The cover image was created by the transcriber and is placed in the public domain.
Title: The Dawn of Modern Medicine
Author: Albert H. Buck
Release date: January 19, 2020 [eBook #61196]
Most recently updated: October 17, 2024
Language: English
Credits: Produced by Turgut Dincer, Barry Abrahamsen, and the Online
Distributed Proofreading Team at http://www.pgdp.net (This
file was produced from images generously made available
by The Internet Archive)
The cover image was created by the transcriber and is placed in the public domain.

PORTRAIT OF ANTOINE LAURENT LAVOISIER
The French chemist and biologist who contributed more than anyone
else to our knowledge of the chemistry and physiology of oxygen.
(Copied from the frontispiece of Volume I of Lavoisier’s “Works,”
published by the French Government in 1864.)

The present volume is the third work published by the Yale University Press on the Williams Memorial Publication Fund. This Foundation was established June 15, 1916, by a gift made to Yale University by Dr. George C. F. Williams, of Hartford, a member of the Class of 1878, Yale School of Medicine, where three generations of his family studied—his father, Dr. William Cook Williams, in the Class of 1850, and his grandfather, Dr. William Chauncey Williams, in the Class of 1822.
This work is in the main a continuation of the volume entitled “The Growth of Medicine,” but it is also intended to serve as an amplification of the latter part of that work, which, owing to various circumstances that were in large measure beyond my control, lacked completeness. The most troublesome of these adverse circumstances was the fact that I had failed, during a recent visit to Europe, to find those sources of trustworthy information upon which alone such a narrative could properly be based; and later still, when I made my first attempts to construct the text of the present volume, I again encountered the same kind of obstacles, but in an even greater degree, and was then strongly disposed to abandon the undertaking altogether. At this juncture of affairs, however, I was much surprised and pleased to receive from Mrs. Charles F. Norton, the librarian of Transylvania College at Lexington, Ky., a letter in which she stated that the college had in its possession a large collection of medical works which had been purchased at Paris, France, in 1819, at which period of its history the institution bore the title of Transylvania University and possessed a flourishing medical department; and that the president of the institution would be happy to extend to me every possible facility for utilizing this great mass of historical material. Shortly afterwards, in reply to my request that I might be furnished with a partial list of the books contained in this collection, in order that I might determine how many of them related to the period in the history of French medicine in which I was at that time particularly interested,—the period, mainly, from about 1760 to 1830,—I received a card catalogue of the titles of over 100 French, English and Latin treatises. This information removed all doubts from my mind concerning the wisdom of my visiting Lexington, and I accordingly signified my prompt acceptance xof the cordial invitations extended to me by President Crossfield.
As I write these lines I am prompted to add the further statement that during my stay at Lexington, which covered a period of seven months, I received every assistance from the Transylvania College authorities that I could possibly desire; and in particular I wish to express my deep sense of gratitude to the librarian, Mrs. Norton, for the interest which she manifested in my work and for the valuable assistance which she rendered in hastening its completion.
Cuvier, the celebrated naturalist, in a memoir which he read before the Royal Institute of France, makes the following statement: “It is not through a perusal of the insufficient extracts that are commonly made from the published works of distinguished men, nor through the incomplete indications which the recital of their discoveries may furnish, that we derive the greatest pleasure from the eulogies pronounced after the death of these men. This desirable result is more likely to be obtained when we are made intimately acquainted with their individual traits of character,—when we are, so to speak, permitted to know these men in a social way; when we are given the opportunity of contemplating, close at hand, their distinct qualities, their virtues, yes, even their faults,—provided the facts are plainly stated by one who is skilled in such portraiture. Furthermore, the reader is sure to derive the greatest pleasure, and also to be the most benefited, when every page of the eulogy furnishes evidence of the genuine happiness and wonderful serenity which characterize the lives of those who devote themselves to the culture of the sciences. Compare these men with those who have been intent on securing glory through devastating the world, and note how frequently they live to be septuagenarians or even octogenarians.” Deeply impressed by the wisdom of the advice thus briefly given by the celebrated French naturalist, I have striven, in the following chapters, to act upon it as circumstances might permit.
After making several unsuccessful attempts to classify my chapters according to the special fields in which the different ximen attained distinction, I came to the conclusion that the difficulties which stand in the way of adopting such a classification are well-nigh insurmountable; and chief among these difficulties may be mentioned the fact that many of the leading physicians attained distinction in two or more different fields. Botany, for example, was frequently combined with anatomy and surgery; chemistry with physiology; and so on. On the whole, therefore, it seemed better to rest satisfied, wherever this was found to be practicable, with the simple subdivision according to geographical districts—viz., Northern and Central Germany, Austria, Italy, France, Switzerland and England.
The relatively few Americans who played an important part in advancing the science and art of medicine during the latter half of the eighteenth century and the early part of the nineteenth make it preferable, as it seems to me, to omit all reference to them in the present work, leaving to the writer of a volume devoted to modern medicine, the duty of honoring their achievements.
Cornwall, Orange County, N. Y.
October 3, 1919.
| PAGE | |
| Preface | ix |
| Chapter I. Théophraste Renaudot, Physician, Philanthropist, and Founder of the First French Newspaper | 3 |
| Chapter II. Low State of Medical Affairs in Germany at the Beginning of the Eighteenth Century | 15 |
| Chapter III. Physicians who Attained Distinction in Some of the Departments of Medicine during the First Half of the Eighteenth Century | 18 |
| Chapter IV. Distinguished Swiss Physicians who Played a Prominent Part in the Development of the Science and Art of Medicine in Germany | 34 |
| Chapter V. The Earliest Publication in Europe of a Systematic Treatise on Hygiene, Public Health and Medico-Legal Science | 43 |
| Chapter VI. Two Eminent German Surgeons of the Pre-Antiseptic Period | 48 |
| Chapter VII. A General Survey of German Medicine at the End of the Eighteenth Century | 52 |
| Chapter VIII. Gerhard Van Swieten | 59 |
| xiiiChapter IX. Anton Stoerck, Van Swieten’s Successor, and the Progress of Medical Affairs at Vienna under the Management of Joseph II | 71 |
| Chapter X. Prochaska, Hyrtl and Rokitansky, Three of the Most Distinguished Teachers at the Medical School of Vienna during the Early Part of the Nineteenth Century | 79 |
| Chapter XI. Baglivi, Morgagni, Scarpa, Spallanzani, Tissot and Galvani; Italy’s most Illustrious Physicians during the Eighteenth Century | 91 |
| Chapter XII. Measures Adopted for the Control of Small-Pox; Inoculation, Vaccination | 107 |
| Chapter XIII. The English and French Chemists Contribute Their Share toward the Advance of Medical Knowledge | 119 |
| Chapter XIV. English Leaders in Medicine and Surgery during the Eighteenth and Early Nineteenth Centuries (First Group) | 129 |
| Chapter XV. English Leaders in Medicine and Surgery (Second Group) | 139 |
| Chapter XVI. English Leaders in Medicine and Surgery (Second Group continued) | 150 |
| Chapter XVII. Bordeu and Bichat; The Beginning of Experimental Physiology and Experimental Pathology in France | 159 |
| Chapter XVIII. Types of French Physicians who Flourished about the Time of the Reign of Terror | 171 |
| Chapter XIX. Laënnec and the Invention of the Modern Method of Auscultation; Paul-Joseph Barthez | 195 |
| Chapter XX. Early Studies of the Disease now Universally called Typhoid Fever: Bretonneau | 202 |
| Chapter XXI. The Harmful Effects of Broussais’ Teaching | 207 |
| Chapter XXII. J. L. Petit, of Paris, and his Contemporaries in Surgery—Sabatier, Chopart, Desault and Dupuytren | 215 |
| Chapter XXIII. Workers in Special Departments of Surgery: Demours, Descemet, Delpech, Fauchard, Jourdain, Gariot | 230 |
| Chapter XXIV. Military Surgery in France, as represented by Desgenettes and Baron Larrey | 241 |
| Chapter XXV. Hospital of “La Maternité,” the Great French Midwifery School | 253 |
| Chapter XXVI. Further Details Concerning the Paris Faculté de Médecine and Concerning some of the Larger Hospitals of Paris | 258 |
| Chapter XXVII. Armand Trousseau, one of the last of France’s Great Clinical Teachers | 265 |
| List of the More Important Authorities Consulted | 271 |
| General Index | 277 |
| Footnotes | 300 |
| Portrait of Antoine Laurent Lavoisier, the French chemist and biologist who contributed more than anyone else to our knowledge of the chemistry and physiology of oxygen. (Copied from the frontispiece of Volume I of Lavoisier’s “Works,” published by the French Government in 1864.) | Frontispiece |
| Loudun. This photograph, which was taken from one of the highest points in the village of Loudun, shows its elevated position above the surrounding country and affords a bird’s-eye view of the adjacent river, the Martray. (Courtesy of Monsieur le Pasteur Paul Barnaud, of Sainte Foy la Grande [Gironde], France.) | 4 |
| Cardinal Duc de Richelieu. (From a portrait engraved on copper by Nanteuil in 1655.) | 6 |
| Statue of Théophraste Renaudot at Loudun, France. (Courtesy of Monsieur le Pasteur Paul Barnaud, of Sainte Foy la Grande [Gironde], France.) | 8 |
| Hufeland. (From Eugen Hollaender’s “Medizin und Plastik,” by permission.) | 28 |
| Albrecht von Haller | 34 |
| Vignette from the title-page of Haller’s “Elementa Physiologiae,” Lausanne, 1757 | 36 |
| Gerard Freyherr Van Swieten | 60 |
| Medal commemorating the discovery of vaccination. (From Eugen Hollaender’s “Medizin und Plastik,” by permission.) | 108 |
| Edward Jenner. (Copied from Thomas J. Pettigrew’s “Medical Portrait Gallery,” London, 1838. The original portrait was painted by Sir Thomas Lawrence, Royal Academy.) | 110 |
| Sir Astley Cooper. (Copied from a print in the possession of the New York Academy of Medicine.) | 136 |
| William Hunter. (Copied from Thomas J. Pettigrew’s “Medical Portrait Gallery,” Fisher & Son, London, 1838. The original portrait was painted by Pyne; the engraving was done by J. Thomson.) | 140 |
| xviiJohn Hunter. (Copied from Thomas J. Pettigrew’s “Medical Portrait Gallery,” London, 1838. The original portrait was painted by Sir Joshua Reynolds; the engraving was done by G. H. Adcock.) | 144 |
| Sir Benjamin Collins Brodie, Bart., F.R.S., Sergeant Surgeon to the Queen. (Copied from Thomas J. Pettigrew’s “Medical Portrait Gallery,” London, 1838. The original portrait was painted by H. Room; the engraving was done by J. Brain.) | 148 |
| Sir Charles Bell. (Copied from a print in the possession of the New York Academy of Medicine.) | 154 |
| Bichat | 162 |
| Costume worn by Paris physicians in the eighteenth century. (From Alfred Franklin’s “La Vie Privée d’Autrefois,” Paris, 1892.) | 172 |
| Gaspard Laurent Bayle | 182 |
| A candidate for the degree of “Doctor of Medicine” defending his thesis before the examining committee of the Paris Faculty of Medicine. (From “La Vie Universitaire,” Paris, 1918.) | 184 |
| Corvisart. (Copied from an old French print in the possession of the New York Academy of Medicine.) | 188 |
| Laënnec. (Copied from an old French print in the possession of the New York Academy of Medicine.) | 196 |
| The Faculté de Médecine and the Cathedral at Montpellier, France. (Courtesy of Monsieur le Pasteur Paul Barnaud, of Sainte Foy la Grande [Gironde], France.) | 198 |
| The “Court of Honor” of the Faculté de Médecine at Montpellier, France. (Courtesy of Monsieur le Pasteur Paul Barnaud, of Sainte Foy la Grande [Gironde], France.) | 200 |
| Montpellier. Vestibule of the Faculté de Médecine at Montpellier, France. (Courtesy of Monsieur le Pasteur Paul Barnaud, of Sainte Foy la Grande [Gironde], France.) | 202 |
| Charles A. P. Louis | 204 |
| Broussais | 208 |
| Jean-Louis Petit | 216 |
| Dupuytren | 226 |
| Desgenettes | 242 |
| Baron Larrey | 244 |
| Eighteenth-century plan showing the relations of the Paris École de Médecine to Hôtel-Dieu, the Cathedral of Nôtre Dame and the River Seine. (Reduced copy of the cut printed in Franklin’s “La Vie Privée d’Autrefois,” Paris, 1892.) | 258 |
| xviiiSide of the Paris Faculté de Médecine which fronts on the Rue de l’École de Médecine. (From “La Vie Universitaire.”) | 260 |
| View of the former École de Médecine since it has been incorporated with the new structures of the Faculté de Médecine. (From “La Vie Universitaire.”) | 260 |
| Musée Dupuytren. Formerly the refectory of the Convent of the Cordeliers (Franciscans), in the fifteenth century. (From “La Vie Universitaire.”) | 260 |
| Device of the École de Médecine de Paris. (Adopted by the Faculty in 1597.) (Three storks, each holding a twig of origanum in its beak; and at the top of the design the motto “Urbi et Orbi Salus” [Health to the City and to all the World].) | 262 |
| Hôpital Saint-Louis, Paris. Planned and drawn by Claude Chatillon, architect, in 1608. (Copied from Tenon’s “Mémoires sur les Hôpitaux de Paris,” Paris, 1816; reduced about one-half.) | 264 |
| Trousseau | 266 |
| Velpeau. A contemporary of Trousseau and one of France’s most distinguished surgeons. (Copied from a print in the possession of Transylvania College, Lexington, Kentucky.) | 268 |
FOUNDATION OF THE FIRST NEWSPAPER IN PARIS, FRANCE, AND THE ESTABLISHMENT OF PRIVATE AGENCIES FOR AIDING THE POOR
THÉOPHRASTE RENAUDOT, PHYSICIAN, PHILANTHROPIST, AND FOUNDER OF THE FIRST FRENCH NEWSPAPER (1586–1653)
Prefatory Remarks.—As the present volume purports to deal with events that occurred chiefly during the eighteenth century, the reader may think it strange that I should introduce here a sketch which relates to a physician whose life covers a period nearly one century earlier. My reason for departing, in this instance, from the proper chronological order, in the arrangement of my text, is of a twofold nature. In the first place, I did not discover Gilles de la Tourette’s interesting memoir—almost the only satisfactory source of information available concerning Renaudot—until about February 1, 1918—that is, nearly one year after “The Growth of Medicine” had been published; and, second, on looking over the principal treatises on the history of medicine, I failed to find any adequate account of the remarkable work accomplished by Renaudot. Puschmann, so far as I have been able to learn, is the only authority who gives this great philanthropist due credit for the important part which he played in reflecting honor upon our profession.
Théophraste Renaudot was born at Loudon, a small town in Western France, picturesquely situated on a high hill about thirty miles northwest of Poitiers. His parents, who were wealthy Protestants, died while he was still a mere lad. Théophraste, who inherited the entire fortune left by his parents, developed at a remarkably early age strong humanitarian ideas, and it was under the stimulus of these that he shaped his course in life. With a clear idea of the kind of training that would best fit him for the work which he proposed to undertake, he decided to study medicine, 4as this career, better than any other, would enable him to accomplish his purpose. Accordingly he went to Montpellier, took the regular course of instruction in the university, and received the degree of Doctor of Medicine in 1606, before he had reached his twentieth year. Recognizing the fact that a physician should be of a certain age before he can reasonably expect to command the confidence of his fellowmen, he decided to utilize the time following his graduation in visiting some of the more important capitals of Europe. The first country which he visited was Italy, where he undoubtedly gained some familiarity with the manner in which the monts-de-piété (the prototypes of our modern pawnbrokers’ shops) were managed under the guiding control of the popes. It is also highly probable that he visited in turn the universities of Holland and Belgium as well as the two great English universities—Oxford and Cambridge. Then, upon his return to France, he went to Paris and began the study of chemistry at the Collège de Saint-Côme. During his stay in the French metropolis, he was made painfully aware of the prevalence of poverty, the streets being filled everywhere with shameless beggars, and Hôtel-Dieu, the great city hospital, being overcrowded with the sick, among whom were large numbers of children affected with contagious diseases and infants starving to death from lack of wet-nurses. The first thought that occurred to the practical mind of Renaudot was to find work for many of these poor people; but when he set about doing this he at once encountered many obstacles; and finally, in despair over his lack of success, was forced to abandon further efforts in this direction and return to his home in Loudon. While there, he frequently met the influential Capucin Monk Leclerc du Tremblay, commonly known as his “Gray Eminence,” and through him he was brought to the notice of Cardinal Richelieu, then or soon afterward, Secretary of State of Marie de Médicis, the queen-mother of Louis XIII. Although the cardinal, for political reasons, antagonized the Huguenots, he personally entertained no unfriendly feelings toward men of the Protestant faith, and consequently he was quite prepared to aid Renaudot when he laid 5before him, as he did shortly after his return to Paris, his schemes for the betterment of the poor in that great city. One of these schemes called for the establishment of a “bureau d’adresse ou de rencontre,” an office depot where, by the payment of three sous, anybody was entitled to have the address of his place of business entered upon the registers of the bureau; and where also employer and employee might meet for arranging terms. If any person wished to learn the address of any given place of business, the desired information would be furnished upon the payment of a fee of the same value; but no charge whatever was to be made in the case of a poor person. This scheme proved a complete success in a very short time. Then, as a further step in the development of his bureau, Renaudot joined what he termed “ventes à grâce troque ou rachapt”—that is, “sales with the privilege of exchange or redemption.” This was the first step toward the establishment of his “mont-de-piété,” an institution which was not fully organized by him at Paris until 1637. The tax upon loans was fixed at 3 per cent—just enough to pay the expenses of running the bureau. His motto was: “Loan money without expectation of profit.” His solution of the social problem was summed up in the following aphorism: “In every organized community or state the rich shall afford aid to the poor, all harmony between the two classes ceasing when one of them grows richer at the expense of the other.”

Loudun. This photograph, which was taken from one of the highest points in the village of Loudun, shows its elevated position above the surrounding country and affords a bird’s-eye view of the adjacent river, the Martray. (Courtesy of Monsieur le Pasteur Paul Barnaud, of Sainte Foy la Grande [Gironde], France.)
At the time when Renaudot came to Paris, there existed no such thing as the “Journal”—that is, a printed periodical such as he contemplated and afterward founded. At an interview with Cardinal Richelieu, the Secretary of State of Louis XIII., Renaudot proposed that all the news received from the outside world, the king’s edicts, and treaties made with other nations should be brought together and published at stated intervals in a single printed sheet. The cardinal at once saw how important the proposed journal would be for his own interest, especially if its management were intrusted to a man who agreed with him in regard to political questions. Then, in addition, the mere fact that it was an official sheet, the only strictly French periodical, 6would be of special value at that moment, when the princes of the blood were forming alliances with the enemy. So, on May 30, 1631, Louis XIII. granted to Renaudot “the privilege to make, print and sell, through any agent whom he might select and wherever it seemed to him best to sell copies, the news, the official appointments and accounts of all events occurring both within and outside the kingdom.” The first number of the “Gazette de France”—which was the name that Renaudot gave to his periodical—appeared on the day mentioned above. The price at which this sheet of four pages sold was two liards.[1]
One year later, the size of the Gazette was increased by the addition of four separate pages which bore the title, “Nouvelles,” and simultaneously the price of the entire journal (8 pages) was increased to one sou. It is scarcely necessary to state that the Gazette was directly inspired by Richelieu, and that even the king occasionally took a hand in editing it. Gilles de la Tourette, the author of the memoir from which I have compiled the present brief sketch, says that he examined all the issues of the Gazette from 1631 to 1653 but failed to find in them a single réclame—advertisement or editorial puff.
From the very day on which it was first published, the Gazette proved a brilliant success. I should have mentioned, at the beginning of this sketch, the fact that for a certain length of time Renaudot contributed liberally from his own funds toward the support of his pet schemes of benevolence, but it does not appear, in the account given by de la Tourette, whether the Gazette enterprise should not be counted as one of these schemes. At the same time, the thought naturally suggests itself that this physician’s motive in advocating the publishing of an official newspaper like the Gazette was probably a strong desire to win for his humanitarian schemes the strong support which the Cardinal and the King would be able to grant. Whether this be true or not, the idea of creating an official newspaper 7under the protection of the highest authority in France certainly showed far-sighted wisdom on the part of Renaudot. In 1640,—i.e., nine years after the founding of the Gazette as an official dispenser of political and civic news,—Renaudot changed its scope by adding to it the character of a medical journal. After 1640, therefore, the Gazette may rightly be classed as representing the first attempt to publish a medical periodical in France.
CARDINAL DUC DE RICHELIEU
(From a portrait engraved on copper by Nanteuil in 1655.)
Another important feature was added by Renaudot to his philanthropic scheme in this same year 1640. He obtained from the King a decree authorizing him to establish a “Bureau de Consultations Charitables pour les Pauvres Malades.” The manner in which this Bureau was to be conducted may be briefly explained in the following words. At certain fixed hours fifteen physicians, all of them friends of the founder, and a smaller number of apothecaries presented themselves at the Bureau, where, seated at a few separate tables, the physicians listened to the statements made by the poor people who had come there in the hope of obtaining relief from their maladies. In the simpler cases, a single physician was fully equal to the task of prescribing whatever the patient’s condition called for, but in those of a more obscure nature, two or three of the physicians present joined in a consultation. After the question of a suitable treatment had been decided, one of the apothecaries in attendance prepared the remedy or remedies which had been prescribed, and at the same time a written statement of the diagnosis was handed to the patient. If the ailment happened to be of a surgical nature, the measures required for its treatment were carried out on the spot. Some of the patients who presented themselves at the Bureau were easily able to pay for professional advice; and, when such a person appeared, an opportunity was afforded for dropping into a suitable box the fee which he or she was disposed to give. This money was utilized in paying for the remedies furnished the poor. In exceptional cases, it was perfectly evident that drugs alone could not afford the desired relief; the need was rather for more and better food. Fully realizing this need, and acting under his strongly benevolent 8impulses, Renaudot not infrequently placed money in the hands of these suffering dispensary patients when they were about to return to their homes. The exact amount of these gifts is not known, but they must in the aggregate have been large; for his biographer says that, in addition to the sums which his more prosperous patients placed in his hands for the benefit of the poor, he contributed annually out of his own purse, toward the maintenance of these free consultations, the sum of 2,000 livres (the “livre” being of about the same value as the franc). The success of the Bureau was so great that in the course of a few months it became necessary that a certain number of physicians should be at the consulting rooms of the institution at all times during the day.
As a natural result of this increase in the Bureau’s popularity the celebrity of Renaudot also increased, until it extended to every part of the kingdom; and, as a further result, the institution itself now began to take on the character of a school for clinical instruction—an entirely new feature; for at that period no facilities of this kind were provided by the Paris Faculty of Medicine. When Renaudot observed this new and unexpected development of the work carried on at the Bureau he petitioned the King for permission to erect, at his own expense, in the Faubourg St. Antoine, the most populous quarter of the City of Paris, a “Hostel des Consultations Charitables”—in other words, a free hospital for the poor.

Statue of Théophraste Renaudot at Loudun, France. (Courtesy of Monsieur le Pasteur Paul Barnaud, of Sainte Foy la Grande [Gironde], France.)
Up to the year 1638 Renaudot had got along very amicably with the Paris Faculty. He had often consulted with them and he had entered the names of his two sons, Isaac and Eusebius, as students at the medical school. Furthermore, there could not have existed any prejudice against him on religious grounds as—upon the advice of Richelieu and Father Joseph (Leclerc du Tremblay, or “His Gray Eminence”)—his two sons had been educated in the Roman Catholic faith. It appears, however, that these favorable considerations were not strong enough to prevent professional jealousy, on the part of the Paris physicians, from setting to work to undermine all Renaudot’s good work. 9The real truth—viz., that the newcomer’s success was robbing them of some of their paying practice—was not confessed by these men openly, but instead they objected to his having, with the King’s permission (granted in 1640), established furnaces for the manufacture of chemical remedies. They also claimed that he was injuring the profession of medicine through his doctrine that good effects were obtainable from the employment of both opium and antimony as internal remedies, and also through his maintenance of the new doctrine (1616) of the circulation of the blood. Were not these professional sins, they claimed, sufficiently heinous to justify them in summoning him before the magistrates as an impostor? They believed that they were fully justified in so doing; and accordingly they proceeded without further delay to bring suit against Renaudot.
It would require much additional space to furnish here even a condensed account of the events which characterized this disgraceful attack by the Paris Faculty—and especially by Guy Patin, who was at that time its Dean—against Renaudot, and I have therefore no hesitation in omitting all but one or two further details of this part of Renaudot’s history. In the first place, Cardinal Richelieu and the King stood firmly by Renaudot to the very end; and, on July 14, 1641, the King’s Council condemned the Faculty on all points of their charge, and in this manner granted complete authorization to Renaudot’s work. He himself, notwithstanding the great victory which he had won over his unscrupulous enemies, all of them physicians of high social position, resumed his efforts to win them over to a friendly attitude—not toward himself individually, but toward the benevolent schemes which he was doing his best to establish on a firm footing. All his efforts, however, toward pacification proved of no avail.
Not long afterward Renaudot’s two sons, both of whom had by this time completed the regular course of studies at the Medical Schools, made a respectful request to the Faculty for permission to appear before them for the examination to which all candidates for the degree of Doctor of Medicine were obliged to submit. In the meantime, 10as if to show his approval of the request which Renaudot’s sons had made, Richelieu had taken Eusebius with him as his physician-in-ordinary when he joined Louis XIII. at the seat of war in the southern part of France. But neither this kindly act on the part of the Cardinal, nor any of the other efforts made by Renaudot’s friends in behalf of his two sons, seemed to make any impression upon the Faculty. They refused point blank to grant the desired opportunity for an examination. As a last resort, Isaac appealed to Parliament “to issue a decree to the effect that the Faculty of Medicine must confer the degree of M.D. on both Isaac and Eusebius Renaudot within fifteen days; and declaring that, if the decree should not be obeyed within the prescribed limits of time, the decree itself should serve as full equivalent for the title in question.” The Faculty duly entered the decree upon their registers, but in secret they determined that the two Renaudot brothers should be excluded from all their official meetings. Théophraste Renaudot protested and the Faculty of the University of Montpellier pleaded warmly in his behalf, but it was of no avail. After the death of Richelieu the Paris Faculty had no difficulty in thwarting nearly all the excellent schemes of Renaudot. He was obliged to abandon the plan of building, at his own expense, a hospital, and his two sons were not permitted to practice medicine in Paris. He continued, however, to edit the Gazette up to the time of his death in 1653.
Gilles de la Tourette, in his interesting memoir, makes the following reflection upon the career of this pioneer journalist:—“All the innocent inventions of this benefactor of humanity are prospering to-day. In addition to his plan for building a hospital, he was the first to organize the whole scheme of Public Assistance—viz., charitable consultations (not unlike our dispensary work) and gratuitous visits at the residences of the poor. And, in addition to these, he introduced the Monts-de-Piété into Paris and also his Bureau of Addresses of exchange and redemption. To this man whose guiding maxim was ‘Lend money to the poor without expecting any return,’ posterity owes some reparation, 11and I hope that soon it will be possible to erect in one of our public squares a monument that will perpetuate the memory of the greatest philanthropist of the seventeenth century.”[2]
MEDICINE IN NORTHERN AND CENTRAL GERMANY DURING THE EIGHTEENTH CENTURY
LOW STATE OF MEDICAL AFFAIRS IN GERMANY AT THE BEGINNING OF THE EIGHTEENTH CENTURY
The intellectual activity of Germany was very low during the first half of the eighteenth century, and this statement applies with equal truth to all the departments of learning. It was only at the time of the French Revolution and for a few months previous to this period that the signs of an awakening began to show themselves. The prevailing unrest and turmoil in the political world are commonly assumed to have furnished ample cause for this widespread intellectual inactivity; and yet, on the other hand, it is conceivable that it was these very disturbances in the domain of politics which had the effect of stimulating the marked increase in mental activity which soon followed. This certainly seems to have been true of general literature, for it was toward the end of the period named that what are admitted to be the classical works of German authors—for instance, the writings of Klopstock, Lessing, Herder, Gellert, Wieland, Goethe, Schiller and the philosopher Kant—were first published. In medicine, says August Hirsch, one of the leading German historical authorities, other influences, beside those of a political nature, contributed powerfully toward the advancement of the science of medicine. The medical students and the younger practitioners, according to his statements, began at this period to show evidences of a wish to become more learned in things relating to their calling and to possess greater refinement in their manners and habits. Trips were made by them more and more frequently to the leading cities of France, Italy and England for the purpose of acquiring additional knowledge of medical science. Thus, little by little, the medical profession of 16Germany gained increased standing and respect from the community. Beginning with Prussia the governments of the different German states, one after the other, established examinations for the purpose of determining the fitness of the applicants for the right to practice medicine. Then, following the example of their rulers, members of the aristocracy adopted the practice of taking a physician with them on their travels, and the wish to be chosen for this privileged office acted upon the younger physicians as a decided stimulus to acquire greater skill and knowledge. Thus gradually the family physician, in many instances, came to be considered an adviser of greater importance than the clergyman. Then, beside, the knowledge that he had acquired this increased power and that he was held in greater esteem by society, reacted upon the physician’s character, rendering him more and more ambitious to excel and to deserve confidence.
While, during the earlier part of the eighteenth century, medical affairs in Northern and Central Germany were in the condition described above, there was taking place at Vienna, the capital of Austria, the most effective revival of medical science of which we possess any record. Of this important event, however, I will say nothing further at present. A reasonably full account will be found in one of the later chapters.
Although I have spoken of the early and middle portions of the eighteenth century as constituting a barren or stagnant period in the history of medicine, I would not wish to convey to my readers the impression that it was a colorless and uneventful period. Far from it. There was nothing colorless, for example, in Hahnemann’s eventful career, and yet to all appearances he was not contributing in any way to the genuine and solid advance of the science of medicine. Then, again, Hufeland is not commonly supposed to have contributed in any material degree to the advance of medical science, and yet his “Makrobiotik,” his “Art of Prolonging Life,” is a veritable mine of useful information that the practitioner of medicine can scarcely afford to classify as trivial. Hufeland also deserves the credit of 17having founded one of the earliest medical journals, a periodical which still, in many of its numbers that were issued during the later years of the eighteenth century, furnishes reading matter that to-day possesses the power to entertain even a twentieth-century reader. At a somewhat later date (1779) J. Peter Frank founded the first journal or archives distinctly devoted to hygiene and medico-legal science. Farther on I will supply a few details concerning these two rather important contributions to medical knowledge.
Finally, there are a few men who, during this same relatively barren period of German medical science, made permanently valuable contributions to our stock of knowledge. Among these stands out conspicuously Johann Christian Reil (1759–1813). Although lack of space prevents me from doing anything like full justice to these worthy representatives of our profession, I will endeavor to furnish in the next chapter at least sufficient information concerning their work and characters to enable the reader to place them in their proper niches in the history of medicine.
PHYSICIANS WHO ATTAINED DISTINCTION IN SOME OF THE DEPARTMENTS OF MEDICINE DURING THE FIRST HALF OF THE EIGHTEENTH CENTURY
In looking over the list of medical men who attained distinction during the first half of the eighteenth century, one can scarcely fail to note two important facts, viz., that they hailed from widely separated localities in Western Europe,—for example, from England, Holland, Northern Germany, France, Austria, Switzerland and Italy,—and also that the advances which they effected in medical knowledge were not confined to one or two departments of this science but included very nearly all the fundamental branches. Hence it could not rightly be claimed by a citizen of any one of these countries that his own nation was entitled to be considered the leader in this advance. It would be a waste of time, and would require more space than can be spared for such a purpose, to furnish here even an incomplete list of the anatomists, biologists, chemists, pharmacologists, diagnosticians, therapeutists and surgeons who during the period named took a very active part in the work. Probably Boerhaave of the University of Leyden, Holland, of whose career I have given some account in the preceding volume, deserves to be reckoned one of the first physicians who exerted a strong stimulating influence upon the movement as a whole. From a superficial examination of his writings the modern physician finds it difficult to understand why Boerhaave attained so great a degree of popularity as he indisputably did,—a popularity, too, which was of the best sort; for during the period of his professorship both students and practicing physicians flocked to Leyden from all parts of Europe, and they never tired of speaking 19about the great benefit which they derived from Boerhaave’s teaching. Many of them attributed this popularity more especially to his practice—which at that time was a novelty—of laying great stress upon bedside teaching and upon the importance of studying disease from direct observation of its manifestations in the living subject. Then, in addition, there is evidence that, as a teacher, Boerhaave undoubtedly possessed the gift of exerting a personal charm upon his auditors.[3]
Not a few of those who were privileged to receive instruction from this celebrated physician became themselves distinguished afterward as teachers or authors, and thus Boerhaave’s method of teaching was perpetuated. Among the physicians to whom reference has just been made were such men as Albrecht von Haller, of Berne, Switzerland, Van Swieten, of Vienna, and Hoffmann, of Halle, Prussian Saxony, many of whom are well known to-day in a general way to students of the history of medicine, but who, nevertheless, in at least a few instances, are worthy of having their careers described in further detail. In the following pages I propose to supply biographical sketches of these men and to show in what respects they exerted a beneficial influence upon the great body of their confrères, and also to what extent they made contributions to the science of medicine in its various branches.
It will undoubtedly surprise some of my readers, as it did me, to learn that during the comparatively barren period of the eighteenth century, to which brief reference has been made on a previous page, there were in Northern and Central Germany several anatomists and biologists who did creditable work as original investigators in these departments of medicine. Of this small number, however, I shall mention here only one—Reil. While he spent the greater part of his life in Germany, he was in reality a native of Holland.
Johann Christian Reil was born at Rhaude, East Friesland, in 1759. His father, who was the pastor of the village 20church, gave his son an excellent preliminary training, which enabled him, at the age of ten, to enter the high school (Gymnasium) in the neighboring town of Norden. On attaining his twentieth year, Johann entered the University of Goettingen, but he remained there only a short time, as he had become convinced that the Halle University offered greater facilities for those who intended, as did Reil, to follow a medical career. Three years later, armed with the degree of Doctor of Medicine, he began the practice of his profession at Norden. In the course of five years he managed to build up such a reputation as a successful practitioner that the University of Halle invited him to occupy the position of Professor Extraordinary of Clinical Medicine. Then, after the lapse of only a short year from the time of his acceptance of this invitation, he was promoted to the full professorship. Almost simultaneously he was appointed (1789) to the position of City Physician of Halle. It was probably while serving in the latter capacity that he began to reveal to the Government that he was not only an excellent physician but also possessed, at the same time, unusual executive ability.
Between the years 1789 and 1806, at which latter date the German army met with a disastrous defeat at the hands of the French (battle of Jena), the almost constant warfare brought all official university work to a stop. But Reil was not idle during this long period, for it was at this time that he devoted himself chiefly to laboratory research work with reference to the anatomy and physiology of the brain and nerves. The products of this work are recorded in the Archives of Physiology which Reil published in 1796 in association with Autenrieth, and they are pronounced by Sudhoff to be masterly. One of the cerebral structures which Reil was the first to describe is that known to all anatomists as “the island of Reil.”
Another important series of studies which were made by Reil were published by him under the title: “On the Diagnosis and Treatment of Fevers” (Halle and Berlin, 1799–1816; 3d edition, 1820–1828).
Finally, mention should be made of a memoir on “Vital 21Force” which Reil published in the first volume of his Archives, in July, 1795; an essay which—according to Sudhoff—should be read with very close attention, for it, more than all his other published writings, has carried Reil’s name (and will continue so to carry it in the future) triumphantly through the history of the science of biology. The author states his final conclusion as to the nature of vital force in the following words: “Every part of an organism accomplishes its work through its own inherent power, and the latter is a characteristic phenomenon that is dependent upon the manner in which the material of which it is composed is mixed and also upon the form that it takes.” Dezeimeris gives a slightly different rendering of this passage, viz., “It is absurd to search for the source of life (vital force) elsewhere than in the tissues themselves, and in them the vital phenomena vary partly according to the manner in which their elements are mixed and partly according to the form in which they are arranged.” Farther on in this volume, as I shall show, Claude Bernard, the distinguished French biologist, furnishes a third definition of “vital force.”
When the terrible fighting that occurred at the battle of Leipzig in 1813 necessitated the rapid construction and organization of hospitals large enough to accommodate the many thousands of sick and wounded[4] that had accumulated after this battle, the King of Prussia promptly assigned to Reil the entire management of this important business; and the result proved that he had entrusted this work to the right man.
Reil’s death from typhus fever occurred at Halle on November 12, 1813.
Sudhoff thus sums up the most striking traits of this distinguished physician’s character: “He was never satisfied with half-way measures, and bold schemes and great undertakings occupied his thoughts at all times. At the bedside he gave himself up unreservedly to the interests of the patient.”
22Samuel Hahnemann was born at Meissen, Saxony, in 1755. Although his parents were poor he managed to obtain a good education, not only in the fundamentals usually taught at the schools, but also in the knowledge of the various languages, such as Latin, Hebrew, Arabic, Spanish, English, French and Italian. In his medical training he advanced so rapidly that already at the comparatively early age of thirty-five he was recognized as one of the leading physicians of Germany. Even Hufeland, who at this period (about 1790) was the highest medical authority in the nation, accorded him full confidence both as a man and as a chemist; and yet at the same time there is no evidence to show that he frankly adopted his teachings with regard to the new doctrine of homoeopathy.
Hahnemann’s first experiments in relation to the action of drugs—says Wheeler, the most recent translator of the “Organon”—were made upon cinchona bark, which at that period was universally admitted to possess remarkable power in relieving and curing “ague,” as the usual form of malarial disease was then termed. “Hahnemann’s experiment”—he goes on to say—“consisted in taking a large dose of cinchona bark while he was in good health and noting its effects upon his healthy body. To his surprise he found reproduced upon himself all the chief phenomena (and even many of the minor symptoms) of a paroxysm of ague. When the attack passed off, a second dose produced a second paroxysm, and Hahnemann was presently face to face with the fact that this drug, which so often cured ague, was capable of reproducing in his own healthy body the phenomena of ague. Like, in fact, cured like.... As soon as the cinchona experiment suggested to Hahnemann the possibility that the principle of like to like (similia similibus) might prove a general law of healing, he began a systematic study of the records of medicine in the search for instances.... Over and over again he found that a drug prescribed empirically had proved itself capable of curing conditions similar to those which it could produce. The records of medicine, in fact, gave plenty of encouragement 23to his now dawning belief that similia similibus is a genuine Law of Cure.”
It is at this point, as it seems to me, that Hahnemann displays the first and most important defect in his reasoning machinery. He allowed what seemed to him to be a most important and highly beneficent therapeutic truth immediately to take possession of his whole being,—indeed, to take such complete possession that, from this moment forward, throughout the remainder of his life, he was utterly unable to weigh with a calm and unprejudiced mind the various facts and considerations which ultimately relegated homoeopathy to its proper place in the medico-historical museum, alongside those hoary relics of methodism, incantations, the weaving of charms, Stahlism, Brunonianism, etc. In short, he lacked those immensely important mental characteristics which enabled Harvey to discover the more important facts relating to the circulation of the blood, and which made it possible for Jenner to place in the hands of his fellow men an effective weapon of defense against the deadly ravages of small-pox. If asked to say what are these characteristics, I would reply: A state of mind so open and so unprejudiced that it can weigh with absolute fairness all the evidence laid before it, and an imagination so clever and so fertile in resources that it is able to invent the means of reproducing at will all those phenomena which it is desirable to study more closely. These, I believe, are the characteristics which Hahnemann lacked and which are absolutely necessary for the creation of a permanently useful creed and principles of therapeutics.
In Hahnemann’s “Organon,” he provides quite a long series of aphorisms in which the new doctrine is somewhat fully developed. I have transcribed, below, a few of these in order that my readers may be able to learn at first hand just what their author had in mind when he wrote them.[5]
Aphorism 5.—It may be granted that every disease must depend upon an alteration in the inner working of the human organism. This disease can only be mentally conceived through its outward 24signs and all that these signs reveal; in no way whatever can the disease itself be recognized.
Aphorism 6.—... A thing or a condition demands a first proximate cause only in order to come into existence; where the thing or condition actually exists it requires no further originating, no first and proximate cause, for its continued existence. Thus a disease, once established, endures independently of its proximate, exciting, primal cause: endures without further need of its cause: endures even if its cause no longer exists. How, then, can the removal of the cause be held to be the principal condition of the cure of the disease?
Aphorism 8.—The unprejudiced observer ... is unable, however acute he may be, to take note of anything, in any single case of disease, except the changes in the condition of the body and soul which are perceptible by the senses, the so-called disease phenomena, symptoms in fact; in other words, he can note only such fallings away from a former state of health as are recognizable by the patient himself, the friends in attendance, and the physician. All these perceptible signs make up together the picture of the disease.
Aphorism 9.—... And thus this symptom-complex ... is the only means whereby it is possible to discover a remedy for it (the disease), the only means which can indicate the most appropriate agent of cure.
Aphorism 13.—Now since, when cure is effected through the removal of the whole range of the perceptible signs and symptoms, the inward change which caused the symptoms is also removed (that is, the totality of the disease), it follows that the physician has only to clear away the entire symptom-complex in order also to get rid of the inward alteration—in other words, to remove the whole disease, the disease itself, a feat which must always be the only aim of the rational healer; for the essence of the art of medicine consists in compassing the restoration of health, not in searching for the change in the inward and hidden things; a quest which can tend to nothing but fruitless speculation.
And then follows, in the form of an “Author’s Note,” the subjoined commentary by Hahnemann:—
It is only through a misuse of the desire to reach the eternal, sown in the spirit of man for nobler purposes, that these impudent attempts have been made upon the realm of the impossible, those speculative broodings over the essential nature of the medicinal powers of drugs, over vitality, over the invisible working of the 25organism in health and over the changes of this hidden inner working which constitute disease—in other words, over the inner nature and essence of illness.... When the physician maintains that research into such things is necessary, then he shows a misconception of the capacities of men and a misunderstanding of the requisites for the work of healing.
... If only it had served the practice of medicine in the slightest degree,—if all this subtile investigation had revealed the true remedy for the least of diseases, it might yet pass for desirable!
Aphorism 31.—The great homeopathic law of cure rests on this law of man’s nature, revealed by experience, that diseases are only destroyed and cured by similar diseases. The homeopathic law may be thus formulated: that a disease can only be destroyed and cured by a remedy which has the tendency to produce a similar disease, for the effects of drugs are in themselves no other than artificial diseases.
The preceding more or less disconnected portions of the text of Hahnemann’s great work—“Organon of the Rational Art of Healing”—are quoted here, not with the idea that they will convey to the reader a very clear idea of the doctrine of homoeopathy and of the way in which it is to be applied in the practice of medicine, but rather for the purpose of showing the extraordinary manner in which Hahnemann utilized his reasoning powers in his efforts to create a new pathology and a new system of therapeutics that would harmonize with this new doctrine.
A further inquiry into the manner in which the disciples of Hahnemann acted upon these principles of homoeopathy in the practice of their profession establishes the fact that they believed in the remedial efficiency of doses that contained as small a quantity as the billionth or the decillionth of a grain of the drug. In a report which he makes to the Medico-Chirurgical Society of Edinburgh, James J. Simpson, the distinguished professor of midwifery in the University of that city, comments (1851–1852) upon these infinitely small doses in the following terms:—
If a grown-up man were gravely and seriously to assert to the world that two and two make five, the world would be inclined to look upon him as doubtfully rational, inasmuch as he defied the principles of common sense. And when other grown-up men tell 26the world that they can cure this or that disease with a billionth or decillionth of a grain of this or that common and probably inert drug, they express an opinion perhaps even more intensely and directly absurd than the doctrine of two and two making five; but they do not equally see through the absurdity and impossibility of the more complicated, but equally ridiculous idea, of the billionth or decillionth of a grain of oyster-shell, or chamomile, or belladonna, or the like, having any possible effect whatever upon the economy, for, resting contented with the mere name, they never once think or dream of what in reality a billionth or a decillionth amounts to.... For it is a sum the mere figures of which can scarcely give us any conception of its infinitesimal amount, viz., 1 followed by sixty ciphers.... Surely men holding such fantastical doctrines, are not men mentally fit to be members of such a Society as this.
In further corroboration of Dr. Simpson’s remarks, I may be permitted to furnish here a few brief extracts from Jahr’s “Manual of Homoeopathic Medicine” (Vol. I., pp. 386 et seq.):—
Symptoms produced by common House-Salt.—Rigidity of all the joints, which crack when they are moved,... Bad effects of a disappointment.... Frightful dreams of quarrels, murders, fire, thieves, etc.... Typhus fever with debility.... Awkwardness.... Numbness and insensibility of one side of the nose.... Speech embarrassed in consequence of the heaviness of the tongue.... Loss of appetite, especially for bread, and repugnance to tobacco smoke.... Numerous flaws in the nails.... Redness of the great toe, etc. (The list contains at least thirty additional symptoms.)
At the present day it is hard to believe that as recently as during the first half of the nineteenth century there existed an editor who was willing to publish such childish reading matter as the above. And yet one is obliged at the same time to admit that the appearance of text like this in a reputable book furnishes good evidences that there was no lack of readers to whom the information imparted proved acceptable.
Between the years 1850 and 1860, homoeopathy assumed a good deal of prominence in the city of New York. Many of the leading families during this period turned their backs on the regular practitioners,—the “Allopaths,” as they 27were then frequently called,—and confided themselves and their maladies to the care of members of the new school. This naturally led to much bitterness of feeling between the two groups of physicians, just as had happened at an earlier date in the larger towns of England and Scotland; and this condition of things lasted for at least twenty years. Hostile action on the part of the county and state medical societies proved of very little use in diminishing the popularity of the new method of treating diseases; and so it was finally decided to withdraw all further opposition to the new sect and to see what an attitude of indifference and the stopping of all persecution would accomplish. Thanks largely to this wise and sensible policy, homoeopathy gradually lost its short-lived ascendancy, and the more sensible members of the community returned to their former allegiance. What I have said in regard to the rise and fall of homoeopathy in New York is, I am confident, true in a general way of its fate in most of the other large cities of the United States, but I am personally familiar only with the conditions that prevailed in my native city.
I wish that I might speak with a larger measure of authority in regard to the causes that led to the favorable reception of this new sect in New York, but I am not able to do this, and I doubt whether anybody among my contemporaries is able to do much better than merely to suggest some of the more obvious causes which favored the popularity of the new school of practice. Among such causes I may mention the fact that in those days the practitioners of the regular school were in the habit of prescribing drugs in large doses and with very little effort to render them palatable. Take, for example, senna tea, of which bad-tasting medicine the patient was expected to take a large teacupful shortly after the early crowing of the cock; and if, a day or two later, a repetition of the same dose was ordered by the attending physician, can anybody wonder if the remedy was quickly pronounced by the patient much worse than the disease? Experiences like the one just narrated were by no means uncommon, and, as a consequence, many families did not hesitate to transfer their patronage to a class of 28physicians who never prescribed any remedy that had a bad smell or taste or that caused the slightest bodily discomfort. Then, beside, it is a well-known fact that, during the period now under consideration, the regular practitioners had, in not a few instances, been guilty of prescribing therapeutic measures which actually inflicted harm. Such, for example, were the giving of mercurial preparations in too large doses, the too frequent resort to bloodletting, etc. For all these reasons, it is not at all strange that for a period of several years (1850–1875) homoeopathy flourished in New York. In all fairness, therefore, it may be said that the great improvement in the manner of administering drugs which took place, both here and in European countries, during the period from 1860 to 1880, may be attributed indirectly to the influence of the new sect.
Hahnemann died in Paris in 1843, at the age of eighty-eight.

HUFELAND
(From Eugen Hollaender’s “Medizin und Plastik,” by permission.)
Christoph Wilhelm Hufeland, who was born in 1762, at Langensalza, in the district of Thuringia, Central Germany, founded, about the year 1795, a medical journal that bore the title, “Hufeland’s Journal der Practischen Heilkunde,”—the first German medical journal that was devoted largely to matters of interest to the practitioner. It was published regularly every month and was in almost every respect similar to the best medical journals of the present day. It was kept in active circulation up to the time of the founder’s death in 1836, and was highly appreciated by physicians generally. Hufeland’s reputation, however, rested less upon this journal, notwithstanding its great popularity, than it did upon his famous treatise entitled “The Art of Prolonging Life” (Makrobiotik). This book, which has been translated into every modern language, and which during the past century and a half has never had a rival in the field of which it treats, continues to-day to furnish entertaining reading to hundreds of men and women, laymen as well as physicians, who desire to learn the well-established facts regarding human longevity. Farther on, I will furnish a few extracts from both of these publications, thus 29enabling those of my readers who have not yet had an opportunity to become acquainted with Hufeland’s writings or with his work as a journalist, to learn something more definite about the man.
So far as I am able to ascertain, Hufeland’s only other important activities were those connected with the positions which he held in the Universities of Jena (1793–1798) and Berlin (1798–1835). In the former institution, he held the Chair of Medicine; in the latter he held the same chair, but he was also acknowledged to be the guiding spirit in all matters relating to the organization and management of that important centre of medical education.
Among the items of special interest in Hufeland’s “Makrobiotik,” I find the following:—
On the 2nd of August, 1790, a carabinier named Petit jumped into the Rhine from one of the windows of the Military Hospital at Strassburg. Half an hour later,—as nearly as could be learned from an inquiry that was made at the time of the occurrence,—his body was taken from the water and carried into the hospital. To all appearances the man was dead; no evidences of life were discovered. Nevertheless, efforts were made to revive him. The body was placed in a thoroughly warmed bed, with the head lying high up on a pillow, the arms resting on the trunk, and the legs extended side by side. The only other measures adopted were the following: At short but regular intervals of time heated cloths were placed over the region of the stomach and over the legs; and heated stones wrapped in cloths were placed in different parts of the bed. At the end of seven or eight minutes a slight twitching of the man’s upper eyelids was observed, and a short time afterward his lower jaw, which up to that moment had been in firm contact with the upper jaw, became separated from it and permitted a little frothy mucus to escape between the lips. After this discovery had been made, a little wine was cautiously introduced into the man’s mouth. Apparently it was swallowed, and then other small doses of wine were administered, all of them apparently being swallowed. Under this stimulation the pulse beats at the wrist became perceptible, and at the end of one hour the man was able to answer questions.
In his comments upon this interesting case of restoration of life after apparent death from drowning, Hufeland makes the following remarks:—
30It is evident, therefore, that artificial heat acts with the same vigor immediately after the appearance of what seems to be death as it does at the very first dawn of life; it gradually fans into a living flame the few vital sparks which may still be present in the body.
In the preceding account of the means adopted for resuscitating the soldier who was believed to be dead from the effects of drowning, no mention is made of friction of the surface of the body as a procedure of some value. Hufeland, very properly, lays great stress upon the need of applying heat. Friction, however, if employed intelligently, may prove a most efficient adjunct; and, when I use the expression “intelligently,” I mean that friction may be utilized as a powerful agent for propelling toward the heart the artificially heated blood contained in the cutaneous blood-vessels, thus contributing in no small degree toward the reëstablishment of the circulation. The kind of friction required—it seems scarcely necessary to say—should always be directed from the extremities toward the heart.
In another part of the same work Hufeland gives an account of several instances of exceptional longevity. One of these relates to Terentia, the wife of Cicero, who, despite the sore trials to which she was subjected, and despite the occasional attacks of gout with which she was afflicted, attained the great age of 103. A second instance is that of Livia, the wife of the Emperor Augustus, a woman who possessed a domineering and passionate character, but who, nevertheless, was blessed with a full share of happiness. At the time of her death she was ninety years old. Two other Roman women are mentioned by Hufeland as having attained a great age. They were both of them distinguished actresses. The first one, whose name was Luceia, began her theatrical career at a very early age and was 112 years old on the occasion of her last appearance on the stage; her entire theatrical career having covered a period of one hundred years. Galeria Copiala is the name of the other actress, who was at the same time famous as a danseuse. Ninety years after her first appearance on the stage she took part in a complimentary performance in honor of Pompey; 31and even at a still later date she acted in a play which was intended to celebrate the distinguished reign of the Emperor Augustus.
Hufeland mentions further instances of great longevity which he had gleaned from Jewish history, and from these I select the following: Abraham lived to be 175 years old, and his wife, Sarah, the only woman of that remote period of time of whom we possess a precise knowledge, died at the age of 127; Isaac attained the age of 180; Jacob lived to be 147; Ishmael, a son of Hagar (one of Abraham’s hand-maids) and a man of warlike habits, attained the age of 137; and Joseph, the next to the youngest of Jacob’s sons, a political leader and a man of great wisdom, died at the age of 110. Moses, a man of conspicuous intellectual capacity and possessing a strong will, lived to be 120 years old. But even he complained that “the life of a man usually lasts only seventy years, or, in exceptional instances, eighty years”—a statement, says Hufeland, which justifies the belief that 3000 years ago the duration of human life was about the same as it is to-day. Joshua, who led a very active life and was a good deal of a warrior, died at the age of 110; Eli, the High Priest, a man of a phlegmatic temperament, lived to be a little over ninety years of age; and Elisha, who despised all the conventionalities of life and cared nothing for wealth, lived far beyond the limit of 100 years.
The Greek philosopher Pythagoras, who recommended care in the choice of one’s food, moderation in eating, and the cultivation of gymnastic exercises, attained a good old age. He claimed that after a man reached his eightieth year, no matter how great an age he might afterward attain, he should be reckoned among those who have ceased to live.
The measures which Hufeland enumerates as being specially conducive to longevity are those with which my readers—it may safely be assumed—are already familiar. The list comprises both those things which a man or a woman should carefully avoid, and those which often prove helpful in prolonging the period of one’s life, and which may be summed up in that old device: “Moderation in all things.”
On turning over the pages of the volume of Hufeland’s 32Journal in which are contained the issues of the first half of the year 1833, I came across the report of a very unusual case that was observed by a Dr. Heymann in the village of Oldendorf. His report reads as follows:—
A very poor working-woman, who in addition to her poverty was obliged to live in a house that was overrun with mice, retired to her bed one night in company with her child who was about three years old. One of the last things she did, after going to bed, was to hand to the latter a crust of bread, in the hope that the little one might thus, by quieting its hunger, fall asleep more readily. Having done this the mother herself soon fell asleep. But shortly afterward she was awakened by the terrified cries of the child, who insisted that there was a mouse in its throat. Having quickly obtained a light the mother discovered that not only was the child retching violently, but that it was bringing up visible quantities of blood from the stomach. In the contortions caused by the pain the child indicated the pit of the stomach as the source of all its agony. The severe pain persisted for about two hours and then suddenly ceased, but the retching and bringing up of blood continued at intervals for some time longer. On the following morning the child was given plenty of sweetened milk to drink. At the end of forty-eight hours the remains of the mouse were found in the stool. The creature’s body presented a collapsed appearance and the skin lacked its covering of fur in several places.
For quite a long time subsequently the child remained in an ailing condition, with symptoms of disordered digestion. Its death, however, which occurred at a somewhat later period, was apparently dependent upon an entirely different disease,—one that had no connection whatever with the incident just described.
After reviewing all the evidence in this extraordinary case, Hufeland sees no reason for doubting the correctness of the preceding report in all its essential features. As to the manner in which a mouse may find its way into the human stomach, the following statement is permissible. To begin with, it is a matter of common knowledge that mice often run about an occupied bedroom at night in search of food, and that their sense of smell is extraordinarily acute. Furthermore, it is easy to understand how a mouse, after tracing the odor of food to the partially open mouth of a sleeping child, would not hesitate, if pressed by hunger, to 33enter that cavity for the purpose of securing possession of the particles of food lodged therein; and it is also easy to understand how the intruder might then be caught as in a trap by the closing of the mouth which spontaneously followed. Under such circumstances the creature’s choice of the oesophageal route into the stomach as a way of escape was most natural, and equally so were the efforts made by the beast—as shown by the pain at the pit of the stomach and by the retching of a bloody fluid—to gnaw its way through the gastric mucous membrane.
Although Hufeland yielded to the prevailing tendency among German physicians of the eighteenth century to adopt doctrines, both in pathology and in therapeutics, which are based upon hypotheses rather than upon facts established by experimentation, or by direct observation at the bedside or at the autopsy, and which as a consequence played a very small part in the genuine advance of the science of medicine, he nevertheless, as I have tried to show in the preceding pages, should be classed as a most useful and honorable member of our profession.
Remember—he is reported to have said to his younger confrères—that there are two maxims which you should keep in mind, viz.:—
1. Natura sanat, medicus curat morbos;
(Nature cures disease, the physician merely does what he
can to facilitate the operations of nature);
and
2. Ne noceas, si prodesse credis.
(In your efforts to afford relief be careful not to do permanent
harm.)
DISTINGUISHED SWISS PHYSICIANS WHO PLAYED A PROMINENT PART IN THE DEVELOPMENT OF THE SCIENCE AND ART OF MEDICINE IN GERMANY
Among the men who may properly be included in the present class of distinguished German physicians I have no hesitation in naming von Haller and Zimmermann, notwithstanding the fact that both of them were natives of Switzerland—that is, German Switzerland.
ALBRECHT VON HALLER
Albrecht von Haller, whose many contributions to the science of medicine have assured him a permanent and very high position in the temple of fame, was born October 16, 1708, of parents who belonged to two of the old patrician families of Berne, Switzerland. In childhood he suffered from rachitic symptoms and was constantly ailing; but, despite these drawbacks, he manifested at a very early age evidences of possessing to an unusual degree certain intellectual gifts and of having a genuine love for work. Thus, for example, he began—shortly after he had learned to write—recording in alphabetical order all the words that he had been taught and the meaning of which had been explained to him. At the age of ten he prepared for his own use a vocabulary composed of Chaldean, Hebrew and Greek words, and two years later he compiled, from the dictionaries of Moreri and Bayle, a collection of concise biographies of the men who had achieved celebrity in the more important branches of science, and he surprised his teachers by his ability to compose verses in Latin as well as in his native language, German. Before he reached his fifteenth year he had attained considerable distinction, both as an anatomist and as a poet, a combination of gifts extraordinarily 35rare. He received his early training in anatomy and general medicine at the University of Tübingen, under the guidance of the two Duverneys, father and son, and of Elias Camerarius, all three of whom were professors of considerable celebrity in their respective departments. Jean Guichard Duverney (1691–1759), for example, was the first anatomist to furnish a complete and very thorough description of the solar plexus.
An incident which occurred during his student days at Tübingen reveals so strikingly von Haller’s strength of purpose and his unwillingness to permit anything to divert him from the path which he had decided to follow, that I shall not hesitate to relate it briefly here. In company with a few of his fellow students he participated in one of those beer-drinking bouts which are of such frequent occurrence in German university towns, and was in due course of time made acquainted with the legitimate effects that follow such excessive indulgence—effects that are felt as “seediness” and a sense of physical misery (symptoms to which the Germans have given the striking but untranslatable name of Katzenjammer). This single experience sufficed to impress upon von Haller’s mind the folly of such indulgence and he never afterward permitted himself to take part in an excess of this nature.
Although von Haller, upon the death of his father, had been left with very slender financial means, he managed, under the guidance of Albinus, on leaving Tübingen in 1725, to visit Leyden, in Holland, where he was able to prosecute his anatomical researches and at the same time to follow the instruction of Boerhaave, who was still at that period in full possession of his powers as a teacher. Extraordinary as it will appear to the physicians of to-day, von Haller, when only nineteen years old, passed successfully the required examinations at Leyden and was given the degree of Doctor of Medicine (1727).
From Holland von Haller went first to London, where he accepted the invitation of James Douglas, the anatomist, to assist him in his studies of the structure of the bones. Then from there he next visited Paris (1728), where he had 36for his teachers Le Dran, the distinguished French surgeon, and Winslow, the well-known anatomist. It was his original intention to make a prolonged stay in the French metropolis, but, unfortunately, his ambition to get ahead as fast as possible in the study of anatomy led him to disregard certain precautions which, in the early part of the eighteenth century, it was not at all safe for men interested in this branch of medical science to neglect. Recognizing the fact that, in order to advance his knowledge of anatomy, he must have a certain amount of human dissecting material at his command, and finding that he could procure this material in no other way than by the process commonly known as “body-snatching,” he decided, in association with one of the prosectors of the medical school, to adopt that method of procuring the material needed. The plan was successfully carried out, the disinterred body was transferred to von Haller’s apartment, and the two enthusiastic anatomists had already done a certain amount of dissecting when an unexpected obstacle was encountered. The layman who occupied the adjoining room overheard enough of the conversation that was being carried on between von Haller and his friend to suspect strongly the true nature of the work in which they were engaged. But, to make sure that his surmise was correct, he bored a peek-hole through the partition wall, and thus was able to remove from his mind all doubt about the nature of this work. The police were promptly notified, and von Haller was summoned to appear before the authorities to answer the charge of having disobeyed the law relating to dissections of the human body. Not being able to furnish a satisfactory reply to this charge, and wishing to escape from the severe penalties that would certainly have been inflicted upon him had he been apprehended, von Haller went at once into hiding in Paris and eventually succeeded in making his way over the border into Switzerland.
LAUSANNÆ,
Vignette from the title-page of Haller’s “Elementa Physiologiæ,” Lausanne,
1757
In 1729 he began the practice of medicine in his native city, after having taught anatomy for a short time in Basel; but he took only a subordinate interest in the treatment of disease, his preference being strongly for the scientific and 37literary parts of medicine. In 1734 or soon afterward he published a collection of his own odes and letters in German verses. These reveal very fully the nobility of his character, his good sense and the high standard of his philosophy. Dezeimeris says that von Haller offers the very first example of a man who has been able to develop to an equal degree his talents of poet and of anatomist.
In 1735 he was appointed Chief Custodian of the Public Library at Berne, and while he held this office he prepared a catalogue raisonné of all the books contained in that collection. At the same time he wrote a classified, chronologically arranged list of the 5000 or more coins and medals which are preserved in the library.
In 1736 the Hanover Regency offered him the professorship of anatomy, botany and surgery in the University of Goettingen, and agreed at the same time to furnish all the money needed for carrying out the extensive plans which he had formed for improving the facilities for teaching these branches of medical science. Von Haller unhesitatingly accepted the invitation, and during the following seventeen years (1736–1753) devoted his time and his best efforts to the fulfilment of the duties which his triple chair involved. Not only did anatomy, botany and surgery greatly thrive during this long period of time, but the university through his intelligent efforts gained in many other directions. It was upon his advice, for example, that the beautiful anatomical theatre at Goettingen was built and equipped. The botanical garden was another of the creations at Goettingen which owed its existence to von Haller. If I were to furnish a list of the improvements which, one after the other, were carried out in the university at his suggestion I would certainly be obliged to mention among other things the following: an establishment in which pupils might receive proper training in anatomical and botanical drawing; the creation of a cabinet of anatomical specimens and of a college of surgery; and finally the founding of a school for midwives. In short, it was largely due to von Haller’s enlightened conception of what such an institution of learning requires and to his untiring efforts that the University 38of Goettingen became, toward the end of the eighteenth century and during the first half of the nineteenth, one of the leading universities of Europe. Indeed he might justly be called its founder.
Von Haller’s health suffered under this long strain, and he was therefore more than justified in asking the Regency of Hanover for permission to resign and take up his residence in Switzerland. His request was unhesitatingly granted; and, after resting for a few months from his recent labors, von Haller resumed those quiet literary undertakings which he loved so keenly and which enabled him to publish such famous works as the following:—
“Primae Lineae Physiologiae” (First Lines of Physiology), Goettingen, 1747 (also 1751)—the very first systematic treatise on physiology of which we have any knowledge. A German edition was not published until 1759–1776.
Commentaries on Boerhaave’s “Institutiones Medicinae,” 1739–1744.
“Elementa Physiologiae Corporis Humani,” 8 vols., Lausanne, 1757–1766; the most important of all his works.
“Bibliotheca Anatomica,” 2 vols., 1774–1777.
“Bibliotheca Chirurgica,” 2 vols., 1774–1775.
“Bibliotheca Medicinae Practicae,” 4 vols., 1776–1788.
“Expériences sur les Parties Sensibles et Irritables,” 4 parts, Lausanne, 1759.
These titles represent only a small part of the numerous books and elaborate essays published by this tireless worker. In 1749 he was ennobled by the Emperor, thus gaining the right, so highly esteemed in Germany, of placing a “von” before his name.
In the middle of the eighteenth century there appears to have existed considerable confusion in the minds of scientific men regarding the distinction between the terms “sensibility” and “irritability,” and to von Haller is due the credit of having once and for all defined the correct meaning of these words. As early as in 1747, when he published the first edition of his treatise on physiology, von Haller taught that the contractile force of muscles is supplied by the nerves, and that in this way they acquire 39irritability, a force which they cannot exercise except through the influence of the nerves. Irritability, therefore, is not a characteristic that originates in muscular tissue but is conferred upon it by the nerves. Von Haller’s experiments reveal the fact that the heart possesses the maximum degree of irritability. Next in order come the intestines and the diaphragm, the ordinary red muscles possessing a lesser degree of irritability.
In order that the reader may form at least some idea of von Haller’s manner of treating physiological topics I give below a rough translation[6] of the first three paragraphs which occur in Chapter XX of his Primae Lineae Physiologiae (edition of 1751):—
564.—The power which a person in perfect health possesses freely to exercise the different senses and to perform voluntary movements is called wakefulness or the state of being awake; the absence of the power to make voluntary movements and to utilize the different senses, combined with the quietude of all of them, bears the name of sleep.
565.—In sleep the mind either stops thinking entirely of the things which have been stored up by the individual in his memory or which are well-known facts, or else it busies itself exclusively with certain ideas or with impressions that produce upon the mind, at the time, pictures almost as vivid as the actual things or occurrences which they represent would produce. The term “insomnia” is employed when it is desired to designate the latter condition of the mind, and the mental pictures thus presented produce the effect that—although voluntary motions are at the time all in abeyance, and although the mind is absolutely quiet in all other respects—there remain certain directions in which it continues to operate 40actively, thus producing an elevation of the spirits (i.e., a certain degree of excitement) and more or less wakefulness. Sometimes a certain number of voluntary movements are associated with these mental impressions, and this may occur in such a degree that the organs of speech and many of the joints—indeed at times all of them—are compelled to act in harmony with the mental impressions. When this degree of insomnia is reached the person so affected is called a “somnambulist.”
566.—But in sleep the distribution of the humors of the body goes on without let or hindrance; and, similarly, the circulation of the blood, the peristaltic action of the stomach, intestines and sphincters, and the respiratory movements continue their activity. This complex state of affairs—viz., the coexistence of quietude of certain parts of the body with continued motion in other parts—has made it difficult to ascertain the mechanical cause of sleep.[7]
In his investigations into these subjects, von Haller placed his reliance mainly on vivisections and on experiments made upon animals. “A single experiment of this nature,” he said, “is often sufficient to disprove the deceptive conclusions or views that have prevailed through a period of years.” It is to John Hunter of England, however, says Puschmann, that the greatest credit is due for the introduction of the experimental method as a means of 41ascertaining the truth in questions of pathology; and von Haller was unquestionably one of the first German physicians to adopt the method.
Von Haller died at Berne on December 12, 1777.
Johann Georg Zimmermann was born in 1728 at Brugg in the Canton de Berne, Switzerland. Left an orphan at the age of eighteen, and obliged without aid from outside to choose the career which he would follow, he decided to study medicine; and with this object in view he went to Goettingen, Germany, where he was received into the family of Albrecht von Haller, who was at that time a professor in the university. Five years later (1751), when he took his doctor’s degree, he chose for the subject of his thesis, at von Haller’s suggestion, the doctrine of irritability. Upon his return to Berne in 1752, he began the practice of medicine and shortly afterward accepted the position of official physician for his native town of Brugg. It was during this period of his life that he wrote those treatises which made his name famous throughout Germany, viz., “On Solitude,” Zuerich, 1756; “On Experience in the Practice of Medicine,” Zuerich, 1763 and 1767; “On National Pride,” Zuerich, 1768 (5th edition); and “On the Epidemic of Dysentery which prevailed during the year 1765,” Zuerich, 1767 (later edition in 1789).
In 1768, through the influence of Dr. Tissot, of Lausanne, he was given the appointment of Physician to the King of England at the Court of Hanover. During the last years of his life he took a great interest in political events, recognizing with remarkable foresight the approach of an immense revolution. So strong was his belief that current events pointed to the approach of such a catastrophe, and so depressing were the effects of this belief upon his naturally hypochondriac type of mind, that the last years of his life were thereby rendered most painful. He died on October 7, 1795, not long after the full effects of the Reign of Terror had developed in France.
Tissot, who had known Zimmermann well for more than forty years, has written a most interesting notice of his life 42and has placed a just estimate upon the value of his writings. (Dezeimeris.) Sprengel, the author of a well-known and highly esteemed history of medicine, speaks in the following terms of Zimmermann’s treatise “On Experience in the Practice of Medicine”:—
The manly and brilliant style in which it is written, its fascinating eloquence, and the special talent which the author displays in rendering marvelously clear—without at the same time robbing them of any of their accuracy—the most obscure topics, make this book of Zimmermann’s a veritable chef-d’oeuvre.... The importance of genuine experience, its difference from false or blind routine, the advantages which real erudition confers and the necessity of combining it with experience, the nature of the obstacles which an observing spirit must overcome, the absolute need of good observations and the useful qualities which they should possess, the effects of genius, and the manner in which conclusions are to be drawn by analogy and by induction—these are the questions with which the author of this classical treatise deals.
THE EARLIEST PUBLICATION IN EUROPE OF A SYSTEMATIC TREATISE ON HYGIENE, PUBLIC HEALTH AND MEDICO-LEGAL SCIENCE
In the early part of the eighteenth century municipal and private-house sanitation existed in comparatively few cities of Europe, and then only in the wealthier quarters. Such a thing as sanitary police was practically unknown, and public health was considered only when the inhabitants were threatened with a serious epidemic like that of cholera, the plague, or leprosy. This indifference to public sanitation persisted down to the end of the nineteenth century. On arriving in Paris in the spring of 1857, at a time when the city was overcrowded with travelers, my friend and I were glad to secure a room on the fourth story of a modest hotel situated in the central part of the city, quite near the Palais Royal. We found no good reason to complain of the room itself; it was clean and adequately well ventilated. But the toilet facilities were such as one might expect to find in a hotel of the fourteenth or fifteenth century. On the roof of our building a lean-to had been constructed alongside a broad brick chimney, and this shack, which was distant at least forty feet from the doorway that led by a short stair-case to the fourth story of the hotel, could be reached only over a narrow plank walk that was wholly unprotected by a railing. Then again, on a bicycling trip which I made in 1896, through the central part of France, my friend and I experienced more than one surprise of a similar nature. For example, in several of the smaller towns we found that the ancient practice of throwing the slops out of the second-story windows into the middle of the narrow street, still persisted. But, in a matter of this kind, nothing is to be gained by entering into many details; “enough is as good 44as a feast.” I merely wish to emphasize the fact that even France, where civilization was so far advanced in many respects, was fearfully slow in adopting the first principles of house and municipal sanitation. It was only toward the end of the nineteenth century that London, the birthplace of the finest types of house and municipal sanitation, began to give serious attention to this subject. During the early part of the eighteenth century, however, even this great metropolis was very backward in manifesting any marked desire to improve the sanitary condition of its dwellings; for, was it not the Earl of Chesterfield who, at this very period of time (about 1750) made the statement, in a letter to his natural son, that “the lanes or narrow passage-ways in Holland are cleaner than the houses are in London?”
It was in Germany, many of my readers will doubtless be surprised to learn, that the first really serious attempt was made to present to the world a scientific treatise on this subject, a work which was published in several consecutive volumes and which even to-day is consulted as a most trustworthy and remarkably complete authority on municipal and private-house sanitation. The work referred to was written by J. P. Frank.
Johann Peter Frank, more commonly spoken of as Peter Frank, was born in 1745 at Rothalben, a village located in territory which at that time belonged to the Grand Duchy of Baden. He received a good preliminary training at the High School of Pont-à-Mousson, and then afterward took courses at the Universities of Heidelberg and Strassburg. His medical degree was bestowed upon him in 1766 by the first of these institutions, the subject of his thesis being “Medical Police.” Two years later he commenced the practice of his profession at the city of Baden-Baden, and in 1769 was appointed Court Physician at Rastatt.
During these early years of his career he did not lose interest in the subject which he had chosen for his thesis, but continued to work upon it until, in 1768, he was ready to submit to a bookseller the manuscript of Vol. I. The latter, after receiving from a so-called medical expert an 45unfavorable report on the quality of the text, expressed his unwillingness to publish the work. Frank’s discouragement over this result was so great that he proceeded without delay to throw the manuscript into the fire. Then, after further reflection, he decided to begin work afresh on the same theme, and thus it came about that he devoted the following eleven years to the preparation of a new text for Vol. I. In 1779 this first volume was published. In 1780, 1783, 1788 and 1813 four more volumes were issued. Volume VI and two supplementary volumes were issued between the years 1817 and 1819.
“Notwithstanding its defects,” says Puschmann, “this work is one of the most important, one of the greatest and most creditable pieces of medical literature of which the Germans may rightfully boast. Blumenbach called it a classic, the first treatise of its kind and indeed possessing a unique character.”
Of the other works published by Peter Frank, works which deal with pathology and the practice of medicine, the most important is that entitled “De Curandis Hominum Morbis Epitome” (“An abridged treatise on the diseases to which man is liable”). As he progressed with the writing of this treatise Frank undoubtedly discovered that he could not, with any degree of satisfaction, accomplish his original design of compressing what he had to say into an “epitome”; and so, from this time forward, he carried on the work, without paying any further attention to his original plan of an abridgment, until the book had reached its sixth volume; and even then it was not completed.[8] Despite its incompleteness this work passed through several editions, for it was highly appreciated for its practical character and for the clearness of its descriptions of disease.
In 1785 Frank accepted an invitation to take charge of the clinical instruction at the University of Pavia, in the place of Tissot who had resigned. Through Frank’s advice and 46persistent efforts the medical department of the Pavia University was enriched by the addition of a chair of physiology and comparative anatomy, an anatomical theatre capable of seating 400 auditors, and a collection of pathologico-anatomical preparations to which all the hospitals of that part of Lombardy were obliged to contribute suitable specimens. The establishment of a surgical clinic was another of the improvements in the teaching facilities of the University that should be credited to Peter Frank. The length of the medical course was at his suggestion extended to five years. Among his associates in the Faculty at this period were the following distinguished men: Scarpa, in the chair of surgery, Scopoli, in that of pharmacology, and Volta in physics.
In November, 1795, Frank returned to Vienna and was almost immediately appointed Director of the Allgemeine Krankenhaus and Professor of the Medical Clinic with a salary of 5,000 florins and the privilege of occupying rent-free a house that was located in the immediate neighborhood of the hospital. At the same time the title of Aulic Councillor (Hofrath) was conferred upon him. One of the first improvements which he effected in the clinic was to have the small wards for male and female patients materially enlarged so that when twenty-five or thirty patients were present, as was often the case, the air might not become noticeably contaminated and thus rendered unfit for all who were present to breathe.
In his teaching Frank never forgot, on all possible occasions, to impress upon the students the importance of thinking independently on the subjects that were brought before them, as in this way they would learn to distinguish the false from the true. Whenever he discovered that he had made a mistake in one of his statements he did not hesitate to confess the fact. His son, Joseph, is responsible for the statement that his father never seemed to him happier than when he had an opportunity of making to his auditors some such speech as the following: “Gentlemen! Strike out this or that line in one of the volumes of my work! When I wrote it I believed that it was correct; but now I am convinced 47that the very opposite is the truth!” When Brunonianism was first transplanted from Great Britain to the Continent and was received enthusiastically by many physicians, Frank was not disposed immediately to accept its teachings, and yet at the same time he did not believe that it was quite fair to ignore the thing altogether. Not a few men inferred from this hesitating attitude on his part that he rather favored Brown’s system. As a matter of fact he was an eclectic in his views and was always ready to appropriate whatever seemed to him good in any system or school of doctrines. As Director of the Allgemeine Krankenhaus he adopted the plan of having the leading physicians and surgeons of the Clinic first report publicly once a week what were the important diseases that had come under observation during that period; and then he would call upon the auditors to discuss the subject freely.
Peter Frank died at his home in Vienna on April 24, 1821.
TWO EMINENT GERMAN SURGEONS OF THE PRE-ANTISEPTIC PERIOD
Johann Friedrich Dieffenbach, born in 1794 at Koenigsberg, an important city of Northern Prussia, received his early medical education in France; first under Boyer, Dupuytren, Larrey and Magendie, at Paris, and then later at Montpellier, under Delpech. After his return to Germany in 1823 he devoted his efforts largely to surgery, and soon distinguished himself so greatly in this department of medicine that in 1840, after the death of Karl von Graefe, he was chosen his successor in the office of Director of the University Surgical Clinic at Berlin. His death occurred in 1847.
Dieffenbach was universally considered a very clever operator, particularly in the field of plastic surgery. He was distinguished by a high degree of manual skill, remarkable presence of mind under the most trying circumstances, and boldness combined with prudence. His triumphs in the reconstruction of damaged parts of the body, effected largely by the transplantation of flaps of normal skin, were quite remarkable; he seemed to know just what steps were required for restoring a mutilated soft palate, ear, nose, eyelid, etc. But his interest was not confined to plastic surgery; he also performed successful operations in tenotomy, myotomy, transfusion of blood, and the injection of drug infusions into the veins.
The Schleswig-Holstein campaign, says George Korn in his “Progress of Medicine during the Nineteenth Century,” furnished a great stimulus to the advance of German surgery, by providing an extensive field for the activity of such men as von Langenbeck, Stromeyer and his 49son-in-law, Esmarch. The scantiness of available space, as well as of satisfactory sources of information, compels me to give here only the briefest details concerning these three distinguished surgeons.
The founder of modern German surgery, says George Korn, was Bernhard von Langenbeck (1810–1887). When he began active work as a surgeon he was already thoroughly familiar with human anatomy, physiology and pathology, and with the experimental methods of research. His first appearance as a teacher was at the University of Goettingen, where he remained for a few years, and then moved to Berlin, to occupy the chair of surgery vacated in 1847 by the death of Johann Friedrich Dieffenbach. In 1882 he gave up his professorship in Berlin and retired to Wiesbaden, where he spent the remainder of his life in quietude.
Before von Langenbeck’s day much stress was laid in Germany upon the importance of anatomy in its relationship to the science of surgery. It was a common practice in the medical schools, for example, to combine in one the two chairs of anatomy and surgery, and, imbued with the idea that this viewpoint was the correct one for them to adopt, the leaders in surgery, with few exceptions, strove to make advances in their branch of knowledge by cultivating energetically the study of anatomy. The efforts of von Langenbeck and his followers, on the other hand, were directed to giving new life to surgery by calling to its aid physiology, pathological anatomy and pathological histology, as well as experiments upon animals, sources of information which before von Langenbeck’s time had been very little utilized by the surgeons. Korn, in his comments upon the preceding statement, begs the reader not to interpret it as signifying that von Langenbeck permitted himself to neglect anatomy in the slightest degree. Quite the contrary, he continued to insist upon it that a knowledge of anatomy was the most useful foundation upon which a surgeon could build. As corroborative evidence of the correctness of Korn’s statement I will quote here the remarks made by an English 50physician who visited Goettingen in 1818 (London Quarterly Journal of Foreign Medicine and Surgery, Vol. 1, 1818–1819):—
We were pleased in observing the great attention which Professor von Langenbeck paid in these clinical exercises to relative anatomy. He omitted no opportunity of impressing on the students that the mere dissection of bodies could never make them good anatomists, and that, as surgery without the knowledge of anatomy would be a dangerous art, so anatomy without a constant reference and application to the living body would be vain and futile....
The foundation of the surgical hospital at Goettingen is entirely due to Professor von Langenbeck. In 1807, at his representations, a certain sum was appropriated to its support from the Cloister-fund. In 1808 the professor built the present hospital, which is still his own property, the Hanoverian Government paying him a yearly rent for it. The beautiful collection of surgical instruments also belongs to the professor.... The whole as it now (1818) stands is undoubtedly the first in Germany. It comprises all instruments that have ever been used in surgery from the earliest days to the present time.
Professor von Langenbeck, as a practical surgeon, is unrivalled in Germany. We have seldom seen a man so enthusiastically devoted to any pursuit, or who brought to the profession of surgery more capability of excelling in it.... As an operator, he is unrivalled in his own country, and we are not aware that he is excelled in any. He is clear and decisive in his judgments.
This account certainly places von Langenbeck on a very high pedestal, and reveals the true reasons of his great popularity as a teacher. Upon a close analysis these reasons may be stated thus: they were whole-heartedness in his chosen work; readiness to sacrifice himself, if necessary, in order to secure every possible advantage for his pupils; and the possession of the rare gift of knowing how best to impart knowledge to those who show a strong desire to acquire it. It is not to be wondered at, therefore, that von Langenbeck was such a favorite with such pupils as Hueter, Trendelenburg, Gurlt, Luecke, von Esmarch and Billroth, all of whom in time acquired celebrity as surgeons.
One more point deserves to be mentioned here: von Langenbeck was an accomplished master in the technique 51of operative work, and he took pains to transmit his skill to his pupils. One of his great feats, as narrated by those who often witnessed incidents of this nature, is briefly described as follows:—von Langenbeck would appear from time to time at the operating table dressed in a light summer suit of clothes, and would immediately proceed to his work without putting on a gown or taking other measures to protect himself from the soiling which so frequently is associated with operative work; and yet, when the operation was completed, the closest observation failed to discover a single spot of blood or other pathological product upon his clothes. The narrator of this tale evidently believed, and perhaps rightly, that the incident showed how thoroughly familiar von Langenbeck was with the distribution of the blood-vessels that supplied the region upon which he was operating and also how skilful he was in the handling of his scalpel. The incident, it should be remembered, occurred many years before it was thought necessary to take certain precautions against the spread of infection.
A GENERAL SURVEY OF GERMAN MEDICINE AT THE END OF THE EIGHTEENTH CENTURY
Among those who read the present chapter there may be some who will express surprise at the gloomy character of the picture which I draw of the state of medical affairs in Germany at the period of time now under consideration. In answer to this implied criticism I would state that I am in no degree responsible for the unpleasant impression conveyed by the picture, as I have simply reproduced, without the slightest exaggeration, the account which such excellent authorities as August Hirsch, of Berlin, and George Korn, of Munich, give in their published writings. Furthermore, I have not hesitated to quote, wherever I could do so without obscuring the clarity of my account, the actual statements of these authors. However gloomy, therefore, the picture here presented may appear, this unattractive characteristic must be attributed to the actual condition of medical affairs in Germany during the period named.
At the end of the eighteenth century and at the beginning of the nineteenth culture entered upon an entirely new phase of development in all parts of the civilized world; more quickly in certain parts than in others because the seeds of such development had already begun there to take root. In this work of development John Locke, the English philosopher, was a conspicuous leader. His philosophy formed the starting-point of the new development of the natural sciences, first in France and afterward in Germany and other European countries. Voltaire was the first among the French philosophers to advocate the teachings of Locke in opposition to those of Descartes (i.e., realistic 53rather than as the result of a priori reasoning). Condillac, another great French philosopher (1715–1780), also expressed himself as approving the views set forth by Voltaire,—that is, in favor of Locke’s philosophy. Diderot and others among the encyclopaedists sanctioned the same teachings. As Hirsch expresses it:—
These ideas broke like a thunderstorm over the thinking classes of France and spread rapidly to the other countries; the French Revolution cleared the atmosphere in all the different walks of life; it cast off the fetters of feudalism or at least materially loosened their hold; it greatly increased tolerance of religious beliefs and placed limits upon superstition.
At this period of time Germany was still living under deplorable conditions. The after-effects of the Thirty Years’ War still lingered. Those Germans who wished to lay some claim to culture were obliged to think, speak and write in French. The great mass of the people, however, were still bound hand and foot under the dominion of their spiritual and state tyrants. The learned classes still cultivated a barbaric Latin in their university lectures and in their writings. They considered it beneath their dignity to cultivate their own tongue. In the schools and universities the teaching had reached a decidedly low ebb. “The humanistic spirit” had vanished; the teaching was directed to the acquisition of the science of bread-winning. The Roman Catholic Church at this time was entirely in the hands of the Jesuits; the Protestant Church was no longer guided by the high ideals of its founder. A hollow dogmatism had put a stop to all further search for the truth; the one important thing was orthodoxy. There had developed a Protestant hierarchy that exerted as stupefying an influence upon the great mass of the people as did the Jesuits in the Roman Catholic Church. Superstition and charlatanry permeated the medical profession. These superstitious beliefs found lodgment in the minds of even such otherwise great physicians as Friedrich Hoffmann, Georg Ernst Stahl and Anton de Haen, one of Boerhaave’s distinguished pupils and a celebrated clinical teacher.
After the lapse of a few years—that is, in 1842—there 54was founded a new German periodical, the Archiv für Physiologische Heilkunde, under the management of Wunderlich and Roser. According to the Prospectus it was to be devoted to physiological medicine, or—to be more precise—to the cultivation of physiological methods in the treatment of disease. The introductory article in the first number of this new periodical bore the title: “The Defects of German Medicine as Taught to-day and the Importance of Giving it a Decidedly Scientific Tendency.” From the convincing style in which the article is written there can be no mistake, says Petersen, in ascribing its authorship to Karl August Wunderlich (1815–1877), a member of the Tübingen Faculty of Medicine. The following brief extracts from this article will suffice to give the reader a fair idea of this writer’s views on the subject of which he treats:—
We are establishing to-day an organ which is intended to promote the interests of physiological medicine. Henceforth it should be the aim of all enlightened minds to place pathology upon a physiological basis.[9] Nothing of a dogmatic character may be tolerated in these pages; every law here promulgated must be accompanied by proofs showing that it is justified; all the facts, observations and experiments that have led to its acceptance as a law must form a part of the account. Although for a long time past the necessity of following the course here outlined has been appreciated and has been unostentatiously adopted by all good observers, nevertheless, it is believed that the time has now come when this important fundamental truth should be announced loudly and in no uncertain terms, and should be defended again and again with untiring energy, until it shall have received universal acceptance.... People are already beginning to make a distinction between the doctrines taught in the books and those which are derived from a direct observation of what takes place in nature.... But this scepticism is only too often based upon mere assumptions and consequently fails to produce any useful results.... We believe that the time has at last arrived when this sort of scepticism should be organized into something like a system, and that intelligent criticism 55should persevere in testing the correctness of those observations which have been cited as actual facts and as the bases upon which the hitherto prevailing medical theories, so it is claimed, deserve to receive acceptance.
We further believe that to-day is the time when an attempt should be made to construct, out of the clinical materials that are now in our possession and that have been brought together with great care and without bias, a positive science, a science which in the course of time cannot fail to lead to sound therapeutic methods. This is what we mean by the expression “Physiological Medicine.”
Up to this point in his article Wunderlich says nothing to which any of my readers are likely to object. Quite the contrary; the first impression which the text makes is something like this: At last Wunderlich has discovered a road by following which closely one may eventually develop a really scientific practical medicine. But, when one reaches the end of the article, one can scarcely fail to experience no small degree of disappointment on finding that it does not furnish the slightest evidence of the manner in which the author’s seemingly admirable scheme is to be realized; nor—as we are assured by Petersen—is any further enlightenment upon this subject to be found in any of the succeeding volumes, either in the seven which were published under the joint editorship of Wunderlich and Roser, or in those which were issued after Wilhelm Griesinger had been accepted as an associate in the management of the Archiv. The old evil which carried Broussais as it were by storm into the dictatorship of medical thinking and of medical practice in France was here being reëstablished in Germany. Men seemed to find it impossible to go on patiently collecting facts; they could not resist the temptation to build theories first. So far at least as the treatment of disease is concerned, we are forced to admit that the collecting of any large body of facts is well-nigh an impossibility. Only after the lapse of very many years would it be possible to realize the desirable results which Wunderlich had in mind.
A short time before his death the Hollander, Gerhard van Swieten, who was one of the last physicians of European celebrity to give up the habit of conversing in Latin with his professional brethren, made the following remark, in a letter which he wrote to one of his friends in the Medical Faculty of Halle: “Praxis medica quotidie me convincit quot et quanta sint quae ignoro.” (In my medical practice I realize more and more clearly every day how many and how important are the things concerning which I am ignorant.) This epigrammatic remark, which throws such a flood of light upon the character of van Swieten, may appropriately be placed at the head of the following brief biographical sketch of this distinguished founder of the Vienna School of Medicine.

GERARD FREYHERR VAN SWIETEN
Van Swieten’s Early Professional Career.—Gerhard van Swieten was born at Leyden, Holland, on May 7, 1700. His parents, who died while he was still a child, left to him an ample fortune, which enabled him to obtain an excellent education. His guardians, however, were either negligent or quite incompetent to look after his best interests during the period of youth and early manhood; but, despite this fact, his own industriousness, his native talents, his ambition to excel and his purity of mind carried him safely and creditably through these early years. At the age of sixteen he entered the High School of Louvain, near Brussels, and during the following two years the study of Latin and Greek and of philosophy chiefly engaged his attention. Then, upon his return to Leyden, he began in earnest to prepare himself for the career which he had chosen—viz., 60that of the practice of medicine. Boerhaave, who, at that period of time, represented by universal consent the leading medical authority of the world, was the regular professor of medicine in the university (1710–1738), and was held in such high esteem as a teacher that students flocked by hundreds from all parts of Europe to benefit from his instruction. Among this number were two young men,—Albrecht von Haller, of Berne, Switzerland, and the subject of the present sketch,—both of whom afterward became celebrated for the important parts which they played in the advancement of medical science. Boerhaave appears to have taken a special liking for the latter and to have entertained great confidence in his ability as a physician. In 1727, when Boerhaave, by reason of a gouty affection of his legs, began to experience considerable difficulty in attending to his official duties in the university, van Swieten, upon whom the degree of Doctor of Medicine had been conferred only two years previously, was from time to time authorized by his superior to lecture in his place. As the years passed by, and as the pupil showed more and more clearly that he was entirely competent to perform this important duty in behalf of his teacher, van Swieten came eventually to be accepted as the worthy interpreter of Boerhaave’s teachings. This practice continued for nearly twenty years, and with ever increasing confidence in and affection for the pupil on the part of his distinguished teacher. Boerhaave’s death in 1738, however, put an end to van Swieten’s substitute professorship. All the available evidence goes to show that Boerhaave hoped that, in the event of his death, van Swieten would be chosen his successor; but the records of the university fail to show that the latter held at any time an official position in the teaching body. During Boerhaave’s lifetime no opposition of any kind was offered to van Swieten’s continued yet officially unauthorized occupancy of the Chair of Medicine, although it was well known that he was a Roman Catholic; but, after Boerhaave’s death, the most active opposition to van Swieten’s candidacy was immediately organized by his rivals. The claim was made by them that he could not legally be chosen to fill the vacant 61chair, by reason of the fact that the university had been founded on a Protestant basis and that consequently it would not be either legal or proper to elect a Roman Catholic to fill the vacancy. When the personal friends of van Swieten and a large body of the students begged that, despite the legal obstacle, he might be chosen the regular successor of Boerhaave, he himself at once exerted all his authority to stop the movement. Nevertheless, he felt keenly the loss of his position in the University of Leyden, for he loved the work of teaching which he had carried on so successfully during the previous two decades.
Van Swieten’s retirement from the duties of a teacher in the university brought with it certain important compensations. In the first place he was now able to devote himself fully to his private practice which had by this time grown to be very large, and the way was also opened for him to begin work at once upon his “Commentaries,”—a book of which he completed the first volume in 1742, and which contained matter of decided importance in promoting an advance in the science of medicine. Some authorities claim that if one wishes to obtain a clear understanding of Boerhaave’s teachings, he will have to read van Swieten’s elaborate work, which in its completed state consists of five large volumes.[10] Strange as it may appear, a Dutch translation of the work has never been published; from which fact two conclusions are warranted: first, that already as early as 1754 van Swieten must have severed all connection with his native land; and, second, that the number of physicians in Holland who might be tempted to purchase a Dutch version of the work was undoubtedly very small.
In November of the year 1744 van Swieten was called to Brussels to see, in consultation with her regular medical attendants, the Archduchess Marianne, wife of Charles Alexander of Lorraine, and the sister of Maria Theresa, Empress of Germany. She had recently been confined, 62after having been in poor health for several months before this event. It was therefore not surprising that at the delivery, on November 5, the child was found to be dead. Shortly after the confinement the condition of the Archduchess became rapidly worse, and it was then that Maria Theresa sent her own physician, Dr. Engel, from Vienna to consult with van Swieten and with her sister’s regular medical attendants. It appears that these two leading physicians frequently disagreed as to what was the best treatment to adopt; but van Swieten was so tactful in his advocacy of the measures which he thought advisable and so courteous in his intercourse with his professional associates that Prince Kaunitz, the Imperial Austrian Chancellor, who happened to be in Brussels at this time, wrote to the Empress in strongly commendatory terms of the impression which van Swieten had made upon him. However, the hope which the latter had held out with regard to the patient’s ultimate recovery was not realized; she died on December 12. Notwithstanding his failure to predict correctly the outcome of the Archduchess’ illness van Swieten had succeeded so completely in impressing all the patient’s immediate friends with his skill as a physician and with a genuine esteem for his personal character that they had only praise to bestow upon the man in their reports to the Empress. Maria Theresa’s mind was now entirely made up as to the wisdom of calling van Swieten to Vienna and entrusting to him the work of reorganizing the hospital management and the university medical teaching in her capital, matters in which she took a very deep interest. As soon as the decision reached by the Empress became generally known in Vienna certain physicians of that city lost no time in taking steps to thwart her plan. Scheming of this sort, however, had to be done very cautiously, for it was not safe openly to oppose the will of the sovereign. The first evidence of the existence of this intrigue to prevent the appointment of van Swieten to a position of such commanding importance in the medical world of Vienna appeared in a Frankfort newspaper of January 9, 1745. After announcing the death of the Archduchess Marianne at 63Brussels the article in question added the following remarks: “The fatal issue, it appears, is to be attributed to the unsuccessful treatment that was carried out by the local physicians with whom van Swieten of Leyden was associated as the chief consultant; it having been predicted from the very first by Dr. Engel, the imperial Austrian physician, that this treatment, if adopted, would terminate badly.” The Empress closed her ears to this and all similar calumnious reports, and wrote to van Swieten that it was her warmest wish that, when he came to Vienna, he might not experience any unpleasantness. “I would rather,” she added, “abandon completely my personal interest in this matter than have you made unhappy by the contemplated visit to Vienna.” While these gracious words from the Empress were greatly appreciated by van Swieten he was not willing to appear in Vienna in the rôle of a censor or a reformer; and so one is not surprised to learn that he did not take up his residence in the Austrian capital before June 7, 1745.
Van Swieten’s Work as a Medical Reformer.—So far as the teaching of medicine was concerned van Swieten found everything in the University in a state of confusion; indeed, nothing worthy the name of medical science existed in Vienna at that period of time. He had left a city in which the teaching of this branch of knowledge had reached a high degree of development and had come to one where the very foundations of such work had yet to be laid. He recognized at the first glance just what steps would have to be taken, and he was much encouraged by the thought that he could count upon the powerful support which Maria Theresa was only too glad to give him. According to Mueller, he realized that the most serious obstacle in his way was sure to be the very great influence wielded by the Jesuits, who had for many years controlled all educational matters in the Austrian Empire. He began his work by delivering a course of lectures on methods of treatment and on Boerhaave’s Principles of Medicine (“Institutions”), and he managed within a comparatively short time to 64attract large numbers of auditors, in whose minds was thus created a strong interest in the personality of the lecturer. At the same time van Swieten remained conscious of the fact that many of the members of the Faculty had not ceased to look upon him with keenly jealous eyes. In his memorial to the Empress on the progress which had thus far been made in the study of medicine he wrote: “Although the Faculty have not included my ‘Commentaries’ in the list of books which they recommend to the students, they emphasize by this very act the fact that physicians everywhere—as shown by the publication of five separate editions and two translations of my book in only six years—do not agree with these gentlemen in regard to the value of this work.” The continued favor shown to van Swieten by the Empress and the consciousness that he was doing his full share toward advancing the science of medicine compensated in large measure for the ungenerous spirit which animated his colleagues.
Reorganization of the Vienna Medical School.—But van Swieten rendered valuable services to the university in other ways than by lecturing, by acting as the Director of the Royal Library, and by serving as the private physician of the Empress, its great patron. For example, it was his duty, after a certain time had elapsed, to select additional professors for the Medical Department, and in this work he also manifested excellent judgment; but he was not called upon to exercise this particular function until after he had been settled in Vienna for about four years. As the first step in building up the teaching force van Swieten invited Anton de Haen (1703–1776), a native of Leyden and one of Boerhaave’s former pupils, to carry on the clinical teaching which he himself had already in some measure organized at the university. Speaking of de Haen’s qualifications for this important office, Hecker, the author of a history of modern medicine and a person entirely competent to pass judgment upon a matter of this kind, makes the following comments: “Vienna has seen few teachers as well fitted as de Haen for inspiring enthusiasm and for 65making clinical teaching effective, and few so capable as he was of showing his auditors with persuasive force how they should study Nature by direct observation, and not from books or lectures. Possessing no inclination whatever to indulge in social pleasures or in amusements of any kind, he found his chief enjoyment in tireless work. Knowledge was the priceless treasure which, by the aid of an unfailing memory and remarkable skill, he sought to win. Possessing, as he did, a quick temper, he became at times very angry under even slight provocation. Although such outbursts of temper did not conduce to his popularity they enabled him to boast that he had attained his lofty position wholly through merit, and not—as was in some measure true of van Swieten—through abstention from self-assertion.” Despite all his faults, adds Hecker, de Haen was a great physician and an extraordinarily clever teacher. He gained considerable reputation from the treatise which he published under the title: “Ratio Medendi” (The Philosophy of Treatment). He was a violent opponent of the practice of inoculation.
The next six men selected by van Swieten were also distinguished teachers, well fitted to uphold the growing celebrity of the Vienna Medical School. They were: Anton von Stoerck, commonly spoken of as van Swieten’s favorite pupil; Maximilian Stoll, one of de Haen’s pupils; Lorenz Grasser;[11] Heinrich Crantz, another of van Swieten’s talented pupils; Robert Laugier; and Nikolaus Joseph Jacquin. While the addition of these unquestionably strong names to the list of professors in the medical department of the university was recognized as a move in the right direction, the retention of a few incompetent teachers led to considerable worry on the part of van Swieten. Although he was convinced that it would be better for the University to get rid of these men he did not dare to act on his own responsibility, fearing the disturbance that was likely to result from their 66dismissal. Maria Theresa, to whom the situation was fully explained, begged him not to hesitate any longer, but to take whatever steps seemed best for the good of the university and the public. Thus encouraged, van Swieten proceeded to remove first one and then another of the men who seriously interfered with his plans for improving the teaching in the Medical School. In 1757, on the death of Archbishop Trautson, who held the position of “Protector of the Studies in the University,” this office was abolished. Already in the preceding year, at van Swieten’s suggestion, the Rector of the Jesuits was no longer permitted by the Empress to take part in the regular conferences of the Consistory of the University. Gradually other members of the Jesuit Order were excluded from the management of the affairs of the University. Finally, in 1759, van Swieten accepted the office of Censor of Medical and Philosophical Writings, and up to the day of his death he performed the duties of his office most satisfactorily to all concerned. Thus was he made the virtual Commander-in-Chief of the teaching forces in the Vienna Medical School.
While the changes described above were taking place the Empress, under the inspiration given by van Swieten, inaugurated certain improvements in the housing and equipment of the Medical School. In 1752 she gave the necessary orders for constructing a new building that was to contain a fine anatomical theatre, a chemical laboratory, lecture rooms for the different professors, a general assembly hall, etc. This fine structure was completed and formally inaugurated in April, 1756.
Finally, all the hospitals in Vienna were greatly improved during this period of time, not only as regards their accommodations and equipment, but also in respect to their management.
Inauguration of Clinical Teaching.—As the sequel showed, Vienna, under the inspiring cooperation of the Empress, continued for a long series of years the Mecca toward which physicians and medical students turned their steps from all parts of Central and Northern Europe and 67even from the United States of America and from Canada. It is now universally recognized that this extraordinary popularity of the Vienna Medical School, which began toward the middle of the eighteenth century and has continued almost up to the present time, was chiefly due to the clinical teaching which de Haen inaugurated at van Swieten’s suggestion. Sylvius and, after him, Boerhaave had already given this method a trial at Leyden, but for various reasons it had not proved entirely satisfactory. De Haen’s plan was to let each student, at the bedside of the patient, make his own diagnosis and then whisper it to the professor, who in turn announced it to the remainder of the class. If the diagnosis proved to be correct the professor found it unnecessary to say anything additional on the subject; but, if it happened to be incorrect, he presented the truth to the class in such a manner as not to give the slightest offence to the student who had committed the error. This plan encouraged his pupils to feel confidence that, whenever they made an erroneous diagnosis, they would not be subjected to ridicule on the part of their classmates. This exercise in diagnosis was duly followed by an exposition of the treatment adopted; and, whenever it happened that a patient whose case had been studied by the class, subsequently died, a post-mortem examination was conducted in their presence, and appropriate explanatory remarks were made by the instructor.
In further explanation of the extraordinary popularity which the clinical teaching at Vienna attained it is interesting to learn that de Haen (and probably also Stoll, who succeeded him) was in the habit of rising at an early hour that he might visit the hospital and learn, in advance of the arrival of the students, how the patients in the section set apart for teaching purposes were getting on, how their condition differed from that which they presented at the time of his visit on the preceding day, and what special provision, if any, should be made for the approaching clinical lesson. In short, no pains were spared to make each séance as attractive and as instructive as possible to the students.
While I am here giving to de Haen and Stoll all the credit 68that is their due for the very wise and skilful manner in which they carried out the teaching of medicine at Vienna it must be remembered that van Swieten was the real founder of clinical instruction in the famous university; de Haen and Stoll having simply put in practice the ideas introduced by him.
At this point in my sketch the question may with propriety be asked, Where may one find in history another instance of such beneficent interference on the part of a queen in behalf of a higher standard of medical education? Certain it is that, without the powerful and sympathetic assistance which Maria Theresa granted him at every stage of his work, van Swieten could not have accomplished in so short a period of time the extraordinary results which I have here briefly recorded.
Van Swieten’s Contributions to Therapeutics.—In his treatment of disease van Swieten practiced conservative methods and prescribed remedies with great caution and with strong common sense. In the case of small-pox, for instance, he did not approve of the practice of inoculation as a method of diminishing the mortality of that disease or possibly of rendering the severity of its manifestations less pronounced. He evidently believed the attendant risk to be too great. It was particularly in his treatment of syphilis, however, that he accomplished results of a most beneficial character. In St. Mark’s Hospital, in which patients affected with this disease were lodged, it had been the rule—previous to the date of van Swieten’s arrival in Vienna—to subject all the cases, without regard to the severity of the infection, to a course of mercurial salivation. As a natural result of this plan of treatment it happened not infrequently that a patient’s life was severely threatened or that he was left with lifelong sequelae of a lamentable character. The physician under whose management this mode of treatment flourished was dismissed from his position by van Swieten as soon as he was able to overcome the obstacles which stood in his way as he advanced toward the accomplishment of this end. Maximilian Locher, who 69was put in charge of the hospital after the dismissal of his predecessor, was instructed to use a solution of the bichloride of mercury in the treatment of the cases that came under his care; and the results that followed were so astonishingly good that the remedy soon came to be known everywhere as “Swieten’s” liquor.[12] For many subsequent years this solution retained its popularity among European physicians.
As regards the other remedies which van Swieten was in the habit of employing in his treatment of various maladies it is stated that he clung persistently to those advocated by Boerhaave and enumerated at the end of Vol. V of the Commentaries,—remedies which were characterized by their simplicity and by the fewness of the ingredients that entered into their composition.
Van Swieten’s Contributions to Medical Literature.—In addition to his famous “Commentaries” van Swieten wrote only one other treatise to which it seems desirable to call the reader’s attention. I refer to the book that bears the title “Constitutiones Epidemicae” and that was first published by Stoll after the author’s death. According to the statement of Mueller “this work is a sort of ‘Physician’s Day-Book,’ covering the period 1727–1744, and reveals the fact that van Swieten was a very close observer of the different diseases that came under his notice.... It constitutes a valuable supplement to the history of Boerhaave’s therapeutic methods.”
Finally, it should be stated, on the authority of Hecker, that van Swieten wrote a small manual for the use of military surgeons. It was published by Johann Thomas Trattnern, Court Printer and Bookseller, Vienna, Prague and Trieste, 1758. Van Swieten’s name—says Hecker—does not appear anywhere in the volume; and, furthermore, serious doubts have been expressed as to the correctness of the claim that van Swieten is the author of this little manual.
70After van Swieten’s death in 1772, the bust of this distinguished physician, which already three years earlier the sculptor F. X. Messerschmied had been commissioned by the Empress to prepare, was set up in the auditorium of the Medical School; and in addition an elaborate monument in his honor was erected in the Hofkirche, the Royal Chapel.
ANTON STOERCK, VAN SWIETEN’S SUCCESSOR, AND THE PROGRESS OF MEDICAL AFFAIRS AT VIENNA UNDER THE MANAGEMENT OF JOSEPH II.
After the death of Maria Theresa, in 1780, her son Joseph, who had previously been associated with his mother in the government of the empire, became the Emperor in the full sense of that term. Fortunately for the best interests of the science and art of medicine he had long been familiar, and fully in sympathy, with the plans and purposes of Maria Theresa; and he was therefore quite ready to advance the good work which she had begun. One of his first acts was to remove every possible disability from those officers and instructors who were non-Catholics, thus enabling them to gain all the facilities and honors which their Catholic associates had up to that time enjoyed. In their ultimate effect upon the growth and prosperity of the university these special measures undoubtedly were advantageous, but they were carried out with too great rapidity. According to Puschmann the Emperor strove to accomplish in a comparatively short period of time what required not less than a century. His efforts met with strong opposition in certain quarters, and before his death in 1790 he had the disheartening experience of witnessing the upsetting of many of his cherished plans. After his death, however, he received full credit for what he had attempted; the Viennese speaking of him as “the friend of the poor and the miserable, the upholder of justice and the champion of spiritual freedom and of education.”
Anton Stoerck and the Manner of Teaching Medicine in the University of Vienna.—Anton Stoerck, van Swieten’s 72successor, was the first to enjoy in large measure the fruits of the latter’s reformation of medical teaching in Vienna. His elder brother, Melchior, had already before this date been appointed Professor of Theoretical Medicine in the University; and then, in 1760, Anton himself was elevated to the important position of Court Physician. He gained his chief distinction, however, through his enthusiastic cultivation of experimental pharmacology. In this field, which had previously received very little attention, he was probably the first to appreciate the fact that the gap between theoretical medicine and actual practice could be bridged only by a resort to experimentation. Among the drugs which he tested in this manner were the following: datura stramonium, hyoscyamus niger L., clematis erecta and pulsatilla nigricans L. Van Swieten, so long as his state of health permitted, encouraged Anton to go on with his experimental work; de Haen, on the other hand, was rather skeptical about the success of his efforts.
Ultimately—after van Swieten’s death—Anton Stoerck became the leading spirit in the affairs of the Vienna medical world. The instruction in medicine was graded by him, with the Emperor’s consent, in the following manner: The medical students, before they were permitted to begin the course of instruction, were obliged to furnish satisfactory evidence of possessing adequate general scientific knowledge and of having previously attended lectures in natural history and experimental physics. In the next place, they were further obliged to attend the lectures on botany, chemistry, anatomy and physiology, and to pass a satisfactory examination in these branches before they were permitted to take up the study of pathology and materia medica. It was only after having passed a satisfactory examination in these subjects that they were allowed to receive clinical instruction. At the final examination they were called upon to make a report on a few cases of actual disease and to set forth especially the details of the treatment adopted; to write a certain number of prescriptions; and, finally, to defend publicly, in the presence of the Rector and the Chancellor of the University, the Deans of the four Faculties, and 73one Professor of the Medical School, a thesis on some medical doctrine. After which the formal ceremonial of conferring the degree was carried out in the presence of the same university officials. And here again, the Emperor effected a most marked reformation; he abolished all those religious ceremonies which it had been customary to observe in connection with the bestowal of the degree of M.D. and the right to practice medicine. He also adopted measures for enlarging the equipment of the University libraries, and among other things he abolished a large number of monasteries and turned over their collections of books to the libraries of the university. Recognizing, as he did, the fact that the proper training of medical men who intended to follow the career of surgeons was at that time lamentably inadequate, he instituted, at the earliest moment practicable, such changes in the teaching, in the duration of the course, in the requirements for graduation, etc., that the surgeons would thereafter be on the same level, with regard to education and practical training, as the physicians.
At first (1780), the Faculty consisted of nine professors, who gave instruction in the following branches: anatomy, physiology, natural history, chemistry and botany, general pathology and therapeutics (including pharmaceutics), internal medicine and clinical instruction, theoretical surgery, clinical surgery, and obstetrics. In addition to these there were several assistants and a prosector (demonstrator of anatomy). The Emperor Joseph II., after expressing serious doubts with regard to the “possibility of teaching the theory of surgery, bandaging and the various surgical operations in six months,” gave orders that the following scheme should be adopted:—
First Year: Anatomy and physiology, together with chemistry and botany (for physicians only) and operative work, bandaging and obstetrics (for surgeons only).
Second Year: (For physicians) Materia medica, pathology and clinical medicine.
(For surgeons) Clinical medicine, clinical surgery, and obstetrics.
Third Year: Entirely given up to practical work at the hospital and the Clinic.
74At a later date the course was extended to four years; and from that time forward, according to Puschmann, surgeons were looked upon with consideration.
Hirsch, speaking of the majority of physicians of that period, says that they sought to quiet the demands of the public for satisfactory information about their maladies by employing, in their responses, the meaningless terms of Graeco-Latin terminology; and he quotes Immanuel Kant, the famous Prussian metaphysician, as having expressed the same idea when he said: “These men thought they were rendering their patients a great service when they gave them a name for their disease.”
As regards the therapeutic measures which these so-called physicians employed, Hirsch adds: “they generally consisted of pills and plasters, drugs of various kinds, clysters and repeated blood-lettings which at times produced such a degree of exhaustion that only patients with a strong constitution were able to rally from the effects of this loss of blood.... The title ‘Doctor of Medicine’ afforded no guarantee that the individual who bore it possessed the requisite degree of medical knowledge.” Fortunately for the public there were at that time in almost every community a few men to whom the description given above does not in the slightest degree apply. I have already mentioned the names of several physicians of this higher stamp, and the number of such honorable representatives of our profession rapidly increases as we approach the nineteenth century.
Reorganization of the Hospital Work in Vienna toward the End of the Eighteenth Century.—In the preceding sections mention has been made of the important changes effected by the Emperor Joseph II. in the scheme of teaching adopted by the Medical Department of the University. It now remains for me to give some account of his reorganization of the Vienna hospitals and of his founding that famous general hospital known as Das Allgemeine Krankenhaus. That there was need of reorganization in at least some of the hospitals is shown by the following 75anecdote which is related of Professor Boer, who held the Chair of Obstetrics. When the authorities who had special charge of the Lying-in Ward complained to him that he prescribed too liberal a diet for this class of patients, he replied somewhat impatiently that he could not feed, “with water, Epsom salts and ‘Arcanum Duplicatum’ [a secret remedy that was popularly believed to be efficacious], the women who were already a good deal weakened by their pregnant state as well as by sorrow, anxiety and insufficient nourishment; for a liberally supplied kitchen and a good wine cellar were more important than drugs.”
To furnish a complete and satisfactory description of Das Allgemeine Krankenhaus would require more space than can properly be devoted here to the consideration of this single topic. Those who take a special interest in the subject will find full details in Puschmann’s monograph (See Bibliography); for the majority of readers the following brief account will probably suffice.
The Allgemeine Krankenhaus consists of a very large group of three-story buildings in which there are numerous individual spaces large enough to serve as wards, as small lecture rooms, or as reception rooms for ambulant patients (eye, ear, throat, skin and minor surgical cases). The ceilings are usually high and the openings for windows are of such dimensions as to furnish excellent ventilation and liberal daylight illumination. Ample facilities are provided for bathing, for cooking the needed food, and for preparing and dispensing remedies; and the individual buildings are grouped in such a manner as to afford numerous small park-like spaces in which the patients may obtain outdoor exercise or may enjoy the fresh air and some social intercourse with their fellows. Although in 1784 the buildings were almost ready for occupancy and the park-like surroundings completed, it was only at a much later date that the institution was really prepared for the reception of patients. Somewhere about the year 1830 it had been so thoroughly organized that physicians and students came from different parts of the world, and especially from Great Britain and from America, to enjoy fully those extraordinary facilities for 76the study of every possible form of disease which were to be obtained only in the city of Vienna. Whereas in London, New York, Philadelphia and Boston, it was necessary at that time for all but a few of the students to waste many precious hours and much physical strength in traveling from one hospital to another in order to acquire by direct observation some familiarity with disease, here in Vienna was provided, in a single group of buildings, ample provision for all the clinical teaching that the most eager and serious student of medicine could possibly desire.
New Methods of Diagnosis, and First Appearance of Instructors in Special Departments of Medicine at Vienna.—It was during van Swieten’s lifetime that Auenbrugger’s new invention “for detecting, by means of percussion, the obscure diseases of the chest,” was published for the first time (1761) in Vienna. The value of this discovery, which was termed by him “Novum Inventum,” was not appreciated by physicians at that time. Even van Swieten and de Haen rather looked down on the method; and its importance was not fully recognized until Corvisart, the celebrated Paris physician, published a French translation of Auenbrugger’s book in 1808. This work, in which Corvisart gave his own experience and added many notes and comments, served to popularize Auenbrugger’s method as a valuable aid to diagnosis in affections of the chest. In his preface Corvisart announced that he was well aware of the small glory that came to translators and to those who simply comment on the work of others, but notwithstanding this fact he preferred that the major part of the glory should go to Auenbrugger who had rendered such a great service to the Profession by his invention.
Auenbrugger, who died in 1809 at the age of 87, lived long enough to enjoy the pleasure of this triumph. His private practice grew to be very large, and he performed, more often than any other physician of his time, the operation of thoracentesis. He was universally loved and respected in Vienna.
77One of the first specialties to take root in Vienna toward the end of the eighteenth century was that of ophthalmology, and the physician who first succeeded in bringing it to a high stage of development was George Joseph Beer, who was born at Vienna in 1763. During his student days and for a short time subsequently he acted as a draughtsman for Joseph Barth, the professor of anatomy and physiology in the Vienna University, and in this way he obtained unusual opportunities for acquiring a knowledge of both the normal and the pathological anatomy of the eye. Already in 1793 he applied for, and was granted, permission to treat, in the Allgemeine Krankenhaus, such poor people as were suffering from cataract, and to perform the requisite operations. Each year, during the months of May and June, a suitable room was gotten ready for Beer in the hospital, and here, during this most favorable season of the year, he performed many cataract operations.
In 1812 he received the double appointment of Director of the Eye Clinic and Professor Extraordinary of Ophthalmology; and from this time forward he rapidly gathered about him a great crowd of pupils, among whom were men who—like C. F. von Graefe, Philip von Walther, T. W. G. Benedict, F. Jaeger, Rosas, Quadri, J. N. Fischer, Mackenzie, Reisinger, Chelius and others—were soon to be known in every part of Austria, Germany, Italy and England as the leading eye surgeons of their respective countries. Beer therefore exerted a most decided influence on the development of ophthalmology.
Beer’s early writings, the first of which date from the year 1791, also exerted a great influence. Such, for example, were his “Practical Observations on the Gray Form of Cataract” and on the “Different Eye Diseases which Owe their Origin to Some General Disease”; and also his “Treatise on Diseases of the Eyes.” The last-named passed through several enlarged and improved editions between 1813 and 1817. In 1799 he issued a Summary of all the treatises on ophthalmological topics which had been published up to the end of 1797; and soon afterward he published an account of his method of extracting a gray cataract together 78with its capsule. Still other memoirs of decided value were published by him in the following years; and among them one especially deserves to be mentioned, viz., that on the affliction known as “Pannus,” of which condition he was the first to give a correct explanation.
In 1819 Beer was stricken with an illness of a serious nature, and two years later he died. He was succeeded by Anton Rosas, whose death occurred in 1855.
PROCHASKA, HYRTL AND ROKITANSKY, THREE OF THE MOST DISTINGUISHED TEACHERS AT THE MEDICAL SCHOOL OF VIENNA DURING THE EARLY PART OF THE NINETEENTH CENTURY
George Prochaska, born at Lipsitz, Moravia, in 1749, was appointed Professor of Anatomy and Ophthalmology at the Prague Medical School in 1778. Eight years later he was transferred to the Chair of Physiology. In 1791 he received the appointment of Professor of Higher Anatomy and Physiology in the University of Vienna. In 1819 he resigned this chair, probably owing to poor health; and his death occurred during the following year.
Between 1780 and 1797 he published, in Latin, important monographs on the physiology of man. Later, these were thoroughly revised and then published in German under the title of “Physiology, or the Doctrine of the Nature of Man.”
Prochaska was esteemed very highly as an eye surgeon of exceptional skill and wide experience, no fewer than 3000 cataract operations having been performed by him. His greatest achievements, however, belong in the domain of physiology. Already as early as in 1797 he hinted at the possibility that, in the case of the spinal nerves, one of the portions might transmit centripetal and the other centrifugal impulses. It was reserved, however, for the great English physiologist, Sir Charles Bell, to establish firmly, several years later, the law governing these two currents.
Prochaska’s ideas with regard to the nature of “vital force”—that question which in those days gave biologists so much trouble—may be inferred from the following quotations:—
In the performances of the nervous system there occur manifestations 80which bear a striking resemblance to the phenomena produced by electricity.... In my opinion it is not permissible to conceive of vital force as an independent power, one that depends upon a single and special principle, but rather as an aggregation of all the forces of Nature, representing in one set of instances the cause and in another set the effect of these forces, and combining in this body of ours, by their foreordained harmony, to create what we call life. Therefore, among the powers that are commonly meant when we use the expression “vital power,” there are no specific forces, but only the general forces which exist in Nature; but at the same time they are combined under a special relationship,—in fact, they are entangled the one with the other in such an inextricable snarl that it is simply impossible for us to gain a clear conception of their causes and effects.
Finally, it is quite remarkable, says Puschmann, how closely Prochaska’s ideas regarding the formation of bone agree with the teachings of our modern authorities. Here is the paragraph in which he formulates these ideas in full detail:—
The business of nutrition is carried on in such a manner that, when new conditions arise, whole organs which for some time previously were performing useful work, are swept out of existence, and new ones, better adapted to the work required of them, are put in their places. As an instance in point we may mention certain cartilages which, for a limited period of time during childhood, take the place of bone structures, and which at the same time play the part of really necessary aids to the growth of the bone. These cartilages gradually become converted into the latter tissue, the process reaching the stage of completion at different times, but yet at a fixed and definite time for each particular bone. Thus, in the case of the long bones, the cartilage becomes completely ossified somewhere between the twenty-second and the twenty-fourth year. This process of ossification does not consist in a simple hardening or change of the cartilage into bone; the essential features of the process may more correctly be described as follows: the cartilage, in the depths of whose substance bone-tissue centres are being nourished and are progressively undergoing development, is steadily being crowded to one side and ultimately destroyed. At the same time there appear here and there in the cartilage a few blood-vessels which, so far as one is able to judge, spring, in the majority of instances, from the neighboring fully-formed bone substance. 81And, as a further stage in the process of growth, there appear alongside the new blood-vessels centres of ossification, which in due time become foci of genuine bone tissue. Then, as these foci increase in size, the surrounding cartilage steadily dwindles in quantity until nothing remains but a few scattered cavities or hollows, which persist for only a short time before they disappear altogether.
Prochaska’s discoveries in regard to the growth of bone excited the admiration of his contemporaries, and well they might, for they involved prolonged investigations with the aid of the microscope and much close and careful thinking. It is safe to say that at this early date (end of the eighteenth century) original investigations like the one just described must have been very few indeed in Austria.
Carl Rokitansky, who was born at Koeniggratz, Bohemia, in 1804, received his medical training at the universities of Prague and Vienna. For several years after he had been given the degree of Doctor of Medicine he served as an Assistant in the Pathologico-Anatomical Institute, and in 1832, after the death of Johann Wagner, the Custodian of the Museum that formed a part of the Institute, he was appointed his successor, not only in this particular office but also in those which were closely related to it—viz., the office of Prosector of the Allgemeine Krankenhaus and that of Judicial Anatomist for the City of Vienna. The duties which he had to perform in connection with these offices and as an Instructor in the Medical Faculty of the University left him very little time for anything else. His pet ambition was, not merely to do well the work which these different official positions entailed upon him, but also to build up, so far as in his power lay, a systematized knowledge of the relationship that subsists between the different pathological conditions revealed at the post-mortem examination and the clinical phenomena manifested during the patient’s lifetime. Therefore he was accustomed to insist that a reasonably full history of the case should be submitted with every corpse on which he was asked to make a post-mortem examination. This afterward became a firmly fixed 82practice at the hospital. After he had read these case-histories and had compared them with the facts revealed by the corresponding autopsies he prepared, at proper intervals, a report on the diseases which were then prevalent at the hospital. This method of procedure, it will easily be seen, constituted an important advance beyond the practice of simply studying and then recording the various pathological lesions which develop in the different organs of the body. It established a connecting link between these lesions and the lifetime manifestations of disease; in other words, it revealed a way in which the medical practitioner at the bedside might, by a proper use of his reasoning powers, infer from the symptoms and physical signs what changes were taking place in the unseen organs of the body. From this time forward, therefore, physicians began to place before their mental vision—in every case which they were called upon to treat—a picture of the anatomical changes that were taking place in the patient’s body, instead of symptom groups. In the words of that distinguished Tübingen physician, Wunderlich, “Rokitansky was endeavoring with untiring zeal to convert pathological anatomy into an anatomical pathology.” The reader will, I am confident, agree with me when I say that there are very few instances in the history of medicine where an advance toward a better knowledge of the art of diagnosis is more clearly revealed than in the work which Rokitansky carried on so patiently, so conscientiously and so successfully during the early years of the nineteenth century. Compare the record of the work accomplished by Morgagni with the remarkable results reached by the Vienna pathologist, and it will be quickly appreciated how little fitted the former searcher after truth was to carry out successfully the advance which Rokitansky effected and which I have tried to describe in these pages.
Rokitansky’s earliest contributions to medical literature consisted in quite a large number of memoirs which were published at different times in the “Medicinische Jahrbücher des Oestreichischen Staates.” They deal with topics like the following: “Incarcerations and Intussusceptions of 83the Intestines”; “New Formations of Bone on the Internal Surface of the Skull in Pregnant Women”; “Spontaneous Rupture of the Aorta”; “So-called Duplication of the Uterus”; “Strictures of the Intestinal Canal and Other Abnormal Conditions that give rise to Constipation and to Ileus”; “Perforating Gastric Ulcer”; “Contributions to our Knowledge of the Different Forms of the Curvature of the Spine”; etc. Subsequently he published in three volumes his great work on Pathological Anatomy; Vol. 3 appearing in 1842 and Vol. 2 in 1844. These last two volumes were devoted to special pathological anatomy. The first volume of the series, which deals with general pathological anatomy, was not published until the year 1846. In these volumes, which are rich in newly discovered facts, the author keeps constantly in mind the needs of the general practitioner; and how great was the importance which he attached to this feature of his work may be inferred from the frequent reference which he makes to it in other parts of his writings. Thus, for example, in the Preface to Vol. 1 he says: “In regard to the manner in which I have planned and constructed the present treatise I will briefly remark: ‘I have tried from the very beginning, and all through the work, to look at the subject from the viewpoint of the practicing physician, and I believe that, in adopting this course, I have accomplished a thing which was most urgently needed in our time; and I also believe that I have utilized the gigantic mass of material that was at my disposal in a worthy manner.’” Then, again, farther on in the Introduction, he says: “The first attempt to treat the subject of pathological anatomy in the manner which I have just described,”—an attempt, by the way, that was crowned with brilliant success,—“was made by Laënnec in his discussion of the subject of diseases of the chest.”
In strong corroboration of Rokitansky’s belief in the importance of pathological anatomy stands the statement attributed to the celebrated anatomist Vesalius, to wit: “I am very sorry not to have devoted to pathological anatomy the large amount of time and strength which I spent on physiological anatomy.”
84Rudolf Virchow calls Rokitansky the “Linnaeus of pathological anatomy.”
It was my original intention to furnish at this point a few brief extracts from the original text of Rokitansky’s great treatise, in order that the reader might learn, from this pathologist’s own words, just how he managed to teach pathological anatomy in the manner best adapted to subserve the interests of the practitioner. After looking in vain, however, for a section of the desired degree of shortness, I came to the conclusion that it would be better to abandon the attempt altogether and rest satisfied with a simple enumeration of the captions of some of the more important subsections that treat of alterations in bone. Here are those which I selected: “Bone Deficiency and Bone Excess”; “Anomalies in Size and Shape”; “Bone Atrophy”; “Anomalies of Bone in its Connection with other Bones”; “Anomalies in Consistence”; “Break in Continuity and the Manner in which Healing Takes Place”; “Callus Formation and New Joints”; “Healing of Bone by First Intention”; “Healing of Bone through the Medium of Suppuration”; “Healing of Wounds in Bone with Loss of Substance”; “Inflammation of Bone”; and “Bone Caries.”
Not being specially interested in pathological anatomy I have read only small portions of the text of this celebrated treatise; but, judging from this superficial examination and from the unanimous testimony given by men who are expert judges in this department of medical science, I feel confident that satisfactory answers will be found in this great work to nearly every question that may arise in a physician’s mind concerning the pathology of some part of the human body. It is a book, however, that is intended for reference purposes, and not for reading as one would read Trousseau’s work; and this undoubtedly explains why, so far as I am able to discover, no English version of this treatise exists.
I may here call attention to the fact that the first edition (1842–1846) of Rokitansky’s treatise contains no cuts, but that of 1855 is well furnished with illustrations.
After Rokitansky had held for ten years the position of 85Professor Extraordinary of Pathological Anatomy in the University of Vienna he was promoted in 1844 to that of Ordinary Professor.
As an evidence of Rokitansky’s popularity as a teacher I will mention the following fact. In my student days at the College of Physicians and Surgeons, New York, my father, the late Dr. Gurdon Buck, frequently referred to the benefit which he had derived from the lectures and dead-house instruction which he received from Rokitansky during his stay in Vienna (about 1833 or 1834). From the statement made by Prof. Alfred C. Post of New York, I learn that he and my father were Rokitansky’s first American pupils.
Rokitansky’s death occurred in 1878.
Joseph Hyrtl was born at Eisenstadt, Hungary, in 1811. His father was a professional musician (Capellmeister) in the service of Prince Esterhazy. He received his medical training in Vienna, and in 1833, while he was still only a student in the university, he was given the appointment of Prosector in the Anatomical Institute. Two years later he received his doctor’s degree, and in 1837 he was chosen Professor of Anatomy at the University of Prague. According to Puschmann “Hyrtl handled his pen with the same skill as he did the scalpel, and also in his spoken lectures he manifested to a wonderful degree the gift of making dry facts interesting to his auditors, thus keeping them fascinated by his remarks and stimulated to advance in that branch of medical science. The remarkable manner in which the teaching in the Vienna Medical School increased in popularity at this period of its history was in no small degree due to the fact that Hyrtl had, a short time before (in 1845), been called to occupy the chair of anatomy in that institution.” In confirmation of Puschmann’s estimate of Hyrtl’s power to write entertainingly upon anatomical and physiological topics which are commonly classed as “dry” I will furnish here a few extracts from Hyrtl’s General Treatise on Anatomy. And, if the reader will pardon me for referring once more to my father’s interest in those who 86played a part, either as teacher or as simple friend and companion, in his student life at Vienna, I will preface these extracts with the statement that, more than once in the early sixties, I surprised my father reading with evident pleasure, after the day’s work was over, this very treatise on anatomy.
In his preface Hyrtl says: “A general treatise on anatomy should not confine itself to the mere teaching of this branch of the science of medicine, but should also inspire the students who read the book with a love for this science and the ambition to make original investigations.”
Speaking about the behavior of an artery after it has been divided with the knife Hyrtl explains why, in the living body, the complete division of such a blood-vessel produces a narrowing of the lumen at the point where it has been divided, whereas a similar division of the vessel, if carried out upon the dead body, results only in a retraction of the tube in the direction of its length; in other words, in the corpse the diameter of the lumen remains unchanged as a result of such division. From these and other facts (which he mentions, but which the lack of space compels me to omit) Hyrtl draws the inference that the contractility of the wall of an artery is a phenomenon that occurs only in the living vessel. Then he goes on to remark:—
Beginning at the point where the ligature has been applied the artery loses its symmetrical shape, both above and below the site of the ligature, as far as to the spot where the next collateral branch is given off. At first this distortion of the vessel’s shape is due simply to the fact that its calibre is filled with clotted blood (provisional obliteration). Later, a solid plug takes the place of the soft clot. It is composed of plastic material that, becoming fused with the clot (thrombus), gradually undergoes organization and permanently attaches itself to the wall of the artery through actual growth of tissue (definitive obliteration). Thus there is formed, as the final result of all these changes, a firm and solid cord the circumference of which is smaller than that of the artery from which it springs in direct continuity.
The ligating of one of the larger arteries—as, for example, the brachial or the crural artery—does not interfere seriously with the circulation in the parts located below the point where the ligature 87has been applied; for the blood continues to flow into these parts although with diminished energy, owing to the fact that it is obliged to travel through roundabout channels (anastomoses).... I once owned a dog upon whom, in the days of my youthful sinning in the domain of physiological experimentation, I performed, within the short period of a single year, the operations of tying the innominate artery and both crural arteries; and, notwithstanding the fact that the blood needed by the adjoining regions was thereby forced to travel to them by unaccustomed routes, the dog’s health did not seem to be in any way affected.
Among the anatomical remarks which Hyrtl makes at various points in the course of his formal treatment of the subject under consideration I find several that seem to me to be worthy of reproduction here. In one place, for instance, he makes the statement that voluntary movements of the auricle of the ear are by no means a rare phenomenon, and in support of this statement he quotes Haller as mentioning (“Elementa Physiologiae,” Tomus V., p. 190) many instances of this kind; he also narrates how B. S. Albinus (1697–1770), the greatest anatomist of the eighteenth century and a colleague of Boerhaave at the University of Leyden, was in the habit of removing his wig whenever he wished to exhibit to the students how great was his control over the movements of the auricle of the ear.
In another place Hyrtl calls attention to the not uncommon error of giving, to the structureless membrane which Descemet described in 1758, the name of Membrana Descemetii. According to him it was first described by the Englishman E. Duddel, twenty-nine years earlier, in his “Disease of the Horny Coat of the Eye,” London, 1729.
In addition to his famous general treatise on anatomy, of which, in the course of 38 years, no fewer than 17 editions were printed, Hyrtl published in 1845 a memoir on the organ of hearing, and in 1860 a “Manual for the Use of Dissectors.”
His death occurred in 1884.
BAGLIVI, MORGAGNI, SCARPA, SPALLANZANI, TISSOT AND GALVANI; ITALY’S MOST ILLUSTRIOUS PHYSICIANS DURING THE EIGHTEENTH CENTURY
Giorgio Baglivi, the most distinguished Italian physician of the seventeenth century (1669–1707), was probably the first medical author in that country to lay stress upon the importance of studying disease through direct observation rather than from books. In his treatise on the practice of medicine, which was first published in Latin at Rome in 1696 and afterward translated into several modern languages (London, 1704; Paris, 1757), he makes the following remarks:—
There are several obstacles which have hitherto stood in the way of a more general adoption of the maxim that direct observation constitutes the best method of studying disease. They are the following: the widespread contempt for the authority of the physicians of antiquity; the false opinions and prejudices to which men became attached as if they were idols; the habit of making erroneous comparisons and of drawing hasty conclusions, as well as the formulating of analogies that are based upon untrustworthy reports; reading books which have been unwisely chosen or reading without exercising a discerning judgment; incorrect interpretation of the author’s meaning; the craze for reducing everything to a system; and the abandonment, by authors, of the habit of expressing their thoughts in the form of maxims.
Giovanni Battista Morgagni, one of the greatest anatomists of the eighteenth century and the prince of anatomo-pathologists, was born on February 25, 1682, at Forli, an Italian town situated about forty miles southeast of Bologna. The death of his father when the boy was only seven years old made it necessary for his mother to assume 92entire control of his early education. She performed this duty so faithfully and with such excellent judgment that, by the time Giovanni had attained his fourteenth year, he was so thoroughly familiar with the literature of Italy, and also of European countries generally, that the Academy of Forli unhesitatingly accepted him as a member of that organization. Two years later Giovanni went to Bologna and began the study of medicine under the guidance of such distinguished teachers as Hyppolyte Albertini and Antonius Valsalva; and three years later (in 1701) he was given the degree of Doctor of Medicine.
Morgagni’s biographers say little or nothing about his personal traits of character and about the manner in which he spent the larger part of his time during the early years of his professional career. His published writings, however, make it perfectly clear that almost from the very first his chief interest was centred in the study of anatomy as revealed to him by dissections of the dead human body; and, as the years rolled past, he evidently grew more and more strongly interested in the changes which take place in the organs and tissues of the body as the result of accidental injuries and of disease. From these same writings one learns further that he was in the habit of writing down, with the most painstaking minuteness, all the various departures from the normal standard as fast as they revealed themselves to his critical vision. He left no opportunity for the occurrence of errors due to a defect in his memory.
In 1706 he published a treatise bearing the title “Adversaria Anatomica.” It was this work which first laid the foundation of his reputation. In 1716 he was given the Chair of Anatomy at the University of Padua, and he continued to hold this position up to the time of his death in 1771.
Relatively late in life—that is, in 1767—he published his treatise “De Sedibus et Causis Morborum” (on the seats and causes of different diseases). This work, says Rokitansky, stands for all time, notwithstanding its defects, as a monument in honor of its author, by reason of the great industry and perseverance which it displays, and because of 93its wealth of detail, orderliness of arrangement, acuteness of reasoning, and excellence in the choice of methods,—in short, because of its originality. Théophile Bonnet’s great work on the same subject (“Sepulchretum”) was published in 1700, but, like its successor, its usefulness to-day is limited, at least in large measure, to that of a huge museum of pathological specimens. Rokitansky, of Vienna, was in reality the first anatomist who appreciated at its full value the fact that these lifeless specimens furnish most useful lessons in the theory and practice of medicine.
Lazarus Spallanzani was born in 1729 at Scandiano, a small town in the northeastern corner of the Apennines, about fourteen miles from Modena, Italy. At the age of fifteen he began to study physics, mathematics and philosophy at the University of Bologna, under the guidance of his relative, Laura Bassi, one of the most distinguished members of the Faculty of the Bologna Institute of Science. At the same time he cultivated a knowledge of Greek, Latin and French, as well as of his native language. As his father was anxious to have him do so, he also studied jurisprudence for a certain length of time, but he abandoned this study when his father, who had been persuaded by Antonio Vallisnieri, Professor of Natural History at the University of Padua, that the lad was much better fitted to follow the career of a biologist than that of a jurist, gave his son full permission to adopt whatever line of studies best suited his tastes and inclination. Accordingly, from this time forward Spallanzani devoted himself with increased zest to the study of mathematics and the dead and living languages.
In 1754 the University of Reggio—a town which is only a few miles distant from Scandiano—elected him to the Chair of Logic, Mathematics and Greek; and this position he continued to hold with credit to himself during the following six years; and during this period he devoted all his leisure hours to the observation of Nature. In this way he was able to make a few discoveries concerning the animalcules that are found in infusions; and it was not long before these discoveries attracted the attention of those distinguished 94Swiss naturalists—von Haller, of Berne, and Bonnet, of Geneva.
In 1760 Spallanzani was invited to occupy a chair in the University of Modena, and he taught in that institution for a period of eight years. During his term of office at this institution he published two memoirs—one on the animal nature of microscopic animalculi, and a second on the changes effected in the shapes of stones by the action of running water.
In 1767, the Empress Maria Theresa decided to render the University of Pavia more effective as a scientific institute, and with this purpose in view she established certain new professorships, and among the number one on natural history. As the first incumbent of this new chair she called (in 1768) Spallanzani, who by this time had acquired a great reputation in the scientific world as a biologist. His extensive knowledge in a variety of departments was associated with a remarkable genius; his methods were simple and easily understood, and—to speak figuratively—he took his auditors by the hand and led them to a clear understanding of the truth, or to the point where they could appreciate that the truth was not far distant and was certainly attainable in the near future. He possessed the art of interpreting Nature by her own methods, and by this art he was able to render wonderfully clear all the subjects with which he dealt in his lectures. All those who heard him speak gave him credit for being at times positively eloquent.
Lack of space will not permit me to furnish more than a few details of the original investigations which he made at this period of his career. Although at first glance it may be thought that Spallanzani’s work had very little to do with the science of medicine, on closer examination it will be seen that a study of the vital processes in the lower forms of life (which was Spallanzani’s chief occupation) are largely the same as those which characterize the higher forms, and therefore—since great difficulties attend the study of the same processes in man—it is of the very greatest importance that the search for light on this subject should be conducted on the lower organisms, even on 95the minute organisms which are found in stagnant water. Spallanzani was therefore engaged, in a very direct manner, in laying the foundations of the true science of medicine. Von Haller, the great Swiss pioneer in biology, was fully aware of this fact when he dedicated the fourth volume of his “Elementa Physiologiae”
To that most illustrious man, Lazarus Spallanzani, to whom credit is due for the fact that, although he had already explored the most minute and inaccessible of Nature’s pathways, he still sought to learn whether the existing limits of our knowledge of the truth might not be extended.[13]
In 1780, during his residence at Pavia, Spallanzani published two new volumes containing memoirs on vegetable and animal physiology. In one of these he discusses with great thoroughness the subject of digestion, and describes the difficult experiments which he made, largely upon birds, in order to ascertain the nature of this process. In this manner he ascertained that, in a very large number of animals (insects excepted), digestion is effected by a juice or fluid which dissolves the alimentary substances that have been introduced into the stomach. “One is filled with admiration,”—says his biographer and friend, Jean Senebier, of Geneva, Switzerland,—“as one peruses Spallanzani’s account of this series of experiments, and notices with what scrupulous care he formulates the conclusions which he draws from them with regard to the causes of the phenomena observed.” And yet, in 1786, John Hunter, the distinguished English anatomist and biologist, published a memoir (“Observations on Certain Points of the Animal Economy”) in which he dissents—somewhat sharply, says Senebier—from these conclusions. In 1788 Spallanzani published his reply to the observations made by Hunter and in this he points out, “with a logic so clear and convincing that it permits of no reply,” the errors of the English physiologist’s criticism.
96In several other published memoirs Spallanzani deals with the problems of generation, the circulation of the blood, the respiration, etc.
To this very brief and imperfect sketch of one of the greatest biologists of the eighteenth century, I will simply add the statement: His death occurred, after a brief illness, February 11, 1799. In the parish church of Scandiano there has been erected a magnificent mausoleum in honor of Spallanzani.
Antonio Scarpa (1747–1832), a native of Motta near Treviso, Northern Italy, received his medical education at the University of Padua. He was particularly devoted to the study of anatomy, and, already in the second year of the course, he had made such progress that he was allowed to act as one of the prosectors. Morgagni, who was his teacher, became very much attached to him and did everything in his power to advance Scarpa’s interests. While he was still in the student stage of his career Scarpa went to Bologna and devoted himself for a few months to the cultivation of surgery. On his return to Padua he passed successfully the required examinations and was given the degree of Doctor of Medicine. Not long afterward he was called to fill the Chair of Anatomy and Surgery at the Medical School of Modena. After eight years of service in that institution he resigned and then visited France and England for the purpose of gaining further knowledge in those branches of medicine in which he was specially interested. In 1783 he accepted a call from the University of Pavia to occupy the Chair of Anatomy, and remained undisturbed in this position for twelve years. In the year 1796, however, at the time when Pavia became a part of the newly founded Cisalpine Republic, Scarpa was asked to take the oath of allegiance to the new government, an oath which was required of all the functionaries of the university. Not being willing to do this he was obliged to resign his professorship. In 1805, Napoleon, after being crowned King of Italy at Milan, passed through Pavia on his way back to Paris. On this occasion he asked to have the university 97professors presented to him, and, failing to find Scarpa among those who attended the reception, he asked what had become of him, for his great reputation as an anatomist was well known to him. Then he learned how Scarpa had been compelled, by reason of his unwillingness to sign the oath, to resign his position in the university. “Well,” replied Napoleon, “what if he did refuse to take the oath, and what have political opinions to do with teaching anatomy? Scarpa confers honor upon the University and upon the country which I now govern, and I wish that he be restored to his former position.” He was accordingly restored to his professorship and during the following seven years—that is, up to 1812—Scarpa continued his work of teaching anatomy and of conducting the surgical clinic. During the later years of his life he was a great sufferer from calculous nephritis and chronic disease of the urinary bladder, and these diseases finally caused his death on October 31, 1832.
Dezeimeris, in his estimate of the part played by Scarpa in advancing the science of medicine, lays particular stress upon the following two things: first, he was very active and persisted in his efforts to impress upon surgeons the importance of considering a knowledge of anatomy as affording the only safe and sure route to progress in the surgical art; and, second, he furnished a number of beautiful examples that showed the necessity of throwing additional light upon the different diseases by the employment of demonstrations in topographical and pathological anatomy.
His more important published works are—aside from the value of the text—chefs-d’oeuvre of iconography. Such, for example, are the following: “De Structura Fenestrae Rotundae Auris etc.,” Modena, 1772; “De Grangliis et Plexubus Nervorum,” Modena, 1779; “Anatomicae Disquisitiones de Auditu et Olfactu,” Pavia, 1789; and “Opuscoli di Chirurgia,” Pavia, 1825–1832, 3 vols.
Samuel-Auguste-André-David Tissot (1728). The Tissots are of Italian origin. Alessandro Tissoni, the youngest son of one of the first families of Spoleto, accompanied 98Prince Louis on his crusade to the Holy Land in 1147, and, after escaping from the disasters incident to the siege of Damascus, he managed to regain his native land along with the forlorn remnants of Louis’ army. As he had joined the expedition contrary to the wishes of his parents he felt that it would not do for him to return to Spoleto. At first, therefore, he was a homeless wanderer in his own country. Fortunately for him, however, three of his companions in arms bequeathed to him all their property just before they died from their wounds; and consequently one of his first cares, after he returned to Italy, was to gain possession of his legacies. In the case of one of the three men there was a sister living, and so—partly from love and partly in order to escape any unpleasant legal complications—Alessandro married her, and the couple took possession of the deceased brother’s landed property. Some of this property, it so happened, was located in Franche-Comté, near the present city of Besançon, and it was while he resided in this part of France (1152) that he changed his name to Tissot, thus putting an end to the possibility that his relatives in Spoleto would ever be able successfully to claim any part of his property. Samuel-André’s father, Pierre Tissot, a land surveyor who resided in Grancy, not far from Lausanne, entered his son’s name (May 15, 1741) at the Academy of Geneva, in the department of belles-lettres. In August, 1745, he received the degree of M.A., and on the fourteenth of the following month of September he started on his journey to Montpellier where he was to study medicine. Four years later he passed all his examinations creditably and was given the degree of M.D. He chose Lausanne as his place of residence, and was successful, at the end of one year, in obtaining the position of Physician of the Poor. Early in 1745 he made the acquaintance of Albrecht von Haller, the celebrated physiologist of Berne, and about the same time he became deeply attached to Dr. Théodore Tronchin, a native of Geneva, but engaged in active practice at Paris. These two men were the most distinguished Swiss Physicians of that period.
Eynard, Tissot’s biographer, says that up to the end of 99his life he preferred to carry on his epistolary correspondence in Latin; and yet at the same time he was the author of several medical treatises that were extremely popular. One of them in particular (“L’Avis au Peuple”) passed through many French editions,[14] and was translated, in the course of the next twenty-five years, into all the leading European languages. Strange as it may appear to us moderns, this book was not written originally for the general public, but only for the peasants of the Canton de Vaud, who were constantly falling victims to charlatans and itinerant quacks; and yet the universities of Goettingen and Giessen recommended the work as proper reading matter for their students. In order to show the high degree of esteem in which Tissot was held by his fellow citizens of Lausanne, the authorities conferred on him the rights and privileges of citizenship “on account of his praiseworthy efforts to improve the condition of its inhabitants”; and as, in the course of time, the limits of the city were extended, the name “Avenue Dr. Tissot” was bestowed on one of its finest residence streets.
In 1765 Stanislas Augustus, King of Poland, invited Tissot to accept the office of First Physician of his Majesty at Warsaw. Although the invitation was couched in the most friendly terms, Tissot was not willing to leave his beloved Lausanne. All sorts of influences were brought into play by the King to make him change his mind, but his resolution remained fixed. In his reply to the letter Tissot said:—
My first reason for declining your highly flattering offer is this: I am very much attached to my father and mother and to my uncle, who have brought me up from infancy with the tenderest care, and who, owing to their advanced age, are likely at any time to need my aid and advice, and who would be heartbroken if I were to go far away from them. My second reason consists in the sentiment that I am not in any way fitted to fill such a position with entire satisfaction to all the interests concerned, for it involves many important duties beside that of watching over your health—as, for example, the superintendence of the different institutions in your kingdom which are devoted to the preservation of the health of 100your subjects; the duty of reporting to you any evidences of mismanagement that I may discover and the suggestion of such new measures as are likely to remedy any such deficiencies; the promotion of the efficiency of your schools of medicine, surgery, midwifery, pharmacy, etc.; and, last of all, there is the important consideration that my position here in Lausanne is in every respect most satisfactory to me. Why, then, should I abandon these surroundings in which my life is most happy, for a position in which I might easily lose a large part of this happiness?
Notwithstanding Tissot’s decided refusal to accept the flattering offer made by King Stanislas, the latter did not give up all hope of persuading him eventually to accept the position of First Physician. Three times in succession, at short intervals, he sent him a renewal of the invitation, each time adding some fresh inducement in the hope of overcoming Tissot’s objections; and, just as the latter had nearly made up his mind to yield to the King’s urgent request—the death of his much-beloved uncle a few days previously having removed one of the strongest obstacles in the way of his acceptance—the ruling authorities of the Academy of Lausanne notified him that a Chair of Medicine had been created by them and that he had been appointed its first occupant. Stanislas then at last recognized that he must definitely abandon his cherished project, and he accordingly sent a fine portrait of himself to Tissot, with a charming letter in which he said:—
I am truly afflicted by your decision, but I take comfort in the thought that probably my persistent efforts to bring you to Warsaw had something to do with hastening the decision of the Berne authorities to establish the Chair of Medicine at Lausanne for your benefit. I congratulate you on your good fortune and your compatriots on their having had the wisdom to appreciate the value of your services to Switzerland. I pray God, Monsieur Tissot, that He may have you in safe keeping.
Warsaw, March 5, 1765.
Lausanne in 1765, it should here be stated, still recognized the Bernese Government as its overlord. It was only at a somewhat later date that it acquired entire independence.
101In closing this brief account of Tissot’s correspondence with the King of Poland, I ought to add that it was largely through the intercession of Albrecht von Haller, the distinguished physiologist and himself a citizen of the Swiss metropolis, that the senators at Berne were induced to found a Chair of Medicine at Lausanne for the express purpose of preventing Tissot from leaving Switzerland. I also should state that Tissot himself was entirely ignorant at the time that von Haller had been instrumental in effecting the establishment of this new professorship at Lausanne.
Here is an anecdote which is told by Lantier in his book “Les Voyageurs en Suisse.” While it relates only indirectly to Tissot it furnishes an amusing illustration of what may easily happen in the experience of any physician who has a large office practice:—
A certain Adolphe D. called at Tissot’s residence and rang the door bell. An elderly female servant, who opened the door, said that her master, the doctor, was not at home. “But,” she added, “if you have come to consult him about some malady, I warn you that you will lose your money and have nothing to show for your trouble. For the past twenty years I have had a pain in my stomach, and the doctor has not been able to cure it.” Tissot, to whom I related the incident, joined me in a hearty laugh over the affair.
In November, 1779, Tissot was urged to visit Paris in company with his adopted son, who was studying medicine. Believing that the young student would be greatly benefited by such a visit to the French capital he at once decided to undertake the trip. But, very soon after his arrival in Paris, he discovered that he was to have no rest so long as he remained there. His celebrity brought him almost at once many people who wished to consult him about their ailments. Often, says his biographer, the Rue des Petits Augustins, where his temporary residence was located, was filled with a long line of carriages belonging to the distinguished patients who awaited their turn to interview the great physician from Lausanne. This sort of medical practice was not at all to his taste; and when he was not busy with professional work he was attending an endless series 102of dinners and receptions. At the end of a few months he returned to Lausanne, and would have been well pleased to remain there permanently; but he soon recognized that, in the interest of his adopted son, he should take up his residence in some German or Italian city where there was a university. Just at this juncture of affairs Borsieri, the distinguished Professor of the Theory and Practice of Medicine at the University of Pavia, Tuscany, a man well advanced in years, sent in his resignation. Whereupon Joseph II., Holy Roman Emperor and King of Austria, immediately urged his brother Leopold II., Duke of Tuscany, to offer the position to Dr. Tissot. The latter took the invitation seriously under consideration and in due course of time accepted. His honorarium was fixed at 3000 German florins (about $1500 U. S. currency) and in addition he was accorded various important privileges—such, for example, as a suitably furnished residence; a ward equipped with six beds and arranged in such a manner that clinical instruction might be conveniently given in it; and the right to carry on private practice in the district of Milan and also outside the limits of that district whenever this could be done without interfering with his duties at the university. Further, he was permitted to resign his chair at the end of two years if he should so desire. Finally, he was reimbursed for all his traveling expenses, and was absolved from attendance upon any functions or ceremonies that might conflict with his conscientious scruples as a Protestant. For a Government that was strictly under the control of the Roman Catholic Church these terms were remarkably liberal.
Tissot appears to have been very successful, both as a teacher and in his social relations with the people whom he met during his short stay of two years at Pavia. In a letter which Spallanzani wrote on December 31, 1781, to Charles Bonnet, the distinguished naturalist of Geneva, he speaks of Tissot’s arrival at Pavia in the following terms:—
He seems to be pleased with our university, with our colleagues, and with our students. Everybody in Pavia likes him. His lectures are most instructive and well adapted to the character of our 103young men who have come hither from every part of Italy to profit from the teaching of this Swiss Hippocrates. Apart from the knowledge which he possesses, and which certainly is very extensive, Monsieur Tissot is the most polished, the most amiable man I have ever met.
It would be a pleasure to furnish here a résumé of the detailed account which Tissot’s biographer gives of his lectures and of his most practical clinical instruction, but I perceive that I have already drawn out my sketch to an inordinate length, and I must therefore stop at this point. I will simply add one more item of information. Early in 1783 Tissot publicly announced his intention of resigning his professorship at the end of the period of service that had originally been agreed upon—viz., two years; and on June 12 of the same year, at which date the academic year ended, he delivered his farewell address to the students of the university. To perpetuate the memory of this occasion those students who were permanent residents of Pavia set up in one of the lecture rooms a suitably inscribed marble tablet; those who came from other parts of Europe (72 in all) prepared their memorial in the form of a small printed volume (104 pages) of sonnets written in Latin, Greek, Italian, German, French and English, and grouped together under the title:—
Sentimenti d’Affetto e di Riconoscenza Degli Studenti di medicina Verso il Loro Immortale Precettore, il Signor S. A. D. Tissot.
On the 21st of June, 1783, in company with his nephew, Tissot left Pavia for Switzerland by way of the Simplon Pass.
Already in 1794 his health began to show unmistakable signs of breaking down under the influence of a progressive pulmonary tuberculosis, and it was not long afterward that his death occurred (June 13, 1797) at his residence in Lausanne.
Aloysius Galvani, born at Bologna, Italy, on September 9, 1759, and appointed public lecturer in anatomy at the university in 1762, published in 1791 a treatise in which he announced his discovery of a new force to which he gave the 104name of animal electricity, but which subsequently received that of “galvanism” in honor of its discoverer,—a name which it has retained ever since. By a mere accident Galvani discovered the fact that when two different metals—iron and copper, for example—are brought in contact with muscular tissue there results from this contact a force, seemingly an electric current, which causes the muscle to contract. Six years later—that is, in 1797—the Cisalpine Republic was formed by the joining together of what were known as the Cispadane and the Transpadane Republics—two political organizations that occupied respectively, as their names imply, territories situated the one on the north side and the other on the south side of the river Po, and both of which organizations owed their existence to the action of Napoleon Bonaparte. When the professors of the University of Bologna, which was located in the Transpadane territory, were called upon to swear allegiance to the new republic, Galvani was the only member of the Faculty who refused to take the oath, and as a consequence he lost his professorship. His death occurred in 1798.
About the year 922 of the present era the Arabian physician Rhazes wrote and published (in MS.) the earliest known report of the malady now called Variola or Small-Pox. From this fact the inference should not be drawn that the disease first came into existence in the time of Rhazes, for it can scarcely be doubted that it had already existed in the East for ages before the period mentioned. Since the thirteenth century it has appeared repeatedly in epidemic form in widely separated countries, causing, especially among the eastern nations, a fearful mortality. Sydenham, the great English physician, succeeded during the seventeenth century in devising a method of treatment that in some degree diminished the mortality of this affection, at least in Great Britain. It was, however, in no sense a preventive procedure, and the spread of small-pox continued unchecked until Jenner, in 1796, introduced vaccination; and even then the efficiency of this method was not promptly acknowledged by the Medical Profession; indeed, several years had to elapse before even the best London physicians, the men who possessed the most complete facilities for ascertaining the whole truth with regard to Jenner and his new method, became convinced that a great and most efficacious protection against small-pox had at last been found. In the meantime—that is, for almost half a century—the procedure known as “inoculation” was accepted by the upper classes of the community in all parts of Europe as affording the maximum amount of protection attainable against the disease.
108There were in Europe, during the last half of the eighteenth century, two physicians—Baron Thomas Dimsdale, an Englishman, and Dr. Théodore Tronchin, of Geneva and Paris—who obtained considerable celebrity as inoculators.
The first-named, Baron Thomas Dimsdale, was born in 1712 and began to practice his profession in 1734 at Hertford, twenty-four miles north of London. Already as early as in 1741 he had acquired so great a reputation for his success, both in performing the operation and in carrying the patient safely through the resulting infection,—that is, through the attack of small-pox thus artificially produced,—that he was sent for to inoculate first the Czarina of Russia, then the Grand Duke Paul, and subsequently the children of many of the first families of the Russian Empire. Shortly after his return to England he was made a member of the Royal Society, and at a still later date the city of Hertford chose him as their representative in the House of Commons. In 1781, on the occasion of his second visit to Russia, he inoculated the Czar Alexander and the Grand Duke Constantine. His death occurred on December 30, 1800.
Among Dimsdale’s published works relating to small-pox and inoculation the following deserve to receive special mention: “The Present Method of Inoculating for the Small-Pox”, London, 1766, 1767 and 1772; “Thoughts on General and Partial Inoculation,” London, 1776; and “Account of a Voyage to Russia and Report of the Procedure Carried out in the Cases of Catherine and Paul.”
Baron Dimsdale, it seems scarcely necessary to add, was not the inventor of the practice of inoculation but simply the individual who revived and made popular, first in England and afterward on the continent of Europe (more particularly in Russia), a practice which long before had been employed in China.
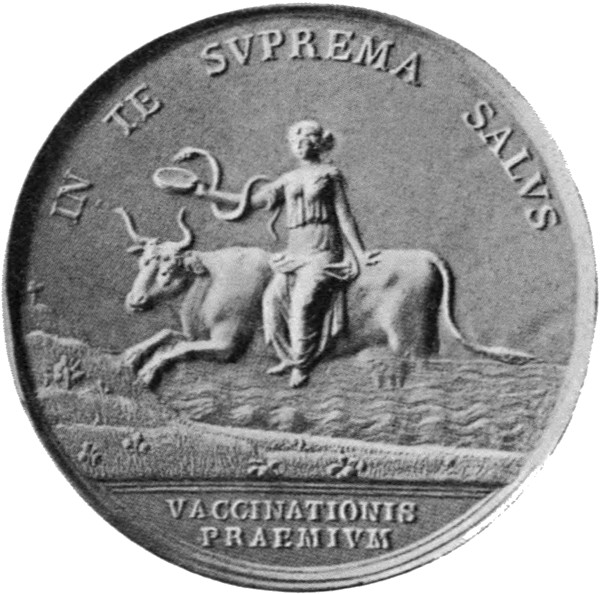
Medal commemorating the discovery of vaccination. From Eugen Hollaender’s “Medizin und Plastik,” by permission.
Théodore Tronchin, the second inoculator mentioned above, was a native of Geneva, Switzerland,[15] and was highly 109esteemed in France as a practitioner of medicine during the period that is now under consideration (1750–1785). Furthermore, it was widely known that he was the family physician of Louis Philippe, Duke of Orleans, as well as the medical adviser and intimate friend of Voltaire, both of which facts undoubtedly aided him in gaining popularity among the members of the fashionable set of Paris. It is therefore easy to understand why, when he espoused the cause of inoculation, he should have so rapidly attained celebrity as a successful inoculator, not only in Paris but also throughout Europe. On the other hand, it is not at all clear why the inoculation method should have been looked upon with any favor by the educated classes, for it soon became increasingly evident that the operation was attended with considerable risk through the danger of introducing other infective agents into the system; and, in addition, no satisfactory evidence was forthcoming that these inoculations possessed the slightest degree of genuine protective power. To-day we are unable to discover in this procedure any other advantages than the following:—The patient is thereby enabled to select the time when, and the surroundings in which, he or she will submit to an attack of small-pox; for, it must be remembered, no well-grounded hope was held out by the inoculators of the eighteenth century that the artificially produced disease would prove less fatal than that which is acquired accidentally. And yet some such hope was apparently cherished by the people of that period, for Benjamin Franklin, writing in 1788, makes the following remark in relation to this very question:—
In 1736 I lost one of my sons, a fine boy of four years old, by the small-pox, taken in the common way. I long regretted bitterly, and still regret, that I had not given it to him by inoculation. This I mention for the sake of parents who omit that operation, on the supposition that they never should forgive themselves if a child died under it; my example showing that the regret may be the same either way, and that, therefore, the safer should be chosen.
These bitter regrets expressed by Franklin show plainly 110that he, like others of his time, had strong confidence in the efficiency of inoculation.
Edward Jenner, the discoverer of vaccination as an effective means of protection against small-pox, was born at Berkeley, Gloucestershire, England, on May 17, 1749. After the death of his parents while he was still a mere child, Edward passed under the guardianship of his eldest brother, the Rev. Stephen Jenner, and was brought up by him with affectionate care and judicious guidance. At a very early age he showed a decided taste for natural history; and after leaving school he began to receive instruction in the elements of surgery and pharmacy from a Mr. Ludlow, an eminent surgeon of Sodbury, near Bristol. As the next step in his education he spent two years under the direction of the celebrated experimental pathologist, John Hunter, of London, in whose family he resided for two years. He was about twenty-one years of age when he went to London.
Already at this early period he showed unmistakable evidences of being a close observer, scrupulous and accurate in his examination of the objects of his studies. He was also gifted with much enterprise and perseverance, characteristics which greatly aided him in mastering difficulties that would have seriously obstructed the progress of an individual possessing an inferior mind. Mr. Hunter, who was at this time in the prime of life, completely won the affection and respect of his pupil, who particularly admired the boldness and independence of his teacher’s character. Jenner was peculiarly alive to virtues of this kind. After completing his professional studies in London he retired from Hunter’s house, but the intimate relations which had been established between these two men persisted up to the time of the latter’s death in October, 1793.

EDWARD JENNER
(Copied from Thomas J. Pettigrew’s “Medical Portrait Gallery,” London, 1838. The original portrait was painted by Sir Thomas Lawrence, Royal Academy.)
Immediately after his return from London Jenner took up his residence with his brother Stephen, at Berkeley, and began his career as a practitioner of medicine. At the same time, as opportunity afforded, he continued to pursue his favorite studies in natural history. Thus, in a comparatively 111short period of time, he accumulated a series of specimens illustrative of comparative anatomy, and sufficiently numerous to form a museum of no inconsiderable magnitude.
In describing the manner in which Jenner’s attention was first seriously directed to the subject of cow-pox Dr. Baron, his biographer, uses the following language:—
Jenner was pursuing his professional education in the house of his master at Sodbury; a young country-woman came to seek advice; the subject of small-pox was mentioned in her presence; she immediately observed, “I cannot take that disease, for I have had cow-pox.” This incident riveted the attention of Jenner. It was the first time that the popular notion, which was not at all uncommon in the district, had been brought home to him with force and influence. Most happily the impression which was then made was never effaced. Young as he was, and insufficiently acquainted with any of the laws of physiology or pathology, he dwelt with deep interest on the communication which had been casually made known to him by a peasant, and partly foresaw the vast consequences which were involved in so remarkable a phenomenon. He was the more stimulated to meditations of this sort by frequent opportunities of witnessing the ravages of small-pox; and by retaining the most vivid and painful recollections of the severe discipline which he himself had not long before passed through, preparatory to his inoculation for that disease. “There was”—to use his own words—“bleeding till the blood was thin; purging till the body was wasted to a skeleton; and starving on vegetable diet to keep it so.” The possibility of averting such evils could not arise in a mind like Jenner’s without possessing it fully; and he resolved to let no opportunity escape of acquiring knowledge on so important a subject.... It was not till some years after his return from London that he had an opportunity of examining into the truth of the traditions respecting cow-pox. This was about the year 1775, a date which corresponds with the period specified by him in his tract on “The Origin of Vaccine Inoculation.”
Although during the following five years Jenner’s efforts to learn the full truth about cow-pox brought him very little nearer the goal which he was aiming to reach, he nevertheless pursued with zeal and vigor his studies concerning the nature of this disease and concerning its relations to 112small-pox. Among the facts which he ascertained during this period the following deserve to receive mention here: (1) There are several different diseases to which milkers are liable when they handle infected cows; but (2) only one of them possesses the power of furnishing protection against small-pox. The discovery of these facts made it easy to understand why vaccination with the virus of what was commonly called cow-pox not infrequently failed to protect the individual so vaccinated from genuine small-pox.
As a result of still further investigations Jenner felt warranted in drawing the conclusion that small-pox, cow-pox and swine-pox had a common origin,—in fact, were varieties of the same disease. Dr. Baron mentions the following incidents or experiences as affording a strong corroboration of the truth of the statements just made:—
In November, 1789, Jenner inoculated his eldest son Edward, who was then about one year and a half old, with swine-pox matter. The progress of the disease seemed similar to that which arises from the insertion of true small-pox matter when the disease is very slight. He sickened on the eighth day; a few pustules appeared; they were late and were slow in their progress and small. Subsequently, at five or six different periods, variolous matter was carefully inserted into his arms without the slightest inflammation being excited in the part.
On April 7, 1791, variolous matter was again inserted by two small incisions through the cutis.
April 9, parts evidently inflamed.
April 10, an efflorescence of the size of a shilling spread around the inferior wound.
April 11, the incision assumed a kind of erysipelatous elevation; the efflorescence much increased.
April 12, still further increase in the efflorescence; a vesicle about the size of a large split pea, and containing a brownish clear fluid, had also formed close to the superior incision; and a still larger one was visible near the edge of the inferior incision. The erysipelas extended to the shoulder and then quickly subsided. The child showed no signs of indisposition the whole time.
In March, 1792, a fresh inoculation was made. A well-marked inflammatory reaction followed.
At a later date Jenner learned that there were well-authenticated instances to prove that when the true cow-pox broke out among 113cattle at a dairy and was communicated to the milkers, even they had subsequently contracted small-pox. The discovery of this fact perplexed him greatly. Indeed, in the case of most men the discovery would probably have led to the abandonment of all further experimentation. But Jenner did not allow himself to be discouraged. It occurred to him that the virus of the cow-pox itself might have undergone some change whereby its specific virtues were lost; that, in this deteriorated state, it might have been capable of producing only a local disease upon the hand, but no such influence upon the constitution as is requisite to render the individual unsusceptible of contracting small-pox. In other words, he believed it possible that the same cow might one day communicate a genuine and efficacious preventive, and, the next, nothing but a local affection that would exert no beneficial influence whatever on the constitution. This most ingenious and forcible reasoning, supported by analogies drawn from the well-known properties of the virus of small-pox itself, received an ample confirmation from experience, and was the basis on which some of the fundamental rules for the practice of vaccination were founded. It was ascertained that it was only in a certain state of the pustule that virus was afforded capable of imparting to the constitution its protecting power; that matter taken after this period might excite a local disease, but not of such a sort as to render the individual proof against the effects of variolous contagion.
In 1796 Jenner had an opportunity to carry his investigations a step further.
“Hitherto,” says his biographer, “he had only observed the casual disease and investigated its laws; it yet remained to be proved whether it was possible to propagate the affection by artificial inoculation from one human being to another, and thereby, at will, communicate security to all who were liable to small-pox. An opportunity occurred, on the fourteenth of May, 1796, of instituting this experiment. Matter was taken from the hand of Sarah Nelmes who had been infected by her master’s cows, and inserted by two superficial incisions into the arms of James Phipps, a healthy boy eight years old. He went through the disease apparently in a regular and satisfactory manner; but the most agitating part of the trial still remained to be performed. It was needful to ascertain whether he was secure from the contagion of small-pox. This point, so full of anxiety to Dr. Jenner, was fairly put to issue on the first of the following July. Variolous matter, immediately 114taken from a pustule, was carefully inserted by several incisions, but no disease followed.”
Shortly afterward Jenner wrote to his friend Gardner:—
You will be gratified in hearing that I have at length accomplished what I have been so long waiting for, viz., the passing of the vaccine virus (the virus of cow-pox) from one human being to another by the ordinary mode of inoculation.... I was astonished at the close resemblance of the pustules, in some of their stages, to the variolous pustules. But now listen to the most delightful part of my story. The boy has since been inoculated for the small-pox, which, as I ventured to predict, produced no effect. I shall now pursue my experiments with redoubled ardor.
My readers can easily imagine with what deep anxiety mingled with an intense desire for a completely successful result, Jenner, from this time forward, prosecuted his labors. Unfortunately, he was not able, owing to the disappearance of cow-pox from the dairies of the region in which he lived, to resume his experimental work before the spring of 1798. He was also not willing to make a public announcement of the important results which he had obtained until he should have amply confirmed their accuracy by further experimentation. It was therefore not until during the early part of the summer of 1798 that he issued a printed pamphlet of a little more than seventy pages, in the quarto form, and bearing the title “An Inquiry into the Causes and Effects of the Variolae Vaccinae.”
On April 24, 1798, about two months before the publication of his pamphlet, Jenner repaired to London for the purposes of exhibiting the cow-pox and of demonstrating to his professional friends the truth of his assertions. Although he remained in the metropolis nearly three months he was unable to procure a single person on whom he could exhibit the vaccine disease.
Some of the cow-pox virus which Jenner carried with him was consigned to Mr. Cline, a London physician, who, toward the end of July, inserted it by two punctures into the hip of a child. A few days later he reported that “the cow-pox experiment had succeeded admirably.”
As happens in practically every important discovery in 115therapeutics, there arose soon in many quarters serious doubts as to the prophylactic powers of the method advocated by Jenner. Some men even went so far as to question the accuracy of his statements and to impugn his authority to advocate the practice of vaccination. On the other hand, there were many, and they too of the most learned and respectable, who immediately did justice to the merits of Jenner, and who cordially acknowledged the many important consequences which were involved in the subject that he had so ably and so modestly brought before them.
From a letter which Jenner wrote to one of his friends only a few weeks after he had published the “Inquiry” it appears that already at that early date he foresaw the probability that there would occur, in the further evolution of vaccination as a prophylactic measure, those very complications which, from that time to the present, have interfered so seriously with the universal acceptance of this procedure as a measure of vast beneficence to the human race. These so-called complications were, in the great majority of instances, manifestations of septic infection, brought about by carelessness in the handling of the inoculation wound; but this fact was not at all appreciated in Jenner’s time. During the years immediately following that in which the discovery of the new procedure was announced to the physicians of England vaccination made fairly rapid progress in public favor. Already as early as in June, 1800, Jenner, while on a visit to Oxford, was there presented, by the leading physicians of that city, with a testimonial in which it was declared that cow-pox is an effectual prophylactic agent against the small-pox. Two years later the English Parliament voted Jenner a grant of £10,000 as a reward for the very valuable discovery which he had made and for his prolonged labors in rendering the procedure of great utility to the public.
Strange as it may appear to those who are not familiar with the lives of the most meritorious and most unselfish physicians of bygone centuries this bestowal of £10,000 by Parliament upon Jenner did not add materially to his comfort; in the long run it rather detracted from it. Some of 116his friends, shortly after he had received the Parliamentary grant of money, induced him to give up his country practice and establish himself in the fashionable part of London; they maintained that his widespread reputation as the discoverer of vaccination and as the physician most capable of conducting this operation in the safest and most effective manner, would speedily bring him a large increase in private practice. Such, however, did not prove to be the case; and Jenner—who, unfortunately, had been overpersuaded to follow this advice,—after the lapse of three or four years, and appreciating the fact that his income was not large enough for such a style of living, removed his residence, first to Cheltenham and not long afterward to Berkeley. He died of cerebral apoplexy in the spring of 1823.
A medal commemorating the discovery of vaccination is pictured in the figure which faces page 108.
THE ENGLISH AND FRENCH CHEMISTS CONTRIBUTE THEIR SHARE TOWARD THE ADVANCE OF MEDICAL KNOWLEDGE
During the latter part of the eighteenth century the chemists of England and France manifested a new and decidedly stronger interest in their branch of natural science; indeed, they seemed to have suddenly appreciated the fact that observation and experience afforded the only route by which they might secure a genuine and useful increase of their stock of knowledge. In the departments of physiology and pathology, for example,—not to mention also that of therapeutics,—there were at that period many questions which still remained unsettled and which could not be satisfactorily answered until a further advance had been made in the existing knowledge of chemistry. Hence the great importance of the movement to which I have just referred. To cite only one of these unsettled questions I will mention here that relating to the nature of the change which occurs in the blood when it loses its venous hue after passing through the lungs, and also, vice versa, when it loses its arterial color after passing through the tissues in other parts of the body. Harvey’s discovery had gone no further than to reveal the pathway of the blood in its winding course throughout the body, but now physiology demanded an explanation of the changes which this fluid undergoes in its travels along that pathway. The answer to this last question, as will now be shown, was not gained through the efforts of a single individual but by the researches that were made by several very able English and French scientists, more particularly by Joseph Priestley, the English chemist, and by Lavoisier, the French biologist and chemist. During the preceding fifty or sixty years the physicians of Europe 120had been obliged, for want of a more satisfactory explanation, to accept Stahl’s phlogiston theory (that all combustible materials contain an element to which he applied the name of “phlogiston”), at least as a basis or starting-point for the desired explanation.
Joseph Priestley, who was born at Fieldhead, near Leeds, England, in 1733, received his early education at a Dissenting school; and in 1755 he became a Dissenting minister at Needham Market. So far as the available evidence affords any clear indication of Priestley’s bent of character the inference is permissible that he was first and chiefly a scientist, but yet possessing a profoundly religious type of mind which the influences surrounding his boyhood doubtless helped to intensify. Thus, during his ministerial work he managed to devote a large part of his time to original investigations in the domain of chemistry; and, as early as in the year 1774, he succeeded in obtaining a gaseous product to which he gave the name of “dephlogisticated air.”[16] A detailed description of this discovery of oxygen—the name which was given to the new gas at a later date—will be found in Vol. 2 of the second edition of Priestley’s “Experiments and Observations on Different Kinds of Air,” London, 1784. Broadly speaking, Priestley obtained the new product by heating the red oxide of mercury. Subsequently he discovered that respiration took place more easily, and that combustion progressed more actively, in the presence of this gas. But it is to the French chemist Lavoisier that we owe the knowledge of the full significance of oxygen. On the other hand, it was the English chemist Cavendish who confirmed Priestley’s discovery that atmospheric air is composed of water and different acids. Lavoisier, it is claimed, discovered that all the acids which he examined contain oxygen.
Speaking, at a later date, of his attempt to produce a work on the chemistry of the air, Priestley says: “I find it absolutely impossible to produce such a work that shall be 121anything like complete. My first publication I acknowledged to be very imperfect, and the present, I am as ready to acknowledge, is still more so. But, paradoxical as it may seem, this will ever be the case in the progress of natural science, so long as the works of God are, like himself, infinite and inexhaustible. In completing one discovery we never fail to get an imperfect knowledge of others, of which we could have no idea before; so that we cannot solve one doubt without creating several new ones. Travelling on this ground resembles Pope’s description of travelling among the Alps, with this difference, that here there is not only a succession, but an increase of new objects and new difficulties.”
Here is the description to which Priestley refers:—
On the 14th of July, 1791, there occurred a serious riot at Birmingham, where Priestley was at that time settled as a Dissenting minister. On that day a banquet was being given in honor of the French Revolution, those who organized this feast being in large measure Episcopalians. There were numerous fraudulent cards of invitation which, rumor said, were issued by Priestley. On the occasion itself numerous toasts were offered in which sentiments antagonistic to those generally entertained by the originators of the feast, were expressed. As the festival progressed the crowd became more and more excited and everybody seemed to be imbued with the idea that in some way or other Priestley was mixed up in the matter. The truth was, however, he had nothing whatever to do with it, was not present at the banquet, and even did not know that such a feast was being given. Nevertheless, the crowd would not listen to reason, 122and insisted that Priestley was the cause of the whole trouble. Accordingly they secured lighted torches and hastened to Priestley’s house which was located about half a mile from the city limits, and proceeded to set it on fire. Thus were destroyed, in the course of a few minutes, all his books, all his valuable scientific apparatus, all the registers of experiments covering a period of eleven years of unremitting toil. Priestley, who was then nearly seventy years old, lost practically everything that he possessed. For three days the rioting continued, many of the houses of Priestley’s friends being also destroyed by fire. Even the daily newspapers asserted that among Priestley’s papers were found evidences showing that a great conspiracy existed,—but for what evil purpose it was not stated. Insults of all sorts were heaped upon the innocent man, until finally he was compelled, by the situation of affairs in Birmingham, to leave the country. Fortunately for him, Priestley’s brother-in-law left him in his will the sum of £10,000 and also an annuity of £200. Thus provided for, Priestley left England in 1794 and settled in Pennsylvania. His death occurred in 1804.
Antoine Laurent Lavoisier was born in 1743 at Paris, and at an early age displayed a fondness for serious scientific studies. In 1768, although he had attained only his twenty-fifth year, he was chosen a member of the French Academy of the Sciences; and a very short time afterward he received the appointment of Fermier Général (Government Collector of Taxes), an appointment which showed how highly he was esteemed for his ability as well as for his integrity. At first, Lavoisier, like nearly all his contemporaries, accepted Stahl’s phlogiston doctrine and his views with regard to animism (see pp. 432 and 433 of my work entitled: “The Growth of Medicine”); but gradually he entertained more and more serious doubts with regard to their correctness, and finally he came out boldly as an opponent of these doctrines. The experiments which he himself made, as well as those which were carried out by other scientists of the same period, forced him to conclude 123that, in all chemical processes, no such thing as an actual creation of something new takes place, nor is anything ever lost. This truth, he claimed, applies as well to living beings as to inanimate objects. In the middle of the eighteenth century the treatises on chemistry did not acknowledge this teaching as true. Vauquelin, for example, pointed to what he believed to be a fact, viz., that animals actually produce lime, inasmuch as hens—so he claimed—produce more lime than they ingest with their food. Lavoisier’s remarkable experiments showed that Stahl’s doctrine of animism, as well as the phlogiston theory, was untenable. Stahl maintained, for example, that there exists in all combustible bodies a special element which is set free during the combustion of such bodies, and to this element—as I have already stated on a previous page—he gave the name of “phlogiston.” Lavoisier, on the other hand, made it clear that combustion represents simply the combination of the two elements, carbon and oxygen; and at the same time he showed that the act of respiration in animals is a species of combustion, in the course of which oxygen combines with certain elements of the body to form water and carbonic acid. He did not, however, rest satisfied with these results, but—aided by Seguin—pushed his experiments to the point where he demonstrated the quantities of gas expired both by man and by animals; thus greatly increasing our knowledge of the phenomena of life.
Furthermore, Lavoisier was also the discoverer of a method of analysis (still employed to-day) by means of which it is possible to demonstrate the important fact that all organic bodies are composed of carbon, hydrogen and oxygen, sometimes in association with azote (lifeless matter). In a word, he brought physiological chemistry to such a stage of perfection that his successors have been able only to make additions to the facts which he discovered, but not to alter them in any essential respect.
Lavoisier’s mind seemed always preoccupied with questions relating to the grandeur and progress of humanity in its entirety. Here is a single example of the truth of this statement:—
124When he learned from his own observations that the exhalation of carbonic acid increased during physical work, he drew the conclusion that men who are obliged to perform severe labor stand in need of a more abundant nourishment than is required by ordinary workmen in order to recover the carbon which had been expended in their severe labors; and he immediately urged that an effort be made to furnish the working class with better nourishment. The public functionary—he wrote at the end of his treatise on respiration (published in 1789)—is not the only individual who works for his country. The man of science, he added, is also fulfilling his patriotic duty when he teaches, by his investigations, how the misery which exists in the world may be alleviated. And if he accomplishes nothing more than to add a few years, or even only a few days, to the average duration of the life of man, he still may with justice claim the right to be given the glorious title of “benefactor of humanity.” (J. Rosenthal.)
France, at the time when Lavoisier wrote his treatise on respiration, was in the throes of a great revolution, out of which came the Republic. But this republic showed no gratitude to Lavoisier for the services which he had rendered to his country; for, on the 8th of May, 1794, it executed him without any specific charge having been brought against him, simply because he had held the hated office of Government Collector of Taxes. When one of Lavoisier’s personal friends, just before the prisoner was removed to the guillotine, called the judge’s attention to his scientific merits, this functionary replied: “We no longer have any use for men of science.”
Before closing this necessarily brief and somewhat superficial account of the work accomplished by the great French chemist, Lavoisier, I must beg permission to refer very briefly to the views which he entertained on the subject of heat-production. The chief significance of these studies of the fundamental phenomena of animal life is this: they afforded for the first time a solid basis for the theory of heat-production in living animals. This theory, formulated in greater detail, may be stated in the following terms, which I copy in all important respects from the memoir published by Rosenthal:—The tissues which compose the body of the animal, and which are themselves composed of carbon, 125hydrogen, oxygen and azote, possess the power of assimilating a further quantity of oxygen, a quantity somewhat greater than that which they already contain; and, by reason of this fact, they are able, as combustion advances, to accomplish two things—first, to combine with the surplus oxygen furnished by respiration; and, second, to form carbonic acid, water and certain azotic matters that are discharged from the body. It is this process of combustion which gives rise to heat in the animal’s body and in addition is associated with a certain loss in its weight. This loss, however, is limited, for the furnishing of new elements is going on simultaneously with the casting off of the old, thus restricting the loss of weight.
It is to Lavoisier that the imperishable honor belongs of formulating the chemical theory of respiration, and of thereby founding a new era in physiology—the modern era. (Claude Bernard.)
Too much stress cannot be laid upon the truth of this declaration made by Claude Bernard, the great modern authority in physiology, concerning this, the most important advance secured for the science of medicine during the eighteenth century. But alas! many years had to elapse before the physiologists of that period were able to appreciate the importance of Lavoisier’s discovery. Very soon after the announcement of this new theory the leading chemists of Europe returned almost as a single body to the old phlogiston doctrine.
Lavoisier’s portrait is shown in the frontispiece of the present volume.
ENGLISH LEADERS IN MEDICINE AND SURGERY DURING THE EIGHTEENTH AND EARLY NINETEENTH CENTURIES
First Group: Fothergill, Abernethy, James and John Douglass, Percival Pott and Sir Astley Cooper
The desire to start the science of medicine on a new course of growth seemed to develop at the same time in England that it did on the continent of Europe—that is, during the first half of the eighteenth century. The prolonged wars had for a long period of time turned men’s thoughts entirely aside from scientific inquiries of any kind; but, the moment the outlook seemed bright for a renewal of peaceful relations between the warring nations, there arose, among the men of the different sciences, a strong impulse to resume their normal labors in the various fields of research. Some of the evidences of the truth of this statement have been furnished in the earlier pages of the present work, and already, during the period which we have now reached in this brief historical sketch, the proofs are not lacking that the first fruits of this new harvest are before us and that we may safely form some idea as to their quality.
Of those who should be classed as physicians Fothergill and Abernethy certainly deserve to be named first. The latter, I am well aware, is usually classed among the surgeons, and he certainly deserves to be so classed; but he seems to me to occupy an equally high position as a medical philosopher.
John Fothergill, one of the most distinguished English physicians of the eighteenth century, was born at Carr End, Yorkshire, March 8, 1712. He received his early medical 130training at Edinburgh, under the teaching of Monro, Alston, Sinclair and Plummer, all three of whom had been pupils of Boerhaave, at Leyden, Holland, and was given the degree of Doctor of Medicine by the University of Edinburgh, in 1736. During the years immediately following this event, he visited in turn the principal medical schools of Holland, Germany and France, and then settled definitively in London. In 1746 he met with marked success in the treatment of an epidemic of “putrid sore-throat,” which was raging in England at that period, and which showed a tendency to develop into a gangrenous condition. The physicians of that day employed largely purgatives and bloodletting in their treatment of this disease, but Fothergill depended mainly on the cautious use of emetics, mineral acids, bitters and light wines, the favorite practice among Spanish physicians. The success which attended his plan of treatment brought Fothergill a great increase in reputation as well as in fortune; and thus he was able, in 1762, to purchase at Upton, in Essex, a large tract of land which he developed into a splendid garden, where exotic plants of all sorts were cultivated. He also gathered at this place a very large collection of zoölogical and mineralogical specimens, which in the course of time became one of the most complete that was to be found anywhere in England. From 1765 onward, in order to relieve his health from the almost constant strain of so much business, he adopted the habit of absenting himself from London, regularly every year, for a period of two months; and with this object in view he chose for his retreat an attractive residence near Carr End, the town in which he was born. He died on December 26, 1780, at the age of sixty-nine, and bequeathed his entire fortune—aside from a modest stipend which he left to his sister—to the poor. The inscription written on his tombstone reads as follows: “Here lies Doctor Fothergill, who spent two-hundred thousand guineas for the relief of those in distress.” “I do not believe,” said the immortal Franklin, “that there ever existed a man who was better entitled to receive the esteem and veneration of all mankind than was Fothergill.” (Vicq-d’Azyr, in the Report of the Société Royale, of Paris.)
131Fothergill did not write a single large treatise, but he published, in the Philosophic Transactions and elsewhere, no fewer than forty-one short memoirs on a great variety of topics.
John Abernethy was born of Irish parents about the year 1764. In 1787 he was appointed Assistant Surgeon at St. Bartholomew’s Hospital, London, and was promoted to the position of Surgeon in 1815. From that date to 1827 he served the hospital with great distinction, attaining wide celebrity as a daring and skilful operator and also as a lecturer of great power. In his lectures he laid much stress upon two principles: First, that local diseases had a constitutional origin; and, second, that this origin could generally be traced to disorders of the digestive system.
George G. Sigmond, M.D., contributed to the London Lancet, of November 11, 1837, a brief but most satisfactory biographic sketch of Abernethy, and from this I copy such portions of the text as are likely to convey to my readers a more perfect picture of this great physician and surgeon than I could possibly provide by resorting to a mere compilation of the facts. Here is his account:—
Few individuals who have adorned our profession, possessed a more clear and accurate knowledge of the principles of our science than Mr. Abernethy, and no one ever explained them with greater simplicity, or with less of the entanglement of barbarous and uncouth names; he was, to the highest degree, plain, and, therefore, thoroughly intelligible. He had none of the deep learning and research of his two contemporaries, Dr. Young and Dr. Mason Good, but he was infinitely their superior in the explanation of his views, for he did not, as they have done, encumber his writings with the hard and unintelligible phrases of the Greeks, nor did he attempt to establish systems founded upon artificial arrangements. He watched the powers of Nature, he recalled the surgeon to the path of physic, he showed to him the effect of local disorders upon the constitution, and the reciprocal operation of constitutional disorders upon local diseases; he pointed out that the digestive organs may be affected by local disorder, and that upon the due functioning of these organs the health of man mainly depends. His object was to excite, by means of medicine, a more copious and healthy secretion.... 132To the knowledge of the necessity of great attention to the excretions, may chiefly be attributed the increased longevity of man, and his freedom from many of the diseases of former days.
Mr. Abernethy’s mode of pursuing his mercurial course [calomel and blue pill] was cautious and regular. He prescribed only small doses, taking care that the error so often fallen into, of increasing the quantity, when any benefit was perceptible, should be avoided.
His death occurred in 1831.
James Douglass, who was born in Scotland in 1675, died in London in 1742. During his residence in the English metropolis he practiced midwifery and taught anatomy. He was one of those exceptional men (like John Hunter, for example) who were able both to practice the art of medicine and to do a great deal of research work. Among other things he interested himself in the history of medicine and also took high rank as a botanist. The following list of the titles of some of his more important contributions to medical literature illustrate his great versatility:—“Myographiae comparatae Specimen,” or “a comparative description of all the muscles in a man and in a quadruped,” London, 1707; “Description of an Instrument for Extracting Teeth,” in the Philosophical Transactions, Vol. V.; “History of the Lateral Operation for Extracting the Stone by making a Wound near the Great Protuberance of the Os Ischii,” London, 1726; “A Description of the Peritonaeum and of that part of the membrana cellularis which lies on its outside, with an account of the true situation of the abdominal viscera,” London, 1730; “Appendix to the History of the Lateral Operation for the Stone,” London, 1731.
John Douglass, a younger brother of the preceding, also became celebrated as a surgeon. He lived in London, was connected with the Westminster Hospital, and attained special distinction through his having revived—after the lapse of nearly two centuries—the suprapubic operation for stone in the bladder (Pierre Franco’s “haut appareil”). His first operation of this nature was performed in 1719. John Douglass died in 1759.
His best-known published treatise bears the title: 133“Lithotomia Douglassiana,” or a “New Method,” etc., London, 1719.
Percival Pott was born at London on December 26, 1713. Four years later his father died, leaving his widow and son in possession of very scanty means. In 1729, when sixteen years of age, Percival was bound an apprentice to Mr. Nourse, one of the younger surgeons of St. Bartholomew’s Hospital and a lecturer on anatomy in a private medical school which he established in the heart of London. As it was Pott’s duty to prepare the subjects for demonstration he thus enjoyed unusual opportunities for grounding himself well in the knowledge of anatomy. At the same time, through his relationship with Mr. Nourse, he found unlimited opportunities in the hospital for witnessing surgical operations and for becoming thoroughly familiar with disease in its different forms. English surgery at this early period was very crude and unscientific, and—as will be readily understood—most painful. In his study of different surgical affections Pott followed the plan advocated by Lord Bacon, viz., to take up one subject or one region of the body at a time and to devote all his attention to that particular subject or region until he had exhausted all available sources of information relating to the subject.
In 1736, having finished his apprenticeship, he began at once making the necessary preparations for entering upon the practice of his profession. For his residence and place of business he rented an attractive-looking house in a good part of London, and took with him his mother and her daughter by her first husband. Thanks to the brilliancy of his talents, to an untiring industry and to an attractive personality and agreeable manners, he soon won for himself a considerable clientèle; while at the same time acquiring many friends among the most influential members of his own profession as well as among the élite of London society in general. These early friendships, says his biographer, proved to be permanent; indeed, it may be claimed that few physicians acquired and retained through life more firm or more respectable friends.
134In 1744 Pott was elected an Assistant Surgeon, and in 1749 one of the Principal Surgeons, of St. Bartholomew’s Hospital. From 1744 to 1787 he was unremitting in the surgical work which he performed in this institution. One of the most important services which he rendered to the science of medicine may justly be said to consist in the additions which he made to the scanty knowledge of that period concerning the nature and proper treatment of that disease of the spinal column which for many years has borne the name—in honor of this distinguished surgeon—of “Pott’s disease of the spine.” His first published memoir concerning the disease was published in 1779; but it was, as might be expected, only a preliminary sketch of the subject. Four years later he gave a complete description of this affection, the importance of which had for such a long period not been properly appreciated. In 1786 he received from the Royal College of Surgeons in Edinburgh a diploma accompanied by a letter expressive of the high degree of appreciation in which he was held by that institution. This honor was greatly enhanced by the fact that Pott was the first person on whom it had been conferred.
Pott’s biographer (Sir James Earle, Surgeon Extraordinary to the King) places the following estimate upon his character and upon his attainments as a surgeon:—
He was the most eminent of his time as a writer, as a teacher, and as a practitioner in surgery; and his merits in each of these characters were most extensive. Possessed with an enthusiastic love of excelling, without which genius is inert, he was not contented with any kind of mediocrity in himself.
As an author, his language is correct, strong and animated.... He introduces anatomy and physiology, whenever it is necessary, to illustrate and distinguish diseases; but never confuses his reader with uncertain hypotheses in pathology, founded on physiological principles. He was of opinion, and it is the opinion of Newton, that hypothesis has no place in any physical science.... His remedies always strongly marked his intention; they were decided and consistent; and he was the principal author of that simplicity which distinguishes the present practice from that of our ancestors....
As a teacher, he had acquired the faculty of speaking readily, 135with great point and energy, of delivering the most prolix and intricate sentences with incredible perspicuity and correctness, and of enforcing what he said with a most harmonious and expressive elocution....
As a practioner in surgery, we must apply to him all the essential qualifications—sound judgment, cool determination and great manual dexterity....
In the transaction of business there was a freedom and openness in his manner, which evidently arose from a consciousness that the opinion which he delivered was founded on experience.... This conduct in all situations was an appeal to the good sense of mankind. Thus he acquired the universal confidence of the profession; and, without any accidental or external help, he raised himself to the greatest dignity which man can attain—the first rank in a liberal profession.
Percival Pott wrote a treatise on the necessity of amputation in certain cases, and in this he strongly refutes the opinion of a Prussian army surgeon who maintained that in almost any case it was not necessary to amputate. The title of the treatise in which this opinion is expressed is “De membrorum amputatione rarissime administranda, aut quasi abroganda.” Shortly afterward Dr. Tissot, of Lausanne, Switzerland, spoke in even stronger terms against this surgical procedure, even going so far (see his treatise entitled “Sur l’inutilité de l’amputation des membres”) as to urge surgeons to abandon the “murderous and cruel method of amputation”—Pott’s criticism of the views expressed by these two writers is most charitable: “However, as we must suppose that the doctrine which these gentlemen have promulgated arose from humane motives, and upon a conviction of its being well founded, we must at least applaud their intention, though we cannot approve their judgment.”
Astley Cooper was born at Brooke, in Norfolk, England, August 23, 1768. As a boy he was fond of all the sports that are commonly cultivated at English schools, and even at that early age he manifested a bold and enterprising spirit, and yet at the same time he was noted for his social and friendly spirit. His biographer, Pettigrew, who witnessed many of the operations which Sir Astley performed 136at Guy’s Hospital in the earlier years of his career, speaks in strong terms concerning the impression which he made upon the regular pupils and the casual physicians who from time to time attended him on his rounds through the hospital:—
I can never forget the enthusiasm with which he entered upon the performance of any duty calculated to abridge human suffering. This enthusiasm, by the generosity of his character, his familiar manner, and the excellence of his temper, he imparted to all around him—the pupils imbibed the same spirit; and the extent of the obligations of the present and of after ages to Sir Astley Cooper, in thus forming able and spirited surgeons, can never be accurately estimated.
He was the idol of the Borough School—the pupils followed him in troops, and, like to Linnaeus, who has been described as proceeding upon his botanical excursions accompanied by hundreds of students, so may Sir Astley be depicted traversing the wards of the hospital with an equal number of pupils, listening with almost breathless anxiety to catch the observations which fell from his lips upon the several cases presented to his view. But, on the days of operation, this feeling was wound up to the highest pitch—the sight was altogether deeply interesting; the large theatre of Guy’s crowded to the ceiling—the profound silence obtained upon his entry—that person so manly and so truly imposing—and the awful feeling connected with the occasion—can never be forgotten by any of his pupils. The elegance of his operation—without the slightest affectation—all ease—all kindness to the patient, and equally solicitous that nothing should be hidden from the observation of the pupils—rapid in execution—masterly in manner—no hurry—no disorder—the most trifling minutiae attended to—the dressings generally applied by his own hand ... Sir Astley was, at that time (about 1805–1810), decidedly one of the first operators of the day, and this must be taken in its widest sense, for it is intended to include the planning of the operation, the precision and dexterity in the mode of its performance, and the readiness with which all difficulties were met and overcome.
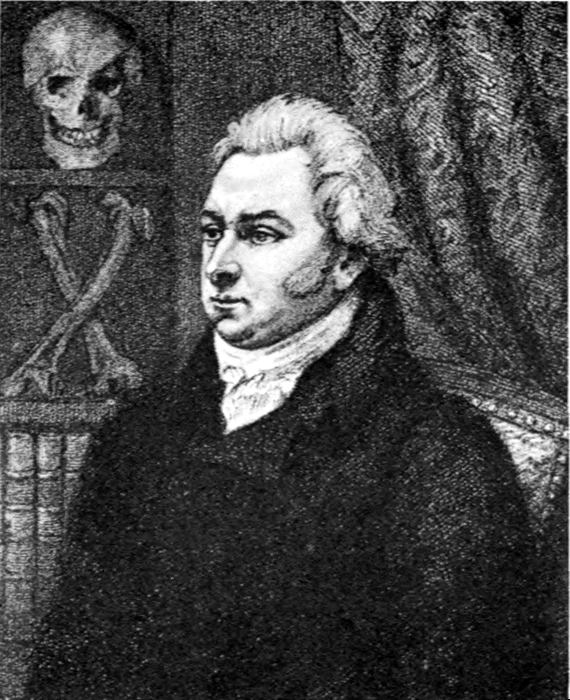
SIR ASTLEY COOPER
(Copied from a print in the possession of the New York Academy of Medicine.)
Among the contributions which Sir Astley made to the science of medicine the following deserve to receive special mention:—In 1798 he published the report of a remarkable case of strangulated hernia in which a part of the abdominal viscera was protruded into the left cavity of the chest, 137through an opening in the diaphragm. The viscera were much displaced from their natural situation, and the great arch of the colon, together with a large portion of the omentum, was pushed through the aperture in the diaphragm. The existence of this opening, which represented a congenital malformation, was first ascertained after death. It seems almost needless to add that, even if this unusual condition of the parts had been known during the patient’s lifetime, no possible means of relief could have been afforded.
Another of Sir Astley’s contributions—one, namely, which he published in 1804—deals with the subject of inguinal hernia, a topic concerning which very little was known before Cooper’s time. The Spanish surgeon, Gimbernat, had—it is true—published at a still earlier date a masterly description of the anatomy of the parts concerned in this form of hernia, but the fact had been entirely forgotten until Sir Astley called attention to its importance. Mr. Lawrence, the distinguished English surgeon, makes the statement (1806) that “no complete description and accurate delineation of even the common kinds of hernia, as the inguinal, femoral, and umbilical, existed previously to the late excellent works of Camper, Cooper, Scarpa, Hesselbach, Cloquet and Langenbeck.”
In Vol. I. of the Transactions of the Medico-Chirurgical Society (1808) will be found a report, by Sir Astley, of two cases of aneurism of the carotid artery. Pettigrew says that the first of these two cases was treated by ligature upon the vessel—the first of the kind on record, and establishing a practice which has since been pursued and successfully adopted. The second one of the two cases mentioned at the beginning of this paragraph—also a case of aneurism of the carotid—was treated by ligature and with a completely successful result. This patient lived until 1821, at which time Sir Astley published an account of the dissection made by him of the parts involved in the region of the earlier aneurism.
Sir Astley Cooper is the first surgeon to whom we are indebted for the performance of an operation designed to 138remedy in a measurable degree—in a few cases even to cure—the malformation known as Spina bifida, a condition which consists of a deficiency of the spinous processes of the vertebrae by which the theca enclosing the spinal marrow distends and protrudes to such a degree as to form a tumor, any opening into which has been commonly considered as necessarily attended by fatal effects. Sir Astley attributes the successful issue of the cases under his care to the employment of needles, and not the lancet, to discharge the fluid.
Many other instructive cases were reported by Sir Astley in later years, but the lack of space does not permit me to mention them here. It is enough for me to state that in his “Lectures on the Principles and Practice of Surgery” (published by Mr. F. Tyrrell, Surgeon of St. Thomas’s Hospital) very full details are furnished concerning all of Sir Astley’s operative work.
Among the honors conferred upon this distinguished surgeon during the later years of his life the following deserve to be mentioned: President of the College of Surgeons in 1827; Surgeon to the King in 1828; and Vice-President of the Royal Society in 1830. His income is said to have risen in 1813 to the very large sum of £21,000 ($105,000). His death occurred in 1841.
ENGLISH LEADERS IN MEDICINE AND SURGERY DURING THE EIGHTEENTH AND EARLY NINETEENTH CENTURIES
Second Group: William and John Hunter and Sir Benjamin Brodie My information concerning the Hunter Brothers is based upon data which I found in Pettigrew’s “Medical Portrait Gallery,” Parkinson’s “Hunterian Reminiscences,” and a few other published documents.
William Hunter, the elder of the two brothers who attained such marked distinction in the world of medicine during the eighteenth century, was born in 1718 in the west of Scotland. During his early manhood he devoted his attention to the study of theology at the College of Glasgow; but, losing soon his interest in these studies, he turned his attention to medicine, a branch of science which he found much more congenial. His advance in this new field of labor was rapid, for already at the age of twenty-eight he was invited by a society of naval surgeons to deliver a course of lectures on operative surgery. Two years later (in 1748) he became connected with the Middlesex Hospital and the British Lying-in Hospital, and from that time forward his chief interest was centred in obstetrics. Rising rapidly in public favor it was not long before he acquired a large fortune. In 1764 he became Physician Extraordinary to Queen Charlotte, and in 1768 was appointed Professor of Anatomy in the Royal Academy.
His greatest work, which was begun in 1751 and published in 1783, bears the title: “An Anatomical Description of the Human Gravid Uterus and its Contents.” Pettigrew speaks 140of this work, which eventually comprised thirty-four plates (drawn from Hunter’s dissections and engraved by some of the best English engravers),
as one of the most splendid medical works ever published. It is not, perhaps too much to say that the engravings have never been surpassed.... A period of thirty years was necessary, to obtain sufficient instances to develop all the changes occurring in the human uterus during the progress of gestation.... The treatise upon this subject was intended to be a separate production; but Dr. Hunter did not live to publish it. It remained for his nephew, Dr. Baillie, to submit this to the profession, which he did in 1794, as an “Anatomical Description of the Gravid Uterus and its Contents.”
One of Dr. Hunter’s cherished ideas was to establish in London an anatomical school upon a most extensive scale; for, strange as it must now appear, no regular courses of anatomy were given prior to 1746, and as a consequence surgery and physiology made but slow advancement. As a first step toward the realization of his pet scheme he submitted a memorial to the Earl of Bute, the First Lord of the Treasury, setting forth the great need of such a school, and furnishing with the memorial a suitable plan for establishing a museum in which the necessary instruction might be carried on. The memorial and accompanying plan were submitted to the King, but the proposal eventually fell to the ground. In view of the lack of interest manifested by the Government, Hunter decided to devote his own fortune and the collections which he had gathered up to that time to the establishment of the contemplated school. Accordingly he purchased an extensive piece of property and built upon it a large cabinet or institute in which every facility was provided for anatomical work: laboratories, amphitheatre, etc. In his will a provision was made that this institute with all its equipment should remain in London until thirty years had elapsed from the date of his death, and then it should be transferred to Glasgow. His death occurred on March 30, 1783.
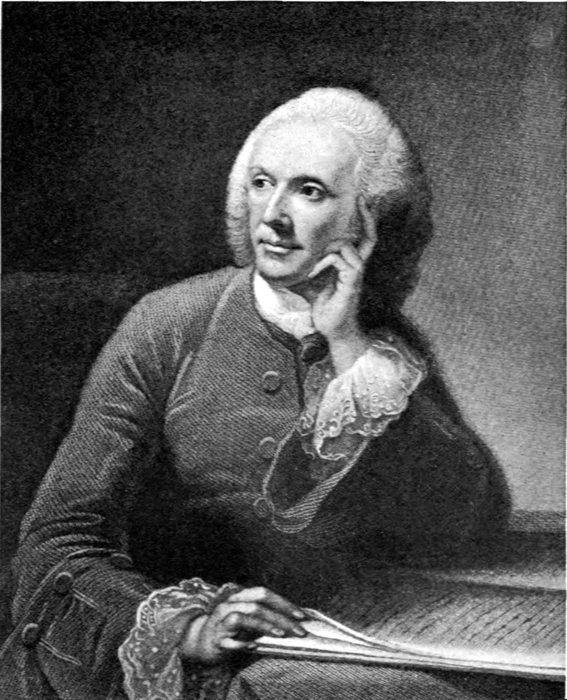
WILLIAM HUNTER
(Copied from Thomas J. Pettigrew’s “Medical Portrait Gallery,” Fisher & Son, London, 1838. The original portrait was painted by Pyne; the engraving was done by J. Thomson.)
The institute which Dr. William Hunter founded was “for the improvement of anatomical knowledge, surgery and 141physics,” and it may therefore with justice be claimed that Dr. William Hunter was the founder of the anatomical schools of Great Britain upon a rational and extended plan. His nephew, Dr. Baillie, speaks of him as a teacher and scientific worker in the following terms:—
No one ever possessed more enthusiasm for his art, more persevering industry, more acuteness of investigation, more perspicuity of expression, or, indeed, a greater share of natural eloquence. He excelled very much any lecturer whom I have ever heard, in the clearness of his arrangement, the aptness of his illustrations, and the elegance of his diction. He was, perhaps, the best teacher of anatomy that ever lived.
John Hunter, who was born July 14, 1728, was the youngest member of this large family of children, and, as a natural result, his early education was greatly neglected. Then, as a further misfortune, he lost his father by death before he himself had attained his eleventh year. Although he was regularly sent to school he did little else, up to the age of twenty, but waste his time. Then, bored to death by the aimless sort of life he was leading, and learning about this time what a fine reputation his brother William was building up through the work that he was doing in London, he asked him by letter whether he could not give him some regular occupation in his laboratory, stating, at the same time, that if he could not do this, he (John) would immediately enlist as a soldier. William wrote to his brother to come on to London and he would see what he could do for him. Immediately after John’s arrival in the great metropolis he was given anatomical work to do, and, to the astonishment of his brother William, he soon displayed such a remarkable degree of skill as a dissector that there could no longer be any reasonable doubt about his ability to gain eminence in this line of work; and so he was encouraged to give it a full trial. William took special pains to point out to his brother the best technical methods of procedure, and in every possible manner aided him in his efforts to advance. Thus, for example, he gained admission for him to Oxford University, and in due time obtained opportunities for him 142to witness the operative work of the leading surgeons in several of the London hospitals. With the lapse of time, during the following years John became more and more closely associated with his brother in his different activities,—lecturing in his place whenever he was called away by other matters of importance, making those beautiful anatomical specimens which even to-day are such a striking feature of the Hunter Museum in London, and guiding the students in their work of dissecting. But the field in which he displayed a tireless activity, and in which up to the very end he gained the greatest personal satisfaction from his labors, was that of comparative anatomy and experimental physiology and pathology. It was in this field that he performed the largest amount of original work, and almost always with a view to learning how the different classes of animals were equipped for the performance of one and the same function. About the year 1761 his health began to give way and he was obliged to spend nearly two years in efforts to regain it. With this object in view, he accepted the position of surgeon in the army, and during the period covered by the years 1761 and 1762 visited Belle-Isle, on the west coast of France, and also Portugal. On his return to England with improved health he resumed work on the anatomy of the uterus and especially on the lymphatics of that organ, and made not a few actual discoveries in this his new field. This work was conducted by him with great zest, and as a result he soon began to be the recipient of honors from different scientific societies. He was made a member of the Royal Society of London, and associate of the Society of London Surgeons and also of several German and French scientific societies, and Attending Surgeon of St. George’s Hospital, Surgeon Extraordinary to the King, Surgeon-General of the English Army, etc. In 1783 he experienced his first attack of angina pectoris, and these attacks continued to occur with increasing frequency until the final one, which ended his life on October 16, 1793.
In his biographical notice of John Hunter, Odier quotes Lavater, the famous physiognomist, as saying—after he had gazed for a few moments on Hunter’s portrait: “This man 143is accustomed to do his own thinking.” Lavater’s judgment, adds Dezeimeris, is amply justified by the facts. “No matter what was the subject upon which he wrote—whether surgery, medicine or physiology—he always added to it a certain measure of originality. In reading his writings one is constantly tempted to question the correctness of the opinion which one may have previously formed with regard to the particular subject under consideration, and it is in this respect—viz., by suggesting thought—that Hunter rendered very great services to his art. And yet, at the same time, it is precisely in his writings that the evidences of neglect in his early education stand out in the strongest relief; a neglect which showed itself most conspicuously in incorrectness, obscurity and slovenliness of style.” (Dezeimeris.) This critic adds that ample proof of the correctness of this judgment may be found in Hunter’s treatise “On the Blood and Inflammation,”—a book which is “full of grand and beautiful ideas that are literally choked in a chaos of conflicting conceptions, unfinished phrases, new words or words used in a sense different from that in which they are commonly employed.” I should add here, however, that the fault of which the biographer last quoted complains appears to be entirely absent in certain of Hunter’s reports of cases, as for instance in that which contains the account of a fractured thigh. At the same time it must be admitted that the physician who presumably prepared this report from notes which he took when Hunter delivered the lectures upon which the report is based, may have so edited the text as completely to eliminate the objectionable features. In our ignorance of the exact truth, it is more agreeable to assume that, in this particular instance, the lecturer revealed his ability to avoid entirely the faults to which the critic refers and to set forth the facts and his accompanying comments with perfect clearness.
Here follows the report as it is printed in the “Hunterian Reminiscences”:—
Granulation is not always confined to a breach of the solids by suppuration; for parts are capable of making new animal matter 144internally, in cases where it ought to have been healed by the first intention. What gave me the first idea of this was the following case, and the appearance observed on dissection, as exhibited in the preparation of the parts.
Case.—I was called to a man with a fractured thigh, and employed the usual means, but without success, for no union of the fractured parts was formed in the usual time; and at about the end of four weeks the man died with some other complaint. Upon examination of the parts I found that the upper end of the bone rode considerably over the under, and, consequently, there was a great cavity in the soft parts, the parietes of which were thickened by the adhesive inflammation, though not so much as if the parts had been better disposed for the adhesive inflammation. There was no extravasated blood, nor matter, nor coagulable lymph, to be found, except a few threads, which probably were the remains of some extravasated blood. Here the parts had lost two chances of being united, the one by the extravasated blood, the other by the coagulable lymph thrown out by the adhesive inflammation; and nature had here begun a third, which was that of forming granulations of new animal matter on the ends of the bones, and the surface of the surrounding cavity; and adhesions, you see, have taken place between the bones and soft parts, by which the bones would have been united by bony case: hence we find that granulation may take place without suppuration. This mode of union by granulation is much more extensive, I believe, than has been imagined; this third bond of union taking place when the parts have missed the first and second, as just mentioned. In the exposure of cavities of abscesses we have granulations going on hand in hand, and following suppuration. As the suppurative inflammation follows injuries with exposure, it seems that this inflammation is in general necessary to granulation in these cases. Granulation is an accretion of new animal matter, the old vessels being extended, and new ones formed, the vessels passing from one edge of the surface toward the other. Granulations are always of the same nature with the part on which they are formed: if that is diseased, as with any specific disease, so are they also. The granulating surface is convex, and covered with prominent points; the colour is of a deep florid red, but, when unhealthy, is of a livid colour, which, perhaps, may be produced by the circulation through them being exceedingly slow; this change of colour may also be an effect of difference of position.
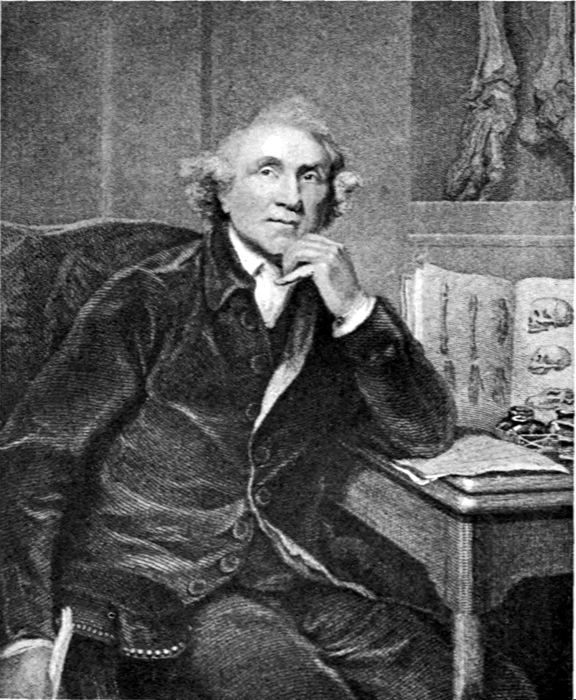
JOHN HUNTER
(Copied from Thomas J. Pettigrew’s “Medical Portrait Gallery,” London, 1838. The original portrait was painted by Sir Joshua Reynolds; the engraving was done by G. H. Adcock.)
Hunter’s biographer in the “New International Encyclopaedia” 145speaks of him as a man of great industry, the boldest and best operating surgeon of his day as well as the greatest anatomist known and a marvelous zoölogist.
Some idea of the intensity of Hunter’s devotion to the cause of science may be obtained from a perusal of the following incident, which is related in A. M. W. Stirling’s “Coke of Norfolk and His Friends”:[17]
Epping Place may be said to have been the centre of his [Coke’s] operations; and there was in these days a celebrated Irish giant O’Brien or O’Bryne who came to live there solely for the sake of joining Mr. Coke’s hounds whenever he allowed himself any recreation. O’Brien was eight feet high in 1780 and apparently went on growing, for in 1782 he measured two inches more and after his death in 1783 he was found to measure eight feet four inches, yet no other member of his family was unusually tall. He was crazy about hunting and became so attached to Jones, Mr. Coke’s huntsman, that he paid the latter a visit at Holkam and was there solemnly introduced by Jones to Mr. Coke and his guests. O’Brien’s end was curious. With extreme simplicity he invested all his property in a single banknote of seven hundred pounds which, needless to say, he lost; and grief at his loss combined with excessive drinking brought about his death. John Hunter, the celebrated surgeon, was extremely anxious to secure his skeleton; and learning that the giant was dying he set his men to watch the house in order to be sure of getting the body. O’Brien hearing of this, and having a horror of being dissected, left orders that his corpse should be watched night and day until a lead coffin could be made, in which it was to be conveyed to the Downs and sunk in twenty fathoms of water. O’Brien died, and his body started for the Nee, escorted by a walking wake of thirty Irishmen who drank deeply en route. Howison, Hunter’s man, who watched closely, informed the surgeon when he might catch the bodyguard off duty at the public house, and Hunter went thither to bribe them. He offered fifty guineas to one of the men to allow the body to be kidnapped, and the man consented on his own account, but said that 146he must first consult with his companions, who, perceiving Hunter’s eagerness, raised their price, first to one hundred pounds and finally to five hundred before they would agree. Hunter borrowed the money to pay them, and the coffin consequently went on its way filled with stones, while the body of the dead giant journeyed back to London in a spring cart, until John Hunter’s own carriage met it, after dark, and drove it to his house in Earl’s Court. There, for fear of detection, he did not dare to dissect it; but, separating the flesh from the bones by boiling and cutting, he quickly skeletonized it. Hence in the Museum of the Royal College of Surgeons may be seen, to-day, the skeleton—brown from boiling—of the giant whose greatest joy when living was a gallop with Mr. Coke’s hounds and the friendship of Mr. Coke’s huntsman.
At the time of Hunter’s death, his museum contained 10,563 specimens and preparations illustrative of human and comparative anatomy, physiology, pathology and natural history. He died, however, in comparative poverty, and his collection was purchased, two years after his death, by the Government for £15,000 and was presented to the Royal College of Surgeons.
John Hunter, says Pettigrew, had some very good ideas regarding the educational training of the pupils who placed themselves under his guidance. One of these is revealed in his practice of receiving certain pupils into his house. In this way several of England’s most distinguished physicians came to be, for varying periods of time, inmates of his home, and among this number—to mention only a single instance—was Dr. Jenner, the inventor of vaccination. One or more physicians from the United States—if I am rightly informed—also enjoyed this privilege. Valuable as this practice must have been to those who were thus given the opportunity of frequent informal intercourse with a most inspiring master, it certainly could not have been an easy matter, even in those more primitive days, to fit these pupils into the régime of the teacher’s home life; and, under the conditions of modern life, the arrangement would certainly prove impracticable.
Benjamin Collins Brodie was born at Milford, near Salisbury, England, on June 9, 1783. In 1803, when he was 147twenty years of age, he became Sir Everard Home’s pupil at St. George’s Hospital, London. Two years later he began to assist Mr. Wilson in teaching anatomy, and during the following four years he filled the position of Demonstrator of Anatomy. In 1808, a year and a half before he began private practice, he was appointed assistant to Sir Everard Home at St. George’s Hospital, and retained the position up to the time (1822) when he was appointed full surgeon at that institution. About six months after Mr. Brodie received his appointment as Assistant Surgeon, he began lecturing on surgery and continued giving instruction on this subject up to 1830. In addition, he gave clinical lectures regularly to large classes, and this most important part of his work, which he began in 1813, was kept up by him through a long period of years. In 1819 he was appointed Professor of Anatomy and Surgery to the Royal College of Surgeons, a position which he held until 1823. In that year, upon the death of Sir Everard Home, he was appointed one of the Serjeant-Surgeons to the King. Two years later a baronetcy was conferred upon him, an honor which gave him the right to be addressed as Sir Benjamin Brodie.
In the history of medicine one can find only a few instances of men who were very clever surgeons and at the same time highly gifted physiologists. A study of the life and writings of Sir Benjamin Brodie reveals clearly that he is a conspicuous instance of this kind. The very limited space at my command does not permit me to furnish more than a few incomplete proofs of the truth of what I have just stated. Such are, for example, the following:—
In 1810 Sir Benjamin Brodie delivered the Croonian lecture before the Royal Society, the subject chosen being “On some Physiological Researches respecting the Influence of the Brain on the Action of the Heart, and on the Generation of Animal Heat.” His experiments, according to the account given by his biographer, “go to show that if respiration can be maintained, even artificially, the heart will continue to contract with strength and frequency, even though the spinal cord be divided from the brain.” Sir 148Brodie contrived an apparatus to effect this, and at the same time carefully noted the circumstances connected with the secretion of the urine, which in these experiments was found to be suppressed. The conclusions he has drawn from this inquiry, conducted with great precision and detailed with equal perspicuity, are the following:—
1. The influence of the brain is not directly necessary to the action of the heart.
2. When the brain is injured or removed, the action of the heart ceases, only because respiration is under its influence; and if under these circumstances respiration is artificially produced, the circulation will still continue.
3. When the influence of the brain is cut off, the secretion of urine appears to cease, and no heat is generated; notwithstanding the functions of respiration and the circulation of the blood continue to be performed, and the usual changes in the appearance of the blood are produced in the lungs.
4. When the air respired is colder than the natural temperature of the animal, the effect of respiration is not to generate, but to diminish animal heat.
In 1811 Sir Benjamin Brodie reported to the Royal Society the results of various experiments which he made on the different modes in which death is produced by certain vegetable poisons (for example, alcohol; the essential oil of bitter almonds; the juice of the leaves of aconite; the infusion of tobacco; the empyreumatic oil of tobacco; the curare; etc.). During the following year he reported to the same society the results of a similar series of experiments which he made upon the effects produced by certain mineral poisons (for example, arsenic, muriate of barytes, tartar emetic, and corrosive sublimate).
The preceding brief references to the experimental work carried on by Sir Benjamin Brodie must suffice to show how thoroughly he deserved to be ranked as one of the leading English experimental physiologists of his day.
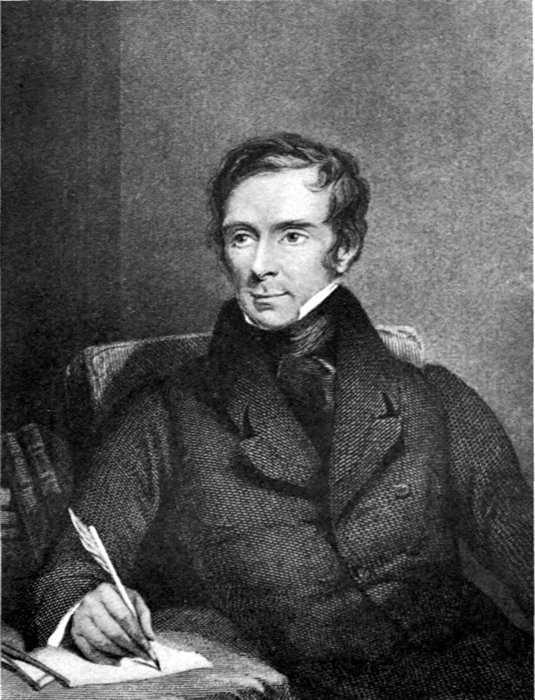
SIR BENJAMIN COLLINS BRODIE, BART., F.R.S.
Sergeant Surgeon to the Queen
(Copied from Thomas J. Pettigrew’s “Medical Portrait Gallery,” London, 1838. The original portrait was painted by H. Room; the engraving was done by J. Brain.)
Among Sir Benjamin Brodie’s contributions to the science of surgery are many that may be classed as of the first importance. Such, for example, are his researches respecting the diseases of the joints; his remarks on a case 149of ununited fracture of the femur, in the course of which he praises the method of treatment first proposed by Dr. Physick of Philadelphia; his observations on the treatment of varicose veins of the legs; pathological and surgical observations relating to injuries of the brain—a contribution of very great value; and pathological and surgical observations on the diseases of the joints. The latter treatise, which already, in 1836, had reached its fourth edition, is mentioned by his biographer as “a book which must ever form an essential part of the library of every surgeon.”
Like all his predecessors who have given instruction in the art of surgery, from John Hunter to Desault, Sir Benjamin Brodie laid great stress upon the importance of an intimate knowledge of anatomy and physiology—of the inseparable connection of these branches of science, and of the interest derivable from a contemplation of the organization and functions of animal bodies, the laws which regulate the phenomena of life and the changes which matter undergoes, and the form which it assumes when associated with this mysterious and active principle.... “He believes them to be incapable of explanation, except on the hypothesis of there being in living bodies something superadded to organization, without which, he says, ‘they would be as incapable of executing their functions as the pendulum of a clock would be of vibrating, or its wheels of revolving, if they were deprived of the spring or weight, in which the cause of their motion resides.’” (Pettigrew.)
The matters referred to above are only a few of those which Sir Benjamin Brodie has discussed in so instructive a manner in the numerous short essays and larger treatises which he published between the years 1809 and 1837. His death occurred in 1862.
Among the contemporaries of Sir Benjamin Brodie there were several London surgeons who, by reason of the important parts which they played in building up this branch of the science and art of medicine, fully deserve such consideration in the present review as my limited space will permit, and also as the sources of information upon which I am forced to depend for guidance may or may not prove helpful. Most fortunately for me at this juncture of affairs was the finding—among the rich treasures of the Medical Library of the former Transylvania University, at Lexington, Kentucky—of Professor Roux’s account of a visit which he made to the English metropolis in 1814 for the purpose of learning at first hand precisely how the English surgeons of that day were dealing with the more important problems which they were called upon to solve. A more competent and fair-minded authority than Dr. Roux could scarcely have been found at that time for the task which he set before himself. In the first place he was himself an eminent surgeon, in fact the Professor of Anatomy, Physiology and Surgery at the Faculté de Médecine of Paris, and at the same time he was wholly free from the animosity which most naturally pervaded a large part of the French nation in 1814 (just before the battle of Waterloo). And the very best evidence that he performed his judicial task to the entire satisfaction of the medical men of Great Britain is to be found in the fact that an English translation of his elaborate report reached a second edition in 1816. I therefore feel confident that, in basing my résumé 151largely upon Dr. Roux’s report regarding the condition of English surgery in the second decade of the nineteenth century, I shall not go far astray from the truth.
In his review of past events in the broad domain of surgery Roux says that the English attribute the first idea of the circular amputation of limbs to Cheselden, whereas the French give the credit for this operation to J. L. Petit. Then there are other operations which were devised or revived simultaneously by English and French surgeons—as, for example, in external aneurism, the tying of the diseased artery above the tumor (Desault and John Hunter), and the operation for Fistula in ano—an operation which was brought to the greatest degree of simplicity by Pott, Desault and some others.
On the other hand, there are many operations which were devised or perfected exclusively by French surgeons—for example, the method of extracting the crystalline lens, by Daviel; the treatment of fistula lachrymalis by dilating the nasal canal; the treatment of strangulated hernia by Goursand, Pipelet, Louis and others; the lateral operation (perinaeal) for removal of a calculus in the bladder; the operation of Frère Jacques; hypogastric lithotomy by Pierre Franco, and perfected by Frère Côme; etc.
The English surgeons may similarly claim priority in proposing certain operations, as for example, that of perforation of the os unguis for establishing an artificial passage for the tears, by Woolhouse; Cheselden created the operation of the artificial pupil; he is also to be credited with the operation of perforating the duct of Steno, on the inside of the mouth and some distance from its natural orifice, for the relief of salivary fistula; Pott’s description of and treatment for what is known as Pott’s disease of the spine; etc.
Then, passing from what may be termed the history of ancient English surgery, Roux devotes his attention next to the work which was being done, at the time of his visit to London, by some of the leading surgeons of that city; and among his most striking brief comments I find the following: “There are many able surgeons in London at 152the present time”; and “The English seem to have a strong taste for surgery.” Farther on, he discusses at greater length the reasons why the English surgeons maintain such pleasant relations with one another, and notes with pleasure how greatly the prevalence of such professional harmony conduces to the general advancement of the science and art of surgery—or, for that matter, to the advancement of any art or science. His words read as follows:—
If anything can contribute to keep alive the taste for an art or science, to extend its progress, and to make a greater number of men excel in it, is it not that those who cultivate it should live in perfect intelligence together; that they should compose one family; that they have frequent meetings with one another, in which each one, sacrificing his own private interest, brings, without pride or without presumption, the fruit of his own reflections; that, strangers to the arts of intrigue, and, never giving their minds to the vile insinuations of envy, they should rival one another only in zeal and knowledge? Well, this fraternal spirit, this absence of all jealous rivalry; and more, an ardent desire to communicate, reciprocally, their views, their thoughts, exists in a very high degree amongst the men who are at this moment the honour of medicine and surgery at London. This is what I have observed by being amongst them, I will not say with surprise, but with the highest satisfaction. To these common sentiments is joined, on the part of those men already advanced in their career, an esteem altogether peculiar, for those whose reputation is but beginning; and, on the part of the latter, the greatest regard, the most sincere respect for those who were their masters.
At this point I beg to remind my readers that effective surgical anaesthesia had not yet at that early period been discovered, and this fact, I scarcely need to add, must have deterred many men from undertaking some of the more serious surgical operations.
At the end of Roux’s account he sums up the results of his observations of English surgery in the following words:—
If I must conclude by a summary opinion, I would say that, with respect to the art of surgery, as with respect to its habits and institutions; in whatever light we consider it, England is the place 153for contrasts. By the side of the most brilliant features, English surgery exhibits glaring imperfections—French surgery is more generally good.
While we are now considering various matters relating to the condition of surgery in England and her colonies during the early part of the nineteenth century, it may not seem out of place to mention here a discovery which was announced just about that time, and which, I suspect, is known to-day to comparatively few American physicians. During the eighteenth century the opinion was widely held that gonorrhoea is simply one of the manifestations of syphilis and that consequently mercury is required for its cure. The existence of such a belief among the physicians of that day explains the following statement which I find printed in Vol. I. of the Quarterly Journal of Foreign Medicine and Surgery for 1818:—“Dr. Francis Balfour, a physician highly esteemed in Calcutta, states that when he was a student in Edinburgh he attempted to establish the idea that gonorrhoea is a disease distinct from syphilis and does not require mercury for its cure. He put forward this doctrine in a paper which he presented to the Medical Society of Edinburgh, and which still, we believe, graces its records. This was as early as the year 1766. Next year he made it the subject of his inaugural dissertation.... It was nearly twenty years after this period that Benjamin Bell, by his ingenious and able investigations, supported and further confirmed the opinion, and thus contributed much to bring it into public notoriety and favour.”
At the time of Dr. Roux’s visit to London Charles Bell, who had taken up his residence in that city in 1804, was already well advanced on the high road to distinction as a surgeon. Born at Edinburgh, Scotland, in 1774, he had attained considerable reputation as an anatomist and physiologist by the publication (1798–1800) (in association with his brother, John Bell) of a very useful “System of Dissection of the Human Body,” in which he describes not only the normal conditions but also the alterations produced 154by disease. The text is interspersed with instructive remarks concerning human physiology. Particularly clear and interesting—says his biographer—are the descriptions which Bell gives of the structure of the heart and blood-vessels. He refutes in strong terms the teachings of Hunter regarding the vital force of the blood and the doctrine of Crawford with regard to animal heat; and “his explanation of the physiology of respiration is the clearest and most satisfactory of any of the accounts that are to be found in the textbooks.”
In the domain of experimental physiology Charles Bell discovered, at a later date, that, in the case of certain nerve trunks (e.g., the trigeminus), what appeared to be a single nerve was in reality made up of two entirely different (physiologically speaking) nerves, one of which is now termed the portio major, while the other bears the name of portio minor. Bell also demonstrated experimentally the important law that the anterior roots of the spinal cord nerves are the outgoing (centrifugal) motor nerves, the posterior the incoming (centripetal) sensible nerves. These results were subsequently fully confirmed by the great German physiologist, Johannes Mueller. In ancient times the question was often discussed whether one and the same nerve might not carry both sensory and motor impulses. The discovery just mentioned is one of the most important ever made in physiology.
Great as was the reputation attained by Charles Bell as an experimental physiologist,—a reputation which won for him the honor of knighthood on the accession of William IV. to the throne,—he soon, as was predicted by Roux, became one of the most celebrated surgeons of London. His work as an operator was carried on chiefly at the Middlesex Hospital. Roux speaks of him as a “graceful operator without being affected.”
As an author he should be credited with the following treatises:—“Anatomy of Expression” (1806); “System of Operative Surgery”; “Animal Mechanics” (1828); “Nervous System” (1830).

SIR CHARLES BELL
(Copied from a print in the possession of the New York Academy of Medicine.)
Sir Charles Bell’s death occurred in 1842.
155Sir Charles Bell’s older brother, John Bell, born at Edinburgh in 1763, was also a distinguished anatomist and surgeon. After traveling for a short time in Russia and the north of Europe he returned to Edinburgh in 1786 and began to deliver lectures on surgery and midwifery. From this time forward his private practice as a consulting and operating surgeon steadily increased, until finally, in 1796, he was obliged to discontinue his lectures and devote his entire time to his patients and to the preparation of the several publications of which he was the author. Early in 1816 he was thrown by a spirited horse, and was so seriously injured that he never entirely recovered from the effects of the accident. His death occurred in 1820.
Among the works which he published the following deserve to receive special mention: “The Anatomy of the Human Body” (1793–1802), in the third edition of which work (1811) are to be found a number of plates that were drawn by his brother, Charles Bell; “Engravings of the Bones, Muscles and Joints,” drawn and engraved by himself (1794); “The Principles of Surgery” (1801–1808); and “Letters on Professional Character.”
Speaking of the second volume of the first-mentioned work (“The Anatomy,” etc.) Sprengel, the author of an important German history of medicine, says: “It is remarkable in two respects, viz., for the unusual number of interesting facts which it contains and also for the marked excellence of the plates that accompany the text.”
BORDEU AND BICHAT; THE BEGINNING OF EXPERIMENTAL PHYSIOLOGY AND EXPERIMENTAL PATHOLOGY IN FRANCE
Théophile Bordeu was born at Iseste, in the region of the Pyrenees, on February 22, 1722. He received his preparatory education at the College of the Jesuits, in Pau. Later, he entered the Medical School at Montpellier, and received his doctor’s degree from that institution in 1744. After graduation he devoted much of his time to giving instruction in anatomy, believing, as he did, in Seneca’s motto—“Doceo ut Discam” (I teach in order that I may learn). Notwithstanding the demands made upon his time by his private practice and by his numerous other engagements (inspection of the mineral springs in the neighboring region, courses of lectures to midwives, etc.) he managed to accomplish considerable research work, and one of the first fruits of these original studies is to be found in a mémoire which he wrote on the articulations of the bones of the face. This treatise, which he sent to the Académie Royale des Sciences, was received with marked favor, as shown by the facts that it was published by that body in their Recueil des Savans Étrangers and that its author was elected a Corresponding Member. In this treatise Bordeu calls attention to the fact that all the bones which form the background of the face are arranged in such a manner as to offer efficient resistance to the repeated upward impulses of the lower jaw, which impulses, acting upon the superior dental arch, have a constant tendency to push upward or to drive apart outwardly the bones into which the teeth of this arch are implanted. To appreciate fully the very creditable character of this essay the reader must remember 160that Bordeu had not yet reached his thirtieth year and that the ideas which he sets forth in this essay are the strict product of his own thinking and anatomical researches.
In 1752 Bordeu moved to Paris, and soon afterward published one of his best contributions to the science of medicine, viz., a monograph entitled: “Recherches Anatomiques sur la Position des Glandes, et sur leur Action.” The publication of this important and exhaustive mémoire occurred so soon after its author reached Paris that one is justified in assuming that all or the greater part of the research work upon which the essay is based was carried on at Montpellier. The object aimed at by Bordeu in this mémoire was to prove that
“the secretions which issue from these glandular organs represent a veritable elaboration of the liquid the elements of which are supplied by the blood, and are not merely a simple separation, as the term ‘secretion’ would seem to imply. This function,” says Bordeu, “is the result of the activities belonging properly to the gland as an organ, and does not in any sense—as some would have us believe—represent a mere mechanical relationship between the blood-vessels of the gland and the volume of the globules (blood corpuscles) that are carried into the organ through them. Nor does the function represent in the slightest degree the result of a chemical affinity between the fluid product secreted and the substance of the gland. Furthermore, the excretion (i.e., the expulsion) of this fluid product is due wholly to the vital action of the glandular organ; for it is a well-known fact that the adjacent muscles and organs occupy such positions in relation to the glands themselves that they are quite powerless to compress them and thus to favor expulsion of the fluid which they have secreted. Indeed, their influence is of quite the contrary character; instead of compressing these organs in the manner claimed they do no more than to communicate to them from time to time such trifling shocks and movements as favor their glandular activity.... Modern physiologists have added nothing of importance to what Bordeu has set forth in this mémoire, which deserves to be looked upon as one of the finest monuments that has ever been erected in honor of the science of man.” (Richerand.)
Bordeu’s mémoire, it seems, created a great sensation among the physicians of Paris, many of whom were still at 161that period ardent supporters of the mechanical and chemical doctrines taught by Boerhaave; and, as a matter of course, there was also unbounded curiosity among the better-educated physicians of the capital to see and make the acquaintance of the newcomer—this “young athlete,” as Richerand calls him,—who had not feared to enter the lists against such a formidable array of adversaries. The marked popularity that fell to Bordeu’s lot as a private practitioner in Paris after this brilliant beginning was not, however, of long continuance. Professional jealousy rarely fails to develop promptly when a physician manifests his ability to win patients from those of his colleagues who, for a certain number of years, have been established in practice, and this is precisely what happened in Bordeu’s case. The new mémoires which he published during the succeeding years—one on the pulse (in 1756), a second on “Metallic Colic” (in 1761–1763), a third on the “Colic of Poitou” (a year or two later), and a fourth on the “History of Medicine” (in 1768)—showed unmistakable evidences of the great talents which he possessed, but they attracted comparatively little attention and did not add to his popularity as a private practitioner. Furthermore, he derived very little if any material advantage from his appointment as one of the attending physicians at La Charité hospital.
The last two years of his relatively short life were attended with not a little suffering from attacks of gout, which compelled him to give up his private practice and to live exclusively upon the scant income which he derived from the small fortune (80,000 francs—$16,000) that represented his savings from a practice that had apparently been quite successful. His death occurred from cerebral apoplexy on November 23, 1776, when he was not quite fifty-four years old.
Bordeu did not live to see the ultimate triumph of his ideas with regard to the true nature of the secretions supplied by glands. The careful consideration of what this author has written upon the applications of the accessory sciences (chemistry and mechanics) to physiology should put us on our guard, says Richerand, against drawing incorrect 162conclusions with reference to the nature of vital processes.

BICHAT
Marie François-Xavier Bichat was born on November 11, 1771, at Thoirette, France, in the Department of the Jura. His father, who was a practicing physician at the neighboring town of Poncin, and who at the same time held the office of mayor, was a man of considerable cultivation. Cherishing, as he did, the hope that his son might eventually adopt medicine as his vocation, he planned the latter’s education with special reference to this possibility; and, as medicine proved to be the very vocation which the son preferred, all this well-planned training counted as so much valuable time gained. François, who showed himself to be an apt scholar, made most satisfactory progress in all the prescribed studies of early boyhood, and after passing creditably through the regular course of the Collège de Nantua, a thriving town among the western foot-hills of the Jura range of mountains, he began the study of medicine at Lyons, in 1791. At first he devoted himself almost exclusively to anatomy and surgery. Marc-Antoine Petit, the celebrated surgeon of the Hôtel-Dieu of Lyons, was his teacher in these branches of medical science, and from the very first took special pains to aid his pupil in his studies in every possible manner. François manifested an unusual degree of interest in anatomy, a branch of medical science to which at that period only those who had the intention of practicing surgery paid any attention; and in addition he developed, almost at the very start, a strong disposition to learn the precise purpose of each tissue and organ as it was encountered in the course of his dissections. In other words, François-Xavier Bichat was already, at the early age of twenty, making original investigations in the department of physiology. This fact, says his biographer, should be classed as something very remarkable, for, at the period which we are now considering, practically not one of the students of medicine was giving any thought except to the wonderful surgical work that had been accomplished, a few years earlier, by the famous Parisian surgeon, J. L. Petit 163(1674–1750), by F. de Lapeyronie of Montpellier (1678–1747), by S. F. Morand of Paris (1697–1793), by the famous lithotomist, Frère Côme (1703–1781), of whose achievements I gave a brief account in “The Growth of Medicine,” and by another celebrated teacher of surgery in Paris, viz., Pierre-Joseph Desault, who, during the period which we are now considering occupied by far the most conspicuous position among the men classed as healers of disease, and who, by the very prominence of his position, compelled almost everybody who took any interest in medicine to keep their eyes riveted on him. These and other circumstances that happened to exist at that period strongly favored among the younger men a leaning toward the career of surgeon. One of these favoring circumstances was the need of army surgeons, for France was in the throes of the French Revolution. It was therefore not strange that at first Bichat devoted the greater part of his time and thought to the fundamental work of a surgeon’s training. A little later he accepted a subordinate position at the Hôtel-Dieu of Lyons, under Marc-Antoine Petit, the head surgeon of that great hospital. Favored in every legitimate way by this eminent and most kindly surgeon, young Bichat made rapid progress. But there arrived a time, shortly after the siege of Lyons, when it was no longer safe for a young man to remain in Lyons, and so Bichat was forced to flee to Paris. There he joined the crowd of students who were regularly following the practical instruction given by Desault.
It was at that time an established custom in the medical school for certain pupils, who had been previously selected for this work, to read (in turn) to the assembled group of students, just before the arrival of the attending surgeon, a résumé of the previous day’s lecture. In this way the man whose turn it was to read the résumé which he had prepared, secured a most valuable bit of training, and those who simply listened were afforded an excellent opportunity for refreshing their memories with regard to the lecture of the previous day. On these occasions the First Assistant was always present and was therefore in a position to 164report to his Chief just how successfully each reader of such a review had performed the duty assigned to him. At one of his lectures Desault entered more elaborately than usual into a description of his manner of treating fracture of the clavicle, demonstrating among other things the proper manner of applying what has since become known as “Desault’s bandage.” The student who had been assigned to the duty of preparing a résumé of that day’s lecture happened to be absent on that particular occasion, and so the First Assistant asked the members of the class whether perhaps one of their number would be willing to act as a substitute. Bichat volunteered his services, and he thereupon prepared a résumé which, when read on the following day, proved to be so clearly expressed and covered the ground so thoroughly that the class, after listening to it in profound silence, expressed its approval by the most pronounced applause. When Desault was told by his First Assistant, Manouty, of what had happened he was very impatient to make Bichat’s acquaintance; and, after he had talked with the latter for a short time, he became so impressed with the extent of the knowledge which he had already acquired, with his earnestness of purpose, and with his amiability of character, that he did not hesitate to invite him to become one of his household. Indeed, the favorable impression which Bichat made upon him led him promptly to decide that, if nothing happened later to change the impression which he had first received, he would do all in his power to make this young man his successor.
This kindly reception on the part of his honored preceptor made a deep and most cheering impression on Bichat and stimulated him to put forth his best powers to justify the confidence shown by Desault. At the latter’s request he took charge of part of Desault’s private practice, and he also accepted the position of Hospital Attending Physician to the Outside Poor. Furthermore, he acted as Desault’s corresponding secretary, answering for him all the requests for advice that came to him from every district of France. Then, in addition, he assisted him in all his operations in private practice. Finally, as if he were not already burdened 165to the limit of his strength with all this mass of work, he not infrequently spent a portion of the night in aiding Desault to solve various problems in experimental surgery, problems relating chiefly to diseases of the bones. Whenever a lull occurred in this series of engrossing labors he devoted all the available time to the performance of operations upon the cadaver and to experiments in relation to physiological problems that suggested themselves to his own mind.
Already as early as in 1797—that is, when he was twenty-six years of age—Bichat gave his first course in anatomy. The room in which the instruction was given was quite small, for he was confident that only a few pupils would feel disposed to subscribe for such a course, and in addition no provision for laboratory work had been made. At first, the teaching was limited to simple demonstrations, but very soon discussions with regard to physiological questions began to occupy some of the time of the sessions. Finally, Bichat found it desirable now and then to carry out experiments on living animals, in order to verify certain seemingly well-known facts and also to determine the exact points at which new investigations should be instituted. When this first course in anatomy came to an end he surprised his friends by beginning a course on operative surgery. “I wish,” he remarked to one of his intimates, “to demonstrate that even a young man may be quite as capable as one of mature age, to operate with the requisite degree of precision.” The course proved a great success, and demonstrated perfectly the truth of his statement.
Under all this strain upon his vital energy, it soon began to be apparent that Bichat’s health was giving way, and it was not long before a pulmonary or bronchial hemorrhage forced him to desist from his work. At one time, indeed, his physical condition was such as to make his friends fear for his life. In the course of a few months, however, he seemed to regain his health; and then he forthwith made arrangements for a much more complete course in anatomy than that which he had carried through so successfully the year before. A laboratory provided with accommodations 166for eighty dissectors was constructed, and, before the course began, every one of these eighty seats was engaged. (This was in 1798.)
It was a great source of amazement to his friends—and it continues to be a great source of amazement to the physicians of the present day—how Bichat managed to accomplish successfully such a number of things as he, at this early period of his life and with a decidedly precarious state of health, had taken in hand.
One thing was now very noticeable, namely, that he was devoting a much larger part of his time and attention to experimental physiology—that is, to the phenomena and the laws of life—than he had hitherto done to anatomy. After he had finished the work which belonged properly to the daylight hours he devoted no small portion of the nighttime to the work of revising the writings of his beloved teacher and friend, Desault.
Among the anatomical structures about which almost nothing was known toward the end of the eighteenth century, but of which the structure and functions were fully exposed to light by Bichat’s labors, the synovial membranes deserve to receive the very first mention. His researches concerning these membranes were first made known in the public lectures which he was giving at that time to the medical students, but they did not appear in print until a later date, viz., in the second volume of the “Recueil de la Société Médicale d’Émulation.”
At a somewhat later period Bichat abandoned all further attempts to cultivate either the knowledge or the practice of surgery, and concentrated all his efforts upon the extension of our knowledge of the principles of physiology. He made very careful researches into the nature and functions of serous membranes, and published the results of his labors in a volume which met with great favor at the hands of a large part of the medical profession, and yet at the same time brought out strong manifestations of envy on the part of other physicians. As Buisson justly remarks, these manifestations of envy furnished the very best sort of 167proof that Bichat, who paid no attention whatever to these criticisms, had done his work remarkably well.[18]
In the same year (1800) Bichat published a third treatise, under the title “Recherches Physiologiques sur la Vie et la Mort.” (A later edition appeared in 1805.)
One day, as Bichat was descending the main staircase of Hôtel-Dieu, his foot slipped and he fell in such a manner as to strike his head with considerable force against one of the steps. When somebody came to his assistance it was found that he was unconscious. In a short time, however, consciousness returned, and Bichat was able, though with some difficulty, to regain his home. On the following day he suffered from a severe headache, but insisted, nevertheless, on making a few professional calls. The exhaustion which he felt after making these visits compelled him to take to his bed as soon as he reached his residence. Death took place on the fourteenth day after the occurrence of the accident; that is, on July 22, 1802.
Bonaparte, who was at that time First Consul of the French Republic, gave orders, upon hearing the news of Bichat’s death, that a monument should be erected in the vestibule of Hôtel-Dieu to commemorate the distinguished services rendered to humanity in that institution by Desault and Bichat. The following is the inscription which it bears:—
Ce marbre dédié a la Mémoire des Citoyens Desault et Bichat a été posé pour attester la reconnaissance de leur contemporains, pour les services qu’ils ont rendus, le premier à la Chirurgie Française dont il est le restaurateur, le second à la Médecine qu’il a enrichée de plusieurs ouvrages utiles, et dont il eût aggrandi le domaine si l’impitoyable mort ne l’eût frappé dans sa 31me année.[19]
168Aside from his scientific attainments and from his untiring zeal in prosecuting his researches in anatomy and physiology, Bichat possessed certain traits of character which caused him to be greatly beloved by his pupils. He was of a very kindly disposition, and it was not an easy matter to excite him to anger or even to cause him to show impatience.
The first feeble beginnings of experimental physiology are to be credited to the Swiss physician, Albrecht von Haller, whose death occurred in 1777. Then followed, a few years later, the more serious efforts that were made in the same field of scientific inquiry by John Hunter, of England. The real birth of this new science, however, took place in France, under the fostering care of Lavoisier, Bichat, Magendie and others. The establishment in Paris, by Bichat, of a large laboratory where such research work could be carried on advantageously, constituted the first act in the creation of an organized experimental physiology. Several years later (1867), Claude Bernard induced Monsieur Duruy, who was at that time Minister of Public Instruction in France, to establish at the Jardin des Plantes a laboratory where general physiology might be studied experimentally.
TYPES OF FRENCH PHYSICIANS WHO FLOURISHED ABOUT THE TIME OF THE REIGN OF TERROR
Louis-Guillaume Lemonnier, member of the Academy of the Sciences and First Physician of the King (Louis XV. and also Louis XVI.), was born at Paris, June 27, 1717. His father and his brother were both of them members of the Academy, the former in his character of Professor of Physics at Harcourt, and the latter as one of the most celebrated astronomers of France. At the age of twenty-two he was sent (1739), with Carsini de Thury and Lacaille, to the south of France to extend the meridian of the Observatory of Paris, the task of making scientific observations along the route followed by his superior associates being specially assigned to him. He noted the existence of mines of ochre, coal, iron, antimony and amethysts in Auvergne, of mineral waters in Mont-d’Or, and of mines of iron in Roussillon. He also made analyses of the mineral waters of Barèges, and determined the poisonous nature of certain species of mushrooms. In the same year he received the appointment of Physician to the Hospital at St. Germain-en-Laye, near Paris.
During this period of his career Lemonnier made the acquaintance of an expert floral gardener by the name of Richard, and in his company soon developed a keen interest in flowers and garden plants. The Duke of Ayen, who was one of the King’s favorites and well known for his love of flowers as well as for his boldness of speech in telling the truth to the royal household, made frequent visits to Richard’s garden and in this way acquired a friendship for Lemonnier, who entertained him greatly with his talks about botanical matters and about the cultivation of trees. 172As a result the Duke’s extensive park in time became the home of rare plants and numerous species of noble trees, many of which were still flourishing during Cuvier’s time. After a while Louis XV. was induced by the Duke to accompany him on some of his visits to Richard’s garden, and on one of these occasions the King asked that Lemonnier should be introduced to him, as he wished to become acquainted with the man who had so successfully aided the Duke in establishing an attractive botanical garden. At this first interview Lemonnier made a most favorable impression upon the King,—so favorable, indeed, that the latter, after a few further interviews had taken place, placed this physician and enthusiastic botanist in charge of the botanical garden at the Trianon, in Versailles; and not long afterward he appointed him his First Physician, a position which carried with it a liberal salary. Cuvier, in accounting for the enthusiastic love for botany which develops in certain men, makes the following remarks:—
In our dealing with plants nothing of a painful nature is encountered; no sad images are ever presented to our eyes; there is absolutely nothing to recall to our minds our passions, our disappointments, our misfortunes; love is never associated with jealousy, beauty exists without vanity, force is never accompanied by tyranny, and death takes place without agony; in brief, there is nothing to remind one of the human species.
The only use that Lemonnier made of his pleasant relationship with the King was to secure his sanction of the plan of sending competent botanists to different parts of the globe with instructions to bring or send back rare plants, first to the Trianon garden at Versailles and, after the death of Louis XV. (in 1774), to the Jardin du Roi (Jardin des Plantes) at Paris. In accordance with this scheme men were despatched to Persia, to the coasts and islands of the Mediterranean, to the banks of the Euphrates, to Cayenne in South America, to the Atlas Mountains, to Liban, to China and to the East Indies.
Costume worn by Paris physicians in the eighteenth century.
(From Alfred Franklin’s “La Vie Privée d’Autrefois,” Paris, 1892.)
As Lemonnier was not in the habit of publishing anything on botanical subjects, he was comparatively unknown to the public. Were it not for this fact, says Cuvier, he would 173easily have taken rank among the most celebrated botanists of France. When his friends chided him for having neglected to avail himself of this mode of obtaining well-earned recognition he replied that the time spent in instructing others is lost so far as his own self-instruction is concerned. Furthermore, he was timid in regard to publishing. “There is sure to be a great deal of unjust criticism about anything a man may write, and I cannot easily bear such injustice. I therefore prefer to keep silence.”
Upon the death of Louis XV. Lemonnier lost his position of First Physician to the King and he was not reappointed by Louis XVI. until 1788. Thus, during a period of fourteen years, he was deprived of the large salary which is attached to that position, and was obliged to live upon the relatively small income which he derived from private practice. During the continuance of his official connection with the Court he invariably refused to accept any fees from those individuals who belonged to the Court circle but yet held no official position. On the other hand, he was most generous in giving the best of his service, gratis, to the poor. As a consequence, his popularity among the lower classes was very great. He reaped the reward for this disinterestedness on the occasion when the mob, in 1792, invaded Versailles and carried off the King and Marie Antoinette to Paris. As soon as the palace was vacated Lemonnier sought safety in one of the small pavilions in the adjoining park; but the rabble broke into the building and were carrying off Lemonnier as a prisoner when suddenly a man, who seemed to be one of the leaders of the mob, stepped out from the crowd and ordered the physician to follow him. Thus Lemonnier was conducted to his room in the Luxembourg palace in Paris, all the time under the guidance of this strange, rough-looking man, who nevertheless, when they arrived at the Luxembourg, acknowledged to the doctor that he intended, from the very first, to save his life if he possibly could, because he was sure, “from the kindly and venerable expression of his countenance, that he could not possibly have had anything to do with the abuses of which the rabble complained so bitterly.” Thus was Lemonnier 174rewarded for all his past services to the poor of Paris and Versailles.
During the last years of his life—he was eighty-two years old when he died—he enjoyed, in the quiet society of his former friends, who stood by him faithfully to the end, what he termed the happiest years of his life.
Charles Louis Dumas, born at Lyons, France, on February 8, 1765, was the son of a practicing surgeon. At the age of seventeen he began the study of medicine at Montpellier, Barthez and Grimaud being at that time the most distinguished members of the Medical Faculty of that university. From the very first he manifested a keen interest in his studies. In 1785 he received the degree of Doctor of Medicine, the title of his graduating thesis being: “An Essay on Life, or the Vital Faculties.” In 1787 he visited Paris, and during the following two years devoted his attention chiefly to chemistry and to the study of human anatomy. It was during this period that he became warmly attached to Vicq-d’Azyr.
In 1790 he returned to Montpellier and took part in a competition for the chair of surgery left vacant by the death of Sabatier. Although the judges decided in favor of another competitor they were most favorably impressed with the talents which Dumas exhibited. A year later, upon the death of Barthélemy Vigaroux, Dumas accepted the position of Vice-Professor of Surgery in the same university, but, owing to the political troubles which developed at this time in Lyons, he was obliged to resign his chair at the end of one year and return to his native city. After the termination of the siege of Lyons he was expelled from the city, narrowly escaping with his life. In 1793 all teaching of medicine at the University of Montpellier ceased, and two years later a new school of medicine was organized, and the duty of teaching anatomy and physiology was assigned to Dumas. In 1798 he was chosen President of the school and Dean of the Faculty of Medicine of Montpellier. He died on March 28, 1813, at the early age of forty-seven.
The more important of the treatises written and published 175by Dumas are the following:—“Principes de Physiologie,” Paris, 1800–1803, 4 vols., and “Doctrine Générale des Maladies Chroniques, etc.,” Montpellier, 1812, and a second edition (2 vols.) in 1824.
Pierre-Jean-Georges Cabanis was born June 5, 1757, at the village of Conac, in the Department of Corrèze, France. During his early youth he gave no evidence whatever of possessing an inclination to study, but at the age of fourteen he was taken to Paris, and then, for the first time, he manifested great eagerness to acquire all kinds of knowledge. After having completed his preliminary course of literary training he accepted the position of private secretary to Prince Massalsky, Bishop of Wilna, and accompanied him on his return to Poland. A residence of two years in that distracted country convinced him, however, that he had better return to France and seek there for an opening to some useful career. Accordingly he went to Paris, and, upon learning that a prize for a French translation, in verse, of a part of Homer’s Iliad had been offered by the Académie Française, he devoted all his time and energy to the writing of such a translation. Richerand, from whose eulogy on Cabanis I have derived most of the information furnished in the present sketch, does not state whether these efforts were or were not rewarded by the capture of the coveted prize. His account, however, makes it perfectly clear that Cabanis was an enthusiastic admirer of the poetry of Homer and that he would gladly have devoted his life to the cultivation of literature if he had not, at the same time, been deeply impressed with the idea that a good citizen should devote a large share of his time and his talents to things of real use to his fellow men and to his native or adopted country. Accordingly, in due course of time, he set aside his purely literary employment and began in earnest the study of medicine, to which vocation he now transferred his allegiance with all the ardor of which he was capable. Hippocrates, whose accurate descriptions of disease and whose high standard of professional duty excited his admiration as much as had the writings of 176Homer, furnished him with the first models that were to serve as guides in his newly chosen career. To add to his good fortune he had the privilege of studying medicine under the guidance of Dubreuil, a teacher of the very highest order, a philosopher, and a man of whom the pupil always spoke in strong terms of admiration and affection.
After taking his doctor’s degree in 1784 Cabanis devoted all his energies, during the few years which elapsed between this event and the breaking out of the French Revolution, to the practice of his profession. Aside from these duties he accepted only one official responsibility, viz., that of Administrator of the Hospitals of Paris, and this duty he performed with entire success. It is a fact worth noting that he was one of Mirabeau’s intimate friends, and he believed thoroughly in the principles of the French Revolution, but he did not approve of the excesses which characterized its progress.
Some idea of the importance of the position which Cabanis held in the esteem of his associates in the Parisian world of science and politics may be gained from the following statements:—Early in his career he was introduced by Turgot, the former Controller-General, to Madame Helvétius, the widow of the well-known littérateur, Claude Adrien Helvétius, and a woman whose weekly receptions (salons) brought together at frequent intervals some of the most famous men at that time residing in Paris. Thus he became acquainted with Franklin and Jefferson, of the United States, as well as with Diderot and d’Alembert, the famous writers connected with the French Encyclopædia. He was also presented to Voltaire, who received him in the most kindly manner. Although from 1789 to the end of his life he published a number of useful pamphlets on different topics connected with public affairs and especially with public charitable institutions and undertakings, he rarely permitted his name to appear as the author of such essays. In 1799, when the Consulate was entrusted with the government of France, Cabanis accepted a seat in the Senate and took an active interest in public questions. During the last three years of his life the increasingly bad state of his 177health did not permit him to do much work of any kind; and finally, on May 6, 1808, an attack of cerebral apoplexy put an end to his life.
The two most important works published by Cabanis are the following:—“Rapports du Physique et du Moral de l’Homme,” Paris, 1802 (2d edition in 1805); and “Du Degré de Certitude de la Médecine,” Paris, 1797 (3d edition in 1819).
Félix Vicq-d’Azyr, who was born in 1748, was distinguished chiefly as an anatomist and physiologist, and also as a writer on scientific topics. The Faculty of Paris, not being pleased with his rapid advance in popular favor, refused to allow him the privilege of lecturing in their anatomical theatre. Then Antoine Petit, who was at that time Professor of Anatomy at the “Jardin du Roi,”—an institution which was located in what is now known as the Jardin des Plantes and was in a limited sense a rival of the École de Médecine,—befriended him and did everything in his power to make him successor to himself in the Chair of Anatomy. In this attempt, however, Petit failed, for Portal, whose candidacy was backed by the more influential Buffon, eventually received the appointment. Just at this juncture of affairs Vicq-d’Azyr met with a stroke of good luck. A niece of the celebrated naturalist, Daubenton, who spent a large part of his long life in work connected with the Jardin du Roi, happened one day to have a fainting fit just as she was passing in front of Vicq-d’Azyr’s residence. This physician, who chanced to be at home when the fainting occurred, did everything in his power to restore the lady to consciousness; and in this he was perfectly successful. In fact, not many months elapsed before they were married; and from this time forward Daubenton did everything in his power to advance Vicq-d’Azyr’s career as a scientist. He aided him, for example, in procuring a great variety of foreign animals which the latter needed for his researches in comparative anatomy; and, in addition, he promoted his candidacy for membership in the Académie des Sciences, to which organization he received an election 178in 1774. Soon afterward he gained the esteem and friendship of Lassonne, the First Physician of the King, and through his influence Vicq-d’Azyr was commissioned to carry assistance to the people living in certain districts of France where an epidemic disease was raging. Later, Lassonne aided him in organizing the Société Royale de Médecine, the function of which was to perfect all the departments of medical activity. Eventually Vicq-d’Azyr was made Secrétaire Perpetuel of this society. The Faculty, as had happened before under similar circumstances, showed itself jealous of this new organization, and systematically did all in its power to undermine the influence of Vicq-d’Azyr, whom it recognized as the guiding spirit of the scheme. Despite these malicious efforts the public at large, recognizing their origin and the mean spirit of jealousy which prompted them, lost no opportunity of bestowing praise upon Vicq-d’Azyr. In 1788 the Académie Française chose him as Buffon’s successor, and in 1789 he succeeded Lassonne as the First Physician of the Queen.
Vicq-d’Azyr’s purely scientific writings are very numerous and of marked importance. They cover a wide extent of subjects—medicine, anatomy (both human and comparative), and the veterinary art. His death occurred on June 25, 1794, from some acute affection of the chest.
The treatises and memoirs which he wrote were first published separately at different dates, but in 1805 a fairly complete collection was published at Paris by Moreau.
Jean-Noel Hallé, born at Paris, France, toward the end of the eighteenth century, was one of the most distinguished physicians of that period. Cuvier, the famous naturalist and the author of the biography upon which the present sketch is based, makes the following statement:—
Those physicians who can steer their way successfully through such a maze of difficulties as existed during the French Revolution, and who at the same time can inspire their patients with a feeling of entire confidence in their ability to bring them safely back to health, deserve our highest admiration and respect. But when we wish, in giving an account of a physician of this calibre, to furnish 179clear proofs of the truth of what we say, we find it exceedingly difficult to produce the necessary evidence. The names of three such men occur to me, viz., Hallé, Corvisart and Pinel.
In the further course of his narrative Cuvier states that, in his charitable gifts to the poor, Hallé studiously concealed from them the source of the aid which they received. Many a patient, he adds, upon his recovery from the attack for which the doctor had treated him, was astonished to find that all the expenses incurred during his illness had in some mysterious manner been defrayed. “How rarely indeed,” says Cuvier, “does one learn of such a perfect carrying out of the injunction: ‘Let not thy right hand know what thy left hand doeth.’”
About the year 1794 Hallé’s father and his grandfather were made members of the Order of Saint-Michael, an honor which conferred nobility not only upon them but also upon himself. Unfortunately for the doctor, who was residing in Paris at the time, this patent of nobility made him subject to the new law which had been passed by the Convention, and which drove into exile all members of the nobility. An exception, however, was made in his case because he held the office of Physician to the Poor, and also—doubtless—because he was universally known throughout Paris to be a staunch friend of the poor. Having thus received permission to remain in the capital Hallé at once bethought himself how he might aid those unfortunates who were confined in prison. He was permitted, for example, to visit Malesherbes, Minister Turbot’s associate, who was awaiting his death by the guillotine. Not only was he thus enabled to speak words of comfort to the unfortunate prisoner, but he received from him such farewell messages for his distressed family and friends as he desired to send. Hallé was also one of those friends of Lavoisier who interfered actively, but in vain, to save his life from the executioner’s block. Those were terrible times and it required great courage to do what Hallé did in behalf of these innocent victims of the murderous Jacobins.
Fourcroy, the celebrated chemist and naturalist, who was 180authorized by the Convention in 1794 and 1795 to organize a new École de Médecine, to take the place of the one which the rabble had destroyed in 1783, appointed Hallé Professor of Medical Physics and Hygiene. Then, later still (1796), Corvisart, who by that time was in the full exercise of his functions as medical adviser to Bonaparte,[20] appointed Hallé his associate in the professorship at the Collège de France. Shortly afterward he gave up the Chair entirely to Hallé.
Between the years 1800 and 1812 Hallé, more than any other French physician, exerted his influence—and with decided success—in overcoming the remaining opposition to vaccination, not only in France but also in Italy.
Corvisart left to Hallé in his will the portrait of Stoll, the distinguished Vienna professor, and added a memorandum to the effect that he made this gift because he esteemed Hallé more highly than he did any other physician.
Many anecdotes have been told concerning the peculiarities of Hallé in his dealings with patients. The following two may perhaps prove of interest to my readers:—If, for example, the patient happened to be an artist, Hallé refused to accept a fee from him; and, when asked why he did this, he replied: “Because from way back I belong to a family of artists.” Then, in the second place, he was not willing to accept fees from ecclesiastics. “If they have only just enough to live upon, they should not be subjected to any diminution of that small stipend. On the other hand, if they have more than is absolutely necessary for their legitimate living expenses, this excess belongs to the poor.” The following anecdote is told of one of his experiences:—
One day, when he returned to his office, worn out with a hard day’s practice, he was told that a lady was waiting to consult him. “Ask her,” he said to the attendant, “kindly to consult some other physician, as I am too tired to see her.” She sent back word that she had not the courage to do this, as she was not able to pay for the services of this other physician. “If that is the case,” Hallé promptly replied, “tell her I will see her.” To himself he said: “I have no right to send her away.”
181Hallé’s death occurred on February 11, 1822. Laënnec succeeded him at the Collège de France.
Gaspard Laurent Bayle was born on August 18, 1774, at the village of Vernet in the Department of the Basses-Alps. The country in this part of France is very picturesque but not at all fertile; lofty mountains surround it on all sides. At an early age Gaspard manifested a high degree of intelligence and a strong inclination to study natural phenomena. He was barely ten years old when he began making a collection of insects, and he even went so far as to give names to the individual species. He was only twelve years old when he was sent to the High School of Embrun; and in this institution he made such advances in his studies that the principal, Father Rossignol, a Jesuit, looked upon him as one of the most promising of the pupils under his charge; more than this, he felt a strong affection for the boy. As the curriculum of the school studies did not include mathematics and natural history Father Rossignol took particular pains to furnish Gaspard with instruction in these branches of knowledge. The warm friendship which thus developed between the scholar and his instructor, continued unbroken up to the time of the latter’s death in 1813.
Laboring under the impression that it was his duty to become a priest Gaspard enrolled his name at the theological seminary in 1790, and devoted the following year to the study of philosophy and theology; but, after the lapse of a certain length of time, doubts began to enter his mind as to the wisdom of the choice which he had made, and accordingly, after consultation with his father and older brother, both of whom were lawyers, he abandoned the study of theology and entered his brother’s law office.
In 1793, when the storms of the French Revolution had reached their acme of violence, young Bayle, who was then only nineteen years old, attended a political meeting at Embrun and made such a stirring appeal to the mountaineers there assembled, in regard to their duty as Republicans, that he completely won their confidence, and was accordingly chosen to represent them at the approaching 182reception of the Proconsuls Barras and Fréron, who had been sent by the Convention to persuade the inhabitants of that district to carry out the violent measures which had been planned against the city of Digne. The Proconsuls, who in the meantime had arrived at Digne, quickly discovered that public sentiment was not in favor of the measures advocated by the Convention; and accordingly, in the fear that an uprising of the citizens might imperil their own lives, they promptly fled from that city; but, before leaving, they made arrangements for the arrest of the young orator who had produced such a strongly antagonistic impression upon the people. As soon as Bayle’s father and brother had learned these facts they quickly took all the steps necessary for secretly getting Gaspard out of Digne and sending him as speedily as possible to Montpellier, where—by enrolling himself among the students of Medicine—they believed that he might reasonably expect to escape the clutches of Barras and Fréron. These measures proved successful, and thus Bayle’s life was saved and his attention diverted from the Law to Medicine, a career in which he was destined to gain great credit.
After spending three years at Montpellier Bayle was sent, as an Officier de Santé, to serve at a military hospital temporarily established at Nice, in the south of France. And here let me remark, parenthetically, that this title should not be translated by the corresponding English term “Health Officer.” In 1795 a new type of medical school was established in France, the object of this innovation being to provide a class of practitioners who could meet all the ordinary medical needs of the peasants at a charge considerably less than that demanded by the graduates of the high schools. The course in these new schools covered a period of only two years, and the graduates were classed as “Officiers de Santé.”

GASPARD LAURENT BAYLE
As Bayle’s duties here at Nice were not very exacting he divided the time which he had at his disposal between the bedside observation of cases of actual disease and the study of treatises relating to pathology. In 1798 he went to Paris and followed several courses of instruction, more particularly 183that given by Corvisart on pathological anatomy. In 1799, at a competitive examination, he won the position of Assistant in Anatomy, and from that time forward he devoted a large part of his time to the work of making post-mortem examinations.
In 1802 Bayle received his degree of Doctor of Medicine. The thesis which he wrote on this occasion created a great sensation, partly because it described an entirely new form of gangrene, and even more on account of the philosophic manner in which he defended all his statements when called upon to do so at the public cross-examination which, at all the foreign universities, commonly precedes the bestowal of the degree upon the candidate. Two of Bayle’s friends who were present on this occasion, secured shorthand notes of the discussion that took place between the candidate and the professors (Petit-Radel, Pinel, Alphonse Leroy and Percy) whose duty it was to question him with regard to the views put forward in the thesis. The report based upon these shorthand notes covers nine printed pages of the biographic sketch which lies before me, and is not—as will readily be appreciated by my readers—suitable for reproduction here in its entirety; nor would a digest of such a report serve any useful purpose. The most that seems to me permissible under the circumstances is to furnish here two or three brief extracts, from a perusal of which it will be possible to form at least some idea of the character of this cross-examination. It should be stated, however, by way of preface, that Professor Petit-Radel had, just before the discussion began, raised objections to Bayle’s failure, in his thesis, to include in his list of inflammatory affections “the whitish engorgements observed at times in different organs”; and he then added the following remark: “You are not disposed, I assume, to recognize the existence of Boerhaave’s ‘white inflammation.’”
(Here follows the first part of the stenographic report of the cross-examination.)
BAYLE: “If in the affection to which you refer the swelling is accompanied by pain, and if it terminates by undergoing resolution or by suppuration, then I should say that it bore some relationship 184to inflammation; but if there is neither redness, pain, fever, nor suppuration, I should declare that it possesses none of the characters which distinguish inflammatory affections, and that consequently this so-called ‘white inflammation’ should be considered by us as something imaginary. At the same time I should not like to have anybody get the impression, from what I have said, that I deny the existence of such things as white tumors or swellings, indolent in character, and either elastic or permitting the pressure of a finger to leave the mark called ‘pitting’; I simply wish to emphasize the fact that these affections do not manifest any of the characteristics of an inflammatory disturbance.”
PETIT-RADEL: “Do you not believe that there exist certain kinds of humors which possess the power of giving rise to a white variety of inflammation?”
BAYLE: “As I do not know what this ‘white inflammation’ really is, you must not expect me to entertain a clear idea of what its immediate causes are; and even if I were personally familiar with this type of ‘inflammation,’ it is more than likely that I would wander far from the truth if I were to attempt to define the particular kind of humor which causes this affection. It is easy to say that bile, or some other humor that possesses a sufficiently acrid character, is the exciting cause; and then I might print what I have to say on the subject in a beautiful book.[21] But of what use are all these hypothetical deductions; why resort to pure operations of the imagination when we seek to explain natural phenomena? Is it not better to say simply ‘I do not know’ than to erect a pompous edifice on a foundation of moving sand?”
PETIT-RADEL: “Very well, let us speak now of the treatment which you recommend. Was it a wise thing to prescribe bleeding and purgatives in the treatment of the gangrenous pustule which you describe in your thesis?” etc.

A candidate for the degree of “Doctor of Medicine” defending his thesis before the examining committee of the Paris Faculty of Medicine.
(From “La Vie Universitaire,” Paris, 1918.)
The remainder of the stenographic report is fully as interesting as the first part, but I do not feel warranted in omitting equally important text in order to find room for the report in its entirety. I will simply state that, before the cross-examination was completed, Bayle had boldly expressed the opinion that “there is nothing more harmful 185to the advance of practical medicine than the cultivation of the spirit of system.”
Not long after Bayle received his degree of M.D. he succeeded in obtaining, as the result of a competitive examination, one of the two positions of House Physician (“elève interne”) which existed at La Charité Hospital; and here, having at his disposal an extraordinary amount of valuable material both clinical and pathological, and being aided by the experienced guidance of Corvisart and Dumangin, he enjoyed for about two years the most extensive opportunity for self-culture which it is possible for a young physician—Bayle was only twenty-eight in 1802—to have placed at his disposal. Being very industrious and also extremely ambitious to excel he accumulated a great stock of knowledge concerning the different forms of disease to which human beings are subject. Not only did he store this knowledge up in the chambers of his mind, but he also kept written records of everything that seemed to possess value, for use at a later period of his life. This fact should be remembered, for those who have had occasion to consult the numerous treatises which Bayle has published, cannot have failed to wonder that he should have been able to furnish so many and so complete histories of cases that came under his personal observation. But alas! he failed to realize that this sort of work was sapping his strength, and he also seemed to ignore the fact that he was carrying within himself the seeds of a pulmonary disease which was sure sooner or later to put an end to his labors. Already as early as in August, 1804, he was seized with such a violent nostalgia, such an irresistible longing for his beloved mountains, that he was obliged to drop all work at La Charité and return to his home in the south of France. In addition to the nostalgia there were loss of flesh, insomnia and a sense of oppression in the chest. This change of scene, air and occupation proved rapidly beneficial, for, at the end of fifteen days, he felt much stronger and was able to sleep much more soundly than for many previous weeks. His morale, too, was markedly improved; his hunger for mountain scenery and air was now satisfied. Then, for several 186years after his return to Paris, he remained in comparatively good health, and was able to attend to an enormous amount of hospital and private practice, in addition to literary work. But in 1813 the threatening chest symptoms again compelled him to visit his beloved Alps and to spend several months with his wife and children in their mountain home. This time, however, the improvement in his health was much less pronounced than it was in 1804, and very soon he found that he would have to abandon all active work. His death took place on May 11, 1816, at the early age of forty-two.
According to the statement of Bayle’s biographer it was the unanimous opinion of all the physicians who had come in frequent contact with him during his professional career, especially in the course of his official work at La Charité, that no physician of equally varied and great attainments had previously been seen in Paris. Professors Chomel and Cayol, and the famous Laënnec maintained that this was not too great praise to bestow upon Bayle.
Of his published writings I shall mention here only a few of those which attained some celebrity, viz.: “Remarques sur les Tubercules,” in the Journal de Médecine, Chirurgie, et Pharmacie, tome 6, p. 1; tome 9, p. 427; and tome 10, p. 32.—“Traité des Maladies Cancéreuses,” 2 vols., Paris, 1833. (One of the earliest and certainly one of the most elaborate treatises on this subject that is to be found in the entire range of medical literature.)—“Mémoire sur l’oedème de la Glotte,” in the Dictionnaire des Sciences Médicales.
Jean-Nicolas Corvisart, who was born February 15, 1775, at Drécourt, a village in the Department of Ardennes, N. E. France, was destined by his father to follow in his footsteps, in the career of an attorney; but the son disliked the work more and more as time went on. Finally, he found an opportunity of attending one of the lectures of Antoine Petit, who was one of the most eloquent lecturers on anatomy in France during the eighteenth century. He was completely fascinated by what he heard, and at once determined 187that this was the only profession that he cared to adopt. Accordingly, during the next few months he made a practice of rising very early in the morning and finishing the clerical work which had been assigned to him in his father’s office; thus gaining time to attend the lectures of Petit, Louis, Desault and Vicq-d’Azyr. When the father discovered what his son had been doing he made up his mind that it would be useless to make any further attempts to keep him occupied with work calculated to fit him for the career of an attorney. Accordingly he allowed him to follow the regular course of studies prescribed for those who intended to become physicians. At that early date (about 1770), however, the regular medical course of training carried out by the Faculty of Medicine was most unsatisfactory. For example, the so-called regular course of lectures was not well adapted to form an adequate basis of education for the student of medicine, and, in addition, there was nothing that could be called clinical teaching. In short, the student was obliged to pick up the knowledge which he needed, in large measure by the exercise of his own wits. But Corvisart was both eager to learn and very persevering, and he possessed such a genius for picking out as his guides the very men who were best fitted for imparting useful knowledge, that he managed to make satisfactory advances despite all these obstacles. The instructors in whom he placed the greatest confidence were Desbois de Rochefort, Head Physician of La Charité Hospital, and Desault, Chief Surgeon of Hôtel-Dieu. These two men, says Cuvier, were the most distinguished medical men of their day in the art of curing disease. Desbois de Rochefort, for example, was the first of the Parisian physicians to give regular clinical instruction in the hospital with which he was connected, and Corvisart followed this instruction regularly throughout a period of several years. He was also present at most of the post-mortem examinations which took place during de Rochefort’s service; in fact, he took the very deepest interest in this part of the work. A prick of one of his fingers while he was dissecting caused an infection which nearly cost him his life. It was on this occasion 188that Desault, by his skill and by his untiring efforts to control the manifestations of the disease, rendered him splendid service.

CORVISART
(Copied from an old French print in the possession of the New York Academy of Medicine.)
Under such persistent and intelligent training it was not long before Corvisart was himself able to give courses of instruction in anatomy and physiology,—courses which rapidly became very popular with the students.
So far as dress was concerned, Molière succeeded in driving out of fashion the gown and pointed bonnet which the physicians of that day were still, in accordance with the custom of centuries, wearing; but he failed to induce them to abandon the wig which they were expected to wear when engaged in actual service in the hospital wards. This practice continued in force until Hallé and Corvisart both got themselves into trouble by refusing to wear a wig. In the case of Corvisart the following story is told:—A well-known Paris lady (Madame Necker) had just founded a fine hospital to which Corvisart hoped to be appointed the Physician-in-Chief. When he first appeared in one of the wards in his natural hair, the lady founder was much shocked, and declared positively that she was not willing to assume the responsibility of sanctioning any such novelty. Corvisart remained firm in his resolution and the position was given to another physician.
Compensation for this disappointment, says Cuvier, came to Corvisart soon afterward, in the following manner:—Père Potentine, the Superior of the monks connected with La Charité Hospital, had been struck with the faithful manner in which Corvisart had cared for the sick under his charge. So, when Desbois-Rochefort, the pioneer clinical teacher in Paris, died in 1788, he quickly determined that he would, if possible, secure for Corvisart the important position which had just been vacated. His efforts proved successful, and in a short time the new appointee was attracting to La Charité a large number of students who were just as appreciative of Corvisart’s clinical teachings as they had been of the instruction given by his predecessor.
A few years later still—in 1802—he was asked to see in consultation Bonaparte, who was suffering from an acute 189pulmonary attack; and on this occasion he had the good fortune not only to discover the real cause of the trouble but also to recommend the measures which resulted in curing the disease.
Despite his great success, both as a teacher and as a practitioner, Corvisart experienced his full share of professional disappointments, and was, in consequence, often very much depressed by them. He was wont to express in very plain terms his dislike for those treatises in which the author assigned to each disease a list of sharply defined characteristics, and which caused the reader to believe that the course which it pursued was invariably the same; which spoke of disease, in short, in such a manner as to convey to young men the impression that the science of medicine was one of the physical sciences, and that both diseases and the remedies to be employed might well be reduced to a comparatively few forms. No such simplicity exists in nature; the number of combinations is infinite, and each day the combination is likely to be completely changed. The numerous autopsies which he had made convinced Corvisart that similarly the internal changes vary just as greatly as do the external signs and symptoms.
The two most important treatises of which Corvisart was the author are his “Treatise on Diseases of the Heart” and his “Commentary on Auenbrugger’s Work.” Nowhere in medical literature, says Cuvier, will one find a more methodical or a more clearly written treatise on this subject than the first of these treatises. In the second one the author analyzes the different alterations in the lungs, bronchi and pleura which may be distinguished by means of Auenbrugger’s method. In the form which Corvisart has given to this second work we obtain the clearest evidence of his generous character. Rather than rob this man who had long been dead, and who was entirely unknown to him, of even a small portion of what was his due, Corvisart preferred—to use the expression employed by Cuvier—to immolate his own glory. It appears that before he had learned anything whatever about the work that Auenbrugger had published in 1763, he had himself made the majority of the 190discoveries set forth in that author’s treatise and was making preparations to publish them to the world. Just at this moment, however, he unexpectedly found a copy of a French translation of Auenbrugger’s dissertation, whereupon he abandoned his original plan and published instead the “Commentaries.” In his preface he gives the following explanation of the course which he adopted:—“I might have—if I had so wished—sacrificed the name of Auenbrugger to my own vanity; but my object is to revive the knowledge of his splendid and legitimate discovery.”
In 1789 Corvisart published the MSS. which Desbois de Rochefort had left to him as trustee. Already in 1788, as stated on a previous page, he had been appointed, by a unanimous vote, Physician to La Charité Hospital. From the very start he took up with enthusiasm the work of clinical instruction in this hospital, and kept it up for nearly twenty years, thus gaining for himself—according to Dupuytren—the reputation of being the leading medical practitioner of his day, and adding great distinction to French medicine. In 1795, when the first École de Médecine was created, he was made “Clinical Professor of Medicine”; and from this time forward, for a period of several years, he carried on the work of clinical teaching practically without a rival.
In addition to the positions which he held at l’École de Médecine and at La Charité Hospital Corvisart was connected in some teaching capacity with the Collège de France. At first he gave instruction in this institution only in the theory of medicine, but after 1795 he was formally installed in the College as a teacher of practical medicine; and from this time forward he was able so to arrange his lectures that those students who attended his clinical instruction at La Charité, would be able to hear him, later in the day, explain more fully the diagnosis, treatment, etc., which he had adopted in the morning. In his manner of conducting these sittings Corvisart was largely guided by Stoll’s “Aphorisms,” a practical work which combined the genius of Boerhaave and that of Stoll,—a work in which problems and demonstrated truth were most happily combined. 191Corvisart was so impressed with the value of this treatise (“Aphorisms”) that he published a translation of it in 1797.
As a lecturer Corvisart possessed an animated and sparkling style of delivery and great clearness of expression. When asked why he improvised these lectures before the students, instead of writing them out beforehand, he said: “In lecturing I like to feel absolutely at my ease and not to be under the restraint which one feels after a formal preparation beforehand.”
In the hospital it was his practice to submit to the students for inspection and consideration only the most serious and the most typical cases. From the bedside he went, in company with the entire class, to the amphitheatre, and there entered upon a more complete description and discussion of what they had witnessed in the ward. If the patient died, then he took them with him to the dead-house and showed them whatever the autopsy revealed. Before doing so, however, he read to them a brief history of the case, in order to refresh their memory. Then, after the autopsy had been completed, he reviewed and compared the two sets of facts. As the author of this particular eulogy remarks, “One can imagine with what intense interest the students followed this last act in the course of instruction which Corvisart gave them.”
When Bonaparte was made Emperor of France one of his early acts was to appoint Corvisart, who had been instrumental in effecting his recovery from a serious pulmonary attack, his First Physician. This position was not, as might easily be imagined, that of a mere personal adviser; it was a much more important office, or at least it became so in the hands of Dr. Corvisart. He felt very strongly that he must use this great increase in his personal influence, not for himself nor for his immediate circle of friends, but for the benefit of the nation and for the advancement of the science of medicine. As an illustration of the spirit in which Corvisart interpreted the attitude which he should maintain in the face of his new responsibilities I will mention the following incident:—On one occasion, when the Emperor 192startled him with the announcement that he held in his hands the official appointment of his brother to a position connected with the Government, Corvisart remarked: “Allow me, your Majesty, to decline, for my brother, this position; he does not possess the necessary capacity. I know that he is poor, but that is a matter which concerns only myself.” After Corvisart left the room Napoleon, turning to one of his ministers who happened to be present, asked him: “Do you know of many men like this man?” On another occasion, when Corvisart happened to be the subject of conversation, the Emperor remarked: “He is an honest and skilful man, but a little brusque.”
Among his numerous acts of generosity toward his friends and benefactors there were some which showed that he did not forget his teachers nor even the hospitals. He established at l’École de Médecine a prize fund which had for its purpose to aid those who found it impossible, through lack of funds, to continue their scientific experiments.
Finally, it should not be forgotten that it was Corvisart who suggested to Bonaparte,[22] the First Consul, the propriety of erecting at Hôtel-Dieu the monument in honor of Desault and Bichat. (See page 167.) By reason of the various responsibilities which very soon began to burden Corvisart he was obliged to give up, one after the other, his clinical teaching and finally his practice; it had become impossible for him to do justice to so many things. Thus, he resigned his Chair of Clinical Medicine in 1807, and in 1814, after the fall of Napoleon, he retired to his countryseat, where he hoped to regain in some measure the health which had begun to break down under the numerous burdens which he had been carrying. His death occurred on September 18, 1821.
From among the comments that were published by his contemporaries soon after Corvisart’s death I select the following as well adapted to complete the portrait of this remarkable man:—
Among his professional brethren Corvisart was admitted to have gained a high degree of skill in the power to diagnose 193diseases of the chest by means of percussion, and especially to have advanced our knowledge of affections of the heart and its annexes. No less important are the services which he rendered to physicians through his valuable and inspiriting clinical teaching. It was particularly in this form of teaching that he showed in what a rare degree he possessed the power of interesting his auditors in the case which happened to be at that moment under consideration. Corvisart was equally successful as a teacher of pathological anatomy, and nobody, since the time of Bichat, did more than he to develop in France the love of researches in pathological anatomy. However, despite their fascination with the study of the pathological lesions presented by the different organs of the body after death, these pupils rarely seemed anxious to harmonize them with the symptoms manifested by the patient during his lifetime. They persisted in forgetting the remarks made by their teacher on this very point, to wit:—
The most desirable thing, the thing which we should particularly strive to find out because it is that which is most important in practical medicine, is not what are the peculiarities discernible in the cadaver, but to recognize the existence of these pathological lesions from certain signs and symptoms manifested during life.
The only works which Corvisart has handed down to posterity are the following:—
“Essai sur les maladies et les lésions organiques du coeur et des gros vaisseaux,” Paris, 1806. (3d edition, 1818.)
“Nouvelle méthode pour reconnaître les maladies internes de la poitrine, par la percussion de cette cavité,” par Auenbrugger; ouvrage traduit du latin et commenté par J. N. Corvisart, Paris, 1808.
Corvisart’s comments constitute a large and important part of the book last mentioned, and virtually make of it an original work by Corvisart. Auenbrugger’s original treatise was published in 1763 and was then, according to Dezeimeris, entirely forgotten, notwithstanding the fact that in 1770 it was translated into French by Rozière de la Chassagne. Auenbrugger was the first physician who recognized 194the fact that, by percussion of the walls of the chest, a diagnosis may be made of some of the diseases affecting the organs contained therein. Corvisart practiced Auenbrugger’s percussion method during a period of twenty years and was in the habit of demonstrating it to the numerous students who attended his courses in clinical medicine. It was this long experience in the practice of percussion that enabled him to extend, correct and modify the method as it was set forth in Auenbrugger’s little treatise. If he had not done this and had not published the results in his French translation (of 1808), Auenbrugger would not have won the credit for his glorious discovery. The delicately considerate manner in which Corvisart engineered the whole scheme throws a flood of light upon the noble character of Napoleon’s First Physician.
LAËNNEC AND THE INVENTION OF THE MODERN METHOD OF AUSCULTATION; PAUL-JOSEPH BARTHEZ
René Théophile Hyacinthe Laënnec (1781–1826) was born at Quimper in Brittany, France. I am not able to furnish any details concerning his early history. His subsequent career as a physician, however, and especially his writings, show very clearly that he must have received a very careful and thorough education. Previous to 1816 auscultation of the chest was carried out in the same manner as it was in the time of Hippocrates,—that is, by applying the examiner’s ear, either directly or through an interposed piece of linen, to the surface of the skin overlying the particular part which he was desirous of examining.
In 1816 I was consulted [writes Laënnec] by a young woman who presented certain general symptoms that pointed to the existence of some disease of the heart, and in whom, by reason of her embonpoint, simple palpation and percussion could scarcely be expected to furnish satisfactory information in regard to the nature of the disorder. The age and sex of the patient not permitting me to make such an examination as I have just mentioned I was compelled to adopt some other measure; and I then recalled to mind the acoustic phenomenon with which everybody is familiar, to-wit: if the ear be applied to one end of a wooden beam it will perceive with perfect distinctness the sound made by the scratching of a pin’s point on the opposite end of the beam. From this circumstance I inferred that in the present case I might advantageously utilize the principle underlying this phenomenon. Accordingly I rolled up into a cylinder-shaped, stiff-walled tube several sheets of writing-paper, and, resting one end of the cylinder on the skin of the precordial region, I applied my ear to the other end of the tube. I found to my surprise and pleasure that I was now able to hear the 196pulsations of the heart much more distinctly than I had ever before heard them when I applied my ear directly to the chest-wall.
This first experience made such a deep impression on the mind of Laënnec that he promptly instituted a series of experiments which had for their object (1) the determination of the form of instrument that would best answer the desired purpose, and (2) the discovery of the various cardiac and pulmonary conditions that might advantageously be studied by the use of this instrument. Such were the first steps taken in one of the most useful medical discoveries of which we have any record. Auscultation, the importance of which had been dimly foreseen by Hippocrates the Great, became now for the first time, in the early part of the nineteenth century, one of the most effective aids to the physician in ascertaining the true nature and extent of certain diseases located in the cavity of the chest, in watching their progress, and in regulating their treatment in accordance with the physical conditions revealed by the aid of the method. The history of medicine has few more important events to record than this discovery made by Laënnec, one of France’s greatest physicians.
As a result of the experiments to which I have just referred there was soon substituted for the crude thin-walled paper cylinder a solid column of light wood, hollowed out centrally throughout its length by a narrow tubular channel. To this new instrument the name “stethoscope” was given. It would require too great an amount of space to give here the full and very explicit instructions supplied by Laënnec regarding the manner in which this instrument is to be employed in actual practice; and, furthermore, they are to be found in the best modern textbooks which deal with diseases of the chest.

LAËNNEC
(Copied from an old French print in the possession of the New York Academy of Medicine.)
Stethoscopic auscultation is by no means the simple operation which many physicians believe it to be. It is an art which must be learned through long practice, and is attainable to its fullest extent only by those who possess, in the first place, a thorough knowledge of the anatomy of the organs contained within the thoracic cavity,—both the gross 197anatomical relations of the different organs and the minute structure of the different subdivisions of the pulmonary mass. A good knowledge of the mode of action of all this vascular and respiratory machinery, under normal conditions, is also necessary. He who really becomes an expert in the art of successful auscultation must necessarily be equipped with a knowledge of the different acoustic phenomena that present themselves to the examiner’s hearing under the various pathological states to which both the heart and the lungs are liable. All these facts are brought out with great fulness of detail by Laënnec in the second edition (1826) of his treatise. (I have not examined the English translation of Laënnec’s treatise, but presumably all these details have been accurately reproduced in that version.) A man without a delicate sense of hearing and a well-trained imagination,—which latter gift may truly be said to be possessed by comparatively few of those who practice medicine,—will soon confess to himself that he is able to gain only a very meagre modicum of satisfactory information from the practice of the art of auscultation.
Laënnec reports a large number of cases in which various pulmonary and pleural disorders developed as complications of the original affection, and in each such case he mentions in full detail all the phenomena that were discovered on auscultation and percussion of the chest. Some of these histories are extremely interesting; they constitute a rich mine of clinical data from which the practicing physician may draw a great fund of useful information. A mere list of the headings of these reports would fill several of the pages of this treatise. From the statements already made the reader is likely to infer that Laënnec is particularly strong in his presentation of the facts relating to the pathological anatomy of pulmonary and cardiac diseases, as well as in his treatment of the subject of auscultation in all its phases; and in drawing this inference he would be wholly in the right. Laënnec’s treatise furnishes an exhaustive and thoroughly practical discussion of the various diseases of the heart and lungs, and stands for all time as a glorious monument in his honor.
198Magendie, speaking before a class of medical students at Hôtel-Dieu about the difficulties which the physician occasionally encounters in his efforts to interpret correctly the significance of certain sounds heard during auscultation, narrates the following experience:—
Here, gentlemen, is the heart of a young woman who recently died in this hospital. I believe that I have already published an account of her case, which is one of exceptional interest; but, however this may be, I remember perfectly well all the details of the results ascertained (during life) by a careful auscultation of her heart. The first sound was heard without any difficulty, but the second one was entirely lacking. What, it will be asked, was the cause of this phenomenon? At first I was disposed to believe that she was affected with hydrothorax, but, when I came to make a more careful examination, I was obliged to reject this hypothesis; and, although I suspected that the absence of the second sound was due to an obstacle of a mechanical nature,—one that nullified the stroke communicated by the heart to the sternum,—I was unable to form any idea as to the real nature of this obstacle. The present autopsy furnishes the desired explanation. As a result of a former attack of pericarditis the anterior surface of the heart was covered with a thick layer of false membranes; ... the tip of the organ, on the other hand, still preserved its usual smooth and polished aspect.... In my judgment the interposition of false membranes, which had been deposited upon the surface of the heart, acted as a cushion, thus preventing the transmission of the sound by annulling the shock which would otherwise result from the blow upon the sternum. Lower down, at the tip of the organ, where no false membranes had been deposited, the blow upon the thorax, caused with each systole of the heart, produced the normal degree of noise.
(From Magendie’s “Leçons sur les Phénomènes Physiques de la Vie.”)
I should perhaps add here the statement that Laënnec’s researches into the question of auscultation of the chest were made at the Necker Hospital in Paris, and extended over a period of eighteen years.
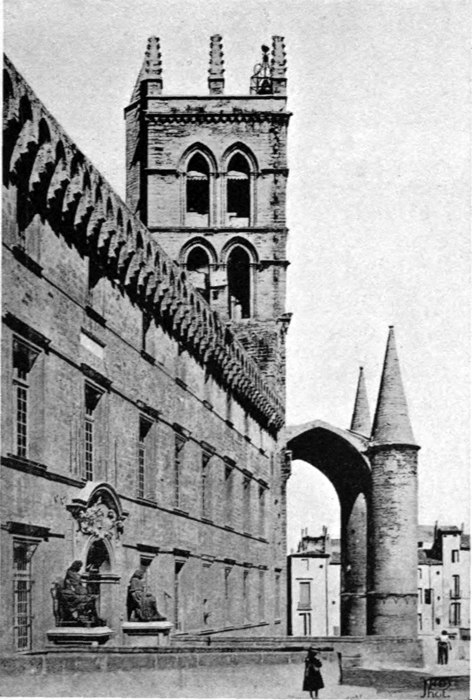
The Faculté de Médecine and the Cathedral at Montpellier, France.
(Courtesy of Monsieur le Pasteur Paul Barnaud, of Sainte Foy la Grande [Gironde], France.)
Paul-Joseph Barthez, one of the most distinguished physicians of France during the eighteenth century, was born at Montpellier on December 11, 1734. His father, who was a civil engineer and well known as a clever mathematician, 199practiced his profession at Narbonne, and it was there that the son spent the first years of his life. At a very early age he manifested a decided love for study, and his parents took great pains with his education. During the period of youth he displayed two marked characteristics—sincerity and very little inclination to indulge in social pleasures. On more than one occasion he submitted to chastisement rather than to tell a lie. As he advanced in age he showed a marked tendency to choose an ecclesiastical career, but his father was not at all disposed to encourage him in such a choice, and finally induced him to give the preference to medicine. Accordingly, Paul-Joseph, during the month of November, 1750, was enrolled as a medical student at the University of Montpellier. Three years later he passed the required examinations with great credit and was given the degree of Doctor of Medicine. In 1761 he made his first appearance at Montpellier as a lecturer and met with a fair degree of success. Up to this time he had experienced a good deal of anxiety caused by his pecuniary troubles, but during the succeeding years his practice steadily increased and he was soon relieved from this source of trouble. In 1781, after the death of Dr. Tronchin, he was called to Paris to take the doctor’s place as the private physician of the Duke of Orleans. In the meantime, despite the greatly disturbed condition of political affairs in Paris, and also despite the persistent efforts of his enemies to drive him out of the capital, Barthez managed to accumulate a fortune amply sufficient for all his reasonable needs. In 1802 the First Consul, Bonaparte, appointed him and Corvisart Government Physicians,—Barthez for Montpellier and the southern part of France, and Corvisart for Paris and the northern part; and, a little later, Barthez was appointed Bonaparte’s Consulting Physician.
Toward the end of his life Barthez suffered a great deal from bladder trouble, which proved eventually to be dependent upon the presence of a calculus. Instead of submitting at this time to a surgical operation, the only measure that offered him any chance of permanent relief, he put his faith in the use of lithontriptics; and then, when these proved to 200be impotent to give him relief, he expressed his willingness to submit to an operation. But by that time his general condition had become so unfavorable that it was not considered safe to operate. His death occurred on October 15, 1806, after he had passed through several weeks of very great suffering.
In order that one may form a correct estimate of Barthez’ professional career it is necessary that certain facts should be borne in mind. In the first place, he was endowed with a prodigious memory, a remarkable capacity for grasping facts, unlimited patience in studying their different aspects, great ability in ascertaining their relations to one another, and wonderful facility in following out the connections between abstract ideas. Then, in addition, his acquaintance with both ancient and modern languages made it easy for him to familiarize himself with the sayings of the philosophers and scientific men of all times and countries.
The “Court of Honor” of the Faculté de Médecine at Montpellier, France.
(Courtesy of Monsieur le Pasteur Paul Barnaud, of Sainte Foy la Grande [Gironde], France.)
In 1785, after the death of Imbert, who at that time occupied the important position of Chancellor of the University of Montpellier, the highest medical office in the southern half of France, Barthez was chosen his successor.
Were it not for the difficulty presented by the lack of space I should be glad to add here, by way of example, a reproduction, in English, of one of Barthez’ “Consultations,” some of which are most instructive, and which furnish at the same time an excellent picture of the manner of procedure followed by this celebrated French diagnostician and teacher of the science and art of medicine. Merely to furnish a résumé of one of these chapters would not serve a sufficiently useful purpose, and I must therefore abstain from making any attempt whatever to supply the desired portrayal. To those, however, who are interested more particularly in the subject of syphilis I will venture to suggest the perusal of Consultation XXXVI. (pp. 381–396), in which Barthez gives a very complete report of the infection, with that disease, of an entire family (father, mother and several children). This report is well worth reading. In addition to the “Consultations de Médecine,” which was 201published in 1820 by Lordat, Barthez wrote the following treatises:—
“Nouveaux Eléments de la Science de l’Homme,” Montpellier, 1778 (1 vol.); Paris, 1806 (2 vols.); “Traité des Maladies Goutteuses,” Paris, 1802 (2 vols.); “Nouvelle Mécanique des Mouvements de l’Homme et des Animaux,” Carcassonne, 1798; “Discours sur le Génie d’Hippocrate,” Montpellier, 1801.[23]
EARLY STUDIES OF THE DISEASE NOW UNIVERSALLY CALLED TYPHOID FEVER
Up to the year 1829 the disease now universally called “typhoid fever” was known by a great variety of names, all of them more or less objectionable and therefore not acceptable to the majority of physicians. Here are a few specimens of these terms: “gastritis” or “gastro-enteritis”; “enteric fever”; “slow nervous fever”; “gastroentero-cephalitis”; “abdominal typhus”; “pathogenic fever,” etc. It is only in the last-mentioned name that we find evidence of an attempt—only a very feeble attempt, it is true—to suggest some connection between the term proposed and the real cause of the disease. Chomel, in 1834, very quickly disposed of the first two names suggested when he wrote: “At the present time no physician who is a careful observer of disease and who at the same time is well versed in pathological anatomy, looks upon typhoid fever as a gastritis or a gastro-enteritis.” At about the same time Philippe Pinel, the distinguished author of the work entitled “Nosographie Philosophique,” made the following statement with regard to typhoid fever: “In this disease one cannot fail to observe that there exists, toward the end of the small intestine, a violent inflammation of the mucous membrane.” To go back farther still in the history of medicine I will mention here the fact that Galen attributed this and other epidemic fevers to the drinking of infected water. Huxham and Pringle, two of the best English authorities on fevers, frequently mention, as a cause of typhoid fever, the drinking of polluted water in which are contained decomposing animal matters. So far as I am able to ascertain, however, Johann Peter Frank was the first to throw doubt upon the correctness of this mode of causation, 203or at least upon the correctness of the form in which the statement is made. Putridity alone, he says, does not satisfactorily explain the characteristic features of the disease. “The cause of these nervous fevers,” he adds, “is not to be found in putrid matter but rather in some principle, or primary element, which easily combines with it,—an element the nature of which is unknown to us.” Putrid matter, then, was recognized by Frank as being simply the vehicle of the cause of the disease (viz., a special contagium vivum). Budd, in 1856, held very much the same view; and Murchison, in 1857, agreed in the main with Budd.
Montpellier. Vestibule of the Faculté de Médecine at Montpellier, France.
(Courtesy of Monsieur le Pasteur Paul Barnaud, of Sainte Foy la Grande [Gironde], France.)
The next suggestion of a new name for typhoid fever came from Bretonneau, of Tours, France; his proposition being that the disease should be called “Dothiénentérite” (from δοθιὴν, the Greek word for pimple, and έντερον, intestine). Certain authors attributed the associated fever to these pimple-like lesions in the small intestine, but Bretonneau held that the latter are the products of an infection and not the cause of the fever; and that view has been universally accepted as correct ever since his time. This new term for typhoid fever, however, was not favorably received, and was very soon forgotten. On the other hand, the expression “typhoid fever” (from τῦφος, stupor, and εὶδος, form), which simply described the most noteworthy feature of the disease, was promptly adopted. Charles A. P. Louis,[24] Chief of Clinic at the École de Médecine of Paris, and Member of the Académie Royale de Médecine, to whom we are indebted for the final settlement of this troublesome question, gives the following brief account of the considerations which led him to urge the final acceptance of the term “typhoid fever”: “After seeking carefully for a term that would express the anatomical features of this disease, without jarring too decidedly upon the ear, as ‘dothiénentérite’ does, and having failed to discover any better expression than ‘typhoid fever,’ I finally decided to employ it in 204preference to all others.” And since that time no physician has succeeded in supplanting it with a term more acceptable to the Profession. As to the real underlying cause of typhoid fever I shall have nothing to say, as this is a matter which belongs strictly to the domain of modern medicine; and I have no wish to trespass upon the territory of the writer of this most important section of the history of medicine.
As to the contagiousness of typhoid fever Louis states that, out of 117 cases which he had observed, there were only three that might be imputed to contagion.
A few words more concerning Charles A. P. Louis, to whom I have already referred briefly in connection with the subject of selecting a suitable name for typhoid fever. Marshall Hall, the famous English physician, characterizes him as the greatest pathologist of any nation or of any age. In another place he says:—
Monsieur Louis is the Bacon of Medicine; he has taught us how to observe, and how to deduce important laws from the facts observed.... Monsieur Louis is a man of such talent, labour, exactness, truth, and probity, as I never met with in any other man. His labours I shall consider as the chief ornament of these lectures, and my chief claim to your consideration.
In still another place Marshall Hall quotes Louis’ own account of the early years of his professional career, as follows:—
After having practised as a physician in a foreign country, I returned to France, at the age of thirty-three, determined to give myself up to the observation of disease; and, in order to obtain my end more effectually, I resolved to forego all other employment. I pursued this course for nearly seven years; in other words, during that time I devoted myself exclusively to the observation of all the cases admitted into St. John’s and St. Joseph’s wards at the hospital of La Charité. Three years elapsed before I ventured to publish, at the request of a friend, my first memoir, on the perforation of the small intestines; my object being to observe for myself, and not to describe what I might have observed.

CHARLES A. P. LOUIS
François Joseph Victor Broussais was born in 1772 at Saint-Malo, a seaport on the north coast of France, in the Department of Ille-et-Vilaine (formerly a part of Brittany). His early medical training was obtained at Paris, where he attended for a short time one of the courses of instruction given by Bichat. On reaching the age of forty-two he entered the service of the Military Hospital at Val-de-Grâce, and not long afterward was chosen Professor of General and Special Pathology and Therapeutics at the University of Paris. The lectures which he delivered on these subjects so fascinated the students and the numerous physicians who attended the course in increasing numbers, that—as Pagel expresses it—a general impression was created, during a period of several successive years, that the whole of French medicine was represented in the person and doctrines of Broussais. The correctness of Pagel’s statement is corroborated by the following extract from “J. L. H. P’s sketches”:—
Monsieur Broussais is unquestionably the most remarkable medical writer of the present age. Splendid works, celebrated lectures, and a great number of proselytes, have in a few years spread far and wide his name and his opinions.... There are, on the other hand, many physicians, who, too old to return now to their studies, and witnessing with no pleasure all these innovations, say that the professor of Val-de-Grâce is only a sectary, in whom passion holds the place of genius, and hardihood of force.... His brutal attacks on men, whether dead or living,—French or foreigners, surrounded with the esteem and admiration of all,—have found approval only among the personal enemies of the contemporaries whom he criticises, and this too in a generation greedy of novelty, and imposed upon by his rough manners and bold speech.
208The extract also shows that not a few French physicians refused to accept the “fascinating” doctrines promulgated by Broussais, and reported by him to be “founded on physiological principles.” As Broussaism played such an important part, during the early years of the nineteenth century, in hindering the advance of the real science of medicine, my readers will pardon me, I am sure, if I devote considerable space in the attempt to elucidate the meaning of Broussaism. These revolutionary ideas regarding “physiological medicine” were first published in book form in 1816. Two later editions followed,—one in 1821 and another in 1829. The text is arranged in the form of propositions or “physiological principles,” of which there are 568. Pagel describes them as “not being related in the remotest degree to modern physiology.” In the following paragraphs I have reproduced (in the form of translations) a few of these “Propositions de Médecine” as they are printed in the edition of 1829:—
II.—Heat, from whatever source it may be derived, is the first and most important of all stimuli; and, when it ceases to exert its vitalizing power upon the economy, all other stimuli lose their power to produce any effect upon it.
IV.—If heat is withdrawn for a certain period of time all those phenomena of the economy which are of a conservative, reparative or medicative nature cease all activity; and the same is true when oxygen is withdrawn.
XX.—Assimilation, which is a phenomenon of the very first order, cannot be explained by the assumption that it is due to the action of sensibility and contractility; it should be looked upon only as a manifestation of a creative force,—as an act of vital chemistry.
XLII.—Instinct consists of nervous impulses or stimuli—sometimes associated with consciousness and sometimes not—which originate in one of the viscera, and which call upon the central nerve power to execute such acts as are necessary to the exercise of the functions of that viscus.
XLIV.—Acts which are originated by instinct are most frequently 209observed in infants, and are witnessed with diminishing frequency as the child’s intelligence becomes more perfect.
XLVII.—As may be said with equal truth of insanity the passions furnish an example of the triumph of the viscera—that is to say, of instinct—over intelligence; and, on the other hand, it is well-known that the passions themselves produce insanity.
LI.—The intellectual faculties may be exercised without any participation of passion, but never without an accompaniment of either pleasure or pain.
LXIV.—An excess of haematosis or sanguification in an organ increases at first the sum total of its vitality, but this increase is subject to limitations. If, for example, the excitation is kept up beyond a certain length of time the continued hyperaemia establishes in that organ a condition which deserves to be called disease.
XCIX.—When irritation causes the blood to accumulate in a part or tissue, and when, further, this accumulation of blood is accompanied by such an exceptional degree of swelling, redness and heat as to threaten the disorganization of the part thus irritated, it is customary to apply to this complex phenomenon the name of “inflammation.”
CXXVII.—Tubercles, cancers, etc., of the brain owe their origin to a chronic inflammation of that organ.
CLXVIII.—I have never seen tubercles of the lungs except in cases where these lesions had developed from an antecedent inflammation; and it does not appear to me that the tubercles which are observed in the lungs of infants at birth, may rightly be considered as having originated independently of inflammation.
CXCV.—All the different varieties of acute and subacute inflammation possess the power to produce cancer.
CCCVII.—He who does not know how to manage properly a case of irritability of the stomach will never be able to treat successfully any other malady. In short, the key to a knowledge of pathology is to be found in an intimate acquaintance with gastritis and gastro-enteritis.
CCCXLII.—Pulmonary phthisis may be prevented by putting an end, by means of antiphlogistic remedies and revulsives, soon after its presence is discovered, to any existing irritation of the respiratory apparatus.

BROUSSAIS
These dozen or more of Broussais’ “Propositions” or fundamental medical doctrines should suffice, it seems to me, to give the reader a correct idea of the kind of physiology and pathology that found favor in France during the third and fourth decades of the nineteenth century, and that too despite the thoroughly sound and admirably logical, but less fascinating, teachings of such authorities as Morgagni, Bichat, Ch. A. P. Louis, Bayle, Corvisart and Laënnec.
It was toward the end of this same year (1821) that Laënnec began teaching his new method of auscultating the chest by means of the stethoscope—which had first been made known to the world by Auenbrugger in 1761, but which had been completely ignored until Corvisart published a French translation of Auenbrugger’s book in 1808. As early, however, as in 1819 Laënnec had published reports of a number of instances in which, by means chiefly of this method of exploration, he had correctly diagnosed the presence of tuberculous and other deposits in the lungs of certain patients. The publication of these reports evidently excited very much the wrath of Broussais, for in the new edition of his book (viz., that of 1821) he criticises Laënnec’s statements most unjustly and in a manner that reveals how completely his mind was saturated with the belief that what he calls “inflammation” is at the bottom of most of the pathological phenomena encountered in medical practice. Lack of space will not permit me to quote here more than one or two of Broussais’ comments on the conditions reported by Laënnec:—
The pathological alterations, considered by themselves, are simply curiosities, and are not of the slightest utility to anybody who may feel disposed to study them; because they are all either the products of simple inflammation, or else they owe their origin to some cause which does not fall legitimately in the domain of physiological pathology.
(Copied from pp. 674, 676, 677, and 679 of Vol. II., edition of 1821.)
Further on in the same volume, speaking of melanotic cancers, Broussais says:—
... this is all that it is important for the physician to know; 211and, as to what Monsieur Laënnec has written about black cancers, I may say that it is simply the product of his imagination, a gloomy romance, which I found difficulty in reading from the beginning to the end.
It seems proper that I should furnish some information concerning Broussais’ methods of treatment in different diseases. In the last analysis it will be found that in nearly all cases he adopted such remedial measures as tended to allay or arrest inflammatory action. Thus, in beginning pulmonary consumption he prescribed the application of leeches to the infraclavicular region; in jaundice they were to be applied in the hypochondriac region, in pharyngitis and tonsillitis to the side of the neck, in dysentery to the anus, in articular rheumatism to the neighborhood of the affected joint, and, in maladies that were not distinctly localized, the epigastrium was the region to be chosen by preference. When simple irritation was present Broussais prescribed revulsives—such, for example, as blisters, emetics and laxatives. As a rule, however, he gave the preference to direct antiphlogistic measures. He is credited with having had a profound contempt for the vis medicatrix naturae. It was said that his pupils showed a tendency to push his pathologic teachings to an extreme. Desruelles, for instance, was in the habit of treating his syphilitic cases, not with mercury or any other of the specific remedies commonly employed at that period, but with leeches applied locally.
As early as in 1816 Broussais announced that, as a result of his doctrine, “the mortality of Val-de-Grâce had greatly diminished, to the grand astonishment and admiration of the world.” This assertion not having been noticed, Monsieur Broussais, in 1821, went a step further. He then predicted, in the Preface to his “Examen des Doctrines,” that his doctrine would soon exert an influence on population more marked than that exerted by vaccination. This was pretty strong, but not, however, sufficient; for in 1822, “the Prospectus of Les Annales de la Médecine Physiologique declared that, in the hospitals where the physiological doctrine was adopted, the mortality was only one in thirty, 212while in the others it amounted to one in five.” These results, which caused great astonishment, induced Monsieur Brasquet, a physician, to inspect the records with a view to ascertaining the exact facts. Thus it was discovered that, during the five years from 1815 to 1819, Monsieur Broussais had lost more patients than his contemporaries had lost during the same period; his mean mortality having been one in thirteen. (The results of Monsieur Brasquet’s inquiry were published in the Revue Médicale.) “Monsieur Broussais replied in Les Annales de la Médecine Physiologique, but his reply was not at all satisfactory. He did not deny the correctness of the figures published in the Revue Médicale, but he maintained that they proved nothing against him.” The proof, however, that he had lost one patient in thirteen, and not one in thirty, as he had claimed, remained unshaken.
It was probably this experience that marked the beginning of the downfall of the doctrine known as “Broussaism”; but many years had to elapse before this doctrine vanished entirely from the accepted medical textbooks. August Hirsch, in his “History of the Medical Sciences in Germany” (1893), passes the following judgment upon Broussais’ work: “Under the title of ‘Physiological Medicine’ Broussais presented to the world a system which for narrowness of scope, for arbitrariness and for the perniciousness of the treatment which was deduced from the premisses that grew out of the theory, could be compared only with Rasori’s therapeutic method.”
Broussais died in 1835.
J. L. PETIT, OF PARIS, AND HIS CONTEMPORARIES IN SURGERY—SABATIER, CHOPART, DESAULT AND DUPUYTREN
In the history of surgery in France there is a conspicuous absence of distinguished names from the list of men who succeeded Ambroise Paré, until we reach that of J. L. Petit, a surgeon whose career shows him to have been worthy of all the praise and esteem which the French have lavishly bestowed upon him.
Jean-Louis Petit was born at Paris in 1674, and already at the early age of twelve manifested a strong inclination to adopt a surgical career. By the time he had reached his sixteenth year he had become so expert as a dissector that he was entrusted with the duties of a demonstrator of anatomy, a position which he filled to the entire satisfaction of both the students and the superior authorities of the medical school. Two years later,—that is, in 1692,—he entered the military service and was given the position of Army Surgeon. He was present at the siege of Namur, and served through all the succeeding campaigns up to the year 1697, at which time he was placed in charge of the Military Hospital at Tournay. In 1700 he retired from the army and returned to Paris, where he engaged in private practice and at the same time gave instruction in anatomy and surgery. From this time forward his reputation as a skilful surgeon rose rapidly until he was universally acknowledged to be the leading surgeon of the capital, a fact which was confirmed by his election to the position of Director of the Royal Academy of Surgery.
It was said of him by a very competent critic (A. Richet) that Petit was one of the boldest and most skilful surgeons 216of his day. He possessed a profound knowledge of the anatomy of almost every region of the body, and at the same time was remarkably skilful in the handling of his bistouri. He also seemed to possess, on the spur of the moment, an intuitive knowledge of what he should do in any situation of affairs that might suddenly develop in the course of an operation. The reflections which he made as he progressed in the work with which he happened to be busied, were most original, and led somebody to say of him, on a certain occasion: “He must have invented surgery.” On reading his treatise on surgical maladies one is struck with the originality of his remarks, with the profoundness of his thinking, and with the closeness and accuracy of his observations. His writings make most attractive reading for the surgeon.
In order that my readers may judge for themselves how cleverly and how wisely Petit dealt with some of the surgical problems which presented themselves for solution in the course of his private practice I will give here, in the form of very brief translations, three instances which seem to me to possess to-day a peculiar interest in that they reveal the important fact that a correct diagnosis may occasionally be made without the aid of some of the complicated and expensive machinery which not a few of our modern surgeons think indispensable to the ascertainment of the truth. I should perhaps modify this last remark by stating that the extraordinary cleverness and practical wisdom exhibited by J. L. Petit are gifts not often bestowed by Nature upon physicians, and that therefore the X-ray and other modern inventions which compensate for the infrequency of such gifts, are to be considered in the light of very important blessings conferred upon suffering humanity.
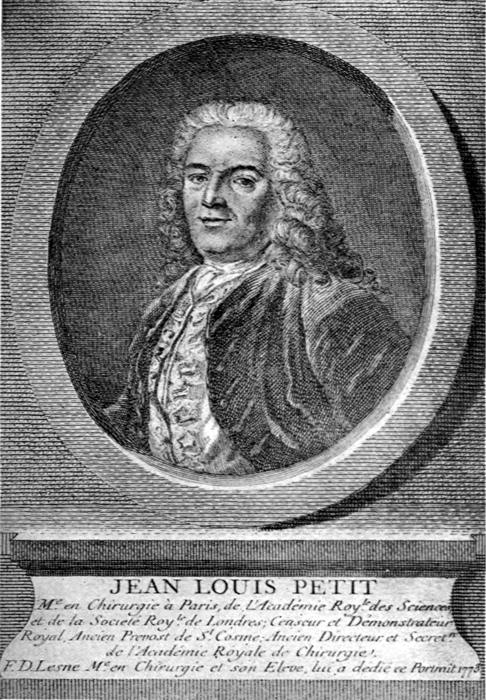
JEAN-LOUIS PETIT
(1) “The man, whose case history I am about to relate, said that the symptoms from which he had suffered, during the preceding twelve months, were the following: a frequent but dry cough, with loss of appetite; almost constant thirst; difficulty in obtaining sleep; night-sweats, more marked in the region of the head and neck than elsewhere; and irregular chills and fever. The physicians 217whom he had consulted were led to believe that he was affected with consumption, and they treated him in accordance with this belief, but so far without success.—On examination I found that two of his teeth were carious, and I advised their extraction. A rapid restoration of the patient’s health followed in less than a fortnight.”
(2) “The late Princess of Condé had interested herself greatly in a young girl whom she had taken into her service. Upon her return to Paris she took the girl with her, in the hope that the physicians of that city would be able to cure her of the hemicrania (‘Migraine’) from which the girl had frequently suffered during the preceding five years. Bloodletting was the remedy adopted at that period for nearly every malady, and these Paris physicians let her have a full taste of this remedy, prescribing in rather rapid succession twenty such bleedings, the arm, the foot and the region of the throat being the localities selected for this operation. Medical students were thought to be quite sufficiently competent for the management of the arm and foot bloodlettings, but it was I who was obliged to officiate when it became necessary to carry out the bleeding from the neck. As this was the first occasion on which I saw the patient I asked her a number of questions in order to learn the more important facts concerning her malady; and then, failing to discover any that seemed to me to justify the numerous bleedings to which she had been subjected, I examined her mouth, not as a casual matter, but because she had told me about having experienced a sense of heaviness and numbness in her lower jaw. Observing some irregularity in the arrangement of her teeth I counted them, and discovered that there were eighteen instead of the sixteen which are usually present; and it also seemed to me that the second molar tooth on each side was crowding the others. After stating these facts to the Princess, and obtaining her approval of the step which I proposed to carry out, I had the two molars extracted; whereupon, to the great astonishment of her ladyship and all of us, the girl found herself, at the end of twenty-four hours, entirely cured of a malady which had often, during the preceding five or six years, been so distressing that she could not perform her regular duties.” (Copied from Petit’s “Traité des Maladies Chirurgicales,” etc.)
(3) In another part of the same volume Petit reports in detail the history of a case of middle-ear inflammation in which, after the lapse of a few weeks, there developed symptoms that pointed very strongly to the presence of a subdural collection of pus behind and above the inflamed middle-ear. Whereupon, at a consultation that 218was held between the physicians in attendance upon this patient, Petit urged the desirability of trephining the skull in order to give vent to the contents of this assumed abscess. Such a proposition, however, was promptly voted down by the other consultants. (The events here described, it should be remembered, occurred somewhere between 1750 and 1774.) Two or three weeks later, the patient’s pain having become in the meantime more severe, the timid consultants at last withdrew their opposition, and Petit performed the trephining with success. Much foul-smelling pus was evacuated, and after the lapse of a few weeks the patient was pronounced cured.
It would be easy to furnish here, from the printed record already mentioned, additional instances showing the courage, wisdom and skill exhibited by J. L. Petit in his practice of the art of surgery. But the instances already cited amply suffice, as it appears to me, to show the admirable character of the man and his right to be considered the worthy successor of Ambroise Paré.
Petit’s death occurred in 1760.
Petit made comparatively few contributions to medical literature, and of these the shorter ones will be found in the “Journal des Savants,” the “Recueil des Mémoires de l’Académie des Sciences,” and the “Mémoires de l’Académie Royale de Chirurgie.” His great work, which was published in three volumes at Paris in 1774 (also a later edition in 1790), bears the title: “Traité des Maladies Chirurgicales et des Opérations qui leur Conviennent.”
Raphael-Bienvenu Sabatier was born at Paris on October 11, 1732. His father, Pierre Sabatier, was one of the earliest members of the Académie Royale de Chirurgie, and it was therefore quite natural that Raphael chose medicine for his profession. There was nothing remarkable about his early career. He worked hard at his studies of anatomy and cultivated at the same time experimental physiology. At the age of twenty-four he succeeded Balleul as Professor of Anatomy at the Royal College of Surgery. In 1773 he was made a member of the Académie des Sciences, and a few years later, when the war broke out, he was ordered to report, as a consulting surgeon, at the headquarters of the 219Army of the North, at Mons. But, his strength not permitting him to perform the duties of this new position for any length of time, he was soon allowed to return to his private practice. Toward the end of his life Napoleon appointed him one of his consulting surgeons, and at about the same period of time the decoration of the Legion of Honor was conferred on him. When the École de Santé was established he accepted the Chair of Operative Surgery. His death occurred on July 19, 1811.
Sabatier was highly esteemed by his professional brethren. Unlike Desault he brought forward no new inventions or methods of treatment, but he constantly sought how he might introduce some little improvement in existing well-established methods. He was not of an enthusiastic temperament and rarely did anything to call forth opposition on the part of his associates. As a consequence he led a most peaceful life.
Sabatier’s contributions to medical literature were fairly numerous, and among them the following deserve to receive particular mention:—
“Traité d’Anatomie,” 3 vols., Paris, 1764.
“De la Médecine Opératoire,” 3 vols., Paris, 1796; a second edition appeared in 1810; and a third (in 4 vols.) in 1821–1824.
François Chopart was born at Paris in 1743. During his youth he received a thorough preliminary training. From the very beginning of his medical course he showed a decided preference for surgery. Then, for a certain length of time, he served as an interne at Hôtel-Dieu. Afterward he was transferred first to La Pitié Hospital and then to Bicêtre, where he devoted his attention mainly to syphilitic affections. In 1767 he divided the prize offered by the Académie de Chirurgie for the best memoir on the subject of “The Nature and Treatment of Wens.” In 1768 he was given an “Honorable Mention” for his memoir on “Injuries of the Head produced by Contrecoup.” In 1770, after passing with great credit the examinations required, he was given on July 20, 1770, the degree of Master of Surgery; and only one year later he was appointed Professor of 220Practical Surgery. His pupils were very much attached to him on account of the interest which he manifested in their work and because his teaching was so methodical and was so clearly delivered. On March 13, 1782, he was chosen successor to Bordenave, the Professor of Physiology; and a little later he was elected to the Chair of External Pathology. While on a visit to England he made the acquaintance of John Hunter, and kept up an active correspondence with him during the following years. He was also one of Desault’s intimate friends. Being open-minded and frank he got along pleasantly with all who came in contact with him. He died in 1795 from an attack of cholera morbus.
Among his writings which deserve special mention are the following: “Traité des Maladies Chirurgicales et des Opérations qui leur Conviennent,” Paris, 1780, 2 vols.; and “Traité des Maladies des Voies Urinaires,” Paris, 2 vols., 1701, and a later edition in 1821.
Chopart is known to American and English surgeons chiefly through the fact that he devised an amputation of the foot which is commonly known as “Chopart’s amputation.” The procedure is thus briefly described by Dr. Thomas L. Stedman in his Medical Dictionary: “Disarticulation at the metatarsal joint, leaving only the astragalus and calcaneum, with the soft parts of the sole of the foot to cover the stump.”
Pierre-Joseph Desault was born on February 6, 1744, at Magny-Vernois, a small village in the Department of Haute-Saone, on the western slope of the Vosges mountains. At the time of his birth his parents were living upon the income derived from a modest fortune, and they found it very difficult to support their family of seven. As soon as Pierre was old enough to receive regular instruction he was placed under the care of a private teacher at the neighboring village of Lure, the chief centre of that district. In this way he acquired an elementary knowledge of Latin and was fitted, by the time he reached the age of twelve, to enter the fifth form or class at the Jesuits’ college in Lure. His favorite study, as soon became evident, was mathematics, and 221this branch of knowledge he cultivated with such assiduity and success that already at the age of seventeen he had reached the point where all the elementary treatises to which he had access no longer afforded him any satisfaction. At a somewhat later period of his life, when he could no longer receive help from his parents, this decided preference for mathematics stood him in good stead, enabling him to contribute to his own support by giving lessons in geometry. It also aided him in making useful applications of its principles to the art which he was soon to cultivate with such conspicuous success—viz., surgery. He took special delight at this time in the perusal of Borelli’s celebrated treatise “on the movements of animals,” and even went so far as to write a long commentary on this work. Nothing, however, is now known about the fate of this document, as Desault never published it nor showed at any time a wish to become an author.
Bichat, from whose eulogy of Desault I have derived most of the facts which are reported in the present brief sketch, says that during the years immediately preceding the period which is now under consideration, surgery was cultivated by artisans rather than by artists; and that, in consequence of this situation of affairs, it was very slow in making any advances which were worthy to be characterized as genuine steps of progress. “Genius, when not appreciated, escapes as mere froth; its efforts result in nothing unless glory is the reward. Little by little, as the public learned more and more how great was its need of surgery, this art began to receive a larger share of consideration; and thus, as it became more honorable, it was cultivated to an ever greater degree, and as a result it advanced at a more rapid pace toward perfection. In its different branches, which were all working to accomplish some useful purpose, new discoveries were constantly being made, and thus it came about that from the middle of the eighteenth century onward French surgery rapidly outdistanced the surgery of all the other nations.” (Bichat.)
It was at this period that Desault began his career as a surgeon, and in the course of that career he did at least his 222full share in the work of supplying the deficiencies that were observed in some of the methods commonly employed at that period, in removing the positive defects that were discovered in others, and in devising entirely new procedures. At the same time Desault did not fail to recognize the importance of making the foundations of his knowledge as solid and firm as possible, and with this idea in mind he spent all the time that he could possibly spare from the clinical lessons which he was then giving, in utilizing the anatomical material available in the dead-house of the hospital. As his rivals stuck closely to the old methods of instruction, and in addition were not endowed with his remarkable gifts of teaching, of drawing all sorts of interesting inferences from the anatomical relations of the part or limb that was under consideration at the moment, Desault rapidly outdistanced all his competitors. He was, so far as I am able to learn from the printed records of this period (1766), the pioneer of this particular type of instruction (anatomical, pathological and clinical) in surgery in the great Paris hospital Hôtel-Dieu. The young men who attended these courses in ever increasing numbers were fascinated by what they heard and saw,—for Desault always taught with the cadaver or the living subject before him,—and it soon became very noticeable that the attendance upon the lectures given by his rivals (i.e., the regular professors) was falling off. Actuated by bitter jealousy these men managed at first to have his permit to teach taken away from him. But Antoine Louis and La Martinière, two of the most influential surgeons of Paris, at that period, interfered and so arranged matters that Desault was able to resume his private courses. In fact, Louis made it clear, by his presence at several of the sessions, that he approved of this teaching and that he proposed to protect Desault against all interference on the part of rivals. Desault’s method of teaching, says Bichat, constituted the first development, in France, of what is now known as surgical anatomy, a very extensive and important department of the art of surgery.
Another striking feature of Desault’s manner of giving instruction is to be found in his invariable practice of demonstrating, 223whenever it was possible for him to obtain the materials necessary for doing this, the alterations which are produced in a part by disease or by accidental injuries, and also the influence exerted by these lesions upon the neighboring tissues or organs. In these demonstrations he never allowed his mind to wander in the direction of pointing out something akin to a discovery in pathology; he stuck closely to the questions that were under immediate consideration, thus giving preference, over everything else, to what was of chief importance to the students.
By thus conducting his teaching always with an eye single to the best interests of his pupils Desault became, in the course of a very few years, the most celebrated teacher of surgical anatomy in France. His rivals laid stress upon this particular feature of his fame in the hope of thereby belittling, in public estimation, the equally important celebrity, which he was now shortly to attain, of being also a great surgeon. It is in some such words as these which I am using that Bichat, who was his favorite pupil and righthand man during this period of his career, records the efforts made by his jealous rivals to interfere with Desault’s professional success.
In the early stages of his career as a surgeon Desault gave instruction in operative surgery, but in a comparatively short time he advanced beyond this stage and showed that he possessed considerable originality. He invented a very effective method of treating a fractured clavicle by the application, to the shoulder, the elbow and the chest, of a bandage which even to this day is known as “Desault’s bandage.” In planning this bandage its inventor first calculated with great care the forces which play the principal part in causing the displacement of the two segments of the fractured clavicle. This manner of attacking the problem of how best to treat such a fracture was, so Bichat declares, not that which had usually been followed by his predecessors, but it nevertheless proved to be the correct way of finding the right remedy. He believed, for example, that, inasmuch as the external segment or fragment is pulled downward by the weight of the shoulder and forward and 224inward by the action of the muscles, the right course to pursue must, first, be to furnish proper support to the shoulder, and at the same time to draw the external fragment outward and backward. He realized that by the employment of continuing extension it would be practicable to effect these results. So, placing a cushion over the chest, to serve in some measure as a point or angle of resistance, and resting the arm firmly against it, he was able, by pressing the lower part of the arm closer to the chest, to cause the upper part, together with the fragment attached, to stand out from this part of the trunk. Thus, as it were by a single stroke, he succeeded in obtaining a result which, for a very long period of time, had eluded the best efforts of the surgeon’s art. This was a great triumph for Desault, but its importance was not immediately appreciated. The bandage was successfully used at the Salpétrière, one of the larger hospitals of Paris, but the full recognition of its value came only after the lapse of many years,—indeed, not until after the death of its inventor. To-day it occupies an important place in the history of surgery.
Of the other improvements in surgical procedures that we owe to Desault I will mention here only one—that of ligating the exposed ends of the larger arteries which had been divided in the course of the amputation of a limb. Ambroise Paré, it will be remembered, was the first to introduce this practice in France (early in the seventeenth century), but it failed to meet with general acceptance and was then abandoned for more than a century. At Bicêtre, another of the large hospitals of Paris, the practice of immediately ligating the divided blood-vessels after an amputation was first revived by Desault, and not long afterward Ferrand also introduced the revived method at Hôtel-Dieu. From this time onward it became the standard method of procedure.
In 1788 Desault succeeded Ferrand as Chief Surgeon of Hôtel-Dieu, and from this time forward, for five years, he conducted with great success regular instruction in clinical surgery. Then, toward the end of May, 1793, he was thrown into the prison of the Luxembourg, the charge brought 225against him being that he had refused to give his professional services to those wounded in the affair of the previous 10th of August. He was retained as a prisoner only three or four days; but from this time to the day of his death (June 1, 1795) he was kept in almost constant fear of being prosecuted, and was consequently prevented in large degree from doing any useful work in surgery.
In his analysis of Desault’s career as a surgeon Bichat calls attention to the fact that the establishment of a clinical school at Hôtel-Dieu was not the only benefit which he conferred upon that hospital. He did much more than this; he improved the arrangement and the ventilation of the different wards, established better methods of distributing the food systematically among the patients, increased their comfort by making rules whereby their wants would be more promptly supplied, etc. All matters of this nature occupied the first place in his thoughts and drove out of his mind, long before he died, all ambition to accumulate a fortune. Despite the stormy conditions which prevailed during the Revolution and which upset completely all the existing arrangements in Paris, he managed to keep up a good part of his clinical courses.
Speaking of Desault’s personal traits of character Bichat says that he was somewhat quick-tempered, but that he promptly got over his bad temper and was then once more gentle and reasonable in his speech.
He had his full share of enemies. In nearly all cases this enmity sprung from jealousy. But what really great man, adds Bichat, ever passed through life without being annoyed by enemies through jealousy? On the other hand, Desault had excellent friends, men who—as he expressed it—were the joy of his life.
Desault was not of a scientific turn of mind; he never wrote articles or took active part in any discussions. Some of the best of the pupils who attended his courses took full notes of his lectures, and these, after Bichat had revised them and edited them, were published under the title of “The Surgical Works of Desault.”
226Guillaume Dupuytren was born at Pierre Buffière, France, October 5, 1778. He commenced the study of anatomy and physiology at an unusually early age, and was appointed Prosector at the Paris École de Santé before he had reached his eighteenth year. In 1802, very soon after he had received the degree of Doctor of Surgery, he was given the appointment of Attending Surgeon to Hôtel-Dieu. Of this early period of his career very little need be said. He lost none of his enthusiasm for his chosen work and was recognized by all his associates as a surgeon of great promise. From the position of simple attending surgeon at Hôtel-Dieu he rose in 1808 to that of Adjunct Surgeon-in-Chief. Finally, in 1815, after the death of Pelletan, he was made full Surgeon-in-Chief of that great hospital. So far as it was possible for Dupuytren to advance in the endeavor to gain official recognition as a surgeon, he had by this time risen to the highest point that it was practicable for him to reach. Let us now consider some of the other aspects of his career.

DUPUYTREN
After the death of Bichat in 1802 Dupuytren turned his attention from what was supposed to be normal anatomy to pathological anatomy. The change was greatly favored by the fact that, in the course of his regular work as prosector, he was constantly encountering all sorts of pathological conditions, and thus he gradually acquired a strong interest in pathological problems. Pathological anatomy, as newly interpreted, was no longer a mere observing of the abnormal changes which take place in different structures and organs of the body,—the sort of “cold work” which had occupied in large measure the minds of Bartholinus, Mangetus, Bonnet of Geneva, Morgagni of Bologna, and Lieutard, and which involved practically no study of the origin of such changes,—but what might be termed a living pathological anatomy, in which the effort is made to ascertain the beginning, the gradual progress and the termination of the process. Ample material for this sort of study was constantly passing through Dupuytren’s hands, and he made the most of his opportunities. Professor LeClerc, who is my chief authority for the present sketch of Dupuytren, 227says that by means of this new pathological anatomy much light was thrown upon both diagnosis and symptomatology. At first the courses which Dupuytren gave in the École de Santé ran in large degree parallel with those of Bichat, but after the latter’s death Dupuytren had the field almost entirely to himself. He taught anatomy, pathological anatomy, and physiology, and increased the interest in his teaching, on the part of the pupils, by furnishing a variety of facts drawn from his wide experience. His great skill as a dissector enabled him to demonstrate all sorts of fine details—as, for example, not merely a limited portion of a nerve, but nerves throughout their entire course.
After Dupuytren became full Surgeon-in-Chief at Hôtel-Dieu he ceased teaching operative surgery and devoted himself largely to clinical surgery. He adopted the habit of visiting the hospital at an early hour, long before the time appointed for the arrival of the class, and thus he was able to examine the patients leisurely and to give all the necessary instructions to his assistants. By the time the class arrived he was entirely ready to receive them. He was extremely punctual in attending to his hospital duties.
In 1814 Dupuytren took an active part in caring for the wounded soldiers on the field of battle; and again in 1830, during the civic disorders of that period, he had the care, at Hôtel-Dieu, of many cases of wounds from firearms.
A French physician whose identity is concealed under the initials J. L. H. P., has published a very complete pen-portrait of Dupuytren’s most prominent personal and professional characteristics, and Elisha Bartlett, M.D., of Boston, has furnished us with an excellent English translation of this work. From this book I shall take the liberty of quoting here several sections that seem to me to be particularly interesting.
Monsieur Dupuytren is, in my opinion a surgeon of the most exalted merit.... He has a coup d’oeil of most admirable precision, a sure and steady hand, a coolness and self-possession always imperturbable, and that innate instinct or tact so necessary in all the arts. A man is born surgeon or physician, as a man is born poet or painter.... Monsieur Dupuytren is particularly remarkable for 228his diagnostic foresight.... Arrived at the bedside of the patient, his fine senses are all awake; in a few minutes of question and researches, his examination is finished. One might often believe that he has given to the case only a superficial attention, but his subsequent lecture will prove that he has seen everything and seen it thoroughly.... He describes a pathological alteration, yet hidden in the interior of an organ, as though it were visible, and, when the scalpel has dissected and uncovered it, the truth of his description is verified by all who witness it.... Monsieur Dupuytren is not less skilful in treating surgical diseases than he is in detecting them.... I do not fear that I shall be accused of exaggeration in saying that very few surgeons have given proof of so much surgical genius in the invention of modes of operating or so much expertness in their execution. Monsieur Dupuytren possesses in the highest degree a creative and inventive spirit....
So much for Monsieur Dupuytren as a practitioner; Let us now consider him as an instructor....
Since 1815, the surgical clinic of Hôtel-Dieu has lost none of its ancient reputation. No other clinical course in France can be compared to this, whether for the number of students, the abundance of cases, or, finally, for the genius of the professor. In effect, Monsieur Dupuytren comprehends perfectly in what clinical instruction consists; a thing that ought to be somewhat difficult, seeing how few there are who succeed in it. Lessons of clinical surgery have no resemblance to a course of surgery.... A clinic is altogether a different thing. The professor has need here to speak continually without preparation, because the material of his lesson cannot be regulated by himself, in advance, but is dependent upon chance, which brings him, to-day, a strangulated hernia, to-morrow, a fracture; and, in the same day, four or five different cases....
An excellent practitioner, Monsieur Dupuytren thus really possesses the most essential quality of a clinical professor. But to this first fundamental qualification others ought to be united. The professor ought to have a free command of language and the talent of extemporaneous speaking; he should possess a memory sufficiently good to recall distinctly all the circumstances of diseases, and the peculiarities of the different treatments that he has directed; it is necessary, that, thoroughly understanding the necessity and obligations of his instruction, he should accustom himself to return every day to things which he has a thousand times repeated, unmindful of the fatigue resulting from such repetition; above all, he should remember that he is occupied with inexperienced 229hearers, to whom it is not sufficient to say things imperfectly; hearers who may easily be dazzled and led astray, but who ought to be instructed, an end that cannot be attained without patience. In respect to all these things, Monsieur Dupuytren is almost irreproachable.... As to myself, instructed by my personal experience, and by the numerous comparisons that I have made, I do not hesitate to believe and to say that the clinic of Monsieur Dupuytren may be offered as a model of this kind of instruction.
In his memoir concerning the medical schools of Paris, John Gross, an English surgeon, says that no lectures at the École de Médecine were so numerously attended as were those delivered by Dupuytren on operative medicine. He adds that at the lecture which he attended on the operation for inguinal hernia, there were present about 1200 students, the greatest number that the theatre is capable of containing. “But I must confess that I have seldom learnt less from any good practical lecture than I did from this. I was too far off to distinguish well what I saw, or comprehend what I heard; and I returned home with a feeling of regret, that what is grand should be so far remote from what is most useful.”
Dupuytren’s health began to break down in 1833, and he was obliged to take a trip to Italy. A certain amount of improvement resulted from this journey, but only for a brief period of time. On February 7, 1835, he died, leaving in his will the sum of 200,000 francs to l’École de Médecine for the establishment of a chair of pathological anatomy. Before his death, however, he assented to the proposition that the École should assume the responsibility of providing funds sufficient for founding the professorship and thus enable the authorities to utilize the legacy in establishing an anatomical museum, the Musée Dupuytren, where all sorts of pathological specimens may be carefully preserved and exposed to view in well-constructed cabinets. (See photograph of this museum in the plate facing page 260.)
WORKERS IN SPECIAL DEPARTMENTS OF SURGERY: DEMOURS, DESCEMET, DELPECH, FAUCHARD, JOURDAIN, GARIOT
In modern times such special departments as those devoted to the care of the teeth, mouth and jaws, to the remedying of defective eyesight and other affections of the eyes, to the care of the organ of hearing, and to the cure of the different disorders of the pharynx, larynx and nasal cavities, have assumed the importance of independent fields of surgical activity, and as such they demand and are receiving to-day the attention which they deserve. But during the eighteenth century the practicing physician was expected to possess the knowledge and skill necessary for the relief or cure of all such bodily ills, and he was forced to accept the duties growing out of these problems as a regular part of his day’s work. In the estimation of the general public the holder of the degree of M.D. was credited—up to a comparatively recent date—with the possession of knowledge sufficient for the cure of all bodily ills; and one can now easily imagine how greatly most of these men must have suffered from the feeling that they were playing a false and ignoble part whenever they accepted—as they did in many cases of this nature—a degree of responsibility which they were wholly unable to bear.
In the present chapter I shall discuss very briefly only these three specialties: eye surgery, orthopedic surgery and dental surgery.
In the Middle Ages there seem to have been at least two men who were really skilled in eye surgery and who were widely known in the southern portion of Europe as possessing exceptional knowledge and skill in the treatment of this class of maladies. I refer to Pierre Franco, of Lausanne 231and Orange, and to Demosthenes of Marseilles. (Brief references to the work of these two will be found in the volume on “The Growth of Medicine.”) Then at Vienna, Austria, as I have stated on a previous page, there were, in the early part of the eighteenth century, Beer, Rosas, and perhaps one or two others, who did excellent work in eye surgery, and whose writings on this subject are still to-day held in high esteem as trustworthy authorities. In France, on the other hand, there were only two men who, in the early part of the eighteenth century, seem to have devoted their time and skill to the relief of affections of the eye—viz., Demours and Descemet.
Pierre Demours was born at Marseilles in the early part of the eighteenth century, began the study of medicine at Avignon, and then went to Paris for the completion of his professional training. He received his doctor’s degree, however, at Avignon in 1728, probably because the graduation fees in the latter city were not so large as those required in Paris. At a still later date he returned to the capital for the further prosecution of his professional studies, and while there he was given the appointment of Assistant to Duverney, the celebrated anatomist, who at that period, despite his advanced age (eighty years), was still actively engaged in research work. Two years later, upon Duverney’s death, Demours was invited to accept the associated positions of Demonstrator and Custodian of the Cabinet of Natural History at the Jardin du Roi. He had occupied these positions only a short time when Jean-Louis Petit, the celebrated French surgeon, who had observed the excellent character of the work performed by Demours, advised him to direct his studies more particularly to the anatomy and maladies of the eyes. Demours was quite ready to accept this advice, and thus it came about that in a few years he acquired considerable reputation as a successful practitioner in affections of the eye, a reputation which he continued to hold up to the time of his death on June 26, 1795.
Among the contributions which Demours made to the 232literature of ophthalmology the following deserve to receive special mention:—
Letter to Petit giving the report of an eye complication that developed as the result of an inoculation with the virus of small-pox; together with an account of some new observations relating to the anatomy of the eye and a few general comments on diseases of that organ; Paris, 1767.
A new series of remarks upon certain features in the anatomy of the cornea; Paris, 1770.
Observations on the structure of the corpus vitreum; Paris, 1741.
Observations on the cornea; Paris, 1741.
Dissertation on the mechanism of the movements of the pupil and on certain characteristics of the fibrae rectae of the uvea, in “Mémoires des Savans Étrangers,” tome II.; and the following articles in the “Journal de Médecine” edited by Vandermonde: “On an affection of the eyes which sometimes develops after a perfectly faultless cataract operation (extraction),” in tome XVI.; “Reply to Monsieur Descemet’s article on the cartilaginous layer of the cornea,” in tomes XXXI. and XXXIII.
Jean Descemet, born at Paris on April 20, 1732, was the pupil and friend of Duhamel-Dumonceau, one of the greatest teachers of that period and an enthusiastic scientist, but not a physician. Vicq-d’Azyr says that the list of the papers which he published during his lifetime (he was eighty-two years old at the time of his death) is very long and reveals the fact that he was interested in a great variety of topics, the majority of them relating to commerce, the arts, vegetable physiology, agriculture, and marine questions. To Descemet the influence of such a powerful mind, so enthusiastic and yet so precise in all its operations, could not fail to have been very great, and one of its earliest effects was to lead him to take a strong interest in botany and in anatomical research work. His graduation thesis, which—in accordance with the prevailing custom—he publicly defended early in 1758, dealt with the subject of the minute anatomy of the cornea and the lens. As the investigations which he made in regard to these important structures were strictly original, the scientific authorities accorded to him the honor of having his name attached to the membrane 233which lines the internal face of the transparent cornea, and which at the same time envelopes the aqueous humor. The reason why this membrane was selected by preference was this: Descemet was believed to have been the first person to describe in great detail this previously unknown structure. Demours, in 1767, published an article in which he claimed that the honor of this discovery belonged to him and not to Descemet. I cannot pretend to decide upon the justice of this claim; but, so far as I am able to learn, nobody has in modern times seriously disputed the propriety of retaining the name “Descemet’s membrane.”[25]
Descemet was held in high esteem by all his associates in the Paris Faculty of Medicine. He was generally recognized by the medical men of France to be a skilled anatomist and a careful and trustworthy observer. The various offices which he held at one time or another in the course of his active life give further proof of the correctness of the estimate which I have furnished of this admirable French physician. His death occurred at Paris in 1810.
Among his published writings the following deserve to receive special mention:—
“An sola lens crystallina cataractae sedes?”—Paris, 1758.
“Catalogues of the garden plants cultivated by the apothecaries of Paris,” Paris, 1759.
“Mémoire et observations sur la choroïde, etc.,” in “Mémoires des Savans Étrangers de l’Academie Royale des Sciences,” tome V., 1768.
In the last-named article valuable information is furnished with regard to the membrane which bears his name. Here, for instance, is revealed the fact that with advancing age the attachment of the membrane to the cornea gradually becomes less firm until finally, at the age of about sixty, it becomes completely detached.
Jacques Delpech was born at Toulouse, in the south-western part of France, in 1772. After he had completed his preliminary studies at Toulouse he went to Montpellier, 234took the regular course in medicine at the university, and was given the degree of Doctor in Surgery in 1801. While residing in that city he acted as an Officier de Santé in one of the military hospitals. The following year he was given the position of Instructor in Anatomy at the Toulouse Medical School, which at that period bore the title of “Société de Médecine et de Pharmacie.” It was here that he first manifested his great gifts as a teacher, his success in this respect being truly remarkable. In 1812 he offered himself, along with several other competitors, as a candidate for the chair of clinical surgery in the Faculty of the Montpellier Medical School, and was given this coveted position. It should be stated, however, that previous to this event, for a period of several years following his brief service as an instructor in anatomy at Toulouse, he had devoted himself with great zeal and thoroughness to the study of surgery in Paris, and was therefore specially well prepared for this competitive test. In the new field in which, from this time forward to the end of his career, he worked with unflagging enthusiasm, Delpech had ample opportunity to show to the world his great talents as a teacher of surgery.
There was one branch of surgical work in which he took a greater interest than in all the others, made many ingenious discoveries, and thus gained great distinction; I refer to the pathology and treatment of deformities, the science of orthopedics. He not only built up a large practice in cases of this nature, but he also wrote a valuable treatise on the subject. This work, which was published in Paris in 1828–1829, bears the title: “De l’Orthomorphie, par Rapport à l’Espèce Humaine, ou Recherches Anatomico-Pathologiques sur les Causes, les Moyens de Prévenir, Ceux de Guérir les Principales Difformités, et sur les Véritables Fondemens de l’Art Appelé Orthopédique.” It is, briefly stated, a complete treatise on the pathology and treatment of deformities of the human frame, one of the first (possibly the very first) of its kind published in a modern language. From statements which he makes in the course of his text it appears that Delpech recognized at an early date 235that it is upon the muscles surrounding a joint that its solidity is chiefly dependent, and consequently that all lesions involving the muscular apparatus in the neighborhood of a joint are very potent factors in the causation of deformities. In addition, he states that the absence of exact fitting of two opposite articular surfaces, one upon the other, during the period of development of the skeleton, constitutes another and very important cause of deformities both in the limbs and in the trunk. To these general causes, he says, there may be added the following: muscular debility, the effects produced by certain attitudes of the body, by the paralysis and also by the contractures of certain muscles, by the effects of rheumatism, by softening of the bones, etc.
In other sections of the treatise he discusses in a most practical and interesting manner the subjects of diagnosis and treatment of deformities. In the remarkable orthopedic hospital which he established in Montpellier he treated, with enthusiasm and untiring faithfulness, large numbers of patients suffering from deformities of all sorts, thus gaining a wide experience in this particular class of cases, and constantly increasing his skill in treating them successfully.
In the earlier years of his practice Delpech also published an important paper on the subject of hospital gangrene, under the title: “Mémoire sur la Complication des Plaies et des Ulcères, Connue sous le Nom de ‘Pourriture d’Hôpital’”; Paris, 1815. This memoir is esteemed by his biographer to be the best treatise that had been written on hospital gangrene up to the year 1834.
Delpech, says his biographer, will always be classed as one of the most distinguished professors of the Medical School of Montpellier during the early part of the nineteenth century.
On the 28th of October, 1832, he was assassinated by a merchant of Bordeaux upon whom he had operated for varicocele during the preceding year, and who, immediately after killing his victim, destroyed his own life.
236Pierre Fauchard, A. Jourdain and J. B. Gariot.—Although it is the general belief that dentistry did not become a separate and independent branch of surgical practice until a comparatively recent date, there is nevertheless some evidence that efforts were made by certain surgeons, many years ago, to engage in this special field of work. The earliest record of this fact, so far as I have been able to discover, is furnished by Francis Gribble in his book entitled: “Lake Geneva and its Literary Landmarks.” According to his statement a dentist, toward the end of the sixteenth century, applied to the Governing Body of Geneva, Switzerland, for permission to settle in that city and practice his profession. As the civic authorities, however, did not appear to comprehend just how much risk, either to the bodies or to the souls of the Genevese, was involved in granting the desired permission, they referred the question to Théodore de Bèze, the great theologist, who, in the temporary absence of John Calvin, was acting as the Syndic or Mayor of the city. We are not told by Gribble how the matter was at last decided, but there can be scarcely any doubt that the dentist was finally permitted to hang out his shingle and go to work.
The explorations made among the ruins of ancient Egypt show that even at that remote period, three or four hundred years before the Christian Era, there were men who knew how to fill carious cavities in human teeth and to perform other surgical acts which call for the skill and knowledge of the practical dentist. But the discovery of such isolated facts does not demonstrate clearly that dentistry was practiced at that early period as a special department of the surgical art; and, furthermore, many centuries after that date elapsed before there was discovered any further evidence that dentistry had survived during the long intervening period. In fact, the records do not throw much light on this subject until we reach the seventeenth century. Then it appears that a certain Alexandre Poteler, during the latter part of that century, attained considerable celebrity, in France, as a skilful and experienced dental surgeon. Further details concerning this man are lacking.
237Sprengel, in his history of medicine, mentions the names of several men—Germans, French and English—who during the early part of the eighteenth century occasionally performed operations in the field of dentistry, but among this number I find only three who appear to have attained eminence in their special line of work—viz., Pierre Fauchard, A. Jourdain, and J. B. Gariot. I will furnish here the few details which I have been able to obtain concerning the career of these men.
Pierre Fauchard was born in France toward the end of the seventeenth century. After receiving the regular training of a physician he entered the service of the Royal Navy, ultimately attaining the rank of Surgeon-Major. Subsequently, having first taken a special course of instruction under Alexandre Poteler, he settled at Paris and practiced dentistry in that city for a period of more than fifty years. During the course of his career he published a treatise on the surgery of the mouth, and in the preparation of this work he received efficient aid from Jean Devaux (1649–1729), one of the most learned surgeons of his time in France. This treatise, according to the testimony of his biographer, contains many reports of cases which were observed by Fauchard in actual practice; and, he adds, the book still possesses considerable value as a work of reference. Among the unusual pathological conditions described and occasionally pictured the following deserve to receive special mention:—“Abscess or Softening of the Dental Pulp without Recognizable Alteration of the Cortical Substance” (relief was obtained by trephining the tooth); “Defective Teeth of Many Different Kinds,” and the proper manner of remedying such defects, both in cases where only a part of the tooth is defective, and also in those where it is found necessary to supply an entire tooth or even several teeth; “On the Art of Remedying Defects in the Palate”; “On the More Extensive Employment of Lead Fillings, etc.” The treatise here referred to bears the following title: “Le Chirurgien Dentiste, ou Traité des Dents, etc.,” with 40 engraved plates; 2 vols., Paris, 1728; a second 238edition, which was published in 1746, contains many important additions.
Anselme-Louis-Bernard-Brechillet Jourdain, who was born in Paris, November 28, 1734, was one of the most distinguished French physicians of the eighteenth century who devoted himself largely to the study and practice of dentistry. He was also interested in medical science generally, having acted for several years as an associate editor of the Journal de Médecine. Among the treatises which he wrote on topics relating to dentistry the following deserve to receive special mention:—“Nouveaux Élémens d’Odontalgie,” Paris, 1756; “Traité des Dépôts dans le Sinus Maxillaire, des Fractures et des Caries de l’Une et de l’Autre Mâchoire; Suivi de Réflexions et d’Observations sur Toutes les Opérations de l’Art du Dentiste,” Paris, 1760; “Essai sur la Formation des Dents, Comparée avec Celle des Os, Suivi de Plusieurs Expériences, tant sur les Os que sur les Parties qui Entrent dans leur Constitution,” Paris, 1766; and “Traité des Maladies et des Opérations Réellement Chirurgicales de la Bouche et des Parties qui y Correspondent, Suivi de Notes, d’Observations Interessantes, tant Anciennes que Modernes,” Paris, 1772, 2 vols.
Jourdain’s death occurred on January 7, 1816.
Jean-Baptiste Gariot was born in France during the latter half of the eighteenth century. The French records furnish very scanty information concerning his professional career. For example, among other matters of minor importance, it is stated that he was a member of the Royal College at Madrid, that he was the dentist of the King of Spain, and that he published a treatise which bears the following title: “Traité des Maladies de la Bouche,” together with an account of the structure and functions of the parts that enter into the formation of the mouth, the diseases to which these parts are liable, the means that may be employed for maintaining them in health and beauty, and the different operations which belong specially to the domain of the dentist; with 15 plates, Paris, 1805.
The two most distinguished military surgeons in Europe during the eighteenth and nineteenth centuries were Desgenettes and Baron Larrey, both of them natives of France.
Aimé-Nicolas Dufriche Desgenettes was born at Alençon, France, in 1762. His early medical training was obtained at the University of Montpellier, and the degree of Doctor of Medicine was bestowed upon him in 1789. Four years later he entered the French military service and participated in the campaign of Egypt and Syria, during which he rapidly rose to the position of Chief Physician in that part of the army which was officially designated as the Army of Italy. In 1802, after the close of the campaign, he was appointed First Physician of the Military Hospital at Paris, and at the same time was given the position of General Inspector of the Health Department of the Armies. From that time to the year 1814 he visited, in his official capacity, Russia, Prussia and Spain; and amid scenes of carnage and destruction he never failed to display the character of a high-minded physician, a benevolent and guardian spirit. His career as a medical officer was largely that of a man of action, who exhibited at the same time a keen sympathy for those who stood in need of his services. To quote the words of his biographer, “he extended his cares to the sick of all nations,—to the Turk and the Christian, to the men of the South as well as to those of the North, and, as disinterested also as the Great Hippocrates, he retired poor from his labors, though he might easily have made himself rich. Often placed in opposition to military power and faction, he always exhibited an unwavering inflexibility and energy of character. His thorough knowledge 242of men and things, his skill in the practice of his art, and his vigorous and unbending mind distinguished him for more than twenty years at the head of the medical service of the French armies.”
This splendid showing, I venture to remark, could scarcely have been realized if Bonaparte had not been endowed with two admirable traits of character. In the first place, he seemed to possess almost infallibly correct judgment in his choice of men who were to act as generals or as chief surgeons of his various armies; and then, in the second place, he was in the habit of supporting these men loyally whenever, later on in their career, disputes arose as to the wisdom or patriotic purpose of their decisions. The history of the wars that occurred from 1793 to 1814, between France and the different European nations which opposed her, abounds in instances that confirm the truth of what I have just stated. Corvisart, it is also highly probable, deserves much of the credit for Bonaparte’s loyal treatment of his chief army surgeons.
The biographer of Desgenettes relates two occurrences which throw additional light upon the nobility of character of this admirable physician. These occurrences are briefly narrated as follows:—
A contagious disease appeared in the Army of the East and spread rapidly from one man to another. The soldiers were struck with terror and despair, and were ready to die, merely because they considered death imminent and inevitable.... Monsieur Desgenettes assured them that the hideous buboes with which they were covered were not symptoms of the plague, and he proved it. How? By the following heroic experiment. He took the matter of these buboes and inoculated himself in the presence of the soldiers. This proof was conclusive in their eyes, hope was again kindled in their bosoms, and the mortality diminished. Here is one of those brilliant actions which history delights to preserve and transmit from age to age.

DESGENETTES
On another occasion Desgenettes manifested equally great courage. The occurrence is narrated by his biographer in these words:—
Made prisoner in the retreat from Russia, he demanded boldly 243his liberty, not as a favor, but as a right; he invoked the sacredness of his ministry and in particular the cares which he had lavished alike on the Russians and on the French. An imperial ukase immediately rendered him his liberty. The Emperor Alexander called him into his presence and expressed to him his sentiments of high esteem and regard. He received soon after from Sweden the order of the Polar Star.
Desgenettes’ death occurred in 1837. He made no contributions to medical literature; and his enemies brought against him the charge that, when he delivered a lecture, he spoiled it by telling too many anecdotes about the different wars in which he took part.
Jean-Dominique Larrey was born in 1776 at Baudéan, a French village at the foot of the Pyrenees. At the age of thirteen years, shortly after the death of his father, he quitted his native village and came under the care of his uncle, Alexis Larrey, who was Surgeon-Major and Professor at the Hospital of Grave, near Toulouse. Under the wise and kindly guidance of the latter he pursued his studies so earnestly and with such intelligence that he was able, on attaining his twentieth year, to pass successfully the examinations required for an appointment to the position of Assistant Surgeon in the French Navy.
The sloop-of-war “La Vigilante,” the vessel in which he gained his first experience in the naval service, met with disaster and Larrey was nearly shipwrecked. As soon as possible after this thrilling experience he went to Paris and took service in the great Hospital of Hôtel-Dieu, under the orders of the famous surgeon Desault. This was at the beginning of the severe winter of 1789, an eventful time in the history of France. The Revolution was now in full swing, and Larrey not only was an eye-witness of the troubles which characterized its early stages, but he also had the opportunity, under the orders of Desault, to render professional service to the first victims of those tragic days. Three years afterward, while serving in the Army of the Rhine, under the command of Marshal Luckner, he was able to put to good use all the admirable surgical training which he had received under Desault at the Hôtel-Dieu.
244When Larrey was about twenty-one years old and while he was attached to that part of the French Army which was then stationed in the vicinity of Milan and Venice, he interested himself actively in the establishment of an army ambulance service. Already three or four years earlier he had become sensible of the inconveniences of the French ambulances which were then in use. In the first place, these vehicles were of such a type as to be ill-suited to the work which they were intended to perform; they were too heavy to be driven with reasonable speed to and from the battlefield, and they were also so rigidly constructed that at every irregularity in the ground over which the wheels passed the wounded soldier experienced a painful jolt. Then, in the second place, aside from the faulty construction of these vehicles, the regulations governing their management were so badly planned as to leave the wounded lying unaided on the battlefield sometimes for several hours together. It was customary, for example, to station the ambulances at a spot about three miles distant from the troops who were shortly to engage in combat, and they were not despatched to the battlefield until after the fighting had ended. In this way hours often elapsed before the wounded could receive any aid whatever from the surgeon.
In working out a solution of this complex problem Larrey’s very practical mind quickly reached certain conclusions: first, that it was most important to remove the wounded from the battlefield to a place of safety much earlier than had hitherto been the custom; and, second, that the type of ambulance then universally employed was altogether too heavy and too rigid to serve well the purposes for which it was needed. He realized fully that this last part of the problem was the more important part, and that, if he could invent a less ponderous and at the same time more elastic vehicle for use as the field ambulance, he would by this very act be placed in a position where he could effect in a large measure a solution of the second half of the problem.

BARON LARREY
Larrey promptly set about the work of providing a new type of field ambulance and in a short time was successful 245in obtaining a most useful vehicle for the purpose. It is described by his biographer in the following words:—
This invention of Larrey’s was a kind of carriage hung on springs, uniting great strength and solidity with lightness. Such indeed was its lightness that it was able to follow all the movements of the advance guard with as much speed as flying artillery. These ambulances volantes, as they were called, were first used by the French in a defile of the Rhine near Koenigstein. Here the ambulances invented by the talented and benevolent French surgeon bore the wounded rapidly away from the neighborhood of the enemy instead of leaving them either to die or to sustain a protracted agony on the field of battle.
In this work of inventing a field ambulance of a greatly improved pattern Larrey revealed an exceptionally fine trait of character, viz., a strong desire to utilize his talents and the opportunities afforded by his official position for the benefit of his fellow men, both the wounded of the French army and those of the enemy forces. He revealed the same trait in many other ways—as, for instance, when he took infinite pains, after a battle, to provide proper shelter, food and care for the wounded in the town or village nearest to the site of the conflict, and that too in a part of the country which belonged to the enemy. He revealed it again in the fighting which took place in Eastern Prussia and in the course of the numerous retreats which Napoleon’s army was forced to make in the Russian campaign.
Among the incidents which occurred during that long and disastrous retreat of the remnants of Napoleon’s army from Moscow there was one which reveals in a very clear light the high sense of duty that characterized Larrey’s actions as Surgeon-in-Chief of the French Army and the complete faith which the individual soldiers composing that army—or at least the better disposed among them—placed in his disinterested and loyal service in their behalf. The incident to which I have reference occurred while the disorganized French troops were crossing the Beresina River and is thus described by Larrey’s biographer:—
The Russian general arrived at the head of 50,000 men and began the fire among the division of General Partonneaux, the soldiers of 246which division immediately wished to cross the Bridge all at once. The conveyances collided with one another, and some of the unfortunate men were crushed, while others, losing all spirit, threw themselves into the stream.... There was throughout a frightful mixture of imprecations, of clashings, and of strugglings, whence arose indescribable disorder and a breaking of the overloaded bridge. The Russian Army approached, and with its formidable artillery tore the ranks of the French mob of soldiers.... In this immense disaster what had become of the distinguished Surgeon-in-Chief of the Grand Army? After having crossed over the Beresina with the Imperial Guard, he discovered that requisites for the sick and wounded of his countrymen had been left on the opposite bank. With equal humanity and heroism, he recrossed the river, and hardly had he done so when he was surrounded by a wildly excited crowd. He was almost suffocated in the midst of it.... No sooner was he recognized than he was carried back with great rapidity in the arms of the soldiers across the river. On all parts was heard the cry, in nearly these words, “Let us save him who saved us!” The soldiers almost forgot their own safety in their desire to preserve an officer whose tender kindness they had so often experienced.
I believe that I have now shown with sufficient fulness of detail what were the prominent characteristics of Larrey as a man and as an executive army medical officer. It still remains for me to furnish some evidence of the excellent judgment which he displayed in his work as a practical surgeon.
In one of the French hospitals, during the war, Larrey’s attention was called to a Russian soldier who had been shot in the forehead by an iron ball weighing 217 grammes. This projectile had pierced the frontal bone above and a little to the outside of the right eyebrow, and had penetrated into the interior of the skull. Despite the bulk of this iron ball, the opening which was perceptible in the bone did not exceed six or eight millimeters in diameter, and, by introducing a small probe, one might feel the ball. The smallness of the opening in the bone, says Larrey, may be explained by the elasticity of the osseous fibres, some of which the ball would have to push aside in order completely to penetrate the outer table of the frontal bone, and which consequently would yield instead of fracturing. In the present 247case the bony angles at the edge of the circular opening were cut away by the surgeon and the opening itself was made large enough to permit the removal of the ball by means of an elevator and pincers. A great quantity of coagulated blood and some small fragments of bone were then evacuated. The brain itself presented at this spot a depression of about seven millimeters in depth. In a short period of time the wound healed, and apparently complete recovery followed.
In order to judge correctly of the credit which rightfully belongs to Larrey for his successful treatment of this case of gunshot wound of the skull and underlying brain, one must remember that in the early part of the nineteenth century it was considered a very bold surgical act to operate upon the injured brain, and particularly so in the almost complete absence of adequate surgical equipment.
As an instance of Larrey’s quickness in meeting an emergency I will narrate here very briefly an experience which he had at Smolensk, Russia. When the French troops entered that city, after a severe battle, they found that the inhabitants had already fled, owing in part to the fact that many of their dwellings had been destroyed by fire. Larrey, as soon as was practicable, converted fifteen of the largest buildings which had not been devastated by the flames, into hospitals for the wounded. Unfortunately, all supplies or stores of any kind had either been destroyed by the enemy or removed by them in their orderly and premeditated retreat. For the large number of wounded there was a deficiency of linen and splints; but Larrey discovered a store of archives in one of the buildings which had escaped the fire, and he promptly substituted sheets of paper for linen and utilized the thick parchment covers for splints. He toiled with little intermission night and day, and the French surgeons generally, in imitation of their chief, were indefatigable in their attention to the wounded, who were about 10,000 in number.
Las Cases, in his “Memorial of St. Helena,” published after he had returned to Europe, reports Napoleon as having uttered the following words on October 23, 1816: “What 248a man, what a brave and worthy man is Larrey! What care was given by him to the army in Egypt and everywhere! I have conceived for him the highest esteem. If the army were to raise a column to the memory of any one, it should be to the memory of Larrey. He has left in my mind the idea of a truly honest man.” In his will Napoleon wrote: “I bequeath to the Surgeon-in-Chief of the French Army, Larrey, 100,000 francs. He is the most virtuous man I have ever known.”
The reader will pardon me, I am sure, if I furnish here additional proof of Larrey’s sound judgment in questions of a purely surgical nature. He insisted, for example, on the importance of promptly resorting to amputation in cases where the gunshot wound had caused a complicated fracture of the bone or had inflicted serious destruction of the soft parts; and he particularly recommended this course of action in the case of individuals who were cachectic or below par. He expressed himself in favor of the circular incision in preference to that which was intended to furnish flaps. (From “Mémoire sur les Amputations, etc.,” Paris, 1797.)
In another place Larrey mentions, somewhat in detail, the reasons why primary amputations are to be given the preference in military surgery. They are the following:—
(1) The inconvenience which attends the transportation of the wounded from the field of battle to the military hospitals on badly constructed carriages; the jarring of these wagons produces such disorder in the wounds and in all the nerves, that the greater part of the wounded perish on the way, especially if it be long, and the heat or cold of the weather be extreme.
(2) The danger of remaining long in the hospitals. This risk is much diminished by amputation; it converts a gunshot wound into one which is capable of being speedily healed, and obviates the causes that produce the hospital fever and gangrene.
(3) In case the wounded are of necessity abandoned on the field of battle: In this event it is important that amputation should have been performed, because—when it is completed—they [the wounded] may remain several days without being dressed, and the subsequent dressings are more easily accomplished. Moreover, it 249often happens that these unfortunate persons do not find surgeons sufficiently skilful to operate, as we have seen among some nations whose military hospitals were not organized like ours. (From Vol. 2 of Larrey’s “Memoirs of Military Surgery.”)
(In judging the quality of the advice given here the reader should not overlook the fact that it was pronounced in the early part of the nineteenth century.)
Larrey’s death occurred on July 24, 1842. A few years previous to this date he had received the title of Baron.
A FEW OF THE IMPORTANT HOSPITALS AND THE PRINCIPAL ORGANIZATIONS IN PARIS FOR TEACHING MEDICINE AND MIDWIFERY
John Cross, the author of an excellent memoir entitled “Sketches of the Medical Schools of Paris,” has written such a full and satisfactory account of la Maternité and its admirable teaching machinery that I shall not hesitate to use it freely as my guide in preparing this and the following chapters. I am the more ready to adopt this course because, first, I have had no personal experience whatever with this department of medical science, and, second, because Dr. Cross’ account is not compiled from the writings of other physicians, but is based upon his own personal observations and upon information which he derived at first hand from Monsieur Chaussier, the Physician-in-Chief of the hospital. Here is what he writes (1815) upon this important subject:—
The midwifery department of l’Hôpital de la Maternité is converted to an admirable purpose by being made a school for the educating of Sages-Femmes (midwives); and I was not a little surprised at my first entering this hospital with Monsieur Chaussier, the Physician-in-Chief, to find the wards crowded with female students. This midwifery-school was founded about twelve years ago (about 1803), since which time young women have come annually from all parts of France to study there. Some pursue their education at their own expense; but most of them are chosen by the Prefets of the different Départements of France or by the governors of country hospitals, by whom all expenses are paid. For six-hundred francs these women are lodged, boarded and educated, during one year. They reside in the hospital, and cannot go out of its precincts without permission. After a twelve-months residence and an examination, they receive their diplomas from l’École de Médecine—or the Faculté de Médecine—to practice as midwives.... 254They follow the Physician and Surgeon in their daily visits, and each pupil makes a clinical report in writing of the patients under her care. The accuracy and minuteness of some of these reports, presented to Monsieur Chaussier during his visit, could not have been greater if they had been made by an experienced practitioner....
During the first five years of the existence of this École d’Accouchement, nearly five-hundred well-educated women were sent to practice midwifery in different parts of France.... In June, 1814, the month in which the new students are admitted, and those who have finished their education are dismissed, one-hundred and thirty, who had followed the lectures and practice of midwifery at la Maternité during the preceding year, were examined, and received certificates of their being qualified to practice as accoucheuses.... Monsieur Baudelocque was, to the time of his death, a zealous promoter of this school of midwifery, and a copy of his catechism sur les Accouchements is given to each pupil as soon as she is admitted. This school is an institution which, from the novelty and excellence of the plan, the manner in which it is carried on, and the benefits that must spring from it to society, does honor to the country which has founded and supported it.... Les Élèves Sages-Femmes who reside for twelve months at l’Hôpital de la Maternité, and about whose instruction so much pains are taken and so much attention bestowed by the medical men attached to it, are, there can be little doubt, quite as good practitioners at the completion of their education, as the male students in midwifery in any country.
What is here written by Dr. Cross refers to the condition of la Maternité as he found it in 1815,—that is, after the institution had been in successful operation for nearly if not quite twenty years. To go back to the time when it was first organized I should state that, upon the breaking up and disorganization of the Faculté de Médecine and the École de Chirurgie, there was erected, upon the ruins of these, l’École de Santé, in which Baudelocque was given the place of Professor of Obstetrics; and at the same time he was appointed “Surgeon-in-Chief and Accoucheur” of the recently established Maternité. From the very first both the general public and the great majority of physicians reposed almost absolute confidence in Baudelocque, and 255consequently it is not strange that he was the guiding spirit in the development of this important hospital and training school.
Sprengel, the author of one of the earliest and best histories of medicine, gives unlimited praise to Baudelocque for the clearness, practical character and conciseness of his writings on the subject of midwifery. His treatise on obstetrics, he adds, is decidedly superior to that of the English surgeon, Thomas Denman, whose writings, which cover the same field, were published at about the same period of time.
As to the details of the management of la Maternité, the mortality experienced, the number of infants born, etc.... I must refer the reader to Dr. Cross’ memoir, in which he gives, in addition, an account of the somewhat similar work done at the famous Dublin Lying-in Hospital. There remain, however, a number of interesting details concerning the life and career of Baudelocque which cannot well be omitted from this sketch, and I will therefore proceed at once to supply them here.
Professional jealousy, which seems to have existed in those days in a particularly virulent form, left Baudelocque very little peace of mind and undermined his health to a serious degree. One of the most striking experiences of this nature is the following:—
A certain Dr. Sacombe set out to increase his reputation—or, rather, to gain notoriety for himself—by attacking violently all those physicians who sanctioned the operation of Caesarian section as permissible in certain cases; and, inasmuch as Baudelocque was the most distinguished one among these physicians, he directed his most violent efforts against him. There having recently occurred, in the latter’s practice, a case of tedious labor in which it had been found necessary to remove the head of the foetus by amputation, Dr. Sacombe intimated that Baudelocque in this instance had been guilty of what apparently amounted to a double murder. Both public opinion and the courts were very prompt in judging this to be an infamous calumny on the part of the accuser. Although Baudelocque was completely exonerated from the charge, he nevertheless suffered 256keenly from the brutality of this attack upon his character. In fact, it was believed that the cerebral affection from which he died on May 2, 1810, was brought on by the worry which was associated with Dr. Sacombe’s attack. Shortly before his death the news reached him that he had been chosen to take charge of the Accouchement of the Empress, Marie Louise, but even this vindication failed to be of any benefit at that late hour.
The two most important treatises published by Baudelocque are the following: “Principes de l’Art par Réponses, en Faveur des Élèves Sages-Femmes,” Paris, 1775. This work was written entirely for the guidance of midwives, the Government purchasing 6000 copies. “l’Art des Accouchements,” Paris, 1781, 2 vols. Later editions were published in 1789, 1796, 1807, 1815 and 1822. Baudelocque also published a number of memoirs and reports of cases.
The success of la Maternité as the great French Lying-in Hospital and Training School for Midwives was probably as much due to the wise and painstaking management of the widow Lachapelle as to the skill and great experience of Baudelocque. It is therefore only fitting that I should give here a brief biographic sketch of this admirable woman.
Veuve Lachapelle, whose maiden name was Marie-Louise Dugès, was born at Paris on January 1, 1769. Her mother, Marie Jonet, was at first a sworn midwife (“Sage-Femme Jurée”) at the Chatelet Hospital, but later (1775) she was promoted to the position of Midwife-in-Chief of Hôtel-Dieu, the largest hospital in Paris. Madame Jonet made her home in Hôtel-Dieu, and she performed the duties of her very responsible office with such zeal, such conspicuous ability, and such faithfulness that the Government awarded her, when she retired after a long service, a liberal pension. The daughter Marie, who had been brought up with great care under the constant supervision of her mother, and who had lived from day to day as it were in the midst of pregnant women and women actually undergoing confinement, absorbed unconsciously a great deal of 257information, both theoretical and practical, concerning the art of midwifery. Although she married, in 1792, Monsieur Lachapelle, the Resident Surgeon of the Hôpital Saint-Louis, she continued her residence at Hôtel-Dieu, with her mother, to whom she was strongly attached; and after the death of her husband, which occurred not long after they had been married, this attachment rather increased. Madame Lachapelle, who from this time onward was known as Veuve Lachapelle, showed such a keen interest in her work and performed all her hospital duties with such skill and such excellent judgment that in 1795 the Government appointed her the Associate Chief Midwife of Hôtel-Dieu.
At a somewhat later date, during the administration of Minister Chaptal, the Maternité Hospital was organized, and Madame Lachapelle was made the Resident Directress of the new institution. Baudelocque was appointed Surgeon-in-Chief and Professor of Obstetrics, and Madame Lachapelle was given the position, under him, of Instructress in Midwifery. François Chaussier, Baudelocque’s successor and one of the most distinguished French physicians of that period, declared that Madame Lachapelle was a most successful teacher of the art of midwifery, and added that her usefulness in this field extended far beyond the period of her active connection with the Maternité Hospital; for she had made a regular practice, during her residence in that institution, of keeping an immense number of carefully prepared records of the cases which came under her observation, and these, which form the basis of the volumes published after her death, by her nephew, constitute—as Chaussier believes—a most useful work of reference, second in value only to the great work of Baudelocque.
Veuve Lachapelle’s death occurred on October 4, 1821. The work referred to in the preceding paragraph bears the following title: “Pratique des Accouchemens, ou Mémoires et Observations Choisies sur les Points les plus Importans de l’Art,” publiées par Antoine Dugès, neveu de l’auteur, Paris, 1821–1825, 3 vols.
FURTHER DETAILS CONCERNING THE PARIS FACULTÉ DE MÉDECINE AND CONCERNING SOME OF THE LARGER HOSPITALS OF PARIS
The present chapter is intended to supply, in as condensed a form as possible, some of the facts relating to the growth of the Paris School of Medicine, and also information concerning one or two of the larger hospitals of Paris. As such details are not likely to possess interest for more than a comparatively small number of my readers I unhesitatingly advise all others to skip this chapter.
“The Medical Schools[26] of the Rue de la Bûcherie,” says Chereau, “are still in existence to-day (1866), although somewhat altered in appearance. They stand at the angle formed by the Rue de la Bûcherie and the Rue de l’Hôtel Colbert. These buildings, however, masquerade under singular forms. Since the day when our fathers in medicine abandoned the Temple of Aesculapius (1775) it has been put to a great variety of uses, such as a public lavoir, a tap room, a cabaret where thieves meet, rooms equipped each with a number of beds, and a lupanar, where the fee charged was twenty sous a sitting; the room in which Riolan taught anatomy converted into a low-down billiard saloon; the ground over which Femel walked, soaked with all sorts of nasty fluids; the office in which sat the employés of the school—those vigilant guardians of the rights and dignity of the Faculty—plastered with police ordinances; the chapel, in which the doctors were wont piously to attend mass, now occupied as a miserable lodging-house; etc.”

Eighteenth-century plan showing the relations of the Paris École de Médecine to Hôtel-Dieu, the Cathedral of Nôtre Dame and the River Seine.
(Reduced copy of the cut printed in Franklin’s “La Vie Privée d’Autrefois,” 1892.)
In 1808 the Faculté de Médecine was given the splendid quarters of the Collège de l’Académie de Chirurgie, where 259it is still to-day located. Clinical instruction was carried on at Hôtel-Dieu, La Charité and certain other hospitals. The school itself is no longer called “l’École de Médecine,” but “la Faculté de Médecine,” and the old building, suitably modified, has been preserved—not as a part of the present school, but as a sort of clubroom or social hall for the use of all the university students. (See accompanying illustrations facing page 260.)
Écoles de Santé.—When the statement was made before the Convention that the Army of the Republic had lost about 600 medical officers, and that the troops in the eastern Pyrenees were almost entirely without physicians and surgeons, a law was passed (December 4, 1794) authorizing the organization at Paris, Montpellier and Strassburg, of three medical institutes or secondary medical schools (designated as “Écoles de Santé”). They were originally intended to be simply temporary organizations where “officiers de santé” might be trained for service in the hospitals,—more particularly the military and naval hospitals. Each of the Départements of France was entitled to send one pupil to be educated at one of these military medical schools, at the expense of the nation, for a period of three years. In accordance with this scheme Paris received 300 pupils, Montpellier 150, and Strassburg 100. Owing to the lack of places or schools where young men might, at their own expense, be trained as physicians, it soon became necessary to permit men of this class to attend these schools. And so in 1796 the Medical School at Paris was reorganized and provision made for the following twelve professorships:—
In 1798 a chair for pathological anatomy was added, and there were also organized several special clinics—one, for example, for sexual diseases; and among the names of the professors who taught at this period are to be found those of Sabatier, Chopart, Pinel, Corvisart, Baudelocque, Lassus, and P. A. O. Mahon. The last-named lectured on the history of medicine. No fees were charged for tuition. Under this new régime the Paris Medical School rapidly rose in favor, until in 1799 the attendance had reached the extraordinary total of 1500. In addition to the regular students who expected to receive a medical diploma if they passed a satisfactory examination at the end of the course, there was a large attendance of quacks, at all three of these schools (Paris, Montpellier and Strassburg). Neither a diploma nor any special permit, however, was required of those who wished to engage in the practice of medicine. This state of affairs soon led to frightful abuses, and the Convention accordingly passed a new law (March 10, 1803), which stated that, for the future, only those who had passed a satisfactory examination in the fundamental branches (anatomy, physiology, pathology, materia medica, pharmacy, chemistry, hygiene, obstetrics, surgery and internal medicine) would be permitted to engage in practice. The duration of this course of training was four years, and the candidate was further required to furnish satisfactory evidence that he had completed the regular Lyceum course of studies (equivalent to the undergraduate course at one of our American Colleges) before he entered upon the medical course.
1. The side of the Paris Faculté de Médecine which fronts on the Rue de l’École de Médecine.
(From “La Vie Universitaire.”)
2. View of the former École de Médecine since it has been incorporated with the new structures of the Faculté de Médecine.
(From “La Vie Universitaire.”)
3. Musée Dupuytren. Formerly the refectory of the Convent of the Cordeliers (Franciscans), built in the fifteenth century.
(From “La Vie Universitaire.”)
On the plea that the people who dwelt in the country districts live simpler lives, etc., and consequently are subject to illnesses of a less complicated nature, there was passed by the National Convention another law in accordance with which a lower grade of doctors was created—i.e., practitioners who were called Officiers de Santé. At first these men were given permission to practice after they had completed 261the third year of the regular course of studies, but later they were absolved from the necessity of taking any part of the regular course, provided they could show that they had spent five years in work connected with a hospital or had been in the service of a regular physician during a period of six years. Gradually, as the number of the regular physicians increased and as the country became more prosperous, the Officiers de Santé diminished in number. In 1847 there were 7456 such practitioners, but already in 1872 the number had fallen to 4653. On the other hand, the regular doctors of medicine had increased during the same period from 10,643 to 10,766.
In 1864 an attempt was made in the French Parliament to abolish the institution of Officiers de Santé, but one of the members, Bonjean, opposed the motion and it fell through. The argument which he brought forward and which is quoted by Puschmann, is essentially the following:—
When simple people belonging to the poorer class of the community are taken ill they want a physician who is himself simple and poor like themselves, a man who is able to comprehend the language and the needs of his modest patients, and who, because of his low birth, because of the fact that he has been habituated from early childhood to the plain and simple living of the peasant’s cottage, and also because he has been put to comparatively small expense to secure the grade which permits him to practice the profession of medicine, is quite contented to accept a modest fee for his services. The Officier de Santé is, for all these reasons, admirably fitted to fulfil his mission of modest devotion; for him, under these circumstances it will be comparatively easy to act as the confidant, the counsellor, and the sympathetic friend of the patient.
It is not possible for me to state (1919) how far the recent war has upset all the arrangements mentioned above.
Parisian Hospitals.—Of the three large hospitals which existed in Paris at the beginning of the nineteenth century—the Hôtel-Dieu, la Charité and la Salpétrière—I am not able to furnish more than a few scanty details. According to an editorial which I find in the London Lancet for November 25, 1837, the management of the English hospitals 262destined for the relief of the sick poor during the period now under consideration was inferior to that of the similar institutions in France. There are good reasons for believing, however, that, after the lapse of a few years, the English hospitals became in every respect the equals of those in France. In Tenon’s elaborate report on the Parisian hospitals examined by him in 1816 I find it stated that la Salpétrière was used in part as a prison and in part as an asylum for the insane; but, in another part of this report, he states that at one time this hospital sheltered as many as 8000 persons, the great majority of whom were legitimate hospital patients.
Of Hôtel-Dieu John Cross, in his memoir concerning medical education in Paris, makes the following remarks:—
The patients at l’Hôtel-Dieu vary in number from 1500 to 2000, and generally approach near to the latter number. Beside the wards for medical and surgical patients, there is a ward for the reception of women actually in labor or suffering abortion. The medical patients are far the most numerous, and eight or nine physicians are attached to Hôtel-Dieu.... The number of dressers is not limited; when I was at l’Hôtel-Dieu, above one-hundred were attached to it.... Les élèves internes of the Parisian hospitals correspond to our house-surgeons; the number of them to each hospital is limited, and at l’Hôtel-Dieu there are nearly twenty. They have their separate apartments in the hospital, are boarded in it, and have, beside board and lodging, an annual salary of about twenty guineas each. They may retain their situation for two years.

Device of the École de Médecine de Paris. (Adopted by the Faculty in 1597.) (Three storks, each holding a twig of origanum in its beak; and at the top of the design the motto “Urbi et Orbi Salus” [Health to the City and to all the World].)
Paris possesses a fourth large hospital, which as regards architectural beauty and the great consideration shown by the architect for a wise and convenient disposition of the different available spaces, certainly stands first among the hospitals of the French capital. I have introduced here a reduced copy of the plan of this hospital (Hôpital Saint-Louis), which dates back to the seventeenth century, but, much as I should like to do so, I am not able to furnish a description of the details relating to the precise purposes and the management of the institution at the present time. 263It is said to be largely devoted to the treatment of affections of the skin.
Tenon’s Criticisms on Hôtel-Dieu and Hôpital Saint-Louis.—Speaking of the wards in the Hôpital Saint-Louis Tenon, who wrote his treatise in 1786, says that it was a mistake to make the ceilings only eleven feet high; they should have been sixteen feet high. He commends strongly the complete separation of the hospital from the adjacent city by high surrounding walls. Only one kind of contagion, he says, should be admitted into any single ward. This precaution had not previously been observed. In the Hôpital Saint-Louis the water-closet arrangements were about as bad as they could possibly be. The same remark applies to Hôtel-Dieu, where overcrowding was at times scandalously bad. In the latter hospital there are, in the wards destined for men, 600 beds—of which number 378 are beds of the larger size, and 222 of the smaller. In the wards for women, he adds, the same predominance of large beds exists—viz., 355 larger beds, 264 of the smaller size.
Tenon says emphatically: “Beds for two or more persons should not be permitted in any hospital. These beds, on certain occasions, are occupied by four—yes, even by six persons—and as a result they are infested by vermin. Sleep is practically unattainable under such circumstances.”[27]
Planned by the architect Claude Chastillon, of Paris, in 1608.
A. Wall surrounding hospital grounds.
B. Main entrance.
C, D. Court separating the first and second enclosed spaces.
C. Entrance to second enclosure, through the porter’s lodge.
D. One of the four buildings placed at the corners of the principal square; the members of the Religious Sisterhood occupy the building as their convent.
264E. Gallery of communication between the convent and the wards of the hospital.
F. Another of the four corner buildings; it is destined for the use of the priests and the surgeons, and communicates with the hospital wards by means of a covered gallery like that shown at E.
G. Entrance to men’s promenade, to the reservoir, and to the cemetery.
H, I. Buildings in which may be lodged, during the prevalence of an epidemic, such citizens as may be affected with some contagious disease.
K, L, M, and N. Gardens belonging respectively to pavilions L, H, F, and D.
O. Lodge occupied by four gardeners.
P. Royal pavilion, not used after the Revolution.
Q. Open space planted with trees.
S. Church.
T. Kitchen, etc.
U. Bakery, wine cellars, etc.
V, X. Lodging rooms for cooks and bakers.
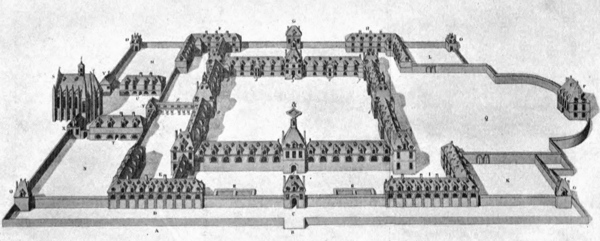
Hôpital Saint-Louis, Paris. Planned and drawn by Claude Chatillon, architect, in 1608.
(Copied from Tenon’s “Mémoires sur les Hôpitaux de Paris,” Paris, 1816; reduced about one-half.)
In the preface to his “Bibliothèque de Thérapeutique,” which was published first in 1828, A. L. J. Bayle says that the art of treating diseases has been greatly neglected, in comparison with the enthusiastic efforts made to promote some of the other branches of the science of medicine, especially that of pathological anatomy; and, as a result, this art has in reality actually retrograded. Indeed, he goes on to say, quite a large number of agents which, up to a recent date, had been considered efficient remedies, have been entirely forgotten or even, in some instances, proscribed. This unfortunate tendency, he adds, may be attributed to many different causes. One of the most important of these, he believes, is to be found in the fact that certain physicians have allowed the idea to take root in their minds that the lesions which have been discovered in the different organs of the body at post-mortem examinations were the cause of the symptoms that, taken in the aggregate, constitute the particular disease under consideration; and, acting under the influence of this idea, they have assumed that their therapeutic efforts should be directed solely to these lesions. “Experience has not confirmed the correctness of this theory; on the contrary, it has shown that, if pathological anatomy is useful to the practitioner, it is chiefly so because it throws light upon the course and prognosis of certain diseases, and not because it has furnished a basis upon which the treatment may be built up.”
There is still another equally strong reason, says Bayle, why the art of therapeutics has been prevented from making a satisfactory advance, viz., the propagation of the 266physiological doctrine (Broussaism), a doctrine which admits the existence of practically only one disease—irritation, in its varying degrees of intensity, together with a single class of remedies—anti-irritants. Modern therapeutists reject most of these ideas, and experience also shows that, in the matter of therapeutics, these anti-irritants often produce harmful results. “A treatise on therapeutics,” he goes on to say, “should contain the substance of all the good memoirs that have been published on the treatment of the different diseases and on the remedies employed; it should also mention all the circumstances which indicate or contra-indicate the employment of remedial agents, the best forms in which the latter may be administered, all the cases in which they have succeeded in affording relief as well as all those in which they have failed to accomplish this result; all the authors who have written on the subject under consideration; and, finally whatever additional facts may give the practitioner confidence in the reality of the results proclaimed.”
There came under public notice, at about this period of time, a French physician who evidently held very much the same beliefs as were put forward by A. L. J. Bayle and which I have very briefly stated in the preceding paragraph. I refer to Armand Trousseau, who was born (1801) in Western France, and who received his early medical training under that prince of physicians, Bretonneau, of Tours. In association with his friend, Hermann Pidoux, he published (in two volumes, Paris, 1836–1839) an excellent treatise on materia medica and therapeutics. The spirit which guided him in the preparation of this treatise is well expressed in his own words as follows:—
Medicine is both a science and an art.... It is an art when it becomes necessary to apply it to a human being who is ill, and this is especially true when the manner of treatment is under consideration. It is in this art that the physician reveals how much talent he possesses; he reveals himself as a true artist by the particular form of remedial preparation which he decides to administer to his patient, by the felicitous choice which he makes between remedies, and by the favorable manner in which he combines them.
TROUSSEAU
267Dujardin-Beaumetz then adds the important statement that in his belief Trousseau was—at the time when he gave utterance to these words—the living personification of the truth of what he said, for nobody had carried the therapeutic art to a higher state of perfection than he had. To this statement may be added, with perfect truth, the opinion held by many of his contemporaries to the effect that the publication of the Trousseau-Pidoux treatise promoted effectively the growth of a sound and trustworthy therapeutic code. The mere fact that in 1875 this treatise had already reached its ninth edition furnishes strongly corroborative proof of the correctness of this opinion.
The scantiness of the space which I consider it proper to devote to this single memoir appears to me to justify the omission, from this point onward, of everything that does not add to the description of Trousseau’s career as one of the greatest clinical teachers in the domain of internal medicine in France. I am the more strongly impelled to adopt this course because so many of my personal friends among the physicians who returned to New York, during the years 1860–1864, spoke in such terms of praise of the success attained by Trousseau in this particular branch of medical education.
His profound earnestness as a clinical teacher and his incessant watchfulness over the interests and rights of the patients who served as material for his bedside lectures are brought out so clearly in one of his addresses to the class at the beginning of one of his regular courses that I shall be pardoned, I am sure, for reproducing it here in considerable fulness of detail:—
Gentlemen:—Before making any remarks to you about my service at the hospital I feel impelled to tell you what I understand by the expression ‘clinical instruction’ and to put before you what I consider to be the respective duties of the professor and of those who regularly follow his lessons.—It is for me a very pleasant thing, as you may readily imagine, to see, crowding around the beds in the ward and seated on the benches of the amphitheatre, a large number of pupils; but the consciousness that I am fulfilling a useful mission and am sowing in the minds of these young men 268ideas that will later be fertilized, affords me a much greater pleasure. However, both as regards the professor and also as regards the pupils who listen to his teaching, there are needed certain conditions in the absence of which the clinical instruction must necessarily prove sterile.
Although clinical instruction represents the crowning stage of your medical studies, I would not have you believe that this particular part of your medical training should not be begun until you reach the last period of your student career. From the very day when a young man decides that he wants to be a physician he should lose no opportunity of visiting hospitals. It is desirable that he should see sick people—not occasionally, but as frequently as possible. The materials which are thus at first stored in one’s memory in a confused and disorderly condition are nevertheless excellent materials. While they may not to-day appear to possess a useful character, you will find them at a later period stored away among the genuine treasures lodged in your memory. To-day I have reached the period of old age, and yet I remember distinctly the patients whom I saw forty-three years ago when I took the very first steps in my career of physician; I recall the most important symptoms, the pathological lesions, even in some cases the patient’s name or the number of the bed which he occupied. The recollections are at times of service to me, they even afford me instruction, and occasionally you may hear me refer to them at our bedside conferences. I therefore urge upon even the youngest among you, the practice of visiting regularly every day the hospital. On the whole I believe that you will find it more profitable to give the preference at first to the medical rather than to the surgical wards.... You will not derive real profit from frequenting the latter until after you have acquired some knowledge in anatomy, whereas the possession of a few superficial conceptions regarding physiology will be found sufficient for the student who is beginning his first medical studies.
Little by little you will find that you are becoming more and more able to judge, from a mere inspection of the patient’s face and expression, how serious is the malady with which he is affected; you will learn how to feel his pulse and to appreciate correctly its different qualities; and you will begin to acquire some knowledge of auscultation and percussion; etc....
I cannot too often repeat to you the fact that a knowledge of anatomy is not to be acquired by listening to lectures upon the subject; in order to gain such knowledge you should have before 269you, a human cadaver—a cadaver around which sit two or three other students besides yourself, all busily engaged in the work of dissecting, and near you there should be an older and more experienced pupil upon whom you can depend for guidance. Similarly, knowledge of actual disease is to be learned by the student only at the hospital, and with the aid of one of the resident physicians or of a chief of staff, who is competent to teach you how a patient should be questioned and how a systematic examination of the case should be conducted.... And here let me remind you that the patients who are to be found in our wards are poor people, people who are compelled by their suffering and by their lack of money to take refuge in a hospital. A knowledge of this situation of affairs should lead us to show them some consideration and respect. So far as the men are concerned I admit that it is permissible for us to treat them with less delicacy. From the viewpoint of modesty there is very little indelicacy in removing the clothes from a man in order to make an examination of the surface of his body; on the other hand, it is not right to do this if the examination is at all likely to affect his health unfavorably. And now that we are discussing this subject, I am obliged to confess that young men are only too apt to forget that, after the clothing has been removed from a man whose skin is wet with perspiration, it is very dangerous to expose him even for a short time to the contact of a chilly air. It is also not permissible, even in the interest of science, to prolong a physical examination or to carry out the manipulations required in auscultation and percussion if you find that it is exhausting the poor patient’s strength. In the latter case it is better to leave the examination incomplete than to increase the feebleness of a patient who is already in such a state of weakness....
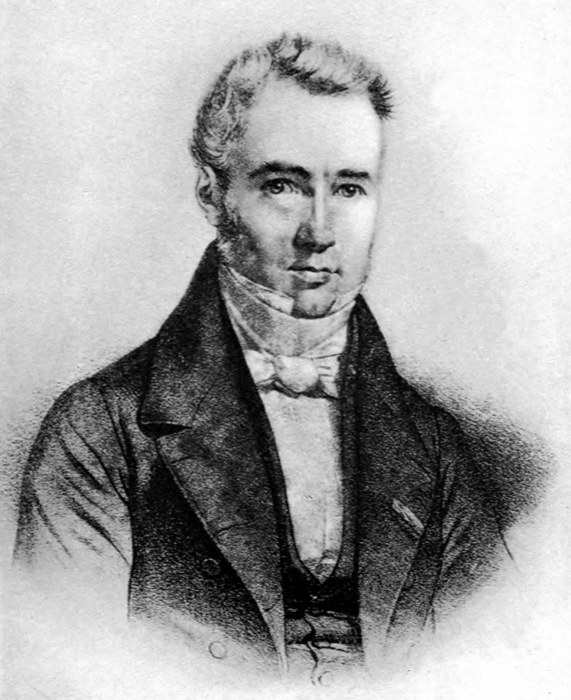
VELPEAU
A contemporary of Trousseau and one of France’s most distinguished surgeons.
(Copied from a print in the possession of Transylvania College, Lexington, Kentucky.)
It was my intention to introduce at this point a citation from Trousseau’s “Clinique de l’Hôtel-Dieu” of sufficient length to reveal fairly well his manner of conducting clinical instruction at the bedside of a patient. My decision to do this was based upon the assumption that I should find among the printed accounts of these supposedly impromptu lectures one or more which would serve the required purpose. I soon discovered, however, that not a trace of the off-hand character of such instruction remained in these reports. As they appeared in print they were elaborate and quite exhaustive memoirs, suited for the edification of men who had already long since passed the undergraduate 270stage of medical training, and I was therefore obliged to abandon the plan which I had so much desired to carry out. If I had, from the very first, given more serious thought to the scheme which I had in mind I would have quickly realized the fact that no teacher of wide experience and universally recognized as an authority in the diagnosis and treatment of disease would be likely to commit to print lessons which were meant to be useful to medical students who had only just reached the threshold of their professional career.
Trousseau died on June 23, 1867, in his seventy-second year. The only important treatises which he published are the two which I have already mentioned.
ALIBERT, J. L.: Éloges Historiques, etc., Paris, 1806.
BAGLIVI: The Practice of Physic Reduced to the Ancient Way of Observations, translated from the Latin, London, 1704.
BARON, JOHN: The Life of Edward Jenner, 2 vols., London, 1838.
BARTHEZ, P. J.: Nouveaux Elémens de la Science De l’Homme, Montpellier, 1778; Paris, 1806.
—— Consultations de Médecine (ouvrage posthume), Paris, 1820.
BAUDELOCQUE, JEAN-LOUIS: L’Art des Accouchemens, 2 vols., Paris, 1807.
BAYLE, A. L. J.: Bibliothèque de Thérapeutique, 4 vols., Paris, 1828–1837.
BAYLE, G. L.: Traité des Maladies Cancéreuses; ouvrage posthume, Vol. I., Paris, 1833.
BÉCLARD, P. A.: Additions to the General Anatomy of Xavier Bichat, Translated from the French by George Hayward, M.D., Boston, 1823.
BELL, SIR CHARLES: Institutes of Surgery, 2 vols., Edinburgh, 1838.
BERNARD, CLAUDE: Leçons sur les Phénomènes de la Vie Communs aux Animaux et aux Végétaux, Paris, 1878.
BONNET, THÉOPHILE: Sepulchretum, 3 vols., Lyons, 1700.—A still earlier edition (1675) exists.
BORDEU: (See under RICHERAND.)
BOUILLAUD, J.: Clinique Médicale de l’Hôpital de la Charité, 2 vols., Paris, 1837.
BOUILLET, J.: Précis d’Histoire de la Médecine, Paris, 1883.
BRETONNEAU ET SES CORRESPONDANTS, 2 vols., Paris, 1891. (Review in the Revue Scientifique of July 23, 1892.)
BROUSSAIS, F. J. V.: Examen des Doctrines Médicales, troisième edition, 4 vols., Paris, 1829–1834.
BUDD: Typhoid Fever, its Nature, Mode of Spreading, and Prevention, London, 1873.
272BUISSON, F. R.: Précis Historique sur Bichat, in Vol. I. of this Author’s Anatomie Générale, Paris, 1801.
CABANIS, P. J. G.: Du Degré de Certitude de la Médecine, 3d edition, Paris, 1819. (Also contains Richerand’s eulogy of Cabanis.)
CARTER, H. W.: A Short Account of Some of the Principal Hospitals of France, Italy, Switzerland, and the Netherlands, London, 1819.
CHEREAU, ACHILLE: Notice sur les Anciennes Écoles de Médecine de la Rue de la Bûcherie, Paris, 1866.
CHOMEL: Leçons sur la Fièvre Typhoïde, 1834. At a still earlier date (1821) Chomel published a general treatise on Fevers.
CORRY: Life of Joseph Priestley, 1804.
CROSS, JOHN: Sketches of the Medical Schools of Paris, London, 1815.
CUVIER: Éloges Historiques lus dans les Séances Publiques de l’Institut Royal de France, 3 vols., Strassbourg, 1819.
DAREMBERG, CHARLES: Histoire des Sciences Médicales, Vol. 2, Paris, 1870.
DEZEIMERIS, OLLIVIER ET RAIGE-DELORME: Dict. Historique de la Méd. Anc. et Mod., 3 vols., Paris, 1828–1837.
DUJARDIN-BEAUMETZ: “Leçons de Clinique Thérapeutique,” Paris, 1883.
DUPUYTREN, see under PAILLARD ET MARX.
EYNARD, THÉODORE: Essai sur la Vie de Tissot, Lausanne, 1839.
FRANK, JOHANN PETER: System einer vollständigen medicinischen Polizey, 6 vols., Mannheim, 1780–1788.
FRANKLIN, BENJAMIN: Life and Writings of, Published by J. M. Dent & Sons, London and New York, 1908.
GAZETTE MÉDICALE DE PARIS, Tome III., 1835.
GILLES DE LA TOURETTE: Théophraste Renaudot, Plon et Cie., Paris, 1884. Reviewed in La Revue Scientifique, April 9, 1892.
GRIBBLE, FRANCIS: Lake Geneva and its Literary Landmarks, Westminster, England, 1901.
GUARDIA, J. M.: La Médecine à travers les Siècles, Paris, 1865.
GUÉNEAU DE MUSSY: Clinique Médicale, Vol. III., Traité Théorique et Pratique de la Fièvre Typhoïde ou Dothiénentérique, Paris, 1884.
273GUEYRARD: La Doctrine Homoeopathique Examinée sous les Rapports Théorique et Pratique, Bruxelles, 1834.
HAESER, H.: Lehrbuch der Geschichte der Medicin, Zweite Ausgabe, Jena, 1868 (3d edition, 1875).
HAHNEMANN, SAMUEL: Organon of the Rational Art of Healing, translated from the German by C. E. Wheeler; published by C. M. Dent & Sons, London, 1913.
VON HALLER, ALBRECHT: Bibliotheca Medicinae, 4 vols.; Primae Lineae Physiologiae, Goettingen, 1751; and a later edition of this work in two volumes, printed at Lausanne, Switzerland.
HECKER: Geschichte der Neueren Heilkunde, Berlin, 1839.
HIRSCH, AUGUST: Geschichte der Med. Wissenschaften in Deutschland, Muenchen and Leipzig, 1893.
HOLLAENDER, EUGEN: Plastik und Medizin, Stuttgart, 1912.
HUFELAND, CHRISTOPH WILHELM: Kunst das Menschliche Leben zu Verlaengeren (Makrobiotik), Berlin, 1823, 5th edition.
HUNTERIAN REMINISCENCES, from notes taken by James Parkinson; London, 1833. (These notes were taken from a course of lectures delivered by the late John Hunter in 1785.)
HYRTL, JOSEPH: Lehrbuch der Anatomie des Menschen, Wien, 1873.
JACKSON, SIR GEORGE, K. C. H.: Diaries and Letters, 2 vols., London, 1872.
J. L. H. P.: Sketches of the Character and Writing of Eminent Living Surgeons and Physicians of Paris, translated from the French by Elisha Bartlett, M.D., Boston, Mass., 1831.
JAHR: Manual of Homoeopathic Medicine, Vol. I.
KORN, GEORG: Die Heilkunde im Neuenzehnten Jahrhundert, Berlin, 1899.
LAËNNEC, R. T. H.: Traité de L’Auscultation Médiate et des Maladies des Poumons et du Coeur, deuxième édition, 2 vols., Paris. 1826.
LARREY, BARON: Mémoire sur les Amputations des Membres à la Suite des Coups de Feu, Paris, 1797.
—— Mémoires de Chirurgie Militaire, et Campagnes, 3 vols., Paris, 1812.
LAS CASES: Mémoires d’E. A. D., Comte de las Cases, 1819.
LAVOISIER, ANTOINE LAURENT: “Oeuvres de Lavoisier publiées par les soins de son Excellence le Ministre de 274l’Instruction Publique et des Cultes,” 6 vols., quarto, Paris, 1864.
LITTRÉ: Dictionnaire de Médecine, de Chirurgie, de Pharmacie, de l’Art Vétérinaire et des Sciences qui s’y Rapportent, Paris, 1886.
LONDON LANCET, THE, of NOV. 25, 1837; editorial comparing the management of the large hospitals in the two countries—France and England.
LOUIS, CH. A. P.: Recherches Anatomiques, Pathologiques et Thérapeutiques sur la Maladie Connue sous les Noms de Gastro-entérite, Fièvre Putride, Adynamique, Ataxique, Typhoïde, etc., Paris, 1829.
MAGENDIE, M.: Leçons sur Les Phénomènes Physiques de la Vie, Paris, 1855.
MARSHALL HALL: Lectures on the Theory and the Practice of Medicine, in the Lancet, London, Oct. 7, 1837.
MÉMOIRES DE L’ACADÉMIE ROYALE DE MÉDECINE, Vol. I., Paris, 1828.
MIQUEL, A.: Lettres à un Médecin de Province ou Exposition Critique de la Doctrine Médicale de Monsieur Broussais, 2me édition, Paris, 1826.
MONFALCON, I.: Précis de Bibliographie Médicale, Paris, 1827.
MORGAGNI: De Sedibus et Causis Morborum, 1767. An English version of this work, in 3 volumes, was published at London in 1769, and a French version was issued a few years later.
MUELLER, WILLIBALD: Biographie von Gerhard van Swieten, Wien, 1883.
PAGEL, JULIUS: Einfuehrung in die Geschichte der Medizin, Berlin, 1898.
PAILLARD ET MARX: Traité des Blessures par Armes de Guerre, d’après les Leçons Cliniques de Monsieur le Baron Dupuytren, 2 vols., Paris, 1834.
PETERSEN, JULIUS: Hauptmomente in der Geschichtlichen Entwickelung der Med. Therapie, Copenhagen, 1877.
PETIT, J. L.: Traité des Maladies Chirurgicales, et des Opérations qui leur Conviennent, Nouvelle édition, Paris, 1790.
PETTIGREW, THOMAS J.: Medical Portrait Gallery. (Biographical Memoirs of the most celebrated physicians, surgeons, etc., who have contributed to the advancement of medical science.) 2 vols., London, 1838.
PINEL: Nosographie Philosophique, Paris, 1798.
POTAIN: La Médecine en Province (containing certain data 275relating to Bretonneau, of Tours); in the Revue Scientifique of Nov. 10, 1894.
POTT, PERCIVAL: Chirurgical Works, 2 vols., Philadelphia, 1819.
PRIESTLEY, JOSEPH: Experiments and Observations on Different Kinds of Air, 2d edition, London, 1775.
PUSCHMANN, THEODOR: Die Medicin in Wien waehrend die Letzen 100 Jahre, Wien, 1884. —— Geschichte des Medicinischen Unterrichts, Leipzig, 1889.
QUARTERLY JOURNAL OF FOREIGN MEDICINE AND SURGERY, Vol. I., London, 1818–1819.
REVUE SCIENTIFIQUE for March 24, 1894. (Article on the proportion of homoeopathic practitioners to those of the regular school in some of the cities of the United States.)
RICHERAND: Oeuvres Complètes de Bordeu, précédées d’une notice sur sa vie et sur ses ouvrages, 2 vols., Paris, 1818.
RICHET, A.: L’Histoire de la Chirurgie, in the Revue Scientifique, Nov. 19, 1892.
ROKITANSKY, CARL: Pathologische Anatomie, 3 vols., 1855. (Illustrations in the edition of 1855, but not in the first edition.)
ROSENTHAL, J., article in the Revue Scientifique of Jan. 10, 1801.
ROUX, P. J.: Narrative of a Journey to London in 1814; Translated from the French, 2d edition, London, 1816.
SCHEUTHAUER, GUSTAV: article on Carl Rokitansky, in Hirsch and Gurlt’s Biographisches Lexikon.
SCHULTZ, C. H., Article on Homoeopathy in Hufeland’s Journal der Praktischen Medicin, Bd. LXIX., No. 5.
VON SIEBOLD: Versuch einer Geschichte der Geburtshuelfe, Berlin, 1845.
SIGMOND, GEORGE G.: On the Effects of Mercury, in the Lancet, London, Nov. 11, 1837.
SIMPSON: Homoeopathy, etc., 3d edition, 1853.
SPALLANZANI: Mémoires sur la Respiration; traduits de l’Italien par Jean Senebier, Genève, 1803.
SPIESS, G. A.: J. B. Van Helmont’s System der Medicin, Frankfort am Main, 1840.
SPRENGEL, KURT: Histoire de la Médecine, Paris, 1815. (Traduite de l’Allemand par A. J. L. Jourdan.)
SUDHOFF, KARL: J. C. Reil von der Lebenskraft, Leipzig, 1910.
TENON, M.: Mémoires sur les Hôpitaux de Paris, Paris, 1816.
276TROUSSEAU, ARMAND: Clinique Médicale de l’Hôtel-Dieu de Paris, 3d edition, 3 vols., Paris, 1868.
TROUSSEAU ET PIDOUX: Traité De Thérapeutique et de Matière Médicale, 9th edition, 2 vols., Paris, 1875.
VELPEAU: Traitment des Maux de Gorge et de quelques inflammations des autres membranes muqueuses par le sulfate d’alumine et de potasse, in the Gazette Médicale de Paris, 4 avril, 1835.
WUNDERLICH UND ROSER: Archiv fuer Physiologische Heilkunde, Bd. I., 1841.
1. The liard was a small copper coin worth at that time one-quarter of a sou. The latter coin was about as large as a silver quarter of a dollar or a one-shilling piece (English money).
2. The view of the small town of Loudun (see opposite page 4), which has been copied from a photograph of quite recent date, shows that Gilles de la Tourette’s hope has already been realized.
3. See Haller’s comments on Boerhaave’s personality, at bottom of page 445 of “The Growth of Medicine.”
4. In the city of Leipzig alone there were no fewer than 30,000 wounded and sick soldiers belonging to all the different nations engaged in the war.
5. The following quotations are from Wheeler’s English Translation of the Organon.
6. Several weeks after I had sent my completed manuscript to New Haven I received, from a London dealer in second-hand books, a catalogue in which the following item appears:—
Haller (Albrecht von) First Lines of Physiology. Translated from the Third Latin Edition. To which is added a Translation of the Index composed for the Edinburgh Edition printed under the Inspection of Dr. William Cullen. Edinburgh, 1801.
It is evident, therefore, that I was in error when, after a very limited search, I was led to believe that no English version of the “Primae Lineae” exists, and accordingly I ventured to translate a few brief selections of the text.—A. H. B.
7. To make sure that any errors rightly chargeable to me as translator shall not be imputed to von Haller I will add here the original Latin text.—A. H. B.
Chapter XX. Somnus.
Section 564.—Aptitudo ad sensus et motus voluntarios libere exercendos in sanis organis, VIGILIA vocatur: ineptitudo ad eosdem et quies omnium cum sanis organis SOMNI nomen fert.
Section 565.—In somno anima vel omnino nihil cogitat, quod memoria retineatur, quodque notum fit, vel unice occupatur in speciebus, sensorio communi receptis, quarum vividae repraesentationes in mente eo tempore omnino similes perceptiones producunt, quales objectorum externorum impressiones insensuum organa faciunt. Hae repraesentationes INSOMNIA vocantur, et efficiunt, ut reliquo toto emporio sensuum et voluntariorum motuum quiescente, aliqua tamen particula aperta sit, spiritibus perfluatur, et vigilet. Aliquando cum his perceptionibus animae aliqui motus voluntarii conjunguntur, ut loquelae organa, ut artus multi, omnesve, ad nutum illarum preceptionum regantur. Huc SOMNAMBULI.
Section 566.—Sed in somno pergit omnium humorum in corpore humano distributio, circulatio, vis peristaltica ventriculi, intestinorum, sphincterum, respiratio denique ipsa simili modo exercetur. Haec compositio in quiete certarum partium, aliarum motu, cognitionem causae mechanicae somni difficilem reddidit.
8. A French physician by the name of Goudareau has published a translation of the work under the title: “TRAITé DE MéDECINE PRATIQUE,” 2 vols., Paris, 1820–1822.
9. At this point one of Wunderlich’s critics makes the comment that Ludwig Traube may more justly be considered the real founder of experimental pathology in Germany.
10. “COMMENTARIA IN HERM. BOERHAAVE APHORISMOS DE COGNOSCENDIS ET CURANDIS MORBIS,” Paris, 1755–1773, 5 vols. in quarto. There exist also English and French translations of these commentaries.
11. It has often been stated that Lorenz Gasser was the discoverer of the nodal swelling of the trigeminal nerve which bears the name of “Gasserian ganglion.” Hyrtl, however, declares that the credit for this discovery belongs to A. R. B. Hirsch, a Viennese anatomist, who named it in honor of his teacher, Lorenz Gasser, Professor of Anatomy in the University of Vienna.—A. H. B.
12. A solution of bichloride of mercury, 4; chloride of sodium and chloride of ammonium, each 1; water 500.
13. “Illustrissimo viro Lazaro Spallanzani summo naturae in minimis et difficilimis, indagatori, ob ejus in veri finibus extendendis, merita, D. D. D. Hallerus.”
[The letters D. D. D. are an abbreviation for “dat, donat, dedicat,” commonly employed in inscriptions.]
14. Those of 1775 and later years, printed by Grasset, of Lausanne, are considered the best.
15. At the period which is now under consideration Geneva belonged strictly to France. It was not until the year 1815 that it was incorporated with the Confederation of Swiss Cantons.
16. Some authorities state that William Scheele made the same discovery independently in 1775.
17. Published, in 1908, by John Lane, New York and London; and, for the reader’s further enlightenment, it should be stated that “Thomas William Coke of Holkam, Norfolk, England, was a famous country gentleman who lived from 1754 to 1842, becoming, late in life, the Earl of Leicester. He was known throughout the world of his time as a scientific and accomplished agriculturist. Owning great country estates he was a skillful sportsman, and as an influential member of Parliament sided with the Americans and against George III and his ministers in our Revolution.”
18. The title of this memoir is: “TRAITÉ DES MEMBRANES EN GÉNÉRAL ET DES DIVERSES MEMBRANES EN PARTICULIER,” Paris, 1800.
19. Free Translation into English.—“This monument has been erected in honor of citizens Desault and Bichat by their contemporaries, who wish in this manner to show their appreciation of the valuable services which these two men have rendered to medicine: Desault by the important part which he played in renewing the life and vigor of French Surgery, and Bichat by his untiring efforts, both by teaching and by research work, to extend the limits of the domain of Medicine. Successful as were these efforts the results would certainly have been much greater if death had not put an end to his work before Bichat had completed his 31st year.”
20. Bonaparte was not made Emperor until 1804.
21. This—says the author of the biographical sketch from which I derive my information—is a bit of sarcasm suggested to Bayle’s mind by the fact that Petit-Radel was well-known at that period to be particularly fond of favoring systems in his contributions to medical literature.
23. For additional information concerning Montpellier’s famous Faculté de Médecine, see farther on under the heading “Jacques Delpech” (page 233).—A. H. B.
24. To prevent confusion I beg to remind the reader that there were two men living in Paris at this period who both bore the name of Louis and who were almost equally celebrated, viz., Antoine Louis, the surgeon, and Charles A. P. Louis, the subject of the present remarks.
25. As stated on page 87 the Vienna anatomist, Hyrtl, claims that Duddal, an English physician, was the first person who described this membrane.
26. By the word “schools” Chereau evidently means the buildings in which the different classrooms were located.—A. H. B.
27. Voltaire says (p. 328 of “Pages Choisies des Grands Écrivains,” Paris, Librairie Armand Colin, 1910): “That Piarrou de Chamousset (1717–1773), a wealthy philanthropist, built a model hospital in which every patient had a bed to himself or herself. Since that time the practice of putting two patients in one bed has been abandoned.”