Gouty Arthritis.
Note large tuberous swellings on knuckle and metacarpo-phalangeal joints due to uratic deposits.

Title: Gout, with a section on ocular disease in the gouty
Author: Llewellyn J. Llewellyn
Contributor: W. M. Beaumont
Release date: January 24, 2023 [eBook #69874]
Most recently updated: October 19, 2024
Language: English
Original publication: United States: C. V. Mosby Company, 1921
Credits: Mark C. Orton and the Online Distributed Proofreading Team at https://www.pgdp.net (This file was produced from images generously made available by The Internet Archive)
Gouty Arthritis.
Note large tuberous swellings on knuckle and metacarpo-phalangeal joints due to uratic deposits.

BY
LLEWELLYN JONES LLEWELLYN, M.B. Lond.
GOVERNOR AND SENIOR PHYSICIAN, ROYAL MINERAL WATER HOSPITAL, BATH;
FELLOW OF ROYAL SOCIETY OF MEDICINE; AUTHOR OF “ARTHRITIS DEFORMANS”;
CO-AUTHOR OF “FIBROSITIS”; CO-AUTHOR OF “MALINGERING, OR THE SIMULATION
OF DISEASE”; CO-AUTHOR OF “PENSIONS AND THE PRINCIPLES OF THEIR
EVALUATION”; CONTRIBUTOR TO LATHAM AND ENGLISH’S “SYSTEM OF TREATMENT,”
ALSO TO “OXFORD ENCYCLOPÆDIA OF TREATMENT” AND TO “STUDENT’S
TEXT-BOOK OF SURGERY.”
WITH A SECTION ON
OCULAR DISEASE IN THE GOUTY
BY
W. M. BEAUMONT
CONSULTING OPHTHALMIC SURGEON TO THE SOUTH-WESTERN
REGION OF THE MINISTRY OF PENSIONS; AUTHOR OF “INJURIES
OF THE EYES OF THE UNEMPLOYED, PROBLEMS IN PROGNOSIS,” ETC.
ST. LOUIS
C. V. MOSBY COMPANY
1921
Printed in Great Britain.
Dedicated
TO
MY WIFE
“A knowledge of the real nature of gout ... is, in my opinion, at the very foundation of all sound pathology,” wrote Todd many years since; and the passing years have but invested his reflection with deeper significance and something of prophetic insight. For who can doubt that he who would elucidate the pathological groundwork of gout must be at once a clinical physician, a bio-chemist, a bacteriologist, a morbid anatomist? and well may we ask, Who is sufficient for all this?
How vivid the light thrown upon the problems of clinical medicine by the bio-chemists! The story of the fate of protein and purin substances in the animal body, at one time a medley of guesses and gaps, is gradually evolving into one of relative certitude and completeness. Revolutionary, in truth, the change, and many a cherished shibboleth has been ruthlessly cast aside! With admiration not unmingled with awe we see them laying well and truly the foundations upon which in the ultimate scientific medicine must inevitably rest.
Of these the very corner-stones are chemical physiology and chemical pathology, the rapid evolution of which is profoundly altering our conceptions of health and disease. Those vital processes of the organism that but yesterday we saw “as through a glass, darkly,” are now in great part illumined, and the distortions wrought in them by disease made more manifest.
How pregnant, too, with warning their findings! Processes that to our untutored minds seem simple are revealed as infinitely complex. Through what a maze must we thread our way if we would disentangle the intricacies of metabolism! Intricate enough, forsooth, in health, but how much more so in disease! For, as Sir Archibald Garrod eloquently phrases it, “it is becoming evident that special paths of metabolism exist, not only for proteins, fats, and carbohydrates as such, but that even the individual primary fractions of the protein molecule follow their several katabolic paths, and are dealt with in successive stages by series of enzymes until the final products of katabolism are formed. Any of these paths may be locked while others remain open.”
It is with chastening reflections such as these that we may best approach our study of gout, that riddle of the ages upon which so many physicians from time immemorial have expended their dialectic skill. But, vast though the increase in our knowledge[viii] of the chemical structure of uric acid and its allies, uncertainty still dogs our steps, and, doubtful of the pathway to solution of the pathological mystery of gout, we must perforce approach the problem in a more strictly catholic attitude.
Uric acid has apparently failed us as the causa causans. Neither this substance nor its precursors can be held responsible for the fever, local inflammation and constitutional disturbances in gout, being, as they are, practically non-toxic. Albeit, though I hold this view, I do not for one moment suggest that uric acid has nothing whatever to do with gout. The fact that tophi, its pathognomonic stigmata, are compounded of biurate of soda, would per se stamp such an attitude as untenable. On the other hand, uric acid must be viewed at its proper perspective as a concomitant or sequel of gouty inflammation, the essential cause of which must be sought elsewhere.
“The old order changeth, giving place to new,” and happily with the advent of bacteriology our views, or rather our hazards, as to the nature of joint diseases underwent profound modification. But, strange to say, though quick to apprehend the significance of infection, its causal relation to other joint disorders, we still seem unaccountably loth to discard our timeworn conception of “gouty” arthritis as of purely metabolic origin. This to my mind is the more remarkable in that the onset, clinical phenomena, and course of acute gout, and no less the life history of the disorder as a whole, are emphatically indicative of the intrusion of an infective element in its genesis.
The extreme frequency with which infective foci are met with in the victims of gout, the frequency, too, with which exacerbations of the disorder are presaged by acute glandular affections of undeniably infective source, is by no means adequately realised. For our forefathers gout began, and, forsooth, often ended, in the “stomach,” or it was the “liver” that was impeached. But the portal to the alimentary canal was for them only a cavity, the contained structures of which, albeit, to their mind often betrayed evidences of a “gouty diathesis.” They distinguished “gouty” teeth, “gouty” tonsillitis, “gouty” pharyngitis, even “gouty” parotitis; but all these they classed as tokens or sequelæ of gout, not possible causes or excitants thereof.
Now as to the true significance of these acute glandular affections held by clinicians of repute to be of “gouty” origin. What of “gouty” tonsillitis, pharyngitis, parotitis? Still more, what of our deductions regarding the relationship of these same when met with in association with non-gouty forms of arthritis? Do we not hold them each and all as evidences of infection? and, we may well ask, why not in gout?
The marvel then is that even to-day many still hold that the tonsillitis, pharyngitis, even the gingivitis, like the subsequent articular lesions, are one and all attributable to the underlying gout. We certainly should not do so in the case of any arthritis other than “gouty,” and to my mind the time is ripe for a change of attitude.
The “gouty” throats, like the “gouty” teeth, should be regarded not as symptomatic of gout, but etiologically related thereto. We should cease to talk of “gouty” throats, teeth, etc., should renounce the prefix, for there is nothing specific of gout either in the tonsillar, pharyngeal, or dental lesions. We should instead view these various local disorders in their true perspective as foci of infection, causally related to the subsequent and secondary “gouty” arthritis.
Similarly, when we come to analyse the component elements of an acute paroxysm of gout, how strongly indicative of the intrusion of an infective element the following features: the onset, temperature curve, character of local articular changes of the disorder, the presence of leucocytosis, with secondary anæmia and enlargement of the lymphatic glands! Again, how suggestive the occasional complication of acute gout by lymphangitis and phlebitis! Of like significance, too, the paroxysmal nature and periodicity of the disorder, and the compatibility of the morbid anatomical changes and the cytological content of the aspirated joint fluid with their genesis by infection.
As to correlation of the metabolic phenomena of gout with the postulated infective element, I would suggest that, although abnormalities of metabolism form an integral part of gout, they are of themselves inadequate to achieve its efflorescence. As we shall see when we come to consider those elemental manifestations of gout, i.e., uratic deposits, or tophi, neither the purely physical nor the purely chemical theory of their origin will suffice, nor, for that matter, can any solution of their formation be gleaned from even a blend of the twain. In short, such hypotheses are too mechanical.
The intrusion of some other factor, “something vital, something biological,” seems essential for the elucidation of uratosis, i.e., uratic deposition. For this, not uricæmia, is the specific characteristic phenomenon of gout. If we cannot explain uratosis on physical or chemical grounds, then how much less, in view of the non-toxicity of uric acid, can we on this basis account for the inflammatory phenomena of the disorder!
Now inflammatory reaction is, I hold, an invariable antecedent in all gouty processes, whether of articular or ab-articular site. Granted that inflammatory reaction is a necessary prelude, the[x] specificity of gout is attested by the fact that the same is followed by local deposition of urates. But while this sequential uratic deposition invests all forms of “gouty” inflammation with a specific character unshared by any other disease, it follows that the cause of the said inflammation must, if possible, be ascertained.
Now, as I believe, “gouty” subjects are ab initio victimised by innate tissue peculiarities, doubtless reflected in corresponding obliquities of tissue function and metamorphosis, and through their medium the general resistance of the body to invasion by infections is lowered; in other words, under the influence of these morbific agencies the latent morbid potentialities of the gouty become overt and manifest. For in the gouty, as Walker Hall observes, “a slight injury or indiscretion of diet, an overloaded intestine, or increased toxicity of the intestinal flora, may be followed by a disturbance of the general nuclein metabolism and a local reaction in certain tissues.”
Enough has been said to disclose the dominant trend of this work, and although there are many aspects of the subject in regard to which I hold somewhat iconoclastic views, yet exigencies of space forbid me even to allude to them in this foreword. I hasten therefore to discharge the pleasing duty of acknowledging my great indebtedness to the acumen and discrimination which has been brought to bear on this subject by a long succession of eminent physicians, in proof of which I need only adduce the names of those giants of the past the illustrious Sydenham, Sir Thomas Watson, Sir Charles Scudamore, Jonathan Hutchinson, not to mention Trousseau, Charcot, Lecorche, and Rendu. But I should fail in my duty did I not in a special sense express my deep indebtedness to the classic and epoch-making work of Sir Alfred Garrod. For the rest, too, I have derived much enlightenment from Sir Dyce Duckworth’s treatise and the various works on the subject by Luff, Lindsay, and others.
From the bio-chemical aspect I owe much to the researches of Walker Hall, and to those of our American confrères Folin, Denis, Benedict, Pratt, McLeod, Walker Jones, Gideon Wells, etc.
Reverting to my own colleagues at the Royal Mineral Water Hospital, Bath, I would tender my deep thanks to the Honorary Physicians, Drs. Waterhouse, Thomson, Lindsay, and King Martyn, for the uniformly generous manner in which they afforded me opportunities for studying cases under their care.
To Dr. Munro, our senior pathologist, I am especially beholden for invaluable, nay indispensable, help in the matter of blood examinations, the cytological study of joint fluids, and the microscopic verifications of tophi. To Dr. MacKay also my[xi] cordial thanks are due for the skiagraphs contained in this work.
For the section dealing with the ocular disorders met with in the gouty my most sincere thanks are due to Mr. W. M. Beaumont, of Bath, whose singularly wide experience in this sphere renders him unusually equipped to deal with this highly controversial aspect of gout. To Drs. Cave and Gordon, of Bath, also I am indebted for many valuable suggestions kindly afforded me while writing this volume. To my brother Dr. Bassett Jones I am under deep obligation for unwearying assistance in our joint endeavour to ascertain the exact relationship of gout to lumbago, sciatica, and other types of fibrositis.
For the preparation of the index of this work I would proffer my grateful thanks to Mr. Charles Hewitt and to Miss Donnan and Miss Crosse for having undertaken the arduous task of typing the manuscript thereof.
Lastly, I would express my thanks to my publisher, Mr. Heinemann, for much consideration and many courtesies.
LL. J. LL.
31, Upper Brook Street, W. 1.
| CHAPTER I HISTORICAL AND INTRODUCTORY |
|
| The Antiquity of Gout. Prevalence of Gout in the Anglo-Saxon Period. Views of the Humoralist. The Aphorisms of Hippocrates. Introduction of the Word Gout. Early Views as to the Nature of Tophi. The “Honour of the Gout.” That Gout confers Immunity from other Disorders. Growing Infrequency and Attenuation of Gout | pp. 1-13 |
| CHAPTER II THE PEDIGREE OF GOUT |
|
| Tardy Dissociation of Chronic Gout. Identification of Muscular Rheumatism. Differentiation of Chronic Gout from Arthritis Deformans. Cleavage of Arthritis Deformans into Two Types. Elimination of the Infective Arthritides | pp. 14-20 |
| CHAPTER III EARLIER THEORIES OF PATHOGENESIS |
|
| Garrod’s Theory. Antagonistic Views. Histogenous Theories. Antecedent Structural Changes. Hepatic Inadequacy. Hyperpyræmia. Nervous Theories. Growing Scepticism as to Garrod’s Pathogeny of Gout | pp. 21-34 |
| CHAPTER IV DEFINITION, CLASSIFICATION, ETIOLOGY, AND MORBID ANATOMY |
|
| Definition. Classification. Suggested Classification of Articular Gout. Etiology and Morbid Anatomy. Bodily Conformation and Individual Temperament. Locality, Race, Climate. Food, Drink, Occupation. Lead Poisoning. Mental and Physical Over-exertion. Summary. Morbid Anatomy | pp. 35-58 |
| CHAPTER V PATHOLOGY OF GOUT-PROTEIN METABOLISM |
|
| Revelations of the Bio-chemist. The Formation of Urea. Fate of the Amino-acids. Seat of Formation of Urea. Amino-acids in Relation to Gout. The Glycocoll Theory of Gout. Urea Excretion in Gout. Creatine and Creatinine. Inborn Errors of Metabolism | pp. 59-70 |
| CHAPTER VI NUCLEIN METABOLISM |
|
| The Isolation of Nucleic Acid. Researches on Spermatozoa. The Discovery of Purins. Uric Acid a Derivative of Nucleic Acid. The Chemistry of Uric Acid and the Purin Bodies. Chemical Constitution. Properties of Uric Acid. Uric Acid in the Blood. Gudzent and Schade’s Theories. Organic Combinations. Complexity of the Problem | pp. 71-82[xiv] |
| CHAPTER VII SOURCES OF URIC ACID |
|
| Exogenous Purins. Exogenous Uric Acid Excretion. Fate of the Unexcreted Purins. Endogenous Purins. Source of Endogenous Purins. Proteins and their Derivatives. Amino-acids and Dicarboxylic Amino-acids. Endogenous Uric Acid Excretion. Factors influencing Endogenous Uric Acid Excretion. Physiological Conditions. Pathological States. Ingestion of Certain Drugs. Synthetic Formation of Uric Acid | pp. 83-97 |
| CHAPTER VIII FORMATION AND DESTRUCTION OF URIC ACID |
|
| Distribution of the Enzymes. Stages in Disruption of Nucleic Acid. Destruction of Uric Acid | pp. 98-106 |
| CHAPTER IX URIC ACID IN RELATION TO GOUT |
|
| Uric Acid Excretion in Gout. Uric Acid Variations in Acute Gout. Uric Acid Variations in Chronic Gout. Retarded Exogenous Uric Acid Output. Lowered Endogenous Uric Acid Output. Other Anomalies in Excretion in Gout. Purin Metabolism in other Disorders. Purin Metabolism in Chronic Alcoholism and Plumbism | pp. 107-116 |
| CHAPTER X THE RENAL THEORY OF GOUT |
|
| Anomalies in Uric Acid Excretion in Gout. Uricæmia in Nephritis. The Relationship, if any, between the Amounts of Uric Acid and of Urea, and Total Non-protein Nitrogen in Human Blood. Uricæmia not necessarily due to Renal Defect. Uricæmia not Peculiar to Nephritis. Uricæmia does not necessarily Portend Gout. To what may be ascribed the Deficient Eliminating Capacity of the Kidney for Uric Acid. Uratic Deposits in Nephritis. Differentiation of Uratic Deposits in Gout and Nephritis. Clinical Associations of Gout and Granular Kidney | pp. 117-132 |
| CHAPTER XI URICÆMIA IN GOUT |
|
| Folin and Denis’s Method. Uric Acid a Normal Constituent of Blood. Effect of Exogenous Purins. Uric Acid Content of Blood in Gout. Hyperuricæmia in Non-gouty Arthritis. Variations in Uric Acid Content of Blood independently of Diet. What Relationship, if any, Exists between the Uric Acid Content of the Blood and Attacks of Gout. Discussion of the Foregoing Data. The Significance of Uricæmia. Sources of Fallacy in Uric Acid Estimation. Disabilities of Modern Tests. Need for further Investigations | pp. 133-148 |
| CHAPTER XII URATOSIS IN RELATION TO GOUT |
|
| Constitution of Tophi. Mode of Formation. Localisation of Uratic Deposits. The Causation of Tophi. Solubilities of Uric Acid. Tophi in Relation to Uricæmia. Tissue Affinities for Uric Acid. Retention Capacity of Tissues for Uric Acid. Clinical Evolution of Tophi. The Cause of the Inflammatory Phenomena. Non-toxicity of Uric Acid. Are the Precursors of Uric Acid Toxic? | pp. 149-170[xv] |
| CHAPTER XIII THE RISE OF THE INFECTIVE THEORY |
|
| Boerhaave’s Forecast of the Infective Theory. Ringrose Gore on Infective Origin. Leucocytosis in Acute Gouty Polyarthritis. Chalmers Watson’s Researches on Gout in a Fowl. Trautner’s Suggestion of a Specific Infection | pp. 171-176 |
| CHAPTER XIV GOUT AS AN INFECTION |
|
| Local Foci of Infection: Dental, Nasal, Pharyngeal, etc. Gastro-intestinal Disorders. Variation in Free HCL. Intestinal Disorders. Infection or Sub—infection | pp. 177-187 |
| CHAPTER XV GOUT AS AN INFECTION (continued) |
|
| Analysis of the Acute Paroxysm. The Evolution and Life History of Gout. Analogies between Gout and the Specific Infective Arthritides. Correlation of the Metabolic Phenomena of Gout with the Postulated Infective Element | pp. 188-199 |
| CHAPTER XVI CLINICAL ACCOUNT |
|
| Acute Localised Gout. Prodromal Symptoms. Dyspepsia. Premonitory Symptoms of Tophus Formation. Premonitory Articular Pains. The Acute Paroxysm. Detailed Consideration of Phenomena. Mode of Onset. Localisation. Nature of Pain. General Phenomena. Pyrexia. Changes in the Blood. Uric Acid Excretion. Local Phenomena. Tophus Formation | pp. 200-213 |
| CHAPTER XVII CLINICAL ACCOUNT (continued) |
|
| Acute Gouty Polyarthritis. Mode of Invasion. Distribution of Lesions. Local Characters. Constitutional Symptoms. Changes in the Blood. Leucocytosis. Collateral Phenomena of Gout. Lumbago, Sciatica, etc. Incidence of Gouty Stigmata in Various Types of Fibrositis | pp. 214-224 |
| CHAPTER XVIII CLINICAL ACCOUNT (continued) |
|
| Chronic Articular Gout. The Joint Deformities of Chronic Gout. Tophi: Their Evolution and Distribution. Other Sites of Tophi. Affinities between Gout and other Diseases. Gout in Relation to Glycosuria. Gout in Relation to Phlebitis. Cutaneous Disorders. Gout and Nephritis. Prognosis in Gout | pp. 225-246 |
| CHAPTER XIX ETIOLOGICAL AND CLINICAL DIAGNOSIS. |
|
| Articular Gout. Etiological Diagnosis. Clinical Diagnosis. Introductory Remarks. The Diagnostic Status of Tophi. Tophi in Relation to Arthritis. Frequency of Tophi in True Gouty Arthritis Underestimated. Difficulty of Detecting Tophi | pp. 247-257[xvi] |
| CHAPTER XX CLINICAL DIAGNOSIS (continued) |
|
| Acute Articular Gout. Localised Variety. Differential Diagnosis. Infections. Acute Gonococcal Arthritis. Traumatic Lesions. Acute Osteoarthritis. Static Foot Deformities. Hallux Valgus with Inflamed Bunion. Hallux Rigidus. Metatarsalgia. Gout in the Instep. Gonococcal Arthritis. Tuberculosis and Syphilitic Disease of the Tarsal Joints or the Related Joints. Pes Planus. Gout in the Heel. Referred Pain. Local Sources of Fallacy. Post-calcaneal Bursitis. Synovitis of the Tendo Achillis. Gout in the Sole. Plantar Neuralgia. Erythromelalgia. Anomalous Sites for Initial Outbreaks | pp. 258-267 |
| CHAPTER XXI CLINICAL DIAGNOSIS (continued) |
|
| Acute Gouty Polyarthritis. Differential Diagnosis. Acute Articular Rheumatism. Acute Gonococcal Arthritis. Etiology. Onset. General Symptoms. Distribution of Lesions. Local Characters. Associated Phenomena. Secondary Syphilitic Arthritis. Acute Rheumatoid or Atrophic Arthritis. Age and Sex. Onset. General Symptoms. Distribution of Lesions. Local Characters. Associated Phenomena. Infective Arthritis of Undifferentiated Type | pp. 268-274 |
| CHAPTER XXII CLINICAL DIAGNOSIS (continued) |
|
| Chronic Articular Gout. Chronic Monarticular Gout. Monarticular Gout in Large Articulation a Rarity. Chronic Gout of Oligo-articular Distribution. Its Confusion with Chronic Villous Synovitis. Villous Synovitis Static and Non-gouty in Origin. Clinical Symptoms of Villous Synovitis. Bilateral Hydrarthrosis. Peri-synovial and Peri-bursal Gummata. Chronic Gout of Polyarticular Distribution. Differential Diagnosis. Osteoarthritis. Local Characters of Joint Swellings. Rheumatoid Arthritis. Local Characters of Joint Swellings. Nerve Arthropathies. Hæmophilic Arthritis | pp. 275-285 |
| CHAPTER XXIII CLINICAL DIAGNOSIS (continued) |
|
| Skiagraphy. Significance of Local Areas of Rarefaction. The Radiographic Types of Gouty Arthritis. Differential Diagnosis. Infective Arthritis. Hypertrophic or Osteoarthritis. Rheumatoid or Atrophic Arthritis | pp. 286-292 |
| CHAPTER XXIV IRREGULAR GOUT |
|
| Historical Account. Murchison’s Views. Retrocedent Gout. Gout in the Stomach. Cardiac and Cerebral Forms. Other Irregular Manifestations. Conclusions. Infantile Gout | pp. 293-307 |
| CHAPTER XXV OCULAR DISEASE IN THE GOUTY |
|
| Evidence of Gout in the Eye. Deposition of Urates. Gouty Diathesis. Significance and Location of Tophi. Relative Incidence of Iritis. Metastasis. Arthritic Iritis. Gouty Iritis not a Clinical Entity. Ocular Symptoms in Hyperuricæmia. False Gout. Retinal Hæmorrhage. Neuro-retinitis. Glaucoma. Conclusions | pp. 308-326[xvii] |
| CHAPTER XXVI TREATMENT OF GOUT |
|
| Radical Treatment of Local Foci of Infection or Toxic Absorption. Diet in Acute and Chronic Gout. The Fallacy of Fixed Dietaries. Thorough Physical Examination a necessary Prelude to Dieting. Need for Collaboration of Clinician and Bio-chemist | pp. 327-341 |
| CHAPTER XXVII TREATMENT OF GOUT (continued) |
|
| Regulation of Diet in the Gouty. The Individual Foodstuffs, Proteins, Carbohydrates, Fats, Vegetables, Fruits, Condiments. Special Dietaries. Amylaceous Dyspepsia. Hyperchlorhydria | pp. 342-371 |
| CHAPTER XXVIII MEDICINAL AND OTHER MODES OF THERAPY—ACUTE GOUT |
|
| Initial Purgation. Colchicum in Acute Gout. Method of Administration. Preparations and Dosage. Colchicine, Salicylate of Colchicine. Atophan. Alternative Remedies in Acute Gout. Salicylates. Alkalies. Quinine. Thyminic Acid. Anodynes in Acute Gout. Local Measures. Analgesics. Liniments, etc. Ionisation. Massage. Surgical Methods | pp. 372-388 |
| CHAPTER XXIX MEDICINAL AND OTHER MODES OF THERAPY (continued)—INTER-PAROXYSMAL PERIOD |
|
| Prophylactic Measures. Treatment of Atonic Dyspepsia. Hyperacidity due to Organic Acids. Treatment of Hypochlorhydria. Alkalies, Atophan, and Colchicum as Prophylactics | pp. 389-396 |
| CHAPTER XXX MEDICINAL AND OTHER MODES OF THERAPY (continued)—CHRONIC ARTICULAR GOUT AND ASSOCIATED MORBID CONDITIONS |
|
| Alkalies. Contrasts between Salts of Sodium and Potash. Differential Indications for their Usage. Alternatives. Salicylates. Benzoates. Hexamine. Iodides. Iodine. Albumen Compounds. Collosol Preparations of Iodine. Guaiacum. Local Measures in Chronic Articular Gout. Treatment of Tophi. Ionisation. Surgical Measures. Treatment of Associated Morbid Conditions. Fibrositis. Lumbago. Sciatica. Acute Brachial Fibrositis. Local Massage. Oxaluria. Glycosuria. Hyperchlorhydria. Gouty Phlebitis. Gouty Eczema. Gouty Nephritis | pp. 397-417 |
| CHAPTER XXXI CLIMATO-THERAPY, HYDRO-THERAPY, ETC. |
|
| Climate. Choice of Residence. Clothing. Exercise. Massage. General Hydro-therapy. Importance of thorough Physical Examination. Individual Reactive Peculiarities. Prophylactic Measures. Contra-indications and Untoward Complications. Methods of Application of General Hydro-therapy. Immersion Baths. Aix and Vichy Massage. Vapour Baths. Indications for Sub-thermal Baths. Local Hydro-therapy. Varieties of Douche. Treatment by Hyperæmia | pp. 418-430[xviii] |
| CHAPTER XXXII MINERAL SPRINGS AND CHOICE OF SPA |
|
| Difficulties of Definition and Classification. Radio-activity. General Principles of Spa Treatment. Physiological Action of Radium Emanation. Activation of Body Ferments. Influence of Uric Acid Metabolism. Increased Excretion of Uric Acid. Subjective Phenomena of Gout in Relation to Blood Content and Excretion of Uric Acid. Therapeutic Action and Application. Alimentary Disorders. Glycosuria. Raised Blood Pressure. Choice of Spa. The Spare and the Obese. Waters Suitable for Various Types of Dyspepsia. Bickel’s Experiments. Mineral Waters in Associated Morbid Conditions. Glycosuria. Oxaluria. Phlebitis. Respiratory Disorders. Fibrositis. Gouty Eczema. Uric Acid Gravel. Arterio-sclerosis. Chronic Nephritis. Concluding Remarks on Spa Treatment | pp. 431-465 |
| INDEX | pp. 457-469 |
“Teeth, bones, and hair,” quoth the Sage of Norwich, “give the most lasting defiance to corruption,” and were it not that “Time which antiquates antiquities and hath an art to make dust of all things hath yet spared these minor monuments,” it might perhaps have been inferred that gout was the primordial arthritic disease that afflicted mankind.
That it was the first articular affection to achieve clinical individuality may be allowed, but, from the aspect of antiquity, gout is relatively modern—the appanage of civilisation. True, Hippocrates, discoursing in the famous Asclepion at Cos, enunciated his aphorisms on gout some 300 years before the Christian Era, the dawn of which moreover found Cicero in his discussions at Tusculum lamenting its excruciating tortures “doloribus podagræ cruciari” and the peculiar burning character of its pains “cum arderet podagræ doloribus.”
But what of that? For did not Flinders Petrie in the hoary tombs of Gurob (dating back to the 28th Dynasty 1300 B.C.) find in mouldering skeletons of bygone civilisations unequivocal evidence of osteoarthritis.[1] But despite these sure though silent witnesses of the prevalence of this disorder among the ancient people of Egypt, yet in contrast with gout, no hint transpires in the writings of Greek or Roman physicians, nor those of much[2] later date, that the condition was recognised clinically, as a joint disorder, distinct from others of the same category.
Small call to marvel thereat, for how much more arresting the clinical facies of gout, with its classic insignia—tumor, robor, calor, et dolor—than of osteoarthritis, its etiolate tokens indicative rather of infirmity than of disease. Apart from this, it may well be that the early Egyptians owed their relative immunity from gout, and alike their proneness to osteoarthritis, to living hard laborious days, unenervated by that luxury and sloth, which in the first century A.D. drew upon the ancient Romans the caustic reproofs of Pliny and Seneca. For the old philosophers lamented the growing prevalence of the disorder, almost unknown in the early, more virile days of the Empire, rightly seeing in it but another harbinger of impending decadence, clearly attributable as it was to riotous living and debauchery.
Indeed, we have it on the authority of Galen that “In the time of Hippocrates there were only a few who suffered from podagra, such was the moderation in living, but in our own times, when sensuality has touched the highest conceivable point, the number of patients with the gout has grown to an extent that cannot be estimated.”
Nothing, in truth, seems more clearly established than this, that gout is the Nemesis that overtakes those addicted to luxurious habits and dietetic excesses. On the testimony of eminent travellers we are assured that amongst aborigines the disease is unknown. The indigenous native tribes of India are immune, but not so the immigrant flesh-loving Parsees. Strange to relate, Anglo-Indians of gouty habit, while resident in the Orient, seem exempt, some say, owing to cutaneous activity, but more probably because quâ Rendu “these are countries in which we cannot survive unless we are frugal.”
Nations too, like individuals, when fallen on hard times, lose their gout. Thus the Arabs, at the zenith of their mediæval Empire, were prone thereto, but in these latter days are almost exempt from its ravages. But, on the other hand, if we are to believe Professor Cantani, in no other disorder are the “sins of the fathers visited upon the children” with such pertinacity, claiming as he does that its marked incidence in Southern Italians is a direct heritage from the ancient Greeks and Romans.
Reverting to our own country, what evidences as to its antiquity are forthcoming? This much may at any rate be affirmed, that according to Mason Good “Gout is one of the maladies which seem to have been common in England in its earliest ages[3] of barbarism. It is frequently noticed by the Anglo-Saxon historian, and the name assigned to it is Fot-adl.”
Cockayne, in his “Leechdoms Wortcumming and Starcraft,” of early England, has it that the word “addle” appears to have been a synonym for ailment, thus “Shingles was hight circle addle.” That gout should have flourished so among our Anglo-Saxon forbears is perhaps a matter for regret but not for astonishment, when we recall their coarse Gargantuan feasts, washed down with doughty draughts of ale, “sack and the well spic’d hippocras.”
Gout, we see then, even in our own land, is full ancient, and the word, as Bradley as shown, may be traced in the English tongue right through the literature of the various periods.[2] This not only in the brochures of physicians, but also as in the days of Lucian in the works of historians, and the satires of poets, which indeed abound with allusions to the disease.
The Greek physicians, quite familiar as they were with the overt manifestations of gout, did not, as far as its nosology was concerned, commit themselves to any appellation that might imply their adherence to any theory as to its causation. They contented themselves with a mere topographical designation, terming the affection, podagra, chirargra, etc., according as foot or hand was the seat of the disorder, while for polyarticular types the generic term arthritis was invoked.
Nevertheless the old Greek physicians had their views as to its pathology. Thus the source of the peccant humours resided for them in the brain, which they had invested with all the functions of an absorbent and secreting gland. This hypothesis in time was displaced by the true humoral theory, according to which the[4] bodily fluids, those found in the alimentary canal, the blood stream, and the glandular organs, were the primordial agents of disease. No need, albeit, for gibes on our part, for how true much of their conception of the genesis of disease even to-day. Indeed, what else than a fusion of the foregoing views? the modern theory of Sir Dyce Duckworth, who would ascribe gout to the combined influence of neural and humoral factors. And now to consider briefly the individual views of the fathers of medicine.
In the eyes of the pioneer priest-physician, the disorder was attributable to a retention of humours, and many of his dicta have stood the corroding test of time. He noted, like Sydenham, its tendency to periodicity, its liability to recur at spring and fall. Also that eunuchs are immune and youths also, ante usum veneris, while in females its incidence is usually delayed until after the menopause.
The curability of the disease in its earlier stages was affirmed, but that after the deposit of chalk in the joints it proved rebellious to treatment, which for him resided in purgation and the local application of cooling agents.
In the first and second centuries Celsus, Galen, and Aretæus the Cappadocian recounted their views as to its nature and therapy, while the Augustan poet in his Pontic epistles, like Hippocrates, laments that his gouty swellings defy the art of medicine.
To Celsus, venesection at the onset of an attack seemed both curative and prophylactic. Corpulence of habit a state to be avoided, and conformably he prescribed frugality of fare and adequate exercise. Galen (130-200), more venturesome than his contemporaries, voiced his belief that tophi were compact of phlegm, blood, or bile, singly or in combination. For the rest, he enjoined bleeding and purgation and local applications, contravening, by the bye, Hippocrates’ claim as to the immunity of eunuchs in that in his (Galen’s) day their sloth and intemperance were such as readily begat the disorder.
About this period Lucian of Saramosta enumerated the various anti-gout nostrums vaunted as specifics in his day. Though in his comic poems, the Trago-podagra and Ocypus he rightly holds up to scorn the charlatanism rampant at the time, still it is quite clear that he possessed no mean knowledge of the clinical vagaries of gout and was quite alive to the mischief of too meddlesome treatment thereof.
Said the hero of the Trago-podagra:
Again, Seneca, in a jeremiad on the decadent habits of Roman ladies of the patrician order, observes: “The nature of women is not altered but their manner of living, for while they rival the men in every kind of licentiousness, they equal them too in their very bodily disorders. Why need we then be surprised at seeing so many of the female sex afflicted with gout.” That the old philosopher’s misgivings were but too well founded is obvious when we recall that so widespread were the ravages of gout among the Romans in the third century that Diocletian, by an edict, exempted from the public burdens those severely crippled thereby, in sooth a blatant illustration of political pandering to national vice.
But to return to the researches of physicians, those of Aretæus seem to have been the most enlightened of his time. A succinct account of the mode of invasion of gout and its centripetal spread in later stages to the larger joints is followed by enumeration of the exciting causes of outbreaks. Anent these, he quaintly notes the reluctance which the victims display to assigning the malady to its true cause—their own excesses—preferring to attribute it to a new shoe, a long walk, or an injury. Noting that men are more liable than women, he tells us, too, that between the gouty attacks the subject has even carried off the palm in the Olympic games. The white hellebore, to his mind, at any rate in early attacks, was the remedy par excellence. But, for the true nature of the disease, he, with humility and piety, avows that its secret origin is known only to the gods.
Not so his successor Cælius Aurelianus, who affirmed it to be not only hereditary but due to indigestion, over-drinking, debauchery, and exposure. Under their maleficent influence morbid humours were generated which sooner or later found a vent in one or other foot, with a predilection for tendons and ligaments; these structures he averred being the locus morbi. An abstemious dietary with exercise was his sheet anchor in therapy, with local scarification in preference to cupping and leeching, but violent purging and emetics he decried, and drugs to him made little appeal.
More ambitious than his predecessors, Alexander of Tralles, in the sixth century, held that there were many varieties of gout, some due to intra-articular effusions of blood, reminding us of Rieken’s view (1829) that hæmophilia is an anomalous variant of gout. Other cases, Alexander averred, were the outcome of[6] extravasation of bile or other peccant fluids between tendons and ligaments. Abstinence, especially from wine and blood-forming foods, was enjoined and a plentiful use of drastic purgatives, elaterium, etc., with local sinapisms and blisters. For the absorption of chalk stones he commended unguents containing oil, turpentine, ammoniacum, dragon’s blood, and litharge.
Aetius, a contemporary, is noteworthy in that during the intervals of attacks he highly eulogised the use of friction while, like Alexander of Tralles, he seems to have been much impressed with the virtues of colchicum, of which he says, “Hermodactylon confestim minuit dolores.” Planchon, in 1855, in his treatise, “De hermodactes au point de vue botanique et pharmaceutique,” claims to have proved that the hermodactylon of the ancients was Colchicum variegatum, of similar properties to the Colchicum autumnale.
Paulus Ægineta, like most of his confrères, regarded gout and rheumatism as the same disorder, differing only in their location. He subscribed whole heartedly to the prevailing humoral theory, but inclined to think the site of the discharged humours was influenced by weakness or injury of the parts. He noted, too, that mental states, sorrow, anxiety, etc., might act as determining causes.
Nor will any historical résumé rest complete without a reference to the numerous works of the Arabian physicians—Avicenna, Rhazes, Serapion, and Haly Abbas—who one or other all maintained gout to be hereditary, rare in women and due to peccant humours, developed in the train of depletions, debaucheries, and the like.
In the thirteenth century the Greek terms “podagra,” “chirargra,” etc., were to a large extent abandoned, and following Radulfe’s lead gave way to the use of the generic term “gout,” derived from the Latin “gutta.” Its adoption was doubtless traceable to the prevailing humoral views of the origin of the disorder, as due to some morbid matter exuding by “drops” into the joint cavities. Indeed, according to Johnson, the word “gut” was used as a synonym for “drop” by Scottish physicians even in his day.
In any case, the term found little difficulty in installing itself among all nations, taking in French the form “goutte,” in German “gicht,” in Spanish “gota,” etc. Trousseau thought it “an admirable name, because in whatever sense it may have been originally employed by those by whom it was invented, it is not now given to anything else than that to which it is applied.” In contrast[7] therewith, that trenchant critic Pye-Smith complained of the laxity with which the Germans invoked the word “gicht.” He says it is popularly credited with all the pains which are called “rheumatics” in England. “Sometimes ‘gicht’ is nothing but bad corns and is rarely true gout.” Albeit, Pye-Smith did not, as we shall see later, hold even his English confrères in this respect void of offence.
From these remote times onwards through the Middle Ages to the present day, an almost continuous series of historical records testify that not only has gout always been with us, but that its clinical characters throughout the ages have remained unaltered, conforming ever to the primitive type. During the seventeenth and eighteenth centuries many physicians, both British and continental, ventilated their views as to the nature of gout, all swearing allegiance to the old humoral pathology, notably Sydenham, Boerhaave, Van Swieten, Hoffmann, Cadogan, etc.
The English Hippocrates, as Trousseau christened the illustrious Sydenham, displayed his catholic outlook by the pregnant words: “No very limited theory and no one particular hypothesis can be found applicable to explain the whole nature of gout.” A live-long martyr himself thereto, he brought all the strength of his dominating intellect to bear upon its elucidation. As to its causation, he held it to be due to a “morbific matter,” the outcome of imperfect “coctions” in the primæ viæ and in the secondary assimilating organs. He refrained from speculating as to the constitution of the materia peccans, but as Trousseau observes, “he made his morbi seminium play the part which modern chemistry attributes to the products it has discovered. Take it all in all,” he says, “the theory of the great English physician is much more medical than the theories of modern chemists.”
The word “tophus” or “tofus,” the Greek τοφος, seems to have been applied to rough crumbling rock, the disintegrated volcanic tufa. As to its constitution it is clear from the above quotation that Virgil evidently associated it with chalk, a shrewder guess than the fanciful hypothesis of Galen, though the views of Paracelsus (1493-1541) enunciated some centuries subsequently, were even more grotesque, a “mucous essence,” a “Tartarus” burning “like hell fire.”
Nevertheless, our contempt need be chastened when we recollect[8] that, up to the latter half of the eighteenth century, equally weird assumptions found acceptance. By some “various excrementitial humours,” by others “checked and decomposing sweat” were deemed the basis of tophi.
A mucilaginous extract, derived from the solid and liquid intake, appealed to some as an explanation of their formation, while to others, tophi were compounds of subtle and penetrating salts.
But the later view, doubtless the reflex of etiological hypotheses, was that tophi were of tartareous nature, closely similar to that encrusting the interior of wine casks. Hoffmann declared that the materies morbi actually was a salt of tartar circulating in the blood. His investigations of tophi and also of the stools, saliva, and urine of gouty subjects, convinced him that the peccant matter was tartar of wine.
Hoffmann’s views, however, were laughed to scorn by M. Coste as being obviously absurd, inasmuch as gout was not uncommon amongst those who had never partaken of wine, ergo, never of tartar. How infinitely more physicianly the inference of Sydenham, who, like some of the older humoralists held the tophus to be “undigested gouty matter thrown out around the joints in a liquid form and afterwards becoming hardened.”
So it went on until, alchemy being displaced by chemistry, uric acid was in 1775 discovered by Scheele, and in 1787 Wollaston established its existence in tophi, and to the further elaboration of our knowledge of this substance we shall allude later. Here we would only observe that Wollaston’s researches marked the coming substitution of the humoral and solidist theories by a chemical hypothesis as to the etiology of gout.
The absurd delusion, not wholly dissipated even to-day, that to have the gout, “Morbus Dominorum,” was highly creditable, a mark of good breeding, was firmly ingrained in our forefathers. We all recall the story of the old Scottish gentlewoman who would never allow that any but people of family could have bonâ fide gout. Let but the roturier aspire to this privilege, and she scouted the very idea—“Na, na, it is only my father and Lord Gallowa’ that have the regular gout.” As to the origin of this mistaken ambition, it most probably was the outcome of the fact that it was peculiarly an appanage of the great, the wealthy, and alas! those of intellectual distinction!
Statesmen, warriors, literary men and poets loom large amongst its victims. Lord Burleigh suffered greatly therefrom, and good[9] Queen Bess on that account always bid him sit in her presence, and was wont to say, “My Lord, we make much of you, not for your bad legs, but for your good head!” With more humour, Horace Walpole complained, “If either my father or mother had had it I should not dislike it so much! I am herald enough to approve it, if descended genealogically, but it is an absolute upstart in me, and what is more provoking, I had trusted in my great abstinence for keeping it from me, but thus it is!”[3]
Of warriors, Lord Howe, Marshal Saxe, Wallenstein, and Condé were among its victims; while of literary men and poets thus afflicted may be mentioned Milton, Dryden, Congreve, Linnæus, Newton, and Fielding. Of physicians, the great Harvey was a martyr to gout, and was wont to treat it after the following heroic fashion. Sitting, in the coldest weather, with bare legs on the leads of Cockaine House, he would immerse them in a pail of water until he nearly collapsed from cold. Mrs. Hunter, wife of John Hunter, in a letter to Edward Jenner about her distinguished husband, dated Bath, September 18th, 1785, laments that “He has been tormented with the flying gout since last March!” In short, the disorder, with a notable frequency, figures in the life history of some of the ablest men in all ages, hence the complacency with which lesser men, often without good reason, affect to have the gout.
“But nothing,” as Sir Thomas Watson says, “can show more strongly the power of fashion than this desire to be thought to possess, not only the tone and manners of the higher orders of society, not their follies merely and pleasant vices, but their very pains and aches, their bodily imperfections and infirmities. All this is more than sufficiently ludicrous and lamentable, but so it is. Even the philosophic Sydenham consoled himself under the sufferings of the gout with the reflection that it destroys more rich men than poor, more wise men than fools.”
“At vero (quod mihi aliisque licet, tam fortunæ quam Ingenii dotibus mediocriter instructis, hoc morbo laborantibus solatio esse possit) ita vixerunt atque ita tandem mortem obierunt magni Reges, Dynastæ, exercituum classiumque Duces, Philosophi, aliique his similes haud pauci.
“Verbo dicam, articularis hicce morbus (quod vix de quovis alio adfirmaveris) divites plures interemit quam pauperes, plures sapientes quam fatuos.”
The Scotch at one time regarded gout as fit and meet punishment for the luxurious living of the English. But, as was pointed out, the cogency of the moral was somewhat spoilt by the fact that the disorder was found to exist even among the poor and[10] temperate Faroe Islanders. In truth, although “the taint may be hereditary, it may be generated by a low diet and abstinence carried to extremes.”
The fallacy that longevity and freedom from other maladies was ensured by gout was prevalent among our forefathers. In satire of this, one Philander Misaurus issued a brochure entitled “The Honour of the Gout,” and purporting to be writ, “Right in the Heat of a violent Paroxysm; and now publish’d for the common Good” (1735). “Bless us,” says he, “that any man should wish to be rid of the Gout; for want of which he may become obnoxious to fevers and headache, be blinded in his understanding, loose the best of his Health and the Security of his Life”; and forthwith in his zeal for the common good gives us the following invocation:—
He quaintly suggests that Paracelsus, if he would ensure men against death, had but to inoculate them with gout. Gout, indeed, was held to be a jealous disorder, intolerant of usurpation by any other disease, recalling the remark of Posthumus to his gaolers:—
Still the fallacy that gout was salutary died hard, and although it seems incredible, yet, Archbishop Sheldon is said not only to have longed for gout but actually to have offered £1,000 to any one who would procure him this blessing; for he regarded gout as “the only remedy for the distress in his head.” How ingrained the notion may be gathered from the fact that in the early part of the last century, M. Coste in his “Traité Pratique de la Goutte,” observed: “A popular error, which I wish to expose in a few words, is this prejudice, which has already lasted more than two[11] thousand years, and which has reached even the thrones of princes, where the disease commonly shows itself, viz., that gout prolongs life (que la goutte prolonge la vie). This error,” says he, “has taken the surest method of introducing itself, by making flattering promises, by persuading its victims that there is a singular advantage in having gout, and that the malady drives away all other evils, and that it ensures long life to those whom it attacks.”
In like refrain, our own countryman Heberden deplores that people “are neither ashamed nor afraid of it; but solace themselves with the hope that they shall one day have the gout; or, if they have already suffered it, impute all their other ails, not to having had too much of that disease, but to wanting more. The gout, far from being blamed as the cause, is looked up to as the expected deliverer from these evils.” Such deluded views being prevalent, it is hardly a matter for surprise that misguided persons deliberately courted a “fit of the gout” by resorting to excess and intemperance.
But alas, while the initial visitations of gout, after their passing, may leave behind them a renewed sense of well-being, it is no less certain that, when once installed, the intervals of respite grow shorter and shorter. Crippledom grows apace, the general health breaks and untimely senescence overtakes the worn-out victim, and, as Heberden puts it, “that gout causes premature death, when all the comforts of life ...
are destroyed, and the physical powers either insensibly undermined or suddenly crushed by an attack of paralysis or apoplexy, should hardly be reckoned among the misfortunes attending the disease.”
But for our encouragement it may be observed that not always does gout carry with it such a terrible Nemesis. “Gout is the disease of those who will have it,” said a wise physician, and though the inbred gouty tendency may be so strong as to cast defiance at abstinence, yet it is by no means always so. A man may inherit gout, but he need not foster it by self-indulgence. Much less need he, as so often happens, acquire it by depraved habits of life. In no disease do sobriety and virtuous living ensure so great a reward. As Sir Thomas Watson long since said to those inheriting this unwelcome legacy: “Let the son of a rich and gouty nobleman change places with the son of a farm servant, and earn his temperate meal by the daily[12] sweat of his brow, and the chance of his being visited with gout will be very small.”
So accurate and graphic were the clinical pictures of gout depicted by the ancient physicians that there is no doubt the gout of to-day conforms to the primitive type as met with among the Greeks and Romans. This certainly as regards the arthritic phenomena of the disease; for in those remote ages little or no account seems to have been taken of its irregular or ab-articular manifestations. While disregard of the latter group renders more credible their claims as to the widespread prevalence of the affection, nevertheless, I think there can be no doubt that the frequency of gout amongst the ancient Greeks and Romans was probably over-estimated.
Can it be questioned that a large percentage of the cases of gout in those bygone times consisted of undifferentiated infective forms of arthritis. Syphilis and gonorrhœa must have existed then as now, and their specific forms of arthritis, how easily confused with “rich man’s gout!” Surely too, they, like ourselves, must have suffered with states of oral sepsis, pyorrhœa alveolaris, etc., not to speak of infective disorders, with their correlated arthritides. In short, the differentiation of arthritic disorders was then hardly in its infancy, and it is in light of this disability that we must appraise their clearly extravagant assertions as to the widespread ravages of gout in their day.
But passing to more recent times, there is little doubt that the classical type of podagra is very much rarer to-day than, say, in the time of Sydenham. Indeed, it may be said to be becoming progressively infrequent. Thus, writing in 1890, Sir Dyce Duckworth tells us that some twenty-six years prior to that date, Sir George Burrows informed him that “he then saw fewer cases of acute gout than he was accustomed to see in his earlier practice.” It may be recalled, too, that Sir Charles Scudamore, in retrospect of his own experience, of still earlier date, was led to much the same conclusion. Moreover, not only is the disorder less frequent, but its virulence seems to have suffered attenuation, and this to a marked degree.
Again, Ewart, writing in 1896, observed that “goutiness” is becoming relatively more common than declared gout. This, he thought, by reason of the increasing attenuation in transmission of the “gouty” taint. In this, as well as the more mitigated[13] character of the arthritic manifestations, he saw hope of “an ultimate extinction of the bias in ‘gouty’ families.” For, as he rightly says, side by side with “the tendency to a reproduction of morbid parental peculiarities, there is a yet stronger tendency in Nature to reproduce the healthy type of the race in each successive generation.”
But while there is a general consensus of opinion as to the growing rarity of acute regular gout, on the other hand, many, as if loth to part with the disorder, claim that pari passu with the decline of regular types the incidence of irregular manifestations grew proportionately.
In my experience the incidence of regular gout has appreciably diminished during the past twenty years. Moreover, such examples as one has met with incline much more in character to the asthenic than to the sthenic variety of podagra. But, in contrast to many, I have observed no increase in the irregular manifestations of gout. On the contrary, a steady diminution in the nebulous content of this category, but to this vexed subject we shall recur in a subsequent chapter dealing with the propriety or not of retaining this ill-defined term in medical nomenclature.
My conclusion, then, is that not only is arthritic gout becoming less prevalent, but that the type of the disease also has suffered attenuation. Probably this dual change is the outcome of many factors, not the least of these an increase in national sobriety. For as Sir Alfred Garrod long since observed, “There is no truth in medicine better established than the fact that the use of fermented liquors is the most powerful of all the predisposing causes of gout; nay, so powerful, that it may be a question whether gout would ever have been known to mankind had such beverages not being indulged in.
Under the vague term “articulorum passio” or “arthritis” the physicians of antiquity handed down to posterity the clinical description of a disease in the varied symptomatology of which we may descry at one time the features of gout and anon those of rheumatism. But centuries had to elapse before gout became differentiated from rheumatism. For there is no doubt that not only the Greek and Roman physicians, but those also of the Græco-Arabian school, confounded these two disorders, or more accurately failed to differentiate rheumatism.
So it is that Charcot, reviewing the antiquity of gout, while he pays a graceful tribute to the ancient physicians for their masterly disquisitions thereon, at the same time deplored their silence on the subject of articular rheumatism.
This absence of allusion thereto is the more remarkable in that the term “rheumatism” or “rheumes” dates from a very remote period. Both words, in truth, were indifferently enlisted to denote all those diseases deemed attributable to the defluxion of some acrid humour upon one or other part of the body. Used by the ancients more in accordance with its etymological sense, the term “rheumes” or “rheumatism,” finds a place even in the writings of Pliny and Ovid. But our modern conception of the disorder differs widely from “the flux of humours” which the Greeks named rheumatism, or “the sharpe and eager flux of fleam” which for them characterised an attack of the “rheumes.”
The early English authors, too, invoked the word as a general term descriptive of various forms of disease. Sir Thomas Elyot, in his “Castel of Health,” so scoffed at by the faculty in his day, inculcates abstemiousness in those afflicted with the “rheumes,” and in “Julius Caesar,” Brutus is warned by Portia not to tempt “the rheumy unpurged ayre of night,” a clear indication that the term was used as a synonym for fluxions, humours and catarrhs of all sorts. But as to the malign articular forms of the affection, never a word; and this almost inexplicable silence led Sydenham, Haecker and Leupoldt to surmise that articular rheumatism was a modern disease unknown amongst the ancients.
Hallowed by tradition, this erroneous conception of the identity of gout and rheumatism endured until 1642, when Baillon, in his treatise “De Rheumatismo et Pleuritide,” effected a cleavage, at any rate between the acute varieties of these two diseases.
Dissociating the term “rheumatism” from its primitive interpretation, Baillon restricted its usage to that particular group of symptoms we now call acute articular rheumatism. In the same century Sydenham, in his “Classical Observations,” materially clarified the existing clinical confusion, defining with his customary lucidity the essential differences between the two disorders.
Bearing in mind the centuries that elapsed before the acute articular forms of gout and rheumatism were dissociated, one ceases to marvel that the task, incomparably more difficult, of discriminating between the chronic forms of these diseases is even now barely accomplished.
“Rheumatissimus agnatus podagræ” said our forefathers, the axiom postulating not the actual identity of the two affections, but a near relationship, and in this non-committal phrase we may, I think, descry the birth of that modern term “L’arthritisme,” so beloved of the French physicians. Even as late as the beginning of the nineteenth century Chomel at the Saltpetrière taught his pupils that gout and rheumatism were but clinical variants of an underlying “arthritic diathesis,” his successor Pidoux being still more insistent that the two disorders sprang from one common root. Even Charcot and Trousseau, convinced as they were of the essential distinctness of the two disorders, nevertheless admitted that at the bedside their chronic manifestations were with difficulty dissociated, the former pointing to the terms “rhumatisme goutteux” and “rheumatic gout” as tacit acknowledgments of our impotence.
Nor did this view that gout and alike rheumatism are the outcome of a basic arthritic diathesis fail of doughty supporters in this country. Thus Hutchinson, in his “Pedigree of Disease,” observes “gout is but rarely of pure breed, and often a complication of rheumatism. It so often mixes itself up with rheumatism, and the two, in hereditary transmission, become so intimately united, that it is a matter of considerable difficulty to ascertain how far rheumatism pure can go ... when this complication exists. It shows its power, we may suspect, by inducing a permanent modification of tissue, and it is to this modification that[16] the peculiarities in the processes (transitory rheumatic pains in joints, fasciæ, and muscles, chronic crippling arthritis, destructive arthritis with eburnation, lumbago, sciatica) are due. Hence the impossibility under many conditions of discriminating between gout and rheumatism.”
Laycock also subscribed to Charcot’s view, and Sir Dyce Duckworth confesses that the conception of “a basic diathetic habit of body called arthritic has well commended itself to my mind,” while as to the clinical commingling of the two disorders Sir Charles Scudamore spoke with no uncertain voice. That an individual may in youth suffer from acute articular rheumatism, and later in life develop gout, is undeniable, as also the reverse, that a gouty subject may be harassed by manifestations of chronic rheumatism or fibrositis. But this mutual trenching of the one upon the clinical territory of the other must not be allowed to impair our views as to the essential distinctness of gout and rheumatism. It is undeniable that the difficulty of differentiating between the chronic forms of these two disorders is great, for not even the revelations of skiagraphy, in the absence of a clinical history, will suffice to effect a discrimination. But to a further consideration of this vexed matter we refer the reader to the coming chapters on Diagnosis.
But to resume our thread, one great step forward we owe to Cullen, who not only differentiated acute from chronic articular rheumatism, but also clearly portrayed the clinical distinctness from both of muscular rheumatism. In so doing, he materially assisted in the differentiation of these same disorders from gout. But at the same time, owing to his immoderate advocacy of “chill” as the one great cause of rheumatism in all its forms, he undoubtedly retarded progress. For immediately there arose a cloud of witnesses who claimed a “rheumatic kinship” for a myriad visceral disorders, the victims of which had suffered exposure. Thus throughout the seventeenth and eighteenth centuries many of the conditions now assigned to irregular gout were affiliated instead to rheumatism.
Apart from Cullen’s contribution the eighteenth century was unmarked by any further advance in differentiating the mass of heterogenous joint affections, indifferently classed as gout and[17] rheumatism. The physicians of this period, indeed, appear not only to have done little themselves, but had omitted to utilise the useful indications furnished by their predecessors.
Thus how much more swiftly would the clinical distinctness of chronic articular gout from rheumatoid arthritis have been realised had Sydenham’s dicta in the seventeenth century regarding this intricate problem been duly appreciated. Up to his time, the clinical descriptions of rheumatoid arthritis appeared now under gout, now under rheumatism. As for Sydenham himself, he placed the disorder, nosologically speaking, under chronic rheumatism, of which he believed it to be an apyretic variety. But the importance of his researches resides in this—he pointed out that it differed essentially from gout, but that, in resemblance thereof, it might endure throughout life, its course diversified by remissions and exacerbations. Also he tells us that its excruciating pains, even when of prolonged standing, sometimes cease spontaneously, noting also that the joints are, so to speak, turned over, and that there are nodosities, especially on the inside of the fingers.
Nevertheless, if we except Musgrave’s work (1703), “Arthritis ex Chlorosi,” which included some undoubted examples of rheumatoid or atrophic arthritis, no note was taken of Sydenham’s contention until a century afterwards. True, John Hunter in 1759 described the morbid anatomy of osteoarthritis or the hypertrophic forms of arthritis deformans, but not until 1868 was the true significance of Sydenham’s work appreciated, a most generous tribute being then accorded him by the great French physician Trousseau.
In 1800 Landre Beauvais published his clinical description of rheumatoid arthritis under the title “goutte asthenique primitif.” That Beauvais, as Sir Archibald Garrod contends, included under this title some cases of true gout is beyond doubt. But the words “Doit admettre une nouvelle espèce de goutte,” go far to justify Charcot in his claim that Beauvais, despite the title of his brochure, fully realised that the disease differed from gout.
A few years later (1804-1816), Heberden, in his Commentaries, insisted on the essential distinctness of rheumatoid arthritis from gout. Thus he wrote, “The disease called chronical rheumatism, which often passes under the general name of rheumatism and is sometimes supposed to be gout, is in reality a very different distemper from the genuine gout, and from the acute rheumatism, and ought to be carefully distinguished from both.” As to its salient features he noted its afebrile nature, the lack of redness in the skin over the affected joints, the relative absence of pain, and that it displayed no special tendency to begin in the feet. It was further marked by a protracted course involving severe crippling,[18] while the peculiar nodosities on the fingers are still associated with his name.
In 1805 Haygarth published his classical essay, “A Clinical History of the Nodosity of the Joints,” the opening sentence of which shows that, comparably with his successors, he lamented the laxity with which the term “rheumatism” was invoked and applied “to a great variety of disorders which beside pain, have but few symptoms that connect them together.” A purist in nosology, he equally deplored the term “rheumatick gout” as tending to perpetuate its confusion with gout and rheumatism, and suggested the term “Nodosities,” in the hope that “as a distinct genus it will become a more direct object of medical attention.”
Alas, even as late as 1868 Trousseau deplored the retention of the term “rheumatic gout” by Garrod and Fuller and his own countryman Trastour. But, in common justice to Garrod, it must be allowed that in the third edition of his work he definitely applied the term rheumatoid arthritis to the disorder in question. Nor can we refrain from recording Fuller’s words that “the natural history of rheumatic gout accords but little with that of acute rheumatism, and is equally inconsistent with that of true gout.”
In reviewing the researches of the foregoing writers it will be clearly seen that though they did yeoman service in differentiating broadly gout from the disorders grouped under Arthritis Deformans, there is little doubt that not for many years afterwards was their distinctiveness sufficiently realised. This may be in large part attributed to the fact that they still awaited the next great process of fission as applied to chronic joint disorders.
I allude in the first place to Charcot’s momentous discovery of the nerve arthropathies, and secondly, to the cleavage of arthritis deformans into the rheumatoid or atrophic, and the osteoarthritic or hypertrophic varieties.
It is to Vidal that we are indebted for the first clinical description of the atrophic type. Charcot in his lectures refers to it as the “Atrophic form of Vidal,” noting that in this variety “induration of the skin, a sort of scleroderma develops, the cutaneous covering is cold, pale, smooth, polished, and will not wrinkle, adding also that in such cases atrophy of the bones and muscles accompanies the wasting of the soft tissues.”
Notwithstanding this, Charcot, to our mind, unquestionably refers to the category of chronic articular gout certain of these examples of Vidal’s atrophic type of arthritis deformans. The[19] reasons he adduces for their gouty nature are, to say the least of it, both conflicting and unconvincing. On the one hand, he admits that they are clinically indistinguishable from Vidal’s type, in respect of their pronounced atrophic changes; on the other, he postulates them as gouty even though the uratic deposits “either do not exist at all, or only mere traces of them, or when only the articular cartilages are invaded by the urate of soda.” It must be conceded that chronic articular gout and rheumatoid or atrophic arthritis are totally distinct affections.
Now as to the hypertrophic variety, or osteoarthritis, which, of the twain, more closely resembles gout, and whose confusion therewith is far from infrequent even at the present time. Sir Dyce Duckworth, while he recognises with Charcot a tophaceous form of chronic articular gout, postulates the existence of another type, arthritis deformans uratica. Unlike Charcot, however, he seems only to have included under this term instances of the osteoarthritic or hypertrophic variety. But like Charcot, his claim that this particular variety is of gouty nature seems to rest on equally frail foundations, as witness his statement that they “may be complicated with visible or invisible tophaceous deposits!”
That osteoarthritis and gout may coexist in the same individual is certain, and equally sure is it that uratic deposits may supervene in joints the seat of osteoarthritis. But it is now, I think, generally conceded that, despite these coincidences, gouty arthritis and osteoarthritis are wholly distinct disorders, of wholly different origin.
At this period of our historical résumé we see that by the withdrawal of these three great groups—rheumatism, the nerve arthropathies and arthritis deformans—the domain of gout has, through these several allotments, undergone substantial shrinkage.
Yet again was the territory of gout destined to undergo further restriction, and this largely owing to the rise of the science of bacteriology. For in light of recent improvements in diagnostic methods, who can escape the conviction that under the term “gout” had been wrongfully included many forms of arthritis, now known to be due to specific infections. What, for example, of Hippocrates’ aphorism that gout was unknown in youths—ante usum veneris—who can doubt that some of his reputed cases of gout were examples of gonococcal or syphilitic arthritis?
What, too, of all the other infective arthritides—influenzal, pneumoccocal, scarlatinal, typhoidal, meningococcal—to mention only those actually affiliated to some specific organism. For gout,[20] be it noted, confers no exemption from other arthritic diseases, but how in time past were such to be differentiated therefrom?
Again, gouty subjects, as has been recently emphasised, are notoriously prone to pyorrhœa alveolaris, and how difficult, given the supervention of an arthritis in such to define the causal agent—gout or sepsis, which? Small wonder then, that the clinical content of gout, not only to ancient, but also to latter day physicians, loomed large, swollen as it undoubtedly was by the inclusion of infective arthritides, not to mention those of traumatic or static origin.
That more of these alien joint disorders—les pseudo-rheumatismes infectieux, as M. Bouchard terms them, were relegated to the “rheumatic” than to the “gouty” category, may perhaps be allowed, but still gout was undoubtedly allotted its full share and to boot. Moreover, if to “rheumatism” was wrongly affiliated the lion’s share of the infective arthritides, on the other hand to “gout” accrued a host of unrelated visceral disorders, not to mention affections of the nervous and vascular structures, etc.
In endeavouring to summarise the results of our brief retrospect, the somewhat chastening fact emerges, viz., that the isolation of articular gout has been achieved not so much by an increase in our knowledge as to what is gout, but through our growing perception of what is not gout. For of the causa causans of gout we are still as ignorant as in the days of Sydenham. But, in contrast, our enlightenment as to the clinical and pathological features of other forms of arthritis has steadily progressed. In this way, shorn of many alien joint disorders, gouty arthritis has slowly but surely asserted itself as a specific joint affection, distinct both from rheumatism and arthritis deformans.
In the course of our sketch, too, we have traced the evolution of the modern opinion that at least two separate conditions, “rheumatoid arthritis” and “osteoarthritis,” are comprised under arthritis deformans. This most tardily arrived at differentiation has done more than any other to clarify our conceptions as to what constitutes true “gouty arthritis.”
If to this be added the further differentiation, not only of the nerve arthropathies, but also of the infective arthridites—both specific and undifferentiated forms—it will be seen that the term “gouty arthritis,” once the most comprehensive perhaps in all medical nomenclature, has now been brought within, at any rate, reasonable distance of more or less exact definition.
The fanciful views of the humoralists as to the etiology of gout exercised almost undisputed sway up to the latter half of the eighteenth century. At that time the great Scottish physician, Cullen, took up arms against a doctrine which appeared to him unjustifiable in conception and baneful in practice. He inclined to the solidists rather than to the humoralists, claiming that gout was the outcome of a peculiar bodily conformation, and more especially of an affection of the nervous system. While he categorically denied that any materia peccans was the cause of gout, he yet admitted that in prolonged cases a peculiar matter appeared in gouty patients. But, in view of latter day revelations, Cullen, with singular prescience, maintained that the said matter was the effect and not the cause of gout.
Albeit, notwithstanding the almost universal deference accorded to Cullen, his theory, promulgated in 1874, though previously adumbrated by Stahl and afterwards reinforced by Henle, secured but few adherents. The source of this was not far to seek. For ever since the discovery of uric acid by Scheele in 1776, and its detection in tophi by Wollaston, an increasing body of opinion inclined to the view, that in some obscure way the life history of gout was bound up with that of uric acid.
Still, despite able advocacy in this country by Sir Henry Holland, Wollaston, and others, not to mention Continental authorities, such as Cruveilhier, it was felt that scientific proof of the truth of their contention was still lacking. But not for long were they left in doubt. For, in 1848, Sir Alfred Garrod’s momentous and epoch-making discovery of the presence of uric acid in the blood of the victims of gout allayed all doubts, and seemed then and for long after an all-sufficient explanation of the protean manifestations of the disease.
This distinguished physician enunciated his views in a series of propositions which embodied the result of his researches and incidentally laid the foundations of the uric acid theory.
This great physician held that, in true gout, uric acid in the form of urate of soda was, both prior to and during an attack, invariably present in the blood in abnormal quantities, and was moreover essential to its production; but with this reservation, that occasionally for a short time uric acid might be present in the circulating fluid without exciting inflammatory symptoms. This comparably with what obtains in lead poisoning, and on this account therefore he did not claim that the mere presence of uric acid therein would explain the occurrence of the gouty paroxysm.
He further averred that gouty inflammation is always accompanied by a deposition of urate of soda, crystalline and interstitial, in the inflamed part. Also that “the deposited urate of soda may be looked upon as the cause and not the effect of the gouty inflammation. Moreover, that the said inflammation tends to destruction of the urate of soda not only in the blood of the inflamed part, but also in the system generally.”
In addition, Garrod postulated implication of the kidneys, probably in the early, and certainly in the chronic stages of gout; and that the renal affection, though possibly only functional at first, subsequently became organic, with alterations in the urinary secretions.
As to the anomalous symptoms met with in gouty subjects, and alike those premonitory of a paroxysm, he ascribed them to the impure state of the blood, and due principally to the presence therein of urate of soda. Of causes predisposing to gout, if we except those attaching to individual peculiarities, they are either such as will lead to increased formation of uric acid or to retention of the same in the blood.
On the other hand, the determining causes of a gouty fit are those which induce a less alkaline condition of the blood, or which greatly augment for the time the formation of uric acid or such as temporarily check the eliminating powers of the kidneys. Lastly, his final axiom was that—in no disease but true gout is there a deposition of uric acid.
No tribute to Garrod’s masterly achievement could err on the side of generosity. A truly scientific physician, he built on the rock of sound clinical and pathological observations. For measured restraint, he stands out in pleasing contrast to those who, lacking his clinical acumen and sound judgment, brought not grist to the mill, but vain imaginings based on Garrod’s hard-won facts. His researches in truth constitute a landmark in the history of the pathology of gout, with their substitution of facts for pure hypotheses. True, though it was that, for half a century[23] before, there was a growing suspicion that lithic (uric) acid was the malign factor in the induction of gout, still it was not till Garrod’s discovery of uric acid in the blood and tissues of the “gouty,” that any definite step towards the elucidation of the problem presented by gout was attained.
One aspect of Garrod’s theory that much exercised the minds of his contemporaries was that for him uric acid was the alpha and omega of the disease, and as Ewart remarks, “If we are not over-anxious as to the stability of this mid-air foundation, everything is evolved smoothly from it on the lines of the theory.” Fortunately, however, for the progress of the art of medicine, men were over-anxious as to the why and wherefore of that accumulation of uric acid in the blood which Garrod held to be a necessary antecedent of gout. He himself, as we know, attributed it to a functional renal defect which may be inherited or acquired. To others, however, this assumption of renal inadequacy was not wholly satisfying, hence the origin of the many widely differing hypotheses from time to time advanced as to the pathogeny of the disorder.
Broadly speaking, the various conceptions proffered as to the causation of gout fall into one or other of the following categories. The primary alteration in gout is variously assumed to be:—
(1) In the blood or tissues, the so-called histogenous theories.
(2) In the bodily structures, either inborn or induced.
(3) In hepatic inadequacy.
(4) In hyperpyræmia.
(5) In the nervous system.
In his classic work, “On Urine” (1860), Parkes expressed his scepticism as to the valency of Garrod’s assumption of a primary renal inadequacy. In shrewd forecast of latter day views he was of opinion that both uric and phosphoric acids existed in some untoward combination in the blood or organs, and that this same impeded its excretion. As he says, “If this be the case, the deficient elimination is, as it were, only a consequence of more important antecedent aberrations in metamorphosis of which impeded excretion is a natural sequence. What these are, however, is quite unknown; but an unnatural formation of uric acid, either from food or tissues, may possibly be part of them.”
In 1866 Barclay lodged another objection to Garrod’s hypothesis, viz., that the baneful influence of uric acid was exercised passively and physically. Not only did he regard it as “far too mechanical,” but he also strongly dissented from his axiom that[24] gouty inflammation was invariably attended by uratic deposits. Thus he asks, “Must we of necessity find urate of soda in the stomach and the bronchi before we can admit gouty gastritis, or gouty bronchitis?” Seemingly he believed in the existence of these two clinical entities, and inasmuch as urate of soda had not been detected in situ in these disorders, he felt justified in denying that “true gouty inflammation is always associated with, or caused by, the deposit.” Moreover, this conclusion, he considered, derived colour from the fact that, “though the deposit and the inflammation were associated together in the joints, the urate of soda was seen in other parts without any evidence of its exciting inflammation there.”
His own view was that the primary change lay in the blood corpuscles, this being induced by the serial ingress of “gout producing elements” into the blood stream. As to the retention of uric acid, he deemed it not the cause, but merely a symptom, a consequence of gout. Thus he says, “The good living and the stimulants do not simply cause an excess of uric acid to form, but they end by causing some more permanent change, and probably one affecting the blood globules, which reacts on the kidney, putting a stop to the excretion of uric acid, and causing its retention in the serum, where, passing in the round of the circulation, it is very apt to become deposited as urate of soda.” Moreover, his observations of the effect of colchicum in checking a gouty paroxysm, seem to indicate, “that there is a disease to which the name ‘gout’ is applied, distinct from the excess of uric acid in the blood serum which attends its progress.”
The imaginative insight of Barclay is very remarkable. If we substitute the white for the red corpuscles we see how closely his views accord with those prevalent at the present time, when so important a rôle in the genesis of gout is attributed to the leucocytes. Moreover, as Ewart observed, the views of Barclay and Parkes approximate in principle to those afterwards propounded by Ord and Ebstein, that the bodily tissues “take an active share in determining the deposition of uric acid.”
It is, however, but fair to note that, long prior (1854) to Barclay, Gairdner held that “the disappearance of urea and uric acid in the urine and their accumulation in the blood” was but symptomatic and not causative of gout, coupling with it the suggestion that there was some antecedent nerve influence at work.
Laycock, too, it may be noted, considered Garrod’s theory inadequate, adding that “Gout is characterised not by urates in the blood but by the genesis of uric acid in the tissues, and its action thereon, and is especially characterised by peculiar changes in the innervation of the individual.”
In 1872 Ord took up the novel standpoint that there was an inborn tendency in the fibroid tissues of gouty subjects to undergo a special type of degeneration, which same might be inherited or acquired. Also that this innate peculiarity was attended by excessive formation of urate of soda in these tissues, and which subsequently gaining entry therefrom into the blood, was deposited promiscuously in the body with a predilection for relatively non-vascular structures, viz., cartilages.
As to the local inflammations typical of gout, Ord’s attitude was somewhat ambiguous. Thus he maintains, “The local inflammations do not necessarily depend upon the deposit of urate and the deposit is not a consequence of inflammation; at the same time, it is probable that excess of urate in the blood produces irritation of tissues.” Neither did he believe that the local inflammatory reactions were of necessity in every instance specific, viz., due invariably to mechanical irritation by uratic deposits, but that they might be initiated by injuries, exposure to cold, etc. Lastly, as to the migration of the disorder from place to place, he believed that for its explanation direct or reflex nervous agencies had to be invoked, for he held the opinion that the local gouty “degeneration and inflammation tend to infect the rest of the system through the blood, and to set up similar actions elsewhere through reflex nervous influence.”
We see, therefore, that for Ord gout, as Ewart observes, was “a mode of decay” or a “disease of degenerations.” “The local tissue degeneracies supply a basis for the uratic deposits and the general degenerative changes multiply the sites exposed to an infiltration from the contaminated blood; whilst reflex mechanisms step in as additional determining agents.”[4]
Reminiscent of Ord’s view is the hypothesis associated with the name of Ebstein. As the outcome of experimental study he arrived at the conclusion that the primary factor in the causation of gout was a disturbance of tissue nutrition culminating in death or necrosis of the damaged textures. The initial nutritional derangement was ascribed by him to the irritant effect of soluble neutral sodium urate. This necrotising agent, following the development of “free acid” during the process of necrosis, was transmuted into the acid urate. Subsequently this same was deposited in crystalline form in the necrosed area. He held these areas of necrosis quite as typical of gout as the uratic deposits, and postulated their combinations to be necessary for the production[26] of a true gouty focus, claiming that he had detected such foci in cartilage, tendons, kidneys, and connective tissue.
Experimentally, Ebstein endeavoured to induce a gouty condition in fowls by ligaturing both ureters, thus thrusting upon the circulation the dammed-up uratic secretion. In other instances he administered to the same animals subcutaneous injections of neutral chromate of potassium, attributing to this substance the power of inhibiting the excretion of uric acid viâ the kidneys through its action on the renal parenchyma. Subsequently, after death he noted the incidence of uratic deposits in joints, muscles, tendon sheaths, and liver, the same being more copious in those animals subjected to chromate injections.
His conclusions were: (1) That necrosing and necrotic processes are developed in various organs as a result of some irritant. (2) That uratic deposits occur in the necrosed area resembling those met with in gouty subjects. (3) That an inflammatory reaction with small cell infiltration ensues in the vicinity of such necrotic areas.
But, in regard to these experimental investigations, they are obviously incomparable to the morbid processes that presumably occur in gout in man. Moreover, as shrewdly pointed out by Levison, experimental ligation of both ureters would certainly engender uræmia rather than anything approximating to gout.
Again, his experiments with urates and uric acid, by which he claims to have demonstrated their action as chemical irritants capable of inducing necroses in tissues, have proved fallacious. This, for the very cogent reasons pointed out by Luff, which run as follows: “Not only is there no proof that the neutral sodium urate upon which he depends for the starting of the gouty changes, ever exists in the human body, but, on the other hand, very strong evidence to show that it never can exist in the human body.”... “The neutral sodium urate is an extremely caustic and unstable compound, and is decomposed in the presence of carbonates, so that it is impossible for it to exist in the blood. The first factor upon which Ebstein relied for his theory for the causation of gout therefore disappears.”
Again, Ebstein’s fundamental proposition that in gout uric acid was produced in many tissues not normally concerned in its production, was ruled out by Horbaczewski’s establishing the fact that in health uric acid is a by-product of the metabolism of almost all tissues. Lastly, the strong toxic properties accredited by him to solutions of the urates was disproved by Pfeiffer’s experiments. This observer showed that urates, in such degrees of concentration as may exist in the human body, are incapable, when injected into the tissues, of inducing necrosis.
In summarising the doctrines of Ord and Ebstein, it may be observed that if the latter’s contentions have been disproved, Ord’s claim that the tissues of gouty subjects exhibit a specific tendency to degeneration has also as yet not been substantiated. Albeit, we must not forget that in 1883 Ralfe subscribed to Ord’s views as to the tendency to textural degenerations in gouty subjects, either through heredity or acquirement. For this observer, however, the basal factor in the production of the disease was a diminished alkalinity of the blood, due to a surcharging of it with acid and acid salts. Disagreeing with Garrod’s assumption that deficient renal elimination was the prime cause of the retention of uric acid, he was of opinion that “the first step in the process lies in the failure of the tissues to reduce the acid, as it occurs in health.”... “In the large glands or where the current of the circulation is free, the uric acid is carried into the blood and gradually reduced to urea; in tissues outside the current of the circulation, the insoluble uric acid is not so readily carried off, and so on the slightest disturbance is deposited, as is the case in cartilages of the joint, the ear, etc.” As to the determining cause of the gouty attack, he invokes the agency of the nervous system to explain its incidence, for he held it probable that the primitive failure of the tissues to reduce uric acid eventually led to derangement of some special nerve centre, which disturbance occasioned the gouty outbreak, with resultant “accumulation of uric acid in the blood and deposition of urate of soda in the tissues.”
In 1895 Berkart propounded a mode of genesis which may be regarded as a variant of Ord’s theory. The severity of the symptoms of acute gout were such as he deemed incompatible with their production as a result of simple mechanical irritation by crystals of biurate of soda. Uric acid, he held, must be afforded a humbler rôle than that of a proximate cause. It was, for him, but an epi-phenomenon, the accompaniment of a panarthritis, the origin of which was as follows:—
While not postulating the identity of rheumatoid arthritis in gout, he yet held that both disorders originated in some obscure form of atrophy of the bone substance, and that the degenerative change also overtook the cartilages and fibrous tissues of the joints. Subsequently, there ensued a necrosis in the tissues in and around the joint. The degeneration and subsequent necrosis, he held, were the outcome of a profound “vice of nutrition.” The pain, inflammatory reaction, œdema, and cuticular desquamation were the direct result, he thought, of the necrosis. The excess of uric acid in the blood he referred to leucocytosis, and in part to disintegration of the tissues.
That some obscure connection obtained between gout and hepatic disorder has been for long an axiom in high favour, with both clinicians and pathologists. This hypothesis found its chief exponents in Murchison and subsequently Latham, and to discussion of their individual views we now proceed. The first named authority held gout to be either merely a result or a variety of what he termed lithæmia. In other words, gout was the outcome of a depraved condition of the blood, due to faulty digestion and functional disturbance of the liver.
Now the conditions that lead to functional derangement of the liver are in the main such as favour the development of gout. Nevertheless, such hepatic disturbances do not inevitably culminate in outbreaks of gout, at any rate of classical type; but, unquestionably, such may eventuate in symptoms currently recognised as distinctive of incomplete gout, e.g., headache, palpitation, cramps, dizziness, sleeplessness, etc. Moreover, if the faulty habits leading to such hepatic derangement be persisted in, they are but too likely to induce outbreaks of frank gout. “Articular gout,” said Murchison, “is so to speak a local accident which, though sometimes determined by an injury, yet may occur at any time in persons in whom the normal process by which albuminous matter becomes disintegrated in the liver into urea is persistently deranged.” Following such hepatic disturbance, the secretion of bile decreased with resultant abnormal metabolism of proteins, and in this way was produced an accumulation of uric acid. This, moreover, according to Murchison, was, especially in the later stages of gout, reinforced by the concurrence of renal inadequacy, which he also postulated as a factor in the production of the disorder.
The tendency to lithæmia Murchison held to be hereditary, and in this was supported by Goodhart, who, discussing its occurrence in young children, was strongly of the opinion that it was due not to dietetic irregularities but to a “constitutional tendency on the part of the individual”; a conclusion, as he thought, strongly supported by the fact that it is more commonly met with in the children or descendants of the “gouty.”
But we have to recollect, as Duckworth observes, that lithæmia, “even when persistent and not due to accidental causes, is not by itself gout.” Moreover, gout is not the only morbid condition in which urates are in excess in the blood, for such obtains, e.g., in leukæmia, pneumonia, anæmia, Bright’s disease, etc. Also, underlying Murchison’s theory is the further unwarrantable assumption, viz., that the “gouty” diathesis is identical with the “uric acid” diathesis.
Now, as we hope to show later, whatever be the proximate cause of gout it is at any rate not uric acid. The fact, too, that higher degrees of lithæmia are to be met with in conditions, not even remotely connected with gout, renders it impossible to accept the view that the excess of urates in the blood is responsible for all the varied symptoms accredited by Murchison and his followers to lithæmia. For the same reason, it is difficult to uphold the hypothesis that “the tendency to lithæmia in early life may be an early expression of the ‘gouty’ diathesis.”
In short, excess of uric acid in the blood or lithæmia is not pathognomonic of gout, much less of “potential” gout. But further discussion of this assumed relationship of lithæmia to gout may well be postponed until, in the light of recent blood analyses, we come to consider more narrowly the contention at one time widely held, that lithæmia is an irregular manifestation of gout.
If we are compelled to adopt a more judicial attitude in regard to lithæmia, what of the similar assumptions as to the relationship of lithuria or lithiasis to gout? Now lithuria, like lithæmia, was and probably still is by some held to be an inherited “gouty” proclivity. Sufferers in youth from lithiasis were deemed likely to develop gout in later years. Not only was lithiasis observed to precede but also to be a concomitant or sequel to gout. Nevertheless, although uric acid, gravel and calculi, sometimes arise in those of “gouty” diathesis, these instances are but isolated, so rare indeed as to entitle them to be regarded as mere coincidences. Moreover, when we recall the fact that the formation of calculi takes place in the urinary passages, i.e., outside the economy, it renders even more improbable the hypothesis that the two morbid phenomena are diverse expressions of the “gouty” diathesis.
As a matter of fact, the large bulk of “gouty” subjects are immune from gravel. Conversely, only a negligible percentage of the victims of gravel develop gout. The geographical distribution of the two disorders is wholly distinct one from the other. The Indian native is a martyr to stone, but notably exempt from gout. Coming nearer home, we find stone relatively common in Scotland, but gout rare. Plowright’s researches, too, revealed no correspondence between the incidence of gout and the prevalence of stone in the several counties of England. In some counties in which the mortality from gout was high that from stone was low, and Norfolk, the one most prolific of stone in England, enjoys comparative immunity from gout.
Reverting now to Latham’s views as to the hepatic origin of gout, we find them very similar to those formulated by Murchison. He held that the defective transmutation of glycocine into urea was[30] responsible for the occurrence of uric acid in the urine. These chemical irregularities were attributed by him to functional disturbance or partial suspension of the normal hepatic metabolism. This, again, was referred back by him to some obscure change in the central system, viz., that part of the medulla oblongata from which the vagus takes origin.
Excess of carbonaceous materials in the blood was considered by Hare to be an essential, though by no means the sole factor in the genesis of gout. This same “hyperpyræmia,” as he terms it, was also, he believed, responsible for migraine, asthma, epilepsy, and other paroxysmal neuroses. For the alternation of attacks of acute articular gout with paroxysms of migraine, asthma, and epilepsy, seemed to him to indicate a kindred origin. The same inference, also, he deemed might be drawn from the well-ascertained fact that the temporary or even permanent cessation of long standing asthma, migraine, and epilepsy, might exactly coincide with the onset of acute gout.
These alternations and substitutions seem to suggest that the preceding alterations in metabolism are similar in nature, finding expression indifferently in gout, asthma, epilepsy, etc. Carbon foods, he considered, are much more likely to accumulate in the blood than the nitrogenous. Ingestion of the latter is swiftly reflected in increased elimination of nitrogenous excreta. On the other hand, following the intake of carbonaceous foodstuffs, no such rapid and proportionate increase in the excretion of carbonic acid ensues. In other words, the capacity of the organism to deal with or katabolise in response to the absorption of excess of carbon foods, is strictly limited. Muscular exercise and exposure to cold, factors which but slightly influence protein katabolism, are largely responsible for adequate carbon katabolism. Accordingly, given deficient exercise, excess of carbonaceous food and a warm temperature, an accumulation of the carbon content of the blood is favoured.
Hare considered that present day habits of warm clothing, warm rooms combined with excessive intake of starch and sugar, are precisely the favourable conditions for producing a state of hyperpyræmia. Increased fat formation would of course tend to diminish such a tendency to carbon accumulation, but this capacity in many subjects is conspicuously lacking, and may already have attained its limit.
Hare contended also that excessive intake of starch and sugar by inducing a state of “glycogenic distension” of the liver, might[31] through compression of the intra-hepatic portal capillaries, lead to congestion of the retro-hepatic portal venous system, and sequentially of the gastric and intestinal mucosa. Through consequent inhibition of digestion and absorption, a condition of hyperpyræmia is induced. This, under varying conditions, may eventuate in acute gout, the coincident pyrexia of which is curative of the underlying hyperpyræmic state, and of all those hyperpyræmic manifestations (irregular or suppressed gout) which so often are the harbingers of an on-coming articular outbreak.
It may be noted en passant that the influence of the nervous system was frequently invoked directly or indirectly in many of the theories already discussed. Stahl, it will be recalled, was the pioneer in this direction, and later Cullen and Henle propounded the view that “the origin of the affection was probably to be found in the central nervous system.” Gairdner, too, by implication, as also Laycock, postulated a neural origin for at any rate some of, the phenomena of gout.
But it was reserved for Edward Liveing (1873) explicitly to advocate the nervous origin of the disease, his reflections on the paroxysmal nature of the attacks, its tendency to periodicity leading him to suspect its kinship with other neuroses.
Those inclining towards the neural conception were later strengthened in their convictions by Charcot’s momentous identification of the nervous origin of certain arthropathies. Accordingly, in 1880, we find Sir Dyce Duckworth advocating the view that gout was “a primary neurosis,” “a functional disorder of a definite tract of the nervous system.”
The gouty neurosis, Duckworth contended, may “be acquired, intensified, and transmitted; also that it may be modified variously and commingled with other neuroses; that it may suffer metamorphic transformations, or be altogether repressed.” Arguing by analogy, Duckworth saw in the paroxysmal attacks, the tendency to periodicity and alternation in the manifestations, evidence of an alliance between gout and the various neuroses.
He further postulated that “this diathetic neurosis determined a disorder of nutrition and led to the perverted relations of uric acid and sodium salts in the economy.” He also held that the localisation of attacks, and the determination of urate of soda to the affected part was also due, in all probability to nervous influence. And the temporary renal incapacity for excretion of uric acid was also attributed by him to the same nerve inhibition.
We see, therefore, from the above, that Duckworth was well[32] justified in describing his view as a combine of the humoral and neural hypotheses. His pathological differentiation between primary or inherited gout and secondary or acquired gout is as follows: In the primary type “the toxæmia is dependent on the gouty neurosis ... and is therefore a secondary manifestation.”
In secondary or acquired gout, “the toxæmia is directly induced by such habits as overload the digestive and excretory organs, and consequently prevents complete secondary disposal of nutritional elements of food; that if, together with such toxæmia, distinctly depressing and exhausting agencies, affecting the nervous system, come into operation, the special neurotic manifestations of the gouty diathesis will occur, and be impressed more or less deeply upon the individual and his offspring.” It is generally conceded that Duckworth’s theory as to the genesis of gout is pre-eminently catholic in conception, because, as Ewart rightly remarks, “it represents the most complete theory published in this country on the general pathology of gout,” and because “the able advocacy of its propounder has given it the support of arguments derived from pathological analogy and from clinical influence which will demand careful examination and searching criticism before they can be either disproved or adopted.”
Albeit, it must be frankly admitted that Duckworth’s perception of gout as a tropho-neurosis of central nervous origin has never gained wide acceptance; this no doubt largely because it was insusceptible of proof. In an endeavour to remove this reproach. Sir Willoughby Wade promulgated the view that the causal change in gout was partly in the central nervous system, partly in the peripheral nerves of the inflamed limb. In other words, he regarded gouty arthritis as the outcome of a local neuritis, this latter being set up in the first instance by the faulty blood state, viz., uricæmia. On the other hand, the central nerve centres might occasion or aggravate the general gouty tendency through their influence over “recognised seats of metabolic activity.” Also the same might, through the medium of the vaso-motor nerves, determine the incidence of local attacks. It will be seen that Wade’s theory is but a variant of that propounded by Duckworth, viz., neuro-humoral.
It will be recalled that as far back as 1889 Duckworth displayed disquietude as to the adequacy of the purely chemical or purely physical view of the pathogeny of gout, as sufficing for an explanation of all its varied phenomena. Thus he writes: “It is incumbent, I believe, to invoke not only a chemical and physical basis for gouty disease, but to include also, in a comprehensive view,[33] the marked determining influence of the nervous factor in the problem.”
Whether we agree or not with Duckworth’s view of gout “as a diathetic neurosis, due to a central neurotic taint, and originating from prolonged toxæmia,” it does, I think, mark the dawn of a reaction from the uric acid theory of its causation. Still, this latter conception continued to dominate the field until seriously called in question by the results of Magnus Levy’s researches. His revelations were, in truth, almost revolutionary, and doubts now accumulated as to the propriety of the terms “uric acid diathesis,” “uric acid intoxications,” “lithæmia,” etc., so long credited as being responsible for not only nearly all the minor ailments flesh is heir to, but especially those relating to joints and muscles, all alike attributable to the presence of excess of uric acid or urates in the blood.
To hasten the process of disillusionment there came from the side of the physiologists the announcement, almost unanimous, that uric acid, though in minimal amounts, is a normal constituent of the blood, organs, and tissues. Thoroughly purged now of their obsession as to the pathological potency of uric acid, there awoke a spirit of inquiring scepticism. On all sides it was felt that the whole problem must be looked at afresh, untrammelled by previous conceptions, no matter how high the sanction. How else, indeed, could the chaff be winnowed from the grain, the illusions born of inaccurate observations be replaced by the substantial form of truth?
Still, it would be ungracious to withhold our due meed of admiration for the masterly manner in which the views of the earlier physicians as to the causation of gout were elaborated, the shrewd and often prophetic inferences, well buttressed by arguments based on clinical and pathological analogies; these the more wonderful when we recall the meagreness of the positive material at their disposal, and that little, alas! how often ambiguous!
In light of latter day views, too, we may well admire the swiftness with which the inadequacy of Garrod’s theory to explain all the protean phenomena of gout was realised. Like Duckworth, they rightly apprehended gout to be “something beyond the resultant effects of aberrant relations of uric acid; that it consists in something more than a perversion of animal chemistry; that it is not to be explained as a mere outcome of gastric or hepatic distemper; and that it is not the appanage only of the middle-aged or elderly high liver, and intemperate drinker, because, as is well known, it affects also sometimes in early life the high thinker and the laborious bread-winner.”
That the uric acid theory should more than any other have found[34] ready acceptance, is not so much to be wondered at. The one solitary pathological fact that emerged out of the mist of hypotheses was that established by Garrod, viz., the excess of uric acid in the blood. It survived and still survives the corroding test of time. Surely such must be the fons et origo mali, and how obtrusive the uratic deposits, so ready to hand, objective affirmations of the truth of their contention.
This apparent simplicity how delusive! yet not wholly unprofitable. For if in these latter days our knowledge of the life-history of uric acid and purin bodies in the organism has evolved from “a state of chaos and guesswork to one of system and scientific accuracy,” the seeds thereof were sown by these hardy pioneers, their, to us crude, researches in the dark regions of bio-chemistry.
Here it would appear opportune to outline our plan of procedure in approaching this abstruse subject—gout. In the coming chapter we shall attempt to define and classify the various types of the disorder before passing on to discuss its etiology and morbid anatomy.
Now all will agree that the more recent revelations of chemical physiology and chemical pathology have an intimate bearing on the problem to be considered. We shall therefore, before proceeding to the more purely clinical aspects of the disease, deal with the modern conceptions of protein and purin metabolism, more especially the latter. Subsequently our scrutiny will be narrowed to consideration of the chemical structure of uric acid, its solubility, sources, mode of formation and destruction. In possession of these facts the relationship of uric acid to gout will be dealt with, in regard to respectively uric acid excretion, uricæmia, and uratosis.
The inadequacy of the uric acid theory of the causation of gout will then be discussed and the possible intrusion of an infective element in its genesis advocated. This accomplished, we shall proceed to the section dealing with the clinical aspects of the disorder, its regular and so-called irregular manifestations. Thence we shall proceed to the diagnosis of gout, while the terminal chapter will be devoted to that all-important subject—the prophylaxis and treatment of the affection.
Said Locke long since, “There are some words which will not be defined,” and surely of these is gout; for reflection upon the proffered definitions thereof is apt to leave one with the depressing impression that the disorder is both “incomprehensible and infinite.”
But have we not by unjustifiable and unwarrantable assumptions deliberately complicated the issue, in recklessly relegating to the gouty category a myriad affections of the intimate nature of which we are as ignorant as we are of gout? Doubtless, this is in part the outcome of a too slavish adherence to tradition, an undue reverence for authority. In all deference, our forefathers were somewhat too hasty in their speculations as to the causation of gout. Dominated by the prevalent philosophy of their days, they strove to interpret the phenomena of gout through its lights, endeavouring to reduce the study of its pathology to philosophical order when the very elements of philosophical order were lacking.
The same is reflected in the earlier, and to a lesser extent in the latter day definitions or descriptions, as some of them more aptly may be designated, notably that put forward by Sir Charles Scudamore.
“A constitutional disease, producing an external local inflammation of a specific kind; the susceptibility to it often depending on hereditary bodily conformation and constitution, but with great frequency wholly acquired; almost never occurring before the age of puberty, not frequently under the age of five-and-twenty, and most commonly between the ages of twenty-five and forty; affecting chiefly the male sex, and particularly persons of capacious chest and plethoric habit; in the first attack invading usually one foot only, and most frequently at the first joint of the great toe; but in its returns, affecting both feet or other situations, as the hands, knees, and elbows; and not only in the articular structure, but also in the other textures belonging to the moving powers, different parts being affected together or in succession; often accompanied with sympathetic inflammatory fever, which is usually marked by nocturnal exacerbations and morning remissions; much disposed to return at periodical intervals, and for the most part preceded by some premonitory symptoms.”
In extenuation of this prolixity, Scudamore observed that, “In an attempt to mark the general characters of gout, I feel the necessity of entering into a description rather in detail, instead of confining myself to[36] a brief definition, because the disease is too complex in its nature to be distinguishable with certainty by a few signs alone.”
Trousseau, in his lectures on gout, refrains, perhaps wisely, from attempting any definitions of the disorder, resting content with the reflection that, “The production in excess of uric acid is a pathological phenomenon, inherent, like all others, in the disease, and, like all the others, it is dominated by a specific cause, which we know only by its effects, and which we term the gouty diathesis.”
Sir William Roberts defines gout “as a constitutional disorder characterised by paroxysmal attacks of inflammation of the joints, associated with the formation of chalk-like concretions in and about the joints.”
Sir William Osler regards gout as “a nutritional disorder, one factor of which is an excessive formation of uric acid, characterised clinically by attacks of acute arthritis, by the gradual deposition of urate of soda in and about the joints, and by the occurrence of irregular constitutional symptoms.”
For myself, I would proffer the following definition, which, of course, the reader must accept provisionally, viz., pending the perusal of subsequent chapters, dealing with the pathology and clinical features of gout, and the inferences drawn therefrom as to the nature of the disease.
Definition.—Gout is an hereditary disorder, the intrinsic element of which is an inborn instability of nuclein metabolism which may remain latent, but under the influence of extrinsic factors, infections, becomes manifest, as betokened by local inflammatory tissue reactions in joints or elsewhere the specific character of which is attested by the associated uratic deposition.
At the present time, under the most liberal interpretation, the word “gout” comprises the following conditions, viz., acute and chronic articular gout, and the so-called ab-articular forms. But it is clear that not only the latter or irregular manifestations, but even the former or regular varieties of the disorder seem destined to undergo considerable pruning.
As to the classical podagra—acute articular gout—no question can arise as to the propriety of its retention in this category. But as to the chronic articular types we are on less certain ground, and to discussion of this vexed question we now proceed.
Let us take, for example, Sir Dyce Duckworth’s classification of the arthritic types of gout. He distinguishes the following forms:—
the latter (2) further subdivided into—
Of these twain the “tophaceous” form need not detain us, and why? Simply and solely this—the uratic deposits stamp the seal of specificity on the disorder. In short, the presence of tophi places the “gouty” origin of the arthritis beyond the pale of cavil.
Now, if we accept, as we must, the fact that uratic deposition is the solitary unequivocal clinical criterion of gout, we are not, I contend, justified in classing any chronic arthritis as “gouty,” the victim of which does not exhibit tophi of articular or ab-articular site, either clinically demonstrable or deducible from skiagraphic revelations.
Nevertheless, be it noted tophi do but bespeak the “gouty diathesis,” not necessarily the “gouty” nature of an associated arthritis. For clearly tophi, of ab-articular location, may coexist with an arthritis of gonococcal or other origin. But given uratic deposits, either in the joint proper or its related structures, all reasonable doubts as to the true “gouty” nature of the arthritis are disposed of. On the other hand, in the absence of tophi, the diagnosis of an arthritis as “gouty” is presumptive, not absolute. This even in acute classical outbreaks in the big toe, viz., pending the finding or subsequent eruption of tophi.
In saying this, I do not for one moment depreciate the diagnostic value of the clue afforded by location of the initial outbreak of the disorder, in the vast majority of instances, in the big toe. It is an invaluable, but not an infallible clue; for, unfortunately, acute arthritic diseases other than gout may elect to announce themselves in the great toe.
Moreover, there is nothing specific in the external characters of acute “gouty” inflammation, nothing in the objective changes which would stamp them on sight as “gouty,” save only their location in the great toe; nothing distinctive about the angry blush, œdema, and engorged veins, all of which may be met with in infective arthritis. There may be, as Garrod with good reason affirms, a local intra-articular deposit of urate of soda, but this lies beyond our ken, presumptive but undemonstrable.
Let but the initial outbreak of gout occur elsewhere than at the big toe, say, e.g., in the wrist, hand, ankle, or knee, and we are at once, diagnostically speaking, en l’air. In this impasse how impotent are we, and how painfully we realise that our diagnosis of acute gout is largely topographical, not etiological! Not, strictly speaking, etiologically diagnosable pending the eruption and detection of tophi. In short, location per se in the big toe is strongly suggestive but not diagnostic of “gout.” (Vide Chapters on Diagnosis.)
If this be done in the green, what then shall be done in the dry?[38] In other words, if so precarious our diagnostic foothold in acute, how much more so in chronic articular gout! for in the latter even topography may wholly fail us, what then our diagnostic criterion?—tophi and tophi alone—aye, and demonstrable at that.
Yet both Charcot and Duckworth would have us recognise not only a tophaceous but a non-tophaceous variety of chronic articular gout, for that is what it amounts to. They apparently feel justified in labelling a chronic arthritis as “gouty” even though tophi “may not exist” or “be invisible”! Deformity, say they, is its hall-mark, not tophi, and its character forsooth, they add, is not only not peculiar to gout, but clinically indistinguishable from the similar defacements met with in arthritis deformans. Nor is Duckworth alone in his contention, for both Ewart and Luff also recognise what they term “chronic deforming gout.”
Tophi, I contend, notwithstanding, are essential for the diagnosis of gout. In their absence, the designation of an arthritis as “gouty” is unjustifiable. Either tophi are, or tophi are not the sole pathognomonic feature of gout. If the latter, then gout ceases to exist as a clinically recognisable entity.
Holding tophi indispensable for the diagnosis of gout, I maintain that Charcot and Duckworth’s plea for the recognition of a chronic type of articular gout, apart from the tophaceous variety, is untenable. Fraught, moreover, with risk, as I am satisfied that their so-called, “deforming” type is largely made up of the atrophic and hypertrophic forms of arthritis deformans.
For myself, as to the classification of the articular types of gout, I would divide them into:
Under the first group I would place not only the acute localised type, but also those acute varieties of polyarticular distribution. As to the second category, I would exclude therefrom, for the reasons cited, the so-called “deforming” varieties of chronic articular gout, recognising only the so-called tophaceous form. But I would place a different interpretation on this term in opposition to that generally accepted; for, by most writers the word tophaceous is apparently limited in its application to examples which, so to speak, exhibit tophi of phenomenal size or number. Scudamore was the chief offender in this respect. As a consequence, he found tophi in only 10 per cent. of his cases of gout. Accordingly, he went so far as to postulate for such victims as did present this peculiarity an idiosyncratic tendency to chalk-stones![39] In other words, he would seem to suggest that there is a gout within gout, that one displays chalk-stones, the other not. By inference, Duckworth and his followers, by differentiating tophaceous gout, tacitly concur, and so “confusion twice confounded” results.
This usage of the term “tophaceous” is unjustifiable and misleading. The significance of tophi is qualitative not quantitative. One tophus bespeaks the “gouty diathesis” as surely as a myriad concretions. Solitary though it be, the same, given elimination of all other sources of arthritis, will suffice to establish the “gouty” nature of an associated joint disorder. It is in this more catholic sense that I would translate the term “tophaceous gout.” The conclusion, then, to my mind, is obvious—there is but one form of articular gout, and one only, viz., an arthritis, the victim of which exhibits uratic deposits in situ or elsewhere in his body. On this and on no other grounds can a chronic arthritis, with any show of certitude, be certified as truly “uratic” or “gouty.”
This rigid attitude may not commend itself to some, but I feel convinced that, only by holding on grimly to the tophus, shall we steer a safe course through all the pitfalls that beset the diagnosis of the chronic arthritides. Only in this way, too, can we preserve for ourselves a clear conception of gouty arthritis as a specific disorder, the which otherwise loses its identity, submerged in a medley of joint diseases. Prior to the differentiation of gout, on the one hand, from rheumatism and arthritis deformans, and on the other from the nerve arthropathies and the infective arthritides, such laxity might be condonable, but not, we think, in the present stage of our knowledge.
In drawing to a close my remarks on the classifications of articular gout, it will be noted that I have made no reference to that variety known as retrocedent gout, but to this I shall allude at a more favourable juncture, viz., in the chapter devoted to the clinical account of articular gout. Conformably, too, it will, I think, be more convenient, to defer any criticisms of the term “irregular gout” to the chapter I purpose devoting to consideration of the varied clinical content of the same.
To the antiquity of gout and no less its distinctive clinical facies, when of classic type, we owe not a little. Its salient phenomena have endured unchanged from the time of Hippocrates onward through the ages. So it is that, even allowing for the enhanced powers of discrimination of latter days, we are in no doubt that the gout of the ancients is the gout of to-day. How signal the advantage thus accruing, when we come to consider the conditions[40] which engender or tend to engender the disease! For, quâ its broad etiological factors, we find ourselves in accord with the physicians of old, our experience a confirmation of their old-time findings.
Our forefathers, like ourselves, realised the innate complexity of the problem, that in the development of the disorder both heredity and environment played a rôle. In other words, that in the genesis of gout not only intrinsic but extrinsic agencies were concerned. Of the intrinsic influences the most important are age, sex, heredity, bodily conformation, and individual peculiarities.
Age.—Gout is slow in evolution, tardy of appearance, confined in the main to the middle and declining years of life. Said Sir Thomas Browne, “Leprosie awakes not sometimes before forty, the gout and stone often later.” Experience but confirms the dictum, for, as Cullen long since observed, it rarely declares itself under the age of five-and-thirty. This relative immunity of youth is not the least striking feature of the disorder; whence the Hippocratic aphorism, “Puer non laborat podagra, ante veneris usum.” Both Sydenham and Heberden were also doubtful of its occurrence before the age of puberty. Gairdner, however, records the incidence of fits of gout even in infants at the breast! and in one death therefrom. Garrod, too, met with two cases of classical type in girls, both of them under ten years of age. But Scudamore states that he never witnessed more than one example of a first attack before twenty, or any after sixty-six.
For myself, I have never seen a case under thirty-five years of age, and am sceptical as to the occurrence of infantile gout of regular type, believing with Scudamore that “the commonly asserted cases which represent the existence of the gout in very early youth are really examples of rheumatism.” Nor am I less but more inclined to cavil at the claims of Comby and others, as to the frequency in children of irregular manifestations. As Osler dryly observes, “The tendency in some families is to call every affection gouty. Even infantile complaints such as scald-head, naso-pharyngeal vegetations, and enuresis, are often regarded, without sufficient grounds, I believe, as evidences of the family ailment.”
To sum up, the majority of cases of gout ensue between thirty-five and fifty years of age. But, given a strong hereditary taint, it may break out in youths and young adults, or haply even in children. But such, in my experience, are phenomenally rare. Indeed, it may be said of gout that only exceptionally is it met with at either extreme of life; though Garrod records several examples in which the initial attack was postponed until nigh eighty years of age;[41] while in one instance, a lady experienced her first classical attack of podagra in her ninety-first year.
Sex.—In the matter of liability to gout the sexes stand in marked contrast, the disorder being infinitely more common in males. Out of eighty cases submitted to the French Academy, seventy-eight were men and only two women; but according to other authorities, this is an under-estimate. Thus in James Lindsay’s series of cases of gout, 84·7 per cent. were males, 15·3 per cent. females, percentages which he notes “are in accordance with the observations of other writers.” J. Lambert, out of 125 examples of gout, noted that 102 were men, i.e., 81·6 per cent., twenty-three women, i.e., 18·4 per cent.
From my own experience, the figures submitted to the French Academy probably represent the ratio of incidence in males as opposed to females. This certainly, if regular, in opposition to “irregular,” types of gout be the criterion; for it must be admitted that regular gout does occur in women, though exceptionally rare either prior or subsequent to the climacteric.
As to the current opinion that the regular manifestations of gout in women are of asthenic as opposed to sthenic character, this has, I think, often proved a source of fallacy. At any rate, in many of these cases the assumed gouty inflammation resolves itself into one of inflamed bunion. Again, in but too many instances, women, showing Heberden’s nodes, are held to have gout or “rheumatic gout.” The latter term, as Pye-Smith observed, “is a bad name for osteoarthritis,” to which category Heberden’s nodes belong.
Judged by the one unequivocal diagnostic criterion, i.e., tophi, gout in women is extremely rare. If to this be added the further fact, viz., the rarity in their sex of classical attacks in the great toe, we see clearly that the diagnosis of gout in women is often a matter of assumption rather than of certitude.
Moreover, having regard to the fact that the diagnosis of gout in women is frequently based on so-called “masked and irregular manifestations,” I must admit that, to my mind, statistics, purporting to indicate the percentage incidence of gout in women and men, are not very convincing.
As to the why and wherefore of the relative immunity of women it may be due to the fact that their habits and mode of life are less calculated to evoke the disorder. There is also the further possibility that the catamenial discharges to a certain extent are protective against gout, for most authorities support Hippocrates’ aphorism, “Mulier podagra non laborat nisi ipsi menstrua defecerint.”
Heredity.—By the ancient physicians gout was held to be[42] hereditary, and even to-day most will agree that “From father to son its seeds are transmitted, and bear fruit in exact proportion to the degree in which circumstances prove favourable to their growth.” Cullen, indeed, went further and held it purely hereditary; but, on the other hand, the belief, that it is often acquired is widely countenanced.
That gout is an hereditary disease is, I think, beyond question, and certainly, of all arthritic disorders, gout furnishes by far the greater number of instances in which parents and children are victimised by the same articular affection. Scudamore in 522 cases found that 332 could trace their disease to the father, mother, grandfather, grandmother, or aunt. But in the remaining 190 no evidence of the existence of gout in their forbears could be elicited. Out of eighty examples submitted to the French Academy an hereditary predisposition was established in thirty-four, and in the residue it appeared to have been acquired. Garrod found that 50 per cent. of his hospital examples of gout were hereditary, and of his private patients nearly 75 per cent. came of gouty stock. Again, Sir William Roberts found that “fully three-fourths of the cases of gout occurring among the easy classes, can be traced back distinctly to a gouty ancestry.” Luff’s estimate is even higher, inasmuch as analysis of a series of 300 examples disclosed a “definite family history of gout in 81·3 per cent.”
Nevertheless, Garrod’s experience, he tells us, convinced him that “in this country gout is frequently acquired even at a moderately early age, for in many most inveterate cases not the least hereditary influence could be discovered.” For myself, I find it difficult to appreciate the attitude of those who, like this observer, postulate innate or static morbid proclivities on the part of the “gouty,” and in the same breath, as it were, are equally insistent that it may be “acquired” de novo. Now, in the taking of family histories positive evidence is more valuable than negative. Surely, therefore, in the light of Garrod’s and Luff’s findings, it is obvious that heredity plays not merely an important, but an essential and indispensable rôle in the genesis of gout. To my mind, accordingly, the balance of evidence is more in favour of the same ancestral taint, though apparently undiscoverable, being present in the remaining 20 or 25 per cent., than that the disease in their instance was wholly and newly acquired.
Personally, I therefore question whether the alleged acquisition de novo of gout is not apparent rather than real. My own opinion is that the innate predisposition thereto is always inherited, and the predisposing factors, that we presume may originate gout, are in reality merely excitants or determining agents. In other words,[43] the remote, the primary or essential cause of gout, is an inborn morbid tissue potentiality, and in the absence of this intrinsic warp the various contributory or exciting causes are impotent to evoke the disorder.
Apart from statistical proof of heredity, how else, save on the basis of an organic predisposition to the disease, can we explain the fact that of a large number of individuals, of slothful habit, and given to alcoholic and dietetic excesses, not one may get gout; while others who lead literally “a godly, sober, and righteous life,” become martyrs thereto. How escape then the conviction that in gout “breed is stronger than pasture”? for, apart from gluttony and indolence, gout is much more prone to arise in persons in whose pedigree it can be traced than in others.
It is not gout, but the predisposition thereto, that is inherited. This proclivity, moreover, may descend to the children of those who, in their own persons, have never suffered from the disease. In Luff’s series it was so in 27 per cent. of the cases, i.e., the disease was transmitted from grandparents to grandchildren without the fathers or mothers suffering from “active gout.” In other words, the morbid potentiality may lie latent until evoked. Thus, the females of “gouty” families, infinitely more often than not, escape overt gout, but hand on nevertheless their inborn liability thereto to their offspring. Looked at in this light, I see no difficulty in accepting the fact that gout may skip a generation. The son of a gouty parent, happily warned by the excesses of his father, may remain immune, while in turn his son, forgetful of his evil heritage, may bring it again to fruition.
The more one reflects on the essential cause of gout, the more inevitable seems the conclusion that gouty individuals, as Walker-Hall contends, “possess some inborn defect or alteration of nuclein metabolism.” And the vague phrases “constitutional” or “nutritional,” as applied by older writers to the disorder, are only explicable on the basis of inherited structural peculiarities, with their correlated perversions of tissue function.
That such constitute the pathological groundwork of gout, is, I think, further indicated by the fact that “gouty” inflammation, in virtue of its associated uratic deposition, is sui generis. No tissues, other than the gouty, react in this specific fashion. Does not this seem to indicate that the inborn tissue peculiarities dictate, so to speak, the character of the pathological reaction; this indifferently, whatever the nature of the so-called predisposing causes which, if our assumption be correct, are merely provocative of gout, in other words, do but evoke or make manifest what is already latent.
To sum up, on statistical, and more cogently, general clinical and pathological grounds, my own conclusions are that—
(1) Gout is always an hereditary disease.
(2) The factors currently regarded as predisposing agencies are in reality merely determining agents, not the cause of gout, but the occasion of its appearance.
(3) In the absence of an hereditary taint, these same are powerless to evoke the specific manifestations of true “gouty” inflammation as estimated by associated uratic deposition.
Bodily Conformation and Individual Temperament.—Of the hereditary character of gout no doubt remains, but as to the influence of physical build and temperament no such certainty prevails. Said Cullen, “Gout attacks especially men of robust and large bodies, men of large heads, of full and corpulent habit, and men whose skins are covered with a thicker rete mucosum, which gives a coarser surface.” Doubtless, in its more sthenic form, gout affects persons like Falstaff, of sanguine temperament and corpulent habit. But its milder or more asthenic manifestations occur often in men like Cassius, of lean and nervous type.[5]
Of objective stigmata, I know of none, save tophi, that can be[45] truly regarded as pathognomonic of the outward semblance of the “gouty.” The skin of the face may be coarse, unctuous, and studded with ramifying venules. Such appearances, though not always, betray the tippler. Indeed, such stigmata as these are only of value as indicating the habits of the individual, favourable or not, to the development of gout.
Again, it has become a tradition with us that gout produces characteristic teeth. The mere fact that they are “ground down” so as to display the dentine in section is held as evidence of a “gouty” diathesis, or of lithæmia. The teeth of the gouty, it is true, often appear long and square-topped; but the gouty, no more than others, are immune from early recession of the gums. Again, we must recollect that there are several causes which may lead to the teeth being worn down more quickly than normally. Thus the formation of the jaw may be such that the upper and lower incisors meet edge to edge instead of overlapping. This so-called “edge to edge bite” subjects the incisors to marked attrition. Also we must recall that these effects may be aggravated by the nature of the diet. All of us are familiar with the fact that in old horses the teeth are ground down to the gums. The same also is observed in races condemned to live on coarsely prepared flour and hard vegetable food.
In conclusion, having regard to the marked frequency with which disorders leading to early recession of the gums are met with in the “gouty,” and the ease with which the early attrition of the teeth is explicable on tangible mechanical reasons, I am inclined to refer such changes to their combined agency, rather than to the nebulous “gouty” diathesis.
Again, despite Duckworth’s assertion that “the gouty throat is like no other,” I am convinced that it presents no specific appearances. Nor have I been able to satisfy myself that striated and fluted nails of, it is usually affirmed, exceptionally brittle nature, are distinctive of gout any more than the premature whitening of the hair so frequently accredited to the subjects of this diathesis.
One point, however, I would emphasise is, the frequency with which potentially gouty persons suffer from local syncopes and asphyxias of the hands. They are precisely similar to those met with in rheumatoid or atrophic arthritis, certain cases of which, as we shall see later, have another affinity with gout, viz., retardation in the output of exogenous purin.
Locality, Race, Climate, etc.—As to the geographical distribution of gout, the salient fact would appear to be the almost complete restriction of the disorder to the temperate zone. Among the natives of Africa gout, according to Livingstone, is unknown.[46] Neither apparently is it to be met with in Turkey, China, Japan, Peru, and the Brazils. The indigenous peoples of India, and the East Indian Archipelago, also seem exempt, though the immunity does not extend to Europeans resident in these tropical climes.
It is significant that Duckworth, inquiring of practitioners from foreign parts as to their experience of gout, found that little or none was forthcoming “save where Europeans have formed part of the community.” This statement, to my mind, does but add cogency to my contention that gout is always hereditary.
If we restrict our purview to the British Isles and the Continent, we find that as a nation we have achieved the unenviable distinction of being facile princeps in point of the liability to and incidence of gout. The bulk of examples, too, are met with in England, the disorder being much less frequent in Scotland and Ireland. Moreover, in the two latter countries, the disorder is practically restricted to the upper classes. By contrast, in England it has extended to the lower orders also, in respect of which peculiarity we stand unique as compared with all other countries.
Reverting to the Continent, gout appears to be more common in France than in Germany, Austria, and Italy. Indeed, it is said to be endemic in Normandy, Burgundy, and the Rhone Valleys. In Holland, according to Duckworth, there is practically no gout, and the same is true of Russia, save in Petrograd and the Baltic Provinces.
In Belgium, also, gout is not common, and in Greece it is much less prevalent than in France or England.
In regard to the incidence of gout, its greater prevalence in temperate as opposed to tropical climes, and the disparities between different countries, it would be unsafe to assume that the variations are the outcome solely of climate. Thus the immunity of, e.g., strict Mohammedans is attributable in part to their sobriety and the less highly nitrogenous character of their food. But, if seduced into the ways of the “infidel,” their exemption, it is said, ceases. Europeans, of “gouty” heritage, may, if temperate, escape gout when resident in the tropics, otherwise they fall victims thereto just as surely as at home.
Gout, indeed, is more a matter of morals than climate. In the palmy days of the Roman Empire, when luxury and indolence were rampant, gout flourished, but declined following the installation of a republican form of government. In like fashion and for similar reasons, the inhabitants of modern Greece suffer infinitely less from the ravages of gout than of yore. In short, the climate of Italy and Greece has presumably endured unchanged, but the “habits” of their peoples have altered.
Formerly it was held that the incidence of gout in any country[47] or district varied according as to whether the population drank wine and malt liquors, or distilled spirits. Where the taste for the latter predominated, the disease was relatively rare, whence the comparative immunity of Scotland, Russia, Poland, and Denmark. But what of the rarity of gout in the wine-producing country Spain? Nor for that matter have I ever seen it claimed that gout was especially prevalent in Portugal, the home of “port,” that bête noir of the “gouty.” In truth, dogmatism is here out of place, for though overeating and overdrinking are undeniably important factors in eliciting gout, they are not the sole factors.
In reviewing the statements made as to the geographical distribution and the race incidence of gout it is but too manifest that they are largely provisional; indeed, such information as we do possess as to its relative frequency in various countries, must be taken cum grano salis. Thus, who can doubt that the various affirmations must have been very largely influenced by the “personal equation,” that what one authority would define as gout would by another be deemed inadmissible to this category. Moreover, many of the original statements were made at a time when the differentiation of arthritic disorders, as we now know it, was but in its infancy. For obvious reasons, therefore, no researches in this sphere can ever be satisfactory, until the opinion of the profession at home and abroad be crystallised into some definite pronouncement, some precise definition, of the exact criteria by which the diagnosis of gout stands or falls.
In justification of these strictures, may I cite some opinions as to the frequency of gout in the United States. In 1890, Sir Dyce Duckworth affirmed that in America gout was “practically unknown.” But a few years later, we find Sir William Osier convinced that gout was often unrecognised in the United States. More pertinent still, only twenty years after Duckworth’s affirmation, Luff quoted the statistics of the Johns Hopkins Hospital, Baltimore, from which it appeared that during a period of fourteen years 0·26 per cent. of the total admissions thereto were examples of gout. This he contrasts with the number of cases of gout admitted to St. Bartholomew’s Hospital, London, during a similar period. Mirabile dictu, the percentage was only 0·37, but a third more than that of the Johns Hopkins Hospital!
Yet again, J. H. Pratt, of Boston, writing in 1916, observes “the greatest confusion exists in the minds of many practitioners in America to-day regarding this disease (gout) and its diagnosis. In some parts of the country the diagnosis is frequently made in conditions that are not gout; in other sections there seems to be a skepticism in the minds of many practitioners regarding the[48] existence of such a disease. In New England I have found that chronic gout, even when tophi occur, is often mistaken for rheumatism or arthritis deformans. Some physicians of large experience assert that they see gout frequently. Enquiry has shown that they mistake typical cases of arthritis deformans for gout, and the swellings about the joints and even Heberden’s nodes for ‘gouty’ deposits.”
Can it for one moment be denied that even to ourselves, living in England, the so-called “home of gout,” these trenchant criticisms are but too applicable. So long, then, as such confusion exists as to what does and what does not constitute gout, how can we, with any show of scientific precision, presume to discuss, much less lay down, dogmatic statements as to the geographical distribution and the race incidence of gout?
Food, Drink, and Occupation.—Gout, it has been well said, is the “Nemesis of high living,” for, unquestionably overeating is most fertile in evoking any latent tendency thereto. Attempts to throw all the blame on particular foodstuffs, e.g., red meats, etc., on the ground that these highly nitrogenous substances engender excessive formation of uric acid, have failed of their object. Even the much-maligned “purin bodies” have of late been largely absolved of blame, and the virtues of a “purin-free” diet, e.g., milk, are probably referable to the intestinal asepsis that such a regimen promotes.
My experience, like that of others, is, that it is not the quality, but the quantity of the food that is responsible. Moreover, I believe that the toxicity of the blood plasma thus produced exerts its evil effects indirectly, viz., by lowering the vis resistantiæ of the individual to microbic invasion. Nor have I any doubt that it is this same but too common tendency to gluttony on the part of the “gouty” which is in part responsible for the cardio-vascular, hepatic, and renal changes so frequently associated with gout in its later stages.
Reverting to alcohol, there are many who regard it as par excellence the predisposing cause of gout, and some even question whether gout would have evolved had alcohol been unknown to mankind. But the interesting point is, that all forms of alcohol are not equally pernicious in this respect, and the difference in their potency in this direction is apparently little or at all referable to their percentage content of alcohol. Port, madeira, sherry, burgundy, strong ales, and stout are far more provocative of gout than distilled spirits. In England, where gout is prevalent, malt liquors are the common drink, whereas in Scotland, where the predilection is for whisky, the disorder is much more rare, and the same applies to Ireland. In the Burgundian province of[49] France gout is common, but exceptional in the Rhenish district of Germany, where hock is largely consumed. The why and the wherefore of these vagaries is not as yet explicable; but of those forms of alcohol, most conducive to gout, neither their acidity, sugar content, etc., can be impeached as imparting to the alcohol its predisposing influence in this direction. Incidentally, to those who advocate the primary renal origin of gout, one would propound the question, why is it that distilled spirits are less provocative of gout than wines, seeing these particular liquors are so fruitful of granular kidney?
Again, if alcohol be such a potent factor in gout, why is it so rarely met with in habitual drunkards, and how account for the comparative rarity in gouty subjects of hepatic cirrhosis, or for that matter of other disorders of alcoholic origin? Beset by these eccentricities of behaviour, Sir William Roberts was tempted to regard gout as “rather an incident of the legitimate dietetic use of alcoholic beverages.”
The relationship of alcohol to gout is as erratic as it is to atrophic cirrhosis. Thus an individual may drink hard through life, and escape cirrhosis; another luckless wight, though he be quite temperate, yet falls a prey thereto; still another, who may never have tasted alcohol, acquires cirrhosis; lastly, cirrhosis is occasionally met with in the lower animals, into whose diet alcohol does not enter.
In like fashion, an habitually intemperate man may pass through life without incurring gout. Another, handicapped by his heritage, though he be strictly abstemious, yet falls a prey thereto. Even a total abstainer, when coming of gouty stock, may develop gout, haply through overeating.
To my mind, the only supposition deducible from these facts is that some individuals are born with a tendency to gout, and that this tendency may never assert itself as actual disease; that in others the dormant proclivity, under the influence of alcohol, forthwith becomes manifest; lastly, in some again, so nicely poised is the equilibrium of their nuclein metabolism, that the most venial alcoholic indulgence suffices to evoke an outbreak.
I incline, therefore, to the view that alcohol per se is not a cause of gout; in other words, alcohol will not, in the absence of a gouty heredity, produce gout. On the other hand, given an innate proclivity thereto, alcohol, especially certain forms of it, will almost infallibly evoke the disease; this often though the subject be conspicuously moderate in its use.
That alcohol will produce the disorder even more swiftly and surely if reinforced by overeating also, cannot, I think, be gainsaid. As to the modus operandi of alcohol in inducing gout, I believe that[50] it acts indirectly, viz., by slowly sapping the protective mechanisms of the body, and so paving the way to infections.
Much stress has been laid on the fact that certain occupations conduce to gout; but, if we exclude plumbers, painters, or other workers in lead, no other callings in life can be held to entail a specific predisposition to its development, save in so far as they promote overeating, overdrinking, and inactivity.
It is well established that workers in lead are specially prone to develop gout. I take pride in noting that two of my predecessors at the Royal Mineral Water Hospital, Bath, William Falconer (1772) and Caleb Hillier Parry (1807), drew attention to the frequent occurrence of gout in those exposed to the action of lead; nevertheless the major part of our knowledge of lead as a predisposing cause of gout we owe to Sir Alfred Garrod (1854). This authority noted that at least one out of every four gouty patients that had come under his care at King’s College Hospital had at some time in their lives been the subjects of plumbism, and for the most part were plumbers or painters. Out of 136 undoubted examples of gout, Sir Dyce Duckworth noted that of these twenty-five males showed signs of lead poisoning, and were either plumbers, painters, compositors, or workers in lead mills. My colleague, James Lindsay, out of a total of 482 instances of males afflicted with gout, found that 108, or 22·4 per cent., were workers in lead.
In light of these findings the question naturally arose as to whether lead impregnation per se could produce gout. It was then elicited that the association of lead with gout was noticeably less frequent in Scotland and in the North of England than in London. On this interesting point Dr. T. Oliver observes, “We do not see in the north that intimate relationship between gout and saturnine poisoning. Workmen from the south develop it in the North of England. The natives of the north, though equally exposed, seldom become gouty even when the kidneys are affected.” Again, Osler tells us that in America lead-gout is comparatively rare, though chronic lead poisoning is frequently met with in that country in association with arterio-sclerosis and contracted kidneys. Again, Frerichs, out of 163 cases of plumbism in the Berlin Hospital, found not a single case of true gout.
Some remarkable instances illustrating the influence even of medicinal doses of lead in determining outbreaks of gout are on record. In a man aged 25-30, suffering from chronic diarrhœa, Sir Lauder Brunton prescribed lead and opium pills. In less than ten days he returned with gout in one of his joints, though he had never previously suffered from an attack. My colleague, Dr. Munro, tells me of an even more striking case. A lady under his[51] care had used a hair wash, for many years, with apparently no ill effects. She recommended a friend of hers to try the same lotion, and within a few days she developed acute arthritic gout, though she had never previously experienced the disorder. Analysing the preparation, Dr. Munro found the clue in the contained lead.
As to proffered explanations of lead-gout some have sought it in the production by this poison of arterio-sclerosis and chronic nephritis. But this is scarcely satisfying when we contrast the frequency of chronic plumbism and associated arterio-sclerosis and contracted kidneys with the relative rarity of lead gout.
The balance of evidence would appear to be in favour of the view that lead per se cannot produce gout. For the incidence of lead-gout is scarcely appreciable, save in a population amongst whom from other causes gout is prevalent. In short, lead in the absence of an hereditary bias, is impotent to evoke gout.
As to its modus operandi, I think it exerts its effect through derangement of the intestinal secretions, and so favours the migration inwards into the system of pathogenic bacteria.
As for occupations other than those concerned with lead, it is certainly notorious that gout is extremely frequent in those that are rich in opportunities for overeating, overdrinking, and sluggish habits. This point has never been more clearly illustrated than by James Lindsay, whose analysis I take the liberty of transcribing.
Thus, out of 482 males the victims of gout, eighty-one were cabmen, coachmen, grooms, stablemen, and bus drivers; fifty-one were draymen, publicans, barmen, cellarmen, potmen, innkeepers, maltsters, coopers, storekeepers, brewers’ travellers, and brewers’ labourers; twenty-five butlers, men servants, ship’s stewards, and hotel servants; while forty-five were labourers, and of the residue, although all kinds of trades and occupations were represented, yet no other class reached ten in number.
Of these various stations and occupations, it cannot be held that, in themselves, these callings necessarily contain the “seeds of the gout.” The banefulness resides in the associated habits of living; for but too frequently repletion, intemperance, and indolence go hand in hand with these vocations. In other words, dietetic excesses, overloaded intestines, and too much alcohol, what more likely to impair the digestive functions, to increase the toxicity of the intestinal flora, and in turn to upset the equilibrium of general nuclein metabolism, with its associated specific local reaction in certain tissues?
Mental and Physical Over-exertion, etc.—Sydenham said of gout that it destroys “more wise men than fools,” and in a letter to Dr. Short, he complains, “I send you a short tract upon Gout and[52] Dropsy instead of the thicker volume, which in my own mind I had determined on, viz., a history of such chronic diseases as my practice has most especially met with. By applying my mind, however, to its utmost, and by bringing all my powers of thought on the subject, I brought on a fit of gout, such as I had never before suffered from; so that the fact itself warned me to lay aside, even against my own will, such lucubrations, and to take care of myself; well satisfied with having, in some measure, dealt with these two diseases. Whenever I returned to my studies, gout returned to me.”
It is doubtful if, in the absence of an hereditary proclivity, intellectual strain would promote the development of gout. On the other hand, there is, I think, no doubt that immoderate mental exertion will indirectly precipitate an outbreak. I can well understand that the illustrious Sydenham, absorbed in his life study, forgot to take a normal amount of exercise. Perhaps, like the renowned Jenner, he would have said, “I never walk at all except from my house into my carriage. I hate walking, and if I could, I would get my servants to carry me to bed.” Nevertheless, I doubt not that Sydenham’s intellectual efforts necessarily entailed sedentary habits, which brought in their wake digestive and intestinal derangements, whence his occasional gouty outbreaks.
Gout, indeed, has taken its full toll of the “Intellectuals.” Thus Scudamore tells us that “The late Mr. Pitt and his father had gout at a very early period of life. The father was never a votary of Bacchus, and neither of Venus (as we are told), but both were ardent students.” Probably, in many instances, however, the evils of immoderate study are reinforced by more reprehensible excesses. The ancients insisted on sexual debauchery as favouring outbreaks of gout. Whence the Latin verse:
Doubtless, in some instances of this supposed origin, a gonococcal arthritis was confused with gout. Doubtless sexual neurasthenia with diatetic excess favours the onset of gout. In the same way grief, anxiety, and other depressing emotions are provocative of gout in that they impair the digestive functions, lead to hepatic torpor, and sluggish bowels.
In conclusion, we have now dealt with those factors currently regarded as predisposing causes of gout. Personally, as I have before said, the differentiation of the foregoing from the so-called[53] exciting causes of gout is purely arbitrary. Thus even those who countenance such division are forced to admit that many of the predisposing causes will, “if at any time suddenly increased,” immediately excite a fit of gout.
In other words, the difference is quantitative rather than qualitative. Thus, a moderate drinker, if perchance he exceed his usual limits, pays the penalty by an outbreak. Another habitually addicted to the fleshpots eclipses himself, and a similar retribution is exacted. Or, he exposes himself to a chill, with subsequent gastro-intestinal or hepatic functional derangement. Yet again, the cessation of wonted exercise, and more often the taking of it when unaccustomed, may determine the onset of a paroxysm.
But far more arresting are the numerous and well authenticated instances in which local trauma not only determines an outbreak but also its locality. How frequently, too, have blows, strains, sprains, fractures, dislocations, or other trivial or severe injuries, been the signal for an attack. Now, as we hope to show later, local foci of infection are extremely common in the gouty. Such are especially frequent in the teeth, tonsils, naso-pharynx, etc. Is it not then extremely probable that organisms may, viâ the blood-stream, find their way to a joint, the resistance of whose tissues has been lowered by a trauma, however slight its degree? This I apprehend to be the true explanation of the undoubted intimate connection between traumatisms and arthritic outbreaks of gout.
Of similar significance, too, the numerous instances on record in which acute attacks of gout have followed acute tonsillitis, acute pharyngitis, acute parotitis, etc. How frequently, also, competent observers, such as Garrod, noted that boils and carbuncles frequently appeared to be excitant of acute attacks. But to this important point, the intrusion of an infective element in the genesis of gout, we shall return in a later chapter entitled “Gout as an Infection.” It will suffice here if we record our belief that—
(1) Heredity is the sole predisposing factor in gout.
(2) That the differentiation between the usually cited predisposing and exciting causes is unwarrantable.
(3) That both alike are merely determinants.
(4) That their influence as such in exciting outbreaks is exerted through the medium of infection, this achieved either directly or indirectly.
It has been truthfully affirmed that we know more of the results or products of gout, and less of its essential nature, than of almost any other disease. Thus the post-mortem history of the disorder is concerned almost exclusively with more or less graphic[54] accounts of the uratic deposits, their sites of predilection, and the changes that they induce. Hence it is that the morbid anatomy of gout relates for the most part to its regular or articular manifestations, for it is in and around the joint structures that the deposits for the main part occur.
As to the assumed localisations of the disease in the internal organs, there is no anatomical evidence that they are due to an invasion of the “gouty” inflammation. Not even the renal changes, despite the attestation, as it were, of the gouty process by uratic deposits in the papillæ, can be held as distinctive of gout. Norman Moore found them present in only twelve out of eighty cases. As Osler said, “The presence of uratic concretions at the apices of the pyramids is not a positive indication of gout. They are not infrequent in this country [U.S.], in which gout is rare.... It is not possible to say in a given case that the condition has been due to gout unless marked evidence of the disease co-exists.”
If, then, nothing distinctive can be claimed of the renal, how much less can we construe as “gouty” the anatomical alterations that may or may not be met with in other organs in this disorder. In short, it may be said of the renal as well as the other visceral lesions, so often met with in association with gout, that they are met with even more frequently in its absence, and most certainly fail to attest their “gouty” nature by the appearances which they present.
The only morbid structural changes, therefore, that can legitimately be defined as specific of gout relate to its regular or articular lesions. As to the anatomical alterations in the articulations, their specificity depends essentially on the uratic deposits, rather than upon the associated inflammatory and degenerative processes.
Given death during an acute paroxysm, examination reveals the usual tokens of inflammation, hyperæmia, effusion, and swelling of the ligamentous tissues. The synovial lining is injected and spongy, while the exuded fluid is thick, scanty and turbid, containing polymorphonuclear leucocytes as well as crystalline deposits. Charged therewith, not only is the synovia thick, but of a milky appearance. Examined microscopically, it is found to contain the acicular crystals of sodium biurate. The synovia has occasionally been found covered with blood, but no pus formation has ever been known to occur in uncomplicated acute gouty arthritis. The reaction of the synovial fluid is generally neutral or alkaline, but exceptionally Garrod found it acid.
Uratic deposit has a predilection for cartilage, and in some instances is strictly confined thereto; but in the more chronic forms it permeates all the component elements of the articulation. In the synovial membrane and fringes deposition takes place in[55] the subepithelial and subserous layers. It invades also the ligaments, the tendons, and even the periarticular fibrous tissues become impregnated with biurate. Moreover, like the synovial sheaths of the tendons, the neighbouring bursæ are specially prone to deposits, which again encroaching upon the subcutaneous connective tissues, infiltrate the skin itself, forming chalk stones or tophi.
Inspected after death, the articular cartilages are seemingly overlaid with a white mortar or chalk-like material, i.e., sodium biurate. Their surfaces, however, though defaced by stains, streaks, or dull patches, nevertheless, at any rate at first, retain their pristine smoothness. This because closer scrutiny reveals that the deposit is not in reality upon the surface of the cartilage, but is located interstitially in its substance.
Microscopic examination of a vertical section, taken at the site of the deposit, shows clearly that it is composed of felted masses of acicular crystals. Lying in the matrix of the cartilage, they are more densely packed just below its free surface. The crystals do not penetrate further than one-third or one-half of the depth of the cartilage. Becoming more and more sparse towards the deeper layers, those near the bone are entirely free from deposit. This clearly indicates that the uratic matter originated from the synovial fluid bathing the articular ends and was precipitated therefrom.
As to the primary site of the deposition, it usually takes place at the centre of the articular cartilage. Opinions differ as to whether the cartilage cells are foci of deposition. Garrod thought so, but Duckworth found no relationship between it and any histological elements, while others locate it in the matrix.
While, as before stated, the cartilage at first retains its smoothness, later it becomes pitted in patches. Ultimately the cartilage, through atrophic changes and erosions, may disappear, the joint cavity becomes filled with a plaster-like material, and the joint structures undergo more or less disorganisation. Pari passu with the central atrophy of the cartilage, hypertrophic outgrowths form at its free margin. In late stages the bones, too, undergo changes; their outer layers become more dense through proliferative osteitis, while their spongy tissue becomes rarefied, and the cells of the marrow fatty. Duckworth held that uratic deposits might occur primarily in the bone without any similar implication of the related cartilage. On the other hand, Garrod dissented, claiming that when the bone was involved, it was only secondarily to uratic deposition in the cartilage, of which indeed it was but an extension.
In reviewing the foregoing findings, it must be admitted that[56] morbid anatomy fails to shed light on the essential cause of gout. This, at any rate, is true of the older studies with which, up to the present, we have been engaged. Still, as Berkart’s more recent researches show, our knowledge of even the morbid anatomy of gout is as yet but in its infancy.
Histological examination of the articular ends adjacent to gouty joints reveals the presence of certain cystic changes in the diaphyses. Thereupon Berkart propounded an hypothesis, explanatory of the acute phenomena of a paroxysm of gout. His view was that these cysts in the bone, at first minute, gradually enlarge. Ultimately, through concomitant thinning of the surface bone, there comes a day when the cyst bursts into the joint, its content voided into the cavity thereof.
An interesting point noted by Berkart was that in many cases of “acute” gout the articular cartilage was found apparently normal and devoid of uratic deposits, and this although the attack had been sufficiently severe. This would appear to contravene Garrod’s dictum that “gouty inflammation is invariably attended with deposition of urate of soda.” The same inference was drawn from a case of Sir Dyce Duckworth’s. The subject had had two attacks of gout in the right great toe joint. Yet at the autopsy neither toe joint contained a speck of uratic deposit. Nevertheless, this does not prove that uratic deposition had not ensued during the gouty attacks. All it can be held to prove is, that such deposits are not always permanent, and that, under certain conditions, they may undergo resolution. That this is so is almost certain, seeing that tophi in the ear have been seen to come and go, and equally certainly, after an acute attack, tophi in the neighbourhood of a joint may lessen even though fresh ones form coincidently at another site.
Albeit, the importance of Berkart’s hypothesis and histological findings resides in the fact that they suggest strongly that a pathological process, more vital and biological than the mechanical uric acid theory, is at the root of the clinical phenomena of a gouty paroxysm. It does not put out of court Garrod’s assumption that uric acid is an invariable accompaniment of acute gouty inflammation, but it militates strongly against his contention that uric acid deposition is the cause of acute gouty inflammation. It indicates the reverse, viz., that the uratic deposition is the consequence of a more vital underlying morbid process.
Let us revert now more in detail to Berkart’s findings. The bones adjacent to gouty joints were fully prepared for microscopic examination. Investigation of the first metatarsals, and in some instances of the phalanges also, revealed the presence of cystoid degeneration. Its starting point is in the epiphyses. Thence[57] it extends to the articular cartilage, through which it bores at one or more points. The contents of the cyst then find their way into the joint through the fistulous openings in the cartilage, with a resultant acute “perforative synovitis.”
The cysts, at first minute, may be either single or multiple. Small in size, they are easily concealed by the fat marrow, unless the bone is properly prepared for microscopic examination. The isolated cysts eventually coalesce, and so lead to considerable excavation.
As to the contents of the cysts little is known, as, save through accidents or surgical operations, they are rarely available for examination. When of relatively recent origin they apparently consist of a coagulable substance which later on become serous or hæmorrhagic. So long as the fistulæ thus formed in the cartilage remain pervious, a direct way into the articular cavity is provided, and through this, if of sufficient calibre, the necrotic matter periodically gains entry into the joint, with ensuing periodic outbreaks of acute synovitis. In other instances in which the cysts are located in proximity to, or within, the diaphysis they may fail to extend to the cartilage, and no perforation ensues. In this event, through accumulation of its contents, the cyst enlarges, and the bone is gradually expanded through pressure.
Berkart holds that the histological changes in the affected epiphyses indicate that the cystoid degeneration is the outcome of an anomaly of the vascular and osseous structures. The degenerative area contains an abundance of dilated and thin-walled veins, evidence of a condition of chronic congestion. In consequence thereof, the trabeculæ undergo decalcification, and the adjacent fat marrow becomes fibrous. The areas of fibrosis thus formed, owing to thrombosis of the related veins, become softened and transmuted into cysts.
Now, as we all know, some persons, after indulging in wine, almost immediately experience sharp twinges in the small bones of their hands or feet. Garrod attached diagnostic importance to such swift response as a sign of gout. These pains he attributed to uric acid deposition. In contrast, Berkart attributes the twinges to atony and consequent over-distension of the related vessels, which lack the normal support afforded by the osseous trabeculæ.
As far as we are aware, these findings of Berkart’s are as yet unconfirmed. Nevertheless they provide us with a much more probable explanation of the phenomena of acute gout than the older uric acid theory, which, not to mention the many other obstacles to its acceptance, has always laboured under the aspersion of being too “mechanical” in conception.
Moreover, his studies clearly indicate that not only the intra-articular surfaces but the adjacent bone-ends and marrow must, as the somewhat rare opportunities present themselves, be exhaustively investigated. For myself, I cannot believe that so passive an agent as an “anomaly of the vascular and osseous systems” is the fons et origo mali in gout. Some more vital element must, I feel convinced, intrude, and I incline to think an infection. Berkart himself brings forth evidence in favour of this contention, inasmuch as he noted the frequent co-existence of lymphangitis, so pronounced that the whole of the affected leg became the seat of a leuco-phlegmatic œdema.
Not only is the proximate cause of gout unknown, but the essential nature of the disease is still shrouded in obscurity; for the obliquity in trend of protein metabolism, manifested though it be by striking phenomena, is clearly only the outcome of some, as yet undetermined, derangement in the mechanism of intermediary metabolic or bio-chemical change.
This is, of course, but to restate the problem we are confronted with. Wholly to solve the enigma would postulate ability on our part to trace ingested foodstuffs through all their vicissitudes from the moment of entry into the blood or lymph-stream till flung out as effete matter through the various avenues of excretion; but, unhappily, we know the story only in part, its beginning and end, but not what lies between.
We know much of the complex changes that take place in food prior to absorption, and of the modus operandi of the latter not a little. Comparably, too, we can gauge the quality and quantity of end-products, the chemical outcasts, as they escape in the urine, sweat or breath, and largely how achieved; but of the intermediate steps between absorption and excretion we catch but a glimpse here and there. The sequestered path by which the inanimate molecules of food uprise to Life, and anon go down to decay and death, are still hidden.
In other words, little do we know of the relationship of labile, or food-protein, to tissue protein. True, the coarse fact of abnormal protein loss in renal disease may be revealed in the urine, as likewise the waste of albumoses in myeloma, etc., and the incidence of amino-acids in disease of the liver. Similarly, the appearance of cystin or of alkapton in the urine bespeaks flaws in protein metabolism, failures in the normal disruption of amino-acids. All these are of the grosser anomalies of protein metabolism, but more subtle those of gout!
Complex, in truth, the problem here presented, than which none more subtle exists in the realm of bio-chemistry. True, quantitative variations in the content of the urine as to urea, uric acid, etc., undoubtedly bear a direct relation to protein metabolism, but they give us little, if any, substantial clue as to the particular[60] metabolic warp responsible. We see this particularly in regard to uric acid, so long accredited with an essential rôle in gout.
Thus we cannot, on the basis of the variations in its excretion only, presume to diagnose “gout.” This because even more extensive variations occur in healthy persons. On the other hand, attacks of gout never occur when urates are absent from the blood. To reduce the amount of these urates is clearly then of importance, and obviously to this end a knowledge of their source is essential. We have an analogy to hand in diabetes, in which the somewhat similar problem relating to glycosuria has been partially solved.
But before proceeding to the more strictly biological aspect of the relationship of uric acid to gout, we must, as in the study of any other problem of metabolism, place ourselves in possession of the main facts relating to the chemistry of protein, and more particularly of purin or nuclein metabolism; for it was just this same lack of even the most rudimentary facts, especially regarding the chemistry of uric acid, that vitiated the conclusions arrived at by the earlier workers in this sphere. Disabilities of technique of necessity rendered inaccurate the results obtained by these pioneers in research, while the significance of the facts they laboriously gleaned was likewise misinterpreted.
But with the advent of highly trained organic chemists, well skilled in the investigation of bio-chemical problems, a basis of accurate chemical facts was established. The story of the fate of protein and purin substances in the animal body, at one time a medley of guesses and gaps, was brought to one of relative certitude and completeness. The change involved has proved in truth revolutionary, and many the cherished shibboleth that has been ruthlessly cast aside.
How vivid the light thrown upon the problems of clinical medicine by the bio-chemists! With admiration not unmingled with awe we see them laying well and truly the foundations upon which in the ultimate scientific medicine must inevitably rest. Of these the very corner stones are chemical physiology and chemical pathology, the rapid evolution of which is profoundly altering our conceptions of health and alike disease. Those vital processes of the organism that but yesterday we saw “as through a glass darkly,” are now in great part illumined, and the distortions wrought in them by disease made more manifest.
How pregnant, too, with warning their findings! Processes that, to our untutored minds, seemed simple are revealed as infinitely complex. Through what a labyrinth must we thread[61] our way if we would unravel the intricacies of metabolism! Intricate enough, forsooth, in health, but how much more so in disease!—for as Sir Archibald Garrod eloquently phrases it, “It is becoming evident that special paths of metabolism exist, not only for proteins, fats and carbohydrates as such, but that even the individual primary fractions of the protein molecule follow their several catabolic paths, and are dealt with in successive stages by series of enzymes until the final products of catabolism are formed. Any of these paths may be blocked, while others remain open.”
It is with chastening reflections such as these that we may best approach our study of gout, that Riddle of the Ages, upon the elucidation of which so many physicians from time immemorial have expended their dialectic skill. Would that we could affirm that the bio-chemists of to-day had found the “Open Sesame!” But, alas, it is not so! The chamber is still sealed.
Vast though the increase in our knowledge of the chemical structure of uric acid and its allies, uncertainty still dogs our steps. Doubtful of the pathway to solution of the pathological mystery of gout, we must perforce approach the problem in a more strictly catholic attitude. Uric acid has apparently failed us as the causa causans. We can, therefore, no longer restrict our enquiry to purin, but must take cognisance of protein metabolism as a whole, for some, perhaps not unnaturally despairing of the uric acid hypothesis, are turning therefrom to other end-products of metabolism, e.g., creatinine. In keeping with this altered outlook, it will not be out of place if we, at this juncture, allude, though in brief, to the later revelations as to protein metabolism, before we pass on to more detailed consideration of those relating to the purin bodies.
No longer can we, like the older physiologists, envisage protein as being absorbed as such from the alimentary canal and forthwith incorporated with the body tissue, for the researches of Fischer have revealed that the complex protein molecule must previously undergo complete disruption into the a-amino-acids, its ultimate “building stones,” this through the hydrolytic action of the digestive enzymes of the alimentary tract. The fact that Fischer[6] was able to maintain nitrogen equilibrium in animals[62] fed with completely digested protein mixtures is, of course, direct evidence in favour of his contention, viz., that proteins undergo disruption into amino-acids.
The question as to whether urea, the end-product of general nitrogenous catabolism, was derived from the amino-acids, brought in the portal blood to the liver, was for long a vexed one. This because the earlier attempts to detect amino-acids in the portal blood, during the digestion of copious amounts of protein, proved futile. On the other hand, the same workers found that free ammonia was present in greater amounts in the portal vein than in the systemic circulation.
This, to their mind, seemed to indicate that the amino-acids, during their passage through the intestinal mucous membrane, underwent deaminisation. According to this view the ammonia, thus split off from the amino-acids, was the precursor of urea.
But the claim that more free ammonia was present in the portal vein than in the systemic circulation was disproved by Folin and Denis. Invoking more delicate methods of hæmo-analysis, they found that the amount of ammonia and urea in the portal blood was not increased during the absorption of amino-acids from the lumen of the intestine. Moreover, they found that the ammonia present was of minimal amount, produced in the main by putrefactive bacteria. Lastly, they discovered that amino-acids were actually present in the portal blood.
In the gastro-intestinal tract the complex food proteins, under the hydrolytic action of enzymes, break down into a variety of substances, all of which belong to the group of a-amino-acids. These same absorbed from thence into the blood are transported to the various organs and tissues. Arrived thither the amino-acids are subjected to a process of sifting. Thus some are invoked for the reconstruction of broken down proteins, i.e., are re-synthesised into the body’s own characteristic tissues.
The surplus amino-acids, viz., those not required for purposes of cell repair, undergo deaminisation. Two residues then result,[63] one represented by ammonia, and the other by the remaining relics of the amino-acid molecule. The former is excreted as urea and the latter is oxidised to produce energy.
But there is yet another source of amino-acids, viz., the disintegration of tissue protein. To this end almost all bodily tissues possess intracellular enzymes capable of converting their proteins into the same simple products from which they took origin.
Comparably with those of exogenous origin, these amino-acids of endogenous formation undergo a like deaminisation; in other words, the bulk of their carbon, oxygen, and hydrogen is oxidised to form CO₂ and water, the residue combining with nitrogen to form urea, etc.
The main end-product, then, of protein metabolism is urea, with traces of its forerunner ammonia. But there are also other waste nitrogenous metabolites. Thus, of the various amino-acids that become built up into tissue protein, some subsequently break down into products not belonging to the amino-acid category, viz., creatine and creatinine. Some of the amino-acids, too, are excreted unchanged in the urine. Lastly, to these must be added those closely related substances, the purin bodies, the end-products of nuclein as opposed to general protein metabolism, of which latter urea is the terminal product. To sum up, in a man on ordinary diet about 90 per cent. of his total nitrogen is excreted as urea, about 3 per cent. as ammonia, the residue of the nitrogen appearing in the form of other nitrogenous metabolites.
The liver, it is generally held, is the main centre wherein urea is produced from the amino-acids; but not exclusively so, for it has been definitely established that, even after removal of the entire liver in animals, its production may not cease.
Moreover, some researches of Otto Folin and W. Denis into urea formation seem to indicate that the older views call for revision. Experimenting on cats, they injected them with alanine and glycocoll nitrogen and other amino-acids as well as Witte’s peptone. They were able to prove definitely that, at the end of an hour or more, the formation of urea from the absorbed amino-acids was unmistakably demonstrable. Also they noted that interesting fact, that the “urea nitrogen obtained from the hepatic blood is not larger than the urea in the blood obtained at about the same time from the iliac artery.” This they claim indicates that “the liver has not brought about any demonstrable specialised deaminisation.”
The experimental data forthcoming in their researches, while[64] they prove that the absorption of amino-acids is very swiftly followed by the formation of urea, does not afford any definite evidence as to the site of urea formation; but, as they rightly contend, we have no satisfactory proof that deaminisation and urea formation is localised. Consequently “we are not justified in assuming that the process is a specialised process in the sense of being confined to some particular organ.”
Indeed, they bring forward evidence that the process of urea formation, far from being localised to any particular organ, i.e., the liver, is almost ubiquitous.
Thus, experimenting with the injection of alanine, they noted that prior to the same the muscle content of non-protein nitrogen and urea nitrogen was respectively 194 and 26 mg.; but 180 minutes after the injection the non-protein content in muscle had risen to 232 and that of urea nitrogen to 41 mg. Working with glycocoll, the non-protein and urea nitrogen in muscle before injection of the same was 248 and 42 mg. respectively, while 240 minutes after injection the figures were 304 and 54 mg.
The significance of these figures is more striking when contrasted with the fact that in the same subjects the urea nitrogen content of the hepatic blood did not exceed that obtained almost simultaneously from the iliac artery. The deduction made by Folin and Denis is that—
(1) “The urea-forming process is one characteristic of all the tissues, and by far the greatest amount of the urea is, therefore, probably formed in the muscles.”
(2) “The negative results, so far as any localised urea formation is concerned, is almost satisfactory proof that there is none, for if there were one central focus from which all or nearly all of the urea originated we could scarcely fail to find it.”
The vista opened up by these advances in physiology suggested investigations into the amino-acids, their association with the output of uric acid in gouty patients. No less than eighteen different amino-acids enter into the constitution of protein, but of these the most interesting from our point of view is glycocoll or amino-acetic-acid. Now, glycocoll plays a great rôle in the organism as a detoxicating agent, rendering innocuous, e.g., benzoic and cholic acids by transmuting them into hippuric and glycocholic acids. In short, the body always has glycocoll at its disposal for coupling or combination purposes.
Now it appears likely that glycocoll can be split off from all the amino-acids, a probability reinforced by the results of the[65] researches of Embden and Reese and Lipstein, these observers having shown that amino-acids are present in all urines to about 1 per cent. of the total nitrogen output.
Ignatowski, working with the urine of gouty patients, found amino-acids present in large amounts; not that it was peculiar to such subjects, for he found it in other diseases, but only traces were detectable in the urine of healthy individuals. Again, Walker Hall, investigating urines drawn from the subjects of gout, the victims of other diseases, as well as healthy and diseased children, determined the presence of glycocoll in about 70 per cent. of the cases. His researches, to his mind, confirmed the conclusion that “normally a certain amount of glycocoll escapes through or is eliminated by the renal filter.”
Burger and Schweriner, from their researches on gouty subjects, have confirmed Walker Hall’s findings as to the excretion in excess of amino-acids, especially glycocoll. Lastly, Almagia has in gouty urines detected the presence of glyoxylic acid. What its significance may be is uncertain, but it is at least interesting to note that, as MacLeod suggests, the synthetic formation within the body of glycocoll may very probably result from the interaction of ammonia and glyoxylic acid.
Excessive meat feeding in dogs, according to Kochmann, induces degenerative changes in the liver and kidneys. Similar tissue alterations were noted by Walker Hall in rabbits, after injection with hypoxanthine, while the same was observed by Kionka in mice. These findings suggest that, although anatomical lesions are not apparent in the livers of “gouty” men, it is at least probable that functional damage results from the overeating of meat.
Now, if glycocoll be added to a solution of (neutral) dialkali-urate, it expedites the appearance of the (acid) mono-alkali-urate, a reaction more noticeable with the sodium salt. Urea, in contrast to glycocoll, markedly inhibits the formation of the acid salt. But if glycocoll be added to a solution of the (neutral) dialkali-urate and urea, the latter parts to some extent with its powers in this respect, and the mono-alkali-urate is deposited.
It is reasonable, then, to suppose that if, as testified by Ignatowski and Walker Hall, glycocoll is present in gouty urine, it is also present in the tissue fluids of the gouty individual, and so the precipitation of uric acid is favoured. Glycocoll, normally, is almost entirely transmuted into urea by the urea-forming ferment of the liver.
Impressed by these considerations, Kionka advances the hypothesis that gout is due to:
(1) Functional changes in the liver, a depressed urea-ferment action.
(2) A deficient uric acid excretion by the kidney, possibly due to the changed uric acid combinations in the blood.
(3) These pathological conditions may be “hereditary” or “acquired,” from overeating, alcohol, lead, etc.
In other words, given deficient action of the urea ferment in the liver, then more glycocoll will be present in the blood-stream, and the uric acid may be thrown out of solution.[7]
For it is possible, as Kionka suggests, that normally uric acid, on its way to urea, may pass through a glycocoll stage. Now, in the gouty individual the glycocoll may not be entirely transformed to urea, and its excess in the tissue fluids may lead to uric acid deposits. Perhaps, as Walker Hall observes, “since hepatic deficiency is generally admitted in the gouty, diminished destruction of uric acid and glycocoll may go hand in hand.”
In healthy cartilage glycocoll is undemonstrable. But, according to Kionka, if bruised or damaged, a considerable amount thereof is formed. Now, when blood, rich in uric acid, circulates through injured cartilage, the presence of glycocoll favours precipitation of the urates, a possible explanation of the formation of tophi. Unfortunately for the valency of this theory, Aberhalden and Schittenhelm show that the methods employed by Frey, to isolate glycocoll from cartilage, were such as yield errors which would quite account for the amount obtained by this worker. They, therefore, deny the presence of glycocoll in damaged cartilages. But, in conclusion, Kionka’s plea for a primary hepatic functional disability derives colour from the fact that the drugs which have gained most approval in the treatment of gout are those which increase the quantity of bile without augmenting the amount of bile acids; and the which are excreted in combination with glycocoll, for instance, salicyclic acid combines with glycocoll, and is excreted as salicyluric acid, and benzoic acid, which combines with glycocoll to form hippuric acid. Albeit, we must not overlook the fact that the presence of glycocoll is not peculiar to gouty urine, but, as shown by Walker Hall and Embden, is met with in other disorders. The glycocoll hypothesis as to the origin of gout is, though attractive, therefore still unproven.
According to Tilden Brown, the rhythm of urea excretion constitutes a warning as to the approach of gout. A very lowered elimination thereof he holds to be an excellent and pathognomonic symptom. The excretion of urea may at times run so low as to lead to a suspicion of renal disease. He considers that this sign may find a place in the prophylaxis of gout, a signal for the initiation of treatment with the object of lessening the severity of symptoms (viz., extent of toxic action as manifested by destruction of proteid, etc.).
This point was advanced by Brown (1905) during a discussion at the Harvard Medical Society, but as far as we know it has not been confirmed. Presumably it rested upon the assumed existence of a normal ratio of uric acid elimination to that of urea with the corollary that every deviation therefrom was due to a pathological cause. Haig held this view, which was, however, disproved by Herringham, Groves and Luff. The latter authority estimated the daily eliminations of uric acid and urea in a healthy adult man on a mixed diet for a period of fifty days, and clearly showed that no constant ratio exists in a given individual between the excretion of uric acid and urea.
Also, it is obvious that, before attaching any valency to Tilden Brown’s dictum, it is essential that it be established that the cases were instances of pure gout, unaccompanied by nephritis. Moreover, modern workers tend more and more to rely not on analyses of the urine but of the blood, especially in the unravelling of so-called metabolic disorders. Also, it may be added, that their findings in this sphere indicate no harmony between the urea and the uric acid content of the blood. Thus, Otto Folin observes, “One most interesting fact which we constantly meet with in blood analysis is that there is no correspondence between uric acid and the total non-protein nitrogen in the blood. In gout or lead poisoning, or leukæmia, the blood is uniformly rich in uric acid, yet the total non-protein nitrogen or urea nitrogen may be normal.”
As before pointed out, it has been suggested that these substances may be in some obscure way related to the genesis of gout. To this end a great amount of research has been expended on the metabolism of creatine and creatinine. But although, as far as I am aware, the revelations hitherto forthcoming have disclosed no link between these substances and the development of gout, still, by reason of the potentialities possibly resident therein, a brief digression is permissible.
The exact origin of creatine and creatinine is still obscure. All we know is that they are, in the main, the outcome of chemical processes in the tissues, viz., products of endogenous metabolism. Also of the creatine and creatinine present in food a moiety may appear as creatine in the urine.
Creatinine occurs in the urine of adults, and is practically independent of the protein intake. The amount excreted varies with the size, and not with the weight of the body. In other words, it varies with the volume or mass of the voluntary muscles, which structures have the highest content of creatinine and creatine. MacLeod, discussing this relationship, tells us that, “in the muscular atrophies creatine excretion is distinctly below normal.” It must, he adds, be the “mass of the muscles rather than their activities that is the determining factor, for the creatine excretion does not become increased by muscular exercises.” Otto Folin, discussing the clinical application of pathological chemistry, observes, “Nothing definite is as yet known concerning the creatinine output in abnormal metabolism, except that in fevers and other diseases there is an increase, sometimes a very large increase.” But this much we do know that creatine, after ingestion, is almost quantitatively excreted in the urine. Creatine, in considerable amount, is a normal constituent of children’s urine, but in normal adults hardly a trace occurs, though in some diseases it is met with even in their case. In boys it gradually dwindles and disappears at about seven years of age. On the contrary, in girls creatine is excreted until puberty. Subsequently, its presence in the urine is intermittent, its incidence confined to the menstrual cycles, the period of pregnancy, and for some days after parturition.
From our point of view, the most interesting of the above revelations is the fact that the largest percentage amount of creatine and creatinine is located in the muscular tissues. On this point we cannot do better than quote the following words of Otto Folin:—
“It is to be noted that we are as yet entirely ignorant of the origin and significance of the creatine which is so abundant in muscles, and it is scarcely to be doubted that fundamentally important metabolism problems somehow are connected with the muscle creatine and urinary creatinine, but these are as yet problems of normal metabolism, and it is too early to say whether, or in what way, light may be thrown on clinical problems by studies of these products. The fact that the muscles of mammals, including man, contain 0·3-0·4 per cent. of creatine, and only traces of the chief nitrogenous waste product urea, constitutes to my mind strong presumptive evidence that creatine serves some important function, and it is quite conceivable that metabolism[69] diseases of one kind or another may be associated with this curious substance, but investigations rather than hypotheses are needed in the study of such obscure problems.”
Apart from its intrinsic fascination, the tracing out of analogies, clinical or pathological, between diseases apparently diverse has often proved a fruitful source of enlightenment, for the natural history of disease is such that one disorder trenches upon the clinical territory of another, symptoms overlap and similarity if not community of origin is revealed.
Few will gainsay that gouty individuals are the victims of some inborn defect or eccentricity of metabolism, and instinctively the thought arises, are there no other disorders of like character? Immediately we bethink ourselves of alkaptonuria, cystinuria and pentosuria. Sir Archibald Garrod, as we know, classed these disorders as “chemical malformation” of hereditary origin. In other words, all are the outcome of an abnormality in intermediary metabolism.
In alkaptonuria the metabolic warp concerns the aromatic groups, in cystinuria the sulphur-containing radicles of the protein molecule. On the other hand, in pentosuria the origin of the endogenous pentose is variously ascribed to the nucleo-protein of the cell nuclei or to galactose. Lastly, in gout it is in the metabolism of nucleo-protein, or rather of the nucleic acids of the cell nuclei that the flaw resides.
We see, therefore, that Langdon Brown, discussing gout, is well justified in observing that, “We may look upon a person who is readily poisoned by purins in the same light as the person who has cystinuria, alkaptonuria, or pentosuria, i.e., they all lack a link in the chain of protein katabolism, so that intermediate products appear in the urine instead of the usual end-products.” In other words, they all display a pathological kinship, viz., in that they are all due to inborn errors of metabolism.
Certain broad clinical resemblances also obtain. All members of the group, including gout, display hereditary tendencies. All occur much more often in males than in females. They all alike tend to persist through life. Lastly, their distinctive chemical products, including uric acid, are all apparently of low toxicity.
But when we pass to the realm of their symptomatology, resemblance, if it does not cease, becomes relatively obscured. Cystinuria and pentosuria appear to be “harmless anomalies,” and the same is true of alkaptonuria. The cystinuric, albeit, does suffer with[70] urinary concretions, and we may recall that some authorities hold that gout and uric acid calculi are not unrelated. As to alkaptonuria, it has this attenuated link with gout that in its later stages the victims thereof tend to develop a degenerative type of arthritis, while the frequently associated pigmentary change, ochronosis, has a predilection for deposition in the cartilages of the ears and joints.
But how colourless the clinical features of alkaptonuria, etc., as contrasted with the vivid arresting phenomena of gout! how remote the latter disorder from these “harmless anomalies”!
Apart from this general distinction, before gout could with justice be relegated to the same category of disorders, it would be necessary to prove that uric acid was an intermediary and not a terminal product of metabolism. All modern research, however, tends to indicate that uric acid is an end-product, and, moreover, that there are no uricolytic ferments within the body whereby its destruction can be accomplished. The term “chemical malformation,” therefore, though strictly applicable to alkaptonuria, cystinuria, etc., is inapplicable to gout. In other words, though, for example, the homogentisic acid met with in alkaptonuria is a “chemical malformation,” uric acid cannot be regarded as such. We see, therefore, that though gout may, superficially regarded, appear to have kinship with alkaptonuria and its congeners, yet in reality there is a profound and essential difference between it and this fascinating group of disorders.
No hard and fast line can be drawn between the metabolism of protein and that of nuclein. For though, morphologically speaking, the nuclei of cells are sharply differentiated from the circumambient cytoplasm, and exhibit equally distinct staining reactions, yet, chemically, the differences between them are quantitative rather than qualitative.
But while, as far as chemical changes are concerned, nuclein metabolism is comparable with that of protein, nevertheless the former in respect of its “energy” and its bearing upon growth and production, is infinitely more vital, incomparably more active; for it is in nuclear changes that we may best discern evidence of the initiation of oxidation processes and other varieties of enzymatic activity. Moreover, as Walker Hall points out, “the presence of masked iron phosphorus and certain forms of fat in the cell nucleus strengthens this view, and thus we are led to recognise the important part played by the nucleus in the life of the cell, and to appreciate the influence of nuclein heredity in cellular exchanges.”
So much by way of prelude, but the story of the growth of our knowledge of nuclein as opposed to protein is so fascinating as to be worthy of a slight digression.
Functionally regarded, the nucleus is the essential element of the cell. Embedded within the cytoplasm, its isolation therefrom, and this in quantities sufficient for analysis, may well have dismayed the earlier workers. But the resources of Friedrich Miescher were equal thereto. Treating surgical bandages soaked with pus with a dilute solution of sodium sulphate, he extracted the heavy pus cells. These, then, by careful decantation, were easily disengaged. The pus cells, still intact, were then subjected to the digestive action of artificial gastric juice. The protoplasm was thus dissolved, but not the more resistant nuclei, which remained as an insoluble grey powder. In this manner cell nuclei, free from protoplasm, became available for chemical analysis. Treating the insoluble nuclei thus obtained with dilute sodium carbonate, a solution was formed. Acetic acid added thereto produced[72] a flocculent precipitate which was found to contain phosphorus, and responded to protein colour tests. This substance Miescher christened by the name of nuclein. Subsequent observers prepared nuclein from the nuclei of yeast cells and the red blood corpuscles of birds. All nucleins are insoluble acids which form soluble salts with sodium. But while they respond to protein colour reactions they differ from protein in that they contain phosphorus and resist the solvent action of artificial gastric juice.
Migrating some ten years afterwards (1897) from Tubingen to Basle, Miescher entered upon his celebrated researches into the habits of the Rhine salmon. He found the belief had long been current that the fish, during their passage from the sea up the Rhine to their spawning haunts, never partook of food. That this belief was well founded he was able to prove; for, saving isolated and easily explicable exceptions, he noted that their alimentary canal was devoid of food débris, while their digestive juices were as a rule inert. One startling change he noted, that while, on the one hand, their muscular tissue profoundly wasted during their migration, their organs of reproduction enlarged enormously, the inevitable conclusion being that eggs and spermatozoa had been created from muscle protein.
Struck by the opportunities for scientific investigation during the spawning season, Miescher determined to resume his work upon nuclein. Spermatic fluid or lachsmilch, being readily obtainable in great quantities, he had to hand a mass of material admirably adapted for chemical examination of the cell nucleus. The conclusion that the heads of the spermatozoa might be regarded as a metamorphosed nucleus seemed obvious, and the opportunity too good to be lost.
On examination he found the “sperm heads” protein-free, made up almost entirely of a single chemical entity, a salt of an organic base rich in nitrogen and an organic acid containing phosphorus. The former was protamine, the latter nucleic acid.
The presence of this salt protamine nucleate led to the conclusion that nuclein was merely a salt of protein and nucleic acid.
Miescher, who had already isolated nuclein and nucleic acid, came nigh to one other equally important discovery. Heating a specimen of protamine with nitric acid, he noted that a yellow spot formed which turned to bright red when moistened with alkali.
Alive to the import of the reaction, Miescher requested Piccard[73] to examine salmon sperm for purin bases. Extracting the same with hydrochloric acid, Piccard found guanine, and what he thought was hypoxanthine, but which was in truth adenine.
Another distinguished worker in this sphere, Kossel, noted that, subjected to the action of hydrolytic agents, nucleins always yield purin derivatives; also that the same were derived, not from the protein of the nuclein, but from the nucleic acid. Thus it was to Kossel that we are indebted for the discovery of the purin bases, hypoxanthine, xanthine, guanine, and lastly adenine. It was, indeed, through his brilliant achievements that nucleic acid became recognisable as a definite entity, distinguishable from proteins and other body elements, this latter differentiation by token of the purin bases which are contained in nucleic acid.
Moreover, it led to the dissipation of the old belief that uric acid was an intermediate product of protein metabolism, for the revelation of purin bases as decomposition products of nucleic acid carried with it the inference that uric acid also had chemical affinities therewith. The chemical structure of the purin bases and that of uric acid betrayed a common likeness, and, therefore, a presumptive physiological connection; in other words, that a chemical nexus obtained between the cell nucleus or nucleic acid and uric acid.
The physiological derivation of uric acid from nucleic acid did not long lack experimental proof. In 1886 Minkowski found that, given extirpation of their livers, the urine of birds contained ammonium lactate, evidently a substitute for the uric acid normally present, notwithstanding the uric acid never entirely disappeared from the urine. This indicated the derivation of uric acid from two sources:—
To clear up the obscurity regarding the latter, V. Mach, after extirpating the livers of geese, injected them subcutaneously with hypoxanthine, finding that the same was converted into uric acid, which was excreted in the urine. In this way the capacity of the organism to elaborate uric acid from a purin precursor was demonstrated.
Despite V. Mach’s revelation, the origin of uric acid from nucleic acid was still to seek. In the year following (1889) Horbaczewski traced it to this source, and in the following manner. Mixed with water, the pulp of the calf’s spleen was put to digest at 50° until putrefaction began. The fluid was then sterilised[74] with a solution of lead acetate, and arterial blood being added it was kept at 50°, a current of air meanwhile being passed slowly through the mixture. Subsequently the fluid was found to contain uric acid; but the experiment being repeated, without the passage of air, xanthine and hypoxanthine and not uric acid resulted.
While Horbaczewski’s experimental findings were amply confirmed, some of his deductions therefrom were subsequently proved faulty. (Thus, he thought putrefaction an essential factor; also he believed that the formation of uric acid ensued before the purin groups were disengaged from the nucleic acid, and definitely affirmed that the uric acid was not produced by the oxidation of free xanthine or hypoxanthine.)
But, nevertheless, this pioneer established that in both man and rabbits uric acid was derived from nucleic acid. Also, having observed that when after starvation the food intake was resumed, a leucocytosis occurred, he announced his belief in the following theory. Thus, he noted that leukæmics, whose blood showed a high leucocyte count, excreted an unusually large amount of uric acid; consequently, he came to the conclusion that uric acid was formed from defunct leucocytes. Also that nuclein-rich food, when ingested, contributed to the formation of uric acid only in so far as it induced leucocytosis. Hence the origin of the increased uric acid excretion which occurs when feeding is resumed after starvation.
This increased excretion of uric acid after the ingestion of food rich in nucleic acid has been amply confirmed; but all the earlier attempts to achieve an increased excretion by the ingestion of free purin bases, as opposed to the combined purin bases, existing as such in nucleic acid, failed, although tried repeatedly.
So much for the various stages by which our knowledge of the purin derivatives of nucleic acid has been gradually acquired, for though purin bases had, from early times, been known to exist in animal tissues, their presence there could not be rationally accounted for prior to the discovery of nucleic acid.
It still remains for us to deal in detail with the further developments of our knowledge which concern the disruption of nucleic acid in the body and the process by which uric acid is derived therefrom.
But before proceeding to consider in detail the complex series or enzymatic transformation that this entails, it will, I think, be wiser to deal first with the chemistry of uric acid, its solubilities, and its sources, whether exogenous, endogenous or synthetic.
Much of the vague philosophy of disease in past times may fairly be attributed to the complexity and mystery of action inherent in living matter. The subjects of physics, chemistry and biology, in their wider acceptation, were unevolved, and scientific pathology, the offspring of this ancestry, was yet unborn. How much we owe to physics, chemistry, and biology, those handmaids of medicine, is inestimable! But something at least of our debt thereto will be revealed in the following pages.
Of the purins in human urine, the most important is uric acid, and far behind comes xanthine, while traces of hypoxanthine, guanine, and adenine are also detectable. Some years ago the current view was that the metabolism of any protein gave rise to uric acid. This assumption has now proved to be erroneous, for it is known that only certain foodstuffs lead to an increase in the uric acid excretion; in other words, on a diet rich in purin the output thereof is considerably higher than on a purin-free diet, this being due to the large amount of nuclein and purin bases in flesh foods, especially those containing glandular substances. Under ordinary conditions the excretion of uric acid ranges from 0·3-1·2 gm. per diem, or 0·02-0·10 per cent. The oscillations in output vary with the state of health, diet, and personal idiosyncrasy.
The empirical formula of the uric acid molecule, C₅H₄N₄O₃, has for long been known, but it was reserved for Emil Fischer to reveal the chemical structure thereof. Through his labours we now know that uric acid is one of a group of substances which owe their kinship to their possession in common of the heterocyclic ring termed by Fischer the “purin nucleus” (1898).
The intimate relations of the purins of bio-chemical interest to the purin nucleus, and alike to each other, will be rendered more intelligible by examination of their structural formulæ as hereafter given. All, as will be seen, are derivatives of a synthetically formed body purin which, though unimportant in itself, is yet interesting in that it is the basic substance from which the following take origin:—
| Purin | C₅H₄N₄ | |||
| Hypoxanthine | C₅H₄N₄O | Monoxy-purin | } | |
| Adenine | C₅H₃N₄NH₂ | Amino-purin | } | |
| Xanthine | C₅H₄N₄O₂ | Dioxy-purin | } | Purin Bases. |
| Guanine | C₅H₃N₄ONH₂ | Aminooxy-purin | } | |
| Uric acid | C₅H₄N₄O₃ | Trioxy-purin | } |
It now devolves upon us to note the arrangement of the atoms in the purin nucleus. To each atom is affixed a number indicating the exact location of the various atoms and groups attached to the said nucleus. The manner in which the various purin bodies are built up around the purin nucleus C₅N₄ will become apparent from a study of the following structural formulæ culled from Wells’ “Chemical Pathology”:—
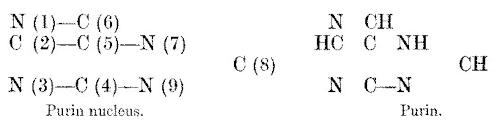
To describe the individual derivatives of purin we have to indicate to which particular atom of the purin nucleus the combining groups are attached. Thus, for example, adenine in structure is classed as a 6-amino-purin, and accordingly has the following formula:
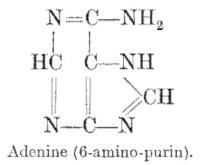
Other important bodies built up round the purin nucleus C₅N₄, variously designated as xanthine, alloxuric and nuclein bodies:—
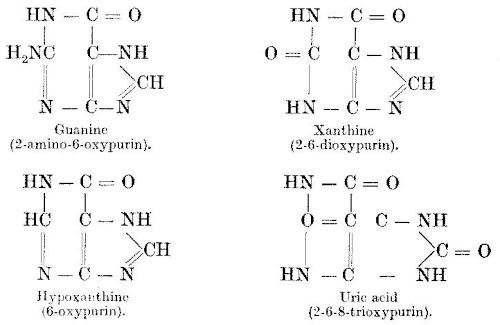
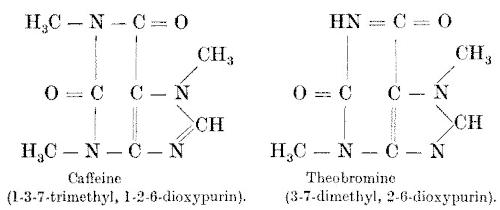
It will be seen that the purin bases stand in very close chemical relationship to uric acid in that the latter also is marked by the possession of a group called the purin nucleus; indeed, the relationship of uric acid to the purin bases is more intimate than to urea (CON₂H₄), close though this latter be as may be seen from the study of its constitutional formula. (For uric acid may be regarded as composed of two urea radicles, linked by a tricarbon chain. By oxidation and hydrolysis, two molecules of urea may be obtained from one of uric acid, and conversely uric acid is produced by the condensation of urea with hydroxy acids).
The first product of the oxidation of purin is hypoxanthine, long recognised as a constituent of meat extracts. Adenine, the amino derivative of hypoxanthine, is met with in combination with other substances in nuclear material. The second oxidation product of purin is xanthine, and its amino derivative guanine, both of which are found in the same substances as hypoxanthine and adenine. Further oxidation of purin gives rise to uric acid. We have to recognise, also, that in addition to the purins of animal origin there are some also derived from vegetables, viz., the methyl purins, caffeine, theobromine, and theine.
Now, as will be seen later, certain compounds, containing nitrogen and phosphorus, constitute the chief, if not the exclusive, source of uric acid. These substances, long known as nucleins or nucleo-proteins, exist in the animal tissues, and in special abundance in those largely made up of cell nuclei, viz., thymus, lymph-glands, etc. The important and, indeed, the distinguishing component of the nucleins or nucleo-proteins is nucleic acid. This, in that through the action of ferments, it is from the nucleic acids that uric acid and the purin bases are derived.
But, apart from this, we have to recollect that nucleic acids yield constituents other than purin bases, viz., the pyrimidine bases, phosphoric acid, and a carbohydrate group. From a study of the structural formulæ of the pyrimidine bases it will be seen that they are closely related to the purin bases, lacking, however, one of the urea radicles. Moreover, it is believed that, though included[78] in the makeup of nucleic acid, they are not derived from purin but are primary products.

To sum up, the characteristic constituents of nucleic acid are the purin bases (adenine, guanine, hypoxanthine, and xanthine), pyrimidine bases (uracil, cytosine, thymine), phosphoric acid and a carbohydrate group.
We have now discussed the chemical structure of uric acid and its relationship to the purin bases; but before proceeding to consider the various sources from which uric acid is derived, it will I think be convenient to consider (1) the physical properties of uric acid and (2) the condition in which it circulates in the blood.
When pure, uric acid is white in colour and crystallises in rhombic form. In contrast to urea it is very insoluble, but much less so in blood serum than in distilled water, viz., ⅟₄₀₀₀₀ of water as opposed to ⅟₁₀₀₀ parts of plasma. It yields with alkalies two series of salts, viz., the biurate or mono-basic, and the so-called neutral or bi-basic urate, the latter of which is much more soluble. In water the mono-basic urate forms a colloidal solution from which the crystalline salt gradually precipitates.
The greater solubility of uric acid in blood plasma was, by Garrod and Haig, attributed to the alkalinity of the plasma. But it must be recalled that the earlier workers in this sphere judged of the alkalinity of the plasma by its reaction to litmus, a crude procedure as compared with the use of phenol-phthalein, and Frankel’s electro-potential measurements. Working with these as criteria, it has been shown that blood is normally alkaline in only a minority of cases, and indeed, according to Flack and Hill, the plasma is in reality neutral.
In the urine uric acid and the urates are held in solution by the neutral phosphates. This because the decomposition of the urates into uric acid by the acid salts of the urine is inhibited by the di-sodium phosphate present therein. Its maintenance in solution is possibly also reinforced through the influence of other constituents in the urine, notably, the urinary pigments and sodium chloride.
As to the form in which uric acid circulates in the blood, Sir William Roberts believed that when dissolved in blood serum it was transformed into the relatively soluble sodium quadriurate.[79] This authority held that in gout, either through deficient excretion or over-production, the quadriurate accumulates in the blood. Circulating therein, in a medium rich in sodium carbonate, it takes up an additional atom of the base, and is transmuted into the biurate, which is less soluble and less easily excreted by the kidneys; consequently, the biurate is hoarded up in the blood, at first in gelatinous, and later in an almost crystalline form, when its precipitation is imminent or actually ensues. This, moreover, was apt to occur at sites where the circulation was poor, the temperature low, and more particularly in regions in which the plasma contained a relatively high percentage of sodium chloride, e.g., synovial sheaths.
But, unfortunately for the valency of this otherwise plausible theory, it was proved by Tunnicliffe, Rosenheim, and others, that quadriurates do not exist as definite chemical compounds; in short, it is generally conceded that their existence should no longer be accepted.
Gudzent was of opinion that uric acid can only exist in the blood as the mono-sodium-urate, of which there are two isomeric varieties, the easily soluble unstable lactam, and the stable relatively insoluble lactim urate. It is the former, or lactam, variety that accumulates in the blood in gout and, according to Gudzent, it is the transmutation thereof into the lactim modification that determines the precipitation of urates in the tissues. The lactim urate is soluble only to the extent of 8·3 mg. per 100 cc. serum, whereas the lactam form is soluble up to 18 mg.
Others, like Bechhold, maintain that the urates are present in the blood in a colloidal form, impossible of excretion by the kidneys. Thus Schade contends that, in the presence of alkalies (hydrates), uric acid or its salts may pass into a state in which it is far more soluble than usual. Moreover, on its path to crystallisation from this over-saturated solution, it passes through a colloid stage in which it is relatively stable. The maintenance of this colloid stage and consequently the retardation of precipitation is promoted by certain substances, i.e., glycerine, urea, serum, albumen, nucleic acid, etc. But hitherto the therapeutic possibilities suggested have not been invoked.
It will be recalled that purin bodies cannot be detected in the blood in health, though their administration by the mouth results in an increase in the excreta. Minkowski, to account for this, suggested that the purins in the blood were circulating in a combination[80] which prevented them from giving the usual reactions, typical of their presence therein. We have an analogy in the masking of arsenic and iron in the cacodyl compounds and the ferrocyanide ion.[8]
The explanation proffered by Minkowski was elaborated by Von Noorden. His view was that lying at the disposal of the normal organism are a certain number of organic substances. These latter can combine with uric acid and render it soluble. It is then in this form passed through the blood in the kidneys, which eliminate from it the uric acid. Now, in gout these organic substances are deficient or wanting, and the result is that the uric acid is passed into the blood in the form of urates, the elimination of which only proceeds with difficulty; in other words, the purins normally circulate in organic combination and abnormally as salts of sodium.
It is worthy of note that, from a solution containing albuminous substances, Burian and Walker Hall found that while it was easy to remove the bulk of the purins, a certain percentage always remained which it was difficult to extract.
The view that uric acid is probably carried in the blood in combination with some other organic body and not, as was formerly supposed, with sodium salts, rapidly gained adherents, but the nature of the organic complex is still not accurately known. Many believe that at least a moiety of the uric acid circulates in combination with nucleic (thyminic) acid, but no such compound has yet been isolated from the blood. Nevertheless, as MacLeod suggests, this theory, were it proved correct, would account for the fact that some purins at least are katabolised in the body when they are given in a combined state, as thyminic acid, but are excreted unchanged when ingested in a free state. Thus, certain purins, e.g., adenine, when given freely, cause inflammation and calculous deposits in the kidneys of dogs which, however, does not ensue when they are fed with thymic acid.
But Walker Hall, discussing the good results obtained by Schmoll and Fenner from the administration of thyminic acid,[81] states that his experiments do not indicate that the improvement is at all associated with any change in the uric acid excretion.
To sum up, it is obvious, from the mere variety of the hypotheses advanced, that we are still much in the dark as to the actual form in which uric acid circulates in the blood. While on the one hand the quadriurate theory appears no longer tenable,[9] on the other the nature of the suggested uric acid organic complex is still unknown.
Nay, more, Walker Hall, writing in 1913-14, states “there are many who consider that the sodium mono-urate is the only possible compound;” while Wells, in his “Chemical Pathology” (1918), claims that the best evidence points to uric acid existing in the blood “in a free state and not combined, as was at one time urged by several students of gout.”
How complex, indeed, the task of the bio-chemist may be gathered from some reflections of Walker Hall. He reminds us that the oxidation and deaminisation of the nuclein derivatives, nucleins, nucleotides and nucleosides, is never complete. For purin bases and pyrimidin bases run side by side in the blood-stream together with uric acid. Also, that the unstable but soluble biurate is constantly changing into a less soluble type, viz., from one isomer to another. Moreover, since the red blood corpuscles abound in potassium, urates of potassium must also occur, and to these may be added, too, ammonium and calcium compounds in small quantities.
But more striking is his inference that the occurrence of isomeric forms of uric acid suggests that isomers of purins and pyrimidins also may occur. For the purin ring or pyrimidin nucleus, with their numerous receptors for the linking up of other substances, offer wide potentialities in the direction of isomerism.[10] Some of these, he hazards, may be born of one type of cell nucleus, some of another, while it is not inherently improbable that, “In[82] response to abnormal stimuli or excessive demand, other isomers may be formed.”
Now, though uric acid and the urates can be extracted from the blood, it does not, as he remarks, necessarily follow that they circulate as such in vivo; for, despite modern achievements, “the best of the existing methods for the determination of uric acid in the blood are nearly barbarous in their crudity and intensity.” The various procedures available for such estimates fall short of distinction between the several tautomeric forms of uric acid, much less do they furnish any information as to the associations or combinations of purins or pyrimidins with other substances.
For himself, recognising the generally more complex nature of biological processes, he considers that “the circulation of the purins as sodium mono-urate and its simple extraction by kidney cells, seems almost too simple to be true.”
As to the solubilities of uric acid and urates in gouty blood he points out that the suspension capability of the blood-stream for uric acid much transcends the highest amount of uric acid as yet found in the gouty subject. Accordingly, to him, therefore, it seems that “neither chemical nor physico-chemical processes suffice to explain the problem. There must be something more, something vital, biological.”
Having ascertained as far as possible the measure of our knowledge in regard to the foregoing points, we shall, in the succeeding chapter, proceed to discuss the sources of uric acid, whether of intrinsic or extrinsic origin.
Uric acid, like the “purin bodies” (xanthine, hypoxanthine, guanine, and adenine), is derived from nucleins, i.e., from the breaking down of tissues rich in cells. The end-product of purin or nuclein katabolism uric acid represents but a further stage in the oxidation of the purin bodies. To the serial enzymatic transformations that mark its derivation from nucleic acid we shall allude later, but at this juncture we are concerned not with the mode of formation of uric acid, but with the sources thereof.
In this sphere we are greatly indebted to the pioneer researches of Burian and Schur. These observers noted that on a diet rich in nucleins (sweetbreads, liver, kidneys) the total daily excretion of uric acid was considerably higher than on a milk or purin-free diet. This difference in response to varying dietaries, in respect of the excretion of uric acid, led Burian and Schur to the conclusion that the purins excreted must be partly of exogenous and partly of endogenous origin; in other words, the exogenous purins are derived from the nucleins ingested in the food, whereas the endogenous are the outcome of the breaking down of the cellular tissue of the organism itself.
Here it may be noted that all the ingested purins are not excreted in the urine as uric acid, for some pass away as purins. Moreover, the amount excreted will vary with the kind of purin ingested, and also with the species of the animal that consumes it. Thus, in man “only one half of the hypoxanthine administered as such appears as uric acid in the urine, and but one fourth of the purin in nuclein when that is fed. In the dog, compared with man, about ten times as much purin disappears in its passage through the organism; in the rabbit, about three times” (Flack and Hill).[11]
In amount about 0·4-0·7 gramme of uric acid is excreted in human urine daily, and the purin bodies, hypoxanthine, xanthine, and adenine, in small quantities.
Beyond exogenous and endogenous purins there is yet one other possible source of uric acid, viz., its synthetic formation within the organism. This supposition took origin in Horbaczewski’s discovery that in the laboratory he was able to produce uric acid by the interaction of urea and glycocine, a finding afterwards confirmed by Latham. The theory was then advanced that a similar synthesis might be effected by the kidneys; but it was found that glycocine and urea, even when given in excess to mammals, caused no change in the uric acid excretion.
So much by way of preface to our detailed discussion seriatim of the various sources of uric acid, and to which we now pass on.
The foodstuffs that cause an increase in purin excretion are divisible into three groups:—
Amino-purins.—In man the taking of food rich in nucleated cells and therefore in nucleo-protein and nucleins, increases the quantity of uric acid in the urine. Thymus gland, pig’s pancreas, and herring roe, containing the characteristic conjugated proteins of nuclei, or Liebig’s meat extract, rich in purin bases, when ingested, lead to a distinct increase in purin excretion.
The researches of Kossel and Horbaczewski showed that such augmentation was mainly due to the production of uric acid from the nuclein substances of the food; in other words, it was due to the katabolism of nuclein, the cleavage products of which comprise adenine derived from thymus, and guanine from the pancreas, both of these bodies being amino-purins. According to Burian and Schur, of the amino-purins ingested, a fourth is excreted as purin.
Oxy-purins.—To this group belong xanthine and hypoxanthine. These substances occur in muscle, and in great abundance in meat extract, and Minkowski noted that the ingestion of xanthine bases markedly augmented the amount of uric acid excreted. In man, given ingestion of hypoxanthine as such, only one half thereof appears as uric acid in the urine. It may here be mentioned that not all the purin bases ingested exist bound up in the nuclein substances. An appreciable amount is present in the tissues in a free state, e.g., hypoxanthine in the muscles; consequently, a moiety of the intake of purin bodies, especially in the animal constituents of the food, is to hand ready formed, and does not require the disruption of nucleic acid for its liberation.
Methyl-purins.—The nuclei of vegetable cells also contain nucleo-protein, and, therefore, can add their quota to the purin intake. The most important are caffeine, theobromine, and theophyllin, the active principles of tea, coffee, and cocoa. It may here be recalled that of the purins administered in food, not all are excreted as uric acid, but some as purins. Now it is doubtful whether the methyl-purins lead to the formation of uric acid in the organism, or whether they are excreted as purin bases in the urine. According to Stewart, a fractional part of the purin bases in the urine is composed of heteroxanthine, 1-methyl-xanthine, and paraxanthine derived from the active principles of coffee, tea, and cocoa when consumed as beverages. As stated by Burian and Schur, one third of the methyl-purins ingested is excreted as purin.
From the foregoing data it will be obvious that the exogenous urinary purins are derived from nuclein and certain free xanthine bases, and that the influence of other nitrogenous foodstuffs in this direction is practically negligible.
As to the amount of exogenous purins that, when administered orally, can be recovered from the urine, it would appear that a certain rough parallelism obtains between the purin content of the food and that of the urine. The amount of the exogenous urinary purin differs for different forms of food, a variation well illustrated by the following table, giving the results of Burian and Schur’s researches.
| Diet. | Total percentage of purin substances in diet. |
Percentage of exogenous urinary purin. |
|---|---|---|
| Beef | 0·06 | 0·030 |
| Coffee | 0·20 | 0·075 |
| Calf’s liver | 0·12 | 0·060 |
| Calf’s spleen | 0·16 | 0·080 |
| Calf’s thymus | 0·40 | 0·100 |
Walker Hall, experimenting with various purin-containing foods, found that (1) with chicken 54·4 per cent., (2) with plaice 58·7 per cent., (3) with beef 47·4 per cent., (4) with haricot beans 55 per cent. of the food purin appears in the urine as exogenous purin. These findings of Walker Hall’s, like Burian’s and Schur’s,[86] reveal that, roughly speaking, 50 per cent. of the purin content in food is excreted in the urine.[12]
These figures must be taken as a broad average relating only to healthy individuals upon diets capable of perfect assimilation.
More recently, Mendel and Lyman found that about 60 per cent. of injected hypoxanthine, 50 per cent. of xanthine, 19-30 per cent. of guanosine, and 30-37 per cent. of adenine were excreted in the form of uric acid. While this is true of free purins, on the other hand, when bound purins, i.e., nucleins are administered, only a small proportion thereof appears as uric acid in the urine. But before proceeding to canvass the fate of the missing purin, it will, we think, be helpful if we interpolate here a table (Taylor and Rose), illustrative of the variations in uric acid excretion that attend a purin as opposed to a purin-free diet.
The subject of the experiment was, for three days, fed on a purin-free diet of milk, eggs, starch and sugar. At the end of this period a portion of the total nitrogen (3 grams) was administered in the form of sweetbreads, thymus gland, etc., with a high percentage content (0·482) of purin nitrogen. During the succeeding four days still more (6 grams) of the total nitrogen was replaced by sweetbread nitrogen. Subsequently the person was placed on the original purin-free diet.
| First period. Purin-free diet. |
Second period. | Third period. | Fourth period. Purin-free diet. |
|
|---|---|---|---|---|
| Total urinary N | 8·9 | 8·7 | 9·1 | 8·8 |
| Urea N and NH₂ | 7·3 | 7·1 | 7·1 | 7·05 |
| Creatine | 0·58 | 0·55 | 0·56 | 0·47 |
| Purin N (total) | 0·11 | 0·17 | 0·26 | 0·10 |
| Uric acid N | 0·09 | 0·14 | 0·24 | 0·07 |
| Remainder N | 0·91 | 0·88 | 0·18 | 1·18 |
From a study of the table it will be noted that, following the introduction of sweetbreads rich in nucleins, the uric acid content of the urine markedly increased, to sink again when a purin-free diet was substituted. But it will be seen also, as MacLeod points out, that “the increase of uric acid accounted for less than half of the purin nitrogen ingested. This appeared as uric acid, the excretion of purin bases being practically unchanged.” In other words, a moiety of the bound purins, i.e., nucleins ingested, appears as uric acid in the urine.
As to what becomes of that portion of the ingested purin that, so to speak, disappears in the body, is largely a matter of speculation. As MacCallum states, “the liberation of guanine and adenine is well in the line of uric acid formation,” but “the fate of the pyrimidin groups, thymine and cytosine, is still uncertain.” According to this observer, Levene has hitherto been unable to find an enzyme which will decompose the nucleoside in which they occur, and that since they cannot form uric acid, they are possibly excreted as urea or in other forms. He adds that only 50 per cent. of the nucleic acid nitrogen can be counted on for the production of uric acid, viz., that in the guanine and adenine groups.
MacLeod, discussing this same point, suggests that some of the unrecovered purin may undergo decomposition in the intestine, but why so much should, after absorption of the blood, disappear is, as he remarks, difficult of explanation; for while uricase, which can decompose uric acid, exists in the tissues of the lower animals, no such ferment is found in man, and uric acid is excreted as such. According to MacLeod, too, “the destroyed purins cannot be shown to influence any of the other well-known nitrogenous metabolites of the urine.”
Lastly, Stewart, discussing the ultimate destiny of the absorbed products of nucleic acid digestion, suggests that, when undergoing further cleavages, “they may be in part utilised for the synthesis of nucleo-proteins, replacing those destroyed in the process of cell metabolism;” or, that it is “possible that they may be wholly disrupted into their components, and these again re-synthesised.”... “Finally, and this fate is probably not long delayed in the case of the surplus of purin compounds contained in ordinary dietaries, both the purins of the food and the purins arising from the waste of the tissues, are for the most part converted into uric acid and excreted in the urine.”
Also, it should be recollected that the purin bases normally found in human fæces are in part of exogenous origin, and are increased in amount after the ingestion of meat extract or thymus.
Even if we entirely eliminate all purin substances, by restricting the diet to purin-free foodstuffs (bread, milk, cheese, eggs and butter), purin in the form of uric acid is still excreted in the urine.
To this moiety the term endogenous purin is applied; for the continued excretion of purin on such a diet is explicable only on the view that they are derived from the waste of the tissues, the[88] daily “wear and tear” of cells. In other words, it is the outcome of the katabolism of the nucleo-protein of the body tissues.
Is the nuclear destruction of localised or generalised distribution?
Mares (and subsequently many other observers), having noted that, following the ingestion of purin-free protein food, a marked increase in endogenous uric acid excretion ensued, suggested that the said augmentation was the outcome of the “wear and tear” entailed upon the nuclear material of the secretory glands of the gastro-intestinal tract, following such intake.
The effects yielded on uric acid excretion by those antithetic drugs, atropine and pilocarpine, certainly seem to lend colour to Mares’ hypothesis.
Following the injection of atropine, the rise in uric acid output, that normally follows the ingestion of protein, was inhibited. But in sequence to pilocarpine, an excitant and not like atropine, a depressor of secretory activity, a marked increase in uric acid excretion followed. The contrast in response was naturally translated as striking evidence of the important rôle played by the digestive glands on uric acid excretion; in other words, it was held that the major portion of the endogenous uric acid was the reflex of such intensified glandular action.
In opposition, however, Burian, as the outcome of his experimental studies, maintained that a fractional portion only of the endogenous uric acid could be derived from the nucleo-protein of the body cells. This, inasmuch as it would entail a far too extensive katabolism of nuclear substance. Accordingly he propounded the view that the endogenous uric acid in the main was derived from the hypoxanthine of the inosinic acid present in muscular tissue. In this connection it may be noted that, on a diet approximating to Voit’s standard, 0·5 gram of purin is excreted daily. This, it is calculated, is equivalent to nearly 100 grams of thymus or allied tissue, which probably far exceeds the amount that could be gleaned from cellular katabolism.
A comparison of the influence of proteins as contrasted with that of their digested products, the amino-acids, it was thought, might furnish a clue as to the extent of which the alleged activity of the digestive glands was responsible for the increased uric acid output that followed the intake of non-purin protein food.
Such was the supposition entertained by H. B. Lewis, M. S. Dunn, and E. A. Doisy. Alive, moreover, to the deficiency of[89] the older procedure in use for the determination of small amounts of uric acid, Lewis and his collaborators invoked the more accurate colorimetric method of Folin and Denis (as modified by Benedict and Hitchcock).
The experiments were conducted with great care, and with as complete control as possible of the variable factors concerned. The investigators realised that, if any significance was to be attached to fluctuations in uric acid excretion following the intake of proteins and their derivatives, it was essential that accurate information be obtained as to the extent of the variations to be expected normally in the subjects when fasting. “Controls,” therefore, in which no food was consumed throughout the experiments, were instituted at frequent intervals so as to make sure that the level of endogenous uric acid metabolism was not altered by the long-continued purin-free diet.[13]
Passing now to the results obtained, it was noted that, after the intake of three types of purin-free protein food (egg white, cottage cheese, and glidine), there ensued a rise in uric acid output, reaching its maximum during the third or fourth hour after their intake. No quantitative differences in the uric acid output after ingestion of these three types of protein were observed; in short, the findings did but confirm what had been repeatedly demonstrated, viz., that the excretion of the endogenous uric acid is increased by purin-free protein food.
But the further interesting fact emerged, viz., that glycocoll and alanine, end-products of protein digestion, also augmented uric acid excretion; moreover, this even more swiftly than proteins, the maximum being reached within two hours after their intake.
In addition, like results followed the ingestion of the dicarboxylic amino-acids (glutaminic and aspartic acids), the increase in endogenous uric acid excretion being even more pronounced than with glycocoll or alanine.
Now, it must be recalled that the amino-acids represent the end-products of protein digestion. Accordingly, Lewis and his co-workers argue that “since no digestive processes are required for the utilisation of amino-acids, it can hardly be considered that the rises in endogenous uric acid observed following the ingestion of four different amino-acids can be attributed to the work of the digestive glands.” The effect, they held, is more probably attributable to “a direct stimulation of the body cells by amino-acids or their katabolism products, a stimulation of nuclear metabolism,” for it is known that amino-acids disappear very swiftly from the blood-stream to be stored up temporarily in the tissues.
The question that now confronted the observers was whether the stimulation of nuclear metabolism was an inherent property of amino-acids. If so, “substituted amino-acids might be expected to exert a similar influence.” But, if on the contrary, it was due not to the amino-acids as such but “either to the cellular work of their katabolism or to the intermediary products of their breakdown, a substituted amino-acid which does not follow the normal path of amino-acid catabolism would in all probability be devoid of the power of stimulation.”
To this end, they selected sarcosine or methyl-glycocoll to elucidate the point at issue; this, inasmuch as it has been found to pass through the organism for the most part unchanged. The result justified their inference, for no perceptible influence on uric acid excretion was noted. Hence, on the basis of this experiment, they inferred that the stimulation of uric acid metabolism was not an inherent property of amino-acids; in other words, that if an amino-acid when ingested does not undergo disruptive katabolism, it is without effect on uric acid excretion.
Now deaminisation is the first stage in the katabolism of amino-acids, yielding as products ammonia and a-ketonic or hydroxy acids. The ammonia thus formed normally undergoes conversion into urea and is excreted as such. In order to ascertain whether the ammonia stimulated uric acid excretion, ammonium chloride was administered, but no rise in the uric acid output above the normal level ensued. Also, the ingestion of urea seemed to entail no appreciable increase in the uric acid elimination; in other words, these katabolic products of the nitrogenous moiety of the amino-acids are without effect. As to the non-nitrogenous intermediary products of the katabolism of amino-acids, i.e., the a-ketonic or hydroxy acids, it was impossible to investigate the influence of these on the endogenous uric acid elimination.[14]
Lusk also has brought forward evidence that in the presence of amino-acids cellular activities are intensified markedly. According to Taylor and Rose, too, not only nuclear katabolism, but also nuclear anabolism, may be accelerated by the presence of large amounts of amino-acids.
Lewis and his collaborators consider that the results of their researches militate against Mares’ hypothesis, viz., that the origin of the increased amounts of endogenous uric acid that follow the intake of purin-free protein stuffs is referable to intensified activity of the digestive glands.
They hold that “it can be accounted for equally well as the result of a general stimulation of all cellular metabolism by the products of digestion of proteins the amino-acids.”
The recorded increases in endogenous urinary purin are, they consider, far too great to be the outcome of the stimulation of so small a proportion of the cells of the body as those of the digestive tract. On the other hand, they do not deem it necessary to assume that the whole of the endogenous uric acid is the outcome of nuclear disruption, concurring with Burian’s view, that a moiety thereof may be derived from the hypoxanthine of muscular tissue.
The researches of Leathes and his collaborators permit the deduction that endogenous uric acid excretion bears a definite relation to the activity of cellular processes. Given unchanged physiological conditions, e.g., muscular exercise, the amount of the endogenous uric acid excreted is, for the same individual, fairly constant, and this irrespective of diet; but it is not the same for different individuals, even those of identical body weight.
According to MacLeod, the endogenous excretion in an adult man fluctuates between 0·12 and 0·20 per cent. purin nitrogen. The average daily endogenous uric acid output of a normal adult, as stated by Walker Hall, is about 0·5 gram, while that of a gouty individual is 0·45 gram.
Now Burian and Schur’s original contention was that, in a given individual on a purin-free diet, the endogenous purin output was constant, and this despite marked variations in the amount of the purin-free food digested.
Recent researches, however, of Folin and of Hopkins and Hope, indicate that this dictum must be modified to this extent, viz.,[92] that although it is true that the endogenous excretion continues remarkably constant, with moderate variations in the amount of purin-free food, it is not so in the presence of marked variations.
The subject (Hopkins and Hope), after a fast of six hours, was given a meal of bread and potatoes, and at every subsequent hour estimates were made of the amount of urea and uric acid excreted in the urine.
| Time. | Urea. Grams. |
Uric acid. Milligrams. |
Amount of urine. C.C. |
|---|---|---|---|
| 10-11 | 1·07 | 26 | 175 |
| 11-12 | 1·13 | 27 | 118 |
| 12-1 p.m. | 1·07 | 24 | 164 |
| 1-2 (meal). | 0·64 | 21 | 60 |
| 2-3 | 1·12 | 22 | 43 |
| 3-4 | 1·16 | 38 | 41 |
| 4-5 | 0·84 | 40 | 53 |
| 5-6 | 1·16 | 56 | 59 |
| 6-7 | 1·20 | 39 | 56 |
| 7-8 | 1·37 | 30 | 95 |
| 8-9 | 1·47 | 33 | 183 |
| 9-10 | 1·33 | 24 | 155 |
| 10-11 | 1·33 | 23 | 180 |
It is clear from the results obtained that a very definite increase of endogenous purin excretion ensued, and that the said increase occurred sooner as regards uric acid than urea. This bears out what Mares demonstrated many years ago, viz., that the greatest increase in uric acid excretion occurs in a few hours after a meal, whereas the increase in the case of urea comes more tardily, not reaching its maximum until some hours after.
Horbaczewski referred such increase in uric acid excretion to a digestive leucocytosis; in other words, that the uric acid was the outcome of destruction of the leucocytes, and consequent formation of purin from the released nucleic acid. Unfortunately for this theory, the period of most marked augmentation in uric acid excretion ensues when the leucocytes are most in evidence in the blood-stream, not after they have disappeared, as would be the case if uric acid was derived from the purin product of the nucleic acid liberated by leucocytic destruction. We have a parallel instance in the case of pneumonia, in which it has been shown that the elimination of uric acid and other purins is at its acme when the leucocytes are most abundant; in other words, the highest uric acid output coincides with the period of most marked leucocytosis, whereas during the post-critical stage, viz., when leucocytes are being destroyed in great numbers, the output of uric[93] acid is very markedly lowered. Discussing Horbaczewski’s theory in light of the above criticisms, MacLeod suggests, “that the facts appear to indicate that the purin substance is a metabolic product of the living leucocytes,” and not, so to speak, the chemical outcast of their disruption and death.
Lastly, Walker Hall, discussing endogenous uric acid excretion, emphasises the necessity of discriminating between the uric acid output and the total purin output. He reminds us that the actual cell nucleins belong chiefly to the group of amino-purins, i.e., guanine and adenine, and that the oxypurines, xanthine and hypoxanthine, are intermediate products on their way to excretion, another and more advanced intermediate product being uric acid. Now, only a proportion of these intermediary products appears in the urine, this commonly cited to be approximately 50 per cent.
But this, as Walker Hall states, must be taken only as a very broad estimate, for in the same individual the output varies with the number of conditions, not as yet fully determined. But the point most emphasised by him is, that though “the uric acid output varies considerably, the total purin output does not show similar variations; for when the uric acid excretion wanes that of the purin bases usually rises. As a consequence, the total purin output is more constant, less influenced by circumstances, than the output of uric acid.”
This being so, we shall now pass on to consider other conditions influencing endogenous uric acid excretion.
The output of endogenous uric acid excretion is influenced by (1) Physiological conditions, (2) Pathological states, and (3) The ingestion of certain drugs.
It is now recognised that the purin bases of the body exist not only in the bound form (nucleic acid), but also free, especially in muscular tissue. Also, that from such free purin bases uric acid can be readily formed as from those liberated by the disruption of nucleic acid. Thus, inosinic acid, a nucleotid first isolated from meat extract, yields phosphoric acid and the purin base, hypoxanthine. In possession of these facts, we shall be better able to appreciate the significance of the researches of Burian and others.
(a) Muscular Exercise.—According to Burian a large increase in the excretion of uric acid was found to follow muscular exercise. The same observer also noted the presence of hypoxanthine in[94] defibrinated blood after its perfusion through the hind legs of a dog whose muscles had been thrown into tetanus. Moreover, subsequent to contraction, the muscles themselves contained an increased amount of oxypurine. From these findings Burian concluded that hypoxanthine was a product of muscular action, and that this substance or its precursor, inosinic acid, was an important source of endogenous uric acid. The uric acid thus formed by oxidation was then partly destroyed in the liver and partly excreted by the kidneys. But Burian noted also during activity of the muscles that a certain amount of the purin bases failed of oxidation, and consequently a larger amount of the same, as compared with uric acid, passed into the circulation.
Kennaway, discussing the effect of muscular exercise on the excretion of endogenous purins, noted that during unaccustomed exercise the uric acid output of the kidneys diminished, but that of the purin bases is relatively augmented, but, on the whole, he found that the total purin output (bases plus uric acid) was not very much increased.
Leathes and others, investigating the effects on uric acid excretion of strenuous exercise, established the occurrence of a distinct increase. Given that the same kind of exercise is practised on the day following, the said increase is much less marked. If, however, some different form of muscular activity is undertaken, another increase in uric acid follows. It would appear, therefore, that, despite conflicting evidence, the balance of opinion favours the view that muscular activity does lead to increase in endogenous uric acid excretion.
(b) Periodic Variations.—Leathes noted diurnal and nocturnal variations in the excretion of endogenous uric acid, the maximum occurring within the early waking hours, and sinking to a minimum towards the evening. His experiments, he held, indicated a variation in the actual formation of endogenous uric acid at different periods of the day. Rockwood also found that an increase occurred during the daytime, and Pfeil, that there was a morning rise in the amount of uric acid passed. The fact that doubt still obtains as to whether muscular exercise has any effect on endogenous uric acid excretion, renders explanation of this diurnal variation difficult. This especially as there are no fluctuations in the urinary functions that could in any way account for it.
Endogenous uric acid is increased under certain pathological conditions. Leathes’ recent work confirmed the view that there is an increased production of nitrogenous waste in fevers. After taking a large dose of anti-typhoid serum his temperature rose to 103° F. Experimenting on himself, he found his output of urea, uric acid, and creatinine all increased, but of all[95] three uric acid showed the most marked alteration. The question now arises as to whether such is due to increased production or diminished destruction. Some further experiments conducted by Leathes on himself may serve to elucidate this point. Subjecting himself for a prolonged period to cold baths, a similar increase in his uric acid output ensued. This would appear to indicate that, through increased loss of heat, the bodily processes of combustion were augmented to maintain the body temperature, with, as a consequence, increased uric acid excretion.
In leukæmia protein-destroying forces are at work, and the urine contains large quantities of uric acid. The same is attributed to the formation and destruction of enormous numbers of leucocytes, but the urinary findings in this respect have been extremely variable. While increased uric acid elimination has been vouched for by many authors, some have noted increase in the purin bases, sometimes with, and sometimes without increase in the uric acid; while others again have even noted a decrease in uric acid and phosphoric acid excretion.
Apart from these contradictory findings, it would appear, according to Magnus-Levy, that in acute leukæmias the relation between the number of leucocytes and the uric acid output is most variable. Lastly, the different types of leukæmia present differences in regard of their uric acid output, the increase in the myelogenous variety being much more marked than in the lymphatic form.
Wells, discussing these conflicting data, considers that they are but the reflex of the “known fluctuations in the course of the pathological processes of leukæmia; the number of leucocytes, the size of the lymphatic organs, and the general condition of the patient all vary greatly from time to time, often with remarkable rapidity and the excretion of products of metabolic activity must vary likewise.” Continuing, he observes that the enormous increase in the amount of lymphoid tissue in the body and blood must give rise to a greatly augmented nuclein katabolism, with sequential appearance of uric acid, purin bases, and phosphoric acid in the urine. This he holds to be well demonstrated by the increased elimination of uric acid and purin bases, together with a general increase in the nitrogen output such as has been frequently noted in sequence to the therapeutic use of X-rays in leukæmia, this attributable to the increased autolysis known to be induced by X-rays.
As to this question of the relationship of leucocytosis to uric acid excretion, it must be borne in mind that the number of leucocytes and the excretion of uric acid do not always vary directly. Parallel studies of the blood and urine have shown that leucocytosis does[96] not invariably accompany increased uric acid excretion. Indeed, Hutchison and MacLeod have recorded cases of leucopenia without any reduction in the amount of uric acid eliminated.
Also, we have to recall that on a purin-free diet the amount of endogenous uric acid is more than can come from nuclein destruction in the body. As suggested by Burian, some may be derived from the hypoxanthine in muscular tissue. In short, while nuclein disintegration is the outstanding source of endogenous purin, yet, for the reason cited, it cannot be regarded as the sole source, for the exact origin of all the endogenous purin is not as yet established.
In conclusion, it would appear that some drugs influence more or less markedly the excretion of endogenous uric acid, notably, atophan; but discussion of these will, we think, be best postponed to the section dealing with the medicinal treatment of gout. Meanwhile we shall proceed to consider the vexed question of the formation within the organism of uric acid by synthesis.
Birds eliminate most of their nitrogen in the form of uric acid, and, undoubtedly, in their instance synthetic formation of uric acid in the liver takes place on a large scale. Thus, when blood containing ammonium lactate is perfused through the liver of the goose, an increase in the uric acid content of the blood occurs. Also the ingestion of lactic, pyruvic and other organic acids leads to augmented output of uric acid; in short, it is generally agreed that in birds synthesis is the chief mode of formation of uric acid, homologous with the formation of urea in the liver of mammals.
If this be true of birds, on the other hand, splitting and oxidation of nucleins is in mammals the most important source of uric acid, but there is evidence that it cannot all be accounted for in this way. As before remarked, the old belief that purin excretion remains almost constant on a purin-free diet, despite great variations in the amount of the ingests, is not strictly true. Thus, using swifter and more reliable methods for the estimation of nitrogenous metabolites, Folin noted, on an absolutely purin-free diet, that an increase in purin excretion ensued, given marked variations in the intake of food. Again, the Dalmatian dog, as we have seen, excretes uric acid in his urine. S. R. Benedict was therefore able to demonstrate that a very distinct increase in his uric acid output ensued in sequence to increase in the amount of his non-purin food; moreover, that even when such non-purin foods were continued for a year, “the total amount of uric acid excreted was at least ten times greater than could have come from the traces unavoidably included in the food” (MacLeod).
Also Ascoli and Izar, experimenting with dog livers, noted on incubation thereof and passage through the same of oxygen that the uric acid disappeared; but on the substitution of carbon dioxide an accumulation thereof ensued. Wells, however, was unable to confirm this re-synthesis of uric acid by dog livers, and Spiers also failed to corroborate their findings.
On the other hand, there is evidence pointing to the fact that a certain small percentage of synthetic formation does take place in the organism. Thus certain chemical substances, and these not purin, do cause an appreciable though slight increase in the purin excretion of mammals, and a very marked augmentation of the same in birds, viz., lactic, tartronic and B-oxybutyric acids.
But, as MacLeod, discussing these experimental and clinical findings, observes, there are to hand even more direct proofs that purin synthesis occurs in mammals. Thus, as McCallum has pointed out, we cannot escape the admission that young mammals are able to synthetise the purins essential for their growth, and this from food containing no purin, e.g., milk. Again, prior to incubation, a hen’s egg contains practically no nucleic acid, whereas after development its content in the same increases by great strides. The eggs of insects, too, with the progress of development, amass purin very rapidly.
Again, Miescher noted long since that salmon, on leaving the sea to ascend rivers for the object of spawning, have at that time well-developed muscles; but on arriving at the upper reaches, marked muscular wasting ensues, while the testes undergo enormous enlargement. MacLeod, reflecting on these observations, argues that, “as the fish takes no food during the migration, there must be conversion of the protein of the muscles into the cellular tissue of the sexual glands, and nucleic acid must be produced.” MacLeod’s conclusion is that “Purin synthesis undoubtedly occurs in the mammalian body, but it is difficult to recognise in metabolism investigation, because it is a slow continuous process ... whether or not changes in the activity of purin synthesis occur in conditions of disease, is a question which awaits investigation.” Lastly, the opinion of most authorities is that, while they concede the possibility of synthetic formation, the amount of uric acid produced in this manner is negligible, and that by far the most important mode of formation in mammals is by the splitting and oxidation of nucleins; in other words, that uric acid in the main is derived from the amino-purins by deaminisation and subsequent oxidation, and from the oxy-purins directly by oxidation.
The chemical structure and sources of uric acid having been dealt with, we are now in a position to resume our narrative, and to take up the thread at the point when Horbaczewski revealed the derivation of uric acid from nucleic acid. It now devolves upon us to scrutinise more narrowly the process by which the formation of uric acid from nucleic acid is achieved. Incidentally, it will not be unprofitable to note, if only briefly, the steps by which the necessary expansion of our chemical and physiological knowledge of nucleic acids has been acquired.
As may be imagined, the primary difficulty was to prepare nucleic acids of such purity as admitted of their elementary chemical analysis. The necessary researches were to a large extent confined to two types of nucleic acid, one derived from yeast, and the other from the thymus gland; in other words, to representatives of the only two nucleic acids in nature, one derived from the nuclei of animal cells, the other from the nuclei of vegetable cells.
A feature common to nucleic acids of animal and vegetable origin is that, on hydrolysis with boiling mineral acid, they yield two purin derivatives, guanine and adenine, and a pyrimidin derivative, cytosine. From thence as regards their remaining constituent elements they display distinctions. Thus animal nucleic acids yield thymine, and contain a hexose group in their molecule. On the other hand, vegetable nucleic acids give forth uracil and possess a hexose group.
To sum up, nucleic acid is a chemical complex, made up of phosphoric acid with purin bases, pyrimidin bases and carbohydrate radicles. Moreover, nucleic acids, whatever their source, show a striking similarity in structure, containing always two amino-purins (adenine and guanine), two pyrimidines (either cytosine and uracil, or cytosine and thymine), and a carbohydrate. Now, while purin bases are always present, yet, in respect of their carbohydrate group, nucleic acids display variations; this, according as they are of animal or vegetable origin. If the former, the carbohydrate group is a hexose (contains six carbon atoms) with thymine. If the latter, it contains pentose (five carbon atoms) with uracil.
The constancy in the content of the various nucleic acids is such that Levene and Jacobs have felt justified in putting forward the following provisional formula as to the constitution of a nucleic acid of animal origin.
Structural Formula of Nucleic Acid
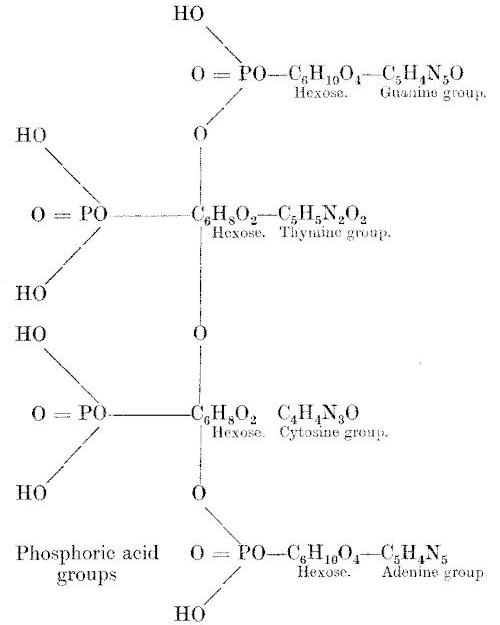
The enzymes responsible for the disruption of the nucleic acid complex are not to be found in all the body tissues. Moreover, the distribution of the enzymes in the various organs and tissues varies in different species of animals. Of the various organs the liver, spleen, thymus, and pancreas more particularly contain enzymes in abundance. As to their varied location in different animals, it may be noted that the enzyme responsible for the oxidation of xanthine into uric acid, viz., xanthine-oxidase, is found in man only in the liver. In other animals, also, it is of localised distribution, being as a rule only found in the liver or in the liver[100] and kidney. The dog, however, appears to be an exception, xanthine-oxidase being found in a variety of its tissues.
Adenase, the deaminising enzyme, is not to be found in any organs in man. Neither does it exist in any of the tissues of the rat. Consequently, if adenine be injected subcutaneously in rats, it undergoes oxidation, without abstraction of its amino group.
On the other hand, guanase, also a deaminising enzyme, is in man to be detected in the kidney, lung, and liver, but not in the pancreas or spleen. In the pig, however, guanase is lacking, and its absence no doubt explains why deposits of guanine may occur in the muscles constituting the so-called guanine gout met with in swine. It is worthy of note also that in pigs’ urine the content of purin bases exceeds that of uric acid.
To sum up, in man the enzyme, xanthine-oxidase, which forms uric acid from xanthine, is located chiefly or exclusively in the liver. This, of course, represents the final stage of purin metabolism, but the antecedent chemical processes involved in the disruption of nucleic acids are initiated by the action of enzymes in the intestinal juices and wall, and to a consideration seriatim of these changes we now proceed.
As might be expected from the complex structure of the nucleic acid molecule, a number of ferments are concerned in its disruption. The gastric and pancreatic juices contain not a trace of any enzymes. Thus, when nucleo-protein is subjected to the gastric juice a moiety of protein is readily split off and hydrolysed to peptone and other products of proteolysis.
But the nuclein element remains unacted upon until it comes under the action of the pancreatic juice. Hydrolysis then ensues, and the ingested nuclein is broken down into nucleic acid and protein. The nucleic acid remains unaffected by the pancreatic juice, but, coming in contact with the succus entericus, it undergoes partial decomposition through the action of a ferment called nuclease or nucleic-acidase. Under its disruptive effect the nucleic acids or poly-nucleotides are further split up into groups known as nucleotides. The two pyrimidine nucleotides split off and undergo no further change. But, through the action of another ferment, nucleotidase, the purin nucleotides are further decomposed to yield nucleosides (substances of the glucoside class made up of a combination of a purin base with a carbohydrate group of the nucleic acid with which also phosphoric acid is linked).
No further stage in hydrolysis of nucleic acid occurs in the intestine, but the nucleosides are again in turn split up after reaching the tissues, particularly in the spleen, liver, and thymus. This,[101] under the action of specific enzymes, nucleosidases, which succeed in breaking the nucleosides down into the so-called “building stones” of the nucleic acid molecule, phosphoric acid group, carbohydrate group, pyrimidine and purin bases, especially adenine and guanine. The adenine and guanine thus formed are, by the action of the ferments adenase and guanase, converted and, by the removal of their amino group, transformed, adenine into hypoxanthine, and guanine into xanthine, thus:—
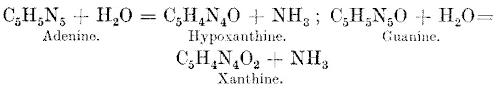
By the action of oxidases also present in the tissues hypoxanthine is changed into xanthine and xanthine into uric acid (trioxy-purine), this by a specific ferment xanthine oxidase.
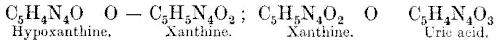
Scheme Illustrating the Probable Stages in the Passage of Purin through the Body (Walker Hall)
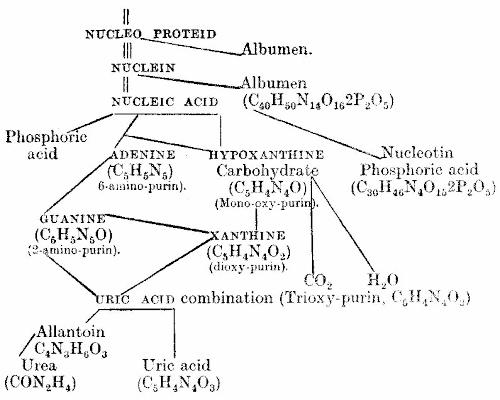
It will be seen that the disintegration of nucleic acid involves many stages, and its complexity is such that we make no apology for drawing upon the masterly monograph of Walter Jones for[102] further elucidation of this intricate question. In relating the history of nucleic acid in the animal body Jones has found it convenient to introduce certain terms wherewith to designate the various elements of the nucleic acid molecule. Thus, the molecule in its entirety is termed a tetra-nucleotide. The cleavage of this complex is initiated by the action of two specific enzymes. Through their agency the tetra-nucleotide is first cloven into two di-nucleotides, which immediately divide up into four mono-nucleotides. These ferments are:—
(1) Phospho-nuclease (which splits off the phosphoric acid radicle, leaving a nucleoside, guanosine or adenosine).
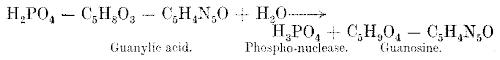
(2) Purin-nuclease (which splits off the purin radicle, viz., separates out both phosphoric acid and carbohydrate groups, leaving free purin bases).
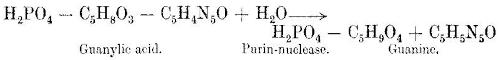
Now, in sequence to either of the foregoing cleavages by the phospho- or purin-nucleases another set of enzymes come into the field. Under their deaminising effect the amino group is abstracted, with the formation of either free oxy-purins or oxy-purins still bound in glucoside-like combination with sugar.
If the oxy-purins are free, the following is the reaction:—

Should, however, the guanine glucoside be present:—
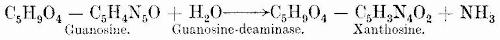
In the latter instance a hydrolysing enzyme, xanthosine-hydrolase, by its action, splits off xanthine. We see, therefore, that by either route the end-product is the same. Following a like series of changes, the adenine radicle is transmuted into hypoxanthine. This either directly by the action of adenase:—
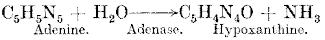
or indirectly through the agency of adenosine-deaminase, the hypoxanthine-glucoside (inosine) is formed, and subsequently the hypoxanthine is split off.
Xanthine and hypoxanthine are, therefore, now to hand, and given the presence of oxygen, their oxidation to uric acid ensues:—
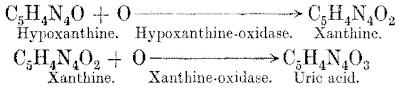
Now, in man and the anthropoid apes, uric acid is the end-product of purin catabolism. In contrast therewith in most mammals only a minimal amount of the exogenous or endogenous purins escapes in the urine as uric acid. Most of it undergoes further oxidation into allantoin,[15] this change taking place in most mammals chiefly in the liver. According to Schittenhelm, if nucleic acid be given to dogs, pigs or rabbits, from 93-95 per cent. thereof appears in the urine as allantoin, and only 3-6 per cent. as uric acid, and 1-2 per cent. as purin bases.
Disruption of Nucleic Acid Molecule (Amberg and Jones).
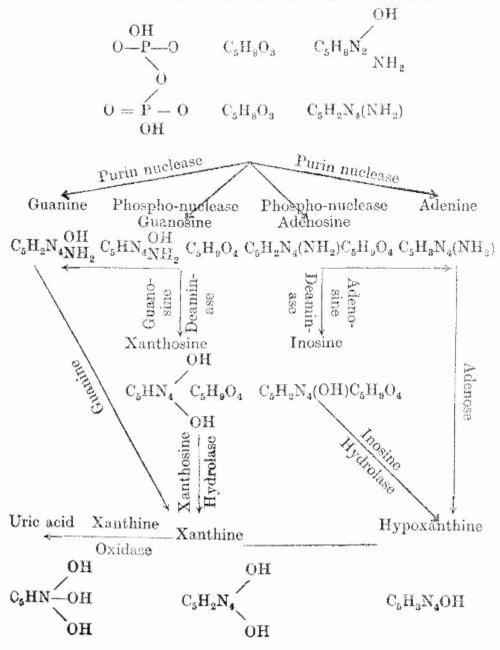
In man, as in most mammals, uric acid is formed chiefly in the liver from purins, and in the preceding table Amberg and Walter Jones schematically represent the various steps by which disruption of the nucleic acid molecule is attained, and uric acid formed.
Uricolysis, or the destruction of uric acid, is, in most mammals, achieved through the agency of the oxidising enzyme uricase, which oxidises uric acid to allantoin. Consequently, in their instance, purin bases, ingested as such or set free in the tissues, appear in the urine, not as uric acid, but in the form of allantoin. On the other hand, both in man and in the anthropoid apes, this particular enzyme uricase is absent. In accordance therewith, only a trace of allantoin is to be found in the urine of man and the higher apes, while in the lower animals, e.g., dogs, pigs, and rabbits, a large proportion of the purin excretion assumes this form.
Now, the absence of uricase, in man, is held to be proved by the fact established by Wiechowski and others, viz., that uric acid, if injected subcutaneously, may be almost wholly recovered in the urine, and moreover, unchanged. On the other hand, the total excretion of uric acid and the other purin bodies by no means tallies exactly with the amount of the uric acid ingested as purin bases in the food and that produced from the tissues; in other words, it has been found that, when given by the mouth, nucleic acid or purins are by no means quantitatively excreted in the urine, even though not only uric acid, but also allantoin and the purin bases, are included within the estimate. According to most experiments, a considerable proportion of the purin-nitrogen intake, about 50 per cent., is excreted as urea.
The question then arises as to what becomes of that moiety of the food purins which fails to appear in the urine as uric acid. Now the amount of allantoin that appears in the urine is negligible. Moreover, Ackroyd, having shown that the organism cannot destroy allantoin, it is possible that the minimal amounts excreted thereof in the urine are all derived from the food.
Accordingly, if, as experimental feeding with purins or nucleic acid appears to indicate, purins are destroyed in the body they[105] “pass through some other route than allantoin, and possibly, that part of the purin which is destroyed does not pass through the stage of uric acid.” Such is Wells’ opinion, and he reminds us that in vitro the destruction of uric acid can be attained by other routes than through allantoin. Thus, it can be broken down into glycocoll, ammonia, and CO₂, or by another method of disintegration it furnishes first alloxan (C₄H₂N₂O₄), then parabanic acid (C₃H₂N₂O₃), which in turn yields oxalic acid and urea.
But while it is probable that there is more than one way in which uric acid can be decomposed in the body, nevertheless there is, according to Wells, no evidence that either of the alternative routes above suggested is ever affected in the animal body. In this impasse Siven suggests the further possibility, viz., that the moiety of the food-purins which fail of recovery from the urine undergo partial destruction in the intestine by bacteria.
Stewart, however, in his “Physiology,” discussing uricolysis, maintains that a considerable destruction of uric acid and other purin bodies goes on in the body and mainly in the liver. He reminds us that when uric acid is heated in a sealed tube with strong hydrochloric acid, it breaks down into glycin, carbon-dioxide and ammonia, and he maintains that “there are grounds for believing that a similar decomposition takes place in the body, and that the products are then transformed into urea in the liver”; this, through the agency of a special ferment called the uricolytic enzyme.
Also, Flack and Hill, discussing the metabolism of nuclein, hold that some of the uric acid thus formed may be transmuted into urea by an uricolytic ferment present in the liver, muscles, and kidneys. This same agent they consider “probably destroys a considerable amount of the uric acid formed in the body. Indeed, uric acid, even when given in the food, owing to the presence of this enzyme, causes no increase in the uric acid output of the body.”
On the other hand, Wells, discussing the destruction of uric acid, observes that repeated investigations show “that the tissues of man have no power whatever to destroy uric acid in vitro; the earlier reports of positive uricolysis undoubtedly being erroneous.” His final conclusion, after weighing all available evidence, is that it is highly probable that in man “most of the purin absorbed from the food, and practically all the purin from cell metabolism, is converted into uric acid and excreted as such.” MacLeod, however, reflecting on the fact that uric acid is not destroyed when extracts of the organs are incubated at body temperature with uric acid or its precursors, bids us bear in mind that, “although the uric acid is thus shown not to[106] be destroyed in vitro, it may nevertheless be destroyed in the living animal.”
We see, therefore, that the question, Whether uric acid can undergo destruction in the human body? is still a matter of dispute, and must, pending further investigation, remain sub judice. Still, despite the conflict of evidence, clinicians have felt justified in assuming that one of the factors in the genesis of gout may be an entire absence or a diminution in the amount or activity of this uricolytic ferment.
But the awkward fact remains that all researches up to date have failed to establish the presence in the human body of any enzyme which can decompose uric acid. Should, therefore, future investigators place beyond the reach of cavil the claim that no uric-acid-destroying enzyme exists in the body, it would seem that, ipso facto, man, through lack of this capacity for rapid oxidation of uric acid, is, by this same disability, rendered a potential victim of uric acid retention and deposition.
Elucidation of this vexed point seems more probable in view of the striking discovery recently made by R. Benedict, viz., that in one particular breed of dog, the Dalmatian, uricase is wholly absent. In respect of this lack of a uric-acid-destroying ferment, the Dalmatian breed of dog has a purin metabolism apparently identical with that of man.[16] Thus, if fed on a purin-free diet, he passes large quantities of uric acid, and if the latter be injected subcutaneously, elimination in quantity as such ensues; this, in striking contrast to what obtains in all other animals in whom, as before noted, uric acid is mostly oxidised to allantoin before excretion. Now, as MacLeod observes, investigation into the metabolism of nucleic acid has, in man, been hampered greatly, in that the absence of uricase from his tissues, prior to Benedict’s discovery, rendered experimental researches on the lower animals valueless. But, in light of the above revelation later by R. Benedict, it may reasonably be hoped that in the near future our knowledge as to the location and nature of the intermediary chemical processes occurring in the metabolism of nucleic acids may be materially clarified.
It will be recalled that at the close of our chapter on Pathogenesis we referred to the growing scepticism of Garrod’s views as to the pathogeny of gout. Still, if we except Edward Liveing’s pertinent observation that uricæmia was not peculiar to gout, naught, save alternative hypotheses, unsupported by pathological data, was advanced. Consequently, Garrod’s facts never being seriously called in question, his position remained unassailable, until, in the year 1898, his original observations as to the lowered alkalinity of the blood in acute gout, and the increased uric acid content thereof during the same, were definitely contradicted by Magnus Levy.
Working with more modern and more reliable methods of technique, this observer, in a series of seventeen cases of acute gout, found no evidence of any lessening in alkalinity of the blood or of any augmentation of its uric acid content as compared with the inter-paroxysmal period.
Again, as to Garrod’s claim that there was a diminished excretion of uric acid during the attack, this also, while supported by Minkowski, was called in question by Pfeiffer, Levy, and Badt, who found the reverse to be the case, i.e., a notable increase in the excretion of uric acid during the paroxysm.
These results were again in 1900 confirmed by Chalmers Watson. An exhaustive study of a series of cases of acute gouty polyarthritis convinced him that:—
(1) The alkalinity of the blood is not diminished during the attack.
(2) The excretion of uric acid is not lessened during the paroxysm, but the reverse; there is, therefore, no ground for the supposition that there is a temporary diminution in the capacity of the kidneys to excrete uric acid.
(3) The amount of the uric acid in the blood is not greater during the attack than in the intervening period, and if these points be accepted, we must start de novo in search of the cause of the acute paroxysm.
The iconoclastic revelations of the foregoing researches may[108] well form a preface to our discussion of gout from the triple aspect of:—
The earlier investigations as to the behaviour of uric acid in the organism were necessarily restricted to the noting of any variations in the uric acid output in the urine. That the findings and, alike, the deductions proved bewilderingly contradictory is not to be marvelled at when we recall the many factors that govern the amount of uric acid excreted in the urine.
How fallacious, it now transpires, were the assumptions based upon the mere uric acid output in the urine, and how little understood even to-day the many conditions that determine its variations.[17] But, fortunately, we can now to some extent control and review our urinary findings in light of the uric acid content of the blood. But we anticipate, and meanwhile let us confine our discussion to the variations in uric acid excretion that occur in gout, and this as revealed by more modern students of the disease. This will be more conveniently dealt with if we consider first the oscillations in uric acid output in relation to acute attacks of the disorder, and subsequently the same as met with in its more chronic manifestations.
Generally speaking, there appears to be a consensus of opinion on the following points:—
(1) That in the intervals between acute attacks of gout the elimination of uric acid lies within the normal limits, but that
(2) For one or two days prior to an acute attack an appreciable decline in the output of uric acid occurs. This, however, is not so marked as the subsequent
(3) Increased output of uric acid during the acute attack. According to Magnus Levy the increase may reach from 0·3-0·5 gram, daily, and more, and may sometimes last for a week or even two.
(4) Following attack a tardy decline in uric acid output to former level.
To sum up, during an attack of acute gout the uric acid output stands at a relatively low level between the paroxysms. But one or two days before the oncoming attack a diminution in uric acid output ensues. In contrast with the outbreak of the attack, the uric acid excretion increases markedly, this enduring for a week or more, when the output again declines. The augmented output during the paroxysm is more constant than the diminished excretion antecedent thereto. Now, while it may be taken that the foregoing variations in uric acid output, prior, during, and subsequent to, acute attacks, obtain as a general rule, such behaviour is not invariable; for, unfortunately, as Wells reminds us, instances are met with in which “the uric acid excretion shows no variation from that of normal persons.”
It must never be forgotten that the elimination of uric acid displays wide variations, this even when the subject under investigation is on a constant diet. Consequently, as Folin has pointed out, “even in the case of gout, which is distinctly associated with uric acid, it is an extremely difficult matter to prove by means of urine analyses that the uric acid elimination is not entirely normal.” And he adds, “If it had not been for the fact that uric acid, because of its insolubility, is so easily found in the joints, it would unquestionably have been a very long time before any definite relationship between uric acid and gout could have been established.”
None can gainsay the truth of these reflections, for, when placed on a fixed diet, the uric acid output in the victims of chronic gout differs but little from that of normal individuals on a similar regime; save in this respect, that, following the intake of purin-containing substances, the period of augmented uric acid excretion that ensues is prolonged as compared with the normal.
In 1901 Vogt showed that in gout the excretion of exogenous purins was not only delayed but diminished. Giving simultaneously to a gouty subject and a healthy individual a diet rich in purins, he found that, in the former, retention and delayed[110] excretion of purins ensued. Vogt’s findings were confirmed by Reach, Soetbeer, Pollak, Mallory, and others.
Brugsch and Schittenhelm also observed that, following the intake of purin-containing substances, the exogenous uric acid excretion was retarded and reduced; in other words, the percentage of exogenous nitrogen excreted as uric acid nitrogen is less than in normal individuals, although the increased elimination extends over a longer period of time.
On the other hand, Walker Hall finds that, though there is retardation, there is no diminution in the output in gouty subjects. Thus he states: “When an adult takes a meal consisting of half a pound of beef and a quarter of a pound of sweetbread, containing about 0·620 gram purins, the moiety which usually occurs in the urine, say 0·300 gram, is not fully excreted until 6-10 hours have elapsed. When a similar meal is taken by a gouty individual the full 0·300 gram is eliminated, but the rate of output is delayed, some 48-72 hours being necessary.”
The same observer states that, given intravenous injection of acid into a normal man, its elimination is spread over several days, and the total amount injected fails to appear in the urine. But if the injection be administered during a course of atophan, then the uric acid excretion is completed within twenty-four hours, and the whole amount injected can be recovered from the urine. Now if in a gouty subject the same method of procedure be adopted, the sequence of events is precisely similar, and like results have been reported, following the administration of sodium salicylate to vegetarians of five or more years’ standing. To sum up, the above findings would appear to indicate that:—
(1) A gouty subject can excrete exogenous purins as adequately as a normal man, but he takes longer to do so.
(2) If the extra purins be taken during a course of atophan, even this departure from normal is obliterated, i.e., the customary delay in excretion is obviated.[18]
But, unfortunately for the diagnostic valency of this symptom[111] in gout, viz., retarded exogenous purin output, it has not been found to be invariable. Thus Magnus Levy has shown that, in some instances of gout, the elimination of exogenous purin is neither reduced nor protracted. Pratt, too, has confirmed this observer’s findings, while, as we shall see later, this authority, also McClure, Mallory, and others, have placed on record the still more disconcerting fact, viz., that a diminished and retarded output of exogenous purin is not peculiar to gout.
The inference then would appear to be that:—
(1) Reduction and retardation of the excretion of exogenous purin, though common in gout, is not invariable.
(2) The same is not peculiar to gout, but occurs in other disorders.
(3) Its diagnostic valency, as a characteristic feature of gout, is correspondingly depreciated.
As a rule, gouty subjects, on a purin-free diet, excrete less endogenous uric acid than normal persons. Thus, according to Walker Hall, the average daily endogenous urinary uric acid output of a normal adult is about 0·5 gramme, while that of a gouty subject is about 0·45 gramme. Brugsch and Schittenhelm hold that in about 80 per cent. of cases the average endogenous excretion is lower than normal.[19]
According to these same observers, “the maximum fluctuation during attack-free periods was at first believed to be less than in the normal cases; more recent examinations, however, have shown that in the same case of gout there may be periods of high, and periods of low, endogenous uric acid excretion.” These variations, they hold, are not to be accounted for by either mild or severe attacks of gout, for they occur in the attack-free period.
Again Laird, investigating the elimination of endogenous uric acid in a case of chronic gout, noted that the output thereof was sub-normal, and, as Brugsch and Schittenhelm observed, the same presented marked variations. The leucocyte counts he found normal, but the phosphorus output and the acidity were sub-normal. Bloch again, while he agrees that endogenous purin excretion is usually below the average in gouty subjects, found that the output thereof is at its minimum before an acute attack of gout.
The foregoing observations would suggest that the retention[112] or delayed excretion of uric acid applies both to exogenous and endogenous purins. But, when we come to analyse the foregoing findings as to the variations in uric acid output, both in acute and chronic gout, one feels inclined to agree with O. Folin, “that the clinically useful contributions obtained by urine analysis have not been very numerous.” Thus we cannot, on the basis of the variations in uric acid excretion, presume to diagnose gout; in other words, if we take urine analysis alone, it is extremely difficult to prove that the uric acid elimination in gout is really and truly abnormal. Our uncertainty, moreover, is the more pronounced when we realise that in some cases of rheumatoid arthritis, etc., there is a disturbance of purin metabolism which in some of its features is reminiscent of that obtaining in typical gout. But, before proceeding to discuss this interesting resemblance, it will, we think, be convenient here to recall that the obliquities in metabolism found in gout are not wholly restricted to uric acid.
As Levene and Kristeller have shown, side by side with the delayed excretion of ingested purins, there occurs also a tardy elimination of the other nitrogenous products of protein food. Vogt observed that fluctuations in nitrogen retention and nitrogen loss are quite typical of gouty subjects. As to the why and wherefore, however, of this variability, it remains a mystery. Nor do we know the form in which the nitrogen is retained, though Vogt maintains that the uneliminated moiety takes the form of purin bodies. According to Brugsch, it is during the acute attacks of gout that the nitrogen loss reaches its zenith, and he suggests that the nitrogen retention in the inter-paroxysmal periods is in part compensatory. On the other hand, the gain in weight that ensues is not adequate to account for the sum total of the nitrogen retention; while, as before observed, in gout there occurs, not only retarded elimination of exogenous purins, but also of other nitrogenous products of protein food. Yet, according to Heffter, the ratio of purin bases to uric acid is unaltered in the urine of gouty subjects.
Again, all nucleins contain a phosphoric acid group, and Futcher found that the curve of the uric acid output ran in a striking parallel with that of phosphoric acid. But the attempts of subsequent investigators to show that the two end-products of nuclein disintegration—uric acid and phosphoric acid—go hand-in-hand prove contradictory. Hence Wells, in regard to phosphoric elimination, observes that, “it seems probable that it shows no characteristic alterations in gout.” Lastly, we will[113] recall to the reader that in the chapter on protein metabolism it was pointed out that the amino-acids, especially glycocoll, are found in excess in “gouty” urines.
In conclusion, it must, we fear, be admitted that the results of urinary analyses have proved insufficient of themselves to unravel the intricacies of metabolism in gout, and, after a brief digression, we shall proceed to ascertain whether, on the other hand, chemical analysis of the blood by modern methods can in any way shed further light on this obscure problem.
Working at the Research Hospital for the Study of Special Diseases at Cambridge, Strangeways (1910) commented on the striking resemblance that obtained between certain cases of so-called rheumatoid arthritis and gout, as evidenced by X-ray findings and section of the joints. Their similitude in these respects suggested that the nature of the apparent kinship of the two disorders might be elucidated by a study of purin metabolism in instances of rheumatoid arthritis.
To this end Ackroyd studied the purin metabolism in eleven persons, the victims of rheumatoid arthritis. His conclusion was that there was no important variation from the normal. To quote his own words, he states that “it may be (1) completely normal, or (2) while normal as regards endogenous excretion, the period of increased uric acid excretion which follows the administration of hypoxanthine may be prolonged for more than four days. It is more likely that this effect is individual, than that it is characteristic of any particular form of the disease, excepting those cases in which the prolongation is accompanied by active manifestation of the disease.”
W. J. Mallory, critically analysing Ackroyd’s cases, points out that he used only hypoxanthine in his studies; also that, while hypoxanthine has this advantage, that it is of definite and known chemical composition, furnishing a known quantity of basic nitrogen, it labours under this drawback: “It is by simple oxidation converted into uric acid, and probably calls into action only a limited part of the ferment system concerned in the formation of uric acid.” As a consequence, therefore, the amount of information on metabolism that can be gleaned through its usage is more restricted than if nucleinic acid were invoked in its place; for this substance, on the other hand, calls into action all the various enzymes concerned in the disruption of nuclein or nucleic acid.
Alive to these advantages, Mallory, in addition to hypoxanthine,[114] used nucleinic acid in his investigations of purin metabolism in a series of eight “undoubted cases of so-called rheumatoid arthritis.” The value of the inclusion of nucleinic acid is revealed by the fact that some of the cases, when given exogenous purin in the form of hypoxanthine, showed no deviation from the normal. On the other hand, when given nucleinic acid, a prolongation of the period of increased uric acid excretion ensued; this even though the total amount of basic nitrogen in nucleinic acid is less than in hypoxanthine. Thus 4 grams of nucleinic acid have 0·2632 gram of basic nitrogen, while 0·75 gram hypoxanthine has 0·309 gram of basic nitrogen.
Apart from his own series of cases, Mallory analysed those of other observers, and his conclusions are as follows: “Of nineteen cases of rheumatoid arthritis in which the purin metabolism has been studied by three different observers, nine cases, or 47·3 per cent., show a marked variation from the normal in their reaction to purin-containing substances while they are on a purin-free diet.
“In these cases the period of increased uric acid excretion which follows the administration of purin-containing substances is much prolonged. Following the administration of purin-containing substances, a considerable number of cases suffer from attacks of sub-acute arthritis, accompanied in some cases by an increased uric acid excretion.”
It will be seen that in virtue of:—
(1) The prolongation of the period of exogenous uric acid excretion, and
(2) Increased uric acid excretion during attacks of sub-acute arthritis,
certain cases of rheumatoid arthritis manifest a certain resemblance to gout, though, as Mallory remarks, “other features characteristic of that disease are lacking.”
It may be observed that the attacks of sub-acute arthritis that ensued in rheumatoid subjects followed the administration of hypoxanthine, as shown in Ackroyd’s series. That this reaction to exogenous purin is suggestive of a relationship between rheumatoid arthritis and gout derives colour from the fact that it has been repeatedly induced in gouty subjects by the same means. Thus, Brugsch and Mallory (1910), after giving 0·5 gram of hypoxanthine to a gouty patient, noted a typical outbreak of gout. Again, Brugsch and Schittenhelm, in the same year, reported attacks of arthritis following the administration of nucleinic acid to gouty subjects.
Another feature worthy of note is that, in the cases of rheumatoid arthritis investigated by Ackroyd and Mallory, the percentage of[115] exogenous purin nitrogen excreted as uric acid nitrogen largely exceeds that observed in any case of gout available for comparison by these authors.
Mallory’s final conclusions were that “there seemed to be sufficient data to show that, in certain cases of so-called rheumatoid arthritis, the purin metabolism is not normal. Whether these cases are real gout, or only resemble that disease in certain features, must be determined by further studies.”
Quoting from Mallory’s contribution, we note that Pollak investigated the purin metabolism in a series of cases of chronic alcoholism. In five of the examples a marked derangement of purin metabolism was noted and manifested, “partly in retention, and partly in delayed excretion, or a combination of the two.” Having observed these variations in cases of what he considered were non-gouty alcoholics, Pollak felt justified in attaching but limited diagnostic import to the results of the examination of uric acid metabolism in gout, this though he realises the importance of alcoholic excess as a cause of disturbed purin metabolism.
Mallory’s observations, too, on uric acid excretion in gout complicated by lead poisoning are highly interesting. In two cases of this nature he noted that the percentage of uric acid nitrogen excreted was relatively small—in this respect in full accord with previous observations of Brugsch and Schittenhelm on a gouty patient with a history of plumbism, with this reservation, that in the latter observers’ example there were indications of early renal disease, while in Mallory’s two cases such was absent, the urine being normal, and likewise the blood pressure.
Again, Pollak in a case of lead gout noted an extremely low endogenous average, viz., a daily average endogenous excretion of 0·06 gram uric acid in a period of five days. Eschemburg, quoted by Pollak, has recorded an instance of gout with plumbism in which the excretion fell as low as 0·02-0·04 grams. It may be noted that Pollak’s was the victim also of incipient renal disease.
Reverting to Mallory’s conclusions, this observer’s studies of examples of gout with lead poisoning seem to indicate that “these cases differ from normal persons to a greater degree than do other cases of gout.” It may, he thinks, be affirmed that the subjects of gout and plumbism, as a rule, show “some or all of the following characteristics in a much more marked degree than do cases unassociated with lead”:—
(1) Slight fluctuation in the endogenous excretion.
(2) Low endogenous average.
(3) Small percentage of exogenous purin nitrogen excreted as uric acid nitrogen.
To sum up, then, we see that poisons, other than those responsible for gout, may engender obliquities of general metabolism, with disturbances of purin assimilation and output, viz., lead, alcohol, and the causa causans of rheumatoid arthritis. Also, in respect of lead poisoning and alcoholism, further affinities with gout are discernible in that, like the latter disorder, they tend in their later stages to be associated with arterio-sclerosis and renal inadequacy.
Apart from the fact that gouty arthritis may occur in young children, Comby and other observers have noted that children born of gouty parents display a tendency to inflammatory changes in the cutaneous tissues and also in the mucous membranes.
These proclivities are difficult of explanation, but some further observations by Czerny, Paltauf, Escherich, and Pfaunder are also worthy of note. Under the headings of “exudative diathesis” or “neuro-lymphatismus” they have described a symptom complex marked by lymphatism with asthma, occasional vomiting, defective nervous equilibrium, and eosinophilia. These varied phenomena also are common in the descendants of gouty, diabetic, and arthritic subjects.
The clue to the true nature of these phenomena may possibly reside in the fact noted and emphasised by Uffenheimer, viz., that these children exhibit a purin metabolism identical with that met with in gouty patients.
From the foregoing consideration it is clear that further observations are called for in the sphere of purin metabolism, and it is, perhaps, not too much to hope that extended investigations of the uric acid content of the blood may clarify and illumine the conflicting results obtained by urine analysis.
As before stated, we had intended in the next chapter dealing with the question of “Uricæmia in Gout,” but on second thoughts it appears desirable to us to interpolate a chapter devoted to discussion of the primary renal origin of gout; for we take it that, with the phenomena of uric acid excretion in gout fresh in our minds, it will be more easy at this juncture to attempt solution of this very intricate problem. This achieved, we shall resume our thread and pass to the consideration of uricæmia and subsequently uratosis in gout.
This time-worn hypothesis as to the pathogeny of gout has, perhaps, provoked more controversy than any other etiological problem in the sphere of clinical medicine. Nor, unfortunately, despite the endless laborious research expended upon its solution, the dialectic skill exercised in attempts at its elucidation, can we claim even to-day that its complexities have been wholly unravelled. But, perhaps it will be wiser to postpone decision, pending detailed analysis of the several grounds upon which the theory of the primary renal origin of gout rests.
Broadly speaking, the arguments adduced tend to concern themselves with or rather to arise out of certain apparent abnormalities in uric acid excretion, currently held distinctive of gout, certain resemblances also suggestive of a hidden nexus between gout and renal disorders, viz.:—
(1) Anomalies in uric acid excretion in gout.
(2) Uricæmia, a condition common to gout and nephritis.
(3) Uratosis, a feature also common to both disorders.
(4) Occasional co-existence of gout and nephritis.
As to the variations in purin excretion that occur in gout, it must be admitted that, notwithstanding the magnitude of the researches, no very striking departures from normal have emerged. Such as have been elicited occur in relation to (a) the acute paroxysm, (b) the excretion of exogenous purin.
The Acute Paroxysm.—Garrod, it will be recalled, claimed that during an acute attack of gout the excretion of uric acid was diminished, and that coincidently therewith the uric acid blood content rose. But these findings in the blood and urine, which constituted the basis of his hypothesis that gout was due to renal inadequacy, have, as previously noted, been categorically disproved.
Turning to the more modern findings upon which such refutation of Garrod’s view was achieved, one point emerges that appears to favour the assumption of renal block. It is that, one or two days prior to an acute attack, an appreciable decline in the output of uric acid occurs.
But this, be it noted, is neither so marked nor so constant as the subsequent increase; in short, at the zenith of an acute attack, an augmented output of uric acid ensues. At the very time when presumably the alleged functional renal impediment would be most pronounced, the impermeability of the organs for uric acid accentuated! Surely such behaviour seems scarcely compatible with the supposition that there is even a temporary diminution in the capacity of the kidney to excrete uric acid. Does it not in truth constitute strong proof of the reverse? Moreover, the said vagaries that herald the oncoming and that chequer the course of the paroxysm are not invariable, an obvious caveat against hasty etiological inferences therefrom. Any tendency thereto should also be curbed by the reflection that, viewing the character of the uric acid excretion in gout as a whole, the variations therein are not more extensive than in healthy individuals, and assuredly, on the mere basis of the fluctuations in uric acid excretion, no diagnosis of gout is possible.
Retarded Purin Elimination.—The mainstay in argument, however, as advanced by more modern advocates of the renal theory of gout, is that a retarded output of exogenous purin is typical of this disorder; but, here, again, there is no room for dogmatism. Thus Walker Hall reminds us that “the quantity of purins present in the food does not overstep the solubility of urates in the blood-stream, for once the material is metabolised and ready for removal the amount of blood, so far as solubility goes, places the whole amount of purins within the reach of the renal cells in less than twenty-five minutes.” We see, therefore, as far as rapidity of transport to the kidneys is concerned, there is no delay in presentation of the opportunity for the excretion of exogenous purin. While the alleged tardiness of output is attributed to defective action of the kidneys, it is at least equally possible that the delay, as Walker Hall states, “may be due to a defective or idiosyncratic nuclear metabolism, which results in the formation of isomeric purins or incomplete purin combination, and which makes greater demands upon the selective activities of the renal cells;” for it must be recollected that as yet we are ignorant as to the exact form in which uric acid circulates in the blood-stream, whether as sodium mono-urate or in organic combination.
Moreover, experimental injections of uric acid into the tissues or veins show no impairment in the elimination capacity of the kidneys for uric acid. Thus, Wells cites evidence that “the kidney in gout shows no lack of ability to excrete uric acid injected into the tissues.”
Again, given intravenous injection of uric acid into a normal man, its excretion occupies several days, and it fails to appear quantitatively[119] in the urine. But if administered during a course of atophan, then the whole amount injected is excreted within twenty-four hours. If the same procedure be followed in a gouty individual, precisely the same results are obtained; in other words, both normal and gouty kidneys react in identical fashion to atophan. Given an inherent functional defect, quâ uric acid excretion, in the gouty kidney, one would scarcely expect a wholly normal reaction thereto. Surely some disparity would be disclosed, some aberration in response as compared with normal renal organs.
Again, while McLester and others claim that atophan exerts “a selective stimulating influence on uric acid excretion,” it is quite possible that its rôle may be otherwise explained. May it not influence the actual formation of uric acid, or, failing this, the form in which it is presented to the kidneys for excretion? Nicolaier and Dohrn, indeed, believe that atophan influences in some way purin metabolism within the muscles and so leads to increased formation and excretion of uric acid. At any rate, whatever be the explanation of the action of atophan, the fact that healthy and gouty kidneys react alike thereto cannot be interpreted as proof of defective capacity for uric acid elimination in gouty subjects, indeed the reverse.
Moreover, in all our attempts to saddle the kidneys with the responsibility for the delay in exogenous purin excretion, we are for ever hampered in that we know not whether the alleged renal impairment is primary or secondary to the gout. That the kidneys are frequently functionally inefficient in the later stages of gout may be conceded. But what of the initial phases of the disorder? Some talk very glibly of subjects who are, they say, “potentially gouty.” But has the rate of disposal of ingested purins been investigated in persons suffering from so-called “goutiness,” or, perhaps more pertinently, in those individuals, not uncommon, who, while exhibiting auricular tophi, have yet experienced no frank attack of gout?
In this connection we may note that McClure has recently emphasised the fact that the kidneys, in the later stages of gout, are often functionally deficient, and that, accordingly, the faulty elimination of exogenous uric acid by gouty persons may be simply the result of such functional renal depression; in other words, not due to gout, but to the secondary or associated renal deficiency. Hence, having regard to the frequency with which renal inefficiency is met with in gout of any standing, he is inclined to discount the value of studies of exogenous uric acid elimination as an aid to the diagnosis of gout. Consequently, he holds that before the diagnostic status of retarded[120] purin elimination, as a symptom of gout, can be established, an investigation of the output of uric acid in the different types of nephritis is essential.
From the foregoing it will be seen that we stand in urgent need of further studies of early or oncoming gout and of early nephritis before we can with certitude impeach the kidneys as responsible for the delay in exogenous purin output. Meanwhile, too, we must be careful not to overlook the further disconcerting fact, previously adverted to, that the retardation and diminution of exogenous purin output is not invariable in gout. Nor, for that matter, is it peculiar to gout, considerations both of which, if confirmed, will still further discount the diagnostic significance of this phenomenon.
Von Jaksch and Klemperer noted long since that in chronic interstitial nephritis urates are always present in the blood. Now, according to Folin and Denis, human blood contains 1·5-2·5 mg. of uric acid per 100 c.c.; but if the eliminating powers of the kidney be deficient, the uric acid content thereof rises, sometimes to as high as from 15-20 mg. per 100 c.c.
But more interesting still the fact noted by Fine, viz., that even in early interstitial nephritis the same feature is well marked, i.e., the blood may contain 4-8 mg. of uric acid per 100 c.c. Indeed, according to this authority, increase in the uric acid content of the blood is the first signal of impaired renal efficiency. This, be it noted, without any coincident proportional increase in the blood content of urea or creatinine. The sequence would appear to indicate that the damaged organ encounters greater difficulty in excreting uric acid than these other metabolites.
But, pari passu with the advance of the renal disease, retention of urea is superadded, and still later creatinine. So constant, indeed, the sequence that, by determining the percentage amount of these three metabolites in the blood, the measure of the renal mischief may be gauged.
But of striking significance is the further point established by Myers and Fine, viz., that the blood content, in respect of uric acid, urea, and creatinine, in early nephritis, is an almost exact replica of that met with in typical cases of gout. The same is well illustrated in the following table, in which the blood content, in respect of these three metabolites, in cases of gout and early and late nephritis is contrasted. The percentage of the retained metabolites in relation to the severity of the case is gauged by the blood pressure findings.
| Diagnosis. | Uric acid. |
Urea N. Mg. to 100 c.c. blood. |
Creatinine. | Systolic blood pressure. |
|---|---|---|---|---|
| Typical cases of gout. | 9·5 | 13 | 1·1 | 230 |
| 8·4 | 12 | 2·2 | 164 | |
| 7·2 | 17 | 2·4 | 200 | |
| 6·8 | 14 | 1·7 | ||
| Typical early interstitial nephritis. | 9·5 | 25 | 2·5 | 185 |
| 8·0 | 37 | 2·7 | 150 | |
| 5·0 | 37 | 3·9 | 130 | |
| 7·1 | 16 | 2·0 | ||
| 6·6 | 24 | 3·3 | 185 | |
| 6·3 | 18 | 2·1 | ||
| 8·7 | 20 | 3·6 | 100 | |
| 7·0 | 33 | 2·6 | 117 | |
| 6·3 | 31 | 2·1 | ||
| 6·3 | 23 | 2·4 | 150 | |
| Chronic diffuse and chronic interstitial nephritis. | 8·0 | 80 | 4·8 | 240 |
| 4·9 | 17 | 2·9 | 170 | |
| 8·3 | 72 | 3·2 | 238 | |
| 5·3 | 21 | 1·9 | 145 | |
| 9·5 | 44 | 3·5 | 210 | |
| 2·5 | 19 | 1·9 | 120 | |
| 7·7 | 67 | 3·1 | ||
| 6·7 | 17 | 1·6 | 165 | |
| 8·3 | 39 | 2·9 | ||
| 6·5 | 24 | 3·0 | 200 | |
| Typical fatal chronic interstitial nephritis. | 22·4 | 236 | 16·7 | 210 |
| 15·0 | 240 | 20·5 | 225 | |
| 14·3 | 263 | 22·2 | 220 | |
| 13·0 | 90 | 11·1 | 265 | |
| 8·7 | 144 | 11·0 | 225 |
(Myers and Fine: “Arch. Int. Med.,” 1916.)
The salient feature of the table is, however, the fact that in early interstitial nephritis the retention of uric acid precedes that of urea or creatinine.
Its importance resides in the reflection that it lends support to those who contend that renal change, leading to failure of excretion of uric acid, is the primary cause of gout; in other words, it gives colour to Magnus Levy’s contention that the phenomena of[122] gout are referable to “a deficient and restricted secretory power of the kidney.” The existence of such a selective excretory incapacity, i.e., for uric acid, does not, he considers, predicate a genuine nephritis. He maintains that such disability on the part of the kidney for uric acid excretion may exist without morphological change; in other words, he thinks it conceivable that a single function of the kidney can become almost exclusively insufficient, though later real damage to the organ and a nephritis frequently follow.
Reflecting on the above theory, it is obvious that, if carried to its logical conclusion, it would appear to postulate that gout is nothing more than a form of renal disorder, marked simply by functional inability to excrete uric acid. The postulate is no mean one, for, as Sir Archibald Garrod says, “If the fault is in the kidneys alone, gout must be removed once and for all from the category of metabolic disorders, and placed among the sequelæ of renal inadequacy, at least in so far as the uric acid phenomena of the disease are concerned.”
Furthermore, Levy’s hypothesis involves the assumption that the excreting functions of the kidney for uric acid and urea are separate and independent of each other, and to discussion of this we now pass on.
Taking samples of human blood from (1) unselected insane subjects and (2) chronic nephritics, Folin and Denis determined the amounts therein of urea, total non-protein nitrogen, and uric acid. The figures obtained showed that “there is apparently no relationship between the amount of uric acid and the amount of urea or total non-protein in nitrogen, in human blood.”
That such a discrepancy should obtain is doubtless of profound though as yet imperfectly grasped significance. These authorities rightly assume that, since the kidney is practically the sole avenue for nitrogenous waste excretion, it follows that the urea and total non-protein nitrogen of the blood must in the main be inversely proportional to the general efficiency of the renal organs. Then, obviously, the same law, too, should, in lack of some other plausible explanation, govern the excretion of uric acid also. But, as the above generalisation portends, it is apparently not so.
Fortunately, Folin and Denis prosecuted their study still further, taking in examples of gout (with and without clinically recognisable nephritis), also instances of leukæmia and lead poisoning.
The blood, again, in these disorders betrayed the same peculiarity, viz., that while containing an excess of uric acid, it did not contain correspondingly large amounts of urea or other waste nitrogen; in other words, the findings in the blood in gout were in full accord with the above generalisation, i.e., the apparent lack of any relationship between the amount of uric acid and that of urea or total non-protein nitrogen in the blood.
Now in leukæmia the cause of the uricæmia is over-production of uric acid, but in this instance the same is correlated with an increased elimination of uric acid by the kidneys.
Turning to lead poisoning, the medicinal administration of lead acetate results in a great diminution of uric acid excretion, a response consistent with the view that lead inhibits the excretory power of the kidney for uric acid, the change, at first functional, becoming later organic; for it is held that the uricæmia, associated with plumbism, proves that the action of the lead is not due to inhibition of the formation of uric acid.
Lastly, as to gout, opinion still wavers as to whether or not the excretion of uric acid in this disorder is appreciably lowered. On the other hand, it is significant that the reverse is never claimed, viz., that in gout the uric acid output is abnormally raised. Now, as we saw in leukæmia, the high uric acid blood content is accompanied by a correspondingly high uric acid output; but, on the contrary, in gout, despite the accumulation of uric acid in the blood, there is no parallel increase in its elimination.
Reflecting on the above considerations, Folin and Denis claim that “the mere fact that the uric acid may accumulate in the blood of the gouty without being accompanied by an increased elimination constitutes definite proof that the gouty kidney is damaged with reference to its ability to eliminate uric acid.”
In all deference, we doubt the legitimacy of the inference, if only for the very excellent reason that, to quote Von Noorden’s words, even to-day “it remains uncertain whether the retention of urate arises because the outlet is blocked, or because the uric acid is held fast by chemical affinities.”
Apart from this, there are several objections to Folin and Denis’ assumption.
Thus Pratt, in some examples of his cases of gout, found that there was no apparent diminution or delay in the output of exogenous purin in the urine. On the other hand, he observes that “our study of the blood shows that a marked increase in retention of uric acid in the blood may result from the ingestion of purin bases even when no evidence of retention is found on examination[124] of the urine.” This would appear to indicate that the uricæmia, sequential to exogenous purin intake, ensues independently of and apparently despite the absence of any delay or diminution in uric acid elimination.
Again, Walker Hall, discussing the metabolism of exogenous purins, reminds us that a gouty subject excretes an excess thereof as completely as a normal individual, with only this difference, that he takes a longer time to do so; but even this disability is removed by a simultaneous intake of atophan. His comment is that “the gouty kidney, therefore, is not poisoned beyond compensating for and responding to an extra load.” “Perhaps,” he says, “the situation may be summed up in the observation that the uricæmia of the gouty is maintained in spite of a fair renal elimination.”
Again, a grave obstacle to the acceptance of Folin and Denis’ inference is that uricæmia, though incidental to nephritis, is not peculiar thereto.
Thus Roy Upham and Higley noted its presence in 85·6 per cent. of their cases of nephritis; but, on the other hand, they found that no less than 40 per cent. of another series of clinical cases, not suffering from nephritis, also showed uricæmia.
This would appear to indicate that, while uricæmia is an exceedingly common symptom of early chronic interstitial nephritis, it is by no means specific for that disorder; in other words, its diagnostic valency as a symptom of nephritis is distinctly limited.
Reverting now to gout, what evidence is there that the uricæmia therein is due to defective eliminatory capacity on the part of the kidney for uric acid? Certainly there is no proof that the kidney, at any rate in the initial stages of gout, suffers from this particular functional disability. Indeed, the fact that, at the very acme of an acute attack, the output of uric acid is not only not diminished, but actually increased, constitutes strong proof of the reverse.
Again, as modern investigations show, the variations in the uric acid content of the blood, re the incidence or intensity of attacks, are most erratic. Far from its being essential that uricæmia be present, acute attacks may occur with even a sub-normal uric acid blood content; in short, the variations are so erratic as to seem quite out of keeping with the assumption that the uricæmia in gout is primarily of renal origin.
If it were so, one would expect no such vagaries in the uric acid content of the blood. One would rather, given the existence ab initio of a renal functional defect, look for not only a permanent uricæmia, but further, from time to time, augmentations and[125] diminutions thereof, synchronising with the rise and wane of gouty paroxysms; in other words, that in gout the clinical course and crises of the disorder would be linked up with harmonious variations in the degrees of uricæmia.
If it were so, why does not every case of nephritis develop gout? The researches of Myers and Fine have shown that uric acid is the nitrogenous metabolite that first accumulates in the blood in early interstitial nephritis. Only in its later stages do urea and other waste nitrogenous products undergo like retention therein.
Now let us review these findings, re nephritis, in light of another statement by Folin and Denis, which runs as follows:—
“In pure gout, unaccompanied by any abnormal urea retention in the blood, the kidney is damaged (so far as we yet know) only with its function of removing down to the normal level the uric acid of the blood.”
Is it not clear, then, that in the early stages of nephritis, viz., prior to retention of urea and other waste nitrogen, we have precisely that isolated functional renal disability, i.e., inability to excrete uric acid, that we postulate to be in operation in the initial stages of gout?
Yet, notwithstanding this similitude in the blood content of the two disorders, cases of nephritis do not necessarily develop gout. Indeed, as a matter of fact, examples of nephritis, of all grades and intensities, may run to their full end without manifesting any symptoms even remotely reminiscent of gout. Even Magnus Levy, ardent advocate as he is of the primary renal origin of gout, could not but admit that this salient clinical obstacle barred the way to acceptance of his otherwise plausible view. However, he fails to proffer any other solution of the problem.
To our mind, albeit, the disparity carries with it the inevitable postulate that in gout some other factor intrudes, some tertium quid, something vital, something biological, haply an infection. For even if we grant, for the sake of argument, that renal retention, if it were proved, might explain such anomalies in the excretion of uric acid and other nitrogenous metabolites as occur in gout, yet, nevertheless, no one could possibly contend that this factor alone could explain the nature of gout, could adequately account for its dramatic and protean phenomena.
Naturally the advocates of the renal theory had to account in some way for the alleged functional disability of the kidney. Thus,[126] Sir Dyce Duckworth, recalling the occasional occurrence in hysteria of anuria, held that, judging from the general phenomena of acute gout, “the influence of the nervous system ... must not be left out of account as a possible determining factor for renal inadequacy.”
Others, with whom Duckworth disagreed, propounded the view that the deposition of urates in the renal tissues was essential for the initiation of a nephritis in the gouty. Duckworth, on the other hand, held that nephritis could develop in their absence.
Croftan considers the renal changes in gout identical with those of chronic plumbism. From experiments with hypodermic injections of xanthine and hypoxanthine over a prolonged period, he concludes that the presence of minute quantities of purin bases in the circulation is capable of producing marked renal changes. On the other hand, uric acid, injected into the circulation of healthy animals for a period of over three months, produced no renal change whatever.
As to this possibility, viz., that the circulating uric acid might lead to nephritis in the gouty, some reflections of Folin and Denis are instructive. Normal blood, according to these observers, contains not less than from 1-2 or 2-5 mg. per 100 grams, while that of gouty blood does not, in their experience, exceed 6 mg. Continuing, they observe, “There is, however, no reason to suppose that a uric acid concentration of 4-6 mg. per 100 grams of blood is very much more irritating or stimulating to the kidney than the somewhat more dilute solution represented by normal blood. Disregarding the insolubility of uric acid, the elevation of its threshold of elimination from 2-4 or 6 mg. (per 100 grams of blood) is certainly a small one. Kidneys in which the threshold of elimination for urea has risen by 10-20 mg. (per 100 grams), or even more, are extraordinarily common.”
While they consider that such urea and total nitrogen retention may possibly bespeak latent or incipient nephritis, they recognise that no appreciable effects on health have as yet been determined in connection therewith. But more pertinently to our point, they make the further pregnant observation, “In the case of uric acid it seems to be purely a matter of insolubility that corresponding or even smaller degrees of kidney insufficiency with slight uric acid accumulation should result in all the serious consequences involved in the development of gout”!
Again, some have attempted to account for the assumed renal incapacity as being part of the tissue peculiarity of the gouty subject. “Without doubt,” says Duckworth, “there are peculiarities of tissue in the gouty, and with this may very possibly be associated peculiarities of tissue function and metabolism.”
Naturally this suggests the further question, Are there any distinctive histological changes in the gouty kidney? On this point Walker Hall has some apposite reflections. Taking Folin’s figures as a basis, it transpires that in acute and chronic nephritis, also in arterio-sclerosis, there is an average content of 2·5 mg. uric acid per 100 grams of blood. Now, notwithstanding the fact that in these conditions an appreciable quantity of the renal tissues is, functionally speaking, temporarily or permanently out of action, nevertheless “the extraction of uric acid from the blood and its subsequent excretion are practically normal.” The inference is that a relatively small moiety of renal tissue suffices for the excretion of the daily quantum of uric acid in the urine.
Now in contrast thereto, the blood content in gout and lead poisoning is about 4·5 mg. uric acid per 100 grams of blood, or “an increase of about 50 mg. in the total blood-stream at any one moment (an increase from the normal 70 up to 120 mg.).” Continuing, Walker Hall observes that “the gouty kidney per se, even when arterio-sclerotic conditions prevail, does not show anything like the amount of cellular damage which occurs in acute or chronic diffuse nephritis.” Thence he argues if histological changes be taken as a criterion of functional efficiency, then the gouty kidney should be more capable of excreting freely than the diffuse nephritic organ.
How does this work out in actual daily life? he asks. “0·5 gram, in a normal adult, represents the average daily endogenous uric acid excretion in the urine, while that of a gouty subject is about 0·45 gram. Now, assuming that the type and extent of the endogenous metabolism is identical in each instance, then the balance, i.e., 0·05 gram, is distributed between the uric acid pent up in the tissues and the uratic deposits, i.e., tophi.” Walker Hall tells us it has been stated that about 0·01 gram suffices to cover the amount deposited as tophi every twenty-four hours. The residual 0·04 gram runs to swell the amount in the blood and lymph-streams. “The increase is 0·0114 to 0·0118 gram per litre of blood; in other words, the actual increase of uric acid circulating through the kidneys is about 0·00047 per hour,” which, as Walker Hall contends, “seems to be a very trifling difference, especially as it is one of amount and not a type.” In other words, it is quantitative, not qualitative. But, trivial as the disparity is, to what may it be referred? To Walker Hall’s mind, if we are to appreciate the standpoint of those who maintain that the gouty uricæmia is referable to renal inadequacy, it is necessary to postulate the presence of a poison acting upon the renal tubules specifically.
In the gouty uric acid excretion is maintained at a “low physiological level to the very end,” and it is easier, he thinks, to adopt the[128] above hypothesis as to its cause than “to conceive of a poison acting upon the nuclear processes in such a way as to induce a persistently low uniform level” of purin excretion.
This view, viz., of a toxin acting specifically upon the uric acid excreting cells of the kidney, seems to be the only reasonable assumption available. But even this is difficult of adherence when we recall the fact that the effect of the toxin is so readily neutralised by a few grains of atophan. Always we have to recollect, too, that under normal conditions, even given a constant diet, the elimination of uric acid displays wide variations. Also the uric acid output in the subjects of chronic gout, when placed on a fixed diet, differs but little from that of normal individuals on a like dietary. At most the excretion but tends to fall to, or slightly below, the lower normal limits of uric acid elimination.
From the foregoing considerations it is but too obvious that those who render obeisance to the primary renal origin of gout have not only yet to prove that the functions of the kidney are defective, but also upon them lies the onus probandi why gouty subjects should exhibit, or acquire, such a disability.
Here, again, we light upon another point of contact between gout and nephritis, for an interesting feature of the latter disorder is that the retained uric acid, purins, and other excretory products are deposited in cartilage and serous membranes. At these sites they are frequently detected post mortem, though they fail of ante-mortem recognition.
Impressed by the fact that, at post-mortems, uratic incrustation of the articular cartilages was frequently observed in persons who had never suffered from overt gout, Ord and Greenfield sought to ascertain the frequency with which such uratic deposits were associated with renal disease. Out of ninety-six cases presenting renal lesions, no less than eighteen exhibited uratic deposits in the joints.
A still more elaborate research in this sphere was undertaken by Norman Moore. Out of forty-nine cases of chronic interstitial nephritis, uratic deposits were present in twenty-two instances. Again, out of nine cases of chronic parenchymatous nephritis, deposits were found in the joints in two cases. With respect to the first group he observes that “chronic interstitial nephritis is not invariably accompanied by deposits in the articular cartilages, though usually accompanied by traces of degeneration in some of the articular cartilages.”
Levison, too, an ardent supporter of the primary renal origin of gout, noted that all the subjects dying at the Communal[129] Hospital, Copenhagen, of granular kidney disease (during a period of fourteen months) exhibited uratic deposits in one or other of their joints, although they were never known to have had any definite attack of gout.
Luff, in the following table, shows the results of the examination of the joints in seventy-seven cases of granular kidney disease.
| No. of cases. | Uratic deposits in joint or joints. |
|
|---|---|---|
| Known to have had gout | 10 | 10 |
| Never known to have had gout | 67 | 31 |
| Totals | 77 | 41 |
Of the ten cases known to have suffered from gout, the renal condition was in every instance defined as “markedly granular,” or “fairly granular.” Uratic deposits were invariably present in one or more joints. Of the sixty-seven examples not known to have had gout, uratic articular deposits were found in 46 per cent., which approximates, more or less closely, to Norman Moore’s findings. It is noteworthy that in several of the instances, lacking uratic deposits in the joints, the kidneys were described as “slightly granular,” or “faintly granular.”
| No. of cases. | Uratic deposits in joint or joints. |
|
|---|---|---|
| Marked granular kidney disease | 26 | 20 |
If of the sixty-seven cases there be selected only those described as “markedly granular,” or “typical granular kidneys,” the incidence of uratic deposits in the joints, as revealed by the second table, reaches no less a figure than 77 per cent.
Another authority, discussing the frequency of incidence of uratic deposits in the joints in cases of chronic interstitial nephritis, states that, at post-mortem, from 50-80 per cent. show their presence—this, moreover, in cases known not to have had gout.
Uratic deposits, it is true, occur in both these disorders. But it is with a difference. In gout the uratic deposit assumes the[130] form of tophi, whereas in nephritis it is not so. In the latter the uratic deposit is in the nature of a passive deposition—an uratic incrustation of the articular cartilages.
Again, in gout the deposition is sudden and associated with an acute paroxysm; while in nephritis it is gradual and unassociated with inflammatory reaction.
In gout the uratic deposits are overt, manifest as tophi; in nephritis, occult and unrevealed (ante-mortem).
Uratic deposits in the form of tophi occur in gout, in the absence of clinically recognisable interstitial nephritis. But tophi do not occur in nephritis if uncomplicated by gout.
In conclusion, the mere fact that uratic deposits affect such widely disparate forms in these two disorders is to our mind a sure indication that their mode of origin and formation is equally diverse—the one vital, biological; the other passive, mechanical.
It cannot be denied that gout and granular kidney are frequently met with in close association. But neither can it be disputed that in these disorders, as in many others, their outward affinities do but hark back to inward disparities. The occasional overlapping of the two affections, the trenching of the one upon the clinical or pathological territory of the other, must not blind us to the essential distinctness of the two morbid entities. Doubtless to the earlier advocates of the renal theory their not infrequent co-existence bespoke some hidden nexus, and at least seemed confirmatory of their views as to the pathogeny of gout. But, even if we allow that the connexion between the two disorders seems superficially intimate, it cannot be gainsaid that it is neither constant nor essential. For we have to recollect that—
(1) Some gouty subjects never develop granular kidney.
(2) Some individuals with granular kidney never develop gout.
Also we have to recall that—
(1) Paroxysms of gout often occur for many years before the symptoms of interstitial nephritis develop.
(2) In persons of gouty stock acute attacks may ensue at an age at which nephritis is practically unknown.
Apart from the difficulty of reconciling these disparities, we cannot overlook the fact that both gout and granular kidney are very common diseases, sufficiently common, as Samuel West pointed out, to be not infrequently associated accidentally, without any cause or connection. Again, both affections, be it observed, are prone to develop in the middle and later decades of[131] life. In light of this, is it not readily conceivable that both may arise independently, mere coincidences, both evidences of pre-senilism? Hastings Gilford, indeed, classes gout with syphilis, lead, and alcohol as amongst “the chief promoters of pre-senility.”
Again, certain toxic agents which predispose to or initiate renal mischief also favour apparently the incidence of gout, e.g., lead and alcohol. Samuel West, discussing the relationship of both gout and lead to granular kidney, maintains that, though each may produce chronic change in the kidney, neither of them causes granular kidney. But the presence of granular kidney, he holds, greatly enhances the liability of the victim to gout on the one hand and plumbism on the other; also, to both together and in each affection alike markedly increases the gravity and the risk.
Sir William Roberts, too, has some wholly relevant observations on this point. Thus all will agree with him that “it is difficult to conceive that plumbism induces the same constitutional diathesis as that which obtains in true gout.” He held that gout and plumbism, though they differ in all other respects, yet have one point in common, a tendency to uratic deposition. But such precipitation, he contended, was the outcome of a gouty tendency, reinforced by lead poisoning; or if, on the other hand, uratic deposits occurred in plumbism, the same had but accentuated a pre-existing gouty diathesis. In this connexion, too, it should be recalled that the frequent association of gout and lead poisoning which exists in London is not seen in the North of England or in North America.
Is it not clear, then, that reflection on the broad clinical affinities exhibited by gout and granular kidney does but emphasise the essential distinctness of the two morbid entities? Inferentially, too, it lends no colour to the assumption that gout is of primary renal origin.
That the victim of gout, despite uricæmia and those unequivocal tokens, tophi, may, notwithstanding repeated arthritic outbreaks, be in the intervals in sound if not exuberant health, is a clinical truism. His kidneys, too, may, as far as can be ascertained, be normal; and his blood pressure not beyond what might be expected at his age. His output of uric acid may but touch the lower normal limit or a little less, and his metabolism of purin-rich foods be but a little protracted. Thus he runs his course, more frequently than not a strenuous one, chequered by occasional outbreaks which not seldom he regards as salutary rather than otherwise. Then, sooner or later, in one, two, or even three decades, that Nemesis of age, arterio-sclerosis overtakes him with its correlated chronic nephritic change.
Is not this very reminiscent of what Walker Hall reminds us of,[132] the sequence of events in lead poisoning and alcoholism? “These poisons affect the general metabolism adversely and are connected with disturbances of purin assimilation and output. At a later stage they produce arterio-sclerosis and renal insufficiency.” And as he shrewdly observes, “It is, therefore, of importance to exactly appraise the stage of the disease when interpreting the results of experiments upon gouty individuals. When this obtains widened application, many generally accepted statements will have to be re-written.”
In conclusion, therefore, we see that the weight of clinical evidence is against the primary renal origin of gout, for not only are renal changes frequently slight, but they are often entirely lacking in gout. Confronted with these difficulties, the question inevitably rises as to whether there does not exist a special morbid entity, gout, which develops independently of renal abnormalities?
In the summer of 1848, Garrod made his momentous announcement that “the blood in gout always contains uric acid in the form of urate of soda, which salt can be obtained from it in crystalline state.” Some eleven years later in his classic work on gout, he reiterated his affirmation, but appended thereto the words, “in abnormal quantities.” Garrod’s analyses were mainly qualitative, but, at any rate, in one instance, he obtained from a gouty patient the equivalent of 5 mg. of uric acid per 100 gm. of blood serum, maintaining, however, that this amount was much below that really present.
But not until 1895 was a series of quantitative estimates undertaken when Klemperer in three gouty subjects passing through an attack found the blood content of uric acid to be 6·6 mg., 8·8 mg., and 9·5 mg. per 100 c.c. of blood. Some years later, Magnus Levy, investigating seventeen gouty individuals, found that the amount of uric acid in the blood ranged from 2·1-9·5 mg. per 100 c.c.
Brugsch and Schittenhelm noted that, in gouty victims, uric acid was still present in the blood even when they had been on purin-free diet for weeks or months. They held endogenous uricæmia to be a constant symptom in gout. Even as late as 1913 the former investigator contended that, in a healthy person on a purin-free diet, the presence of uric acid in the blood cannot be satisfactorily demonstrated. But it must be recollected that the precipitation (ammonical silver and cupric bisulphite) method was beset with disadvantages. An approximate estimate only of the blood content of uric acid was with difficulty to be achieved even when large quantities were available.
Fortunately, however, our powers of analysis in this direction became greatly enlarged with the introduction in 1913 of the colorimetric method of Folin and Denis.
This colour reaction is so sensitive that one part of uric acid in a million parts of water can be detected. Moreover, unlike the older methods which required from 75-100 c.c. of blood or more, determinations can be made with 20 c.c., and if the blood be rich in uric acid only 10 c.c. Walker Hall observes that the procedure “has many advantages and does not take up much more time than[134] some of the qualitative methods when once the technical difficulties are overcome.” He described it as follows:—
Twenty cubic centimetres of blood are withdrawn into a wide-mouthed, tared bottle containing 0·1 gramme of finely-powdered potassium oxalate. The flask and contents are then weighed. Five times the weight of n/100 acetic acid is heated to boiling. The oxalated blood is poured into the boiling acetic acid solution, and the heating continued until the solution has begun again to boil. The mixture is filtered hot. The clear filtrate and wash waters are acidified (0·5 c.c. of 50 per cent. acetic acid) and evaporated to 3 c.c. Five drops of a 3 per cent. silver lactate solution, two drops of magnesia mixture, and ten to fifteen drops of strong ammonia hydrate are next added. The mixture is centrifugalised. The supernatant fluid is removed. To the residue five drops of freshly-saturated hydrogen sulphide water and one drop of strong hydrochloric acid are added. The tube is placed in a beaker of boiling water for ten minutes in order to remove the hydrogen sulphide. The supernatant fluid is added to 2 c.c. of a solution containing 100 grams of sodium tungstate and 80 c.c. of 85 per cent. phosphoric acid in 1,000 c.c. of water and 10 c.c. of a saturated sodium carbonate solution. The resultant blue solution is then compared with a standard uric acid solution, and the result obtained by the following formula:—
(20V)/(RW) mg. of uric acid per 100 grams blood,[20]
where 20 represents depth in millimetres of standard solution,
Up till quite recently it was held that in normal persons the amount of uric acid in the blood was too small to be detected; also that uric acid was not demonstrable in the blood of normal individuals when on a purin-free diet. On the other hand, if the subject’s blood was found to contain uric acid, while on a purin-free diet, it was held a characteristic feature of gout and of prime diagnostic import.
But, since the introduction of Folin and Denis’s method, it has been established that uric acid is constantly present, in demonstrable amounts, in human blood. These authorities, using their colorimetric method, found that the uric acid content of the blood ranged from 0·7-3·7 mg. per 100 grams. They believe that 1-2 mg. of uric acid per 100 grams of blood is well within the normal variations, but “are not prepared to say that they represent the full variations.”
However, before applying their colorimetric method to human subjects, Folin and Denis conducted some researches into the uric acid blood content of a variety of animals, the results of which appear in the following table:—
(The Figures represent Milligrams per 100 grams of Blood.)
| Uric acid. |
Non-protein nitrogen. |
Urea nitrogen. |
|
|---|---|---|---|
| Rabbit (6 cases) | 0·05 | 31 | 13 |
| Sheep (mixed blood) | 0·05 | 28 | 13 |
| Pig (mixed blood) | 0·05 | 32 | 14 |
| Horse (1 case, anti-toxin animal) | 0·05 | 54 | 28 |
| Monkey (1 case, poliomyelitis) | 0·05 | 60 | 38 |
| Beef (mixed blood) | 0·2 | 24 | 14 |
| Cat (2 cases, diet, liver) | 0·2 | 60 | 34 |
| Cat (2 cases, diet, milk and eggs) | 0·2 | 67 | 37 |
| Cat (2 cases, diet, rice and cream) | 0·2 | 31 | 20 |
| Chicken (6 cases, mixed blood) | 4·9 | 32 | 8 |
| Duck (4 cases, mixed blood) | 4·8 | 34 | 7 |
| Goose (1 case) | 4·8 | 26 | 8 |
The most striking feature of these findings is the marked contrast between the uric acid blood content of mammals as opposed to avians. In the former the amount is minimal—0·2 mg. or less per 100 grams of blood. On the other hand, in the blood of birds, in whose instance the origin of uric acid is so different, it is present in relatively large amounts. As Folin and Denis observe, the[136] small amounts of urea in the blood of birds, as compared with that of mammals, is also worthy of note.
Reverting now to the findings in human subjects, as observed by Folin and Denis, these have been summarised as follows by Walker Hall:—
(The Figures represent Milligrams per 100 grams of Blood.)
| Uric acid. |
Non-protein nitrogen. |
Urea nitrogen. |
|
|---|---|---|---|
| Human, group 1 | 0·8 | 36 | 19 |
| Human, group 2 | 1·5 | 34 | 18 |
| Human, group 3 | 2·8 | 36 | 19 |
| Human, with blood pressures of 160 | 2·9 | 50 | 33 |
| Human, with blood pressures of 200 | 1·2 | 50 | 22 |
| Human, with blood pressures of 220 | 2·7 | 40 | 19 |
| Human, with blood pressures of 260 | 3·9 | 52 | 20 |
| Human, alcoholic | 1·0 | 43 | 29 |
| Human, chronic gout | 3·9 | 25 | 13 |
| Human, chronic gout | 4·4 | 30 | 15 |
| Human, chronic gout | 5·2 | 20 | 13 |
| Human, lead poisoning | 4·7 | 50 | 31 |
| Human, lead poisoning | 4·8 | 52 | 32 |
| Human, leukæmia | 3·1 | 33 | 14 |
| Human, acute nephritis with arterio-sclerosis | 2·7 | 40 | 19 |
| Human, chronic nephritis with arterio-sclerosis | 2·5 | 38 | 19 |
Interesting and valuable as are the above findings, Folin and Denis are careful to point out that, even as regards the first three groups in the above table, “the figures can scarcely be said to represent the strictly normal variations, for no attempt was made to select physically normal persons.” The samples of blood were drawn from patients newly admitted to the Boston Psychopathic Hospital.
It may be noted that of all the mammals examined the blood of man contains by far the greatest amount of uric acid. Also that in humans the uric acid blood content varies in different persons, and, moreover, as Walker Hall points out, “the figures lend support to the view that there may be groups or families exhibiting similar features.” It will be seen, too, that the blood uric acid in gout and lead poisoning stands at a high level, though not so elevated as was formerly maintained. From the figures, too, it may be gleaned that apparently no relationship obtains[137] between the amount of uric acid and that of the urea or total non-protein nitrogen in the blood.
At the same institution in Boston, Adler and Ragle conducted a similar series of investigations, though on a more extended scale. These observers, taking 156 unselected psychopathic patients, found that in 107 examples the uric acid content of the blood was from 1-2 mg., in thirty-eight more than 2 mg., and in eleven instances less than 1 mg. To sum up, the uric acid content varied from 0·7-4·5 mg. per 100 grams of blood, an average of 1·7 mg.
As before stated, it was until recently maintained that in the blood of normal individuals, on a purin-free diet, uric acid was undemonstrable. But McLester, utilising Folin’s method, found uric acid in the blood of fifteen healthy individuals, who had been on a purin-free diet for at least three days, and this in amounts ranging from 0·5-2·9 mg. per 100 grams of blood, an average of 1·4, as contrasted with 1·7, the average amount in Adler and Ragle’s series. Pratt, discussing these findings, considers that the fact that the average amounts approximate so nearly in the two series is worthy of emphasis. This especially as all McLester’s examples were young healthy adults on a purin-free diet, while the patients studied by Adler and Ragle were of all ages and on a mixed diet.[21]
As we are aware, the amount of uric acid excreted in the urine increases markedly on a purin-rich diet. But recent researches[138] appear to raise doubts as to whether the uric acid content of the blood rises correspondingly. Thus, according to Walker Hall, “a state of uricæmia is said to exist if the amount of uric acid in the blood exceeds 0·8 mg. per 100 c.c.” The figure he considers is probably too low for, after an average meat breakfast, the blood uric acid rises to 1 or 2 mg. per 100 c.c. in normal adults, or even higher after an excessive intake of purin-rich foods.
On the other hand, Denis, investigating the effect of ingested purin on the uric acid content of the blood, found that in normal individuals no increase in the circulating uric acid follows the intake; in other words, the kidney, in normal persons, is quite capable of excreting any excess of uric acid presented to it, thereby keeping the uric acid of the blood at the same level as obtains when only the endogenous moiety thereof has to be eliminated.
Moreover, another factor, according to Folin and Denis, that operates in the same direction is the binding capacity of the tissues for uric acid. Pratt of Boston’s observations, too, appear to indicate “That the uric acid derived from exogenous purin does not accumulate in the blood unless there is a disturbance in the uric acid metabolism.”
On the other hand, given damage to the kidney (even when this has not progressed to the point when nitrogen retention is apparent, as shown by the non-protein nitrogen values), an accumulation of uric acid takes place in the blood after a short period of purin feeding.[22]
Now, as to the second regulating factor, the retention capacity of the tissues for uric acid, it may be said that the amount, in normal subjects, would appear to be small. But Fine, it may be noted, found that the uric acid content in divers tissues was relatively proportionate to that of the blood, whether normal or increased in amount.
But, to resume, Denis also demonstrated that the uric acid content of the blood in patients suffering from various chronic diseases other than gout was also not increased on a purin-rich diet. To sum up, the researches of Denis would appear to indicate that:—
(1) In normal subjects no increase in the uric acid content of the blood follows exogenous purin intake.
(2) The uric acid content of the blood in patients suffering from chronic diseases, other than gout or renal disease, is similarly not augmented on a purin-rich diet.
(3) The uric acid content of the blood is increased more or less markedly, after a short period of purin feeding, in the presence of defective renal elimination.
In amplification of the second of the foregoing postulates some observations by Pratt may be quoted. This authority is of opinion that the low amount of uric acid present in the blood of unselected psychiatric patients on a mixed diet (Folin and Denis, Adler and Ragle) shows that a retention of uric acid in the blood in any considerable amount for twenty-four to twenty-eight hours rarely occurs. For, as he informs us, these patients at the Boston Psychopathic Hospital, when on ordinary diet, are eating purin-containing food daily, and they might take as much or more purin during the forty-eight hours preceding the blood analysis as is contained in a single sweetbread meal. Now, as Pratt argues, if the uric acid thus derived accumulated in the blood, the amount found would be considerably greater than that of individuals on a purin-free diet. But, on the contrary, it transpires that the average amount of uric acid found by Adler and Ragle in the blood of patients on an ordinary diet was only 0·3 mg. more than that found by McLester in normal individuals on a purine-free diet. The diagnostic significance of these observations will be better appreciated when we come to discuss the sequential increase of the uric acid content of the blood in gouty subjects after the ingestion of purin-rich substances.
Taking 1-3 mg. per 100 c.c. as the normal, the uric acid content of the blood, in typical cases of gout, according to MacLeod, rises to nearly 10 mg. Gudzent, from his studies, maintains that the blood, in almost all cases of gout, contains as much or even more mono-sodium urate than it can hold in solution (1-8 mg.), in other words, it is in effect a supersaturated solution of the relatively insoluble lactim urate.
Pratt, working in Folin’s laboratory, investigated a series of cases of gout, selecting only those in which (1) Tophi were found, (2) A history of characteristic attacks of acute gout was obtained, or (3) Typical symptoms developed while under observation.
At the time of examination the average uric acid content, irrespective of the diet or condition, was 3·7 mg. In three patients on ordinary diet, who were seen during attacks, the amounts were 4·5, 4·8 and 5·7 mg. of uric acid. In two other patients, also seen during attacks, and while on a purin-free diet, the uric acid in four estimates ranged from 2·4-5·1 mg., viz., an average of 3·6 mg. None of these patients were taking atophan.
Seven patients, on a mixed diet, and free at the time from symptoms of gout, contained on the average 4·3 mg. of uric acid in their blood.
On the other hand, examination of the blood in six patients on a[140] purin-free diet, at the time manifesting no acute symptoms of gout, revealed an average uric acid content of 3 mg.
From the foregoing considerations it may be deduced that:—
(1) In gout there is a condition not of uricæmia, but of hyper-uricæmia.
(2) That on the average the blood in gouty subjects contains twice as much uric acid as that of non-gouty subjects, as evidenced by comparison of the average uric acid content of the blood in Pratt’s series of gouty cases (4·5 mg.) with Adler and Ragle’s non-gouty examples (1·7 mg.).
(3) In contrast with non-gouty subjects, the uric acid content of the blood in gouty subjects is augmented on a purin-rich diet.
(4) Both in the inter-paroxysmal periods and during attacks the uric acid content of the blood, when on a mixed diet, is higher than when on a purin-free diet.
Pratt, of Boston, has found that a condition of hyper-uricæmia is sometimes demonstrable in joint disorders other than gouty; but he maintains that the following distinction obtains, viz., that while in gout the hyper-uricæmia is generally constant, in other forms of arthritis it appears to be transient.
He cites a case of infective arthritis, not exhibiting the clinical features of gout, in which the first analysis of the blood by Denis revealed a uric acid content of 7·6 mg.; but on a subsequent examination, seven months later, only 0·8 mg. was found, this, though the patient at the time was on a purin-rich diet. This difference is response to exogenous purins in gouty, as opposed to non-gouty arthritics, is well illustrated in the following table.
According to Walker Hall, the following example illustrates the effect of purin-free as opposed to purin diet on the uric acid blood content in a gouty subject:—
| Uric acid. |
Non-protein nitrogen. |
Urea nitrogen. |
|
|---|---|---|---|
| Mgs. per 100 gms. of blood. | |||
| Gout with purin dietary | 5·5 | 52 | 36 |
| Gout with purin-free food | 3·4 | 40 | 18 |
| Gouty Polyarthritis (Pratt). | |||
|---|---|---|---|
| Milligrams of uric acid in 100 gms. of blood. |
Milligrams of uric acid in 100 gms. of blood. |
||
| D. N. Gout. Purin-free diet. | 3·1 | 52 hours after eating 280 grams haddock roe. | 5·8 |
| 3 days after eating 300 grams roast beef. | 6·2 | ||
| K. Gout. Purin-free diet. | 2·4 | 24 hours after eating 270 grams roast beef. | 3·0 |
| H. Gout. Purin-free diet. | 1·7 | 3 days after eating 150 grams thymus. | 3·6 |
| P. Gout. Purin-free diet. | 2·1 | 3 days after eating 160 grams thymus. | 3·4 |
| J. N. Gout. Purin-free diet. | 2·2 | 48 hours after eating 190 grams thymus. | 8·7 |
| Average | 2·2 | Average | 5·1 |
| Non-Gouty Polyarthritis (Pratt). | |||
| Milligrams of uric acid in 100 gms. of blood. |
Milligrams of uric acid in 100 gms. of blood. |
||
| McC. Chronic polyarthritis. Purin-free diet. | 1·7 | 24 hours after eating 100 grams of thymus. | 2·2 |
| M. Chronic polyarthritis. Ordinary diet. | 2·0 | 24 hours after eating 225 grams of thymus. | 1·8 |
| H. Chronic polyarthritis. Ordinary diet. | 2·9 | 47 hours after eating 190 grams of thymus. | 2·5 |
| Average | 2·1 | Average | 2·2 |
As Pratt points out, if the figures in the two tables be compared, it will be seen that, prior to the sweetbread meal, the average uric acid content of the blood in the gouty and the non-gouty patients was identical. But twenty-four hours to three days, after the purin intake, the average uric acid content of the blood in the gouty was 5·1 mg., while in the non-gouty subjects it was only 2·2 mg.; in other words, in the five gouty individuals a pronounced hyper-uricæmia was produced from one to three days after a purin meal. On the other hand, in the non-gouty subjects the uric acid content was found to be practically unaltered twenty-four to forty-eight hours after the same purine intake.
It would seem, therefore, that some diagnostic importance may be attached to the hyper-uricæmia that is induced in gouty subjects[141] after exogenous purines, as compared with its non-occurrence in non-gouty subjects.
Another interesting point elicited by Pratt was that in his gouty examples, although, after a purin meal, the uric acid content of the blood rose markedly, yet there was no apparent delay or diminution in the output of exogenous purin in the urine. Thus, in one example, after the intake of 190 grams of thymus gland, the uric acid in the blood, in the first twenty-four hours, rose from 2·2 mg. to 4·4 mg., reaching, on the third day, a maximum of 8·7 mg., which, on the fourth day, sunk to 2·7 mg. Nevertheless, 26·2 per cent. of the ingested purin nitrogen was excreted as uric acid. Now, as pointed out in the preceding chapter, it has been shown by many observers that in gouty subjects the excretion of exogenous purin is diminished and retarded. But Pratt’s study of the blood shows that a marked increase and retention of uric acid in the blood may result from the ingestion of purin bases, even when no evidence of retention is found on the examination of the urine.[23]
The clear inference from this is that it is desirable that our urinary findings in respect of uric acid should be reviewed and controlled in light of blood examinations to the same end.
Considerable variations in the uric acid content of the blood, according to Pratt, may occur both in gouty and non-gouty subjects, and which cannot be attributed to any purin intake. Such oscillations, moreover, may ensue within a short time. A patient of his, admitted to hospital suffering from a severe attack of gout, was placed upon a purin-free diet. Twenty-four hours afterwards examination revealed only 2·7 mg. of uric acid in his blood. Subsequently, after having had no food containing purins for fifteen days, it contained 5·1 mg.
Marked variations in the uric acid content of the blood may likewise occur in non-gouty subjects. After being on a purin-free diet for two days, a patient of Pratt’s, with recurrent iritis, had 2·2 mg., while a few months after, when on a mixed diet, his blood contained only 0·8 mg.
Again, great oscillations in the blood content of uric acid, independent of diet, are sometimes found in cases of non-gouty arthritis. Thus, in one chronic case of this nature, the blood when first examined contained 7·6 mg. of uric acid, but a few months later, when on a purin-rich diet, only 0·8 mg. were present. In another instance of primary polyarthritis the same was strikingly exhibited. Aged twenty-two years, the subject in October was on ordinary diet. His blood at that period showed 2·7 mg. of uric acid per 100 mg. of blood; in December, on a purin-free diet, 5·0; and in May, on a similar dietary, 1·6 mg.
As to whether in healthy individuals, on a purin-free diet, similar variations in the uric acid content of the blood occur, is not sufficiently ascertained. The solitary example that may be[143] cited is by McLester, who, as a result of four examinations of the blood in a normal person on a purin-free diet, found that its uric acid content was practically constant.
The deductions that may be drawn from the foregoing findings are:—
(1) That in gouty subjects pronounced variations of the uric acid content of the blood may occur which are not attributable to the purin content of the food.
(2) That in non-gouty arthritis similar fluctuations in the blood content of uric acid, irrespective of diet, also occur.
(3) That in normal persons, on a purin-free diet, the blood content of uric acid, as far as is ascertained, does not show such variations.
If uric acid be causally related to gout, it would seem reasonable to expect that the blood content thereof would stand in some clear relation to the incidence or intensity of attacks.
But, according to Pratt and others, no variations indicative of such a relationship obtain. For, independently of acute attacks, and, moreover, in the absence of any pronounced renal inadequacy, the blood of gouty subjects, even on a purin-free diet, contains, as a rule, 4-9 mg. of uric acid.
More pertinently to our point, in the experience of Daniels and McCrudden, it transpires that, contrary to the usually accepted teaching, typical acute attacks might occur without any variation in the uric acid content of the blood or its excretion.
Nor did their iconoclastic findings cease here, for, mirabile dictu! attacks ensued even when the uric acid blood content was at a sub-normal level; this latter, owing to the victims being at the time on atophan, which increases uric acid elimination. In this connection it is worthy of note that, according to Pratt, the uric acid content of the blood may at times be low, even when atophan has not been taken. In one of his cases, on a purin-free diet, only 1·7 mg. was present, and in another case, on a mixed diet, 1·9 mg.
Daniels and McCrudden, too, note that the uric acid content of the blood in gouty subjects may be persistently lowered, even under the normal average. His, again, has recorded an instance of a gouty subject, with multiple tophi, whose blood did not contain an excess of uric acid. Bloch, also, took 200 c.c. of blood from a man, aged twenty-five, suffering at the time from a typical attack of gout in the big toe; but uricæmia was not present.
Bass and Herzberg injected uric acid into the blood of gouty[144] subjects until its content thereof reached 10 mg. per 100 c.c., this without any joint symptoms supervening. The same observers, aspirating joint fluids in non-gouty subjects, noted that the uric acid content was approximately the same as that of the blood. But, in contradistinction thereto, in two gouty subjects, victims of uræmia, they found in the joint fluids 18·5 and 20·8 mg. of uric acid, while the blood content was only 10 mg. and 8·2 mg.
Furthermore, intravenous injection of uric acid engendered a lesser degree of uricæmia in the gouty—this despite impaired renal excretion. To their mind, therefore, the inference was that the bodily tissues in gout display an enhanced capacity for taking up uric acid.
Lastly, Walker Hall, discussing the question as to whether any relation obtains between the degree of uricæmia and the onset of acute attacks, observes that, “the evidence is more general than specific.” Thus he reminds us that excessive intake of purin food has sometimes been followed by, or associated with, an acute outbreak. Also, that the leucocytic destruction which occurs during acute lobar pneumonia and after the use of X-rays has occasionally coincided with an acute paroxysm. To this, again, must be added the fact that atophan curtails the duration of acute attacks, apparently by exciting an increased uric acid output. Superficially regarded, these facts might appear to be conclusive; but, as Walker Hall states, it must be recalled that overeating, overdrinking, trauma, mental disturbances, atmospheric vicissitudes, and bacterial infections have also preceded acute outbreaks.
To sum up, the main conclusions deducible from the foregoing clinical and experimental findings would appear to be that:—
(1) No constant relation has as yet been established between the uric acid content of the blood and acute attacks of gout.
(2) No variations in the same apparently herald or accompany typical acute paroxysms.
(3) Attacks may occur with a sub-normal uric acid blood content.
(4) The tissues of gouty subjects apparently possess an enhanced binding capacity in respect of uric acid.
(5) Given impaired renal excretion in gouty subjects, the uric acid content of the joint fluid rises markedly, exceeding that of the blood.
While the researches of the past decade have proved distinctly encouraging, yet we must not blind ourselves to the fact that the foregoing findings, and alike our deductions therefrom, are largely provisional; for we stand in grave danger of over-emphasising the[145] significance of the results forthcoming from the investigation of isolated samples of blood from different individuals. The recorded estimates of the uric acid content of the blood in strictly normal persons are all too few, the findings in diseased subjects too conflicting, to warrant dogmatic inferences, wide generalisations. In truth, the problem is by no means as simple as may at first sight appear, and this but a slight digression will suffice to make clear.
The Significance of Uricæmia.—It is generally maintained that the blood content of uric acid in gout is above normal. Yet the excretion of uric acid, save during acute attacks, rests within physiological limits. Again, à propos of our claim that the blood is surcharged therewith, we have the awkward fact, as yet inexplicable on chemical or physico-chemical grounds, that the blood-stream can hold in suspension far more uric acid than has ever yet been met with in gout, according to Bechhold and Ziegler no less than 50 mg. of uric acid per 100 c.c. of blood serum before deposition tends to occur. On the other hand, urates are less soluble therein, not exceeding 2·5 mg. per 100 c.c. How remote from the limit of saturation the highest figures observed in gout! What a large margin of solubility is still available!
Again, the uric acid blood content in gout is far less than was formerly thought. Only by a few milligrams does it transcend that found in normal individuals. Can this slight disparity have such profound potentialities as to determine the incidence or not of gout? and this with the saturation point still so remote. The urates, too, being practically non-toxic, how difficult to conceive that the almost trivial excess of the uric acid blood content over the normal is adequate to produce the fulminant and dramatic phenomena of acute gout.
Again, though we speak of uricæmia as a dominant characteristic of gout, we are uncertain whether the alleged increase in the uric acid content of the blood is real or merely apparent. We can, it is true, extract uric acid and urates from the blood-stream, but it does not necessarily follow that it is as such that they circulate in vivo. We need walk circumspectly here for, despite the most modern methods of blood analysis, we are still ignorant as to the exact form in which uric acid exists in the blood-stream; whether the purins of the food appear in the blood-stream as sodium monourate, or in organic fusion. Accordingly, in the interests of progress, it were well to bear in mind the pitfalls that beset uric acid estimation, the insufficiently eclectic capacity of even the most modern tests, and to consideration of these more chastening aspects we now proceed.
Sources of Fallacy in Uric Acid Estimation.—With Folin’s findings as his basis, Walker Hall estimates that, excluding the[146] lymphatics and lymph spaces, the entire blood-stream contains normally 70 mg. of uric acid, i.e., 2 mg. of uric acid per 100 grams of blood, 3,500 c.c. (total quantity of blood).
Thence he argues that, inasmuch as about 1 litre of blood traverses the kidney per minute, the total content thereof of uric acid would gain access to the renal organs in three and a half minutes. Now the average total output of the kidneys is 500 mg. per twenty-four hours. Accordingly, assuming that the blood arriving at the kidneys contains as a constant the above 70 mg. uric acid, the total daily output would pass through these organs in twenty-five minutes.
Now, given immediate extraction of all the uric acid by the renal cells, then the blood in the renal veins will become free of uric acid. If so, the estimates of the uric acid content of the blood will reflect exactly the measure of the endogenous or exogenous nuclein metabolism. But, “if the renal vein blood is not purin-free, then the estimations will fail to yield a true picture of the activities of nuclein exchange.”
Again, as to the precise import of isolated estimates of the uric acid blood content, we must recollect that the excretion of purins is not distributed evenly over the twenty-four hours, varying as it does under the influence of food, exercise, sleep, and other factors. A propos of this, Pratt’s observations clearly show that both in gouty and non-gouty subjects fluctuations in the uric acid blood content also occur, and this independently of diet. To what, then, may these variations be referred? Obviously a question of great moment, especially when we recall the eccentric behaviour of the blood uric acid in relation to the incidence of acute gouty attacks. For, until the inward meaning of these vagaries is revealed, the value of recorded estimates must necessarily be discounted considerably.
We must recall, too, that a certain moiety of the purins derived from nuclein metabolism lags in the lymph spaces and lymphatics, and this, as Walker Hall reminds us, must reduce the quantity present in the blood-stream at any one time. Also, as the same authority reflects, the lymph stream being probably richer in sodium ions than the blood, the entry of the nucleins therein may be retarded and so lead to a still further reduction of the blood content.
There is yet another possibility, he reminds us, viz., “that the purin content of the blood varies in the peripheral pulmonary hepatic and osseous streams, and that, while in some parts the purins are being carried to the kidneys for excretion, in others they are being transported from one organ to another for further metabolism.”
For, as before pointed out, the enzymes responsible for the ultimate disruption of the nucleosides are scattered in different organs, and Walker Hall suggests that “a transport of half metabolised nucleotides from one organ to another may form a part of the normal processes of nuclein metabolism.” This may well lead us on to consider the limitations that beset even the most modern tests in use for uric acid determination.
Disabilities of Modern Tests.—With all its outstanding advantages, even the Folin method of uric acid estimation has its drawbacks. As Curtman and Lehrman have pointed out, different workers have, even on identical blood samples, arrived at results which vary widely. Nor, disconcerting though it be, do the limitations of this mode of hæmo-analysis cease here.
Thus we know from Gudzent and Apolant that the soluble but unstable biurate is constantly being transmuted into an insoluble stable type, in other words, metamorphosis from one isomer into another. But, unhappily, the tests to hand fail of differentiation of the several tautomeric forms of uric acid. Also, as isomers of uric acid actually exist, then quâ Walker Hall, why not isomers of purins and pyrimidins also? But here again our tests are insufficiently eclectic. They give us no clue as to the affinities or blends of purins or pyrimidins for or with other substances.
Again, as our criteria fall short of identifying the exact form of the “purin combinations” it follows, therefore, that they tell us nothing as to whether “the increase is due to a more active transport of purins from one organ to another for further metabolism or simply to a transport to the kidneys for elimination.”
In other words, hampered by the above disabilities in our tests, it is beyond our power to determine whether “the increases denote a supernormal nuclein metabolism or an unusual type of nuclein cleavage.” Should it ultimately transpire that the increase in the purin blood content is a real one, viz., made up of “an excess of normally formed and normally bound purins,” a great step forward will have been achieved. For, to account for the same it will, as Walker Hall observed, be necessary to postulate a supernormal nuclear activity of generalised or localised distribution.
Need for Further Investigations.—While none can doubt that, by means of chemical investigation of the blood, the clinical problem of gout will be elucidated to a much greater extent than has been possible by means of urine analysis, still much remains to be done before recent findings can be applied to the solution of the etiology of gout.
The results of blood analyses up to now have afforded us no clue as to the intimate nature of the warp in nuclein metabolism. At[148] the most, the researches in this sphere do but make it increasingly clear that uricæmia is not the cause but the result of gout.
Albeit, this conclusion does not justify us in putting out of court all thought of uric acid in connection with gout. Any tendency thereto will be immediately checked when we recall that uratic deposits, i.e., tophi constitute the solitary unequivocal token of gout, and to this aspect of the question the ensuing chapter will be devoted.
Meanwhile, systematic investigations of the purin content of the blood, not only in gouty but in normal subjects, would surely dissipate much of the obscurity that envelops this complex question. It were well, too, that blood and urine analyses go hand in hand in our investigations. How illumining these have been in connection with atophan, the increased urinary output of uric acid having been found to be correlated with a simultaneous sinking in the level of the uric acid of the blood.
Again, the excretion of urinary purin ebbs and flows with the intake of food and the degree of muscular activity, while sleep also exerts an influence, not to mention constitutional disturbances, e.g., fever infections, etc.
Can it be doubted that the blood content of uric acid varies with these same vicissitudes? Walker Hall tells us that the data to hand, “as to the rapidity of the appearance of purins in the blood-stream after food, infections, fever, etc.,” though few in number, yet suggest that “the excretion by the kidney is tidal in character, and that the blood uric acid has similar characteristics.” In light of these possibilities, we may well pause before attempting to appraise exactly the significance of isolated blood examinations.
What, too, as the above authority observes, of the influence on the gouty uricæmia of infancy, puberty, the menopause, and for that matter the pre-senile and senile periods of life with their associated vascular lesions? The researches of Uffenheimer prove that even in young children the disorders of purin metabolism distinctive of gout are to be met with, i.e., “infantile gout.”
We stand also in urgent need of knowledge as to the uric acid blood content in the early as opposed to the late stages of gout; in need, too, of further examinations of the blood to this end, not only during the passage of acute attacks, but even more under those conditions which are presumed to determine their incidence.
But, despite these gaps in knowledge, these disabilities of technique, there is no need for despair. “It is a slow progress along the zigzag which leads to the centre of the ‘gouty maze,’ but the researches of the last decade have opened up many new and possible pathways thereto.”
The two salient features of the gouty diathesis are:—
(a) The tendency to excess of uric acid in the blood, i.e., hyper-uricæmia, and
(b) The tendency to uratic deposition, i.e., uratosis.
With the former we have dealt, but before passing to discuss the latter, it will, we think, be advisable to review both these morbid tendencies in relation to gout.
Hyper-uricæmia and uratosis, though they both occur in gout, are by no means of identical pathological valency or significance. In hyper-uricæmia the uric acid, either in a free state or combined, circulates in the blood and lymph. In uratosis the uric acid is anchored in solid form in the substance of the tissues. In the former, then, the uric acid, if it be noxious, acts as a chemical poison, in the latter as a mechanical irritant.
But the more striking contrast is that while hyper-uricæmia is not restricted to gout, but occurs in many other disorders; on the other hand, uratosis is absolutely confined to the gouty state, constituting its pathognomonic stigma.
Again, hyper-uricæmia may exist for prolonged periods without producing uratosis. But uratosis cannot, as far as is ascertained, occur without a co-existing hyper-uricæmia. From these disparities it may legitimately be inferred that the factors responsible for the genesis of hyper-uricæmia and of uratosis, are not identical; in other words, that in uratosis some other agency or agencies are at work over and beyond those that beget hyper-uricæmia.
Lastly, inasmuch as uratosis stamps the seal of specificity upon gout, it follows, from this and the above considerations, that there is a more intimate relation between gout and uratosis than between gout and hyper-uricæmia, and that the factors which make for uratosis have a more intimate bearing upon the pathogeny of gout than those which lead to hyper-uricæmia.
The view that tophi were composed of chalk prevailed for centuries. As we see such was the conception of Virgil, and in our[150] own country John Hunter entertained the same erroneous notion, while amongst the laity this view as to their nature is held widely even to-day as it was in the time of Dryden.
Albeit, the term “chalk-stones” is a misnomer, as tophi, when pure, may be wholly devoid of lime. Modern analyses, too, have failed to demonstrate the presence of calcium carbonate, the essential ingredient being urate of soda.
On the authority of Rendu, we have it that Tennant and Pierson were the first to demonstrate the presence of uric acid in gouty deposits, which discovery was later confirmed by Fourcroy and Wollaston (1797), these latter observers showing that they consisted almost exclusively of urate of soda.
Subsequently to Wollaston’s day, many analyses have been conducted, by Marchand, Lehmann, Wurzer, and Langier, L’Heretier, Ebstein and Sprague. Of the various findings we append those by Marchand, Lehmann and one of later date by Ebstein and Sprague.
| Urate of soda | 34·20 |
| Urate of lime | 2·12 |
| Carbonate of ammonia | 7·86 |
| Chloride of sodium | 14·12 |
| Animal matter | 32·53 |
| Water | 6·80 |
| Loss | 2·37 |
| 100·00 |
| Urate of soda | 52·12 |
| Urate of lime | 1·25 |
| Chloride of sodium | 9·84 |
| Phosphate of lime | 4·32 |
| Cellular tissue | 28·49 |
| Water, loss, etc. | 3·98 |
| 100·00 |
| Uric acid | 59·70 |
| Tissue, organic matter | 27·88 |
| Sodium oxide | 9·30 |
| Potassium oxide | 2·95 |
| Calcium oxide | 0·17 |
| MgO, Fe, P₂O₅, S | Traces. |
It will be seen that all of them agree more or less closely as to the essential ingredients being uric acid and soda. According to Ebstein and Sprague they consist usually of almost pure biurate of sodium and potassium. But, as a rule, after a time calcium salts are deposited. Dunin, it may be noted, has found deposits resembling gouty tophi, which contained only calcium salts. Kahn, again, claims that tophi do not always consist solely or even largely of urates, but that these may be replaced by calcium salts. It may be added, too, that M. B. Schmidt has recorded, under the designation of “Calcium gout,” a case in which there existed a generalised deposition of calcium, and this in tissues other than those usually involved in “metastatic calcification.” But, to sum up, although there may be admixture of lime salts and organic matter, the salient chemical constituent of tophi is biurate of sodium.
Gouty tophi, like all pathological concretions, are laid down in accordance with a definite law. In the first instance, a central nucleus is essential. To this must be added a “binding substance” or structural framework of different nature from the main mass of the concretion.
Garrod, discussing the intimate structure of “chalk-stones,” observes that, “the large amount of phosphate of lime occasionally met with is probably derived not only from the tissue in which the chalk-stones have been developed, but likewise from secondary deposition, the result of ordinary inflammation around the original nucleus (urate of soda) which acts as a foreign body.”
It is, however, quite possible that some substance other than urate of soda constitutes the primary nucleus, for, as we now know, concretions most frequently gather around masses of mucin, clumped bacteria, desquamated cells, precipitated proteins, etc. Thus, the renal uric acid infarcts, supposed to result from disruption of the nucleo-proteins of the fœtal nucleated red corpuscles, take origin around injured epithelial cells, which latter form the nucleus.
As to gouty tophi, too, it has been suggested that they form in response to any toxin, resistance to which may involve death of the tissue cells with consequent disruption of their nucleins and formation of urates. Such was the view held by Woods. Hutchinson, who also thought that the calcareous accretions might be regarded as “protective,” analogous to the formation of shells in the invertebrates, the process here consisting in the deposition of lime salts in cells already saturated with uric acid and urates.
In any case, whatever be the exact nature of the nucleus, the[152] urate of soda collects thereupon, the acicular crystals tending to assume the form of radiating needles. But the successive depositions not being of regular incidence, the surface of the crystals, in the intervals of quiescence, becomes covered by mucin, animal or earthy matter. Hence, the concretions display not only a radiating, but a concentric or laminated structure.
The mucin acts as the “binding substance,” the crystals lying in its meshes, and, moreover, remaining as the framework of the concretion even after the crystals are dissolved out; in other words, the gouty tophus is made up of a blend of crystalloids and colloids, evolved from solutions of the same character.
The importance of recognising the true nature of this binding substance, i.e., mucin, merits a brief digression, in light of Ebstein’s view that local tissue necrosis is a necessary antecedent to uratic deposition. Now, exhaustive studies of the histology of uratic deposits, both those experimentally induced and of spontaneous gouty origin, have been conducted by Freudweiler, His, Krause, and Rosenbach.
All their results, according to Gideon Wells, “indicate that uric acid and urates excite some slight inflammatory reaction, cause a slight local necrosis, and seem to act as a weak tissue poison.” According to Rosenbach, however, this sequence is not invariable, inasmuch as he noted that such deposits may occur without inducing necrosis. More pertinently to our contention, however, is it that Krause’s experience seems to indicate that errors of interpretation were possible. Thus, he suggests that part of the material in the areas of uratic deposits merely constituted the framework of a crystalline deposit, though such were currently regarded as strands of necrotic tissue.
But, to resume, tophi being blends of crystalloids and colloids, we must recollect that the suspension capacity of colloidal solutions for crystalloids is much superior to that of simple solutions, by reason of the fact that at the surface of each colloidal particle there exists a zone in which the crystalloids are much more closely aggregated than elsewhere, thus permitting more crystalloids to be dissolved in the solvent between the colloidal particles. But, be it noted, this same tendency to concentration of the crystalloids at the surface of the colloidal elements leads to the colloids acting as determinants of precipitation when crystalloids are in excess. Accordingly, when the crystalloids pass out of solution, they form crystals or precipitates intimately blended with the colloids. Thus, for example, when uric acid crystallises out of urine it carries with it the colloidal pigments. On the other hand, if the colloids are precipitated, the solvent capacity of the solution being[153] consequently depreciated, the crystalloids are deposited in intimate relation with the colloids.
Again, Schade has pointed out that colloids may precipitate in reversible form or not. If in irreversible (e.g., fibrin) form, the concretion will remain permanent. But if the colloidal precipitate is reversible, it may be redissolved, as happens with the uric acid infarcts of the infant’s kidney. In conclusion, we see, therefore, re crystalloids and colloids in animal juices, that the conditions of their solubility are most complex, and though they do not explain the nature of gout, the variations doubtless stand in intimate relation to the formation of tophi.
Uratic deposits evince a decided predilection for cartilages, tendons, muscles, and skin. This localised distribution of the depositions would seem to suggest their dependence on local tissue peculiarities. Now the presence of sodium salts in a solution diminishes the solubility of urates therein. Consequently, in seeking to explain the incidence of tophi, it was suggested that cartilage and tendons, being richer in sodium ions than the blood, this might account for the fact that urates tend to be precipitated in these particular structures.
Again, Almagia, working in Hofmeister’s laboratory, noted that thin sections of cartilage, if left for some hours in a solution of sodium urate, will take up uric acid. Direct inspection readily reveals the presence of white foci and diffuse opacities due to uratic deposits. The marked affinity of normal cartilage for uric acid is again attested by the fact that, given injection thereof in quantity into the peritoneal cavity of rabbits, the uric acid may often be detected by the murexide reaction in joint cartilage, though apparently not in other tissues.
This behaviour would appear to justify the conclusion that the observed accumulation of uric acid in the cartilages in the presence of states of uricæmia, may be explicable on this same basis. In any case, this marked affinity of even normal cartilage for uric acid seems to disprove the necessity of Ebstein’s postulate, viz., that the dissolved uric acid sets up inflammation, and that an antecedent necrosis precedes the deposition of urates. Still, even if we concede the fact that normal cartilage has a marked affinity for uric acid, how is it that in leukæmics, despite their high blood content of uric acid, no uratic deposits ensue? Does not such disparity seem to indicate that in gout some other factor intrudes? in other words, that the excess of sodium ions in particular tissues, while it may favour deposition therein, is[154] inadequate of itself to actually determine the formation of tophi.
Many and divers are the theories that have been propounded to account for the genesis of tophi. For some their incidence would appear to predicate something abnormal in the conditions of uric acid solution and circulation. Others have pinned their faith to some affinity on the part of the bodily tissues for uric acid—an enhanced retention capacity on their part for this substance. Some again, impressed by the objective changes that mark the clinical evolution of tophi, have been led to regard them as concomitants or sequels of gouty inflammation. But, be the true explanation what it may, we may well preface our discussion of the various theories by the obvious comment, viz., that the origin of tophi must doubtless depend in the ultimate upon constitutional or systemic, as well as local, factors.
In the older conceptions of the pathology of gout the hypothesis that found most vogue was that the separation of uric acid from the blood into the tissues was due to diminished alkalinity of the blood and tissue juices; but, as before pointed out, it has been established that the alkalinity of the blood is not reduced, and the theory has consequently been abandoned.
But, with the advent of Gudzent’s findings, viz., that uric acid existed in two forms—one soluble and unstable, and the other insoluble and stable, and that the former is constantly changing into the latter—another conception of the origin of tophi arose. It was supposed that, by reason of the disparity in solubility of these tautomeric types of uric acid, the blood in gouty subjects must at times be in a state of super-saturation with uric acid; and, moreover, that equilibrium could only be restored through abstraction of the urates by crystallisation.
Unfortunately for this theory, it has been shown that the blood of gouty subjects is not super-saturated therewith; indeed, over and above the highest increments hitherto met with in gouty blood, a considerable margin of solubility for uric acid is still available. In truth, the problem is by no means so simple; for the conditions governing the solvency of uric acid in the blood are bewilderingly complex, subject as they are to the manifold variations in solubility exhibited by crystalloids in the presence of the many divers colloids.
But, to resume, Minkowski, it will be recalled, noted that[155] from a mixed solution of uric and nucleinic acids the former cannot be precipitated by either acetic acid or alkaline ammonio-silver-magnesia mixture. Accordingly he advanced the view that uric acid “primarily exists in the blood and the tissue juices in combination with nucleinic acid, and that, not only the conversion of the purin bases into uric acid, but also the solubility and transportation, as well as the further changes of the uric acid in the living body, is regulated by this linking with a nucleinic acid rest.”
But, unfortunately for the value of this hypothesis, there is no proof that nucleinic acid is actually present in the blood; for, as Fürth remarks, is this inhibition of the precipitation of uric acid, in the presence of nucleinic acid, “necessarily indicative of a true acid combination with nucleinic acid,” “but such inhibition of precipitation is rather to be referred to the general group of variations of solubility which are manifested by crystalloid substances in the presence of all sorts of colloids.”
Complex phenomena of solubility of this nature must be considered in connection with the circulating uric acid. Nucleinic acid is not the only important substance, but “the general mass of the blood proteins must be particularly thought of.”
Continuing, Fürth reminds us that uric acid is much more soluble in blood serum than in water, and forthwith envisages this disparity in light of the factors that affect solubility of uric acid in the urine. The latter is markedly influenced by the presence of urea and di-sodium phosphate, and the relation of this to mono-sodium phosphate. Nor, he reflects, is there any doubt “of the importance of such inter-relations, too, in the formation of uric acid deposits in the tissues.” But he adds, “Although the importance of these complex conditions of solubility as they prevail among colloid and crystalloid substances in the animal juices may be accepted in relation to the formation of uric acid concretions, there is no real reason for seeking the explanation of gout in this sphere.”
It might be thought that some relationship might be established between uratic deposits and the degrees of uricæmia, but the data to hand give no countenance to the assumption. Thus, His has recorded the case of a gouty subject with multiple tophi whose blood did not yield an excess of uric acid. Pratt, again, could trace no relation between the amount of uric acid in the blood and the severity or character of the disease. Two of his patients had[156] numerous and widely distributed large deposits of sodium urate beneath the skin, yet the blood content of uric acid in both was less than the average amount found in gout. Thus, on a purin-free diet, one had 2·4, the other 2·2 mg. These findings, he considers, show that the presence of multiple tophi is no indication that a state of hyper-uricæmia exists.
Walker Hall, discussing this same question, holds that there is but little evidence “as to the relation of uricæmia to the formation of tophi.” He asks the question whether the deposition is the outcome of abnormal purin combination in the blood and lymph stream? which latter at present, he states, are regarded as passive carriers of the urates. For, he says, the small purin increase in gouty blood cannot surely make all the difference, seeing the large volume of solubility still available. The physico-chemical hypothesis, he claims, is inadequate to explain the relationship between uricæmia and the tophi, and hazards the suggestion that after all it may be that “the uricæmia plays little or no part in the depositions, and that these are due to the defective removal of substances resultant from local nuclear activities.” He asks, moreover, whether such substances differ in type from those of normal nuclein metabolism and so fail to be suspended in the surrounding lymph in such a way as to ensure their entrance into the blood-stream? Like others, he notes that atophan brings about a removal of some of the deposited urates. But such diminution of the tophi may, of course, he says, be due to increased flow of serum to the inflamed part; though, on the other hand, the more massive deposits “are surrounded by layers of young granulation tissue and phagocytes and peritophal fibrous tissue, and these in turn offer some hindrance to the permeation of serum or drugs.”
In reviewing the foregoing views as to the formation of tophi, it is obvious we stand in urgent need of more knowledge. Neither the chemical nor the physical theory or a combination of the twain seems adequate. This for the salient reason that, as far as the existing evidence permits us to draw conclusions, it would seem probable that not only local but constitutional or systemic conditions play an important rôle in tophi formation.
But as far as our discussion has advanced, we may, we think, be justified in the following deductions:—
(1) That tophi are blends of crystalloids and colloids and subject to the complex conditions of solubility attaching to such combinations.
(2) That the relatively high sodium content of certain tissues, e.g., cartilage, favours the incidence of uratic deposits therein.
(3) That tissue necrosis is not necessarily an antecedent to uratic deposits.
(4) That no relationship can be established between the incidence or multiplicity of tophi and uricæmia.
It will be seen from these conclusions that the proximate cause responsible for the genesis of tophi is yet to seek, and in pursuance of our quest we turn to another aspect of this complex subject.
Injecting uric acid intravenously into gouty subjects, Umber noted that at times the whole was retained, but on some occasions was excreted in fractional portions. On the other hand, a normal individual under similar circumstances eliminates it completely. In explanation thereof, he proffered the opinion that this failure on the part of gouty persons to excrete exogenous uric acid was due to a special affinity of their tissues for uric acid.
As to intravenous injection of uric acid, however, modern investigation has established that, both in normal as well as gouty subjects, its excretion is spread over several days, and the whole is not recoverable from the urine. Now this incomplete excretion or retention of uric acid was attributed to defective elimination by the renal cells; but, as shown in a previous chapter, this conception fails of demonstration. Nor, for that matter is there any proof either that the retention is due to fixation of the uric acid in the blood serum. Accordingly, to our minds, it is permissible then to canvass the further possibility adumbrated by Umber, viz., that an increased affinity of the tissues for uric acid may haply account for the diminished purin excretion, the excess of uric acid in the blood, lymph, and tissues, and that these same may lead to uratic deposition.
This last hypothesis derives colour from the findings of Schmoll, Magnus Levy, Vogt, Reach and Bloch, who noted that, after giving thymus to gouty persons, they found far less uric acid in the urine than in the case of normal subjects. Also, that the ingestion of thymus by the victims of chronic gout repeatedly resulted in acute outbursts of the disease. Moreover, as we saw when discussing the sources of uric acid, there are cogent reasons for avoiding a too restricted conception which would make the leucocytes, the muscles, or the digestive glands alone responsible for the endogenous production of uric acid; in other words, that a more catholic attitude on our part is indicated, one which would envisage it as the outcome of continuous and general cellular wear and tear. That an increased cellular destruction, as induced experimentally, e.g., by exposure to Röntgen[158] rays, is capable of raising the blood content of uric acid in a gouty subject, and of precipitating a gouty paroxysm, may be inferred from the researches of P. Linsen.
It may be recalled that Wiechowski and others observed that in man, of parenterally introduced uric acid, 80-90 per cent. reappears in the urine. Accordingly, Schittenhelm and Wiener argued that, if uric acid is indestructible in the human body, then, given retarded elimination, the tissues should contain considerable quantities thereof. Subsequently, in 1914, they sought to investigate human tissues as to their content of uric acid. Their studies were conducted on three examples, a case of anuria, one of pernicious anæmia, and one of gout.
The case of anuria occurred in a male, aged sixty-two, in sequence to thrombosis of both renal veins following operation. Two-hundred gram samples of the following tissues, lung, heart, spleen and liver, were examined for uric acid with wholly negative results. The residue of the organ was worked up together, but only 0·01 gram of uric acid was isolated.
In the case of pernicious anæmia no uric acid was demonstrable. The gouty subject had for twenty-five years suffered from typical attacks and exhibited many auricular tophi. The following organs, in their entirety, were analysed, the liver (1,550 gram), no uric acid; spleen (290 gm.), 10 mg. uric acid (3·5 mg. per 100 gm.); kidney (270 gm.), no uric acid; lung (930 gm.), 15 mg. uric acid (1·6 mg. per 100 gm.); muscle (440 gram), no uric acid; and intestine (420 gram), no uric acid.
It will be seen that uric acid was either absent or present in minimal amounts, and these results Schittenhelm and Wiener interpreted as confirming their long advocated contention as to the destructibility of uric acid in the human organism.
Morris S. Fine, from the results of similar investigations, considered the failure of these observers to isolate uric acid in these cases of anuria and gout as most remarkable. He considers “their results may in part be ascribed to the use of hot sodium hydroxide previous to the precipitation of the proteins in the extraction of the tissues, as the instability of uric acid in alkaline solutions is a well-known property.”
In this criticism Fine would appear to be fully justified, in view of the marked contrast between the findings of Schittenhelm and Wiener, and his own data is recorded in the tables on p. 159.
While it is unfortunate that Fine’s theory contained no instances[159] of gout, his findings are a definite proof that, to quote his own words, uric acid can be demonstrated in considerable concentrations in human tissues. Incidentally, also, his tissue analyses are flatly contradictory to Schittenhelm and Weiner’s persistent contention, viz., that the human organism can decompose uric acid.
Gideon Wells states that in normal individuals the tissues contain but little uric acid, and this not in quantities sufficient to permit readily of its isolation in a pure state. Albeit, Wells found considerable amounts of uric acid in the tissues of a young woman who, in sequence to poisoning with HgCl₂, died after complete suppression of urine for nine days.
| Case. | E. E. Uremia. | T. D. Uremia. | S. H. Uremia. | M. F. Diabetes. | C. M. Diabetes. | S. T. Amputation. | H. J. Pneumonia. |
|---|---|---|---|---|---|---|---|
| mg. | mg. | mg. | mg. | mg. | mg. | mg. | |
| Blood | 15·4 | 14·3 | 17·0 | 0·7 | 0·7 | 0·7 | |
| Pleural fluid | 16·7 | 15·9 | |||||
| Ascitic fluid | 18·0 | ||||||
| Pericardial fluid | 14·3 | 18·0 | |||||
| Subcutaneous fluid | 18·0 | ||||||
| Spinal fluid | 2·8 | 2·0 | 4·7 | ||||
| Skeletal muscle | 8·0 | 3·9 | 5·8 | 0·7 | 2·6 | 2·0 | |
| Heart muscle | 10·0 | 7·3 | 8·8 | 1·2 | |||
| Liver | 18·0 | 15·6 | 11·5 | 5·0 | 4·0 | ||
| Spleen | 12·6 | 14·3 | 9·1 | 1·2 | Trace | ||
| Skin | 13·0 |
| Tissue. | Uric acid. |
|---|---|
| mg. | |
| Pectoral muscle | 2·5 |
| Uterine muscle | 2·0 |
| Uterine muscle | 2·5 |
| Uterine muscle | 1·2 |
| Mixed tonsils | 1·7 |
| Thyroid | 0·0 |
Again, as before alluded to, Bass and Herzberg found that[160] intravenous injection of uric acid caused less uricæmia in the gouty, despite diminished renal excretion. Hence, they concluded that in gout the retention capacity of the tissues for uric acid is augmented.
Fürth, an ardent advocate of Umber’s hypothesis, emphasises the fact that Wiechowski was never able to detect any evidence of uricolysis in the human body. Continuing, he observes, if we reject all idea of uric acid retention in the tissues, “It would be a particularly difficult thing to understand why gouty patients do not simply expel by a compensatory hyper-excretion the uric acid which is accumulated from a supposed failure of uricolysis; precisely as in leukæmia the patient compensates simply by an exaggerated excretion of the excessive uric acid which is mobilised in the body from the excessive purin decomposition.” His conclusion, therefore, is that, “In the gouty individual there must exist some cause which makes a compensatory uric acid excretion impossible; and that is plainly a retention affinity of the tissues, because of which the uric acid is actually held in the tissues.”
In light of Fine’s revelations the retention capacity of the bodily tissue for uric acid may, we take it, be considered as fairly well established. But, in view of the precipitation or anchoring of urates in the tissues in gout it is most desirable that further investigations be made to discover whether in gouty subjects the tissue retention capacity for uric acid is enhanced.
“The impression,” says Fürth, “grows on one that this hitherto little considered factor, of an increased affinity of the tissues for uric acid in the gouty subject is very much closer to the real kernel of the gout problem than, for example, the question of the fixation of uric acid in the blood about which there has been so much contention, and with which of necessity we are compelled, at least, to some little extent to concern ourselves.” The results of modern researches tend to support this more catholic conception. We would recall that Lewis and his co-workers, seeking the source of the increased endogenous purin excretion that follows ingestion of purin-free food, were forced to reject the view that it was solely derived from katabolism of the nuclear substance of the digestive glands, and to refer it instead to “wear and tear” of the body cells as a whole. Precisely the same change in attitude, we may remind our readers, has overtaken us in regard to the site of urea formation, viz., that not only the liver cells, but those of the muscles also participate in its production.
While admitting that dogmatism is out of place, still to our mind this theory of tissue retention makes strong appeal. In light of it the nebulous “gouty diathesis” seems on its way to become incarnate in some inborn peculiarity of tissue-function, a falling[161] short of full physiological activity, or, as M. Rendu termed it, a “primordial vice of nutrition.”
In other words, in gout there is no rift nor lack of finish in the orderly sequence of enzymatic reactions that eventuate in uric acid. Uric acid is formed and, as far as we know, after a normal fashion. But, here comes the flaw, viz., the uric acid, when formed, fails of transport and elimination. It is precipitated and anchored in the tissues, from whose grip it fails to detach itself. In short, it is not the formation of uric acid, or its failure of further metamorphosis, but the retention of uric acid, and more pertinently, its fixation in the tissues that constitutes the salient feature of gout.
Now, all modern research tends to indicate that uric acid is not an intermediary, but a terminal product of metabolism, and, moreover, that there are no uricolytic ferments within the body whereby its destruction can be accomplished.
If we grant that—
(1) Uric acid is not an intermediate but an end-product of metabolism; and
(2) That the human body is devoid of uric acid-destroying enzymes,
then it follows that man, ipso facto, is potentially liable to uric acid retention and deposition, the same objectivated as tophi. In this innate potentiality of and to uratosis resides the “gouty” diathesis.
If the postulates (1) and (2) be established, then, though it sound rank heresy, it follows that gout is not, chemically speaking, an “error of metabolism.” Not, at any rate, in the ordinary acceptation, viz., not a failure in the transmutation of uric acid into urea and intermediate products. If uric acid be an end-product, then no further cleavage into urea, etc., occurs, and in this connection the failure to discover uricolytic enzymes is significant.
We have before proffered the suggestion that not only local, but constitutional, or systemic influences also play a part in the origin of tophi. Provisionally, therefore, we would infer that—
(1) The tissues of gouty subjects display an abnormal affinity for uric acid, i.e., an increased retention capacity for the same;
(2) That certain chemico-physical factors, previously alluded to (content of sodium ions, etc.), favour the incidence of uratic deposits in particular tissues.
In other words, we have in these two elements haply the constitutional and local factors that we postulate as essential to the formation of tophi. Albeit, they represent but latent tissue[162] potentialities, inadequate of themselves to determine the eruption of tophi.
Moreover, be it recalled that the causa causans of gout must be responsible not only for the incidence of tophi, but also for the more dramatic features of gout, its arthritic outbreaks, etc. To dissociate the cause or causes of the uratic deposits from that of the joint inflammations would indeed appear impermissible.
But, taking this view, it is clear that, apart from the constitutional and local factors above postulated, tophi and, alike, the arthritic phenomena of gout, demand for their production the intrusion of some further element, some tertium quid, vital and biological. To this end, therefore, we purpose reviewing tophi in their clinical aspects, as herein possibly we may find some further clue to their exact mode of genesis.
As to the clinical characters that mark the genesis and maturation of tophi not a little conflict of opinion seems to obtain. Do tophi arise painlessly or not? Do the uratic depositions occasion any local inflammatory reaction? Or, are they merely concomitants or sequels thereof?
With what wearisome iteration has the same question been propounded in regard of gouty arthritis. Are the attacks of pain and inflammation due to deposits, or do the deposits take place at the site of inflammation?
But, restricting our enquiries to tophi, we may remind the reader that Aretæus, writing in the second century, A.D., made the following observations: “Callosities also form in the joints; at first they resemble abscesses, but afterwards they get more condensed, and the humour being condensed is difficult to dissolve; at last they are converted into hard white tophi (Πῶροι στερροὶ λευκοὶ), and over the whole there are small tumours like vari and larger, but the humour is thick white and like hailstones” (Περὶ Αρθριτιδος). To our mind, it would be difficult to emulate, much less to surpass, the succinct and, as we believe, accurate picture here drawn of the various stages that mark the life history of tophi. It will be noted that Aretæus says that in their initial stages they “resemble abscesses,” and, turning to the writings of the elder Garrod and others, we find abundant evidence that it is so.
Discussing the more frequent incidence of tophi in the hands than in the feet, Garrod describes the physical characters presented by tophi in the making as seen in one of his examples of gout. “On the dorsal surface of the second phalangeal joints of three fingers, small rounded protuberances were observed, the[163] skin over them being red; these bulgings appeared soft, as if containing a thick fluid, but not the slightest indication of white matter could be seen through the skin; they might have been either gouty concretions in their early stage of formation or some other form of swelling; from a simple inspection I could form no opinion as to their true nature, but their history convinced me that they arose from a deposit of urate of soda. Upon puncturing one of the little swellings, full light was thrown upon the case, as a thick white fluid immediately exuded, a drop of which placed, under the microscope, with the use of polarised light, gave the appearance represented in Fig. 1; the crystals were proved by analysis to consist of urate of soda.”
We see, therefore, that Aretæus and Garrod were at one in their observation that tophi in their initial stages are betokened by small red swellings; in other words, as Aretæus says, they “resemble abscesses.” Garrod also held that uratic deposits probably form during an attack of gout, but occasionally they appear shortly afterwards. Thus, in one of his cases no auricular tophi were found when the subject left hospital, but within ten days, on re-examination, a deposit was detected. “Perhaps,” he reflects, “some fluid was effused during the fit, but being at first transparent, could not easily be distinguished.”
That Garrod held the swellings to be inflammatory in nature is clear from his writings. Thus, he says, “When tissues little liable to take on inflammatory action become infiltrated (with urate of soda), but slight vascular disturbance is produced. This is especially the case with the fibro-cartilage of the ear, and although we now and then meet with patients aware of the formation of these little nodules, who experience in fact a gouty fit in the ear, yet in the majority of cases attention has never been directed to the part, so slight has been the inflammation caused by the effusion.”
Again, James Moore, whose graphic description of tophi formation is quoted by Garrod, also held that “this process is usually preceded and accompanied by inflammation.” Hilton Fagge, too, says, “it appears probable that the deposition of lithate of soda causes inflammation in other tissues besides the joints. It does, as we have seen, in the ear and occasionally in the skin.” But, he also states, “in the pinna of the ear, in fact, gouty concretions commonly form without any indications of previous inflammatory action. In some instances the patient experiences sensations of heat and pricking, and the part is tender, but more often he is quite unconscious of the fact that such concretions in the pinna are present.”
Duckworth also noted that uratic deposits are not always painless[164] during their formation, and he noted that not only may auricular tophi be painful at this stage, but that, following the subsidence of acute gout in a joint, painful swellings may develop in its vicinity, which subsequently proved to have been tophi in process of formation.
For myself, I am of opinion that each and every process of tophus formation is preceded by local inflammatory reaction of varying grades of severity. In a matter of this sort, positive is more valuable than negative evidence. We see that all the authorities quoted admit that tophi are associated with inflammation and some measure of pain, though they add the reservation that in many instances, if not the majority, these phenomena have apparently been absent. Apparently, we say advisedly, for conceding that the pain attending the formation of auricular tophi is but slight, how all too easy for the subject to have wholly forgotten it when he comes later under notice. By this time the tophi, from being latent, have become overt. The initial soft red swellings, their nature probably misinterpreted at their initiation, are now transmuted into pearly concretions of hard or semi-solid consistence. Small wonder, then, that attempts to elicit the history of slight pain and pricking or tenderness often prove barren; for, be it noted, tophi take months to mature, as Garrod long since pointed out.
Moreover, we would emphasise the fact that tophi, more often than is thought, occasionally precede by some years the outbreak of arthritic attacks. Both Duckworth and Garrod are quite definite on this, and we can confirm them.
In such instances, then, even granted that our attention be drawn to them in their initial stages, how easy to misinterpret their true nature! Thus, we have known tophi in their early stages of formation confused with chilblains. In this connection we might remind the reader that, according to Duckworth, amongst the peculiarities of tissue in those goutily disposed is feebleness of the peripheral capillary circulation, “a condition leading to disorders of chilblain-type, the vessels filling slowly after being emptied.”
We repeat that the cause or causes of tophi and, alike, of the arthritic phenomena of gout are, and must be, one and indivisible, for the process of tophus formation is but an attack in miniature of gout. Although he may never have had an arthritic outbreak, the individual who exhibits a tophus undeniably has gout. More certainly so than if he had had an inflammatory outbreak in his great toe; for this, at any rate, may be of non-gouty origin, but the tophus, never!
Reflecting on the foregoing considerations, we would submit—
(1) That tophi are always preceded by local inflammatory reaction of varying grades of severity, and that the uratic deposits are sequels thereto;
(2) That in their early stages their presence is betokened by soft red swellings associated often with sensations of pricking and tenderness;
(3) That their transmutation into white pearly concretions is a process that takes months to mature;
(4) That tophi and arthritic outbreaks have a common causal origin.
The question that now thrusts itself upon us is,—What, then, is the cause of the inflammatory phenomena which determines the eruption of tophi, and alike of the arthritic outbreaks?
Garrod’s discovery that uric acid was present in the blood in gout not unnaturally led to the assumption that herein lay the origin of its symptomatology, and what else than confirmatory could be the deposition of uratic deposits here and there in the body. The corollary seemed obvious that, given the presence of a certain proportion of uric acid in the blood, then gout must result. But, unfortunately, it was not so; for, lo! and behold, an excess of uric acid in the blood is in no sense pathognomonic of gout.
Thus, the blood in leukæmia contains a high percentage of uric acid, in some cases exceeding that found in gout, and enduring, moreover, for a longer period. Yet no symptoms distinctive of gout appear, nothing that can be referred to uric acid. But it was contended the reason why gout does not ensue is because simultaneously with increased formation there is increased elimination of uric acid. But, unfortunately, despite augmented excretion, the percentage of uric acid in the blood is still maintained at a high level, and still no gout occurs.
Moreover, it is met with also in nephritis, simple and pernicious anæmia, intestinal inflammation, certain fevers, notably in malaria between attacks, and in typhus after the febrile stage, pneumonia, plumbism, etc. Indeed, the ubiquitousness with which uric acid is found in the blood, and this in conditions wholly distinct from gout, would of itself seem sufficient to dissipate any lingering doubts as to its being anything more than a symptom of gout and not its proximate cause.
Obviously, with these revelations the uric acid theory was within measurable distance of being uprooted. Deposed from its high[166] estate as a causal agent, and accredited with only a symptomatic value, the question arose whether indeed this bogey, “uric acid,” was even capable of fulfilling a minor rôle, of originating any symptoms, much less gout, in its entirety. In other words, is uric acid toxic or non-toxic?
The adherents of the uric acid theory did not hesitate to attribute to its toxic action, not only the severe phenomena of acute attacks, but even all the functional disorders of so-called irregular or visceral gout. By the more ardent advocates, such as Haig, we were treated to a word picture of how solid crystals of uric acid erupted out of the blood-stream, and anchoring themselves in nerve sheathes, the renal substance and the mucous membrane, gave birth to chronic neuralgias, nephritis, rhinitis, and so forth. But, alas, there is very serious doubt as to whether uric acid or the urates are capable of acting even as mechanical, much less as true toxic irritants.
Perhaps the most cogent evidence of the slight toxic effects of uric acid or urates is that derived from a study of the uric acid infarcts so frequently noted in infants dying within the first two weeks of birth. According to Gideon Wells, “little or no change occurs in the renal tubule as a result of these depositions, except such as can be attributed to their mechanical effect.” This same observer, discussing this question of the toxicity of uric acid, observes, “It may be safely stated that at the present time there exists no good evidence which makes it probable that uric acid is responsible for any pathological conditions whatever, except uric acid calculi, uric acid infarcts in the kidneys, and certain manifestations of gout.” His further conclusion is that uric acid possesses but a very slight degree of toxicity, and that an actual intoxication of the organism with this substance probably never occurs.
Again, we have the fact that in instances of malnutrition in children excess of uric acid may occasionally be found in the blood. Yet no symptoms comparable to gout occur, even though uric acid calculi form. Also, as has been pointed out, showers of uric acid may be present in their urine, and yet no symptoms arise, save those referable to mechanical irritation of the renal or vesical tissues.
Turning to experimental researches, the evidence is cumulative as to the non-toxicity of uric acid. Rabbits and dogs seem quite irresponsive, either to its ingestion in large quantities in their food, or to repeated intravenous injections of 1 or 2 grammes[167] thereof, save only that the urine showed a large increase in uric acid.
Again, Ransom, of New York, found that no systemic disturbance ensued in two cases of chronic nephritis, following the taking by the mouth of 3 grammes of uric acid per diem for three days in succession. All that resulted was a notable increase in the uric acid output. In one case, he went further, and on the fourth day administered 6 grammes, but nothing happened.
Walker Hall, with commendable devotion, took large doses of uric acid with resultant headache and malaise, which endured for some hours. But as Luff shrewdly observes, “almost any substance, however (common salt for example), will produce toxic effects if taken in very excessive quantities.” Despite his brief indisposition, Walker Hall maintains that uric acid is rather a symptom of, than the precise materies morbi in gout.
Nor, apparently, even in gouty subjects can aggravation of the condition be induced by intravenous injection of uric acid. Bass and Herzberg did so until the blood content of uric acid reached the high level of 10 mg., and yet no joint attack supervened. Neither, for that matter, has it been possible to establish any relationship between degrees of uricæmia and the incidence or severity of gouty paroxysms.
Again, taking a typical instance of acute gout in the big toe, how difficult to conceive that the same owes its origin to uric acid circulating in the blood especially when we realise that the blood content of uric acid in gout exceeds but by a few milligrammes that in normal blood. Moreover, if it does so, then why does it fail to ensue in leukæmia and in other states associated with uricæmia. Also, we like to think that the penchant of acute gout for the toe is that the circulation is inefficient at this peripheral site. But how often is the circulation all too vigorous in gout, and for that matter frequently feeble in leukæmia and in ill-nourished children. But, notwithstanding that in the two latter conditions, uricæmia exists yet, despite favouring circulatory conditions, they develop no gout.
Garrod contended that the violent pain, intense inflammation, and profound constitutional disturbance of acute gout were due to mechanical irritation occasioned by the sudden deposition of biurate crystals in the delicate interior of the implicated joint. Also, that the absence of constitutional disturbance in the inter-paroxysmal periods was because the deposition of urates, being gradual, the tissues acquired tolerance, and yet, forsooth, this same substance is held responsible for the fulminant outbreak that ensues anon.
But it is, as Ringrose Gore shrewdly observed, “against the[168] usual laws of nature that, if an irritant foreign body remains in any organ the symptoms should quickly subside, while the irritant actually increases, for after each attack, and during the intervals between the attacks, the deposits of such biurate enlarge.” In conclusion, is it not infinitely more probable, as Gore states, that the inflammatory reaction precedes the deposition of urates and that these latter, in short, are the consequence and not the cause of the gouty arthritis?
Reverting to tophi, their experimental production, it is claimed, has been achieved by His.[24] Administering alcohol to dogs and simultaneously injecting them locally with sodium mono-urate, he produced deposits which seemed identical with tophi produced spontaneously in gout. But, unfortunately, up to the present, it has been found impossible to induce their formation by flooding the circulation with urates. The utmost, indeed, that His and other workers in this sphere feel able to postulate is that uric acid is a “weak tissue poison.”[25] Scarcely the words in which to describe the poison responsible for gout! for, as we have before stated, the agent that is responsible for tophi must also be capable of inducing the arthritic phenomena and other features of the disorder.
The sum of our reflections is that the toxicity of uric acid has been grossly over-estimated, and that, like its relative urea, it is practically non-irritating and inert; in other words, it cannot any longer be regarded as the essential cause of the acute or chronic forms of gout, whether of articular or ab-articular site. Moreover, far from its presence in excess in the blood being pathognomonic of gout, it must, as Walker Hall contends, be held merely “as symptomatic of conditions which help or prevent its solubility and excretion and does not itself cause lesions which accompany uricacidæmia.”
Naturally the upholders of the uric acid theory were loth to find their fetish uric acid was allotted a meaningless rôle. That it should be deemed inert was to dislodge the very corner-stone of the imposing superstructure they had been at such pains to raise. Uric acid not responsible for the genesis of gout! But, haply, maybe their position was still unassailable; for what of the purin bases, the forerunners of uric acid? Might not the blame lie with these?
Straightway xanthin, hypoxanthin, adenin, etc., were credited with pernicious potencies.[26] Nor did they lack apparent support from the experimental side. Thus, Mandel affirmed that purin bases, apart from infection, might originate pyrexia. Others, again, noted that in dogs and rabbits fed on adenin, degenerative changes in the kidneys ensued, with deposits resembling uric acid and urates in their substance. The fact, too, that guanin-gout was occasionally met with in swine, also lent colour to their views.
Moreover, that ingestion of these congeners of uric acid led in animals to renal lesions, seemed to support the contention of many, that renal disorder might be the primary cause of gout. But, unfortunately, Kolisch and Weintrand’s assertion that the alloxur bases were found in increased quantities in the urine of gouty patients was contradicted by Schmoll, His, Laquer, and others.
Still more cogent, apparently, the announcement in 1910, by Brugsch and Mallory, that they had seen a typical attack of gout ensue in a gouty patient in sequence to a dose of 0·5 gram of hypoxanthin. Nor did this reaction of gouty persons fail of confirmation, as in the same year, Brugsch and Schittenhelm, in gouty patients, noted attacks of arthritis, after the administration of nucleinic acid.
Nevertheless, we must beware of laying too much stress on isolated experiments of this nature, so hypersensitive are some of the victims to any strange or unaccustomed ingesta. Were all the myriad other determinants of gouty attacks eliminated, over-drinking, trauma, mental disturbances, etc.? for be it recollected, all the victims of these experiments with hypoxanthin and nucleinic acid were gouty subjects, i.e., potentially liable to attacks at any moment.
Even admitting the ingestion of, e.g., hypoxanthin was followed by a gouty outbreak, it must be insisted that mere sequence does not establish causation. Clinically, on the whole, there is little or nothing to support the contention that the purin bases have much to do with the pathogeny of gout. “The proof of the pudding is in the eating,” and contrary to the view, at one time so prevalent, that purin foodstuffs were most deleterious, it has been found that, for the average gouty person, a purin-free dietary is not only not essential, but prejudicial. Those, therefore, who may be inclined to see in the above sequence proof of a causal connection, would do well to recall Bacon’s dictum that “there is in the[170] human mind a peculiar tendency to dwell on affirmative and to overlook negative instances.”
In conclusion, we must affirm our belief that neither uric acid nor its precursors is responsible for the fever, local inflammation, and general constitutional disturbance in gout, for uric acid and the urates are themselves practically non-toxic. Albeit, though holding this view, I do not for one moment suggest that uric acid has nothing whatever to do with gout. The fact that tophi, its pathognomonic stigmata, are compounded of biurate of soda, would per se stamp such an attitude as untenable. On the other hand, uric acid must be viewed in its proper perspective as a concomitant or sequel of gout, the essential cause of which must be sought elsewhere.
With the abandonment of the uric acid theory of the causation of gout we see a reversion, curiously enough, to the hypothesis held by the ancient physicians as to its pathogeny. Like Cælius Aurelianus and Paulus Ægineta, we now incline to refer the origin of the disorder to some derangement of the gastro-intestinal tract. This conception indeed endured up to the latter half of the eighteenth century, and was definitely maintained by Van Swieten in his commentary on the aphorisms of his great preceptor, Boerhaave. For him the fons et origo mali in gout was disturbance of the functions of the alimentary tract.
“Indigestio viscorum pro origine proxima hujus morbi habitur.”
The English Hippocrates, too, Sydenham, in his classic treatise observes: “The more closely I have thought upon gout, the more I have referred it to indigestion, or to the impaired concoction of matters both in the parts and juices of the body.”
Not only in regard of the initial site are we reverting to the views of old-time physicians, but the tenor of our reflections upon the nature of the disorder exhibits a like trend. Thus the older physiologists, doubtless impressed by its fulminant onset and clinical features, ranked gout amongst the fevers, describing it indeed as a “tertian fever terminating in fourteen days.”
Indeed, the great Boerhaave avowed his belief that gout was contagious—a forecast, we may take it, of the modern theory of infection. Subsequently his pupil, Van Swieten, went a step further, maintaining that sometimes wives, while nursing husbands afflicted with gout, contracted the malady!
Passing now to relatively modern times, it will be noted that in 1864 Laycock classed acute gout with rheumatic fever as an “excretory fever,” while Parkes even prior to this, in 1860, wrote: “I define gout after Garrod as a febrile infection with inflammation about the joints leading to a deposition of urate of soda.”
But it must be freely acknowledged that, subsequent to Garrod’s discovery of uric acid in the blood in gout, the spell exercised by the uric acid theory was such that it dominated medical thought almost to the exclusion of all other possibilities.[172] All energies were forthwith centred upon endless laborious researches into possible modes of uric acid formation, but which, alas, did little to purge men’s minds of their obsession that uric acid was the proximate cause of gout.
Still it would be unfair to infer that the disabilities attaching to the uric acid hypothesis were wholly unrealised. Indeed, it may be fairly said of Duckworth’s reflections on the pathogeny of gout that they definitely foreshadowed the infective theory. His views postulated what may be termed a toxic tropho-neurosis, wherewith to explain the paroxysmal nature, the periodicity and protean symptomatology of the disorder.
But in the early part of 1900 we may, I think, discern in some words of Chalmers Watson a change coming over our thoughts as to the pathology of gout, this as the result of some studies of a series of examples of acute gouty polyarthritis. The results of his researches were such that he challenged the accuracy of Garrod’s original observations as to the lowered alkalinity of the blood during acute attacks, also his claim that the uric acid content of the blood was increased and the uric acid excretion diminished during the paroxysm. If these points be accepted, he says we must start de novo in search of the cause of the acute paroxysm.
He noted also the interesting fact that during acute attacks of gout a very marked leucocytosis was present. Another outstanding feature was the presence in large numbers of peculiar myelocyte-like cells, half as many in number as the ordinary finely granular oxyphil leucocytes. Reflecting on these findings, he observes: “It would, I think, be well if much less attention were centred on the excretion of uric acid alone as the all-important factor in the disease, whether in its acute or chronic form. The results obtained by the line of investigation here followed suggest the advisability of more attention being devoted to the histo-chemical characters of the blood, the ratios of uric acid to other important products of metabolism, and, if opportunity be afforded, an examination of the bone marrow.”
To other interesting features of these researches of Watson’s we shall allude later, but, concerned here more with tracing the evolution of the infective theory of gout, we would hasten to add that in September of the same year Ringrose Gore, discussing the inadequacy of the uric acid theory, boldly avowed and ably propounded his belief in the infective origin of the disorder.
Thus he writes: “I consider a toxin to be the cause of this disease. If so, such toxin must be formed in the intestine. As the symptoms of gout are constant, it must be a definite toxin, the product of a definite bacillus acting upon the intestinal secretion.[173] As gout is capable of being caused in any subject, it must be one of the bacilli normally found in the intestinal canal.”
Nor did Gore lack supporters in his suggestion that the alimentary tract was the primary source of the changes in the metabolism of gout. For in the same year Minkowski, Le Gendre, and in this country Watson, hazarded the view that intestinal derangements, through the medium of their resultant toxins, initiate disturbances in the liver, and these in turn determine those obliquities of metabolism typical of gout.
At the same time their contentions derive colour from the researches of Grübe, who, despite traditional views, maintained that in gout the hydrochloric acid of the gastric juice, far from being increased, was in most cases diminished or wholly lacking, while, on the other hand, lactic acid was present in some instances.
In 1903 Woods-Hutchinson ably contended that “gout and lithæmia are mere symptom names for a miscellaneous group of chronic toxæmic processes of widely varied origin, characterised by the production of uric acid and the urates.” He held that the uric acid in gout as well as the associated phosphoric acid are merely a criterion of the measure to which the nucleins of the body cells (chiefly probably of leucocytes) have undergone destruction in consequence of their invasion by a toxin or toxins of organic or inorganic nature. He furthermore contended that the rôle of the liver in gout was purely negative, consisting in its inability “to absorb or transform into harmless excretory substances the excess of toxins brought to it by the portal vein.”
In 1904 Falkenstein furnished collateral evidence that the starting point of gout lay in a diseased condition of the gastric glands, those responsible for the secretion of hydrochloric acid. The supply of hydrochloric acid being deficient in the gouty, their digestive capacity is distinctly lowered. Abnormal fermentation ensues with insufficient oxidation, and “the substances containing quantities of nuclein are partly prevented from being further split up, and partly favour the synthetic formation of uric acid.” He would thus refer the excessive formation of this latter directly to the diseased glands. He further observes that, despite the deficiency of hydrochloric acid, the gastric juice is often hyperacid, this being due to the presence therein of organic acids, such as butyric, lactic, and acetic acids.
In the same year Chalmers Watson, as the outcome of investigations into gout as it occurs in the fowl, held that:—
(a) There is ample evidence to prove that the uric acid in the blood is not the primary factor in gout, and
(b) Uric acid can be deposited in cartilages and other tissues,[174] even in considerable amount, without the association of any inflammatory phenomena.
He concludes that the last-mentioned point clearly proves that:—
(c) Uric acid is not the factor which causes the inflammatory phenomena characteristic of the acute attack.
He then proceeds to inquire as to the nature of the toxic principles in the blood, and the factors that influence their passage thence into the tissues. In connection with these queries he emphasises the necessity of envisaging the all-important part played by the alimentary canal, holding that herein doubtless resides the clue to the solution of the problem.
Post-mortem examination of the fowl revealed marked catarrh of ileum, duodenum and large intestine, while the pancreatic duct was filled with catarrhal products. The congested spleen, apart from proliferation of its endothelial elements, exhibited a marked increase in the number of granular leucocytes in the capillaries and sinuses as compared with the features of the control sections, which, as Chalmers Watson observes, is the characteristic reaction of this organ to invasion by bacteria or their products. The kidneys on examination revealed here and there uratic deposits surrounded by inflammatory tissue. The relationship of these to the inter-lobular arteries was such as to suggest an infection by the blood stream.
The collecting tubules in the deeper part of the cortex and medulla were markedly dilated and choked with granular leucocytes. Sections of the organs were examined bacteriologically by Muir, the necrosed areas revealing the presence of “rod-like bodies of the size of large bacilli massed together in dense clusters; the appearance suggested that these rods were either degenerated cell products of an unusual character, degenerated bacteria, or crystalline in nature.” Examination of the same by polariscope by Marshall disposed of the possibility that they were crystalline. Finally it was thought that the appearances generally favoured the view that the rods in question were bacteria which had lost their reaction to bacterial stains owing to bacteriolytic or other changes.
As to the inference that the defunct fowl fell a victim to acute gout, Watson based it on the existence of the uratic deposits in the tissues, the changes in the synovia, the widespread thromboses, and the renal necroses. As to the other lesions, the chief interest centres in those located in the intestine, pancreas and kidney. The state of the pancreatic duct raises the question as to whether it points to any connection between these changes and the common occurrence of glycosuria in gouty subjects. The alteration in the leucocytes merits notice in that similar changes were found[175] by Watson in the blood in acute gouty polyarthritis, the same, moreover, being subsequently confirmed by Bain.
Chalmers Watson’s final conclusion was that “the clinical features of gout—regular or irregular, acute or chronic—are more adequately explained by the light of our present knowledge of infections, relapses, and immunity than by any other theory. The distinctive feature of this infection in gout is that the toxin or toxins have a special property of disturbing nitrogenous metabolism in a manner favourable to the deposit of uric acid in certain tissues.”
It will have been noted that, despite the growing number of adherents to the infective theory, no attempt had been made to saddle any particular organism with the responsibility of initiating gout. But in 1905 Trautner, holding mucous colitis to be one of the initial manifestations of gout, affirmed his belief that the bacillus coli communis was the responsible microbic agent.
He claimed that this particular organism, during its passage through the system, gives rise to a reducing agent which is subsequently transmuted into xanthin and uric acid. This is, of course, but a variant of Gore’s original view that the toxin of gout is a product of certain bacteria normally present in the intestine, but which under certain conditions take on a pathogenic action.
The microbic theory fast gained ground. Thus Luff, who in the first edition of his work advocated the renal origin of gout, subsequently renounced the same in favour of its infective origin. To sum up, the opinion generally was that it was more than probable that gastro-intestinal derangements, with their altered secretions, exert an influence on the intestinal flora with resultant formation of toxins, and that these same, acting chiefly on the liver, put in motion those obliquities of metabolism which eventuate in gout.
Sikes, however, in 1907, discussing the rôle of gastro-intestinal disorders, expressed a doubt as to whether the same are primarily or secondarily related “to the actual chemical processes at the base of the disease.”
He thinks it at least as probable that the gastro-intestinal disorders are due to an alteration in the intestinal secretions from an internal cause as that they are due to bacteria in the formation of toxins, or, he suggests, to some alteration in the epithelial cells, so that they take up chemical compounds of different nature from the ordinary. To him it does not seem at all probable[176] that gout will ever be found affiliable to any specific micro-organism, inclining rather to the belief that a solution of the riddle will only be found in a closer and more extended study of that most difficult subject, the actual chemistry of the cell protoplasm.
“The old order changeth, giving place to new,” and the uric acid theory having failed us, it is essential that we cast round for some other solution of the problem, carrying with us, however, this guiding principle, that uric acid, having lost its etiological status, be viewed in its right perspective as not the cause, but the consequence, of gout.
Happily, with the advent of bacteriology our views, or rather our hazards, as to the nature of joint diseases underwent profound modification. But, strange to say, though quick to apprehend the significance of infection, its causal relation to other joint disorders, we still seem unaccountably loth to discard our time-worn conception of “gouty” arthritis as of purely metabolic origin. This, to my mind, is the more remarkable in that the onset, clinical phenomena, and course of acute gout, and no less the life history of the disorder as a whole, are emphatically indicative of the intrusion of an infective element in its genesis.
In developing this hypothesis I purpose devoting the present chapter to consideration of the frequency with which local foci of infection are met with in gout, the frequency, too, with which exacerbations of the disorder are presaged by acute glandular affections of undeniably infective source. The latter part of the text will concern itself with the rival claims of auto-toxæmia and infection or sub-infection. In the subsequent chapter we shall analyse critically the component elements of the acute paroxysm of gout, their compatibility or not with an infective origin. The affinities between gouty arthritis and the specific infective arthritides will then be noted, and, finally, an endeavour made to link up the specific stigmata of gout—its uratic deposits—with the postulated infective element.
The extreme frequency with which infective foci are met with in the victims of gout is by no means adequately realised. Moreover, we are only now beginning to appreciate the grave significance of such “nests” of infection and how devious are the ways in which they work their malign influence. For our forefathers gout began, and, forsooth, often ended, in the “stomach,” or it[178] was the “liver” that was impeached. But the portal to the alimentary canal was for them only a cavity, the contained structures of which, albeit, to their mind often betrayed evidences of a “gouty diathesis.” They distinguished “gouty” teeth, “gouty” tonsillitis, “gouty” pharyngitis, even “gouty” parotitis; but all these they classed as tokens or sequelæ of gout—not possible causes or excitants thereof.
Nevertheless, their observations on “gouty” teeth are of deep interest, though their significance was misinterpreted.
Thus, Duckworth, for example, wrote: “The tendency to shed sound teeth has been noted with some frequency in middle or later life in goutily disposed persons, and they are more than others liable to occasional and fugitive attacks of pain in several sound teeth at a time, with a sensation as if these were starting from their sockets, being tender to bite upon.” In truth, a succinct picture of pyorrhœa alveolaris, of unprejudiced source, hence the more valuable.
Garrod again tells us that he saw an initial attack of gout supervene after extraction of a tooth, a sequence attributed by him to loss of blood. How interesting this, in light of the fact that exacerbations of joint disease have frequently been seen to follow the removal of septic teeth. The same authority also noted the incidence of a primary attack of gout following epistaxis, and the same after copious hæmatemesis, and Todd several times observed such articular outbreaks after venesection.
Lastly, says Garrod, “cases illustrative of the effects of the suppression of an habitual hæmorrhoidal discharge are by no means uncommon, and ... numerous instances arising from boils and carbuncles have come under my notice.” By Garrod and his contemporaries all these various determinants of gouty paroxysms, i.e., loss of blood, etc., were believed to exert their influence viâ the nervous system, with consequent disturbed equilibrium of nutritive processes throughout the body. But while it may be admitted that depression of the vis resistantiæ plays a part, it does so, I believe, by favouring the occurrence of infection.
Let us turn now to modern findings, and we shall see that they do but confirm those of the older clinicians. Lambert in 125 cases of gout found the teeth unsound in 82 per cent. of males and 1 per cent. of females, while in 9 per cent. of the former and 17 per cent. of the latter there was associated chronic dyspepsia. Two years after (1909) Wynn, Wirgman and Turner noted the invariable correlation of gout with local foci of infection. In the majority, pyorrhœa alveolaris was present. Tonsillar sepsis, too, was not uncommon, and much more rarely nasal disorders.[179] Again, out of fifty-two examples of so-called “gouty” throat Edward McCracken found pyorrhœa alveolaris to be present in thirty-nine, and Fenner also tells us that this affection is common in the subjects of gout.
In truth, the victims of gouty arthritis are no more immune from dental lesions than those of other types of joint disease. Thus, Mr. Macdonald, dental surgeon to the Royal Mineral Water Hospital, Bath, informs me that this form of oral sepsis is extremely common in gouty individuals, and in my experience it is but rarely that evidences of its presence are not forthcoming in these subjects. The desirability of early recognition of such foci—in light of their highly probable etiological significance—can scarcely be overestimated. For their consequences, both local and remote, are of paramount importance.
Thus, G. I. Stewart’s recent observations have conclusively demonstrated that “bad teeth” are causally related to tonsillar affections. How illumining this, in view of McCracken’s experiences in “gouty throats.” As we saw, pyorrhœa alveolaris was present in more than half the examples. But, more pertinently to the point at issue, he comments on the frequency with which the victims of gout develop acute tonsillitis, of lacunar or parenchymatous type, also that such attacks frequently precede outbreaks of arthritic gout. Duckworth again noted the same liability of the gouty to unsound teeth and tonsillitis, and that the latter was often followed by articular outbreaks. Luff also observed that “gouty” tonsillitis was occasionally a precursor of articular gout, always subsiding on the appearance of the latter complication.
Again, acute and chronic pharyngitis are proverbially common in “gouty” subjects. Moreover, in both types the subsidence of the throat affection has frequently been signalised by an articular outbreak of classic site. Parotitis, too, has been repeatedly met with in gout, and, according to Luff, “rapidly subsides on the appearance of regular gout in one or more joints.”
In truth, whether we peruse recent or older works on gout, we cannot fail to remark the unanimity of opinion as to the frequency of incidence of these glandular affections—these states of oral sepsis—in the subjects of gout. Equally noteworthy is their insistence on the constancy with which such local affections have proved harbingers of oncoming articular outbreaks. Lastly, the mere fact that our forefathers dignified these local disorders with special appellations, “gouty” tonsillitis, pharyngitis, etc., is cogent proof that they regarded them as among the integral features of gout.
Now, as to the true significance of these acute glandular affections,[180] held by clinicians of repute to be of “gouty” origin. What of “gouty” tonsillitis, pharyngitis, etc.? Still more, what of our deductions regarding the relationship of these same when met with in association with other joint disorders? Do we not hold them each and all as evidences of infection—“acute rheumatism,” “gonorrhœal arthritis,” etc.?—and we may well ask, Why not in gout?
Says Duckworth, “Angina tonsillaris—very painful but not suppurating—may in the gouty suddenly yield to an acute articular attack.” Is it not here more than likely that the tonsil was the initial site or portal of infection, and the arthritis secondary thereto? Is not this same interpretation in all probability true also of all forms of “gouty” throats when followed by arthritic outbreaks?
The marvel, then, is that not only have we held, but apparently many still hold, that the tonsillitis, pharyngitis, even the gingivitis—like the subsequent articular lesions—are one and all attributable to the underlying gout. We certainly would not do so in the case of any arthritis other than “gouty,” and to my mind the time is ripe for a change of attitude. The “gouty” throats, like the “gouty” teeth, should be regarded not as symptomatic of gout, but etiologically related thereto. We should cease to talk of “gouty” throats, teeth, etc., should renounce the prefix, for there is nothing specific of gout either in the tonsillar, pharyngeal, or dental lesions. We should instead view these various local disorders in their true perspective as foci of infection, causally related to the subsequent and secondary “gouty” arthritis.
Gastro-Intestinal Disorders.—It is a matter of common experience that acute attacks of gout are often preceded by or associated with flatulence, heartburn, acidity, loss of appetite, confined bowels, scanty, high-coloured urine, and a feeling of lassitude. In short, nothing is more certain than that exacerbations or relapses very commonly follow symptoms referable to gastro-intestinal and hepatic disorders.
How well established is it that these subjects after unusual, though not necessarily excessive, indulgence at the table, almost inevitably, and sometimes almost immediately, suffer twinges in the big toe, if not frank outbreaks of gout. Such reaction seems to indicate clearly that the functional disturbances in the alimentary tract stand in some causal relation to the subsequent arthritic phenomena. The assumption gains colour, too, from the very certainty with which freedom from such gouty manifestations is attained by abstinence from, or more moderate indulgence in, articles of diet predisposing to such ebullitions.
So much by way of prelude as to the probability—attested by clinical observation and the results of treatment—that the intestinal canal is often the source of the responsible microbe or toxin. Let us now pass to consider what factors other than an oral sepsis may favour the incidence of functional disorders of the alimentary tract.
Variations in Free HCL.—Some years ago Grübe and Falkenstein found that in gout the hydrochloric acid of the gastric juice, far from being increased, was in most cases diminished or wholly wanting.
Now, as we know, the gastric juice when of normal acidity is quite capable of dealing with moderate quantities of pathogenic bacteria. But in the presence of oral sepsis it is probable that a greater number are swallowed than can be satisfactorily coped with.
Given therefore excess of pathogenic organisms and relative insufficiency of free HCL, conditions favourable to the growth of bacteria ensue, while incidentally the chance of such reaching the intestine is materially enhanced.
When, however, the defensive barrier is wholly withdrawn, viz. when there is an absence of free HCL, then of course the necessary inhibition of microbic growth fails of achievement. Moreover, also owing to diminished acidity, ill-digested protein substances gain access to the intestine, and their subsequent putrefaction is favoured.
In opposition to the foregoing, many hold that an excess of free HCL in gout is not uncommon, and unquestionably some are thus troubled. The pernicious effects of the hyperchlorhydria are accentuated by the fact that intestinal indigestion ensues secondarily, owing to the acid chyme completely antagonising pancreatic secretion and thus impairing digestive capacity.
Intestinal rather than gastric indigestion is, I think, more typical of the gouty subject. It will be recalled that the food nucleins are unaffected by the gastric juice, and though the protein moiety is split off from the nucleinic acid by the pancreatic ferments, yet neither the poly- nor the mono-nucleotides are thereby acted upon. It is in truth the succus entericus with its nucleotidase that plays the most important digestive rôle as regards nucleins, breaking them up into nucleosides which are, to a large extent, absorbed as such.
To resume, this condition of intestinal indigestion may arise from a variety of causes: excess or deficiency of gastric juice, defective motility, and diminished secretion of intestinal juices, and in all cases improper food may determine such intestinal derangement.
The clinical features presented are very variable. It is often[182] difficult, if not impossible, on the basis purely of the subjective symptoms, to decide in any given instance how far the symptoms are referable to intestinal stasis, or to a chronic infection, with a resultant catarrhal state of the mucosa, or to both causes combined in varying proportions.
But, be the explanation what it may, in our experience the most common antecedent or concomitant of gout is intestinal dyspepsia. Its secondary consequences are far reaching, especially if the small bowel be involved, catarrh of which may lead to reduction in the secretion of bile and pancreatic juice.
How commonly in these cases do we meet with symptoms indicative of sluggishness of the hepatic functions, such as turbidity of the urine, a pale or abnormally dark colour of the alvine evacuations. Also, whatever be its true etiology, they exhibit not so uncommonly sugar in the urine, the so-called “gouty” glycosuria.
Now, as a mere glance will show, diminution and impairment of the biliary and pancreatic secretions have far-reaching consequences. Foodstuffs undergo abnormal changes, are less easily absorbed, and simultaneously chemical products are formed which irritate the intestinal mucosa. Nor do the baneful effects cease here, for, owing to the unusual nature and reaction of the intestinal content, the bacterial flora in the bowel undergo modifications.
Thus, organisms normally present only in small numbers in the small intestine find the altered medium more suitable for their growth and multiplication; while others, whose usual habitat is the large bowel, migrate upwards, and infect the ileum and duodenum, and ultimately the biliary and pancreatic passages.
In the presence of such deficiency in the intestinal juices, proteins are imperfectly digested, and putrefaction under microbic action favoured. At the same time the digestion of carbohydrates is impaired, organic acids are formed, and gases in larger amounts liberated. Ultimately, owing to absorption of these irritating products, a condition of chronic toxæmia results.
It now devolves upon us to decide whether the phenomena of gout are best explicable as the outcome of auto-intoxication, or of infection or sub-infection. The uric acid theory was in truth one of auto-toxæmia, the varied manifestations of gout being attributed to mechanical or toxic irritation by uric acid, the end-product of purin metabolism. But, as we hope to have shown conclusively, uric acid is not toxic, and per se is apparently as innocuous as those other and intermediary products of metabolism which give rise to cystinuria and alkaptonuria.
The question then arises, Is gout haply due to a retention of other metabolites? That outbreaks of gout follow fast on the heels of dietetic irregularities is proverbially true. But there is no certain evidence that the symptoms generally ascribed to auto-toxæmia are referable to substances derived from the foodstuffs under the action of the digestive juices. Toxic as are peptones and primary proteoses when they gain direct access to the tissues, the symptoms produced in no way resemble those affiliated to alimentary toxæmia, much less those of gout. Rather, according to Adami, do they approximate to those typical of anaphylactic shock.
Normally, too, the mucous membrane proves an efficient barrier, these poisonous bodies during their passage through it being transmuted into harmless substances. Nor can we refer the symptoms of gout to a toxæmia secondary to intestinal stasis or other causes. In other words, it cannot be attributed to assumed toxic action on the part of the intermediary and terminal products of protein disintegration. For seemingly these chemical outcasts of the economy become progressively less toxic on their downward path to effete matter.
The diamines, too, produced by bacterial action on foodstuffs, are so minimal as to be negligible, while the toxicity of cholin and neurin is unestablished; and as for indol and skatol, they are with difficulty absorbed from the healthy colon. Experimental researches on carbohydrate and fatty disintegration have likewise proved sterile, while there is no evidence that the anaerobes present in the digestive tract produce ecto-toxins, or undergo lysis with release and absorption of their endo-toxins.
In short, it is but too clear from the foregoing brief résumé of recent experimental findings that, if uric acid cannot be held responsible for the causation of gout, there is no evidence likewise that the disorder owes its genesis to any other of the as yet isolated chemical products of gastro-intestinal digestive activities. Having dealt with this aspect of the question, we shall now pass on to consider whether the phenomena of gout can be more adequately explained on a basis of infection or sub-infection.
Infection or Sub-infection.—Our knowledge as to the exact manner in which local foci of infection work their malign effects almost daily undergoes expansion. It will be recalled that Stewart has shown that “bad teeth” are often etiologically responsible for tonsillar inflammation. It further is well established that streptococci are of common incidence in the tonsils, and Rosenow and Brown from experimental observation have established that these hemolysing organisms, migrating viâ the blood stream, exhibit a marked predilection for forming a fresh nidus in the gall bladder. Here they may initiate a cholecystitis, and secondly[184] gallstones, and in sequence thereto the symptoms associated with gall-bladder-dyspepsia. The same formidable list of sequels may follow infection of the gall bladder from the teeth, stomach, or intestines, notably from the vermiform appendix.
In like fashion the origin of appendicitis may be traced back to septic foci in the mouth, tonsils, naso-pharynx, or to the gastro-intestinal tract. Here again there ensue the symptoms of so-called appendix-dyspepsia. As in the case of the gall-bladder variety, the primary lesion in the appendix may be latent, and the exact diagnosis may be a matter of great difficulty, often indeed only to be achieved retrospectively, viz., when abatement of the symptoms follows ablation of the appendix.
We see, therefore, how far-reaching are the consequences of local foci of infection in the mouth or elsewhere. Now, the gouty subject enjoys no immunity from the remote sequels of local sepsis. But as a rule, unfortunately, whatever be the nature of his dyspeptic symptoms, they are, like his dental anomalies, his tonsillar inflammations, forthwith dismissed as symptomatic of gout, not etiologically related thereto.
Now, I have seen pyorrhœa and chronic appendix-dyspepsia running side by side in the same subject with recurring classical attacks of gout in the big toe. The faulty teeth were extracted, and later the chronically inflamed appendix removed; and though he had an attack of gout shortly after the operation, there has as yet been no recurrence thereof.
Again, by the older writers “gout in the liver” was most firmly believed in—as one authority puts it, “a subacute catarrh of the intrahepatic biliary system which may lead to a subacute parenchymatous hepatitis”! But more pertinent to my point is the insistence of older authors upon the frequent association of gout and gall-stones. Senac, of Vichy, claimed indeed that out of 166 cases of biliary lithiasis 95 had gout or an hereditary predisposition thereto. Judging by modern experience, this is probably a gross over-estimate. In contrast, our own countryman Murchison dwelt upon the frequency of jaundice in gout independently of biliary colic. And, as we shall see later, Brinton held that many of the dramatic phenomena accredited to “retrocedent gout” were unrecognised examples of biliary colic.
But, controversy aside, the point I would lay stress on is, that we should refrain from labelling offhand “dyspeptic” symptoms in a “gouty” subject as gouty, this when we are so constantly confronted with local foci of infection in the mouth, or elsewhere, which afford us an explanation of the gastro-intestinal symptoms at once more obvious and more rational. This also the more[185] especially in that—as far as subjective symptoms go—those deemed typical of so-called “gouty” dyspepsia are indistinguishable from those met with in appendix- or gall-bladder-dyspepsia. Indeed, I might go further and point out that the variations in free HCL in the gastric juice—as observed in gout—conform to those met with in the above disorders. Thus, in “gouty” dyspepsia, the free HCL may be normal, in excess, or wholly absent, as in gall-bladder or appendix-dyspepsia. I would therefore plead that in any “dyspepsia” arising in a genuinely gouty subject we endeavour to elucidate the exact nature of the underlying lesion, but to this we shall return again when discussing diagnosis.
Again, the fact that gall-bladder or appendix lesions may be the outcome of septic foci in the mouth enables us the more easily to explain the not infrequent co-existence of gout and glycosuria. For an infected gall-bladder may by extension determine a chronic pancreatitis.
Lastly, what of the relationship of local foci of infection to “gouty” synovitis and arthritis? Is one focal infection more than another particularly related to arthritides? Whatever be the true inference, if we take arthritides as a whole, nothing seems so efficient a cause of their production as oral sepsis. Accordingly, some are inclined to think that organisms, e.g., streptococcus viridans, at the roots of the teeth or others in the tonsillar crypts, pass, viâ the blood-stream, direct to the joints. Others, again, hold that, given oral sepsis, infection of the stomach and lower levels of the alimentary tract and its accessory cavities ensues. And in sequence thereto infection of the joints may take place from local foci throughout gastro-intestinal tracts.
Those who favour the view that direct infection viâ the blood from foci of oral sepsis is the more probable modus operandi are wont to produce the following points in support of their view. Arthritis, they say, is relatively rare in enteric fever. In yet another disorder, dysentery, which gives every chance of absorption from the intestine, arthritis when it occurs is seldom very acute, while in appendicitis it is distinctly uncommon.
On the other hand, we must recall that even in normal animals the alimentary and respiratory tracts, and alike the liver and kidneys, constantly afford cultures of pathogenic and non-pathogenic bacteria. Such was established by Adami and his co-workers, who moreover found that such organisms, through the agency of leucocytes, continually pass into the system, where subsequently in the healthy animal they as constantly undergo destruction.
If, however, inflammatory processes are at work, their migration into the tissues is favoured. For under such conditions leucocytes aggregate at the reactive focus, and concurrently, their migration being more active, larger numbers of bacteria achieve entry into the system. The subsequent course of events is determined by the number and virulence of the organisms that effect a lodgment in the tissues, where under favourable conditions they originate other foci of infection or sub-infection.
By sub-infection is understood the fact that microbes carried into the system undergo slight, if any, numerical increase, and do not set up foci of suppuration. Here we may note that “gouty” inflammation, however intense, never ends in pus formation. But, to resume, the bacteria, instead of multiplying, undergo lysis, and, their endo-toxins being released, the more highly specialised tissue cells in the vicinity are destroyed. Coincidently the lower grade connective tissue elements are by the self-same poisons stimulated to proliferate, and an area of chronic interstitial fibrosis is formed.
Incidentally this is interesting, inasmuch as the visceral organs in gout evince a tendency to fibrosis. But, as Gideon Wells observes, “the actual increase of uric acid in the blood and tissues in gout is so slight that we are not warranted in saying that the usual tendency to sclerosis in all the organs in gout is due to the action of uric acid rather than to some other unknown agent or agents.” In view of these revelations, is it not infinitely more likely that the chronic interstitial fibroses in gout are the outcome of such sub-infection?
The assumption gathers weight in light of the experimental proof adduced by Adami that not only tubercle bacilli, but streptococci and other organisms, taken orally, can gain an entrance into the system. Upon this basis we get a clear conception of the possible relationship of gout to local foci of infection. Thus, whether it be a condition of oral sepsis—pyorrhœa alveolaris, tonsillar sepsis, sinus disease, intestinal disorders, constipation, and so forth—we see that it is highly probable that organisms at any one of such infective foci may gain access to the blood-stream with subsequent installation of local lesions in joints or other structures.
Now, as pointed out, inflammatory states or functional derangements of the alimentary tract, whether focal or diffuse, favour the ingress into the tissues of organisms. Is it not reasonable, therefore, we ask, to suppose that the functional derangements which so commonly precede or accompany gout may modify the character of the intestinal flora, and promote their migration inwards in greater numbers? The inevitable swiftness with which relapses[187] or exacerbations of this disorder follow even venial dietetic indiscretions distinctly favours this assumption, one, moreover, substantiated by the amelioration or immunity which follows abstention from the offending foodstuffs. The often prolonged course, too, of gout, and its marked liability to periodic recurrence, would be explicable as the outcome of a continued or intermittent series of sub-infections.
My conclusions then are that:—
(1) The majority of cases of gout are marked by the presence of local foci of infection, pyorrhœa alveolaris, tonsillar, pharyngeal or nasal sepsis, etc., or by gastro-intestinal derangements, constipation, etc.
(2) The said local foci should be regarded not as symptomatic of, but etiologically related to, gouty arthritis, and that the same is strongly indicated by the fact that
(3) Acute glandular affections of undeniably infective source—tonsillitis, pharyngitis, etc.—frequently and immediately precede acute paroxysms of articular gout, and, lastly,
(4) The gastro-intestinal defects, secretory or motor, which chequer the course of gout, enhance the pathological activities of the intestinal flora, and incidentally the liability to infection, at various sites of the alimentary tract.
If we reflect on the general features and local characters of an initial outbreak of gout they are precisely such as would, did they occur anywhere but at the classic site, the big toe, suggest an infection. The abrupt onset, the local signs, the crisis, and no less the subsequent swift restoration to health, how strikingly reminiscent of an exanthematous fever! Moreover, does not this outward clinical resemblance seem to predicate an inward pathological similarity? And now to scrutinise more narrowly the component elements that make up the content of a paroxysm of gout.
Its fulminant onset, with shivering, if not a definite rigor, in a person in sound and sometimes exuberant health, irresistibly reminds one of the sudden onfall of an infective disorder. Doubtless, as Duckworth says, “the conditions leading up to the attack have been some time previously in operation.” But, as he rightly contends, “some determining factor must now be invoked to explain how, as it were, the train is fired.” Quite so, and what more likely to call into the open these latent morbid potentialities than an infection?
The constitutional disturbance is often profound, certainly out of all proportion to the severity and extent of the local phenomena. Especially prominent are the nervous concomitants—the excruciating pain, the irascibility, etc. Viewing these in light of the paroxysmal nature and periodicity of gout, Duckworth postulated a kinship between the disorder and the paroxysmal neuroses. But, given an infective element, what more plausible than to attribute the nervous phenomena of gout to the simultaneous action of its toxins on the higher centres?
The temperature curve, again, is obviously compatible with this conception. It begins abruptly, its course punctuated by daily remissions. No specific peculiarities apparently differentiate it from other arthritides of established or assumed infective origin, but its relatively low grade pyrexia recalls that typical of gonococcal[189] arthritis. Its most striking feature, however, is the disproportion between the level of the pyrexia and the intensity of the general and local phenomena. Moreover, the temperature is not only low, but relatively ephemeral in duration, while the inflammatory reaction in its violence emulates that of the most sthenic forms of arthritis.
Albeit both the febrile disturbance and the local reaction display infinite grades of severity. Thus, acute gouty polyarthritis may be afebrile and the asthenic varieties of the affection marked by little inflammatory reaction. All these vagaries, however, are quite compatible with infection—the reflex, as it were, of varying degrees of toxæmia.
Says Duckworth, “The pyrexia proper to acute gout is paroxysmal with remission, and the pain of gout is likewise paroxysmal. One is reminded of the influence of marsh poison upon the nervous centres. This paroxysmal no less than periodic element in gout stamps a nervous character upon the malady and binds it in alliance with other well-recognised neuroses.”
How interesting these reflections by this distinguished physician in light of latter-day revelations! For, in so far as these features in gout are reminiscent of malaria, they disclose an affinity, not for a malady of nervous, but one of established infective, origin.
Simultaneously with the onset of pyrexia the pulse quickens. The blood shows that increase in fibrin characteristic of inflammation, a fact noted by Gulland, Cabot, Buchanan and others. But more significant is the presence of leucocytosis. It may be of high grade. In a case of acute gouty polyarthritis recently under my care the leucocyte count reached 27,000. Even in a subacute example of the classic monarticular type the leucocyte count attained 25,920. It was of leucoid type and attended by moderate anæmia due to deficiency of red corpuscles.
Nor is leucocytosis restricted to the periods of exacerbation, but it may be met with in the inter-paroxysmal stages. In my experience, even in cases of definitely chronic type it may reach 14,000. The higher grades of leucocytosis are obviously very suggestive of an infection, and that lesser degrees should be encountered in examples of definitely chronic type seems to point to gout being of the nature of a chronic or serial infection.
I would here add also that the converse of leucocytosis, viz., leucopenia, is sometimes met with in chronic cases. Dr. Munro and I have met with two instances of such in chronic gout in the intervals between paroxysms. This decrease in the number of leucocytes (leucopenia) is, of course, deeply interesting and, needless to say, quite compatible with infections, e.g., enteric,[190] malaria, tuberculosis. In fact, it suggests that gout may be the outcome of divers infections, and not due to any specific organism.
Enlargement of the lymphatic glands was, by older authors, believed not to occur in gout. But obviously the lack of macroscopic evidence does not exclude the possibility of microscopic changes in these structures. The likelihood of such, moreover, is enhanced by the occasional occurrence of lymphangitis in connection with the inflammatory articular lesions. Buzzard, indeed, long since claimed that there was “clinical evidence of subacute gouty inflammation of lymph spaces in certain regions due to uratic deposit and influence.”
As a matter of fact, enlargement of the lymphatic glands does occur. Thus, my colleague James Lindsay cites an instance thereof. The subject, a painter, fifty-three years of age, had gout of some three years’ standing. During an acute paroxysm thereof “there was a mass of glands in the right groin, synchronous with an acute inflammation affecting the right knee and periarticular tissues. On the subsidence of the gouty inflammation the glands became smaller, but never entirely disappeared during the four weeks he was subsequently under observation.”
Splenic enlargement, states Duckworth, has been met with in many cases of gout, and occasionally infarcts. But such splenic enlargement is, he thinks, not specifically related to gout, but is due to associated conditions. Personally, I have not as yet met with splenic enlargement in gout.
This aside, is it not palpably significant of infection that Paget, Garrod, and others, repeatedly noted the incidence of acute phlebitis in a limb the seat of acute articular gout? Did we observe such a complication in any arthritis other than gouty, should we not inevitably regard it as indicative of the spread of an infection from the joint to the related veins?
Reverting to the local articular phenomena, they are not only compatible with, but emphatically suggestive of, an infective source. The typical signs of inflammatory reaction are swiftly installed in acute classical gout, and this with an intensity unrivalled save by the most sthenic types of acute arthritis. Witness how insistent were our forefathers, e.g., Scudamore, on the differentiation of acute gout, not so much from acute rheumatism as from erysipelas or phlegmon. Garrod, indeed, held that “if a medical man, by chance entirely ignorant of the nature of gout, were to see a toe affected by this disease in its full intensity, swollen, hot, red, and tender, he would probably think that the affection must of necessity terminate in suppuration, yet I believe this never happens as the result of simple gouty inflammation.” This leads us to note a salient[191] feature of gouty inflammation, viz., it never results in pus formation. Now, allowing for the increased powers of discrimination that happily to-day are ours, is it not, I ask, significant that the disorders deemed most likely of confusion with acute gout belong to the frankly infective category?
That Garrod’s caveat was not uncalled for I feel sure, having myself known an acute gouty arthritis incised in the hope of evacuating pus. Sometimes the error in judgment is reversed and pyæmic or septic conditions in or near the great toe joint confounded with gout. Thus, Sir James Paget tells of an instance in which a pyæmic abscess forming near the great toe and consequent upon ligaturing of piles was thus confused. I recall, too, another example in which the supposed gouty arthritis of a great toe was of pyæmic nature, the outcome of a suppurating otitis media. Garrod, it may be recollected, ranked pyæmia as one of the disorders to which gouty subjects were especially liable.
Gouty inflammation resembles most other forms of the same morbid change, but some, however, contend that the association of œdema therewith is pathognomonic. Indeed, by some of the older authors this concomitant feature of gouty inflammation ranked as a criterion differentiating it from “true rheumatic inflammation.” Œdema, of course, is not distinctive of gouty as opposed to other forms of inflammation. But its occurrence therein is, we would submit, but another token of its affinity with the infective arthritides. We need but recall the constancy with which local œdema is met with in, e.g., gonococcal arthritis. More typical of gout, however, is the desquamation of the cuticule that follows the subsidence of the acute arthritis. Here we are reminded of the similar peeling of the skin that occurs in another infective disorder associated with arthritis, i.e., scarlatina.
Acute gout is definitely paroxysmal. The attack, at any rate when primary, is relatively ephemeral, lasts but a few days, and after it has passed, as Cullen says, “leaves the person in very perfect health, enjoying greater ease and alacrity in the functions of both body and mind than that for a long time before experienced.”
In short, acute gout would appear to be a self-delimited disease, its fleeting duration predicating that if an organism be responsible, the same is short-lived. Even in chronic gout, though it never quite loses its grip of those it has made its prey, yet nevertheless there are intervals of respite between the attacks, however long the latter may be. In other words, the disease never loses its paroxysmal character, which to my mind is very suggestive of a serial infection.
The periodicity of gout was, as we have seen, well known to the[192] ancients. Its recurrence in early spring and late autumn has even been celebrated in verse:—
Scudamore referred its prevalence at these particular seasons to their attendant vicissitudes of heat and cold (the strongest of all the exciting causes of gout). Trousseau states that “gout with successive paroxysms shows itself early or late in the year, at the beginning of spring or late autumn, the wherefore I know not.”
This tendency on the part of acute gout to seasonal rhythm is ultimately lost. For, once the disorder is established, no period of the year confers absolute immunity. Whatever be the explanation of the vernal and autumnal incidence of gout in its early stages, this peculiarity is at any rate not incompatible with its infective origin. In this connection it may be recalled that it was once described as “a tertian fever terminating in fourteen days.”
Again, further evidence may be obtained from the action of colchicum, our sheet-anchor in the treatment of gout. Thus, Dixon and Malden have shown that colchicine has no action on the metabolism of purins or on the kidney. On the other hand, it causes a primary diminution followed by a marked increase in the number of leucocytes, which suggests the possibility that it exerts its beneficial effects by combating infection.
Lastly, turning our attention to the anatomical changes as disclosed after death during an acute articular paroxysm, these present appearances quite compatible with their infective origin. Dr. Munro, in one of my examples of acute gouty polyarthritis, aspirated the knee joint. The results of cytological examination were precisely such as are deemed characteristic of arthritides of infective source.
The results of our analysis of the component elements of an acute paroxysm of gout are, for the following reasons, strongly indicative of the intrusion of an infective element:—
(1) The onset, temperature curve, the character of the local phenomena, and course of the disorder.
(2) The presence of leucocytosis with secondary anæmia, and exceptionally of leucopenia.
(3) Enlargement of the lymphatic glands, and possibly of the spleen.
(4) Occasional complication of the acute articular disorder by lymphangitis and phlebitis.
(5) The paroxysmal nature and periodicity of the disorder.
(6) The compatibility of the morbid anatomical changes and the cytological content of aspirated joint fluid with their genesis by infection.
If the onset, phenomena, and course of acute gout are reminiscent of infection, so, also, does a review of the life history of the disease, as a whole, carry with it the same inference.
For the course of gout, like other arthritides of chronic type, is not one of steady, uninterrupted progress, but one marked rather by periodic or intermittent advances, as if seemingly due to a series of successive infections or sub-infections. One is reminded of gonococcal arthritis in its more severe forms, the acute exacerbations which chequer its course being generally referred to intermittent absorption of fresh doses of the toxin from some smouldering infection in the prostatic urethra.
Now, if the general course or evolution of gouty arthritis is notably similar to that of the specific infective arthritides, so, also, do the clinical features approximate. Thus its onset, more often than not, is abrupt and attended by pyrexia of irregular or septic type, with an occasional leucocytosis.
Again, that not all cases of gout are of acute fulminant type may be admitted. We know that it may assume the guise of a fleeting arthralgia or “flying gout,” a transient synovitis, as well as an acute arthritis of mono-, oligo-, or poly-articular extent. This same polymorphism in respect of the joint lesions in gout is a replica of that met with in the specific infective arthritides. The milder varieties betokened by arthralgia or synovitis tend commonly to disappear, as it were, spontaneously in precisely the same manner as the arthralgias or synovites that follow the exanthemata, and we presume that, comparably with these latter, the source of infection dries up and restitutio ad integrum of more or less completeness follows.
But with repeated attacks, as in the specific infective arthritides, progressive infiltration and thickening of ligaments, capsule, and related tendinous and aponeurotic structures ensue. As far as these anatomical changes are concerned, gouty arthritis and the specific arthritides are at one, but with this outstanding difference, the associated uratic deposition. Save in respect of this last, the analogy is complete, and herein resides the specificity of gouty arthritis.
Chalmers Watson, from his observations of “gouty deposits” in human subjects in their relation to tendons, cartilage, and bone, came to the conclusion that the tout ensemble of the pathological lesions was very reminiscent of that typical of the more chronic types of infective disorders. Thus necrotic areas in gouty tendons stood in such clear relationship to the vascular supply as to suggest some infection viâ the blood-stream. Again, areas of erosion in the cartilage were found to be due, not to uric acid, but to the disintegrating action of small round cells of the nature of granulation tissue.
As to uratic deposits located in the bones, it was noted that their vicinity was characterised by marked vascularity, the existence of giant cells, and an accumulation of the small round cells so commonly correlated with the action of bacterial toxins.
In reviewing the foregoing clinical and pathological data and, alike, the inferences as to their significance, it cannot, we think, be gainsaid that, collectively, they are more readily explicable as being due to an infection than to any other morbid source.
A striking parallel can be drawn between the varied manifestations of gout and those met with in specific infections. But, to begin with, we must recall that our attitude towards infective disorders, e.g., acute rheumatism, gonorrhœa, etc., is altered in that we regard them now, not as local, but general, systemic infections.
Thus, following the revelations of bacteriologists, we now, for example, recognise that in gonococcal infection not only may there be articular involvement, but that muscular and nervous lesions may be associated therewith. This same, also, in acute articular rheumatism. True, its causal organism is still sub judice, but data accumulate as to the frequency with which the muscles are involved, and, to a less extent, the sheaths of nerves.
Take dysentery, again; it, too, as Sydenham pointed out, may be complicated, not only by arthritis, but by myalgias, while more recent experience emphasises the frequency with which neuralgias are associated therewith. In syphilis, also, the association of articular, muscular, and nerve lesions is well attested; and by French physicians it is insisted that, in tubercle, myalgias and neuralgias, as well as joint disorders, are infinitely more common than is generally realised.
To sum up, this triad of arthritic, muscular, and nerve lesions, either serially or simultaneously, is the most common complication[195] of specific infections. Now, is not this same congeries of articular, muscular, and nerve disorders precisely the clinical content of gout?
Thus its articular manifestations constitute the most striking feature of the disease. As to the muscular troubles, there is a consensus of opinion as to their relative frequency. Inflammatory foci with associated uratic deposit have been found in muscles and tendons. We may here recall that the purin bases of the body exist, not only in the bound form (nucleic acid), but also free, especially in muscular tissue, also that from such free purin bases uric acid can be as readily formed as from those liberated by disruption of nucleic acid.
Clinically, one meets with all forms of fibrositis in actual association with acute articular gout. Such may affect either the neck, shoulder, loin, or sciatic nerve. In their work on “Fibrositis,” Bassett Jones and Llewellyn have shown that the disorder develops with significant frequency in the victims of gout. This but confirms the conviction held by Gowers, Garrod, Hilton Fagge, and others, viz., that the muscular and nervous types of fibrositis are frequently and obviously related to gout.
How noteworthy the well-established proclivity of gout to involve bursæ, tendon sheaths, and fasciæ, especially the plantar! Is not this exactly paralleled in certain infections? Note the predilection of post-scarlatinal rheumatism for bursæ and tendon sheaths; that of the gonococcus for these structures as well as fasciæ, not to mention the frequency with which bursal enlargements are traceable to syphilitic, tuberculous, and other infections.
We see, therefore, that in virtue of its tendency, not only to arthritic, but also to muscular and nerve disorders, gout falls into line with the specific infections. Its predilection for bursal and fascial structures is but another evidence of affinity with this group of disorders. In view of these similitudes, one may well ask, Are not these gouty manifestations, all of them, susceptible of a like explanation, viz., that they are the outcome of an infection?
For, in reviewing the foregoing analogies, it cannot, we think, be denied that in the aggregate they are emphatically suggestive of an infective origin.
In essaying this difficult task, we must recall to the mind of the reader our findings or deductions from the data disclosed in preceding chapters.
The outstanding conclusions that we felt justified in formulating were that:—
(a) Uric acid is not the cause but the consequence of gout.
(b) Inflammatory reaction is, we believe, an invariable precursor in all gouty processes.
In other words, we suggest that, although abnormalities of metabolism form an integral part of gout, they are of themselves inadequate to achieve its efflorescence. Thus, when we came to consider the elemental manifestations of gout, i.e., uratic deposits or tophi, we saw that neither the purely physical nor the purely chemical theory of their origin would suffice, nor, for that matter, could any solution of this complex problem be gleaned from even a blend of the twain. In short, such hypotheses are too mechanical. The intrusion of some other factor, “some vital something biological,” seems essential for the elucidation of uratosis, i.e., uratic deposition. For this, not uricæmia, is the specific characteristic phenomenon of gout. If we cannot explain uratosis on physical or chemical grounds, then how much less, in view of the non-toxicity of uric acid, can we, on this basis, account for the inflammatory phenomena of the disorder?
Inflammatory reaction is, we hold, an invariable antecedent in all gouty processes, whether of articular or ab-articular site. Granted that inflammatory reaction is a necessary prelude, the specificity of gout is attested by the fact that this same is followed by the deposition of urates. But while the sequential uratic deposition invests all forms of “gouty” inflammation with a specific character, unshared by any other disease, it follows that the cause of the said inflammation must, if possible, be ascertained.
For Walker Hall “the contention that gout lowers the general tissue resistance, and so opens the way to bacterial infections, is so obvious that it need hardly be formulated.” In light of this, we need have the less diffidence in hazarding our opinion that the morbific agent responsible for “gouty” inflammation is an infection or sub-infection. Now, in all forms of arthritis other than gouty, the intrusion of a germ is held to be self-explanatory and final; in short, all the local morbid changes and constitutional disturbances are held satisfactorily accounted for by the organism or its toxins.
The problem of gout, however, is not so simple. Its arthritis is peculiar in that it is always accompanied or followed by uratic deposition, which, be it noted, is not an ordinary sequel of inflammation. It is, in short, the outcome of inflammation supervening in an individual of gouty diathesis. What do we know of this latter?
The researches of the bio-chemists reveal that uric acid is the[197] end-product of nuclein metabolism—the summation of a long chain of enzymatic reactions. Some indeed have thought to find an adequate explanation of gout in enzymatic abnormalities. Thus, Adami and McCrae suggest that gout is the outcome of insufficient oxidation, whereby the precursors of uric acid and similar bodies are not fully oxidised, and, by their accumulation and toxicity, set up morbid changes, and the uric acid formed is, in its turn, imperfectly oxidised and accumulates. This diminished oxidation is due to a constitutional deficiency of oxydases, inherited or acquired.
This opens up the old problem as to whether uric acid is an intermediary or a terminal product of metabolism. But, from evidence cited in preceding chapters, it appears probable, if not certain, that uric acid is an end-product. Moreover, as Gideon Wells observes, “the failure of recent studies on the enzymatic transformation of purins to locate anywhere in the human body an enzyme-destroying uric acid makes hazardous the attempt to explain gouty metabolism as a result of enzymatic abnormalities.”
Indeed, in view of this, as hitherto ascertained, absence of uricolytic enzymes, there can, as Wells says, “be little doubt that the fundamental reason for the existence of uric acid gout in man lies in the inability of the human organism to destroy uric acid. Consequently, inasmuch as man, unlike other mammals, cannot destroy uric acid rapidly by oxidation, he is always a potential victim of uric acid retention and deposition.”
Now we have, we hope, shown that there is no evidence that the uric acid retention in gout is due to functional inability on the part of the kidney to excrete uric acid. This being so, we have, as Von Noorden rightly says, no right to do violence to the facts by assuming that, in a case lacking any other evidence of nephritis, a condition of “latent nephritis” is the cause of the uric acid retention and deposition.
Similarly, there is at present no evidence forthcoming that the retention of uric acid is due to abnormal purin combinations in the blood. Nay, according to Wells, on the best evidence obtainable, uric acid exists in a free state in the blood, and not combined, as has been urged by many workers in this sphere.
But if the cause of uric acid retention lies neither in the kidneys nor in the blood, there must exist something abnormal in the gouty individual which renders impossible what may be termed a compensatory uric acid excretion. Now, as disclosed in the previous chapter, experimental research, in diseases other than gout, has shown that the bodily tissues have an appreciable capacity for retention of uric acid (Fine). This, moreover, gains probability from the fact that Wiechowski, in his prolonged studies as to the[198] possibility of uric acid decomposition in the human body, was never able to detect any evidence of uricolysis. Furthermore, on the clinical side, the fact that intravenous injection of uric acid does not produce a corresponding degree of uricæmia seems, as Bass and Herzberg suggest, to indicate that in gout the retention capacity of the tissues for uric acid is augmented. Lastly, in the precipitation and anchoring of urates in the tissues in gout, we have objective proof, i.e., tophi, that the uric acid is actually held in the tissues.
Does not this seem to indicate that there are peculiarities of tissue in the gouty? What, then, the subtle change that determines the retention and deposition of urates in the tissues in gout?
May we not, with Walker Hall, hazard the reflection that there may be differences between the nucleotides of normal and gouty tissues? For, doubtless, if there be peculiarities of tissue in the gouty, these will be reflected in abnormalities of tissue function and metamorphosis.
Gowlland Hopkins, discussing the metabolism of purins, holds that in gout there is some disturbance or defect in the fermentative functions of the tissues. Of a verity the range of intranuclear activities offers scope enough when we recollect that the cells of all tissues contain not only nucleinase, but also nucleotidase and nucleosidase. Even so, the resultant nucleins, the nucleotides, and nucleosides, have still further changes of deaminisation and oxidation to undergo, these carried out in the liver and elsewhere!
We may talk of defects in the enzymatic functions of the tissues, but, viewing gout clinically, and more particularly the hypersensitiveness of its victims to the most varied stimuli, dietetic and other, one inclines rather to predicate in their instance an inherent instability of nuclein metabolism. For in the gouty, as Walker Hall observes, “a slight injury or indiscretion of diet, an overloaded intestine, or increased toxicity of the intestinal flora, may be followed by a disturbance of the general nuclein metabolism, and a local reaction in certain tissues.”
With this pronouncement all clinicians will be in accord, and herein, too, we may, I think, discern how the latent tissue idiosyncrasies of the gouty are evoked, i.e., by infection; in other words, that, under the influence of these morbific agents, the innate morbid potentialities of the gouty become overt and manifest.
The exact modus operandi whereby the assumed organisms or their toxins determine the efflorescence of gout is uncertain. We know that, following the intake even of non-purin-containing foodstuffs, an increase in uric acid excretion ensues, and that the same is the outcome of the stimulation of general nuclein metabolism.[199] Is it not conceivable that the responsible toxin acts in like fashion, and haply by disturbing the orderly sequence of those exquisitely delicate enzymatic reactions which culminate in the formation of uric acid, and with which potentialities every living cell in the organism is dowered? Further than this we, pending future researches by the bio-chemists, may not go, for “the positive material is much too insufficient, and much too ambiguous.”
In conclusion, I would postulate that in gouty subjects:—
(1) There is an inherent abnormality or instability of nuclein metabolism, and conjoined therewith an enhanced tissue affinity or augmented retention capacity for uric acid.
(2) These latent tissue peculiarities, through the agency of infections or sub-infections, become manifest as gout.
(3) The said organism or organisms excite inflammatory reaction with sequential uratic deposition, either of articular or ab-articular site.
(4) The predilection of such uratic deposition for certain particular tissues is determined by their greater content of sodium ions as compared with the blood.
(5) The local and general phenomena of gout, its paroxysmal nature and tendency to periodicity, are most readily explicable on the basis of a chronic infection supervening in a subject the victim of those innate peculiarities of tissue with their correlated obliquities of function which connote what we term the “gouty diathesis.”
If we would clarify somewhat the obscurity that enshrouds the genesis of disease, our watchword must here, as in other spheres, be “Despise not the day of small things.” We know not the proximate cause of gout, it is true, nor the exact modus operandi of those agents, infective or other, which bring to fruition the latent morbid potentialities of its victims. But, even if so handicapped, we should be quick to descry those portents of the coming storm, those minor backslidings from physiological righteousness, that doubtless foreshadow the outbreak of the disorder.
For it cannot be doubted that the evil potentialities which make for gout are for long in operation before their definite installation in its chosen seat, the joints, ensues. As Trousseau puts it, “The diathesis is in action before there is time for the local affection to show itself in a precise form.” In short, given imminence of an attack, the whole system is charged with gout, or, as Sydenham laconically expressed it, “Totum corpus est podagra.”
While we recognise that local inflammatory reaction in the joints is more particularly characteristic of gout, it is no less necessary that we take cognisance of the general precursory symptoms that often, if not always, usher in its onfall. Gout begins in a disorder of function.
Uncomfortable sensations may obtain days and weeks before the incidence of the fit. To old time sufferers they are sufficiently alarming. But their significance, as heralds of an initial attack, by victim and too often by physician also, is usually only appreciated when the threatened fit becomes an actuality. Speaking of premonitory phenomena in gout, Sydenham remarked, “Its only forerunner is indigestion and crudity of the stomach, of which the patient labours some weeks before,” and doubtless this is in the main true.
As Trousseau long since observed, the patient’s appetite often becomes capricious. He likes his meat strongly spiced, and craves for acids. But his satisfaction is short-lived. For eating is followed by drowsiness, feelings of oppression and fulness, with unpleasant eructations, or more rarely definite retching. The bowels are generally costive, but in exceptional instances diarrhœa has been noted. The state of the urine is variable. Generally scanty and high-coloured, it may in some be copious and pale.
Uneasiness in the right hypochondrium and even slight swelling of the liver was noted by Trousseau and also by Scudamore. Such congestion of the portal system and hepatic enlargement may be only fugacious, but often the same is permanent, a penalty of the same cause—free living—which leads to the production of gout. For in many instances but too true is it that “for years together,” as Sydenham said, “a man has drunk and feasted, has omitted his usual exercise, has grown slow and sluggish, has been over-studious or anxious, in short, has gone wrong in some important point of life.”
But more palpable to his friends than to himself are the concomitant changes in his disposition and character. From being good-natured and easy-going he becomes morose and irritable. The irascibility of the gouty is proverbial, and the explosive mental outbursts to Duckworth appeared at times to be “a metamorphic substitution for a more overt and regular attack,” or, as Sydenham expressed it, “Non rectius podagræ quam iracundiæ paroxysmus omnis dici potest.”
Sometimes his mental vagaries are exchanged for or accompanied by neuralgia, painful cramps in the limbs, etc. In truth, the premonitory phenomena of gout are protean, inasmuch as, given any prior weakness or functional derangement of any viscus, the symptoms of oncoming gout are masked by aggravation of the same, it may be by cardiac irregularities, vesical irritability, or in an old bronchial subject by increase of cough, etc.
But it may be objected, there is nothing specific about these various functional disturbances. They are not more common in the gouty than in others. Moreover, the habits of life productive of gout favour the development of gastric and hepatic derangements. The mental irritability, the gastric disturbances, etc., may be quite as well accounted for by overeating and overdrinking as by gout.
Now, if there be nothing specific of gout in these so-called prodromata—“heartburn, acidity, flatulence, etc.”—then what is their true significance? For, obviously recognition of their true import is most essential. Now to my mind the said “dyspeptic”[202] symptoms should be regarded not as symptomatic of gout, but as etiologically related thereto.
For, though the etiology of gout is still much debated, the same obscurity will certainly not be clarified, if we merely content ourselves with dubbing such “dyspeptic” symptoms as “gouty.” On the other hand, if we, at this early stage, endeavour to elucidate the true origin of the “dyspeptic” symptoms, who will deny that this is the more rational and scientific mode of procedure? The timely elimination of septic foci in the mouth, tonsils, and naso-pharynx conjoined with modification or restriction of food intake and recognition betimes of the signs of intestinal infection and constipation would perhaps stave off or avert the threatened articular outbreak.
It has been suggested that there is some statistical evidence that “acute rheumatism” has declined in frequency since the introduction of tonsillectomy. In the same way, I cannot help thinking that the growing infrequency and attenuation of gout is in part due to increasing appreciation by the laity and the profession of the vital importance of oral hygiene and timely and radical treatment of local foci of infection. The fact that in children, victims of so-called infantile gout, the purin metabolism may show those same derangements held typical of the subjects of gout, is surely an indication that the disorder begins betimes, and that we too must not tarry if we would prevent these evil potentialities coming later to fruition.
Now, if there be nothing specific of gout in the “dyspeptic” derangements held prodromal thereof, the reader may well ask the pregnant question, Are there any symptoms or signs that will enable one to identify the victim of these minor discomforts as being “actually” or “potentially” a “gouty” subject? In attempting to answer this reasonable query one would emphasise the fact that tophi in the ears or at other sites sometimes antedate articular outbreaks.
Now given that an individual exhibits auricular tophi, one or many, can anyone deny that he is “gouty,” nay more, that he has gout, this even though he never has had, or may never have, an articular outbreak? In truth, the eruption of a tophus in the ear is as essentially a “fit of gout” as if it had occurred at the classic site, the big toe.
How vivid the light then thrown upon the import, the etiological significance, of otherwise inexplicable functional derangements! How grim the potentialities of, e.g., “dyspeptic” symptoms as revealed by detection in the subject of a tophus! Whether viewed from the diagnostic or prognostic aspect, its importance cannot be overestimated. For let us not forget that the tophus is the one[203] incontrovertible token of the “gouty diathesis.” This morbid localisation is the sole outward expression of the inward and dominant pathological trend.
The great Charcot did not despise its aid. He narrates the case of a man thirty-five years of age, a sufferer for some months from “acid dyspepsia,” in whom he predicted a fit of gout from noting an uratic concretion in one ear. Is not the moral obvious that in an individual complaining of gastric or hepatic disturbances, etc., we should, at any rate, examine the ears for tophi?
For, far more often than is currently realised, their eruption antedates the articular outbreaks.[27] Moreover, they may not be solitary, but numerous, the cutaneous gravel of older authors. In truth, these cases of tophi, uncomplicated by articular lesions, seem to merit some distinguishing term, representing as they do a purely ab-articular form of gout.[28] They constitute what might be termed primitive elemental gout, of which the subsequent articular outbreaks are but an extension, a further manifestation of the “gouty diathesis.” For it is just this same tendency to uratosis or deposition of sodium biurate, and this alone, that to our mind constitutes gout, this “primordial vice of nutrition,” not the congeries of distempers that with the passing ages have clustered around the primitive gout, well-nigh submerging its identity.
Premonitory Symptoms of Tophus Formation.—While tophi may antedate articular attacks, we do not always meet with them as mature concretions easily recognisable as such. We must have regard therefore to the symptoms and signs indicative of their impending eruption. Consequently in a patient complaining of the various functional disturbances that so frequently anticipate gout we should never dismiss as trivial any complaints of pricking or tenderness in the ears.
Sometimes the pain in the ears is acute, the tenderness such as forbids their pressure on a pillow. Graves, of Dublin, not only noted that the pain in some instances was agonising, lasting a few hours, but he himself suffered also from such attacks of auricular pain, which only disappeared when gout supervened in his fingers. I have myself frequently known the pain and soreness referred to chilblains, though later their tophaceous nature was disclosed.
Given such auricular pain and tenderness, we should examine the pinna for small red swellings.[29] These, when definitely localised, should be punctured and the thick white fluid which exudes examined microscopically for urate of soda crystals. In some instances the creamy-like exudate does not yield a crystalline deposit, and Dr. Munro and I are inclined to believe that there is a pre-uratic stage in the evolution of tophi. We have observed this absence of crystalline deposits in apparently unmistakable tophi, as evidenced by the usual pearly white concretions in the rim of the ear. I recollect that the late Sir William Osler, when visiting our laboratory, was deeply interested in this possibility, as suggested by Dr. Munro, of a pre-uratic stage. Needless to say, all local sources of fallacy—Woolner’s tip, fibroid nodules, sebaceous cysts—were excluded, while, in the lack of crystalline proof, the evidence in favour of the associated arthritis being gouty rested on its being at the classical site, the great toe. Moreover, as an alternative explanation we have the possibility of reabsorption. We may recall Duckworth’s well-known example where a man had two attacks of gout in the right great toe joint, yet autopsy revealed no speck of uratic deposit. We know, too, that, following an acute attack, tophi may diminish in size or even disappear, while coincidently fresh tophi form at other sites.
Premonitory Articular Pains.—Again, when, in association with indigestion or other premonitory symptoms, twinges in the toe recur from time to time, especially after consuming wines or certain articles of food, these same are very suggestive of impending gout. Garrod is very definite on this point: “I have no doubt that many persons experience extremely slight attacks of gout before the development of the affection in an acute form, and several of my patients have assured me that for years before their first severe attack in the great toe they have felt slight periodic twinges. I am of opinion that when such twinges occur deposition has already taken place.”
In conclusion, we would urge that, given gastric or hepatic disturbances, etc., in a subject predisposed by heredity or habits to gout, we should note the presence or absence of the following:—
(1) Pain, pricking, or tenderness in the ears, with or without small red swellings.
(2) Similar sensations at site of finger joints, with dorsal swellings over which the skin may be red or unchanged.
(3) The existence or not of pearly white concretions, i.e. mature tophi (as tested microscopically), at the above sites or elsewhere.
Further signs that may be sought for in cases of doubtful nature, i.e. unevidenced by tophi, would be:—
(4) The presence of uricæmia.
(5) A lowered or sub-normal output of uric acid in the urine.
(6) Diminution or retardation of the output of exogenous purin.
To take up the thread of our narrative regarding the prodromal symptoms which at any moment may give place to an articular outbreak. The determinants or exciting causes having been already dealt with in the section on etiology, we shall here only note those symptoms or signs that portend the imminence of the paroxysm. These are very variable. But it is suggestive if without any change in the habits the “dyspeptic” symptoms abate somewhat or disappear.
Indeed, it is well recognised that, whatever the nature of the prodromal phenomena, they all tend to cease just before the oncoming attack. Occasionally a pre-existing depression gives way to a feeling of exuberant health or well-being. We recall the instance of a celebrated physician whose lectures always just prior to an attack took on an added brilliance.
Reverting to more definite harbingers, it has been noted that the urine becomes scanty, and its content of uric acid much diminished, some three or four days before the paroxysm, though such is not invariable. Easier of note and widely recognised is the fact that in those exhibiting tophi pricking pains or tenderness are experienced at their site. Scudamore, Garrod, and Duckworth are all agreed on this point. Another sign noted by Sydenham was that the veins of the part about to be affected become engorged—a feature confirmed by Trousseau and others.[30]
A brief interlude, lasting a few hours or a day, frequently intervenes between cessation of the prodromal discomforts and the onset of the attack. This delusive sense of well-being deceives none but the uninitiated, for to the old time sufferer it is but the truce before the threatened assault.[31]
Still the subject feels better and more placid than his wont, seeks his bed, and sinks to sleep (“sanus lecto somnoque committur”).[206] But suddenly, more commonly an hour or two after midnight, he awakes to a pain in the foot, usually in the ball of the great toe, though more rarely in the heel, instep, or ankle. Simultaneously he becomes chilly, shivers, or has a rigor. But as the pain, at first bearable, grows in intensity, these feelings lapse, giving way to feverish restlessness. Posture after posture is renounced, but, toss as he will, he strives in vain to find a place[207] of ease for the tortured limb. Even the pressure of the bedclothes is intolerable. But towards morning (“sub galli cantu”) the pain remits as suddenly as it began. Anon the sufferer breaks into a gentle sweat, falls asleep, and wakes to find the painful part red, swollen, tense, and shiny, surrounded with œdema and turgid veins.
The same series of events recurs, though often in mitigated form, for some days and nights. During the day his pain is lulled, but towards evening it gathers in intensity to cease or diminish towards morning. The cycle continues from eight to ten days; then pain ceases, redness fades, œdema subsides, and the inflamed cuticle peels, with itching. The temperature meanwhile has sunk to normal, the local tenderness and stiffness gradually pass off, and health is restored. “Gout is the cure of the gout,” said Mead long since, and certainly recovery from the first attack of gout is usually speedy and complete. A renewed sense of bien-être ensues, free from the discomforts that led up to the outbreak. Indeed, in exceptionally rare instances the disease seemingly exhausts itself in a single paroxysm, or decades may pass before another visitation. Sir William Roberts tells of a Yorkshire squire who sustained a classical attack in his twenty-seventh year, the next in his eighty-ninth year. Frequently a second attack may not occur for one, two, or even three years. But the tendency to recurrence usually becomes more and more pronounced as the years roll on, and eventually the gouty man resigns himself to the doleful expectation of an attack once or twice a year, during spring or fall, with some approach to periodic regularity.
Initial attacks of gout are usually monarticular, but consideration of the polyarticular variety will best be postponed until we come to consider acute gouty polyarthritis. Also we think it will be more convenient for us to defer discussion of retrocedent gout to the chapter dealing with the irregular or anomalous types of the disorder. Meanwhile we will now proceed to detailed description of the individual phenomena that make up the clinical content of acute gout.
Onset.—From Sydenham’s classical account it might be inferred that the onfall of gout is always fulminant. But this is far from being the case. For I find myself in agreement with Hilton Fagge that in many, if not the majority of instances, even the initial outbreak of the disorder is installed in a far less dramatic manner. Certainly in not a few cases its manner of approach is insidious, not to say stealthy. At onset then the nature of the case is therefore frequently misinterpreted both by victim and physician. The free liver, fearing that Nemesis has overtaken him, is fertile[208] in suggestion. He has overwalked, his boot pinched him, or it is a sprain. Local appearances may be non-committal. There may be no swelling nor redness, and no access of pain at night. Still there is discomfort when he walks. The so-called sprain lingers, and one morning the great toe, instep, or ankle, is swollen, tender, flushed, and the victim’s fears and the physician’s suspicions are converted into certainty: it is gout!
Still in this matter of the onset I must not overlook the findings of my colleague James Lindsay. In 569 cases, the onset was sudden in 458, and in the remaining 111 examples gradual. It was noted that only 14·5 per cent. of the male cases were of gradual onset. But no less than 47·1 per cent. of the female cases developed after this fashion.
Again to resume, it is by no means invariably the case that the onset is nocturnal. For, as Duckworth has pointed out, many attacks begin during the day, and this is perhaps more often the case after the disorder is fully established.
Locality.—Gout in its classical form is monarticular in distribution. In 375 out of 512 initial seizures, Sir Charles Scudamore found that the metatarso-phalangeal joint of the great toe of one or other foot was the joint affected. Garrod, too, noted that, excluding the great toe, in not more than 5 per cent. were other joints implicated. As to the frequency of incidence in joints other than the big toe, opinions differ. For Scudamore it is the ankle, for Garrod the instep, and afterwards the outer side of the foot and the knee. In contrast, Hilton Fagge holds that next to the great toe gout vents its initial fury with greatest frequency upon the metacarpo-phalangeal joint of the index finger, adding, “certainly not the thumb.” Most authorities however agree that gout in its early stages rarely attacks the joints of the upper limb, and even in its most inveterate form the shoulder and hip joints are immune. Personally, I have never seen a case of gout in the shoulder or hip; such cases are usually examples of osteo-arthritis.
Exceptionally, even in first seizures, more than one joint may be affected. Thus it may migrate from one big toe to its fellow, or travelling further afield, may invade ankle, knee, wrist, or elbow, or small joints of hand. W. Gairdner held that in gout the joints of the left were more commonly attacked than those of the right limb. But James Lindsay’s figures would appear to indicate precisely the reverse, viz. a predilection for the right side of the body.
Pain.—If we may accept the lurid imagery of its victims, even the tortures of the Inquisition failed to transcend in agony the—
Sydenham said that at its onset the pain was as that of a dislocation (ossium dislocatio). At its zenith it was as if the flesh was being gnawed, squeezed in a bootscrew, or scalded by molten lead or boiling water. Sensory perversions are superadded, and, as Ambrose Paré said, “some patients say they burn, while others complain of icy coldness.”
Its peculiarly exasperating nature is well illustrated by Hosack, an old time Professor of Medicine of New York, who thus delivered himself: “Some compare it with the gnawing of a dog, the pressure of a vice, or the pain of the actual cautery; this probably is not far from the truth, judging from the anecdote I have heard of a man subject to gout. This man falling asleep barefooted before a large fire, the fire fell, and a large coal found its way to his foot; half awake and half asleep, he cried out: ‘There’s that d——d gout again!’ He at length awoke, when he found a large coal frying his great toe. The sensation of the two evils was probably the same.”
The pain is aggravated in that frequent “startings” of the limb prevent the victim keeping the foot at rest. The slamming of a door, or the incautious shaking of the bed, so quickens its throbbing intensity as provokes a literal frenzy of rage. But fortunately it is not always so. For though the pain of gout is unquestionably severe, at times excruciating, yet it presents infinite grades of severity. Also one must recollect that but too many of its victims are already in a high state of irritability before the outbreak. Moreover, their powers of self-control are too often sapped by unbridled self-indulgence, and they have but slight reserves of patience and fortitude to draw upon.[32]
Apart from the personal factor, in subacute cases the pain is notably less severe than in the acute sthenic form. The pain of gout, as a rule, is more intense than that of acute rheumatism, and, I fancy, than that of all other varieties of acute arthritis.[33] Sir Thomas Watson in his fascinating lectures tells of a witty Frenchman who, comparing acute gout and acute rheumatism in respect of pain intensity, remarked: “Screw up the vice as tightly as possible, you have rheumatism; give it another turn, and that is gout.”
Lastly, in respect of the duration of the pain, it is not always true that it wholly intermits at the approach of dawn. It does so frequently, it is true, but in some instances pain, more or less severe, continues during the day as well as the night. Occasionally,[210] on a crescendo scale, it continues increasing almost up to the crisis. Generally speaking, too, the shorter the duration of the paroxysm the more intense the pain, and the more prolonged the less the degree of suffering.
Following the crisis, the pain gradually becomes less and less, giving place to a feeling of numbness of the toe, which in older subjects may endure for some days.
General Phenomena.—Symptoms, other than those referable to the affected part, vary widely in different cases. In this respect the acute sthenic forms contrast with the acute asthenic types. In the former the pulse quickens; the temperature rises, but rarely exceeds 101°-102°, though Garrod saw it reach 104°. The tongue is furred, the breath foul, with anorexia and thirst. Though the appetite is frequently impaired or lost, yet in some instances it is retained. Dyspeptic symptoms, hiccough, eructations, etc., are sometimes prominent, but often wholly lacking. The bowels are constipated, as a rule, the stools pale, or dark and extremely offensive. The urine is generally scanty, high-coloured, with a lateritious sediment on cooling. It may contain a trace of albumen. Severe cramps affecting muscles of the leg, thigh, and upper parts of the body, are more or less prominent symptoms in a considerable number of instances.
The pyrexia appears to be symptomatic, more or less in proportion to the acuteness of the local phenomena. Comparably the highest temperatures are usually met with in sthenic forms in relatively young or robust middle-aged subjects. Duckworth noted the interesting point that “a preliminary rise is commonly noted for one, two, three or four days before a joint is actively involved.” With the articular outbreak the febrile movement becomes more active. The temperature runs up to 100° or over, but with the morning abatement sinks to normal or nearly so. The following evening it rises again frequently to a higher level, 102° with a morning remission, and so it continues for a variable number of days, it may be only two or eight to ten. It then subsides, and frequently for a few days remains sub-normal. Lastly, the acute asthenic forms, that occur often in women (Garrod), may be wholly afebrile.
Changes in the Blood.—Apart from its increased content of uric acid, further morbid changes take place in the blood in gout.
Neusser in 1894 described what he termed “perinuclear basophilic granules” over and about the nuclei of the leucocytes in the blood of gouty patients. He held that the dark granules constituted the mother substance from which uric acid was derived, and that their presence in the blood was distinctive of the “gouty diathesis.” Subsequent researches, however, by Futcher and[211] others appear to have shown the absence of any interrelationship between the amount of these granules and uric acid elimination, though Neusser claimed that cases showing them excreted uric acid in excess.
More significant, however, is it that the blood in acute gout may show a high grade leucocytosis with secondary anæmia.
In a case under my care of acute gout at classic site, though by no means of unusual severity, the following was the content of the blood picture:—
Blood Count.
| Red corpuscles, per c. mm. | 3,692,000 | = | 73·8 | per cent. |
| Hæmoglobin | 80 | ” | ||
| Colour index | 1·08 | ” | ||
| Leucocytes, per c. mm. | 25,920 |
Differential Count.
| Lymphocytes | 8·0 | per cent. | = | 2,074 | per c. mm. |
| Large mononuclears | 3·5 | ” | = | 907 | ” |
| Polymorphonuclears | 87·0 | ” | = | 22,550 | ” |
| Eosinophiles | 0·5 | ” | = | 130 | ” |
| Mast cells | 1·0 | ” | = | 260 | ” |
| 100·0 |
The salient feature of the blood picture is the high grade leucocytosis of leucoid type with moderate anæmia—appearances quite compatible with, and suggestive of, an infective arthritis. To these interesting blood changes we shall again refer when dealing with the acute polyarticular variety, the above case being of monarticular type, i.e., the big toe.
Uric Acid Excretion.—If when on a purin-free diet a gouty subject develops a paroxysm, the curve of uric acid excretion in the urine is so characteristic as to be almost pathognomonic of the disorder. As His pointed out, immediately before the onset of the paroxysm the endogenous uric acid sinks to a lower level (termed by Umber the anacritical stage of depression). With the onset of the attack the uric acid content of the urine quickly increases, to reach its zenith on the second or third day. F. Pfeiffer, who first noted this point, termed it an uric acid wave. Subsequently, with the gradual subsidence of the paroxysm, it again drops into what Umber termed the post-critical stage of depression. While this curve of endogenous purin excretion may be modified by oft recurring exacerbations, still Umber holds that nevertheless it is of decided value in differential diagnosis.
Local Phenomena.—The site and character of the pain having been dealt with, we now pass on to consider the objective changes in the affected part. The local engorgement of veins that precedes the articular outbreak becomes more pronounced, extending from the vicinity of the painful joint as far as the leg. The overlying[212] skin of the joint quickly becomes red and tumid. It is not a bright, but a dark red, the superjacent skin taking on a shining smoothness that has been compared to the peel of an onion. Indeed, in its more violent form it resembles but too closely the ordinary appearance of an abscess, over which the skin is becoming thin. The redness is not strictly confined to the surface of the joint, but spreads a little beyond, and where it ceases œdema is perceptible.
The redness in its intensity attains its zenith in from twenty-four to forty-eight hours, and then in hue becomes more violaceous. On the other hand, the œdema may go on increasing for some days. At first, owing to tension, the presence of œdema may not readily be elicited. But with the subsidence of inflammation the swollen parts readily pit on pressure. It is scarcely possible to detect intra-articular effusion unless it be the ankle joint that is involved.
According to Duckworth, in the more sthenic forms there may be local ecchymoses. With the crisis the redness, œdema, and venous turgescence die down. The previously distended skin becomes wrinkled, and with complete subsidence of inflammation desquamation ensues. This process is generally attended with troublesome itching. It is most noticeable about the feet and hands, but more rare at other sites. Scudamore said that in seventy-eight out of 234 cases no peeling occurred, but, as Garrod observed, it may readily be overlooked unless especially sought for.
The exquisite sensitiveness of the parts, as before noted, gives way to numbness. The diminished sensibility, coupled with stiffness of the joint, renders walking difficult for some days, and, indeed, a month or more may elapse before the joint, even in favourable cases, recovers its customary mobility.
In acute asthenic forms great contrasts appear. Pain and tenderness in the toe may be moderate, but there may be little local heat or redness and no pyrexia. But œdema is generally in evidence, and the usual desquamation of skin follows.
Tophus Formation.—To the local changes that mark their eruption at ab-articular sites we have already alluded. Here we would only reiterate that their formation follows the local joint inflammation. Consequently if a few days after the attack local pain or tenderness, with or without swelling in the vicinity of the joint, should be complained of, it should not be dismissed as of no account, but the affected parts should be scrutinised carefully and, where possible, at short intervals. This in the interests of diagnosis of a joint affection which may at the time have been of doubtful nature, more especially if the primary attack occur elsewhere than at the classical site. Some observations of[213] Trousseau are well worth quotation: “Physicians who have watched the progress of the evolution of tophus believe that it is formed during the paroxysm of gout. They are mistaken: the deposit appears during the interval between attacks, or at least when the attacks have not been of long duration, and when they do not recur in such rapid succession as to run into one another, in which cases their secretion has commenced during the preceding and continued during the succeeding attack.”
While gout may throughout its life history confine its ravages to the foot, if not solely to the toe joints, it may, even in the initial attack, involve many articulations. Such cases usually, if not always, occur in persons of marked gouty heredity. In its simplest forms the orthodox monarticular seizure is simply exchanged for a sequential implication of each big toe joint. If so, as Trousseau pointed out, the joint that is the last to be involved is least affected, and the soonest to get well again, while the accompanying œdema is of shorter duration. But in more severe cases not only the big toe, but the tarsal joints, the knee and the hand, may be invaded in the first attack. Occasionally, too, the disorder displays concomitantly its tendency to involve other structures, tendons and aponeuroses, e.g., the tendo Achillis, plantar fascia. Such widespread initial involvement is usually preceded by prodromal phenomena of unusual severity and prolonged duration. These initial attacks of polyarticular distribution are extremely rare.
Far more commonly acute gouty polyarthritis supervenes after several attacks of classic location have been suffered. The gouty inflammation in these cases invades the joints after a serial fashion. But each joint as it becomes involved goes through the same painful cycle. Thus, for five or six days the pain goes on increasing, then abates, and finally the wished-for crisis comes. So it happens that the gout may be raging simultaneously in several articulations, though in each at different stages of evolution. Consequently the symptoms do not pursue an even tenor, but are made up rather of a series of little attacks—series et catena paroxysmulorum, to invoke Sydenham’s expression.
Frequently periods of apparent recovery take place. The temperature remains normal for some days, and welcome convalescence seems established, when, to the victim’s despair, the temperature again rises, and the same weary cycle, though perhaps shorter, is yet to be endured. Running this chequered career, the disorder may last for six weeks or two or three months.
In such attacks not only the feet, knees, hands, and elbows, may be promiscuously involved, but often also the ligaments, bursæ, tendon sheaths, and aponeuroses. The suddenness with which the disorder shifts its seat from one joint to another, or from joints to bursæ or muscles, often leads to its confusion with acute rheumatism. In other words, that fixity distinctive of gout in its monarticular forms is here exchanged for mobility, that specific quality of acute rheumatism.
Naturally, the implication of so many varied structures casts its impress on the clinical picture, inasmuch as the physical characters vary with the different textures involved, their capacity for inflammatory distension, etc. On the dorsum of the hand and foot redness and œdema will be prominent, and Scudamore noted that the flush might be widely diffused, simulating erysipelas, with here and there small ecchymoses.
When structures more deeply placed, i.e., tendon sheaths at ankle, knee, and wrist, are singled out for attack, swelling is less marked and redness of the skin more patchy in distribution. The bursæ at the elbow or back of the knee may swell with extraordinary rapidity. The parts become exquisitely tender and painful, while the overlying skin takes on an angry blush. They may subside, but more often continue permanently enlarged, defiant of reduction.
Involvement of the olecranon bursa is very typical of gout. Pratt, of Boston (1916), tells of a case in which the subject had during twenty-seven years suffered from recurring attacks of acute gouty polyarthritis. The eight or ten physicians who had treated him had all regarded the disease as rheumatic fever. Pratt himself observes: “I did not feel sure of the diagnosis until I saw the swelling on his elbow, which presented the typical picture of a chronic gouty olecranon bursitis.”[34] Occasionally the bursæ when filled with uratic deposit undergo suppuration following injuries. The bursa in connection with the great toe frequently becomes acutely inflamed, and Scudamore in a gouty hand saw an old ganglion take on the same inflammatory reaction.
The tendon sheaths when involved lead to great disablement, as even the most tentative attempts at movement give rise to sudden and agonising cramp. The tendo Achillis is a favourite site, or the tendons of the wrist, or the ligament of the patella. The same is true of the aponeuroses, the predilection being for the lumbar or gluteal fascia, in which instance it may extend to the sheath of the sciatic nerve. These extensions of gout to[216] tendon and nerve sheaths frequently outlast the articular lesions, and may become the dominant element in the clinical picture.
Naturally, when not only joints, but bursæ and other structures, are involved and implicate both upper and lower limbs, the victim presents a pitiful spectacle, one of almost complete helplessness. Œdema and general venous turgescence may be very pronounced in one or more members, giving a subjective sensation of almost overwhelming weight in the limb.
Reverting to the constitutional symptoms, the outstanding feature is that, notwithstanding the widespread involvement of joints with manifest local inflammatory reaction, the pyrexia is of moderate grade, and so frequently, indeed, is it afebrile that this peculiarity is of diagnostic significance.
Changes in the Blood.—The findings are extremely interesting in view of the high grades of leucocytosis to be met with both in pyrexial and apyrexial examples.
In a case of acute gouty polyarthritis under my care the blood picture was a very striking one. The patient had suffered from gout for some eleven years, with recurrent acute exacerbations. There was widespread involvement of the joints both in upper and lower limbs. On the dorsum of the mid-phalangeal joints small semi-solid swellings were present, the exact nature of which was somewhat puzzling. But inasmuch as the pinna in both ears was studded with tophi, this seemed to provide a clue. The auricular tophi were verified microscopically. The extra-articular phalangeal swellings were then aspirated with a hypodermic syringe. A turbid straw-coloured fluid issued, which microscopically was found to contain biurate crystals. His temperature rose nightly from 101° up to 102° F., with morning remissions. The left knee and wrist were the seat of effusion, and some of the small finger joints were inflamed.
Blood Count.
| Red corpuscles, per c. mm. | 4,432,000 | = | 88·6 | per cent. |
| Hæmoglobin | 60 | ” | ||
| Colour index | ·68 | ” | ||
| Leucocytes, per c. mm. | 27,200 |
Differential Count.
| Lymphocytes | 9 | = | 2,450 |
| Large mononuclears | 13 | = | 3,540 |
| Polymorphonuclears | 78 | = | 21,220 |
| Eosinophiles | 0 | = | 0 |
| Mast cells | 0 | = | 0 |
| 100·0 |
The left knee joint was aspirated by Dr. Munro. A clear fluid of straw yellow tint was withdrawn, which yielded some fibrin on standing. The cytological examination gave the following results:—
Total Count.
| 44,800 per c. mm. (nearly all leucocytes). |
Differential Count.
| Polymorphonuclears | 92 |
| Lymphocytes | 7 |
| Large mononuclears | 1 |
| Eosinophiles | 0 |
| Basophiles | 0 |
| 100 |
Attempts at culture on broth and agar proved sterile. In addition three separate blood cultures, taken at intervals of a few days, on agar slopes and broth, all gave negative results.
In another instance of polyarticular distribution the subject was seen during the inter-paroxysmal period. He displayed auricular tophi, the crystalline content of which was verified microscopically.
Blood Count.
| Red corpuscles, per c. mm. | 5,732,000 | = | 194·6 | per cent. |
| Hæmoglobin | 65 | ” | ||
| Colour index | ·57 | ” | ||
| Leucocytes, per c. mm. | 13,200 |
Differential Count.
| Lymphocytes | 34 | = | 4,490 |
| Large mononuclears | 3 | = | 400 |
| Polymorphonuclears | 61·5 | = | 8,120 |
| Eosinophiles | ·1 | = | 130 |
| Mast cells | ·5 | = | 66 |
Chalmers Watson some years previously investigated the blood in cases of acute gouty polyarthritis both during an exacerbation and in the inter-paroxysmal period. His findings were as follows:—
During the attack the films showed very marked leucocytosis. Also there was present a large number of peculiar myelocyte-like cells, these more than half as numerous as the ordinary finely granular oxyphil leucocytes.
“Each of these cells contained a large oval or horse-shaped nucleus, poor in chromatin. The nucleus occupied about half of the total area of the cell. It did not stain uniformly, and it was usually situated to one side, coming right up to the cell outline, and occupying from a third to a half of the total circumference. In many of these cells the nucleus was almost round, with but one slight indentation; in others the indentation was pronounced. The whole cell stained a pale blue, presented a degenerated appearance, and contrasted markedly with the ordinary leucocyte[218] seen in the same film, with its brilliant blue nucleus and bright red eosinophil granules. The special cells under description were also remarkable for their size, measuring about 15 m. in diameter, a few being smaller, about 10 m. Some of them contained vacuoles in the cytoplasm. The general appearance of these cells suggested exhaustion in so far as the cytoplasm did not contain the typical fine oxyphil granules characteristic of the myelocyte. From the character of the nucleus and cytoplasm, they were undoubtedly distinct from lymphocytes. The large lymphocytes were scarce; small lymphocytes were numerous. True eosinophil cells were also scarce. The main bulk of the leucocytes consisted of the ordinary finely granular oxyphil leucocytes and the peculiar myelocyte cells described.
“Blood plates.—Some of the blood-plates were large (4 m. in diameter), and often formed very irregular torn-looking masses. The red cells were apparently normal.”
Shortly after Chalmers Watson, Bain published his results of blood examination in acute gouty polyarthritis. He also noted the presence of a distinct leucocytosis. A differential count disclosed a marked increase of the eosinophil cells, and he adds: “There was present a moderate number of the peculiar myelocyte-like cells originally described by Chalmers Watson.”
Dr. Munro, though he carefully examined the gouty blood films to this end, was unable to identify the myelocyte-like cells noted by these observers.
Recently, through the kindness of my colleague Dr. Waterhouse, Dr. Munro and I had again an opportunity of examining the blood in a case of this kind during the inter-paroxysmal period. The subject, a male, had had repeated attacks at the classic site, with subsequent extension to other joints. Multiple tophi were present in both ears, and the crystals of uric acid were demonstrated microscopically.
Blood Count.
| Red corpuscles | 7,364,000 | = | 147 | per cent. |
| Hæmoglobin | 74 | ” | ||
| Coloured index | 0·5 | ” | ||
| Leucocytes | 21,400 |
Differential Count.
| Lymphocytes | 28·5 | per cent. | = | 6,099 | per c. mm. |
| Large mononuclears | 2·5 | ” | = | 535 | ” |
| Polymorphonuclears | 64 | ” | = | 13,696 | ” |
| Eosinophiles | 3·5 | ” | = | 749 | ” |
| Basophiles | 1·5 | ” | = | 321 | ” |
The blood picture, it will be seen, is one of erythræmia—a marked leucocytosis, a normal differential percentage count, pronounced secondary anæmia.
Da Costa also notes, in a case of gout, erythræmia (7,125,000) with a leucocyte count of 14,000. Ewing, too, records an instance[219] of chronic gout with huge tophi, seen in an acute exacerbation, in which the blood gave a leucocyte count of 21,000 with 70 per cent. hæmoglobin. In another severe instance of subacute type the same observer again met with leucocytosis (15,000).
In regard to these interesting blood findings, it is to be cordially hoped that as the somewhat rare opportunities occur they will be taken full advantage of.
As to the other general clinical features the nervous system, as might be expected, is often greatly perturbed, and the mental distress and anxiety in some instances appear to cause even more irritation than the bodily pain. Febrile movement when present accords with that observed in monarticular sites, save only in the tendency to relapses. Sweating is not a common feature, as in acute rheumatism. Neither does acute endocarditis occur in gout. On the other hand, as this acute polyarticular form may recur throughout years, it may in its later stages be complicated by nephritis.
Furthermore, in its differentiation from acute rheumatism the more advanced age of the sufferer, always over thirty-five and more often nearer fifty or over, will be of help. The presence of an hereditary taint, the nature of the occupation and personal habits, and more pertinently the history of a classical attack in the great toe, may give a clue.
But in this, as in all other varieties of gouty arthritis, the one and only unequivocal objective proof of the nature of the disorder is the presence of tophi. Lamentable indeed is the frequency with which this fact is forgotten, to our confounding and the patient’s detriment. As Hilton Fagge, discussing the diagnosis of gout, long since observed: “All those parts which are apt to be the seat of tophi should be examined. If a single deposit of urate of soda can be found it settles the question.”
In conclusion, before passing to consideration of chronic articular gout, it will be convenient here to discuss certain concomitant phenomena of the acute types. We refer to the muscular and nerve forms of fibrositis, which, we hasten to add, are of common occurrence also in the chronic types of articular gout.
The liability of acute articular gout to be complicated by muscular and nerve disorders has already been briefly alluded to. Also it was pointed out that in respect of this tendency gout displayed an analogy with the specific infections, viz., in that these latter too are prone not only to arthritic, but to muscular and nerve, lesions also.
Our forefathers, greatly exercised by this apparent overlapping[220] of “gout” and “rheumatism,” in their efforts at discrimination drew fanciful contrasts between the subjective sensations produced by gout and rheumatism, but all to no end, for said Heberden, “It must be owned that there are cases in which the criteria of both are so blended together that it is not easy to determine whether the pain be gout or rheumatism.”
Gradually, however, a change in attitude made itself felt. It became no longer customary to regard such examples as blends of gout and “rheumatism,” but to hold the muscular and nerve disorders as also attributable to the underlying gout. Thus, so impressed was Garrod with the frequency of the incidence of lumbago and sciatica in gouty subjects that he was doubtful as to whether they ought to have been classed by him as among the “diseases to which gouty persons are particularly liable.” He thought “they might perhaps have been properly classed among the forms of irregular gout.”
Duckworth, again, felt sure “that much so-called ‘muscular’ rheumatism is really gouty,” and forthwith ranked its manifestations among the irregular forms of gout. Hilton Fagge was likewise convinced that the muscular types of fibrositis are frequently and obviously related to gout; while Sir William Gowers, discussing this same muscular fibrositis, is even more explicit: “It is currently associated with gout, and the truth of the belief is soon impressed upon the practitioner. But it is gout with a difference: it may occur in those who are gouty in the common sense of the word, but some of the most severe cases I have seen, especially the brachial form, have been in those who have inherited a tendency to gout, but have not merited its development.”
Turning to the nerve manifestations, Charcot long since pointed out that gout and sciatica might co-exist, while Gowers is insistent that “underlying most cases of sciatica is either the state of definite gout, or that ‘rheumatic diathesis’ in which the fibrous tissues suffer, especially those that are connected with the muscles, a form closely connected with common gout by co-existence or descent.”
As to my own opinion, I have, in collaboration with Bassett Jones, discussed in detail this relationship of gout to fibrositis in our monograph on the latter disorder, and I shall largely transcribe our remarks therein on this vexed point.
Of all the conditions reputed to be etiologically related to fibrositis, in none of them is the connection more obvious or more easily traceable than between this affection and gout. Whether or no the hyperplasia of the connective tissues be directly due to the gouty toxin must perforce for the present remain uncertain. But there is no doubt as to the relatively frequent incidence of[221] fibrositis in “gouty” subjects. It is as true to-day as when Scudamore wrote it that occasionally “a patient when he has gout in the regular situations suffers, in consequence of some partial exposure to cold, a rheumatism in other parts, as in the muscles of the neck, or in the shoulder joints; and a seizure of lumbago at the time of the invasion of the gout is also not uncommon.”
Apart from the simultaneous incidence of gout and fibrositis in the same subject, it is equally certain that the victims of a “gouty” heritage are unusually prone to develop fibrositis.
Thus, in a series of 1,000 cases hereditary or acquired gout was present in no less than 281—viz., a percentage incidence of 28·1. While this taint was more in evidence in fibrositis of the joints, it obtained appreciably in regard to all muscular types of the affection, more especially lumbago, its influence also being very obvious in the case of sciatica and other types of nerve sheath involvement.
In light of this, we must admit being somewhat nonplussed by those who confidently affirm that “gout” plays little or no part in the production of “fibrositis.” Speaking from an extensive experience, we confidently believe the reverse is the case, and that the gouty element is but too frequently overlooked in examples of this affection.
Approaching another aspect of this vexed question of the relationship of gout, what of the ambiguous attitude of those who, while denying it any share in the causation of lumbago and other types of muscular fibrositis, yet at the same time attribute to gout an important etiological rôle in the allied conditions sciatica and brachialgia?
Thus, they maintain that the fleeting attacks of lumbar fibrositis or lumbago which ensue after dietetic indiscretions have no relation to gout, but are simply indicative of some digestive disability on the part of the individual for certain articles of diet. Hardly to our mind a satisfactory mode of differentiation; much less can it be held to put out of court the influence of gout. For are not the gouty precisely the very persons who display this inability to cope satisfactorily with unusual or excessive meals? Hence the frequency with which in their instance attacks of lumbar fibrositis, often transient, almost invariably ensue when any unwonted excess of purin-containing food has to be disposed of, and especially when at the same time katabolic changes have been stimulated in the body by the ingestion of alcohol, not necessarily excessive in amount.
That the lumbar regions should have been singled out is the more remarkable, for, if there be one form of fibrositis more than another prone to be associated with gout, it is precisely lumbago.
Our difficulty, moreover, in appreciating the cogency of this plea for excluding the influence of gout in muscular fibrositis is the more accentuated in that those who advocate it claim that this very gout is the salient etiological factor in sciatica and brachialgia.
This position is untenable, and for the following reasons: the pathological lesion in both instances is the same—viz., fibrositis; in lumbago and deltoid rheumatism it implicates the sheaths and interstitial tissues of the muscles, in sciatica and brachialgia the similar investments of the nerves.
Strictly speaking, therefore, any differentiation that we can effect between muscular and neuralgic types of fibrositis is perforce merely topographical. To draw etiological distinctions is well-nigh impossible, for the very continuity of the fibrous tissues favours the passage of one type into the other. Hence clinically we find that the bulk of our cases of sciatica are preceded by lumbago, and similarly many cases of brachial neuralgia or neuritis develop by extension out of a pre-existing deltoid fibrositis.
In light of such transitions of muscular into neuralgic types of fibrositis, it seems inconsistent to postulate a gouty origin for the latter and at the same time to deny it any share in the production of the former. For ourselves, we fully recognise gout as the most potent predisposing factor in sciatica and brachialgia, and ergo in the closely associated and often antecedent muscular types of fibrositis.
While insisting on the importance of gout as a predisposing factor in fibrositis, we feel called upon to emphasise the fact that we are not sheltering ourselves under that nebulous term “latent” gout, for our contention is based on the ground that in the vast majority of the cases for which we claim a gouty origin unequivocal proofs of gout, such as tophi, etc., were present.
Out of 343 instances of fibrositis of the joints such stigmata of gout were present in 118 males and nine females. Of muscular types, taking as our example lumbago, we find that out of twenty-seven examples no less than ten displayed definite evidences of a gouty taint. Similarly, out of thirty-eight cases of lumbago complicated by other manifestations of fibrositis eleven males and one female were of gouty habit. Also in twenty-three cases of lumbago associated with arthritic fibrositis six males, but no females, displayed the same[223] proclivity. Lastly, out of thirty-eight cases of lumbago complicated by right or left sciatica ten were of the same diathesis.
Passing in turn to consider this same factor in relation to sciatica, we note that out of 142 examples twenty-four men and three women were gouty. Occasionally, too, apart from glycosuria, it appears to be responsible for bilateral sciatic pains, for in three examples of this nature gout was present.
James Taylor is also very definite on this point, that, glycosuria aside, affections of individual peripheral nerves occur frequently in the gouty. There is little doubt, he says, that sciatica is “frequently present in the gouty and is sometimes directly due to that state.” While admitting that in many, if not most, cases of sciatica there are associated arthritic changes in the hip joint, he yet affirms his belief that “there are some in which the neuritis is a primary condition.”
With this statement my own experience accords, but with a reservation, viz., that the sciatic neuritis is apparently secondary to a lumbar or gluteal fibrositis, with sequential involvement of the sciatic nerve sheath and extension to the nerve trunk.
Taylor holds also that anterior crural and brachial neuritis may be directly due to gout. As to brachial neuritis, he says: “I have known it occur apart from any recognisable arthritic change in a patient who was the subject of gout.”
Having regard to the flippant manner in which the term “neuritis” is but too frequently bandied about, it is refreshing to note that in all Dr. Taylor’s cases “the existence of the neuritis” was shown “by the tenderness of the nerve trunks, the spontaneous, often severe, pain, and atrophic changes both in the skin and the muscles—the glossy skin and atrophied muscles.”
As for the involvement of other nerves, trigeminal neuralgia is held to be the most common; but, for myself, I have never felt justified in claiming any such example as gouty. Nor am I satisfied that persons of gouty habit are more prone than others to attacks of migraine.
Lastly, I cannot confirm out of my own experience Duckworth’s statement that “herpetic attacks in all varieties of ‘gout’ are common.” Nor have I seen shingles co-exist with acute gout, neither have I come across any examples of so-called gouty spinal meningitis!
In conclusion, I would submit that:—
(1) Acute articular gout is not infrequently complicated by fibrositis.
(2) The same infection that determines the articular outbreak[224] is responsible for the concomitant muscular and nerve phenomena.
(3) Persons of gouty heritage are especially liable to fibrositis, notably lumbago and sciatica.
(4) Gout predisposes to fibrositis in that the inherent pathological attributes of gouty tissues favour the incidence of infection.
In regard of this last postulate, it is well known that gouty persons who contract gonorrhœa are more prone than the non-gouty to develop gonorrhœal rheumatism, in other words, to sustain a widespread infection involving the fibrous tissues, not only of the joints, but of the muscles and even of the nerve sheaths. With this concrete example to hand, is it not reasonable to suppose that such a constitutional taint will favour the incidence also of other infections or sub-infections, and that this may explain the relative frequency of fibrositis, not only in the actually gouty, but in those of gouty heritage, this the more cogently having regard to the fact that so much exact evidence is forthcoming in favour of local infection as the cause of all types of fibrositis?
In delineating the features of the acute polyarticular variety, we have to a certain extent trenched on the clinical territory of the chronic form; this is scarcely avoidable, inasmuch as the line drawn between acute and chronic gout is purely arbitrary. Thus one authority remarks of acute gout: “If the disease continue beyond three or four weeks, it is to be considered as persistent or chronic” (Flint). Trousseau, again, discussing the acute variety, more particularly the acute polyarticular type, states that it “may last for some weeks, or even for three months,” adding: “Should it extend beyond that period, it is no longer acute gout; it is chronic gout.”
The truth is that articular gout in this respect is very prone to vagaries. Thus, in rare instances an attack of acute or sub-acute gout, more particularly the latter, may merge without break into the chronic form of the disease.[35] Far more commonly the tragedy is more slowly played out. The unfortunate victim, after passing through several more or less classical attacks, finds that the intervals become shorter and shorter until they merge, as it were, one into the other. Fortunately its course is not one of continuous uniform severity. Remissions, but not complete intermissions, occur, and every now and again intercurrent acute attacks take place.
But, the reader may observe, surely this is very reminiscent of acute gouty polyarthritis, with its serial content of acute paroxysms?[36] Quite so; but there is this difference, that, although such may last six weeks or three months, still there is a period put to the sufferings. A respite of months or years of immunity, and relative health may then supervene.
Not so, unfortunately, when such paroxysmal waves sweep over the subject of long-standing or chronic gout. Not only do the[226] recurrent acute outbreaks occur with increasing frequency, but also with increasing length of duration. It is here no longer a question of the intercurrent acute attack lasting days, but weeks. Also during such exacerbations either four, five, or six joints are simultaneously attacked, or in such rapid sequence that before one joint is free another is involved.
But a word here as to the variations in distribution of the articular lesions in chronic gout. The well-marked penchant of acute gout for the great toe continues throughout the life history of the disorder, the predilection for this site being equally a characteristic of the chronic type. As to the subsequent articular involvement, Garrod held the sequence to be as follows: heels; ankles; knees; the smaller articulations of the hands; lastly, the shoulders and hips. It has never been my lot to see either the shoulders or hips involved; but I have seen osteo-arthritis of the hip in men displaying auricular tophi, and I am inclined to think that, in the presence of the latter, it has sometimes been assumed that the hip mischief was of gouty nature—the “hip gout” of the older authors.
Moreover, the order of sequence is by no means invariable, for oftentimes a local circumstance, i.e., injury or sprain, determines the location. Again, chronic gout is very erratic in respect of the number of joints implicated. In some almost all the joints may be affected, while in others, no matter how ancient the disorder and how oft its recurrence, it remains localised to but a few joints; or it may progress after a leisurely fashion, with each attack invading different joints in succession.
Naturally, if the disorder confine itself to a few joints, and these, and these alone, are the seat of the oft-recurring attacks, permanent changes sooner or later make their appearance. Nor are the morbid effects limited to the joints, but they invade the continuity of the limb, for the oft-repeated inflammatory reactions lead to engorgements of persistent nature. The contour of the affected members is distorted by the œdematous tumefaction, which, more pronounced at the level of the joints, extends in lesser degree beyond their confines. The skin, too, especially over the fingers, undergoes a change in texture, often becomes smooth and glossy, and through its dusky pink subjacent uratic deposits may be discerned.
Old gouty subjects are often of sallow or parchment-like complexion. The blood in these cases of polyarticular gout conforms in attenuated degree, in the matter of leucocytosis and secondary anæmia, to that observed in the more acute types, as witness the following blood pictures.
All were males, the subjects of chronic articular gout of many[227] years’ standing. They all exhibited tophi, which were verified microscopically. The examinations were conducted during the inter-paroxysmal periods.
(1) Blood Count.
| Red corpuscles, per c. mm. | 4,832,000 | = | 96·6 | per cent. |
| Hæmoglobin | = | 64 | ” | |
| Colour index | = | ·66 | ” | |
| Leucocytes, per c. mm. | 11,000 |
Differential Count.
| Lymphocytes | 42 | = | 4,620 |
| Large mononuclears | 4 | = | 440 |
| Polymorphonuclears | 52·5 | = | 5,775 |
| Eosinophils | 0 | = | 0 |
| Mast cells | 1·5 | = | 165 |
(2) Blood Count.
| Red corpuscles, per c. mm. | 5,040,000 | = | 100·8 | per cent. |
| Hæmoglobin | = | 72 | ” | |
| Colour index | = | 0·72 | ” | |
| Leucocytes, per c. mm. | 13,400 |
Differential Count.
| Lymphocytes | 15 | = | 2,010 |
| Large mononuclears | 2·5 | = | 335 |
| Polymorphonuclears | 78 | = | 10,452 |
| Eosinophils | 1 | = | 134 |
| Mast cells | 3·5 | = | 469 |
(3) Blood Count.
| Red corpuscles, per c. mm. | 4,280,000 | = | 85·6 | per cent. |
| Hæmoglobin | = | 66 | ” | |
| Colour index | = | 0·77 | ” | |
| Leucocytes, per c. mm. | 12,000 |
Differential Count.
| Lymphocytes | 23 | = | 2,760 |
| Large mononuclears | 3 | = | 360 |
| Polymorphonuclears | 74 | = | 8,880 |
| Eosinophils | 0 | = | 0 |
| Mast cells | 0 | = | 0 |
In these chronic forms, save during exacerbations, there may be little or no febrile movement, and local pain, heat, and redness may be slight or wholly lacking. But the articular swellings never wholly disappear, and the mobility of the joints is never entirely regained. The articulations, few or many, become stiff, ankylosed, and deformed, by the growth of tophaceous deposits. But to detailed description of these latter we shall return later.
In inveterate cases of this nature the victim grows more and more crippled and infirm, the inroads of the disease upon the constitution more and more palpable. Pelion is heaped upon[228] Ossa, as one ailment sets in after another, now of the digestive organs, now of the heart, or of the kidneys. These subjects of chronic gout are more often than not dyspeptic, show signs of arterio-sclerosis. Their blood pressure is raised, their vessels tortuous and thickened, and the left ventricle enlarged.
As to the variations in uric acid excretion, these, as before remarked, show no appreciable deviation from normal. Occasionally, however, there is a tendency to uric acid gravel. Of more sinister significance, albeit, is the fact that in many of these cases the urine is copious, of low density, paler than normal, and shows a trace of albumen with hyaline casts.
As the disease marches to its fell end the appetite becomes impaired, gastric catarrh and diarrhœa may sap the waning strength, or palpitations, fits of dyspnœa, or angina-like attacks, sometimes fleeting, but often of organic source, may portend a fatal issue. Ripe for the sickle, a kindly “stroke” perchance puts an end to his protracted misery. Or symptoms, long since manifest, of progressive renal failure may usher in the closing scene, and happy the victim if he pass muttering, half conscious, into that dream-like stupor drifting by insensible graduations to death.
So much in attempted portraiture of the long-drawn-out tragedy of inveterate chronic gout. But, fortunately, it is not always thus, and nowadays, at any rate, the evils wrought on the constitution by the malady are seldom so malignant. For not only, as before stated, has gout become less frequent, but its virulence also much attenuated. States of so-called “gouty cachexia” were, however, more familiar to our forefathers. It more commonly ensues in subjects of strongly hereditary tendency, and particularly in those in whom the initial attacks ensue before thirty years of age. I recall the instance of a colonel who sustained his first attack of gout when a subaltern of but eighteen, brought on, as he thought, through exposure while shooting snipe in Peshawur. It is in such cases that this so-called “gouty cachexia” may overtake a man while yet in his prime, and vest him untimely “with all the characters of age.”
As to the milder types of regular chronic gout, such usually arise, not in youth, but in men past the meridian of life. In their instance the recurrence of gouty paroxysms is often erratic. Periodicity becomes less pronounced or wholly lost. The life[229] history of the disease may be summed up in a few sporadic outbreaks, occurring irregularly throughout a long life. Even when at first the attacks occurred regularly in the spring and fall the rhythm of incidence becomes broken. An attack comes before its time, is belated, fails of appearance wholly, or an intermediate paroxysm comes as a surprise. Moreover, in many such the gouty manifestations with the passing years tend to become more and more attenuated, maybe even to extinction. Thus, a man who in the middle decades was a martyr to gout in old age gains freedom from its visitations, the disease having apparently exhausted its vicious potentialities.
Reviewing articular gout as a whole, one cannot but realise that it does in respect of the recurrence of gouty paroxysms exhibit inexplicable vagaries, inexplicable in that, as Sir William Roberts long since said, “in many instances they are dependent neither upon medical treatment nor upon altered dietetic habits, but are due to spontaneous changes in the constitution. They form part of the natural history of gout; and it is important to bear their existence in mind when we seek to estimate the value of therapeutic means in order to prevent ourselves from becoming the dupes of misinterpreted sequences.”
Albeit, we would not end on too sombre a note. For, in respect of the graver consequences of gout, it is unquestionable that right living, aided by efficient therapy, may arrest the course or mitigate the severity of the disorder. Moreover, as long as the attacks do not follow quick upon each other, but are separated by long intervals, there is little fear of a cachectic condition supervening. Life may not be appreciably shortened, and such textural degenerations as may ensue, though frequently attributed to gout, may often with at least equal plausibility be assigned to advancing years, but this with reservation, for, as Duckworth says, “the wilful libertine is likely soon to become cachectic, while the prudent man may altogether avoid this state or avert its evils for many years or decades of years.”
The palpable changes in the affected joints differ widely in different cases, and why is not apparent. Thus, the first attack, if of prolonged duration, may bequeath a legacy of crippledom comparable to that met with after repeated paroxysms. On the other hand, some, although they have suffered from the disorder off and on throughout their lives, yet escape those consecutive deformities which in others deform and cripple the hands and feet, though the disease may be of relatively brief duration.
But in the less fortunate cases the continued ravages of gout lead to a pitiful disablement of the affected limbs, reaching its acme in the hands and individual fingers, flail-like and semi-paralytic as they so frequently become.
Not only are the digits variously distorted, their joints more or less ankylosed, but the overlying skin, distended by the ever increasing subjacent uratic deposits, becomes thinned and purplish red in hue, and occasionally ulcerates. Similarly at ankle, knee, wrist and elbow thickening and deformity ensue as the concretions accumulate in and around the affected joints, these further accentuated by the correlated inflammatory and degenerative processes. Coincident deposits in the tendon sheaths and related bursæ contribute their quota, and at knee and elbow the bursal masses may reach extraordinary dimensions. Not only do the joints become deformed, but distorted also, through reflex muscular spasm and instinctive adoption of unnatural attitudes for the avoidance of pain.
So much for the broad outline of the picture presented, but a still closer scrutiny is called for. The deformities produced are the outcome of uratic deposits, which, as Charcot long since pointed out, take on the shape of “irregularly rounded or ovoid swellings, bunched, and either large at the base or just the opposite, i.e., provided with a pedicle.”
As shown in the coloured plate, the favourite site for their development is the dorsum of the hand or the vicinity of the metacarpo-phalangeal or mid-phalangeal joint. The resultant disfigurement of the hand is very characteristic. Irregular tuberous swellings surmount the knuckles, and spreading laterally, obliterate the fossæ between them and their fellows. The same extend forward over the first phalanges, from nigh the distal end of which again arise similar bossy excrescences over the mid-phalangeal joints. Encroaching thus upon the length of the first phalanx from either end, but little of its shaft is ultimately left exposed. In like fashion the mid-phalanx may be buried in uratic deposits, its contour wholly lost; and, the terminal phalanx participating, the digits become almost pedunculated, the nails projecting from the ends thereof—the “parsnip hand” of Sydenham. Such is the appearance presented in inveterate chronic gout.
Fortunately such examples are relatively rare, and a study of the condition in its earlier stages reveals some interesting features. The uratic deposits, it is important to note, are not located exactly at the level of the articulation. Unattached as they are to the articular ends, they are not compelled to, nor do they in any way, adapt themselves, as it were, to the contour or shape thereof. In short, the tophaceous formations are erratic, are not like[231] osteo-arthritic nodules, erupted from and continuous with the articular bone ends. Again, relatively independent of the contiguous tissues, they, unlike osseous outgrowths, are slightly movable in lateral directions.
When of recent incidence, their consistence is soft, and, be they never so ancient, they do not attain the density and hardness of bony outgrowths. The overlying skin, to which they are sometimes adherent, takes on a peculiar glossy and satin-like texture, its dusky pink blotched with spots of dead white colour, i.e., subjacent uratic deposits.
In other particulars also they differ from bony outgrowths. The tophaceous masses may soften and disappear after exacerbations of arthritis, and others may form at different sites. Following such absorption or difference in their location, some increase in joint mobility may happily ensue. This same fortunate occurrence may follow discharge of the uratic masses through ulceration and perforation of the skin.
In our chapter on Uratosis we dealt with the chemical nature and mode of formation of tophi. Also we affirmed our belief that tophi, whether articular or ab-articular in site, were always preceded by local inflammatory reaction, and to the clinical tokens of their impending eruption we need not recur. Albeit this point, i.e., antecedent inflammation, is of such prime importance that we have not hesitated to append to our text a lengthy footnote,[37] this because, as Garrod, who quotes the same in extenso,[232] rightly claims, the genesis and evolution of tophi has never been so graphically depicted as in Moore’s description.
It will be seen that this observer holds that tophus formation “is usually preceded and accompanied by inflammation.” Garrod, as we know, believed uric acid to be the cause, and not the consequence, of gouty inflammation. But he emphasises the fact that the phenomena attendant on the eruption of auricular tophi are “exactly the same as when a joint is affected, and constitute, in fact, a true gouty paroxysm, commencing with infiltration of the tissue and subsequent inflammation.” Still, though venturing to differ as to the sequence of events, we gladly invoke this authority’s observations in proof of the fact that the inflammation even in the ear is not always of negligible grade: “I have seen many cases in which the ear symptoms have proved very annoying, so that patients have been unable to rest their ears on the pillow.”[233] Subacute gout sometimes occurs in the ears, says Duckworth, who furthermore believed that the indurations in the cartilage observed by him in gouty subjects were the outcome of such attacks. Laycock, too, long before noted that the ears of gouty subjects often appeared to be “soldered.”
Pain or discomfort in auricular tophi often presages an oncoming articular paroxysm. “Those gouty persons,” said Scudamore, “who are affected with concretions (chalk-stones), experience for a short time before the fit pricking pains in the parts where they are situated. This is described even by those who have minute points of concretions in the lobes of the ears and in no other parts of the body.” Hence tophi have a prognostic as well as diagnostic valency in that the incidence of pain at their site may foretell the oncoming of articular outbreaks.
While, as before emphasised, the eruption of tophi may antedate the occurrence of articular gout, on the other hand tophi may be present at the joints, but lacking in the ears and all other ab-articular sites. Auricular tophi, extracted occasionally by patients, are sometimes shed spontaneously. According to Duckworth’s statistics, in one-third of all well-marked cases of gout the ears present tophi in the helix, the anti-helix and its fossa and the lobule, and in some cases they may be situated on the posterior surface of the pinna.
Apart from the external ears, tophi are apt to form in various localities. Most frequently they are situated in the vicinity of the joints and bursæ, especially that over the olecranon. As attack follows attack at short intervals the tophaceous matter is heaped up around the joint, and in this way many articulations may be involved, even all of them, says Trousseau, “as happened to Gordius, who composed on himself the following jocular epitaph:—
Uratic deposits sometimes attain a prodigious size. I have seen them the equivalent of a small hen’s egg. The largest tophi are invariably found in the neighbourhood of some joint, and the upper extremities furnish the most marked examples. But even when of considerable magnitude they may be non-adherent, the skin gliding freely over their surface. As John Hunter wrote: “The chalk shall remain for years without producing inflammation, and seldom produces it at all but from quantity.”
Often, however, their presence at length induces irritation of the[234] overlying integument. As they approach the surface the skin assumes a purple hue, becomes thin, and ulcerates. The uratic ulcers thus formed have generally an indolent fungous base. As the deposits extrude or are removed they are continually redeposited, and in this manner ounces of urates may be discharged. The same is followed by great relief and diminution of deformity.
Discussing such lesions, John Hunter tells us that “when the interior surfaces are exposed they hardly take on common inflammation and suppuration, healing more readily than a sore of the same magnitude from any other cause; even a joint shall be exposed, yet common inflammation shall not come on, nor shall it suppurate: only a watery fluid shall come out, bringing the chalk with it occasionally, and it shall heal up kindly.”
A glance, too, at the preceding footnote shows that Moore also agreed with Hunter as to the absence of common inflammation and suppuration. Moreover, even of recent years it has been suggested that, because gouty tophi do not suppurate even when ulcerated through the skin, the urates have antiseptic properties. But Bendix (Zeit. klin. Med., 1902) failed to demonstrate such qualities experimentally. The truth would appear to be that, though gouty inflammation never ends in suppuration, yet abscess formation very commonly occurs in the peri-tophal tissues. Such more often ensues in subjects of frail health or of definitely cachectic type. Garrod saw as many as five or six open at one time in each hand, and others on the feet. In his experience they give rise to but little constitutional disturbance. Scudamore, speaking of the same, says the sores produced are “unusually tender, aching, and sometimes very painful as the fit is making its approach.”
Ultimately the gouty ulcers thus formed dry up, and this indifferently whether or not the uratic deposits are wholly extruded in the discharging pus. The wound then closes, leaving a small scar, which, however, given a fresh attack of gout, is but too likely to break down, and this process may occur repeatedly. Bursal sacs containing tophi not infrequently suppurate, constituting abscesses containing urates.
An interesting fact noted by Garrod was that so long as such abscesses were discharging freely the subjects enjoyed comparative immunity from overt gout. But, given healing of the same, in several instances he had seen it the signal for a sharp outbreak. Duckworth, too, states that “whenever ulceration and flow of tophaceous matter occurs it is rare to meet with paroxysmal attacks anywhere in the body. With the cessation of the discharge renewed fits may intervene.”
While they tend to aggregate themselves round the joints, yet[235] tophi sometimes invade the integument of the limbs. They have been seen in the skin over the ulna and tibia, and commonly over the olecranon and patella. Pye Smith recalls the instance of a man in whom a number of small ulcers, discharging urate of soda, formed in the middle of his thighs and legs. The case is not an isolated one, but the incidence of subcutaneous uratic deposits in the limbs, save over articulations, is exceptional.
In the palms of the hands and the pulps of the fingers, the knuckles and phalanges, tophi are found not infrequently; and Trousseau tells of a lady of sixty in whom the cutaneous palmar folds of both hands were “marked with radiating white lines such as are seen in those who have long been employed in tempering plaster.”[38] Similar deposits have been noted in the plantar surface of the feet.
Reverting to the trunk, uratic deposits have been found in the scapular region, also in the perineum. I have twice seen tophi in the corpora cavernosa of the penis. In the face, apart from the ears, they have been found in the alæ of the nose. In the eyelids Duckworth noted uratic deposits in streaks resembling xanthoma; they were chemically tested, and proved to be of this nature. Speaking of “gout in the eye,” Garrod states: “I have witnessed many cases in which conjunctivitis and sclerotitis appear to be distinctly connected with the gouty diathesis, and in two cases there existed deposits of urates on the surface.”
As before stated, we recognise only one type of gout, viz., the tophaceous variety. But even so it must be noted that in some instances the process of tophus formation is greatly accentuated. In other words, the tophi may not only be of prominent size, but of unusually widespread distribution. Indeed, poetic exaggeration has it that one Baylas and one Acragas were entombed while alive in their own uratic deposits. But, apart from such imaginative flights, there are unquestionably some cases in which tophi are most widely diffused. Thus Plater tells of a patient whose whole body, even the eyelids, was studded with them: “ex toto corpore, per poros, adeo ut etiam palpebræ oculorum non exemptæ fuerint, ejusmodi materia gypsœa, circa poros cutis mox in tophos mutata, prodisset.”
These cases of multiple tophi are far more common in men. Duckworth met with some well-marked cases in women. They may occur also in persons who have been lifelong abstainers. Sometimes trauma seems to have played a part in determining their localisation. Garrod held that, given prodigious uratic[236] deposition, the kidneys might be held as unsound and undergoing sclerosis; and, according to Duckworth, the rule commonly holds good.
Whatever be the explanation, no fact in practical medicine is better established than this, viz., that certain disorders are peculiarly liable to arise in gouty subjects. Of these the more noteworthy are glycosuria, phlebitis, certain cutaneous disorders, and nephritis. While, for myself, I prefer to regard these affections as merely diseases to which the gouty are especially subject, nevertheless each and all of them, by one authority or other, have been classed as among the irregular manifestations of gout.
This, on the assumption that these several morbid entities may precede, alternate with, or follow arthritic seizures, frequently also on the basis of their alternation in hereditary transmission with arthritic gout. Thus, in a family of marked gouty proclivity, while one son, despite a temperate life, may have severe articular gout, on the other hand his brother may suffer only with irregular manifestations, i.e., phlebitis, eczema, etc.
As to whether these particular disorders, phlebitis, glycosuria, etc., are directly caused by the toxin of gout, or whether their not infrequent association with gout is merely accidental, is a moot point. But to the sources of fallacy in this connection we shall allude more in detail when dealing later with irregular gout. Meanwhile extended knowledge of the intimate etiology of phlebitis, glycosuria, etc., tends to an attitude more critical than that of our forefathers, who, faute de mieux, relegated a large number of conditions whose pathology was inexplicable to the nebulous domains of irregular gout.
That some obscure link existed between glycosuria and gout was long since suspected. Prout noted it as far back as 1843, and Bence Jones discussed the subject under the title “Intermitting Diabetes” (1853), while in the following year Gairdner announced that he had long surmised the kinship between the two disorders. About the same time Claud Bernard remarked that gout and glycosuria might alternate, and so did Trousseau, and many since that day have ranked glycosuria as one of the forms of irregular gout, whether legitimately or not is an open question, but at any rate it does not affect the established clinical fact that glycosuria occurs with significant frequency in gouty individuals.
Gouty glycosuria is more common in males than females. The subjects are usually robust, middle-aged, and of full habit. Sugar is found intermittently in their urine in small amounts, but no acetone bodies. It is as a rule unaccompanied by thirst or wasting. It quickly responds to dietetic restrictions. As Gull long since observed, gouty glycosuria does not “discover itself,” but is “not uncommonly discovered.” This tersely sums up the clinical difference between this affection and true diabetes, albeit, as in all glycosurias, there is always the risk that carbohydrate excess, mental strain, or other adverse circumstances may aggravate the disorder and the case merge into one of true diabetes.
Following the installation of glycosuria, the tendency to paroxysmal articular outbreaks often ceases. The converse also has been observed, viz., that when, in sequence to dietetic restrictions, the sugar disappears, the articular pains may reappear. The fact that attacks of glycosuria may alternate with attacks of gout led to the assumption that a positive antagonism existed between the two disorders. Hence the phrase “the more sugar the less gout,” and vice versâ. This, however, with reservations, for a fugitive glycosuria has been seen during an acute articular paroxysm, and a classical outbreak in the toe has been known to supervene in the course of a well-established glycosuria.
It is generally held that glycosuria is most commonly associated with irregular forms of gout. But, in view of our ignorance of the intimate nature of even regular gout, I should myself deprecate affixing the prefix “gouty” to any glycosuria other than one that has supervened in sequence to, or alternates with, gouty arthritic seizures. Moreover, the glycosuria of gout is usually the alimentary glycosuria of fat elderly people, in whom the sugar excreted represents the unconsumed surplus of carbohydrate food. But fat elderly people are not necessarily “gouty,” neither is every so-called benign glycosuria inevitably linked on to a gouty diathesis. In fact, the relegation of glycosuria to the gouty category is but too often not a matter of diagnostic certainty, but rather an inference. Hence my plea that the prefix “gouty” would best be restricted to glycosurias occurring in individuals who suffer regular attacks of gout, or those displaying those objective tokens pathognomonic of the disorder, i.e., tophi.
Again, James Taylor has recently reminded us that, if nerve affections are relatively common in true diabetes, the same may be met with in gouty glycosuria, even when of temporary duration. Thus symptoms indicative of peripheral neuritis may occur, i.e., lost knee jerks, paræsthesiæ, and paresis of the lower limbs. Now, as this authority pertinently observes, the subjects of gouty glycosuria are frequently given to alcohol. Consequently the question[238] whether or not the symptoms are due, not to sugar, but to alcohol, arises forthwith.
In some undoubtedly the alcoholic factor plays a rôle, but such symptoms may, on the contrary, arise in very abstemious individuals. This notwithstanding, James Taylor holds that the clinical complex differs substantially from that met with in true alcoholic neuritis. It is slighter in degree, the paresis usually restricted to lower limbs, while the exquisite tenderness to pressure on nerve trunks so typical of alcoholic neuritis is little or not at all in evidence. Nor is there the same tendency to contractures in muscles as met with in the alcoholic variety, and withal there is an absence usually of the mental changes—loss of memory—associated therewith. Accordingly Taylor holds that we must recognise the existence in the gouty of a true glycosuric peripheral neuritis quite independent of alcoholic peripheral neuritis.
Other concomitant nerve troubles noted in this association are severe intercostal neuralgia and, even more commonly, neuralgia of the fifth nerve, and to this may be added migraine and that other neurosis asthma. Intense mental irritability and depression is not an infrequent sequel in gouty glycosuria. According to James Taylor, melancholia even may result, especially if the glycosuria have merged into true diabetes—a sequel, he says, especially prone to occur in Jewish subjects.
Having seen and suffered many painful disillusionments through too flippant relegation of neuralgias or neuritides to diatheses “gouty” or “rheumatic,” I would emphasise the necessity for great caution. In other words, before labelling a neuralgia or neuritis as “gouty,” all possible causes, infective or other, should be excluded, this always, but pre-eminently so in brachialgia, sciatica, and trigeminal neuralgias. Nor even, should there be a history of classic outbreaks or blatant tophi present, should we be less vigilant.
By all means recognise the gouty diathesis. It often avails much in treatment, but not if, e.g., dental caries, antral disease, cervical rib, or pelvic growth be overlooked, not to speak of recent or concurrent sources of infection or toxic absorption.
Lastly, we should always recollect that gouty glycosuria, as Gull said, “does not discover itself”; it is not writ large on the subject like true diabetes. But given the incidence of nerve troubles in a gouty person, i.e., a paræsthesia, itching, neuralgia, etc., we should always suspect its presence.[39] Incidentally our search may reveal not only sugar, but also albumen, and the latter may explain much that appeared inexplicable.
It is to Sir James Paget that we are indebted for recognition of the fact that phlebitis occurs with significant frequency in gouty subjects. This great surgeon held that the disorder was the outcome of a modification or transformation of gout, the result of “morbid conditions changing and combining in transmission from parents to offspring.” At the present time some regard it merely as a complication of gout, others as one of the irregular manifestations of the disease.
It occurs most commonly in men, women being rarely the subjects of gouty phlebitis. It may install itself insidiously with but mild local discomfort, and yet on examination a cord-like hardness is detected. In others it announces itself with pain, in rare instances intense, this more commonly if the deep veins of the calf are its seat.
Its predilection is for the veins of the lower extremity, the superficial rather than the deep vessels. If the former, a faint blush over the affected veins may be seen, but if the deep veins, then œdema and tenderness may be the sole token of its presence.
Frequently the phlebitis is patchy in distribution and migratory. Thus, as Paget says, it may on one day be located in a short length of the saphenous vein, flitting the next day to some other portion thereof, or, it may be, to the corresponding vein of the opposite limb. This tendency on its part to metastasis and symmetry led Paget to the conclusion that “the essential and primary disease is not a coagulation of the blood, but an inflammation of portions of the venous walls.”
Its duration is not uncommonly prolonged, and it displays a marked tendency to recurrences, the latter determined by blows, unusual exertion, or, according to some, exposure to cold. Most cases end favourably, but death from embolism sometimes occurs. Occasionally, given occlusion of the large veins, some degree of swelling lingers permanently.
The instances most indicative of a gouty origin are those in which the veins of a limb, the seat of acute gout, are simultaneously attacked by phlebitis. In three cases of this nature recorded by Garrod, the subjects, despite their suffering from acute articular gout, persisted in leaving their beds to record their votes in the parliamentary election of 1884. This type of case, according to Garrod, is usually confined to men, and, with the exception of the cases above noted, a varicose condition of the veins of the legs of long standing existed in his series of examples.
Garrod recognises in addition a second type, in which phlebitis,[240] “usually of a much less acute character, ensues without the previous development of gouty inflammation in the neighbourhood of the part.” Here we may recall that, according to Paget, the incidence of phlebitis in an elderly person without any external cause warrants the suspicion of gout. Perhaps the chief justification for such an assumption rests on the fact that phlebitis appears sometimes to be hereditary. Paget cites the instance of a man who suffered from phlebitis of both saphenous veins during an attack of acute gout. On the maternal side his mother, two uncles, a grandmother, and two cousins had been the subjects of phlebitis.
In conclusion, for myself, I would suggest that the term “gouty” phlebitis be restricted to those instances in which a limb, the seat of acute articular gout, is complicated by phlebitis of the veins of the affected part. Here we are dealing with what is palpably an extension of the gouty inflammation from the affected joint to the veins, and which, I venture to assert, is strongly confirmatory of the view that an infective element intrudes in “gouty” arthritis. We may recall that, e.g., gonorrhœal phlebitis of the lesser saphenous veins is not so uncommon, while the frequency with which phlebitis complicates infections calls for no emphasis.
Leaving aside these rare instances of acute gout complicated by acute phlebitis, I think there is a too flippant tendency to regard any phlebitis occurring in middle-aged or elderly subjects as being of this nature, this often in the absence of any evidence, hereditary or other, of a gouty element in the case. Frequently, too, the subjects are women with varicose veins of long standing, and ipso facto potentially liable to phlebitis. But why, in the absence of ancestral or acquired gout, dub such cases forthwith as “gouty”? We may, it is true, as in Paget’s classical instance, elicit a familial tendency to phlebitis, but even so I doubt the legitimacy of the inference that the phlebitis is necessarily “gouty.” Is it not equally true that the tendency to varicose veins is hereditary, and ergo predicates an enhanced liability to phlebitis?
The incidence of tophi in the skin naturally engendered the conception that gout was responsible for many and diverse types of cutaneous affections. In accordance with this, every effort was made to prove that they were the outcome of uratic infiltrations, but in vain.
Objective proof of this nature being lacking, the older clinicians found their justification in the alternation of arthritic attacks with cutaneous disorders, and their alternation in inheritance was laid great stress upon, this especially by French dermatologists,[241] notably Bazin, but at the present day Jacquet’s non-committal pronouncement is probably representative of the attitude of the French school as a whole towards “arthritic” affections of the skin: “Le lien admis entre le groupe de maladies dites arthritiques est très mal connu dans son essence, mais il serait tout aussi contraire à l’esprit scientifique de le nier avec rigueur que de l’affirmer avec presomption.”
As to the skin disorders associated with acute types of gout, perhaps the most interesting and well ascertained is herpes. It may precede an acute attack, may alternate with it, or be a sequel thereof. Rendu noted that acne, boils, and carbuncles also might occur prior to, in alternation with, or in sequence to acute attacks, and Scudamore noted the same in respect of erysipelas.
The noteworthy liability of the gouty to these disorders is but another proof that gout predisposes its victims to infections. The fact that acute gouty arthritis might follow acne, boils, etc., lends colour to our contention that the same may be of infective origin. But unfortunately the suspicion also intrudes that some of the arthritides occurring in such association may, on insufficient grounds, have been diagnosed as “gouty,” this especially if the joint disorder were located anywhere save at its classic site, the big toe.
Passing to skin affections associated with chronic gout, it must be admitted that as a whole the contention that they are “gouty” in origin is, to say the least of it, doubtful. French dermatologists claimed that the cutaneous eruptions of the “gouty” might be recognised by their polymorphism, circumscribed location, etc., but these are no more distinctive peculiarities than the concomitant pricking, hyperæsthesia, and hyperalgesia upon which Bazin laid such emphasis in their diagnosis.
In short, sequences, coincidences, and alternations are the basis of much that has been written upon so-called “gouty” cutaneous affections, criteria all of them fruitful sources of fallacy.
As to psoriasis, I have met with it so frequently in association with non-gouty arthritides that I have never felt justified in claiming any example as “gouty.” So-called “gouty” pruritis and prurigo, these when they occur in the “gouty” are frequently referable to an associated glycosuria, and when this is not the case, it is frequently a senile prurigo. The claim that urticaria is “gouty” may be dismissed without comment.
As to frequency of incidence in the “gouty,” eczema undoubtedly must be awarded the palm. But whether the scaliness of skin on extensor surfaces of arms and legs and back of neck, which ultimately, under the influence of skin infection through scratching, develops into a dermatitis which assumes the character of eczema,[242] can be, strictly speaking, held as of “gouty” origin, is questionable. Certainly, whatever be the origin of the pruriginous scaliness of the skin, there can be no doubt that the later dermatitis is the outcome of infection by skin organisms. Frequently the presumption that the eczema is “gouty” rests upon general rather than specific grounds, on “goutiness” rather than “gout.” Accordingly I think it would be wiser to regard eczema as an occasional complication of gout rather than an integral element thereof.
Lastly, there can be no doubt that many of the so-called “gouty” cutaneous disorders ensue at what may be called the arterio-sclerotic stage of life. It is when renal and cardio-vascular changes are present that we meet with exudative erythema, pityriasis, exfoliative dermatitis, and purpuric eruptions. All these have at one time or another been foisted upon gout, whereas they are far more closely related to the cardio-vascular and renal changes with which the disorder is so frequently associated.
The association between gout and renal disease is admittedly intimate, in so far as gouty subjects often have granular kidneys, while gout is a frequent complication of this type of renal disorder. Nevertheless, the clinical relation between the two diseases is ill defined and, moreover, somewhat erratic. In most instances the renal defect is engrafted upon the antecedent gout, or the sequence is reversed; and, again, the two conditions may arise contemporaneously. Lastly, in sharp and disconcerting contrast to this mutual overlapping of the two disorders, we have the awkward fact that more commonly gout and granular kidney run to their fell end quite independently of each other.
Thus, Sir William Roberts observed: “It is quite common to see articular gout, even of chronic and inveterate character, run its entire course without any accompanying signs of structural disease of the kidneys.” The same, to be sure, is equally true of granular kidney, which may pass to its close without any suspicion of gout.
Now, as we have seen, the primary renal origin of gout fails of demonstration. Is gout, then, causally related to granular kidney, or is there some less direct relation between them?
As to this, to begin with, it is extremely rare that a “gouty” subject develops acute nephritis. In the exceptional instances when it does occur it is either purely accidental or else the outcome of an exacerbation of a previously existing interstitial nephritis.
The question then arises, Can gout when long continued originate per se the condition we are pleased to term “gouty kidneys”? As seen above, such renal lesions are by no means an inevitable sequel or concomitant of long-standing gout. Moreover, there is nothing specific of gout in the so-called “gouty” kidney. It is an interstitial nephritis, which may assume the appearances of the ordinary “contracted kidney” or the “arterio-sclerotic” type. There may be uratic deposits at the apex of the pyramids, or even an uric acid calculus; but even so that of itself constitutes no proof of the renal changes being “gouty” in origin. In short, the prefix “gouty” as applied to these types of renal lesion is just as unscientific and unwarrantable as used in regard of “phlebitis,” “eczema,” and so forth.
Nor, quâ gout as a causal factor, are we in better case if the renal disorder be of the “arterio-sclerotic” type. No direct relationship is established between gout and arterio-sclerosis beyond the fact that both are usually met with in middle-aged or elderly people. Moreover, a man may develop arterio-sclerosis and arterio-sclerotic kidneys, yet never have any vestige of gout.
There being nothing specific of gout in the lesions of so-called “gouty” kidneys, we must revert to the clinical findings to refute or establish any causal connection between gout and the renal disorder. Now, gout is a disease of middle and late life, and rarely of itself proves mortal. On the other hand, it appears increasingly probable that the seeds of granular kidney are laid in earlier life, and, on the average, its course is shorter than that of gout. Also the two disorders have clinical facies absolutely distinct the one from the other.
From the above considerations it is, I think, clear that, whatever the hidden nexus between gout and “granular kidney,” it is neither essential nor constant. It is rather, I believe, of the nature of a coincidence. Furthermore, as applies to so many problems pertaining to gout, and, for that matter, to “granular kidney” also, we labour under the grave disability that both terms are, especially “gout,” very vaguely applied and when used are often a matter of personal opinion. Consequently, as Samuel West shrewdly observes, “it is difficult to discuss satisfactorily the relation of two conditions to each other when neither condition admits of precise definition, for some authorities are more easily satisfied in the diagnosis of gout than others; and, while some place all forms of chronic interstitial nephritis in one and the same category, others are not so comprehensive, and regard granular kidney as a definite clinical disease, of which the interstitial nephritis is only a part.” Under these circumstances, the[244] need for further and more exact researches in this sphere is but too obvious.
Meanwhile, accepting the general opinion as to the frequency of the co-existence of gout and granular kidney, is there any explanation thereof? For myself, I am inclined to believe that the common overlapping of the two disorders is in large measure due to this, that the factors, i.e., excess in alcohol, overeating, etc., that make for the eruption of gout, are largely identical with those that promote the development of granular kidney. Hastings Gilford holds “there is very little doubt that syphilis, lead, and gout do not so much originate Bright’s disease as excite it into activity when it already exists in a smouldering or latent condition.”
With this view I feel much in accord, and if to the malign effects of gout be superadded the effects of alcohol or, haply, lead also, how incalculably greater the chances of fanning into flame any latent tendency to nephritis—a legacy, perhaps, of some long bygone infection.
Gout per se rarely, if ever, proves fatal. Certainly, as Sir Thomas Watson long since said, “gout in the extremities is not a mortal disease.” When death did occur during or in close relation to an acute paroxysm, it was by our forefathers attributed either to its retrocession or to some misplaced or irregular manifestation. Indeed, their attitude was very much that of the French physician who observed: “La goutte articulaire est celle dont on est malade, et la goutte interne est celle dont on meurt.”
But, as we shall see later in our chapter on Irregular Gout, most, if not all, of their instances of the assumed translation of the materies morbi of gout to some vital organ are without foundation. The demise, often dramatically sudden, was not due to gout, but to some insidious, unguessed-at organic degeneration, or to one of the accidental intercurrent maladies to which these subjects seem especially liable. To sum up, the immediate danger to life from regular gout when uncomplicated is slight.
Not that gout is salutary, lessens the liability to other diseases, or promotes longevity. Very much the reverse—“a tendency to recurrence is a law of the disease.” Broadly speaking, the more pronounced the tendency to recurrence of articular outbreaks, the more protracted the isolated paroxysms, the worse the outlook, the more sombre, too, the greater the number of joints involved. Conversely, if the disease, though it recur, restrict itself to the classic site, the big toe, the longer, as a rule, the intervals of[245] freedom, the brighter the prospects of long life. Lastly, the more the subject is crippled, the more pronounced the tendency to tophaceous deposits, the more likely is the disease to pursue a downward course, the greater the risk of associated degenerations in renal and vascular tissues.
While these reflections are in the main, we think, justifiable, we must recollect that in gout, as in other maladies, the elements of prognosis reside in the individual, not the disease. Does he come of a long-lived stock?—not uncommonly a feature of gouty families. If so, the outlook is favourable. If he come of a short-lived breed, then in all probability, no matter how carefully he lives, he will not likely make “old bones,” this, certainly, if the gout makes its appearance early in life, say under thirty.
As to the axiom, generally accepted, that the earlier in life gout makes its début, the more unfavourable the outlook, there are exceptions. Where longevity marks the stock, they usually are true to type. Thus, even if the first outbreak occurs in the twenties, I have known them reach the allotted span and over. Nor if their urine show traces of albumen is this necessarily of grave import, for these gouty veterans may for many years, even to old age, exhibit traces of albumen without apparently developing genuine Bright’s disease.
“There dies not above one of a thousand of the gout, although I believe that more die gouty,” wrote Graunt long years since; and this contains a kernel of truth, for the prognosis of gout rests in the main not on the gout, but the conditions correlated therewith—the absence or not of complications. For, be it always remembered, gout, though it may appear in youth, is chiefly an appanage of the middle and later decades, in short of the regressive period of life.
This last is, I think, apt to be forgotten, and gout vicariously saddled with all the infirmities of age. Thus, out of 2,680 examples of arterio-sclerosis Huchard held gout and lithiasis responsible for no less than 693. An appalling indictment, but what of the long arm of coincidence? For age unquestionably is the chief factor in the production of arterio-sclerosis, though many allot gout a dominant rôle in its genesis. This certainly is by no means proven. Still, whatever be the relationship, gout and arterio-sclerosis are very often found in association. If so, the prognosis will obviously rest, not on the gout, but on the vascular disease—the pulse tension. If therewith be correlated albuminuria and a displaced apex beat, the outlook is unfavourable.
Again, is the subject lean or obese? If the former, so much the better, for corpulency and gout are a sinister combination.[246] Gout in itself, as previously observed, favours microbic invasion, and obesity accentuates the liability. Moreover, the gouty obese are prone to arterio-sclerosis and granular kidneys, with sometimes a superadded glycosuria, or even true diabetes. In such subjects also the presence or absence of signs of cardiac mural degeneration must enter into our forecast, which at best is but gloomy.
Apart from arterial degeneration, we have to recollect the tendency to phlebitis of recurrent type. This when present always carries with it the risk of embolism and sudden death. Cases therefore displaying this proclivity to phlebitis must be judged accordingly. The gouty glycosuric, too, is always subject to the risk that the condition may develop into one of true diabetes. The absence of response to dietetic restrictions, viz., persistent sugar in the urine, the onset of thirst, polyuria, or other concomitants of diabetes, will darken the prognosis.
Also I myself believe that the presence of local foci of infection gravely prejudices the course of gout, accentuates any tendency to recurrence of the attacks, and incidentally reinforces any latent proclivity to vascular and visceral degenerations.
Last, but not least, what of the subject’s habits? The “internal environment” of the tissue cells of the gouty is presumably of itself none too good; but if to this be added the poison of alcohol, lead, or the toxic products of gluttony, it is incalculably worse. The painter or the plumber, if he can, would be wise to change his calling. If the alcoholic be deaf to remonstrance or the glutton continue to gorge, their chances of life dwindle proportionately, and if given to both vices, still more so.
In conclusion, the prospects of long life in gout depend in the main on the presence or absence of associated morbid states. If there be no complications such as I have indicated, the disease, in my experience, is not likely to shorten life materially, always provided that the victim is amenable to what should be the watchword of the gouty,—
The intimate cause of gout is unknown—a humiliating reflection, albeit salutary, if it but engender a more catholic attitude on our part when seeking to unravel the nature of this obscure joint affection. For, to secure ideal ends, diagnosis must be, not only clinical, but etiological. This is the more likely to be attained if we shed all preconceived ideas and prejudices.
Confronted, then, with a suspected case of gout, whether acute or chronic, what shall be our way of approach? Not the easy and hazardous path of lightning diagnosis affected by those who plume themselves on their so-called clinical “instinct,” but the slow, laborious route of clinical “observation,” that leads more surely to the vantage ground of truth, this assuredly in all diseases, but in none more so than in joint disorders, whose outward resemblances so oft hark back to inward disparities.
First, as to the manner of man, while one would not decry the hints obtainable from physiognomical peculiarities, it is often hard, if not impossible, to fit the subject to the so-called “gouty diathesis.” They are not all of the John Bull type; not a few are spare in build. Hence the danger of too ready inference from so-called “gouty” traits, to be regarded rather as ancillary to, but not substitutes for, more exact criteria.
Now, as to heritage, for, despite the fallacies that surround inquiries into family predispositions, they often furnish valuable hints as to the metabolic trend of the stock. True, ancestral stories often prove indefinite, but fortunately less so in the “gouty” than in those of “rheumatic” tendency. For, as Sir Dyce Duckworth points out, even the laity are quick to recognise what they term “chalky” gout, and so “if a history be given of ancestors or relatives thus affected, there need be no hesitation in pronouncing for true gout amongst them, and for the probably gouty nature of such arthritic ailments as may be complained of by the patients under examination.”
Turning to the individual himself—for the subjects of regular gout are rarely women—what is his age? If he is over thirty-five and has never previously had an arthritic disorder, it is much more likely to be gout than rheumatism, this only as a broad generalisation.
What occupation does he follow? What are his habits? Is he of the “idle rich” who “fare sumptuously every day”? Is he a plumber, a painter, or a butler, coachman, or club waiter, these last being men who, as Sir Thomas Watson observes, “often live more luxuriously and more idly a great deal than their masters”? In short, we must search for any evidence of overeating, overdrinking, and indolence. For of this triad of vices is gout too oft begotten.
As to illnesses, his past may tell of classic outbreaks, one or more in the great toe, and if to this be added a visible tophus, we stand face to face with a “gouty diathesis.” More eloquent this than a “cloud of witnesses” as to previous attacks of migraine, asthma, eczema, etc. All these and more may emerge during the subject’s recital, and by all means let them be ascertained. But forget not that they often arise in the non-gouty. Above all, though, miss not the significance of heightened blood pressure, a cardiac lesion of degenerative type, sugar or albumen in the urine. For these are of the things that will out, but let it not be to our discomfiture!
Even presuming that all facts and observations up to now point to a “gouty” origin of the arthritis, the end is not yet. What has evoked the arthritis? We seek a cause. For to call an arthritis “gouty” is but to restate the problem. How clear the need then for a meticulously careful investigation, in the hope of achieving not a merely nosological, but an etiological, diagnosis.
To narrow our field, we should, in the first place, exclude gonococcal infection, and failing this, influenza, syphilis, or any of the zymotic or other disorders prone to be followed by or associated with joint affections.
If none of such be forthcoming, we should search for local foci of infection. The mouth and its accessory cavities first claim attention. It should be closely scanned for the presence of oral sepsis, the most fruitful source of which is pyorrhœa alveolaris. If dentures are worn it is wise not to take the subject’s word that all his teeth have been extracted. Like others, I have in such found the broken-off stumps still in situ. The condition of “bridges” should be noted, fruitful sources of sepsis as they are. Clinical examination of the mouth may prove inadequate, as buried roots, cysts, or abscesses, not to mention alveolar rarefaction, etc., demand for their detection radiographs.
The pharynx and tonsils should be thoroughly investigated, for disorders of these same are by no means uncommon in “gouty” subjects. Any history of aural or nasal discharges demands the same careful local examination; and, needless to say, the same course must be pursued in regard of any local infections of the genito-urinary passages. In short, in gouty, as in non-gouty, forms of arthritis, thorough and routine examination of every patient by modern bacteriological methods is imperative.
Ignorant of the precise etiology of gouty arthritis, we can ill afford to overlook any associated infective foci which may prejudice the well-being of the victim, as, for aught we know to the contrary, we may be overlooking the very fons et origo mali. Compare our attitude towards other arthritides of cryptic origin, how systematic our search for infective foci, and what a light has thereby been shed on their intimate etiology!
Here may we lodge a plea for routine examination of the blood in all cases of gout? For, as shown, the findings, leucocytosis, etc., have doubtless some profound significance. Apart from this, the routine employment of complement-fixation tests for the organisms responsible for local infections might illumine the obscurity that overhangs this complex problem of their relationship to remote pathological lesions.
If up to now our search for local foci prove futile, it remains for us to note the presence or absence of functional derangements of the alimentary tract, or its accessory glands. We must not, because we think perhaps that the patient “looks gouty,” assume that his dyspeptic symptoms are of like origin. It is our duty to ascertain, if possible, the precise nature and origin of the dyspepsia.
We know that, given oral sepsis, sequential infections of the appendix and gall bladder are not uncommon. Recently it has been remarked that many gouty patients suffer with attacks of pain in the region of the appendix, and simultaneously tenderness over the gall bladder. That the subjects of gout enjoy no immunity from appendix or gall bladder disorders is certain, and at this we need not be surprised, seeing the frequency with which they suffer from alleged causes thereof, i.e., dental sepsis, etc.
But what we would insist upon is that we should not be content merely with dubbing these symptoms “gouty,” as they are much more likely to be, not symptomatic of gout, but etiologically related thereto. If then we are to arrive at the exact nature of the underlying lesion, the probable site of infection or toxic absorption, we must invoke all modern methods of investigation. Thus, how valuable the existence of an X-ray barium or bismuth meal in furnishing positive evidence of gastric or duodenal ulcer on the one hand or of gall bladder or appendix disease on the other. What[250] an aid to the location of adhesions the demonstration of ileal and cæcal stasis, etc.!
In obscure cases the fæces may have to be scrutinised for evidences of pancreatic inefficiency, viz., bulky pale stools, undigested meat fibres, and excess of neutral fat. Their bacterial content, too, if abnormally high, should be noted. As in other arthritides of unknown origin, the results following the administration of vaccines prepared from the predominant organisms have been such as to suggest a causal connection.
The urine should be subjected to chemical and bacteriological examination. As to uric acid, the delusion still widely prevails that gouty subjects excrete large amounts thereof. How frequently is “the degree of acidity” of the urine or “its content of uric acid” held to justify a diagnosis of gout. The deduction is quite unjustifiable. Equally so the assumption that the reverse, a defective excretion of uric acid, is an invariable feature of the gouty diathesis. For though when on a purin-free diet the output of uric acid in the gouty is low, it rarely, if ever, falls below the level of normal. The truth is that we cannot on the mere basis of the variations in uric acid excretion in the urine presume to diagnose gout.
To have any semblance of diagnostic value, the patient should be on a purin-free diet, and a long series of exact quantitative examinations made. C. v. Noorden, to gauge the limit of tolerance of his patients, gives them increasing amounts of purin, and so determines the quantity the subject can deal with without showing retention. But, as Von Fürth satirically observes, “when a physician allows a quantitative analysis to be made of any arbitrarily collected specimen of urine of his patient and then makes a diagnosis of the presence or absence of a ‘gouty diathesis’ after a glance at the list of data of the analysis, he is really not proving by his actions his possession of diagnostic acumen as much as he is laying bare his total ignorance of bio-chemical matters.”
So much for the diagnostic valency of uric acid estimates in chronic gout, but if the patient be on purin-free diet, and an acute attack ensue, the curve of uric acid excretion is fairly characteristic. In other words, for a day or two preceding the outbreak, the uric acid output falls below the usual level, but early in the attack rises markedly, to be followed by a secondary fall.
Some aid in diagnosis has been afforded by the fact that after ingestion of purin-containing food the gouty individual does not, like a normal person, eliminate the excess of uric acid, but the excretion is “spread out over a number of days.” But this retardation and diminution in the excretion of exogenous purins[251] has been seen in non-gouty forms of arthritis, not to mention some cases of nephritis and chronic alcoholism. Hence delayed nuclein exchange, though highly suggestive of gout, is not infallibly diagnostic thereof.
As to uric acid in the blood, it will, I fear, not for long, if ever, be easy to prevail on patients to submit to withdrawal of the amount of blood necessary, even by modern methods, for its estimation. Fortunately, our American confrères appear to be more successful in securing such opportunities. Pratt states that in his twenty-one cases of genuine gout the uric acid content of the blood, irrespective of diet, was 3·7 mg. per 100 grams, as opposed to 1·7 mg., the average amount in 156 non-gouty cases studied by Adler and Ragle. Still Pratt noted that in a few cases of undoubted gout the uric acid content of the blood was within normal limits, though it never fell, even on a purin-free diet, below 1·4 mg. Nevertheless he holds that there is conclusive evidence that the uric acid content of the blood is in gouty individuals notably increased both in the intervals and during attacks.
He has found the sweetbread meal an aid in diagnosis, and the following is his method of procedure: “The patient is placed on a purin-free diet, and the daily output of uric acid in the urine determined. After having been on this diet for at least four days the blood is analysed for uric acid, and 150 to 300 grams of sweetbread (weighed raw) are fed. The purin-free diet is then resumed. The blood of gouty subjects forty-eight to seventy-two hours after the sweetbread meal has shown in every case examined an abnormally high amount of uric acid, while in control subjects this was not found. It is not improbable that this rise in the uric acid content of the blood may occur in certain cases of nephritis and other pathological conditions.”
A bacteriological examination of the urine should be undertaken. Trautner held mucous colitis as one of the initial manifestations of gout, and believes that the bacillus coli communis is the primary agent in gouty affections. He suggests that it produces a reducing substance which during its passage through the body is transmuted into xanthin and uric acid. Be this as it may, there is increasing evidence that an etiological potency may attach to coliform bacilli, streptococci, and other organisms. Dr. Munro in his researches at the Royal Mineral Water Hospital, Bath, noted that the blood serum in one of my cases of acute gout agglutinated B. coli. He has also found streptococci in the urine in acute gout, and these subjects certainly enjoy no immunity from other forms of bacteriuria.
It is beyond the scope of this volume to outline the methods of differentiating and determining the exact organisms which may[252] be responsible for gouty arthritis. But if we aim at rational as opposed to purely haphazard serum or vaccine therapy, we must effect a differential specific diagnosis in a bacteriological sense. How searching our investigations must be in these cases we learn from Adami’s brilliant address on sub-infection when he laid down the axiom that in all cases “there ought to be routine blood cultures, routine examination and reports on the stools and their predominant bacterial types, blood counts, hæmoglobin examination, in fact the full clinical study of each case, so that nothing is neglected.”
No apology is needed for our insistence on the imperative necessity of routine systematic investigation from all sides of these cases of gouty arthritis. For its origin still remains hidden, and who can doubt that, to remove this long-standing reproach, we must approach our study of these cases in a more catholic attitude of mind, one bent on etiological, not merely nosological, diagnosis?
The word gout itself is void of offence, innocent of scientific pretensions, neither expressing nor violating any article of pathological belief. But let us not forget that the term is neither self-explanatory nor final. Derived through the French goutte from the Latin gutta, it but expresses laconically the fanciful doctrine of those who so christened it.
What the old humoralists saw was the tophus, and would that they had clung more steadfastly to this as their sheet anchor in diagnosis! but casting their moorings, they launched forth on the uncharted seas of abstract philosophy. Even in the writings of the nineteenth century physicians we trace the influence of their disquisitions, and we are tempted to think that some even of our day still bide beneath their thrall.
But, with the advance of pathology to the dignity of a natural science, we must assert our independence of misty hypotheses, rendering obeisance only to facts. What then, may we ask, is the outstanding fact of the “gouty diathesis”? It is, in a word, the tophus! Even as the vague and shadowy constitutional warp known as the “rheumatic diathesis” finds expression, or rather becomes incarnate, in fibrous nodule and induration, so also does the equally nebulous “gouty diathesis” become objective, crystallised in the tophus.
This problem calls for more critical consideration than is usually accorded thereto. The tophus is, in truth, the touchstone[253] of gout, yet not a little controversy obtains as to the frequency of its incidence in “gouty” subjects.
At one extreme we find Sir Charles Scudamore maintaining that tophi have occurred in only a few individuals “of particular ‘gouty’ idiosyncrasy,” in, according to him, less than 10 per cent. of the victims. At the other Sir Alfred Garrod, discussing these figures, observes: “From my own experience I consider these numbers far below the real proportion, from their being deposited in parts of the body scarcely to be expected.”
Now as to these distinguished physicians, who shall doubt that of the twain Garrod stood on firmer ground than his predecessor? In arriving at their diagnoses of gout, Scudamore rested on clinical “instinct,” Garrod on clinical “observation.” To the more scientific mind of the latter the tophus appealed with all the insistence of a fact, while the former was yet in bondage to abstract philosophy, dominated too much by crude and unproven hypotheses.
Given the presence of tophi, the diagnosis of a “gouty diathesis” is assured; in their absence it is but speculative.
It is upon this dictum that we would take our stand, and this without depreciating in any way the pioneer researches of Garrod. For it must be recognised that the increasing differentiation of joint diseases has proceeded apace. How many are now affiliated to specific germs, not to mention the undreamt-of light thrown on their inward characters by X-rays! Scudamore’s work appeared exactly a century ago, Garrod’s in 1876. The conclusion then seems inevitable that many of their alleged cases of gout—at any rate, those unattested by tophi—would now be relegated to widely different categories.
But this zeal for infinite cleavage and subdivision, so characteristic of the modern school, far from diminishing, does but accentuate, the diagnostic valency of the tophus. It still remains the infallible criterion of diagnosis, and, for myself, I feel convinced that infinitely more good than harm would ensue if we refuse to recognise any individual as being of the “gouty diathesis” unless he exhibit these objective stigmata thereof.
Of course to some such a rigid attitude will spell anathema. I hear them say in oracular tones: “Never forget gout, or awful indeed will be your awakening.” More harm, say they, is wrought by failure to recognise gout than by diagnosing gout where none is. Doubtless they are right in counselling us not to forget gout, but not to the exclusion of all else. For, at issue with them, I hold it better to miss gout than to miss syphilitic, gonorrhœal, and other forms of arthritis.
“A name being so readily found for an obscure disease, the[254] practitioner considers himself as excused from the difficult task of nicer discrimination.” Thus wrote Scudamore a century since, a rebuke and a warning for all time.
How elated we are, and rightly, when in an obscure form of arthritis we pounce on these objective criteria of gout, how apt to deem our diagnostic quest as ended, and with what fatal glibness the time-worn “gout” slips from our lips, sure, alas, of ready and almost complaisant acceptance. Fallacious inference, all too prevalent, that the presence of tophi stamps any concomitant arthritis as “gouty.”
True, tophi are pathognomonic of gout, but their existence does not confer on their host immunity from all other forms of arthritis. In view of the increasing light shed upon joint disorders, who can doubt that (and this not only for our forefathers) the tophus has too often proved a veritable snare, allaying all diagnostic doubts, lulling us into false security? For an individual may, for example, exhibit auricular tophi and be the victim also of an arthritis, but the latter is not inevitably “gouty.” All that can be assumed at sight is merely that the joint disorder, whatever its nature, has ensued in a subject of “gouty diathesis.”
For it may be of specific infective origin, gonococcal, syphilitic, pneumococcal, etc. Quâ a concomitant arthritis, then, the diagnostic significance of tophi, at any rate when of ab-articular site, must not be overrated. It is at once a beacon and a warning. In other words, the diagnosis of a co-existent arthritis as “gouty” should not be entertained pending the exclusion of all other forms of arthritis.
Conversely, in the absence of tophi, the diagnosis of an arthritis as “gouty” is not absolute, but presumptive.
For in the lack of these objective stigmata how can the authenticity of our diagnosis be established? Is it not when achieved a nosological rather than a diagnostic feat? Put otherwise, is not our diagnosis, especially in initial attacks, largely topographical? Not that we would for one moment decry the advantage of realising the predilection of certain organisms for this or that particular joint: of the gonococcus for the sterno-clavicular, of typhoid for the hip, post-scarlatinal rheumatism for the phalangeal joints, etc. But we would drive home the fact that our diagnosis in initial attacks of “gout” is very largely topographical. Let but inflammatory trouble ensue in the big toe, and forthwith we assume it gout, as if, forsooth, this particular joint were immune from all other forms of disease, this, too, while in the same[255] breath we comment on its extreme liability to injury. So, indeed, we maintain, is the marked predilection of gout for the toe joint explained. Is not this a little crude? Does not the same circumstance increase its liability to infection and, we may add, not less important, its proneness to static deformities? But to this we shall recur when discussing differential diagnosis.
To return, how often, apart from the above pitfalls, is the diagnosis “gout” arrived at without any search for tophi wherewith to support the assumption. Our contention is that even in primary attacks of gout our search for tophi should be exhaustive. If undiscoverable, why not be honest with ourselves and recognise that our diagnosis is presumptive pending their development?
Sir William Roberts on this point observes: “As a rule, diagnosis of acute articular gout is easy, but exceptional cases of difficulty occur. The gouty character of the inflammation is affirmed by the discovery of uratic concretions in the rim of the ear or elsewhere.”
Again, Sir William Osier, discussing the diagnosis of acute gouty polyarthritis, remarks: “We have had of late years several cases admitted for the third or fourth time with involvement of three or four of the larger joints. The presence of tophi has settled the nature of a trouble which in previous attacks has been regarded as ‘rheumatic.’”
One may, we think, gather from these two statements the inference that both these distinguished authorities hold tophi to be the only infallible criterion upon which to base a diagnosis of gouty arthritis. In my own practice I must affirm that I never feel justified in christening any arthritis as gouty unless I have discovered tophi, and then only when to the best of my ability all other known causes of arthritis have been excluded.
In reviewing the statistics of authors as to the frequency of the incidence of tophi in their cases of assumed gouty arthritis I am inclined to think their relative infrequency is apparent rather than real, in other words that many of their cases of alleged “gouty” arthritis which lack tophi would, if investigated by modern methods, have been shown to be due to other causes of arthritis, this especially as regards their assumed cases of chronic gout. For who can doubt that prior to the discovery of X-rays many cases of osteoarthritis, etc., were thus erroneously labelled? Nor indeed, as we hope to show later, is it improbable[256] that similar fallacies obtained even in regard to acute types of gout, particularly when of polyarticular distribution.
It will be noted that we confine our criticisms to those examples of “gouty” arthritis unassociated with tophi. But if, as we maintain, our scepticism be justifiable, then it follows that it diminishes to an unknown extent the percentage of cases of genuine “gouty” or uratic arthritis which lack tophi.
Apart from the probability of such erroneous relegation to the “gouty” category of non-gouty arthritides, there remains this further consideration, the ease with which tophi, even when superficial, may be overlooked. We look for pearly white concretions, and if none are seen we straightway assume that tophi are absent. This, I am sure, is a very common pitfall. At their inception tophi are neither white nor hard. They are largely fluid and soft to touch. The skin over them may be unchanged in colour or reddened. Only when mature, and the overlying skin is thin, do they assume the ordinary aspects of a tophus. These observations apply not only to tophi in the ears, but to those in the vicinity of the small joints of the hands and feet or elsewhere. I would urge that in the case of all soft localised swellings of dubious nature in the neighbourhood of the phalangeal joints aspiration with a hypodermic syringe will often prove very helpful. If fluid can be withdrawn and the same microscopically examined, it will more often than is supposed reveal the presence of biurate crystals.
More information is badly needed as to the relationship of their formation to acute attacks of gout. Garrod on this point remarks: “The deposits are probably formed during an attack of gout, but occasionally they appear shortly afterwards. In one case, of which I have notes, the ears were carefully examined without result when the patient left the hospital, but within ten days, on re-examination, a deposit was found. Perhaps some fluid was effused during the fit, but being at first transparent, could not be easily distinguished.” Sir Dyce Duckworth, too, observes: “After acute attacks of gout have passed off there may follow renewed pain in the neighbourhood of the joint, and later there is discovered a nodular or soft swelling. In the latter case there may be fluctuation, indicating a liquid collection of urates. This should never be opened. In a few weeks this tumour tends to indurate, grow more compact, and a so-called ‘chalky’ concretion is established.”
Reflection upon the foregoing considerations leads me to the[257] conclusion that not only was Garrod right in his affirmation that “gouty inflammation is invariably attended with the deposition of urate of soda,” but more that examples of true uratic arthritis which lack tophi are exceptional, and that in their absence their diagnosis as such cannot be with certitude established.
We have now, we trust, sufficiently defined our attitude towards the tophus, the salient objective stigma of a “gouty diathesis,” and the indispensable rôle it plays in enabling us to establish the diagnosis of articular gout.
The nonchalance with which not a few writers dismiss the diagnosis of acute gout when located in the great toe or elsewhere in the foot is, to say the least of it, somewhat remarkable. “It is a very easy matter,” say they, and as an earnest of their good faith are silent as to the many pitfalls that await the unwary. Should they deign to differential diagnosis, they are at pains to discriminate between it and acute articular rheumatism, which re classical outbreaks in the toe seems a little superfluous! But not a word of traumatic lesions, infective processes and static deformities, all infinitely more likely stumbling-blocks.
Did all cases conform to the classic type, acute sthenic gout, it might be held relatively easy. But such are not, to say the least of it, common nowadays. More often than not our examples are, as Garrod terms them, of acute asthenic character. As he observes: “There may be indeed pain and tenderness in the toe, and some amount of swelling, but accompanied with little heat or redness, and all febrile disturbance may be absent; still œdema is generally observed and itching and desquamation follow.”
That diseases, like their victims, alter with environment is but too clear. Who can doubt that the gout of the Regency has to-day assumed a milder clinical facies? Physicians of those days were haunted with the fear of confounding it with erysipelas and phlegmon. Still, while no such fears apparently beset us to-day, it were well to walk circumspectly.
Thus, recently a friend of mine came across an instance of what he deemed acute gout in a metacarpo-phalangeal joint. Its failure to respond to colchicum and the growing intensity and extent of the local inflammation suggested incision, when, lo, pus issued, to the subject’s comfort, but to his own chastening!
There are, however, many more likely sources of fallacy, these, too, of the most diverse type, inasmuch as they differ according to the exact location in the foot of the assumed gouty process. For while the big toe is the site of predilection for the initial manifestation, it is not always so. The primary outbreak may be located in any of the smaller joints of the foot, or outside them in related structures: in the heel, the sole, or the tendo Achillis.[259] These vagaries greatly enhance the difficulties of diagnosis. For the process of differentiation will vary according to the particular joint or structure involved, the predilections of certain infective processes, not to mention the marked liability of the foot to painful disturbances of static origin.
Inasmuch as the primary outbreak may be located in any part of the foot, we purpose, for reasons just cited, dealing seriatim with gout in (1) the big toe; (2) the instep; (3) the heel; (4) the sole.
Infections.—There is no â priori reason why any of the infections may not find a nidus in the first metatarso-phalangeal joint. Thus, Garrod, as we know, held gouty subjects specially liable to pyæmia. In rare instances, the primary focus has been in or near the great toe, and has consequently been mistaken for gout. The rapid progress of the disease would of course soon clear up the nature of the case. But if the subject has previously suffered from gout, such a diagnostic error at first sight is quite excusable. Accordingly, as a safeguard in all doubtful cases, inquiry should be made as to the existence of bladder troubles, piles, etc., especially any recent operation in this or other regions.
Again, while gout in its articular form is rarely, if ever, met with in children, it must be recalled, on the authority of Sir James Goodhart, that rheumatism in their instance is occasionally limited to one joint. Moreover, this distinguished physician actually saw it localised in the great toe, “in a case in which the subsequent course of the disease showed that it was acute rheumatism.”
Acute Gonococcal Arthritis.—We may recall that Van Swieten, a disciple of Boerhaave, held that sometimes a wife while nursing her gouty husband had contracted the same disorder. A tribute, we fear, to Van Swieten’s diplomacy rather than to his clinical acumen—an euphemism for gonorrhœal rheumatism!
Of course in adolescents or in young adults monarticular pain, with or without swelling, heat, or redness, should not suggest “gout,” but an infective disorder either in the joint or the related bone-ends. At the same time middle-aged men enjoy no immunity from gonorrhœa, and we may add that gonococcal infection of the metatarso-phalangeal joints is not so uncommon. When located in that of the great toe, it is easy to see how readily the acute arthritis may be confused with gout. But, unlike the latter, its duration is measured by months or weeks rather than[260] by days. It is well to recollect, too, that “gouty” persons are more prone to develop arthritis following gonococcal infection. Given therefore a history even remote, we should in doubtful cases recall the longevity of the organism, its persistence in the prostatic recesses, and the need for bacteriological investigation.
Traumatic Lesions.—Its exposed situation renders the big toe very liable to trauma. Often, too, the injury being slight, and not followed by any immediate consequences, the connection may easily be overlooked. A blow or a fall may readily bruise the synovial membrane without at first any external sign. But given trivial hæmorrhage into the cavity or subjacent tissues, an acute synovitis with effusion is induced.
Again, joint disorder following injury is usually monarticular, whereas the same when the outcome of so-called “constitutional” causes is generally oligo- or poly-articular. The relevancy of this is obvious when we recall that initial attacks of gout are monarticular. Accordingly, given a history of definite injury to the toe joint, the question arises, Is it acute gout or acute traumatic arthritis? this especially if the subject has not had a previous attack of gout at this site.
Here I would lay stress on the fact that indirect rather than direct traumatisms are more common antecedents or determinants of gout, viz., sprains or strains. Moreover, in reviewing the writings of the older physicians one is driven to the conclusion that frequently a septic cellulitis, synovitis, or a frankly traumatic arthritis was confused with acute gout.
The following examples cited by Scudamore are, we contend, susceptible of such an explanation: “A gentleman much subject to gout, when considering himself unusually well, underwent the slight operation of having the nail of the great toe cut on account of its improper growth. The toe was much pressed, and gouty inflammation was the immediate consequence.” In another case “the patient, never before having suffered the gout, tore off a broken portion of the thumb-nail, so as to make the part tender. Very soon the thumb and part of the hand put on a swollen and shiny appearance, and was exquisitely painful. A poultice was applied. Suddenly on the third evening the pain quitted the thumb and seized the toe, next the ankle, then the knee, and lastly the great toe of the other foot. Throughout he secured ease and sleep till the first light of the morning appeared, and hence facetiously observed that the gout in this respect assumed all the behaviour of a ghost.” Was not this probably a case of septic absorption with cellulitis and a mild degree of sapræmia, evoking arthralgic pains?
In conclusion, without denying the potentialities of trauma,[261] whether direct or indirect, in determining an outbreak of gout, we would submit that its diagnosis under such circumstances should not be hastily arrived at, but by the slower process of elimination, this especially if the trauma has involved slight abrasions with the possibility of sepsis. A quick response to colchicum would of course be highly suggestive of gout.
Acute Osteoarthritis.—It is perhaps not so widely recognised as it should be that osteoarthritis not uncommonly attacks the metatarso-phalangeal joint of the great toe. It becomes enlarged owing to the hypertrophy of the articular ends. Like similar lesions in the small joints of the hand, the big toe joint from time to time undergoes exacerbation, with increased vascularity and local heat, which, though of minor degree, may by a superficial examiner be readily misinterpreted as gout. The parts are painful, somewhat swollen, hot, and tender, but the local symptoms are never intense, and constitutional disturbance is lacking. The presence of osteoarthritic lesions elsewhere and the revelations of skiagraphy will suffice for differentiation of such cases from asthenic articular gout.
Hallux Valgus with Inflamed Bunion.—Scudamore in his “Treatise on Gout” observes that “the bursal disease over the first joint of the great toe, which is familiarly known as bunion, is a very common complaint with gouty persons.” In view of the fact that no reference is made in the context to the absence or presence in such cases of a condition of hallux valgus, one is led to believe that Scudamore overlooked the deformity and regarded the local bursitis as the outcome of a gouty inflammation of this structure.
Bradford and Lovatt, discussing hallux valgus, observe: “There may be pain and irritability in the great toe joint, and in severe cases extreme pain and difficulty in walking, which is usually attributed by the patient to gout.” We would only qualify this statement by the fact that the local heat, redness, and swelling that in this condition so often follow slight injuries or excessive walking is not only so interpreted by the patient, but far too frequently also by his medical attendant.
Routine examination of the bare foot will minimise the chance of such a fallacy, though of course it must be borne in mind that a gouty subject may present this deformity. But when we recollect that hallux valgus of slight degree “is almost universally present after middle childhood,” we see that, given the presence of this static foot deformity, any inflammatory process in the[262] superjacent structures is infinitely more likely to be due to an inflammatory bursitis than to a gouty arthritis.
Given an inflamed bursa with cellulitis spreading over the dorsum of the foot, confusion with acute sthenic gout is all too easy. But in our experience, mirabile dictu, the ordinary more or less chronic circumscribed redness over the bunion is but too commonly misinterpreted as gout, this particularly in women, despite the rarity with which gout attacks their toe and the frequency with which their footgear is precisely adapted to produce hallux valgus. Given therefore the presence of this static foot deformity, we should in the absence of objective stigmata of gout, viz., tophi, suspend our diagnosis pending observation of the results obtained by local treatment of the displaced toe.
Hallux Rigidus.—This deformity is but too often overlooked, and if marked by pain and more or less rigidity of the first metatarso-phalangeal joint, it may, in lack of adequate examination, be flippantly dismissed as “gout,” this more particularly in its later stages, when, in addition to pain and stiffness therein, the joint is swollen, tender to the touch, and the bony ends actually enlarged. Here again local examination, if carefully carried out, will suffice to obviate such errors, while the quick response to rest and appropriate applications, with correction of the frequently associated sunken arch, will sufficiently attest its true nature.
Metatarsalgia.—As pointed out in our previous work on Fibrositis, “this painful condition is more often than not confused with rheumatism or gout.” We have known subjects wander to nearly every spa on the Continent under such a misconception. Not to mention the financial expense, the dietetic penances imposed, the consequences of such faulty diagnosis, are by no means trivial, for the intensity of the suffering may reduce the walking capacity to a minimum.
The neuralgic pain radiates into the toes and often upwards into the leg, usually comes on while walking, and is relieved by the removal of the boot. For its detection any altered relationship in the position of the third, fourth, and fifth metatarsals, especially their displacement to a lower level than normal, should be noted, and any limitation of the power of dorsal flexion of the foot likewise estimated. The presence of callosities under the heads of the metatarsals is very suggestive of this painful condition.
Next to the metatarso-phalangeal joints, the tarsal articulations are the most frequent site of initial attacks of gout. Here again we would insist on the necessity of excluding infections of[263] the tarsal joints or shafts and even more important, static foot deformities.
Gonococcal Arthritis.—In a table compiled by Garrod from those of Foucart, Brandes, Rollet, and Fournier, the relative frequency of the implication of individual joints in gonorrhœal arthritis shows that out of a total of 119 the tarsus and metatarsus were attacked in five instances. In the more acute cases the periarticular swelling, local heat, and pink blush may be confused with acute gout. The resemblance is enhanced in that, as in gout, the overlying tendon sheaths are liable to become inflamed and distended with fluid.
Tuberculous and Syphilitic Disease of the Tarsal Joints or the Related Joints.—In cases of obscure pain and inflammatory trouble in the instep the possibility of arthritic and bony lesions of this nature should not be overlooked, especially if there be suggestive lesions elsewhere, or if the history afford evidence of the possibility of such contingencies.
Pes Planus.—In all cases of pain and swelling, with or without redness, in the instep, it is well to recollect that, though flatfoot may for a long time exist without giving rise to symptoms, it frequently happens that, in sequence to some unusual strain on the plantar arch, the static disturbance in the foot enters quite abruptly on a painful phase. Congestion and swelling of the foot is common, and actual teno-synovitis of the tibial and peroneal muscles is not infrequent. Tenderness, too, at points of ligamentary strain is almost always present, and more or less constant pain.[40]
The frequency with which the local and referred pains of flatfoot are misinterpreted as “gout” and dietetic restrictions and other useless and uncalled-for methods of therapy enjoined is well exemplified by a case which has just left our consulting room.
The subject, a middle-aged spinster of lean kind, came to Bath for treatment of her supposed gout, and for which indeed she had previously received spa therapy. Her feet when bared showed a condition of double hallux valgus with related bursal thickenings.[264] The occasional inflammation of these latter structures and the recital of doubtful ancestral proclivities were the sole evidence on which was based the diagnosis of gout. In addition, as is so frequent in hallux valgus, there was associated therewith a bilateral flatfoot, and it may be added that in the left foot a hammer-toe had been removed some years since. Unfortunately the neglected symmetrical flatfoot had, as so frequently happens, initiated, through the erroneous deflection of a body weight, a condition of chronic villous synovitis in both knees. This again was misinterpreted as but another proof of her assumed “gouty” diathesis. Reflecting upon human nature, how curious the reluctance with which such subjects elect to part with their “gout.” Women especially hold tenaciously thereto, even those of austere type, clinging to the taint handed down to them from some far-off ancestor whose “superfluity of naughtiness” was a by-word among his generation. To exchange gout, morbus dominorum, for “flatfoot” and inflamed “bunions,” savours of degradation, and to couple it with aspersions on their footgear is well-nigh insupportable. Nor are the “lords of creation,” we fear, exempt from this failing. We recall during the War being consulted by a highly placed officer who complained of gout. A well-preserved man of nigh sixty years of age, he obviously prided himself on being immaculately booted. As such patients frequently do, he brought his own diagnosis of “gout.” Removing his footgear, manifestly too small, his crucified toes stood out with bunions in a state of hot resentment. But impeachment of his boots was too much for him. Persuasion and argument were futile, and I doubt not he walks to-day stiff, a martyr to his vanity. “Il faut souffrir pour être belle.”
In some instances the first manifestations of gout occur in the heel, while in others the sheath of the neighbouring tendo Achillis is the part first invaded. Probably there is no region of the foot in which there exist more pitfalls, and doubly careful should we be before concluding that any painful or inflammatory condition thereof is one of “gout.”
Referred Pain.—Pain in the heel affords many loopholes for misinterpretation. It may, as Sir James Paget pointed out many years ago, be symptomatic of a renal calculus. In my own experience it is sometimes complained of by the subjects of internal hæmorrhoids, the pain waxing and waning with the variations in the rectal trouble, and only disappearing permanently when the piles have been radically treated. It is, again, a[265] symptom sometimes complained of by the victims of enlarged prostate.
If the pain and tenderness be located on the under-surface of the os calcis, there are several misconceptions possible.
(1) Careful examination may reveal a tendency to flatfoot, the pain being referable to strain on the posterior insertion of the plantar fascia.
(2) The root of the trouble may be a gonococcal inflammation of the plantar fascia, or of the periosteum covering the os calcis.
(3) A skiagram may show the existence of a bony spur on the inferior surface of the os calcis.
(4) The bursa under the os calcis may be inflamed.
(5) Also, as Tubby has pointed out, pain in the heel may be referable to shortening of one leg or constant standing, and more rarely to tuberculous disease of the os calcis.
If the pain and tenderness be located on the posterior surface of the os calcis, or in the tendo Achillis, the following should be excluded before assigning the trouble to “gout”:—
(1) Post-calcaneal Bursitis.—Inflammation of the bursa lying between the os calcis and the tendo Achillis is not uncommon. It may be uni- or bi-lateral, and in the majority of instances is attributable to violent exercise, or chafing of the heel by ill-fitting boots. The local swelling and tenderness at the site of the inflamed bursa and its aggravation by plantar flexion of the foot will afford a clue to its true nature. (An exostosis projecting from the hinder surface is sometimes a cause of post-calcaneal bursitis.)
(2) Synovitis of the Tendo Achillis.—Symptoms very similar to those above described have been met with in a teno-synovitis of the tendo Achillis, as evidenced by swelling of the sheath, tenderness, and silky crepitus.
There is a wide disposition to regard all painful or unpleasant sensations in the sole of the foot as evidences of “goutiness.” It may be recalled that Strabo, according to Plutarch, apostrophised heat or itching of the feet at night as “the lisping of the gout.” Duckworth, too, emphasised the frequency of this symptom in the gouty, and Sir Charles Scudamore also held heat and dryness of the sole as frequent harbingers of acute attacks. Now, did we[266] but confine our hazards as to gout only to cases marked by heat or itching in the sole, possibly little harm might result; but unfortunately there is a flippant readiness to relegate all obscure pains or abnormal sensations in the sole to the “gouty” category. Needless to say, this is quite unjustifiable. We need not reiterate the bounden necessity of excluding all static foot deformities, but we should in addition recall the various types of plantar neuralgia.
Plantar Neuralgia.—Occasionally, as we have pointed out elsewhere, the pain is of almost unendurable severity. It constitutes one of the types of so-called partial sciatica, the pain and paræsthesia being confined to the plantar nerves. Indeed, pain, numbness, hyperæsthesia, or sweating of the sole are often symptomatic of a definite neuritis. Such may follow typhoid fever or caisson disease, and in this latter be of aggravated type. When we realise that the pain in these cases may be limited to the tips of the toes or the ball of the great toe, we see how readily it may be confused with “gout.” Fortunately plantar neuralgia is exceptionally rare; but even after exclusion of the foregoing causes we should, before pronouncing any such neuralgia to be “gouty,” recollect that plantar neuralgia or hyperæsthesia is very common in alcoholism and hysteria.
Erythromelalgia.—Among the exceptional cases that find their way to spas are examples of this rare disorder. Almost invariably they come under the diagnosis of “gout” or “rheumatism.” When we reflect that in the majority of instances the initial burning pain typical of the disease is located in some part of the sole of one foot, and that the associated redness and vascularity may be delimited to the ball of the great toe, the heel, or outer or inner side of the foot, we see the danger of its being too easily referred to “gout.”
If seen at the zenith of an attack, the severe pain, the local heat, the intense purplish redness, the distension of the veins, and in some instances œdema, how close the resemblance to gout! Precisely also, as in gout, the simulation of a deep-seated inflammatory process is very pronounced. Indeed, in not a few examples of erythromelalgia fruitless incisions have been made. Accordingly in all cases of pain, redness, and swelling in the sole of the foot, we should canvass the possibility that we may be face to face with an instance of erythromelalgia, a disorder which, like gout, is most frequently met with in men of middle age.
In drawing to a close our remarks on the diagnosis of acute gout in the foot, we would emphasise the fact that in all such cases the bare feet should be thoroughly examined. For, apart from infective and traumatic lesions, the frequency with which the various static foot deformities are confused with “gout” is[267] incredibly common. That gout may co-exist with hallux valgus or other distortion we readily admit, but this does not absolve us of our responsibility—correction of the static deformity. Combine this, if you will, with constitutional treatment if there be evidence, i.e., tophi, of a “gouty” diathesis, but, we repeat, correct the mechanical defect. For gout may come and go, but static errors remain. In so doing, the victim will be saved much preventable suffering, and, for aught known to the contrary, the removal of irritation and local congestion may haply minimise the chances of subsequent gouty outbreaks.
While primary attacks are in the vast majority of instances localised to the foot, if not actually to the toe, it is well to recollect that very rarely the knee, the wrist, elbow, or ankle may be the chosen spot. In such cases there is need for exceptional caution before committing oneself to a diagnosis of gout. Certainly not until all other known causes of acute arthritis of monarticular type have been excluded.
If in the knee or wrist, any possibility of injury or strain should be thoroughly canvassed. To make assurance doubly sure, a radiograph should always be taken. Specific infective forms of arthritis then call for careful elimination—i.e., gonococcal, etc. If there be no history of such, a painstaking search should be made for any local foci of infection, e.g., mouth and accessory cavities. If any be found, they should be radically treated, as it is much more likely that the arthritis is due thereto than to gout.
If, notwithstanding a meticulously careful investigation, no cause can be assigned, we may entertain the possibility of its being gout, the more legitimately if the subject be a middle-aged man coming of gouty ancestry and exhibiting himself tokens of this diathesis, i.e., tophi. It would be confirmatory, too, if, apart from its exceptional localisation, the joint disorder in its course conformed to that typical of gout in the toe, in other words if it was of sudden nocturnal onset, showed marked daily remissions in temperature and pain, responded swiftly to the action of colchicum, and was not protracted beyond the usual week or ten days.
Sir Hale White, discussing the diagnosis of acute gout of unusual localisation, remarks: “The real difficulty in acute cases comes when it is suggested that an acute arthritis with pyrexia and swelling and redness of a joint other than that of the great toe is caused by gout. I have recently seen the difficulty in one patient in the wrist, in another in the knee. Such cases, if they are not gout, are some bacterial arthritis.”
In the pathways of medicine, as in other walks in life, we are apt to become stereotyped, to fall into grooves, and sooner or later the inevitable rude awakening comes. Thus, so prone are we to think of gout as belonging, so to speak, to the foot, that when it erupts elsewhere it is often the last contingency to dawn upon us. If we diagnose it too often and too readily in the foot, we do so too seldom when it appears in joints remote.
Now, while in initial outbreaks of gout it is exceptional for more than one joint to be affected, it is not always so. For sometimes in those strongly predisposed by heredity not one, but many joints, may be implicated in the primary attack. Such cases, however, are extremely rare.
As a rule, this acute gouty polyarthritis occurs in individuals who have already experienced articular paroxysms at the classic site; but in the subsequent polyarticular attacks the toe joints are often unimplicated, and the disease is located in the larger articulations—the knees, ankles, wrists, or elbows. Herein resides the difficulty of diagnosis in these cases: the likelihood of confusion with other polyarthritides.
Confronted then with an acute polyarthritis of obscure nature marked by pain, redness, swelling, and pyrexia, what are the points necessary to establish it as being of gouty origin?
The sex and age should be noted, also the heritage, habits, and occupation. A history of previous attacks located in the big toe would be of prime value. The presence of a cardiac valvular lesion, while it would suggest a previous attack of acute rheumatism, would in no wise negative the possibility of the subject developing gout in later life. Here I may say that if the subject is over thirty-five and has never had acute rheumatism or acute gout, it is much more likely at his time of life that his acute polyarthritis is of gouty than of rheumatic origin.
As to the character of the pyrexia, it is usually of low grade; but if the condition be afebrile, it is even more suggestive of a gouty arthritis. But recollect, too, that the pyrexia in gonococcal arthritis is also of low grade or absent.
There is nothing distinctive of gout either in the character or distribution of the articular lesions. The ankles, knees, hands, wrists, are most commonly involved, much more rarely the elbows, shoulders, or hips. Naturally the local changes will differ according to the joint involved and the structures implicated; but these local variations in appearance, including œdema, may all be met with in any form of infective arthritis.
As to uric acid excretion, Osler, who was deeply interested in this type of arthritis, held that any lowering of the ratio of the uric acid to the urea excretion would be significant of gout. Also we should, as these cases of acute gouty polyarthritis are of the nature of successive paroxysms (“series et catena paroxysmulorum,” to use Sydenham’s expression), note any variations in the uric acid output ensuing pari passu with their rise and wane.
Last, but most important of all, a thorough search must be instituted for tophi, not only in the ears, but elsewhere. If anything could emphasise the indispensable rôle played by tophi in the diagnosis of gout, it would be our utter inability to effect in their absence a diagnosis of these acute types of gouty polyarthritis. The establishment of the existence in situ of such articular uratic deposits disposes forthwith of all possible doubts as to the true nature of the case; but if, as so frequently happens, the tophi when present are of ab-articular site, then we must withhold our decision pending the exclusion of certain other joint disorders, to the differentiation of which we now proceed.
The class of disorders that call for discrimination are those of infective origin. In the first place, acute articular rheumatism must be excluded; nor is it less necessary that we should eliminate gonorrhœal and syphilitic types; while, last, but not least, that vast group, the undifferentiated infective arthritides, is but too often a source of confusion.
Unquestionably many cases of acute gouty polyarthritis have been confounded with acute articular rheumatism, and vice versâ. Garrod on this point remarks: “That many cases of acute gout have been mistaken for acute rheumatism I do not doubt, and, on the other hand, that some few cases of acute rheumatism have been regarded as of a gouty nature I am no less certain. I may refer to the oft-quoted case related by Dr. Haygarth in which[270] gout was supposed to have been transferred from the extremities to the heart as an example of the latter error.”
It is only, of course, with that type of acute gouty polyarthritis accompanied by pyrexia, and not the afebrile variety, that confusion with acute articular rheumatism is possible. What then are the points of discrimination?
| Acute Articular Rheumatism. | Acute Gouty Polyarthritis. | |
|---|---|---|
| Age and sex | Most common between ages of fourteen and thirty. Predominance of males after twenty. | Maturity and old age. Males. Females markedly exempt. |
| Heredity | Very disputable. | Very pronounced. |
| Onset | Usually abrupt and often with tonsillitis. | Insidious, with premonitory gastro-intestinal symptoms. |
| General symptoms | High fever, sometimes hyperpyrexia. Profuse acid sweats. | Moderate pyrexia. Marked daily remissions. |
| Distribution of lesions | Preference for large joints and markedly mobile. | Small joints, hand or foot often involved. Fixity typical. |
| Local characters | Joints exhibit slight reddish flush. No subsequent desquamation. No residual change. | Scarlet hue and œdema with later peeling of cuticle and itching. Tendency to involvement of bursæ and tendons. |
| Pain | Chiefly evoked by movement. | Spontaneous, more intense. |
| Duration | Twenty to thirty days, sometimes longer. | Six weeks to three months. |
| Associated phenomena | Cardiac lesions common. | Tophi. Occasionally glycosuria and albuminuria. |
| Therapeutic test | Salicylates a specific. | Not so in gout, but colchicum takes this rôle. |
This disorder, as we know, is sometimes of oligo- or poly-articular distribution. Moreover, as the attendant pyrexia may be slight or absent, it may readily be confounded with the afebrile variety of acute gouty polyarthritis. Osier, discussing diagnosis of the latter condition, observes: “A patient with three or four joints red, swollen, and painful in acute rheumatism has fever,[271] and while pyrexia may be present, and often is, in gout, its absence is, I think, a valuable diagnostic sign.”
This is of course true, but it still remains necessary, for reasons above cited, to eliminate acute gonorrhœal arthritis. The tendency to such confusion has been emphasised by Sir Rose Bradford and Sir William Roberts, and I would urge the necessity of being alive to this possibility even in middle-aged men. One thing is certain, viz., we should be extremely chary of pronouncing any coincident urethral discharge to be a so-called “gouty urethritis”; nor should we translate any coincident conjunctivitis or iritis as further evidence of the articular affection being “gouty.” It is far more likely to be gonococcal. Apart from these inflammatory ocular affections, the relics also of previous attacks—viz., irregularity in contour or inequality in size of the pupils—have before now put me on the right track in obscure types of polyarthritis.
To sum up, the following are distinctive characters of generalised gonorrhœal arthritis:—
Etiology.—History or presence of urethral discharge and isolation of the gonococcus.
Onset.—Insidious, seldom acute.
General Symptoms.—Absent or slight relatively to extent and severity of joint mischief. Pyrexia, low grade or absent.
Distribution of Lesions.—Preference for large joints. Special liability of sacro-iliac, chondro-costal synchondroses, sterno-clavicular, tibio-fibular, and temporo-maxillary joints.
Local Characters.—Persistent passive effusion or peri-articular boggy swelling, with redness and local heat. No tendency to migrancy. Joint swelling very persistent.
Associated Phenomena.—Involvement of fasciæ, especially plantar, and of tendon sheaths, very distinctive, while coincident iritis or conjunctivitis is almost diagnostic.
The ease with which a subacute arthritis of this nature may be confounded with “gout” or “rheumatism” calls for comment. We have met with cases despatched to spas under this impression. The customary intermittent fever of secondary syphilis is usually present. The detection of periosteal nodes in addition to the joint swellings should arouse suspicion, while the presence of secondary syphilides and the rapid response to specific treatment will be confirmatory.
I well recollect some years ago a young farmer being sent to me by a medical man as suffering from gouty arthritis with gouty[272] eczema. The eruption was a typical roseola, and the condition promptly cleared up under anti-syphilitic treatment.
While the old term “rheumatic gout” still clings to this affection, it has now achieved its isolation from gout on the one hand and rheumatism on the other. The fact that it occurs in young women in whom gout never occurs, and has a very marked clinical facies of its own, should almost preclude the possibility of its being a source of confusion. Still, for the sake of completeness, we append its chief characteristics.
Age and Sex.—Most common in young women.
Onset.—More or less acute.
General Symptoms.—Continuous low grade pyrexia, quick pulse, and rapid emaciation, and commonly concomitant gastro-intestinal derangements.
Distribution of Lesions.—Polyarticular. Beginning in the small joints, it spreads centripetally, with a tendency to symmetry. No migrant trend, but a steady, progressive involvement of joint after joint, including temporo-maxillary and cervical articulations.
Local Characters.—Overlying skin of affected joint white or semi-asphyxial in tint. Contour spindle-shaped, but in terminal stages shrinkage from atrophy of articular structures sets in. Muscular wasting and contracture conspicuous features.
Associated Phenomena.—Trophic and vasomotor changes prominent, but no tendency to cardiac lesions.
It were well in approaching any acute polyarthritis of obscure nature to bear in mind the axiom that any or all infections may be complicated by arthropathies, also that if the said polyarthritis does not respond quickly to colchicum or salicylate of soda we are almost certainly dealing with an infective arthritis either of specific or undifferentiated type. The specific forms of infective arthritis, as far as seems necessary, have been dealt with, but those rarer forms not referred to, viz., influenzal, pneumococcal, dysenteric, meningococcal, etc., have also to be borne in mind, if the history reveal any recent occurrence of these disorders.
Still far more common than any of these are the acute infective arthritides of undifferentiated type. As we before remarked, an extraordinary general clinical resemblance obtains between these types of joint disorder and acute gouty polyarthritis. Indeed, in the absence of tophi, their differentiation is well-nigh impossible.[273] Even the blood picture in both types of the disorder is strikingly similar in the matter of leucocytosis and secondary anæmia.
Recently Dr. Henry A. Christian, lecturing at a clinic of the Harvard Medical School, emphasised this clinical similarity and the difficulty of discriminating between these two types of joint disorder. As he rightly says, “while there is a definite acute gouty polyarthritis (as evidenced by external tophi or deposits in bone or cartilage with variations in uric acid output) and also an equally definite infective arthritis, yet between those two there is a very considerable number of cases that present some of the factors suggestive of gout and other factors suggestive of an infectious arthritis, and there is where the difficulty comes.”
This is precisely the state of affairs, and one may well ask where gout ends and infection begins. Let us take an example. A man exhibiting tophi, the subject also of pyorrhœa alveolaris, develops an acute polyarthritis. What then is the nature of the joint disorder? There is a gouty element in his case, as attested by tophi, also an infective element, as evidenced by oral sepsis.
Now are we to regard such a case as one of infective arthritis of undifferentiated type occurring in a gouty subject, or are we to proceed on the assumption that the presence of tophi negatives the possibility of infection and forthwith to class it as a case of acute gouty polyarthritis of so-called metabolic origin?
This is no theoretical quibble. In the Royal Mineral Water Hospital, Bath, one constantly meets with cases in which the very elect would be puzzled as to whether they should be placed in the category of gouty or in that of infective arthritis. I have at present in my wards a middle-aged man, stout of body, rubicund of face, with well-marked auricular tophi and widespread arthritis. There are no tophi round his joints. On X-ray examination his phalanges show Bruce’s nodes, and his phalangeal joints show changes indistinguishable from those constantly met with in infective arthritides occurring in non-gouty subjects.
Indeed, this overlapping may proceed still further, the gouty and the infective characters neighbouring in such proximity as to suggest actual fusion, a community of origin. What else in truth can be the inference, when one meets with examples in which the peri-articular tissues are the seat of demonstrable uratic deposits, while the X-ray changes within the joint proper, the bone and cartilage, are typically those met with in infective arthritis?
Now, who will deny that if tophi were absent in such a case we should without hesitation hold the case to be one of infective arthritis? My own contention is that even in the presence of tophi the same appellation is indicated. In other words, I submit that acute gouty polyarthritis is itself but a form of infective[274] arthritis which derives its specific character from the associated uratic deposits.
As to differentiation of the latter from these cryptic infective arthritides, this will rest mainly on—
(1) The presence of tophi;
(2) A history of previous attacks in the great toe;
(3) A swift response to colchicum.
In addition, acute gouty polyarthritis is confined to middle-aged males, while no period of life is immune from infective arthritis, and both sexes are equally liable.
Again, acute gouty polyarthritis may be afebrile. Pyrexia when present is moderate in grade, its curve undulating as the paroxysms rise and wane. In infective arthritis the temperature curve is irregular and erratic.
Lastly, the uric acid output in acute gouty polyarthritis drops a day or two before the paroxysm, rises markedly after its inception, then sinks again. Also we may add that occasionally glycosuria or albuminuria is present.
In conclusion, I would allow myself a brief digression regarding these infective arthritides of undifferentiated type. They constitute the bulk of the cases of arthritis that find their way to the Royal Mineral Water Hospital, Bath, under one or other of the appellations “gout,” “rheumatism,” and “rheumatic gout.” It is within this category that most of the cripples met with at spas fall, and their obduracy to “drug” treatment accounts for their belated despatch thereto.
I would that I could sufficiently emphasise the imperative necessity of early recognition of the true nature of these cases. Colchicum is a most valuable drug, and so is salicylate of soda. But they have their limitations. They act swiftly or not at all. Persistence with them in the absence of any response is worse than futile: it is definitely prejudicial. Because of our unreasoning devotion, our almost fetishistic addiction, to these drugs, I often feel that these agents, especially salicylate of soda, have made more cripples than they have saved. For, unfortunately, unqualified reliance on these drugs is apt to blind us to the surgical necessities of these cases. Foci of infection pass unnoticed, joints stiffen at unfavourable angles, and not infrequently a potential bread-winner is lost.
I make no apology for this digression, for it is, strictly speaking, wholly apposite, this in view of the fact that failure of quick response to the action of colchicum or salicylate of soda, say within a week, speaks in favour of the infection having ensued in a non-gouty as opposed to a gouty subject.
If the diagnosis of acute types of articular gout often presents difficulties, these same are, if anything, accentuated when we approach its chronic manifestations. For, apart from uratic deposits, the anatomical lesions that ensue in joints the seat of long-continued gout have no specific character. In short, there is nothing pathognomonic of gout in the changes produced, and which, as a matter of fact, we know to be capable of production, by many different morbid agencies. Surely this lack of specificity in its structural lesions should make us very chary of admitting to the category of chronic articular gout any examples of arthritis destitute of uratic deposits.
In our chapter on classification we emphasised the desirability of restricting the usage of the term chronic articular gout to that type long since known as tophaceous gout, this because there is little, if any, doubt that that variety known as chronic deforming gout (syn. arthritis deformans uratica) is largely made up of examples of rheumatoid or atrophic arthritis and hypertrophic arthritis or osteoarthritis.[41]
As to osteoarthritis, I do not for a moment deny that uratic[276] deposits may be met with in its victims. One frequently meets with patients, the subjects of osteoarthritis of the hip, who at the same time exhibit tophi in the ears.
But such to our mind are to be regarded as merely instances of osteoarthritis occurring in subjects of “gouty diathesis.” This apparent blending of the two disorders must not be allowed to impair the clarity of our conception as to the essential distinctness of gouty arthritis and osteoarthritis.
Sir W. Hale White has some pregnant observations on this point. Many patients, he says, “with chronic arthritis are quite wrongly said to have gout; usually they have osteoarthritis. The presence of bony outgrowths is strongly against gout, though it is not conclusive, for such may occur in true gout either more or less all round the joint or in the form of little nodules, but they never attain the considerable size common in arthritis,” and he adds: “If no urate of soda is visible anywhere the diagnosis may be very difficult.”
To proceed, the general and local phenomena of chronic articular gout are such as scarcely lend themselves to succinct definition, and for their description we would refer the reader to the chapter dealing with its clinical aspects. As that careful observer Sir Alfred Garrod states: “Chronic gout is at times confined to one or two joints, but sometimes numerous articulations are involved.” In other words, chronic articular gout may be mono-, oligo-, or poly-articular in distribution; and naturally the process of differentiation is modified accordingly.
This being so, I purpose dealing in the first instance with chronic monarticular gout, and in succession with the types of oligo- and poly-articular location.
Occasionally gout in its recurrences clings obstinately to the great toe and tarsal joints. But since the advent of radiography there should be little or no difficulty in differentiating a chronic gouty arthritis of the great toe from the only other arthritic lesion with which it is likely at this stage to be confounded, viz., osteoarthritis. But at the same time we would refer the reader back to the chapter dealing with the differential diagnosis of the localised variety of acute gout, as therein we dealt fully with other possible sources of fallacy, i.e., static deformities, etc. We shall therefore now proceed to discuss those exceptional cases in which chronic gout is located not in one of the small, but in one of the larger, articulations.
Given a chronic arthritis of one of the larger joints, say the ankle, knee, or elbow, we should be careful not to jump too readily to the conclusion that it is of “gouty” nature. The more obscure it appears the more need for caution. Needless to say, if the objective changes be but minimal and the condition be, so to speak, practically a mere arthralgia, there rests upon us the paramount necessity of careful discrimination before labelling it as “gouty” in kind.
Thus, if it be the knee, it may be a referred pain due to hip disorder, e.g., osteoarthritis or tuberculous disease, or it may be symptomatic of an inflammatory process, or, having regard to the usually mature or advanced age of the subject, it may be a neoplasm in the bones.
On the other hand, suppose the subject come complaining not much of pain in his joint, but more troubled because of its enlargements. If now on examination we find also that there is little or no tenderness, but simply a condition of peri-articular thickening or intra-articular effusion, what shall be our method of procedure? Certainly not to leap forthwith to the conclusion that it is gouty. No, not even if he exhibit tophi in his ears.
Now, as to pain and tenderness, it is a blessed feature of gouty arthritis that, generally speaking, in the chronic forms pain becomes much attenuated. But let us at the same time recollect that syphilitic arthritis, both secondary and tertiary, is relatively painless. But it is the much rarer tertiary form, be it remembered, which is usually monarticular. By the bye, too, we should never forget that a Charcot’s joint is also painless.
Coming now to the objective phenomena, is the case predominantly one of peri-articular infiltration or intra-articular effusion? As to the former, while you never know, still tuberculous joint disease is exceptionally rare at the age at which we usually meet gout. On the other hand, gummatous synovitis, with or without osteoperiostitis, is occasionally met with. It is just such a case as this that may be confounded with gout, the irregular lumpy thickening of the sub-synovial tissues with effusion being wrongly attributed to a gouty process with uratic deposits. Do not be misled if a history of injury be forthcoming in such cases, for it is not uncommon and may be given in good faith.
Now what if synovial effusion of chronic or recurring form be the striking objective feature of the case under review? In this event always recollect that of all the causes of monarticular disorder injury is far and away the most frequent. Not a few cases of monarticular joint disease come annually to the Royal[278] Mineral Water Hospital, Bath, under the diagnosis of “gout” and “rheumatism.” But in all too many the symptoms are referable in truth to ligamentary strain, displaced cartilage, or foreign bodies, lesions always to be sought for and excluded in monarticular joint affection. Duckworth has it that hydrarthrosis is met with in chronic articular gout, in his deforming variety. He states that “hydrarthrosis is less commonly due to gout than to rheumatism,” but, we would remark, apart from traumatic lesions, more commonly due to gonorrhœa or syphilis than to either of them.
But the reader may say, this dissertation notwithstanding, Where does gout come in? Precisely so, and if his experience tallies with mine, he will find that chronic articular gout localised in one of the larger joints, and one only, is exceptionally rare. Personally, I should never feel justified in making the diagnosis unless I had elicited a history of (1) recurring classic outbreaks in the great toe with (2) an absence of traumatic infective and nerve arthropathies and, on the other hand, (3) demonstrable existence of uratic deposits in situ in the peri-articular tissues, the cartilage or bones as revealed by skiagraphy, or in the related bursæ.
In conclusion, if all these various pitfalls have been avoided, it will almost without exception be found that the final differentiation in doubtful cases will rest between gout and osteoarthritis; and in the vast majority, I had almost said all, it is the latter morbid process that will be found responsible.
This all too lengthy disquisition will not have been in vain if it instil caution. For it is in the monarticular types of joint affection that errors of catastrophic proportion occur more commonly than in any other form of joint disorder.
The course of chronic articular gout, as has been observed, may be chequered by acute outbreaks involving three, four, or more of the larger joints. But, apart from this, there are those so-called asthenic and afebrile types of gout in which two or more joints may be the seat of a chronic gouty arthritis. In my experience it is the knees that are most frequently attacked. The joints are enlarged, the seat of more or less effusion, but the distinctive feature is the presence of deformity due to the irregularly rounded or ovoid swellings produced by uratic deposits. Enlargement of the patellæ is also present, and they lose their sharp edges, and sometimes they as well as the neighbouring articular ends are studded with small bony outgrowths, but of minimal size compared with those met with in osteoarthritis. The related bursæ, too,[279] are often the seat of deposits, a valuable clue to diagnosis. Needless to say, such marked cases are nearly always the outcome of oft-repeated attacks, the ultimate deformity being the result of successive accretions of urate of soda laid down in the trail of the exacerbations.
The frequency with which this misconception occurs is very noticeable. If a middle-aged woman of florid complexion and corpulent habit begins to complain of pain and stiffness in her knees with more or less swelling thereof, there is a very prevalent tendency to attribute not only her joint disorder to gout, but any gastric or nervous symptoms that she may simultaneously complain of are translated as being confirmatory of the assumption. It gathers weight too from the traditional and widespread belief that “the change of life” is the period par excellence at which women develop the morbid vagaries associated with “irregular gout.”
Now, as Bassett Jones and I have pointed out in a previous work, this condition, symmetrical villous synovitis of the knees, is a very common joint disorder in women at or near the menopause. Frequently they give a history of numerous pregnancies, or of rapidly increasing obesity, while with or without this latter they display a faulty postural attitude, indicative of lowered muscular and ligamentary tone. Following in the wake of these, the subject develops a symmetrical flatfoot, which, according to the stage at which it is seen, may be of flexible or rigid type.
Now, such is the mutual static interdependence of the component parts of the lower limb that this condition of flatfoot promotes or favours the incidence of villous overgrowths in the proximal joints, the knees. As to the modus operandi we have put forward the following explanation: “The everted foot, with its sunken arch, as before stated, determines an alteration in the normal coaptation of the articular surfaces in the knee, and this incongruence is revealed in skiagraphs by the marked prominence laterally of the external tibial tuberosity beneath the external femoral condyle. Coincidently, and for the same reason, additional strain is thrown upon the internal lateral ligament. This in turn favours a state of passive congestion or hyperæmia of the synovial membrane, which becomes relaxed and thrown into folds, especially at its reflexions near the edges of the cartilages. If, as often happens, the individual is the subject of varicose veins or suffers from a general lack of tone in her muscular or ligamentary structures, this tendency to venous engorgement of the knees is much enhanced.”
“Under the influence of these mechanical factors and their associated circulatory disturbances, thickening and enlargement of the synovial fringes ensue. The inflammatory condition thus produced tends to increase automatically, as, owing to the articular incongruence, the enlarged fringes are very prone to become caught between the joint surfaces; in other words, a vicious circle is produced, as with the increasing villous hypertrophy the liability to internal traumatisms increases pari passu.”
In short, the joint disorder is fundamentally of static or mechanical origin, and, this being so, the results of anti-gouty treatment are open to a further misinterpretation. The victims, as we have said, exhibit very generally a tendency to obesity. Now, Ebstein and many others hold the view that obesity and gout have affinities. Ebstein, moreover, believes that treatment directed to the reduction of body weight will check the appearance of gouty arthritis or ameliorate the same when avowed. What happens is this: these corpulent subjects are placed on a special dietary. Hydrocarbon foodstuffs are limited, bread, amylaceous food and liquids being also restricted. Naturally, pari passu with reduction in their body weight, their overburdened joints become more equal to their office. But those who assume that the chronic arthritis is of gouty origin attribute, and, we think, wrongly, the beneficial results attained to correction of the underlying “gouty” habit.
We prefer to subscribe to the simpler or mechanical theory, and in view of the widespread and, as we believe, erroneous belief in the gouty nature of this arthritis, we take the liberty of appending the salient features of these cases, while adding further a few remarks on the differential diagnosis of other symmetrical affections of the knees which may also be wrongly attributed to gout.
The onset is gradual and insidious. Stiffness is the salient symptom, but sometimes the subject is more distressed by a sense of weakness, distension and unreliability. Pain is slight or absent, save when during walking pseudo-locking occurs. The mobility of the joints is usually unimpaired, and if any limitation exist it is the power of full extension that is usually restricted.
Objectively the joint shows either general enlargement or swelling localised to the supra- or infra-patellar regions. Intra-articular effusion which comes and goes is a very characteristic feature. On palpation a peculiar soft silken crepitus will be heard[281] and felt as the patient alternately flexes and extends the limb. The enlarged fringes are also easily to be felt as knots or nodules which can be moved up or down on the underlying bone. The ease with which they can be appreciated depends upon the degree of effusion present at the time. Judging from their symptomatology, it seems probable that some of the cases included in Sir Dyce Duckworth’s category, chronic deforming gout, are of this description.
The diagnosis of villous synovitis should not be considered complete without skiagraphy being undertaken to reveal or exclude osteophytic outgrowths. For the subjective symptoms and signs of early osteoarthritis are practically identical with those of villous arthritis, and although the presence of osteoarthritic lesions elsewhere would be suggestive, skiagraphy alone will enable us to effect a differentiation with certainty. Indeed, Bassett Jones and myself are strongly of the opinion that the life history of osteoarthritis involves two stages: (1) a primary or pre-osteophytic phase, often of prolonged duration, whose clinical characteristics are those of villous hypertrophy; (2) a secondary or terminal stage, in which bony and cartilaginous outgrowths make their appearance.
Other symmetrical disorders of the knees that may be wrongly ascribed to gout are hydrarthrosis and gummatous synovitis.
Bilateral Hydrarthrosis.—Given effusion into both knees which is passive, copious, and persistent rather than recurrent, then its possible infective origin must be carefully canvassed. The common sources are gonorrhœa, syphilis, and tubercle. The history or presence of an urethral discharge and detection of the gonococcus will identify the first named. In syphilis the existence of other lesions, the response to Wassermann’s test and specific treatment are the points on which to rely, and in tubercle, the detection of visceral foci and the sero-reaction will give the clue.
As to the intermittent type of hydrarthrosis, the remarkable periodicity in incidence of the effusion will suffice to obviate any possibility of confusion.
Peri-synovial and Peri-bursal Gummata.—Affecting as they do commonly the knee joints of adults, these may, in the absence of a history of infection, be a source of error. The uneven and nodular swelling may quite easily be confounded with uratic deposits. Pain is slight and mobility but little impaired. The presence of neighbouring scars, a positive Wassermann reaction, and a favourable response to anti-syphilitic therapy will clear up the diagnosis.
The clinical portrait of tophaceous gout when of widespread distribution is one of the most striking to be met with in the whole domain of medicine, but for the broad outlines of the picture presented we would refer the reader to the chapter dealing with the clinical description of chronic articular gout.
In these polyarticular forms the most distinctive joint deformities are those met with in the hands or feet, more particularly the former. The excrescences produced are the outcome of successive uratic deposits. These latter when massive can scarcely be confused with any other disorder, for the superjacent skin, distended by the ever-increasing underlying uratic deposits, becomes thinned and purplish red in hue, and occasionally ulcerates. I have at present in my wards a case of this nature, and the subject hoards up the exuding “chalk” in a small bottle.
Fortunately such marked examples are relatively rare, though easily recognised; but it is the less marked types that occasion difficulty in diagnosis. The point at issue of course is the differentiation of moderate-sized or small tophaceous swellings from bony outgrowths. Frequently the task is impossible of achievement without resorting to puncture, when, if anything can be withdrawn, microscopic examination may reveal the presence of biurate crystals.
For the rest, attention to the following points will prove helpful in enabling us to differentiate clinically between gouty arthritis and other chronic joint disorders attended by deformities:—
(1) Tophi when of recent incidence are soft, and when of long standing are never so dense or so hard as bony outgrowths.
(2) The overlying skin is thin, and through its substance the subjacent white concretions may sometimes be discerned. It may be adherent, or the seat of ulcers.
(3) Uratic deposits are not located exactly at the level of the articulation. They do not adapt themselves to the contour or shape of the bone-ends.
(4) Unlike osseous growths, they may be slightly movable in lateral directions.
(5) Tophi may soften or disappear after exacerbations of arthritis.
The conditions likely to be confused with chronic polyarticular gout are osteoarthritis, rheumatoid arthritis, and the multiple[283] arthropathies met with in affections of the central nervous system.
Its chief characteristics may be summarised as follows:—It is a disease rarely met with under forty years of age. The mode of onset is generally insidious, never really acute. In this respect it contrasts with gout, the initial outbreak of which is invariably acute. Osteoarthritis attacks both sexes equally. Although it may be polyarticular, its specific tendency is towards a mono- or, more accurately speaking, oligo-articular distribution, with no marked leaning to symmetry. It has a pronounced predilection for attacking the hip, the shoulder, and the spine—sites rarely, if ever, attacked by gout.
Unlike gout, constitutional symptoms, pyrexia and so forth, are generally absent; muscular atrophy is slight, hardly ever pronounced, likewise muscular spasm and contracture.
These are best appreciated in the small joints of the hand. Osteoarthritis has an affinity for terminal joints—the so-called Heberden’s nodes. Another favourite site is the carpo-metacarpal joint of the thumb, while the preference of gout is for the metacarpo-phalangeal joint thereof and for the same articulation in the other digits.
The overlying skin, as a rule, is unchanged, and never assumes, as in gout, a dusky red or purplish hue. The margin of the articular surfaces, instead of being smooth and rounded, is broken and irregular, its nodular contour being due to osseous outgrowths studding the line of junction of the bones entering the articulation.[42]
In this respect they contrast with tophi, which are located near to, but not at, the level of the joint fissure. Again, unlike tophi, bony outgrowths are fixed, immutable, undergoing no change save in the direction of progressive enlargement. While the tendency of an osteoarthritic joint is to expand and increase, still the enlarged and gnarled joints never attain the colossal bulbous appearance presented by inveterate examples of tophaceous gout.
This affection differs from the foregoing disorder as well as gout in that it is most commonly met with in persons under forty years of age. Moreover, it attacks women much more frequently than men. Of polyarticular distribution, it evinces a marked tendency to symmetrical invasion. Like gout, it has a pronounced preference for the smaller joints, while, similarly, it avoids the hip and shoulder.
Constitutional symptoms are conspicuous: pulse quickened, temperature raised, extreme wasting not uncommon. Intense and widespread muscular atrophy with contracture is a prominent feature, also trophic disturbances of varied nature and degree.
In early stages the skin over the joint is waxy white or semi-asphyxial in tint, outline of joint smooth, rounded, and spindle in shape, with, as a rule, no irregular bony projection at the level of the articulation. If seen at a later stage, the swollen joint will be found shrunken from atrophy of all the articular structures as well as the skin. Ultimately it becomes reduced even below its normal size, the small “end-joint” of atrophic or rheumatoid arthritis. The deformities due to muscular spasm are usually in the direction of luxation and hyperextension, and differ from those of gout and osteoarthritis, in which there is more generally lateral displacement.
The joint disorders incidental to tabes and syringomyelia do occasionally find their way to spas for treatment under the mistaken conception that they are instances of “gout,” “rheumatism,” or “rheumatic gout.” In the case of tabes the mistake is often referable to the confounding of its lightning pains with “gout” or “rheumatism,” with subsequent relegation of the swollen joints, whether single or multiple, to one or other of these categories. In the syringomyelic it is, I think, the close resemblance that obtains between the joint lesions and those of osteoarthritis or so-called “rheumatic gout” that accounts for their uncalled-for and utterly useless transference to spas. I have known a case of syringomyelia with multiple arthropathies in the hands sent to Bath under the mistaken idea that they were of “gouty” origin.
These remarkable joint affections will be distinguished by their[285] fulminant onset with marked effusion and absence of pain, tenderness, and heat. In addition, associated phenomena will be present, viz., ataxic pupillary changes and lost knee-jerks in tabes, while syringomyelia is characterised by dissociated anæsthesia, trophic disturbances of bones, progressive muscular atrophy with paralysis.
It will be recalled that Rieken held the view that so-called “bleeders” were prone to attacks of gout, and that sometimes these alternated with intra-articular hæmorrhages. Nor was he devoid of supporters, for Sir Dyce Duckworth maintained that a definite hereditary relationship obtained between gout and hæmophilia, while that astute observer Jonathan Hutchinson also contended that the vascular weakness was the outcome of gout and aggravated by serial hereditary transmission. Wickham Legg, however, in his masterly contribution questioned the correctness of Rieken’s proposition.
Personally, I cannot out of my own experience confirm or rebut the view that “bleeders” come of gouty stock, nor have I ever met an avowed gouty subject who was likewise the victim of hæmophilia. Quâ its joint complications, hæmophilia to our mind would appear to display closer affinities with peliosis rheumatica than with gout; but, in view of Duckworth and Hutchinson’s claims, it were wiser on our part to withhold judgment, while paying them the deference of being alive to the possibility of there being some obscure connection, though not proven, between the two disorders. Again, as emphasising the necessity for discrimination, we would draw attention to the fact that Konig recognised three stages in hæmophilic arthritis: (1) hæmarthrosis; (2) an inflammatory process, with pyrexia and spindle-shaped swellings apt to be confused with tuberculosis; (3) extensive arthritic changes reminiscent of arthritis deformans. Confusion with gouty arthritis clearly is only likely in the second or third stages, and in the matter of diagnosis the personal and family tendency to hæmorrhages is the most important clue.
As an aid to the differentiation of gouty from non-gouty forms of arthritis skiagraphy has scarcely fulfilled the somewhat optimistic claims at one time made on its behalf. As to acute gout, radiography reveals nothing abnormal in the bones, though Tousey holds that this of itself at once enables us to exclude osteomyelitis, which, he says, “these cases sometimes resemble.”
Turning now to chronic articular gout, Huber in 1896 drew attention to certain focal areas of rarefaction, or diminished density, in the distal extremities of the phalanges. These localised transparent areas in the bone-ends are discrete, circular, or oval in shape. When located near the edges of the bones, they are of segmental contour, and, viewed in profile, give the appearance of small punched-out holes, simulating syphilitic dactylitis. Despite their proximity to the diseased joints, they apparently do not communicate with the articular cavities.
These bony changes Huber held distinctive of gout, and Koehler, Drinberg, and Jacobsohn and other subsequent writers confirmed Huber’s findings, and, like him, held these areas of rarefaction to be the result of uratic deposits at their sites. Strangeways has dissected bones in which these transparent areas were demonstrated by X-rays. The examination revealed that the bone was definitely excavated, filled with a gelatinous-looking substance, and in advanced cases of gout, moreover, a characteristic deposit of urates clung, as it were, to the margins of the cavities.
Similar focal areas of decreased density were noted by Strangeways in certain cases of rheumatoid arthritis, and both he and Burt found it impossible on the X-ray findings to differentiate between these and gout, i.e., without invoking the aid of clinical data.
Radiographs of the Foot and Hand, showing extensive bony and other changes in long-standing Gout.
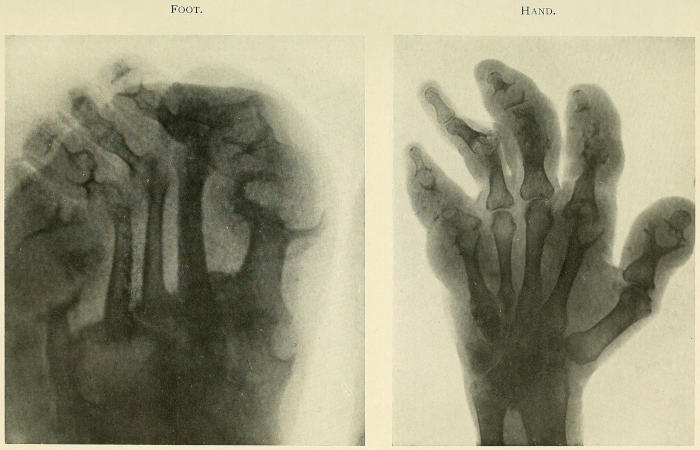
Apart from these transparent areas, Wynne many years ago pointed out that small nodes or bony deposits are sometimes met with flanking the sides of the phalanges. More recently Ironside Bruce by radiography has again drawn attention to these bony outgrowths near the extremities of the phalanges (Bruce’s nodes).[287] At first these were thought by Bruce to be composed of urates, but Strangeways from a study of macerated specimens has demonstrated their true bony nature, and also that uratic deposits are not opaque to X-rays, as was formerly thought.
In skiagrams of chronic gout all stages of ankylosis may be seen in the interphalangeal joints. In some it is merely fibrous, in others merging therefrom into bony, and not infrequently true synostosis is observed. Deflections or subluxations are frequent features, due either to the thrust of tophi or small bony outgrowths or to peri-articular contractures.
So much for the skiagraphic findings in chronic gout, and now to discuss their valency as aids to diagnosis of this arthritic disorder. The chief controversy centres around the significance of the focal areas of rarefaction which have been found in the bones of the wrists, hands, ankles, and feet of gouty subjects. Here we may comment on one grave handicap, viz., the lack of certainty as to whether the cases radiographed by different observers were true instances of gouty arthritis.
To justify our expression of doubt we may take, for example, the series reported by Drinberg and Jacobsohn. The said “transparent areas” were present in all the eighteen cases, but the presence of tophi was only established in three. Now, as McClure and McCarty rightly contend, “since the tophus is the only universally accepted pathognomonic sign of gout, for studies of that disease only those patients should be chosen in whom tophi are found, and sodium urate crystals from them microscopically demonstrated.” No one can, I think, gainsay the legitimacy of this stipulation.
In accordance with their contention, McClure and McCarty record their radiographic findings in a series of cases all of which exhibited tophi, and from which sodium urate crystals were isolated. Now, in all these cases the focal areas of diminished density, generally held to be peculiar to gout, were present; but they add that “similar changes were present in two other cases which were clinically gout, but in which no tophi were demonstrated.” Also “in another case without tophi, but which was clinically gout, the focal areas of decreased bony density were not found.”
In addition, they examined the skiagrams of 100 cases of chronic arthritis which “had not been diagnosed clinically as gout.” In thirteen of the examples “the focal areas of decreased density, the so-called gouty bony changes, were found, and were fully as well defined as in the cases of true gout.”
Judging from the skiagraphic appearances, there seemed no reason to suppose that the factors responsible for the production[288] of these rarefied areas were in any way different from those at work in true gout. Now, most authorities have claimed that the bony changes were due to uratic deposits in the bones; but it is at least possible that their origin may be otherwise explained.
Thus Nichols and Richardson have shown that, given focal absorption of lime salts, changes apparently identical with those currently attributed to the presence of tophi may result. These same, though they may not be demonstrable either macroscopically or microscopically, are detectable by X-rays.
Such foci of absorption, viz., areas of decreased density, frequently are located in regions subjected to pressure. Thus they may occur at the inner surfaces of the heads of the first metatarsal bones, or they may form underneath large tophaceous deposits in the soft tissues.
Now, Strangeways has shown that it is impossible by radiography to detect tophi in bones. Accordingly we have at present no means of deciding in any given case whether the localised transparent areas in the bones are due to tophi or to focal absorption of lime salts. If we are to cling to the conception that they are due to tophi, then it is clear that tophi in the bones are more common than is currently suspected, and that, ergo, the frequency of gouty arthritis is underestimated. For these transparent foci in bones, according to McClure and McCarty, occur in from 10 to 12 per cent. of cases of chronic arthritis “which clinically are not gout.”
Yet these authorities hold that, despite the fact that they occur in cases of non-gouty arthritides, they have some diagnostic significance. For, taking the work of other observers in conjunction with their own observations, they come to the following conclusions:—
(1) The focal areas of decreased density, heretofore considered as peculiar to gout, are rarely absent in that disease.
(2) Their absence would be some evidence against the existence of gout in a given case.
(3) On the other hand, their presence is no more than suggestive of gout, since they are found in from 10 to 12 per cent. of cases which clinically are not gout.
(4) The focal areas of decreased density, usually held due to tophi, are probably very often merely focal areas of absorption of lime salts.
In continuation these authorities have endeavoured to identify the nature of the arthritis that occurs in gout. Like other workers in this sphere, the study of the radiographs obtained of gouty joints reveals that a variety of changes occur in the bones and[289] joints of the hands and feet in gouty subjects. These, they consider, may be classified conveniently as follows:—
(1) Cases marked by focal areas of rarefaction, without any other perceptible change;
(2) Cases presenting, in addition to these translucent areas, minor degrees of lipping at the articular margins;
(3) Cases in which the changes in (1) and (2) are conjoined with either localised atrophy of the bones entering into an affected joint, or with generalised atrophy of all the bones in the affected limb;
(4) In addition to all the above changes, narrowing of certain joint spaces with marked proliferative and atrophic changes occurs.
In reviewing these findings of McCarty and McClure, it is important to recollect that they were found in a series of cases all of which exhibited tophi. Moreover, it will be seen that the radiographic changes in some are reminiscent of atrophic or rheumatoid arthritis, in others of hypertrophic arthritis or osteoarthritis, while, lastly, the appearances typical of infective arthritis are also represented. In addition, if we recall that focal areas of rarefaction, indistinguishable from those met with in gout, also occur in all types of non-gouty arthritis, we at once see how impossible it is to detect anything in the radiographic findings distinctive of gouty as opposed to non-gouty arthritides.
McClure and McCarty, comparing the radiographic changes in gouty as opposed to non-gouty arthritis, observe that, though rarefactive foci occur in all varieties of non-gouty arthritis, they are conjoined with other bony or joint changes. On the other hand, translucent areas unassociated with any bone or joint alterations have been found only in gout. But whether this can be claimed as distinctive of gouty arthritis is, they think, uncertain, since relatively few opportunities for X-ray examination of non-gouty arthritis in its early stages have been forthcoming.
Continuing, of their four radiographic types of gouty arthritis the second resembles osteoarthritis; but the third and especially the fourth group, they consider, “fall into a peculiar class,” this inasmuch as their characters resemble the infective type of non-gouty arthritis. They claim, however, that a differentiation, radiographically speaking, can be effected, this because of the “sharply localised” extreme degree of bony atrophy which occurs in the infective type of non-gouty arthritis. However, as they admit that radiographs of the latter (infective non-gouty arthritis) have been noted which “closely resemble” the “atrophic and proliferative changes occurring in gout,” their final conclusion is that in the skiagrams even of typical gouty arthritis there is[290] nothing in the bony or arthritic changes that is diagnostic of gout.
For myself, I must admit that I have come to the same conclusion as McClure and McCarty, viz., that the skiagraphic findings in gouty and non-gouty arthritis trench so much the one upon the characters of the other that I should be loth indeed to base a diagnosis of gout simply on the revelations of skiagraphy. The chief interest to my mind, as I have previously observed, centres round those examples in which peri-articular tophi are associated with underlying bony and arthritic changes (as revealed by X-rays) indistinguishable from those typical of infective arthritis of non-gouty type.
We have seen also that local foci of rarefaction may be met with in infective arthritis of non-gouty type. Moreover, the proliferative and marked atrophic bony changes found in some instances of gouty arthritis are quite compatible with their infective origin. Witness how impossible it is to differentiate skiagraphically between atrophic arthritis and gouty arthritis, and at the same time let it not be forgotten, on the other hand, that the dividing line between the infective arthritides and the more acute forms of atrophic or rheumatoid arthritis is by no means sharply defined. Review this also in light of the fact of the close resemblance that obtains between acute articular gout, especially the polyarthritic variety, and types of arthritis of avowedly infective origin, and we see at once how close is the clinical similitude. We turn to radiography, and here again we are met with the same family resemblance, suggestive of a probable community of origin. How clear then the inference that it is on tophi, and tophi alone, that we must base an absolute diagnosis of gouty arthritis. Moreover, since tophi are not detectable by skiagraphy, our mainstay must be physical examination directed to their detection. As for those cases of so-called “clinical gout,” viz., unattested by tophi, it is probable that their absolute identification, as such, will never be attainable on purely clinical, but on bacteriological, data, which, it is to be hoped, will before long be forthcoming.
Infective Arthritis.—According to Goldthwait, of Boston, no changes can be detected by skiagraphy in bone or cartilage in infective arthritis. The density of the former is in no way diminished, while the cartilage retains its normal thickness. If, however, the infective arthritis is of destructive character, new bone may be thrown out in the process of repair. If then in such cases sole reliance be placed on the X-ray appearances without any reference to the clinical history and course of the disorder,[291] then, as Goldthwait says, this irregular formation of bone is likely to be confused with the X-ray findings in osteoarthritis. It is, however, possible, according to him, to distinguish the nature of the case by careful scrutiny of the skiagraphs.
The new formation of bone in these destructive forms of arthritis conforms in every way to that seen as a result of septic osteitis or periostitis. In other words, the osteophytic outgrowths take origin at the focus of infection, wherever that may be, and not, as in gout and osteoarthritis, at the margin of the cartilage. Still one must recollect that in gout exostoses (Bruce’s nodes) develop sometimes at the sides of the phalanges. These outgrowths are not peculiar to gout, but may be met with in infective forms of arthritis. I am inclined therefore to refer their origin to a local osteitis or periostitis of infective source. That Bruce’s nodes, though not diagnostic of gout, are frequently met with therein, is, I submit, but further evidence of the intrusion of an infective element in the genesis of gouty arthritis.
Hypertrophic or Osteo-arthritis.—This is marked by proliferative changes at the margins of the articular ends of the bones. With the advance of the disease the shafts of the related bones become increasingly dense. In chronic gout, too, the margins of the cartilages may be studded with little nodules. Radiographically speaking, they cannot be distinguished from those met with in osteoarthritis, save only that they never attain the massive size met with in the latter disorder. The diagnosis in doubtful cases will practically always rest on the clinical history, and more pertinently on the presence of tophi.
Rheumatoid or Atrophic Arthritis.—If the changes in the cartilage and bone in osteoarthritis are active and proliferative, these same in rheumatoid arthritis are retrograde and passive in character. In short, hypertrophy of these structures in the former, atrophy in the latter, constitute the distinguishing features.
The morbid process in the articular ends in rheumatoid arthritis is one of rarefaction and softening. The cartilage may undergo total or partial absorption, a change to be detected in the very early stages. The bones participate in the pathological change, the first evidence of which is an abnormal translucency to the rays, usually, but not always, confined to that portion of the shaft entering into the joint. Eventually the articular ends of the phalangeal and metacarpal bones may undergo erosion, in some cases to a very marked degree, the bones more or less telescoping into each other.
Now, owing to the fact that in gout also considerable disintegration of the bone may result, the appearances in some instances may resemble those found in the skiagraphs of rheumatoid[292] joints. Stress has been laid on this similarity by Strangeways, and it was also previously remarked by Goldthwait. The latter, however, claims that while in atrophic or rheumatoid arthritis the bone, though thin, maintains its outline, on the other hand in gout the outline of the bone is not distinguishable owing to its more complete destruction by the morbid process. Goldthwait holds that the resemblance of chronic articular gout to rheumatoid arthritis is most noticeable when the articular ends of the bone in both instances are the seat of the disease. In other examples, however, the shafts of the bones being affected by the gouty disorder, they may show punched-out areas. These latter, however, are but focal areas of rarefaction seen in profile, and inasmuch as they may be met with in infective arthritides of non-gouty type, too much reliance cannot be placed on their presence as distinctive of gout, much less as a criterion of differentiation from other arthritides.
We have to remember, too, that marginal proliferative changes may occur in rheumatoid arthritis. They are, like those met with in gout, miniature replicas of the bony outgrowths of osteoarthritis.
In conclusion, the resemblance between the skiagrams of chronic gout and rheumatoid arthritis is so close as absolutely to forbid our sole reliance on skiagraphy to effect a differential diagnosis. In short, skiagraphy, though of great and probably increasing value, cannot for one moment be allowed to usurp the place of careful clinical observation, to which it must be held always subsidiary. Last, but not least, pending fresh radiographic revelations, our diagnosis of chronic articular gout and alike its differentiation from rheumatoid arthritis and other arthritides must rest on the one unimpugnable criterion, the presence of tophi.
“It is not a sacred disease. There will therefore be no profaneness in handling it freely,” affirmed Benjamin Rush of gout some hundred years since.
Nevertheless one approaches with diffidence this debatable ground, so hedged in by high sanction and tradition. Albeit reverence for authority must, in the interests of progress, be tempered by that spirit of inquiring scepticism which would sift the chaff from the grain, this the more emphatically in that of all morbid conditions “irregular” gout, by the very vagueness of its clinical content, lends itself the more easily to unbridled inference, hazardous conjecture, and fanciful surmise.
As for the unlicensed freedom too often exercised in relegating disorders to this category, Rush would appear to have out-heroded Herod, pace the following rhetorical reflections, for they could scarcely rank as clinical observations. “The great toe and the joints of the hands and feet are no more its exclusive seats,” said Rush, “than the stomach is the throne of yellow fever. In short, gout may be compared to a monarch whose empire is unlimited. The whole body crouches before it.... The gout affects the glands and lymphatics. It produced a salivation of a profuse nature in Major Pearce Buller, which continued for two days. It produced a bubo in the groin in a citizen of Philadelphia. He had never been infected with the venereal disease. Of course no suspicion was entertained by me of its being derived from that cause.... Scrofula and all the forms of dropsy are the effects in many cases of a disposition of the gout to attack the lymphatic system.... A distressing collection of air in the rectum, which renders frequent retirement from company necessary to discharge it, is likewise a symptom of gout.”
It is difficult to conceive that any such pronouncement could have emanated from a physician of Rush’s standing and repute, a contemporary, be it noted, of Heberden, to whose masterly commentaries on the history and cure of gout all posterity is indebted. Nevertheless as recently as 1854 Sir Spencer Wells claimed that “any attempt to describe the nervous diseases of[294] females caused by gout would lead to an enumeration of almost all forms of their diseases, especially those usually considered as hysteric. The intestinal derangements with tympanitis, neuralgia, or colic, the hysteric pain in the right epigastrium, the cardialgia and gastrodynia, the hysteric vomiting and epigastric spasms, the morbid sensibility of the pharynx and fauces, hysterical palpitation, asthma or bronchitis, loss or alteration of the voice, some forms of hysteric paraplegia or hemiplegia more or less complete, chorea or tetanus, some of the curious paroxysmal affections observed in hysteria, and all the varieties of neuralgia and simulated inflammation, commonly called hysteric, frequently arise from the presence in the blood of the impurities which are the true characteristics of gout.”[43]
Truly, in light of this heavy indictment, one scarcely wonders that Rush classed the domain of gout as limitless. But one must recollect that, nosologically speaking, our forefathers were sadly hampered. Anomalous symptoms and disorders had to be referred to one or other of the available titles of disease, and what term more elastic than the timeworn “gout,” so easy to saddle with vicarious responsibilities?
But pari passu with advancing knowledge of the pathology of the nervous system and the rise of hysteria to the status of a clinical entity gout was shorn of the excrescences heaped on it by Laycock, Wells, and others.
But nevertheless the emancipation of gout from nervous and other alien disorders was slow of achievement, and largely, I think, through the wide acceptation of Murchison’s theory of a pathological state allied to gout and termed by him “lithæmia,” or the “uric acid diathesis.”
According to this authority, the deposit of lithates in the urine is a “manifestation of a morbid condition of the blood and of the entire system,” the outcome of a functional derangement of the liver. Such hepatic disturbance might endure for years without manifesting any other symptom than a frequent deposition of urates and occasionally uric acid in the urine. But, added Murchison, the same if neglected “may ultimately be the means of developing gout.”
Clinically it manifested itself by a variety of symptoms—depression[295] of spirits, irritability, lethargy, headache, pains and aches in the limbs, vertigo, insomnia, dyspepsia, palpitation, raised blood pressure. Such were the motley group of disorders affiliated by Murchison to lithæmia. But his disciples, more ardent, set no limit to the manifestations of uric-acidæmia.
Not only gout, but rheumatism and allied disorders, were amongst its progeny, and Osler tells us that one writer enumerates not fewer than thirty-nine separate morbid conditions associated with lithæmia. But leaving aside the extravagant claims of Haig and his followers, the impression even now is but too prevalent that gout and lithæmia are convertible terms. There is little or nothing to justify the assumption that an increased output of uric acid in the urine or deposition of urates therein is diagnostic of gout. Such, moreover, presupposes the further assumption that uric acid is the cause of gout.
We may affirm that certain symptoms betoken malassimilation of food or defective tissue metabolism. But it is by no means certain, as Murchison held, that a functional disorder of the liver is the fons et origo mali, much less that uric acid is the sole noxious substance. Yet in a masterly discussion of the subject Pratt, of Boston, tells us that as recently as 1895 a “leading clinical teacher” affirmed that “headache, migraine, depression of spirits, shooting pains, cramps, palpitation, vertigo, are a part of the symptomatology of lithæmia.”
Surely, if we are to make any pretence of reducing the phenomena of lithæmia or irregular gout to a scientific precision worthy of the present status of medicine, we should fight shy of such sweeping assertions. The caveat, we fear, is not superfluous. For as that judicial physician, Austin Flint, once satirically observed, “the designation ‘uric acid diathesis’ is used by some physicians in a rather indefinite way to describe various morbid states which may not at any time be accompanied by deposits of urates, and in which there is no proof of an excess of uric acid in the blood.”
Caustic as was this stricture, it was no less prophetic than apposite. For recent blood analyses have, as Pratt states, demonstrated that there is no increase of uric acid in the blood in that medley of disorders attributed by Murchison and his followers to “lithæmia,” or “the uric acid diathesis.” Here we would inveigh strongly against the too prevalent habit of stigmatising as “gouty” such symptoms as headache, vertigo, palpitation, etc., not only without any evidence of their being of this nature, but frequently when no attempt has been made to eliminate “errors of refraction,” aural disorder, etc. Moreover, granted that such possible sources have been excluded, we have no justification[296] in invoking “gout.” For, as noted, all modern observations fail to demonstrate the presence of uricæmia. Under such circumstances, given that the anomalous symptoms are inexplicable, would it not be wiser to content ourselves with the assumption that their presence postulates, not lithæmia, but a toxic condition of the blood plasma? This at least carries with it the inference that a search should be made for the focus of toxic absorption, whereas for but too many the term lithæmia, even when undemonstrated, is held to be self-explanatory and final.
Turning to another aspect of this subject, we are reminded by Duckworth that Hutchinson “directed attention to various maladies affiliated with what he terms rheumatic gout and gout, but differing somewhat from both, and these include various eye troubles, such as iritis, hæmorrhagic retinitis, and some forms of glaucoma, lumbago, sciatica, chronic rheumatoid arthritis, Heberden’s nodes, and possibly hæmophilia.”
As to the so-called “gouty” origin of the various eye troubles, these will be dealt with separately by Mr. Beaumont in his section. For the rest, hæmophilia may, we think, be safely discarded, Heberden’s nodes relegated to osteoarthritis, while rheumatoid arthritis has long since vindicated its claim to clinical individuality.
But as to lumbago and sciatica, these cannot be so easily disposed of, as a reflection of Heberden’s brings home to us. “It must be owned,” says he, “that there are cases in which the criteria of both are so blended together that it is not easy to determine whether the pain be gout or rheumatism.” Our own attitude towards this vexed point was precisely defined in a previous chapter in which we dealt with the affinities between gout and other diseases.
Having dealt with the broader and more extravagant claims made on behalf of the clinical content of irregular gout, we now restrict our purview to those disorders, chiefly visceral in site, which even to-day are referred by some to this category. We shall in the first instance deal with that variety known as retrocedent gout, and shall subsequently proceed to discuss other so-called irregular manifestations of the disorder.
The term retrocedent or suppressed gout still lingers in medical nomenclature, largely, we think, as a tribute to tradition, for rarely indeed is it invoked in current literature. Known since the days of Galen and Aretæus, it originally signified a condition in which sudden inhibition of the acute joint affection is followed[297] by or coincides with the development of serious internal symptoms referable either to the gastro-intestinal, cardio-vascular, or nervous system. Thus, there may be, e.g., vomiting, diarrhœa, dyspnœa, cardiac arrhythmia, cerebral hæmorrhage, delirium or coma.
Naturally for our forefathers the abrupt subsidence of the joint disorder with the incidence, as fulminant, of severe and alarming visceral symptoms appeared to be an example of true metastasis. That death, tragically sudden, so often ensued, but rendered more imperious the necessity for explanation; and, in the then state of knowledge, the proffered assumption could hardly be regarded as anything other than a perfectly legitimate and useful hypothesis.
The retrocession of the articular affection in acute examples of gout ensues abruptly, but in chronic types it usually transpires more gradually. Often no cause is assignable, but frequently the so-called metastasis has followed exposure, chill, or the imprudent application of cold to the inflamed joints. The late Dr. Parry, of Bath, in one winter saw two instances of apoplexy follow “the removing of gout in the extremities by immersing the feet affected in cold water.” In some, following the same revulsive procedures, severe cardiac pain has ensued with syncopal attacks, sometimes fatal, while in others gastro-enteric symptoms of like gravity have developed.
It is the asthenic types of gout that, according to Duckworth, are most prone to metastasis. When the phenomena occur rapidly, flitting from place to place, they have been designated “flying gout.” Nevertheless, as before said, the most dramatic examples arise in acute sthenic gout, though in their instance less likely to occur spontaneously than in sequence to depressing external agents, e.g., cold lotions, etc.
Reviewing the recorded examples of retrocedent gout in the light of latter day experience, it is, we think, most significant that no such dramatic examples apparently occur nowadays, at least none to which the term “retrocedent gout” appears applicable. The designation, indeed, bids fair to become obsolete. What then is the explanation? That even to-day cases of acute articular gout yield to, or are replaced by, functional visceral disturbances, of varying degrees of gravity, is certainly true. But, partly through increase of knowledge and partly through the growth of a more critical attitude, we seldom, if ever, feel justified in ascribing them to gouty metastasis.
Take “gout in the stomach,” to which organ, in the days of the Regency, it appeared to fly on the slightest pretext, a “vulgar belly-ache taking rank by courtesy” as such, before Sir Thomas[298] Watson pricked the bubble of these pretentious ailments by his suggestion that “gout” (so called) in the stomach sometimes turned out, under the test of an emetic, to be nothing more than pork in the stomach. A caustic stricture, but doubtless well merited. For the symptoms held typical of “gout in the stomach” are but those of gastric irritation, with nothing to suggest that they are of “gouty” origin.
Again, as Brinton in his classic exposure of this clinical myth observes, some of the recorded instances doubtless derive their melodramatic aspects from unrecognised biliary colic. As he rightly says, some of the cases instanced by Scudamore were jaundiced usque ad unguem. Gallstones, too, are among the many derivatives of the so-called “gouty” habit. The age incidence of both disorders is identical, whence doubtless the conception of the relationship. But what of the abdominal catastrophes attached to gallstones, all wholly unguessed at in those days? What, too, of the unrecognised and doubtless frequently coincident renal disease, with its menace of uræmia—pain, vomiting and prostration, not to mention Buzzard’s reflection that some cases of gout in the stomach were probably referable to gastric “crises,” i.e., tabes dorsalis?
If we recall that none of these sources of fallacy—and we have named but the more common—were eliminated, and also the absence of any anatomical proof post mortem of gastric lesions, one may well ask with Brinton, “Is there any ‘gout in the stomach’ left after the subtraction of these various affections?” Personally, I can say with Brinton that “I know of no such case; have never seen one; have never been able to get trustworthy evidence of one from some of the most accomplished physicians living, or from the best records.”
Reverting to the cardiac and cerebral phenomena that have sometimes followed the retrocession of acute gout, the same difficulties confront us. The conclusion that they are examples of retrocedent gout is drawn from premises which really do not support it. Strictly speaking, there is nought but the time relation to go upon, and the laconic comment “Non sequitur” is obvious.
To continue, the more we know of the causes and effects of disease, the less relevant becomes the time relation, and the nearer do our conceptions of cause and effect approximate to the more truly valid conception of ground and consequence. But what grounds have we for assuming that the anginal, the syncopal attack, or the apoplexy is the consequence of gout, that it is exclusively due to the materies morbi of gout?
The very disparity between the local lesions seems to exclude[299] the possibility of their being due to one and the same cause: in the joint, acute inflammation; in the heart and brain, degenerative changes. Where then the nexus? Surely it is but a time relation, a coincidence, the outcome of, concurrent though unrelated cardiac and vascular lesions. In short, the cases of so-called retrocedent “cardiac” and “cerebral” gout usually resolve themselves into cardio-mural degeneration, arterio-sclerosis, or renal disease.
The more dramatic examples of retrocedent gout, as before stated, occur mainly in the acute varieties of the disorder. But the same visceral metastases are occasionally linked up with the less severe articular manifestations, or with that vague clinical entity known as “goutiness,” the same being frequently known as “wandering” or “flying” gout. Most of the examples met with in the present day belong to the last category. This may possibly find its explanation in the growing infrequency of the more acute or sthenic types of gout.
Both of the mild and of the severe forms of metastasis the same pathological interpretation is hazarded. The gout is described as “suppressed” or “retrocedent.” According to the former conception, the gouty process itself suffers inhibition, while the latter term signifies deflection of the materia peccans of gout from the joint into the viscera. Of the twain the former hypothesis seems to me the more plausible. Thus, given an acute gout at its inflammatory zenith, it is conceivable that, if abruptly checked, the same might reflexly precipitate the occurrence of internal lesions in structures undermined by insidious and pre-existing degenerative changes. In other words, the aborted attack is not the cause, but the occasion, of the cardiac failure, the apoplectic stroke, the uræmia, etc.
On the other hand, given that such were due to actual transference of the gouty poison, one would expect that it would induce the same inflammatory phenomena in the viscera as in the joint. But there is no anatomical proof that such occurs, no evidence of an actual invasion of the impeached viscus by the gouty inflammation. Uratic deposits have, it is true, been found post mortem at the site of visceral lesions, but, be it noted, generally in degenerating tissue altered by other morbid processes. Some, however, affirm that in such the gouty process has quâ the uratic deposits left, so to speak, its attestation behind it.
But any degenerative focus may in a gouty subject become the seat of such a deposition. Yet it would be presumptuous to infer[300] its gouty origin from this fact alone. Such are common in chronic nephritis, and this apart from gout. What need for wonder then that the same should occur in gouty subjects, with their blood surcharged with uric acid?
Were such uratic deposits located at the site of inflammatory as opposed to degenerative visceral foci, it would to our mind give more colour to the assumption that they were the outcome of a true gouty process; in other words, that, as in the joints, they were the sequel or concomitant of acute gouty inflammation. But it is not so.
As for the structural or organic degenerations met with in gouty subjects, very many, if not all, as Longstreth rightly says, “belong to some one of the great general classes of tissue changes, some of which are due to special causes, but the most of them own many causes. One of these many causes can be under certain circumstances gout, but there is really nothing special in the appearances by which we can unequivocally pronounce them of gouty origin.” With this view few would join issue, save only the reservation that the scleroses so commonly met with in gout, if due thereto, must owe their origin to some more vital agent than uric acid, a few milligrammes more or less in the blood content thereof.
It will be seen then that the anatomical evidence that gout can affect the internal organs is wholly lacking. The criteria then upon which the assumption is based that this or that functional disturbance is a manifestation of irregular or visceral gout are wholly clinical.
Doubtless the conception of irregular gout was derived from “the unaided operation of custom.” Thus, when one clinical event, A, was noticed frequently to precede another, B, the idea of an association between A and B was generated, and by virtue of this association A was said to be the cause of B. But obviously the fact that B has followed A does not establish any necessary connection between the two clinical events. In other words, the idea of a causal relation is in a sense a purely intellectual feat, a clinical inference presumptive and retrospective.
The evidence that a relationship exists between irregular and regular manifestations of gout rests upon the following sequences and alternations of clinical events:—
(1) The subsidence or disappearance of functional visceral derangements following the development of articular gout;
(2) Their occurrence directly after an articular paroxysm has been apparently suppressed;
(3) Their recurrence and alternation with arthritic outbreaks, this in some instances repeatedly;
(4) Lack of any appreciable cause for the functional derangements and their indefinite anomalous character;
(5) Their favourable response to specific gouty therapy.
As before noted, digestive troubles frequently precede the initial outbreak of articular gout. The same likewise are frequent in chronic cases between the intervals of arthritic seizures.
Now it has been customary to regard the alimentary or other disturbances that precede an initial articular attack as “gouty,” and likewise those that intervene between the gouty paroxysms in long-standing cases. In other words, in light of the subsequent articular outburst, what was mysterious ceases to be a mystery. All the vague “acidities, flatulencies, megrims, and biliousnesses, of whatever occult kind,” are forthwith hailed as “gouty,” this merely upon the ground of the sequence of clinical events, because the symptoms have disappeared from, e.g., the stomach to reveal themselves in the joint or joints, or vice versâ.
Now my own view is that the antecedent hepatic or digestive disturbances that so frequently precede initial attacks of gout are in all probability, nay assuredly, not gout. They should rather be regarded as the cause, the foundation, of the malady than its effect, a cause inoperative save in the presence of individuals victimised by inherent morbid tissue potentialities. For similar symptoms are but too common in the non-gouty. They are very common antecedents of, e.g., rheumatoid or atrophic arthritis. Nevertheless we do not when the arthritic disorder subsequently manifests itself talk of the preceding digestive disturbances as “rheumatoid” dyspepsia. Then why this presumptive and retrospective diagnosis of similar prodromal phenomena as “gouty” dyspepsia? For there is pending the articular outbreak nothing distinctive in the digestive derangements, nothing that would enable us to diagnose them as “gouty.” They might, for aught we know, be significant of oncoming rheumatoid arthritis.
Now in the case of the latter we regard the prodromal digestive phenomena as probably indicative of some infection located somewhere in the alimentary tract. It would be wiser, I think, to adopt the same attitude in regard to our “gouty” examples. Moreover, as we know, such dyspeptic symptoms recur from time to time throughout the life history of both rheumatoid and gouty arthritis. In the former disorder we regard them as indicative of recurring infection, followed as they so uniformly are by exacerbations of the joint trouble. Is it not time we adopted the same attitude towards the gastric or hepatic functional disorders that punctuate the course of chronic gout with a periodicity that rivals that of the articular paroxysms?
Unquestionably to my mind when we have regard to the extreme frequency with which local foci of infection, e.g., oral sepsis, etc., are found in gouty subjects, this would be the more rational attitude, the one more in conformity with modern medical thought.
But if we would condemn those who, in the presence of unequivocal tokens of gout, label antecedent or intercurrent dyspepsias, etc., as “gouty,” what are we to say of those that even in patients who have never had regular gout or exhibited tophi yet presume to classify their associated digestive troubles as “gouty”? This, I contend, is wholly unjustifiable. I would say more, that such conjectures are hazardous in the extreme, this both in the overtly gouty as well as in the non-gouty. I recall the instance of an individual who suffered from classical articular gout which palpably alternated with attacks of abdominal pain, but the clue to the true nature of the latter symptoms, as revealed at operation, was a chronically inflamed appendix. If so in this case, how many so-called “gouty” acidities have resolved themselves into appendicular or gall-bladder dyspepsia!
My conclusion then is that the gastro-intestinal disorders attributed to gout cannot legitimately be regarded as examples of irregular gout. They should not be held “symptomatic” of, but etiologically related to, gout, a view more calculated to lead to exact diagnosis and rational therapy, and incidentally to elucidate the true nature of gout.
In respect of other organs and the symptoms connected with them in “gouty” persons the case is very much the same. Always and ever are we confronted with the same difficulty, inability to determine whether antecedent, co-existing, or consecutive affections in certain examples of gout, are not associated merely by coincidence.
Disturbed cardiac action is not uncommon in gouty subjects, palpitation and arrhythmia and syncopal threatenings, and frequently symptoms difficult of differentiation from true angina pectoris.
I am reminded of an old physician whom I saw in consultation some years ago, who suffered from alarming attacks of precordial anxiety. He was well on in the sixties, and very obese. He was convinced that his cardiac irregularities, etc., were of gouty origin, and often exclaimed regretfully: “If I only dared to take two bottles of port, and got it in my toe, all would be well.” He had never had an articular outbreak, and based the diagnosis of his case on the fact that from time to time his urine for long since contained excess of urates. Having suffered much of many physicians, he at last grew restive, took the bit between his teeth, rushed to a[303] spa, and forthwith embarked on a very strenuous course of “waters and baths.” At once he got a severe attack of acute polyarthritic gout, and mirabile dictu, all his cardiac troubles straightway ceased.
Retrospectively viewed, many would regard the preceding cardiac condition as of “gouty” source. That the old gentleman, of florid countenance, plethoric build, and lethargic habit, was potentially “gouty,” there is no doubt. But he was also abnormally fond, not of alcohol, but, curiously enough, of sweetmeats and cakes of all sorts, hence “dyspeptic.” He had a feebly acting heart, but no detectable valvular lesion, though mural degeneration seemed likely. My own diagnosis was flatulent dyspepsia with secondary cardiac disturbance, and finally acute gout, the exciting cause of which, as I have so frequently seen, was a course of hydrotherapy. The patient never regretted his venture, and, I am glad to say, lived for some years.
Such cardiac paroxysms are not uncommon in the “gouty,” and, alarming though they are, I question if purely functional disturbances of this nature ever prove fatal. As to the valvular lesions and mural degenerations observed in the “gouty,” there is little or no evidence that they are dependent on gout. Indeed, the lack of a tendency to endocarditis is one of the criteria distinguishing gout from acute rheumatism. I note that in one textbook pericarditis is classed among the cardiac manifestations of irregular gout. But it must not be forgotten that renal disease, a frequent concomitant of gout, predisposes to pericarditis, which, indeed, occurs in granular kidney even when unassociated with gout.
As to the respiratory organs, such chronic maladies as bronchitis and asthma are very frequent in the “gouty,” but I question if they are more so than in non-gouty subjects. In any case their symptomatology and course are the same whether gout be present or not. Much, too, has been made of the fact that asthmatic and arthritic manifestations may alternate. But we must recollect that asthma per se has a paroxysmal tendency; it has a tendency to periodicity and a liability to be excited or aggravated by much the same factors as favour outbreaks of gout. It is said, too, that there is a “gouty” pneumonia, and that the same has been replaced by an acute articular paroxysm. But, in respect of all these alleged “gouty” respiratory disorders, would it not be more scientific to cease talking of them as “gouty” and instead to speak of them as bronchitis and asthma occurring in “gouty” subjects? This, I may remark, is not to say that we should take no count of the reigning diathesis in our treatment of all associated affections.
Of the nervous phenomena relegated to gout we hear nowadays less and less. “Gouty” headaches are almost a thing of the past. The acute “gouty” delirium of older writers in many cases was but an euphemism for alcoholism, and likewise the spinal paralyses; while the convulsions and comas were certainly almost always attributable to uræmia. It would be held rash to-day to speak, like our forefathers, of “gouty” cystitis, urethritis, or orchitis, for there is no evidence of any pathological connection between them; and the same stricture is also applicable to the many cutaneous affections affiliated without sound pretext to the materies morbi of gout.
In the early part of the nineteenth century the French school were most insistent on the prevalence and variety of the cutaneous manifestations of l’arthritisme; but even by them the all-pervading influence of gout in the etiology of skin disorders is no longer held even as a working hypothesis.
Conclusions.—The sum of my experience and reflections on so-called “irregular” gout leads me to regard it as an “abstraction” rather than as a proven clinical fact. Moreover, if I may judge by the “admission certificates” to the Royal Mineral Water Hospital, Bath—a fair test, as I maintain—many are of the same mind as myself, for during the past ten years I do not recall a single instance in which a patient sought admission thereto as suffering from “irregular” gout.
But some writers on gout—indeed, I think I may say all—whatever doubts they entertain as to the propriety of retaining the term, yet qualify their pronouncement in favour of some particular variety of anomalous gout, visceral, cutaneous, or other. Still, in justification of my own uncompromising attitude, I must say that dispassionate analysis of their eclectic claims, in light of present day knowledge, to my mind fails to show any adequate reason for the faith that is in them. Of some of them I feel sure that sub-consciously they have been influenced by a respect for tradition, forgetful of Pliny’s sentiment,—
“Quamvis enim cedere auctoritati debeam, rectius tamen arbitror, in tanta re, ratione quam auctoritate superari.”—Lib. i., Ep. 20.
But, to resume, this much at any rate may be affirmed, viz., that there is no proof that visceral disturbances or cutaneous disorders are due to uric acid. On the other hand, in view of my contention that the inherent morbid potentialities of the “gouty” demand for their fruition the intervention of an infection, the reader may rightly ask whether the same agent may not be capable of evoking the visceral or cutaneous, as opposed to the arthritic, manifestations of gout.
Trousseau, a whole-hearted advocate of irregular gout, drew an analogy between gout and syphilis. Somewhat contemptuously he observes: “To those physicians in whose eyes localisation constitutes the particular disease the differences in appearances are so many different diseases, while to those who consider that the disease consists much more in the aggregate of the general phenomena, in their evolution, in their progress (and that, thank Heaven! is the direction in which sound observation leads), these affections, differing in appearance, are only multiplied expressions of the same species of morbid action. To the real physician exostosis, alopecia, psoriasis, roseola, bubo, and chancre are always syphilis—syphilis in different garbs.” In the same way he held that the infinitely varied manifestations of irregular gout were all affiliable to one and the same morbid agent. He claimed, too, that visceral gout was “the result of a sort of imperfect inflammation analogous to that which manifests itself in the joints.”
Unfortunately for the cogency of the argument, there is no proof that such visceral inflammations as do occur in the “gouty” are of gouty origin. Unfortunately, too, the microbic agent that we postulate as responsible for “gouty” arthritis is as yet unisolated. If this disability be removed, it might be found that the said organism was capable of originating, not only the arthritic, but the alleged visceral, forms of gout. But pending such discovery I am of opinion that the term “visceral” gout should be abandoned, in other words that we should cease to talk of, e.g., bronchitis, dyspepsia, etc., as “gouty,” and should talk of them as bronchitis or dyspepsia occurring in the gouty. In this way we may escape, or, better, render uncalled for, the scathing criticism of Pye Smith:—“It has become common to ascribe bronchitis, dyspepsia, gastralgia, iritis, gravel, cystitis, and even psoriasis to the ‘gouty’ diathesis; but the evidence is very slight, and the ‘gout’ to which such evidence as there is applies is the distillation of morbid humours which belong to a bygone pathology.... There is no reason to believe that gout ever flies to the stomach, but over-indulgence at the table may produce acute dyspepsia as well as inflammation of the great toe. Elderly people are liable to gravel, gout and cough; and while lead and drink may lead to gout and chronic Bright’s disease, cirrhotic kidneys favour an attack of gout.”
While subjects of gout have told me that they had had an attack in their teens, I have never myself seen an instance. Still less[306] can I claim to have seen what I felt justified in calling “gout” in children. On the other hand, if, as one authority states, “tonsillitis (quinsy), enlarged tonsils, granular states of the pharynx, and catarrhal conditions of the throat and respiratory mucous membranes are not infrequent expressions of gouty inheritance in children,” then, of course, all of us must be quite familiar with “infantile gout.”
But even this formidable list of legacies from gouty parents is eclipsed by a more recent writer, J. Comby (1902), who, discussing “infantile arthritism,” divides children coming of gouty stock into two types: the “lymphatic” and “nervous.” The children of the former class suffer from fleeting swelling of the lymphatic glands, rhino-pharyngitis, tonsillitis, and, if they be girls, from chlorosis. Also they are given markedly to tachycardia, bradycardia, and vasomotor ataxia. They are also especially liable to asthma and the crises of dyspnœa, and pulmonary congestion may alternate with urticarial and eczematous eruptions. Truly, their lot is hard, for they fall a ready prey to colic, constipation, all varieties of dyspepsia, not to mention nocturnal and diurnal enuresis!
Comby also claims that these gouty children are especially liable to recurrent or cyclical vomiting. In this matter he is confirmed by J. Thomson, who noted that these children not infrequently give a history of having had asthma, urticaria, eczema, stammering, and other nervous complaints, also that in many instances uric acid crystals or a copious deposit of urates have been noted in their urine.
As to the “nervous” type, they labour with insomnia, night terrors, convulsions, and when older with migraine. To these liabilities must be added undue proneness to acne, seborrhœa, psoriasis, chilblains, angio-neurotic œdema, urticaria, etc., not to mention muscular and joint aches and pains.
Whether this medley of distempers can with any pretensions to scientific reason be affiliated to a gouty heritage, or whether they can be regarded as expressions of a budding “gouty diathesis,” is, I submit, of the nature of pure speculation. That the child who suffers with cyclical vomiting may show uric acid crystals or urates in his urine is certainly no proof that he has inherited gout, much less that he is actually “gouty.” In uro-lithiasis the uric acid is precipitated in the urinary passages, viz., strictly speaking, outside the body, whereas in gout the pathological error originates within the organism. More apposite is Uffenheimer’s observation, previously noted, that children of this type suffer the same disturbances of purin metabolism as are met with in adult gouty subjects.
If the fact is confirmed that the output of exogenous purin in such children is diminished or retarded, it would certainly be a most interesting finding, possibly with a now unguessed-at significance. But we should recall that even in the subjects of regular gout such is not invariable, and, moreover, occurs in diseases other than gout. Pending further exact investigations I think it would be wiser not to indulge in such vast generalisations, mindful of the sentiments expressed by the illustrious Sydenham in his letter to Dr. Gould:—
“I have bin very careful to write nothing but what was the product of careful observation. So when the scandall of my person shall be layd aside in my grave it will appear that I neither suffered myselfe to be deceived by indulging in idle speculations nor have deceived others by obtruding anything to them but downright matter of fact.”
With the passing of Jonathan Hutchinson disappeared the premier British exponent of l’arthritisme, that generic term so attractive to our French confrères. Whether gout and rheumatism are branches of one common stem need not detain us, for it is an abstraction more suitable to the philosophic age of medicine before pathology emerged as an exact science. Be this as it may, there has been in the past, and there still remains in the present, as a bond of union, a universal belief that both are subtle causes of disease of the eye. But the age of hypothesis is giving place to the era of facts, and we find in recent writings a more cautious expression of individual opinion, a less dogmatic positivism regarding the relationship of gout and rheumatism to ocular disease.
In referring to modern text-books we find Parsons[44] describes gout as one of the “alleged causes” of iritis. In rheumatic iritis he states that the patients “are often gouty.” The gouty nature of iritis is indicated by the similarity of onset of some cases of iritis with that of gout. “Iritis in an elderly patient is likely to be gouty, often starting suddenly in the night and sometimes ushering in an attack of gouty arthritis.” In episcleritis “rheumatism and gout are commonly indicated as the chief causes.”
Werner[45] includes gout in a list of disorders of metabolism which produce iritis “by means of toxins of a chemical nature.”
Sim[46] considers that iritis occurs in gout “as the result of some toxic influence”; and in addition he says, “Iritis is to be met with in gout.”
These authors express accurately, I think, the present views with regard to gout as it affects the eye; with each there is a tone of restraint and suggestion rather than of boldness and assertion, and the contrast to Hutchinson’s emphasis is noteworthy: “I believe,” he tells us, “that iritis due to the arthritic diathesis is a common malady.”
Among the many and indiscriminate diseases of the eye which have been considered to be due to gout are included blepharitis, conjunctivitis, episcleritis, scleritis, orbital cellulitis, neuro-retinitis, retro-bulbar neuritis, optic neuritis, optic atrophy, iritis, cyclitis, choroiditis, glaucoma and retinal hæmorrhage. Truly an all-embracing rather than an eclectic list, a medley of diseases without any melody.
Evidence of Gout in the Eye.—When we inquire what is the evidence which justifies the belief that gout causes ocular disease we find little more than a traditional hypothesis inherited in a long line of succession from the Fathers of Medicine. Nevertheless the opinion that there is a connection is widespread, not only in Europe, but also in America.
In considering this relationship we cannot overlook the effects of the diathesis on other viscera. How in these is a diagnosis of gouty origin arrived at? It would appear that the assumption of an irregular form of gout is based upon the following observations:—
(i.) That it sometimes happens that an undoubted attack of articular gout aborts and is followed by symptoms referable to a grave visceral disorder, e.g., gout in the stomach (retrocedent gout);
(ii.) That sometimes the converse occurs, viz., that an attack of visceral disorder may suddenly be replaced by an acute articular manifestation;
(iii.) That such visceral derangements may alternate, not only with articular, but also with other, such as cutaneous, outbreaks;
(iv.) That eye disease has been known to wax and wane in unison with concurrent arthritic gouty manifestations;
(v.) That occasionally in gouty people an attack of iritis of sudden onset in the night has been followed by remission of the symptoms in the day[47];
(vi.) That visceral symptoms in the gouty are anomalous and inexplicable on any other basis;
(vii.) That the treatment usually advocated for gout has a favourable influence.
Deposition of Urates.—Two cases are recorded by Garrod in which there was a deposit of urates in the sclera. These instances do not appear to have been confirmed by other observers, and they may be regarded as exceptional cases, occurring, it should be noted, in the outer envelope of the eye. But though these[310] tophaceous deposits may occur in the sclera and in the eyelid, they have never been known to invade the intrinsic structures, such as the iris or ocular media. The eye, in fact, is on all fours with the sites of urates elsewhere—deposition occurs in parts of relatively low vitality.
Although urates are not found within the eye, there is in other morbid ocular conditions quite frequently a deposition of foreign matter, such as alien crystals, of varied description. For instance:—
In the sclera on rare occasions we find osteomatous degeneration.
In the choroid there may be true bone which forms a cup so extensive that it can be felt by the finger, or, again, there may be calcareous plaques.
The retina may undergo colloidal changes or be the site of carbonate of lime or of cholesterin.
The vitreous may sparkle with showers of cholesterin.
The lens may contain both tyrosine and cholesterin.
The aqueous shows similar crystals.
In the iris degenerative calcareous or osseous deposits are occasionally seen.
The cornea may be affected by hyaline degeneration with deposition of lime salts.
The conjunctiva may be calcareous.
In all these cases the foreign particles, whether crystals or otherwise, are usually the retrogressive changes of senescence proclaiming that the forces which make for degeneration are more potent than those which make for regeneration.
But urates are not found in the eye, even though the patient is gouty. On the other hand, both in gouty joints and in other similarly affected parts of the body we find a deposition of urate of soda.
Gouty Diathesis.—From the days of Sydenham—himself a martyr to gout—diathesis has been a name to conjure with, and an all-sufficient diagnosis. In the podagrous patient any intercurrent disorder, any inexplicable ache or pain, was ascribed to gout, and patient and doctor were alike satisfied. “Tempora mutantur,” but still we are prone to call morbid conditions gouty when they occur in gouty people.
If we accept the theory that gout is due to an excess of uric acid in the blood, the view which I have expressed elsewhere[48] that gout does not cause iritis is directly challenged. For if it be granted that a sudden outpouring of so non-toxic an acid causes an acute inflammation—for instance, in the synovia of the great[311] toe—why should not our faith incline us to go further and find in this malevolent, though bland, acid a source of inflammation affecting the fibro-muscular meshwork of the iris?
If, however, we adopt the infective theory, then the association of the uratic deposits no longer dominates our creed—we view them as mere clinkers and by-products erupted from the furnace.
The infective theory of gout also lends plausibility to an association with iritis, for this latter is a disease of infective origin. For the intimate relationship of all forms of asthenic arthritis with iritis is of very frequent occurrence, but is practically never seen in the more sthenic arthritides: rheumatic fever, acute gout and traumatic arthritis.
Nearly fifty years ago Jonathan Hutchinson drew up a “Report on the Forms of Eye Disease which occur in connection with Rheumatism and Gout.”[49]
At the present day it is not easy to differentiate his 117 cases according to modern classification, but he includes gout, rheumatism, rheumatic arthritis, etc. The differential diagnosis between gout and rheumatism was simplified by the creation of a mule—“rheumatic gout”—and upon its back were packed the doubtful cases.
Hutchinson’s views regarding the essential difference between gout and rheumatism are crystallised in his statement that in rheumatism there is an arthritic susceptibility to weather, in gout an arthritic susceptibility to diet.
Osteoarthritis also seems to have been included as one of the gouty diseases, probably because post-mortem examination revealed uratic deposits in the disorganised cartilage. This, however, would appear to be an epi-phenomenon, and must not be allowed to obscure the essential distinction between true gout and osteoarthritis. It is a sign of articular disorganisation of long standing, and is the homologue of the similar deposition of crystals, etc., already referred to as occurring in the eye as the result of chronic disease therein.
The significance of tophi, as the touch-marks of gout, is undoubted, but even if they are detected in the eyelids or elsewhere, we are skating on thin ice if we rashly declare that a coexisting intra-ocular disorder is gouty. Most forms of iritis betray the same clinical facies, although the etiological causes are diverse. But in none do we find any appearances pathognomonic of gout.
The argument that because a patient has tophi therefore the[312] iritis is also gouty does not hold good, for gout does not confer immunity from other diseases, and even though we cannot prove an alibi for the diathesis, we can often in these cases also indict gonorrhœa, pyorrhœa or some other pathogenic agent.
The favourite site for tophi is one in which blood-vessels are sparse; but, although the cornea is void, imbibition of blood from the marginal looped plexus of capillaries and an abundant lymph supply provide amply for nutrition, and tophi are not found in this locality. The sclerotic, however, has a meagre supply of vessels, and for some unexplained reason tophi rarely invade it. In the eyelids, on the other hand, possibly from the cartilage being rich in sodium, tophi are occasionally seen. If we accept the tophus as the one unequivocal criterion of gout, we are not justified in labelling an iritis as gouty in its absence. If we do, our diagnosis is presumptuous and not absolute. Strictly speaking, the diagnosis cannot be made. We may the more readily admit our limitations, inasmuch as they are a blessing in disguise, and suggest a further etiological search.
In Hutchinson’s list of eye diseases which occur in association with rheumatism and gout there is a history of gonorrhœa in twenty-six cases, syphilis in seventeen, of both gonorrhœa and syphilis in six. Herpes occurred in two, pustular acne in one, eczema in one, albuminuria in one, ague in one. Bad teeth are reported in two. In all the total was fifty-seven cases out of 117 (48·7 per cent.) in which there was a possible source of infection. It is probable that this percentage would have been materially increased if at that time it had been recognised how great is the influence of pyorrhœa and other sources of infection in the etiology of irido-cyclitis.
With regard to all infections it is only in the present day that full advantage is taken of bio-chemical and bacteriological methods of differentiation. How frequently the true origin of disease must have been overlooked when the pallid spirochæte was unknown, when the Wassermann test was not applied, and when the complement fixation test for gonorrhœa was not recognised.
With regard to a combined cause it has been maintained that gonorrhœa is always more severe in the gouty than in other people, and it may be that the more intense the gonorrhœa the more likely may it be to produce constitutional symptoms, of which iritis is one. In all such the combination of gout and iritis would indelibly impress upon the mind of the surgeon the intimate association of joint and eye. It was long ago recognised that many forms of joint disorder were associated with iritis, and, as the cause of the arthritis was not always gout, Mackenzie introduced[313] the generalisation “arthritic iritis.” “Not being able,” he tells us,[50] “to determine the diathesis which predisposes to this ophthalmia” (iritis), “I use arthritic as a conventional term, without adopting it in the strict sense of gouty.” The expression is well worthy of retention for the reason that it warns us to be prepared for an attack of iritis in many forms of arthritis and arthralgia.
In the following articular diseases the triad joint, muscle and nerve disorders is not uncommonly linked with iritis:—
In the following forms of arthritis iritis is less common:—
Iritis occurring in these last suggests the possibility of error in the diagnosis of the putative parent disease. Especially is the clinical similarity of gonorrhœal (polyarticular) rheumatism to rheumatoid arthritis to be borne in mind.
The Relative Incidence of Iritis.—In the text-books it is often stated that the syphilitic form of iritis is the one most frequently met with, and that gouty iritis, if it is met with at all, is much more rare. But in these comparative statements we have no clue to the frequency of iritis with syphilis, nor of iritis with gout. For a true analogy we do not want the syphilographer to tell us the aggregate number of cases of iritis that he has seen, but what is the percentage of cases of syphilis in which iritis occurs, and we want the gout physician to state his percentage of iritides in gout, or, negatively, what is the percentage of cases in which iritis does not occur.
If gout is a more prevalent disease than syphilis, it does not follow that “gouty” cases of iritis will be more numerous than those due to syphilis. Let us suppose, for the sake of clearness, that 1 per cent. of people suffering from gout get iritis, and that also 1 per cent. of people infected by syphilis get iritis, and that in a certain town there are two hundred people who are gouty and one hundred people who are syphilitic. It is probable that there will be two persons suffering from gouty iritis (always[314] supposing there is such a disease), but only one from syphilitic iritis. The absolute totals will differ, but the relative will be identical. It is clear, then, that infectivity cannot be gauged by the statistical enumeration of the consulting-room. Gout is a rarer disease than our patients would have us believe, but accepting their views, even then we should expect to see more cases of iritis caused by it, if such existed; we should expect to find more definite proof of a causal connection, and less frequently a history of gonorrhœa, of pyorrhœa, and of syphilis.
No Uratosis, no Gout.—If we pin our faith to the equation
Hyperuricæmia + Uratosis = Gout,
we can at once exclude all cases of ocular disease as gouty in the absence of either factor. According to Garrod, “true gouty inflammation is always accompanied with a deposit of urate of soda in the inflamed part.” We should therefore expect that uratosis would occur in situ if an iritis were gouty. But it does not: the touch-mark is absent, and there are no chemical, pathological or clinical signs of urates in the iris after the inflammation has subsided. What then is the alternative? Either Garrod’s aphorism is inaccurate or iritis is never gouty. In other words, we must postulate that an iritis may be regarded as gouty without uratic deposits. If this be the case, the so-called gouty iritis may well rank with the occult migraines, flatulencies and acidities which are termed irregular, suppressed or latent gout. Strictly then it would be a latent gouty iritis fit to rank with that last refuge of the uric acid enthusiasts, the “latent nephritis” which they worship as the fons et origo mali of gout.
Metastasis.—The predilection of the gonococcus for synovial membranes is seen not only secondarily to urethral infections, but also in ophthalmia neonatorum, in which the joints of infants are affected sequentially to the eyes.[51]
The gonococcus also has been found in cases of peritonitis, pleurisy, pericarditis, etc., but it is said to have only once been isolated in the eye in iritis.[52]
It is not only the gonococcus which can initiate a metastasis from the eye to the joints, to the peritoneum, or elsewhere. The same process may be started by the bacillus typhosus, by the streptococcus of erysipelas, and by that of puerperal septicæmia.
De Grandmont[53] records the case of a young man recovering from typhoid, complicated with jaundice and nephritis, who was attacked by iritis with posterior synechiæ and hypopyon. Paracentesis was done, and the pus of the anterior chamber was transferred to agar-agar. Two days later a pure culture was obtained presenting all the reactions and characteristics of the bacillus of Eberth. Of this culture a small quantity was injected into the vitreous of a rabbit. A month later the rabbit was killed, when the liver and intestines were found to be infiltrated with the same bacillus of Eberth.
In erysipelas de Grandmont has seen a hyalitis from which a culture was grown on gelatine that presented all the morphological characteristics of erysipelas.
He has also met with a case of hyalitis associated with puerperal septicæmia, and he has no doubt that it was the result of a similar microbic invasion of the vitreous.
Gout does not render patients immune from tuberculous, syphilitic or gonococcal disease, and when in such so-called diathetic stocks an iritis occurs, especially in gonorrhœa, years after the primary disease, it is probable that gout, rather than lues, will be assigned as the cause.
The local appearances of iritis are identical in gonococcal and other infective iritides; they resemble clinically those seen in syphilis and tubercle except that in these there are sometimes condylomata of the iris in the one and tuberculous nodules in the other. To be comparable a gouty iritis should be characterised by iritic tophi.
“Arthritic” Iritis.—Forty-eight is a large percentage in Hutchinson’s cases of ocular disease associated with gout and rheumatism, and it is justifiable to assume that there was something more than coincidence in the triple entente of diathesis, arthritis and iritis. But the fact that the poisons of syphilis and gonorrhœa, etc., are potent causes of iritis is indisputable, and therefore the patients might have suffered from it even if they had never had either gout or “rheumatism.” Consequently these articular diseases are both superabundant and superfluous, and they may have no etiological status. A patient afflicted with arthritis is very susceptible to an associated attack of iritis provided that there is a septic focus anywhere in the body.
A practical point to remember, especially in gonorrhœa, is that the onset of joint trouble should warn us to anticipate the possibility of an associated iritis and should prompt us to instil atropine at an early stage. We should forestall the disease by treating[316] the suspicion. The frequency with which gonorrhœa is followed sooner or later by iritis entitles this ocular phenomenon to be considered a secondary symptom of gonorrhœa, as it is of syphilis.
Before the potency of distant infective foci (for example, in nasal disorders, pyorrhœa, sinusitis, etc.) to produce ocular disease was recognised, there was justification for the inclusion of a so-called idiopathic iritis, but it is seldom now that we have to be satisfied with this negative diagnosis. Nevertheless the assignment of a toxæmic etiology must be based on a definitely ascertained focus of toxic absorption, or failing this, at least on symptoms of general malaise which render such a focus highly probable.
Frequency a Factor in Diagnosis.—It was known a century before the birth of bacteriology that gonorrhœa caused iritis. It was also noted that certain constitutional symptoms occurred in syphilis, and that among them not infrequently iritis was one. Observation and deduction was the process with our forefathers, and it seldom led them astray.
If in any sequence of events cause and effect are to be established when there is no obvious proof of connection, we may have to be content with an empirical diagnosis, and this was the position before the discoveries of bacteriology enabled us to place the etiology of iritis on a firm basis. How then did our ancestors know that syphilis and gonorrhœa caused iritis? Was it not—
(1) That the frequency of the association was the essence of the diagnosis,
(2) That there was absence of any other recognised cause, and
(3) In the former disease the effect of anti-syphilitic therapy?
Applying these rules to gout, we find—
(1) No marked frequency of association of ocular disease and gout,
(2) That when iritis does occur there is often some other possible source of origin, and
(3) That anti-gout treatment has only a doubtfully beneficial effect.
“Gouty” Iritis is not a Clinical Entity.—Before a symptom or affection can be classed as secondary to a primary disease there must be evidence of a connection stronger than post hoc, ergo propter hoc. For instance, in syphilis an iritis frequently follows which may be of the specific condylomatous type, and a laboratory examination of the inflamed iris may demonstrate the presence of the spirochæte. On the other hand, an iritis occurring in a gouty patient is indistinguishable from that form which results from infections of undifferentiated type. Moreover, iritis so seldom occurs associated with gout, and when it does there are so often[317] present other well-recognised possible causes, such as pyorrhœa or gonorrhœa, that the doubt about the paternal relationship of gout to the iritis is overwhelmingly strong.
In the following table a comparison is made between types of iritis:—
| Gout. | Syphilis. | Tubercle. | Toxæmia. | |
|---|---|---|---|---|
| Pathognomonic symptoms. | 0 | Gumma of iris. | Tubercles of iris. | 0 |
If pathognomonic symptoms were always present the differentiation of the various causes of iritis would be less difficult. But this is not the case, and consequently, whatever the primary cause, the appearances of the iritis, in spite of the pathogenesis, objectively resemble each other in very many instances.[54]
Medical authorities call certain cases (not varieties) of iritis gouty; they are content to rest the diagnosis on the ground that they occur in gouty people. Yet there is not a single ocular symptom which differentiates the disease from a similar one in non-gouty subjects. Before the dogma can be accepted that because a gouty man has iritis it is therefore a gouty iritis and, like the poet’s primrose, nothing more, it must be shown that irido-cyclitis is proportionately more frequent in people who are gouty than in those who are not. Even then it is suggestive, but not conclusive, for it is conceivable that, although gout is not strictly the cause, yet it may so reduce the resisting power of the iris that it becomes a readier prey to some lurking organism.
It is commonly reported that the existence of a gouty diathesis gives to any inflammatory condition of traumatic origin—synovitis, for instance—a special tendency to chronicity, and I would not deny that it may have the same influence in the case of iritis of traumatic endogenous origin.
If then a gouty man is not immune from other possible causes of iritis, one of these, and not gout, may be responsible for it. Especially is a gouty diagnosis doubtful when there is a focus of suppuration in the tonsils, teeth or elsewhere. Also the prolonged hibernation of the gonococcus, for many years after the attack[318] of gonorrhœa, is apt to be overlooked. The presence of excess of uric acid in the blood, which sometimes occurs in these patients, may mislead us into the belief that we have a true gouty iritis to deal with. But even although it is ascertained that a hyperuricæmia of 4-8 mg. of uric acid is present, it is no proof that the co-existing iritis is necessarily gouty. We might have an even higher content of uric acid in the blood in leukæmia, and yet no iritis be present. It may be admitted that on rare occasions iritis occurs in leukæmia, but no one suggests that the leukæmia or the associated iritis is due to uric acid toxæmia. We should be on infinitely surer ground if not uricæmia, but uratosis, were present. We could then, at any rate, confidently assert that, whatever the origin of the iritis, it had supervened in a subject of gouty habit. I do not think that we, as clinical observers of iritis, should go further than to say: “The man is gouty; his iris is inflamed.” Here in Bath, among hecatombs of gouty people, irido-cyclitis is one of the rarer associated diseases requiring treatment. When it does occur it is usually of obviously septic genesis rather than of gouty origin.
Contrasting gonorrhœa with gout, we find in the former when there is systemic infection, as shown by arthritic complications, there may be also iritis, so often, in fact, that it is legitimate to bracket it as a related symptom. It is a toxæmic condition in which we rely on the frequency of the combination to diagnose the cause.
In writing on iritis in 1908,[55] I referred to the rarity of the association of gout and iritis. In an analysis of 17,197 cases of “rheumatism” and rheumatoid arthritis occurring at the Royal Mineral Water Hospital, Bath, in twenty years, there were twenty patients who suffered from acute or subacute iritis. During the same period there were 2,159 gouty patients not one of whom had iritis. In a special hospital it is possible that the diagnosis of gout might be limited by a stricter nosological differentiation than occurs in private practice. It is, moreover, not uncommon for ophthalmic surgeons to see patients who call themselves gouty, or who say that their doctors have told them that they are, and yet on examination no corroboration is found, no clinical outbreak, or, more pertinent, no tophi. They come to us with an attribution of iritis to gout without the filmiest shadow of evidence.
In considering the correlation of cause and effect it not infrequently happens that we find no obvious connection between the one and the other. In syphilis, for instance, alopecia is a usual secondary symptom, and we rely on the frequency of the sequence[319] to satisfy ourselves that it is no mere coincidence. If it could be shown that alopecia did not occur more frequently in syphilitic people than in non-syphilitic we might justly doubt the connection. The same reasoning may be applied to iritis and gout: the association is so rare that it is negligible. To justify a causal connection between diseases the possibility of a fortuitous concurrence must be excluded, for when the double event occurs only very exceptionally, it is difficult to exclude the long arm of coincidence.
A man has iritis and tophi; ergo we say he has gouty iritis. But why? They co-exist, it is true, but where is the link of attachment of cause and effect? How different is our attitude if we know in another case that our tophaceous iritic patient has gonorrhœa. We then say, gonorrhœal iritis in a gouty subject. Would it not also in the first case be more scientific if we frankly confessed that it was an infective iritis of undifferentiated type occurring in a person of gouty diathesis?
In considering the iritides in relation to gout there are two types which demand our attention. With the possible exception of traumatic iritis, this grouping embraces all the etiological varieties of the affection. In the first are those cases which are due to specific infection, such as syphilis, gonorrhœa and tuberculosis. In the second are those infections of undifferentiated type in which the causal germ has not yet been isolated. Now clearly we must read the latter in the light of their analogues, the specific iritides. In them the modes of onset, the clinical course, are duplicated, presenting similar variations, and they are doubtless the reflexes of the varying grades of intensity of the causal organism.
Concussion iritis would fall into line, for it is possible in this case that the iris is rendered a pars minoris resistentiæ by the blow, and that the iritis which follows is due to a cryptic focus, it may be in the gastro-intestinal tract or elsewhere. The chief sources of iritis are syphilis, gonorrhœa, tubercle and infections from undifferentiated organisms of low grade. If these said iritides occur in a person of gouty diathesis they are unmodified by it clinically or pathologically, macroscopically or microscopically, save possibly in the direction of chronicity—a result, it may be, of those inherent peculiarities of tissue metabolism ingrained in a gouty subject, and in which presumably the iris shares.
And that which has been said of iritis in the gouty applies equally to other forms of so-called gouty ocular manifestations. There are no statistics available to show that there is any differential frequency in those who are gouty compared with those who[320] are not. Authors have laboriously recorded cases of eye diseases which have waxed and waned in unison with podagrous toes, but the publication of these cases is in itself a confession of the rarity of the coincidence, a rarity which destroys the authenticity of any communal kinship. Coincidence is merely another name for the rigid and immutable law of chance, for a cycle of events which occurs with irregular regularity. If it could be shown that a diet rich in purins brought on an attack of ocular disease in gouty people, and if the experiment could be repeated with a similar result and sufficiently often to exclude all probability of coincidence, scepticism would no longer be justified. But until more definite evidence is forthcoming “gout” in the eye is nebulous.
In attempting to define the relationship of gout to ocular disease, there is one author to whose opinion we turn with the respect due to a master. Garrod’s judicial summing up supports the view that there is a connection between gout and ocular disease, but his cautious statement seems to imply that the affection of the eye is modified by rather than due to gout. His statement is as follows[56]:—
“Gout of the Eye.—A form of ophthalmia connected with gout has long been recognised, and appears to be tolerably well established, but as rheumatic inflammation of the eyes is equally allowed to exist, difficulties may at once arise in the diagnosis. I have witnessed many cases in which conjunctivitis and sclerotitis appeared to be distinctly connected with the gouty diathesis, and in two cases there existed deposits of urates on the surface; gouty iritis also occasionally occurs. I once saw a case of acute inflammation of the sclerotic coat and iris which supervened a few days after the operation for cataract in a gouty subject. By active treatment the disease was arrested, but distinct articular gout soon manifested itself.
“Our information on this subject may be thus summed up: patients having a well-marked gouty diathesis now and then experience attacks of inflammation of the different structures of the eye; and it is important to bear in mind the fact that the state of the habit considerably modifies and keeps up such affections, and also that treatment directed to the gouty condition of the system proves very effectual in curing the local mischief.”
It will be observed that Garrod tells us that his two important cases of sclerotitis “appeared to be distinctly connected with the gouty diathesis.” With the reticence of the careful and accurate[321] observer, he does not say they were due to it even though there were deposits of urates on the surface. He would seem to recognise that cases of sclerotitis with uratic deposits were unusual events, and that generalisations cannot be based upon exceptional cases. A gouty man is gouty to his innermost cells, and the eye, like every other part of the body, is a potential uratic site. We must grant therefore that the course of an iritis, however caused, may be influenced, though not necessarily dominated, by the diathesis. Consequently it may be necessary that cases of iritis of undoubted gonococcal or other infective source occurring in gouty people should be treated by iodides, salicylates, atophan or colchicum.
From the academic point of view ocular gout may exist, but from the practical point we should invariably seek, and we shall probably find, some still more important source of infection requiring treatment.
Ocular Symptoms in Hyperuricæmia.—The popular view that gout depends upon uricæmia is so generally accepted that the expressions “uric acid diathesis” and “gouty diathesis” are tantamount to tautology. Nevertheless they are different, the first postulating the supposed cause, the second the inferred result. There is a commingling of cause and effect. Uricæmia is a normal condition of the blood, but in certain diseases—gout, leukæmia, plumbism, pneumonia, etc.—a considerable excess of urates is found. No form of ocular disease is included as an associate of hyperuricæmia unless one or other of the ancillary diseases is also present.
In leukæmia when severe there is an extremely pale fundus, with a yellowish tint; hæmorrhages, when they occur, are often pale; the choroidal vessels also, if they can be seen, are pallid; the veins in the retina are full and tortuous. There may also be yellow foci, and occasionally retinitis with white spots. In a word, the leaking vessels tell of vascular disease.
In lead-poisoning we find paralysis of ocular muscles, amblyopia, contracted fields of vision, papillitis and retro-bulbar neuritis. It is the nervous system upon which the stress principally falls.
In pneumonia we do not expect to find any ocular complications; in spite of the uricæmia, the eyes are scatheless.
It seems unlikely that hyperuricæmia can produce such widely different signs in the eyes. Rather, on the other hand, the ocular symptoms conform to the type we should expect to find associated with leukæmic blood in the first and with lead-poisoned nerves in the second.
In this congeries of ocular symptoms, marked by hyperuricæmia,[322] we do not find iritis included, and yet this is a commonly accepted gouty affection of the eye.
False Gout.—It often happens that patients tell us that they are gouty although they do not claim to suffer from attacks in the old-fashioned way. With them there is a wide difference between the substantive “gout” and the adjective “gouty,” the latter apparently implying an attenuated form of the former. Such patients are seen at health resorts and are very frequently those in whom obesity and plethora are present to a marked extent. The full-blooded appearance involves the head, body and limbs, but the eyelids, for some unexplained reason, may escape. The patients have lived not wisely, but too well. On examination an increased quantity of uric acid in the urine is found, and is supposed to justify the diagnosis of gout. Sometimes the malassimilation, is associated with arterio-sclerosis, with diabetes, or with albuminuria. But the patient is almost invariably convinced that he has gout, that it is hereditary, that it has been handed down to him through a long line of ancestry from primeval days, and that an ascetic life would not have prevented it in his case.
Should such a one be attacked by iritis, the circularity of the argument is complete: he has iritis, therefore he is gouty; he is gouty, therefore he has iritis. But usually in the early days of this so-called gout we see no ocular changes; the time for organic disease (inflammatory and hæmorrhagic) has not yet arrived; auto-intoxication has not yet begun. But sooner or later with the maturation of disease come ocular degenerative signs, retinal hæmorrhages, and so on. The sequence is malassimilation, “goutiness,” sub-infection, ocular disease. Thus in diabetes melitus (omitting toxic and traumatic forms) we find pancreatic disease, nutritional changes, and not usually until late retinitis, cataract, iritis, etc. In renal disease retinitis is also late and often ushers in the final scene.
If in these cases of so-called gout we implicitly accept the patient’s nomenclature of disease, we shall find plenty of gouty iritis, but we may overlook the fundamental condition of his arteries, of his kidneys, and of other organs.
The sins of repletion in such patients may be relieved by the virtue of abstinence, not by colchicum.
Retinal Hæmorrhage.—That retinal hæmorrhage may be caused by gout was firmly maintained by Jonathan Hutchinson.[57] This opinion was shared by Gowers, who states that the “influence seems well-established.”[58]
Hutchinson pointed out that in cases of retinal hæmorrhage of[323] renal origin, stellate white deposits occurred, whereas in gouty cases they were absent. By this criterion he classified his cases. In his first patient Hutchinson relates that he can only state from memory that there was no albumen, but that “he seemed in good health and that there was reason to suspect gout, although he had not had a definite attack.” In his second case, a woman who had suffered from rheumatic gout and true gout, there were numerous hyaline casts in the urine, but no albumen. In both cases the hæmorrhages were flame-shaped, and Hutchinson lays stress on the shape in gouty retinitis hæmorrhagica. The group consisted of fifteen patients, eleven men and four women. “Gout had been positively present in six, and was strongly probable in four or five others. In one the gout was complicated, and probably in part produced, by lead poisoning, and this is the only instance in which the urine contained much albumen. In another in which no history of gout was obtained, the patient, a man æt. 67, had diabetes, which was the probable cause of the retinitis.... In about a third of the cases albumen was found in the urine, but it was usually a mere trace and only present occasionally.... In four, including the case of diabetes, white deposits characteristic of renal retinitis were present in small quantity, and in all these albumen was found in the urine.”
Hutchinson sums up his cases with the catholic observation that retinitis hæmorrhagica is a malady the boundaries of which are very indefinite. And when we bear in mind the changes of modern medical opinion with regard to the influence of arterio-sclerosis on the retinal circulation and the effects of vascular hypertension the etiological difficulties regarding retinal hæmorrhages are hardly less illimitable than they were when Hutchinson penned his valuable contribution. In all his cases (as in those which we see now forty-two years later) there are many factors which may have been responsible for the hæmorrhages apart from gout.
In renal disease gout is widely recognised as a possible precursor. So we are again in the same quandary that we experience in considering the relationship of gout to iritis. Are the retinal hæmorrhages due to gout or to the resulting renal disease? The claim of gout to be the deus ex machina once more seems to be superfluous, for retinal hæmorrhages are an end result which may be reached by a variety of pathological routes. Gout may be one, but if so it acts viâ interstitial nephritis. In other words, hæmorrhagic retinitis is the apanage of nephritis and the appendix of gout.
It is impossible to affirm that a retinitis is gouty, for there are no distinctive features, but it occurs in gout when vascular[324] disease has supervened, not gouty retinitis, therefore, but retinitis in the gouty. This is all that can be affirmed when we find albumen in the urine and tophi in the ears, eyelids, etc. Moreover, it is wiser in the interest of the patient to take this broad view. There may be a link between the kidney and the diathesis, but it is invisible.
Neither are we absolved from searching for some other cause of renal disease. The case may be fundamentally one of arterio-sclerosis with a secondarily induced sclerotic kidney, or, on the other hand, the hæmorrhages may be symptomatic of pernicious anæmia and due to toxins. With regard to prognosis it is helpful to remember that retinal hæmorrhages, especially when they are isolated, suggest the possibility of death ensuing suddenly from cerebral hæmorrhage; but albuminuric retinitis is itself frequently a terminal stage of chronic renal disease. We have not sufficient proof to call retinitis gouty, and we should adhere to the more catholic appellation “nephritic retinitis.”
James Taylor, writing on neuro-retinitis in the gouty,[59] states that—
“Commonly, of course, it occurs in association with albuminuria, yet it is met with apart from this even in cases where no very obvious cardio-vascular changes can be demonstrated in other regions. And thromboses in retinal veins, apart from cardiac hypertrophy and demonstrable changes in the arteries or in the blood pressure, are of frequent occurrence. In such cases gout is possibly—in many cases demonstrably—a very important factor in the etiology.”
The opinion that cases of neuro-retinitis may be gouty is based upon (a) the fact of the apparent absence of cardio-vascular disease elsewhere, (b) the lack of any other ostensible cause. Doubtless many cases of retinal hæmorrhage are seen for which we are unable to assign a cause; in some of these there is no suggestion of gout and nothing to support a postulation of a latent form of that diathesis. Taylor’s statement that gout in many cases is demonstrably a very important factor in the etiology cannot be lightly set aside, but as the appearances of neuro-retinitis are similar whether gout is present or absent, it is legitimate to question if the diathesis is really necessary.
Glaucoma.—Brudenell Carter, Hutchinson and Nettleship have claimed that gouty people are more apt than others to suffer from glaucoma, but no convincing argument has been brought forward in proof of any definite nexus.
The conclusion I would arrive at is that it is unwarrantable to speak of “gouty” ocular disease, for there is nothing in the[325] character of the inflammation specific of gout. We renounce the prefix in order—
(1) That we may not be lulled into false etiological security, and
(2) That we may approach the elucidation of the case and the treatment thereof free from preconceptions. The mouth and its accessory cavities are the primary sphere of our investigation. This is no mean task, including as it does the radiography of the teeth, even though these are apparently healthy. In the tortuous route of elimination we look for concealed dental roots, rarefying osteitis, buried tonsils, post-nasal infections, antral disorders.
The view that non-traumatic iritis is only a symptom imposes upon us a wide outlook in our search for a diagnosis. In this no viscus can be overlooked, no organ forgotten. All are members one of another, and the wise physician takes cognisance of their interdependence. The recognition of an inflamed iris is only the first stage in the diagnosis, for iritis is the sequel of a story written elsewhere. It is a question, not an answer.
But we know not what the future has in store, and though, with our present knowledge, I affirm that I can find no evidence that the eye is a locus signi for gout, the day may come when, either from bacteriological or other sources of progress, it may be shown that there is a mystic source of intercommunity. In other words, it may yet happen that the mysterious materies morbi of gout, whether microbic or chemical, may be demonstrated experimentally as capable of inducing, not only the arthritic phenomena, but also those inflammatory lesions in the eyes which provisionally are sometimes called “gouty.”
Lastly, I would enter a plea for more systematic, more scientific, investigation of the true link, if any, between iritis and arthritis. The war has taught us the value of “team-work”; it has taught us that the clinician must be reinforced by the bio-chemist, the bacteriologist and the pathologist. The work and the workers must be co-ordinated in our daily struggle with disease as we meet with it in our individual patients. The realm of medicine, with ever widening borders, is too vast for single control. In the foregoing pages I have said much about iritis, and it is a good example of what I mean. In justice to our patient, we may call for a Wassermann or a complement fixation test; we may require the teeth-roots made visible by an X-ray expert, or, it may be, the passage of a bismuth meal radiographed, hidden tonsils explored by the laryngologist, or the antrum illuminated; the fæces may need bacteriological examination. A gynæcologist may help us regarding a leucorrhœa or a possible ovarian abscess.
With many of our patients, alas! considerations of expense compel us to forego our aspirations.
What is the remedy? Is it not State help, central clinics staffed by highly trained experts engaged in research work? Here the poor could be examined and reports supplied to the attendant doctors free, and less impecunious patients at an inclusive fee. Centres such as these would do much to advance the science of medicine and thereby raise the standard of health and make the sick and ailing healthy citizens of a great empire.
Salus populi suprema lex.
Adaptation is the keynote to progress in therapy—adaptation of our therapeutic measures to the ceaseless advances of pathology. In the history of gout it has ever been so, the changing, oftentimes contradictory, vogues in treatment, always the reflex of equally mutable and conflicting views as to its pathogeny. For who can doubt that the facts of pathology supply the indices of rational as opposed to empirical methods of therapy?
Albeit, much remains to be done before we can claim to fulfil the demands of ideal treatment of gout. For we are still ignorant of its exact etiology, cannot yet boast of our control of the morbid potentialities that constitute the pathological groundwork of the malady. We cannot obliterate the diathesis, and must still deplore with Sydenham that “as for a radical cure, one altogether perfect, and one whereby the patient might be freed from even the disposition to the disease, this lies, like truth, at the bottom of a well; and so deep is it in the innermost recesses of nature that I know not when or by whom it will be brought forward into light of day.”
But although we cannot dissipate the inherent proclivities to the disorder, we can, I think, claim to fulfil the humbler rôle, viz., obviate their coming to fruition. Haply in the fulness of time we may be able to influence the endogenous factors that make for gout, may through the labours of the bio-chemist be able to translate or assess them in terms of functional inefficiency of this or that particular viscus. But meanwhile we must perforce content ourselves with the eradication or control of the exogenous factors of gout—the excitants whereby or through whose agency the malady from being latent becomes manifest and overt.
When discussing the etiology of gout we emphasised the probability of the intrusion of an infective element in its genesis. We commented, too, on the extreme frequency with which local infective foci are encountered in gouty subjects and the imperative necessity of their early recognition and radical treatment. In[328] doing so, we but conform to what should be regarded as the salient canon in the treatment of any form of arthritis, viz., a diligent search for a focus of infection. A monarticular arthritis, such as gout in its initial outbreaks almost invariably is, calls for the same painstaking investigation as a polyarticular, for one never knows when the former may merge into the latter. Nor, if we find one focus, should we rest content, assuming that this is the only one of significance. For in many instances there are probably several foci. Thus, how frequently are septic teeth conjoined with tonsillar and aural troubles, and, as modern investigation shows, these, again, may be associated with remote foci in gall bladder, appendix, etc.
To begin with, a thorough examination of the mouth and nasopharynx is essential. During the inspection any artificial dentures must be removed, lest we overlook concealed and septic stumps. “Bridges,” again, are a notable source of sepsis. The roots upon which they are fixed or the related gums may be infected. Phlebitis, as we know, is a common associate of gout, and C. A. Clark, emphasising the septic potentialities of bridges, cites an obstinate case of phlebitis which only cleared up after removal of a filthy device of this nature.
Again, devitalised teeth that have been “crowned” should always be suspect. Infection at the root is common, with abscess formation. Such are not necessarily painful, and may give no indication of their presence until they find an exit of discharge, maybe by a gumboil or viâ the antrum, etc. These abscesses around the apices of non-vital teeth are difficult of diagnosis in their early stages. Even the X-rays may fail to detect them when minute, this owing to the small amount of pus, or because abstraction of the lime salts from the bone has not proceeded to an extent that may be appreciable by skiagraphy. The first indication of their presence is a small area of rarefaction in the bone around the apex of the root.
It is important to recognise that teeth that appear sound upon external examination are not necessarily so. In short, ordinary clinical examination may be quite inadequate. Not only must the condition of the “crowns” of the teeth, but that of their roots also, be ascertained. For when we reflect that, in addition to abscesses, cysts, buried roots, inflamed and impacted molars may be present, we see, if we are to achieve a full and accurate diagnosis, radiographs of the jaws are essential. A single-plate negative is practically of no value. A series of films taken all round the mouth is the only satisfactory procedure. Such give finer detail, and show up the interstices of the teeth—the sites of predilection for periodontal disease or pyorrhœa alveolaris.
Passing to pyorrhœa alveolaris, which has been defined as the twentieth century scourge, it cannot be denied that if all the evils attributed thereto are to be nipped in the bud, then X-ray examination of the teeth must be resorted to at a much earlier stage than it commonly is. Clean as well as unclean mouths fall a prey thereto, and, as a rule, investigation of the teeth is an after-thought, this particularly in the subjects of gouty arthritis. Usually the gout has been in full swing for years. The patient’s dyspeptic symptoms have been dismissed as “gouty,” and “alkaline stomachics,” etc., have been his lot, though his teeth may be in a foul condition—one which would not have been tolerated probably in any form of arthritis other than “gouty.”
But if to diagnose pyorrhœa alveolaris in its early stages we must needs invoke radiography, on the other hand we should be careful not to overlook its presence when advanced. The gums may be pale and shrunken, at other times red and swollen and very prone to bleed. When pockets form round the teeth, pus and blood may be expressed. Probing may not reveal their true depth, whereas X-rays do.
Sometimes only one or two teeth are affected, at other times many, and these not necessarily adjacent to each other. Thus it happens that the disease is more advanced at one part of the mouth than at another. Exacerbations frequently occur—a blessing in disguise. The affected teeth become tender to bite on and loose in their sockets, but often pain lessens, and the tooth again tightens up, and the all-necessary visit to the dentist is again and again postponed. Sometimes abscesses form, which discharge into the peridental pockets. Eventually the teeth may drop out almost painlessly. Herein resides the danger of the condition, its relative painlessness. Hence the ease with which secondary infections may ensue, e.g., in the tonsils, the gastrointestinal tract, etc., while the original source may be altogether overlooked.
The subjects of gout are often middle-aged or old. We should recollect then that chronic periodontitis may in their instance ensue in sequence to senile atrophy of the alveolus. Recently in a patient of mine nearly eighty, a sufferer from gout and sciatica, a persistent pyrexia, of apparently cryptic origin, forthwith ceased after extraction of his teeth. He lived some considerable time afterwards, but I often regret that his septic teeth had not been drawn long before.
Unfortunately no specific germ can as yet be saddled with the responsibility for pyorrhœa alveolaris, though some would convict the endamœba buccalis. Spirillæ and staphylococci form a large proportion of the bacterial flora met with in oral sepsis, but[330] the results of vaccine treatment would seem to indicate that streptococci, diplococci, and staphylococci are the most frequent causes of complications. Still it must not be forgotten that the streptococcus viridans is by some held to be specially related to arthritis. Hartzell (1915) invariably found it in the teeth and peridental tissues in 220 patients suffering from arthritis. This streptococcus hæmolyticus frequently leads to secondary tonsillar sepsis, and, as previously noticed, to subsequent gall bladder infection, etc.
Passing to local treatment, if oral sepsis or pyorrhœa alveolaris exists, carious teeth when present should be extracted, or their cavities cleansed and filled. Accumulations of tartar should be removed, and unhealthy gums attended to. Thus “pockets” should be swabbed, syringed, or subjected to ionisation. Exacerbations frequently follow the extraction of teeth. Acute paroxysms of gout have followed this simple operation. In cases where the extraction of many teeth is called for, it should be preceded by as thorough a cleansing of the mouth as can be assured. It is a matter of common experience that severe exacerbations of arthritis follow neglect of this precaution, owing to the enhanced toxic absorption from the extensive raw surface.
Unquestionably, whether it be a matter of curettage, of “pockets,” alveolar abscesses, or extraction of teeth, it is wiser to proceed gradatim. Hartzell, when many septic foci exist in the gums and teeth, allows three to six days to intervene between “treatments,” this in order to gain full advantage of what may be called surgical auto-inoculation. For, as he contends, any local measures, curettage, etc., necessarily involve inoculation of the subject with a large number of organisms, thus producing an effect similar to that of an efficient vaccine, “with the added advantage that the constant supply is shut off from the focus disturbed.”
Recurring attacks of tonsillitis—well-recognised determinants of gouty outbreaks—demand thorough local treatment. If this fail, the propriety of removing the tonsils will call for consideration. But, as tonsils may be very misleading in appearance, the aid of an expert is often indispensable. Thus the worst types of tonsillar sepsis may exist in the small “buried” tonsil. In such cases the indications for enucleation are the more emphatic when we note the increasing evidence that tonsillar sepsis may be etiologically related to appendicitis or cholecystitis.
Again, as before pointed out, Wynn Wirgman noted that some cases of gout are associated with nasal disorder, and certainly in non-gouty forms of arthritis expert treatment has reacted very beneficially on the joint condition. Watson Williams has[331] recently drawn attention to “latent sinusitis” as a cause of systemic infections. He cites two cases of chronic rheumatoid arthritis which, previously resistant to treatment, were greatly improved by operation on the sphenoidal sinuses. The washings from the sinuses were free from pus, but on culture showed growths, in the one case of streptococcus albus and in the other of streptococcus aureus and streptococcus brevis.
Needless to say, the genito-urinary tract should be carefully investigated, especially in polyarticular gout, or monarticular when located in unusual articular sites, this if only to eliminate the possibility of a latent gonococcal infection. Apart from this, we should recollect that cystitis is common in gouty subjects, and, according to older authors, might occur as a result of “metastasis,” not to mention the cases of so-called “gouty” urethritis, which, it is claimed, not uncommonly supervenes at the end of an articular attack of gout. Nor should we forget the rectum, for hæmorrhoids are not uncommon in these subjects. Years ago Garrod noted that the cessation of a habitual hæmorrhoidal discharge frequently proved the signal for an outbreak of gout. Moreover, there is increasing evidence that rectal ulcerations may be causally related to some forms of arthritis.
When all the foregoing regions have been thoroughly investigated the lower levels of the gastro-intestinal tract must be thoroughly examined by all modern methods. Diminution, absence, or excess of free HCL may call for determination, while X-ray studies may afford us an explanation of dyspeptic symptoms. Lastly, the urine and fæces may call for exhaustive investigation.
In conclusion, however, if there be any local focus of infection so situated as to admit of radical measures, these should be undertaken prior to resorting to vaccine therapy.
But, obviously for the success of vaccine therapy, it is essential that an accurate bacteriological diagnosis of the case under consideration be accomplished, which of course is comparatively easy if we are able to isolate the particular organism by direct cultural experiment. To this end cultures should be made from the roots of extracted teeth, the gums, tonsils, or nasal or other discharges. Albeit, we must never be content to select haphazard any organism that we may isolate from the patient’s mouth, nose, urine, fæces, or elsewhere. Doubtless the true clue will lie in the institution of complement fixation tests for the organisms responsible for local infections. Research to this end is now in course of progress at the Royal Mineral Water Hospital, Bath, for it is becoming increasingly clear that nothing short of “team-” work will suffice for the full elucidation of the “gouty” and the non-gouty arthritides.
Truly in respect of diet the gouty have “suffered much of many physicians,” have been the butt, so to speak, of all the fads and frailties of medical opinion. Should that chemical outcast “uric acid” but appear in excess in the urine, it was, and still is for many, an infallible index, not only of gout, but of gout maintained and nurtured by improper feeding. The inference seemed obvious: the ideal diet for the gouty was a diet free from any uric acid-forming material. This achieved, the gouty “will be free from his leprosy, and henceforward, if he abide by the prescribed regime, all will be well with him.” But, as Sir James Goodhart, from whom we take this last passage, pertinently asks, “is this so?” The answer is, I fear, in the negative. For who has not met with gouty veterans who, having run the gamut of endless dietetic experiments, still remain “gouty,” though, mirabile dictu, still avid for fresh ventures?
For myself, I know of no stereotyped diet for the “gouty,” for in this respect every man is a law unto himself. “Get the acid out of your system,” is the watchword of many, and, I fear, often to the undoing of their victims. Bent on the annihilation of the disease, they overlook the individual. But, weary of futile chasing of uric acid out of the economy, most students of gout now agree that the aim of all dietetic measures should be to secure, as far as possible, gastro-intestinal asepsis. For, as experimental studies have shown, it is possible, by means of a judiciously selected and varied diet, to modify the character and even to inhibit the growth of the intestinal flora. The far-reaching nature of such an influence is clear when we reflect that all abnormal fermentative and putrefactive processes in the alimentary canal appear to be referable to the action of microbial agents.
Diet in Acute Paroxysms.—The initial outbreak of gout may occur at any age, and respect must be had to this as well as to other individual peculiarities. If the subject be young, say in the forties, and a free liver, he may at the onset experience distaste for food, if not actual nausea. If so, let him follow his bent, and confine himself to hot water, barley-water, or hot weak tea. Such a modified process of starvation is beneficial rather than harmful. Drinking freely of bland diluents promotes the elimination of toxic or waste materials, while the intake of hot water stimulates the hepatic cells and promotes the excretion of bile.
Milk, easy of digestion and rapid absorption by a febrile patient, is the ideal form of nourishment. Moreover, a milk diet constitutes the most effectual means of attaining a comparative degree of intestinal asepsis. From two and a half to three pints may be taken in[333] the twenty-four hours. While some will find no difficulty in assimilating it, others soon experience nausea, vomiting, and even diarrhœa, from the passage of undigested curds. It is therefore advisable to begin with small amounts given at regular intervals. If ill digested, it may be diluted with some alkaline water, or three to five grains of citrate of soda added to each tumblerful.
To obviate monotony the intake may be varied by oatmeal or barley gruel, veal, mutton, chicken, or vegetable broth, but strong soups and animal extracts must be avoided. There is no objection, however, to bread and milk, tapioca, semolina, or sago puddings.
With the disappearance of fever and the decline of acute symptoms fish may be introduced into the dietary, with later on a little white meat or chicken. This may be safely done when local pain and tenderness decline, and alike the tension of the parts, as shown by pitting. Moreover, at this stage the appetite usually asserts itself. Still the return to regular diet must be made slowly and cautiously, if we wish to combat the very common tendency in these patients to functional gastro-intestinal and hepatic derangements. Lastly, in acute sthenic gout occurring in a robust subject there is no need whatever for alcohol in the febrile stage. Also, it may be added, the younger and the stronger the patient, the better will he thrive on a pure milk or a lacto-farinaceous diet, and the less urgent the necessity for relinquishing the same until all fear of a relapse has passed.
On the other hand, in acute asthenic gout in an elderly and perhaps somewhat debilitated subject one must more than ever have regard to the individual, especially if he be an old time sufferer, perhaps with multiple joint involvement. Such a man “has not so much the gout as the gout has him.” He has to be helped to support his burden. In short, the diet for the young and plethoric differs from that suitable for the old and asthenic.
Restriction of such to a milk diet is sometimes positively harmful. The mischief is, that, once begun, every attempt at a more varied diet immediately provokes a relapse.[60] As Sir Thomas Watson wisely observed: “They must be allowed a certain quantity of their accustomed good cheer, or they become an easier prey to the disease. In such cases you must ‘trim’ as well as you can between opposite dangers, between the Scylla of excess and the Charybdis of debility.” In short, you must maintain their vigour and their strength. For this a pure milk diet will not suffice. In addition thereto, pounded or minced chicken, a little fish, sole or whiting, may be given. When also, as often[334] happens, they have been wont to take alcohol, two ounces of mature brandy or whisky, well diluted with Salutaris or other mineral water, may be allowed them every twenty-four hours.
Indeed, if the subject be old and broken down, it may be necessary to increase the amount of stimulant. In such cases to go on treating the disease, heedless of long-established habits, is bad policy. Wholly to withhold alcohol may well precipitate disaster. Homilies on abstinence or temperance are best postponed pending convalescence.
Moreover, these cases of acute gouty polyarthritis, whether in the middle-aged or old, very commonly run an afebrile course. If then, as not infrequently happens in these distressing cases, the patient’s progress is slow and unsatisfactory, there need be no hesitation in renouncing a strictly lacto-farinaceous regimen in favour of a more mixed diet: clear vegetable soups, well-made Julienne, mutton, veal, and chicken broths, lightly boiled fish of the digestible kinds, pounded and minced chicken, etc.
Even when in these cases pyrexia is present, it is rarely continuous, but is diversified by afebrile intervals. If then, while the paroxysm is in full flare, it be deemed advantageous to adopt a milk diet, it is all the more important that in the inter-paroxysmal stages we take full advantage of these periods of enhanced digestive capacity.
Diet in Chronic Gout.—Sydney Smith, writing to the Countess of Carlisle in his seventy-first year, humorously apostrophises his gout: “What a very singular disease it is! It seems as if the stomach fell down into the feet. The smallest deviation from right diet is immediately punished by limping and lameness, and the innocent ankle and blameless instep are tortured for the vices of the nobler organs.”
Precisely so, but what constitutes the “right” diet? We are told that this is good and that is bad for gout. Some would have us eschew red meat and cleave unto white; for others common salt is the devil that must be cast out. Some speak ill of all the fruits of the earth. Strawberries especially, they say, are the bane of gout, yet in these same Linnæus found salvation. For many, again, sugar is anathema, tea and coffee but uric acid solutions, and alcohol in all forms rank poison!
What a trial the gouty subject who, obsessed by his “acidity,” has passed through the furnace of many spas! “Everything I eat turns to acid” is his plaint. He has been all things by turns—a fruitarian, a vegetarian, no meat or all meat, etc. Such persons, in truth, are “uric acid” maniacs. But—forget it not—they are of our making, and often in their multitude of counsellors have found, not wisdom, but starvation! Well would[335] it be if the evil done ceased with themselves, but unfortunately they seek converts to whatever cult they affect.
The Fallacy of Fixed Dietaries.—As Bacon in his “Regimen of Health” (1597) wisely observes: “Some physicians are so regular in proceeding according to art for the disease as they respect not sufficiently the condition of the patient.” The wisdom of this has, I fear, been overlooked by those who hold that the ideal diet for the “gouty” is one destitute of the precursors of uric acid. Its acceptance makes not for flexibility in dieting, but rigid, undiscriminating routine.
Apart from the violation of principle, the direct result is, that the victim runs amok among the carbohydrates, with as a frequent penalty an acute outbreak, this although uric acid is not a direct product of carbohydrate metabolism; nor, as far as is known, does the carbohydrate intake influence the rate of formation of uric acid. Thus do theory and practice come into conflict, and, as usual, the patient pays. How pernicious this obsession that uric acid is a morbid agent! Uric acid is not an etiological entity, and, as Walker Hall rightly observes, “it is high time that every practitioner made a point of fully educating the public in this respect.”
Any attempt to formulate a set dietary proves but a snare and a delusion. No regime is applicable to the “gouty” as a class, nor even to the individual “gouty” subject at all periods of his life history. His disease persists for an indefinite period, and, like most chronic maladies, undergoes variations. Pari passu his digestive capacity rises and wanes. The regime therefore must be adapted and readapted to his varying necessities. For it is the patient, and not the “gout,” dictates the diet. But only too commonly the disease is dieted, the victim ignored—hinc illæ lachrymæ!
Our dietetic ventures must obviously rest on a sounder basis. This we do know, viz., that functional disturbances of digestion generally precede a “gouty” paroxysm, and that their amelioration is followed by relief of symptoms. The aim of our dietetic measures then is the prevention of digestive disturbances, not the routine withdrawal or reduction of uric acid precursors.
The dietetic treatment of the “gouty” is that of the “dyspeptic,” with, if anything, an added discrimination, for an unknown factor intrudes—the “gouty diathesis”—which has also to be reckoned with, but of this later. Now “dyspeptics” cannot be dieted by rule of thumb. Whether they be “gouty” or “non-gouty” matters not. A careful study of the phenomena of digestion, if not essential in every case, is certainly called for in the more obstinate and obscure forms. In short, an attempt[336] should be made to determine the special form of “indigestion.” Is the derangement of function a disorder of motility or secretion? Is it catarrhal or nervous in origin?
That such is the proper mode of procedure is undeniable. For are we not too prone to assume that the “dyspepsias” of the “gouty” are sui generis, all due to one cause, the materies morbi of gout, instead of being merely “excitants” of gout and due to a variety of digestive functional disabilities, and these of equally diverse origin?
Thorough Physical Examination a Necessary Prelude to Dieting.—When we recall that the “dyspepsias” of the “gouty” endure through long years, the suggestion that every effort should be made to localise and establish the exact nature of the underlying derangement seems almost superfluous. Yet how often is the question dealt with offhand, though, ideally speaking, I cannot help thinking that the primary outbreak of gout should be the signal for an exhaustive examination by all modern methods. The consequences of dyspepsia in the “non-gouty” are bad enough, but infinitely more so in the “gouty” subject. But it is the former group, not the latter, that has been the favoured object of study by experts, which is, I think, somewhat unfair.
There is need of a searching investigation, a more common invoking of the tests whereby the functional efficiency of the stomach may be gauged. We know that there may exist on the one hand hyperchlorhydria and on the other hypochlorhydria. But we need to know more as to disturbances in gastric motility, delay or hurry in digestion, not to mention abnormalities in shape, position, size, tone, pyloric end rhythm, etc. In view of the almost general admission that gastro-intestinal derangements are causally related to outbreaks of gouty arthritis, surely our remissness in this matter is somewhat surprising, the more so in light of the heroic procedures, viz., ileocolostomy and colectomy, advocated in rheumatoid arthritis, a condition by many deemed related to gout.
Leaving such aside, none will, I think, deny not only the value of test meals for free HCL variations and experimentation with all kinds of foodstuffs, but also of X-ray examination of the alimentary tract. How subversive of all preconceptions the revelations of radiography in gastric and intestinal conditions, of what infinite value in disentangling the ambiguous significance of purely subjective sensations! Thus, alterations in gastric tone, motility, and peristalsis may hark back to remote lesions in gall bladder or appendix, and these also account for variations in free HCL.
“Great eaters,” said Sydenham, “are liable to gout, and of these the costive more especially”—an observation the truth of which[337] all will confirm. It may be taken as a maxim that nothing for the gouty is more prejudicial than constipation. Here it is obviously of importance that we know the site of delay, whether in the lower coils of the ileum, the colon, or merely the rectum, i.e., dyschezia. How else obtain this information, save through X-ray examination?
Any departure from normal in consistency, colour or content of the fæces should be noted so as to identify hepatic or pancreatic derangements. An analysis of the urine should always be undertaken, its reaction noted, the presence of albumen or casts ascertained. It is important, too, that we do not overlook glycosuria or oxaluria, or substances indicative of excessive intestinal putrefaction. All these bear far more pertinently on diet than estimates of uric acid.
The behaviour of the skin, whether inactive or not, must also be taken into consideration. Moreover, as the subjects of gout are usually middle-aged or old, it is highly important to note the general drift of metabolism, whether in the direction of obesity or undue leanness. Herewith we must take an inventory, as it were, of the subject’s general mode of living. What are his habits in respect of food and drink? Is his diet excessive or improper in quality? Are his meals taken at irregular times? Does he masticate his food properly?
In the matter of exercise, his occupation or pursuits require thought. Do they involve excessive exertion or favour a sedentary habit? For both these factors bear narrowly on his power or not of disposing of ingested material. Indeed, all the foregoing reflections stand in close relationship to the complex processes of digestion and metabolism, and the efficacy of our prescribed regime will depend on how far our suggested innovations meet the particular needs of the subject under review.
Need for Collaboration of Clinician and Bio-chemist.—Before we shall be able to lay down a diet for the “gouty” on truly scientific grounds much remains to be done. Our clinical examinations, in no way to be despised, must nevertheless be supplemented by the more subtle tests of the bio-chemist. Consider the complexity of the problem. We have to diet not only the “gouty,” but the “potentially” gouty.
They shade the one into the other. Even the man who has had gout has his periods of respite, of apparent unblemished health. If seen at such a juncture, he may display the relics of his gouty attacks, i.e., tophi. But can we say of him that he actually now has gout? He has crossed the Rubicon, disclosed his morbid trend, but meanwhile he has apparently recrossed to the vantage ground of normal metabolism. He stands again with those who[338] are about to, but have not yet developed the disorder, i.e., the “potentially” gouty.
Who will deny that it is when a man is, so to speak, gravid with, but not yet delivered of, gout that dietetic measures will avail him most? But this, alas! carries with it as its postulate the diagnosis of latent gout. Now, Walker Hall suggests that “the nuclein metabolism of the gouty patient is run at high pressure or full capacity, instead of the usual normal quarter or at half-pressure capacity, in order to cope with the ordinary processes of assimilation, and that there is very little reserve energy.” Does not this seem to indicate that a fruitful sphere of research might be the invoking of “endurance” tests and other methods of determining the functional capacity or efficiency of the various viscera?
At present we content ourselves with blaming the stomach, the liver, the kidneys, etc., and often on very inadequate grounds. It would be a great step forward if we could determine betimes which particular viscus is functionally deficient. There are signs that this boon will not be long withheld, signs that not only can the functional efficiency of the stomach be tested, but also of the liver, kidneys, and even the spleen.
Thus Labbe and Daughin study the colloidal nitrogen in the urine, and find the ratio to the total nitrogen much augmented when the functional efficiency of the liver is depressed. Again, Bauer and Spiegel use the bilirubin content of the blood to the same end. They maintain that there is a bilirubin threshold, the assessment of which denotes the functional capacity of the liver. In health the blood content thereof is surprisingly uniform. But in passive congestion of the liver it rises very markedly, and the same after administration of cholagogues.
In like fashion the value of blood urea concentration is extolled by Kast and Wardell as a satisfactory index of the functional power of the kidney. The uric acid content of the blood is by Baumann, Hansmann, Davis, and Stevens regarded as a very delicate index of renal function, though unreliable in the presence of œdema, cardiac decompensation, or when the urine is highly concentrated in hot weather. These are but a few of the methods available, and in the same way Frey has devised tests for the functional efficiency of the spleen, while Barton invokes the administration of urea, chlorides, adrenalin, creatine, etc., to assess the functional capacity of the liver, kidney or spleen.
Such is the trend of modern medicine—to link up clinical with laboratory findings—and in gout perhaps more than in any other disease is this collaboration urgently called for. For who can doubt that gout is a malady of mixed intrinsic (endogenetic) and extrinsic (ectogenetic) origin?
We need to know more about the endogenous factor, the basal perversion of cell structure or function, that differentiates the tissues of the “gouty” from those of their fellows. For it is these inherent peculiarities—structural, physical, or chemical—that give to the disease its sui generis character. How then in the “living” subject shall these hidden morbid potentialities be identified? How save through the medium of function, the outward expression of metabolic activities, in other words by appraisement of the functional capacity of the various viscera? For gout primarily is a disorder of function, or, as Rendu phrased it, a primordial “vice of nutrition.” Hence our insistence on the invoking of the various laboratory methods for elucidating the functional powers, the efficiency or not of the liver, kidneys, etc.
This satisfactorily achieved, we may, through their reflected functional disability or disabilities, divine somewhat the nature of the innate tissue peculiarities of the “gouty,” may hope at long last to translate the misty “gouty diathesis” in terms of functional deficiency, deficiency of the working capacities of the stomach, liver, or kidneys, and perhaps find that the basal flaw in some lies in the liver, in others in the kidney, and thus the older clinicians be justified of their claims for “hepatic” or “renal” varieties of gout.
That exogenous factors, i.e., infections, bring to fruition these latent morbid tissue potentialities of the gouty, is my belief. Hence my contention that dietaries for the “gouty” should be such as promote gastro-intestinal asepsis. Albeit, infections are but the “seeds,” and who can doubt that the ideal diet for the “gouty” should also take cognisance of the “soil”—the pathological groundwork of gout?
The “soil” in gout is, I believe, one peculiarly favourable to microbic invasion, and here again recent studies of the cytology of the blood bid fair to yield us some criterion whereby the “degree of body resistance” to infections may be gauged.
But until the bio-chemist reveals to us the why and the wherefore of their peculiar tissue vulnerability our dieting of the “gouty” must perforce consist largely in diminishing the exogenous excitants of the malady. Ultimately, when researches now in progress have fructified, we may be able to influence the endogenous factors, may correct the functional defect of this or that viscus, stabilise the nuclein exchanges, and heighten the resistance of the tissues. In short, as Sir Archibald Garrod puts it, “we must consider the soil as well as the seed which falls upon it, and that he is the best exponent of the healing art who treats the individual patient rather than his disease.”
“The Accessory Food Factors.”—“Due nourishment, not[340] gluttonous delight,” is the true clue to the rational dietetic treatment of the “gouty.” But this question of “due nourishment,” how complex it grows in light of recent revelations. Thus, it is now generally agreed that to satisfy the animal needs for growth and the maintenance of nutrition something more than a due admixture of proteins, fats, carbohydrates, and inorganic salts is essential.
We must, of course, ensure that the caloric value of the food intake be adequate, and the supply of protein sufficient to maintain the nitrogen balance, also that the intake of protein suffice for the exigencies of tissue waste, not forgetting that for this is required a sufficient quota of the individual primary fractions of the protein molecule.
But this, we now know, is not all, for there are other and indispensable dietetic components. In the food we eat are substances of hitherto unguessed-at potency—the “vitamines,” or, as they are now more properly termed, “accessory factors of diet.”
Of these elusive bodies but three as yet have been isolated: fat-soluble A, water-soluble B, and water-soluble C. In infancy absence of the first-named “vitamine” leads to rickets. Lack of the second engenders scurvy, of the third beri-beri.
But, apart from these well-defined “deficiency diseases,” McCarrison has pointed out that the absence of these “accessory food factors” leads to grave functional derangements, especially of the organs of digestion and assimilation and those subserving endocrine functions, not to mention malnutrition of the nervous system and the induction of hyperadrenalinæmia and chronic inanition.
A heavy indictment, but, more pertinently to our subject, McCarrison inclines to think that bilious vomiting, cyclical acidosis, mucous disease, and other metabolic disorders met with in children are very probably due to deficiency of certain “accessory food factors.” In light of this it is interesting to recall that these same symptom complexes are by Comby and others regarded as manifestations of infantile gout.
More arresting still is McCarrison’s observation that all the clinical phenomena distinctive of “deficiency diseases” as a whole are apparently the result of nuclear starvation of all tissue cells. In short, these “accessory food factors” are essential to due nutrition of the nuclear substance. How interesting this in light of the generally accepted view that “gouty” individuals are victimised by some inherent defect or alteration of nuclein metabolism. Does not this seem to indicate that one of the clues to successful dieting of the “gouty” must be adaptation of the nuclein intake to the needs of the individual, in short that[341] we must strive for the stable maintenance or conservation of nuclein metabolism?
Again, as before stated, one of the results attaching to deficiency of “vitamines” is functional derangement of the organs of digestion and assimilation. Such disturbances are prominent in gout, and that “errors of diet” play an important rôle in the genesis of the disorder can scarcely be denied. At the same time there is no proof as yet that the absence of some mysterious “accessory factor” makes for the development of the disorder.
Nevertheless reflection on these findings is, I think, wholly apposite. It should, at any rate, chasten those who affect extreme dietaries on insufficient grounds. They are not justified of results, for, with Sir Archibald Garrod, I venture to doubt “whether by dieting our ‘gouty’ patients we achieve nearly as much as we think we do.”
Such good, moreover, as we do compass, is, I think, exerted indirectly. Even in the inter-paroxysmal periods of the disorder, despite good or perhaps exuberant health, gout is there. Its morbid tissue potentialities are latent, though functionally inactive. To maintain this state of passivity is the aim of all dietetic measures, viz., to diminish or withdraw the dietetic factors that are provocative of gout.
The diet most void of offence is one the least calculated to excite digestive disturbance—one that makes more surely for gastro-intestinal asepsis. At this juncture it is interesting to note McCarrison’s observation that although the absence of certain “accessory food factors” is the essential etiological agent in the genesis of “deficiency diseases,” yet he holds that infections and parasitic agencies are often important causes in determining the onset of symptoms.
Similarly in the causation of gout, “errors of diet” are not the only agencies at work. They are in truth but contributory factors in that such indiscretions favour the incidence of catarrhal states. These again promote increased toxicity of the intestinal flora with sequential disturbance of general nuclein metabolism and associated specific local reactions in certain tissues.
I make no apology for this somewhat lengthy digression. In the sphere of dietetics, as elsewhere, “a little knowledge is a dangerous thing.” We need to walk more circumspectly in this matter of dieting; and to this end reflection on the disabilities that still beset us cannot fail to be salutary, and will form, I think, a fitting prelude to our suggested mode of procedure.
The victim of gout is easier led than driven. Show no “bowels of compassion” for his failings, talk to him in the spirit of a dehumanised disciplinarian, and your tenure of his confidence will likely be short. You deal with a man more often wise than foolish, not merely a digestive tube.
The physician must be authoritative and yet tactful. Thus if the victim be a hearty eater, and you think he eats too much, try and get him to eat less. But do not bid him straightway live as an anchorite. Be a little more diplomatic. A good appetite is not a sin. An appetite over-stimulated by condiments or endless varieties of courses is. He should eat to satisfy his hunger, not to gratify his palate.
Do not irritate the patient with a strict dietary if avoidable. Far more often than not it is the quantity, not the quality, of the food that is at fault. Frequently mere reduction in bulk of the pabulum of all kinds taken will suffice. In short, restriction, not elimination, is the wiser maxim, especially so in indolent or sedentary persons in whom we may with advantage limit the food intake to the minimum consistent with the due maintenance of nutrition.
On the other hand, there is a widely prevalent idea among “gouty” subjects that if they take enough exercise they can eat and drink what they please and as much as they please. That active habits do counteract to some extent the evil effects of overeating and overdrinking is certainly true. Nevertheless, as Sir Thomas Watson reminds us, gout was extremely common in the old time squire, who not only “rode hard,” but “lived hard” also. It is so, though to a less extent, even to-day, and often such subjects prove very refractory. Often a reference to their “weight” will appeal more than any hygienic considerations. Make use, therefore, of their sensitiveness on this point, and so by diplomacy attain your end.
Overeating often goes with overdrinking at meals. I well recall a gouty old sportsman of bucolic type who was accustomed to swill his food down with several whiskies and sodas. Very[343] conservative in all ways, it was not easy to break him of the habit. Fortunately it occurred to me to ask him, “Did you ever see a horse eat and drink at the same time?” Reflecting solemnly, with obvious reluctance came the reply, “Damme, I never did, now that I come to think of it.” That settled the question. I had no more trouble, neither had he. Not often is one so lucky. But “Eat your meals dry” is not a bad rule in cases of sheer overeating. The appetite is sooner blunted.
As to the quality of the food, always recollect that “gouty” people are very prone to idiosyncrasies; but the idiosyncrasy is purely personal, not applicable to the “gouty” as a class. With them it is very much a case of “What’s one man’s meat is another man’s poison.” The physician who rides rough-shod over idiosyncrasies in the matter of foods rides for a fall. Let him rely on his own experience and knowledge in the matter of general dietetic principles; but when it comes to details—the eschewing or not of this or that—let him trust, not in his own, but in his patient’s, experience.
Many of these subjects know perfectly well what suits them and what does not. Their experience is your best guide. Having elicited this information, an appeal to their common sense rarely fails. Of the “gouty” it is especially true that “every man at forty is either a fool or his own physician.” For the fool there is but one corrective—dolor acerrimum naturæ pharmacum. The wise has only to be reminded of his own experience, viz., that certain articles of diet infallibly disagree with him—verbum sapienti satis.
In dieting the “gouty” we should never forget that the main groups of foodstuffs must be duly represented. We may reduce this or that, but never for long will they do well if one or other of the essential ingredients of human food be wholly eliminated. It is, as Sir Archibald Garrod remarks, doubtful whether even a minor constituent, such as the purins, can be continuously withheld with impunity.
Still, even from the more extreme dietaries advocated by some one may glean this useful lesson, that the temporary benefit that often accrues points the moral that simplicity of meals is best for these subjects. If they crowd soup, fish, meat, game, sweets, etc., all into one meal, they always pay the penalty. As Burney Yeo wisely says: “We should not mix up albuminates, fats, and carbohydrates, or flesh, vegetables, fat, and fruit in the same meal. One meal should be composed almost exclusively of nitrogenous food, another of fats and carbohydrates, and another of fruit, at proper intervals, and they will all agree and be suitable, but the contrary will be the case if they are mixed[344] together in the same meal, one hindering the digestion of the other.”
I have often found the old rule, “One meal of meat, one meal of fish, and one of neither,” an excellent way of impressing on these patients the importance in their instance of simple, as opposed to elaborate, meals. Arrangement of their daily bill of fare along these or similar lines is well worth the trouble.
If the food of the “gouty” needs to be carefully selected, it is no less necessary that the cooking be simple and appropriate. For the manner of the cooking is, I am sure, in many instances, more responsible for “gouty” outbreaks than the nature or the quantity of protein or other intake. Twice-cooked food, made-up dishes rich in extractives, are unquestionably pernicious. Nor are pickled or salted meats desirable. Similarly, strong meat consommés, hare soup, and beef extracts are best avoided. The same applies to rich gravies, sauces, spices, etc., all obviously likely to upset the digestion. Again, as to fish, it is better boiled or grilled than fried, and still better not fried in fat. In short, it is the “trimmings” more often than not that do the mischief, these strongly abetted by “second helpings.”
The physician may well insist upon a sufficient interval elapsing between meals. To attain due space between lunch and dinner, I invariably forbid “gouty” subjects to eat anything with their tea. The repasts should be taken in a leisurely fashion, if possible in a cheerful atmosphere. “Unquiet meals make ill digestions.” The nerve element in these cases is so pronounced that caution is anything but superfluous, viewing the inhibitory effects of worry and mental excitement on the secretory mechanisms of the alimentary tract.
The importance, too, of thorough mastication and regularity in meal-times should be impressed upon them. The desirability, too, of postponing the drinking of fluids to the end of the meal, and then only in small amounts, should be emphasised.
Strenuous exercise, mental or bodily, immediately after a meal is undesirable, and if, as is so often the case, there be any gastric disorder, the subject should rest both before and after meals. This is best taken lying down, especially if there be any tendency to gastric dilatation or visceroptosis. The same in hyperacidity, but in this latter sleep is contra-indicated. For it has been shown experimentally that the acidity of the stomach content is greater during rest than movement. But this is just one of those points on which authorities differ, and decision may have to be left to the patient’s own experience.
Lastly, we should always endeavour to ascertain as nearly as possible the actual amount of the food intake per diem. This[345] then must be weighed in light of the subject’s age, body weight, and mode of life. The middle-aged “gouty” person tends more often than not to obesity, and it will fall to the physician to decide whether the food intake be excessive or his habits too sedentary. Far more often than not it will be found that it is not that he walks too little, but that he eats too much. The appetite of youth goes ill with the inactivity of middle age. With these general considerations we will now pass to a discussion of the main elements of diet.
Proteins.—Ruthless cutting off of protein foods, though not so usual as of yore, is still far too commonly practised. The number of unfortunate wretches who are docked of their red meats is still astonishing. The “uric acid” bugbear dies hard. Unless red meat is known to disagree, I never advise a “gouty” subject to abstain wholly therefrom. I feel sure that it is rarely, if ever, called for, and when enjoined has frequently wrought much harm. As far as I know, there is no scientific reason for the very prevalent idea that for the “gouty” white meat is preferable to red. It is certain that both contain an equal quantity of extractives, and equally certain that for some, mirabile dictu, white meat, e.g., rabbit, is more indigestible than red.
Accordingly let your “gouty” patient eat animal food, at any rate at one meal, but let it be of one sort only. Let his appetite be his only sauce, his meat plainly cooked and well masticated. It matters not if it be red or white. What does matter is whether for him it be digestible. Mutton or lamb are more likely to prove so than beef or pork, and chicken, turkey, or fresh game more easily assimilable than duck or goose.
From Walker Hall’s experiments Luff thinks “it would appear reasonable to administer sweetbread to gouty patients, since its nuclein portion is only slightly absorbed, for thymus sweetbread contains principally adenin, which is rapidly excreted, and pancreas sweetbread contains mainly guanin, an amino-purin incapable of increasing the urinary purin output and of exerting any injurious effects upon the tissues.”
Nevertheless I still think that “gouty” subjects are better without thymus, pancreas, and other highly nucleated substances. Despite our ignorance of the true nature of gout, we do know that there is generally an excess of uric acid in the blood, and that to increase the content thereof is undesirable. Again, we know that in normal men, after ingestion of pancreas and thymus gland, the uric acid output in the urine is markedly increased.[346] But, on the other hand, many observers—Magnus-Levy, Vogt, etc.—have noted that after the eating of thymus by gouty individuals they found far less uric acid in the urine than in the case of normal persons. In short, such purin-rich foods in their instance is followed by uric acid retention.
More pointed still is the fact that acute outbreaks of gout have been repeatedly brought on by administering thymus to the subjects of chronic gout. Surely, in light of this, it is impolitic to approve of sweetbreads as desirable ingredients of a “gouty” dietary, this even if only on empirical as opposed to scientific grounds. That some “gouty” persons eat sweetbreads with impunity is undeniable. But certainly if on inquiry a subject overtly gouty admits a penchant for these foods, we should at any rate advise their restriction or elimination.
Fish.—This pre-eminently, with certain exceptions, is very desirable food for the “gouty,” especially those whose digestive powers seem unequal to coping with the stronger kinds of animal food. The white-flesh fishes, i.e., sole, whiting, turbot, brill, cod, plaice, flounder, are the preferable. On the other hand, the red-flesh fish, i.e., salmon, mackerel, herring, sprat, pilchard, eel, etc., contain much fat, and are more likely to upset the “queasy” stomachs of the “gouty.”
But fish, it must be recollected, is less stimulating and satisfying than the flesh of birds and mammals. If wholly denied butcher’s meat and restricted to white fish, the subjects soon tire of it. It is best to prescribe fish for one meal, say lunch, and in addition one type of meat for dinner. Also it is important even in white fish to choose those most easy of digestion, viz., sole, whiting, or flounder, in preference to cod and haddock. Above all, let the fish be fresh, and not “out of season.” Again, fish which is dried, salted, smoked or pickled, is much less digestible than when fresh. If, even when taken in moderation and only occasionally, it has been found to upset digestion, then abstinence is the better course. Caviare is, I think, best abstained from, and hard or soft roes generally only taken in strict moderation.
As to shell-fish, they have the reputation of being most unfriendly to the “gouty.” Toxic symptoms after lobster and crab are held to be more common in their instance than others. But many are, I fear, ready to extend a personal idiosyncrasy on the part of some particular “gouty” subject into a law for all “gouty” subjects. I myself have seen no harm follow them when taken in moderation, this as regards the fleshy parts, more digestible in the lobster than the crab. It is, I think, wise to abstain from the spawn of the female lobster, still more from the sauces for which it is so largely used. As to oysters, I do not think there is any[347] objection to a “gouty” individual eating them raw, and when “in season,” but in moderation.
In conclusion, there is, in the matter of flesh or fish, no rule applicable to all “gouty” persons. Far from being harmful, it is both necessary and beneficial if taken in moderation. No small part of the objections raised to red meat is referable to the other rich foods that often accompany it rather than to the meat itself.
Carbohydrates.—If it be wrong to withdraw recklessly all proteins, it is no less inadvisable, in the absence of special indications, wholly to eliminate sugar or starchy foods. Nevertheless far more often than not “gouty” subjects get the impression that if they wholly eschew sugar all will be well. Latterly, too, I have noticed that the ban is being extended to starchy foods also.
Surely this as a routine procedure is wrong, the more so if, as too often happens, the unhappy subject is left without any guidance as to how long he is to suffer this deprivation. As a temporary measure it is often beneficial. But “gouty” subjects form no exception to the ordinary law that if nutrition is to be maintained, their diet must contain a due proportion of the main groups of foodstuffs. A “due” proportion, not excess, for though quâ uric acid carbohydrates may appear ideally suitable, yet the “gouty” are unfortunately no more immune than others from the dyspeptic disturbances that almost infallibly ensue when sweet foods are taken immoderately.
It is this tendency in some “gouty” subjects to amylaceous dyspepsia that has been wrongly extended into a law for all gouty subjects, whether they exhibit any carbohydrate intolerance or not. The only law is that for the “gouty,” as well as for the non-gouty, carbohydrates, whether taken as starch or sugar, are harmful if eaten to excess.
With this reservation, bread may be given as crisp toast, or rusks, or in the form of Zwiebach. Nor is there any objection to milk puddings—sago, tapioca, etc.—always provided that they are found digestible when taken in moderate quantity. Similarly in regard to sugar there is, as Sir Archibald Garrod says, “no reason to believe that to a gouty man a lump of sugar is poison, and provided that it is digestible it must surely be immaterial whether the allowance of carbohydrates be taken in the form of sugar or starch.”
Fats.—Apart from obesity, there does not seem to be any scientific reason why fats should be denied to the “gouty.” All depends on their digestibility, and in this they display variations. The fat of ducks and geese is well dispensed with in favour of bacon fat and[348] pork fat, which are much more digestible. The fats of meat, when roasted or browned, are best avoided.
Similarly there is no harm in a moderate amount of butter or cream, but fatty sauces and soups are, I think, best refrained from. Ebstein considered the best form of fat for the gouty was good fresh butter. As to cream, Sir James Goodhart, discussing the treatment of uric acid, observes: “In strict moderation it is seldom hurtful, for there is very little in the common objection that it makes one bilious. Those who avoid it are commonly ‘bilious’ because all their organs are starved.” But he makes this further observation for our guidance, that “after middle age cream taken in any excess may associate itself in some with the output of uric acid.”
Vegetables.—The various green vegetables are eminently suitable for the “gout,” not so much on account of their nutritious qualities, but because of the important inorganic salts they supply, notably salts of potash. They give a wholesome variety and relish to food, render the urine more alkaline, and do not favour the deposit of fat. Their indigestible residue, too, stimulates the intestinal coat, and so promotes regular action of the bowels.
Cabbages, greens, savoys, Brussels sprouts, cauliflower and broccoli are familiar examples. These, provided they are fresh and well cooked, are preferable to root vegetables, with the exception of potatoes. Nor must we overlook the fact that green leaves are rich in fat-soluble vitamine. Fortunately, too, in the case of this particular vitamine, the loss involved by ordinary cooking is not serious. Spinach, too, is rich in vitamines, and is laxative, but, being rich in oxalates, is contra-indicated in oxaluria. Sorrel, by reason of its acid oxalates, is also undesirable under such conditions, and the same is true of rhubarb. Tomatoes also in former days were forbidden in gout under the erroneous idea that their content of oxalic acid was high. Cucumbers, I think, when eaten raw, are apt to upset “gouty” people. Asparagus and onions should be taken sparingly, as they are rich in purins.
For “gouty” subjects, of all vegetables, the cruciferous or cabbage tribe is the most suitable, provided they are young, fresh, well cooked, and taken in moderation. In addition to its rich vitamine content, cabbage, like cauliflower and lettuce, is almost purin-free. The excessive intake of meat may often to some extent be counteracted by encouraging such gluttons to eat freely of green vegetables. In this way we obviate that sinking sensation which habitual overeaters suffer on limitation of their pabulum. Lastly, vegetable soups are most suitable,[349] preferably those easily digestible, relatively poor in purins, or rich in potassium salts.
Of the roots and tubers even of potatoes the “gouty,” I think, should eat sparingly. The large percentage of starch in potatoes is apt to upset those of feeble digestion. Much depends on whether they are “mealy” or “floury,” and not “waxy” and “watery.” Steaming is the best method of cooking them. Turnips are best abstained from, and also carrots, parsnips, beetroot and radishes, save at any rate in minimal quantities.
Lastly, the legumes—peas, beans, lentils—because of their high purin content, should always be partaken of sparingly, though perhaps it may yet be found that their purin content may be more than compensated for by their contained vitamines. The edible fungi, mushrooms and truffles are best dispensed with.
Fruits are a valuable food for the “gouty.” They impart alkalinity to the urine, and promote intestinal action, always provided they are not partaken of immoderately or when unripe or overripe, when they are apt to set up gastro-intestinal irritation.
Most fresh ripe fruits are wholesome. Their content, too, of vitamines cannot be overlooked, especially that of oranges. Moreover, the fact that vitamines, as a rule, are destroyed at cooking temperatures seems to indicate that some uncooked food should on principle be taken daily by the “gouty” as well as others. Raw ripe fruits in this respect, like salads, have an advantage over cooked fruits or vegetables.
In my own experience I do not know that there is any fruit, even strawberries, that will infallibly disagree with the “gouty.” One meets now and again with gouty subjects who are unable to eat certain fruits with impunity, but one meets with quite as many of the same idiosyncrasies in the non-gouty. The objections to certain fruits, e.g., strawberries, as to certain vegetables, e.g., asparagus, are largely theoretical rather than practical. Let the subject’s own experience be your guide in this matter, or if he be unobservant, teach him to observe for himself what fruits, if any, disagree with him.
With this reservation I am of opinion that, taken in moderate quantity, fruits are most useful constituents of diet for the “gouty.” In some cases it will be found that they cannot take fruit when mixed up with other food, but both enjoy and derive benefit from it when taken by itself. It is well, again, in others to restrain their immoderate indulgence in lemons, as these frequently, as Sir James Goodhart pointed out, upset gastric or intestinal digestion. It is advisable also to warn them that plums, currants, gooseberries, and other fruits containing large[350] quantities of free acids are apt to have the same effect, while the melon, too, is prone to give rise to gastric disturbance. Peaches and nectarines, on the other hand, are eminently suitable for the “gouty,” also apples, pears, oranges, grapes, cherries, etc.
Condiments.—These substances give a flavour and relish to food, while their carminative properties stimulate appetite and favour digestion. On the other hand, their excessive use is a potent source of gastric irritation. Thus, for example, they are valuable in atonic dyspepsia, though liable to aggravate a condition of chronic gastritis.
The most important and most extensively used is common salt. Some incline to think that its use by persons of the “uric acid diathesis” is prejudicial. But unquestionably it is a necessary and wholesome article for the “gouty” when taken in moderation. In cases of gout complicated by hyperchlorhydria strict moderation in or abstinence from salt seems indicated, this because, the HCL of the gastric juice being wholly derived from the chlorides of the blood, it seems irrational to increase the supply. Some therefore forbid its use both as a condiment or in the cooking of food, making the subject depend on the salts naturally present in foodstuffs.
Vinegar, I am sure, upsets some “gouty” persons’ digestion, and I think Sir Dyce Duckworth is right when he counsels abstinence therefrom. Thus some “gouty” subjects can digest raw cucumber, but not with vinegar. Others find salmon if combined with the same condiment upsets them, but not without. As to the various other condiments—mustard, pepper, horseradish, etc.—there is no objection whatever to their use by the “gouty” in moderation and in the absence of any definite gastric disorder.
So much for our consideration of the individual foodstuffs—their suitability or not—for the subjects of gout. That such a general survey is advisable may perhaps be conceded, but in so far as it may approximate to fixed rules it savours of evil, this at any rate as far as the dieting of dyspeptic derangements of the “gouty” is concerned. To bring into prominence my point, I would lay down the postulate that there is no specific form of “gouty” dyspepsia.
The gastric derangements met with in gout are in no sense peculiar thereto. In other words, they present no symptoms specific of gout, despite the term “gouty dyspepsia.” The term “hyperacidity” as commonly invoked is far too laxly used in regard to “gouty dyspepsia.” The “acid risings” of the “gouty” are of two kinds. Hyperacidity may be due to organic acids,[351] butyric, lactic, or acetic, the outcome of fermentation, or the condition may be one of hyperchlorhydria, or excessive secretion of HCL.
Hyperacidity due to organic acids is met with in some cases of atonic dyspepsia, chronic gastritis, and dilatation of the stomach. The free HCL is either diminished or absent. Differentiation of this type from hyperchlorhydria may be impossible without examination of the stomach contents.
Hyperchlorhydria per se sometimes occasions pyloric spasm, and minor degrees of dilatation follow, this the more commonly as the subjects of gout are middle-aged or elderly. In others the dilatation is part of a general neurasthenia from which the “gouty” no more than others are immune.
Again, gout of long standing is often associated with chronic gastric catarrh. Such is very common in beer-drinkers or men employed in breweries. A state of atonic dilatation of the stomach is a common sequel. In these cases of chronic gastritis in the “gouty” the free HCL may be normal, diminished or absent. Eventually, as the result of oft-repeated gastritis, the parts involved undergo widespread fibrotic degeneration. Also we have to recollect that the “gouty” are very subject to obstinate gastralgias.
We see therefore that the “dyspepsias” of the “gouty” may be not only of varied nature, but may also demand differential dieting at different phases of their evolution. The subject in the early stages of his gout may suffer from hyperchlorhydria, while later chronic gastritis may ensue, with the reverse condition, hypochlorhydria. The protein dietary suitable for the former has in the presence of the latter to be replaced by carbohydrates, despite their tendency to fermentation. Again, if either condition be complicated by dilatation other exigencies must be met. The meal content must be light, not bulky, and the fluid intake restricted.
Again, the foregoing gastric disorders may be complicated by glycosuria or albuminuria, each with separate dietetic indications. How inevitably futile then must be any attempt at stereotyped diet for the “gouty.” In short, the dyspepsias and other morbid states of the “gouty” call for eclectic, not routine, dieting, and to this end I append a few suggestions.
Amylaceous Dyspepsia.—Not a few “gouty” subjects suffer from atonic dyspepsia, with acidity due to organic acids arising from fermentation. Frequently it appears to be the outcome of[352] some previously prescribed regimen forbidding all flesh food, or of too frequent or irregular meals or habitual overfeeding, food-bolting, excessive smoking, etc. Correction of such faulty habits is an essential prelude to any dietetic rules.
In such cases it is advisable to reduce the intake of starchy and saccharine foodstuffs, such as bread, potatoes, pastry, sugar, milk puddings, and the like. Bread should be stale, or dextrinised by dry heat, as in thin toast and rusks. Potatoes, if taken, should be in the form of purées. Sweet dishes should be partaken of sparingly, if at all. They should be encouraged to take the more digestible forms of meat and the lighter kinds of fish. Green vegetables and fresh ripe fruit, raw or cooked, are valuable. Fats of the more digestible sorts are also desirable. Grilled but not fried fat bacon is easily digested.
As to beverages, light China tea is more suitable than strong Indian kinds. Frequently I have found substitution of cocoa most beneficial. But in any case the amount of fluid at meal-times should be restricted.
As a guide to the formulation of a dietary in such cases the following may be suggested:—
On awaking in the morning a tumbler of hot water should be slowly sipped. A squeeze of lemon may be added if liked.
Breakfast.—Boiled or plainly grilled sole, whiting, or flounder, or a slice of crisp grilled bacon or lean cold tongue, or a soft-boiled egg. A slice or two of crisp dry toast or stale bread and a little butter. At close of meal sip slowly one cup of weak China tea, or the same of cocoa or milk and water.
Lunch.—Chicken or game, or lamb, mutton, or beef, hot or cold, roast or boiled. Gravy to be free from fat. One only of the former kinds of meat to be taken with a reasonable quantity of tender, well-boiled vegetables. Spinach, kidney or French beans, sea or Scotch kale, vegetable marrow, or salad may be taken, but without oil, vinegar, or beetroot. Dry toast or rusks. Half a tumbler of water sipped after eating.
Afternoon Tea.—One or two cups of weak tea with milk or one cup of cocoa.
Dinner (two courses only).—Fish of the kinds allowed for breakfast without potatoes, or a slice of any tender meat, e.g., saddle or loin of mutton or thick part of an underdone chop, or small portion of fresh game, without bread sauce or crumbs. One or two slices of stale bread or dry toast. A little well-stewed fruit or custard, junket, or jelly. Half a tumbler of water with from one to two tablespoonfuls of spirit if desired.
If there be any suspicion of chronic gastritis, condiments and stimulants must be renounced, but not in purely atonic dyspepsia,[353] in which they are of value. In either disorder the patient should abstain from salted and cured meats, tinned foods, pastry, sweets, raw vegetables, and cheese. Before retiring a tumbler of hot water with a squeeze of lemon may be sipped slowly.
Hyperchlorhydria.—This, the true “acid gouty dyspepsia,” is the most troublesome type of dyspepsia met with in the “gouty.” Regulation of the diet is the best means whereby to combat the excess of HCL in the stomach. All irritating spices or condiments, mustard, vinegar, etc., should be avoided. Salt especially should be used sparingly or wholly abstained from. As a rule, alcoholic stimulants are not well borne, and may, in the absence of special indications, be prohibited. In a limited number of instances a light wine may be allowed as a stomachic. To avoid irritation, hard substances, such as nuts, should be interdicted, and food thoroughly masticated, and taken neither too hot nor too cold. Bolting large morsels of food may readily excite pyloric spasm.
In these cases of superacidity the most suitable foods are proteins, which combine and neutralise the excess of acid. A liberal meat diet consisting in the main of chicken, beef, mutton or ham, is indicated. Also fish, eggs, hard or soft boiled, are permissible. Farinaceous foods are not well tolerated, and if given must be of the most digestible kind. Vegetables should be mashed and strained to rid them of cellulose, and only the more digestible kinds taken, and in the form of purées. Fats tend to lessen acidity, and are therefore indicated in the form of butter, cream, olive oil, and such like. Of beverages alkaline and mineral waters, Apollinaris, Seltzer, and Vichy, prove very beneficial. Their contained carbonic acid exerts a sedative effect and diminishes the secretion of acid. Milk or stimulants may be profitably diluted therewith.
Coffee is best abstained from, and cocoa and tea freshly made with half milk substituted. Soups are best avoided. If with the hyperacidity there be associated any degree of atonic dilatation, the fluid taken at meals should be restricted. Also in this instance the food should be taken in small quantities and at frequent intervals. Otherwise these cases of hyperacidity do well on three meals per diem provided they are separated by an adequate interval.
If the foregoing measures prove ineffectual the carbohydrate content of the food should be withdrawn, and the patient limited to a strictly meat diet, taken either raw or very slightly cooked. It goes best when finely minced or grated on stale bread. According to Osler, an ample dietary is afforded if three and a quarter ounces of meat and two medium slices of stale bread be taken[354] three times a day, with a glass of Apollinaris water or soda-water, or what in this authority’s opinion is just as satisfactory—spring water. For the bread a little dry toast or twice baked (Zwiebach) bread may be substituted. Some advocate the meals being taken wholly dry, or with two ounces of fluid only; but two hours later a half to two pints of hot water should be slowly sipped. A month or six weeks of such a diet will usually suffice, after which a gradual return may be made to a mixed dietary.
Apart from the binding of excess of acid by the protein substances and consequent relief of discomfort, the so-called Salisbury diet has other advantages. Abstraction of the carbohydrates obviates intestinal fermentation and flatulence. Also, the food administered being small in bulk, and taken more or less dry, a dilated or atonic stomach tends to revert to its normal size.
In conclusion, in regard to these cases of hyperchlorhydria it must be realised that not only their diet and the manner of their eating, but their general habits of living, must also be revised. They must be warned of the great tendency to recurrence and the necessity of orderly and regular habits and of strict abstemiousness in regard to not only alcohol, but tobacco. The nerve element in some of these cases is very pronounced, and sometimes nothing short of a rest cure will suffice.
Hypochlorhydria.—Chronic gastric catarrh due to overeating and overdrinking is not an infrequent complication of gout in its later stages. Such subjects suffer with daily or periodical vomiting of stringy mucus. In such cases the HCL of the gastric juice is deficient or absent. Consequently protein foods are digested with difficulty, and carbohydrates are more easily disposed of. The lighter forms of meat, such as chicken or fish or raw scraped beef, are indicated. Nor, in view of the chronic nature of the derangement and the necessity of maintaining nutrition, should we hesitate to allow such “gouty” subjects other digestible forms of meat, such as sweetbreads, brains, etc. Fats also and carbohydrates up to the limit of tolerance should be allowed. Ingestion, however, of fluid at meals should be reduced as far as possible. Of beverages milk, and especially buttermilk, is particularly suitable.
Despite the deficiency of HCL, they may suffer much with acid eructations or flatulency owing to organic acids arising through fermentation. If so, farinaceous foods must be restricted, particularly potatoes and the coarser vegetables, while of course pastry and sweet foods should be prohibited. Bread should be taken in the form of dry toast or rusks.
Hyperuricæmia.—As far as is known, the endogenous moiety of urinary uric acid is uninfluenced by diet. On the other hand,[355] as has been shown in previous chapters, the exogenous fraction can be reduced by suitable dieting. To this end, in order to prevent the intake of food containing uric acid precursors, the purin-free dietary was devised. Under such a regime both red and white meats must be proscribed, also fish and the legumes—peas, beans, lentils, asparagus, onions and oats—as these last are all rich in purins. Tea, coffee, and chocolate must also be eschewed.
In lieu of these substances more or less poor in purin bodies must be exclusively taken: milk sour or curdled, buttermilk and whey, white bread, butter, cheese, eggs, rice, tapioca, macaroni, sago, cereal foods, nuts and fruit. Even strawberries are permissible, for Weiss noted that the addition to an ordinary diet of 1 lb. of strawberries, 1½ lb. cherries, or 2 lb. of grapes, diminishes the amount of uric acid excreted by almost 50 per cent. With the exception of those interdicted above, all vegetables are allowable, cabbage, cauliflower and lettuce being almost purin-free.
Personally I am not enamoured of purin-free diets for the “gouty,” any more than I am of the purely vegetarian regime, so extolled by some as the means of averting gout. The purin-free diet, if I may say so, smacks too much of the laboratory, its raison d’être the baseless assumption that uric acid is the fons et origo mali.
I am very doubtful of the intrinsic merits claimed for it. I do not think it exerts a direct or specific anti-gouty influence. Such advantages as do accrue are referable, in my opinion, to the greater measure of intestinal asepsis that such a regimen promotes. It is suitable, therefore, in cases in which there are evidences of intestinal putrefaction. Distinctly unappetising, it is useful, too, as a disciplinary measure for those prone to overeating.
Its advocates claim that it tends to diminish the excess of uric acid in the blood. But, as was pointed out when dealing with uricæmia, variations may occur in the uric acid content of the blood independently of diet. Moreover, acute attacks have been observed even when the uric acid blood content was at a sub-normal level.
To place all “gouty” subjects on a purin-free diet as a routine procedure is to my mind wholly impermissible. The fact that prolonged adherence thereto is usually found impracticable is surely an indication that we are violating nature’s laws. It may prove beneficial in a few isolated cases, and then only for a time; but in the vast majority of instances it is frankly prejudicial. Given a carefully revised mixed diet, it will, in my experience, be rarely, if ever, necessary to subject “gouty” individuals to this dietetic penance.
The Reduction of Obesity.—Unfortunately obesity is a common associate of gout, and with it not infrequently comes glycosuria. Middle-aged “gouty” subjects have in their youth often been given to strenuous exercise. But notwithstanding that with advancing years their capacity and disposition for exercise lessens, they nevertheless take the same amount of food as of yore.
It is most difficult to make them realise that, with the alteration of their habits, the amount of food which at one time was but adequate is now excessive. I have found it useful to remind such of Ebstein’s dictum, “The gouty who have grown old in spite of their disease are almost always those who have been able to avoid obesity.” Still it is only fair to add that in some of the gouty obese no accusation of overeating or overdrinking can be lodged, and their aptitude for fattening seems often hereditary.
Reduction of the body weight when excessive in gouty subjects is hardly, I think, sufficiently emphasised. The victim himself is but too often convinced, however, that he ought not to be “lowered,” and sometimes, I think, infects the physician with his apprehensiveness on this score. But, as Harry Campbell rightly observes, “people do not die of starvation so easily as is generally thought, and it is very difficult for the physician to kill his patients in this way.” Yes, and, on the contrary, how often do gouty people “dig their graves with their teeth.”
Again, there is the static element to be considered in these cases. The articular manifestations of gout are by preference located in the lower extremities. It is clear then that excessive stoutness, particularly if of recent development, must inevitably throw increased strain on the already-hampered articulations. The feet of the “gouty” are their most vulnerable point, and the number who are flat-footed is noteworthy. In the presence of this static fault, “strains” or “sprains”—those fertile excitants of gouty outbreaks—are much more liable to occur, and I myself feel sure that in this way the frequency of attacks in the feet and, for that matter, in the knees also, is favoured.
Lastly, the gouty obese is frequently elderly, his vessels somewhat the worse for wear. Also he may show signs of cardiac weakness or a trace of albumen or sugar in his urine. Even so his weight should be reduced if possible. His watchword should, like Falstaff’s, be:—
There are so many dietetic methods of treating obesity that[357] they cannot all be outlined here. The Banting method, like the Salisbury, is too severe for the average patient, while the Weir-Mitchell method has one cogent objection to general adoption, viz., the expense entailed. Nevertheless as regards the last-named, or skim milk, method, it certainly achieves marvellous results in those cases in which there is a mere accumulation of fat without any other complication.
Generally speaking, however, one has to be content with the following suggestions: All varieties of lean meat may be taken, as well as poultry, game, and fish, subject to idiosyncrasies and digestibility. Meat may be taken twice daily, not exceeding six ounces at one time. All starchy and farinaceous food is to be reduced to a minimum or wholly forbidden. Leaf vegetables may be taken freely, but the roots and tubers, such as potatoes, abstained from. Bread should be largely reduced in quantity and thoroughly torrified. Sugar must be prohibited, and saccharine or saxin substituted. Fresh fruits may be eaten, but milk should be avoided, also cream, or very strictly limited. Where feasible, it is often a good plan if the subject can for one day a week content himself with a diet of skim milk.
Alcohol, as far as possible, should be rigidly excluded, or only a very moderate quantity of good whisky or a light wine, such as hock or Moselle, permitted. As a rule, only a little hot water should be sipped at meals. But I think in these subjects of so-called “uric acid diathesis” it is well not to restrict their fluid too markedly. A pint of hot water may be drunk one and a half hours before each of the three meals, and one pint more half an hour before bedtime. Weak hot tea may be substituted, as many subjects find a difficulty in drinking so much plain hot water at one time. If while on this regime the subject lose weight and pari passu gain strength, all is well. If he lose weight and therewith lose strength, further reduction or its continuance is contra-indicated. It should be recollected that the reducing effects of dieting may be markedly enforced by an open-air life, with riding or other outdoor exercise.
Glycosuria.—This condition conjoined with obesity is not uncommon in middle-aged “gouty” subjects. It is of benign type, and the amount of sugar excreted is usually reduced to a mere trace by extraction of the carbohydrates in the food. Thus, we should forbid, e.g., sugar, pastry, sweet wines, and dishes made with flour, rice, or sugar. In these cases von Noorden considers that it is better after reduction of the amount of sugar by dieting to a mere trace to be content rather than to get rid of it wholly by a rigid elimination of all carbohydrates. To this end the patient may be allowed to eat a limited amount of bread, potatoes,[358] and other vegetables, while he may eat freely of butter, bacon, and other fats.
One should recollect also that these “gouty” glycosurics have periods of enhanced carbohydrate tolerance, this, as Burney Yeo pointed out, quite “independently of any therapeutic interference.” In short, at times they can take quite a considerable amount of carbohydrates without passing sugar in their water.
Needless to say, the regime must be adapted to each individual case. The urine should be examined frequently, and the influence on the sugar content of different articles of food noted; also the weight should be frequently taken. It is certainly unnecessary in gouty glycosurics to wholly banish the carbohydrates. By such a plan we are more likely to do material injury than by exceeding by a little their limits of tolerance. Our remarks of course apply strictly to alimentary glycosuria. But we should also remember that exceptionally a case of gouty glycosuria may emerge into one of true diabetes.
Albuminuria.—In the so-called “gouty” contracted kidney, if the amount of albumen in the urine be very large, or when there are symptoms of nephritis, a milk diet for a few days or a week at a time may be given. More often it is unnecessary, or it is frequently badly borne or rejected. Consequently a modified milk diet has to be adopted, and a gradual return to a mixed diet permitted, provided no increase in the quantity of albumen ensues.
But at the same time it must be realised that no rigid rule can be laid down for “gouty” albuminurics. As a guide to the suitability of a diet it is better to rely on the general condition than on variations in the amount of albumen. For, as Professor H. Andrew Smith, of New York, long since said, “if on changing from a non-nitrogenous diet to a nitrogenous one we find a general improvement in the patient’s condition, it is an evidence that the change is beneficial, no matter if the albumen fills a larger portion of the test tube. On the other hand, if we cut off a large proportion of animal food from the diet, and our patient grows more dyspeptic, weaker, more anæmic, more dropsical, it is nothing to the point that only one half or one-third of the former quantity of albumen is found in the urine; the change has done harm, and the sooner we change back again the better. We should, above all things, seek that diet for the patient which he can best digest and assimilate, for we may rest assured that the products of faulty digestion and assimilation will irritate the kidneys more than any amount of normal material they may be called upon to eliminate, while, at the same time, the general system will suffer from lack of support.”
Lastly, up to this juncture all our suggested dietetic modifications[359] have been in the direction of reduction or abstinence. But we must recollect that in practice we find that not a few gouty persons are most careful and prudent in diet. They commit no indiscretions, but nevertheless their gout is still with them. They are of the asthenic type, thin, pale, sallow, and given to neuralgic forms of fibrositis. They do not want “lowering”; to curtail their food is harmful. In their instance, with due respect to digestive idiosyncrasies, a more or less generous diet should be prescribed. Let them forsake dietetic schedules and follow their instincts. Let your advice be that of Sir William Temple: “Simple diet, limited by every man’s experience to his own easy digestion, and thereby proportioning as near as can be the daily repairs to the daily decays of our wasting system.”
It cannot be gainsaid that the beneficial effects of so-called “water cures” are in great measure referable to the increased amount of water ingested during their progress. Absorbed in the main in the small intestine, it passes into the general blood stream, whence it is excreted viâ the skin, kidneys, lungs, and fæces. Its elimination through these various channels sufficiently accounts for its value as a means of flushing the bodily tissues and hastening the excretion of retrograde and toxic products. Indeed, its efficiency as a depurative agent cannot be over-estimated, and nothing is more beneficial for the subjects of a “gouty” diathesis than regular consumption of an adequate quantity of this admirable solvent.
By general consent, the water ingested should be preferably hot. Water of a higher temperature than that of the blood stimulates the hepatic cells, and promotes biliary excretion. It has been shown, moreover, by Glax that while draughts of cold water raise vascular tension and diminish pulse frequency, on the other hand hot water diminishes arterial tension and accelerates the pulse rate.
It is also claimed that the increased elimination of water viâ the kidneys is correlated with an augmented output of the solid constituents of the urine; that the phosphates, sulphates, sodium chloride, and likewise urea are for the time excreted in greater amounts.
The point at issue, however, is whether or no this increase in the amount of urea excreted can be held to indicate enhanced tissue change in the nitrogenous elements in the body fabric.
Winternitz claims that it does, in contrast to Von Noorden, who holds that nitrogenous tissue change and the formation of urea[360] and uric acid are uninfluenced by the amount of water imbibed. In further contradistinction some contend that following the ingestion of water the excretion of uric acid is diminished.
Fortunately for “gouty” subjects, the beneficial effects of water flushing of their systems occur independently of any coincident increase in their uric acid output. This is true even of mineral waters. Thus Bain and Edgecombe noted that following the ingestion of the old sulphur water of Harrogate the excretion of uric acid was diminished. Nevertheless cases of “gout, especially of the asthenic type, derived the most marked benefit from its use.” “This fact is mentioned,” they say, “because some writers attach the greatest importance to an augmented excretion of uric acid in the urine as a necessary concomitant of successful treatment. This we firmly believe to be an erroneous view.”
Indeed, ignorant as we are of the exact etiology of gout, we must at any rate provisionally attribute the proved efficacy of water-drinking in gout to its flushing action on the tissues, its furtherance of the excretion of waste products. Nor can we doubt that the ingestion of hot water, involving as it does equalisation of its temperature with that of the body, must exert a profound and intimate effect upon processes of cell nutrition. Moreover, through its solvent and penetrative quality, its mineral or chemical constituents are enabled to penetrate freely the interstices of the tissues throughout the economy.
It is, therefore, well to advise “gouty” subjects to drink daily on rising from eight to ten ounces of hot water, repeating the same half an hour before lunch and dinner, and finally the last thing at night. For in my experience “gouty” subjects on the whole do better if they drink some time before their meals than during their progress. It is an old belief that hard waters are unsuitable for the “gouty.” Sir Dyce Duckworth believed so, and Sir Charles Scudamore in 1823 delivered himself as follows: “The kind of water denominated hard has always been considered as unfriendly to health, and especially injurious to persons afflicted with gravel or stone. Many probably imagine that the earthy salts which it contains assist in making up the mass of the calcareous concretion.”
But more probably, as Sir Archibald Garrod suggests, the old view that tophi were composed of chalk had probably something to do with the origin of the tradition. That hard waters may be noxious in so far as they favour constipation may be granted. But, on the other hand, we have to reconcile with this the awkward fact that earthy or calcareous waters, e.g., those of Bath, etc., are among those whose efficacy in gout is beyond question.
Again, how can we reconcile with this view the prevalent[361] practice of placing “gouty” subjects, temporarily at any rate, on a milk diet, this although milk is especially rich in lime? That a regime of milk in the young and robust “gouty” subject is often extremely beneficial is beyond question. On the other hand, it is equally certain that others do not thrive thereon. In prescribing it, therefore, we must be guided largely by personal idiosyncrasy.
Lastly, as to tea and coffee, there is a theoretical objection that both contain methyl purins. Albeit, it must be seldom indeed that gout is met with in pure tea-drinkers who at the same time abstain wholly from alcohol. Either tea or coffee, if taken apart from food, usually agrees well with the “gouty,” always provided that they be well made and not over-strong. Of the twain tea is, I think, more generally suitable than coffee, and where both disagree cocoa is an excellent substitute.
Said Sir Thomas Watson: “I am sure it is worth any young man’s while who has had the gout to become a teetotaler.” Few will gainsay the wisdom of this advice. But I would fain go further and impress on gouty parents the incumbent duty of bringing up their children as total abstainers. For gout, once avowed, has a vicious tendency to recurrence. The illustrious Sydenham, I think, would have approved of such advice: “Water alone is bad and dangerous, as I know from personal experience. When taken as the regular drink from youth upwards it is beneficial.”
When, however, gout attacks a man for the first time in middle or late life, most authorities agree that an abrupt change of habit in respect of stimulants is of questionable wisdom. In saying this, I do not for one moment mean that excess should be approved, but that I do not believe that the enforcement of total abstinence is prudent. In such cases restriction, not total elimination, is the better course. One must recollect, too, that total abstainers are by no means exempt from gout, while, on the other hand, many, if not the majority, of drunkards are. The latter have their penalties, cirrhosis, etc., but not inevitably gout.
I agree that gout is infinitely more common in those who take alcohol than in those who abstain therefrom. But nowadays, at any rate, the “gouty” as a class cannot with fairness be ranked as among the confessedly intemperate. With relatively few exceptions, they belong rather to those given to what may be termed the legitimate use of alcoholic beverages. My conclusions then are that:—
(1) The children of “gouty” parents should be brought up as total abstainers.
(2) The incidence of a first attack in a young man should be the signal for abstinence from alcohol in all forms.
(3) Given its occurrence in an older subject who has used alcohol but sparingly and stands in no need of it as a stimulant, the same total abstinence should be inculcated.
(4) In middle-aged or old subjects habituated to the use or abuse of alcohol abstemiousness, not abstinence, is the safer course.
Malt Liquors.—I think we should distinguish between the “strong” and the “mild” varieties, even as we do between “heavy” and “light” wines. “Strong” malt liquors unquestionably are most provocative of gout, and it is not without significance that most “gouty” subjects have, frequently on their own initiative, abandoned their use. So much importance, indeed, do I attach to this, that if I were called to formulate any rule in the matter of alcohol for “gouty” subjects it would be the unsuitability of “strong” malt liquors, which not only increase the tendency to recurrence of the paroxysms, but appreciably lengthen their duration.
The prefix “strong” I use advisedly, as the volume of alcohol contained in different beers may vary by as much as from 1 to 10 per cent. Thus Scotch ale contains as much as 8·5 per cent., and, generally speaking, all “old” ales are usually “strong” ales. Albeit, to condemn malt liquors unreservedly is, I am sure, inadvisable. The truth is that in respect of their gout-inducing power malt liquors, like wines, display great variations.
Thus “strong” malt liquors, like “heavy” wines, are markedly provocative of gout, whereas the “milder” ales, like the “lighter” wines, are relatively impotent in this respect. Said the elder Garrod on this point: “The lighter wines, as claret, hock, and Moselle, although capable of acting as the exciting cause of an attack in gouty subjects, have when taken in moderation but comparatively little inducing power, and in this respect rank with the weaker kinds of malt liquors.” In this connection is it not significant that gout is extremely rare among agricultural labourers, who drink freely of that popular and ancient beverage mild beer? Sydenham on this point is very definite: “This is a rule for the gouty: they may take those liquors which neither chill the stomach nor intoxicate in any moderate quantity. Such[363] is the small beer in our own country, which in foreign countries may be replaced by weak wine-and-water.”
I hold no brief for alcohol, but of the twain I am sure it is wiser to advise a poor man, even though “gouty,” to stick to “mild beer” rather than urge him to betake himself instead to “ardent spirits.” For the rich man, too, while in his prime and still capable of vigorous exercise, I am firmly of opinion that, with due deference to idiosyncrasy, a mild beer not containing more than from 3 to 6 per cent. of alcohol will do him not more, but less, harm than whisky.
I have yet to learn that the working man who has gout and sticks to mild, sound beer in moderation gets attacks more often or more severely than the rich man who affects whisky. “It must,” as Sir Archibald Garrod observes, “be confessed that among hospital patients who could not, if they would, follow out any strict rules of dietary, who seldom pay heed to our advice that they should give up beer, and who, as soon as an acute attack is over, revert to their previous habits of life, the course of gout does not seem to differ materially as regards the character, frequency, and severity of the attacks from that followed in people who are able to adjust their living according to the best advice to be obtained.”
I think then in this matter of malt liquors, their suitability or not for “gouty” subjects, we should be well advised to reconsider our attitude. In other words, I would urge that we draw a distinction between “strong” and “mild” malt liquors. By all means let us continue to condemn the “heavy” varieties, while not extending the ban to the “lighter” forms. I would, however, make the following reservations: that—
(1) It be a “light” beer, in which the “bitter” principles predominate, and the extractives are small in amount[61];
(2) It be “sound” and not “turned” beer, and of course free from any possibility of lead impregnation;
(3) It be taken in moderation, not exceeding one to two pints per diem;
(4) The “gouty” subjects by whom it is taken be physically active;
(5) Due respect be paid to personal idiosyncrasy, reserving its use for those in whom its effects are definitely stomachic and tonic, while discountenancing its use when followed by heaviness, drowsiness, and biliousness.
As to cider, there is no doubt that the partially fermented or[364] sweet variety is more harmful than “dry” or “rough” cider. Still there is no room for dogmatism even here, for a “gouty” man, if he be unaccustomed to cider, may find that, whether “dry” or not, it may provoke an attack. Sir Archibald Garrod tells us that he has known not a few gouty patients who alleged that cider suited them admirably, but he adds: “An experience of some months has usually modified their opinion on this point.”
Wines.—When we come to consider wines, we are on very uncertain ground, this especially if we base our opinion too much on the chemical analysis of this or that variety. The current belief is that the most unsuitable wines are those that contain large amounts of alcohol, sugar, or free acid. Then we discover it is not the amount of alcohol in the fluid that determines the incidence of gout and, in witness to our perspicuity, call to note the rarity of gout in Scotland, where whisky is the favourite beverage; ergo whisky par excellence is the drink for the “gouty,” and so we find ourselves in this impasse: we fulminate against alcohol as the cause of gout, and in the same breath advise our “gouty” patients to drink precisely those fluids containing the highest percentage thereof.
True, when we turn to wines we find that it is precisely those that are richest in alcohol that most potently predispose to gout, e.g., port. But seeing that whisky contains infinitely more alcohol than port, and yet is little gout-provoking, we search round for some other constituent in wine on which to lay the blame. So we decline on the varying degrees of acidity in different wines. But this again on reflection, it is decided, is of little moment. For, on the one hand, port and sherry are among the least acid wines, and yet, like the even less acid malt liquors, most productive of gout, while, on the other hand, the more acid clarets and hocks are deemed relatively harmless. Then the varying quantities of sugar in the different wines come under the ban. But here again no definite line can be drawn. For some wines most provocative of gout have a high sugar content, while others equally potent in this direction contain but small amounts.
Now the most salient deduction from the foregoing considerations is our inability at present on chemical grounds to determine why certain wines are productive, and others are relatively nonproductive, of gout. We can impeach neither the alcohol content, the acidity, nor the sweetness. For on all these points startling exceptions preclude dogmatism. Does not the clue to these varying reactions quâ gout reside in the individual, not in the character of the wine? We are far too prone to say that this or that wine is “gouty,” to say that this wine gives you gout, and that not.
The evil potentialities that make for gout reside not in this or that particular wine, but in the individual. This or that wine does not give him gout, but evokes or brings to fruition a morbid tendency already latent in him. In the absence of this inherent proclivity, it would not have elicited those specific local reactions typical of gout. But for those who would interpret this statement as approval on my part of alcohol or an absolving thereof from any part in the genesis of gout I would issue this caveat: Alcohol will not originate gout in a non-gouty subject, but it will almost infallibly in those in whom there exists by heredity an inborn tendency to gout. In short, the “gouty” are hypersensitive to the evils of alcohol; the greater the need then for abstemiousness and self-restraint.
But, to resume the thread, in the absence of any absolute chemical criterion as to the relative suitability of this or that wine for the “gouty,” what shall be our advice to the “gouty” individual on this point? In a word, his “palate” and his “stomach” are the best criteria of the wholesomeness of this or that particular wine in his particular instance. If he is in the habit of taking wine do not forthwith, as is so often done, forbid him wine in all forms and order him whisky. This is done so light-heartedly that I do not wonder that the subject goes away frequently with the idea that whisky is not only innocuous, but desirable.
The whisky-drinker is not immune from gout, and I have no hesitation in affirming that “light” wines when fine, mature, and of a good quality are, subject to individual idiosyncrasy, quite as suitable for the “gouty” as whisky. Of the many wise warnings given us by Sir James Goodhart none is more apt for the present day than the following. Discussing the “treatment of uric acid,” he observes: “I am as much as ever an opponent of the prevalent dictum, ‘You must not touch wine; you must drink whisky,’ which too often means to the patient, ‘A glass of good wine is poison; I may take as much whisky as I like, and it is harmless,’ one of the most mistaken and mischievous beliefs that ever plagued a world.”
Again, if a “gouty” man takes wine, there is always one special variety that agrees with him, and as certainly one other or more that infallibly upset him. Putting aside all preconceived ideas, find out his personal idiosyncrasies in this respect. In this way you elicit and utilise for your ends the individual’s own experience, the only experience that counts.
A man of a certain age, he generally by the time he develops overt gout has arrived at definite conclusions as to what does and what does not suit him. He will frequently tell you he has had[366] to give up malt liquors, perhaps port and champagne, and now finds that whisky, gin, or the lighter wines agree with him better. Or, as like as not, he may upset all your preconceived ideas. He may be of those gouty subjects—and they are not so few—who can drink champagne in moderation, or even a glass or two of port, daily with apparent impunity. On the other hand, a glass of claret or hock plays the mischief with him. He may, like some individuals cited by Burney Yeo, be one of those exceptional gouty subjects in whom even stout is well borne, Yeo thought largely because they habitually took daily large quantities of alkaline salts.
The sum of these erratic findings is that you must respect idiosyncrasy. It is said that the best wine for a “gouty” subject is the one that causes most diuresis. For myself, I am equally positive that the worst wine for a gouty man is that which upsets his stomach, which gives him some hours afterwards “acidity” or a feeling of “liver.” Often, too, it is not the wine, but the stomach into which it is put, that is to blame. Thus the “gouty” subject with atonic dyspepsia finds a glass of sound wine helps digestion. On the other hand, if he suffers from hyperacidity or chronic gastritis, the reverse will probably be the case.
Again, it is not the name, but the quality, of the wine that counts. It makes all the difference whether the wine taken is fine, mature, and of good quality, or some factitious, mixed, or adulterated product, passing muster, say, as claret. Fine mature clarets or red Bordeaux wines are most suitable for the gouty. But, as Burney Yeo rightly says, “a more injurious beverage than bad claret or imperfectly matured claret—and, speaking generally, all but the more expensive or most carefully selected clarets are bad—was never drunk.”
It seems opportune here to lodge a protest against fashions in wines for the “gouty.” At one time it was claret, then light white wines, Moselle, etc., and anon whisky, and even cider had its vogue. Fashions in wines, as in other spheres, postulate uniformity and lack of discrimination. Any one of the foregoing beverages may suit some particular “gouty” individual, but not all “gouty” subjects.
We have said that in some instances the wine, in others the stomach, is at fault. But intrinsically it may lie in neither, but simply in the quantity of the wine drunk. It may not, as judged by ordinary standards, be an excessive amount, but it may be excessive for that particular man. It is here that a medical man may often intervene with advantage. For a man may, quite unbeknown to himself, be really a heavy drinker, one of those unfortunates who are peculiarly tolerant of alcohol. A[367] tactful reminder of the amount he is consuming per diem will frequently come as a shock, often a very beneficial one.
Apart from this, it is, I am sure, wise to fix the daily amount. The daily habit in the “gouty” is all-important. If accustomed to take one or two glasses, and they stick to it, all may be well; but it is on the occasions when the glass grows into a half-bottle that the trouble comes. Metabolically speaking, the “gouty” subject is most unstable, and disturbance of what one may call his daily alcoholic rhythm is always perilous. Unfortunately it works either way, too, both in the matter of “too little” as well as “too much.” Here experience and sound judgment will alone enable the physician to decide how far he may tamper with long-established habits.
At other times the amount, though, strictly speaking, not excessive, is so when judged in light of the victim’s habits. He may be an intellectual worker, but sedentary, and he must either lessen his drink or increase his exercise, or he may overeat as well as overdrink—a victim of the prevalent idea that the one evil counteracts the other. Between the Scylla of overeating and the Charybdis of overdrinking there is no safe course save by way of reduction of both.
We see therefore that in the matter of the choice of a wine for a “gouty” subject there are many points to be considered. Of these personal idiosyncrasy stands first. By this criterion, and none other, can the suitability of the wine be decided. Then the state of the digestive functions, if deranged, has to be considered. Is the gastric disorder such as will be benefited or, on the other hand, impaired by wine of any sort? Again, glycosuria, albuminuria, raised blood pressure, or cardiac degeneration may intervene to complicate the issue, and so our policy in regard to alcohol has constantly to be adapted and readapted to the varying requirements of the organism.
It will be seen that I have largely refrained from specifying the wines suitable or unsuitable for the “gouty.” To have done so would have been alien to the general tenor of my remarks, convinced as I am that our trend in the matter of alcohol for the “gouty” should be more in the direction of “individualisation” than of “standardisation.” Subject to the reservations that such an attitude portends, I would proffer the following suggestions:—
As a general rule, wines which are “dry” are much more suitable for the “gouty” than those which are “sweet.” Wines are termed “dry” when nearly all the sugar of the grape is transmuted into alcohol, as in “dry” sherries. They are termed saccharine or “sweet” when the process of fermentation is[368] arrested before all the sugar has been exhausted, as in Malaga. Again, wines which are both “strong” and “sweet,” e.g., Malaga, sweet champagne, Tokay, etc., are more pernicious than those which are “strong” yet “dry,” e.g., port, sherry, Madeira.
Sir James Goodhart, discussing wines suitable for the “gouty,” confesses to a “personal leaning in favour of the wholesomeness of a glass of good old sherry in those cases where a little wine seems a judicious prescription.” With this I fully agree, and would suggest that of sherries the “gouty” should favour the “Manzanilla” rather than the “Amontillado” class. The former, save for the addition of a small quantity of spirit, are mostly shipped in the natural state; also they are light and “dry” as compared with the latter, which are generally “sweet” and full-bodied.
It is interesting to recall, too, that Sydenham regarded sherry as preferable either to Rhenish or French wines. He himself in his own person found “sack” or Canary the most helpful. “I have during the fits of the last years tried many things to lessen the symptoms. Nothing, however, effected my purpose so much as a small draught of Canary wine, taken now and then, when the faintness or sickness were most oppressive.” Here one may note that sherry was the first wine to be known as “sack” in this country, and that the wine shipped in Sydenham’s time was of the “dry” variety. Chemically the “sweet” sherry differs from the natural “dry” light wine through its relatively high content of alcohol and sugar.
Turning to port, Sir Alfred Garrod absolutely tabooed its usage by the gouty. But this appears too sweeping, and nowadays, at any rate, it is well recognised that, especially in asthenic types of gout, a glass or two of old port is well borne. Consequently in such cases we should not, in the absence of any adverse symptoms, forbid its continuance. The bad reputation achieved by port is, I am sure, a relic of the Regency. But “three-bottle” men are no longer with us, and, allowing for personal idiosyncrasy, I very much question if sound port taken in moderation wholly merits the aspersions cast upon it. I do not by that for one moment suggest its general adoption by “gouty” people, but that where an old or elderly gouty subject takes port and can be trusted not to extend his glass to half a bottle his inclination may be respected. The sugar content of port varies according to the vintage, ranging from 7 to 15 per cent., and the “gouty” man should favour the “drier” varieties.
As for champagne—a manufactured article rather than a natural wine—there is no question that, if taken at all, it should be a “dry” brand. Such contains from 9 to 12 per cent.[369] of alcohol and from 1 to 4 per cent. of sugar, whereas the “sweet” brands may hold as much as 16 per cent. All depends on the quality of the champagne, and, as Ewart wisely remarks, “it is wiser for the ‘gouty’ patient not to incur considerable risks by trying brands with which he is not familiar, though he may sometimes with impunity, and occasionally with benefit, enjoy a glass of champagne which he can trust from personal experience.”
If, on the whole, the most unsuitable wines for the “gouty” are the strong sweet spirituous or liqueur wines, on the other hand the red or astringent and white wines are the most esteemed. As to the red wines, there is no doubt that the delicate Gironde (Bordeaux) wines are par excellence the most suitable. They have sufficient body and alcohol without being heavy or fiery, while their acidity and sugar content are very low. But of course the quality of the wines varies considerably with the vintage. Subject to this, sound, well-made clarets taken in moderation and somewhat diluted with water are the most wholesome wines we can prescribe for the “gouty.”
The more full, though still not coarse, wines of the Burgundy district are by some denounced. One authority, I note, states that in elderly gouty subjects he had often found that two or three glasses of claret or Burgundy were in the course of a few hours followed by eczema. While such idiosyncrasies may obtain, it is not true of the “gouty” as a class. I should consider a “gouty” subject in any case unwise to take two or three glasses of Burgundy. But I do not hesitate to order one or perhaps two glasses somewhat diluted with water. Being a stronger and more tonic wine than Bordeaux, it is useful in the more asthenic types of gout. The pity is, of course, that the cheaper Bordeaux and Burgundy wines are so largely adulterated, while the more mature clarets are available only for the rich. As good substitutes for French wines Burney Yeo commends the red Hungarian wines, such as Carlovitz, while we may add that some of the Dalmatian wines are of fair quality and somewhat resemble Burgundy.
Reverting to white wines, these, as compared with the red wines of the Gironde, contain less tannin and more free acid. According to Burney Yeo, they exert, too, a more diuretic effect, and to remove their excessive acidity he advises their dilution with some alkaline table water. Most of the white wines come from the Rhine or Moselle districts. The Rhenish are relatively full-bodied and of marked vinosity, while the Moselle wines are mostly light and of a somewhat delicate nature. Light hocks and still Moselles are quite permissible, also the white wines of France, such as vin de Grave, all varieties of the latter being fairly “dry” and[370] light in character. On the other hand, the white wines of Sauterne, like some of the Hungarian wines—i.e., Ruster—are rich in saccharine constituents. In this respect they contrast with the Rhenish and Moselle wines. Of these last Johannisberg contains only 0·42 per cent. of sugar, Rudisheimer 0·39, Zeltinger 0·13, and Stein-Reisling 0·01, while Ruster contains no less than 21·74 per cent. of sugar.
In conclusion, I would re-emphasise the fact that, if wine be taken, the patient’s own experience is the best test as to which particular wine is the most suitable in his case. This elicited, the subject should be counselled to adhere to it, taking it only at meal-times, and establishing a rigid rule as to quantity. The least excess is harmful, and breaking of the ordinary routine in the matter of the amount drunk is a fertile source of “gouty” outbreaks. In any case the quality of the wine should be above suspicion, and if the expense is prohibitive, he had best eschew wine altogether in favour of mature spirits.
Spirits.—Brandy, whisky, and gin are the spirits most in vogue in Great Britain, and it has become an axiom with some that, if alcohol in any form be requisite for the “gouty,” the least harmful is one or other of these beverages when adequately diluted. Of the three whisky undoubtedly has found most favour, and the pernicious and far too prevalent idea is that whisky not only does not beget gout, but is actually beneficial for gout. The consequence is that many “gouty” people take far more whisky than is desirable, seemingly oblivious of the fact that, if whisky in moderation be suitable for the “gouty,” whisky in excess is as deleterious for them as for the non-gouty. In short, like any other form of alcohol, if taken immoderately, it will bring to fruition a latent gout, this, as suggested by Ford Robertson, not by the direct action of the alcohol, but by the “indigestion toxæmia” it sets up.
In advising therefore a “gouty” subject to take whisky we should insist that (1) it should be taken only at meal-times and (2) only in moderation. The habit of occasional “nips” at all times of the day should be unreservedly condemned. As to what constitutes a moderate quantity is often a difficult question to decide.
When feasible, I endeavour to limit the daily allowance to a wine-glassful, distributed over lunch and dinner. But it is quite impossible to lay down hard and fast rules in a matter in which personal idiosyncrasy plays such a strong rôle. Frequently, in addition to the above amount, one has to relent to the extent of a “nightcap,” or but too commonly one has to be content if one can compass reduction to an amount which for the particular[371] individual under review seems apparently compatible with no appreciable damage to health.
Sometimes one of the frequent accompaniments of gout comes to our assistance. It may be raised blood pressure, glycosuria, albuminuria, obesity, etc. In such cases a word in season may reduce an otherwise recalcitrant subject to reason.
Needless to say, in regard to “ardent spirits,” as to wines or malt liquors, we must, when determining the quantity to be taken per diem, review the same in light of the person’s habits, whether active or sedentary, whether associated with overeating or not. For manifestly all these bear on the point at issue.
Lastly, as to whether the subject should take brandy or gin in preference to whisky is a matter for himself to decide. Whichever suits him best is the best for him. Albeit, I confess to a leaning in favour of “dry Plymouth” gin, this being more diuretic than other spirits by reason of the juniper contained therein. But, in whatever form “ardent spirits” be taken, it is most essential that it be sound. Brandy should be of the finest quality, the whisky mature, and inferior kinds of both wholly eschewed.
The illustrious Sydenham, for more than thirty years a sufferer from gout, was clearly in doubt as to whether a cure of the malady was to be attempted or even desired. It was Nature’s prerogative, he contended, to dispose of the peccant matter after her own fashion by depositing it in the joints, whence it might be dissipated by insensible transpiration. Evacuant measures were, he thought, frankly prejudicial in that they occasioned reabsorption into the blood of morbid substances already cast forth from the system into the joints, with haply deflection of the same upon the viscera, with all its added perils.
In view of these conceptions, Sydenham naturally discountenanced any attempt to arrest or control the course of acute gout. “Nay, more,” said he, “I can confidently affirm that the greater part of those who are supposed to have died of the gout have died of the medicine rather than the disease.” Not only were purging, blood-letting, and alike the use of diaphoretics by him condemned, but, more, a policy of “inert expectancy” enjoined. The true rôle of the physician was that of the bystander viewing the workings of the vis medicatrix Naturæ, while for the tortured victim remained the pithy consolation that his gout was to be regarded as a minister of health, whose presence and stay ought by all means to be courted. Long years after Sydenham’s death his laisser faire attitude survived in Meade’s epigram, “the gout is the only cure of the gout,” and in Cullen’s depressing axiom that “in patience and flannel alone” lay salvation. Can we wonder that this policy of masterly inactivity made gout the happy hunting ground of the charlatan?
It may be admitted that an initial attack of gout often leaves the subject better than before, but the deep remedial forces of Nature, at first apparently all-sufficing, later prove unequal to their task. Secondary evils follow the attacks, and “the racking pains, unfitness of motion and other disorders which afflicted him during the greatest part of his life” are at once a proof of Nature’s limitations and the fallaciousness of Sydenham’s doctrines.
So much by way of prelude, but perhaps, as Heberden surmised, the chief reason why Sydenham and his disciples found it advisable to do nothing to curb the violence of gout was that they knew nothing wherewith to achieve such control. Thus, though colchicum had been used from time immemorial by the ancient physicians, it had in Sydenham’s time almost been abandoned as a remedy in gout, when, long after, according to Scudamore, a Mr. Want (“Essays in the Medical and Physical Journals,” No. 185, etc.) drew attention to its specific value in gout, and restored the drug to its pristine status.
In the main the general principles of treatment conform to those adopted for other inflammatory ailments, with, of course, the important reservation that our mode of procedure be adapted to the individual case; viz., due regard must be had to age, the intensity of the attack, and the presence of complications. For obviously the treatment suitable for a robust plethoric subject might prove the very reverse of salutary for a broken-down victim more or less worn out by previous attacks and haply the subject also of arterial and renal changes.
The medicinal treatment of acute gout necessarily divides itself into constitutional and local measures. In pursuance of the first, we seek to control the inflammation and febrile disturbance while assisting the organism to eliminate those toxic substances in the blood that have determined the incidence of the paroxysm.
The attack usually supervenes while the subject is in bed, and, generally speaking, keeps him there. Indeed, rest is imperative, and as far as possible sources of worry should be excluded. The nature of the diet suitable for the acute stages has already been adverted to, and, practically speaking, the first point that calls for investigation is the state of the bowels. Were they prior to the attack open regularly, loose, or confined? Constipation is the usual forerunner, and if so, a swiftly acting purge must be given. Indeed, even if previously the action of the bowels has been free, they usually, with the onset of the attack, become bound, the intensity of the local pain presumably exerting an inhibitory effect.
As to the advisability of initial purgation in acute gout, Sydenham was definitely opposed thereto. In contrast, others, who held with Scudamore that portal congestion was an etiological factor, highly eulogised free catharsis. The truth, as usual, lay between the opposing views. In other words, we must strike the happy mean between adequate evacuation and excessive purgation, for there is good reason to believe that the latter often[374] so to speak, defeats its own end. It may determine more rapid recurrence of the disorder or its perpetuation in a chronic and asthenic form.
Incidentally one may recall that the objections unfairly launched against colchicum took origin in the misconception that its good offices were referable to its cathartic action. Hence by our forefathers the drug was pushed until the characteristic “colchicum stools” appeared, with their attendant nausea and prostration. This of course led to this valuable drug being looked at askance, whereas the error lay, not in the drug, but in the method of its administration, for, fortunately, its specific effect in gouty arthritis may be secured without the induction of depression, nausea, or purgation. Indeed, as Sir Alfred Garrod long since pointed out, it “frequently proves of most benefit when its operation is unattended with increased alvine evacuation.”
Albeit, from the tenor of our digression it must not be inferred that purgation is inadvisable in gout, but only that this salutary purpose must not be effected by colchicum. At the same time we must not think that mere purgation will of itself allay the articular inflammation, for it has been repeatedly shown that it exercises little or no control in this direction; but, on the other hand, it sweeps out irritating matter, promotes the return to a healthy state of the alimentary canal, and in this way reinforces the beneficial effect of colchicum.
My own opinion is that, if seen just before or just after the acute attack begins, it is wiser to secure a free action of the bowels before placing the subject on colchicum, this the more imperatively if it be a case of acute sthenic type supervening in a robust subject evidently labouring under constipation. If there be no palpable derangement of the liver, we may content ourselves with ordering at bedtime a full dose of Gregory’s powder, or Pil. rhei co. gr. 5-8, or Pil. colocynth co. gr. 5-8, followed in the morning by a saline aperient. French physicians, especially Robin, in such circumstances rely solely on sodium sulphate. The salt has the advantage of not lessening the secretion of urine, and the dose advocated is 1 ounce.
If the conjunctivæ show an icteric tinge or the character of the stools suggests that the liver is at fault, small doses of a mercurial preparation, such as calomel (gr. 4) or blue pill, may be given at night, either Pil. hydrarg. gr. 5 or Pil. hydrarg. gr. 1, in combination with Pil. coloc. cum hyoscy. gr. 4, and the same followed in the morning by 1-2 ounces of Mist. sennæ co. The nauseating flavour of the latter is best disguised by 1-2 drachms of Glyl. vanillæ, or for the “black draught” we may substitute 4-6[375] drachms of sodium sulphate, a Seidlitz powder, or a full dose of Carlsbad or Condal water.
When mercurials are contra-indicated or from experience known by the subject to disagree, podophyllin may be prescribed in some such form as the following: Podophyllin gr. ¼ c̄, Pil. coloc. hyoscy. gr. 4.
In other instances the cholagogue effect of the mercurial is procured by substitution for it of a small dose of the Ext. colchici in combination with the compound colocynth pill. Our forefathers, too, frequently prescribed colchicum and mercury conjoined with aloes or colocynth, and the following is an excellent and well-tried formula:—
| ℞ | Ext. colchici acet. | gr. ½ |
| Ext. aloes barb. | gr. 1 | |
| Ext. hyoscy. vir. | gr. 1 | |
| Pil. hydrarg. | gr. 1½ | |
| Fiat pil., 1. | ||
In short, in the matter of the initial purgation the drug chosen must be suited to the individual and the degree of purgation also graded. The old rule was that if the belly is hard, the subject can stand purging, but not otherwise; and it is, I think, a fairly sound index. Mercurials in aged subjects are best avoided, and likewise in those with defective kidneys. Salivation in their instance is easily provoked, and Sir Alfred Garrod held that mercury “in advanced forms of gout should be altogether avoided.” French physicians think saline aperients preferable to the English method of giving calomel, and unquestionably they are eminently suitable for robust and plethoric subjects.
Whatever be its mode of action, colchicum still remains par excellence the remedy for acute gout. As before noted, Dixon and Maiden hold that colchicine has no action on the metabolism or excretion of purins, nor on the kidneys. On the other hand, it influences markedly the leucocytes, their number in the circulation undergoing a primary decrease and a secondary increase. Bain, it is true, found that under colchicum a slight increase in uric acid excretion occurred, but thinks it extremely doubtful if its influence in this direction is invariable.
That colchicine should exert such a marked effect in gout and yet apparently be destitute of any influence on uric acid excretion is of course very striking. It calls, moreover, for more reflection on the part of those who seem to contend that because a drug[376] increases uric acid elimination it must necessarily be beneficial both for the gout as well as for the victim.
Method of Administration.—In initial attacks the drug must be exhibited with caution. Some persons are idiosyncratically sensitive thereto. Attacks of faintness may ensue, or even ordinary doses occasion purging or nausea and vomiting. Their incidence shows either that the subject is abnormally sensitive or the dose too large. Such untoward phenomena indicate its abandonment or drastic reduction. With these reservations, colchicum may be administered in every primary attack and most, if not all, of the succeeding paroxysms.
Albeit, the older the subject and the more ancient the gout, the more warily should we proceed, especially if there is marked irritability of the digestive system, renal disorder, or cardiac degeneration. Robin holds that if visceral gout is present, or the urine contains much albumen, no colchicum should be given.
It is notorious that old persons stand colchicum badly. In their instance we need be the less ready to resort to heroic doses when we recall that acute gout is a self-delimited disease, and while it would be improper to do nothing in elderly subjects exhibiting visceral lesions, etc., it is well that we proceed cautiously, so as to avoid the induction of circulatory depression or the excitation of nausea or a diarrhœa which may be, and often is, difficult of control. Moreover, if these untoward symptoms are allowed to ensue, there is a tendency for the gout to recur as soon as the effects of the colchicum have worn off.
Preparations of Colchicum and Dosage.—Those most commonly in use are the tincture and wine of colchicum, and of these the latter is most in favour. As to dosage, most authorities agree that a full dose—30-40 minims of the vinum colchici—should be given at the inception of treatment and followed by smaller amounts, from 10-20 minims two or three times a day.
By French physicians the tincture of colchicum is preferred, and by Robin that extracted from the flowers rather than the seeds. The dose of our own official Tinct. colchici seminum ranges from 5-15 minims, and by the French Codex the maximum single dose is placed at 25 minims, and the maximum intake during twenty-four hours at 100 minims approximately. It may be noted that preparations from the seeds are more purgative than those derived from the corn. Lastly, we have the official extract of colchicum and the acetic extract. The dose of the former ranges from ¼-1 grain, and it is frequently given in the form of a pill with ipecacuanha and mercury. The addition of a small dose of atropine is often advisable, to obviate the vomiting[377] and diarrhœa often primarily induced by increase of peristalsis. By many the acetic extract is preferred, J. S. Matthews holding that the effective dose ranges from 2-6 grains.
Turning now to discuss the most opportune juncture at which to administer colchicum, certainly in the initial and the earlier paroxysms we may with advantage postpone the giving of colchicum pending free clearance of the bowels. No harm will follow its being withheld until the second day. Indeed, many physicians, both British and Continental, counsel delay in its exhibition until the fit is well established.
Again, in primary paroxysms—viz., while ignorant of the personal equation in respect of colchicum—it is well that our maximum dose should not exceed 20 minims, and when the bowels have not been previously purged, the drug should be combined with sulphate and carbonate of magnesia, as in the following prescription:—
| ℞ | Magnesii sulphatis | gr. 60 |
| Magnesii carbonatis | gr. 10 | |
| Potassii citratis | gr. 30 | |
| Vini colchici | ♏︎ 20 | |
| Aquæ menthæ viridis | ad unciam. | |
| Misce. fiat mistura. Two tablespoonfuls with two of hot water every three hours until bowels have been freely opened. | ||
This achieved, the sulphate of magnesia may be omitted, and the mixture taken every six instead of every three hours; but it is a good plan to keep the original mixture at hand, giving a dose every morning while the acute stage lasts. Then during the day the colchicum should be persisted with either in the form of the wine or the tincture.
Moreover, there are often special indications to be met. Thus the skin in acute gout is often hot and dry, and the urine unusually scanty and high-coloured. In this event the colchicum may with advantage be given with the citrate, bicarbonate or nitrate of potash, so as to produce a diaphoretic and diuretic effect. In other instances acidity is a prominent symptom, and here the combination of colchicum with the citrate of potash and magnesia will be found useful.
As the intensity of the inflammation wanes and the local pain and tension subside the dose of the colchicum should be gradually diminished; but even after convalescence is established it may advantageously be continued for a few days in small doses, say, 5 minims of the vinum colchici three times a day. The condition of the tongue will usually furnish a safe index, as rarely will it clean up prior to abatement of the gouty fit.
In subsequent paroxysms and alike in the acute exacerbations that chequer the course of chronic gout we may, in the absence of idiosyncrasy or other contra-indication, proceed more boldly. Thus, if the bowels have not previously been briskly purged, we may at once prescribe the following formula:—
| ℞ | Vini colchici | ♏︎ 15-20 |
| Magnesii carbonatis | gr. 15 | |
| Magnesii sulphatis | gr. 60 | |
| Aquæ cinnamomi ad ℥j. | ||
| Fiat mistura, ℥ij. statim sumenda et ℥j. quartis horis p.p.a. | ||
The primary dose, as will be noted, will contain either 30 or 40 minims of the wine, and, though Sir Alfred Garrod prescribed up to a drachm, it will scarcely, if ever, be necessary to exceed 30-40 minims. The subsequent dose of from 15-20 minims may after a day or two be reduced, and instead the mixture given in ½-ounce doses three or four times a day. Or, if preferred, the mixture in its reduced dosage may be renounced in favour of a pill containing either the extract of colchicum or, what many consider even better, the acetic extract thereof. Thus the following pill may be taken every night for a few days, and then on alternate nights:—
| ℞ | Ext. colchici | gr. ¼ |
| Aloin | gr. ⅛ | |
| Ext. bellad. alcoh. | gr. ⅛ | |
| Capsicin | gr. ⅟₂₀ | |
| Ext. rhei | gr. 1 | |
| Fiat pil., 1. | ||
The acetic extract may be given in larger doses, and was in great favour as the chief constituent of many so-called “gout pills” in combination with ipecacuanha and mercury:—
| ℞ | Ext. colchici acet. | gr. 1½ |
| Pulv. ipecac. co. | gr. 1½ | |
| Ext. colocynth co. | gr. 1½ | |
| Fiat pil., 1 nocte sumenda. | ||
An excellent formula, in which the colchicum is combined with mercury, has already been furnished on a preceding page. Needless to say, it should, like the above pill, be followed in the morning, if necessary, by a mild saline purgative.
Colchicine.—This, the active principle of colchicum, has of recent years been widely and successfully employed in acute gout, as well as in exacerbations of the chronic type. By some subjects, especially the old, it is often better borne than colchicum preparations. The dose ranges from ⅟₁₀₀-⅟₃₂ grain in a pill. By the French Codex the maximum single dose is fixed at ⅟₃₂ grain, and[379] the maximum administered during twenty-four hours should not exceed ⅟₁₆ grain approximately.
The following is a suitable combination in an elderly subject, and it may be noted that the drug has been found of use, too, in cerebral congestion and uræmia:—
| ℞ | Colchicine | gr. ⅟₁₀₀ |
| Ext. belladon. alcoh. | gr. ⅛ | |
| Ext. nucis vomicæ | gr. ¼ | |
| Fiat capsule or cachet, 1 every three or four hours. | ||
In robust subjects the colchicine may be given in larger doses. Luff states that few patients will tolerate ⅟₅₀ grain, because of the diarrhœa and griping pains produced. He found that colchicine (⅟₇₀ grain), in combination with henbane and nux vomica in the form of a pill, rapidly relieved gout when taken every three or four hours.
Or as a substitute we may use the salicylate of colchicine, the dose of which is ⅟₆₀ grain. Colchicine is readily soluble in methyl salicylate, and is conveniently administered in the form of capsules, each containing ⅟₂₅₀ gram (Martindale). In acute gout one capsule may be given every two hours, or two capsules three or four times a day. These doses are well within the limits of safety, and, if necessary, may be combined with nux vomica and belladonna; but with the alkaloids, as with the colchicum itself, it is essential that the bowels should be kept freely opened. Also with the waning of the pain and inflammation the colchicine or its salicylate should be given less frequently, so as to obviate any depression.
Atophan.—This is a yellowish cream-coloured amorphous powder of the composition 2-phenylchinolin 4-carbonic acid. Its use has been much extolled both in acute and subacute gout. The dose ranges from 30-45 grains daily for three to four days, according to some authorities, but others consider that it may be taken for prolonged periods with advantage. It is most conveniently exhibited in the form of tablets containing 4 or 8 grains. Agotan, a drug identical with that formerly sold under the German registered name “atophan,” is supplied in the form of crystalline powder and in 7½-grain tablets, and appears to be equally efficient.
Atophan is incompatible with sodium bicarbonate and other alkalies in vitro, but Martindale and Westcott “did not find it incompatible with potassium iodide.” It has been repeatedly noted that, following the intake of atophan, the uric acid content of the blood falls and the urinary uric-acid output increases. Weintraud in gouty patients on a purin-free diet noted that after atophan the quantity of uric acid excreted in the urine was[380] more than doubled, but subsequently the excretion fell below normal.
Even in healthy individuals when taking atophan the urine becomes turbid from the presence of urates. This excess of uric acid in the urine may in gouty individuals be precipitated in the urinary tract, and so induce an attack of gravel. Consequently Weintraud advises that the drug be taken with alkalies, either sodium bicarbonate or alkaline waters. Drs. Jansen and Plum, of Copenhagen, during their recent visit to the Royal Mineral Water Hospital, Bath, informed me that they had met no instances of gravel, but in several of their cases atophan had induced urticaria.
As to the simultaneous intake of alkalies, while the precaution is probably desirable, I have known gouty patients take atophan without alkalies for several weeks in full doses without any apparent ill effects. Brugsch, indeed, states that in polyarthritis urica the subjects are able to take 15-30 grains of atophan per diem for a year without any affection of the kidneys. Moreover, uric acid excretion was increased throughout the whole period, and when the drug was discontinued, the pains recurred.
As to the usurpation of colchicum by atophan, I do not think it is at all likely, for it does not, I consider, exert the specific effect of the former on the gouty inflammatory process, taking the humbler rôle of obviating the formation or promoting the absorption and elimination of uratic deposits. In other words, colchicum influences the causa causans of gouty inflammation, atophan only the consequences or sequels thereof.
The most favourable juncture at which to prescribe atophan is at the close of a paroxysm. I have myself been much impressed with the manner in which it produces softening and palpable diminution in the size of tophaceous deposits, so much so, indeed, that I feel sure we have in this drug a valuable agent wherewith to prevent the formation of uratic deposits.
A two or three weeks’ course of atophan after an acute attack is, I have found, very advantageous, in doses of 30-45 grains per diem, after meals. It may, for the special reasons given, be well combined with an alkaline stomachic mixture taken half an hour or more before food.
| ℞ | Potassii bicarbonatis | gr. 15 |
| Sodii bicarbonatis | gr. 20 | |
| Spts. ammoniæ aromat. | ♏︎ 20 | |
| Tinct. zingiberis fort. | ♏︎ 5 | |
| Inf. aurantii co. ad unciam. | ||
| Fiat haustus, thrice daily well diluted with water. | ||
To sum up, our medicinal treatment of acute gout consists in initial purgation, followed by maintenance of an adequate daily evacuation; secondly, the exhibition of colchicum or its active principle and continuance of the same in diminishing doses until pain and inflammatory phenomena have departed. With the passing of the paroxysm atophan should be resorted to in combination with an alkaline stomachic mixture. Supervision of the subject should not cease until the digestive and assimilative functions have, as far as possible, attained functional efficiency, for it is certain that this is the most important point in the management of the gouty constitution. Conjoined therewith, the bowels should never be allowed to become constipated, the urine maintained free from acid lithates, and the skin active by regular exercise.
Alternative Remedies in Acute Gout.—Of the various drugs advocated as substitutes for colchicum the salicylate group alone seems to have evoked something like enthusiasm. Thus Germain Sée affirmed that sodium salicylate was the best remedy for gout, whether of acute or chronic type. In this country Haig strongly upheld its claim. On the other hand, Ebstein, when he used this salt in acute gout, found that the inflammation, though it quickly subsided in one joint, immediately reappeared in another, even though the administration of the drug was continued.
Lecorche, again, though he found it useful in acute gout, was equally certain that it was altogether inferior to colchicum. It did lessen the pain and the violence of the paroxysm, but in no way shortened its duration. But, on the other hand, he attached a prophylactic value to it in chronic gout marked by recurring subacute attacks. His method was to give it in the intervals of paroxysms in doses of from 60-80 grains a day, whereby he claimed to abort attacks, prevent ankyloses, and facilitate absorption of uratic deposits.
As to its mode of action, salicylate of soda, both in gouty and healthy subjects, determines an immediate increase in the uric acid excretion, 30-60 per cent. The increase, however, is but ephemeral, the excretion of uric acid sinking gradually to normal in about forty hours, and this whether the drug be persisted with or not. The increase in total nitrogen excretion does not reach 10 per cent.
Discussing this mode of response, MacLeod (who noted the same after citrates) is of opinion that salicylate of soda and citrate act, not by influencing the metabolic processes that originate uric acid, but by promoting the excretion thereof. Walker Hall and Magnus Levy, albeit, suggest that the increase is due to diminution in the normal destruction of purins in the organism, with resulting[382] transmission of the same in larger quantities to the kidneys for excretion. It is possible therefore that in the presence of sodium salicylate there is diminished oxidation of uric acid.
Bain, however, studying the elimination of nitrogen in a gouty subject, found, contrary to expectation, that after sodium salicylate there ensued only a small increase in the uric acid, with a slight augmentation of the alloxur bases relative to the acid. We see therefore that all the above observers agree that an increased uric acid output in the urine follows the administration of salicylate of sodium, though they differ in opinion as to the manner of its production.
As to the employment of salicylate of soda in acute gout, it must, I think, be seldom called for, save in the presence of idiosyncratic sensitiveness to colchicum. Now, though of this latter much has been written, yet I venture to affirm it is exceptional, and the adverse symptoms are attributable rather to injudicious dosage of the individual than to inherent peculiarities on his side in respect to this valuable drug.
If we should encounter such an instance, there is no objection to our giving the salicylates of sodium or potassium a trial, especially in an acute febrile attack occurring in a healthy subject. In isolated cases the relief to pain may be swift and striking; but, generally speaking, the results are neither so decisive nor so prompt as those obtained in suitable cases by colchicum. The potassium and lithium salicylates are usually given the preference, and they may be combined with citrate or bicarbonate of potash. If the latter salt be used, the draught will prove more grateful if given in effervescent form, viz., by the addition of citric acid or lemon juice.
Frequently it happens that the patient, to begin with, has been placed on colchicum, and, symptoms of irritation having supervened, the drug has had to be withdrawn. The tardy resort then to salicylates is fortunately rather beneficial than otherwise, for, apart from its analgesic effect, it reinforces the increased uric acid output in the urine that follows the attack, and so tends to counteract the tendency to uric acid deposition.
There is yet another contingency in which resort to salicylates may be indicated, viz., in those long-standing cases of chronic gout with recurring exacerbations in which the colchicum, formerly beneficial, has now through acquired tolerance become impotent. Here, either during or immediately after the acute phases, the salicylates may be exhibited, if the stomach be tolerant and there be an absence of cardiac or renal degeneration. As to the employment of salicylates in massive doses in the inter-paroxysmal periods as a prophylactic measure, I think this is better attained by occasional courses of atophan.
Lastly, there are instances in which both colchicum and salicylates appear to be contra-indicated. In this event we may either rely simply on alkalies—and we have Duckworth’s authority that in many cases of acute gout they have proved satisfactory—or we may adopt Sir Alfred Garrod’s plan of giving quinine (2½-5½ grains) suspended by tragacanth in combination with the bicarbonate or citrate of potash. By this means the pyrexia is controlled, and, according to the above authority, any tendency on the part of the disorder to wander from joint to joint; and he holds it especially valuable in those subacute attacks that so commonly chequer the course of chronic gout.
Thyminic or nucleotin-phosphoric acid in doses of 5-10 grains has also been highly eulogised, being held to have an affinity for and a solvent action on uric acid. But Walker Hall, while he agrees that the results obtained in gout are encouraging, yet from his own experiments does not find that “the improvement is at all associated with any change in uric acid excretion—a result which also applies to citerin.”
As to quinic acid and its synthetic combinations, their popularity seems to have been evanescent. It is claimed that “urosin” or lithium quinate speedily controls the acute manifestations of gout, this apparently without any evidences of cinchonism, even though given in 7½-grain tablets ten times daily in acute paroxysms. Others give quinic acid in combination with piperazine, i.e. “sidonal” in doses of 1-1½ grains per diem. But of these, as well as of many other vaunted specifics, I feel inclined to say, with Bianca, “Old fashions please me best; I am not so nice to change true rules for new inventions.”
Anodynes in Acute Gout.—On this point it may be recalled that such was the prejudice at one time against colchicum that Ebstein thought it preferable to relieve the pain of acute gout by hypodermic injections of morphia, which, he thought, acted “quicker, more easily, and with less danger.” Fortunately, however, it is only very exceptionally that colchicum fails to mitigate the pain in acute gout.
In rebellious instances salicylate of soda in full doses for a few hours sometimes succeeds. Hypodermic injections of morphia must rarely, if ever, be called for, and I have never had occasion to invoke them. In fact, opium in any form is best avoided, and if unavoidable is best given in the form of Dover’s powder in combination with aspirin and phenacetin, viz., 2½ grains of each in a cachet at bedtime. Luff in some cases found a full dose of extract of hyoscyamus a very useful anodyne, and if sleeplessness through pain prevails, advises 7 grains of veronal or 10 grains of[384] trional. Sir William Whitla’s “routine hypnotic in gout” is paraldehyde.
All these are preferable to opium in any form, for we deal with a disease in which defective elimination is a prominent feature, and that we should exhibit unnecessarily a drug which inhibits all excretory processes save that subserved by the skin seems wholly irrational. Of this we have an object lesson in the clay stools that in some gouty subjects, as Burney Yeo remarked, persist for some days after even a very small dose of morphia. My own rule is to rely on colchicum as far as possible, and for any extra anodyne effect on local applications, to the consideration of which I now proceed.
The affected limb must be kept at rest on a firm pillow and slightly raised above the body level. The inflamed part should be protected from pressure by a cradle. In the majority of instances, as the elder Garrod long since pointed out, the only local application needed is cotton wool covered with oiled silk, evenly and lightly bandaged. By this means the joint surface is kept both warm and moist, and moisture is important, as dry heat is not grateful and seems to aggravate the pain. The dressing soon becomes wet, requires changing two or three times in the twenty-four hours, when dry warm wool should again be applied, and in this way a local vapour bath of sorts is provided for the inflamed part.
If pain be marked, hot fomentations or stupes or even a foot-bath may be substituted. At one time warm spirituous lotions on lint covered with oiled silk were popular, whisky and water being much in vogue. Others (Pye-Smith) spoke well of a lotion containing 1 drachm of sulphuric ether to 6 ounces of water. Some pack the joint with warm alkaline lotions to which opium or belladonna, or both, are added; but, whether dealing with spirituous or alkaline lotions, all are agreed that cold applications should be carefully shunned.
As to anodyne preparations, we suffer from what may be truly described as un embarras de richesse; but the inexplicable variability of response is such that it is always well to have another shot in one’s therapeutic locker. Practically all the analgesic remedies in use have been recommended by some one or other as useful for the relief of pain in acute gout. The mere enumeration of these might be indefinitely extended, for in truth every one has a favourite remedy wherewith to meet certain indications,[385] and the good results obtained are exactly proportional to the skill displayed in exhibiting their use. We should not, however, resort forthwith to the more potent analgesics. It is wiser to give the simpler remedies a prior trial, such as poppy-head fomentations. If these fail, the liniment or unguentum methyl salicylatis co. may be tried, applied on lint covered with oiled silk and a flannel bandage. Equal parts of chloroform and belladonna or of opium and menthol liniment are also very soothing when sprinkled on lint and covered with cotton wool.
In the more intense cases with great local sensitiveness the following preparations may be lightly applied to the affected area with a brush. Anodyne colloid is one of the most reliable, or we may use glycerine of belladonna or atropine, subsequently covering the part with warm, moist dressings or spongiopiline enveloped in oiled silk, cotton wool, and a flannel bandage. In using atropine preparations, however, care must be exercised, as absorption through the unbroken skin may readily cause toxic symptoms.
In less acute types or as local sensitiveness declines various ointments may be gently rubbed into the affected joint, and in this way the beneficial effects of massage superadded. The most suitable unguents are those containing methyl salicylate in hydrous wool fat with or without menthol, or the methyl salicylate may be mixed with equal parts of olive oil and applied with friction. Used in this way, it is rapidly absorbed, and is much to be preferred to the natural oil of winter-green, which not infrequently proves very irritating to the skin.
Under the influence of one or other of the foregoing methods, the pain in these forms of acute gout is usually quickly subdued. Occasionally, however, owing to incomplete absorption of inflammatory exudate, the case proves more obstinate, and a variable degree of pain and stiffness lingers on in the affected articulation.
If means permit, the ideal course to pursue is for the patient to be sent to some spa where, conjointly with the general treatment, he may enlist the advantage of hydrotherapy, massage, and so forth. In default of such facilities, we must of course fall back upon friction with liniments, being careful not to induce tenderness of the joint. Of these there are endless varieties, those containing ammonia, turpentine, camphor, or capsicum being most in vogue. Inasmuch as their efficacy is largely referable to the rubbing which accompanies their use, we should favour preparations containing oleic acid, either alone or diluted with a fatty oil. As an oily liniment perhaps one of the most useful is the linimentum succini co., containing equal parts of the oils of amber[386] and clove combined with twice the quantity of olive oil, or one of the following excellent combinations may be selected:—
| ℞ | Olei origani vel olei terebinthini | Partes æquales. |
| Linimenti ammoniæ. | ||
| To be applied with friction to the affected part. | ||
| ℞ | Ætheris | 1 drachm. |
| Linimenti belladonnæ | ½ ounce. | |
| Tinct. capsici | To 2 ounces. | |
| To be well rubbed into painful parts night and morning. | ||
When a joint is the seat of fixed pain with definite thickening, it may be necessary to resort to blisters; but frequently they are so utilised as to merit the aspersion of “adding additional distress to unrelieved pain.” They are of course unsuitable for cases with acute serous effusion of recent origin; but are often beneficial when applied over joints, bursæ, or tendon sheaths, when the seat of long-standing passive distension.
Garrod held them of most advantage in gout of asthenic character with lingering effusion; but he thought them inadvisable in the later stages of gout with defective kidneys and where the joints were the seat of massive uratic deposits, as in the last event sores difficult of healing may follow.
In the vast majority of instances such drastic counter-irritation is unnecessary, as the pain usually relents to less strenuous measures. For the dissipation of exudates and thickening nothing is superior to iodine and mercurial preparations. Painting with strong iodine may occasion soreness, but not if the glycerinum iodi be used. Better still is it if we use iodine preparations that admit of gentle inunction. The iodide of potassium and soap liniment is of course most reliable, or we may use one of the proprietary preparations, e.g., leukion. The oleate of mercury (10 per cent.) is often useful, and if pain linger on in the joint, may be combined with morphia (½ grain to 1 drachm). Ichthyol lanoline also deserves mention, and is best rubbed in after a fomentation followed by a dry pack. It is extremely probable that the stimulant and absorbent action of these agents is markedly reinforced by the friction which accompanies their usage.
In conclusion, it must be recalled that the swelling, stiffness, and pain are of dual origin, viz., in part due to inflammatory products and in part to uratic deposits, and it is the former that will be the most influenced by the foregoing measures. As to the means available for the reduction or dissipation of tophaceous matter, we shall best postpone their consideration until we come to discuss the treatment of tophi.
Ionisation in Acute Gout.—The introduction of medicinal substances into the interior of the joints by means of an electrical current is now in extensive vogue, both as a means of relieving pain and promoting absorption in periarticular and synovial affections. It is of course in the more accessible or superficial articulations that its beneficial effects are most easily attainable.
The sensitiveness of the parts in acute gout is such that I have never felt justified in invoking ionisation therein. Nevertheless Finzi tried it in two cases of acute gout. Instant relief of pain and diminution of swelling followed the first séance, while in sequence to a second all local tenderness disappeared. Finzi used a combination of lithium and iodine, the former at the positive and the latter at the negative pole. I would only add that in non-gouty forms of arthritis, if relief of pain be desired, salicylic ions, by general consent, would appear to be the most reliable. As far as I know, most authorities confine ionisation to chronic articular gout, and to this I shall refer later.
Massage.—The success that follows the application of stimulant or absorbent preparations in the after-treatment of acute gout largely depends on the skill and persistence with which the rubbing or kneading is performed. Hence it is that treatment by external medication has been largely superseded, and rightly so, by skilled massage, the outstanding advantages of which find increasing appreciation.
It need hardly be said that massage is contra-indicated in the acute, and its use should be confined to the subacute, stage. Moreover, I would suggest that its aid be sought more frequently during the decline of acute attacks, instead of its being reserved, as it very largely is, for the more chronic varieties of articular gout. In the latter instance organisation of the inflammatory products has already ensued, and their dispersal is correspondingly more difficult, whereas in the former the soft nature of the effused material renders dissipation more easy and, what is more important, minimises the chances of recurrence. Gentle massage also will promote the absorption and resolution of tophi, for the uratic deposits, even when pre-existing, are often found after an attack to be softened and more mobile, and now is the time to profit by these changes, so as to compass their elimination.
In these subacute stages, of course, vigorous excitation must be avoided, effleurage or light stroking being the only permissible measure at this stage; and of course it should be exercised centripetally. In presence of any marked sensitiveness, too, it is advisable that derivative massage of the limb above the joint should always precede any direct friction of the latter.
The measure of success will depend on the technique of the[388] masseur. If he be unskilful or rough, aggravation of the inflammatory process will almost certainly ensue, with prolongation of stiffness and pain. He should proceed tentatively, the energy displayed being gradually increased as the parts grow more tolerant of manipulation.
Again, it is at the close of a massage séance that passive movements are most advantageously employed, and where irritation and pain follow their performance, gentle centrifugal stroking of the actual joint surface will exercise a grateful, soothing effect.
Surgical Methods.—The intensity of the inflammation and swelling in acute gout has, as before said, sometimes led to its confusion with purulent arthritis. It was just such a mishap that led Riedel to discuss seriously the operative treatment of gout when of monarticular type, e.g., in the great toe joint. He cites the case of a man, aged forty-five, suffering with acute gout of classic site which was operated on under the impression that the joint contained pus. None issued, but the synovial membrane was found covered with urates. The latter were removed, the wound healed in five weeks, and no recurrence of articular gout followed till fourteen years after. The second example occurred in a lady seventy years of age, who likewise suffered an acute attack of gout in the right great toe joint. An incision was made and the revealed urates removed, and the wound healed in a few weeks, and no subsequent attacks followed!
Despite the apparent good results obtained, one can scarcely believe that incision and removal of urates during acute gout will ever be seriously considered. Nevertheless the apparent impunity, if not actual benefit, that followed the above operative interference does, I think, indicate that in these aseptic days we need be less timorous; in other words, that, while the operative treatment of acute gout is unnecessary, yet in chronic cases surgery has its sphere. But to this I shall return later, when discussing the treatment of tophaceous deposits in chronic gout.
Despite the fact that heredity plays so dominant a rôle in the genesis of gout, how relatively scanty the attention paid to prophylactic measures! It is the second, never the initial, attack of gout that we endeavour to avert. Surely to inhibit the development rather than to prevent the recurrence of the malady is the better part. The idea is not wholly utopian, for such shrewd observers as Scudamore, Austin Flint, and others, were convinced that by timely and judicious intervention a threatened outbreak might be averted or at least its severity mitigated.
It was to this end that in a preceding chapter I urged the desirability of more attention being paid to the prodromal symptoms of gout and the clarifying light that might be thrown on otherwise inexplicable derangements by the disclosure of a hereditary tendency thereto. The failure to elicit such familial predisposition is but too common, and so those who may be led to expect the gout by inheritance are bereft of all the benefit that might accrue from a prophylactic regimen.
The indications may, indeed, be more explicit, for, apart from hereditary proneness, some subjects, even though they may never have experienced an articular outbreak, yet exhibit tophi, and therewith frequently suffer from gastric or hepatic disturbance. Obviously, is not this the opportune time for prophylaxis—the institution of hygienic and dietetic rules conjoined with the occasional use of medicines? For the “potentially” gouty, as Scudamore said, cannot “too early be taught to pay the most careful regard to their constitution, nor too surely confirm the best habits by long practice.” We hear much nowadays of the “beginnings” of disease, and who can doubt that this is a fruitful sphere for their study?
Unfortunately it is, as a rule, only when the disease has made its invasion that we wake up to our responsibilities in this respect; but happily even then we may do much to prevent consolidation of its tyranny, for even in those who have experienced regular gout there are derangements to correct, warnings to note, if we do but take heed. Of these the more common are dyspepsia[390] and costiveness, signs of portal congestion, etc., not to mention local symptoms, i.e., the onset of pricking and tenderness in already existing tophi, twinges in the toes, etc.
We see therefore that in regard to the prophylaxis of gout the victims fall into two main groups, i.e., firstly, the “potentially” gouty, who as yet have not experienced arthritic outbreaks, and, secondly, those who have, and wish to obviate their recurrence. Happily the premonitory gastric symptoms, though varied in character, are in both instances more or less similar; nor need I say that in either alike medicinal measures are but the smallest part of the prophylaxis, whose chief stay and strength must be the golden rule of temperance in eating and drinking conjoined with adequate exercise. For, whatever our views as to the proximate origin of gout, there is every reason to suppose that the principal exciting cause resides in the alimentary canal. As Sydenham long since said, “The more closely I have thought upon gout, the more have I referred it to indigestion or to the impaired concoction of matters both in the parts and the juices of the body.” Even so to-day do medical men suffering from gout tell me that they, like Sydenham, have found by experience that almost invariably dyspeptic symptoms are the forerunners of attacks, and that their avoidance or timely correction is the best means wherewith to avert paroxysms.
As to the nature of the “indigestion,” it is of subacute or chronic type, and only very exceptionally is it acute. As to symptomatology, there is nothing distinctive about the “dyspepsias” of the “gouty,” save perhaps their marked tendency to recurrence, the facility with which they are occasioned by trivial causes, their frequent obduracy to ordinary measures, and their response to such as take cognisance of the constitutional factor.
Nevertheless such is the frequency and persistence often of gastric derangements in the “gouty” that it may safely be affirmed that the treatment of these subjects in their inter-paroxysmal periods is essentially that of the “dyspeptic.” It is, in truth, the basal indication in their therapy, for correction of the “gouty” man’s digestive disabilities is the surest way to prevent articular outbreaks, or, failing this, to postpone their recurrence or mitigate their severity.
The primary object of medicinal treatment is the restoration to functional efficiency of the alimentary tract and its accessory glands and maintenance of the action of the kidneys and skin. While diet and general hygienic regulations are all essential, we often have to fight the vicious inclination of the victim who is desirous that some medicine may be found which will avert the[391] threatened gout without his being obliged to forego his accustomed indulgence.
He must be promptly and firmly disabused of this fallacy. Indiscriminate drugging is the bane of these cases. They fly from one remedy to another rather than give up this or that excess, and so frequently superimpose a “drug dyspepsia” upon the original disorder.
The most common form of indigestion in the “gouty” is atonic dyspepsia. The primary indication is, of course, to correct the dietetic errors, i.e., to remove the cause, and, secondly, to stimulate the secretory and motor power of the stomach. To this end, the alkalies and alkaline carbonates should be administered shortly before meals in combination with nux vomica, bitters, and carminatives.
| ℞ | Mag. carb. | gr. 10 |
| Sodæ bicarb. | gr. 15 | |
| Tinct. nucis vomicæ | ♏︎ 7 | |
| Spts. chloroformi | ♏︎ 10 | |
| Infus. calumbæ ad unciam, ter in die sumenda ante cibos. | ||
In the milder type of case the above may suffice, supplemented, if necessary, by some gentle aperient. Unfortunately in many instances the condition is apt to become complicated by fermentation with excessive formation of organic acids. It is to these that the “acid risings” are due, and not to excess of HCL. Indeed, the reverse is the case, viz., a deficiency of HCL. It is this that is responsible for the fermentation with the production of butyric, lactic, and acetic acids. Moreover, in middle-aged “gouty” subjects of sedentary habits there is often superadded motor defect, which may end in dilatation.
For treatment of this condition careful dieting alone may suffice. Indeed, attention to general health often succeeds where stomachic therapy alone conspicuously fails. The medicinal indications in these cases will vary according to the stage at which they are seen. In the milder forms we may stimulate the flow of gastric juice by alkalies and bitters before meals, or hydrochloric acid after food may be taken to replace the defect.
Now, theoretically speaking, this may sound very simple, but in practice it is often not so. Moreover, the less the attention paid to correction of diet and faulty habits, the more bewildering and disappointing the effect of drugs. Conversely, the more care expended on the selection of food and hygienic measures, the less need for drugs and the clearer the indications for such as may be helpful.
Thus simply under a revised diet the acid eructations may[392] wholly disappear and the subject suffer only with languor, discomfort, or drowsiness after meals. Here dilute hydrochloric acid combined with strychnine and pepsine after food will be found useful.
On the other hand, many of these patients are impatient of dietetic control, yet nevertheless clamour for relief of their “acid” eructations. In such cases alkalies must be given an hour or so after meals to correct the excess of organic acids. The same may be combined with antiseptics—carbolic, B. naphthol, creosote, etc.—or some artificial digestive, such as papain, pancretin, or taka-diastase.
| ℞ | Bismuth carb. | gr. 15 |
| Calcii carb. | gr. 5 | |
| Acid. carbol. pur. | ♏︎ ½ | |
| Oleum cajeput | ♏︎ 2 | |
| Fiat cachet, 1 or 2 an hour or more after meals. | ||
The calcium and bismuth carbonates are best, inasmuch as, though they act slowly, they give rise to no secondary hypersecretion. Of digestive adjuvants in these cases, Luff speaks highly of taka-diastase (gr. 2½) immediately before meals in addition to bismuth and alkalies. The taka-diastase assists the digestion of carbohydrate foodstuffs, and so lessens or inhibits the formation of organic acids. But as a digestive adjuvant in these cases of “dyspepsia” with acid eructations papain is most useful, acting in acid, alkaline, or neutral media. This indifference on its part enables us to combine it with alkalies, and so attain the dual effect of reinforcing the digestive capacity and neutralising hyperacidity.
| ℞ | Mag. carb. pond. | gr. 15 |
| Sodii bicarb. | gr. 10 | |
| Papain | gr. 3 | |
| Oleum caryophylli | ♏︎ ½ | |
| Fiat cachet, 1 or 2 after meals when acidity is at its height. | ||
Our forefathers in such cases thought highly of rhubarb and magnesia, and certainly in hospital patients some such combination as the following is invaluable in so-called “gouty dyspepsia”:—
| ℞ | Mag. carb. | gr. 10 |
| Sodii bicarb. | gr. 15 | |
| Acid. carbol. pur. | ♏︎ 1 | |
| Tinct. rhei co. | ♏︎ 15 | |
| Spts. chloroformi | ♏︎ 15 | |
| Inf. caryophylli ad unciam, ter in die post in cibos. | ||
Almost always in these cases more or less constipation prevails, which must be corrected. To this end, of course, the magnesia contained in one of the above cachets may be all that is necessary; but often it is not so, especially if the subject be taking bismuth. Moreover, inasmuch as we have to take cognisance of the constitutional taint in these individuals, we may with advantage give an occasional aloetic pill containing colchicum or a nightly dose of guaiacum and sulphur. Again, if the urine be scanty, we may substitute a morning draught of phosphate of soda (¼-½ ounce), which not only stimulates the liver, but exercises also an antacid and diuretic effect.
| ℞ | Ext. colchici | gr. ¼ |
| Aloin | gr. ¼ | |
| Menthol | gr. ½ | |
| Ext. rhei | gr. 1 | |
| Fiat pil., 1 alternis noctibus sumenda. | ||
As soon as the symptoms of fermentation and organic acidity relent to the above or similar measures we should, if possible, dispense with drugs and rely wholly on diet and general hygienic regulations; but unfortunately a case of atonic “dyspepsia,” if of prolonged duration, gradually merges into one of chronic gastritis. Especially in those given to alcoholic indulgence do we meet with a condition of mucous catarrh, with its associated deficiency of hydrochloric acid. Indeed, apart from alcoholic excess, such is the frequency in “gouty” subjects of this form of “dyspepsia,” i.e., fermentation with excess of organic acids, that I am inclined to think that the subacidity which permits of such developing is, if I may say so, the inherent digestive disability in “gouty” subjects. Unquestionably hyperacidity—i.e., excess of organic acids due to hypochlorhydria—is in their instance infinitely more common than hyperchlorhydria, or excess of HCL, that is, much more frequent than the latter as differentiated from organic acidity by the only possible means, viz., an examination of the stomach contents.
Again, accepting the view that infections are the chief excitants of gouty paroxysms, the desirability of reinforcing the antiseptic action of the gastric juice is obvious. In other words, the defensive powers of the stomach against intruding microbes must be raised by prescribing hydrochloric acid. For this purpose it is well to use strong or fuming hydrochloric acid in doses of from 5-10 minims, freshly mixed at the time of administration with 6-8 ounces of water, and the same taken at every meal. The hydrochloric acid may with convenience be placed in a drop bottle, and beginning with 5 minims, an extra minim may be[394] added every few days until 10 or 15 minims are taken at each meal.
Some years ago Armstrong, of Buxton, spoke highly of its value in alimentary toxæmia, which is precisely the condition we are confronted with in gout. Falkenstein, again, highly eulogises it in the latter disorder. He gives from 40-60 drops of pure hydrochloric acid in a large quantity of effervescing water each day. It is taken during meals, and the dilution with water is arranged so that the patient is struck by the acid taste. The diet taken was an ordinary one, and yet Falkenstein noted that the dyspeptic symptoms disappeared and the attacks of gout grew more rare and much less severe. As an alternative to water, either still or effervescing, the hydrochloric acid in from 5-15 drops may be given in mucilage, or, if preferred, we may give the dilute hydrochloric acid in some such form as the following:—
| ℞ | Acid. hydrochlor. dil. | ♏︎ 10-15 |
| Glycerin pepsinæ | dr. 1 | |
| Liq. strych. hyd. | ♏︎ 3 | |
| Tinct. capsici | ♏︎ 1 | |
| Inf. aurantii co. ad unciam, ter die sumenda statim post cibos. | ||
Sometimes it so happens that while taking the above acid mixture the subjects an hour or more after meals complain of acidity. If so, it is due to fermentation, and at the time of its occurrence must be met by an adequate dose of an alkali with or without some antiseptic preparation. It goes without saying that if such can be referred to dietetic errors—food-bolting, etc.—these also must be corrected.
In these cases, too, the liver is frequently inactive, though often their attacks of “biliousness” signify nothing but constipation; but when there are definite signs of hepatic torpor we may substitute for the hydrochloric acid in the above mixture the dilute nitro-muriatic acid. Simultaneously we may occasionally at night give a pill containing calomel, iridin, or podophyllin combined with aloes and belladonna, or we may instead invoke colchicum as a cholagogue, following it up in either case the morning after by a saline purge. As a substitute we may in suitable cases order every morning for some days a full dose of Rubinat, Hunyadi Janos, or other bitter water.
So much for the more common derangements of the inter-paroxysmal period and the measures wherewith to combat them. Collectively their aim is the restoration to functional efficiency of the alimentary canal and its accessory glands, this to the end that, as far as possible, a condition of intestinal asepsis may be attained,[395] with its correlated diminution of the excitants most fertile of outbreaks.
Nevertheless, from time to time, either from failure of the patient’s co-operation or other mischances, our best efforts at prophylaxis fail, and it becomes clear that an attack is imminent. What then, save brisk purgation, can be done to avert the threatened outbreak? Our forefathers, in cases in which the fits recurred periodically and might be forecast with tolerable accuracy, were accustomed some time before the threatened attack to place the subject on a rigorous diet, this in combination with a course of alkalies, those of soda being given the preference in dyspeptic or hepatic disturbance and those of potash when the urine was scanty.
That this was sound treatment and abundantly justified by the results is well acknowledged, and all I would suggest is that this is yet another juncture at which atophan is indicated, viz., immediately before a paroxysm. At this particular time the urinary output of uric acid is often diminished, a clear indication for enlistment of atophan, which increases uric acid elimination. I note that both Retzlaff and Brugsch consider it an especially advantageous time for its exhibition. As a prophylactic measure the former gives 30-45 grains daily for three days at intervals of a fortnight, and if cardialgia or heartburn ensues, adds ¼-½ teaspoonful of bicarbonate of soda to each gramme of the drug.
Lastly, we have to recollect, too, that colchicum is credited with some prophylactic powers. Some, it is true, discountenance its employment in the inter-paroxysmal period, on the plea that it tends to favour recurrence and chronicity of attacks. While I think it is better to reserve it for acute or subacute attacks, still I have not found that colchicum, given in what Sir Thomas Watson called alterative doses, is anything but beneficial, provided that it be taken intermittently, not continuously, for long periods. As to special indications for its employment, I think it is more effectual in aborting a threatened attack when, in addition to dyspeptic phenomena, the imminence of a fit is betokened by what may be termed specific harbingers thereof, i.e., pricking and tenderness in existing tophi, twinges in the toes, etc.
In conclusion, are we not in this matter of the prophylaxis of gout somewhat too prone to resort, both in and out of season, to what we are pleased to term special medication? Almost every week some new and of course infallible “uric acid solvent” is lauded ad nauseam in the press. Are not we ourselves, too, somewhat overanxious to go with the tide in prescribing these vaunted “gout specifics”?
The true aim of prophylaxis is rather to prevent the incidence[396] of those functional derangements that in some subtle way determine the disturbances in nuclein metabolism, with secondary accumulation of uric acid in the organism. That drugs, such as atophan, which diminish the uric acid content of the blood and increase its urinary output, fulfil an invaluable rôle in ridding the system of excessive amounts of this chemical outcast, I fully admit.
Albeit, this achievement does but deal with the consequences or sequels, not the exciting causes, of gout. In truth, there is no short cut to the cure of gout. Only under suitable treatment, applied to meet all the necessities of individual cases, will any long immunity from its onslaughts be secured or their intensity attenuated.
The gastric derangements that precede acute gout nearly always become aggravated when the disease is permanently established. Consequently from time to time many of the measures outlined in previous paragraphs must be resorted to. But there is this also to be borne in mind, that in these later stages of the evolution of the disorder the intervals of relative health grow shorter and shorter. The victim lies more or less always under the shadow of the malady, and its peculiar impress on the constitution becomes more and more ingrained. Therewith his sensitiveness to the exciting causes becomes more and more pronounced.
To detect and thereafter to eliminate the most fruitful excitant of articular outbreaks in individual examples will form no small portion of the task that falls on physician and patient alike. In the majority, it will be some indiscretion of food or drink; in some, insufficient exercise; in others, intellectual strain or worry, etc. By determining the particular nature of the excitant in the individual under review we arrive at his personal idiosyncrasy—a matter of much moment in prophylaxis.
Moreover, with increasing experience the physician cannot help noting that the vulnerability to assaults varies in different subjects. Thus the development of gouty paroxysms in some will be found to be associated with gastro-intestinal or hepatic derangements, in others with defects of elimination through kidneys, bowels, or skin.
In short, these cases must be approached in a catholic frame of mind, and the success of medicinal therapy will depend on the judgment and clinical acumen displayed in meeting the ever-varying necessities of individual instances, not by an almost flippant prescribing of alkalies or, it may be, iodides, colchicum, or guaiacum. All these are valuable, but only if invoked with discrimination, and not after stereotyped or routine fashion.
The joints in these cases are the seat of chronic change, and though they call for due attention, it is the constitutional taint that is of paramount importance. How best shall we influence[398] this? How else save by recognition of the morbid content of the blood and cleansing of the impurities with which it is charged?
I have before stated my belief that functional derangements of the alimentary canal are the determining cause. It is through their agency that the toxicity of the blood plasma ensues. In the vast majority of cases these constitute the dominant departure from physiological righteousness. It is to these that the high uric acid content of the blood may presumably be referred. Yet nevertheless retention of the same in the form of tophi may be relatively slight. Is it that in their instance the avenues of excretion are more permeable?
In others, again—not necessarily those with more pronounced dyspeptic symptoms—the retention of uric acid proceeds apace. Clinically the explanation appears to be that cases with massive tophaceous deposits often display renal changes. In other words, it is the channels of elimination that appear to be at fault.
But, more than likely, these superficial differences hark back to infinitely more subtle inward disparities, to tissue peculiarities of function, with correlated variations in their retention capacity for uric acid. Here again the clinician waits upon the bio-chemist, and meanwhile must base his differential treatment on somewhat coarser indices.
Thus in one class of case the toxicity of the blood seems attributable to dyspepsia or mal-assimilation, and the physician’s efforts must be concentrated on correction of the same. In another type such may be absent, and yet uric acid accumulates, tophi multiply, and his attention turns to the kidneys, the avenues of excretion. In others, again, both symptom complexes may be combined, and his resourcefulness is taxed to the utmost to meet these several necessities, for, as Sydenham wisely said, “the weakness of all the digestions and the loss of natural strength in the several parts are the essence of gout. Each must be dealt with.”
Nor must we forget that long-continued gout engenders not only a depravation of general nutrition, but paves the way also for the insidious production of structural organic changes. In a word, it favours the onset of pre-senilism, with all that such connotes. So it is that in these subjects, too often past the meridian of life, we have not only gout to combat, but the grisly appanage of oncoming age.
It is this larger view of our responsibilities that we must cultivate if our treatment of chronic gout is to be in any sense rational, and not wholly haphazard. Also, if my contention be correct that the alimentary canal is the fons et origo mali, the major source of the provocatives of gout, then the basal and essential part of our[399] therapy must be diet and regimen. As to the subsidiary medicinal indications, it will perhaps be more convenient if I proceed to discuss shortly the use of the various drugs that experience has shown to have been of most avail in chronic gout.
Alkalies.—It was formerly thought that by increasing the alkalescence of the blood its solvent effect on uratic deposits was enhanced and their formation thereby delayed or prevented. But subsequent researches by Sir William Roberts conclusively proved to his mind “that alkalescence as such has no influence whatever on the solubility of sodium biurate.”
Luff, again, from his investigations, held that administration of the ordinary alkalies, of lithium salts, of piperazine, and of lysidine, with the object of removing gouty deposits, appears to be useless. He also claims that no general acidity of the system is associated with gout, and no relationship exists between the acidity of the urine and the alkalinity of the blood.
Nevertheless let us not sin against light, which is exactly what we are very prone to do if we allow ourselves to be obsessed by uric acid and overlook the records of clinical experience. Take Sir Thomas Watson; he, without any reference to uric acid elimination, recommended as a prophylactic against gout 15 grains of bicarbonate of potash in combination with tincture of rhubarb and some light bitter, to be taken every day. Fagge, again, observes, “Alkalies are decidedly useful in gout,” and the same views were held by the elder Garrod, Lecorche, and Dieulafoy, etc.
In short, forgetting for the moment the existence of uric acid and shedding all hope of their dissolving tophi, we find that alkalies have ample justification besides for their employment. They are valuable as antacids, diuretics, and as alteratives, and, moreover, their routine employment has been tried and approved.
In other words, the benefit of alkalies depends, not upon any special solvent effect upon uratic deposits, but upon their remedial influence upon associated and, I believe, causally related gastric and hepatic disorders, and through these on general metabolism. Albeit, let us be guided by rational considerations when we invoke their aid.
The fact that alkalies are incapable of dissolving tophi is a clear indication that that deleterious habit of continuously taking potash and lithia water is not only unnecessary, but undesirable. Alkalies should be prescribed in short courses and to meet special indications, i.e., intermittent, not continuous, administration.
Thus in the minor gastric disturbances which in chronic gout we are constantly called upon to treat there is no doubt as to the superiority of the sodium compounds. Moreover, apart from their[400] value in gastric or intestinal catarrh, we have to note their usefulness in dyspeptic states complicated by torpid liver.
When constipation exists, the sodium bicarbonate may be combined with magnesia, and all will admit the striking benefit attained by short courses of these drugs with the addition of rhubarb, some simple bitter infusion, quinine, or strychnine, all rendered more effective by the addition of some carminative or aromatic.
Sydenham’s electuary was compounded of gastric tonics, and the more recent Portland and Pistoja powders are in this respect but an imitation thereof. Indeed, stomachics are the most valuable tonics in gout. Lastly, it is in the inter-paroxysmal periods of chronic gout that the sodium compounds are indicated, when the joints, though enlarged, are quiescent, and the more prominent symptom in the clinical picture is lack of gastric tone, with or without acidity.
As to the potash compounds, it is during and immediately after articular paroxysms of acute or subacute gout that they find their chief sphere of usefulness. Apart from this, they are, because of their diuretic properties, valuable at all times in cases in which the renal secretion appears to be deficient. The bicarbonate, citrate, or acetate of potash are the most valuable. The last-named is the most diuretic, but is rarely used, the citrate enjoying more favour, being more palatable and most eligible when no direct antacid effect is desired, in which case it should be replaced by the bicarbonate.
In those instances in which the skin is notably inactive Garrod thought highly of the phosphate of ammonium, holding that “there is much clinical evidence to prove its value in the treatment of chronic gout.” Many, like Burney Yeo, believe that a combination of soda and potash compounds acts better than when either is given singly. Thus Garrod in cases in which the action of the liver was defective frequently used the bicarbonate of soda in combination with the citrate of potash.
As to the lithium salts, general opinion has it that their value in the treatment of gout has been greatly over-estimated, and that they are not so serviceable as the potassium and sodium salts. They are also more toxic and lowering, and Luff some years ago issued the following caveat: “I constantly meet with patients suffering from cardiac depression, and even dilatation, as the result of the excessive and continued consumption of lithia tablets, which are so persistently, so speciously, and so wrongly vaunted as curative of gout.”
In conclusion, it will be seen that clinical experience testifies with no doubtful voice to the value of most salines. At the same[401] time it is clear, also, that we should use discrimination, seeing that some, as Garrod says, are “certainly more adapted to particular cases than others.” They should also be given well diluted, in moderate doses, and not continuously but intermittently. These rules should certainly be followed when alkalies are invoked in gout, not for local antacid effect, but for their general influence on metabolism. Moreover, at the close of a course of alkalies for this purpose, we may often with advantage place the subject on acids in combination with quinine, nux vomica, or strychnine.
Alteratives.—Of these the salicylates and the benzoates are, by some, greatly prized, in that they act especially on uric acid, promoting the elimination thereof. The benzoates are favoured in examples in which the kidneys are not above suspicion, the latter disability contra-indicating the use of the salicylates. Some, like Ewart, advocated a course of benzoates in alternation for periods of a week or a fortnight with a saline treatment. By Lecorche and Haig, salicylate of soda in doses of 60 grains or more per diem was advocated continuously for prolonged periods.
In my opinion, salicylates are best used during a paroxysm, when, for some reason, colchicum is contra-indicated, or immediately after, to promote elimination of uric acid and to minimise or inhibit the development of tophi. As to the benzoates of sodium and potassium, they are now rarely, if ever, prescribed, though hexamine is growing in favour as a “urinary antiseptic diuretic and anti-lithic.” Occasionally I have met with B. coli infections in gout, and in such cases one of the preparations of hexamine, with lithium or sodium benzoates, is of value, whilst among the laity urodonal stands in high repute as a means of removing uric acid and allied bodies.
Iodides.—Turning to well-tried alterative remedies, there is no doubt that the iodides well deserve their high repute in the treatment of chronic gout. Thus in subacute and obstinate swelling of the joints, and alike in painful gouty affections of the muscles, fasciæ, and nerve sheaths, iodine in one or other of its forms is par excellence our most reliable remedy.
In no type of case is it more serviceable than when the joint inflammation is of low asthenic type—enlarged, stiff, and painful. It may be given in some such combination as the following:—
| ℞ | Pot. iodidi | gr. 5-10 |
| Pot. bicarb. | gr. 15 | |
| Spts. ammon. aromat. | ♏︎ 20 | |
| Vin. colchici. | ♏︎ 5 | |
| Tinct. capsici. | ♏︎ 1 | |
| Inf. aurantii co. ad unciam ter in die sumenda post cibos. | ||
If colchicum be contra-indicated, a useful substitute to quell pain is tincture cimicifugæ in 15-minim doses. The dose of the iodide need not exceed 3-5 grains, as, from my observation, no appreciable advantage is gained by larger doses. Iodine-albumen compounds may be substituted for the alkaline iodides as less likely to cause derangement of the stomach, inasmuch as assimilation is believed to take place in the intestine. Thus iodo-protein may be administered in doses from 10-15 grains. A tablet containing 10 grains is equivalent to 1 grain of combined iodine. Excretion being taken as the measure of absorption, it has been experimentally shown that, six hours after administration, a lower percentage of iodine was excreted in the case of iodised protein than with potassium iodide. In other words, the iodine-albumen compound yield up their iodine to the system at a slower rate. In short, they disintegrate more slowly and are, therefore, the more likely to exert a longer continued activity.
An organic compound of iodine with vegetable albumen, i.e., iodo-glidine, has been somewhat extensively used in gout, as being non-depressant. Said to undergo almost complete disruption in the intestines, it is slowly absorbed without toxic symptoms. Iodo-casein and seroden, a combination of iodine with blood proteins, are similar preparations, with which, if necessary, the alkaline iodides may be replaced.
More recently the advantages of collosol preparations of iodine have been emphasised, and these colloidal solutions, unquestionably, have an increasing sphere of usefulness in all cases of gout where iodine is indicated. It has been truly said, collosols “are not new drugs, they are simply familiar drugs in a new form—a form in which their therapeutic potency is greatly heightened while their undesirable properties are reduced to vanishing point.”
Doubtless, collosols exist in a form very meet for assimilation, inasmuch as they conform to the essentially colloidal character of all the normal fluids and secretions of the organism. Moreover, toxins or bacterial poisons appear also to exist in colloidal form, and also, according to A. B. Searle, “to a large extent in the reactions which create immunity.”
These physical similarities between collosols and the bodily fluids and tissues ensure their ready assimilation with minimal constitutional disturbance. Inasmuch as the colloidal state, too, predicates low chemical affinity, the combination and absorption of collosol preparations take place gradually and uniformly.
For internal administration colloidal iodine is prepared in[403] aqueous suspension. It is stated that the whole of the iodine is absorbed in molecular combination with protein. An iodo-amino acid results, and ultimately reaches the blood-stream. Arrived there, it, through its reducing action on lipoids, exerts an alterative effect.
The dose of collosol iodine ranges from 1-4 teaspoonfuls daily after meals. It does not cause nausea if the amount be slowly increased, and only exceptionally does it set up iodism. In these respects it has an undoubted advantage over the alkaline iodides. As to whether they will wholly usurp the place of this latter is, I think, very doubtful; this, if only for the convenience with which the alkaline iodides lend themselves to combination with other alterative remedies. But in individuals intolerant of iodide of potassium they are excellent substitutes when the indication is to improve and modify the general metabolism.
Lastly, too, apart from their use in chronic gouty arthritis, we have to recollect that the iodides are the most reliable means we possess of influencing the renal and vascular changes so often associated with gout. Garrod doubted if they possessed any power of promoting the dissipation of uratic deposits, but their power of eliminating lead must not be lost sight of when treating gout in the subjects of plumbism. Obviously, when invoked for this purpose or to arrest or retard degenerative processes in kidneys and vessels, their administration must be continued for long periods—six to eight weeks. The same persistence, too, is demanded to remove the inflammatory products in the joints. Simultaneously or alternately short courses of atophan—30-40 grains for two to three days in a month or oftener in more severe cases—will also be of help in dislodging articular deposits in the form of tophi.
Guaiacum.—Many years ago, Sir Alfred Garrod[62] highly eulogised the value of this drug in the treatment of chronic gout. Said he, “There is no remedy of which I can speak so confidently. I have[404] known patients who have been confined to their beds for many weeks with asthenic chronic gout so far recover within two or three days under the use of this remedy as to be able to walk about.” He held that it exerted a specific action on the fibrous tissues, and advocated its exhibition in chronic forms of gout with feeble[405] circulation. He adds the further interesting differentiation regarding the employment of guaiacum as opposed to iodide of potassium. Both these drugs he held valuable when the fibrous coverings of the joints were especially affected. If the articular pains were increased by warmth, iodide of potassium is “peculiarly indicated”; but, under such circumstances, “the use of guaiacum is either altogether contra-indicated or, at least, it should be administered in combination with iodide of potassium or some other saline.”
As to its mode of action, Bain noted that, while the excretion of urea fell somewhat, that of uric acid was markedly increased. But he found, also, that “neither the phosphorus pentoxide nor the bases showed a corresponding increase—thereby denoting that this drug probably acts, not by increasing the production of uric acid, but by eliminating a part of that stored in the blood.” Moreover, it was noted that the increased uric acid excretion did not cease with cessation of the drug, but continued for some time after, the patient’s condition meanwhile undergoing amelioration. Bain considers that his researches confirm the opinion arrived at, on empirical grounds, by Sir Alfred Garrod—that guaiacum was a powerful prophylactic agent in gout.
Returning to its method of exhibition, it must be admitted that it is most unpalatable when given in the form of a mixture, and is preferably prescribed in a cachet or tablet. The resin of guaiacum may be given in doses of from 5-15 grains, and the larger doses may excite nausea or purging. In smaller amounts, however, it merely exerts a beneficial laxative effect; it is also useful in cases where the liver is torpid. This latter action may be reinforced by simultaneous administration of calomel in fractional doses.
| ℞ | Hydrarg. sub chlor. | gr. ⅟₁₀ |
| Guaiaci resinæ | gr. 3 | |
| Sulph. precip. | gr. 3 | |
| Fiat. cachet. Ter in die sumenda post cibos. | ||
Such is useful as a corrective in intestinal fermentation when given for three or four days, after which the calomel may be withdrawn and the guaiacum and sulphur continued in doses adequate to produce a daily evacuation.
The compound confection of guaiacum or the Chelsea Pensioner Powder have also stood the test of time, and may be taken in the appropriate dose daily for weeks. Personally, I have for years employed a cachet containing guaiacum, iodide of potassium, colchicum, and cinchona as a prophylactic measure in the inter-paroxysmal periods of chronic gout.
I would here, too, advance a plea for the use of guaiacum as the most useful laxative for constipation in the gouty, and in combination with sulphur where there is inactivity of the skin. The following is an excellent and well-tried formula:—
| ℞ | Sulph. precip. | |
| Pulv. guaiaci | ||
| Pot. bitart. āā | ʒj. | |
| Pulv. tragac. co. | ʒij. | |
| Fiat pulv., ½ to 1 teaspoonful to be taken stirred up in water or milk at bedtime. | ||
Such is a useful laxative and, during the day, may be often advantageously combined, in lingering articular gout, with a mixture containing iodide of potash, nux vomica, and cinchona. Luff, by the bye, holds that iodide of potash acts more beneficially when given in the compound decoction of sarsaparilla—the latter also is lauded by Garrod as having properties somewhat similar to guaiacum.
In conclusion, the subjects of long-standing gout not infrequently are anæmic. In such cases iron is often not well borne, and has been said to favour recurrence of acute attacks. Small doses, however, of a less astringent form agree well, always provided that the bowels are kept freely open. The ammonio-citrate, the iodide of iron, or one or other of the organic iron compounds are most suitable. These may be given alone or in combination with arsenic. For improving the general condition and promoting the nutrition of such subjects, Robin speaks highly of the following:—
| ℞ | Acidi arseniosi | gr. ⅟₈₀ |
| Potassii iodidi | gr. 1 | |
| Pulveris rhei | ||
| Extracti gentianæ | āā q.s. | |
| Misce. Fiat pilula i. “Two pills to be taken daily at meal time.” | ||
In drawing to a close our discussion of the drugs most useful in the treatment of chronic articular gout, it will be noted that our usage of them is largely empirical, viz., the outcome of experience. We do not know exactly their mode of action, but this we do know, that they have stood the most searching of tests—that of results. That we should be largely, if not entirely, ignorant of their mode of action is regrettable, but no reason whatever why we should discard them in favour of newer compounds administered on some pseudo-rational basis.
What we need in gout is, rather, what Harry Campbell calls “a broad commonsense-rationalism—not a meddling finnicking pseudo-rationalism.” Ignorant of the intimate etiology of gout, we are not as yet capable of determining the exact nature of the underlying morbid processes. Much less are we in a position to[407] devise a rational system of drug treatment whereby to antagonise the same. For us, then, the wiser, if more humble, rôle of correcting, if we may, such obvious deviations from physiological righteousness as we may discern, but ever mindful that we assist, not thwart, the subtle workings of the vis medicatrix naturæ, whereby the balance of the nuclein exchanges is restored.
When treating of these in relation to acute articular gout, we dealt with the topical applications best calculated to achieve the absorption of inflammatory exudates and mitigation of the pain and stiffness associated therewith. It now remains for us to discuss the treatment of that specific product of gouty inflammation, viz., uratic deposition.
Treatment of Tophi.—Subcutaneous tophi in the neighbourhood of joints sometimes become tense and painful, and restrict the movements of the adjacent articulations. Garrod held that the continuous application of pledgets soaked in solutions of carbonate of lithia or of potash to tophaceous swellings had some power in reducing their size, and even effecting, in some cases, their total absorption. Also, with the intent of dissipating collateral inflammatory thickening, he sometimes used a solution composed of equal parts of iodide of potassium and carbonate of lithia.
More recently, Robin states that the resolution of tophi may be hastened by local applications of mineral waters containing magnesia and sodium chloride or a solution of sodium perborate, these affixed with considerable pressure over the harder parts of the tophus, gentle massage of which, he thinks, at other times, will aid absorption.
Luff, however, on this point, holds that “the application of the so-called solvents externally to affected joints is useless, as they are not solvents of sodium biurate,” and I am inclined to agree with him that but little is to be hoped for from this method of treatment. A more effectual method of local medication is by the electrolytic introduction of drugs.
Ionisation.—We may enlist cataphoresis, either for its analgesic or its sclerolytic effect. If relief of pain be desired, the electrolytic introduction of the salicylic ion from a cathode of a 2 per cent. sodium salicylate solution is most valuable. A current of 20-40 milliamperes, but only gradually raised, should be passed for twenty to thirty minutes. Too frequent applications of the latter strength may cause injury to the skin, and, in Lewis Jones’s opinion, are inadvisable oftener than twice a week.
If we wish to exercise a favourable stimulant effect in alterations of nutrition and atrophy caused by gouty inflammation, the[408] chlorine ion definitely accelerates return to the normal state. Six-fold pads of ample size, soaked in a warm solution of sodium chloride, are used as a cathode and bandaged round the joint. The other “indifferent” electrode, similar in nature, is applied to different parts at different sittings, and in this way the pathway of the current through the joint changed. Currents up to 100 or even 200 milliamperes may be tolerated when applied to the knee; but the intensity of the current should only be raised gradually, as the burns that sometimes ensue occasion no small pain to the subject as well as discomfiture to the operator.
Iodine has a like sclerolytic action, and is commonly held to be superior to that of chlorine. On the other hand, the iodine ion is much less readily tolerated by the skin, and, according to Leduc, the necessary reduction in intensity of the current employed goes far to nullify the greater sclerolytic effect it may possess.
In chronic gouty arthritis we are, as before remarked, confronted not only with inflammatory products, but also with uratic deposits. Fortunately, these latter also are benefited by the electrolytic introduction of the lithium ion under an anode of lithium chloride. The current serves a double purpose in this case, for it not only drives in the lithium, but removes the uric acid ion which is to be found in the electrode. Edison, some years ago, suggested ionisation with lithium in gout, and the good results he obtained have since been abundantly confirmed by others.
The Schnee four-cell bath may be used where ionisation is indicated. It possesses obvious facilities for local or sectional application, as drugs can be added to the water in the cell and carried through the skin by means of the continuous current. Thus, in cases of large gouty deposits, the joint may be placed in a bath containing a 2 per cent. solution of iodide of lithium or of 5 per cent. bicarbonate of potash. The positive electrode is then located in the bath, while the negative pole, moistened with hot water, is applied to the lumbar region. Working with lithium in this manner, Bordier detected the presence of uric acid in the fluid of the bath, thus demonstrating introduction of the cation-lithium and removal of the anion-uric acid at one and the same time. In this way proof is adduced that the lithium penetrates the tissues, and coming directly into contact with uratic deposit, tends partly to dissolve it.
To achieve the dual purpose, viz., absorption of inflammatory and uratic deposits, we may with advantage give the chlorine or iodine ions, for their sclerolytic effect on the tissues, in alternate sittings with the lithium ions. When time is no great object, two or three séances a week will suffice, but where time presses, the sittings, according to Leduc, may be given daily, always provided[409] that the position of the electrode and therewith the direction of the current in its passage through the joint be changed at each application. It is necessary to emphasise the fact that the use of too mild currents is futile, and to secure adequate results a prolonged series of séances is necessary. Also I would suggest that the simultaneous taking of a course of atophan would appear to be indicated.
Surgical Treatment.—In pre-antiseptic days, catastrophes, e.g., erysipelas, gangrene, etc., having occasionally followed the evacuation or removal of tophi, it was deemed inadvisable to interfere with them by any surgical methods. But, the danger of sepsis having been largely removed, it is now regarded as quite permissible to attempt the removal of uratic deposits for aesthetic reasons, or, more cogently, when they give rise to pain or restrict the movement of the related articulations.
Moreover, the old view that incision or evacuation of tophi was followed by obstinate ulceration is not borne out by modern experience. Thus my colleague Lindsay found that healing takes place quite naturally provided the incision is made over the more healthy skin towards the base of the swelling. With this I am in agreement, and furthermore would suggest that tophi when of large size and fluctuating are better opened with aseptic precautions than allowed to evacuate their contents spontaneously, for in this last event suppuration ensues, the sores become troublesome, and remain open for a long time. Sir Alfred Garrod in such circumstances advised touching up of the indolent parts with nitrate of silver.
In my search through the literature I have only come across two instances in which operation has been undertaken for the removal of gouty deposits in relation to tendon sheaths, bursæ, and skin. These were performed by Alexis Thomson. In one the subject was a medical man, aged thirty, the subject of inherited gout. Multiple tumour-like nodules, ranging in size from a pea to a cherry, were located over the knuckles, and the same were attached to the extensor tendons and moved with them. At the patient’s request, they were removed on account of their unsightliness. Their dissection from the tendons was achieved with some difficulty, and healing, though retarded a little by watery discharge from the wounds, was “in the end quite satisfactory.”
The other example occurred in a tailor, aged thirty-seven, in whom massive tophi developed at many sites. The larger deposits were located over the left external malleolus, the left olecranon, and the right malleolus. Because of their exposure to injury and pressure, removal of these various gouty tumours was decided upon. In all save the specially large swelling over the[410] left external malleolus this was easily accomplished by cutting through the surrounding healthy tissues. But that at the site named “was so fixed to the bone that it had to be separated with a chisel; it was then seen that the chalky deposit occupied spaces in the spongy interior of the bone, and in the substance of the internal lateral ligament; the removal of the chalky material in the area of the wound was carried out more satisfactorily by scrubbing the tissues with gauze and hot water than with the sharp spoon. The peronei tendons exhibited a very pretty deposit of urates under the endothelium covering them.”
Healing of the wounds took place very satisfactorily, and nine months later the general health was excellent; no further tophaceous deposits had accumulated, and the scars of the wound had remained quite sound. As Alexis Thomson observed, that though, even as this particular case showed, spontaneous disappearance of tophi may follow a subsequent attack of gout, still such could not be hoped for in the case of a massive deposit in the left internal malleolus, invading as it did the interior of the bone. He sums up his conclusions in the following words: “My own experience is limited. So far as it goes, it establishes not only the safety of the removal of gouty tumours by surgical means, but also the improvement in the general health which follows the removal of large masses of urates from the exposed parts of the body. So far as appearances are concerned, the substitution of linear scars for unsightly tumours is a decided improvement.”
Now, if we take Riedel’s two instances of acute gout and their tolerance of incision and local cleansing of urates and the equally happy tolerance exhibited by Alexis Thomson’s two cases of chronic gout, we see that, in these days of aseptic surgery, even gouty arthritis can no longer be regarded as outside the pale of operative interference. But, as a caveat against rash ventures, I would point out that recently I canvassed the desirability of operation in a case of massive tophaceous deposits in the hands and feet; but fortunately a skiagraph was taken which revealed that several of the phalangeal shafts had at some sites in their length undergone total absorption.
Nevertheless, given sound general health and failure of other modes of treatment, I think that operative measures should be seriously considered, for in the more inveterate types of tophaceous gout the crippledom and painful ulceration renders the victim’s life a misery, and one incapable of appreciable amelioration by medicinal or other methods of therapy.
When dealing with the clinical account, it was pointed out that acute gout is frequently complicated by symptoms pointing to involvement of the fibrous tissues in muscles and nerve sheaths; moreover, that both during acute attacks and alike in the inter-paroxysmal periods gouty subjects are prone to two special varieties of fibrositis, viz., lumbago and sciatica. I may add, too, that in these individuals it is not uncommon for them to suffer with these local varieties of fibrositis from time to time prior to the advent of regular or articular gout.
Fibrositis.—As Bassett Jones and I in our work on fibrositis have dealt exhaustively with the treatment of its various forms, our remarks here must necessarily be devoted largely to the general principles of therapy, and for further details we would refer the reader to our treatise on the subject.
Whatever the type of fibrositis we are confronted with, the therapeutic indications are precisely similar to those advocated for articular gout. In other words, the indispensable preliminary measures are to control the production, absorption, and elimination of toxins. To this end, we must secure adequate evacuation of the bowels, free action of the skin, and diuresis. These ends will the more surely be attained if at the onset a temporary fast be enjoined, or a suitable dietary with copious drinking of bland, unirritating fluid. The general malaise and pyrexia indicate clearly that these cases of acute fibrositis must be treated in accordance with the general rules applicable to the febrile state.
Acute Lumbago.—Brisk purgatives are here our most efficient allies, for there is usually marked functional derangement, with high-coloured urine and dark, offensive fæces. In such cases it is well to give 3-4 grains of calomel at night, followed in the morning by a saline purge, and the same often has to be repeated once or twice during the acute stage. Also the following prescription, preferably rendered effervescent by adding a few grains of citric acid to each dose, may swiftly abate the intensity of the suffering:—
| ℞ | Pot. bicarb. | gr. 15 |
| Pot. nitrat. | gr. 10 | |
| Vin. colchici | ♏︎ 10-15 | |
| Aquæ ad unciam, quartis horis sumenda. | ||
Or, as in acute gout, we may give an initial large dose of 30-40 minims of colchicum wine, with subsequent attenuation of the same. It is in cases with scanty, high-coloured urine and costive bowels that colchicum succeeds best. On the other hand, in some[412] cases of acute lumbago the urine is copious and light-coloured, and the bowels regular, and the fæces normal in appearance. Here the value of the initial purge is not so apparent, and a mixture containing salicylates and alkalies will be more likely to give relief, aided, if necessary, by nightly doses of Dover’s powder, followed by a morning draught of some aperient.
Where the case shows some disposition to linger on in a sub-acute form, and the urine still remains charged with lithates, a mixture of citrate or nitrate of potash, spirits of nitrous ether, and infusion of buchu should be given thrice daily. Sometimes, too, in broken-down subjects with sluggish circulation, we have found the addition of a few minims of tincture of digitalis most helpful in clearing up the condition.
Next to lumbago, pleurodynia is the most common muscular type of fibrositis to be met with in the trunk. I have seen its subsidence prove the signal for an outbreak of acute articular gout in the great toe. This significant sequence indicates the necessity of being alive to the possibility of a gouty basis in such cases and the advisability of combining colchicum with our remedies.
Sciatica.—This almost invariably is the outcome of a preceding attack of lumbago, of which, indeed, it is but an extension. If seen sufficiently early, and certainly when there are febrile symptoms, a mercurial purge, followed by an alkaline and diuretic mixture in combination with colchicum or salicylate of soda, should be resorted to vigorously, so as to abort, if possible, the attack.
If the underlying constitutional anomaly has been correctly diagnosed as gouty, the colchicum will exert its specific effect, and quickly, and the more speedily the sooner it is exhibited in the early stage. But even when seen later it is well worth trying the following combination:—
| ℞ | Quin. hydrochloratis | ½ drachm. |
| Pot. iodidi | 2 drachms. | |
| Vin. colchici | 1 ounce. | |
| Tinct. aurantii | 2 ounces. | |
| Aquam chloroformi | To 8 ounces. | |
| Sig., 2 teaspoonfuls in a wineglass of water twice a day. | ||
Having regard also to the gouty origin, it is hardly necessary to insist on regular and adequate evacuation of the bowels.
Of all varieties of gouty fibrositis the acute brachial type is the most difficult to treat, owing to the marked tendency to prolongation of the acute stages. The only chance of cutting short such an attack is not to treat lightly its earlier manifestations, but to[413] bear in mind its evil potentialities; but only too often they do not come under observation until the condition is well established.
Gowers, who has written so illuminingly on this particular type of fibrositis, obtained the best results in the early stages from a combination of nitrous ether, citrate of lithium, and colchicum, with in addition, in the more intense forms, small doses of perchloride of mercury. Of the salicylates, salicin and aspirin, he speaks with but faint praise, and I have myself known them afford but little aid.
In reviewing the foregoing acute types of fibrositis, I would, as to relief of pain, insist on internal medication of all sorts being held as purely secondary to the infinitely more important matter of procuring rest and fixation for the inflamed structures. Immobilisation, indeed, supplemented by thermic and anodyne applications, hardly, if ever, fails to alleviate the suffering. If these prove futile, aspirin and phenacetin, either singly or in combination, should be exhibited. Here I would remark also on the value of cimicifuga, which I have found strikingly useful. Lastly, only very exceptionally in my experience is morphia called for.
In chronic or recurring forms of fibrositis we should mark any deviation from health in the shape of gastro-intestinal or hepatic derangement, while noting also any inactivity on the part of the kidneys or skin. As to drugs, chief reliance must be placed on the iodides guaiacum, arsenic, and sulphur. They are most useful, of course, when exhibited during the early stages, before organisation of the inflammatory products ensues. When hard and resistant nodules or infiltrations have formed, their administration is of little value.
It is for this reason that I have elsewhere advocated early resort to local massage, viz., at the close of acute attacks, as only by this means can we hope to dissipate these new formations, the persistence of which determines the inveterate tendency to recurrence. In the space at my disposal it will be impossible to consider in detail all the special modes of therapy—electrical, thermal, hydrotherapeutic, etc.—and for this information I must refer the reader to the next chapter.
Oxaluria.—This condition is sometimes met with in the gouty. The subjects are often nervous, irritable, and languid, complaining at the same time of vague pains, most frequently in the loins and along the distribution of the sciatic nerve. It occurs more commonly in persons of sedentary habit, and correction of this, as well as revision of their diet, is almost the only effectual method of getting rid of the complaint.
All vegetables rich in oxalates, such as rhubarb and spinach,[414] must be eliminated, and likewise tea. At the same time, as Sir Alfred Garrod suggests, we should, to influence the proportions of the bases present in the urine, cut off all foods rich in calcium, i.e., milk and eggs. On the other hand, we should advise the intake of such as are rich in magnesium and yet poor in oxalic acid, viz., peas, beans, and coffee, and oxalate-free foods, such as all kinds of meat.
In my own person I suffered for some weeks with obstinate lumbar pain, the cause of which appeared to be obscure until the existing state of oxaluria was discovered by a professional colleague. I would here emphasise the fact that when a case of lumbar or sciatic pain is defiant of cure by the usual methods of therapy we should always suspect this possibility of oxaluria, for commonly the urine is copious and clear; hence perhaps the frequency with which the condition is overlooked.
As to medicinal measures, we should bear in mind that Sir John Rose Bradford pointed out that the production of oxalates was initially due to deficient HCL, with secondary fermentation of foodstuffs, i.e., carbohydrates, especially sugar. The primary indication, then, is to reinforce the digestive capacities by administering hydrochloric acid or, as many prefer the dilute nitric muriatic acid, in combination with nux vomica, and in some cases pepsin. As Sir William Whitla remarks, if organic acidity be prominent, this may be intensified by mineral acids, in which event alkalies combined with a few grains of papain two hours after meals are indicated.
In conclusion, the nerve element in these cases is so pronounced that a thorough change of air and habits is often indicated, combined with freedom from worry, abundance of exercise, and a stimulating course of hydrotherapy.
Glycosuria.—The variety met with in the gouty, being of the alimentary type, is usually very responsive to dietetic measures, and these have been already dealt with. A course of spa treatment is often the best possible mode of therapy for these cases.
As to medicinal measures, these certainly should not be embarked upon until the effect of dietetic revision has been ascertained. If under their influence the glycosuria wholly disappears, then drugs may be uncalled for, save perhaps occasional aperients, antacids, or similar remedies of like nature. If, on the other hand, the glycosuria cannot be kept under control by dietetic measures, then recourse must be had to drugs. Here it may be noted that guaiacum diminishes the amount of sugar excreted, and it may be given a trial before resorting to codeia. Generally speaking, when the case requires codeia it has passed out of the realm of gouty glycosuria into that of true[415] diabetes, the treatment of which grave disorder is beyond the scope of this work.
Hyperchlorhydria.—The disorder is rare in gouty patients, and its diagnosis from organic acidity cannot be made without examination of the stomach contents. Moreover, when found to be present an endeavour should be made to elucidate its cause. If gastric and duodenal ulcer can be excluded and the condition appears to be of the nature of a secretory neurosis, then the underlying nervous defect will call for treatment.
In some cases the exciting cause lies in errors of diet and habits of living. These when faulty require correction; very often in these cases it is not so much the nature of the food as the hurried manner in which it is bolted that is responsible. At times, when free from hurry or worry, they can eat any kind of food with impunity. When the attacks are on, it frequently happens that all types of food, whether easily digestible or not, are equally provocative of acidity. We see then how large a part general hygiene plays in the successful treatment of these cases.
As to diet, this is, of course, of primary importance, the main indications being the reduction or withdrawal of farinaceous foods, and for a short period on a Salisbury regimen or some modification thereof.
The medicinal indication is to afford relief during the acute attacks. Fortunately these are usually intermittent, and when the occasion arises are fairly readily controlled by massive doses of alkalies, frequently combined with an artificial digestive, i.e., papain. While magnesia and bicarbonate of soda are, as a rule, invoked, others speak well of sodium phosphate (5 grams) with menthol (0·25 gram), given two hours after each meal.
Luff, discussing hyperchlorhydria in the gouty, highly extols hopogan (magnesium peroxide), in doses from 20-30 grains, one hour after food, the amount to be reduced if it causes purgation. To inhibit excessive production of HCL, belladonna, in 5-minim doses of the tincture, before meals results in reduction of acid values, both absolute and relative, of the stomach contents, and, moreover, relieves spasmodic contractions. Constipation in these gouty subjects is best combated by an occasional nightly pill containing colchicum in combination with aloes or other laxative. Lastly, when digestion becomes more normal nervine tonics, such as arsenic, valerian, and the like, may be given to correct, if possible, the underlying nerve element in these troublesome cases.
Gouty Phlebitis.—To obviate the risk of embolism, absolute immobilisation of the affected limb is imperative, and it should be slightly elevated and protected by a cradle. In many cases[416] it will suffice if the limb be enveloped in cotton wool and a broad, many-tailed bandage lightly and evenly applied. If the pain be severe, equal parts of glycerine and the green extract of belladonna should be smeared along the course of the inflamed vein and hot fomentations applied. Internally saline aperients should be given to secure daily evacuation of the bowels, and a mixture containing iodide of potassium and ammonium carbonate taken three or four times a day, to promote solution of the clot.
Gouty Eczema.—In these cases the primary indication is to revise thoroughly the diet, to the end of correcting a frequently associated gastro-intestinal derangement, notably any tendency to constipation. If these the basal indications are not fulfilled, all local forms of medication will be futile. As to these last, the primary desideratum is to protect the parts from all accidental irritants, and the chief source of offence is scratching by the victim himself. Otherwise we should take every care to prevent irritation by clothing, hard collars, etc.
While cleanliness is essential, the soaps used should be of the neutral kinds, or bran or barley-water substituted. Ointments and lotions are best avoided. In the milder cases protection of the parts is the essential. In the limbs this may be attained by glyco-gelatine zinc; but on the neck, the groin, the inside of the thighs or lower parts of the abdomen, the tragacanth pastes or similar preparations are more suitable. Both the gelatine and the pastes and varnishes may be readily medicated with drugs of anti-pruritic properties, such as oil of cade, carbolic acid, resorcin, or salicylic acid.
Gouty Nephritis.—This must be treated on the lines recognised as suitable for chronic Bright’s disease, the underlying gouty condition being always borne in mind, as also any contamination with lead. As general measures any excess in eating or drinking must be avoided, the skin kept active, and the bowels open; and where possible favourable climatic conditions should be attained.
Frequently the treatment resolves itself into that of the associated arterio-sclerosis with high blood pressure. This we should endeavour to control by regulation of the subject’s habits in the matter of diet, work, exercise, etc., rather than by flying forthwith to the use of vaso-dilators, premature resort to which has often proved the beginning of the end.
Moreover, I would, like many others, strongly deprecate the far too prevalent practice of dilating to these subjects on the evil potentialities of raised blood pressure. Not a few thenceforth literally walk in the valley of the shadow, and the fear of sudden death is ever before them. It is not only cruel, but frequently unnecessary. Often the increase of tension is no more than their[417] age would account for, and equally often no symptoms indicative of raised blood pressure are complained of. Why then make the subject miserable?
By all means, take the blood pressure, but say as little as possible about it. These people, in my experience, need more often to be reassured than frightened. Only now and again does one meet with individuals who must for their own sake be gravely warned of the dangers incidental to their condition, men who, despite the warnings afforded by giddiness, epistaxis, etc., will not alter their ways of living.
As to medicinal measures, all agree that an occasional blue pill or a dose of calomel, ½-1 grain, for three or four nights in succession, and followed in the morning by a saline purge, is one of the most satisfactory procedures to adopt. Hand in hand with this, a course of iodides, gr. 10-15 three times a day, for some weeks, is also most beneficial. After six or eight weeks of the above we may substitute a course of nitrites, e.g., nitro-glycerine, sodium nitrite, or erythrol tetranitrate. Nothing is better in the milder cases than Sir Lauder Brunton’s formula, the efficacy of which I have often proved:—
| ℞ | Sodium nitrite | gr. ½-2 |
| Potassium nitrate | gr. 10-20 | |
| Potassium bicarb. | gr. 10-30 | |
| Fiat pulvis, to be taken in a tumblerful of water every morning. | ||
Needless to say, vaso-dilators should not be exhibited if signs of waning cardiac power are evident. Also when there is much albumen the use of mercurial purges calls for great discretion, and saline aperients should be given the preference. Insomnia, a frequent trouble in these cases, is best met by bromides, and I agree with Luff that in gouty subjects sleeplessness is better combated by measures which reduce arterial tension than by resort to hypnotic drugs.
Lastly, symptoms of cardiac dilatation and failure, which should be suspected when the arterial pressure falls without the previous use of vaso-dilators, will call for the exhibition of cardiac tonics: digitalis, strophanthus, and strychnine; and threatened uræmia may be postponed by a judicious dietary, saline purgation, and diaphoretic measures.
While, naturally, individuals display wide differences in their capacity of adjustment to variations in climate and season, there is no doubt that the gouty, as a class, are abnormally deficient in their power of adaptation in this respect. Said Hippocrates in one of his aphorisms, “Podagrici affectus vere et autumno plerumque moventur,” and this peculiar influence of season, viz., the aptness of gout to recur in spring and autumn, especially in its early stages, is a very singular feature.
The increased incidence at these particular periods of the year is, I think, a striking proof of their deficiency in the defensive mechanisms that enable normal persons to withstand with comparative impunity sudden transitions from cold to heat, dryness to damp, and so forth. So it is that rapid changes in the surrounding air, in its degree of warmth, or its motion by wind are fertile of attacks. The east and north-easterly winds of spring account for no few examples, as likewise inadequate protection from cold or damp.
In short, a variable climate is the most provocative of gout, that is, most likely to elicit gouty manifestations in one predisposed thereto. Conversely, stability in climate favours freedom from attacks. Thus some obtain exemption from their gout by removing to a hot climate, others when removed to one of cold, dry character. Doubtless these differences in response hark back to individual constitutional peculiarities.
It is the vigorous plethoric persons, who eat too much, that do well in dry, cold climates. The low temperature and dryness of the air stimulate tissue changes, dispose them to active exercise with consequent increased efficiency of digestion, assimilation, and excretion.
On the other hand, many victims of gout are spare feeders, with feeble powers of digestion and metabolism, and for them a mild, moderately warm and not too damp climate is the more suitable, involving, as it does, less strain upon their capacities of adjustment.
If one may be permitted the generalisation, the ideal climatic[419] conditions for the gouty are low relative humidity, abundant sunshine, and a low rainfall. But, alas! too often, permanent residence in such desirable surroundings is unattainable, and the most that can be compassed is a brief sojourn in some more congenial environment.
Still, some discrimination must be shown in the matter of choice, and the physician, while mindful of the gout, must envisage the individual as a whole; for in advocating a change of climate his hope is that he may remove or antagonise certain noxious influences and coincidently restore the physiological machine as near as can be to a state of functional efficiency.
The former purpose will often be fulfilled by mere withdrawal of the subject for a time from his usual calling and environment. How frequently will simple rest and recreation succeed when medicinal and other forms of therapy have wholly failed! And how largely, may we remark, does the Vis Medicatrix Naturæ work through the medium of things psychic, not physical, to achieve its beneficent ends!
Still, not always is it rest that is needed, and some regard must be had to previous habits. Thus, for the sedentary, repair to a bracing climate is indicated, some inland resort of moderate elevation, where oxidation processes are quickened, and where if they eat more they take more exercise, and so adequate elimination is assured.
On the other hand, for the elderly or old, or those enervated by long-continued gout, a sedative climate must be sought, one marked by mildness, dryness, and equability. Bath, with its low diurnal range of temperature, is eminently suitable for this class of gouty patient, who often stand but ill the, for them, too stimulating qualities of more bracing localities, such as Llandrindod, Harrogate, or Buxton, etc.
Frequently, however, our choice is dominated by some associated morbid affection. Our patient may suffer from a so-called gouty eczema; if so, he must avoid cold, damp places, or windy localities, and, for that matter, sea air often, at first at least, aggravates the affection. Or it may be that he suffers with “dyspepsia,” some catarrhal condition of the alimentary canal, or a “sluggish liver.” For him, then, a dry inland health resort of moderate or high altitude is preferable to one of sea level, which will likely find him drowsy, indisposed to exercise, and a prey to what he terms biliousness.
If renal disease be a complication, he should seek a dry, warm climate, and, if he can, winter abroad, say, in Upper Egypt or Algiers, which, though it is warm and dry, is nevertheless somewhat marred by the wide diurnal range of temperature and the[420] not infrequent cold winds. If, therefore, very sensitive to vicissitudes of temperature, the relatively dry, warm marine health resorts of the Riviera are open to him.
If to go abroad is out of the question, one of the mild southwestern seaside resorts at home is eligible, i.e., Bournemouth, Sidmouth, or the more sheltered parts of Torquay, and Falmouth. Again, if he show a tendency to cardiac dilatation, with or without valvular disease, high altitudes will obviously be unsuitable, and dry, inland resorts of moderate or low elevation should be given the preference.
Lastly, before despatching any gouty subject for a so-called change, it is wise to elicit any personal idiosyncrasies that he may be victimised by. In other words, find out his most vulnerable points. Thus some gouty persons are able to brave cold and damp with impunity, but pay dearly for the slightest indiscretion in diet. They must therefore be warned that no climatic change, however suitable, will absolve from the ill-effects of improper or immoderate eating.
Others again—the majority—are extremely sensitive to atmospheric changes, and such good as they might derive from a well-selected climate is nullified through thoughtless omission of simple precautions against “chills.” In short, the victims of gout can only ensure for themselves the beneficial effects of climatic therapy if, at the same time, they vigilantly shield themselves from what experience has shown to be, in their particular instance, the most fertile extrinsic or intrinsic source of relapses or exacerbations of their disorder.
Choice of Residence.—In these days it may savour of irony to talk of a choice of residence where none is. Still, much of the benefit accruing from a change of air will depend not only on the place resorted to, but the situation of the dwelling or hotel, in which the subject takes up his temporary abode. Thus in inland resorts some parts of the town may lie in a hollow, others on adjoining slopes or plateaux at an altitude higher by some hundreds of feet. Sites like the latter are obviously unsuitable for the victims of cardiac dilatation, etc. Again, where the patient’s condition is such that he must perforce spend a large portion of his time indoors, it is a matter of some moment that the situation and aspect of the building and, more pertinently, the subject’s suite or room be ascertained before he takes up residence.
Apart from sanitary and hygienic considerations, the quality of the cuisine, general comfort, class of society, have all to be thought of, if the best results are to be obtained. They are not unimportant details. How often is the benefit of a stay nullified by uncongenial surroundings, by a gloomy outlook, the fret and[421] jar of ill-assorted or discordant elements, that forbid that cheerful intercourse that does much to restore that sense of bien-être so eagerly sought.
In short, attainment of the best results of climato-therapy can only be achieved through the medium of a closer co-operation between those who practise at health resorts or spas and the patient’s usual medical attendant. But, meanwhile, for most of us, our dwelling place doth rest upon our calling, and we may take this for our comfort that climatic vicissitudes may be greatly mitigated by a well-situated and sanitary residence. I allude, of course, here to a permanent abode, and the gouty, if he enjoy any latitude, should live in a house built on a well-drained gravel soil on a slope, sheltered from the north and north-east winds.
Again, with the question of habitation is bound up the equally important matter of clothing. By our forefathers flannel underwear was deemed the most eligible, despite its low or deficient power of absorption. But, without discussing the various arguments adduced in favour of this or that particular fabric, I would myself favour silk as being, perhaps, the ideal underwear; next to this a single woollen or woven linen vesture, and it goes without saying that, prone to excessive sweating as these gouty subjects are, frequent changes are essential. The feet of the gouty are their weak spot, and, apart from the correction of static deformities, flatfoot, etc., it is extremely desirable that they not only be well shod, but be especially careful not to sit about in wet boots or socks.
For the rest, their outer layers of clothing should be light, warm, easy and not tight fitting. Extremely liable as they are to lumbago and sciatica, they should be careful to enlist a thicker fabric than is usual for the back of their waistcoats; while sufferers from sciatica may, with advantage, insert a silk lining to the seat of their trousers.
Lastly, it is most important that the gouty, and of course all persons, should dress according to the prevailing weather and not according to the time of year. For them, more than any other class of person, to doff summer and don winter clothing for no other reason than some arbitrary date is fraught with mischances, freedom from which would be purchased by a little commonsense.
It has been wisely said that “those threatened with gout should imitate as far as practicable and consistent with comfort the habits of agricultural labourers,” for sedentary occupations[422] and idle ways not only favour the invasion of the disorder but hasten its recurrence.
How frequently, indeed, is it the direct outcome of an abrupt change in habits—a hunting man, predisposed to gout, sustains an accident, can no longer ride to hounds and takes to motoring. Unless he forthwith curb his food intake, the disorder overtakes him. Sometimes misfortune proves a blessing in disguise, as in the case related by Van Swieten of an opulent and gouty old priest, who, captured by Barbary corsairs and forced to work as a galley slave, soon lost his gout.
Again, it is notorious that in those in whom the brunt of the disorder falls on the lower limbs, the outlook is more sombre than in those more severely crippled in the hands. In short, capacity for and willingness to take adequate exercise is one of the most potent measures wherewith to fend off the gout. The amount should be in proportion to the age, strength, and previous habits. The exercise should be taken not after a spasmodic but systematic fashion. For erratic, like excessive, exertion often converts the expected benefit into the exciting cause of an attack. The aim should be not exhaustion but wholesome fatigue.
Young and fairly vigorous persons, if previously sedentary or indolent in habit, should take regular exercise, gradually increased. In the middle-aged, especially if obese, it should be graduated according to the capacity of their circulatory organs, and more stress laid on respiratory exercises and dietetic restrictions. For in their instance fatigue or over-exertion is easily induced, often with grave consequences. Also, in long-standing cases, neurasthenic from long-continued pain, it is well to begin more or less tentatively, and in many cases to prescribe a course of massage before proceeding to active exercise. For not seldom such subjects have but a small fund of nerve energy to draw upon.
In the gouty, even the malign influence of bad habits of living is greatly mitigated by active exercise and labour. “The gout very rarely visits the poor man’s cottage.” Nothing can so effectually counteract a predisposition to the disorder, and what Sydenham thought of its value we may guess from his trenchant remarks on horse exercise. “And, indeed, I have often thought if a person was possessed of as effectual a remedy as exercise is, in this and most chronic diseases, and had the art likewise of concealing it, he might easily raise a considerable fortune.”
In conclusion, if healthful exercise of the body is imperative for the gouty, I need scarcely labour the desirability also of congenial and adequate exercise of the mental faculties. Adequate, but not excessive, lest, like Sydenham, it reacts in added sickness.[423] Otherwise absorption in some honourable pursuit will do much to dissipate that tendency to introspection and depression so often born of the consciousness of an ever-constant menace to long-continued health.
In judiciously prescribed and skilfully applied massage we have an agent of pre-eminent value in the treatment of gout. Indeed, Sir William Temple—a martyr to the disease—when speaking of the benefit of “friction,” frankly stated that “No man need have the gout who can keep a slave.” In this there is much truth, for the beneficial results of massage are not confined merely to the affected joints or muscles, but, as a result of the improved circulation, waste products are more readily excreted, the nerve centres regain tone, and a general feeling of bien-être is promoted.
It cannot be doubted that general massage of the trunk and limbs accelerates the elimination of the chemical outcasts of metabolism, and simultaneously, by ensuring a more adequate supply of fresh blood to the tissues, must result in an access of renewed vitality. Many, indeed, have adduced experimental proof that such a quickening of the vital processes does ensue after general massage. We should therefore, in elderly or feeble subjects, or in those of sluggish habits, advocate from time to time a course of general massage for its prophylactic effects.
It is the more especially indicated in those gouty subjects prone to attacks of muscular fibrositis—attacks of which are undoubtedly favoured by the retention of the toxic and waste products of muscular metabolism. Nothing, again, so facilitates the dissipation of exudates, nodules, or thickenings in these structures, for the treatment and prophylaxis of which massage is indispensable.
In enlisting the prophylactic action of general massage, it is not desirable that the séance should exceed forty minutes, and it should in all cases be followed by an hour’s rest; to practise it too soon after a meal is inadvisable, and in those cases in which it favours the advent of sleep it is best undertaken in the late evening.
In conclusion, I would urge the importance of more interest being taken by the physician himself in the technique of massage, as I am assured that, if rationally and perseveringly practised, it constitutes one of the most valuable adjuncts in the prophylaxis of gout.
That hydro-therapy constitutes one of the most effective, if not the most effective, methods of treating gout, is almost a truism, if judged by that most “acid test”—Experience. The particular applications we are about to discuss entail exposure of the whole body. In other words, those measures directed more especially to treatment of the underlying causal state—the correction of that warp of metabolism or auto-toxic state of which the arthritic, muscular, or other lesions are but local manifestations.
It goes without saying that, with this for our objective, there is much need for discrimination in the selection of measures suitable for individual cases, and, naturally, the basis of such differential treatment is thorough physical examination prior to embarking on the course. Yet how frequently on their own initiative do these subjects enter lightly upon a series of baths, mingling stimulant and sedative procedures in haphazard fashion, unwitting that hydriatric measures are capable of infinite harm when misapplied.
For in hydro-therapy the personal equation is of prime importance, varying with individual reactive peculiarities. In short, the character of the response differs widely in different subjects, efficiency or not of the nervous and circulatory functions being the chief controlling factors. Hence accurate appraisement of the reactive powers of the constitution to hot and cold applications is the basis of rational hydro-therapy.
Thus nervous irritability is the outstanding characteristic of some gouty constitutions. They are therefore intolerant of extremes of temperature, and for them sedative or sub-thermal baths are the most suitable.
Others suffer from torpid circulation and sluggish vascular response, and in their instance, stimulant measures, hot or cold, in sequence or in alternation, are indicated. Again, some are obese, and others lean, and while of the twain the former react more feebly, on the other hand, they stand prolonged courses of hydro-therapy more satisfactorily. In contrast, the thin, though they react well, are more readily exhausted, and so apt to suffer from “secondary chill” or other untoward consequences.
Prophylactic Measures.—As we have noted, the “gouty,” more than others, are intolerant of atmospheric vicissitudes. Accordingly, if we would strengthen their defensive mechanisms in this respect, we must endeavour to train them to react more adequately to cold or sub-thermal impressions.
Of the value of thermal applications in chronic gout I am convinced, but, on the other hand, we must not blind ourselves to the value—prophylactically speaking—of their judicious conjunction[425] with sub-thermal or cold procedures. For these latter stimulate oxidation processes, and in chronic gout, according to many, there is deficient oxidation of protein waste, while, apart from this, in the gouty obese there is imperfect oxidation of adipose tissue.
Prophylactic measures to be of any real avail must be continuous, and spas or hydropathic establishments should indeed be more alive to their educational responsibilities in this matter, for the benefits of hydro-therapy as regards prophylaxis are within the reach of all possessed of the convenience of a modern bath-room.
They should be taught to inure themselves by taking daily a tepid bath followed by a cold shower or rain spray. If this be too drastic, let them, while standing in warm or tepid water, briskly rub the rest of the body with a coarse towel wrung out of cold water, into which, if liked, salt has been added to the point of saturation. In this way the tonic effects upon the skin of hypo-thermal or cold applications may be invoked, and thereby its undue sensitiveness is reduced and therewith the liability to subsequent attacks.
It now devolves upon us to consider under what circumstances hydro-therapy is inadvisable, and, incidentally, those ill-effects that indicate its modification or abandonment.
Contra-indications and Untoward Complications.—Authorities generally seem unanimous on this point, viz., that the chief sphere of hydro-therapy is in chronic or subacute gout. On the other hand, they are equally unanimous in proscribing its exhibition in acute forms of the malady. Speaking for myself of the Bath waters, I am quite convinced that the distinguished physician, Caleb Hillier Parry’s pronouncement, “that the Bath waters, in no form whatever, are beneficial during the paroxysms of gout, or in any inflammatory disposition which may exist in the interval,” is not only true but capable of extension to all forms of hydro-therapy as applied at this stage of the disorder.
Nor do I think it advisable if prodromal symptoms suggestive of the imminence of an attack are present. It is too, I think, impolitic—after the subsidence of a severe attack—to resort too quickly thereto, the more especially if there is a disposition to what our forefathers termed “flying gout.” In either event, an acute outbreak is most likely to ensue, and, though there is doubtless some truth in the old idea that a gouty subject feels better after an attack, still it is not, I think, the physician’s rôle to evoke gout, but rather to prevent its explosion. Occasionally mischances of this sort will happen, but only exceptionally, if the foregoing safeguards be respected. Certainly if the patient seems[426] palpably on the verge of an attack it is but discreet to postpone baths until the good effects of free purgation and strict dieting have been derived.
Indeed, I would go further, in that I think that, under all circumstances, a course of hydro-therapy should be preceded by free evacuation of the bowels. We should then hear less of that disturbance of the system known as “well-fever” or “poussée-thermale,” which, it is not sufficiently recognised, may follow not only internal but external use of mineral waters. I allude to dyspepsia, lassitude, or skin eruptions, etc., symptoms which formerly were thought to be of critical or beneficial nature, but which, I agree with Dresch, are probably the result of an auto-intoxication, and, as he thinks, more or less combined with an infection by the bacillus coli. Should such symptoms supervene during a course, the baths had better be omitted for two or three days pending their disappearance under appropriate measures.
In the same way, there are reservations regarding the suitability of baths in chronic gout. Thus, if complicated by advanced cardiac or renal disease, hydro-therapy is often contra-indicated, and, in any instance under such circumstances, has to be undertaken very cautiously. On the other hand, it is wonderful how well many examples respond if due discrimination be exercised. Especially suitable are those cases of gout and renal disease in which the heart is hampered by increased peripheral resistance. Such cases under Aix massage, frequently, as Bain and Edgecombe pointed out, improve strikingly through the consequent reduction of arterial pressure.
Turning now to the untoward results or complications of hydro-therapy, hot baths, if of too high a temperature or too prolonged, may cause vertigo, fainting, or palpitation—an indication for reduction in temperature and duration. Or, if douches are used, the pressure may be excessive. Insomnia, again, may follow over-stimulation, and our measures must be altered accordingly. Loss of appetite and strength, too, may be the outcome of too drastic treatment and excessive reaction.
It is well, also, that during a course of hydro-therapy the patient’s body weight be taken from time to time, and note made whether he is gaining or losing in muscular strength. If weight sink and, coincidently, strength increase, all is well with the gouty obese; but if muscular capacity be waning, excessive demands are being made on the subject’s oxidising and eliminative processes.
Examination of the urine, too, may yield indications of value. A notable increase in the output of chlorides suggests excessive tissue waste, and of phosphates too marked excitation of the nerve[427] centres, and the appearance of albumen or sugar, if previously absent, will indicate reduction in intensity of the hydriatric procedures. In short, we should be alive to the profound influence of hydro-therapy on general metabolism and the consequent necessity of medical supervision throughout the course.
Subject to reservations, stimulant hydro-therapeutic procedures are in chronic gout the special indication. Thermal waters, therefore, are, generally speaking, the most suitable, and cæteris paribus, the higher the temperature the greater the excitant action. Of natural thermal baths, those of Bath, Aix-les-Bains, Gastein, Wiesbaden, etc., enjoy great repute, and, judging from personal experience of the first-named spa, I doubt not that—given due discrimination—all waters of this group are unquestionably beneficial.
Having regard to their radio-active properties, the best results are undoubtedly to be obtained by a combined bath, drink, and inhalation cure. Simple immersion baths, deep or reclining, with or without massive under-current douches, enjoy well-deserved vogue for their general and local effects.
Moreover, as the local douching exerts a sedative as well as a resolvent effect, they prove most useful not only in articular gout, but in the treatment of those frequent concomitants, lumbago and sciatica. Their efficacy is much enhanced by coincident or subsequent massage, and to increase the powers of resistance, such hot baths should be followed by graduated sub-thermal or cold applications.
Sool-Bader, or natural thermal brine waters, exert a similar effect, but such are not available in this country. But cold brine baths—given at temperatures of 98° F. and upwards—are obtainable at Droitwich, Harrogate, and Builth, and are invoked more particularly in long-standing cases with great thickening of the arthritic or related muscular structures.
Again, gouty subjects not seldom suffer with high blood pressure, and our treatment must be modified accordingly. Here we may enlist what are known as Aix massage baths, which tend to lower arterial pressure through the profound influence they exert on metabolism, and the elimination of toxic and waste products. As in warm immersion baths enervating after-effects are apt to ensue unless the tonic-bracing action of a terminal cold application be invoked. On the other hand, in some cases of chronic gout the abdominal musculature is very flabby, with a tendency to visceroptosis and low blood pressure. In their instance, a Vichy[428] bath, inasmuch as it tends to raise the blood pressure, is preferable to Aix massage.
Another powerful method at our disposal for the elimination of waste products is the vapour bath. It is not suitable for the old and feeble, or those with advanced cardiac or renal disease, but it is especially adapted to gouty subjects with harsh, thickened or irritable skin, and those of obese habit.
While the foregoing procedures, generally speaking, are eligible for the more robust type of individual, we must have regard also to those of delicate constitution, whose strength is sapped by long-continued gout, or who show signs of pre-senilism. In such instances, sub-thermal baths (82° to 97° F.) have a great sphere of usefulness. Thus in the presence of high arterial pressure, a course of immersion baths, say, at 93° F., combined with fan douches, and applied according to the Bourbon-Lancy method, are very effectual in reducing arterial tension. Of marked sedative action, such neutral baths are peculiarly eligible also for all types of gout associated with insomnia, irritable skin affections, or showing signs of vasomotor instability.
Moreover, these sub-thermal baths are valuable in articular gout of subacute or lingering character if the douches used are of low pressure, which latter is essential if the joints are sensitive. Their therapeutic action is of course more pronounced in those natural mineral waters which more nearly fulfil the requirements of a neutral bath. Such are possessed in high degree by the waters of Buxton, Ragatz, and Baden-Weiler, the average temperature of which approximates to the point of thermal indifference.
In one form or another, douches have for centuries been used for chronic joint affections. Three factors have to be considered—the volume, pressure, and temperature of the impinging water. The size and form of the stream determine its thermic and mechanical effect, and cæteris paribus, the more massive the volume, the more marked the results produced.
The pressure, again, is a most important factor, as the influence on the circulatory and lymph flow in deep-seated tissues is directly proportional to the force of delivery.
We see, therefore, that in douches we have a weapon of great power for good or ill, and the results achieved will be exactly proportional to the judgment displayed in meeting individual requirements in the matter of their temperature, duration, and pressure.
The space at our disposal forbids entering into great detail,[429] and a few general principles are all that can be enunciated. Thus, while extreme pressures are permissible in selected cases, they are contra-indicated when dealing with regions the seat of pain. In such instances we should always begin with mild measures, viz., a tepid fan or spray douche (80° to 92° F.) of low (4 to 8 pounds) pressure. These later may be replaced by a hot (104° to 110° F.) broken jet, or rain douche, of 10 to 15 pounds pressure, and by such graduated procedures pain will often be relieved.
For the relief of stiffness and swelling alternating jets or sprays are most suitable, the hot and cold douches being each of fifteen to thirty seconds duration. The more remote the extremes of temperature, and the more abrupt the transition from hot to cold, the greater the excitant effect.
Simultaneous massage greatly reinforces the stimulating and absorbing action of douches, which latter also may in various ways be advantageously combined with other local procedures, viz., local vapour, hot air, and electric light baths.
Enhanced oxidation and destruction of nitrogen-containing waste and toxins being one of the primary indications in the treatment of all so-called auto-toxic states, it is not surprising that hot air baths—both luminous and non-luminous types—are so extensively employed in gout, either for their curative or prophylactic action.
For the practical details of their administration I must refer the reader to special works on the subject, contenting myself with a brief reference to their therapeutic indications. While all gouty subjects at some period of their life-history may be eligible for hot air baths, their use is contra-indicated in pyrexia. Nor are they appropriate if the case is complicated by any irritable skin condition, or in the graver forms of glycosuria. They are unsuitable, too, if there are any evidences of hyper-thyroidism, from which the gouty, no more than others, are immune.
Again, in cardiac dilatation they must be exhibited with great caution, and where extreme, are of course impermissible, as also in the later stages of chronic nephritis. On the other hand, they are eminently suitable for the treatment of fibrositis in gouty persons, especially of obese type, nor does the presence of glycosuria in such association constitute a bar to their use.
Moreover, as a prophylactic measure, they are extremely well adapted to those victims of gout who lead sedentary lives, as to a limited extent they counteract the evil effects of muscular inactivity. Here also, by the judicious use of graduated after-applications[430] of cold or hypothermal grade, the undue sensitiveness of the skin in these subjects is reduced, and their liability to so-called “liver chills” diminished.
In conclusion, it is the proper blending of their eliminative and prophylactic qualities, according to individual needs, that constitutes the key to rational treatment by hyperæmia. These same postulates are applicable also to the various peat, mud, and fango baths, whose action in essence depends on the varying degree of hyperæmia they produce, and to which, in all probability, their well-established efficacy in gouty affections is attributable. That there are other valuable accessory methods of treatment—electrical, hydro-electric, etc.—in vogue at spas, I am perfectly aware, but the number of special works available for reference on this point relieves me of the necessity of alluding to them in detail.
Though many have tried, no one has yet been able to define exactly what does and what does not constitute a “mineral water.” Criterion after criterion has been suggested—chemical, therapeutic, thermic, cryoscopic, ionic, etc.—but to all there seem objections, and doubtless will be, pending the advent of more exact knowledge regarding these—the most complex pharmacological compounds in our Materia Medica.
Naturally, “mineral waters” being so refractory of definition, it follows that all suggested classifications are equally perplexing. In fact, all attempts to reduce them to order according to their generic and specific differences are, it must be admitted, unsatisfactory. Perhaps the most serviceable differentiation at our disposal at present is one based on their chemical composition. As Sir Hermann Weber says, “a statement of the salts contained in a mineral water often tells the ordinary medical man something of the nature and probable effects of the water in question, whilst the results of an analysis expressed in ‘ions’ would simply bewilder him.”
“Probable effects,” says Weber, and, I think, advisedly; for in estimating the effects of spa treatment how difficult to discriminate between what is due to “mineral waters” and what is due to change of air, diet, mode of life, and mental occupation. Yet, again, how bewildering the fact that “waters” of the most varying chemical content prove to be equally beneficial in gout. Small wonder, then, that physicians sought to refer their therapeutic efficacy not to their mineral constituents, but to the vehicle common to all of them, viz., to the diluent and solvent action of the water itself, its flushing effects in washing out urates and other toxic substances.
From this it was but a short step to the further assumption that, other things being equal, the drinking of water at home would do just as well as resorting to a mineral spring. But, as has been shrewdly said, the “other things” never are “equal.” What of the daily worries left behind, the change of air and scene, the modifications of diet, the leisure for outdoor exercise, not to mention hydro-therapy and other integral or collateral factors of spa treatment?
But, even frankly admitting our ignorance, the lessons of experience, nevertheless, can neither be flouted nor ignored, least of all in the treatment of gout. “Mineral waters” are but used empirically, says the critic, forgetful that the use of colchicum lies open to the same aspersion. Especially valid the imputation, as he thought, in regard to the so-called “simple” or “indifferent” thermal waters. These—despite the testimony of centuries to their worth—must be discarded in favour of some pseudo-rational method, and this, forsooth, because their mode of action seems inexplicable! Yet, by the irony of Fate, within a brief span these “indifferent” waters were found to contain a substance—“radium”—whose powers few, at present, pretend to gauge or limit. There seems, in truth, a peculiar fitness in the coincidence that it should be in this very group that experimental investigations have proved so fruitful.
Is it not, moreover, a striking fact that the waters of nearly all the natural springs which for centuries have been used in the treatment of gout are thus dowered, and those which are most lowly mineralised seem to possess the greatest degree of radio-activity?[63] It was to their possession in varying measure of this common property that the therapeutic efficacy of waters so widely different in their chemical content was presumably in large part attributable, viz., to their radio-activity.
For alike in simple thermal, sulphurous, alkaline, sulphated alkaline, or muriated waters, the presence of radio-activity has been established. But if, e.g., in the simple thermal, their therapeutic potency is referable to their higher degree of radio-activity and not to their mineral content, in others their relative deficiency in radio-activity is compensated for by their mineral constituents—these present in sufficient quantity to exert a specific action, alterative, aperient, tonic, etc.
In this matter of mineral content we are reminded of the grievous controversy that has long obtained with regard to the use of natural waters, the chief constituents of which are sodium salts. Sir William Roberts, as we know, from his experiments, ascertained that sodium salts promoted the conversion of the quadriate into the biurate, thus augmenting the precipitation of the latter.
This behaviour on the part of the carbonates, bicarbonates, and phosphates of sodium led him to the sweeping generalisation[433] that all sodium salts, including the chloride, were, as far as practicable, to be avoided by gouty subjects. Naturally, in conformity with this view, such patients were warned to flee those spas whose waters contained these peccant salts.
Carried to its logical end, this dictum would have cut the gouty off from, e.g., the carbonate of soda waters of Vichy, the chloride of sodium springs of Homburg, the sulphate of soda waters of Karlsbad, not to mention the muriated (sodium chloride-containing) sulphur waters of Harrogate, Llandrindod, etc., despite the overwhelming clinical evidence as to their efficacy in certain cases of gout.
Fortunately, as Burney Yeo observed, “in spite of all the theoretical denunciations of the use of sodium salts in gout, the gouty, from all quarters of the globe, have resorted, and continue to resort, in steadily increasing numbers, to those Continental springs in which the salts of sodium are overwhelmingly predominant.”
In short, Sir William Roberts’s experiments, while they dissipated the fallacious view of the action of alkalies as solvents in the blood of sodium biurate, have not for one moment imperilled the clinical and practical estimate, deep-rooted in experience, of their general utility in gout.
For myself, I incline to the view of the French authors, who would refer the value of alkalies and alkaline mineral waters in gout rather to their general influence on metabolism than to the now no longer tenable conception of their solvent action on uric acid.
Reflecting on the varied constituents of mineral springs and the claim that each and all of them are of value in gout, one naturally looks for certain conditions common to them all. These are, as Burney Yeo rightly says,—
(1) The quantity of water, more or less pure, taken into the body under regulated conditions daily.
(2) The altered mode of life, the regular exercise in the open air, the modified diet, the early hours, the absence of business cares.
(3) In many foreign spas there is the drier and hotter Continental climate.
(4) The stimulating effect to excretion and “tissue change” which the baths, douches, frictions, and manipulations applied at most of them induce.
Now, admitting, as one freely does, the important influence exerted by these factors on what may be termed the pathological groundwork of gout, still it is equally certain that some cases of gout do better than others at certain spas.
This leads me on to the further reflection that the favourable or unfavourable reaction in different cases depends on the varying nature of what I may term the “excitants” of gout. For the deviations from health that evoke the disorder are manifold and diverse, each carrying with it its own therapeutic indications. Something more is needed than what may be termed a blind or unintelligent “washing out” process. In every gouty patient there is some functional flaw or defect, and cæteris paribus, that natural spring will suit him best whose mineral or other content is best calculated to correct or minimise his particular deficiency.
In short, we must get rid of our too common habit of asserting that this or that particular water is “indicated in all cases of gout,” and its use “attended with the most remarkable results.” The question that we should be more anxious to decide is, whether of all natural springs this or that particular mineral water is par excellence the one that will most surely and most swiftly correct or minimise that particular functional derangement which in the subject under review experience has shown to be the most fertile source of gouty outbreaks. But to this we shall refer later when dealing with the individual peculiarities upon which our selection of a spa will depend.
To sum up, in consonance with these views, the general principles of spa treatment, as I take it, are:—
(1) To correct or relieve those functional derangements, gastro-intestinal or other, that appear to be the determining causes or excitants of outbreaks of regular gout.
(2) To reduce the toxicity of the blood plasma and tissues by promoting the elimination of uric acid and toxins through all avenues of excretion.
(3) To restore the organism as far as possible to a state of health or functional efficiency, and therewith to adopt such prophylactic measures as shall diminish the liability to recurrence of the disorder.
To discuss the application of these principles to all types of mineral waters is beyond the compass of this work, and I shall perforce have to confine myself very largely to discussion of the salient properties of radio-active waters, with subsequently such brief allusions to the salient therapeutic indications of other varieties as may be indispensable to intelligent selection of a spa in any individual case.
As to the physical properties of radium, it is, according to the theory of transformation, a “changing element,” emitting alpha, beta, and gamma rays, and in addition a radio-active emanation.[435] This latter product exists in a gaseous form, and is the outcome of the ceaseless metamorphosis taking place in radium itself, each atom of which continuously ejects at high velocity an atom of helium.
This expulsion of helium having ensued, the parent atom no longer exists as radium, but as radium emanation, or niton, as it has more recently been designated. Now, from a therapeutic point of view, the salient fact is that elicited by Lowenthal, viz., that the active agent is not, as was previously thought, radium itself, but the emanation derived from it.[64]
Now, as a reference to our footnote shows, the Bath waters are radio-active to a remarkable degree, and as Maché, Curie, and Laborde hold that “the higher the emanation from a given spring, the more striking are the physiological results,” a brief reference thereto seems called for.
Physiological Action of Radium Emanation.—When inhaled, radium emanation swiftly passes from the alveolar spaces of the lungs into the blood, and thence to the tissue cells, which, according to their specific solubility, absorb the same. Eventually, if[436] the inhalation is prolonged sufficiently, saturation of the blood therewith ensues, to be followed by its escape viâ the lungs, intestines, kidneys, and skin.
Taken orally, radium emanation, according to Lazarus, in large amount, passes into the arterial blood, an observation confirmed by other investigators experimenting on animals. Its absorption into the blood takes place slowly from the intestines, and its exit thence out of the system is, in like fashion, only slowly effected, taking hours for complete excretion. On the other hand, when inhaled the emanation is quickly absorbed and as swiftly excreted, i.e., within a few seconds. As to its power of penetrating the skin most authorities are sceptical, but Engelmann stoutly contends that he has proved that in immersion baths the emanation does actually pass through the skin; but pending further researches this question of cutaneous absorption must remain sub judice.
Again, radium emanation appears to be endowed with the power of energising or activating the body ferments or enzymes, in other words, can stimulate to greater efficiency the proteolytic, glycolytic, and diastatic ferments that set in motion that long chain of cleavage processes in the various foodstuffs, the necessary prelude to their absorption, assimilation, and ultimate transmutation into live protoplasm. Nay more, for the same mysterious agent, it is claimed, can activate those oxidising enzymes which initiate the equally intricate disruptive processes that mark the disintegration of living protoplasm.
Thus Neuberg, Lowenthal, Edelstein, and others contend that they have demonstrated such an increase of efficiency on the part of the autolytic enzymes responsible for cleavage of the protein molecule into nitrogenous bases and amido-bodies. That radium emanation should exert such a profound effect on organic metabolism, both in its anabolic and katabolic phases, would, if established, go far to dissipate the dark shadow of empiricism that has for so long clouded the practice of mineral water drinking and bathing. For it is precisely in those conditions collectively termed “disorders of nutrition” that radio-active waters have found their traditional rôle.
In 1909 Gudzent, working in His’s clinic at Berlin, affirmed that in gouty subjects uric acid vanishes from the blood in the presence of radium emanation; moreover, that under the same conditions tophi had been observed to melt away. The explanation proffered by Gudzent was, that the emanation inhibited the transmutation[437] of the unstable and more soluble lactam into relatively insoluble and stable lactim urate, this latter being the salt found in the blood of the gouty.
W. His also claims that the gouty individual benefits by this method of treatment, which, he maintains, not only reduces the uric acid content of the blood, but dissipates uratic deposits in the tissues. On the other hand, at the last Congress of Internists at Wiesbaden (1912) Gudzent and His’s views, though stoutly supported by some, were unacceptable to others, who, although they admitted the favourable influence of radium emanation upon the symptoms of gout, yet contended that its effects could with difficulty be interpreted either in the sense of increasing the solubility of the monourate of sodium or its decomposition into CO₂ and ammonia.
Thus E. V. Knaffl-Lenz and Wiechowski, working in the Vienna Pharmacological Institute, were unable to confirm Gudzent and His’s claim that treatment by radium emanations resulted in destruction or increase in solubility of the mono-sodium urate. On the other hand, in view of the admittedly favourable effect of the emanation on gout, they suggest that it might be due to what they term activation of an uric acid oxidase existing in the human tissues. Yet another view is that in some obscure way radium emanation facilitates the elimination of uric acid through the kidneys.
In regard to the claim that radium emanation has the power of keeping uric acid compounds in their more easily soluble forms, it is interesting to recall the conclusion arrived at by the Lancet’s special commission for investigation of the Bath waters: “The thermal waters of Bath exert a distinct solvent action on uric acid; in our experiments, e.g., it was shown that Bath waters dissolved over five times the amount of uric acid that distilled water would similarly take up at blood heat—i.e., just under 100° F. Since the waters are drunk hot and used hot for bathing purposes, this fact may have an important relation to the therapeutics of Bath waters in the treatment of chronic gouty affections and rheumatism.”
Increased Excretion of Uric Acid.—Delayed excretion of exogenous purin is held to be one of the most characteristic signs of gout. Now, following emanation treatment, Lowenthal and others have noted that this disability on the part of the gouty was apparently removed. For when, at the close of the course, the capacity for dealing with exogenous purins was tested by the intake of large amounts of purin bodies, excretion of the same ensued after a normal fashion. It would seem then that there is not only increased uric acid excretion actually during the progress of a[438] séance of emanation, but also that this enhanced power of coping with purins is maintained subsequently.
Subjective Phenomena of Gout in Relation to Blood Content and Excretion of Uric Acid.—Now, as we have seen, it is claimed that uric acid disappears from the blood in the presence of emanation. But, while in the majority of instances amelioration of symptoms follows reduction of the uric acid blood content, in others improvement ensues even though the amount of uric acid in the blood remains unaltered.
Thus in one of His’s patients under radium emanation striking amendment followed notwithstanding that the blood contained uric acid. In another, the subject of multiple tophi, no uric acid was found in the blood throughout the treatment, and yet the victim had repeated attacks of gout during this period.
Turning to the excretion of uric acid in the urine, similar discrepancies emerge. Thus Mandel out of seven gouty patients under treatment by radium emanation found that an increased uric acid excretion ensued in two subjects. Of the remainder, in two no alteration in average excretion took place, in two a slight diminution, and in one a marked increase, to the extent of 50 per cent.
Now in four of the seven cases an undoubted clinical and subjective improvement was observed, although the uric acid curve showed diminution rather than increase. It seems, therefore, clear that the beneficial effect of radio-active waters in gout involves something more than the dissipation of the uric acid in the blood and its increased elimination in the urine.
We have in previous sections emphasised the importance of treating local foci of infection, in view of their possible causal relationship to gout. For, uncertain as we are of the etiology of the disorder, we cannot afford to neglect treatment of any possible source of toxic absorption.
Now a significant number of independent workers contend that in the presence of radium emanation the growth of organisms is retarded, if not actually inhibited. The same bactericidal power has been claimed for radio-active waters even of low grade. Should recent contentions as to the efficacy of the same in states of oral sepsis be confirmed, it will constitute an important weapon wherewith to combat not only the local, but the remote malign, effects of sepsis in the mouth or its accessory cavities.
Again, it is recognised that pharyngeal and nasal affections when present derive benefit from the inhalation of radio-active waters atomised by steam or air. In this connection it may be[439] noted that, by an ingenious apparatus installed at Bath, the natural “niton” gas is now extensively used for inhalation or douching of the mouth and neighbouring cavities.
Alimentary Disorders.—Accepting the fact that gastro-intestinal derangements are the most common excitants of gouty outbreaks, it seems to me highly probable that the good effects of radio-active waters are partly attributable to their mysterious power of activating the body ferments. Thus, through their stimulating action on the digestive enzymes, they may inhibit the formation of abnormal substances, or, through their quickening of the autolytic ferments, may hasten the disruption and excretion of such when formed.
How frequently in these cases do we find that some functional hepatic or gastro-intestinal derangement is the prelude to a gouty outbreak. Again, as pointed out, how often do these subjects suffer with fermentative dyspepsia and “organic acidity,” with associated lowered tolerance for carbohydrates. In such cases, if given in copious quantity and frequently, the radio-active waters prove most beneficial. This is in part attributable to the mechanical flushing of the alimentary canal and tissues, and in part perhaps to their activating influence on the digestive enzymes.
In contrast to the foregoing, such abundant ingestion of the waters is inadvisable in atonic types of dyspepsia marked by dilatation and diminished secretion. But here again, if given in small amounts, radio-active waters undoubtedly exercise a beneficial effect. Also in those gouty subjects who suffer from neurasthenia and nervous dyspepsia a similar favourable reaction is frequently observed. This I apprehend to be due to the fact that radium emanation exerts a sedative effect on the nervous system. Thus it has been noted that guinea-pigs when exposed to radium emanation drop into a state of somnolence and torpor. May not this account for the undoubted fact that highly strung individuals when subjected to a combined bath, drinking, and inhalation cure become less irritable and lose their distressing tendency to insomnia?
Again, intestinal irrigation with these radio-active waters after the Plombières technique is justly esteemed in those cases of gout attributable to intestinal catarrhs and mucous colitis. The constipation these subjects so frequently suffer from is counteracted, and the regular removal of waste and toxic material achieved.
As to the morbid affections associated with gout, notably fibrositis, it is well recognised that muscular and nerve types of this disorder prove very amenable to a course of these waters. Here I would lay stress, too, on the swiftness with which the[440] glycosuria of gouty subjects vanishes under the same conditions. The pruriginous and eczematous eruptions met with are also favourably influenced by a combination of internal and external treatment. I may note, too, that this mode of therapy is not contra-indicated in increased arterial blood pressure. For it has been shown by Deutelmoser, Saubermann, and others that under the influence of radium emanations the blood pressure is reduced.
As regards the administration of radio-active waters, it cannot be doubted that the combined bath, drinking, and inhalation cure is the most advantageous. The subcutaneous injection of radio-active waters does not seem to possess any outstanding advantages, while the danger of sepsis has always to be considered.
As to the relative merits of artificial as opposed to natural radio-active waters, it does not appear to me that the therapeutic action of the former is swifter or more infallible than the products that issue from nature’s laboratory. The limitations and capacities of the latter have been fixed by centuries of experience, and, as far as present researches go, the newly born commercial imitation, at any rate as regards the treatment of gout, has yet to prove itself endowed with a greater range of therapeutic efficacy.
While naturally my attention has been largely centred upon the mineral waters of Bath, I would by no means convey the impression that a thermal radio-active spring is the only one that I think beneficial in the treatment of gout. Far from it, for if, from my description, I appear to have claimed such to be universally applicable to all gouty subjects, the explanation really resides in the fact that the resources of most spas can be readily adapted so as to suit different kinds of cases.
Nevertheless, as I have said, I favour the tendency towards specialisation of spas, as bit by bit the indications for their differential application become more and more sharply defined. In view, then, of this trend, it is manifestly only fair to our patients that we endeavour to select that particular spa that seems most eligible in their particular instance.
Let us assume, then, that the subject is in such circumstances that a certain latitude of choice is permissible. This being so, the physician’s selection will be the more satisfactory if regard is had not only to the gout, but to the individual himself, and not the least important of the considerations involved have been already embodied in my remarks on climato-therapy. For the ideal sought, if I may again say so, is not only physical, but psycho-physical;[441] and the physician who leaves out the mental element will scarcely choose wisely.
Narrowing our field to consideration of the physical requirements of the subject under review, what manner of man is he, metabolically speaking? Is he of spare habit, one in whom katabolic changes hold sway and “the vital fires blaze more fiercely,” or is he obese, one in whom anabolic processes are dominant, with hoarding up of substance?
Now, I have taken these two types, the spare and the obese, as in gout we are dealing primarily with a “disorder of nutrition.” Cæteris paribus, we wish to correct the morbid metabolic trend, in other words provide differential treatment. Obviously the salient indication in the lean individual is that he shall drink of a spring which will tend to enhance digestive capacity and facilitate assimilation of foodstuffs, with as its outcome increase of general nutrition.
To compass such effects, muriated chloride or common salt waters are, other things being equal, most desirable; that is to say, unless they are taken in such quantities as to produce catarrh of the stomach and intestines, they do not cause emaciation. On the contrary, I have, for example at Llandrindod, seen an increase of weight in these persons ensue during, and, moreover, continue after, a suitably arranged course of these waters. Among other muriated waters in this country may be mentioned Llangammarch Wells, which, as Sir Hermann Weber suggested, is suitable in cases of chronic gout, “especially where any emaciation is to be avoided,” and Woodhall Spa also deserves mention in this connection, or, reverting to the Continent, the waters of Homburg, Kissingen, Wiesbaden, Baden-Baden, etc., may be selected.
The muriated (chloride-containing) alkaline waters are also eligible in cases where loss of flesh is to be avoided, such as Ems, Royat, Chatel Guyon, or La Bourboule. They should, for this reason, be given the preference over the simple alkaline waters, such as Vichy, Vals, Neuenahr.
Reverting now to the obese, plethoric type of man, a heavy eater and often of sedentary habit, what is the end to be achieved? Here loss of flesh is to be courted, and a spa sought whose mineral waters will by their action supplement the all-important dietetic and regimenal treatment of the subject.
The class of waters pre-eminently suitable will be those known as the sulphated and the sulphated alkaline varieties, which, taken internally, will through their purgative and diuretic effects assist our purpose. The stronger varieties of the sulphated waters are chiefly used as occasional aperients at home, as, generally speaking, at the site of the spring there is no proper spa accommodation.[442] We allude to Franz Joseph, Hunyadi Janos, Rubinat, and Condal waters, etc.
In England several sulphated springs exist, but, as far as their use is concerned, may be regarded as obsolete. Perhaps the best known is the original spring, no longer used, at Epsom, whence the English term for magnesium sulphate, “Epsom salts.” According to Weber, in Charles II.’s reign these native laxative saline waters were taken at the wells early in the morning, and Pepys in his diary tells how on August 11th, 1667, at seven o’clock on a very cold morning, he found many people drinking the waters at Barnet Wells.
It is, however, the sulphated-alkaline springs that have achieved the greatest reputation in this sphere, notably Karlsbad, Marienbad, Franzensbad, Tarasp Schuls, etc., and perhaps of these Marienbad is the most frequented. But in any case, in exercising a choice, we should take into consideration not only the temperature and mineralisation of the waters and their balneo-therapeutic resources, but also the climate and the time of year. Thus, for example, the climate at Tarasp is alpine, and the altitude of Marienbad is over 2,000 feet, while that of Karlsbad is but 1,200. Another point to consider is whether the obesity of the subject is attended with anæmia. If so we may with advantage choose Tarasp, which, in addition to sulphated alkaline, has chalybeate waters, and the same dual advantages are to be found at Marienbad.
For those unable to go abroad the muriated sulphated waters of Leamington or Cheltenham in this country are available. The flat contour of these spas is very suitable for those cases in which obesity is complicated by cardiac debility. I may note, too, that Bain and Edgecombe, discussing the treatment of obesity at Harrogate, speak well of the strong muriated sulphur water, substituted in anæmic cases by a chalybeate water in conjunction with an aperient.
So much for the broader indications, metabolically speaking, that should guide us in our choice of a spa. And now to consider other special conditions which in the gouty call for consideration, notably digestive disorders.
Dyspepsia and Chronic Gastro-intestinal Disorders.—In these conditions it is especially imperative that we take a broad view, particularly in respect of climate and altitude. Inland spas at moderate or high altitudes are generally preferable. Doubtless the beneficial result is in part due to the influence that change to a mountainous region, with abundant open-air exercise, exerts on the nervous system. But the same has its drawbacks in the “gouty dyspeptics,” for often, as I have observed, they tend at[443] first to overeat. As Weber rightly says: “The feelings of ‘sinking’ and ‘lowness’ in the gouty and dyspeptic are frequently mistaken by the patients themselves as indications for taking food, stimulants, or tonic medicine.” In short, we must in their instance institute immediately at the commencement of their course the requisite dietetic innovations. Again, being in these more bracing localities more disposed to take exercise, the adverse effect on digestion of over-fatigue must be guarded against.
Indeed, in the more aggravated types of so-called gouty dyspepsia there is little doubt that sojourn in a sanatorium may at first be advisable, so that the patient’s digestive disabilities may be thoroughly studied by the help of test meals, while dietetic treatment can be more readily and surely supervised.
Passing to the question of mineral waters, there is no doubt that a previous investigation of the secretory and motor functions of the stomach would supply valuable indications as to the type of “waters” most suitable. Incidentally, too, researches in this line might tend to clear up the obscurity that enshrouds the mode of action of mineral waters in cases of gouty and other forms of dyspepsia. For experimental findings and clinical observations are here somewhat conflicting.
Thus it has generally been supposed that simple alkaline mineral waters promote the secretion of acid gastric juice. But Pawlow, experimenting on dogs, found that alkaline sodium salts tended rather to inhibit than to stimulate gastric and pancreatic secretions. In order, therefore, to reconcile his findings with the well-ascertained benefit that follows their exhibition in gastric disorders, he suggests that they prevent the too prolonged or excessive secretion that is so often a concomitant of catarrhal conditions.
Adolf Bickel, again, has confirmed Pawlow’s conclusion that the simple alkaline group of mineral waters depress rather than stimulate the secretory activities of the gastric mucous membrane[65]; but Sir Hermann Weber, discussing Bickel and Pawlow’s deductions, puts forward, as I think, a more reasonable hypothesis than that advanced by the latter authority.
Thus he suggests that “a possible explanation of the beneficial[444] effects of alkaline salts in many digestive disorders (gouty dyspepsia, irritable hyperacidity, etc.), in tendency to ‘biliousness,’ and in various so-called ‘gouty manifestations’ is that these salts when taken up into the circulation exercise a favourable influence on the metabolic processes generally, thereby improving the general health and thus indirectly, apart from any special local action, helping to remove conditions of dyspepsia, gouty bronchitis, etc.”
From his experiments Bickel came to the conclusion that in conditions of subacidity supervening on chronic gastric catarrh the most suitable are muriated waters, or muriated alkaline waters, or simple gaseous waters.
Gastric Insufficiency, or Atonic Dyspepsia.—Now, as I have before emphasised, this is the functional gastric disorder most commonly met with in the gouty; the hyperacidity is due to excess of organic acids, and this, again, is the outcome of not excess, but deficiency, of HCL. Now in cases of this nature with subacidity of the gastric juice numerous observers—Von Noorden, Dapper, Boas, and others—have reported an increase in the secretion of hydrochloric acid following a course of muriated waters.
My own clinical experience of the muriated waters of Llandrindod abundantly confirms the results obtained by these authorities. The enhanced digestive capacity of the patients is evidenced by relief of epigastric pain and discomfort after meals and the decline of flatulent distension. For, following the increased secretion of hydrochloric acid, their intolerance of carbohydrates, due to subacidity, disappears, and, fermentation no longer taking place, the over-distended walls of the stomach gradually recover tone. It is customary for patients to walk either during or after the consumption of water. But in decidedly atonic conditions of the stomach with dilatation it is better, as Ageron suggests, that such subjects lie down after drinking. Nor must the beneficial effect of muriated waters on the associated constipation be overlooked. The daily thorough evacuation of the intestinal canal minimises or prevents toxic absorption, and at the same time depletes the overloaded portal system.
The sources of blood contamination being removed, the general symptoms of languor, drowsiness, and mental depression give place to a more cheerful tone of mind. At the same time relaxation from business, an outdoor life, and bracing air, with change of scene and society, doubtless contribute to dissipate those feelings of supreme misery which are the bane of the dyspeptic.
As to the foregoing remarks, I have but chosen Llandrindod as a type. Thus some of the Harrogate waters are equally eligible for inclusion in the muriated as in the sulphurous group. Again,[445] to these may be added Builth Wells and Llangammarch Wells, the latter distinguished by its content of chloride of barium, which is said to raise the blood pressure and promote diuresis through its tonic action on the muscular coat of the arteries. Woodhall Spa, too, calls for mention, the presence of iodides and bromides in its muriated waters investing it, according to some, with special alterative properties; lastly, the strong brine waters of Droitwich, which find their special sphere in external application by baths.
As to the Continental springs in this category, the most noteworthy are Homburg, Kissingen, and Kreuznach, the last decidedly radio-active; while of thermal muriated waters Wiesbaden and Baden-Baden are the most representative.
Chronic Gastric Catarrh.—In this condition, not uncommon in the gouty, and which Ewald aptly characterises as “the best fostered and widest spread of this world’s ills,” a deficiency of gastric secretion with impaired motility is constantly present. With this is frequently correlated distension of the small intestine, due to abnormal fermentative and putrefactive changes in the food.
Leaving aside the vexed question as to whether muriated or saline waters can be regarded as direct excitants of gastric secretion, it cannot be doubted that the prolonged and systematic lavage of the stomach, ridding it of viscid mucus and hastening the removal of retained fermenting foodstuffs, must favour restoration of a healthy state of the mucous membrane, and thus indirectly promote its secretory activities. Again, inasmuch as the bulk of saline waters undergoes absorption in the small intestine, the duodenal catarrh usually associated with this condition is also markedly benefited by the removal of toxic accumulations. Indeed, Niemeyer, discussing the therapeutic efficacy of mineral waters in such states, goes so far as to remark that “the results obtained are the most brilliant that have ever been attained in medicine.” To achieve these salutary effects the “waters” must be taken in amounts adequate to produce copious daily evacuation. For, if insufficient to ensure this same, discomfort and distension ensue pending the more tardy removal of the water by the kidneys.
Now, while in these cases the muriated waters above alluded to are suitable, the muriated alkaline are equally eligible. Of these the highest in repute are Royat, Chatel Guyon, and Saint Nectaire, and in Germany Ems, Wildbad, Assmannshausen, and Wildungen.
Here a reservation in regard to Bickel’s researches, viz., it has been found that in some cases of chronic gastric catarrh in robust subjects simple alkaline springs, such as those of Vichy, Vals, and[446] Neuenahr, have, despite his experimental findings, proved actually beneficial. On the other hand, these same waters have this cogent objection, that long courses are apt to cause depression and emaciation, and, moreover, may aggravate the gastric trouble. Worse still, these simple alkaline waters are more likely to produce an attack of acute gout, whereas the muriated alkaline varieties are free from these objections.
Hyperchlorhydria.—Bickel’s experiments led him to this further conclusion, that in organic gastric disorders accompanied by excess of HCL the simple alkaline and sulphated alkaline group are to be preferred to the muriated waters.
Now, inasmuch as some authorities hold hyperchlorhydria as due to a chronic glandular gastritis, it would seem that these should be given a trial. Personally, I have no practical experience that I can draw upon for substantiation or refutation as to the correctness of Bickel’s assumption. Nor have I on this question been able to find any reference in the literature or clinical findings emanating from these spas.
Much controversy, again, obtains in regard of the usage of muriated waters in these cases. Formerly their employment was unreservedly condemned, but more extended experience has modified this too dogmatic attitude. Albeit, that the results obtained in hyperacidity (excess of HCL) are uncertain is undeniable, and unfortunately it is impossible to foretell whether or no any given case will derive benefit. The pronounced nerve element in these cases, with probably other unknown factors, has doubtless much to say to the conflicting clinical results.
But the experience of most of us will accord with that of Dapper and Von Noorden, that muriated waters, such as those of Homburg, Kissingen, etc., often prove beneficial in cases of neurasthenia with hyperacidity. On the other hand, it is equally true that some examples of apparently the same nature derive no benefit, indeed are aggravated. But, according to Von Noorden, such are in the minority.
Fortunately this secretion of an abnormally acid gastric juice is relatively rare in the gouty. Being of the nature of a secretory neurosis, it occurs most frequently in those of neurotic or neurasthenic type. Now, holding the view that many cases of neurasthenia are due primarily to toxic absorption, secondarily to alimentary derangements, the beneficial effects observed are, I presume, probably attributable in large part to the removal of toxic accumulations through flushing. These deleterious substances not being absorbed in such amounts as before, improvement in the general nerve tone ensues, in which doubtless the secretory mechanisms of the digestive system participate.
But, as we have seen, these same muriated waters prove most salutary in precisely the opposite condition—hypochlorhydria, or deficiency of HCL. That such a beneficial effect should ensue in diametrically opposed states, viz., hyper- and hypo-acidity, gives point, I think, to the contention that the action of muriated waters on the digestive organs must in great part be exerted not locally, but indirectly, that is, secondarily to improvement of the general health and toning up of the nervous system.
Indeed, the pronounced nerve element in these cases is probably the explanation why, especially in instances palpably due to mental fatigue, insomnia, etc., a course of baths or hydrotherapy at some simple thermal spa, preferably those at certain altitudes, such as Buxton, Wielbad, Gastein, Plombière, Ragatz, etc., often suffices without any internal treatment.
Functional Hepatic Disorders.—Fothergill held that some persons were born with “congenitally incompetent livers,” an unwelcome legacy unduly incident among those of gouty heritage. Now the intimate interdependence of hepatic and gastro-intestinal disorders has long been recognised; indeed, the swiftness with which retribution, in the shape of so-called “biliousness,” overtakes those who fare not wisely, but too well, is proverbial even among the laity.
Thus chronic hyperæmia of the liver, due to stasis in the portal area, commonly ensues in those gouty subjects who eat and drink too much, especially alcohol. The same Nemesis awaits those who lead too sedentary a life, and in the train of chronic constipation develop such hepatic congestion, with in some instances attacks of catarrhal jaundice.
As to treatment of these cases by mineral waters, a preference must be given to alkaline, sulphated alkaline, or muriated waters, according to the special indications of individual cases. Thus suppose the subject is stout and plethoric, and given perhaps to hæmorrhoids or pruritis ani, then spas with sulphated alkaline waters (Marienbad, Karlsbad, etc.) may be recommended. But equally good results will follow a course at home of muriated waters, or muriated sulphur waters, such as Harrogate, Llanwyrtid, and Strathpeffer, etc.
Bearing in mind that functional hepatic disorders are in large part secondary to gastro-intestinal derangements, it is probable that the beneficial effect of the above types of waters on the liver is exerted indirectly, though we must recollect that the salts of soda have a direct stimulant action on the hepatic function.[66]
Given in adequate doses, they act as mild, unirritating laxatives, the daily evacuations thus produced relieving hepatic congestion and coincidently any tendency to portal engorgement. Through their dual action of flushing the digestive canal and stimulating hepatic and gastro-intestinal secretory activities, we find the explanation of the decided benefit that follows their use in gastric catarrhs, especially of alcoholic origin, also in catarrhal jaundice, incipient cirrhosis of the liver, and so-called abdominal venosity.
As we know, Sir Lauder Brunton long since pointed out that the ingestion of saline mineral waters tends to counteract any tendency to catarrh of the biliary passages, the biliary secretion tending to become less viscid; consequently the passage of gall-sand is promoted. Some, like Hans Kehr, of Holberstadt, advise a course of saline waters after operations for the removal of gall-stones; others advocate their employment before surgical intervention. It is obvious, however, that their range of usefulness in this affection must be limited and is largely to be attributed to their power of mitigating inflammatory or catarrhal changes in the gall bladder and its related ducts.
Intestinal Derangements.—Constipation is, as is well known, the bête noire of the gouty, and, while the basal indications of its therapy have to be carefully ascertained in every individual, still much may be done by a properly chosen and adequately supervised course of spa treatment. This, of course, entails revision of the diet and habits, notably in regard to exercise; in some of sedentary habit a mere change of air to a more bracing climate, with its associated increase of exercise, may suffice; in others of stout plethoric type a visit to one of the sulphated alkaline spas will be of benefit; while in weaker subjects of the lean kind muriated waters will be more suitable.
In many the habitual constipation is due to a catarrhal condition of the intestine. Trautner, as we know, considers that gout originates in a mucous colitis. In France the gaseous muriated waters of Chatel Guyon are in great vogue for chronic catarrhal conditions of the intestines, especially those associated with abdominal plethora and constipation. Indeed, because of its success in these cases, it is sometimes called the French Kissingen.
On the other hand, the Plombières Spa is the one that par excellence devotes itself to the treatment of mucous colitis by a combination of (1) intestinal douches, (2) sedative warm baths, and (3) “under-water” douches directed against the abdomen.[449] Treatment by the Plombières method is now available at most English spas, and, while I can speak highly of its benefits, I think perhaps there is sometimes a tendency to resort to it after a routine fashion irrespective of the presence of any special indications for its usage. The after-results in some cases are not enviable, and recently a distinguished surgeon informed me that he had met with instances in which ill-advised and prolonged usage of such irrigation resulted in an atonic condition of the colon.
Glycosuria.—The more chronic and benign forms met with in gout frequently derive benefit from a course of mineral waters, though, of course, revision of the diet and regimen in general are essential concomitants thereof. Indeed, the high reputation achieved by certain Continental spas—Karlsbad, Vichy, Neuenahr, etc.—in this disorder is in large part due to the care and attention bestowed on these the basal indications.
In the gouty obese, with a tendency to piles and abdominal plethora, the sulphated alkaline and simple alkaline waters, such as Karlsbad, Vichy, Neuenahr, Brides-les-Bains, etc., are suitable, and in this country the muriated sulphurous waters of Harrogate and Llandrindod.
In some of the gouty obese their bouts of glycosuria sometimes alternate with attacks of uric acid gravel, and not infrequently there is also present a slight degree of albuminuria. In these cases the earthy or calcareous waters enjoy a considerable reputation, notably Contrexéville, and not a few with uric acid gravel and slight albuminuria resort to Wildungen.
I have before alluded to the beneficial effects in glycosuria of Bath waters, which, like Contrexéville and Wildungen, have an earthy or calcareous content. For the less robust and lean type of glycosuric Sir Hermann Weber recommends “simple thermal baths, such as can be obtained at many resorts of moderate elevation (Gastein, Wildbad, Buxton, Schlangenbad, and Ragatz).” As an alternative, he states that “the internal use of muriated alkaline or simple alkaline waters (Vichy, Neuenahr, Obersalzbrunn, Royat, La Bourboule), in association with thermal baths or alone, may often be recommended.”
Oxaluria.—This condition, like glycosuria, is often met with in the gouty. It is of course often due to faulty diet, but in many instances there is a strong nerve element in the case. In the former instance dietetic restrictions are the basal indication. In these cases, if there be constipation, a visit to the muriated springs in this country or to Kissingen, Homburg, etc., is advisable.[450] Otherwise, alkaline springs, i.e., Vichy, or alkaline earthy springs, such as Vittel, Contrexéville, or Martigny-les-Bains, may be given the preference. For those instances in which the nerve element is predominant the character of the mineral waters is quite subsidiary compared with the all-important point of procuring the subject freedom from worry.
Gouty Phlebitis.—It is believed that gaseous muriated waters, both internally and in the form of baths, are useful in counteracting any tendency to phlebitis. Obviously, if there be any symptom or sign of existing phlebitis, any such procedure would be fraught with risk. Still patients who have had phlebitis frequently resort to such spas, notably Bagnoles-de-l’Orme, where the resident physicians have made a special study of the constitutional tendencies to chronic phlebitis. The waters are but weakly mineralised, and may be classed in the simple thermal group (81°-84° F.).
Respiratory Disorders.—While, as I have said, I deprecate any notion of specific gouty types of bronchitis, asthma, etc., there is no doubt that gouty subjects, like many others, are prone to bronchial affections, and for such mineral water treatment at a favourable season of the year, is equally beneficial. In gouty bronchitics of plethoric type, courses of sulphated alkaline waters will often do much to relieve the symptoms. Again, many sulphur, muriated alkaline, and muriated spas, have achieved a great reputation in the same sphere, e.g., Ems, Royat, Eaux-Bonnes, Baden-Baden, and Soden. Nor need we go outside our own country, for many of our mountain health resorts are in the summer months equally eligible for treatment of these disorders of the respiratory system.
Fibrositis.—Adequately to describe all the methods, internal and external, in vogue at spas for the treatment of, e.g., chronic lumbago and sciatica, would be quite futile in the space at my command. I have the less compunction in being unusually brief inasmuch as Bassett Jones and I have dealt exhaustively with the subject in our work on fibrositis.
The groundwork of successful treatment will rest on the application of the general principles in force for the treatment of the underlying gout. They will, of course, include internal and external treatment by simple thermal waters, the thermal muriated and thermal sulphurous waters, etc. Frequently, too, cold muriated and other waters artificially heated are invoked for this dual purpose.
The benefits of external treatment by douches of varying character will depend on the measure of discrimination exercised in adapting their application to suit the individual necessities of[451] the case. But I would here lodge a plea against the far too great frequency with which such cases are sent to spas during the acute phases, whereas it is only the subacute or chronic forms that are eligible for treatment by hydrotherapy.
Gouty Eczema.—The climatic suitability of the spa is of primary importance, and while, as a rule, cold, damp and windy localities are to be avoided, still personal idiosyncrasy plays a large part in the decision, some cases of eczema being aggravated by cold, others by heat and sunlight.
The spa treatment of gouty eczema has for its aim the correction of the constitutional taint by the internal exhibition of mineral waters in conjunction with baths. To this end, the eliminative effects of courses of alkaline (Vichy, Vals), muriated (Llandrindod), sulphurous (Harrogate, Strathpeffer, Llanwyrtid), or muriated sulphurous waters (Uriage, Aix-la-Chapelle, etc.), are often invoked with marked benefit.
Again, the thermal muriated alkaline waters of Royat and the arsenical springs of La Bourboule have acquired a great reputation in gouty eczema, and in obstinate but non-pruriginous types the prolonged tepid baths in vogue at Loèche-les-Bains, in Switzerland.
In many instances of senile or atrophic type a course during the summer of simple thermal baths is often beneficial. Buxton is suitable, also Wildbad, Schlangenbad, Ragatz, etc. Lastly, in eczema of seborrhœic type thermal sulphurous waters, e.g., Schinznach, Aix-les-Bains, Bagnères-de-Luchon, etc., are highly commended.
Uric Acid Gravel.—Though, as before stated, there is no specific connection between this disorder and gout, still the gouty no more than others are immune therefrom. For the stout, plethoric, and constipated, sulphated and sulphated alkaline springs are indicated. But if, on the other hand, there is a tendency to diarrhœa, these aperient waters must be renounced in favour of simple alkaline springs. In those of less robust type the simple thermal or earthy waters, notably Contrexéville and Wildungen, are to be preferred, and failing these, the muriated waters.
Arterio-sclerosis.—It is hardly necessary to say that in all but the slightest forms high altitudes are contra-indicated. In these less advanced cases, if the subject be stout and plethoric, the sulphated alkaline waters (Karlsbad, Marienbad, etc.) are useful; while in thin persons the muriated waters are more suitable.
In more advanced cases we may during summer advocate a course of treatment at some simple thermal spa, such as Buxton, and many of these cases do well at Bath during the spring, or they may be sent to Bourbon Lancy, which has been termed the[452] French rival to Nauheim, because of the excellent results obtained in cases of raised blood pressure.
Chronic Nephritis.—Clearly in these cases a quiet life, without mental worry, gentle and not excessive exercise, with residence in an equable climate, are the primary indications. In the early stage, when the patient’s condition is good, the tension not high, and the quantity of albumen small, the subjects derive much benefit from an annual visit to certain mineral springs. Not that mineral waters have any curative influence; they merely help the interstitial circulation and promote flushing.
Of mineral waters the simple thermal or the weak alkaline are generally considered the most eligible, e.g., Vichy, which is useful also in cases of combined albuminuria and glycosuria. In cases with cardiac dilatation care should be taken not to prescribe mineral waters in excessive amount. If complicated by anæmia, chalybeate waters, according to Weber, are “not rarely useful.”
Bain and Edgecombe, discussing gouty albuminuria, state that the magnesia water of Harrogate, in combination with the old sulphur, has a marked effect in reducing the absolute amount of albumen in the urine, e.g., from one-fourth by volume to a mere trace. They add, that if the specific gravity of the urine be low chalybeate water is indicated with, if necessary, a morning aperient draught. If glycosuria and albuminuria co-exist, the “sulphur waters may be tried tentatively” as the specific gravity does not help us in these cases. “When in doubt, it is safer to give an iron water and trust to diet and baths for a diminution in the excretion of these substances.” Not a few of these cases find their way to Bath and Buxton, often for relief of their increased arterial tension, and the experience of most is that in the more robust types a course of Aix massage is advantageous, while for others more advanced in years baths after the Bourbon Lancy method.
It is well that the potency and complexity of spa treatment be realised, involving as it does not only drinking or internal treatment, but also balneotherapy, electro-therapy, and all the other accessory therapeutic methods now at command. With all these powerful weapons to hand, it is obvious that their use demands a corresponding degree of discrimination, this even in cases otherwise suitable, and here a word as to the types of gout most suitable for the internal exhibition of mineral waters.
In this matter the rules laid down for hydrotherapy, or the external use of waters, are in the main applicable. In other words, acute cases of gout are always ineligible, as likewise those[453] instances in which an attack appears imminent or those in which recovery from an acute paroxysm is barely accomplished. On the other hand, mineral waters are indicated in chronic gout and in the inter-paroxysmal periods that mark the early stages of the disorder. Indeed, I know of no other treatment that is as effectual, and, with Sir William Roberts, “I do not think, therefore, that gouty patients, if they can afford the time and expense, should forego the advantages of the time-honoured practice of a visit to a mineral spring.”
But, to attain the best results of spa treatment, not only should the cases be suitable, but they should be despatched at the right season. Even in spas that are open all the year round we should try to select the most congenial month. Thus, if the subject is intolerant of heat, we should not advise him, say, to go to Bath in July or August, or, for that matter, during the hottest summer months to Aix-les-Bains, Baden-Baden, Wiesbaden, Neuenahr, etc. If he has to take his course at this period of the year, and a thermal spring is indicated, Buxton will be more suitable than Bath, and we have a large choice of other spas in more bracing localities, such as Harrogate, Llandrindod, Strathpeffer. In short, some discrimination must be exercised. Again, if a course be indicated in the winter, we should favour those spas where the hotels are in proximity to the springs, so as to obviate unnecessary exposure, e.g., Bath, Wiesbaden, Helouan, etc.
As to duration of a course, there is, I think, in many spas a too great tendency to be dominated by tradition. Not only is the duration of the cure arbitrarily fixed, but, still worse, the drinking of the waters, the bathing, and even the dietaries are frequently in danger of becoming stereotyped, with, as a consequence, a lack of that eclecticism necessary in the best interests of individual cases. A certain amount of routine is unavoidable, and has this advantage, that persons find it easier to submit to irksome restrictions when they see others conforming thereto. But even so there is ample scope for such modifications as may be required, and upon their adoption the success of spa treatment mainly depends.
If arbitrary rules in respect of drinking, bathing, etc., are to be deprecated, the same applies with unvarying fixity to the duration of a cure for all cases. Generally speaking, three to four weeks is the average stay at spas. But obviously it should be varied to suit the patient’s condition, and in many instances of chronic gout it may with advantage be extended to six or eight weeks.
Again, I think perhaps in this country the advantages of an after-cure are insufficiently realised. In this respect our Continental[454] brethren set us an example, attaching the greatest importance as they do to an after-cure, especially after a course of laxative waters, e.g., Karlsbad, Marienbad, and Kissingen. Certainly to plunge forthwith into work immediately after a cure leads but too often to another breakdown and the undoing of any advantages that may have been reaped. Of late I have noted, especially in business men, a tendency to interrupt even their course by travelling considerable distances on non-bathing days to attend to their affairs. The folly of this is obvious, and the results are almost invariably unsatisfactory. Indeed, in these all too strenuous days one almost despairs of after-cures, for it is difficult enough oftentimes to prevail on people to stay even for their course of three weeks, and frequently one is asked to conduct their treatment after a more intensive fashion, and so abridge it to a fortnight or even a week!
As to the nature and site of the resorts suitable for an after-cure it is impossible to lay down general rules, as individual peculiarities have to be considered. But the physician who prescribes such ought, as Sir Hermann Weber remarks, “to be acquainted with the nature of the locality recommended, if possible by personal visits, and the reports of thoroughly judicious people.” For, as he rightly says, there are numerous places in the British Isles perfectly suitable for an after-cure, to mention but a few in England, Ilkley, Ben Rhydding, Malvern, Haslemere, Church Stretton, Crowborough; in Scotland, Braemar, Ballater, etc.; and in Wales, Llanberis, Llangollen, etc.
But brief reflection on the foregoing considerations suffices to make it clear that the various spas and health resorts with which this country, through Nature’s beneficence, has been so bountifully endowed, are but members one of another, in short complementary, not antagonistic, as I fear is sometimes thought. This latter is a view to be discarded in favour of a more rational conception of these various centres from their collective aspect as integral parts of a therapeutic whole.
Now what, in a word, is the outstanding feature of our national life to-day? Co-operation—a veritable furore of national and international effort such as the world has never seen. Spas, too, must fall in line with the national trend, must organise and co-operate, if they would play their full rôle in the drama of reconstruction. Now, from the point of view of the State, the true objective in therapeutics is the achievement and maintenance of national efficiency—the production of healthy citizens, sound[455] economic units. This then is the high purpose with which those responsible for spas must ever be animated—an aim only to be attained by their whole-hearted co-operation one with the other.
The lay custodians, too, of spas must increasingly realise that they do but hold in trust their healing springs to be safeguarded in the interests of the community. Mineral waters, like coal, issue from the bowels of the earth. Both are natural products; both are national assets. I doubt not that the growing movement for effectual popular control so rapidly obtaining a grip over the political and economic life of the nation will shortly be extended to our spas, with, as its outcome, their unification and co-ordination under the controlling influence of a central body of experts vested with plenary powers to inspect, control, and inspire the development of these hydrotherapeutic centres. “Salus populi suprema est lex.”
[1] Ewart, discussing the antiquity of gout, observes that it is “certainly as ancient as civilisation,” and as far as we can identify them in the accounts handed down from remote ages, the etiology, the leading symptoms, the outward characters of the articular gout of the ancients were practically the same as belong to gout in our own times! But of its relative prevalence in antiquity we have no means of judging. Continuing, he holds that “the ultimate lesions of gouty arthritis and its pathology are presumably as immutable as those of osteoarthritis.” This may be so, but such objective evidence as we possess certainly points to the greater antiquity of osteoarthritis as the following quotation from our work, “Arthritis Deformans,” testifies:—
“During the course of some excavations undertaken by the Survey Department of the Egyptian Government in that tract of Nubia lying immediately south of the First Cataract, over 6,000 bodies were brought to light, comprising among them representatives of all periods from early pre-dynastic times down to the fifth century after Christ. As the result of their examination of this vast accumulation of human débris, Professor Elliot Smith, in the Nubian Survey Bulletin, states that “The disease which shows itself with by far the greatest frequency in the bodies of all periods is rheumatoid arthritis” (Osteoarthritis).
[2] 920 (S. Eng. Leg.), “There cam a goute In is knee, of Anguische gret.... So longue, that is kneo to-swal.”
1310 (In Wright Lyric), “A goute me hath ygreythed so, Ant other eveles monye mo.”
1377 (Langl., P. Pl.), “He ... gyued me in goutes, I may noughte go at large.”
1400 (Lanfranc’s Cirurg.), “A man that hath arteticam, that is as myche to seie as a goute.”
1450 (M.E. Med. Bk., Heinrich), “Here wyth anoynte the goutes.”
1566 (J. Alday, tr. Baoystuau’s Theat. World), “Their legges full of gouts.”
1579 (Langham, Gard. Health, 1633), “For all goutes, seethe Leekes and Otemeale with sheepes tallow, and apply them hot.”
1590 (Spenser, F. Q.), “And eke in foote and hand A grievous gout tormented him full sore.”
1697 (Dryden, Virg. Georg.), “From Winter keep Well fodder’d in the Stalls, they tender Sheep.... That free from Gouts thou mayst preserve thy Care.”
1704 (Fuller, Med. Gymn.), “There have been some Gouts ... which nothing could remove but a very low Diet.”
1732 (Pope, Ess. Man.), “So, when small humours gather to a gout The Doctor fancies he has driv’n ’em out.”
1822 (Ld. Eldon, in Twiss Life), “I found the King in bed yesterday. He has had a pretty severe gout.”—New English Dictionary, Oxford, 1901. (Ed. Sir James Murrary.)
[3] Pitt, in one of his last letters to the Marquess Wellesley, deplores his slow recovery from severe attacks of gout with which, by the bye, the statesman Fox was likewise affected.
[4] Both Norman Moore and Bowlby subsequently upheld Ord’s view that uratic deposits only occur in tissues already degenerated. “Ebstein’s view has been modified by Von Noorden, who holds that a special ferment leads to the tissue change, to which the deposit of the urate is secondary.”
[5] Physiognomy of the Goutily Disposed.—Taking the principles as laid down by Laycock, the peculiarities of those thus affected fall under the head of the sanguine arthritic diathesis. (That careful observer did not fail to note the modifying influences of gout upon struma and other cachexia.) Thus may be compared the physiognomy of the diathesis and its associated cachexia (developed in time):—
Blood-vessels numerous; heart large and powerful; blood-corpuscles numerous; skin over malar bones highly vascular (florid complexion); skin fair, firm, oleaginous, perspirable; eyes blue; hair thick, not falling easily; teeth massive, well-enamelled, regular, even, undecayed in advanced life; malar bones flattened; head symmetrical; nasal bones well-formed, nose aquiline or of mixed form; lower jaw massive; lips symmetrical.
Form.—Figure for the most part tall; thorax broad at the summit; ribs well-curved; abdomen full; muscles firm, large; limbs large, robust; gait erect, well-poised. Nutrition active; digestion vigorous; appetite great for animal food and alcoholic stimuli. Respiration deliberate, deep; circulation vigorous; animal heat abundant; locomotion active; aptitude for exercise and outdoor amusements. Reproductive powers active; innervation abundant, the mental powers vigorous and enduring.
Physiognomy of the Sanguine Gouty Cachexia.—Blood-vessels largely developed over the malar bones and varicose; skin oily, yellow from subcutaneous deposit of fat; hair thick and white; teeth numerous, discoloured, crusted with tartar; lips bluish, nose reddish, hypertrophied; arcus senilis; abdomen pendulous; limbs thick; joints nodose; nodosities on the ends of the fingers, lobes of ears, fascia of muscles, and tendons; respiration hurried, wheezing; pulse intermittent, irregular; stomach flatulent; digestion acid; urine loaded with lithates; temper irritable; mind sometimes enfeebled.
The local diseases of the arthritic cachexia are principally seen in adult males past the age of forty-five. They consist especially in chronic inflammation of the muscular and articular tissues; in calcification of the basilar and coronary arteries, and of the cardiac valves. These changes give rise to hæmorrhagic apoplexy, angina pectoris, cardiac hypertrophy and dilation; and to secondary pulmonary affections, as emphysema, pulmonary apoplexy, and asthma. Irritation of the mucous surfaces may give rise to nephritis, pharyngeal and laryngeal coughs, and diarrhœa.—Med. Observation and Research, 2nd edition, pp. 96-98.
[6] According to Fischer the protein molecule can be split up into amino-acids, di-amino-acids, aromatic-amino-acids, nitrogenous derivatives of the benzene ring, pyrimidine bases, pyrrolidine derivatives, cystin, and ammonia. During proteolysis the amino-acids exist in groups, e.g., glycine and leucine (glycyl-leucine), two leucine radicles (alanyl-leucine), etc.—which combinations Fischer termed polypeptides, and some of which he has been able to produce synthetically. Furthermore, Fischer proved that nitrogen equilibrium can be maintained in animals by feeding them upon these polypeptide products of proteolytic digestion which no longer gives the biuret reaction. The derivation of amino-acids, etc., from peptone is the outcome of the action of a special intestinal ferment—erepsin. This enzyme is found not only in the alimentary tract, but in all tissues of the body, its action being especially developed in the renal tissues.
[7] Glycocoll in solution dissociates more H-ions than OH-ions. In the presence of alkalies this acid character is more marked, so that it tends to throw the uric acid salts out of solution. The inhibitory influence of the urea upon the precipitation of uric acid from solutions is due to its basic nature.
[8] Recent researches by S. R. Benedict show that uric acid, in the blood of most mammals, exists in combination, but not in that of the bird. Fresh ox-blood (Folin method) contains only 0·30005 gram, free uric acid per 100 grams of blood. But after boiling the protein-free blood filtrate with hydrochloric acid the uric acid content was about ten times as high. Moreover, this same augmented uric acid content was found to exist “in whole blood that had been allowed to stand for some time, indicating that the uric acid compound can be split by means of an enzyme.” The compound exists, not in the plasma, but in the corpuscles. MacLeod, to whose work on bio-chemistry we are indebted, remarks that “It is of some significance that after thus setting free the uric acid, there should be about 50 per cent. more of it present in the blood of the ox than in that of the bird, where most exists in a free state in the serum, although the urine of the ox contains only the smallest trace of uric acid, and that of the blood is loaded with it. Investigation of the condition of uric acid in human blood is at present in progress.”
[9] According to Sir William Roberts, there are three compounds of uric acid (H₂U)—the neutral urate, M₂U, in which the metal replaces all the displaceable hydrogen, the biurate, MHU, in which half the displaceable hydrogen is replaced by the metal, and the quadriurate H₂UMHU, in which one-fourth of the displaceable hydrogen of two molecules is replaced by the metal.
Hutchison and Tidy suggest “that if Roberts’ salt be considered as NaHU. MH₂U instead of Na. HU, his hypothesis remains unaltered, whilst much of the criticism urged against it is nullified. The possibility of such a substance is shown by the existence of the compound LiHU₄HU. Roberts’ theory, or such a modification, is not inconsistent with Von Noorden’s views if these intermediate salts be regarded as within the tabernacle of organic combinations from which the kidneys can split off and excrete the uric acid.”
[10] “If further investigations yield facts which sustain such an idea, it may be more easy to comprehend the types of the demands which are made upon the renal functions.... One of the next stages of research will be the determination of the behaviour of renal tissue to the various purin isomers. This may lead on to the identification of the types of nuclein derivations and their precise cellular origin. Perhaps this in turn may reveal whether there are any differences between the nucleotides of normal and gouty tissues. To this end progress in the technics of the cultivation of tissues in vitro may furnish a means for the elucidation of some of these questions.”—Walker Hall.
[11] As a further illustration of the differences which may exist in the purin metabolism in different kinds of animals, in man and the anthropoid apes the quantity of purin bases in the urine is small in proportion to the quantity of uric acid. In the pig, which is included among the animals that form allantoin from uric acid, the purin bases exceed the uric acid in amount, whereas in the dog, which likewise excretes allantoin, the purin bases exist in very small amount compared with the uric acid.—Stewart’s “Manual of Physiology.”
[12] The findings of Soetbeer and Ibrahim also indicate that 50 per cent. of the exogenous purin bodies undergo oxidation to uric acid, and 50 per cent. undergo further disruption and are excreted as urea or intermediate bodies.
[13] The subject of the experiments—a healthy male (M. S. D.), 22 years of age and 58 kilos in weight—was placed for over six months upon a meat-free low protein diet, free also from purin-containing beverages. This with the exception of a few meals in the holidays, during which a small amount of meat was taken. “No attempt was made to secure a quantitative uniformity of the diet.” On the evening preceding the day of an experiment a light supper was eaten, and no further food was ingested until the completion of the day’s experiment, save the substance whose influence on uric acid excretion was to be studied. The urine was collected hourly, 200 c.c. of water being ingested hourly throughout the experimental period.—“Uric Add Metabolism,” 11—H. B. Lewis, M. S. Dunn, and E. A. Doisy, “Journal of Biological Chemistry,” 1918.
Two other men also served as subjects. Many of the experiments were duplicated, and similar results obtained with these other subjects, but inasmuch as the experiments with M. S. D. were more comprehensive and extended over a longer period of time, the data of these experiments alone are presented.
[14] Quoting from the same article, Journal of Biological Chemistry, 1918, by Lewis, Dunn and Doisy, these authorities observe that—re glycocoll and alanine, Lusk concluded that “the chemical stimulation of protoplasm which is responsible for the phenomena of increased heat production (specific dynamic action) results from the action of their intermediary products, glycocollic and lactic acids, rather than from the amino-acids themselves. The phenomena of the stimulation of uric acid metabolism by amino-acids run parallel to those of the specific dynamic action of the amino-acids (except in the case of the dicarboxylic amino-acids), and it is possible that the same chemical factors are responsible for both.”
[16] Experimenting on a Dalmatian coach-hound, Gideon Wells was able to confirm Benedict’s observation that it excretes large quantities of uric acid. But inasmuch as the liver of this same dog was able to destroy uric acid in vitro, the inference is that the presence of uric acid in the urine of the Dalmatian is not attributable to the absence of uricase in its tissues. “The kidney did not exhibit uricolytic activity. Neither the liver nor spleen converted xanthine into uric acid, but the liver deaminised both guanine and adenine.”—Journal of Biological Chemistry, 1918.
[17] Wells, in his “Chemical Pathology,” observes that the amount of uric acid that appears in the urine depends upon a variety of factors which may be summarised as follows:—
(1) The amount of purin bodies taken in the food upon which chiefly depends the amount of exogenous uric acid.
(2) The amount of destruction of tissue nucleo-proteins.
(3) The amount of purin bases formed in the muscle tissue.
(4) The amount of conversion of purin bases into the uric acid.
(5) The amount of destruction of uric acid, if any, occurring in the body.
(6) Possibly upon the capacity of the tissues to synthesize uric acid; and in case such power to synthesize uric acid exists upon the presence of the precursors of uric acid in the body.
(7) The retention of uric acid in the blood and tissues.
(8) The power of the kidney to excrete uric acid.
(9) The solubility of uric acid in urine—dependent upon the amount of neutral phosphates present, the temperature, reaction and concentration thereof.
Effect of Atophan on Exogenous Purins. (McLester, in “Archives of Internal Medicine.”)
| Date. | R. E. | Blood Mg. U in 100 Gm. |
Twenty-four Hour Urine. | |||
|---|---|---|---|---|---|---|
| Amt. c.c. | U. Gm. | NH. Gm. N. | N. Gm. | |||
| 5/28 | —— | 2·9 | 1,150 | ·46 | ·58 | 10·26 |
| 5/29 | 7 a.m.: 500 grams thymus. 2 p.m.: Blood | 3·2 | 900 | ·66 | ·69 | 10·96 |
| 5/31 | 7 a.m.: 500 grams thymus. 9 a.m.: Atophan, 2 p.m.: Blood | 1·1 | 1,280 | ·75 | ·76 | 11·16 |
[19] Walker Hall states that: “Taking the total volume of blood at three and a half litres, and the volume passing through the lungs as four and a half litres per minute, and through the kidneys as one litre per minute, and the solubility of lactim-urate as 0·1 grm. per 4,000 c.c. of blood, it would seem that the average daily output of 0·5 grm. could be suspended in the quantity of blood passing through the lungs in five minutes or through the kidneys in twenty minutes normal.”
[20] Criticising the colorimetric method on the ground that “different workers obtain on the same blood samples results which vary considerably,” L. J. Curtman and A. Lehrman have devised a new volumetric method for the determination of uric acid in blood. The following is the summary of their researches:—
(1) An experimental study of a number of metallic salts as precipitants for uric acid in a solution alkaline with sodium carbonate was made. The results showed that nickel is the best of those tried.
(2) A 0·0004 N iodine solution was found suitable for the estimation of small amounts of uric acid provided certain conditions are adhered to.
(3) Based upon the above considerations, a new method has been developed for the determination of uric acid in blood, the chief features of which are (a) the precipitation of the uric acid by means of nickel acetate in a solution alkaline with sodium carbonate. (b) The estimation of the uric acid in the precipitate by means of a dilute solution of iodine.
(4) The method was applied with good results to aqueous solutions of uric acid as well as to blood serum to which known amounts of uric acid were added.
(5) Low and inconsistent results were obtained when the method was applied to sheep’s blood to which known amounts of uric acid were added. This was shown to be due to the inadequacy of the procedure generally employed, for the coagulation and preliminary treatment of the blood. The colorimetric method when used in the analysis of samples of the same blood also gave low and inconsistent results for the same reason.
(6) Comparison tests show that the volumetric method is fully as accurate as the colorimetric method, and possesses the advantage of requiring no special apparatus.
Uric Acid Estimation in Normal Individuals
(McLester, “Archives of Internal Medicine.”)
Milligrams Uric Acid in 100 grams Blood.
| J. C. | 0·5 |
| H. D. | 0·6 |
| M. D. | 0·6 |
| A. B. | 0·8 |
| R. C. | 0·9 |
| H. D. | 0·9 |
| J. G. | 0·0 |
| S. M. | 1·1 |
| R. D. | 1·3 |
| L. S. | 1·4 |
| L. H. | 1·7 |
| R. O. | 2·1 |
| H. H. | 2·5 |
| J. M. | 2·5 |
| R. E. | 2·9 |
Uric Acid of Blood in Disease. (McLester, “Archives of Internal Medicine.”)
Milligrams in 100 grams Blood.
| Mitral lesion | 0·5 |
| Rheumatic fever | 0·6 |
| Acute syphilis | 0·8 |
| Chronic tuberculous pleurisy | 0·8 |
| Pneumonia | 1·2 |
| Pneumonia | 1·3 |
| Sciatica | 1·3 |
| Typhoid fever | 1·4 |
| Ulcer of stomach | 1·5 |
| Pneumonia | 1·6 |
| Amœbic dysentery | 1·6 |
| Neurasthenia (?) | 1·7 |
| Acute tuberculous pleurisy | 1·7 |
| Chronic interstitial nephritis | 1·8 |
| Malaria | 1·8 |
| Pneumonia | 1·9 |
| Uremia | 2·1 |
| Polycythemia | 2·2 |
| Graves’ disease | 2·5 |
| Pneumonia | 2·7 |
| Gout | 3·3 |
| Arterial hypertension | 3·3 |
| Intermittent gastric supersecretion | 3·7 |
| Gout | 4·5 |
[22] However, as Walker Hall reminds us, Taylor, writing in 1912, stated, “That the margin of safety with regard to renal excretion is an exceedingly narrow one, that the kidney excretes uric acid slowly, and that its powers are soon overstepped.”
[23] Magnus Levy and McClure have also noted that the excretion of exogenous purin is not invariably retarded or diminished.
[24] When experimentally injected, the urates are absorbed slowly by phagocytic leucocytes and giant cells.—Gideon Wells.
[25] Because the gouty tophi do not suppurate, even when ulcerated, through the skin, it has been suggested that the urates have antiseptic properties. Bendix (Zeit. klin. Med., 1902 (44), 165), however, could not demonstrate such antiseptic properties experimentally.—Gideon Wells.
[26] Levinthal, in a personal experiment, injected half a gram of xanthin dissolved in piperazine into his cubital vein. A few days later, after a moderate strain upon the limbs through dancing, he was suddenly seized with a fairly acute painful attack in one of his knees, attended with some swelling and local heat.
[27] “Tophi sometimes precede by some years ... the development of gouty attacks in joints. The same is true also of auricular tophi.”—Duckworth: “A Treatise on Gout.”
[28] “While, however, tophaceous concretions generally show themselves after attacks of articular gout, cases occur, as I have already told you, in which the secretion of calcareous matter takes place irrespective of any arthritic attack. This sort of cutaneous gravel, if I may employ a comparison based on the great analogy between the composition of urinary gravel and tophaceous concretions, gravel of the skin, constitutes the sole manifestation of the diathesis, and is accompanied merely by a slight feeling of pain, of pricking unattended by any disturbance of the general health.”—Trousseau’s “Clinical Medicine.”
[29] Redness of the skin overlying a developing tophus is not invariable. In a case recently under my care, the dorsum of the mid-phalangeal joints was the seat of small soft localised swellings. The superjacent skin was unchanged in colour. Aspiration of the contents by a hypodermic syringe disclosed the presence of a turbid white fluid, which, when microscopically examined, was found loaded with the acicular crystals of sodium biurate.
[30] “Quod in omnibus podagricorum paroxysmis solemne est, insignior intumescentia venerum membro vexato intertextarum se in conspectu dat.”—Sydenham.
[31] Sydenham’s classical description: “Towards the end of January or the beginning of February suddenly, and with scarcely any premonitory feelings, the disease breaks out. Its only forerunner is indigestion and crudity of the stomach, which troubles the patient for some weeks previous to the attack. His body also feels swollen, heavy, and windy—symptoms which increase from day to day until the fit breaks out. But a few days before this torpor comes on, and a feeling of flatus along the legs and thighs. Besides this, there is a spasmodic affection, whilst the day before the fit the appetite is unnaturally hearty. The victim goes to bed in good health and sleeps. About two o’clock in the morning he is awakened by a severe pain, generally in the great toe, more rarely in the heel, ankle, or instep. This pain is like that of a dislocation of the bones of these parts, and is accompanied by a sensation as of chilly water poured over the membranes of the suffering joint. Then follow chills and shivers and a little fever. The pain, which was at first moderate, becomes gradually more intense, and while it increases the chills and shivers die out. Every hour that passes finds it greater, until at length at night-time it reaches its worst intensity, and insinuates itself with most exquisite cruelty among the numerous small bones of the tarsus and metatarsus, in the ligaments of which it is lurking. Now it is a violent stretching and tearing of the ligaments, now it is gnawing pain, and now a pressure and tightening. So exquisite and lively meanwhile is the feeling of the part affected that it cannot bear the weight of the bedclothes nor the jar of a person walking in the room. Hence the night is passed in torture and a restless rolling first to one side, then to the other, of the suffering limb, with perpetual change of posture, the tossing about of the body being as incessant as the pain of the tortured joint, and being at its worst as the fit is coming on. Hence the vain efforts by change of posture, both in the body and the limb affected, to obtain an abatement of the pain.
“This comes only towards the second or third hour of the morning (a whole day and night after the first outbreak of the fit), such time being necessary for the moderate digestion and dispersion of the peccant matter. The patient then has a sudden respite, which he falsely attributes to the last change of position. A gentle perspiration is succeeded by sleep. He wakes freer from pain and finds the part recently swollen. Up to this time the only visible swelling has been that of the veins of the affected joint. Next day (perhaps for the next two or three days), if the generation of the gouty matter have been abundant, the part affected is painful, getting worse towards evening and better towards morning. A few days after the other foot swells, and suffers the same pains. The pain in the latter regulates the state of the one first attacked, for the more acutely it is tortured the more perfect is the abatement of suffering and the return of strength in the other. Nevertheless, there is a repetition in the second case of all the misery of the first both as regards intensity and duration. Sometimes during the first days of the disease the peccant matter is so exuberant that one foot is insufficient for its discharge. It then attacks both, and that with equal violence. Generally, however, it takes the feet in succession. After it has attacked each foot the fits become irregular both as to the time of their coming and as to their duration. One thing, however, is constant—the pain increases at night and abates in the morning. Now a series of lesser fits like these constitute a true attack of gout, long or short, according to the age of the patient. To suppose that an attack two or three months in length is all one fit is erroneous. It is rather a series of minor fits. Of these the latter are milder and more limited in their extent than the former, so that the peccant matter is discharged by degrees, and recovery follows. In strong constitutions, when the previous attacks have been few, a fortnight is the length of an attack. With age and impaired habits gout may last two months. With very advanced age, and in constitutions very much broken down by previous gout, the disease will hang on till the summer is far advanced. For the first fourteen days the urine is high-coloured, has a red sediment, and is loaded with gravel. Its amount is less than a third of what the patient drinks. During the same period the bowels are confined. Want of appetite, general chills towards evening, heaviness, and a troublesome feeling even in the parts which are free from the attack, attend the fit throughout. As it goes off the foot itches intolerably, mostly between the toes; the cuticle scales off, and the feet desquamate, as if venomed. The disease being disposed of, the vigour and appetite of the patient return, and this in proportion to the violence of the last fits. In the same proportion the next fit either comes on or keeps off. Where one attack has been sharp, the next will take place that time next year, not earlier.”—Sydenham.
[32] “Pain is better borne by the poor man, as I have had opportunities of seeing, than by the man who acquired or promoted his gout with two or three bottles of port wine daily, with the surroundings which such luxury implies.”—Longstreth, “On Gout.”
[33] “The pain is altogether disproportionate to the other signs of inflammation, and, even more, to the consequent structural changes in the inflamed part.”—Paget.
As to the peculiar character of the pain, Duckworth states: “Nothing at all like it occurs in any other joint disease.”
[34] Sydenham noted that “sometimes the morbific matter is thrown upon the elbows and occasions a whitish swelling, almost as large as an egg, which becomes gradually inflamed and red.”
[35] “Regular gout may supervene suddenly, and be chronic; that is to say, its outbreak need not have been preceded by paroxysms in any way characteristic of acute gout.”—Trousseau, “On Gout.”
[36] As Trousseau puts it: “Regular chronic gout, in respect of the frequency of the recurrence of the paroxysms, resembles acute gout with successive paroxysms, there being this capital difference, however, that its attacks are longer and during the intervals are not entirely absent.”
[37] Mr. James Moore, surgeon to the Second Regiment of Life Guards (Medico-Chirurgical Transactions, 1809, Vol. I.):—
“This effusion” (meaning the milky fluid containing the urate of soda) “occurs not only during fits of gout, but likewise in the intervals; and as the extremities, particularly the hands and feet, are the principal seat of gout, it is there the greatest accumulation of chalk takes place. Though this process is usually preceded and accompanied by inflammation, the chalk is never inclosed in a cyst, like pus in an abscess. It lies usually in the cellular membrane, in the bursæ mucosæ, or in the cavities of the joints. I have even seen it thrown out between the cutis and the cuticle. But, as the gouty inflammation is of the erythematous kind, there is no extravasation of coagulable lymph, and no new-formed covering surrounding the chalk. This point is of the first importance, and explains many of the peculiarities of gout, which is generally considered as a phlegmon. But the absence of coagulable lymph in the inflamed parts I consider as full evidence of the inflammation being erythematous.
“The chalky liquid when first secreted gives to the finger the feeling of fluctuation, and cannot be distinguished from the ordinary serous effusion of gout. But unfortunately the absorbents cannot suck up the chalky particles. The consistence of the liquid therefore becomes thicker and thicker, till at last nothing remains but a hard mass. When even a considerable effusion of this kind occurs, the quantity of chalk which ultimately remains is comparatively small, as by far the greater quantity is merely serum. It therefore usually requires repeated effusions to form any great mass of chalk, and the consistency depends upon its age and the activity of the absorbents. The quantity at last accumulated by repeated paroxysms is in some instances immense, which augments very seriously the sufferings of the gouty. The distress, however, is not owing to any irritating quality in the chalk, but to its obstructing the motion of the tendons and joints, occasioning often complete anchylosis, and pressing and distending the surrounding parts by its bulk. It acts, therefore, by mechanically embarrassing the machine of the body, and not upon the living principle, for it will often remain for years in parts highly sensible without exciting the slightest pain or inflammation. Although these concretions are of so mild a nature, they often are the cause of extensive mischief, bursting externally, occasioning ulcers very difficult to heal. When a violent fit of the gout attacks a chalky tumour, the appearance is frequently very alarming, the new paroxysm being accompanied with a fresh serous and chalky effusion, which, added to the old deposit of chalk, occasions a prodigious swelling; the cutis when distended to the utmost opens, yet sometimes the cuticle remains entire. The chalky or serous liquid may then be seen through the semi-transparent epidermis. The surrounding integuments appear of a deep red, or of a purple hue, threatening mortification, while the pain is excruciating.
“At length the cuticle gives way, a discharge of serum and chalk takes place, and a remission of all the symptoms usually follows. During the whole of this alarming process suppuration never occurs; but soon after the opening has taken place suppuration commences, and pus and chalk are then discharged from the ulcer. There are several unexpected occurrences in the progress of such ulcerations. When an opening is formed, the whole of the chalk never escapes, and its complete evacuation is often a very tedious process; this is owing to its being diffused through the cellular membrane, as in the cells of a sponge. One cell must sometimes give way after another, and small portions of chalk are successively thrown out, so that months and even years pass away before the whole is discharged. It also frequently happens that the orifice contracts and closes over, leaving portions of chalk underneath. This kind of cicatrix sometimes stands its ground, but more commonly breaks out again and again to discharge chalk. Even openings into joints, which are so dangerous when occasioned by other extraneous bodies, are often attended with no serious symptoms when the joint is filled with chalk. On such an accident happening a surgeon unacquainted with these peculiarities might be tempted to propose large openings, or even amputation, as the only resource for hindering extensive inflammation and carious bones. But if he treats the disease mildly, he will find that no such severe plans are requisite, for the parts will probably fall into a very tranquil or indolent state; a sore will continue for a certain period, discharging pus, and occasionally a bit of chalk, till at last the orifice will close up. Independent of the opening formed by a fit of the gout, the skin, stretched over a mass of chalk, is sometimes thinned, absorbed, and pierced by mere pressure. At other times this is effected by common inflammation and suppuration. When openings take place in these milder ways, a less quantity of chalk is usually evacuated; but this depends entirely upon the degree of inflammation. When the suppuration is great, it naturally detaches and washes out a greater quantity of chalk.
“The last peculiarity is the rarest, namely, that a dry, hard piece of chalk shall pierce the skin, and remain like an excrescence, without exciting either inflammation or suppuration.”
[38] According to Adler, about one-tenth as much uric acid is excreted in the sweat as in the urine, sweat containing 0·1 mg. per cubic centimetre.
[39] In this connection the tendency of gouty glycosurics to exhibit boils and sometimes carbuncles should not be forgotten.
[40] Max Strunsky, of New York, discussing the frequency with which by the older physicians gouty forms of arthritis were confused with gonorrhœal, syphilitic, and other undifferentiated forms of infective arthritis, makes the following observation: “Also flatfeet must have added herds of cases, for this pathological entity was as yet unknown. The rich man in pursuit of his pleasure and the poor man from prolonged standing at his labour strained their arches then as they do now, and women by their ultra-fashionable shoes, which fashion decreed upon them in certain periods of history, produced painful feet which were undoubtedly mistaken for gout. That patients with local foot trouble were treated for gout the writer can speak from experience. A typical case is of a woman who came to his office two years ago. She had broken-down anterior arches. Hallux valgus, hammer-toes, and bunions were present, and the heels were small and undeveloped. Her feet were one mass of pain, and they looked infantile, reminding one of a Chinese woman. All her adult life she wore high-heeled, narrow, pointed, tight shoes. She said that for twenty years she had been treated for gout.”
[41] In support of this contention, I would note that Charcot, while he gives us an inimitable account of the tophaceous variety of gout, introduces also another variant, as he deems it, of chronic articular gout. The joint changes in this latter are marked by what he terms “a thorough atrophy,” including the superjacent skin, which “is pale, shining and polished.” With this are associated ankyloses, angular deflections, and partial dislocations. The joints, he states, “may be absolutely free from swelling, for example when the extra-articular urate deposits either do not exist at all, or only mere traces of them, or when only the articular cartilages are invaded by the urate of soda.” It cannot, we think, be doubted that the clinical content of this group is largely made up of rheumatoid or atrophic arthritis. The evidence that these examples, quâ uratic deposits, are of “gouty” nature, is obviously very slender.
Reverting to Sir Dyce Duckworth, this authority also recognises two varieties of chronic articular gout: (a) tophaceous gout; (b) chronic deforming gout, with as its synonym arthritis deformans uratica. As to the clinical content of this latter group he writes: “The fingers, hands, and wrists show various deformities depending on over-growth of articulating ends of bone, cartilage, ligaments, and bursæ. These may be complicated with visible or invisible tophaceous deposits.” As to these anatomical alterations, Duckworth regards them as “similar to, but not the same as, those induced by rheumatic disease.” But he adds: “It is very rare for the deformities of true gout to attain the gross characters peculiar to chronic rheumatic arthritis; they are altogether of lesser degree in the majority of the worst instances.” From a careful study of their anatomical characters, I cannot avoid the conclusion that they were in the main examples of the hypertrophic variety of arthritis deformans, viz., osteoarthritis.
[42] As Sir W. Hale White has pointed out, “pads” not uncommonly develop on the dorsal aspects of the mid-phalangeal joints. They range in size from a split pea to a hazel nut. Histologically they are the outcome of an excessive overgrowth of fibrous tissue beneath the corium. They in no way involve the joints, but, according to Hale White, they have been confused with osteoarthritis. Their frequent association with Dupuytren’s contracture might conceivably lead to their confusion with gout also, inasmuch as that deformity is so widely attributed to a “gouty” habit.
[43] Sir Spencer Wells in his “Practical Observations on Gout and its Complications and on the Treatment of Joints stiffened by Gouty Deposits.”
“Of the many cases related by authors as anonymous disease by far the greater portion were connected with a gouty diathesis, as indicated both by the formation of calculi, by the occurrence of regular paroxysms of gout, and by the descent of the individual from gouty ancestors; they are cases, in fact, which would have been better understood and better treated if they had been termed ‘anomalous gout’; but as the subjects are young females, they are of course set down as ‘anomalous hysteria.’”—Laycock: “Nervous Diseases of Women.”
[44] “Diseases of the Eye” (1918), p. 258.
[45] “Diseases of the Eye” (1919).
[46] “Diseases and Injuries of the Eye” (1913).
[47] Kruckmann, Med. Klinik., 1910, No. 38.
[48] Proc. Roy. Soc. Med., Ophth. Section, 1914, p. 66.
[49] Ophth. Hosp. Reps., VII., p. 287, 1873.
[50] “Diseases of the Eye” (1854), p. 558.
[51] Brit. Med. Journ., 1885, R. Clement Lucas.
[52] Lancet, 1920, Vol. I., p. 500, Browning.
[53] Archives d’Ophtalmologie, Vol. XII., p. 623.
[54] A very rare form of iritis was described by the late Mr. Doyne as guttate iritis (Trans. Ophth. Soc., Vol. XXX., p. 91) because the appearances resembled drops of lymph on the margin of the pupil. In his view it was a true form of gouty iritis, but the diagnosis does not seem to have been confirmed by other observers. Even if we grant that his view is possibly correct, we must beware how we generalise on a basis of exceptions and freaks.
[55] Brit. Med. Journ., 1903, Vol. II., p. 138.
[56] “Gout” (1876), p. 450.
[57] Clin. Soc. Trans., Vol. XI., p. 132, 1898.
[58] “Medical Ophthalmoscopy,” 3rd edition, p. 267.
[59] Practitioner, 1909, Vol. II., p. 61.
[60] Sydenham, discussing a milk diet, observes that “it has done good as long as it has been rigidly attended to. The moment, however, that the patient swerves from it a hair’s breadth, and the moment he betakes himself to the diet of a healthy man (no matter how mild and simple), the gout returns worse than ever.”
[61] “The lighter beers of Germany, Austria, and Scandinavia, appear to be harmless for the gouty unless taken immoderately. Residents in towns goutily disposed, leading sedentary lives, are seldom long tolerant even of light laager beer.”
[62] Sir Archibald Garrod has suggested that guaiacum has a distinct effect in reducing the amount of uric acid excreted, i.e., it was thought that the uric acid is eliminated in some other form, possibly hippuric acid. Accordingly Martindale and Westcott conducted investigations to determine whether this resin increases or decreases the elimination of uric acid from the human body.
A normal individual took guaiacum resin in 5-grain doses daily in the morning, and the uric acid was estimated in the urine the same afternoon. Hippuric acid was also estimated in specimens of the same urine by the method given by Allen, “Chemistry of Urine,” p. 186. After a day’s interval the acids were estimated on several days without administration of the drug. The two series were then repeated on the same lines after an interval. Seeing that the diet of the individual could not well be controlled in weighed amounts of food, as would strictly be necessary for an investigation of this kind, it was thought that to express the results in percentage ratios of uric acid to excess of solids (R.U.A.) over water might yield more comparable results.
Joulie employs this method of indicating the constituents of urine by ratios; cf. Vol. I., p. 736. Thus, taking a specimen of urine with the following “normal” factors in grams per litre:—
| Specific gravity | 1017·8 |
| Excess of solids over water | 17·8 |
| Physiological acidity in terms of H₂SO₄ | 0·849 |
| Total P₂O₄ | 2·083 |
| Cl | 6·865 |
| Urea | 18·75 |
| Uric acid | 0·416 |
| Hippuric acid | 1·3 |
| (mean). |
One may express the constituents as the following percentage ratios:—
| Normal. | |||||
|---|---|---|---|---|---|
| “R.A.”—Ratio of physiological acidity to excess of solids over water | 4·77 |
|
|||
| “R.P.”—Ratio of total P₂O₄ to excess of solids over water | 11·17 | ||||
| “R.U.”—Ratio of urea to excess of solids over water | 100·53 | ||||
| “R.U.A.”—Ratio of uric acid to excess of solids over water | 2·33 | ||||
| “R.H.A.”—Ratio of hippuric acid to excess of solids over water | 7·3 | ||||
| “R.P./R.A.”—Ratio of phosphoric acid to ratio of acidity (Joulie’s factor, cf. Vol. I., p. 737) | 2·45 | ||||
| Ratio of uric acid, for example, is arrived at thus |
|
= 2·33 | |||
The results which we obtained are given in the following table:—
Effects of Guaiacum Resin on the Urine of a Normal Individual.
| Date. | Sp. Gr. | Urea. | Uric Acid. | Hippuric Acid. | “R.U.A.” | “R.H.A.” | |
|---|---|---|---|---|---|---|---|
| With guaiacum | 28/12/11 | 1·0107 | 2·29 | 0·09 | 0·09 | 4·43 | 4·34 |
| With guaiacum | 29/12/11 | 1·0247 | 1·29 | 0·08 | 0·1 | 3·34 | 4·04 |
| With guaiacum | 1/1/12 | 1·0215 | 2·56 | 0·015 | 0·15 | 4·88 | 6·97 |
| With guaiacum | 2/1/12 | 1·0141 | 2·82 | 0·10 | 0·2 | 4·2 | 8·20 |
| Without guaiacum | 4/1/12 | 1·0229 | 2·42 | 0·06 | 0·1 | 2·62 | 4·36 |
| Without guaiacum | 5/1/12 | 1·0249 | 2·42 | 0·08 | 0·2 | 3·16 | 8·03 |
| Without guaiacum | 8/1/12 | 1·0255 | 3·09 | 0·10 | 0·225 | 4·11 | 8·12 |
| With guaiacum | 11/1/12 | 1·0233 | 2·56 | 0·09 | 0·1 | 3·7 | 4·29 |
| With guaiacum | 12/1/12 | 1·0213 | 1·88 | 0·075 | 0·1 | 3·05 | 4·69 |
| Without guaiacum | 24/1/12 | 1·0239 | 2·42 | 0·08 | 0·038 | 3·45 | 1·57 |
| Without guaiacum | 25/1/12 | 1·0229 | 2·15 | 0·06 | 0·05 | 2·61 | 2·18 |
| Average uric acid ratio under guaiacum resin | = | 3·39 |
| Average uric acid ratio without guaiacum resin | = | 3·19 |
| Average hippuric acid ratio under guaiacum resin | = | 5·43 |
| Average hippuric acid ratio without guaiacum resin | = | 4·49 |
The quantity of hippuric acid normally found is known to vary enormously, e.g., between 0·02 and 0·25 per cent. From this we deduced, for purpose of this investigation, a mean normal R.H.A. of 7·3. A number of other investigations were conducted on analogous lines, but need not be recorded.
From the results of these experiments one notices an average increase of uric and hippuric acids during the “+ guaiacum” periods. It is not possible to draw a conclusion without further corroboration. The amount of each acid from day to day is seen to be erratic, and the process of estimation of hippuric acid is not accurate.
[63] “Weakly mineralised thermal muriated waters, such as those of Baden-Baden in Germany, and Bourbon-Lancy in France, which in character and action approach the simple thermal group, may also show great radio-activity. In fact, the Büttquelle of Baden-Baden in this respect rivals some of the most radio-active springs of Gastein. Of Bourbon-Lancy springs, according to A. Piatot, the least mineralised are the most radio-active.”—“Climato-therapy and Balneo-therapy,” by Sir Hermann Weber.
Sir William Ramsay’s Analysis of the Bath Waters.
| Density of the water from King’s Well | 1·0166 | |
| Osmotic pressure equivalent to that of a salt solution containing per litre | 1·09 | grams NaCl. |
Volume of gas in twenty-four hours from—
| Litres. | ||
|---|---|---|
| King’s Well | 4,927 | |
| Cross Spring | 218 | |
| Hetling Spring | 218 | (estimated). |
| 5,363 |
Analysis of gas (King’s Well)—
| Parts per 10,000. |
|
|---|---|
| Carbon dioxide | 360 |
| Nitrogen, etc. | 9,640 |
| No oxygen, no hydrogen, no marsh gas. | |
The nitrogen contains—
| Argon | 73·63 |
| Neon | 23·34 |
| Helium | 2·97 |
From all three wells in twenty-four hours—
| Litres. | |
|---|---|
| Argon | 39 |
| Neon | 12½ |
| Helium | 1½ |
Gases dissolved in Pump-room Water.—This water contains 18·5 volumes of gas per 1,000 of water. Its composition is—
| Carbon dioxide | 6·9 |
| Nitrogen | 11·6 |
It had become somewhat aerated on drawing, but allowance has been made for that.
| Milligrams per million litres. |
|
|---|---|
| Radium in the water of the King’s Well | 0·1387 |
| Niton (radium emanation) in the water of King’s Well | 1·73 |
| ” ” ” ” of Cross Bath | 1·19 |
| ” ” ” ” of Hetling Bath | 1·70 |
| ” ” ” in the gas from King’s Well | 33·65 |
[65] Bickel in a series of experiments in which the acid contents as well as the total amount of gastric juice were considered obtained the following results: simple gaseous waters (Apollinaris, Giesshübl), muriated waters (Rakoczy spring of Kissingen, Wiesbaden, Kochbrunnen), and muriated alkaline waters (Ems, Selters), all of them, as compared to distilled water and ordinary tap water, rather increased than decreased the specific secretory activity of the gastric mucous membrane, whereas simple alkaline waters (Vichy) and sulphated alkaline waters (Karlsbad) had a slight tendency to diminish, and the sulphated “bitter” waters (Hunyadi Janos water) decidedly diminished, the gastric secretory activity, although “bitter” waters sometimes induced a watery flow from the gastric mucosa, which increased the fluid contents of the stomach.
[66] Bain, of Harrogate, from his observations on a man with permanent cutaneous biliary fistula, found that the old sulphur spring of Harrogate increased both the quantity of bile and the bile solids. This, he thinks, may “fairly be taken as an index of the degree to which it stimulates the liver, and is, in fact, the most reliable indication of the value of a cholagogue.”
THE WHITEFRIARS PRESS, LTD., PRINTERS, LONDON AND TONBRIDGE.