbands do not always feel that the expense of employing a doctor, for mere childbirth, is justifiable.
In certain Northern and Western communities, that were considered fairly representative of those sections, conditions have been studied at some length by agents of the Federal Children’s Bureau. They found that about half of the mothers in those communities had no medical attention whatever in childbirth. Untrained women, friends or neighbors, frequently someone’s grandmother, were in attendance. Or husbands or workmen were pressed into service. A few women were entirely alone in their hour of trial. Scarcely a mother among them received prenatal care and instruction worthy of the name.
In the Southern states, the proportion of women delivered by physicians seems to be even smaller than in the North and West, and in some of the mountain regions the conditions are distressing. From one such locality we learn that when a woman goes into labor the first passing teamster is hailed, or perhaps a member of the family hurries down the road for the nearest tanner or blacksmith, or any one else, who in total ignorance will fearlessly rush in to meet the great emergency. The results of this practice—dismembered infants and badly injured or dead mothers,—are too sickening to describe, but may be imagined by any nurse who has seen good obstetrical work and appreciates its value.
From another mountain region in the South comes the contrast in accounts of the work done by Miss Lydia Holman, founder of the Holman Association, as evidence of what skill and desire may accomplish. Something more than twenty years ago this nurse started volunteer visiting nursing among the mountain people, with no precedent to follow and no Board to direct or advise. But there were sick people all about, people needing care, and Miss Holman was not only trained but eager to nurse them, and after all these qualifications are the chief requisites.
After all these years of self-sacrificing, pioneer work, of which American nurses may justly be proud, Miss Holman has the enviable satisfaction of knowing that she has lessened the perils of childbirth for some 600 women and saved practically all of their babies. Much of this in the simplest, most meagerly 422equipped mountain homes. She has even managed to have some of the mothers taken to a nearby town for the repair of lacerations which occurred during labor. And she has a little hospital now up on the mountain top, with doctors and nurses, not only caring for sick people, but, among other things, teaching women and girls how to care for infants and children.
A complete maternity service for rural communities would evidently include small hospitals for primiparæ and abnormal cases and to serve as centres from which nurses and doctors would carry on prenatal supervision and instruction, and give skilled attention at birth; followed by visiting nursing of the young mother and her baby. The prenatal supervision in sparsely settled districts might leave much to be desired, because of the impossibility of seeing each patient as often as is wise. But even a little care would be an improvement upon present conditions. In some localities, it has been found possible to teach some of the more intelligent of these rural mothers a good deal about their own supervision. One nurse tells of a very isolated woman who could only be visited at long intervals whom she taught to test her own urine for albumen, explaining its possible significance and seriousness. One day the report card that came by mail indicated that the last test showed albumen. But the card also carried the remark, “Don’t worry about this. I am drinking lots of water, taking nothing but milk for food and will be in to see the doctor on Tuesday.”
This hints at some of the possible adjustments that must be made in meeting the needs of the patient in unusual circumstances. For we are constantly facing the unalterable fact, that no matter where she is, nor what conditions surround her, the individual woman needs care and supervision, and though conditions vary, the general needs of expectant mothers are the same.
This survey of the situation in cities and rural communities gives us a glimpse of what can be done about it—this problem of mothers and babies who need care—and also what is being done, and we begin to sense an answer to the question, “Is anything more possible?”
It is clear that a wide extension of provisions for prenatal 423care is necessary if all mothers are to be reached; rich, middle-class and poor; in cities, small towns and rural districts alike. We believe that it is possible; and we are sure that wherever provision for prenatal care is made, the achievement of its fine purpose will depend very largely upon the spirit of the individual nurse.
What does it bring to the individual nurse—this survey of the problem as a whole, with the suggestion for its possible solution? The appeal of not a few mothers and babies, only, but of a legion, and of uncounted homes and family circles in danger of being broken. And it brings a suggestion of the immeasurable comfort and influence which the maternity nurse may carry into each home that she enters. For she helps to save lives and health, and through them, homes and family groups, and these are the building blocks of the nation.
For the nurse whose imagination is touched by this appeal, it will exact much—the best and most that she has to give—but in return she will find a deep and enduring satisfaction in her work.
ROUTINE FOR PRENATAL VISITS:
First Visit.—Get acquainted with the patient and get her confidence. Learn if she has made any arrangements for her care at time of delivery. If a doctor or midwife has been engaged communicate with him or her. If the patient is registered with a hospital, or is under other nursing care, note that on your record, also on slip sent to Central Office. Always ask to see patient’s hospital or clinic card, or any card which she may have been given by any nurse or other visitor. Give patient pink card.
Explain simply the reason for an expectant mother seeing a doctor and nurse early and regularly. Invite the patient to come to the Center. Ask her in a general way about herself, when the baby is expected, other pregnancies and deliveries, and illnesses; other members of her family. Direct your conversation so as to get as much data as possible without asking a direct question. Do not attempt a full nursing visit unless the patient meets you more than half way. Every patient is to be encouraged to come to the Center for as much of the nursing care as is possible for that individual woman. In the care of all patients it is the nurse’s responsibility to make every effort to solve (by working 424with every existing agency) such home problems as might effect the health of the mother or baby or disturb the mother’s peace of mind.
Complete Nursing Visit.—Ask the patient about any aches, pains, troubles of any kind, directing your questions to cover all items on record. Select a table, chair, machine top, or end of mantel, to use as work table, and place on it:
Take temperature, pulse, respirations and blood pressure (to take blood pressure adjust sleeve, get radial pulse, pump until obliterated, let out air and read dial at moment pulse returns. See Tycos Manual, sample No. 2, for full detail.) Wash thermometer thoroughly with soap and water, dry and return to case. Scrub hands. Inspect or demonstrate the care of nipples; to be done daily after the fifth month, not before. Use cotton ball (or soft toothbrush previously scalded and kept for this purpose). Thoroughly scrub each nipple with warm water and white soap and dry with a clean towel. Apply albolene, pulling out the nipple. Do not handle breasts. Listen to the fetal heart. If unable to hear make note on record n.h. If fetal movements are felt by nurse put an “x”; if patient says she feels the baby move, put “xx” in space on record for recording fetal heart rate. Look for edema, varicose veins; do not take the patient’s word for these symptoms. Apply bandage for varicose veins (patient to pay 70 cents for bandage, or bandage to be lent to patient as long as needed, to be washed and returned), and teach patient right-angle position. Get specimen of urine, either to take to the station for examination or to examine at once for specific gravity, reaction and albumen, in accordance with instruction given on page 30, Laboratory Technique—Wood, Vogel and Famulener. Have the patient cleanse vulva before voiding, and void in clean vessel. Teach patient proper disposal of urine, emphasizing why kitchen sink is not to be used. If any abnormality in amount, color, specific gravity, or trace of albumen, report to the doctor, midwife or hospital in charge of the patient, if the patient has engaged one; if not, use every effort to get the patient under care of doctor.
Teach patient to measure amount of urine voided in 24 hours. Tell her to void in toilet on getting up in A.M.; then for the rest of that day and night and the following A.M. to void in a suitable vessel and measure in a tomato can (if no suitable vessel, void in a tomato can) and keep count of how many times she fills the can.
425On an early visit examine teeth and show how to keep clean. Where possible urge a visit to the dentist or dental clinic for prophylactic treatment. Explain that it is not wise to have extractions done during pregnancy without consulting a doctor, but that cleansing and temporary fillings may be done with much saving of teeth.
On one visit, as early as possible, ask to see the layette, and advise about it, going over the list of baby supplies. Urge the patient to visit the center to see the model layette, and get help in the choice of materials and patterns. Note on the record if layette is not complete by the eighth month. Demonstrate the preparation of bed for the baby, made from clothes basket, soap box, or in a baby carriage similar to the model at the center. If the patient is to be delivered at home, some time after the seventh month ask to see the mother’s supplies, going over the list. The patient should be advised against the use of oilcloth from the kitchen table as a bed protector, and especially urged to prepare newspaper pads like the model at the center. Note on the report if the mother’s supplies are not complete by the eighth month. Advise about the arrangement of the room for delivery, and demonstrate the preparation of the mother’s bed like the model at the center.
No treatment or medicine to be advised except in accordance with standing orders, private physician’s orders, hospital orders and Maternity Centre Association routine (note on record which).
Form letter signed by the head of the medical board sent to doctors who have been engaged by patients for delivery:
My dear Dr. ......:
Mrs. ...... who has engaged you for her care at delivery, has been referred to this association for nursing care.
In order to make the work of the nurses of this association of a uniformly high standard, the Medical Board has adopted the enclosed routine for the nurses to follow.
May we not have your cooperation in our effort to teach the women of the community the need for, and value of, medical supervision throughout their pregnancy?
May we have your permission to instruct our nurses to visit Mrs. ...... in accordance with our routine, and report each visit to you?
A prompt reply on the enclosed slip will be greatly appreciated.
The Maternity Record upon which a complete history of each case is recorded is divided into four parts, the first section for the social data about the patient, the second for other pregnancies and observation of patient during this pregnancy, the third records delivery and postpartum care, the fourth, post-natal care. (See insert for form.)
Motherhood is natural and normal. If you do as the doctor and nurse ask you to, you have no reason to worry about having your baby.
Eat the food you are used to. Do not eat what you know gives you indigestion. Do not eat too much at any one meal.
Drink 8 glasses of water every day.
Drink all the milk you can.
Do not drink any beer, whiskey, wine or other alcohol. These hurt the kidneys and thus may poison the baby.
Eat meat, meat-soup or eggs and drink tea or coffee only once a day.
At least 8 hours every night with windows open.
Do your regular house work, but lie down several times a day, if only for five minutes. If possible take a walk out of doors. Fresh air is good for your baby. If you cannot get out, keep the windows open while you work indoors. Do not do heavy work; it will hurt your baby.
Wash all over every day with warm (not hot) water, but do not get into a tub after the seventh month.
Do not wear round garters or any tight bands. The nurse will show you how to make suspender garters.
If you are constipated, drink a cup of coffee (no cream or sugar) before breakfast, hot milk (not boiled) with breakfast, go to the toilet at the same time every day (after breakfast best). During the day eat coarse bread, green vegetables, stewed fruit, drink no tea, but all the water you can, at least 8 glasses, hot or cold. Cook 2 tablespoonfuls of senna leaves with a pound of prunes and eat four to six prunes every day. If you have hemorrhoids (piles) hold a cold compress to 428anus for five minutes after bowels move and do not let yourself get constipated. Never take any cathartics unless your doctor, midwife, or nurse tells you to.
Do not have any sexual intercourse after the 8th month. If you have severe headache, vomiting, spots before your eyes, if your face, hands or feet swell, let your hospital, doctor or midwife and nurse know at once.
Labor begins with pains in back or abdomen; with bleeding or watery discharge. If you have any labor pains or bleeding before the time you expect your baby, go to bed and send word to your hospital, doctor or midwife and nurse at once.
If you are going to the hospital, have ready after the 8th month one set of baby clothes, to take with you to put on the baby when you bring him home. Do not take anything else with you, the hospital will supply all you need. As soon as labor begins, go to the hospital.
If you are to be confined at home, as soon as labor begins send for the doctor or midwife. If the doctor is one of the hospital doctors, follow the directions on your card from the clinic.
While waiting for the doctor, boil a large quantity of water in a covered vessel and set aside to cool. Prepare your bed as the nurse has shown you, take a warm sponge bath, braid your hair in two braids, get out a set of baby clothes ready for the nurse to dress the baby. Get out supplies needed for yourself.
The bed pads are made from 6 thicknesses of newspaper open to full size and covered with freshly laundered old muslin tacked in place. No other protection for bed is necessary. As a precaution, when possible, the entire mattress may be covered with oilcloth put on under the bottom sheet. See model at center. All washable supplies for mother and baby should be freshly laundered and put away in pillowcases or clean, ironed paper until they are needed.
The following is a list of the complete outfit of baby clothes and toilet necessities. It may be modified as to material, quantity and quality to suit the individual taste and pocketbook.
Tray—fitted with:
The nurse is urged so to conduct her clinic as to assure privacy to each patient examined, and the same treatment which the patient would receive if she were the only patient in the office of one of our best obstetricians.
Nurse is to wear her graduate uniform during clinic and during her office hours.
Nurse’s Duties
1—Preparation of Clinic Room
Pads of doctor’s record, return visit to doctor, post-partum examination; pencil; examining table; side tables; sterilizers; basins; instruments; supply of clean dry gloves; Department of Health material for taking Wassermanns, cultures and smears; cotton balls; tampons; throat sticks; sheets; pillow cases; sounding towel; adequate supply 430of clinic drugs; solutions; thermometer, in glass of 50 per cent alcohol; glass of cotton; to be ready one-half hour before the time set for clinic.
2—Preparation of Patients’ Dressing Room
Screens or curtains arranged to form individual dressing rooms; a sufficient number of clean clinic gowns; separate chair provided for each patient to leave clothes on, unless room is provided with racks or hooks.
3—Preparation for Urinalysis
Unless the urinalysis is made so near the toilet that the waste urine may be thrown directly into the toilet, a covered pail is to be provided one-fourth full of 1 per cent lysol solution. All waste urine and washings from the test tubes to be thrown into this pail, and under no circumstances is waste urine to be thrown into any sink or wash basin, even though the basin is not used as a wash basin.
Test tubes, sterno, litmus, acetic acid, funnel, filter paper, test tube holder, vessel for collecting specimen, basin of 1 per cent lysol solution and cotton balls for patient to cleanse vulva before voiding, basin for used cotton balls, provision for patient to wash hands, to be in readiness one-half hour before the time set for clinic.
4—Preparation of the Patient for Examination
Each patient to completely undress, except her shoes and stockings, and to put on clean gown supplied by the clinic. Her shoes to be unfastened so that the doctor can examine her ankles for edema, her temperature to be taken and a urinalysis made before the patient is seen by the doctor.
5—Assisting Doctor in Examining Room
Make notes on record pad at the doctor’s dictation, reminding her tactfully of any omissions made in her dictation. Conduct examination in the following order: Head, chest, breasts, blood pressure, abdominal, fetal heart, measurements, ankles, vaginal, Wassermanns or smears when necessary.
Note: Preparation for vaginal examination. Sponge vulva with 1 per cent lysol solution. Give doctor fresh gloves for each patient.
The nurse is responsible for the technique in the clinic room, not the doctor.
If the doctor wishes to do a vaginal examination on a patient more than eight months pregnant, or one who is bleeding, take same precaution as though examining a patient in labor; clip; scrub with green soap and water; then 1 per cent lysol; give doctor freshly boiled, sterile gloves.
6—Arrangement of Examining Room After Clinic
Soiled linen in laundry bags; fresh linen on tables, tables covered; all used instruments to be washed, scrubbed when necessary, boiled five 431minutes, dried and put away; all gloves used to be washed in cool water and green soap and thoroughly rinsed, wrapped in towel, dropped in boiling water and boiled for five minutes, then dried, powdered and put away in a clean towel ready for use at next clinic; solution basins to be emptied, washed and dried; all waste to be securely rolled up in newspaper and put in a house garbage can; supply of drugs to be checked up and replenished when necessary.
7—Records
All “Doctor’s Record” cards to be written up and filed; reports mailed to the central office; reports on the condition of patient sent to nursing agencies caring for the patient and other agencies working on the case; maternity records to be filed in date file before the nurse goes off duty.
Doctor’s Duties as Outlined on Doctor’s Record
8—Duties of Clinic Assistants
At those clinics where a lay woman acts as assistant to the nurse, the following duties (and no others without special permission) may be assigned to the assistant:
Requirements:
Room for examining, and dressing room, screens, running water, gas, near a toilet, urinalysis facilities, good light,
| Chair | 1 |
| Desk | 1 |
| Blotting pad | 1 |
| Blotter | 1 |
| Ink-well | 1 |
| Penholder | 2 |
| Pens, | |
| Erasers, | |
| Ink | 1 |
| Pencil | 1 |
| Red Pencil | 1 |
| Rubber bands | |
| Office: | |
| Clips | |
| Ruler | 1 |
| Waste basket | 2 |
| Hand blotters | 12 |
| Ink, Red and Black | |
| Charities Directory | 1 |
| Map of Manhattan in Sanitary areas | 1 |
| Report on vital statistics | 1 |
| Babies’ Welfare directory | 1 |
| Guide Cards Baby Health Station | 1 |
| Examining Room: | |
| Table | 1 |
| Pad | 1 |
| Pillow | 1 |
| Foot bench | 1 |
| Shelves or side table for supplies, etc. | 1 set |
| Garbage pail | 1 |
| Pelvimeter | 1 |
| Tape measure | 1 |
| Stethoscope | 1 |
| Tenaculum | 1 |
| Scissors | 1 |
| Bivalve speculum | 1 |
| Uterine Dressing Forceps | 1 |
| Blood Pressure machine (Tycos) | 1 |
| Thermometers | 3 |
| Thermometer Glasses (1 for cotton) | 2 |
| Enamel jars for tampons and pledgets | 2 |
| Large basin | 1 |
| Small basin | 1 |
| Erlenmeyer flasks for green soap and Lysol | 2 |
| Medicine Glass | 1 |
| Hand Scrub | 2 |
| Rubber gloves, No. 7½ | 6 pr. |
| Absorbent cotton | 1 lb. |
| String | 1 ball |
| Spatulæ | 100 |
| Hemoglobinometer (Tahlquist) | 1 |
| Needles (skin) | |
| Wassermann Set from D. of H. | 1 |
| G. C. Smear Set from D. of H. | 1 |
| Culture tubes from D. of H. | |
| Bandages (Ace) | 6 |
| Sterilizer | 1 |
| Sterilizer burner | 1 |
| Metal Shelf or table for Gas sterilizer | |
| Scott Tissue Towels | 6 |
| Urinalysis outfit | 1 |
| Test tube rack | 1 |
| Test Tubes | 12 |
| Test Tube holder | 1 |
| Urinometer | 1 |
| Sterno | |
| Matches | |
| Enamel Measure | 1 |
| Dish (Chamber) | 1 |
| Litmus | |
| Acetic Acid 2% | |
| Toilet paper | |
| Funnel | 1 |
| Filter paper | |
| Covered pail | |
| 433Linen: | |
| Sounding towels (for use in listening to F. H.) | 6 |
| Sheets | 6 |
| Pillow cases | 3 |
| Doctor’s gowns | 2 |
| Dusters | 6 |
| Gown’s for patients | 12 |
| Covers for tables | q.s. |
| Laundry bags | 2 |
| Towels | 6 |
| Sewing Bag: | |
| Cotton 70 | |
| Cotton 30 | |
| Needles, assorted | |
| Thimble | |
| Tape measure | |
| Tape | |
| Safety Pins | |
| Plain Pins | |
| Drugs: | |
| K Y | |
| Lysol | |
| Green soap | |
| Boro Glycerin | |
| Alcohol | |
| Iodin | |
| Albolene | |
| Breast Tray: | |
| Castile soap in dish | |
| Small bowl | |
| Bottle of albolene | |
| Jar of cotton balls | |
| Soft toothbrush | |
| Exhibit on Table: | |
| Patterns for baby clothes. | |
| Complete layette. Slip and petticoat open in back. | |
| Basket for baby bed. | |
| Pad (of felt or hair mattress). | |
| Rubber. | |
| Pillow cases. | |
| Blanket (crib). | |
| Doll (baby) dressed. | |
| Suspender garter for mother—abdominal support with garters. | |
| Patient’s bed prepared for time of delivery, newspaper pads. | |
| Toilet Tray: | |
| Jar of boiled water (for washing mother’s nipples). | |
| Jar of oil (mineral oil best). | |
| Jar of boric acid—2% for baby’s eyes. | |
| Jar of breast swabs. | |
| Jar of small swabs. | |
| Absorbent cotton in container (hair receiver). | |
| Soap in dish. | |
| Soap with safety pins, instead of pincushion. | |
| Jar for clean nipples. | |
| Bottle and nipple, or cup and spoon for giving baby water. | |
| Bottle of boiled water (day’s supply boiled fresh each day) and kept corked. | |
| Newspaper cornucopia for waste. | |
434Contents of Nurse’s Bag:
Any nurse may remove from her bag any article not necessary in her district or for any one day’s work, provided she makes note of same on card, which is left in bag pocket, stating where removed articles may be found.
These standing orders may be used at the discretion of the nurses when a patient is under no other medical supervision. When patients are registered with a midwife, may be used with her consent.
Ante-Partum Orders
Post-Partum Orders:
Post-Natal Orders:
Hospital Cases
See patient as soon after she is dismissed as possible, to make sure she understands how to care for baby. Urge her to take baby to nearest baby health station (see Blue Card) when baby is three weeks old. Telephone health station to see if she does register. Urge her to bring baby to your own station when one month old. At that time arrange for post-partum examination: if it is the practice of the hospital, at which the patient was delivered, to instruct patient to return for post-partum examination, urge her to go at time set by hospital; if not, urge her to come to your station for such examination. If she fails to come, visit her to learn condition of baby, and to urge post-partum 436examination. If during the post-natal follow-up work, any abnormality is discovered in baby or mother, report that at once to the resident of the hospital, where patient was delivered, and carry out his orders as to whether patient is to return to him or be referred to gynecological or baby clinic.
Patient Delivered at Home
Urge all pre-natal cases to send you post card when baby is born. When postal is received, visit as soon as possible to see that everything is all right; arrangements made for care of home and children so as to keep mother in bed proper time, etc. If a Henry Street nurse is doing post-partum bedside nursing, make no other visit but urge mother to bring baby to see you at station when the baby is one month old. If a practical nurse or a midwife case, visit every day or so, but do not interfere with her conduct of the case. If you find it necessary to report any irregularity to the Department of Health communicate with the midwife before doing so. After she has dismissed the case follow the routine outlined above. Make special effort to get all midwives’ cases to come for post-partum examination, and also private physicians’ cases if they dismiss case before baby is six weeks old.
The preventive value of post-partum care is now so generally recognized that maternity care by visiting nurses is given not only in the larger cities, but is being extended even to rural communities. The routine of the Visiting Nurse Society of Philadelphia, under the direction of Miss Katharine Tucker, may be taken as an example of effective post-partum care, in which daily visits by a nurse bring to large numbers of patients the minimum of necessary attention. As the same kind of work is effective and possible in smaller communities, the routines and instructions used by the Philadelphia Society are reproduced on pp. 439 to 445. These include
In normal maternity cases, a visit is made once a day for eight days. After that time, if the mother is up and about and the baby is in good condition, the nurse visits at least once a week for supervision until the fifth week, when the case is transferred automatically to the Child Welfare Nurses under the City. If, however, there is any complication with either the mother or baby, the nurse continues daily visits or twice daily as indicated by the condition, until both mother and baby are normal. Instruction to the mother in the care of the baby is one of the important phases of the maternity nurse’s program.
The points observed and recorded on the bedside cards are: condition of breasts, urination, condition of bowels, character of lochia, position of uterus, T.P.R. or any abnormality. If there is any rise in temperature or other abnormality noted, the physician is called by telephone and the situation reported.
438Any one can call the nurse—children, husband, neighbor, doctor, social worker,—and a nurse is sent out on every call. A doctor must be in charge of every case, and if one has not been engaged when the nurse gets there, she sees to it that one is procured. The only exception is in cases delivered by midwives, in which instances the nurse gives any necessary care and supervision, having it clearly understood that if any abnormality occurs, she will first notify the midwife and then the midwife or the nurse will immediately call a doctor.
The doctor ordinarily brings his own equipment for delivery. The contents of the nurse’s bag is the same for delivery as for post-partum care, except for the addition of the nurse’s gown, extra towels and silver nitrate. Perineal pads, cotton, boric solution, etc., are supplied at cost, or free of charge if the patient is unable to pay. Bed linen, nightgowns, layettes, etc., are provided for patients who cannot procure them.
The cost per visit to maternity patients averages one dollar and the cost for services at the time of confinement averages five dollars. Miss Tucker says of the maternity work:
“A complete maternity service which includes prenatal work, service at time of confinement, post-partum care and subsequent supervision of mother and baby is essential if adequate results are to be accomplished. Anything less than this complete service does not give full protection to the life of the mother and the baby. The Philadelphia Visiting Nurse Society has found that the inclusion of service at time of confinement has given a tremendous stimulation to both their prenatal and postnatal service. In the branches where a delivery service has been added, the prenatal service has increased fourfold. Both doctors and patients are enthusiastic and see far more reason for instruction and supervision from a nurse who is going to see the case through than from one who drops out at the crucial moment. It certainly has strengthened our whole maternity service, both as to results accomplished and in our relationship to the doctor and to the community.”
1. Uniforms.
Except in the case of substitutes during their first six months and staff nurses during their probation period, all the nurses are required to wear the uniform of the Society.
2. Bags.
440Lost articles to be replaced at the expense of the nurse.
New equipment may be obtained only in exchange for the worn-out one.
Notebooks, charts, other papers, and pencils to be kept in the long pocket.
Instruments to be boiled before and after dressings.
Brush to be boiled twice a week and after all infectious cases.
3. Thermometer Disinfection.
To be washed before and after using in running water if possible.
After using wrap in cotton soaked in alcohol and leave until the work is finished. Then wash with green soap under running water.
4. Routine in the Home.
General Care:
Partial Care:
Extra articles to be carried in bags: gown, 2 towels, clamps, 2% silver nitrate solution.
The doctor should be called at the same time as the nurse. This should be ascertained when call is taken over telephone.
If the nurse arrives first, she should judge from the progress of labor whether an urgent call should be sent for the doctor and how much time she will have to spend in preparation for the delivery. Unless directed otherwise by doctor, the nurse should proceed as follows:
Have a supply of boiled water and pour some in covered vessel to cool.
Take necessary articles from bag, wash hands, put on gown.
Prepare patient by giving enema, sponge bath, braiding the hair, putting on clean white stockings and a gown which can be rolled up around waist.
Make bed with tight sheet, oilcloth and draw sheet, protect with pads made of many thicknesses of newspaper, covered with old muslin.
Protect floor with newspapers, and place basin for placenta. On 442bedside table, place alcohol, green soap, glass of boric acid solution, silver nitrate, basin containing scissors, clamps, catheter, medicine dropper, cotton gauze, cord tape and dressing, perineal pads, hypodermic, thermometer. Basin of lysol within reach. Prepare a place for baby by covering pillow with blanket and placing hot water bottle. Have olive oil (warmed). Get baby clothes, also gown and binder for mother.
Scrub hands and cleanse patient locally with green soap and water and put on sterile pad.
Assist doctor in any way possible during delivery.
Ask doctor whether he wishes to instill silver nitrate into baby’s eyes. This should be followed by normal salt solution and boric acid.
After delivery, cleanse vulva with warm lysol, put on fresh pad and binder, and make patient as comfortable as possible, giving her something hot to drink.
Weigh, oil, cleanse, dress baby. Unless doctor orders otherwise, instruct mother to nurse every three hours and to cleanse nipples with boric acid solution before and after nursing. The following additional information is to be written on the medical history card of patient attended at delivery:
This technique is given as a general standard but the nurse is expected to use her own discretion in adapting it to the condition of patient, the home surroundings and the wishes of the doctor.
Care of the Baby:
A. Make preparations as for general care.
Have everything ready before the baby’s bath.
Have separate basin for the baby whenever possible.
Test temperature of water with the elbow.
If the room is cold bathe in the kitchen.
Use table whenever possible for the baby’s bath.
If not possible sponge on lap beside the mother’s bed so that she can observe technique.
When cord is off, tub.
Place on paper napkin on third chair, table, or corner of dresser, 443glass of boracic acid sol., olive oil, warmed, cord powder, and dressings, safety pins, band, absorbent cotton, rectal thermometer, vaseline and alcohol. Have baby’s clothes within easy reach. Protect lap with blanket or bath towel.
Remove clothing.
To protect cord dressing, unpin but do not remove band.
Take temperature first and last visit, and when indicated.
Weigh baby on first and last visit.
Examine carefully for any abnormalities and note when found.
B. Eyes.
Unless there is a secretion, let the eyes alone.
When secretion or redness, wash eyes gently with 2% Boric acid sol. using separate pledget for each eye.
C. Mouth.
Examine mouth.
No treatment unless required.
If necessary to cleanse use cotton wrapped around little finger and dipped in boracic acid.
D. Nose.
No treatment unless required.
If necessary use piece of twisted cotton and boracic acid sol.
Never use toothpicks.
E. Wash face and ears gently with wash cloth or absorbent cotton and dry.
Soap head with hands, rinse with cloth and dry carefully. Soap body with hands, rinse with cloth and pat dry with soft towel. Fold binder across abdomen, protect with hand and turn baby on stomach. Bathe the back. Fold diaper and place under buttocks.
F. Genitals should be carefully cleansed.
In the case of boys, the foreskin should be gently pushed back once in every two or three days, and the parts underneath bathed carefully with absorbent cotton and boracic acid sol., removing the white pasty material which causes irritation.
In the case of girl babies, carefully bathe genitalia. If deposit is difficult to remove, soften with olive oil.
G. On first visit wash umbilicus with 70% alcohol and apply dry sterile dressing. Do not remove this dressing except when soiled. After the first time dress with cord powder. Put on clean binder, pinning on side with safety pins. Oil under arms, buttocks and all creases.
Put on shirt.
Pin diaper.
Petticoat and dress should be drawn on over the feet.
Use hot water bottle filled with warm, not hot, water.
If necessary beer bottle, tightly corked, is a good substitute.
444Clear away articles used for the baby.
H. Points to be observed, recorded and reported to the physician if urgent:
I. Instruct the Mother:
J. Do not discharge the baby until cord is off, umbilicus is in good condition and no further nursing care required. Premature babies should be oiled and wrapped in cotton. Premature jackets can be secured from the V.N.S. for 35 cents.
Care of Mother:
Make preparations as for general care.
Extra articles needed:
Take T.P.R.
Give complete bath.
Post-partum dressing:
Douche.
When douche is ordered boil nozzle before and after using.
Boil douche bag before using and wash afterwards—use boiled water.
When sutures, instruct the family how to irrigate after urination and movement of the bowels.
Normal maternity cases should be visited daily until after the 8th day of puerperium and at least once a week for supervision until the 5th week. The case is then transferred to Child Welfare nurse.
Additional visits should be made if the patient is still in bed and there is no intelligent adult to give care, or if the baby’s condition is not satisfactory.
Ingenuity, resourcefulness, and quick wit on the part of an intelligent nurse can almost always apply hospital ideals to circumstances which would at first seem hopeless. It is the nurse’s knowledge of obstetrical nursing and principles, rather than her equipment, that counts in saving lives. The following 446directions given to visiting nurses, by Cecil A. K. Dawkins, R.N., Supervisor of the Outdoor Department of the Montreal Maternity Hospital, indicate the possibility of clean, efficient care in conditions far from ideal:
“Appliances You Are Likely to Find in Any House:
“Bed, table, chair, two boxes, basin, pail, kettle, saucepan, plate, two cups, spoon, several fair sized bottles, sheet, two towels, pillow, pillow case, handkerchief, newspapers, old clean rags, small package boracic powder, small bottle vaseline, soap, baby clothes.
“Doctor’s bag will usually contain towel, clamps, scissors, ergot, chloroform, creolin, rubber apron, hypodermic syringe, nail brush.
CHAPTER XXI. CHARACTERISTICS AND DEVELOPMENT OF THE AVERAGE NEW-BORN BABY. New Functions. Description. Growth and Development. Weight. Height. Head and Chest. Fontanelles. Teeth. Stools and Urine. Skin. Tears. General Behavior.
CHAPTER XXII. NURSING CARE OF THE NEW-BORN BABY. Mortality of First Months and Year of Life. Preventable Causes. Dangers of Babyhood. Essential Features of Early Care. Daily Schedule. Bath. Clothes. Fresh Air. Exercise. Training the Baby. Bowels. Thumb-sucking. Ear-pulling. Crying. Ruminating. Feeding: Breast Feeding. Artificial Feeding. Necessary Characteristics of Artificial Food. Requirements for Milk Used. Articles Needed in Preparing Food. Preparation of Milk. Pasteurization. Boiling. Giving the Bottle. Ingredients of Food. Percentage Feeding. Average Formulae. Mixed Feeding. Commercial Baby Foods. Proprietary Foods, Canned Milks, Milk Powders. Other Articles of Food Sometimes Included in Baby Diet. Travelling. The Premature Baby. Summer Care of the Baby.
CHAPTER XXIII. COMMON DISORDERS AND ABNORMALITIES OF EARLY INFANCY. Malnutrition, Marasmus and Inanition. Diarrheal Diseases: Acute Gastro-enteritis. Symptoms. Treatment and Nursing Care. Acidosis. Colic, Constipation, Convulsions, and Vomiting. Infections: Ophthalmia Neonatorum. Symptoms, Treatment, and Nursing Care. Syphilis. Thrush, or Sprue. Impetigo. Pemphigus. Vaginitis. Abnormalities: Icterus or Jaundice. Cephalhematoma. Club Foot. Engorgement of Breasts. Hare Lip. Cleft Palate. Hernia.
Before undertaking the care of the new-born baby the nurse should stop and consider him for a moment and review in her mind just what he represents; what he has been through; what struggles and dangers are ahead of him; what are the weaknesses of his equipment to meet these perils and what must be the character of her service to him if she is to do all in her power to help him safely over that most hazardous period in the entire span of his existence: the first month of his life.
That little new-born baby is quite as helpless and appealing as he looks, for his chances for present and future health lie very largely in the hands of those who care for him during these early weeks, and any injury which is done at this time, either through acts of omission or commission, can never be entirely repaired.
At the time of birth, the baby makes the most complete and abrupt change in his surroundings and condition that he will make during his entire lifetime.
He has existed and evolved as a parasite for nine months, during which time he has been protected from injury; kept at the temperature which was best for him, and above all has been furnished with exactly the proper amount and character of nourishment necessary for his growth and development.
Suddenly he emerges from this completely protecting environment into a more or less hostile world, where he must begin life as a separate entity with a frail little body that in many respects is only imperfectly developed. And yet the baby must not only continue the bodily functions and activities that were begun during his uterine life, but must also elaborate and establish others which were imperfect or were performed for him. Otherwise he will not live.
452The nurse will recall that the fetus received its nourishment and oxygen, and gave up waste material, through the placental circulation; that the lungs were not inflated and that most of the blood flowed through the foramen ovale instead of through the pulmonary vessels, as it does after birth. The digestive tract, excretory organs and nervous system were not needed during fetal life and therefore are imperfectly developed at birth and are capable of functioning only within very narrow limits.
The pulmonary circulation usually is established immediately after birth, and when the baby cries vigorously the lungs are expanded and filled with air and the respiratory function is inaugurated. The ductus arteriosus, ductus venosus and two hypogastric arteries are gradually obliterated, as the normal circulation of the blood becomes established and the foramen ovale is closed. See Figs. 28 and 29.
The other functions are established more slowly and the care of the baby must be such that the immature, unused organs will not be overtaxed, and yet that their development will be promoted through activity.
The new-born baby weighs 3250 grams, or 7¼ pounds, and is about 50 centimetres, or 20 inches long. The body is well rounded and the flesh firm. The skin is a deep pink, or even red, and is covered with a white, cheesy substance, the vernix caseosa, which is likely to be thickly deposited in the folds of the skin, in the creases of the thighs and axillæ and over the back. Some babies still have the fine, downy lanugo hair over parts or all of the body.
The head and abdomen are relatively large, the chest narrow and the limbs short. The legs are so markedly bowed that the soles of the feet may nearly or quite face each other, but they finally assume a normal position. The bones are largely cartilage and the entire body is therefore very flexible. Some of the bones, which are separate at birth unite later in life and the adult skeleton finally becomes firm and rigid.
Most babies have faded blue eyes at birth, the permanent color appearing gradually, while the amount and color of the hair varies greatly, some babies being bald and others having abundant hair from the beginning.
453The shape of the baby’s head is sometimes distorted at birth, being so elongated from chin to occiput as to give the parents deep concern. But they may be confidently assured that in the course of a few days the head will assume the lovely rounded contour, so characteristic of babyhood. The temporary deformity is caused by a moulding and overlapping of the bones of the skull as it is forced through the birth canal, and sometimes also to a collection of fluid under the scalp, called the caput succedaneum, and which, too, is due to pressure during birth. Both the anterior and posterior fontanelles may be felt at birth.
Growth and Development. The progress during the first year, of average, normal babies who are satisfactorily nourished and cared for, is fairly uniform and the accepted average is suggested by the following schedules which are based upon observations made upon a large number of normal, healthy infants.
Weight. The average baby boy weighs at birth, 7¼ to 7½ pounds and girls a little less, as a rule. There is an initial loss of from six to ten ounces during the first week, through body waste and the passage of meconium and urine, before the full amount of nourishment is taken and assimilated, large babies losing more than small ones. (Chart 5.) From this time the gain is usually from four to eight ounces, each week, during the first five months, after which it is only about half as rapid, or at the rate of from two to four ounces weekly. At six months, therefore, the average baby weighs from fifteen to sixteen pounds, or double the normal birth weight of 7½ pounds, and at twelve months, from twenty to twenty-two pounds, or three times the average birth weight. The weight is perhaps the most valuable single index to the baby’s condition, that we have, but at the same time, it must be remembered that a baby whose food is rich in carbohydrates may be of normal weight, or over, but be incompletely nourished and very susceptible to infection. Other babies who are small and seem to gain unsatisfactorily are sometimes very well and vigorous. And very commonly there are periods in the lives of entirely normal babies when there is little or no gain in weight. This may occur during the period from the seventh to the tenth month, for example, or during very warm weather. But the baby’s weight should be watched carefully, for a loss or prolonged failure to gain may be an evidence of faulty nutrition or disease.
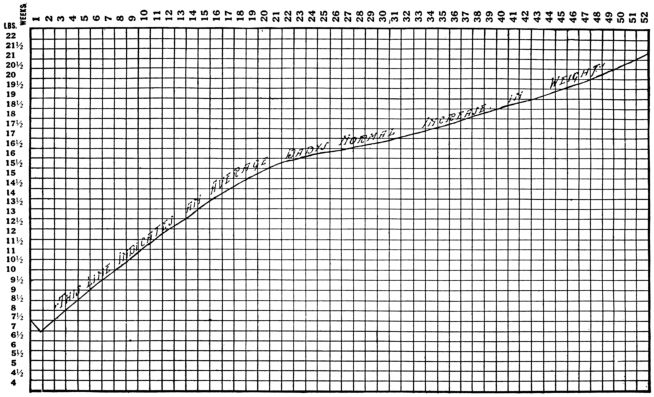
Chart 5.—Weight chart showing average weekly gain during first year of life.
455Height. The average height at birth is 20 inches, though boys may measure a little more and girls a little less; at six months, 25 to 25½ inches and at one year, 28 to 29 inches.
Head and Chest. The circumference of the head and chest are about the same at birth, the chest being possibly a little smaller. Both measure about 13½ inches, increasing gradually to about 16½ inches at six months and 18 inches at the end of the first year.
Fontanelles. The posterior fontanelle usually closes in six or eight weeks but the larger, anterior fontanelle is not entirely obliterated until the baby is eighteen or twenty months old. Closure of the fontanelles is usually late in rickets, cretinism and hydrocephalus and early in cases of malnutrition and microcephalus.
Teeth. Although it occasionally happens that a baby has one or two teeth at birth, the average infant has none until the sixth or seventh month, when the two lower, central incisors appear. After a pause of a few weeks the two, upper, central incisors appear, followed by the two lateral incisors in the upper jaw. At the end of the first year, therefore, the average baby has six teeth, or eight, if the lower, lateral incisors have come through by the first birthday, as they sometimes do. (Fig. 148.) This is the usual course of dentition during the first year, but there are wide variations among entirely well and normal babies, the first tooth sometimes not appearing before the tenth, eleventh or even twelfth month. But as a rule if no teeth are cut by the time the baby is a year old, it is regarded as an evidence of faulty nutrition, perhaps bordering on rickets.
The baby who is properly fed and cared for cuts his teeth with little or no trouble, in spite of the widely current belief that a teething baby is a sick baby. We have no way of estimating the number of babies who die needlessly from infections and digestive disturbances because of this fallacious conviction. For if the baby is sick while teething, the disturbance is all too frequently accepted as a normal occurrence and nothing is done until too late.
456Frail, delicate babies may have convulsions each time that a tooth is cut and if a baby is having digestive trouble it is likely to grow worse while he is teething. But dentition is a normal physiological process and the healthy, properly fed baby suffers little or no inconvenience at this time.
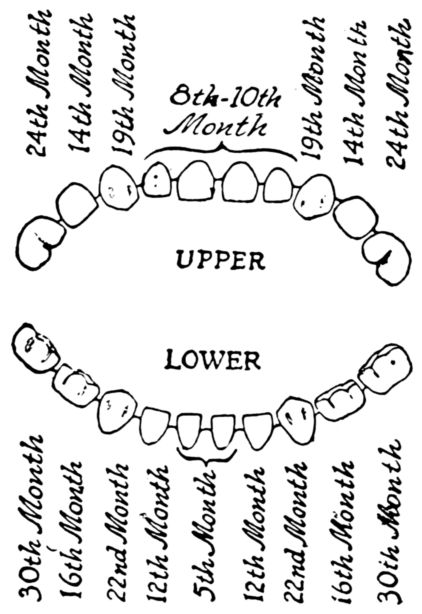
Fig. 148.—Diagram of first or deciduous teeth and ages at which they usually appear.
The care of the baby’s teeth should begin when the first tooth appears. It should be wiped, front and back, with a piece of gauze or cotton dipped in a solution of boracic acid, or sodium bicarbonate or some other weak alkaline wash, to neutralize the acid secretions of the mouth which start decay. After the baby has five or six teeth, the use of a very soft brush, with tooth paste, is often advised, the teeth being brushed with a circular motion or from the gums toward their edges. The teeth should be wiped, or brushed, morning and evening and after feedings. The reason for such close care of the temporary teeth is that they serve as a mould or brace to hold the jaws in proper shape for the permanent teeth which appear later. If the “milk” or deciduous teeth decay or crumble away before the jaws are developed to the point when the permanent teeth appear, these second teeth are likely to be crooked and uneven.
Stools and Urine. During the first two or three days, the stools are of dark green, tarry material called meconium. Meconium consists of cast-off cells from the skin and intestines, fat, mucus, hairs and bile pigment. In the course of two or three days, the stools begin to grow lighter and shortly the normal, milk-feces appear, being bright yellow, of a smooth pasty consistency and having a characteristic odor. During the first month or six weeks the baby’s bowels may move three or four times daily, but after this they usually move but once or twice in 457the course of twenty-four hours. As the diet is increased, the stools grow somewhat darker and firmer and finally become formed.
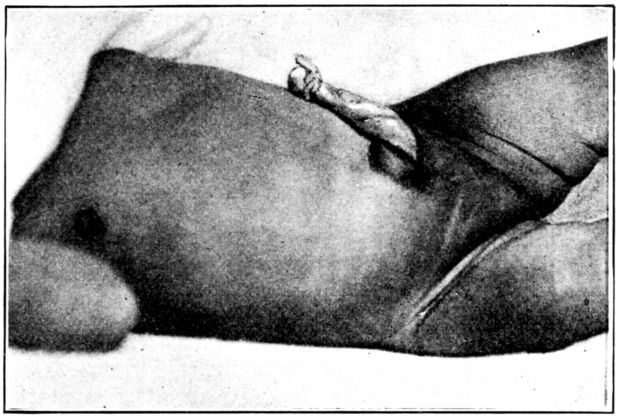
Fig. 149.—Appearance of umbilical cord immediately after birth.
The new-born baby’s bladder usually contains urine which may be voided immediately after birth or not until several hours later. After the first voiding the bladder may be emptied five or six times a day, or oftener. The nurse should watch for the first evacuation of the bowels and bladder, and if they do not occur during the first few hours, the fact should be reported to the doctor, as the omission may be due to an imperforate anus or meatus.
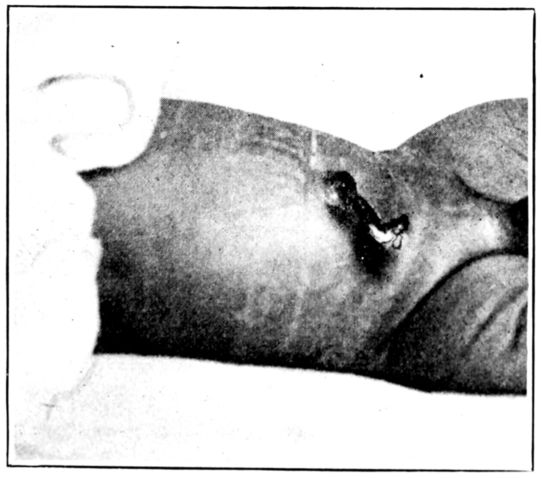
Fig. 150.—Appearance of umbilical cord, four days after birth.
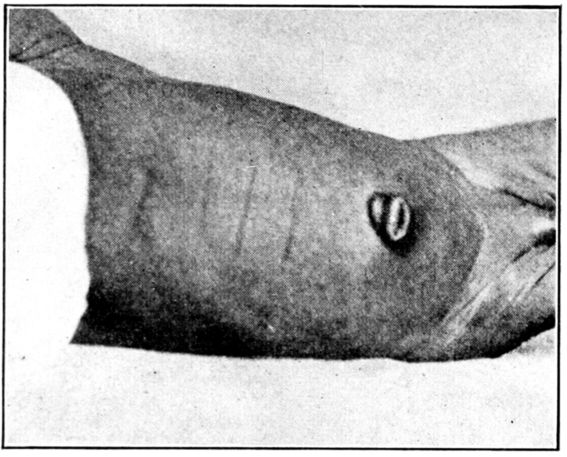
Fig. 151.—Appearance of umbilicus immediately after separation of cord.
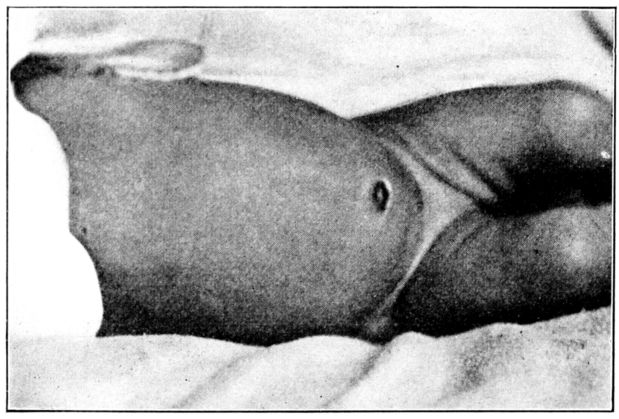
Fig. 152.—Appearance of a well healed umbilicus.
Cord. Within a few days after birth the stump of the umbilical cord begins to shrivel and turn black, and a red line of demarcation appears at the junction of the cord with the abdomen. By the eighth or tenth day, as a rule, the cord has atrophied to a dry black string, when it drops off and leaves an ulcer, or small granulating area which heals entirely in a few days. (Figs. 149, 150, 151, 152.) Before the days of sepsis, infections of the cord were not uncommon and babies frequently died of tetanus, streptococcus and other infections. But at the present 459time an infected cord is a rare, and, it may be added, an almost inexcusable occurrence.
Skin. By the end of the first week any lanugo remaining usually disappears and there is frequently a scaling of the superficial layers of the skin which lasts for two or three weeks, while a delicate pink tint replaces the deeper color of the skin in the course of ten days or two weeks. The baby does not perspire until after the first month, as a rule, when insensible perspiration begins, gradually increasing until perspiration is free by the time the baby is a few months old.
Tears. There are no tears at birth and opinions differ as to whether they appear in the course of two or three weeks, or three or four months. The absence of the lachrymal secretion is one explanation for the necessity of bathing the baby’s eyes during the early days and weeks, for if dust or other foreign material gains entrance it is not washed out by the tears as it is later.
General Behavior. During the first few weeks the average baby sleeps most of the time: that is from nineteen to twenty-one hours daily. He gradually sleeps less, as the special senses develop and will sometimes lie quietly for an hour or more with his eyes open, sleeping only sixteen or eighteen hours daily at six months and fourteen to sixteen hours at the end of a year.
The baby begins to make noises and “coo” at about two months and to utter various vowel sounds when about six months old. By the end of a year these indefinite noises and sounds become distinct words. At about the fourth month, he grasps at objects and smiles and very soon even laughs. He holds up his head at about the third or fourth month; sits up and also begins to creep at six or seven months; while sometime between the ninth and twelfth months he will stand by holding to some one’s hand or the furniture, and will begin to walk with assistance.
These degrees of development at different ages are not to be taken as the only measure of normal progress, for many well babies mature more rapidly and others more slowly than at the rate which is found to be the average.
In addition to these fairly specific evidences of the baby’s condition and progress, such as weight, height and muscular development, there are other and less definite indications of his 460well-being which the nurse must watch for and accord a very high value.
The baby who is well and is being properly fed in all respects, will have good color; his flesh will be firm; he will take his nourishment with a certain amount of eagerness and seem satisfied afterward. He will sleep for two or three hours after each feeding; will sleep quietly at night, and while awake, unless he is wet or uncomfortable for some other good reason, he will seem contented, good-natured and happy.
It is estimated that out of every thousand babies born alive, in this country, forty die during the first month of life, and that more than as many again, or about eighty-five all told, perish before reaching the first birthday.
So hazardous is this period of early infancy, in the United States, that our annual loss of baby life is between seven and eight times as great as was the yearly toll of our young men during the war, for upwards of 200,000 babies less than a year old die each year. That the first month of life is fraught with greater danger than any which follow is shown by the fact that about 100,000 of these deaths occur during the first four weeks.
The tragedy of these figures is made darker by the knowledge that at least half of the babies who are lost die from preventable causes. In other words, they die from lack of proper care.
That is the significant fact for the obstetrical nurse, since more and more frequently she has the young baby in her care during the crucial first month and inevitably plays an important part in increasing his chances to live. She does this by helping to keep the well baby well, rather than by nursing a sick baby.
The dangers which make babyhood such a precarious period may be grouped very largely under the general headings of unfavorable ante-natal conditions, nutritional disturbances and infections. The care and supervision of the expectant mother will remove many of the unfavorable ante-natal causes. Nutritional disturbances and infections must be dealt with after birth.
Faulty nutrition may result in rickets, scurvy, malnutrition, marasmus, acute inanition or the less serious colic, constipation or diarrhea. The most frequent results of infection among young babies are the respiratory diseases in winter, such as bronchitis and pneumonia, and the intestinal disorders in summer, commonly referred to as “summer complaint.” Since 462undernourished babies are very susceptible to infection, the two conditions are frequently coincident.
With the baby’s frailty and imperfect development in mind, as well as the needs of his growing body and the evils that beset his way, we can understand the reasons for the painstaking, protecting care which he is given during the early weeks of his life.
The essential features of this care are as follows:
These requirements seem so rational that one might expect them to be met as a matter of course; but the annual sickness and death rate among babies are a constant reminder that they are not.
The nurse should begin by arranging a daily schedule for the baby’s feedings, fresh air, bath, sleep and exercise, and follow it with unfailing regularity. The hours for the nursings, which vary with different doctors, will constitute the greater part of the daily schedule, and for a baby on four hour feedings, for example, some such program as the following may be arranged:
| 6 | a.m. | Feeding. |
| 8 | a.m. | Orange juice (when ordered). |
| 9 | a.m. | Bath. |
| 10 | a.m. | Feeding. |
| 10.30 to 2 | p.m. | Out of doors. |
| 2 | p.m. | Feeding. |
| 2.30 to 4 | p.m. | Out of doors. |
| 4 | p.m. | Orange juice (when ordered). |
| 4 to 5.30 | p.m. | In-door airing and exercise (when ordered). |
| 5.30 | p.m. | Preparation for the night. |
| 6 | p.m. | Feeding. |
| 10 | p.m. | Feeding. |
| 2 | a.m. | Feeding (when ordered). |
The importance of punctuality in the daily routine cannot be stressed too often and it is one aspect of the baby’s care for which the nurse is absolutely responsible. No matter how well the baby 463is nursed, in other respects, nor how skillfully the doctor directs his care, the baby cannot be expected to progress satisfactorily if his life is irregular.
The Bath. The first office which the nurse usually performs for the new-born baby, and which she repeats daily, is to bathe and dress him. The bath may be given in a tub, under a spray or in the nurse’s lap, according to the wishes of different doctors, while sponge baths are sometimes given with soap and water and sometimes with oil.
The first bath, particularly, is likely to be an olive oil sponge, given immediately after birth, before the baby is taken from the mother’s bedside, and many doctors have the sterile cord dressing and abdominal binder applied at this time. This oil bath is given, not alone for the purpose of removing the vernix caseosa, but also, to lessen the radiation of body heat, which the baby can ill afford to lose. When such a practice is followed it only remains for the nurse to dress the baby and place him in his crib to sleep undisturbed for several hours.
Some doctors have the baby sponged every morning with albolene or olive oil, instead of with soap and water, until the cord separates, when tub bathing is adopted. When the daily bath is given with oil, the baby’s thighs and buttocks are wiped clean with an oil sponge each time that the diaper is changed. Other doctors have the baby’s first bath given in a tub, with soap and water, while still others who fear that the cord may be infected by immersing the baby, have him sponged with soap and water, after the vernix caseosa has been softened with oil.
Sponge bathing is commonly employed for all babies until the cord separates and for frail delicate babies or those suffering from skin trouble. The sponge bath may be given in the nurse’s lap or on a table covered with a pad, either method being satisfactory if the baby is kept warm and comfortable. But one inclines to the idea of having the baby bathed in the nurse’s lap for he seems happier there; more comfortable and less frightened and we cannot be sure that these factors are unimportant.
The best time for the daily bath, during the first three or four months, is about an hour before the second feeding in the morning. After this age the full bath is sometimes given before 464the six o’clock feeding, in the evening, for a bath at this hour is soothing and restful and often helps toward giving the baby a good night.
Preparation for the bath should made with its possible effects, both good and bad, in mind, for the baby may be helped or harmed according to the skill with which he is bathed. He must not be chilled during his bath, and fatigue and irritation must be avoided by giving it quickly and with the least possible handling and turning. These ends may be served by conveniently arranging all of the articles which will be needed, on a low table at the right hand side of the nurse’s chair, before the baby is undressed.
There should be a pitcher of hot and one of cold water; a bath thermometer; two soft wash-cloths; soft towels; bath blankets; Castile, or some other mild soap; boracic acid solution; sterile cotton pledgets; large and small safety pins, or large ones and a needle and thread if the band is to be sewed on; unscented talcum powder; sterile albolene or olive oil; soft hair brush and a complete outfit of clothing. The little garments should be arranged in the order in which they will be put on, the petticoat slipped inside the dress, and all hung before the fire or heater, to warm.
The temperature of the room should be about 72° F. and if it is possible to bathe the baby before an open fire or a heater, so much the better. In any case he must be protected from drafts. A sheet hung over the backs of two straight chairs will serve very well as a screen if no other is available.
The tub or basin should be about three-quarters full of water at 100° F. for the new baby; about 95° after the third month and gradually lowered to 85° F. or 90° F. for the baby a year old. The temperature of the water should not be guessed at, but tested with a thermometer, though in an emergency the nurse may safely use water that feels comfortably warm to her elbow.
It is a good plan to lay a folded towel in the bottom of the tub, before beginning, as babies are often frightened by coming in contact with the hard surface.
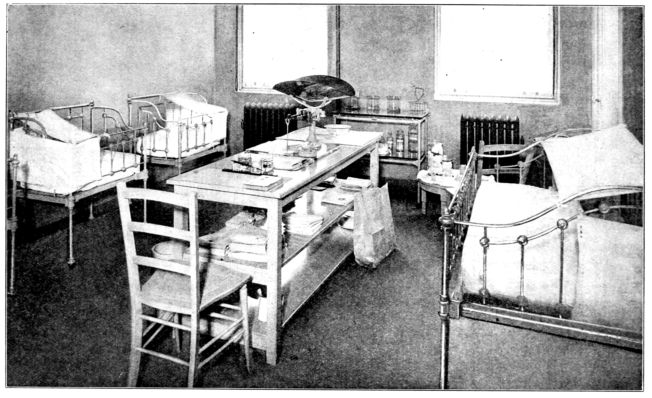
Fig. 153.—Nursery at Manhattan Maternity Hospital. Note beam scales, low table with articles for bath, and method of protecting babies’ heads from drafts.
466The nurse should wear a waterproof apron, covered with one of flannel over which is laid a soft towel until the bath is finished, when it is slipped out, leaving the dry flannel apron to wrap about the baby. She should wash her hands thoroughly with hot water and soap; sit squarely, with her knees together, in a chair without arms; take the baby in her lap and undress him under a blanket.
In order that the bath may be given deftly and quickly, it is a good plan to give the different parts in the same order every day, for practice makes perfect.
It is usually a routine to weigh the baby every morning, during the first two or three weeks and once or twice a week afterwards. Premature babies and those who are very frail are weighed at longer intervals because of the inadvisability of disturbing them so often. The baby is undressed for his bath, wrapped in a blanket, and laid in the scoop or basket of a beam scale (Fig. 153) and a note made of the entire weight, for if he is placed in the scales without protection he is likely to be chilled and frightened. The weight of the blanket is ascertained separately and deducted from the total thus giving the baby’s exact weight.
The eyes should be bathed first, with pledgets of sterile cotton dipped in warm boracic acid solution, each pledget being used but once. To prevent the solution from running from one eye into the other, the baby’s head is turned slightly to one side and the lower eye wiped gently from the nose outward. The lids may then be separated by placing one thumb below the brow and lifting it slightly, and the eye flushed with a gentle stream by squeezing a freshly soaked pledget just above it. The head is turned to the other side and the eye on that side bathed in like manner.
The mouth is swabbed out very gently with boric-soaked cotton wrapped about the tip of the little finger, care being taken not to abrade the delicate mucous lining. The nostrils are cleaned with little spirals of cotton dipped in liquid petrolatum or olive oil.
The face is then washed with warm water, no soap, and patted dry. The scalp, neck and ears are washed with soap and water and thoroughly dried by patting and wiping gently in the creases. The body should then be well soaped, with the nurse’s 467hand, only one part being exposed at a time, to avoid chilling. To place the baby in the tub the nurse may slip her left hand under his head in such a way that his head will rest upon her wrist, her fingers support his shoulders and her thumb curve over and hold the upper part of his arm. She may then grasp his ankles with her right hand and lower the little body into the water, feet first. If his arm and shoulder are firmly held and supported by the left hand it is an easy matter to steady the entire body and keep the baby’s head out of the water while giving the bath with the right hand. (Fig. 154.) The new baby is not usually kept in the tub for more than two or three minutes, but when he is three or four months old he may stay in for five minutes and still longer as he grows older.
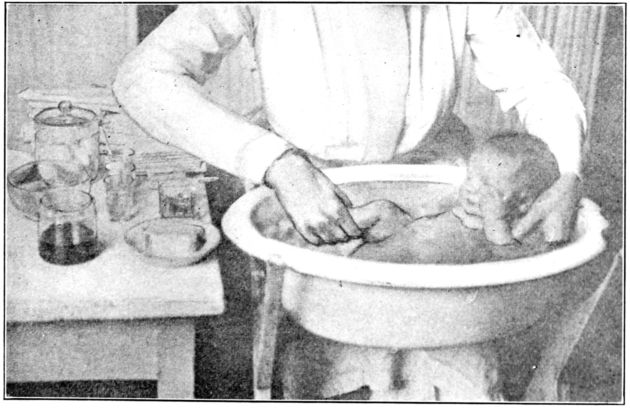
Fig. 154.—Method of supporting baby’s head above water while giving tub bath.
Hot water should not be poured into the bath after the baby has been placed in it but cold water is often added, for a three or four months old baby, or the warm bath followed by a quick sponge with cold water. The little body is quickly patted dry and rubbed briskly with the palm of the nurse’s hand; the legs and arms stroked toward the body; the back from the neck downward and the chest and abdomen with a circular motion. Babies who react well to cold baths are benefited by them but such 468“toughening” methods have to be tempered to the resistance of the individual baby and are employed only under the supervision of the doctor.

Fig. 155.—Preparation for circumcision. (From photograph taken at The Cleveland Maternity Hospital, with description, by courtesy of Miss MacDonald.)
On Table at Left:
Stand at Right:
For Baby:
| Brandy, 1 dram. | } | In sterile medicine glass with dropper. Used for anesthetic. |
| Sterile water, 6 drams. | ||
| Sugar, ½ dram. |
One nurse holds the baby by his knees with his hands under her arms. The second nurse begins the anesthetic, three minutes before doctor begins to operate, by dropping brandy and water on small piece of sterile cotton in gauze in baby’s mouth.
The genitals should be bathed and dried with care; inspected daily and any abnormality reported to the doctor. It is not uncommon for girl babies to have a slight bloody discharge from the vagina. This is unimportant and soon disappears, but a 469purulent discharge is likely to be an evidence of gonorrheal vaginitis. It is routine in many hospitals to retract the foreskin of male babies every morning at the time of the bath by rubbing it back with gauze or cotton, taking pains that it is again pulled forward into the original position after the part underneath has been bathed with boracic acid solution. If retraction is impossible after several successive daily attempts, the baby is not infrequently circumcised. (Figs. 155, 156.)
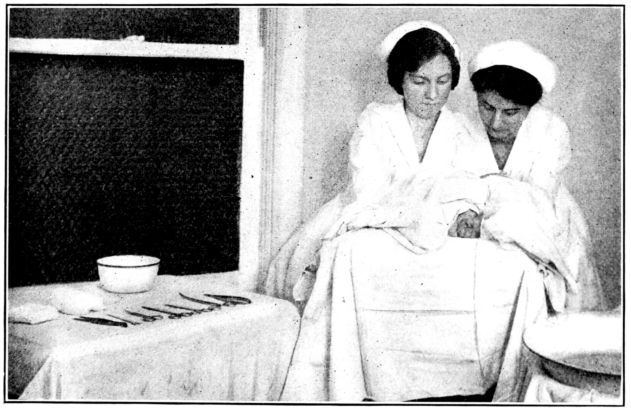
Fig. 156.—Baby in Fig. 155 draped with sterile sheet.
When the entire body, including creases and folds, has been patted quite dry, it may be dusted with an unscented talcum powder, but this powdering must not be resorted to as an aid in drying the skin. In order to prevent chafing, the buttocks and thighs should be wiped clean with oil or bathed with warm water, no soap, patted dry and powdered or oiled each time that the diaper is changed.
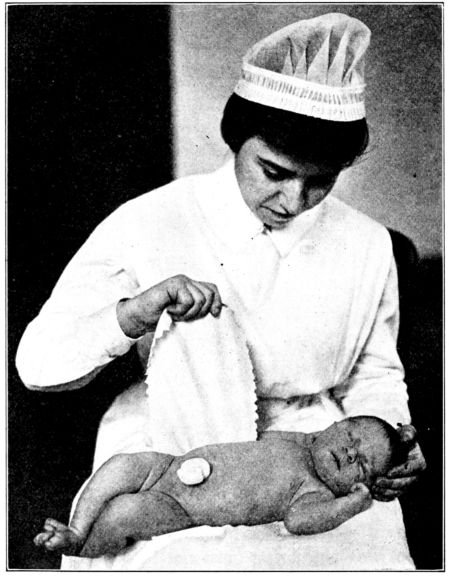
Fig. 157.—Cord stump dressed with dry sterile gauze. (From photograph taken at Johns Hopkins Hospital.)
If the first bath is a tub bath the cord is dressed after the baby is dried and powdered. The form and method of cord dressings vary somewhat with different doctors but in practically all instances the dressings are sterile, to prevent infection, and porous in order that air may gain access to the cord and promote the drying, separating process. The dressing itself may consist of dry, sterile gauze or gauze wet with alcohol, applied to the cord in the manner of a finger bandage (Fig. 157); or it may consist of squares of sterile gauze or muslin with holes in the centres to fit around the cord, and dusted with some such powder as boric acid, bismuth or salicylic acid and starch. These squares are folded about the cord stump which is laid over on the abdomen, being directed upward to prevent its being wet with urine. A gauze sponge is placed over the dressing and the binder applied with firm, even pressure, but not tightly, and sewed on or held in place with safety pins. (Fig. 158.) The 471cord dressing is not removed until the cord separates, unless it is wet or soiled, but as a rule the band is removed every morning at the time of the bath, or whenever it is soiled.
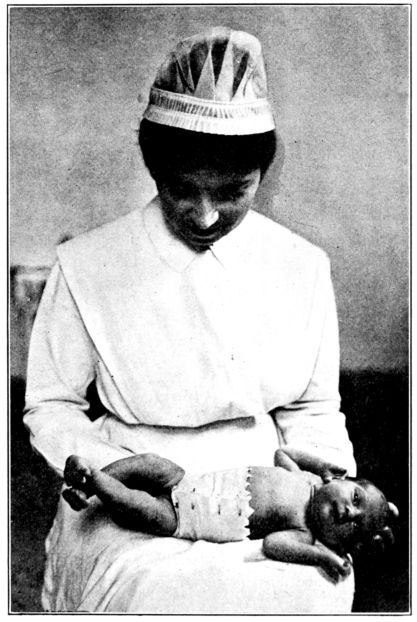
Fig. 158.—Flannel band applied over cord dressing.
After the band has been applied the warmed shirt, diaper, petticoat and dress are put on, with the fewest possible motions, and the baby’s hair brushed upward from the neck and back from his forehead. He should be wrapped in a small blanket, fed and laid quietly in his crib to sleep. If his hands and feet are cold a hot-water bottle at 125° F. with a flannel cover, may be placed beside him.
472When the baby is made ready for the night he may have either a sponge bath or simply have his face and hands sponged with warm water, according to the wishes of the doctor. The clothing which the baby has worn during the day should be replaced by an entirely fresh outfit. The day and night clothing may be worn more than once, if clean and if aired between times, but it is better not to have the baby wear the same clothes day and night.
Clothes. The baby’s clothes may play an important part in promoting his well-being, and to accomplish this they must be warm, light-weight, soft and porous. They should be simple; fit smoothly and be loose enough and short enough to permit the baby to move unhampered. In order that his body may be kept at an even temperature their weight must always be adjusted to the needs of the moment. The general tendency is to dress the baby too warmly, as a result of which he perspires; is listless, pale, fretful; sleeps badly; is susceptible to colds and other infections and has poor recuperative powers. His digestion is likely to be deranged and he may have prickly heat. On the other hand, if the baby is not dressed warmly enough his hands and feet will be cold and his lips blue; he will cry from discomfort and the general result may be lowered vitality and disturbed digestion. If the baby’s clothes are not comfortable, if they pull and drag or have tight bands, he will be fretful and restless, with disturbed sleep and digestion in consequence.
The little wardrobe will be entirely adequate, under ordinary conditions, if it consists of shirts, bands, diapers, flannel petticoats, dresses, flannel wrappers and sacques with a cap and cloak for extra warmth during in- or out-door airing. (Fig. 159.)
The shirts should have long sleeves and high necks; they should open all the way down the front and come well down over the hips. During the cold months they should be of silk, silk and wool or cotton and wool, as all wool shirts are usually too warm, and during the summer months they should be of all cotton and very thin. Size No. 2 is the best size to start with as the smaller size is soon outgrown.

Fig. 159.—An outfit of practical baby clothes:
A. Thin cotton dress, open down the back.
B. Flannel night-gown with set-in-sleeves.
C. “Gertrude” petticoat, open down the back.
D. Shirt, opened all the way down the front.
E. Flannel night-gown with kimono sleeves.
F. Knitted band with shoulder straps.
G. Flannel square with tapes run through casings to form hood of one corner.
H. Bag, with hood, suitable for premature baby or for outdoor sleeping.
474The first bands usually consist of strips of all wool or cotton and wool flannel about six inches wide and eighteen or twenty inches long, torn across the width of the material and not hemmed. This straight binder is worn until the cord dressing is discontinued, when it is replaced by a knitted band with shoulder straps. If the cord dressing is held in place by a gauze binder, the knitted band with straps is used from the beginning. Whether the binder be flannel or gauze, it must be applied firmly and with even pressure, but not tight. It is a mistake to think that a tight band strengthens the baby’s abdominal muscles for it has the opposite tendency. A tight band may give pain or discomfort and even cause colic or vomiting.
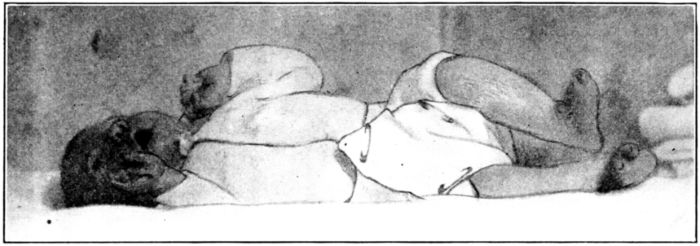
Fig. 160.—Appearance of properly adjusted diaper which has been folded diagonally.
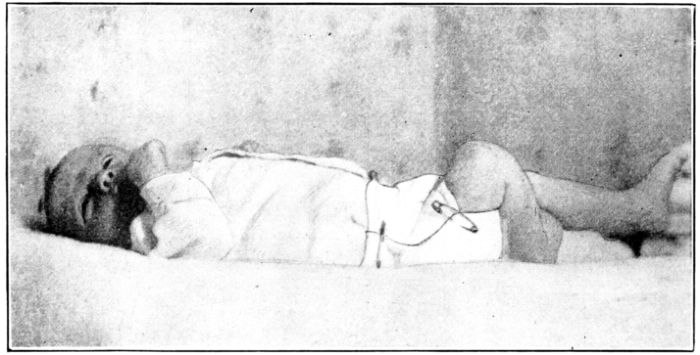
Fig. 161.—Appearance of properly adjusted diaper which has been folded longitudinally.
The knitted band is usually worn for three or four months, particularly in cold weather, to provide a little extra warmth 475over the abdomen. Thin, delicate babies sometimes need this band for a year or more.
The diapers should be of soft, absorbent material, of a loose weave, such as cheese cloth, bird’s-eye, stockinette, thin Turkish towelling or outing flannel; should be 18 or 20 inches square and hemmed. There are two methods of putting on the diaper. One is to fold the square diagonally and bring the diagonal fold around the baby’s waist. One of the lower corners is drawn up between the thighs, the two corners from the sides brought over this and the fourth corner brought up over these and all pinned securely with a safety pin. (Fig. 160.) Small safety pins hold the margins together above the knees. The other method is to fold the diaper straight through the centre, forming a rectangle, twice as long as it is wide; lay the baby on it lengthwise, draw it up between his thighs and pin it on each side at the waist line and above the knees. (Fig. 161.)
In either case the diaper must be put on smoothly and care taken to avoid forming a thick pad between the thighs as this will tend to curve the bones of the legs. Squares of soft, absorbent material, which may be burned, placed inside the diapers, will greatly facilitate the laundry work. In some hospitals a very soft absorbent paper is used for this purpose, sometimes being covered with gauze.
The baby’s diaper should be changed whenever it is wet or soiled, for in addition to making him restless and fretful for the time being, the skin about the thighs and buttocks will grow red and chafed if he is allowed to wear wet diapers. Wet diapers should not be dried and used again but washed with a mild soap, boiled and whenever possible, dried in the open-air and sunshine.
All of this makes it apparent that the regular use of waterproof protectors cannot be justified since the chief reason for putting them on a baby is to avoid the necessity of changing his diaper as soon as it is wet. Under special circumstances such as a drive, a short journey or visit the diaper may be protected by water-proof drawers. Their habitual use saves work for the nurse but makes the baby uncomfortable and unhappy.
The petticoat should be of light-weight, cotton and wool flannel, 476cut after the familiar Gertrude pattern and hang straight from the shoulders. It may fasten in the back or on the shoulders, with small buttons or with tapes. Tapes are often objected to on the ground that the baby tangles them up with his fingers, which annoys him, and often puts them in his mouth. This petticoat is worn practically all the time, except during very warm weather.
The slips or dresses are most satisfactory if cut after the same pattern as the petticoat, with the addition of sleeves which may be set in, or of the kimono style. The dresses serve chiefly to keep the petticoats clean and make the baby look dainty, and are accordingly made of soft cotton material such as nainsook, cambric or lawn. In summer, it is true, the petticoat is often discarded and the thin slip put on over the shirt and diaper.
The night gowns are made like the dresses but are of soft flannel or stockinette, in cold weather, and tape is often run through the hems in order that they may be drawn up, bag-fashion, to keep the baby’s feet warm. During very warm weather the baby sleeps in a thin cotton slip.
In addition to these garments there are many times when a soft little sacque or wrapper is used to keep the baby warm, and one or two flannel squares (one yard), to wrap around him when he is carried about the house are practically indispensable.
The petticoats, dresses and night gowns are cut about twenty-seven inches long and many doctors feel that they offer sufficient protection for the feet of the average baby to make stockings unnecessary until he is from four to six months old. The skirts may then be shortened to ankle length and stockings added to the little wardrobe. Some doctors think it wiser to put knitted socks or part wool stockings on the new baby particularly if he is born during cold weather.
When the baby begins to creep, he should wear soft soled shoes, part wool stockings in cold weather and thin cotton or silk ones during the summer, and firm but flexible soled shoes as soon as he tries to stand alone or to walk.
During the first month or two, the baby scarcely needs special clothing for out-door wear, as he may be warmly wrapped in one of the flannel squares by being placed on it diagonally, the 477upper corner folded about his head to form a hood and held under his chin with a safety pin. The corners on the sides are folded about his shoulders, the lower one brought up over his feet and limbs and the additional blankets tucked in over all. But as he grows older and moves about in his carriage, he will need a cap and cloak or wrap with hood attached. In cold weather the cap should be knitted or wool lined and the cloak of soft woolen material or wool lined. In moderate weather the cap may be of one thickness of cotton or silk, or very light flannel, while on very warm days he will need no head covering.
To sum up: The baby’s clothes should be simple in design, hang from the shoulders, fit smoothly but loosely and have no constricting bands; they should be soft, light and porous, their warmth always adjusted to the immediate temperature so that the baby will be protected from being either chilled or overheated. And his clothing must always be clean and dry.
Fresh Air. An abundance of fresh air is one of the baby’s greatest needs as it increases his resistance and recuperative powers, improves his appetite and aids digestion. In general, the more the baby is in the open air and the more fresh air he has while in the house, the better.
The two factors which must be considered in supplying the baby with fresh air are the condition and vigor of the baby himself and the immediate temperature and state of the weather. His age and the season of the year can be only partial guides because of the difference between individual babies of the same age and the variations in temperature, winds and moisture during any one season.
The air of the room which the baby occupies should be changing constantly in order that it may always be fresh, but the temperature should be equable and the baby protected from drafts. As the tendency here, as with the baby’s clothes, is toward overheating, the nurse will do well to remember that the new baby who lies covered up in his crib, may usually be kept in a colder room than is advisable for an older one who is creeping or walking about.
During cold weather the baby’s bed should not be directly in front of an open window and he should be protected from 478direct currents of cold air by a sheet hung over the head and side of his crib. (See Fig. 153.)
Two or three times daily, while the baby is out of the room, the windows should be opened wide to air the room thoroughly, one of these airings being just before the baby is put to bed for the night.
The usual instructions concerning the temperature of the nursery are to keep it from 68° F. to 70° F. during the day and about 65° F. at night, during the first three months and lower it gradually to 64° F. during the day and about 55° F. at night as the baby grows older. It is customary to begin to open the nursery window at night when the baby is three or four months old, if he is well and the temperature is above freezing.
In planning to take the baby out-of-doors it is wiser, as a rule, to begin with the indoor airing when he is about a month old, except, of course, during the moderate or mild months of the year, when he is taken out at once. If the weather is cold, the baby may be protected with extra wraps and carried in the nurse’s arms, into a room in which the windows are open and kept there for fifteen or twenty minutes. This indoor airing is increased by being gradually lengthened to two or three hours and by having the windows opened wider and wider. By the time he is two or three months old he is taken out of doors on clear, bright days, the best time being between ten and three o’clock, when the sun is high. If he is carried in the nurse’s arms at first the warmth of her body serves as a protection and helps to accustom him to the out-of-door life, when he spends a good deal of his time out of doors in his carriage.
On windy, stormy days or when there is melting snow on the ground the baby may be given his airing on a protected porch or in a room with the windows open. He is not usually taken out if the temperature is below freezing until the third or fourth month. After this time the average baby is taken out when the temperature is not lower than 20° F.
When the baby is dressed in his extra wraps he must be taken out of doors or the windows opened immediately, for otherwise he will become overheated and be in danger of chilling when taken into the colder air.
479Warm hands and feet, a good color and the baby’s tendency to sleep most of the time while out-of-doors are evidences of his being adequately clothed for his airing, while the reverse is true if he is not warm enough.
A robust baby who has been gradually accustomed to being out-of-doors during the day will usually be much benefited by sleeping out at night. But he must be protected from winds and his clothing so arranged that he cannot be chilled. Knitted or flannel sleeping garments or sleeping bags (See Fig. 159) are valuable and in addition, the blankets which cover the baby should be securely pinned to the mattress with safety pins and tucked well under it at the sides and foot. The baby should wear a warm cap and the bed should be warmed before he is put into it. Or better still, he may be dressed for the night, put to bed in a warm room and the crib then moved out on the sleeping-porch.
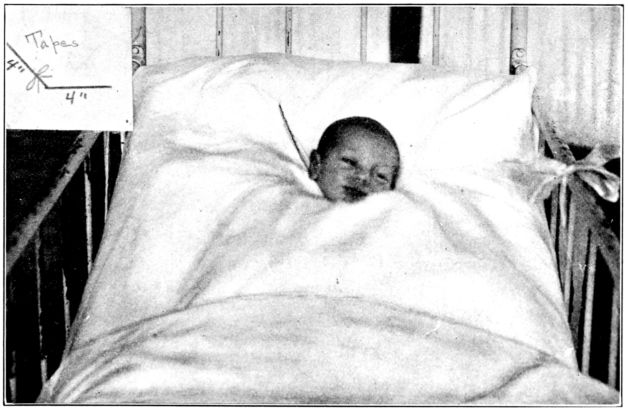
Fig. 162.—Sutton poncho which keeps the baby warm by covering all but his head. The insert shows slit for his head. The regular bedding is temporarily turned back in this picture. (From photograph taken at Bellevue Hospital.)
An excellent device for protecting the baby’s arms and chest 480and keeping him generally well covered is the poncho (Fig. 162) devised by Dr. Lucy Porter Sutton of Bellevue Hospital. The poncho is a rectangle made of flannel, outing flannel or an old blanket and cut large enough to tuck well under the head and sides of the mattress and extend below the baby’s feet. The baby’s head slips through an opening, which is almost a right-angled slit, near the centre of the poncho and about 20 inches from the top. The slit is firmly bound and provided with tapes to tie it together after the baby is put in. The poncho should be put on loosely enough to permit the baby to move about at will beneath it. After it is adjusted the bed is made up as usual with additional blankets.
Under all conditions the baby’s airings must be increased gradually, both as to lowering the temperature and lengthening the time, and always adjusted to the vigor and reaction of the individual baby. He must be warm, but not too warm; he must be protected from wind and dust, and his eyes shielded from glare and from flickering light such as may be caused by a tree in a light breeze.
Exercise. Although the baby should not be handled unnecessarily nor tossed about and played with by friends and relatives, it is important that his muscular development be promoted by regular and carefully planned exercise. It is usually considered best for the baby to lie quiet and undisturbed in his crib most of the time during the first three or four weeks. Dr. Griffith begins the baby’s exercise about that time by having the nurse take him in her arms on a pillow and carry him about for a few moments, several times daily. After a week or two of this form of exercise, the nurse carries the baby without a pillow but supports his head and back.
The position of the baby’s body is changed by being carried about in this way, while the movement of the nurse as she walks about causes a certain amount of motion of the baby’s muscles, constituting a gentle exercise.
This exercise, in the form of picking up and carrying about is regarded by many pediatricians as of great importance. There is a possibility that lack of this form of “mothering” is one reason why babies in hospital practice sometimes fail to progress 481as they should. Certainly lying too long in one position is harmful. The nurse should carry the baby first on one arm and then on the other in order that both sides of his body may be equally exercised. By the third or fourth month he sits up in her arms as she carries him about, and he may be placed on the outside of his crib coverings for a little while every day, to kick and struggle at will. His skirts should be rolled up under his shoulders, or removed entirely, to leave his legs quite free, care being taken that the room is warm and that he has on stockings.
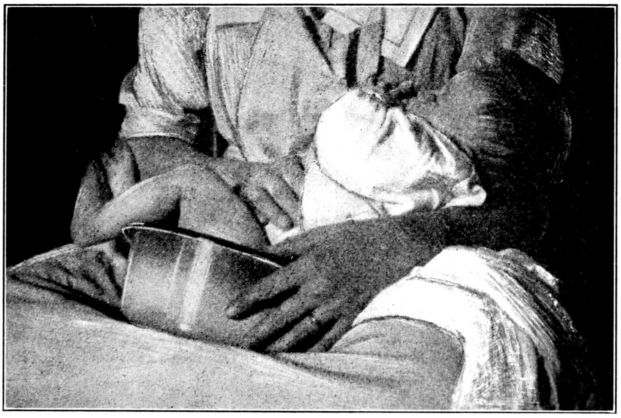
Fig. 163.—A comfortable position for the baby being trained to use chamber.
By about the sixth month he will usually begin to make an effort to creep, if turned over on his stomach and helped a little, and he may be propped up in the sitting position, in his crib, for a few moments every day. As he gives evidence of having enough energy to creep farther than the size of his crib permits, he may be put into a creeping-pen, or upon the floor under certain conditions. It must be remembered that the floor is likely to be cold, drafty and dusty. The nurse must assure herself, therefore, that the floor is warm; must cut off all drafts and spread a clean sheet or quilt on the floor before the baby is put down to creep. When the sheet is taken up, it is folded with the upper surface inside in order that when it is again put down the 482baby will play on the clean side and not on the side that has been next the floor.
A creeping-pen or cariole or some such provision is often more satisfactory than the floor, consisting as it does of a railed-in platform raised about six or eight inches from the floor.
The suggestions for exercise, like those for the baby’s airing, must be very general since it must always be adjusted to the powers of the individual baby and under the doctor’s supervision.
Bowels. It is possible to train even a very young baby to have regular daily bowel movements; this training should be started when the baby is about a month old. At the same hour each day he may be laid on a padded table, or taken in the nurse’s lap, a small basin being placed against or under the buttocks, and a soap stick introduced an inch or two into the rectum and moved gently in and out. This slight irritation will usually result in the baby’s emptying his bowels almost immediately. Or he may be held on a small chamber on the nurse’s lap, in a comfortable reclining position (Fig. 163) or with his back supported against her chest, and the desire to empty the bowels stimulated by using the soap stick.
It is of greatest importance that the position and method which are adopted, be employed at exactly the same time each day. If this is done, and the baby is being properly fed, it will usually be found that, before he is many months old, his bowels will move freely and regularly without the stimulation of the soap stick and only when he is resting on the small basin or chamber. This establishment of a regular bowel movement not only simplifies the laundry work but is of great moment to the baby’s health.
Thumb-Sucking. It is scarcely necessary to remind a nurse that the baby must not be allowed to suck on an empty bottle or a pacifier nor be permitted to suck his thumb. The habits are very dirty and help to spread infections. The baby may swallow air while practicing them, with colic as a result, and he may so deform the shape of his upper jaw that, later in life, the upper and lower teeth will not meet as they should when he masticates; 483his front teeth may protrude in a disfiguring manner; and by narrowing and elongating the roof of his mouth the structure of the air passages is altered, with respiratory troubles and adenoids as a frequent consequence. Thumb-sucking may be prevented by the simple procedure of putting stiff cuffs on the baby’s elbows (Fig. 164) which make it impossible for him to reach his mouth with his thumb. These cuffs may be made by covering pieces of cardboard with muslin and attaching tapes with which to tie them on the baby’s arms. His hands may be put into celluloid or aluminum mitts, or little bags made of stiff, heavy material, which in turn are tied to his wrists, or his sleeves may be drawn down over his hands and sewed or pinned with safety pins. It should be borne in mind that a baby sometimes sucks his thumb because he is hungry or thirsty and gives up the practice when his food is increased or when he is regularly given water to drink.
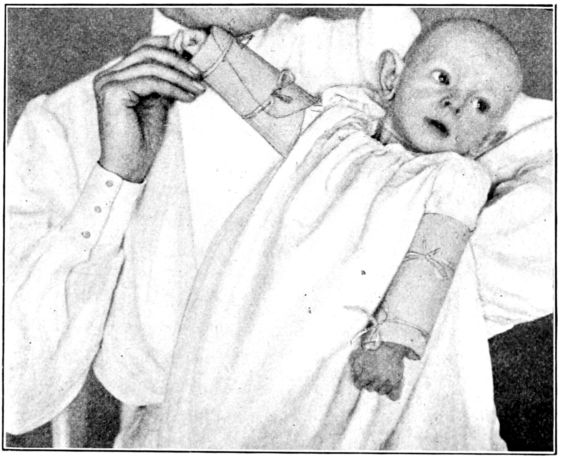
Fig. 164.—Stiff cuffs to prevent thumb sucking. (From photograph taken at Johns Hopkins Hospital.)
Ear Pulling is not uncommon among young babies and if allowed to continue a long, misshapen ear may result. This may be prevented by using a thin, close fitting cap which ties under 484the chin, or by using the same kind of elbow splints as for thumb-sucking.
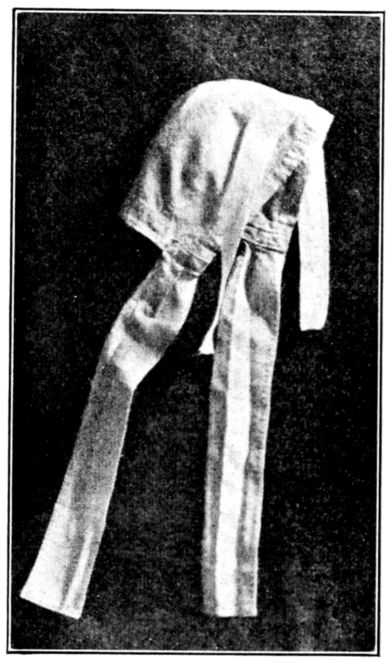
Fig. 165.—Cap, to prevent ruminating. (Devised by Miss Hammer.)
Crying. It is very easy to allow the baby to develop the crying habit, but very difficult to break it up. A baby who is properly fed, kept dry and warm but not too warm, and whose clothes are comfortable will usually cry very little if wisely handled. But a baby may cry because he is hungry, thirsty, wet, cold, over-heated, sick or in pain or simply because he wants to be taken up and entertained and has learned that the way to realize his wish is to cry. By closely observing the baby’s habits and his condition the nurse will usually be able to ascertain the cause of the crying. Very often a drink of fairly warm, sterile water will quiet him, particularly at night. But both the nurse and the mother should refrain from taking the crying baby up and carrying him or holding him when it is discovered that this attention stops his crying. Persistent crying should always be reported to the doctor, as it may have serious significance.
Ruminating. Some babies have the habit, called “ruminating,” of bringing up food; chewing it; moving it about and finally rolling it out of their mouths. Although this habit has not been recognized until comparatively recently, it is now believed to be of fairly common occurrence and often mistaken for vomiting. It is seen as a rule in precocious babies who take more interest in their surroundings than the average, more placid infant, beginning very early to fix their attention upon light, sounds and moving objects. The ruminator begins by bringing up a small amount of his last nourishment, then a little more and a little more until finally he has brought up nearly or quite all of it, apparently deriving a certain amount of pleasure and satisfaction from the procedure. Quite obviously, a continuation 485of this practice results in undernourishment, sometimes even starvation, since the baby actually retains very little if any of his food. As liquids come up more easily than fluids, the first step toward breaking up this habit is usually to give the baby more solid and concentrated food than he has been taking and to carry him about, talk to him and entertain him for about an hour after feedings, for if his attention is otherwise engaged, he is not likely to ruminate. Another efficacious measure is the use of a cap (See Fig. 165) so constructed and tied under his chin that the baby’s jaws are held tightly together and he is unable to make the movements which are necessary to rumination. (Fig. 166.)
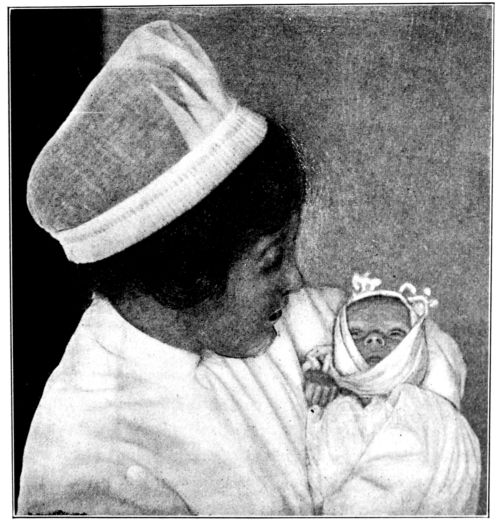
Fig. 166.—Ruminating cap applied. (From photograph taken at Johns Hopkins Hospital.)
Proper feeding is probably the most decisive single factor in the routine care of the baby.
486In order that the food be satisfactory it must be not only suitable in composition for the individual baby, but it must be clean, fresh and at the right temperature; given in suitable amounts and at suitable and regular intervals; it must be given properly—not too fast nor too slowly and it must be given under favorable conditions.
Moreover, the baby himself must be kept in a general condition which will favor the digestion and assimilation of the food that is given to him. Fresh air, suitable clothing, an even body temperature, gentle handling, proper bathing, regular sleep, freedom from excitement, fatigue and irritation, all promote the baby’s ability to use his food to advantage. Reverse influences all work against it.
The character, amount and intervals of the baby’s feeding are definitely ordered by the doctor, but the many factors which influence the baby’s nutrition are so largely a matter of nursing that the nurse has grave responsibilities in connection with his nourishment.
After other conditions have been made favorable, the factors which determine the character of the baby’s food are the kind and amount of food materials which are needed by his growing body and the powers of his digestive organs. If he is given less food than he needs at each stage of his progress he will not be properly nourished; but if he is given food materials in quantities, proportions or character which are beyond the power of his immature alimentary tract to digest, he not only will not be properly nourished but probably will be made ill.
There are three methods of nourishing the baby: breast feeding, artificial feeding and a combination of the two, termed mixed or supplementary feeding.
Breast Feeding. From all standpoints, maternal nursing under normal conditions is the most satisfactory method of infant feeding. If the breast milk is suitable it meets all of the baby’s requirements and the proportion and character of its constituents are exactly suited to his digestive powers.
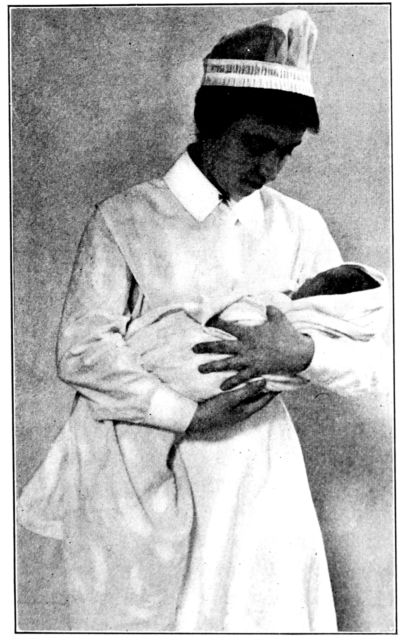
Fig. 167.—Proper method of carrying baby to support head and back. (From photograph taken at Johns Hopkins Hospital.)
In order that the nursing be entirely satisfactory, the condition of both mother and baby must be favorable to its success. The preparation and care of the mother have been described: her general condition and state of nutrition; the care and condition of her nipples, flat or retracted nipples being brought out if possible, and if not, the nursing facilitated by the use of a shield. If the baby’s diaper is wet or soiled, it should be changed before he is put to the breast, partly to make him comfortable and partly to avoid disturbing him after his feeding. His mouth is gently swabbed with boric soaked cotton, if this is ordered, he is wrapped in a little blanket and carried to his mother dry and warm and comfortable. (Fig. 167.) Although nursing is an instinct, the baby sometimes has to learn or to acquire the habit which is one reason for putting him to the breast during those first two or three days when he obtains little or no actual food. (See Chapter XVI.) As he expresses the milk by a squeezing and suction 488made possible only when the nipple is well back in his mouth, he must take into his mouth practically the entire pigmented area which surrounds the nipple. To do this he lies in the curve of his mother’s arm as she turns slightly to one side, and holds her breast away from his nostrils in order that he may breathe freely.
Sometimes even when other conditions are favorable, the baby is unable to nurse because of some physical disability. He may be too feeble; have a cleft palate or find suckling painful because of an abrasion of the mucous membrane which occurred when his mouth was bathed just after birth. The manner in which the baby nurses, therefore, may be significant and should be carefully noted and described to the doctor.
There is a difference of opinion among doctors concerning the interval between feedings which is most satisfactory. Some have the baby nurse every four hours and others every three hours during the early months of life. It is believed by some doctors that although a baby who is fed on a four-hour schedule may regain his birth weight more slowly than the baby who is fed every three hours, he suffers less from digestive disturbances and ultimately makes an entirely satisfactory gain in weight. Another point in favor of the four-hour interval is the longer period of freedom which this gives to the mother and this may influence her willingness to nurse her baby. But other doctors, both pediatricians and obstetricians, feel that the four-hour interval is too long for most babies.
Whether the baby shall nurse from one or both breasts at each feeding is another moot question. Some doctors believe that the results are better if both breasts are partially emptied at each nursing, while others feel that the function of the breasts is more satisfactorily promoted by completely emptying one breast at a time, at alternate nursings. Although the baby should pause every four or five minutes to prevent his nursing too rapidly, which is a common cause of colic, neither he nor his mother should be allowed to sleep during the nursing periods. When he has finished, he should be taken up very gently and placed in his crib and left to sleep. If he is nursing satisfactorily, he will be sleepy and contented after nursing and will sleep for two or 489three hours afterwards; he will seem generally good humored and comfortable while awake; he will have good color; gain weight steadily and have two or three normal bowel movements daily. The normal stool in breast fed babies is bright yellow, smooth and with no evidences of undigested food.
If he is not being adequately nourished, he will present exactly the opposite picture, in some or all of these respects. He will be unwilling to stop nursing after the normal length of time and will give evidence of not being satisfied when taken from his mother. He may be listless and fretful and sleep badly. He will not gain weight as he should, and he may vomit or have colic after nursing.
To ascertain whether or not such a baby is getting enough milk it is customary to weigh him, without undressing him, before and after each nursing. Each fluid ounce of food will increase his weight one ounce. If the baby is not getting a normal amount of milk at each nursing he is often given enough modified milk after each meal to supply the deficit, but at the same time an effort is made to increase the supply of breast milk by improving the mother’s personal hygiene.
The amount which the baby needs at each feeding varies, not only according to his weight and age, but also according to his vigor and activity, and must always be figured for the individual baby. A very general estimate of the amount taken by the average well baby at each feeding, is about as follows:
| First week | 1½ | to | 2½ | ounces |
| Second and third week | 2 | to | 4 | ounces |
| Fourth to ninth week | 3 | to | 4½ | ounces |
| Tenth week to fifth month | 3½ | to | 5 | ounces |
| Fifth to seventh month | 4½ | to | 6½ | ounces |
| Seventh to twelfth month | 6½ | to | 9 | ounces |
Artificial Feeding. There is no entirely adequate substitute for satisfactory maternal nursing, and any other food that is given to the young baby is at best a makeshift. Considering the baby’s delicacy, therefore, and his urgent needs, no pains should be spared to make any artificial food which is given to him as satisfactory as possible. In preparing and giving artificial food it must be borne in mind that normal breast milk:
Cows’ milk, suitably modified, is apparently the best available substitute for mother’s milk, but it must first meet certain requirements and then be handled with scrupulous cleanliness and care, if it is to be at all satisfactory.
The requirements are that the milk shall be:
All of this means that the milk must come from a herd of healthy, tuberculin-tested cows. The milk from a single cow may vary markedly from day to day but that from several cows is nearly constant. The stables and the cows must be kept clean, the udders carefully washed before each milking; the milkers themselves must wear freshly washed clothing, scrub their hands thoroughly and milk into sterile receptacles; the milk must be immediately covered and cooled to a temperature of 45° F. or 50° F. and kept there.
Milk produced under such conditions is usually described as “certified milk” and is often prescribed as infant food without being pasteurized or sterilized. But if there is any doubt about the source of the milk and the method of its handling, it should be strained into a clean receptacle through filter paper or a thick layer of absorbent cotton and subsequently boiled or pasteurized.
When the nurse is in a position to offer advice about the baby’s milk she must explain the importance of always obtaining the freshest, cleanest and purest milk possible, no matter what it costs.
Whether certified or not the milk must always be placed in the refrigerator or some other place at a temperature of 50° F. as 491soon as it is received and it must be kept cool and clean. Mother’s milk, which is being imitated, is clean and sweet and free from disease germs.
Keeping the milk cool means keeping it at a temperature of 50° F. Keeping it clean implies cleanliness of the milk itself, the utensils, the nurse’s hands and the destruction, by sterilization or pasteurization, of disease germs. Those which are likely to be present in infected milk are streptococci, tubercle bacilli, colon bacilli, germs of typhoid, diphtheria and scarlet fever.
The amounts and proportions of the constituents of the substitute feeding will be specified by the doctor, as well as the intervals between feedings and the amount to be given each time. But the doctor’s careful adjustment of the milk formula to the baby’s immediate needs and digestive powers will be set at naught unless the nurse is absolutely accurate in preparing and giving the milk.
The nurse’s invariable responsibility, therefore, is to keep the milk cool and clean and prepare and give it accurately.
The nurse will appreciate the necessity and principles of modifying cows’ milk for the human infant if she will consider for a moment, the differences between mother’s milk and cows’ milk, as indicated by the following table, and the reasons for these differences:
| Mother’s Milk. | Cows’ Milk. | |||||
|---|---|---|---|---|---|---|
| Fats | 3.5 | to | 4. % | 3.5 | to | 4. % |
| Sugar | 6.5 | to | 7.5% | 4.5 | to | 4.75% |
| Proteins | 1. | to | 1.5% | 3.5 | to | 4. % |
| Salts | .2% | .7 | to | .75% | ||
| Water | 87 | to | 88. % | 87. % | ||
It will be remembered that the tissues and bony skeleton are built by the proteins and salts (lime and phosphorus). Accordingly Nature supplies these in greater abundance to the calf, who grows so fast as to double his birth weight in about 47 days, than to the baby who scarcely doubles his within 180 days. The calf begins life with a physical need for the abundance of proteins and salts which are present in cows’ milk, and with digestive organs that can cope with them, but the baby needs less, can digest less and therefore must be given less. 492There are, of course, other and finer differences between the two milks and an attempt is sometimes made to meet these. For example, mother’s milk is slightly alkaline and cows’ milk slightly acid and the curd of cows’ milk is larger, tougher and harder to digest than that formed by mother’s milk. Accordingly some doctors add lime water to cows’ milk to make it alkaline, and render the curd softer, finer and more digestible by boiling it.
It is often not possible to give a bottle-fed baby the full 4% of fat which mother’s milk contains, and some doctors make the protein of the artificial mixture very much larger in amount than is found in human milk. The nurse will see that this is a matter which can be decided only by the physician.
Articles Needed in Preparing the Baby’s Food. A complete equipment for preparing and giving the baby’s milk should be assembled, kept in a clean place, separate from utensils in general use, and never put to any other service. A satisfactory outfit for this purpose comprises the following articles:
Utensils of enamel or aluminum ware are probably the most satisfactory ones to use as they are easily kept clean, while bottles with wide mouths and curved bottoms and inner surfaces 493can be thoroughly washed more easily than those with small necks and sharp corners. Nipples that can be turned inside out to be washed should be selected as it is almost impossible to clean thoroughly those with tubes or narrow necks. New bottles will be rendered less breakable if placed in cold water, which is gradually heated, allowed to boil for half an hour and cooled before the bottles are removed.
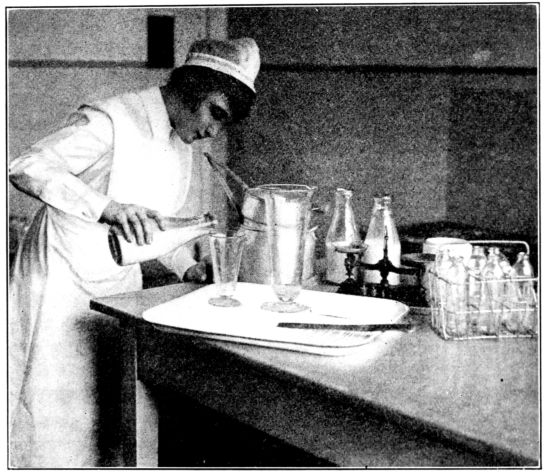
Fig. 168.—Preparing the baby’s milk. (From photograph taken at Johns Hopkins Hospital.)
The bottles should be rinsed with cold water after each feeding and then carefully washed and scrubbed with the bottle brush in hot soapsuds or borax water, containing two tablespoonsful to the pint. They may be kept full of water while not in use or rinsed with hot water and stood upside down until they are all boiled on the following morning, preparatory to being filled with the freshly prepared milk. The baby’s bottles should never be washed in dishwater nor dried on a towel. The nipples should be rinsed in cold water, turned inside out and 494scrubbed with a brush, in hot soapsuds or borax water; rinsed and placed in a jar ready to be boiled with the bottles.
Preparation of Milk. The full quantity of milk which the baby will take in the course of twenty-four hours is prepared at one time and the prescribed amount for each feeding poured into as many separate bottles as there will be feedings. (Fig. 168.)
The nurse should first boil for five minutes all of the articles that will come in contact with the milk, including the full number of bottles and nipples and the jars in which the nipples are kept; remove them with the long-handled spoon without touching the edges or inner surfaces and place them on a clean table, dropping the nipples into one of the sterile jars.
She should wash the mouth of the milk bottle before removing the cap and pour the amount which the formula calls for into the sterile pitcher. To this is added the sterile water in which the sugar has been dissolved in the glass graduate, and the potato or barley water, the lime water or soda solution as ordered. This mixture is thoroughly stirred and the amount for one feeding at a time measured in the graduate and poured into the specified number of bottles which are then stoppered.
If certified milk is used for the milk mixture it is often given to the baby without being pasteurized, in which case the bottles are placed in the refrigerator as soon as they are filled and stoppered. Very frequently, however, the milk is sterilized or pasteurized. The nurse will feel surer of keeping the mouths of the bottles clean if she covers them with squares of gauze or muslin before they are sterilized, holding the caps in place with tapes or rubber bands. Pasteurization as applied to infant feeding consists of heating the milk to 140–165° F. and keeping it at that temperature 20 to 30 minutes.
There are many excellent pasteurizers for home use on the market, or entirely satisfactory results may be obtained by using a wire bottle rack (See Fig. 168) and the large kettle already provided. One method is to place the rack containing the bottles in the kettle which is filled with cold water to a level a little above the top of the milk in the bottles, and allow the water to come to the boiling point. The kettle is removed from the fire, 495covered tightly and the bottles allowed to stand in the hot water for twenty minutes. Cold water is then run into the kettle to cool the milk gradually and avoid breaking the bottles, after which they are placed in the refrigerator, well or spring-house and kept at a temperature of 50° F. until they are taken out one at a time for feedings. If a wire rack is not available the bottles may be stood on a saucer or a thick pad of folded newspapers in the bottom of the kettle.
Pasteurization does not destroy all germs that may be in the milk, but it kills the more important ones and apparently impairs the nutritive and protective properties of the milk less than boiling. However, pasteurized milk must be kept cold and must be used within twenty-four hours, for the nurse will recall that aging of milk is quite as undesirable as souring.
Scalding is another method of destroying germs in milk. The milk is placed in an open vessel and the temperature raised to about 180° F., or until bubbles appear around the edge and the milk steams in the centre, after which it is cooled and kept at a temperature of 50° F.
Many doctors prefer to have the baby’s milk boiled, since boiling insures absolute sterilization and also renders the curd more digestible. Other changes are produced by boiling, however, which make it important to add an anti-scorbutic and cod-liver oil to the baby’s diet at an early date.
Milk may be boiled directly over the flame for a time varying from three to forty-five minutes, or it may be placed in a double boiler, the water in the lower receptacle being cold, and allowed to remain until the water has boiled from six to forty-five minutes. All of these points are definitely specified by the doctor.
When milk is boiled or scalded the other ingredients are added beforehand, as a rule, after which it is measured and poured into the bottles. Or the milk mixture may be poured into the bottles as for pasteurization and the bottles kept in the actively boiling water for any desired length of time.
Giving the Baby His Bottle. At feeding time, the bottle should be taken from the refrigerator, the stopper removed and a nipple taken up by the margin and put on the bottle without touching the mouthpiece. The milk is brought to a temperature 496of about 100° F. by standing the bottle in a deep cup or kettle of warm water and placing it on the fire. The temperature of the milk may be tested by dropping a few drops on the inner side of the wrist or forearm where it should feel warm but not hot. This dropping will also indicate if the hole in the nipple is of the proper size to allow the milk to drop rapidly in clean drops but not to pour. If the hole is too small, the drops will be small and infrequent and the baby will be obliged to work too hard to obtain it; while if the hole is too large the baby will feed too rapidly and may have colic as a result.
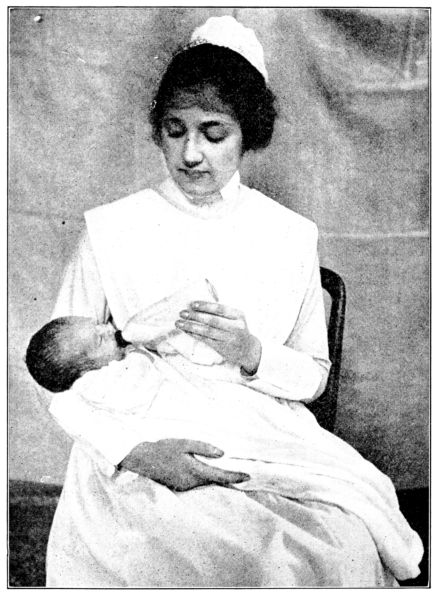
Fig. 169.—Proper position in which to hold baby and bottle during feeding.
497The baby’s diaper should be changed if it is soiled or wet before he is given the bottle and he should be held comfortably in a reclining position on the nurse’s arm while she holds the bottle with her free hand. (Fig. 169.) The bottle should be inclined sufficiently to keep the neck full of milk; otherwise the baby may draw in air as he nurses. He should be kept awake while feeding but he should be allowed to pause every three or four minutes in order not to take his milk too rapidly. Not less than ten nor more than twenty minutes is devoted to a feeding, as a rule, and if the baby refuses a part of his milk, it should be thrown away; never warmed over for another time.
Fig. 170.—Holding the baby upright and gently patting his back to bring up air immediately after feeding.
After being fed, the baby should be held upright against the nurse’s shoulder for a moment or two (Fig. 170), and ever 498so gently patted on the back to help bring up any air which he may have swallowed. He should on no account be rocked or played with after taking the bottle, but should be placed gently in his crib, warm and dry and left alone to sleep. Turning him or moving him about even to the extent of changing his diaper at this time may cause vomiting.
The evidences of satisfactory and unsatisfactory feeding in the bottle-fed baby are about the same as in the baby who is fed at the breast, except that the gain in weight on artificial food may be a little slower and less steady than on maternal nursing; the stools have a characteristic sour odor; are a little lighter in color and may contain white lumps of undigested fat; are usually dryer than in breast-feeding and may be formed in even a very young baby.
It is fairly generally agreed that all babies, whether breast-fed or on the bottle, require a certain amount of cool boiled water to drink between feedings. A small amount is given at first and gradually increased according to the doctor’s instructions, and it may be given from a bottle, a medicine dropper or poured slowly from the tip of a teaspoon.
Ingredients of the Baby’s Food. In referring to the ingredients of the baby’s food we cannot use the terms “sugar” or “milk” as though they indicated definite and unvarying materials.
There are three kinds of sugar which are commonly used in modified milk: cane or granulated sugar; lactose or milk sugar and maltose. Cane sugar, the one most widely used, is the least expensive of the three and it apparently is satisfactory for most babies. Lactose is fairly expensive and while it causes diarrhea in some babies, others digest it more easily than cane sugar. Lactose is lighter than cane sugar, three spoonfuls being equal in weight to two of cane sugar. The maltose-dextrine preparations are easily digested and somewhat laxative. Some babies gain more rapidly when maltose constitutes part of the sugar in their food than when only lactose is used.
The question of milk is somewhat complicated and though the doctor will specify what percentage of fat shall be in the milk which is used in each case, the nurse must know how to 499obtain it from the milk at her disposal. If the formula is made up with “whole milk,” which contains 4 per cent. fat, the bottle in which it was delivered should be turned upside down and shaken vigorously in order that the cream which has risen to the top may be redistributed evenly throughout the fluid.
If the doctor employs what is termed “percentage feeding,” he may use whole milk, skimmed milk, or top milk. What he is endeavoring to do is to prepare a food which contains definite known percentages of the different ingredients, fat, carbohydrates and protein. Where a mixture is desired which contains more fat than it does protein, the milk to be employed is obtained by discarding a certain amount from the bottom of the jar of milk, the remainder being then called “top milk.” When he wishes the fat to be lower than the protein percentage, he discards some of the top milk in the jar, using the rest, which is then a partially skimmed milk. The upper 2 ounces in a quart bottle of milk contains 24 per cent. fat; the upper 8 ounces is 12 per cent. fat; the upper 16 ounces is 8 per cent. fat and the upper 24 ounces is 5 per cent. fat. If the formula calls for 6 ounces of the upper 8 ounces of milk, therefore, the nurse will see that it is very important that she remove the full 8 ounces and use 6 ounces of the milk which she has removed and not simply take the upper 6 ounces, as this would contain a higher percentage of fat than is ordered. (Figs. 171, 172, Dr. Griffith’s tables of fat percentages.)
Top milk may be removed by tipping the bottle gradually and slowly pouring the designated amount into a measuring glass, or it may be removed by pushing a cream dipper, especially made for this purpose and holding one ounce, down into the bottle until the cream flows in. Another method is to syphon off the lower milk through a bent glass tube, leaving in the bottle the desired amount of top milk.
Many doctors feed the baby according to his caloric needs and prepare the formula from whole milk, sugar and water, determining the amounts of each according to the age and weight of the baby.
Under any condition it is so necessary that the amount and composition of each baby’s food be adjusted to his needs, that it is not considered possible to make out any formulae or feeding schedules which would be safe or satisfactory for general use.
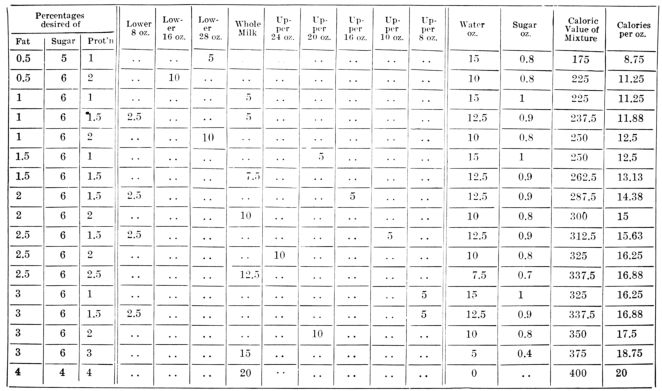
| Percentages desired of | Lower 8 oz. | Lower 16 oz. | Lower 28 oz. | Whole Milk | Upper 24 oz. | Upper 20 oz. | Upper 16 oz. | Upper 10 oz. | Upper 8 oz. | Water oz. | Sugar oz. | Caloric Value of Mixture | Calories per oz. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fat | Sugar | Prot’n | |||||||||||||
| 0.5 | 5 | 1 | 5 | 15 | 0.8 | 175 | 8.75 | ||||||||
| 0.5 | 6 | 2 | 10 | 10 | 0.8 | 225 | 11.25 | ||||||||
| 1 | 6 | 1 | 5 | 15 | 1 | 225 | 11.25 | ||||||||
| 1 | 6 | 1.5 | 2.5 | 5 | 12.5 | 0.9 | 237.5 | 11.88 | |||||||
| 1 | 6 | 2 | 10 | 10 | 0.8 | 250 | 12.5 | ||||||||
| 1.5 | 6 | 1 | 5 | 15 | 1 | 250 | 12.5 | ||||||||
| 1.5 | 6 | 1.5 | 7.5 | 12.5 | 0.9 | 262.5 | 13.13 | ||||||||
| 2 | 6 | 1.5 | 2.5 | 5 | 12.5 | 0.9 | 287.5 | 14.38 | |||||||
| 2 | 6 | 2 | 10 | 10 | 0.8 | 300 | 15 | ||||||||
| 2.5 | 6 | 1.5 | 2.5 | 5 | 12.5 | 0.9 | 312.5 | 15.63 | |||||||
| 2.5 | 6 | 2 | 10 | 10 | 0.8 | 325 | 16.25 | ||||||||
| 2.5 | 6 | 2.5 | 12.5 | 7.5 | 0.7 | 337.5 | 16.88 | ||||||||
| 3 | 6 | 1 | 5 | 15 | 1 | 325 | 16.25 | ||||||||
| 3 | 6 | 1.5 | 2.5 | 5 | 12.5 | 0.9 | 337.5 | 16.88 | |||||||
| 3 | 6 | 2 | 10 | 10 | 0.8 | 350 | 17.5 | ||||||||
| 3 | 6 | 3 | 15 | 5 | 0.4 | 375 | 18.75 | ||||||||
| 4 | 4 | 4 | 20 | 0 | 400 | 20 | |||||||||
| Fig. 171. Table of fat percentages, by permission, from “The Diseases of Infants and Children,” by J. P. Crozer Griffith, M.D. | |||||||||||||||
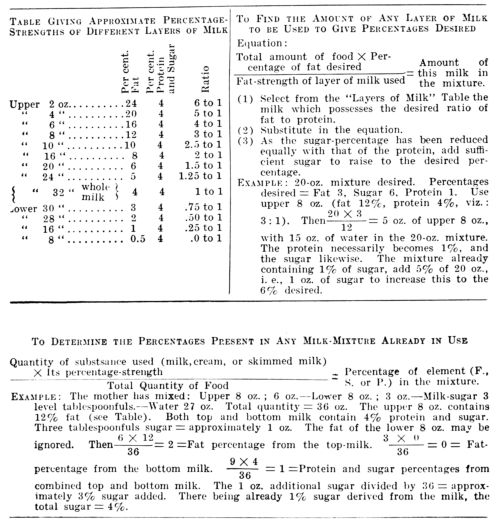
| Table Giving Approximate Percentage-Strengths of Different Layers of Milk | |||
|---|---|---|---|
| Per cent. Fat | Per cent. Protein and Sugar | Ratio | |
| Upper 2 oz. | 24 | 4 | 6 to 1 |
| Upper 4 oz. | 20 | 4 | 5 to 1 |
| Upper 6 oz. | 16 | 4 | 4 to 1 |
| Upper 8 oz. | 12 | 4 | 3 to 1 |
| Upper 10 oz. | 10 | 4 | 2.5 to 1 |
| Upper 16 oz. | 8 | 4 | 2 to 1 |
| Upper 20 oz. | 6 | 4 | 1.5 to 1 |
| Upper 24 oz. | 5 | 4 | 1.25 to 1 |
| Upper 32 oz. whole milk | 4 | 4 | 1 to 1 |
| Lower 30 oz. | 3 | 4 | .75 to 1 |
| Lower 28 oz. | 2 | 4 | .50 to 1 |
| Lower 16 oz. | 1 | 4 | .25 to 1 |
| Lower 8 oz. | 0.5 | 4 | .0 to 1 |
Equation:
| Total amount of food × Percentage of fat desired | = Amount of this milk in the mixture. |
| Fat-strength of layer of milk used |
(1) Select from the “Layers of Milk” Table the milk which possesses the desired ratio of fat to protein.
(2) Substitute in the equation.
(3) As the sugar-percentage has been reduced equally with that of the protein, add sufficient sugar to raise to the desired percentage.
Example: 20–oz. mixture desired. Percentages
desired = Fat 3, Sugar 6, Protein 1. Use
upper 8 oz. (fat 12%, protein 4%, viz.:
3:1). Then 20 × 3
12 = 5 oz. of upper 8 oz.,
with 15 oz. of water in the 20–oz. mixture.
The protein necessarily becomes 1%, and
the sugar likewise. The mixture already
containing 1% of sugar, add 5% of 20 oz.,
i. e., 1 oz. of sugar to increase this to the
6% desired.
| Quantity of substance used (milk,cream, or skimmed milk)× Its percentage-strength | = Percentage of element (F., S. or P. in the mixture.) |
| Total Quantity of Food |
Example: The mother has mixed: Upper 8 oz.; 6 oz.—Lower 8 oz.; 3 oz.—Milk-sugar 3
level tablespoonfuls.—Water 27 oz. Total quantity = 36 oz. The upper 8 oz. contains
12% fat (see Table). Both top and bottom milk contain 4% protein and sugar.
Three tablespoonfuls sugar = approximately 1 oz. The fat of the lower 8 oz. may be
ignored. Then 6 × 12
36 = 2 = Fat percentage from the top-milk. 3 × 0
36 = 0 = Fat-percentage
from the bottom milk. 9 × 4
36 = 1 = Protein and sugar percentages
from combined top and bottom milk. The 1 oz. additional sugar divided by 36 = approximately
3% sugar added. There being already 1% sugar derived from the milk, the
total sugar = 4%.
Moreover, it does not ordinarily devolve upon the nurse to do more than prepare and give the baby’s food as ordered by the doctor, but situations sometimes do arise when the doctor is not within reach which the nurse must meet as best she can. In such an emergency she might be guided by the following suggestions contained in a pamphlet entitled, “Save the Babies,” prepared by Dr. L. Emmet Holt and Dr. H. K. L. Shaw and published by the American Medical Association, remembering that they are intended for the average, normal baby and are not necessarily suitable for all babies:
502“The simplest plan is to use whole milk (from a shaken bottle) which is to be diluted according to the child’s age and digestion.
“Beginning on the third day, the average baby should be given 3 ounces of milk daily, diluted with seven ounces of water. To this should be added one tablespoonful of lime water and 2 level teaspoonfuls of sugar. This should be given in seven feedings.
“At one week, the average child requires 5 ounces of milk daily, which should be diluted with 10 ounces of water. To this should be added 1½ even tablespoonfuls of sugar and one ounce of lime water. This should be given in seven feedings.
“The milk should be increased by ½ ounce about every 4 days.
“The water should be increased by ½ ounce about every 8 days.
“At three months the average child requires 16 ounces of milk daily, which should be diluted with 16 ounces of water. To this should be added 3 tablespoonfuls of sugar and 2 ounces of lime water. This should be given in 6 feedings.
“The milk should be increased by ½ ounce about every 6 days.
“The water should be reduced by ½ ounce about every 2 weeks.
“At 6 months the average child requires 24 ounces of milk daily, which should be diluted with 12 ounces of water. To this should be added 2 ounces of lime water and 3 even tablespoonfuls of sugar. This should be given in 5 feedings.
“The amount of milk should be increased by ½ ounce every week.
“The milk should be increased only if the child is hungry and digesting his food well. It should not be increased unless he is hungry, nor if he is suffering from indigestion even though he seems hungry.
“At 9 months, the average child requires 30 ounces of milk daily, which should be diluted with 10 ounces of water. To this should be added 2 even tablespoonfuls of sugar and 2 ounces of lime water. This should be given in 5 feedings.
“The sugar added may be milk sugar or, if this cannot be obtained, cane (granulated) sugar or maltose (malt sugar).
“At first plain water should be used to dilute the milk.
“At three months, sometimes earlier, weak barley water may be used in the place of plain water; it is made with ½ level tablespoonful of barley flour to 16 ounces of water and cooked 20 minutes.
“At six months the barley flour may be increased to 1½ even tablespoonfuls, cooked in the 12 ounces of water.
“At nine months, the barley flour may be increased to 3 level tablespoonfuls, cooked in the 8 ounces of water.
“A very large baby may require a little more milk than that allowed in these formulas. A small delicate baby will require less than the milk allowed in the formulas.”
These formulas may be tabulated as follows:
| 503 | ||||||||
| Age | Milk | Water | Barley-Water | Lime-Water | Sugar | No. of feedings | Hours | |
|---|---|---|---|---|---|---|---|---|
| Day | Night | |||||||
| 3–7 days | 3 ozs. | 7 ozs. | 16 ozs. | ½ ozs. | 2 teaspoons | 7 | 6–9–12–3–6 | 10–2 |
| 2d week | 5 ozs. | 10 ozs. | 15 ozs. | 1 ozs. | 1½ tablespoons | 7 | 6–9–12–3–6 | 10–2 |
| 3d week | 6 ozs. | 10½ ozs. | 14 ozs. | 1 ozs. | 1½ tablespoons | 7 | 6–9–12–3–6 | 10–2 |
| 1 month | 7 ozs. | 11 ozs. | 12 ozs. | 1 ozs. | 2 tablespoons | 7 | 6–9–12–3–6 | 10–2 |
| 2 month | 11 ozs. | 13 ozs. | 12 ozs. | 1½ ozs. | 2½ tablespoons | 7 | 6–9–12–3–6 | 10–2 |
| 3 month | 16 ozs. | 11 ozs. | 2 ozs. | 3 tablespoons | 7 | 6–9–12–3–6 | 10–2 | |
| 4 month | 19 ozs. | 10 ozs. | 2 ozs. | 3 tablespoons | 6 | 6–9–12–3–6 | 10 | |
| 5 month | 21½ ozs. | 2 ozs. | 3 tablespoons | 6 | 6–9–12–3–6 | 10 | ||
| 6 month | 24 ozs. | 2 ozs. | 3 tablespoons | 5 | 6–10–2–6 | 10 | ||
| 7 month | 26 ozs. | 2 ozs. | 3 tablespoons | 5 | 6–10–2–6 | 10 | ||
| 8 month | 28 ozs. | 2 ozs. | 2½ tablespoons | 5 | 6–10–2–6 | 10 | ||
| 9 month | 30 ozs. | 2 ozs. | 2 tablespoons | 5 | 6–10–2–6 | 10 | ||
Mixed Feeding. Under some conditions the breast-fed baby is given also a certain amount of modified milk, and this combination of natural and artificial feeding is termed mixed or supplementary feeding.
A deficiency in the breast milk, ascertained by weighing the baby before and after each nursing, may be supplied by following each nursing with a bottle feeding; or one or two breast-feedings, in the course of the day may be replaced by entire bottle feedings. In any case the milk mixture to be used as supplementary feeding is prepared with exactly the same painstaking care as is the milk for entire artificial feeding.
If supplementary food is given because of an inadequate supply of breast milk, it is of great importance that the baby be put to the breast regularly, no matter how little food he obtains, for his suckling is the best possible means of stimulating the breasts to secrete more milk and of equal importance is the fact that they will tend to dry up if the baby nurses less than about five times in twenty-four hours. Moreover, even a little breast milk is valuable to him and he should have the benefit of all there is to be had.
An entire bottle feeding is sometimes given to a baby who is nursing satisfactorily at the breast, in order to give his mother an opportunity to take longer outings than are possible between the regular nursings. And sometimes it is to the mother’s advantage, and therefore to the baby’s, to give him a bottle during the night and thus allow her to sleep undisturbed.
Since the baby’s food is prescribed by the doctor, the nurse has little concern with the various proprietary baby foods and 504the canned and powdered milks which are so persuasively advertised to young mothers. It is hoped, however, that the discussions on nutrition in general and on baby feeding in particular, have made it clear to the nurse that these foods cannot be expected to be satisfactory if used as a sole article of diet throughout the bottle-feeding period.
There are many times and circumstances, however, when the temporary use of a prepared infant food or canned or powdered milk is advantageous. In some cases of intestinal disturbance, for instance, or while the mother is traveling and is unable to have freshly prepared milk formulas supplied to her along the way; during the summer, while staying at a hotel or boarding house where the freshness, cleanliness or purity of the milk are uncertain; or during a sudden shortage of fresh milk, as may occur during a strike or severe storm when transportation is interfered with, a proprietary food may be a great boon.
If the nurse is confronted with the necessity of choosing and making temporary use of a prepared food she may be guided by considering the general principles of baby feeding and the character of the materials at her disposal.
The Proprietary Foods may be divided into two general groups: one kind contains milk powder and is usually added to water while the other consists largely of sugar and starch and is added to fresh milk before being given to the baby.
Canned Milk is of two kinds; evaporated, which is unsweetened, and condensed, which is sweetened. Evaporated milk is whole milk from which part of the water has been removed, the milk then being canned and sterilized. The addition of water to evaporated milk restores it to the composition of whole milk in many respects, but it is still milk that has been heated. Condensed milk is evaporated milk to which cane sugar has been added to aid in its preservation. Since bacteria do not grow well in highly sweetened foods, it is not necessary to bring sweetened condensed milk to as high a temperature as the unsweetened product, to prevent subsequent bacterial decomposition. The high percentage of sugar in condensed milk quite obviously renders it unsuitable for continuous use as the sole article in a baby’s dietary.
505Milk Powders or Dried Milks are prepared by rapidly evaporating the water from whole milk, skimmed milk or partly skimmed milk, leaving the solid constituents in the form of a light, white powder. Milk powder readily dissolves in water, forming a “reconstructed milk” which closely resembles the fresh milk from which it was prepared. But it must not be forgotten that reconstructed milk has been heated. Many doctors consider whole milk powder the most satisfactory form of preserved milk which is available for baby food. Should it be used, however, the importance of keeping it tightly covered and in a cold place must be recognized, for the presence of fat renders it likely to become rancid if not kept cold.
Barley Water, sometimes used to dilute whole milk, is made by mixing the barley flour to a smooth paste in cold water, adding boiling water and boiling for twenty minutes or cooking in a double boiler for an hour, straining and adding enough water to replace the amount lost in cooking. The proportions for different ages are as follows:
Potato Water. One tablespoonful of thoroughly boiled potato is mashed into one pint of the water in which the potato was boiled and carefully strained.
Spinach. Spinach is carefully washed, steamed for half an hour and mashed through a fine sieve. It is sometimes started at the sixth month; one teaspoonful daily, gradually increased to one or two tablespoonfuls daily.
Orange Juice. The orange should be dipped in boiling water and wiped on a clean towel before being cut and squeezed, to avoid possible infection of juice. It is usually given to babies getting heated milk, sometimes as young as one month old. It is carefully strained and started gradually by giving one teaspoonful in water once or twice daily between feedings and 506increasing to ½ or 1 ounce by the sixth month and 1½ to 2 ounces by the end of the first year.
Infusion of Orange Peel. This is sometimes used instead of orange juice, and is made by boiling one ounce of finely grated orange peel in two ounces of water, adding a little sugar to counteract the bitter taste and adding enough sterile water to bring it up to two ounces.
Tomato Juice. Canned tomato strained through a fine sieve, is sometimes given to a baby a few weeks old, starting with one dram and gradually increasing to four to six ounces daily.
Whey. One quart of whole milk heated to 98° F. or 100° F. and one-half ounce of liquid rennet or one junket tablet stirred into it and allowed to stand half an hour or until firm and solid, is poured into a cheese-cloth bag and allowed to drain for about an hour without being squeezed.
Protein Milk. The curd from one quart of milk, which remains after the whey is drained, as directed above, is mashed through cheese-cloth in a fine wire sieve, with a potato-masher or bowl of a spoon and the curd washed through with one pint of water. A pint of buttermilk is added and the mixture boiled while being stirred constantly. This is sometimes given in diarrhea.
Beef Juice. One pound of thick round steak, slightly broiled, is cut into small pieces and the juice expressed with a meat press or a lemon squeezer, the amount varying from 2 to 3 ounces. It may be diluted with an equal amount of warm water, or slightly warmed by being placed in a cup standing in hot water, and salted to taste.
Broths. One pound of lean meat, all fat and gristle removed, is allowed to one pint of water. The meat is cut finely and put on in cold water, heated slowly and allowed to simmer for three or four hours, when water is added to replace what was lost in cooking. It is strained, the fat removed and slightly salted.
Oatmeal Water. Two level tablespoonfuls of oatmeal in a pint of boiling water is cooked in a double-boiler for two hours, strained and enough boiling water added to replace the amount lost in cooking.
Fig. 173.—The baby will travel comfortably in a basket converted into a bed. (Courtesy of the Maternity Centre Association.)
The difficulties of traveling with a young baby may be greatly lessened by making certain preparations. If the baby is bottle-fed, the preparations will depend upon the length of the journey and whether or not it will be possible to have freshly prepared feedings, for each twenty-four hours, put on the train from laboratories along the way. If this is not possible and the journey is not to take more than twenty-four hours, the entire quantity of food, ice cold, may be carried in a thermos bottle. The requisite number of sterile nursing bottles may be taken or one bottle which is boiled before each feeding. Or the milk may be prepared as usual and the bottles packed in a portable refrigerator. Such a refrigerator may be bought or one may be improvised. The bottles are placed in a covered pail and packed solidly in crushed ice; this is placed in a second pail or a box with a diameter which is at least two inches larger than the inner pail and the space between the two packed firmly with sawdust. Several thicknesses of newspapers should be pressed down over the top and a tight cover fitted to the outer receptacle.
The sterile nipples may be taken in a sterile jar and a deep cup or kettle will be needed in which to warm the bottle before each feeding. It is usually possible to obtain water on the train which is hot enough for this, or cans of solid alcohol, a stand and a metal tray may be added to the traveling outfit. If fresh formulae cannot be delivered to the train, daily, and the journey is to last more than twenty-four hours, one of the proprietary foods or a powdered milk will often prove to be a satisfactory solution to the problem of feeding.
508The baby will usually travel more comfortably and sleep better if he is carried in a basket. A large market basket with a handle or a small clothes basket will serve. It may be lined with a sheet or a blanket; have a small hair pillow or folded blanket in the bottom and be made up like a crib. (Fig. 173.) If this basket stands on the car seat during the day, and on the foot of the nurse’s berth at night, the baby will be cleaner, quieter and less exposed to drafts than if carried in the arms.
All of the precautions and gentleness which are necessary in the care of the normal baby, born at term, must be greatly increased in caring for the baby who is born prematurely.
As was explained in Chapter III the premature baby’s prospects of living increase with the length of his uterine life, and it is often possible to estimate this by measuring and weighing him. During the last five months the child’s length in centimetres divided by five gives the month of pregnancy, according to the following table by Dr. Williams:[15]
But consideration of the baby’s weight is also of importance when attempting to forecast his chances of living. A baby weighing less than 2500 grams or about 5½ pounds should be regarded, and treated, as premature, unless it is more than 45 centimetres, or about 18 inches long. This length would indicate greater maturity, and therefore greater viability than would be expected from the weight. A baby weighing less than 1500 grams (3 pounds and 5 ounces) can scarcely be expected to live.
The premature baby is not only small, but in general is imperfectly developed, having slenderer powers than the full-term 509baby and at the same time much greater needs. His respiratory and digestive organs are less ready to function than in the full-term baby; his muscles and nerves are feeble; his heat-producing mechanism is unstable and yet there is an excessive radiation of body heat through the relatively large area of skin.
Accordingly, the baby who has been deprived of those valuable last weeks of growth and development is small and limp; lies quietly most of the time and moves very feebly if at all. He is often too weak to nurse at the breast and may swallow with difficulty. His temperature is low, his respirations irregular and he is frequently cyanotic.
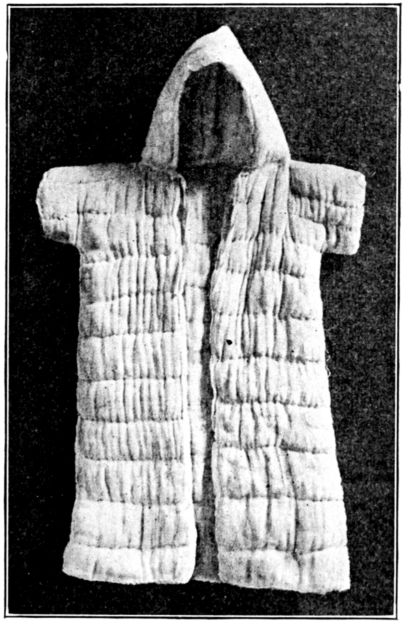
Fig. 174.—Quilted robe, with hood, for the premature baby.
The care of this frail little body practically resolves itself into:
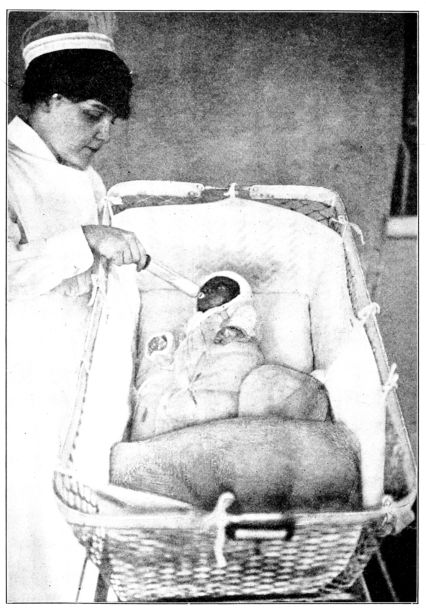
Fig. 175.—Premature baby in basket lined with quilted pad; wearing quilted robe and being fed from a Boston feeder. The blanket is turned back showing hot-water bag. (From photograph taken at Johns Hopkins Hospital.)
511To maintain a normal body temperature it is necessary to give special thought to the baby’s clothing, bed and room. He should be oiled with warm olive oil and entirely wrapped in cotton batting or flannel or enveloped in a quilted garment, with hood attached, made of cheese-cloth or flannel and cotton batting. (Fig. 174.) Diapers are often omitted in caring for very feeble babies, a pad of cotton being slipped under the buttocks instead as this may be changed with less disturbance to the baby than a diaper.
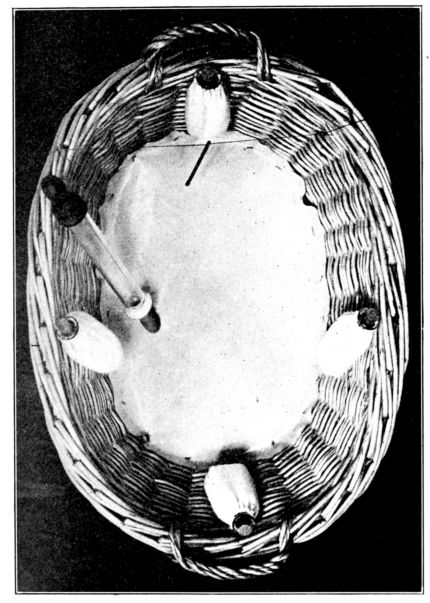
Fig. 176.—Model of improvised bed for premature baby: closely woven clothes basket with padded bottom and four, flannel-covered bottles of hot water attached to the sides. Thermometer and feeder are shown in basket. (By courtesy of Dr. Alan Brown, Hospital for Sick Children, Toronto.)
512His bed consists of a box or basket, with the bottom well padded with several inches of cotton, a small pillow or a soft blanket folded to the proper size, covered with rubber or oiled muslin and a cotton sheet. The sides of the basket should be lined with heavy quilted material (Fig. 175), to shut out drafts and help to preserve an even temperature of the air immediately around the baby. A flannel covered hot-water bag at 110° F. may be placed beside the baby, or two, three or four glass bottles, each holding about a pint, containing water at 100° F. and securely stoppered, may be hung in the corners of the basket. (Fig. 176.) A thermometer should hang in the basket also, and the temperature kept between 80° F. and 90° F. It is easier to keep the temperature even if the bottles are filled in rotation instead of all at the same time.
The amount of heat needed around the baby is decided by taking his temperature (by rectum) at regular intervals; supplying more heat if the temperature is low and less if it is at or above normal. Some doctors have the temperature taken every four hours; others twice daily. As the baby grows able to maintain a temperature of 98° F. to 100° F., unassisted, the surrounding heat is gradually reduced and finally removed, and flannel clothing replaces the quilted robe.
In many hospitals there are special rooms for premature babies, which are divided by glass partitions into cubicles so that each baby is in a three-sided enclosure. The rooms are usually darkened to save the baby from the needless irritation of light, and are supplied with constantly changing fresh, moist, filtered air, the temperature being kept at from 80° F. to 90° F.
In a patient’s home or in a hospital where there is no special room for premature babies, a cubicle may be improvised by placing the basket in which the baby lies, in the corner of a room and placing a screen parallel with one of the walls. Such a room should be darkened, well ventilated and have in it a large open vessel of water.
Since the premature baby’s lungs are not fully expanded, respirations are likely to be shallow and irregular, thus failing to supply the amount of oxygen which he sorely needs. As crying inevitably involves deep breathing, it is a common practice 513to make the premature baby cry at regular intervals during the day in order to promote the respiratory function. Dr. Griffith further recommends plunging the baby into a mustard bath at 100° F. or 105° F. if necessary to make him cry vigorously. It is also important to turn the premature baby from side to side, several times a day to prevent fluid from collecting in the lowermost part of the lung, a condition favorable to the development of pneumonia.
In feeding premature babies, breast milk is ordinarily the most desirable food. If the baby is too feeble to nurse, as frequently occurs, the milk may be expressed from the breast of his mother or a wet nurse, by stripping or pumping, into a sterile receptacle, and if not used immediately it should be covered and placed in the refrigerator. Breast milk is sometimes used whole and sometimes diluted with water, and is given by gavage if the baby is very feeble; from a medicine dropper or a special feeder. Such a feeder consists of a glass tube with a small nipple on one end and a rubber bulb on the other, by means of which the milk may be gently expressed into the baby’s mouth, thus minimizing his effort to obtain it. (See Fig. 175.)
The amount and intervals for feeding the premature baby have to be adjusted to the individual with even greater care than for a normal baby, for he needs more fuel and building material, because of his imperfect development and yet because of that same imperfect development his digestive powers are feebler than those of the full-term baby. During the first day or two, he is sometimes given nothing but water or sugar solution, the milk being started gradually when the baby is from thirty-six to forty-eight hours old. He may be given a very small quantity every two hours, or he may be fed at three- or four-hour intervals, depending entirely upon his condition and progress. It is usually considered very important for the premature baby to have sterile water or sugar solution to drink between feedings, and this is given in the same manner as his milk.
Unlike the normal baby he is not taken from his bed to be fed, unless he nurses at the breast.
The premature baby is weighed as often as is safe for him, 514since the suitability of his food is largely indicated by changes in his weight. But sometimes very young and feeble babies are weighed only once or twice a week because of the inadvisability of disturbing them more frequently.
Avoidance of fatigue and the conservation of the premature baby’s limited strength and energy are accomplished through reducing his muscular activity to the minimum, by very little and very gentle handling; and by minimizing his loss of energy in the form of heat by keeping the little body warm and quiet.
In this connection the daily bath is of considerable importance. It almost always consists of sponging the baby with warm olive oil as he lies in his bed, and with the least possible exposure and turning. It is given every day or every second or third day according to his condition. The eyes are wiped with boric pledgets and the nostrils with spirals of cotton dipped in oil. The buttocks are wiped with an oil sponge each time the diaper is changed.
The premature baby is very susceptible to infection and strongly predisposed to pneumonia. Infection in general is guarded against by having everything that comes in contact with the baby scrupulously clean; protecting him from drafts, chilling and dust; allowing no one with a suspicion of a cold to come near him and by the nurse’s wearing a clean gown and protecting her nose and mouth with a gauze mask while attending him.
The dangers of infancy are greatly increased in summer, more babies dying during the hot months than any other time during the year. The cause of these deaths is variously termed summer complaint, summer diarrhea, acute gastro-enteritis and cholera infantum, and is due to infected or decomposing food or both.
Clearly this malady is practically preventable through care.
Although such care as has been described in the preceding pages largely constitutes the prevention of the much-to-be-dreaded summer diarrhea, there are a few extra precautions 515and safeguards with which the nurse must surround her little patient during the warm weather.
She must bear in mind the character of the illness to be avoided: indigestion associated with infection.
It becomes almost a matter of life or death, then, to give the baby clean, suitable food and avoid deranging his digestion.
Babies suffer from the heat more than adults do and are often excessively irritated and exhausted on warm days. And this overheating, exhaustion and restlessness are of themselves enough to affect his digestion.
Accordingly the scourge of summer diarrhea is prevented by giving the baby proper food and keeping him clean, cool and quiet.
The baby should have maternal nursing if possible, for breast-fed babies fall victim to summer diarrhea much less frequently than bottle-fed babies. He should be fed with absolute regularity, and as a rule, no matter what the nature of his food, it is reduced one-quarter to one-third in amount during very warm weather and he is given an increased amount of cool boiled water to drink. His weight may increase very slightly, or even stand still for a short time, as a result of his decreased food, but this is not usually deplored, if he keeps well, for the important thing is to avoid digestive disturbances while the weather is warm.
Cleanliness, as at other times, applies to the baby’s food, clothing and surroundings. Many doctors think it safer to have all milk boiled during the summer, and of course require flawless technique in its preparation and administration. The baby’s soiled napkins should be placed immediately in a covered receptacle containing water, and not left for even a moment where they can be reached by flies. They should be washed, boiled and dried in the open air and sunshine as promptly as possible.
The baby should be protected from flies and mosquitoes by screens in the windows and netting over his crib and carriage, both because they make him restless and irritable and because flies particularly are carriers of filth and disease—the kind of disease that kills so many babies during the summer. Accordingly the nurse must always regard flies with a deadly fear.
The baby should be kept away from dusty places and from 516cats and dogs. And since babies will put their fingers in their mouths it is a wise precaution to wash their hands several times a day.
The baby should be in the country, in the mountains or at the seashore if possible during the warmest part of the summer at least, but if he is in town there is much that the nurse can do to keep him cool and comfortable. His clothing at this time must be adjusted to his condition and the temperature of the moment just as it is in cold weather. A thin shirt, band, diaper and cotton slip will usually be enough for out-of-door wear, while in the house he may often dispense with the slip and sometimes with everything but his diaper.
During excessively hot days, the baby should have two or three cool sponge baths, in addition to the soap and water bath, one of the sponges being given before he is put to bed for the night. He should sleep on a firm mattress, preferably curled hair but never feathers, and in the coolest, best ventilated room available. During the day it is usually best to take him out-of-doors early in the morning and late in the afternoon, but to keep him indoors during the warmest part of the day, when it is likely to be cooler indoors than out, particularly if the blinds are closed. Quite naturally the nurse will have to take into consideration the size, arrangement and location of the baby’s home in her effort to keep him in cool, quiet, shady places and out-of-doors as much as possible.
He must not be played with, held on hot laps nor subjected to the entertainment and attention which misguided but well-meaning mothers and friends are so eager to lavish on a hot, fretful baby.
Very often during warm weather a fine rash known as “prickly heat” appears on the back of the baby’s neck and spreads over his head, neck, chest and shoulders. This rash is due to too warm clothing or to the hot weather or to both. Less clothing and frequent baths will often give relief, but if the baby is very uncomfortable, he may be greatly soothed by being immersed in cool baths containing soda, bran or starch in the following proportions:
517Soda bath. Two tablespoonfuls of baking soda to one gallon of water.
Bran bath. A cheese-cloth bag about six inches square, partly filled with bran, is soaked and squeezed in the bath water until it is milky.
Starch bath. About eight ounces of cooked laundry starch to one gallon of water.
No soap should be used while the baby has prickly heat and after the bath he should be patted thoroughly dry and powdered with some such soothing powder as the following:
As we look back over these pages of somewhat detailed description of the case of the baby, it is borne in upon us that the nursing of this unfailingly delightful and interesting little patient has special adjustments and adaptations for different seasons and circumstances; but that on the whole the care of all babies the year around resolves itself into the observation of a few general principles, namely: proper feeding; fresh air; regularity in his daily routine; cleanliness of food, clothing and surroundings; maintenance of an equable body temperature and conservation of his forces.
If the nurse fixes these principles firmly in her mind and acts upon them, she will do a great deal to give her baby patient a fair start on his life’s journey.
The common ills of early infancy are due largely either to errors in feeding or to infection or both. Of the nutritional disturbances, rickets and scurvy were discussed in the chapter on nutrition, but the obstetrical nurse will sometimes see also, malnutrition, marasmus, inanition, diarrheal diseases, acidosis, colic, constipation and vomiting.
All of these disorders are practically preventable through suitable feeding, good care and hygienic surroundings. The nurse’s part in this prevention consists in giving the painstaking care which was described in the preceding chapter.
The terms malnutrition, marasmus, and inanition designate different forms and degrees of starvation, and are characterized by loss of weight, prostration, feeble powers of assimilation, general weakness and arrested growth. The temperature is likely to be low, but in acute inanition, a rapid loss in weight may be accompanied by a sudden rise in temperature. (Charts 6, 7, and 8.)
These so-called “wasting diseases” are frequently seen in children who have congenital nervous instability and those born of tuberculous, syphilitic or otherwise delicate parents. The treatment is suitable food; fresh air and sunshine; an abundance of fluid by mouth, rectum, subcutaneously or intraperitoneally; clean surroundings and good nursing care.
These are among the most frequent and most serious illnesses of early infancy. They may result from mechanical causes, such as a mass of undigested food, which produces increased intestinal secretion and peristalsis; from the action of bacteria, or their toxins, together with the inability of an enfeebled digestive tract 519to meet the needs of a rapidly growing body; or from such reflex causes as sudden chilling of the body, excitement, fatigue or the prostration resulting from excessively hot weather.
Acute gastro-enteritis, the diarrheal disease which is so common and so fatal during the hot months of July and August, is often referred to as “summer complaint” or “summer diarrhea.” It is so largely avoidable through good nursing that the methods of its prevention were described in connection with the care of the baby during the Summer, resolving itself, as it does, into feeding the baby properly and keeping him clean and cool and quiet.
Symptoms. While there are different forms of summer diarrhea, the general symptoms are much the same and may develop gradually after some evidence of indigestion, or suddenly with a rise of temperature to 101° F. or 102° F., or even as high as 106° F., accompanied by pain and vomiting. The baby is usually restless, fretful and thirsty and his skin is hot and dry. He gives evidence of pain by shrill crying, drawing up his legs and flexing them on his abdomen. Diarrhea is the conspicuous symptom and there may be anywhere from four to twenty movements in the course of 24 hours. The stools are largely fecal matter at first but they finally become fluid and contain mucus. They may be expelled with a good deal of force and a quantity of gas come with them. The baby grows very weak, thin and hollow-eyed, if the diarrhea persists and unless promptly treated the end may be fatal.
Treatment and Nursing Care. The first step is to stop all food and to give water freely. When water is not retained by mouth it is frequently given by rectum, into the tissues or intraperitoneally. The pain may be relieved by applying hot stupes.
Feeding is resumed very gradually and cautiously for one attack of summer complaint predisposes to another and every precaution is taken to prevent a recurrence. Thin barley water or broth is usually given first, followed by whey, protein milk, buttermilk or diluted skim-milk in small amounts and at comparatively long intervals.
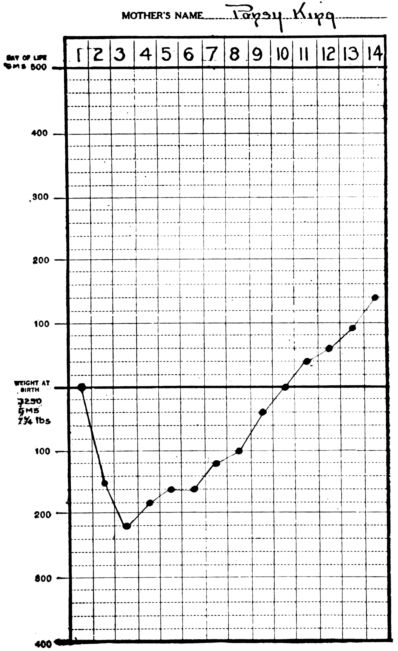
Chart 6.—Weight chart showing normal loss and gain during the first fourteen days of life.
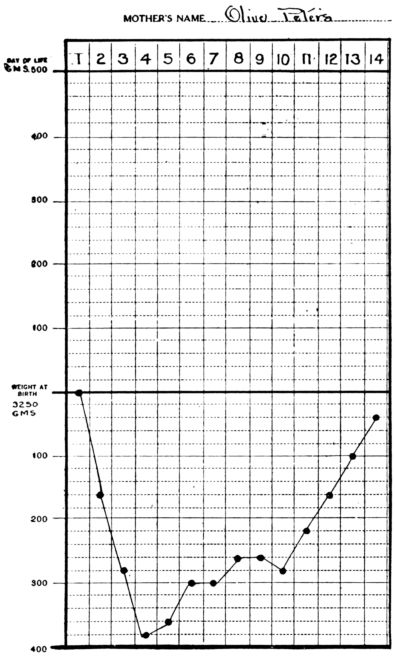
Chart 7.—Chart showing loss of weight in inanition fever.
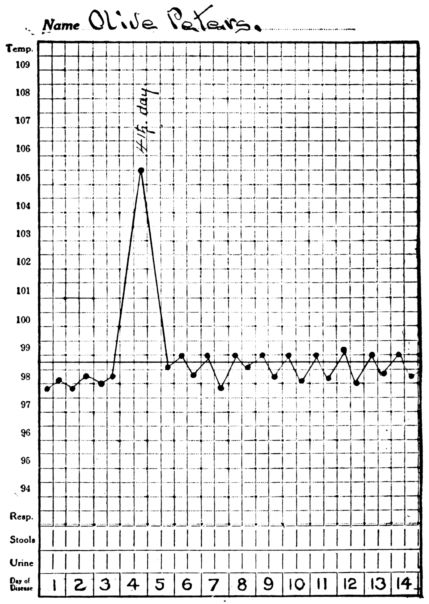
Chart 8.—Temperature chart showing sudden elevation of temperature, coincident with the marked loss of weight, in inanition fever.
521The baby should be lightly clad; should be kept quiet and in a cool, shady place out-of-doors as much as possible. During the warmest part of the day, however, he will often be much better off and more comfortable in the house, in a room with the shutters closed. But while keeping the baby cool, the nurse must bear in mind the harm that will be done by chilling him or exposing him to a cold draft or wind. Several tub baths, daily, are often given, at a temperature of 100° F., rather than cool sponge baths because of the baby’s feebleness and inability to react to cool bathing. Packs are also employed, both for high temperature and restlessness and may be cool (80° F.), tepid (100° F.) or hot (105° F. to 108° F.) according to the doctor’s orders; intestinal irrigations; lavage and gavage.
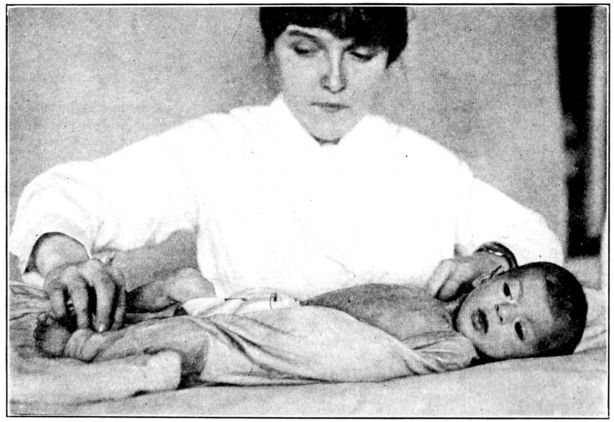
Fig. 177.—Putting the baby in a wet pack.
To give a pack, the nurse will cover the bed with a rubber and sheet and bring to the bedside a basin containing a sheet wrung from water of the specified temperature; a basin containing ice and compresses for the baby’s head, and a flannel covered hot-water bottle at 120° F., for his feet. The baby is laid on the upper half of the folded wet sheet, and an upper corner wrapped about each arm (Fig. 177), and the sides folded around his legs. The lower half is brought up between his feet to cover his entire body and tuck around his shoulders. The hot-water 522bottle is placed at his feet and an ice compress on his head. (Fig. 178.) If the sheets are wrung from warm or hot water, the baby is covered with a blanket after he is put into the pack.
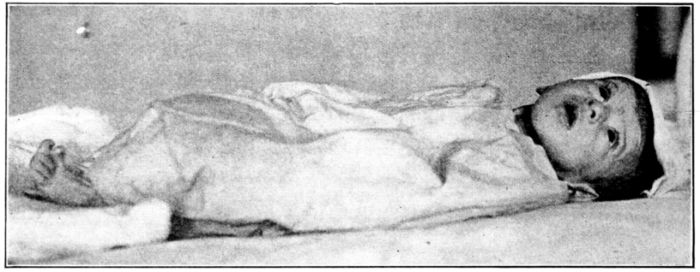
Intestinal irrigations, of normal salt solution are often given to babies suffering from intestinal disorders, sometimes once or twice daily to wash out the lower bowel, or a cool irrigation may be given to reduce temperature, the amounts varying from ½ to 5232 gallons of solution. The baby should be placed on a pillow and rest on a bed-pan, being protected from chilling as for, an enema (See Fig. 186), and provision made for a two-way flow of the fluid. A small catheter attached by means of a connecting glass nozzle to the tubing on the irrigation bag may be passed into a slightly larger catheter, which is inserted into the rectum about six inches, the fluid flowing in through the small inner tube and out through the larger one which encases it. Or a small catheter for the outflow may be inserted in the rectum alongside the one through which the solution is introduced. Normal salt solution, glucose or bicarbonate of sodium solution are sometimes given by the drip method at the rate of 20 to 40 drops per minute. In this case a glass tube is introduced at some point in the rubber tubing in order that the rate of flow may be watched and regulated by means of a clamp or a stop-cock. The catheter is inserted in the rectum about six inches and held in place by strips of adhesive plaster.

Fig. 180.—Baby wrapped in blanket, before being given gavage or eye irrigation, to keep him warm and hold his arms and legs to his sides. (From photograph taken at Johns Hopkins Hospital.)
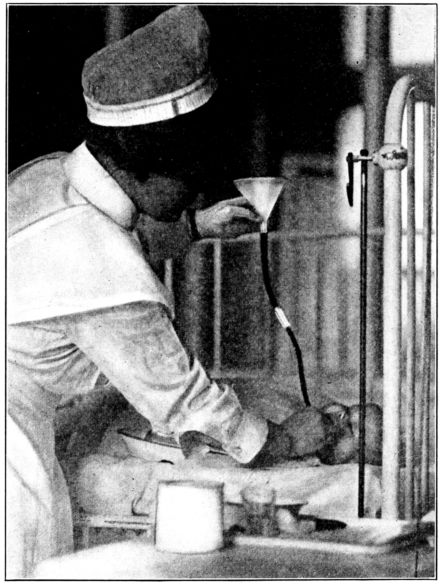
Fig. 181.—Gavage. (From photograph taken at Johns Hopkins Hospital.)
Lavage and Gavage. Sometimes when the baby vomits persistently the stomach is washed out and a small amount of water or nourishment given before the tube is withdrawn. A tray containing the following articles should be carried to the bedside:
A glass funnel attached to a rubber tubing which connects with a small rubber catheter by means of a glass nozzle.
Basin to receive stomach contents.
Small rubber, towel and curved basin to place under baby’s chin.
Glass graduate containing warm water for washing out stomach.
525Food or solution which is to remain in stomach, standing in cup of warm water.
Glycerin to lubricate tube.
Mouth gag, if necessary, or roll of bandage to hold jaws apart.
The baby should be wrapped tightly (Fig. 180) to prevent interference by his struggling and turned slightly to the left side. (Fig. 181.) The catheter is lubricated with glycerin or water and passed back over the tongue and quickly downward until an air bubble is heard as it enters the stomach. The length of tubing which is to be inserted may be anticipated by marking a point on the tube which is the same distance from the end as the baby’s mouth is from its umbilicus. The possibility and the serious consequences of introducing the tube into the trachea instead of into the esophagus must be borne in mind. Although the baby will often choke and struggle when the tube is properly introduced, he will not cough violently and stop breathing as he will if it enters the air passage. Further information is obtained by inverting the funnel in a basin of water after the tube is inserted; if it is in the stomach there will be no result, but if it is in the trachea air will be expelled and bubbles will rise through the water. To wash out the stomach, the funnel is filled with warm water and slightly raised so that the water will run in slowly, after which the funnel is turned upside down into a basin which is lower than the baby’s body, and the stomach contents allowed to run out. This is repeated four or five times, or until the solution returns clear, and the food which is to remain in the stomach is poured in slowly. Before the tube is quite empty it is pinched off with the fingers and quickly withdrawn.
Acidosis. The diarrheal diseases are sometimes complicated by acidosis, a condition in which the relative amounts of acid in the blood are so increased that the normal alkalinity is markedly diminished. This condition may result from an excessive intake of acids; an overproduction of acids in the course of normal metabolism; a decrease in the reserve of normal alkali in the body or a failure in the mechanism by means of which excessive acids are usually neutralized or eliminated. Acidosis is a serious complication and often fatal.

Fig. 182.—Method of obtaining a fresh specimen of urine in a test tube.
The treatment is directed toward preventing the production of more acids within the body; restoring the alkali reserve and promoting elimination of the excessive acids and their salts. Solutions of glucose, bicarbonate of sodium and salt are used and are given by mouth, rectum, intravenously and intraperitoneally. Subcutaneous injections are not wholly satisfactory, because of the small amounts which may be given in this way. From 150 to 400 cubic centimetres are given into the peritoneal cavity and as the solution absorbs readily these injections are sometimes repeated every eight or twelve hours, an infusion bottle and short infusion needle being used. From 75 to 300 cubic centimetres of glucose solution (5 per cent. or 10 per cent.) is given intravenously, while as much as 1000 cubic centimetres is sometimes given per rectum in the course of 24 hours by the drip method. Soda solution (4 per cent.) is often given by mouth, if the baby is able to retain it, or intravenously, as frequently as the condition of the urine indicates is necessary. From 75 527to 100 cubic centimetres is given at one time to young babies.

Fig. 183.—Obtaining a 24–hour specimen of urine through curved glass tube attached to rubber tubing which empties into bottle tied to side of bed. (From photographs taken at Johns Hopkins Hospital.)

In preparing the soda solution it must be remembered that boiling drives off carbonic acid and forms sodium carbonate and that its reconversion into sodium bicarbonate is a complicated procedure. Howland and Marriott[16] say in this connection: “Oscar Schloss has found that sodium bicarbonate in bulk is always sterile. It is probably therefore sufficient to add the bicarbonate with proper precautions to sterile water.”
528Since the results of urine tests frequently indicate the treatment in acidosis, it is of very great importance that the nurse be able to obtain specimens from young babies. (Figs. 182, 183, 184 and 185 for methods of obtaining fresh and 24–hour specimens from babies.)
Colic, Constipation, Convulsions and Vomiting so frequently seen in young babies are symptoms rather than diseases.
Colic usually consists of paroxysms of pain in the stomach or intestines, due to distension or to spasmodic, muscular contractions. The indirect cause may be unsuitable food or food given too rapidly; chilling of the surface of the body, excitement or fatigue. The distension may be due to air swallowed by the baby while nursing or gas formed by carbohydrate fermentation. Excess of protein may form an irritating mass in the intestines and cause a cramp.
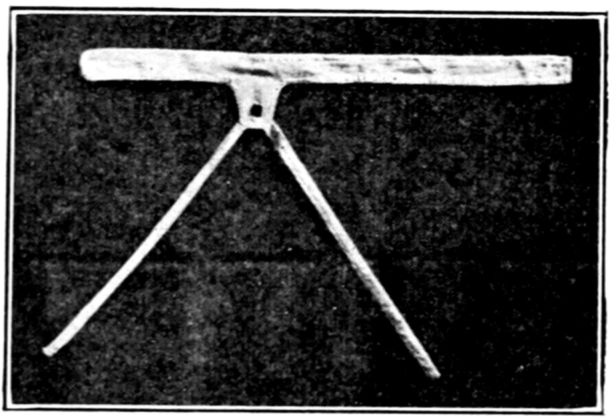
While colic frequently accompanies malnutrition and constipation, it is often seen in otherwise well and happy babies, and usually before the fifth month. The attacks are usually sudden and may occur several times a day after feeding, or only in the late afternoon or at night. The baby cries shrilly; his face is drawn and may be flushed, from crying, or cyanotic; his fists are clenched and pressed to his body and his feet and hands are cold. His abdomen is hard and distended and during a pain the baby flexes his thighs upon it and afterward extends them with a jerk. This painful seizure may last only a few moments or it may persist for hours, leaving the baby exhausted.
The chief preventive measures are found in the precautions and attention to detail which have been described, and which 529should be included in the care of all babies. In a bottle-fed baby it is often found that recurrence of attacks of colic may be averted by a slight change in the milk formula; by giving more water to drink; by lengthening the intervals between feedings; by giving the milk more slowly or by omitting the 2 a.m. feeding, thus giving the baby more digestive rest.
With breast-fed babies, prevention is often accomplished by having the mother nurse her baby more slowly, lengthening the intervals and by improving her own hygiene; particularly by increasing her recreation and out-of-door exercise and relieving constipation. Women who lead sedentary lives and eat rich food very often have colicky babies as do those who are nervous, irritable and inclined to worry. (See chapter on the nursing mother.)
When attacks of colic occur, the pain usually may be relieved by giving half of a soda-mint tablet in a little warm water and an enema of about eight ounces of soap-suds or salt solution at 110° F., given through a small catheter inserted about six inches. The baby will experience almost immediate relief through the expulsion of gas and feces and he may be made still more comfortable by placing a hot-water bag at his cold feet; rubbing his abdomen with vaselin and applying hot stupes. Sometimes the first feeding which falls due after an attack is omitted and a little warm water or barley water is given instead, in order that the digestive tract may rest.
Constipation is very common among young infants and may be manifest by the stools being too small, too dry or too infrequent. The commonest causes are:
The prevention of this very troublesome condition lies largely in suitable food; constant fresh air; regularity in the daily routine and training the baby to empty his bowels at the same time every day.
530When constipation is due to insufficient fat in the food, cod-liver oil is sometimes given, 15 to 30 drops three or four times a day; or a teaspoonful of olive oil two or three times a day. Maltose, malt soup, malted milk, milk of magnesia, liquid petrolatum, oatmeal-water and orange juice are all found among the remedies for constipation; while soap sticks, suppositories and enemata of oil or soap-suds sometimes have to be resorted to.
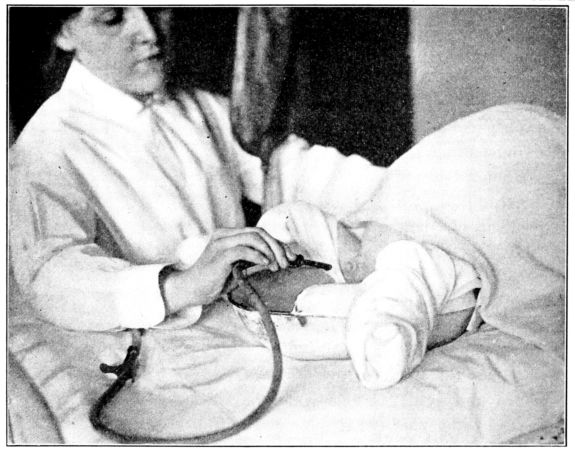
Fig. 186.—Giving an enema. The baby lies comfortably on a pillow which reaches to the bed pan, the latter being covered with a diaper where the baby rests upon it. He is well protected to prevent chilling.
In giving an enema to relieve constipation, the baby should be protected from chilling, laid on a pillow and the pan so placed that he will be comfortable and not inclined to move, and from 100 to 300 cubic centimetres of soap-suds, at 105° F., given with a small hard-rubber nozzle. (Fig. 186.) When warm olive oil is given at night (1 to 2 ounces through a catheter introduced about 6 inches), it is very often retained and the feces so softened that the baby empties his bowels freely the next morning with little or no assistance.
Abdominal massage will often help to increase the intestinal 531tone and make peristalsis more vigorous. The abdomen should be rubbed with a circular stroke, beginning in the right groin and following the course of the colon up to the margin of the ribs, across to the left side and down to the groin. This is often given for about ten minutes every day, preferably at night but never just after a feeding.
Constipation is sometimes entirely cured by a suitable dietary; an abundance of drinking water; an out-of-door life; massage, and above all, the unremitting effort to establish a regular habit. The latter is the nurse’s responsibility and she should exercise the greatest patience in trying to accomplish the desired end.
Convulsions are a symptom of several disorders of early infancy, which may occur unexpectedly and which the nurse may suddenly be called upon to relieve in the absence of the doctor. Convulsions may be due to brain lesions; to spasmophilia or a special tendency to convulsive disorders; gastro-intestinal disorders; toxemia or syphilis. They may be the initial symptom of an acute infectious disease or may occur on slight provocation in a frail, undernourished baby or one suffering from rickets or tetany. For this reason one sometimes sees convulsions in a baby who is teething or has colic or indigestion.
As convulsions are a symptom of some abnormal condition, the doctor will often prescribe a sustained treatment designed to remove or relieve the cause. But when an attack occurs unexpectedly, and the doctor cannot come at once, the nurse may often terminate the seizure by employing measures that will quiet and relax the struggling baby. The room should be quiet and darkened and the baby handled with utmost gentleness because of the extreme irritability of his nervous system. As a rule, the most satisfactory course is to immerse the baby in water at 100° F., and keep him there for five or ten minutes, supporting his head and shoulders meantime. Someone else should place cold compresses on his head and change them frequently. When removed from the bath, the baby should be wrapped in a blanket, kept very quiet and the cold applications to his head continued.
When it is known that the convulsions are due to indigestion the stomach is often washed out and a high colonic irrigation 532given before the baby is quieted by the bath. In tetanoid convulsions the baby may take a long deep inspiration and fail to expire. Respirations should be stimulated, in such a case, by spanking him sharply or by dashing cold water on his face and chest. When the attacks are recurrent the nurse may be instructed to terminate them by giving the baby a few whiffs of chloroform, which, with an inhaler is kept in readiness for instant use.
Mustard baths and packs are sometimes given when the need for counter irritation is indicated. For a bath, one ounce, or six level tablespoonfuls of dry mustard is added to one gallon of water at 105° F. and the baby kept in it for about ten minutes, or until the skin is well reddened. He is then wrapped in a warm blanket and surrounded by hot-water bottles, with cold compresses applied to his head. The mustard pack is given in the manner of other packs, with a sheet wrung from mustard water which is possibly a little warmer and stronger than that for the bath, care being taken that the sheet is not cooled before it is wrapped about the baby. He is usually left in the pack for about ten minutes or until his skin is reddened, and then wrapped in warm blankets, with cold compresses to his head.
It is often helpful to the doctor if the nurse is able to describe the onset of the convulsions and tell him where the twitching began, how it progressed and whether or not it was preceded by a cry.
Vomiting during early infancy is a symptom of any one of several conditions, the nature of which sometimes may be revealed by the character of the attacks. The commonest causes and varieties of vomiting are as follows:
1. Too rapid feeding or too large amounts of food given at one time. The vomiting amounts to little more than regurgitation and is often induced by moving or handling the baby immediately after feeding him.
2. Acute gastric indigestion. Sour stomach contents may be vomited immediately after feeding, or not until several hours later and may be followed by mucus and bile. The baby is usually pale, particularly about the mouth; he may perspire about the forehead and give evidence of pain, being relieved by the vomiting.
3. Stenosis of the pylorus. The vomiting from this cause is 533projectile in character and may occur immediately after food is taken into the stomach, or, some time later without apparent cause, a larger amount of fluid may be expelled than was given at the preceding feeding. The vomiting may begin a few days after birth or several weeks afterwards in a baby who has been well previously.
4. Intestinal obstruction due to congenital obstruction, which causes persistent vomiting from birth; or due to intussusception of the intestines, when vomitus consists first of stomach contents which later becomes bile stained and sometimes contains fecal matter, blood and mucus. It is attended by prostration, and after fecal matter is passed at the beginning, there is frequent evacuation of blood and mucus.
5. Chronic or habit vomiting, sometimes occurring in early infancy, may be difficult to control because of being incited by such slight causes as laughing, crying or being moved.
In addition to being caused by the above mentioned conditions, vomiting in young babies may usher in an acute infectious disease, as a chill does in an adult, or it may accompany such diseases as peritonitis, meningitis, brain tumors and toxic conditions such as uremia.
The infectious diseases which the obstetrical nurse is most likely to see in her baby patient are ophthalmia neonatorum; syphilis; impetigo; pemphigus and vaginitis.
Ophthalmia Neonatorum, inflammation of the eyes of the new-born or “babies’ sore eyes,” is one of the common diseases of infancy and certainly one of the most dreaded because of the tragedy of lifelong blindness which may follow in its wake. In the early days of organized work for the prevention of blindness the term “ophthalmia neonatorum” implied a gonorrheal infection, but it is now known that inflamed eyes and subsequent blindness may result from infection of innocent origin. Accordingly, in those states where it is required that the disease be reported, ophthalmia neonatorum is defined as inflammation of the eyes of new-born babies, irrespective of the cause. The disease is frequently due to the gonococcus, the baby’s eyes being infected from the mother during passage through the birth canal or infected later by her hands or clothing. Or the inflammation may be caused by the streptococcus, pneumococcus 534or the colon, diphtheria, or influenza bacilli while very frequently the infection is mixed.
It is estimated that about 20 out of every 1000 new-born babies have sore eyes, and though many of the infections are mild, between 5 and 8 of these 20 cases are capable of becoming serious and causing blindness if not speedily and skillfully treated. The number of cases which are neglected is suggested by the fact that about 10 per cent. of all blindness, the world over, is due to infant ophthalmia and that about 20 per cent. of the inmates of schools for the blind in this country are sightless from this cause. This does not take into account the unnumbered army of those who are partially blind, or blind in one eye, and thus seriously handicapped, as a result of this disease.
Symptoms. The first symptoms are redness and swelling of the lids, usually accompanied by a discharge of pus from the beginning, and they ordinarily appear during the first few days of life, but sometimes develop as late as the second or third week. The disease may run a very rapid course and cause blindness in 48 hours from the time the first symptoms appear, or it may persist for weeks. Ulceration of the cornea is the dreaded consequence of the inflammation as ulcers are followed by scars. When the scar is small, or to one side of the pupil, there may be little or no impairment of vision, but if it is large and centrally located it forms an opaque screen and causes blindness by shutting out the light, although the interior of the eye behind the scar is sound and uninjured. Sometimes the ulcer causes a perforation of the cornea through which the lens and vitreous humor are discharged.
Attempts have been made to remove the scar following a centrally located ulcer and replace it with a clear cornea from some such animal as a guinea pig, but the operation apparently has not been perfected. When it is, many blind persons may have their sight restored to them.
Prevention. It may be stated almost without qualification that ophthalmia neonatorum is a preventable and curable disease, and accordingly that blindness from this cause is inexcusable. Prevention lies first, in wiping the baby’s eyes immediately after birth and instilling a drop or two of a silver salt, such as 535nitrate of silver, argyrol or protargol, or bathing them with boracic acid solution; and second, in close watching for early symptoms and giving speedy treatment when they appear. This is urgent because there is no way of determining in the beginning whether the infection is mild or virulent. Nitrate of silver solution, 1 per cent., is the prophylactic most commonly employed and its use is now routine in most hospitals and in the practices of many physicians in this country. The solution is sometimes dropped between the baby’s lids, immediately after the birth of the head, and before the birth of the entire body, and sometimes immediately after delivery is completed. Many doctors follow the silver drops with normal salt solution to prevent the slight silver catarrh which so frequently occurs otherwise, and which may be confused with early symptoms of ophthalmia. Still others prefer simply to bathe the eyes with boracic acid solution (unless they know that the mother has gonorrhea) and to watch them closely for the slightest redness, swelling or discharge and give prompt treatment if these appear.
The Credé method, made famous by the Viennese obstetrician who introduced it in 1881, was to drop from a glass rod, a single drop of nitrate of silver, 2 per cent., into each eye immediately after birth. The routine use of this prophylaxis reduced the occurrence of ophthalmia in Credé’s clinics from 10 per cent. to .1 per cent. among the new-born babies.
Since it is now believed that close vigilance and subsequent care are equally as important as the prophylactic drops, the Credé treatment has been variously modified and other and weaker silver solutions are frequently used, and with satisfactory results. The dropping of a germicide into the baby’s eyes kills the organisms which may be present at the time, but it does not protect against subsequent infection. For this reason the nurse cannot be charged too earnestly to watch the baby’s eyes closely for the first evidence of infection, and report it to the doctor immediately, day or night, for the late infections are as destructive of sight as those which occur before or during birth.
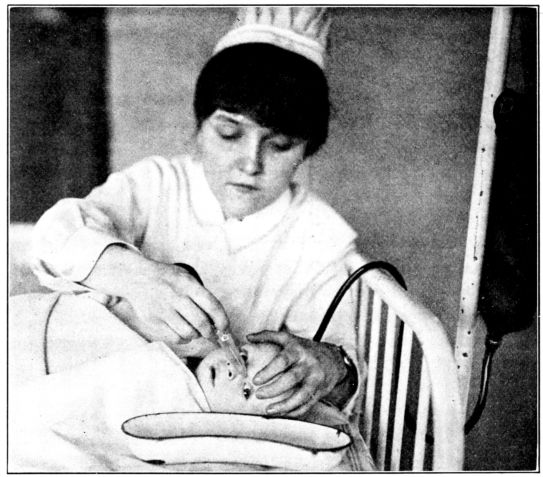
Fig. 187.—Irrigating the eye with a blunt nozzle, the irrigation bag hanging low in order that the stream may be gentle. (From a photograph taken at Johns Hopkins Hospital.)
Treatment and Nursing Care. The treatment and nursing care in ophthalmia frequently require the greatest skill. There may be merely an application of silver and sponging with boracic acid solution or a gentle irrigation with a blunt nozzle (Fig. 187), or the preservation of the baby’s sight may necessitate dressings and treatment which will require elaborate preparation (Fig. 188), and may also require some form of treatment every quarter- or half-hour, day and night and occupy the entire time of two or three special nurses. The nurse’s duties in caring for the eyes will be explicitly defined by the doctor, but in general she must remember that she is nursing a baby suffering from an acutely infectious disease, who should be strictly isolated, and that as a rule she should wear a gown, rubber gloves and protective goggles while caring for him. All of her attentions to the inflamed eyes must be given with the greatest gentleness in order to avoid abrasion of the conjunctiva or injury of the cornea. Moreover, the baby with suppurative conjunctivitis is a sick baby often fighting for his life as well as his sight, and every effort must be made to preserve his strength and increase his resistance. Fresh air and careful feeding are imperative. Breast-fed babies have a distinct advantage over bottle-fed babies and for this reason the mother should always accompany the nursing baby if he is taken from his home to a hospital to be treated for ophthalmia neonatorum, unless there is a wet nurse available at the hospital.

Fig. 188.—Method of holding baby for eye examination or treatment. (Photograph and appended notes by courtesy of Dr. W. Gordon M. Beyers, Royal Victoria Hospital, Montreal.)
“The child’s body is swathed in a sheet or blanket in such a way that the arms are lightly, but securely, fixed against the sides. The nurse can easily support the body with one hand, and with the other draw down the lower lid (as shown in the photograph), or otherwise assist the physician. The doctor sits opposite the nurse, with a rubber sheet across his knees, and upon this a sterile towel. He holds the baby’s head gently, but firmly, between his knees, thus freeing both his hands for necessary manipulations. In the picture the physician is represented as about to apply a solution of nitrate of silver with an applicator of sterile absorbent cotton.
“Close at hand is a table on which are a bowl of boracic acid solution and sterile absorbent cotton for irrigating the eyes; an undine (if one prefers) for the same purpose; a kidney dish for collecting the washings; sterile applicators, and small dishes for nitrate of silver solution and for saline solution (to neutralise): besides bottles containing solutions of cocaine, atropine, and fluorescein. Culture tubes, sterile swabs, cover slips, forceps, and a spirit lamp are ready for bacteriological examinations; and in a glass are displayed lid retractors, which are usually indispensable to a thorough examination of the cornea. On the floor is a paper bag, which, with the contaminated swabs, applicators, etc., is burned on the completion of the treatment. Other articles may be added as required; but the important point is, that everything should be at hand before the examination is begun.
“The physician and the nurse are clothed in surgical gowns; and wear rubber gloves, which heighten cleanliness, and safety and comfort. It is to be carefully noted that they both are provided with protective glasses; for under no circumstances should this precaution be omitted in treating the purulent ophthalmias.
“The conditions here depicted will not always be possible of fulfillment, but they represent the ideal for which one should strive.”
538It is of interest to nurses that the effort to safeguard the eyes of babies through preventive treatment and early care was developed into a national movement by one who also was influential in starting the training of nurses in this country, Miss Louisa Lee Schuyler. The lay work for the prevention of blindness, which is now country-wide, was started by the New York State Committee for Prevention of Blindness, which was organized by Miss Schuyler in 1908. She was its first Chairman and skillfully directed the work of the Committee for ten years. During the Civil War Miss Schuyler was a member of the Sanitary Commission and afterwards was one of the group which was responsible for starting at Bellevue Hospital, in New York City (in May, 1873), the first training school for nurses in this country, planned in accordance with Miss Nightingale’s standards for the organization and conduct of a school for nurses. Later, in 1911, the Bellevue School for Midwives was established as a result of the combined efforts of the Hospital Trustees and Miss Schuyler’s Committee for Prevention of Blindness, the course of training being outlined by a sub-committee composed of Miss Lillian D. Wald, Dr. J. Clifton Edgar and myself. So far as it is possible to learn this school was the first in this country to be conducted along the lines of a school for nurses, or after the manner of the midwife schools in England.
Syphilis, which ranks high among the scourges of mankind, is seen with distressing frequency among young babies. It may be contracted during uterine life, when it is said to be “inherited,” or it may be “acquired” after birth by kissing a syphilitic person or coming in contact with contaminated articles, such as clothing, or nursing from a diseased breast.
539The most conspicuous symptoms are the familiar “snuffles;” the scaling, fissures or eruption on the soles, palms, buttocks and about the mouth; shrill, hoarse crying; swollen painful joints; partial paralysis and a general feebleness and inanition. Some or all of these symptoms may be present when the baby is born or they may develop any time within the first two or three months of life.
Babies of syphilitic mothers are often given mercurial inunctions immediately after birth, even though they have no symptoms of the disease as it is very likely to be present in a latent form. This is one reason for the routine inspection of the placenta, since in it is sometimes found the only indication for treating the baby. An infant who is known to have syphilis is given mercurial inunctions or baths, the ointment being rubbed into the groin, axilla, back and abdomen in rotation on successive days, to prevent irritation of the skin. The nurse should protect herself with rubber gloves, wash the area with warm water and soap and thoroughly rub in the ointment. Sometimes the ointment is put on the inside of the back of the baby’s binder, by which means he rubs it in himself. The syphilitic baby should be isolated and should not be put to the breast of an uninfected woman, but he may nurse from a syphilitic woman without harm to either her or himself. Good general care, including fresh air and sunshine are important to the baby suffering from syphilis.
Thrush or Sprue is a highly communicable disease of the mouth of new-born babies, due to one of the fungi. It is common among sickly, undernourished babies and those living in unhygienic surroundings, but it is seldom seen in healthy babies who are cared for with absolute cleanliness. The disease is characterized by small raised, white spots in the baby’s mouth, frequently on the back of the tongue and inner surface of the cheeks.
Prevention lies in good care and in cleanliness of the mother’s nipples, or the bottles and nipples for artificially fed babies, and of all other articles coming in contact with the baby, particularly his mouth. Some doctors have the baby’s mouth bathed before each feeding, as a preventive measure, while others feel 540that a gentle swabbing once daily is sufficient, if the nipples are kept clean, since an abrasion of the mucous lining is easily caused and is favorable to the development of thrush.
Treatment consists in cleanliness and in gently swabbing the spots, three or four times a day, with sterile cotton wet with an alkaline solution such as borax (10%), bicarbonate of sodium (6%) and sometimes with formalin (1%) or a weak solution of permanganate of potassium.
Impetigo and Pemphigus are highly infectious skin diseases of early infancy which are seen more often in hospitals than in patients’ homes. The treatment of the raised blisters that appear on different parts of the body is entirely a medical question, but in caring for the patients suffering from either of these infections the nurse must take every precaution to avoid extending the trouble on the skin of the infected baby, himself, and of communicating it to other babies in the ward. Strict isolation is imperative; gentle handling and frequent changing of the underclothing to prevent extending the disease to uninfected areas.
Vaginitis. This highly infectious malady is considered troublesome rather than serious, as a rule, though it may be complicated by ophthalmia or arthritis. Gonorrheal vaginitis is the commonest form seen in early infancy and may be due to infection which the baby acquired during its passage through the birth canal or later from the mother’s hands or clothing. The symptoms are a vaginal discharge, which may be thin and serous or thick and yellow and purulent and it may be scanty in amount or abundant; a reddened, swollen condition of the vagina and vulva and sometimes redness and excoriation of the inner surface of the thighs. The nurse’s chief responsibilities are to be constantly on the alert to detect evidences of the disease and report them promptly to the doctor, and to observe strict isolation in caring for the baby while carrying out the doctor’s orders for douches or suppositories.
Icterus or Jaundice, which is so frequently seen in new-born babies, is occasionally a symptom of some septic condition; of 541syphilis or congenital cirrhosis of the liver or obstruction of the bile ducts, but as a rule it is without any serious significance. The jaundiced appearance usually begins on the second or third day and may continue for two or three weeks or it may subside in three or four days. The depth of the color varies, being very pale in some cases and almost green in others. When this discoloration of the skin is unaccompanied by other symptoms, no treatment is given.
A Cephalhematoma is a tumor of blood between the periosteum and the bones of the skull of the new-born baby. It is often due to some injury sustained during birth and is most frequently seen after prolonged labors. Cephalhematoma is sometimes confused with a caput succedaneum, but whereas the caput disappears in a few days the cephalhematoma may not be entirely absorbed for two or three months. Although certain conditions sometimes indicate the advisability of surgical treatment, the nurse’s care consists solely of protecting the tumor from injury.
Club foot is one of the commonest deformities of the extremities of young babies, occurring once in about every 1000 births. It may be congenital or caused by injury or it may be due to such diseases as cerebral paralysis or poliomyelitis. The nurse should watch for any abnormality in the structure or position of the feet, for the earlier treatment is started, the better is the prospect of a cure.
Engorgement of the Breasts. Not infrequently the breasts of new-born babies are engorged, in which state they are easily infected by being rubbed or squeezed. Since the greatest care must be taken to avoid bruising swollen breasts, they are sometimes protected by the application of a pad of sterile cotton. Hot compresses are sometimes applied when there is redness with the swelling, or a tiny ice-bag, made by tying off the fingers and thumb of a rubber glove, and partly filling it with finely crushed ice, after which the wrist is tightly tied.
Hare Lip. The fissured lip, which is not infrequently seen in new babies, may consist merely of a small notch or it may amount to a deep cleft reaching up into the nostril. It is due to a non-union of the frontonasal plate with the lateral processes 542and may occur on one or both sides, thus forming a single or double hare lip. An extensive fissure will usually interfere with suckling and the nurse may need both ingenuity and patience in feeding such a baby, for the prospect of successful treatment, which is surgical, increases with the baby’s age and improved nutrition. The longer she can feed the baby successfully, therefore, the better his chance of recovery.
Cleft palate, a common congenital abnormality, consists of a fissure of the soft, and sometimes of the bony, palate; it may be on one or both sides and may be continuous with a hare lip. The problem of feeding the baby with a cleft palate is very grave since the fissure may make it impossible for him to form the vacuum in the back of his mouth which is necessary for suckling. He is sometimes fed with a medicine dropper or by gavage or by means of a special nipple provided with a flap which fits into the roof of the mouth and closes the opening into the nasal passages. Even more than in the care of the baby with a hare lip is it important to nourish the baby with a cleft palate, and build him up for as long as possible before he is subjected to the strain and shock of the inevitable operation.
Hernia. Umbilical and inguinal hernias are both seen in young babies.
Umbilical hernia is the commoner type and is not uncommon in thin babies and those with indigestion and distension and in babies who cry violently. Such hernias are not regarded as serious if prompt measures are taken to reduce them as they usually respond very readily to treatment. But since neglect may have serious consequences, the nurse should watch for protrusions and report them promptly. She will often be instructed to reduce the hernia and apply adhesive strapping, in which case the following observations by Dr. Griffith will be helpful:
“Usually it is quite sufficient to draw the skin into two folds, one on each side of the hernia and meeting over it; holding these in place by straps of adhesive plaster crossing over the navel, or by a broad horizontal band of adhesive plaster reaching to the lumbar regions. Another method is the following: A silver quarter of a dollar is laid upon the adhesive surface of a piece of rubber plaster about two inches square; over this is placed 543the broad strap referred to, with its adhesive surface next to that of the smaller piece. After reducing the hernia and pressing the sides of the abdominal walls slightly together the band is applied with the quarter dollar directly over the position of the navel. My own preference is for a simple adhesive band without the use of the coin. The dressing should be worn constantly, changing it from time to time as the old one loosens. The dressing must, of course, not be removed during the bath. Several months are required before the opening is permanently closed. Occasionally the plaster produces a great deal of cutaneous irritation, especially in the first few months of life. The employment of zinc oxid plaster tends to avoid this difficulty.”[17]
Inguinal hernia is less common in very young babies but it should be watched for since it usually may be easily reduced by the use of a truss, if discovered and treated early, but may be serious if neglected.
In general, the new baby who is ill, needs the same thoughtful, gentle, painstaking care that the nurse gives to the well baby, but these must be shaped to his immediate requirements and the doctor’s special instructions.
It will be well for us now to take a retrospective view of the various functions of the nurse which are associated with the phenomena of pregnancy, labor, the puerperium and the beginning of a new life. As we see these in perspective, our attention is fixed by a few important principles which stand out from the picture as a whole in clear and shining relief.
We see, for example, that no matter what else may become vague and unimportant, be changed or discarded, there remains the conspicuous, unalterable requirement that the nurse shall do clean work throughout this entire series of experiences. All maternity patients and all babies need scrupulously clean care no matter what else they may have or may lack.
But also must they all be watched throughout these transitional stages, in order that impending disaster may be apprehended and warded off. And that this watchfulness be intelligent, the nurse must of necessity know something of the normal physiological changes which occur during these momentous periods in the lives of her patients, lest she fail to detect evidence of abnormality, should it appear.
Since this invariable cleanliness and close watchfulness are needed by all patients, whether of high or low degree, and by those in the care of doctors with widely varied methods, the nurse must be able to make adaptations to each patient’s environment and temperament and to the doctor as well, if all of her patients are to be well and happily nursed. She must be clean, then, and watchful in her work, and adapt it to every conceivable condition. These features stand out clear and bold in the perspective. But to make these offices effective to their utmost, the nurse’s attitude and her care of her patient must be mellowed by an always deepening sympathy and understanding. She must endeavor, in each instance, to imagine the mental experience 545of the bewildered and timid expectant mother; of the terrified woman in labor and the discouraged young mother—these she must appreciate if she is to give of her best. And so, in the end, the character of the nurse’s work will be influenced, in fact almost determined, by her awareness of her patient’s needs, mental and physical, and the earnestness with which she tries to relieve them. More than this, the nurse whose skill is warmed by a sincere desire to give of her best will, by virtue of this very desire, learn something from each patient, and will be steadily enriched and broadened by her experiences. She will have more to give, and accordingly will derive increasing satisfaction from her service to each succeeding mother and baby that she takes into her care.
One word more. The maternity nurse almost inevitably becomes deeply attached to her baby patient, whether he is sick or well, and she is eager to protect him and safeguard him as long as possible. She may continue to serve him, even after he has passed from her trained hands, if she will teach his mother how to take care of him, should she be inexperienced, particularly if the young mother is to have full charge of her baby after the nurse leaves, or is to have only the assistance of a partly trained nursery maid. In such a case the nurse may often perform her most valuable and enduring service to the baby by gradually teaching his mother how to prepare the milk with cleanliness and accuracy, if he must be bottle-fed; how to give his bath deftly and comfortably, and impressing upon her the importance of fresh air and of regularity in the baby’s daily routine. All of these things, and also how to do the thousand and one other things that seem so trivial and yet mean so much to the baby’s immediate health and future well being.
The first day after the nurse leaves, and the first few after that are often very dark ones for the inexperienced young mother, and if she is alone they are likely to be filled with fear and misgivings. The nurse may rob these days of much of their discouragement by anticipating them; trying to imagine the young mother’s possible perplexities and then teaching her how to meet them. This teaching is perhaps not a part of the nurse’s professional obligation but it is one of the privileges, 546one of the gratifying by-paths of nursing that she may take for the sheer joy of it.
Not infrequently the young mother is so filled with awe over possessing anything so wonderful as her own baby that she is afraid to handle the exquisite little body; is fearful of harming it; and because of her timidity and inexperience she fails to give him the care that he needs, and that she wants to give. On the other hand, all too many young mothers have a blind confidence that the mere act of having a baby vests one, in some instinctive way, with the requisite knowledge and skill to care for it, and in this belief they are supported by a legion of women friends and relatives.
It would be difficult to imagine a single factor that works more destruction among babies than this one of ignorant motherhood. And the damage is equally great whether the ignorance arises from timidity or from overweening confidence.
“Is it not preposterous,” says Herbert Spencer, “that the fate of a new generation should be left to the chance of unreasoning custom, impulse, fancy, joined with the suggestions of ignorant nurses and the prejudiced counsel of grandmothers? To tens of thousands that are killed, add hundreds of thousands that survive with feeble constitutions, and millions that grow up with constitutions not so strong as they should be, and you have some idea of the curse inflicted on their offspring by parents ignorant of the laws of life.”
The nurse is in the most effective position possible, to help in dispelling maternal ignorance, during the long days of pleasant intimacy which she and the young mother spend together in devotion to the baby. And by helping the inexperienced young mother to give skilful care to her baby, with all of the gentleness and tenderness that a mother can lavish, the nurse will not only serve the baby; she also will awaken for many a young woman, an interest that will be ever fresh and absorbing, and point the way to unexpected joys and delights in her motherhood.
1. In the generally contracted pelves, all of the external measurements are shorter than normal, the diagonal conjugate being 11.5 cm., or less. In simple flat pelves, on the other hand, the external measurements are normal, but the diagonal conjugate is 11 cm., or less.
If the distance between the tuber-ischii is only 8 cm., or less, the patient has some kind of a funnel pelvis; simple, if the inlet measurements are normal, but if they also are shortened, the pelvis is described as a generally contracted funnel.
The rachitic pelves present certain characteristic features, one being less difference between the inter-spinous and inter-crestal measurements than is found in a normal pelvis. Another, that the distance between the tuber-ischii is always of normal length and may even be greater than normal. The peculiar deformity of the sacrum, however, is the most characteristic abnormality of the rachitic pelves. The concavity from above downward is markedly increased, in some cases almost forming an angle, while the horizontal concavity is nearly or quite obliterated. The commonest type of a rachitic pelvis is one in which all of the inlet measurements are shortened, the inter-tuberous distance normal, and the sacrum characteristically deformed. This is called the generally contracted, rachitic pelvis. In the flat rachitic pelvis all of the inlet measurements are normal, except the diagonal conjugate, which may be shortened to 11 cm., or less, and the sacrum presents the deformity described above.
2. The Prospective Mother, by J. Morris Slemons.
3. “Obstetrics,” by J. Whitridge Williams.
4. “The Practice of Obstetrics,” by J. Clifton Edgar.
5. “The Value of the Wassermann Reaction in Obstetrics, Based upon the Study of 4,547 Consecutive Cases.” Johns Hopkins Hospital Bulletin, Oct., ’20. “The Significance of Syphilis in Prenatal Care and in the Causation of Infant Death.” Johns Hopkins Hospital Bulletin, May, 1921.
6. Routine preparation of hands at Johns Hopkins Hospital.
7. Written especially for this book.
8. From puer, child, and parere, to bring forth.
9. “The Practice of Obstetrics,” by J. Clifton Edgar.
10. Alfred F. Hess, M.D., and Lester J. Unger, American Journal of Diseases of Children, April, 1919.
11. Alfred F. Hess, M.D., The Journal of the American Medical Association, Sept. 21, 1918.
12. “The Nursing Mother as a Factor of Safety in the Nutrition of the Young.” E. V. McCollum and N. Simmonds, The American Journal of Physiology, June, 1918.
13. “The Life of Pasteur,” by Vallery Radot.
14. The Committee consisted of Drs. J. Clifton Edgar, Ralph Lobenstein and Philip Van Ingen.
15. “Obstetrics,” by J. Whitridge Williams.
16. “Acidosis,” by John Howland, M.D., and W. McKim Marriott, M.D., Pennsylvania Medical Journal, April, 1918.
17. “The Diseases of Infants and Children,” by J. P. Crozer Griffith, M.D.