TRANSCRIBER’S NOTES:
—Obvious print and punctuation errors were corrected.
—Multiple and antiquate spelling of specialistic words, expecially in French and German, have beed manteined out of consistency and due to the impossibility of determining what the spelling whas at the time this work was composed
—The transcriber of this project created the book cover image using the front cover of the original book. The image is placed in the public domain.
MEDICAL
JURISPRUDENCE
FORENSIC MEDICINE
AND
TOXICOLOGY
BY
R. A. WITTHAUS, A.M., M.D.
Professor of Chemistry, Physics, and Hygiene in the University of the City of New York, etc., etc.
AND
TRACY C. BECKER, A.B., LL.B.
Counsellor at Law,
Professor of Criminal Law and Medical Jurisprudence in the University of Buffalo
WITH THE COLLABORATION OF
J. Clifton Edgar, M.D.; D. S. Lamb, M.D.; W. B. Outten, M.D.;
Hon. Wm. A. Poste; Edward S. Wood, M.D.;
E. V. Stoddard, M.D.;
Hon. Goodwin Brown; J. C. Cameron, M.D.; E. D. Fisher, M.D.;
H. P. Loomis, M.D.; Roswell Park, M.D.; Irving C. Rosse, M.D.;
F. P. Vandenbergh, M.D.; J. H. Woodward, M.D.;
George Woolsey, M.D.
VOLUME ONE
NEW YORK
WILLIAM WOOD & COMPANY
1894
Copyright, 1894,
By WILLIAM WOOD & COMPANY
PRESS OF
THE PUBLISHERS’ PRINTING COMPANY
132-136 W. FOURTEENTH ST.
NEW YORK
CONTENTS.
————
| PAGE | |
| Introduction, | v |
| Medical Jurisprudence, | 1 |
| The Legal Relations of Physicians and Surgeons. T. C. Becker, | 3 |
| The Law of Evidence Concerning Confidential Communications. Chas. A. Boston, | 89 |
| Synopsis of the Laws Governing the Practice of Medicine. W. A. Poste and Chas. A. Boston, |
135 |
| Forensic Medicine. | |
| Thanatological, | 293 |
| The Legal Status of the Dead Body. T. C. Becker, | 295 |
| The Powers and Duties of Coroners. A. Becker, | 329 |
| Medico-Legal Autopsies. H. P. Loomis, | 349 |
| Personal Identity. J. C. Rosse, | 383 |
| Determination of the Time of Death. H. P. Loomis, | 437 |
| Medico-Legal Consideration of Wounds. G. Woolsey, | 457 |
| Medico-Legal Consideration of Gunshot Wounds. Roswell Park, | 591 |
| Death by Heat and Cold. E. V. Stoddard, | 627 |
| Medico-Legal Relations of Electricity. W. N. Bullard, | 661 |
| Medico-Legal Consideration of Death by Mechanical Suffocation. D. S. Lamb, | 705 |
| Death from Submersion or Drowning. J. C. Rosse, | 793 |
| Death from Starvation. E. V. Stoddard, | 813 |
INTRODUCTION.
The terms Forensic Medicine, Legal Medicine, and Medical Jurisprudence have heretofore been used interchangeably to apply to those branches of state medicine and of jurisprudence which have to deal with the applications of medical knowledge to the elucidation of questions of fact in courts of law, and with the legal regulation of the practice of medicine.
Medico-legal science therefore includes all subjects concerning which members of the legal and medical professions may seek information of one another, each acting in his professional capacity. It consists of two distinct branches: that treating of medical law, to which the designation of Medical Jurisprudence properly applies; and that relating to the application of medical, surgical, or obstetrical knowledge to the purposes of legal trials, Forensic Medicine.[1]
The term State Medicine, which is sometimes erroneously used as synonymous with forensic medicine, properly applies to a more extended field of medical inquiry; i.e., to all applications of medical knowledge to the public welfare. State medicine, therefore, while excluding medical jurisprudence, includes, besides forensic medicine, public hygiene, medical ethics, medical education, and military and naval medicine.
Toxicology, the science of poisons, may be divided into[vi] medical toxicology, whose object is the prevention or cure of all forms of poisoning, and forensic toxicology, whose aim is the detection of criminal poisoning. In its last-named relation toxicology differs from forensic medicine in one important particular. In all cases other than those of poisoning in which questions involving medical knowledge arise, the answers are entirely within the functions of the physician, the surgeon, or the obstetrician, but the problems of forensic toxicology require for their solution the further aid of the chemist and the pharmacologist.
Forensic medicine is an applied science, partly legal, partly medical, calling for information and investigation in widely divergent lines, and becoming more minutely ramified with the progressive advances in medical knowledge and in those sciences of which medicine is itself an application. Its development has been dependent partly upon the slow though progressive tendency of medicine from the condition of an empirical art toward that of an exact science, and partly upon the more rapid and more advanced development of criminal jurisprudence. Medical jurisprudence had reached a high development during the early history of the Roman Empire, and at a period long anterior to the first recognition of forensic medicine.
Although the literature of modern medico-legal science is very largely written from the medical point of view and by physicians, its earlier history is to be found in fragmentary form, partly in medical literature, but principally in the writings of historians, in the earlier criminal codes, and in the early records of legal proceedings.
In the earliest historical periods the functions now exercised by the priest, the lawyer, and the physician were performed by the same person, who, presumably, made use of what medical knowledge he possessed in the exercise of his legal functions. Among the Egyptians at a very early period it is certain that medical questions of fact were considered in legal proceedings, and that the practice of medicine was subject to legal regulation. According to Diodorus,[2] “when a pregnant woman was condemned to death, the sentence was not executed until after she was delivered.” The same author tells us[3] that “the physicians[vii] regulated the treatment of the sick according to written precepts, collected and transmitted by the most celebrated of their predecessors. If, in following exactly these precepts which are contained in the sacred books, they did not succeed in curing the sick, they could not be reproached, nor could they be prosecuted at law; but if they have proceeded contrary to the text of the books, they are tried, and may be condemned to death, the legislator supposing that but few persons will ever be found capable of improving a curative method preserved during so long a succession of years and adopted by the most expert masters of the art.” With the system of legal trial in use among the Egyptians[4] it is difficult to imagine that the question of the existence of pregnancy in the one case, or of malpractice in the other, would not be the subject of contest, and, if contested, determined without the testimony of obstetricians or of physicians.[5]
Medical knowledge among the Hindoos was further advanced than among the Egyptians. In the Rig Veda (about 1500 B.C.) occur a few medical references, among which is the statement that the duration of pregnancy is ten (lunar) months.
The earliest purely medical Sanskrit texts are the Ayur Vedas of Châraka and Sûsruta, which were probably written about 600 B.C., but which are undoubtedly compilations of information which had been handed down during many centuries before that time. In each of these is a section devoted to poisons and their antidotes (Kalpa), in which it is written that a knowledge of poisons and antidotes is necessary to the physician “because the enemies of the Rajah, bad women, and ungrateful servants sometimes mix poison with the food.” Full directions are also given for the recognition of a person who gives poison, and to differentiate the poisons themselves, whose number, from all the kingdoms of nature, is legion. The age at which women may marry is fixed at twelve years, while men[viii] may not marry before twenty-five. The duration of pregnancy is given as between nine and twelve lunar months, the average being ten. The practice of medicine is restricted to certain castes, and requires the sanction of the Rajah, and the method of education of medical students is prescribed.[6]
It is singular that the Greeks were apparently destitute of any knowledge of legal medicine. Although medicine and jurisprudence were highly developed among them, allusions to any connection between the two are of very rare occurrence and uncertain.
The Hippocratic writings (ca. 420 B.C.) contain many facts which are of medico-legal interest: the possibility of superfœtation was recognized;[7] the average duration of pregnancy was known, and the viability of children born before term was discussed,[8] the relative fatality of wounds affecting different parts of the body was considered,[9] and the Hippocratic oath makes the physician swear that he “will not administer or advise the use of poison, nor contribute to an abortion.” The position of the physician in Greek communities was an exalted one. No slave or woman might be taught medicine,[10] although later free-born women were permitted to practise in their native places. Homer also refers to physicians as men of learning and of distinction.[11] The Greek physician was therefore in a position, both from his information and from his standing in the community, to aid in the administration of justice.
The Greeks were also extremely litigious and possessed a code of criminal procedure which was elaborate, and in many respects resembled those now in use in England and the United States.[12] The writings of the Greek orators, Demosthenes, Æschines, Lysias, Antiphon, Isocrates, etc., which have come down to us substantiate the claim of Ælian that “to Athens mankind[ix] is indebted for the olive, the fig, and the administration of justice.”[13]
The writings of the Greek physicians contain no reference to any legal application of their knowledge, and certain passages in the writings of the orators seem to indicate that, while a physician was called to inspect and treat a wounded person, the testimony as to the patient’s condition was given in court by others.
Thus in the case against Euergos and Mnesibulus, in which an old woman had died some days after an assault, Demosthenes[14] states that he notified the accused to bring a surgeon and cure the woman; but that as they did not do so, he himself brought his own surgeon and showed him her condition in the presence of witnesses. Upon hearing from the surgeon that the woman was in a hopeless condition, he again explained her state to the accused and required them to find medical aid. Finally, on the sixth day after the assault the woman died. He further asserts that these statements would be proved by the depositions.[15]
The third Tetralogy of Antiphon[16] (B.C. 480) relates to a case in which the defence was essentially the same as that which was the subject of a vast amount of medical expert testimony in a celebrated trial for murder in New York not many years ago. A person wounds another, who dies some days afterward. The assailant is accused of murder and sets up the defence that the deceased perished, not from the wounds inflicted, but in consequence of unskilful treatment by the physicians.
In neither of these cases is any mention made of physicians having been called upon for testimony; indeed, the statements would lead to the inference that they were not. In another case in which a poor and sick citizen is accused of malingering to obtain the customary pecuniary aid from the State, Lysias[17] summons no medical evidence but relies entirely upon a statement of his client’s case.[18]
Medical legislation was not more advanced during the ascendancy of the Roman Empire, although medical science was greatly developed, principally by the labors of Celsus, and of Galen and other Greek physicians. A few cases are mentioned by the historians which would seem to indicate a closer connection between law and medicine than had existed among the Greeks, but they refer rather to the custom of exposing the bodies of those who had died by violent means to public view, in order that any one might express his opinion as to the cause of death, than to any appeal to medical science in the administration of justice. Thus Suetonius[19] says that the physician Antistius examined the dead body of Julius Cæsar (B.C. 44), and declared that of all the wounds only that received in the breast was mortal.
Pliny[20] cites an early instance of contested interpretation of post-mortem appearances in the case of Germanicus, who died A.D. 19, by the action of poison, said the enemies of Piso, because the heart did not burn. The friends of Piso, while admitting the fact of non-consumption, attributed it to the deceased having had heart disease. The same author[21] quotes Masurius as having declared a child born after thirteen (lunar) months to be legitimate, in an action for the possession of property, on the ground that no certain period of gestation was fixed. The Emperor Hadrian (A.D. 117-138), according to Gellius, sought medical information in a similar case, and decreed the legitimacy of a child born in the eleventh (lunar) month, “after having considered the opinions of ancient philosophers and physicians.”[22]
Although the Justinian collections, the “Codex” (A.D. 529), the “Institutes” (A.D. 533), the “Digests,” or “Pandects” (A.D. 534), and the “Novels” (A.D. 535-564), prepared by the best legal talent of the age, under the direction of Tribonian, do not provide for the summoning of physicians as witnesses; they contain an expression which indicates that at that time the true[xi] function of the medical expert was more correctly appreciated than it is to-day. His function was stated to be judicial rather than that of a witness.[23] There is also a provision that in cases of contested pregnancy, midwives (who were considered as belonging to the medical profession) should, after examination of the woman, determine whether or no pregnancy exist, and that their determination should be final. The practice of medicine, surgery, and midwifery was regulated. Those desiring to practise must have been found competent by an examination. The number of physicians in each town was limited. They were divided into classes, and were subject to the government of the Archiatri. Penalties were imposed upon those guilty of malpractice or of poisoning. The Justinian enactments contain abundant internal evidence of having been framed in the light of medical knowledge. They contain provisions relating to sterility and impotence, rape, disputed pregnancy, legitimacy, diseased mental conditions, presumption of survivorship, poisoning, etc., which indicate that the medical knowledge of the time was fully utilized in their construction.[24]
The Germanic peoples at about the same period possessed codes in which traces of a rudimentary medical jurisprudence existed. The most ancient of these was the Salic law (A.D. 422), in which the penalties to be paid for wounds of different kinds are fixed. The Ripuarian law, of somewhat later date, takes cognizance of the crime of poisoning. The laws of the Bavarians, Burgundians, Frisians, Thuringians, and Visigoths contain practically nothing of medico-legal interest. The Lex Alamannorum has numerous provisions relating to wounds, and expressly provides that the gravity of the injury shall be determined by a physician.[25]
During the period of about a thousand years, intervening between the Justinian and Caroline (vide infra) codes, the advancement of medicine and jurisprudence suffered almost complete arrest. The guilt or innocence of an accused person[xii] was determined rather by his own confession under torture, or by “the judgment of God” as shown by ordeal or by judicial combat, than by testimony either expert or of fact.
Even during the night of the Middle Ages, instances are recorded in which the opinions of physicians were sought to determine questions of fact in judicial proceedings.
In the duchy of Normandy, in 1207-45, the laws provided for the examination of those claiming to be sick (to evade military service or appeal to judicial duel), of persons killed, and of women.[26]
In a decretal of Innocent III., in 1209, the question whether a certain wound was mortal was determined by physicians.[27]
There is extant in the statutes of the city of Bologna, under date of 1249, an entry to the effect that Hugo di Lucca had been assigned the duty, when called upon by the podesta, and after having been sworn, to furnish a true report in legal cases.[28]
In the kingdom of Jerusalem (ca. 1250) a person claiming exemption from trial by battle because of sickness or of wounds was visited by a physician (fisicien au miége) and a surgeon (sérorgien), who examined him and made oath as to his condition.[29]
Sworn surgeons to the king are also mentioned in letters patent of Philippe le Hardi in 1278, of Philippe le Bel in 1311, and of Jean II. in 1352.[30] That of Philippe le Bel refers to Jean Pitardi as one of “his well-beloved sworn surgeons in his Chastelet of Paris,” whose functions are partly indicated by the extracts from the registers given below.
The registers of the Châtelet at Paris from 1389 to 1392 record several instances in which medical aid was rendered in judicial proceedings. Under date of March 22d, 1389-90, “Maître Jehan Le Conte, sworn surgeon to the king our sire,” reports to Maître Jehan Truquam, lieutenant to the provost, that “upon that day in the morning one Rotisseur had gone[xiii] from life unto death in consequence of the wounds which he had received on the Monday evening preceding.”[31] Under date of July 22d, 1390, is an account of the examination of one Jehan le Porchier, accused of intent to poison the king (Charles VI.), in which there is reference to a very early instance of toxicological expert evidence. In the wallet of the accused certain herbs were found. The account proceeds: “Richart de Bules, herbalist, was summoned, to him the above-mentioned herbs were shown, and he was commanded that he should examine them and consider well and duly, reporting the truth of what he should find. The said Richart, after having examined them with great diligence, reported that in the box in which these herbs were he had found six leaves, namely: one leaf of jacia nigra, and one of round plantain, called in Latin plantago minor, and four of sow-thistle (lasseron), called in Latin rosti poterugni, and says that the leaf of jatria nigra is poisonous, but that in the others there is no poison known to the deponent.”[32] On August 12th, 1390, “Jehan Le Conte and Jehan Le Grant, sworn surgeons of our sire the king,” are present at the torture of a prisoner, but for what purpose does not appear. In another case the same Jehan Le Conte testified that a wound in the head of a deceased person was made with an axe.[33] At a later period in Italy, the infliction of “the question” took place under medical supervision. Zacchias devotes a chapter, De Tormentis et Pœnis,[34] to the consideration of the different methods of torture, the degrees of pain and danger attending each, and the conditions of age, sex, and health which render its application inadmissible.[35]
During this period, as indeed from the earliest times, the practice of medicine was regulated by law. Thus a law of King Roger of Sicily (1129-54) punished those who practised medicine without authority with imprisonment and confiscation of goods; and an edict of Frederick II. (1215-46) imposed like penalties upon those who presumed to practise except after graduation at the school of Salernum.[36]
Medico-legal science was formed in the middle of the sixteenth century by a simultaneous awakening of jurists and physicians to the importance of the subject.
It was in Germany that expert medical testimony was first legally recognized. In 1507, George, Bishop of Bamberg, proclaimed a criminal code in his domains. This was subsequently adopted by other German states, and finally was the model upon which the Caroline Code, the first general criminal code applying to the whole empire, was framed and proclaimed at the Diet of Ratisbon in 1532.[37]
These codes, particularly the Caroline, distinctly provide for utilizing the testimony of physicians. Wounds are to be examined by surgeons who are “to be used as witnesses;”[38] and in case of death one or more surgeons are to “examine the dead body carefully before burial.”[39] They also contain provisions for the examination of women in cases of contested delivery, or suspected infanticide;[40] for the regulation of the sale of poisons;[41] for the detection and punishment of malpractice;[42] and for examination into the mental condition in cases of suicide and of crime.[43]
An early work on the practice of criminal law, based on the Caroline Code, was published by the Flemish jurist, Josse de Damhouder, in 1554. It contains a chapter treating of the lethality of wounds, which should be determined by expert physicians and surgeons,[44] and describes the course which is to be pursued in the judicial examination of dead bodies. This is probably the earliest printed book (other than the laws themselves) containing reference to medico-legal examinations,[45] and antedates the writings of physicians upon the subject.
Although it was only in 1670 that the Ordinances of Louis XIV. gave to France a uniform criminal code, medico-legal reports were made by physicians and surgeons to the courts[xv] more than a century before. Indeed, the earliest medico-legal work written by a physician[46] is the 27th book of the Œuvres d’Ambroise Paré, first printed in 1575, in which he directs the forms in which judicial reports shall be made in various medico-legal cases.[47] During the remainder of the sixteenth century France produced but three treatises on medico-legal subjects.[48] One of these, written by the jurist A. Hotman, distinctly mentions the employment of physicians to determine questions of fact.
In Italy works on medical jurisprudence were published at the close of the sixteenth and beginning of the seventeenth century. The earliest of these was a chapter of Codronchius, treating of the “method of testifying in medical cases,” in 1597.[49] At about the same time, but certainly later, appeared the work of Fortunatus Fidelis, to whom the honor of being the first writer on medical jurisprudence is given by many.[50]
The great work of Paulus Zacchias, physician to Pope Innocent X., was first printed at Rome, 1621-35. This medico-legal classic contains in the first two volumes the “Quæstiones” and in the third the decisions of the Roman Rota. It treats of[xvi] every branch of medico-legal science, and discusses physiological questions of legal interest, besides dealing with questions such as the infliction of torture and miracles.[51]
Although the “Quæstiones Medico-legales” of Zacchias was the first systematic work upon medical jurisprudence, his countrymen in succeeding centuries have contributed but little to this science. It is only during the latter part of the present century that Italians have again become prominent in medico-legal literature.
In France legal medicine progressed but little from the time of Paré to the latter part of the eighteenth century. Several treatises appeared, being chiefly upon legitimacy and kindred subjects,[52] with a few treating of reports, signs of death, etc.[53]
Toward the end of the eighteenth century the labors of Louis, Petit, Chaussier, and Fodéré elevated legal medicine to the rank of a science. The investigations of Louis (Ant. L.) were numerous and important in this as in other subjects,[54] and the “causes célébres” contain reports of many trials in which he threw light upon doubtful medical questions.[55] Antoine Petit, a contemporary of Louis, contributed an extensive work on the duration of pregnancy as affecting legitimacy.[56]
Somewhat later Fr. B. Chaussier, between 1785 and 1828, published at Dijon a number of treatises on infanticide, viability, surgical malpractice, etc.[57] Fodéré, a Savoyard, was the first to publish a systematic treatise on medical jurisprudence in France, which was first printed in 1798 and in a much enlarged[xvii] form in 1813.[58] This last edition is an exhaustive treatise upon all branches of legal medicine and public hygiene, and won for its author the appointment as Professor of Forensic Medicine in the University of Strassburg.
At about the same period appeared the works of Mahon[59] and of Belloc,[60] both of which went through three editions in ten years, and those of Biessy.[61]
The most industrious and original of French professors of legal medicine was Orfila. A native of Minorca, he graduated in medicine at Paris in 1811, and devoting himself to chemical and toxicological investigations, published the first edition of his “Traité des Poisons” in 1814. This work, which may be regarded as the foundation of experimental and forensic toxicology, went through five editions to 1852, and was translated into several foreign languages. The first edition of his “Leçons de Médecine légale” appeared in 1821, and the fourth in 1848. Besides these Orfila published a work on the treatment of asphyxia and a great number of papers on medico-legal subjects, principally in the Annales d’Hygiène, of which he was one of the founders with Andral, Esquirol, Leuret, and Devergie. Orfila occupied the chair of chemistry and medical jurisprudence in the University of Paris for upward of thirty years, and was employed as expert in innumerable cases before the courts.
Contemporaneous with Orfila, and almost as prominent, was Devergie, the first edition of whose “Médecine légale,” in three volumes, appeared in 1836, and the third in 1852.
In 1820 the first edition of the Manual of Briand and Brosson was published. This work, the tenth edition of which was published in 1879, is the first in which a jurist was associated with a physician in the authorship,[62] and is one of five of which one of the authors is a lawyer.[63]
Special treatises on the medico-legal relations of insanity were published by Georget (1821), Falvet (1828), Esquirol (1838), and Marc (1840), and on midwifery by Capuron (1821).
Tardieu, Professor of Legal Medicine in the University of Paris (1861-79), published a most important series of monographs on hygienic and medico-legal subjects,[64] besides many papers, principally in the Annales d’Hygiène, etc., and testified before the courts in many “causes célébres.”
The first work of medico-legal interest to appear in Germany was the “Medicus-Politicus” of Rodericus à Castro, a Portuguese Jew living in Hamburg, printed in 1614, which deals principally with medical ethics and the relations of physicians, but contains chapters on simulated diseases, poisoning, wounds, drowning, and virginity.[65]
It was only toward the end of the seventeenth century that the subject was scientifically treated, and during the latter part of the seventeenth century and the beginning of the eighteenth great progress was made in the development of forensic medicine in Germany. Johannes Bohn, one of the originators of the experimental method of investigation in physiological chemistry and physics, at the University of Leipzig, was also one of the earliest German contributors to the literature of legal medicine. Besides smaller works he published two noteworthy treatises: in 1689 a work on the examination of wounds and the distinction between ante-mortem and post-mortem wounds, and between death by injury, strangulation, and drowning.[66] In 1704 a work giving rules for the conduct of physicians in attending the sick and in giving evidence in the courts.[67] At about the same period M. B. Valentini, professor in the University of Giessen, published three important works, containing collections of medico-legal cases, and of the opinions and decisions[xix] of previous writers.[68] Another extensive collection of cases and decisions was published in 1706 by J. F. Zittmann, from a MS. left by Professor C. J. Lange, of the University of Leipzig;[69] and still another by J. S. Hasenest[70] appeared in 1755.
During the latter part of the eighteenth century, the Germans cultivated legal medicine assiduously, and a great number of works upon the subject were published. Among these may be mentioned those of M. Alberti, professor at the University of Halle;[71] H. F. Teichmeyer, of the University of Jena;[72] A. O. Gölicke, of the universities of Halle and Duisburg, who was the first to prepare a bibliography of the subject;[73] J. F. Fasel (Faselius), professor at Jena;[74] J. E. Hebenstreit and C. S. Ludwig, professors at Leipzig;[75] C. F. Daniel, of Halle;[76] J. D. Metzger, professor at Königsberg, the author of a number of works, one of which, a compendium, was translated into several other languages;[77] J. V. Müller, of Frankfurt;[78] J. C. T. Schlegel, who collected a series of more than forty dissertations by various writers;[79] M. M. Sikora, of Prague;[80] J. J. von Plenck, professor in Vienna, who published a work on forensic medicine and one on toxicology;[81] K. F. Uden, subsequently professor in St. Petersburg, who was the first to publish a periodical journal devoted to legal medicine, which[xx] was afterward continued by J. F. Pyl at Stendal;[82] and J. C. Fahner.[83]
At this period compends for students were published in Germany, which indicate by their number the extent to which this science was the subject of study. Among these those of Ludwig (1765), Kannegieser (1768), von Plenck (1781), Frenzel (1791), Loder (1791), Amemann (1793), Metzger (1800), and Roose may be mentioned.
The Germans of the present century have maintained the pre-eminence in legal medicine achieved by their forefathers. Among a great number of investigators and writers a few may be mentioned: C. F. L. Wildberg, professor at Rostock, was a most prolific writer, edited a journal devoted to state medicine, and contributed a valuable bibliography of the subject;[84] A. F. Hecker, professor at Erfurth and afterward at Berlin, and J. H. Kopp each edited and contributed extensively to a medico-legal journal.[85] A much more important periodical was established in 1821 by Adolph Henke, professor in Berlin, and was continuously published until 1864. Henke also wrote a great number of articles and a text-book on legal medicine.[86] Jos. Bernt, professor at Vienna, published a collection of cases, a systematic treatise, and a number of monographs,[87] as well as the MS. work left by his predecessor in the chair, F. B. Vietz. A handbook containing an excellent history of medico-legal science was published by L. J. C. Mende, professor at Griefswald,[88] who also contributed a number of monographs, chiefly on obstetrical subjects. K. W. N. Wagner contributed but little to the literature of the subject, but it was chiefly by his[xxi] efforts, while professor in the University of Berlin, that a department for instruction in state medicine was established there in 1832. A. H. Nicolai, also professor at Berlin, published a handbook[89] besides numerous articles in the journals. F. J. Siebenhaar published an encyclopædia of legal medicine, and in 1842 established a journal devoted to state medicine, which in its continuations was published until 1872.[90] J. B. Friedreich, professor at Erlangen, after editing a journal devoted to state medicine from 1844 to 1849, established one of the most important of current medico-legal periodicals in 1850,[91] to both of which he was a frequent contributor until his death in 1862. Ludwig Choulant, professor at Dresden, and more widely known as the author of important contributions to the history of medicine, published two series of reports of medico-legal investigations.[92]
The foremost forensic physician of this period in Germany was unquestionably John Ludwig Casper, professor in the University of Berlin and “forensic physician” (gerichtlicher Physicus) to that city, who greatly extended the department established in the university under Wagner. He made innumerable investigations, some of which are preserved in several collections of cases,[93] others in his classic Handbook,[94] and still others in the periodical which he established in 1852, and which is now the most important current medico-legal journal.[95]
It is necessary in this place to make mention of one work by living authors, as its appearance marked a new departure in medico-legal literature, and as in it the fact that forensic medicine[xxii] extends over so wide a field of inquiry as to require treatment at the hands of specialists was first recognized. To Josef von Maschka, professor in the University of Prague, the credit is due of having been the first to produce, with the collaboration of twenty-two colleagues, a truly systematic work on modern forensic medicine.[96]
English works upon this subject did not exist prior to the present century,[97] although physicians were employed by the courts to determine medical questions of fact at a much earlier date. Paris and Fonblanque, in the third Appendix of their “Medical Jurisprudence,” give the text of reports by the Colleges of Physicians of London and of Edinburgh concerning the cause of death as early as 1632 and 1687 respectively.[98]
Lectures on medical jurisprudence were given at the University of Edinburgh by A. Duncan, Sr., at least as early as 1792.[99] The title of Professor of Medical Jurisprudence in a British university was conferred for the first time, however, upon A. Duncan, Jr., at the University of Edinburgh in 1806.[100]
The first English work on medical jurisprudence worthy of consideration is the medical classic known as Percival’s “Medical Ethics.” This was first published in 1803, and contains in[xxiii] its fourth chapter an admirable epitome of legal medicine.[101] A more elaborate work, based very largely, however, upon the writings of continental authors, was published by G. E. Male in 1816.[102] In 1821 Professor John Gordon Smith published the first systematic treatise on forensic medicine,[103] and was one of the first in Great Britain to show the importance of the subject.
Two years later, in 1823, appeared the elaborate and scholarly work of Dr. Paris and Mr. Fonblanque, the first in the English language in whose authorship members of the medical and legal professions were associated.[104] In 1831, Prof. Michael Ryan published the first edition of his “Manual of Medical Jurisprudence” from the memoranda of his lectures on the subject in the Westminster School of Medicine.[105] A similar work was published by Professor T. S. Traill, of the University of Edinburgh, in 1836.[106] The awakened interest in medico-legal subjects among the medical profession during the decade 1830-40 is evidenced by the publication in the medical journals of the lectures of A. Amos, in 1830-31; of A. T. Thomson, at the London University, in 1834-35; of H. Graham, at Westminster Hospital, in 1835; of W. Cummin, at the Aldersgate Street School, in 1836-37; and of T. Southwood Smith, at the Webb Street Theatre of Anatomy, in 1837-38.[107]
Among the noteworthy contributions to the science previous to 1850 are the writings of Dease (1808), Haslam (1817),[108] Christison, the successor of Professor Duncan in the University of Edinburgh, and best known as a toxicologist, Forsyth (1829),[109] Chitty (1834),[110] Watson (1837),[111] Brady (1839),[112] Skae (1840),[113] Pagan (1840),[114] and Sampson (1841).[115]
In 1836, Dr. Alfred Swaine Taylor (b. 1806, d. 1880), the first Professor of Medical Jurisprudence in Guy’s Hospital, published his “Elements of Medical Jurisprudence.” This, the most important work upon the subject in the English language, is now in its twelfth English and eleventh American edition. During forty years of devotion to forensic medicine Dr. Taylor also contributed other important works and numerous papers, published for the most part in the Reports of Guy’s Hospital.[116] In 1844, Dr. Wm. A. Guy, Professor of Forensic Medicine in King’s College, published the first edition of his excellent work.[117] In 1858, Fr. Ogston, Professor of Medical Jurisprudence in the University of Aberdeen, published a syllabus and subsequently (1878) a complete report of his lectures.[118] In 1882, C. M. Tidy, Professor of Chemistry and Forensic Medicine in the London Hospital, who had previously (1877) been associated with W. B. Woodman in the authorship of a valuable handbook, began the publication of a more extended work, which was interrupted by his death in 1892.[119]
The first Spanish work on legal medicine was that of Juan Fernandez del Valles, printed in 1796-97.[120] No further contribution to medico-legal literature was furnished by Spain until the appearance in 1834 of the work of Peiro and Rodrigo, which went through four editions in ten years.[121] Ten years later, in 1844, Pedro Mata, Professor of Legal Medicine and Toxicology at Madrid, published the first edition of a work, which in the development of its subsequent editions, has become the most important on the subject in the Spanish language.[122]
The first Portuguese medico-legal treatise was that of Jose Ferreira Borjes, first printed at Paris in 1832.[123]
A posthumously published report of the lectures of Albrecht von Haller was the earliest Swiss work on forensic medicine.[124]
In Sweden the earliest medico-legal publication was a comprehensive treatise by Jonas Kiernander, in 1776,[125] which was followed in 1783 by a translation of Hebenstreit, by R. Martin. The voluminous writings of the brothers Wistrand (A. T. and A. H.), including a handbook, were published at Stockholm, between 1836 and 1871. Between 1846 and 1873, several articles upon medico-legal subjects were published at Helsingfors, in Finland, by E. J. Bonsdorff, O. E. Dahl, and J. A. Estlander. In 1838 Skielderup[126] published his lectures on legal medicine, delivered at Christiania, and Orlamundt[127] published a handbook at Copenhagen in 1843. The earliest recognition of medico-legal science in Russia was in the lectures of Balk,[128] begun in 1802 at the then newly founded University of Dorpat.
Although dissertations upon subjects of medico-legal interest were published at the University of Leyden as early as the[xxvi] middle of the seventeenth century,[129] and the works of Pineau,[130] Zacchias,[131] Ludwig,[132] von Plenk,[133] and Metzger[134] were printed in Holland, either in Latin or in the vernacular, no original systematic work on legal medicine in the Dutch language has yet appeared.
The only Belgian contribution to the literature of forensic medicine, other than articles in the journals, is a text-book by A. Dambre, first published at Ghent in 1859.[135]
Two medico-legal works have been printed in the Japanese language, one a report of the lectures of Professor Ernst Tiegel, at the University of Tokio,[136] the other a treatise by Katayama.[137]
In the United States the development of forensic medicine has kept pace with that in the mother country. In an introductory address delivered at the University of Pennsylvania in 1810, the distinguished Dr. Benjamin Rush dwelt eloquently upon the importance of the subject.[138] In 1813, Dr. James S. Stringham was appointed Professor of Medical Jurisprudence in the College of Physicians and Surgeons of New York, and a syllabus of his lectures was published in the following year.[139] At the same period (1812-13) Dr. Charles Caldwell delivered a course of lectures on medical jurisprudence in the University of Pennsylvania.[140] In 1815, Dr. T. R. Beck was appointed Lecturer on Medical Jurisprudence in the College of Physicians and Surgeons of the Western District of the State of New York; and soon after Dr. Walter Charming was appointed Professor of Midwifery and Medical Jurisprudence in Harvard University. In 1823, Dr. Williams, in the Berkshire Medical Institute, and Dr. Hale, of Boston, each lectured upon the subject.[141]
In 1819, Dr. Thomas Cooper, formerly a judge in Pennsylvania,[xxvii] and at that time Professor of Chemistry and Mineralogy in the University of Pennsylvania, reprinted, with notes and additions, the English works of Farr, Dease, Male, and Haslam.[142] The works of Ryan, Chitty, Traill, and Guy were also reprinted in this country shortly after their publication in England.
In 1823, Dr. Theodric Romeyn Beck published at Albany the first edition of a treatise as admirable for scholarly elegance of diction as for profound scientific research. This remarkable work, facile princeps among English works on legal medicine, has had twelve American and English editions, and has been translated into German and Swedish.[143]
Papers upon medico-legal subjects or reports of lectures were published by J. W. Francis,[144] J. Webster,[145] R. E. Griffith,[146] R. Dunglison,[147] J. Bell,[148] and S. W. Williams[149] between 1823 and 1835. In 1840, Amos Dean, Professor of Medical Jurisprudence at the Albany Medical College, published a medico-legal work, followed by another in 1854, which with the later work of Elwell are the only treatises on forensic medicine upon the title-pages of which no physician’s name appears.[150]
Numerous papers and tracts upon medico-legal subjects were published by J. J. Allen, T. D. Mitchell, H. Howard, D. H. Storer, J. S. Sprague, J. S. Mulford, J. F. Townsend, and A. K. Taylor between 1840 and 1855. In the latter year appeared the first edition of the admirable work of Francis Wharton and Dr. Moreton Stillé, the first American product of the collaboration of members of the two professions, now in its fourth edition.[151]
Between 1855 and 1860 no systematic treatises on legal[xxviii] medicine were published, although the medical journals contained numerous articles bearing upon the subject. In 1860 the first edition of a treatise written from the legal aspect was published by J. J. Elwell.[152] In 1869 Dr. J. Ordronaux, recently deceased, widely known as a teacher of legal medicine and a graduate in law as well as in medicine, published a treatise which has been extensively used as a text-book.[153] At the present time the great number and variety of articles published in the medical and legal journals, bearing upon every branch of forensic medicine and of medical jurisprudence, and written for the most part by specialists, is evidence of the assiduity with which the science is cultivated.
The wide appreciation of the importance of medico-legal science in the United States is also indicated by the fact that at the present time there are but few medical schools in which the subject is not taught. To ascertain the extent of medico-legal instruction at the present time, a circular of inquiry was sent to the deans of 124 medical schools and of 56 law schools in the United States and British provinces. Answers were received from 103 medical colleges. Of these only 3 are without a teacher of “medical jurisprudence.” In 38 the teacher is a physician, in 50 he is a lawyer, in 5 he is a graduate in both professions, and 3 have two teachers, one a lawyer, the other a physician. The average number of lectures given is 21, and the average in those schools in which the teacher is a lawyer, and therefore presumably teaches only medical jurisprudence, is 15. The medico-legal relations of their subjects are taught in their lectures by the neurologist in 62 schools, by the surgeon in 66, by the obstetrician in 69, and by the chemist (toxicology) in 91. It appears from these reports that not only is the importance of medico-legal science appreciated, but that in the majority of our medical schools the distinction between medical jurisprudence and forensic medicine is recognized in the fact that the instructor is a lawyer, who presumably teaches medical jurisprudence, while the different branches of forensic medicine and toxicology are taught by the specialists most competent to deal with them. Every practising physician requires thorough[xxix] instruction in medical jurisprudence, which, being strictly legal, is best taught by one whose profession is the law. The general practitioner only requires so much knowledge of the different branches of forensic medicine as will enable him to intelligently fulfil his obligations in such medico-legal cases as will be forced upon him as results of his ordinary practice. He can become a medical expert only by a particular study of and a large experience in some particular branch of the subject.
In our law schools the teaching of medico-legal science is not as general as in schools of medicine. Of 35 law schools, only 10 have professors of medical jurisprudence. Of these 6 are lawyers, 1 is a physician, 2 are graduates in both professions, and 1 is a doctor of divinity.
In this work the existence of specialists in the various branches of medico-legal science has been recognized for the first time in a treatise in the English language. Each branch has been assigned to a specialist in that subject, or at least to one who has made it a particular study.
In the arrangement of the matter, the primary division into the three sciences of medical jurisprudence, forensic medicine, and toxicology has been adopted. The division of pure medical jurisprudence is contained in the present volume, while the legal aspects of neurology, obstetrics, etc., will be treated of in future volumes along with the subjects to which they relate. In the division of forensic medicine the classification of Casper has been followed: i.e., Thanatological; including those branches in which the subject of inquiry is a dead body (contained in the present volume). Bio-thanatological; relating to questions concerning both dead bodies and living persons (in the second volume). Biological; relating to living persons (in the second and third volumes). The applications of the microscope to forensic medicine will be treated of in the second volume. The fourth volume will contain the division relating to toxicology.
R. A. W.
MEDICAL JURISPRUDENCE.
THE LEGAL RELATIONS
OF
PHYSICIANS AND SURGEONS,
INCLUDING
THEIR ACQUIREMENT OF THE RIGHT TO PRACTISE MEDICINE AND
SURGERY; THEIR LEGAL DUTIES AND OBLIGATIONS; THEIR RIGHT
TO COMPENSATION; THEIR PRIVILEGES AND DUTIES WHEN
SUMMONED AS WITNESSES IN COURTS OF JUSTICE,
AND THEIR LIABILITY FOR MALPRACTICE.
BY
TRACY C. BECKER, A.B., LL.B.,
Counsellor-at-Law; Professor of Criminal Law and Medical Jurisprudence in the Law
Department of the University of Buffalo; Chairman Executive Committee
New York State Bar Association, etc.
LEGAL STATUS OF PHYSICIANS.
CHAPTER I.
OF THE RIGHT TO PRACTISE MEDICINE AND SURGERY.
Legal Definition and History of the Terms
Physician and Surgeon.
At common law the right to administer drugs or medicines or to perform surgical operations was free to all. And such was the rule of the Roman civil law. But the importance of prescribing certain educational qualifications for those who made such practices their means of gaining a livelihood soon became apparent, and as early as the year 1422, during the reign of Henry the Fifth in England, an act of Parliament was adopted forbidding any one, under a penalty of both fine and imprisonment, from “using the mysterie of fysyck unless he hath studied it in some university and is at least a batchellor of science.”
As a result of this and other statutory regulations, a class of professional men grew up, who were called “physicians,” because they professed to have the qualifications required by such legal regulations to wisely prescribe drugs and medicines for the cure of diseases. A chirurgeon or surgeon—Latin, chirurgus; Greek, χειρουργος, compounded of χειρ, the hand, and ἐργειν, to work—as the derivation of the word shows, was one who professed to cure disease or injuries by manual treatment and appliances.
It would be more interesting than profitable to trace the history of these terms, and of the professions of medicine and surgery from the early times, when the clergy administered healing to the body as well as to the soul, and when barbers were generally surgeons, and blood-letting by the knife-blade and the use of leeches caused the common application of the term “leech” to those who practised surgery.
Definition.—For the purposes of this treatise, however, it will be sufficient to define the term “physician,” as meaning any one who professes to have the qualifications required by law to practise the administration of drugs and medicines, and the term “surgeon,” as meaning any one who professes to have the like qualifications to perform surgical operations, for the cure of the sick or injured.
For a list of the early statutes of England relating to the practice of medicine the reader may consult Ordronaux’ “Jurisprudence of Medicine,” p. 5, note 2.
The present statutory regulations throughout the United States and in England and Canada will be more particularly referred to and synopsized hereafter in this volume.
CHAPTER II.
ACQUIREMENT OF LEGAL RIGHT TO PRACTISE MEDICINE AND SURGERY.
Now Generally Regulated by Statute.—In nearly all of the United States, as well as in England, France, Germany, and other civilized and intelligent communities, the legal right to practise the administration of drugs and medicines, or to perform operations in surgery for the purpose of curing diseases or injuries, has for many years been the object of statutory legislation. The necessity and propriety of regulating by law such practices is generally conceded. It is manifest to all that a person engaging in the practice of medicine or surgery as a profession is holding himself out to the world, and especially to his patients, as one qualified by education and experience to possess more than ordinary skill and ability to deal with the great problems of health and life. He professes to the world that he is competent and qualified to enter into the closest and most confidential relations with the sick and afflicted, and that he is a fit and proper person to be permitted freely, and at all hours and all seasons, to enter the homes, the family circle, and the private chamber of persons suffering from disease or injury. All this he professes and does upon his own account, and for his own profit.
Statutory Regulation of the Right to Practise, Constitutional.—The exercise by the States of these statutory powers is upheld as a valid exercise of the “police power,” to protect the health of the community. When the constitutionality of such enactments has been questioned, it has been attacked upon the alleged ground that the statutes under question unjustly discriminated in favor of one class of citizens and against another class; and as depriving those already engaged in the practice of medicine or surgery of “their property without due process of law.” State v. Pennoyer, 18 Atl. Rep.,[8] 878; ex parte Spinney, 10 Nev., 323; People v. Fulda, 52 Hun. (N. Y.), 65-67; Brown v. People, 11 Colo., 109.
Opinion of United States Supreme Court.—This subject has been carefully considered by the United States Supreme Court in a recent case, and the broad extent of the legislative powers of the States to regulate such matters clearly and fully declared. Dent v. West Va. (129 U. S., 114). The Court say—pp. 121 et seq.—Mr. Justice Field delivering the opinion, in which all the other Justices concur: “The unconstitutionality asserted consists in its [the statutes] alleged conflict with the clause of the Fourteenth Amendment, which declares that no State shall deprive any person of life, liberty, or property, without due process of law; the denial to the defendant of the right to practise his profession, without the certificate required, constituting the deprivation of his vested right and estate in his profession, which he had previously acquired.
“It is undoubtedly the right of every citizen of the United States to follow any lawful calling, business, or profession he may choose, subject only to such restrictions as are imposed upon all persons of like age, sex, and condition. This right may in many respects be considered as a distinguishing feature of our republican institutions. Here all vocations are open to every one on like conditions. All may be pursued as sources of livelihood, some requiring years of study and great learning for their successful prosecution. The interest, or, as it is sometimes termed, the estate acquired in them, that is, the right to continue their prosecution, is often of great value to the possessors, and cannot be arbitrarily taken from them, any more than their real or personal property can be thus taken. But there is no arbitrary deprivation of such right where its exercise is not permitted because of a failure to comply with conditions imposed by the State for the protection of society. The power of the State to provide for the general welfare of its people authorizes it to prescribe all such regulations as, in its judgment, will secure or tend to secure them against the consequences of ignorance and incapacity as well as of deception and fraud. As one means to this end it has been the practice of different States, from time immemorial, to exact in many pursuits a certain degree of skill and learning upon which the community may confidently rely, their possession being generally[9] ascertained upon an examination of the parties by competent persons, or inferred from a certificate to them in the form of a diploma or license from an institution established for instruction on the subjects, scientific and otherwise, with which such pursuits have to deal. The nature and extent of the qualifications required must depend primarily upon the judgment of the State as to their necessity. If they are appropriate to the calling or profession, and attainable by reasonable study or application, no objection to their validity can be raised because of their stringency or difficulty. It is only when they have no relation to such calling or profession, or are unattainable by such reasonable study and application, that they can operate to deprive one of his right to pursue a lawful vocation.
“Few professions require more careful preparation by one who seeks to enter it than that of medicine. It has to deal with all those subtle and mysterious influences upon which health and life depend, and requires not only a knowledge of the properties of vegetable and mineral substances, but of the human body in all its complicated parts, and their relation to each other, as well as their influence upon the mind. The physician must be able to detect readily the presence of disease, and prescribe appropriate remedies for its removal. Every one may have occasion to consult him, but comparatively few can judge of the qualifications of learning and skill which he possesses. Reliance must be placed upon the assurance given by his license, issued by an authority competent to judge in that respect, that he possesses the requisite qualifications. Due consideration, therefore, for the protection of society, may well induce the State to exclude from practice those who have not such a license, or who are found upon examination not to be fully qualified. The same reasons which control in imposing conditions, upon compliance with which the physician is allowed to practise in the first instance, may call for further conditions as new modes of treating disease are discovered, or a more thorough acquaintance is obtained of the remedial properties of vegetable and mineral substances, or a more accurate knowledge is acquired of the human system and of the agencies by which it is affected. It would not be deemed a matter for serious discussion that a knowledge of the new acquisitions of the profession, as it from time to time advances in its attainments[10] for the relief of the sick and suffering, should be required for continuance in its practice, but for the earnestness with which the plaintiff in error insists that, by being compelled to obtain the certificate required, and prevented from continuing in his practice without it, he is deprived of his right and estate in his profession without due process of law. We perceive nothing in the statute which indicates an intention of the legislature to deprive one of any of his rights. No one has a right to practise medicine without having the necessary qualifications of learning and skill; and the statute only requires that whoever assumes, by offering to the community his services as a physician, that he possesses such learning and skill, shall present evidence of it by a certificate or license from a body designated by the State as competent to judge of his qualifications. As we have said on more than one occasion, it may be difficult, if not impossible, to give to the terms ‘due process of law’ a definition which will embrace every permissible exertion of power affecting private rights and exclude such as are forbidden. They come to us from the law of England, from which country our jurisprudence is to a great extent derived, and their requirement was there designed to secure the subject against the arbitrary action of the crown and place him under the protection of the law. They were deemed to be equivalent to ‘the law of the land.’ In this country the requirement is intended to have a similar effect against legislative power, that is, to secure the citizen against any arbitrary deprivation of his rights, whether relating to his life, his liberty, or his property. Legislation must necessarily vary with the different objects upon which it is designed to operate. It is sufficient, for the purposes of this case, to say that legislation is not open to the charge of depriving one of his rights without due process of law, if it be general in its operation upon the subjects to which it relates, and is enforceable in the usual modes established in the administration of government with respect to kindred matters: that is, by process or proceedings adapted to the nature of the case.”
Early Common-Law Rule Concerning Suits by Physicians.
The common-law rule was that the physician could not sue and recover for his services, though he might for the medicines he furnished. The theory of the law followed the etiquette of his profession and forbade him from making a specific contract for pay for his services, and obliged him to receive what his patient chose to give him, which was called his “honorarium.”
The Early Common-Law Rule No Longer in Force.—As time went on this theory vanished from the law. For many years it has lost its place among the rules of professional etiquette. In its stead statutory provisions have been adopted which forbid a recovery for services performed by persons not legally authorized to practise. The right to contract with the patient or with those who employ the medical man, and his remedies to enforce such contracts, will be treated of hereafter.
Statutory Regulations in New York State.—Most of the States of the United States have enacted statutory regulations prescribing in one form or another the necessary qualifications which entitle a physician or surgeon to practise, and prescribing penalties for practising without having complied with such statutory requirements. In the State of New York such matters were regulated for the first time by statute in 1787. This was followed by a general enactment on the subject of the organization of county medical societies, and of State medical societies having boards of censors, to whom was committed the power to examine applicants for license to practise, and of issuing licenses (Laws of 1813, p. 94). This law remained in force, with certain modifications, until 1844, when all acts regulating the practice of medicine and surgery were repealed. A history of the statutory regulations in New York State up to the act of 1844 on this subject will be found in the case of Bailey v. Mogg, 4 Denio, 60.[154]
At the time of the passage of the act of 1813, and for many[12] years afterward, nearly all of the physicians in New York State practised in accordance with the theories and precepts of what is now called the regular or allopathic school of medicine. That act provided that the physicians in the respective counties of the State of New York should meet in the respective counties and organize county medical societies. As a consequence of the fact that the physicians of that day were chiefly of the allopathic school, they necessarily obtained the control of the county medical societies and State medical societies. Hence it became difficult, if not impossible, for physicians who wished to practise upon other theories and tenets than those obtaining in that school, to obtain licenses to do so. With the growth of the homœopathic school of medicine and the eclectic school of medicine, came applications to the legislature asking for those practising under those schools the same rights and privileges of organizing county and State societies as had been extended to physicians generally by the act of 1813; so that in 1857, by Chapter 384, the legislature of New York State enacted that the homœopathic physicians might meet in their respective counties and organize county medical societies, with boards of censors having the same powers and privileges which were granted by the act of 1813; and by other laws similar privileges were granted to the so-called eclectic school. After the passage of the act of 1844, down to about 1874, as hereinbefore stated, there was no limitation upon the right to practise medicine or surgery in this State.
The inharmonious and injurious effect of such policy of the State becoming manifest, the legislature, by Chapter 436 of Laws of 1874, required all persons desiring to practise medicine or surgery to obtain a certificate as to their qualifications from the censors of some one of these medical societies. By the Laws of 1880, Chapter 513, additional and more extensive and particular provisions were made in reference to this matter, and all the physicians then practising were required, on or before the time limited in the act, to file with the county clerks of their respective counties their licenses to practise granted by the censors of their county medical societies, or a diploma of some chartered school of medicine; and those persons who desired to become licensed who were not in practice were likewise required to obtain similar licenses or certificates and file the same.[13] A diploma of a chartered school or medical college was given the same effect as a license issued by the censors.
Recent Legislation in New York State.—The whole matter, however, of licensing physicians to practise has, in the State of New York, been recently regulated by Chapter 468, Laws of 1889, and 499 of 1890, which have reference to the qualifications of persons becoming medical students, and Chapter 507 of 1890, which gives to the Regents of the University of the State of New York power to select boards of examiners from persons nominated by each of the three State medical societies, viz., the New York State Medical Society, Homœopathic Medical Society, and Eclectic Medical Society. These boards prepare questions which are to be approved by the State Board of Regents; examinations are held in different parts of the State upon these questions, the examination papers are certified to that one of these boards of examiners which the student may elect, and that board in turn certifies whether or not the examination has been successfully undergone; and upon its certificate the Board of Regents licenses the student to practise, and his examination papers are filed in the office of the Board of Regents and become a matter of record. These provisions have been enlarged and modified slightly by various statutes since enacted. They are all now embodied in Chapter 601 of Laws of 1893. They will be found carefully synopsized below.
Penal Provisions in New York State.—The New York Penal Code, which went into effect in 1882, enacted that a person practising medicine or surgery, or pretending to be a physician or surgeon, without a license or a diploma from some chartered school, should be deemed guilty of a misdemeanor punishable by fine or imprisonment (Penal Code, Section 356); and the same statute, 357, made it a misdemeanor for a person, whether licensed or not, to practise medicine or surgery, or do any other act as a physician or surgeon, while intoxicated, by which the life of any person is endangered or his health seriously affected.[155]
Giving “Patented” Medicines No Exception.—At one time an attempt was made to claim, that under the patent laws of the United States a person had the right to administer patent medicines without being punishable for practising without a license, but this doctrine was repudiated by the courts. Thompson v. Staats, 15 Wend., 395; Jordan v. Overseers, etc., 4 Ohio, 295.
Courts may Compel Granting of License.—A person who is qualified and complies with reasonable rules of a licensing body, can compel such body to license him. This was held to be the law in the case of The People ex rel. Bartlett v. The Medical Society of the County of Erie, which is also an important authority in respect to a vexed question of medical ethics. It appeared in that case that under the general laws of New York in regard to the organization of medical societies, a medical society had refused to receive as a member a person otherwise qualified, because he had advertised in the public prints a certain cure, including a mechanical appliance used in treating throat troubles; it being forbidden by the code of ethics of the American Medical Association, which the County Medical Society had adopted as one of its by-laws, that a physician or surgeon should advertise. The Court of Appeals of the State of New York held that this constituted no defence to a proceeding instituted by such person to obtain a mandamus compelling the society to admit him to membership, if otherwise qualified.[156]
It has also been decided that a medical society had no right to make a by-law establishing a fixed fee-bill, or tariff of charges, and providing for the expulsion of a member charging at a different rate than that prescribed. Such a by-law was declared unreasonable and void in the case of People v. Medical Society of Erie County, 24 Barb., 570.
The effect of these decisions was, so far as they affect the validity of by-laws, attempted to be avoided in that State by Chapter 445 of Laws of 1866, by which it is expressly enacted that the county medical societies of the State of New York may make such rules and by-laws as they see fit, “not inconsistent with the laws of said State, and may enforce them by expulsion or other discipline.” It may be considered doubtful whether this legislation can accomplish its purpose in the case of the adoption of a by-law void as against public policy.
No Particular Schools Recognized by the Courts.—The general trend of the decisions in all the States, whenever[16] any questions in reference to schools of medicine have been before our courts, is to avoid recognizing any particular system or school. The theory of the New York courts upon this subject is well expressed by the liberal-minded and learned Judge Daly in the New York Court of Common Pleas, in the case of Corsi v. Maretzek, 4 E. D. Smith, 1-5. In that case it was claimed that a certificate of incapacity because of sickness, given by a “homœopathic” physician to an opera-singer, was not binding. It was argued that the employment of a “homœopathic” physician under the contract did not fulfil a provision thereof which required the event of the singer’s sickness to be certified to by “a doctor,” to be appointed by the director.
The Court said: “The system pursued by the practitioner is immaterial. The law has nothing to do with particular systems. Their relative merit may become the subject of inquiry, when the skill or ability of a practitioner in any given case is to be passed upon as a matter of fact. But the law does not, and cannot, supply any positive rules for the interpretation of[17] medical science. It is not one of those certain or exact sciences in which truths become established and fixed, but is essentially progressive in its nature, enlarging with the growth of human experience, and subject to those changes and revolutions incident to any branch of human inquiry, the laws of which are not fully ascertained. The labors of the anatomist, the physiologist, and the chemist have contributed an immense storehouse of facts; but the manner in which this knowledge is to be applied in the treatment and cure of diseases has been, and will probably continue to be, open to diversity of opinion. No one system of practice has been uniformly followed, but physicians from the days of Hippocrates have been divided into opposing sects and schools. The sects of the dogmatists and the empirics divided the ancient world for centuries, until the rise of the methodics, who, in their turn, gave way to innumerable sects. Theories of practice, believed to be infallible in one age, have been utterly rejected in another. For thirteen centuries Europe yielded to the authority of Galen. He was implicitly followed—his practice strictly pursued. Everything that seemed to conflict with his precepts was rejected; and yet, in the revolutions of medical opinion, the works of this undoubtedly great man were publicly burned by Paracelsus and his disciples; and for centuries following, the medical world was divided between the Galenists and the chemists, until a complete ascendency over both was obtained by the sect of the Vitalists. This state of things has been occasioned by the circumstance that medical practitioners have often been more given to the formation of theories upon the nature of disease and the mode of its treatment, than to that careful observation and patient accumulation of facts, by which, in other sciences, the phenomena of nature have been unravelled. I am far from undervaluing the great benefits conferred upon mankind by the study of medicine, and have no wish to minister to any vulgar prejudice against a useful and learned profession, but it is not to be overlooked that, as an art, it has been characterized, in a greater degree, by fluctuations of opinion as to its principles and the mode of its practice, than, perhaps, any other pursuit. That it has been distinguished by the constant promulgation and explosion of theories, that it has alternated between the advancement of new doctrines and the revival of old ones, and[18] that its professors in every age have been noted for the tenacity with which they have clung to opinions, and the unanimity with which they have resisted the introduction of valuable discoveries. They still continue to disagree in respect to the treatment of diseases as old as the human race; and at the present day, when great advances have been made in all departments of knowledge, a radical and fundamental difference divides the allopathist from the followers of Hahnemann, to say nothing of those who believe in the sovereign instrumentality of water.
“In fact, nothing comparatively is known of the philosophy of disease. Its eradication or cure, where the result of human agency is, in the great majority of instances, attributable rather to the careful observation, judgment and experience of the particular practitioner, than to the application of general or established methods available to all. The popular axiom, that ‘doctors differ,’ is as true now as it ever was, and as long as it continues to be so, it is impossible for the law to recognize any class of practitioners, or the followers of any particular system or method of treatment, as exclusively entitled to be regarded as doctors. In adverting to the conflicting views and differences of opinion, that exist and have ever existed in the practice of the healing art, it is not to call in question the value of learned, skilful and experienced physicians, but merely to show the error of attempting, in the present state of medical science, to recognize, as matter of law, any one system of practice, or of declaring that the practitioner who follows a particular system is a doctor, and that one who pursues a different method is not.” And see also White v. Carroll, 42 N. Y., 161; Ordronaux’ “Jurisprudence of Medicine,” 27.
This decision was prior to the statute of 1874 and the provisions of the Penal Code before noted. Since those statutes, it is a misdemeanor to practise except as permitted by the provisions of those statutes.
IN NEW YORK AND ELSEWHERE PRACTITIONER WITHOUT LICENSE CANNOT SUE AND RECOVER FOR HIS FEES.
Since the passage of the New York Act of 1844 (Laws of 1844, p. 406), there has been no precise statutory provision in that State prohibiting in terms persons who practise physic or[19] surgery without a license, from suing to obtain a recovery for services performed. But this is of little consequence, for, as we have already stated, so practising has been declared to be a misdemeanor by the Penal Code of New York.
It is a well-settled principle that when any act is declared by statute to be criminal, a contract calling for the performance of such an act is illegal and void. The early English authorities on this point are fully collated in Wheeler v. Russell (17 Metc., Mass., 258), and the later English and American cases may be found in “American and English Cyclopædia of Law,” title “Contracts,” Vol. III., p. 872 et seq.; see also id., Vol. XVIII., p. 440. Further consideration of the validity of contracts for medical and surgical services will be had hereafter. A full synopsis of the statutes of the different States regulating the licensing of physicians and surgeons in force at the time this volume goes to press will be placed in another chapter.
In a suit between a person who has performed medical and surgical services, and one who employed him, it is said that the person performing the services is presumed to have been licensed to do so.[157] If the State sues for a penalty, a different rule is claimed to prevail.[158]
How may a Diploma or License be Proved in a Court of Law?
It is evident from the foregoing considerations that in any proceedings to punish for practising without license or legal authority, and in actions to recover payment for professional services in the States and countries, where a license or diploma of a regularly chartered school or college is required by statute to entitle the person to practise, it may become important to establish—first, the legal authority to grant the license or diploma; and second, the genuineness of the license or diploma produced. It frequently happens that the diploma or license has been obtained in another State or country. Under the New York statutes, especially the laws of 1880 and 1890, it was made necessary to file a diploma. When it had been issued by a chartered school of another State it must be certified to by some lawfully incorporated medical college in this State, before being received for filing, or regarded by the law as conferring upon its possessor the right to practise in that State.
As to the chief element of authenticity, namely, the legal incorporation or authority of the body or institution granting the diploma, it is clear that the act of incorporation itself would be the best evidence of the incorporation of the college or school, and a special act granting the power to license to a board of censors or other official body or board would have to be produced to show the right vested in that board or body to grant a license. In Georgia it has been held (Hunter v. Blount, 27 Ga., 76), that to prove a diploma given to a physician in another State, the existence of the college, and the fact of its being a chartered institution, must be shown by producing its act of incorporation.
In Thornton’s case (8 Term Rep., 303; same case, 3 Esp., 4), it was held that the mere production in court of a diploma under the seal of one of the universities, is not of itself evidence to show that the person named in the diploma received the degree which the diploma specified. In another[21] and later case, however, Simpson v. Dunmore (9 M. & W., 45; same case, 5 Jurist, 1012), it was held that it was unnecessary for the person producing a license from the Apothecaries’ Company (an incorporated body) to practise as an apothecary, the seal on which license was proved to be genuine, to give any additional evidence of his identity with the person named in the license. The reason for this doctrine is probably to be found in the well-known rule of evidence, that identity of both christian name and family name, is sufficient to raise a presumption of fact that the person bearing the name is the identical person so named in any written instrument.
In Walmsley v. Abbott (1 K. & P., 309; same case, 5 D. & R., 62), proof of the signature of one of the examiners who signed a certificate of examination was held sufficient to warrant the acceptance of the certificate in evidence in the first instance. In another case the proof was that a person previously a stranger to the place went to a town which was the seat of a university, and was told that a certain building was the college, and that a certain person whom he saw there was the librarian, and that this librarian showed him what purported to be the seal of the university, and also a book which the librarian stated was the book of acts or records of the university, and the seal so shown him was compared with the seal of a certain diploma, the genuineness of which was in question, and a copy was made from the said book of acts, of an entry stating that the degree of M. D. had been conferred by the university upon a person bearing the same name as that in the diploma, and this proof was held a sufficient authentication of the diploma, and of the act or authority of the university conferring the degree. Collins case, 1 Addison & Ellis, 695; same case, 3 N. & M., 703.[159]
The Rule in Criminal Prosecutions.—We have seen above,[22] that in a criminal prosecution the burden is on the defendant to produce and prove his license, but to warrant a conviction for practising without a license it must be shown that the accused actually practised. It is not enough to show that he is called by persons whom he attends personally, that is, for whom he prescribes, or to whom he gives medicine or whom he treats. There must be proof shown that he has done this on his own account or for his own profit. But proof of a single act connected with other circumstances, such as tend to show that he held himself out as a physician, is enough. Burham v. State, 116 Ind., 112; Hill v. Bodie, 2 Stew. and P. (Ala.), 56; Pedgrift v. Schiller, 8 C. B., N. S., 200 (same case, 6 Jurist, N. S., 1341). And if he simply practises “massage,” he does not fall within the acts against practising medicine, even though he pretends to accomplish as much good as could have been accomplished by a regular physician. Smith v. Lane, 24 Hun, N. Y., 632. But see also Leech v. Ripon, 12 Cent. L. J., 479; State v. Schultz, 11 Reporter, 701.[160]
Falsely Pretending to be a Licensed Practitioner Generally a Misdemeanor.—In some of the States, and in England, it is not only made a misdemeanor to practise without a license, but falsely pretending to be a licensed practitioner is made a misdemeanor. Such is the provision of the Penal Code of New York heretofore cited. In England such a statute has been somewhat strictly construed in the case of Carpenter v. Hamilton (37 Law Times Rep., 157). In that case it appeared that a person advertised himself as “John Hamilton, M.D.,” of the “Metropolitan Medical College of New York.” It further appeared that he was not registered as required by the law of England. In a prosecution against him for falsely pretending to be a licensed physician, the only proof of his practising being[23] as just stated, an acquittal was sustained by a majority of the court, which held that it was a question of fact to be determined by a trial court whether or not what he did was pretending to be a physician authorized to treat a patient. The Court intimated that the person simply pretended to be what he really was, namely, a doctor of medicine of the Metropolitan Medical College of New York.
State and Local Boards of Health—Powers Governed by Special Statutes.
In addition to the rules and regulations prescribed by the general statutes, modern sanitary science has developed so broadly throughout most of the civilized states and countries, that the different governments have established state boards of health, and in many instances local boards of health, the latter being limited in their authority and operation to specific municipal divisions, to which boards the government has committed the power to pass certain sanitary rules and regulations, which rules and regulations may have an important bearing upon and relation to the practice of medicine and surgery. The jurisdiction and powers of these boards are to be found in the special statutes creating them, and prescribing their powers and duties, and cannot be treated of extensively here. They will be considered further under the special subjects to which they relate.
Physicians Bound to Report Contagious Cases and Not Liable for Mistaken Report.—The duty to promptly report[161] to[24] boards of health every case of contagious or infectious disease is manifest.
CHAPTER III.
OF THE CONTRACTUAL RELATION BETWEEN PHYSICIAN AND PATIENT.
Employment and Rights in Regard To Compensation.
Legal Character of the Employment.—Whatever may have been the theories of the Roman civil law, and following it of the early English common law, as to the character of the employment of physicians and other professional men, it is now so well settled that the reciprocal duties and obligations arising between physician and patient, or attorney and client, and the like, are to be classed under and governed by the law of contracts, that any extended discussion of these theories is unnecessary here.[162] Mr. Ordronaux, in the second chapter of his interesting work on the “Jurisprudence of Medicine,” has considered them fully, and has quoted amply from the books of the earlier and later text-writers, and from the expressions of the judges, to show what these theories and rules were; and he and all later authorities agree that the ancient notion, that professional services are always gratuitous unless a special contract to pay for them is made, has long been abandoned. He observes (pp. 13 and 14): “But in our day the increase in the number of professional practitioners, and their exclusive devotion to a special class of services as a means of living, has essentially modified the practical character of the contracts with their patrons. Although in legal acceptation a mandate, yet from force of circumstances growing out of an altered state of society, the mandate is practically changed into a contract of hire (locatio operis). This doubtless reduces professions to the status of artisanship, and places them on a par with manual labor, conjoined to the special skill of a particular calling. But it also simplifies the contract, removes it from the category of innominate or imperfect obligations, requiring the[26] intervention of legal fictions to furnish a means for their enforcement, and brings it within the pale of consensual agreements based upon a sufficient consideration.”
The physician’s right to sue on contract in England was declared by legislative enactment by Chap. 90 (Sec. 31), 21 and 22 Victoria. It has never been denied in the United States. Adams v. Stephens, 26 Wend., 451-455.
Physicians’ and Surgeons’ Service in a Sense Voluntary.—Though it is true, as in the case of many other doctrines of ancient law which were formulated under social conditions far different from those which prevail in modern times, that these rules and theories have long since lost their potency as distinct rules governing actions at law, nevertheless the legal aspect of the peculiar relationship between physician and patient, is still affected by the idea that the service on the part of the physician is voluntary—that is, the physician or surgeon is not bound to come and perform services whenever or wherever he is called. He is at liberty to refuse any and every patient who attempts to employ him.
Patients may Cease Employing at Any Time, unless there is a Contract for a Certain Period.—And when he is employed, the patient may at any moment discharge him, without incurring liability in damages, unless a special contract has been entered into between them that the services shall be rendered for a fixed period.
Service once Begun by Physician must be Continued until Notice of Intention to Cease is Given by Him.—If, however, the services are begun, they must be continued until notice has been given of the intention to discontinue them, and a reasonable time allowed the patient to obtain the services of another person. The reasons for this rule will be considered more fully below.
Contracts either Express or Implied.—The contract between the physician and patient may be an express one, that is, one in which all the terms are agreed upon or expressed between the parties, or it may be what is called an implied contract, or one in which the patient, or another person, simply calls on the physician or surgeon to come and perform services, and neither party specifically stipulates or agrees upon any of the terms of the employment.
Express Contracts may Include any Stipulation Not Contrary to Public Policy.—In the case of an express contract the agreement of the parties settles and determines their mutual obligations, whether it be written or merely verbal. But an express contract may also be made in such a form that certain conditions are required to be performed by the physician before he becomes entitled to any compensation for his services. It may also embody an agreement that the patient shall pay certain sums at certain times as the treatment goes on, or that no other physicians shall be employed without the consent of the attending physician, or if so employed that they shall be under the direction of the attending physician.
Almost anything may be stipulated which is not contrary to public policy, and a breach of any such stipulation entitles the aggrieved party to rescind the contract and cease from performing it.[163]
Qualifications of the Rule that Express Contracts may Include any Stipulation.—Some qualifications of this rule of law must, however, be noted. A breach by the patient of any one of these stipulations would entitle the physician to treat the engagement as terminated like any other contractual relation, and to bring his action for a recovery for services rendered up to the time of the breach; but it is doubtful whether he would have any action for damages for failure to permit him to perform further services. This doubt arises from the legal doctrine, hereinbefore referred to, that a patient is always at liberty to dismiss his physician at any time without notice, and without assigning any cause, which recognizes and grows out of the fact that if the trust and confidence of the patient are destroyed, or impaired, no matter how unreasonably or unjustly, the relation between them must thereafter be unprofitable to both parties, and dangerous to the patient. On the other hand there is little doubt but that whenever an express contract is made by a physician to treat a patient for a certain length of time for a particular disease or injury, the physician is not at liberty to arbitrarily terminate that relation or his connection[28] with the case, unless he has in the contract specifically reserved the right so to do.
Contracts Making Payment Contingent upon Successful Treatment Valid.—The express contract between the parties may also contain a stipulation, by which the physician makes his compensation contingent upon his effecting a cure. Smith v. Hyde, 19 Vt., 54; Mack v. Kelly, 3 Ala., 387. See also Coughlin v. N. Y. Cen. R. R. Co., 71 N. Y., 443. In such a case, however, if the patient does not permit the physician opportunity to treat him during the time named in the contract, or for a reasonable time, if no specific time is fixed, the courts would probably permit the physician to recover a reasonable compensation for his services for the time during which he treated his patient.
Physician must Allow Reasonable Time to Supply his Place if he Quits his Patient.—In any event, whether the contract be express or implied, conditional or unconditional, the law through motives of public policy, and with a just regard for the welfare of the sick and injured, undoubtedly requires that if a physician has once taken charge of a case, and determines to abandon it, he must give the patient reasonable notice and reasonable opportunity to supply his place. If he fails to do this he is liable in damages for the results that follow as the proximate consequence of his abandoning the case.
This Rule True even in the Case of a Charity Patient.—This is true, it is believed, even when the patient is a charity patient, and the services are gratuitous. Shiels v. Blackburn (1 H. Blacks., 159). For any other rule less strict might entail the most serious consequences. Ordronaux, “Jur. of Med.,” 13 and 14, citing Inst., lib. 3, 26, 11; Pothier, “Du Contrat Mandat,” Chap. I., § 4.
Elements of the Contract Between Physician and Patient.
Duties of Physician.—When the relations between physician and patient are not defined otherwise by express contract, the implied contract is, and the law presumes, that the physician contracts, first, to use the necessary care and attention;[29] second, to use the necessary skill; third, in case the physician furnishes his own medicines (and the obligation to furnish them would probably be imposed, if it was the custom of the school or class of physicians to which the particular physician belonged to do so), that the medicines are proper and suitable. As a corollary of these duties it necessarily follows, also, that the physician contracts that the instruments or appliances which he uses are free from taint or contagion, and are suitable and proper for the uses to which they are put. Upon this theory an action could be maintained against a physician for using impure vaccine.
Duties of Patient.—The patient on his part contracts, first, to give the physician information concerning the facts and circumstances of the case, and full opportunity to treat him properly; second, to obey his instructions and follow his directions, and, third, to pay him the reasonable worth and value of his services. The different branches of this contract are reciprocal. The failure of either party to fulfil the obligation of any one of them which is imposed upon him, would bar him of his remedies against the other party to recover damages for any breach, or any proximate result of his breach, of such obligations. The necessary care and attention required of the physician in such a case are measured by the requirements of the case and the physician’s duties to his other patients, modified, however, by the rule that the physician is presumed to know, at the time he takes up the case, the condition and situation of his other patients at that time. Consequently, if those who have first employed him are so situated at the time that his services for them are likely to be soon and continuously required, he cannot without making himself liable in damages undertake another case and then neglect it, but he should either decline to take it, or should with the full knowledge and consent of the patient make provision for the temporary substitution of some other physician, during the time that his prior obligations engross his attention. Nevertheless, if the situation and condition of those to whom he has first contracted his services is such that he had, although he exercised due professional knowledge and skill, no reason to apprehend that these patients would need his exclusive service, and by a sudden development, arising from those occult causes which obtain in all serious diseases[30] and injuries, any of his prior patients suffer a sudden and dangerous relapse, or from an accession of new and dangerous symptoms and conditions so that he must fly to their aid, he would not be liable to another patient, to whom he had afterward contracted his services, for neglecting his case; still he should in such instances use extra means to obtain the services of some other and equally skilful man.
Only Ordinary and Usual Skill Required.—The degree and character of necessary skill contracted for has been variously defined by the courts. When malpractice is discussed, a more extended consideration of this matter will be required. At present the doctrine laid down in Shearman and Redfield on “Negligence,” paragraphs 433-435, may be adopted. It is as follows:
“Although a physician or surgeon may doubtless by express contract undertake to perform a cure absolutely, the law will not imply such a contract from the mere employment of a physician. A physician is not an insurer of a cure, and is not to be tried for the result of his remedies. His only contract is to treat the case with reasonable diligence and skill. If more than this is expected it must be expressly stipulated for.... The general rule, therefore, is, that a medical man, who attends for a fee, is liable for such want of ordinary care, diligence or skill on his part as leads to the injury of his patient. To render him liable, it is not enough that there has been a less degree of skill than some other medical man might have shown, or a less degree of care than even himself might have bestowed; nor is it enough that he himself acknowledged some degree of want of care; there must have been a want of competent and ordinary care and skill, and to such a degree as to have led to a bad result.... But a professed physician or surgeon is bound to use not only such skill as he has, but to have a reasonable degree of skill. The law will not countenance quackery; and although the law does not require the most thorough education or the largest experience, it does require that an uneducated, ignorant man shall not, under the pretence of being a well-qualified physician, attempt recklessly and blindly to administer medicines or perform surgical operations. If the practitioner, however, frankly informs his patient of his want of skill, or the patient is in some other way fully aware of it, the[31] latter cannot complain of the lack of that which he knew did not exist.”[164]
Average Standard of Skill of any Professed School must be Attained.—It is also a rule that one who professes to adhere to a particular school must come up to its average standard, and must be judged by its tests, and in the light of the present day. Thus a physician who would practise the reckless and indiscriminate bleeding which was in high repute not very many years ago, or should shut up a patient in fever and deny all cooling drinks, would doubtless find the old practice a poor excuse for his imbecility. So, if a professed homœopathist should violate all the canons of homœopathy, he would be bound to show some very good reasons for his conduct, if it was attended with injurious effects. Upon many points of medical and surgical practice all of the schools are agreed, and indeed common sense and universal experience prescribe some invariable rules, to violate which may generally be called gross negligence. Yet the patient cannot justly complain if he gets only that quality and kind of service for which he bargains. If he employs a cheap man, he must expect cheap service. Puffendorf, in his “Law of Nature and Nations,” observes: “We read a pleasant story of a man who had sore eyes and came to a horse-doctor for relief. The doctor anointed his eyes with the same ointment he used among his horses, upon which the man falls blind, and the cause is brought before the judge, who acquits the physician. For if the fellow, says he, had not been an ass he had never applied himself to a horse-doctor.” See also Jones on Bailments, 100; 1 Field’s “Lawyers’ Briefs,” sub. Bailments, Sec. 573; Musser v. Chase, 29 Ohio St., 577; Lanphier v. Phipos, 8 Carr. & Payne, 478.
Degree of Care and Skill Used a Question of Fact.—In[32] an action at law, whether brought by a physician to recover for his services, or by a patient to recover for malpractice or neglect, it is always a question of fact, to be determined by the jury under proper instructions as to the measure of care and skill required, whether or not the physician has in a given case used that degree of care and displayed that amount of skill which might reasonably be expected of a man of ordinary ability and professional skill. These same rules apply to the surgeon. He must possess and exercise that degree of knowledge and sense which the leading authorities have announced, as a result of their researches and experiments up to the time, or within a reasonable time before, the issue or question to be determined is made.[165]
Rule in Leading Case of Lanphier v. Phipos.—In the case of Lanphier v. Phipos, 8 C. & P., 478, already cited, Chief Justice Tyndall enunciated the rule as to the degree of skill required of a physician or surgeon, which has been followed by all the courts since then. He said: “Every person who enters into a learned profession undertakes to bring to the exercise of it a reasonable degree of care and skill. He does not, if he is an attorney, undertake at all events to gain the cause, nor does a surgeon undertake that he will perform a cure; nor does the latter undertake to use the highest possible degree of skill, as there may be persons of higher education and greater advantages than himself; but he undertakes to bring a fair, reasonable and competent degree of skill. And in an action against him by a patient, the question for the jury is whether the injury complained of must be referred to a want of proper degree of skill and care in the defendant, or not. Hence he is never presumed to engage for extraordinary skill, or for extraordinary diligence and care. As a general rule, he who undertakes for a reward to perform any work is bound to use a degree of diligence, attention and skill, adequate to the performance of his undertaking; that is, to do it according to the rules of the art; spondet peritiam artis. And the degree of skill arises in proportion to the value and delicacy of the operation. But he[33] is in no case required to have more than ordinary skill, for he does not engage for more.”
Physician Must Instruct Patient how to Care for Himself, etc.—A corollary of these rules is, that the physician must give proper instruction to his patient how to take care of himself, how to manage a diseased or injured member, when and how to take any medicines that may be prescribed, what diet to adopt, and that in case the physician fails to give these instructions he is liable for any injuries that result from this failure. Carpenter v. Blake, supra.
Patient Must Inform Physician Fully Concerning his Case—His Communications Privileged.—On the other hand, as we have already stated, the patient owes the duty to his physician of informing him fully of all the varied symptoms of his disease, or the circumstances attending his injury, and to freely and with due confidence answer all questions concerning his past history which would tend to throw any light upon his present condition. To battle with the occult forces which play so important a part in determining the course or consequences of disease, it is absolutely essential that the physician should know all that is possible to be known of the patient’s history, and of the history of the patient’s family. As we shall see later on, all such communications are, in most of the States of the Union and elsewhere, by statutory enactment made privileged, and without the consent of the patient the physician or surgeon is absolutely forbidden to divulge any communication or information which he receives in order to enable him to prescribe. This rule applies equally whether the physician or surgeon is acting for hire or is treating the person as a charity patient, and it has been extended by construction by the courts in some States, so as to include examinations made by jail physicians or other physicians sent by the prosecuting officials of the State to examine a prisoner, for purpose of giving evidence, but who allowed the prisoner to suppose that they were there simply to treat him in their professional capacity. People v. Murphy, 101 N. Y., 126. At the same time the courts have been careful to make an exception in the case of advice given for the purpose of enabling the person receiving the advice to commit a crime, and of any information received by the physicians while the persons asking for it were engaged in a criminal[34] attempt. All of these interesting questions will be examined and treated of at length hereafter.[166]
Conditions of Contract Between Physician and Patient Further Considered.—It has been observed that the contract between the physician and patient may be conditional or unconditional. By this it is meant that limitations upon the reciprocal obligations between them may be imposed, or extensions of such obligations made, by special agreement. The physician may contract to cure, and may make the cure a condition precedent to receiving any reward for his services or medicaments, and a breach of such a contract will be enforced by the courts as a bar to an action for services rendered or medicines furnished. The patient may agree to come to the physician’s home or to a hospital or other place agreed upon between them, for the purpose of being treated, or of being operated upon by a surgeon, and a failure to perform such an agreement on the part of the patient absolves the medical man from carrying out his agreement to treat the patient. In the case already suggested of a request by the medical man for information as to the patient’s past history, or that of the patient’s family, or the circumstances concerning the injury or symptoms of the disease, if the patient should give false information, or should wilfully neglect to give true information, the physician would have a right, upon giving reasonable and due notice, and opportunity to employ some one else, as already intimated, to decline to proceed further with his care of the case, and might sue and recover pay for the services rendered.
Physicians Cannot Contract that they shall Not be Responsible for Want of Ordinary Care and Skill.—An important and salutary exception to the general rule that all parties may contract freely as between themselves stipulations measuring their reciprocal obligations, doubtless applies to the relations between physician and patient. It is an exception which has been applied to the contract relations existing between a common carrier and a shipper or a passenger. This is that[35] persons contracting to perform services which are to a certain extent public in their nature, and which, as in the case of the common carrier or in the case of the physician or surgeon, are founded upon conventional relations, and affect the public welfare, are not permitted, from reasons of public policy, to contract for a release or escape from liability arising out of their own negligence or wrong. In short, a physician or surgeon cannot contract with a patient that the patient shall waive any claim for damages growing out of his want of ordinary care and skill. Nevertheless, the physician or surgeon may frankly inform his patient of his want of knowledge and experience as to the particular kind of treatment required by any special and unusual disease or injury. If after full information on this point, and full opportunity to employ some one else, the patient insists that the physician or surgeon go on with such treatment as he is able to give to the case, and injuries result which a more skilful and experienced practitioner might have avoided, it is probable that the courts would hold that the practitioner was not liable under such circumstances, or that such circumstances could be pleaded in mitigation of damages. But it would be the duty of the practitioner in such a case to be exceedingly careful in performing any surgical operations, and not administer any powerful drugs with the strength and medicinal qualities of which he was not acquainted. If he should assume to perform such operations or administer such drugs instead of confining himself to modifying the ravages of disease by the use of well-known simple remedies, or protecting against the consequences of severe injury by the use of ordinary antiseptic dressings and treatment, he would no doubt be liable for any resulting damage, and could not recover pay for his service.
Experiments Not to be Tried on Patients—This Rule Applies to Charity Patients.—For like reasons of public policy it has been held that a physician has no right to try experiments on his patient.[167] In this respect a charity patient will be protected by law and compensated for damages received from experiments on his health and person, just as much as a person from whom a large fee could be expected. Humanity and public policy both forbid that experiments should be tried upon one class of patients any more than another. However this[36] may be, in a case of extreme danger, where other resorts have failed and everything else done that could reasonably be required, and if the patient and his family consent after full information of the dangerous character of the operation, or the unknown qualities and powers of the drug to be administered, the practitioner would be justified and protected if some new methods of treatment not entirely developed or known to the profession, but supposed to be efficacious, should be adopted, although the result might prove unfavorable. In such a case, however, it would be extremely perilous for the physician to stand upon his own judgment alone. He should consult the best talent in his profession available, and abide by the judgment of his colleagues or a fair majority of them; and even then should apply to his course of action the maxim. When in doubt run no risks; better let a patient perish from disease or injury, than while attempting uncertain experiments with the surgeon’s knife or the use of dangerous drugs. The safe rule is to take no chances, unless there is a consensus of judgment of several physicians. It may be objected that if no experiments are tried no new medicines or surgical devices could be discovered, or their effects observed. The answer to this objection is that vivisection, and other experiments upon live animals, permit of experimentation to a considerable degree, and often effectually point out the proper course of treatment of the human subjects. In the case of drugs and medicines the practice is well known of physicians trying the effects thereof upon their own persons, in their zeal and anxiety to give to the world new discoveries. But, as heretofore observed, the law does not recognize the right of the medical or surgical practitioner to tamper with his patients’ health by the use of untried experiments, without imposing upon the practitioner liability for all injuries proximately resulting from their use. All of such matters will, however, fall more properly under consideration when the liability of the physician and surgeon for malpractice is considered.
CHAPTER IV.
OF THE LEGAL RIGHT OF PHYSICIANS AND SURGEONS TO RECOVER COMPENSATION FOR SERVICES.
Liability to Pay for Services.—An important matter for physicians and surgeons is the question as to who is responsible, or liable to pay for their services. If there is an express contract this question does not arise; but in most instances the person performing the services renders them upon call, and it is necessary for him to understand his legal right to recover pay for services in the absence of an express contract.
Person Treated, and not Person calling in Physician, Employs Him and is Liable.—In the first place, it must be stated as a general proposition that the person for whom the services are actually rendered, or upon whom the operation is performed, is bound to pay for them, if otherwise capable in law of making contracts and incurring obligations. And secondly, that one who calls a physician or surgeon to attend a patient is not presumed to have contracted to pay for the services rendered, unless his relations with the patient are such that he would be obligated in law to pay, even if he had not himself called in the medical man.
In the first case it is presumed that the patient is liable, because he receives the benefit of the services, and nothing less than a distinct understanding that he was not to pay will relieve him from this obligation.
Married Women and Infants Generally Not Liable.—Where such a person is a married woman, unless the case arises in States or countries where married women have been declared by statutes to be liable the same as if single, this rule does not obtain. Nor is an infant personally liable when he is living with his parent or guardian. Hull v. Connelly, 3 McCord (S. C.), 6; Klein v. La Amoreaux, 2 Paige Ch., 419; Atchinson v. Bruff, 50 Barb., 384; Wilcox v. Smith, 26 Barb., 341. But the contract of an infant for medicine and medical attendance is[38] deemed a contract for necessaries, and will be held valid and enforced against his estate if there is no person standing in loco parentis who can be held liable. 3 Barn. & Cress., 484; 2 Kent Com., 236. In cases when the parent of the infant or the husband of the married woman is liable, this liability obtains because the services rendered are deemed necessary, and fall within the common-law obligation of such persons to provide and pay for necessaries for those whom they are bound to support and maintain.
Burden upon Physicians Treating Minors to Show Services Necessary.—But even in such cases the burden is upon the person performing the services, to show that they were necessary, and it is his duty to know, or learn, the true legal status of the patient, and the true legal relations of the patient to the person other than the patient from whom payment is to be claimed. As said in the case of Crain v. Baudouin (55 N. Y., 256-261), “in the case of minor children even, the law imposes this duty upon those who would furnish them with necessaries, relying upon the credit of their fathers, and seeking to charge them. (Hunt v. Thompson, 3 Scam., 179; Van Valkinburgh v. Watson, 13 J. R., 480).” “A fortiori, it is so in the case of an adult married daughter living with her husband.” And as to the liability of the husband of a married woman in the absence of statute giving her legal capacity to contract and charge her separate estate. Consult Moody v. Osgood, 50 Barb., 628; Potter v. Virgil, 67 Barb., 578; Crain v. Baudouin, 55 N. Y., 256-261.
Mother of Infant probably Liable after Father’s Death.—It has been a much disputed question whether after the father’s death the mother becomes responsible for necessaries furnished for her minor children. The theory of law upon which a father is made liable proceeds upon the ground that he is bound to support the child and has a right to the child’s services during its minority.[168] It has been held that the mother after the death of the father is entitled to those services. Campbell v. Campbell, 3 Stock. (N. J.), 265; Cain v. Dewitt, 8 Iowa, 116; Furman v. Van Size, 56 N. Y., 435-439, disapproving Bentley v. Richtmeyer (4 Comstock, 38), and approving In re Ryder, 11 Paige, 185. If she is entitled to the services of her child,[39] she must be bound to support and care for it; and so it was held in Furman v. Van Size cited above.
Estates of Insane Persons Liable in a Proper Case.—Persons of unsound mind are liable for necessaries furnished for their benefit, and can be made to pay therefor at reasonable and proper rates, but they cannot make contracts for a specific rate. It is always a question of fact as to what sum should be charged against their estates, if they have any.
Master Not Liable for Services Rendered Servant without Special Contract.—In the case of master and servant, while at common law as between a master and servant the master was bound to provide medicine and food for the servant when the servant was an inmate of the master’s house, this is an obligation which a third person could not enforce, and the master can only be held liable for services rendered to the servant, upon proof of a specific contract with him to pay for them.
Case of Crain v. Baudouin Considered.—The case of Crain v. Baudouin, supra, affords an interesting discussion before the highest court of New York State, as to the question as to how far a father calling a physician for an adult child for whom he is not bound to provide, although lying sick at the father’s house, can be held liable for the services rendered upon such call. In that case the plaintiff attended as a physician upon the daughter of the defendant, who was sick at his house. The daughter was of full age, married and living with her husband, but was brought from that of her husband to that of her father in order that she might be under the care of her mother. Defendant was present when plaintiff made his calls, gave the latter a history of the patient’s illness, and received directions as to her treatment. He told others of the frequency and length of the plaintiff’s visits, and of his opinion of the case, without any disclaimer of liability. The Court held, however, that these facts were insufficient to imply a promise on the father’s part to pay for the services, and that the additional facts that the defendant consented to the calling in of a consulting physician, and that a bill was sent in by the plaintiff, unless acknowledged and acquiesced in by defendant, or that he had before this employed other physicians, were also insufficient to raise an implication of law of such a promise to pay. The plaintiff relied in his argument upon the fact that the patient was a daughter of the defendant, but the Court held that any presumption which might arise from this had the daughter been under age, was overcome by the fact that she was past a majority, and was married and lived with her husband and children. The plaintiff also relied to support his cause[40] of action upon the interest exhibited by the defendant in the course of treatment pursued, and the other facts as to the presence of the defendant when the plaintiff made his professional calls alone and in consultation; his receiving directions as to treatment; his recognition to others of the fact that the plaintiff was in attendance; his reciting to others a knowledge of the frequency and length of the visits of plaintiff without any disclaimer on the part of the defendant of liability. The Court said as to these facts: “It is true that particular acts will sometimes give rise to particular obligations, duties and liabilities. But the party whose acts are thus to affect him must be in such predicament as that those acts have, of legal necessity, a significance attached to them, at the time, which he may not afterward repel.... It has been held that a special request by a father to a physician to attend upon his son, then of full age but lying sick at the father’s house, raised no implied promise on the part of the father to pay for the services rendered.” See Boyd v. Sappington, 4 Watts (Pa.), 247; and so in Veitch v. Russell, 3 Ad. & Ell. (N. S.), 927, it is said: “A physician attends in every case on request; that fact alone is not enough for the inference of a special contract;” and see Sellen v. Norman, 4 Carr. & P., 284. Still less where there has been no special request by the father to the physician, and no more than acquiescence in his calls. As it would be unnatural for the parent of an invalid child, though legally emancipated, or for an intimate and confidential friend of hers, not to know the rise and course of her malady, not to be interested in the state of it as disclosed at any time to skilled inspection, not to be so anxious as to be in waiting when scientific skill was to be applied for its cure, not to be ready to receive directions for treatment in the intervals; so it is not to be implied in the one case more than in the other that, from these manifestations, because unaccompanied with an express repudiation of liability, a liability may be implied. They are to be referred to natural affection and friendly sympathy, rather than to an acquiescence in the rendition of a personal benefit, or counted as acts done under a sense of legal obligation.” The Court further said that “even if it should be assumed that the usage exists that the physician called to consult with him who is in attendance, with the consent of the person who has employed the latter, is in contemplation of law in the hire of that person, still the assent of the defendant to the calling in of the consulting physician, and his expression of desire to be present when he came—until he is shown to have employed the plaintiff—is a basis too weak for an implication of law, that he promised to pay his consultation fees. Still less it is a fact from which to imply a promise to pay the plaintiff.” This case is, however, close to the border line, and it may be well criticised and denied its apparent full weight of authority, notwithstanding the very great learning and ability of the learned Judge Folger, who wrote the opinion, upon the ground that it appears[41] that the father had as a witness expressly denied calling in the plaintiff or authorizing anybody to call him in, or authorizing the employment of a consulting physician, and that on the trial the Court had found upon the whole testimony in the case that the defendant had never employed the plaintiff. Taking the decision as a whole it cannot be regarded as determining that upon such a set of circumstances as is there disclosed, the father could not in any event have been held liable, but rather that the trial court having found upon the whole testimony that the defendant was not liable, having witnesses before it fully able to judge of their capability, the appellate court could not say as a matter of law that a finding in favor of the defendant should be overruled. This case is considered here at some length chiefly for the purpose of affording an illustration to physicians and surgeons which will suggest to them the advisability of care in ascertaining in all cases who is responsible for their charge for services. See also Bradley v. Dodge, 45 How Pr. (N.Y.), 57; Smith v. Riddick, 5 Jones (N. C.), 42.
Liability of Third Persons Calling a Physician—General Rule.
As to liability for services rendered, when the medical man is called by one person to attend another, it may be stated as a general rule that in order to create such a liability it must appear that the person calling either actually intended to become responsible, or acted in such a manner that the physician was led to suppose that he so intended.
Liability of Railway Company Calling Physician in Case of Accident to Employees, etc.—Another more troublesome question has arisen where physicians and surgeons have been called in by employees of a railway company in case of sudden accident or injury. In one case in New York, the Superior Court of New York City held, that although the general superintendent of a railroad company testified that he had general authority to hire and discharge men, and that he had employed a physician, the railroad company was not liable.[169]
This doctrine seems to be opposed to the weight of authority. See cases collated in Vol. 18, “Am. and Eng. Cyclopædia of Law,” p. 434 et seq., some of which are: Toledo, etc., R. R. Co. v. Rodrigues, 47 Ill., 188; Same v. Prince, 50 Ill., 26; Indianapolis, etc., R. R. v. Morris, 67[42] Ill., 295; Cairo, etc., R. R. Co. v. Mahoney, 82 Ill., 73; Atchison, etc., R. R. v. Beecher, 24 Kansas, 228.
Same Rule does Not Prevail in United States in Case of Accidents to Passengers.—The cases just noted were all cases of employees. In the cases of injured passengers it has been doubted whether the same rule applied, some State courts holding that in that case there is no obligation to furnish medical and surgical attendance, but that the physician attending must look to the persons whom they attended. Union Pacific R. R. Co. v. Beatty, 35 Kansas, 265; Brown v. Missouri, 67 Missouri, 122.
Different in England.—In England a different rule prevails—one more humane and in consonance with the moral obligation imposed by the relationship of the parties. In Walker v. The Great Western R. R. Co., a recent case (Law Reports, 2 Exch., 228), Chief-Justice Kelley, in the course of the argument, made this remark: “Must a board be convened before a man who has his legs broken can have medical attendance?”
But in Cox v. The Midland Counties R. R. Co. (3 Wellsby, H. & G., 268), the station master, employed as the chief officer of the passenger and other departments, called in a surgeon to perform an operation upon a passenger injured by a train. The road was held not liable.
On the other hand, in Langan v. Great Western R. R. Co. (30 Law Times, N. S., 173), a sub-inspector of railway police was held to have implied power to employ a surgeon for an injured employee. But in Arkansas an attorney for a railroad company was held not authorized to do so. St. Louis, etc., R. R. Co. v. Hoover, 53 Ark., 377.
Doctrine in Indiana the More Sensible One.—The more sensible doctrine seems to be established in this country, in the State of Indiana at least, in the case of Terre Haute R. R. Co. v. McMurray (98 Ind., 358), in which the Court held that where there was great necessity for the employment of a surgeon, the conductor of a train has authority to employ the surgeon, if the conductor is the highest officer in rank on the ground at the time. But in that case the Court expressly states that this liability grows out of the exigencies of the case; not out of any theory of general authority.
Authority of Railroad Physician to Employ Nurses, etc., Doubtful.—It has also been disputed whether the authority of the company’s physician extended far enough to render the company liable for services performed by nurses employed by him, or for board and lodging engaged by him for injured employees. In Bingham v. Chicago, etc., R. R. Co. (79 Iowa, 534), it was held that the authority was sufficient, but in that case testimony appeared tending to show that an agent of the company who had authority to employ the physician had authorized him to employ two nurses. The converse doctrine—namely, that the fact that a physician of the company was authorized to buy medicines[43] on the credit of the company does not authorize the inference that he has power to render the company liable by a contract for board and nursing of a person injured on the company’s road—was held in Maber v. The Chicago, etc., R. R. Co., 75 Missouri, 495; Brown v. The Missouri R. R., 67 Missouri, 122. To the same effect, see Louisville, etc., R. R. Co. v. McVeigh, 98 Ind., 391; Cooper v. N. Y. C. & C., 6 Hun, 276; and St. Louis, etc., R. R. Co. v. Hoover, 53 Arkansas, 377. 2 Redfield on Railways, 114:
On the other hand, where a physician and surgeon has been duly employed by a sub-officer or servant of the railroad company, ratification of this employment, by those having authority to employ him and to render the company liable, will be inferred from slight circumstances.
Such was the case of Louisville R. R. Co. v. McVeigh, which has been cited.
And in another case where information of the fact of the employment had been conveyed to the company’s general manager, and he had neglected and omitted to repudiate the employment or to terminate it, and the surgeon went on and performed services, it was held that from these facts a ratification will be inferred. Indianapolis R. R. Co. v. Morris, supra. See also Toledo, etc., R. R. Co. v. Rodrigues, supra; Same v. Prince, supra; Terre Haute, etc., R. R. Co. v. Stockwell, 118 Ind., 98.
Presentation and Retention of Doctor’s Bill Raises No Presumption of Liability.—The presentation of a bill to a person containing charges against him for services rendered another person, and his retention of that bill without disclaimer of liability, does not raise a presumption of liability, for it is not necessarily an account stated. To constitute an account stated, there must be not only a statement of account, but acquiescence in it; mere retention of the account is not sufficient.
Bills Presented Not Conclusive as to Amounts Charged.—On the other hand, if a bill is presented which contains charges which are not acquiesced in, the person making out and presenting the bill is not absolutely bound by the charges therein contained, although such a bill affords some evidence as to the value of the services rendered.[170]
Claims Against Estates of Deceased Persons.—A bill for a physician’s services constitutes a claim against the estate of[44] a deceased person, like any other debt. In some States it is a preferred claim.[171] In this connection it should be observed that short statutes of limitation exist in most countries and States applicable to such cases, shorter than the ordinary limitation imposed by law upon the right to sue upon claims for services rendered (which is six years). In order to preserve his legal rights, the physician should as soon as possible after the death of the person for whom his services have been rendered, ascertain who is the administrator or executor of the estate of such person, and file with such representative, personally, proof of his claim.
Patient who Receives Benefit of Services of Consulting Physician Liable.—The liability of a patient for the services of a consulting physician is generally governed by the same rules as his liability to the physician in immediate charge of the case.[172]
Where the patient accepts the services of a consulting physician, although he has not directly requested them, he must pay for them if he receives the benefit of them without objecting, because it will be presumed that he ratified the act of the physician who was in charge of the case, in calling the other physician into consultation.[173]
But, however this may be, it is a principle of professional ethics, which has almost acquired the authority of legal doctrine, that a physician in charge of a case should obtain the full assent of a patient, or of his family and friends, if he is too ill to give his own consent, to the calling of another physician in consultation.
No Other Stranger can be Called into Sick-Room without Assent of Patient.—A limitation upon the authority and right of an attending physician is, that if he desires or attempts to call in a stranger not a physician, he must obtain his patient’s[45] consent. The obligation of a physician toward his patient of secrecy and confidence is regarded as very strict, and if a physician should call in a student or other stranger, without first consulting his patient, or those who are in some measure related to him and connected with him, it would be a very severe stretch of morals and possibly of law. In fact, in a recent case in Michigan, a physician was held liable for damages who called in a stranger, an unmarried man, who was an unprofessional man, to be with him while he was in attendance on a confinement case. In that case both the physician and the person so called in, and who was present at that time, were held liable in damages; and it was further held that the right to recover was not affected by the fact that the patient supposed that the person so called in was a medical man, and therefore submitted to his presence without objection.[174]
The statutes which create the privilege as to professional communications and information necessary to enable the physician to prescribe, might not apply to students or other strangers, and this is probably the reason for the rule of law laid down in the Michigan case. The obligation to preserve inviolate a communication as a privileged communication, including in the meaning of the word “communication” all knowledge or information received while in attendance upon a case, would be held to have been broken by the act of the physician in bringing in a stranger who would not be privileged from testifying.
Measure of Recovery for Services Rendered.
Terms of Express Contract Govern—Reasonable Worth the Rule in Implied Contracts.—In case of an express contract its terms necessarily measure the amount of the charges. In the absence of an express contract fixing the value of the services to be rendered, the measure of damages for breach of payment is like that in any other case of personal services, the reasonable worth and value of the services performed. So likewise if medicines or appliances are furnished, which are not reasonably to be expected and furnished, according to the custom of the school to which the physician or surgeon belongs,[46] the reasonable worth and value at the time of furnishing them, and at the place of furnishing them, is the measure fixed by the law to determine what shall be recovered for them.[175]
Value—How Proved.—When the medical man is compelled to go into court to enforce payment for his services, it has been questioned whether he can testify to the services rendered, and the facts and circumstances surrounding the patient at the time of the treatment, because it has been claimed that he could not do so without violating the statute against the disclosure by physicians of information received which is necessary to enable them to prescribe. The tendency of the later decisions, however, seems to be that the breach of the patient’s contract to pay relieves the physician from his obligation of secrecy, and consequently, that if it is necessary for him to go into court and prove the value of his services, he may testify, within reasonable limitations, to all matters necessary to inform the court fully as to the nature and extent of the disease or injuries of the patient, in order that he may show the responsibility imposed upon him and the extent of the services that he has rendered. This subject will be fully considered under the head of “Privileged Communications.” The usual course of practice where there is not an express contract fixing the charges, is to prove the facts and circumstances showing the treatment and services, and then to produce other physicians who, in answer to a hypothetical question stating the facts and circumstances in the case, assuming them as true, are allowed, if they state they know the value of such services, to give an expert opinion as to what that value is.[176] It has also been said (Ordronaux, “Jurisprudence of Medicine,” § 43), that if a fee-bill of charges for such services has been established by an association of physicians recognized by law, such as a county medical society or a State medical society, incorporated pursuant to statute, such fee-bill can, if properly authenticated as having been adopted by the association, be offered in evidence on behalf of the patient and against the physician. But such a fee-bill in such a case would not be held to be conclusive[47] evidence of the value of the services, but will be received in evidence, if at all, merely for the purpose of showing what was the usual and ordinary charge in such cases. As we shall see later on, under “Malpractice,” a judgment for services rendered, however small, is a bar to an action of malpractice, because a judgment for the value of the services rendered involves proof on the part of the plaintiff, and a finding on the part of the court, that the services had value and were skilfully performed and properly rendered.[177]
Custom of Physicians to Treat Each Other Gratis, Enforceable.—Physicians frequently treat each other, and it has been held, where the custom exists to do so without charge, that such a custom is binding. Of course, this rule does not prevent physicians from making an express contract to waive the custom and agreeing that the services be compensated.
Elements to be Proved in an Action for Service, etc.—General Advice.—The result of these rules may be thus summarized, viz.: The elements to be established in an action for services by a physician against a patient are three in number—(1) the employment; (2) the performance of the services;[178] and[48] (3) the value of the services, that value being either a fixed value determined by the terms of the contract between the parties, or the reasonable worth and value of the services determined by evidence of experts upon that subject. It is, therefore, important that physicians and surgeons should be advised, when entering upon the practice of their profession, to keep a record of their transactions and of their business generally. Because, if they are compelled to go into court to recover for their services, they will be called upon to describe with minuteness the character and extent of the services they have performed in order that the value thereof may be correctly ascertained and determined in the suit. Any person in active practice who is not blessed with a most tenacious and particular memory is liable to forget a great many details which, with a record in hand, properly kept, could be brought to his memory and be testified to with absolute truthfulness and conviction. And the record itself, when properly shown to be a book of original entry, is generally receivable in evidence, as a memorandum of the transaction.[179]
CHAPTER V.
OF THE PRIVILEGES AND DUTIES OF PHYSICIANS AND SURGEONS WHEN SUMMONED AS EXPERT WITNESSES IN COURTS OF JUSTICE.[180]
Introductory—Distinction Between Expert Witnesses and Other Witnesses.—One of the most important positions that a medical man is called upon to assume by virtue of his professional character, is the position of expert witness. Most writers on medical jurisprudence confine themselves, in the discussion of this subject, to presenting the medico-legal rules which appertain to this position, and concede its high importance. Before defining what is meant by the term expert witness, or treating of the rules which determine the status of such witnesses in court, and their duties, it seems advisable to introduce the subject by a brief consideration of the distinction between ordinary witnesses and expert witnesses. When medicine and law are united in the purpose of investigating facts, and bringing about a legal determination as to what are or are not facts, they co-operate with each other in this way. The law furnishes the machinery for the inquiry and the rules which determine how it shall be prosecuted. The medical man, however, is called upon as an assistant to the law, because of his skill and experience in his profession, which enable him to ascertain and interpret the circumstances from which the facts sought to be established are to be inferred. Ordinary witnesses testify concerning matters of observation, the court and jury being endowed with the sole power to determine the credibility of their evidence and the true result of their observations. Yet the border line of distinction between witnesses who testify merely to actual matters of observation, and those who give their[50] opinions upon and draw inferences from established facts and circumstances, is a wavering one. The general rule of evidence is well understood, that hearsay evidence is inadmissible, and yet, like any other rule, this has its exceptions which grow out of the necessities of given cases. This is so because there are and always will be, matters brought before courts for investigation and determination, long after the witnesses who personally saw the facts and circumstances of the particular case in which such matters are concerned have died, or have withdrawn beyond the reach of the process of the court. Possibly no record in writing of such facts and circumstances has been left, or if in writing it lacks the sanctity of being a judicial writing, and hence is no better evidence than any other form of hearsay evidence. For this reason in matters of family history, pedigree, custom, and the like, hearsay evidence is permitted, and is entitled to as much weight as any other evidence, if the witnesses giving it be trustworthy.
In Matters of Common Experience Witnesses in General Often State Conclusions.—Moreover, in matters of common experience, the testimony of any witness, if carefully analyzed, often shows that he is sometimes allowed to draw, and state, his conclusions and inferences, instead of being required to confine his evidence simply to telling in the strictest possible way, and with the closest limitations, what he actually witnessed. A good illustration of this is the case of a person who sees a crime of homicide committed by shooting, and is called upon to testify in court. He would be allowed to testify that the defendant, if he could identify the prisoner at the bar as such, was the person whom he saw fire the shot, although he might not have examined him with close scrutiny, and might never have seen him before the crime. In saying that the defendant was the person who fired the shot, while he would be in terms testifying to a fact, he would still be drawing an inference, and giving an opinion, based upon his recollection of the person whom he saw engaged in the act of firing, and of the likeness or resemblance of such person to the prisoner at the bar, which would be a matter of comparison and of opinion. So, too, although he could not see the bullet take its course from the mouth of the gun and imbed itself in the body of the deceased, yet if he saw the firing, heard the explosion, saw the[51] flash and smoke of the powder, observed the direction in which the accused pointed the weapon, and saw the deceased stagger and fall, he would be allowed to testify in answer to a direct question whether or not the accused shot the deceased. And, yet in making up that answer he would be testifying not simply to a matter of actual observation, but to a conclusion. As it is in reference to the question of identity so it is as to many other matters which come before our courts, in all of which the witnesses are permitted, without objection, to testify to conclusions and to give answers which are the result of inferences which they draw themselves, rather than a statement of their actual observations. The law is not a metaphysical but a practical science, limited and confined by the practical restrictions which experience has shown must be put upon it, in order to enable it to accomplish its object of administering justice between man and man. Men form such conclusions as have been indicated, instinctively and unconsciously, and it would be practicably impossible for them to narrate any occurrence without embodying in their narration some of these natural and unconscious conclusions. The law, therefore, includes among the matters which witnesses are permitted to characterize as facts, those daily and hourly inferences and deductions which all men are accustomed to make, and concerning which no two men who are properly constituted can greatly differ. It is true that this practice sometimes leads to error, but it has grown out of necessity. The greatest safeguard is, that upon the trial of a question of fact both sides are represented by counsel, and the opportunity which cross-examination offers to an advocate of even reasonable and ordinary skill is such, that these conclusions and inferences may be sifted down through the chain of observation, and the process of drawing these conclusions and inferences from a series of facts, tested in such a manner that the improbability, probability, or truth of any given inference or conclusion may be determined with substantial accuracy. The illustrations which have been given above exhibit the simplest form in which so-called direct testimony can be demonstrated to be not always positive and direct testimony, but somewhat a matter of inference. Other examples and illustrations of common occurrence will exhibit still more closely the line between actuality and opinion. At times it[52] becomes essential to the determination of a question, that the courts should know whether or not a person was angry, whether or not he was intoxicated, or whether or not at a given time, when his mental status was under observation, he acted rationally or irrationally. Lay witnesses have for many years been permitted to testify from observation, and without possessing any special qualification to do so, as to the existence or non-existence of such conditions as those just mentioned in a person whose actions are under consideration. It is manifest that in making any such inferences the witnesses’ testimony is mainly a conclusion based on inference. Take the case of anger. How shall that be determined? It is difficult to describe anger. A loud voice, a flushed face, the use of bitter words, nervous, excitable, demonstrative action—all these symptoms might occur, or but few of them might occur. So, too, in the matter of intoxication. It is well known that some individuals exhibit the effects of intoxicants in an entirely different manner and degree from others. Some men who are very much intoxicated, so as to be quite incapable, in the eye of the law, of forming a criminal intent, or of contracting an obligation which would be valid, may still be able to walk perfectly straight, or to talk without much confusion. Others, whose walk and demeanor would indicate a considerable degree of intoxication, might be mentally clear and unruffled and even stimulated by intoxicants to precise mental co-ordination and reasoning. Again, there are persons, as to whom a witness, after stating that he had observed them, and after stating the particular matters and things in which such persons were engaged, might with apparent accuracy state that they acted rationally or irrationally, and yet such persons might nevertheless, upon further examination, be found to have been acting according to a particular custom or habit, or idiosyncrasy of long years’ standing. Thus it is apparent that in each of these cases, when the witness attempts to state what, out of necessity, the court treats as a fact—viz., whether a given person is or is not angry, or intoxicated, or irrational—the witness is really testifying to the result, in his own mind, of his observations of the condition and conduct of the person who is under investigation, when compared with a standard which the witness has erected for himself. Hence such results are really[53] matters of opinion evidence, pure and simple. Other examples of a like character are found in statements as to weight, height, distance, speed, and the like, as to which men of common powers of observation, who are not strictly experts, are, because of convenience and necessity and the probability of reasonable and ordinary accuracy, commonly permitted to give their own judgment and conclusions as evidence.
All Witnesses Often Permitted to Draw and State Conclusions in Matters involving Numerous and Complicated Details.—Thus the practical necessity of the administration of justice has led to the establishment of the rule, that where the details of an occurrence are numerous and complicated, and are incapable of precise description by ordinary observers, witnesses are permitted to use, in testifying, general expressions which really embody their conclusions from the facts or details observed by them. Greenleaf on Evidence, Section 440, note A; Wharton on Evidence, Section 434.
Wharton says that “the distinction between expert witnesses and ordinary witnesses is this: the non-expert witness testifies to conclusions which may be verified by the adjudicating tribunal; the expert, to conclusions which cannot be so verified. The non-expert gives the results of a process of reasoning familiar to every-day life; the expert gives the results of a process of reasoning which can be determined only by special scientists.” See also People v. Fernandez, 35 N.Y., 49. People v. Deacons, 109 N.Y., 374-382.
This learned writer (Wharton) also says, at Section 437 of the same treatise:
“Where conclusions depend upon facts whose evidential weight can only be determined by those familiar with a particular specialty, then these conclusions may be given by experts in such specialty.” Such also is the exact derivative meaning of the word expert, it being derived from the Latin word “expertus,” meaning, literally, “experienced,” and hence skilled by experience.
Functions of an Expert Witness Essentially Judicial.—It is the function of an expert witness to reason about facts, to explain their connection with one another, and to draw conclusions and inferences from them. Hence, a witness, however expert in any ordinary sense in his specialty, when he is called[54] upon merely to narrate facts which he has observed, is an ordinary witness, and is governed by the same rules which apply to the ordinary witnesses. When, however, he is called upon, in addition to recounting facts, to explain or interpret them by reference to assumed facts, he becomes properly an expert witness. It thus appears that an expert witness must necessarily perform a part of the duties which devolve upon the court or the jury. His position is, therefore, essentially judicial, except that he has no power to enforce his determinations by judicial process. The importance and responsibility which the law thus confers upon an expert are of the highest character. He ranks the coequal with the tribunal itself in his peculiar province, so far as relates to his individual responsibility. That this should tend to elevate such witnesses to a high social position, and ought to require the most exact and faithful integrity of purpose and statement, is self-evident.
Difference Between Status of Expert Witnesses in France and Germany and in the United States and England.—In some foreign countries, notably in Germany and in France, experts in medico-legal matters have an assured official position, and are generally not allowed to be selected at hap-hazard according to the will or the length of the purse of those who need their services. The consequence of this method of obtaining expert evidence is, that expert witnesses in those countries command a high measure of respect and honor.
Unfortunately, however, in this country, where the opposite practice prevails, the weaknesses of human nature are such that the common people, newspapers, lawyers, and even the courts in some recorded opinions and decisions, have come to express a great want of confidence in the weight and value of expert testimony. This deplorable result of a bad system of procedure is universally recognized, yet our State legislatures have as yet refrained from attempting to correct it.
Hence, in considering the value of expert testimony in matters of medical jurisprudence, it must be conceded, in the first instance, that the difference between the system prevailing in this country and in England, and that which prevails on the Continent, notably in Germany and France, has not tended to raise but to depress the value of such testimony in the first-named countries. In the latter countries, the experts upon[55] medico-legal questions are officers of the court, or are treated as such. They form, in a sense, a part of the judicial system, and the expression of their opinions consequently carries with it great weight. Moreover, under the system which prevails there, it has been possible for men to be educated up to a high degree of skill and experience in the particular branches of physiological or psychological or physical investigations which they pursue, while here in America, and to a certain extent also in England, experts are such for other reasons, and by the operations of other causes, than the fact of their permanent employment in that capacity. As a general thing they become skilled in their profession or in the particular branches of it in which they practise as specialists, and are summoned to testify simply because they are selected by one party or another to a lawsuit.
Mr. Wharton’s View of this Question in the Main Hostile to the Prevailing System Here.—The effect of the methods which thus prevail has not been entirely to the advantage of the medical profession or of our courts. Wharton, in his work on “Evidence,” Section 454, observes upon this point: “When expert testimony was first introduced it was regarded with great respect. An expert was viewed as the representative of a science of which he was a professor, giving impartially its conclusions. Two conditions have combined to produce a material change in this relation. In the first place it has been discovered that no expert, no matter how learned and incorrupt, speaks for his science as a whole. Few specialties are so small as not to be torn by factions, and often the smaller the specialty the bitterer and more inflaming and distorting are the animosities by which these factions are possessed. Particularly is this the case in matters psychological, in which there is no hypothesis so monstrous that an expert cannot be found to swear to it on the stand, and to defend it with vehemence. ‘Nihil tam absurdo,’ which being literally translated means that there is nothing so absurd that the philosophers won’t say it! In the second place, the retaining of experts by a fee proportioned to the importance of their testimony is now as customary as is the retaining of lawyers. No court would take as testimony the sworn statement of the law given by counsel retained on a particular side, for the reason that the most high-minded[56] men are so swayed by an employment of this kind as to lose the power of impartial judgment; and so intense is this conviction that in every civilized community the retention by a judge of presents from suitors visits him not only with disqualification but disgrace. Hence it is that, apart from the partisan character of their opinions, their utterances, now that they have as a class become the retained agents of the parties, have lost all judicial authority and are entitled only to the weight which sound and consistent criticism will award to the testimony itself. In making this criticism a large allowance must be made for the bias necessarily belonging to men retained to advocate a cause, who speak not as to fact but as to opinion, and who are selected, on all moot questions, either from their prior advocacy of them or from their readiness to adopt the opinion to be proved. In this sense we may adopt the strong language of Lord Kenyon, that skilled witnesses come with such a bias on their minds to support the cause in which they are embarked, that hardly any weight should be given to their evidence.”
This author then proceeds to show that under the civil law system the conclusions of experts were formerly treated as unassailable facts, but under the English and American common law system this is not the case, but their testimony is to be weighed by the court. He says: “The grounds on which the conclusion is reached may be asked for: the expert’s capacity for drawing conclusions, as well as his premises, may be assailed. Cases of conflict are to be determined, not by the number of witnesses, but by the weight of their testimony, and though the opinion of an expert of high character may be entitled to great respect, yet if questioned, its authority must ultimately rest upon the truth, material and formal, of the reasoning on which it depends.”
Judge Davis, of the Supreme Court of Maine, in Neil’s case (cited in Wharton and Stille’s “Medical Jurisprudence,” Vol. I., Section 294), said: “If there is any kind of testimony that is not only of no value, but even worse than that, it is in my judgment that of medical experts. They may be able to state the diagnosis of a disease more learnedly, but upon the question whether it had at a given time reached a stage that the subject of it was incapable of making a contract, or irresponsible for his acts, the opinions of his neighbors, of men of[57] good common sense, would be worth more than that of all the experts in the country.”
Such stinging criticisms as these, and others which might be cited, of a like character, may not be always merited. It is certain that medical experts’ opinions, if fully enlightened by scientific research and free from partisan bias, ought to occupy a position like that of judicial opinions in weight and decisiveness upon the questions submitted to them. Such was the position occupied in the public estimation, and in that of judges and counsel, by the great Dr. Caspar in Germany, and Foedere or Pinel, and others since their time, in France. But this position was acquired chiefly because of the fact already mentioned, that under the system of administration of justice which prevails in those countries these great men were regarded, and acted, as a component part of the judicial system. They were called in as officers of the law to assist the court in forming a judgment, and determining disputed questions of fact, in cases involving life and death, or the devolution of property, where scientific experience, knowledge and skill, not possessed by judges or by counsel, was necessary for the determination of the questions involved. The root of the evil in America is, as already pointed out, to be found in the system which allows parties to retain and pay their own experts without any substantial restrictions. Sooner or later, among the other reforms in our judicial system, it will be found necessary to reform this evil by the enactment of laws requiring that the witnesses in medico-legal cases, particularly those in which a crime is alleged to have been committed, shall be designated by the court, or by some public authority, and paid from the public treasury instead of by the parties. Such experts would then occupy their proper position of special counsel, advising and assisting the legal counsel and the court, but they would not be taken out of this sphere and put in the utterly inconsistent one of witnesses. Their status and their duties would be as clearly distinguished from that of expert witnesses as now known, as the status and duty of the lawyer are from the status and duty of the judge. The present system has been said to be very much like putting a lawyer, who has just argued his client’s case, on the bench to decide it. Whether experts should be appointed as permanent government officials, like our judges, or should be selected[58] specially for each case like juries, referees, or arbitrators, and in the latter event whether they should be nominated by the parties and selected by the court from such nominees, or otherwise, are all questions of detail.
Our judges and lawyers seem slow to recognize the fact that the duties of experts are judicial, or at least quasi-judicial; to pass upon certain facts which neither the court nor the jury can understand without their aid. But, as we have seen from the citations just given, judges and lawyers have fully recognized the unreliability of expert testimony, produced as it now is in England and in this country at the whim and selection of the parties and paid for, much or little, according to the means of the parties.[181]
Method of Preliminary Examination of Experts—On Medical Questions a Licensed Physician Presumed Competent.—As the system exists here, the only power that the court has over the selection of an expert, is to determine, in advance of his testimony and of the elucidation of his opinions, whether or not he is competent as an expert. But this power affords little or no check or restriction, because in the effort to get all the light that is possible upon the questions under consideration, and to avoid unduly interfering with counsel in the conduct of the case at bar, the practice has become universal, and is recognized in the decisions and text writers, of permitting any medical man who has a license to practise his profession, to testify as an expert, and to give his opinion as such on any question cognate to his profession. This is so without regard to the amount of study and experience he may have had in the particular matter under consideration. The naked fact that he is licensed to practise is enough. He then—that is, after testifying that he is a practising physician—is clothed with the garment of authority. The only way in which his knowledge can[59] be tested is by cross-examination as to his experience and skill, and possibly by contrasting him as he appears upon the witness-stand and his history as he gives it, with other and more or less experienced and skilful men who follow him.
The rule is, that when a witness is produced to give an opinion on a medical question, he is interrogated by the counsel who produces him as to his qualifications. At this point, before he is allowed to give his opinion, it is proper and customary that the counsel upon the other side of the case should be allowed an opportunity to cross-examine as to his competency, and then the court determines whether or not he is a competent witness. If the court pronounces him competent, a hypothetical question is put to him stating the facts of the case, as the counsel interrogating him claims them to be established by the evidence, and the expert is then asked to give his opinion on the question at issue, based upon an assumption that the facts stated are truly stated. Then the opposing counsel has the right to cross-examine, and to ask his views and opinions upon the same question at issue, but assuming as true other and different facts or premises, as he claims them to be established by the evidence. This often involves a test of wit and intelligence, and of forensic acumen, between the counsel and the witness, which serves very little useful purpose, except perhaps to elucidate more strongly than has been here stated the defects of the system which now obtains. It is also not unusual, and in fact is the result of the workings of human nature, that under the manipulations of counsel skilled in cross-examination, skilled in methods of indirection in stating facts, and armed with the powerful weapon of the rule which permits them to insist upon a categorical yes-or-no answer to a question, the jury and the court become confused, the witness loses his temper, or becomes affected more strongly than ever before by bias against his persecutors, as he feels them to be, and the examination ends in a farce. This is not always the case, and the illustration given is an extreme one. Like the citations from judicial criticism of expert testimony which have been given, these matters are only adverted to here as danger signals, a warning to both professions, and with an earnest suggestion of the necessity of reform.
EXPERTS, HOW SUMMONED INTO COURT.
They Must Obey the Summons and Appear and be Sworn. In General they need Not Give their Opinions unless Duly Compensated.—An expert witness is brought into court like an ordinary witness by the usual process of the court. This process is, under the American system, an ordinary subpœna, and, being process of the court, whether or not he has been paid or promised compensation for giving his opinion he must obey the process to the extent at least of appearing in court when called, to be sworn. Interesting questions have been raised as to his obedience to the subpœna to the extent of testifying when he has not been compensated. It has been argued, and the argument is sustained by the decisions of courts of high authority in some States, that his knowledge and skill, acquired by study and by experience, is his property, of which he cannot be deprived without just compensation, under his constitutional rights guaranteed to him by the organic law of this country. On the other hand, in some other States it has been held that he is so far a necessary part of the judicial system that he may be called upon to give the results of his experience, knowledge, and skill forming his opinion, without payment other than the ordinary compensation to witnesses. It is believed, however, that the better opinion is the former; that he does not stand on the same footing as an ordinary witness, whose province it is to testify solely to matters of observation of fact, but that he stands in the position of one who has something to give; something to impart in the way of knowledge or experience, which is his property as much as any other thing movable or immovable of which he is possessed.
A somewhat different question has arisen in the case of a witness who, like a family physician or attending physician, has learned facts and has been paid for his attendance, or who exacts payment for his attendance, as a physician from his patient, and this question is; when such a professional man has been called upon to testify to the information he thus attained, whether he can be asked for, and required to give, opinions based on those facts? Necessarily, having learned the facts by observation, such as the appearance, symptoms, and actions of[61] the patient, he is, when testifying as to these matters, nothing more or less than an ordinary witness, because he is testifying to matters of observation. As to these matters public policy requires, except so far as it has been modified, or rather extended, by our statutes which forbid testimony as to privileged communications, that he must testify, the same as any other witness. But suppose that, having so testified to the facts, he is asked to give his opinion; for example, in an insanity case, whether the symptoms that he found in his patient led him to the belief as a professional man of experience and skill that his patient was sane or insane. The question is, Can he be compelled to give that opinion, if he chooses to decline to give it without the promise or assurance of further compensation than the mere per diem fee and mileage of an ordinary witness? The best authority is to the effect that he must so testify, the reasoning of the court being that his opinion is only a part of what he derived from his original relation of physician to his patient. Wright v. The People, 112 Ill., 540; same case, 33 Alb. L. J., 79.
Same Rule in Civil and Criminal Cases.—The rule is the same whether the professional man is called to testify as an expert in civil or criminal cases. In either one he is not obliged to give an opinion as such, independent of a personal knowledge of the facts in the case, without being paid or assured reasonable compensation therefor. His proper course of conduct is, when he has obeyed the subpœna and is in the presence of the court and has been sworn, and the questions put by counsel disclose that the object of his examination is to elicit from him an opinion, to state to the court that he has not been paid any other compensation than that of an ordinary witness, and that he respectfully declines to give an opinion in the case as an expert, without compensation proportionate to the value of his opinion.[182]
Whether Witness Competent a Question for Court in Limine.—After the expert is placed upon the stand, as we have seen, the counsel upon the side of the case by which he is summoned interrogates him as to his capacity, the purpose of the interrogation being that his answers shall qualify him and show him to be an expert. Whether or not he is an expert so as to permit the giving of his opinion as part of the case to go to the jury, is for the court to decide in limine, that is, at the threshold, and as a matter of discretion, and the exercise of that discretion, if fair and reasonable, will not be disturbed upon appeal by the higher court. It is permissible, but also discretionary, after the counsel calls the witness and has apparently qualified him, for the counsel upon the other side to cross-examine the witness as to his qualifications before he is examined in chief, with a view of determining whether or not there are limitations upon those qualifications which should prevent the court from permitting him to testify as an expert. The general rule is as stated by Greenleaf in his work on Evidence, Sec. 440, that it is not necessary that the medical expert should have actually practised his profession. Nor is it essential that the witness should belong to any particular school of medicine. The law does not undertake to pass upon conflicting theories of medical practice, in determining the question of the qualification of a medical expert. It is proper, however, for counsel to inquire as to what school of medicine the witness is an adherent, because of its importance in weighing the value of his testimony after it has been given.
Persons Not Duly Licensed Sometimes Held Not Competent.—It has also been a mooted question in those States where it is necessary, in order to enable a person to practise physic or surgery, that he should be licensed, whether a person practising without a license, however extensive his reading and practice,[63] would be considered qualified as an expert witness in a court of justice. This point, so far as diligent examination discloses, has not been determined in any reported case, although it has been suggested at nisi prius and has been, in one instance within the knowledge of the writer, decided that he is not to be considered an expert in matters involving medical knowledge and skill. The reasoning of the court was that the policy of the State is to prohibit persons not possessing the qualifications required to obtain a license, from acting in any capacity as professors and practitioners of medicine or surgery. If the witness is a member of the profession, legally qualified as such, it has been held that he is sufficiently qualified as an expert if he shows that he possesses the average ability of members of his profession. Hall v. Costello, 48 N. H., 176; Tellis v. Kidd, 12 Ala., 648; Wharton on Evidence, Sec. 446; Rogers on Expert Testimony, Secs. 17 and 18; Slocovich v. Orient Mutual Ins. Co., 108 N. Y., 56.
As to the question whether it is necessary that the witness should actually have practised his profession, see the last-cited text-writer, Secs. 43 and 44, who seems to have entertained views opposite to those stated by Professor Greenleaf.
Wharton on Evidence, Sec. 439, states the rule as follows: “He must have special, practical acquaintance with the immediate line of inquiry more than a mere vague, superficial knowledge. But he need not be acquainted with the differentia of the specific specialty under consideration.... A general knowledge of the department to which the specialty belongs would seem to be sufficient.”
Interested Persons may still Testify as Experts.—Since the law forbidding interested persons from being witnesses has been changed, it has been suggested that an interested person although otherwise qualified might not be a competent witness to give an opinion as an expert. But the established doctrine is that he may give such an opinion; the weight of it, however, would be for the jury to determine. Greenleaf on Evidence, Redfield’s edition, Sec. 440, citing Lockwood v. Lockwood, 2 Curtis, 309; Dillon v. Dillon, 3 Curtis, 96, 102. See also Dickinson v. Fitchburg, 13 Gray, 546.
Testimony of Expert, how Impeached.—Sometimes, on cross-examination or otherwise, the fact becomes known that[64] the witness who is proposed as an expert has expressed an opinion on the subject in hand contrary to that which he has given upon the witness-stand, and the question has been raised as to establishing that fact at the outset and before his testimony goes before the jury, in order to enable the trial judge to determine whether he is competent. The rule in that case is that the testimony as to his prior expression of opinion is not to be received at that time, but will come properly up as rebuttal, he having been asked upon his cross-examination, giving time and place, whether he has made the statements attributed to him. An expert witness may in other respects be impeached like any other witness, that is, by the oaths of persons who know him and have known his reputation, and who testify that his reputation for truth and veracity is bad and that they would not believe him under oath. He may also be impeached by producing witnesses to prove that his special knowledge or technical skill is not reliable or adequate to the undertaking which he has assumed. But this testimony must be from personal knowledge of the man and not from general reputation. Wharton on Evidence, Sec. 437; Le Rose v. Commonwealth, 84 Pa. St., 200.[183]
General Rule as to Required Amount of Skill and Experience Stated.—The general rule may be stated thus, as derived from these and other authorities:
The extent of the previous study and investigation, and the amount of skill and information which must be shown, will depend upon the facts of each particular case. But some special and peculiar knowledge or skill must be established, the amount of it to be determined by the trial judge in his discretion. The possession of such knowledge and skill is presumed in medico-legal cases if the witness is a licensed practitioner.
Some Practical Suggestions as to Conduct of Witnesses on the Stand.—In this preliminary examination, the conduct and demeanor of the witness are of no little importance, because it is then and there that he makes his first impression upon the court and jury. He should be perfectly open and unreserved in stating his means of special information, in explaining what are the limits of his personal experience and the extent of his reading; but, at the same time, it would be well for him to avoid all appearance of self-glorification and all tendency to exaggerate his individual acquirements. Often has it occurred that expert witnesses of undoubted capacity and honesty, who are unfortunately grandiose and self-assertive in their manner, have, however honest and able they might be, lost entirely their weight with the court and jury by undue self-complacency and exaggeration of their personal qualifications, during their preliminary examination. This is a matter requiring tact and judgment and nerve, and should be fully understood between[66] counsel calling him and the witness, before the witness is placed upon the stand. In that event, it will be quite safe for the witness to closely follow the questions of counsel by his answers, and to volunteer little or nothing. If his answers are not full and complete enough, counsel can renew the question in the same or in other form or carry the matter into greater detail. If, on the other hand, his answer is too full or he appears too eager, he may create a prejudice against him which nothing can overthrow, and which the art of counsel upon the other side in cross-examination and in making comments upon his testimony when summing up before the jury, will very effectually use to destroy his weight as an expert.[184]
Scope and Extent of Examination of Expert Witnesses.—Having stated how experts may be summoned and qualified, it remains to consider the scope and extent to which they may be examined.
The advancement of the sciences and the progress of research in special fields of knowledge have made expert testimony of large importance during the present century. The basis of its admission is the fact that there are certain processes of reasoning which an ordinary jury is incapable of performing, even with the assistance of courts and lawyers. Oftentimes in the administration of justice in our courts, proof is given of circumstances which although admitted would have little or no significance in the mind of an ordinary juror, and which he would be unable to contrast and compare with other facts, successfully, without the aid of those more familiar with scientific matters and the inductive process of reasoning than he is. In such cases it is necessary that the jury should be specially enlightened by persons who have, through training, skill and experience, acquired the power to enlighten them. A common instance and illustration of this matter is to be found in the case of homicide by poisoning. A human body is found dead; externally there may be no indicia to show positively the cause of death. Under such circumstances the laws of all civilized countries permit what is called a post-mortem examination by skilled physicians, who, finding no external evidences of the cause of death, are permitted by the officers of the law to remove the internal portions of the body for special and careful examination.[67] If this discloses traces of inflammation or of lesions of an abnormal character, further power is vested in the authorities to have at the expense of the State a chemical examination of the internal organs. If this examination, which is necessarily long and excessively technical, results in the discovery of any poisonous substance, such as would produce death, and if it is found in sufficient quantities to produce death, these persons who made the post-mortem examination and discovered the outward indications of the administration and effects of the poison, and the chemists who discovered the poison itself in the tissues of the body, in sufficient quantities to produce death, are called as experts before the jury. The post-mortem examiners explain what the appearance of the body was, as distinguished from the appearances of the body of an individual who had died from natural causes. The chemist describes his course of experimentation, the various deductions which he made from his experiments, the tests which he applied in his investigation in discovering poison, and is then allowed to testify that the poisonous substance was found in sufficient quantities to produce the physical appearances which the post-mortem examiners have described, and to accomplish the death of the human being in whose body the poison was found. It is obvious that the power of observation and the skill, which the skilled chemists and physicians used as the basis of their reasoning in this case, were such as an ordinary man, unskilled and inexperienced, would not possess, and the ability to use them must have come from the study of treatises on such subjects, and from teaching and experience, to such an extent as to entitle the persons so testifying to be considered by the courts as qualified to express an accurate and sound opinion on the matters and things under investigation. Thus it appears how, in such cases, a departure became essential to the successful administration of justice, from the strict rule that witnesses shall testify solely to matters of fact and observation, and why it has long been considered that some witnesses must be allowed to testify to opinions and conclusions.
Again, in a like case, a body is found bearing evidences of wounds or bruises. The question to be determined is whether they were inflicted before or after death; if before death, whether they were sufficient to cause death. Some wounds and[68] injuries might be sufficiently apparent and dangerous so that the common, inexperienced eye would at once detect that they were sufficient to cause death. But in most instances this is not the case, and in such instances the testimony of experts is required by the necessity of the case, to show that the wounds and injuries were sufficient to cause death.
The General Rules Stated as to Subjects for Expert Testimony.—Hence the general rule is, that wherever the facts to be investigated are such that common experience and knowledge of men do not enable them to draw accurate conclusions, but are such that the study and experience of specialists do enable such specially endowed persons to draw accurate conclusions, then the inferences and deductions they have drawn can be testified to by those who qualify themselves before the court as persons having sufficient skill and experience as such specialists to entitle them to give opinions. The cases in which expert testimony is permitted to be given are set forth in Rogers on Expert Testimony, Sec. 6, quoting from Jones v. Tucker (41 N. H., 546), as follows:
“1. Upon questions of science, skill, or trade, or others of like kind.
“2. Where the subject-matter of inquiry is such that inexperienced persons are unlikely to prove capable of forming a correct judgment without such assistance.
“3. Where the subject-matter of investigation so far partakes of the nature of science as to require a course or previous habit of study in order to the attainment of knowledge of it.”
So also Chief Justice Shaw of the Supreme Court of Massachusetts, in New England Glass Co. v. Lovell (7 Cushing, 319), said:
“It is not because a man has a reputation for sagacity and judgment and power of reasoning that his opinion is admissible in testifying as a witness. If so, such men might be called in all cases to advise the jury, and it would change the mode of trial; but it is because a man’s professional pursuit, or his peculiar skill and knowledge of some department of science not common to men in general, enable him to draw inferences where men of common experience, after all the facts have been proved, would be left in doubt.”
To the same effect see Muldowney v. Illinois Central R. R. Co., 36 Iowa, 472; Wharton on Evidence, Sec. 436; Greenleaf on Evidence, Sec. 441.
Qualifications of this General Rule.—The extent to which an expert witness can go in giving his opinion is limited to matters of science and skill, and does not extend to the expression of views on matters of legal or moral observation, or the manner in which others would probably be influenced if the parties had acted in one way rather than in another. Campbell v. Richards, 5 B. & Ad., 345.
So it has been held that the question whether a physician has honorably and faithfully discharged his duty in a given case, either to his medical profession or to his patient, is not a question of science but of pure ethics, upon which the jury is as competent to decide as any one else, and in such a case an opinion would not be allowed to be given either by another medical practitioner or by a professor in the science of morals. Rogers on Expert Testimony, Sec. 11, citing Ramadge v. Ryan, 9 Bing., 333.
There are also some matters of fact which apparently transcend the dividing line between common experience and judgment and scientific experience and judgment, as to which expert testimony is not receivable, but the jury and court must weigh the facts and draw the inferences for themselves. An interesting example of this is found in the case of Manke v. The People, 78 N. Y., 611 (17 Hun, 410), cited in Stephens’ “Digest of the Law of Evidence,” p. 107, note H, decided in the New York Court of Appeals a few years ago. In that case one Adolf was killed by a gunshot, and pieces of paper were found near the scene of the homicide bearing certain marks. An expert was called upon to say whether they were powder-marks, and whether the condition of the paper was such that in his opinion it was wadding which had been fired from a gun. This evidence was held to be inadmissible by the General Term of the Supreme Court, and this decision was affirmed by the Court of Appeals. These courts held that the question as to whether this was a wad fired from a gun was a matter which the jury was as competent to judge of as the witness. In delivering the opinion at General Term, Presiding Justice Talcott said that this case was very close to the border line, but in his judgment[70] it was beyond the province of experts and within the province of jurors.
Nevertheless, in that case the evidence of chemists who had examined the wadding, and had discovered the marks on it which were said to be powder-marks, and upon analysis had determined that they were powder-marks, or that they were marks of powder which had exploded, would have been clearly admissible.
The subjects concerning which medical men may be called upon to testify as experts are as numerous as the diseases, injuries, mental and physical conditions of the human race which fall within the range of the practice of medicine and surgery. It is therefore practically impossible to give them in detail.[185]
Practical Suggestions and Admonitions Embodied in Rules.—It is deemed advisable that the following practical suggestions and admonitions to physicians, concerning their duties as expert witnesses, shall here be given.
First: A physician should refuse to testify as an expert unless he is conscious that he is really qualified as an expert.
Second: After accepting the responsibility, his first duty should be to make a diligent examination and preparation for his testimony, unless it is upon a subject with which he is familiar and which he is satisfied that he has already exhausted, by reading the best authorities that he can find, and by careful reflection upon particular questions as to which his opinion will be asked.
Third: Where he is to make an examination of facts, such as the post-mortem examination of a body, a chemical analysis or an examination of an alleged insane person, he should insist[71] upon having plenty of time and full opportunity for doing his work thoroughly. He should take particular pains to make his examination open and fair, and, if possible, should invite opposing experts to co-operate with him in it.
Fourth: He should be honest with his client before the trial in advising him and giving him opinions, and upon the trial should preserve an absolutely impartial attitude, concealing nothing, perverting nothing, exaggerating nothing.
Fifth: On the preliminary examination as to his qualifications as a witness he should be frank and open in answering questions. He should state fully the extent and the limits of his personal experience and of his reading upon the subject, without shrinking from responsibility, yet without self-glorification.
Sixth: He should be simple, plain, and clear in his statement of scientific facts and principles, avoiding the use of technical language, and trying to put his ideas in such form that they will be grasped and comprehended by men of ordinary education and intelligence.
Seventh: He should avoid stating any conclusions or principles of which he is not certain, but having an assurance that he is right he should be firm and positive. He should admit the limitations of his knowledge and ability. Where a question is asked which he cannot answer, he should not hesitate to say so; but he should refuse to be led outside the subject of inquiry, and should confine his testimony to those scientific questions which are really involved in the case, or in his examination of the case.
Eighth: And finally, he should always bear in mind that at the close of his testimony an opportunity is usually given to him to explain anything which he may be conscious of having said, which requires explanation; and partial statements which need a qualification to make them a truth. This is the physician’s opportunity to set himself right with the court and with the jury. If the course of the examination has been unsatisfactory to him, he can then, by a brief and plain statement of the general points which he has intended to convey by his testimony, sweep away all the confusion and uncertainty arising from the long examination and cross-examination, and can often succeed in producing for the first time the impression which he desires[72] to produce, and can present the scientific aspects of the case briefly and correctly.
Probably no man was ever so gifted as to be able in practice to carry out all of these principles in giving medical testimony. If he could, he would be the ideal expert witness. But the principles are, after all, simple and easily followed in the main. Any physician who knows his subject and who has a clear head and the ordinary faculty of expression, by observing these principles can make himself invaluable as an expert witness. There is no branch of the profession which brings a broader fame, greater influence, or larger emoluments than this. There is no branch, on the other hand, in which men of real ability make more lamentable failures.
CHAPTER VI.
MALPRACTICE.
Definition.—Malpractice may be defined to be—
1st. Wilful acts on the part of a physician or surgeon toward a person under his care, by which such person suffers death or injury;
2d. Acts forbidden by express statute, on the part of a physician or surgeon, toward a person under his care, by which such person suffers death or injury;
3d. Negligent acts on the part of a physician or surgeon in treating a patient, by means of which such patient suffers death or unnecessary injury.
These various divisions will be considered in the order in which they are above set forth.
Wilful Malpractice.—The cases which fall within the first two divisions of this definition are such acts as render the medical man liable to punishment in a criminal prosecution, and may not necessarily, although in some instances they may, constitute grounds of liability in a civil suit against him.
As examples of the first class of cases may be cited those instances, happily not numerous in the annals of the profession, where a physician or surgeon when treating a female patient has had carnal connection with her, representing that he was using that method of treating her to cure her disease. Such a case was Reg. v. Case, 1 Eng. Law & Eq., 544 (s. c., 1 Den. C. C., 580).[186]
Honest Intent no Defence in Such Cases.—In Reg. v. Reed, 1 Den. C. C., 377 (s. c., 2 Car. & K., 967), it was contended as a defence that the defendant really believed that he was curing his patient by treating her in this extraordinary way. The Court, per Wildes, C. J., brushed aside this contention[74] with scorn, saying: “The notion that a medical man may lawfully adopt such a method of treatment is not to be tolerated in a court of justice;” and in this case and in others, convictions have been sustained for the crime of rape or of attempting to commit rape.[187]
Another example of wilful malpractice would be wilful neglect of a patient by his medical attendant, who became intoxicated voluntarily, though this will generally come under the second subdivision, as most states and countries have enacted statutes making it a criminal offence to practise medicine or surgery when intoxicated.
Acts Forbidden by Statute.—Within the second subdivision of the definition, or acts declared unlawful by statute, fall the cases of committing or attempting to commit an abortion, and cases of prescribing for or treating a patient by one voluntarily intoxicated. If the abortion is attempted without the knowledge or consent of the woman, and under the pretence of performing a necessary operation upon her to cure disease, undoubtedly the physician would be liable to a criminal prosecution by the State for the offence of committing an abortion and to civil action by her to recover damages. If the abortion was committed with her consent, while she would have no right of action against him for damages, he would be liable to criminal prosecution under the statute.
Abortion Not a Crime by the Common Law.—At common law it was not a crime to commit an abortion with the mother’s consent if the child had not quickened. In Mitchell v. Com., 78 Ky., 204 (s. c., 39 Am. Reports, 227), the Court, per Hines, J., says: “After a patient investigation we are forced to the conclusion that it was never called a punishable offence at common law to produce, with the consent of the mother, an abortion prior to the time when the mother became quick with child. It was not even murder at common law to take the life of the child at any period of gestation, even in the very act of delivery.” See also Evans v. People, 49 N. Y., 86.
The inhumanity and danger to society of this rule became manifest at a very early period, and both in England and in[75] this country statutes were adopted, varying somewhat in the degree and kind of punishment and in the nomenclature of the crime, but all of them making the offence of committing an abortion, no matter at what stage of gestation, a crime.[188]
The Common-Law Doctrine Criticised.—Professor Elwell in his valuable work on “Malpractice, Medical Evidence and Insanity,” pp. 250, 251, makes the following remarks upon this subject: “The idea once existed quite generally, and it still exists to some extent, that there is no offence in destroying the embryo or fœtus before there is a manifest knowledge of life by the mother, derived from motion of the child called ‘quickening.’ How absurd to suppose that there is no life until the mother can feel the muscular motions of the child! As well might we deny the vitality of the blood because it cannot be felt. The muscular tissues, and even the bones to which they are attached, must have some degree of substance before there can be motion, and of course this development depends upon life. Though this foolish notion is now fully exploded in medicine, it still lingers in the popular mind, and doubtless leads to much crime. The life of the fœtus or embryo immediately after conception is just as positive physiologically as at any subsequent period. Quickening being an incident or sign in the course of development of the fœtus, it indicates not the commencement of a new state of existence, but only a new manifestation of pre-existing life.... It is uncertain in its appearance, sometimes coming on at three months, sometimes at six months, and sometimes not at all.”
Legal Definitions of Terms, “Quick with Child,” etc.—In Evans v. People, 49 N. Y., 86, following R. v. Wycherly, 8 C. & P., 262, it was held that a woman is “quick with child” from the period of conception after the commencement of gestation, but is “pregnant with quick child” only when the child has become “quickened in the womb.” This distinction has been discussed in State v. Cooper, 2 Zab., N. J., 52, and since the Evans case, the same court in New York State has held that the expression, “woman with child,” means “pregnant woman.”[76] Eckhardt v. People, 83 N. Y., 42 (s. c., 38 Am. Rep., 462).
Death of Child by Abortion.—If, in attempting to produce an abortion, the child is caused to be born alive but before the end of the period of gestation, and when it is not capable of sustaining life, and it dies, the person producing the abortion and bringing the child into the world at this time and in this manner is guilty of murder. Wharton’s Crim. Law, sec. 942; Rex. v. West, 2 Cox Crim. Cases, 500; Com. v. Brown, 14 Gray, Mass., 419.
Death of Mother by Abortion.—So also where in consequence of producing an abortion the death of the mother occurs, the person producing the abortion is guilty of murder at common law. 4 Blackstone’s Com., 201; 1 Bishop’s Crim. Law, 328. In some of the States, however, these offences are declared to be only manslaughter.
Further consideration of the subject of abortion will be had under that title in another part of this work.
Statutes Generally Except Abortions Necessary to Save Life.—It should be noted here, however, that nearly all the statutes which define and punish the crime of abortion, or the crime of manslaughter or murder committed in consequence of abortion, declare that when it is necessary to produce a miscarriage in order to save life, the act of doing so is excepted from the effect of the statute.
Negligent Malpractice.—Under the third subdivision of the definition, viz., when by reason of the negligent acts on the part of the physician or surgeon the patient suffers death or unnecessary injury, may be placed the most numerous cases of malpractice, according to the generally accepted meaning of the term.
Criminal Liability for Negligent Malpractice.—It is manifest that not every degree of negligence which causes death or injury ought to render the physician or surgeon liable to indictment and punishment for a crime. The general theory of the criminal law is based upon the doctrine that in order to constitute a crime there must be either an intent to do the wrong, or such a degree of negligence in the performance of a given act as to supply the place of the intent to do wrong, and require punishment for the protection of society, upon the ground that the carelessness of the defendant is so great as to[77] make it necessary and proper to punish him, in order to deter others from following his example.
Doctrine of Leading Case of Com. v. Thompson.—In Com. v. Thompson (6 Mass., 134), Parsons, C. J., observes: “There was no evidence to induce the belief that the prisoner by his treatment intended to kill or injure the deceased and the ground of express malice must fall. It has been said that implied malice may be inferred from the rash and presumptuous conduct of the prisoner in administering such violent medicines. Before implied malice can be inferred, the judges must be satisfied that the prisoner by his treatment of his patient was wilfully regardless of his social duties, being determined on mischief.... To constitute manslaughter, the killing must have been the consequence of some unlawful act. Now there is no law which prohibits any man from prescribing for a sick person with his consent; and it is not a felony, if through his ignorance of the quality of the medicine prescribed, or of the nature of the disease, or of both, the patient, contrary to his expectations, should die. The death of a man killed by voluntarily following a medical prescription cannot be adjudged felony in the party prescribing unless he, however ignorant of medical science in general, had so much knowledge or probable information of the fatal tendency of the prescription that it may be reasonably presumed by the jury to be an act of wilful rashness at least, and not of honest intention and expectation to cure.”
The Doctrine of the Thompson Case Too Broad.—This lax statement of the law, made by the learned chief justice in this case, has been much doubted and criticised. It appears to be unsound in the length to which it goes in requiring, in order to constitute criminal liability, what may be termed excessive gross carelessness or wilful gross carelessness. It apparently runs counter to the prevailing opinions of the English judges, and to the later decisions of the courts in the United States, although it is followed and approved in Rice v. The State, 8 Mo., 561.
In Rex v. Long (4 Car. & P., 308-310), Park, J., said: “I call it acting wickedly when a man is grossly ignorant and yet affects to cure people, or when he is grossly inattentive to their safety.”
So in Rex v. Spiller (5 Car. & P., 353), the Court said: “If[78] a person, whether a medical man or not, professes to deal with the life and health of another, he is bound to use competent skill and sufficient attention; and if he causes the death of another through gross want of either he will be guilty of manslaughter.”
Bishop, in his work on Criminal Law, lays down the rule that not every degree of carelessness renders a practitioner liable to criminal prosecution, and that it must be gross, or, as more strongly expressed, “the grossest ignorance or most criminal inattention.”[189]
Nevertheless he quotes with approval (2 Bishop Crim. Law, 264) the remark of Willes, J., that a medical man is taking a leap in the dark if he knew he was using medicines beyond his knowledge; and also the remarks of Bayley, J., in Rex v. Simpson (1 Lewin, 172), who said in that case: “I am clear that if a person not having a medical education, and in a place where a person of a medical education might be obtained, takes it upon himself to administer medicines which may have an injurious effect, and such medicines destroy the life of the person to whom they are administered, it is manslaughter. The party may not mean to cause death, or the medicine may produce beneficent effects, but he has no right to hazard medicine of a dangerous tendency when medical assistance can be obtained. If he does, he does it at his peril.”[190]
Gross Negligence Defined.—In general it may be stated that gross negligence is necessary to constitute criminal liability, but this may be predicated upon, or inferred from, such want of ordinary care and skill as shows gross ignorance, or such want of attention as indicates wilful disregard of the well-known laws of life and health.[191]
Gross Negligence Resulting in Injury a Misdemeanor.—It has also been held that although death does not but injury[79] does ensue, as the result of gross negligence or inattention, that constitutes a misdemeanor punishable criminally.[192]
In Determining Degree of Negligence Circumstances and Conditions Govern.—It should be noted, however, that the circumstances and conditions attending the act of alleged criminal malpractice should be given much weight. So also should due weight be given to the advancement of knowledge and education in the world in general, and in the medical profession in particular. In an early English case, one of the judges remarked that not as much knowledge and skill could be expected of a surgeon or physician in a sparsely settled country district as in a city, and that he was at a loss to know what degree of knowledge and skill should be required of such a person. But in Gram v. Boener, 56 Ind., 447, Worden, J., said: “It seems to us that physicians or surgeons practising in small towns, or in poorly or sparsely settled country districts, are bound to possess and exercise at least the average degree of skill possessed and exercised by the profession in such localities generally. It is not true, as we think, to say that if a physician and surgeon has exercised such a degree of skill as is ordinarily exercised in the particular locality in which he practises, that would be sufficient. There might be but few practising in the given locality, all of whom might be quacks, ignorant pretenders to knowledge not possessed by them, and it would not do to say that because one possessed and exercised as much skill as the other, he could not be chargeable with the want of reasonable care and skill.”[193]
Unlicensed Practitioner Causing Death Guilty of Manslaughter.—Since the adoption by most civilized states and countries of the salutary practice of regulating by statute the practice of medicine and surgery, and forbidding persons not duly licensed from practising, and making it a misdemeanor to violate any of these statutes, it is clear that any person not having the requisite medical education and a license, who attempted to administer drugs and medicines or to perform operations,[80] and through want of ordinary knowledge and skill caused the death of another, would be held guilty of manslaughter, because he brought about the death while he himself was engaged in a violation of the law. In some states where no discrimination in this respect is made between misdemeanors and felonies, the crime would be murder, punishable by death; and it has always been the law that an empiric or quack holding himself out as a regular physician is bound to have and exhibit the degree of skill and care which he professes, and will be strictly held to the standard of skill of educated and licensed medical men.[194]
As to the legal meaning of the term “ordinary care and skill,” and the rules of evidence applicable in cases of malpractice, a full discussion will be had below, when considering the subject of civil liability for malpractice.
Civil Liability for Malpractice.
Any person holding himself out to be a physician or surgeon, or any physician or surgeon, who is guilty of malpractice, is liable for damages, to be recovered in a civil action, instituted by the person injured, or by those having a legal right to such person’s services. This is so whether the injured person actually employed the defendant to prescribe or treat him, or not. The liability flows out of the relationship, without regard to the element of employment, and it may result from negligence in treatment, or in prescribing, or in giving information and instructions to the patient as to how to take care of himself when under treatment. The rules of law applicable to the duties of a physician to his patient are stated and the authorities supporting them cited in Chapter IV. of this work.[195]
Ordinary Care and Skill Only Required.—The leading cases in America on the subject of civil liability for malpractice are: Leighton v. Sargent, 7 N. H., 460, and Carpenter v. Blake, 60 Barb., 485 (s. c. on appeal, 75 N. Y., 12). In the former case the Court said: “In a science encumbered[81] with so many sources of error and difficulties, it is obvious what cause we have for proceeding with the utmost caution, and for advancing from step to step with the greatest circumspection. It is in consideration of those peculiar difficulties that beset and encompass the physician and surgeon, that all enlightened courts have held that but ordinary care and skill shall be required of them, and that mere errors of judgment shall be overlooked, if the general character of treatment has been honest and intelligent, and that the result of the case shall not determine the amount of the responsibility to which he is held; and that when unskilfulness or negligent treatment of his patient is charged to a surgeon, it is not enough to show that he has not treated his patient in that mode or has not used measures which in the opinion of others, though medical men, the case required; because such evidence tends to prove errors of judgment, for which the defendant is not responsible, as much as it goes to prove a want of reasonable skill and care for which he may be responsible. Alone it is not evidence of the latter, and therefore a party must go further and prove, by other evidence, that the defendant assumed the character and undertook to act as a physician without the education, knowledge, and skill which entitled him to act in that capacity.”
In Carpenter v. Blake, upon the last appeal (75 N. Y., 12), it was said that the reasonable ordinary care and diligence which the law requires of physicians and surgeons is that which persons engaged in the same general line of practice have and exercise in like cases.[196]
Story’s Statement of the Rule.—Story in his work on Bailments, p. 433, with his usual felicitous method of statement says: “In all cases where skill is required it is to be understood that it means ordinary skill in the business or employment which the bailee undertakes; for he is not presumed to undertake for extraordinary skill, which belongs to a few men only in his business or employment, or for extraordinary endowments or acquirements. Reasonable skill constitutes the measure of the engagement in regard to the thing undertaken.”
Occult Influences Should be Considered by Lawyers and[82] Judges.—In this connection it should be borne in mind by lawyers and judges, that in the case of a physician treating disease, or a surgeon repairing an injury, occult influences frequently play a most important part. Professor Elwell in his work on Malpractice, etc., p. 25, lays great stress on this element of uncertainty. He says: “In the case of physicians, surgeons, attorneys, etc., another and important element besides skill enters into the result, and for this reason the degree of responsibility is to a certain extent and in a manner indicated and influenced. This important element is the operation of causes and influences over which the practitioner has but little or no control. They are occult, and no human foresight is able to anticipate them before they have completely deranged and materially interfered with his plans by bringing about a different result than that confidently depended upon.”[197]
Change and Advancement in Medical Knowledge also to be Considered.—It should on the other hand be clearly understood that the constant change and improvement which are going on in medical and surgical education, in the discovery of new remedies and new methods of treatment, and in the invention of new instruments, tend constantly to elevate the average skill and intelligence of the profession, and with them the standard by which the courts will determine liability for negligence. What would have been, but a few years ago, fully recognized by the courts as ordinary skill in the treatment of disease and the performance of operations, would now be regarded as antiquated and less than ordinary skill, because of the advancement in the knowledge of means which can be devoted to the treatment of disease and injury.[198]
We have already seen that what is the degree of skill to be required of one practising in a small town or a country district sparsely inhabited, and what is required in the case of a city practitioner, may differ to some extent with the circumstances. Quacks and pretenders, however, must be judged by the standard of regular practitioners.[199]
Degree of Care and Skill a Mixed Question of Law and Fact.—What constitutes reasonable care and skill is a mixed question of law and fact, like any other question of negligence. Where the evidence is undisputed and no conflicting inferences can be drawn from the facts presented, it is the duty of the Court to determine whether or not there is sufficient proof of want of ordinary care and skill to be submitted to the jury. Where, however, the evidence is conflicting on that point, or the inferences to be drawn from the facts established might be differently drawn by different men having the same opportunity for observation, and the same circumstances before them, it is for the jury to say whether or not the defendant has exercised reasonable care and skill, guided by proper directions from the Court as to the measure of skill required. This involves the question as to how far the practitioner is bound to be familiar with the methods, appliances, drugs, and methods of treatment of his profession in general.[200]
Experimentation Not Permissible.—Experimentation, whether upon charity patients or pay patients, is equally prohibited by well-settled rules of law. In other words, a departure from known methods of treatment for the purpose of or by way of trying unknown remedies, or operations not usually adopted by the profession, if an unfortunate result occurs, renders the defendant liable (McNevins v. Lowe, 40 Ill., 209).
Measure of Damages.
The measure of damages in cases of malpractice may vary with the kind of malpractice. In the case of wilful malpractice, the element of gross negligence justifies punitive or retaliatory damages, in those States where any such damages are allowed. That is, damages which will not only compensate for the injuries inflicted, but which will, by punishing the wrong done, tend to repress similar acts in the future. The tendency of the courts and of legal authority of the present time is, however, to limit as often as possible the cases in which punitive damages are allowed, upon the theory that if a grossly negligent act is committed it will require criminal prosecution, and that the[84] strong arm of the State should be invoked to punish the wrong, rather than to line the pocket of the injured person.
On the other hand, in cases of malpractice, damages for want of ordinary care and skill are recompensed as in any other cases of negligence. They may include loss of time of the patient, inability to earn his living, such sum as the jury thinks is reasonable to be given as a compensation for the extra pain and suffering, and, where the injury is permanent, such further sum as will indemnify the patient for the injury or deformity which he may suffer on account of the defendant’s neglect. Citation of authority upon this question of damages is almost unnecessary.[201]
Liabilities of Partners, etc.—It has been held that where two physicians were partners, and one of them committed an act of negligent malpractice, both were liable in a civil court for damages.[202]
But the declarations of the partner who is guilty of the negligent act, made as to the act committed, and in the absence of the other partner, are not admissible as against the other partner. And so also is the rule as to declarations of the partner who committed the act after its commission as to the propriety of the treatment, and opinions expressed by him in reference thereto.[203]
It has also been held that one surgeon who recommends the employment of another during his absence from town is not liable for acts committed during his absence.[204]
Suits for Injuries to Married Women and Minor Children.—When the person injured is a married woman, her husband may sue for loss of services on account of malpractice, and when the injured person is a minor child the parent may sue as in any case of negligence. A third person, such as the husband of a woman injured by malpractice, or the father of minor child so injured, can only recover the value of the services thereby lost, and in some cases the enhanced expense of medical attention and nursing thereby rendered necessary.
Inspection of the Injured Person at the Trial—Before Trial Improper.—In an action in which the injury is to a portion of the body which may be seen, such as the shortening of a limb on account of improper treatment of a fracture, the limb may be exhibited to the jury.
It has been much discussed whether the defendant in a malpractice or other negligence case can compel the plaintiff to permit his person to be examined by physicians before trial, to enable the defendant to know the full extent of the injury so far as it is perceptible. In the latest cases the examination of plaintiff before trial was not allowed.[205]
In 1877 the Supreme Court of Iowa in the case of Schroder v. C., R. I. & P. R. R. Co., 47 Iowa, 375, held that the court had inherent power and jurisdiction to compel the plaintiff to submit to such an examination.
This decision has been followed by the courts of several of the western and southern States, while in others the power has been denied. These cases will be found fully collected in Roberts v. O. & L. C. R. Co. and in U. P. R. R. Co. v. Botsford cited above.
The ground of the decision of the United States Supreme Court and of the New York Court of Appeals seems to be, that in the absence of legislative provision permitting a court to order such an examination, it has no inherent power to do so, and did not derive any such powers from the common-law courts of England, which never had exercised such powers.
In some of the cases which deny the right to compel such examination, it is claimed that if such a statute was passed as would confer upon the courts power to compel such an examination, the statute would be unconstitutional, and much is said in those decisions about the sacredness and immunity of the person. It seems difficult, however, to understand why such statutes should be considered as differing in any respect from statutes permitting orders for the examination of witnesses and parties before trial, or for the discovery and inspection of books and papers, and the like, which statutes have been enacted for many years and have never been held to be unconstitutional. Surely an honest suitor having a just claim for damages for[86] personal injuries would not object to such an examination, because the result would often strengthen his case, while a dishonest suitor having a false and unmeritorious claim ought to be exposed and have his false claims defeated, in the interests of justice and truth. On the other hand, a suitor who was honestly mistaken in his belief that he had been disfigured or injured by an act of malpractice might often discover his mistake, and be saved the annoyance and expense of defeat after a trial in open court.
Some of the most frequent cases of alleged malpractice, brought before the courts, are those in which it is claimed that a fractured limb has been improperly set, with the result that it becomes crooked or shortened; when the fact is, as is conclusively shown by Prof. Frank H. Hamilton in a paper published by him many years ago, and quoted with approval by Professor Elwell, in his work on Malpractice, etc., that the percentage of cases, in certain kinds of fractures, in which perfect results are obtained by even the most eminent surgeons, is very small. In such cases as these the true state of affairs might often be disclosed by careful inspection prior to the trial. On the whole more good than harm would seem to be the probable outcome of permitting such examinations, in malpractice cases, if not in all cases of alleged personal injuries.
Evidence in Malpractice Cases.—The prevailing trial practice in malpractice cases is to prove the condition of the patient prior to the employment of defendant and at the time the treatment in question began, the methods of treatment adopted, and instructions given, and the condition of the patient during and after such treatment, and then to place other physicians on the witness-stand, and put to them hypothetical questions involving the facts as established by the evidence, and calling upon them to state whether the method of treatment adopted indicated proper skill and care, or even the usual and recognized methods of the profession.[206]
In some States evidence of the general reputation of the defendant for skilfulness or the contrary is held admissible. In other States such evidence is held inadmissible (see Vol. XIV., Am. and Eng. Encyclopædia of Law, p. 83, and cases collected in Note 6).
Contributory Negligence.—In conclusion it should be stated that the patient is bound to follow obediently all proper directions given him by his physician or surgeon, as to his diet, mode of life, time of taking and quantity of medicine to be taken, or the care of a diseased or injured member. Any disobedience of such directions which contributes to prevent a recovery will bar him from his right of action for malpractice, even though the medical man may have been somewhat negligent. In short, the same rule as to contributory negligence applies in this as in any other case of negligence. This principle has been so long and so well settled that citation of authority in support of it is unnecessary.
THE LAW OF EVIDENCE
CONCERNING
CONFIDENTIAL COMMUNICATIONS
BETWEEN
PHYSICIAN AND PATIENT.
BY
CHARLES A. BOSTON,
Counsellor-at-Law, of the New York City Bar.
CONFIDENTIAL COMMUNICATIONS BETWEEN PHYSICIAN AND PATIENT.
PRIVILEGED COMMUNICATIONS.
Confidential communications between physician and patient not infrequently may relate to matters that are the subjects of inquiry before judicial tribunals. When these communications are by law excluded from disclosure in evidence, they are termed privileged communications. When such a disclosure is forbidden it is upon grounds of public policy,[207] “because greater mischiefs would probably result from requiring or permitting its admission, than from wholly rejecting it.”
COMMON LAW.
The common law required an inviolable secrecy to be observed by attorneys with reference to the communications which they had received from their clients.[208] But writers upon the law of evidence state that under the English rule protection from disclosure in evidence in a court of justice was not extended to communications between a medical man and his patient.[209]
Reasons for the Rule.—It does not clearly appear, in any of the cases usually cited as authority, why the distinction is[92] made between legal and medical advisers, but it is apparent that the privilege does not rest upon considerations of honor nor of confidence,[210] nor even upon the urgency of the situation under which the communication is made; for disclosures are made to a physician frequently to save life, or to a priest for reasons of eternal import, while those made to an attorney insure at most protection from temporal annoyance. The privilege of attorneys seems to be founded upon considerations of public policy in the administration of justice in the courts; attorneys are a part of the system, as are grand jurors, petit jurors, and judges,[211] and even arbitrators;[212] but physicians are no part of that system, and a disclosure of confidences made to them in no way tends to weaken the system or render it ineffectual, while the compulsory[93] examination of lawyers would tend to the suppression of the truth in litigation by discouraging confidence between attorney and client. This, perhaps, can be assigned as the reason for the distinction; a distinction which does not differentiate lawyers from physicians, but agents in the administration of justice from all others.[213]
Criticism of the Rule.—Though the privilege of attorneys was adopted to enforce respect for the law as securing the rights of persons entitled to its protection, by establishing inviolable confidence between them and the officer who represents them in their dealings in the law, and though it was not the purpose of the law to enforce sentiment or to elevate one profession above another, the sentimental idea did not suffer neglect for the want of advocates. Justice Buller lamented the narrowness of the rule,[214] and Mr. Best has criticised it as harsh in itself, of questionable policy, and at variance with the practice in France and the statute law in some of the United States of America.[215]
THE RULE IN THE UNITED STATES.
It is to be assumed, in the absence of statutes varying the rule, and of decisions to the contrary, in the several States of the United States, that in those States which derived their law from England the same rule of evidence obtains as that above enunciated. But many of the legislatures have by statute extended the privilege to communications between physicians and their patients, as well as to other specified confidential communications which it does not fall within the scope of this work to discuss.[216]
States and Territories in which there are No Restrictive Statutes.—The following States and Territories have no statute restricting the nature of the disclosures which a physician may be compelled to make in a court of justice: Alabama, Arizona, Connecticut, Delaware, District of Columbia, Florida, Georgia, Illinois, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Mississippi, New Hampshire, New Jersey, New Mexico, Pennsylvania, Rhode Island, South Carolina, Tennessee, Texas, Vermont, Virginia, and West Virginia.[217]
States and Territories in which there are Restrictive Statutes.—The following States and Territories have statutes restricting disclosures by physicians: Arkansas, California, Colorado, Idaho, Indiana, Indian Territory, Iowa, Kansas, Michigan, Minnesota, Missouri, Montana, Nebraska, Nevada, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, South Dakota, Utah, Washington, Wisconsin, and Wyoming.[218]
The Rule in United States Courts.—In trials at common law in the courts of the United States, the laws of the several States, except where the Constitution, treaties, or statutes of the United States otherwise require or provide, are regarded as rules of decision.[219] Section 858 of the Revised Statutes of the United States prescribes rules with reference to competency notwithstanding color and interest of witnesses, and in actions by or against executors, administrators, or guardians, and then provides that “in all other respects the laws of the State in which the court is held shall be the rules of decision as to the competency of witnesses in the courts of the United States in trials at common law, and in equity and admiralty.” Accordingly it has been held by the Supreme Court of the United States that in an action in the Circuit Court of the United States for the Southern District of New York, on a policy of life insurance, the evidence of a physician, inadmissible under Section 834 of the New York Code of Civil Procedure, was properly excluded.[220] But in criminal prosecutions in United States Courts, the privilege secured by State statutes does not avail.[221]
THE STATUTES.
As the effect of these statutes depends largely upon their language, the construction put upon the law in one State is chiefly serviceable in interpreting that of another State in those particulars where the two are similar.
Statutory Declarations of Policy.—A comparative view of the several laws shows that in the following States and Territory there are declarations of policy prefixed to the prohibition[96] of disclosures, that show the reason of the enactment, namely: California, Colorado, Idaho, Minnesota, Montana, North Dakota, Oregon, South Dakota, and Utah.[222] The declaration is to the effect that there are particular relations in which it is the policy of the law to encourage confidence and to preserve it inviolate, and that therefore the prohibition of the statute is laid.
Analysis of the Statutes.
The common purpose of the statutes is to restrict the rule compelling disclosures so as to protect communications with a physician in his professional capacity; but the limit to which the protection is extended differs in the various States. An analytic comparison of the statutes tends to show how far the interpretation of one is useful in construing another.
I. Nature of the Exclusion.—In California, Idaho, Minnesota, Montana, North Dakota, Oregon, South Dakota, Utah, and Washington the statutes apply only to testimony in civil actions.[223] The other statutes make no distinction between civil and criminal proceedings.
The active words are of course different in the several statutes, but they indicate a purpose to extend a privilege that the person entitled to it may insist upon maintaining, with the single exception of the law of North Carolina, which provides that the presiding judge of a superior court may compel a disclosure, if in his opinion the same is necessary to a proper administration of justice.
Some of the statutes show clearly that it is the patient’s privilege, and suffer the patient or his representatives to waive it, either expressly or by conduct which the law declares to amount to a waiver.[224] Others are silent on this subject.
In California, Colorado, Idaho, Iowa, Minnesota, Montana, Nebraska, Nevada, New York, North Dakota, Ohio, Oregon, South Dakota, Utah, Washington, and Wyoming, it is expressly provided that the patient’s consent is necessary before a disclosure will be permitted.
In Colorado, Kansas, Oklahoma, and Oregon, if the patient offer himself or a physician or surgeon as a witness, that is to be deemed a consent.
In Nevada, in any suit or prosecution for malpractice, if the patient or party suing or prosecuting shall require or give consent, and any physician or surgeon shall give testimony, then the defendant may call any other physicians or surgeons as witnesses without the consent of the patient or party suing or prosecuting.
In Ohio and Wyoming, if the patient voluntarily testify the physician may be compelled to testify on the same subject.
II. The Witness.—In Indiana, Ohio, and Wyoming the privileged witness is termed a physician; in the other States and Territories, the privilege extends to a physician or surgeon.
In Arkansas and Indian Territory the privilege is secured to a person authorized to practise physic or surgery; in California, Montana, and Nevada, to a licensed physician or surgeon; in Colorado, to a physician or surgeon duly authorized to practise his profession under the laws of the State; in Michigan, New York, North Carolina, and Wisconsin, to a person duly authorized to practise physic or surgery; in Minnesota, Oregon, and Washington, to a regular physician or surgeon; in Iowa and Nebraska, to a practising physician or surgeon; in the remaining States and Territories, these statutes do not in terms distinguish between licensed and unlicensed practitioners.[225]
In New York, by the amendment of 1893 to Sec. 836 of the Code of Civil Procedure it is provided that in an action for the recovery of damages for a personal injury the testimony of a physician or surgeon attached to any hospital, dispensary, or other charitable institution, as to information which he acquired in attending a patient in a professional capacity in such institution, shall be taken before a referee. It does not appear whether this amendment is intended to take away the privilege, or merely to regulate the manner of taking such testimony when it is otherwise admissible.[226]
III. The Evidence.—The character of the communications which are privileged differs under the several statutes. In Arkansas,[98] California, Colorado, Idaho, Indian Territory, Michigan, Minnesota, Missouri, Montana, Nevada, New York, North Carolina, North Dakota, Oregon, South Dakota, Utah, Washington, and Wisconsin, they are characterized as information; in Indiana, as matter committed; in Iowa and Nebraska, as confidential communications; in Kansas, Ohio, Oklahoma, and Wyoming, as communications; in Iowa and Nebraska, it is further provided that they be properly intrusted; and in Kansas and Oklahoma, that they be with reference to a physical or supposed physical disease.
In Kansas and Oklahoma, any knowledge obtained by a personal examination of a patient is also expressly privileged.
In Indiana, Ohio, and Wyoming, advice given by the physician is covered by the protection.
In Arkansas, Indian Territory, and Missouri, the privilege is limited to information acquired from the patient; and in Kansas and Oklahoma, to communications made by the patient.
The statutes of Arkansas, California, Colorado, Idaho, Indian Territory, Indiana, Michigan, Minnesota, Missouri, Montana, Nevada, New York, North Carolina, North Dakota, Oregon, South Dakota, Utah, Washington, and Wisconsin expressly limit the protection to matter acquired while attending in a professional capacity; and all of these, save Indiana, as well as Iowa and Nebraska, confine the privilege to information necessary to enable the witness to prescribe or act for the patient.
In New York it is provided that “a physician or surgeon may upon a trial or examination disclose any information as to the mental or physical condition of a patient who is deceased, which he acquired in attending such patient professionally, except confidential communications and such facts as would tend to disgrace the memory of the patient, when the protection has been expressly waived on such trial or examination by the personal representatives of the deceased patient, or if the validity of the last will and testament of such deceased patient is in question, by the executor or executors named in said will, or the surviving husband, widow, or any heir at law, or any of the next of kin of such deceased, or any other party in interest.”[227]
The notable characteristics of the several statutes which thus far have been pointed out are discernible in the express language of the acts. In writing or using any treatise or compilation on privileged communications between physician and patient, it is to be constantly borne in mind that the privilege is of statutory origin; that the statutes are often dissimilar; and that the value of a judicial interpretation of one law in the construction of another varies with the dissimilarity.
JUDICIAL INTERPRETATION OF THE STATUTES.
The judicial decisions which are discussed here are those that deal with the privilege secured by the restrictive laws. The analogy between the privilege of a client with regard to his attorney’s disclosures, and that of a patient with regard to the testimony of his physician, is not so complete as to make it essential to present here, for the sake of their bearing upon the subject now under consideration, a study of the principles to be deduced from the numerous decisions with reference to attorneys as witnesses. The analogous cases of clergymen and priests are also beyond the scope of this treatment.
Rules of Construction.—The restrictions are in derogation of the common law[228] and in accordance with the rule of interpretation ordinarily adopted should be strictly construed,[229] but the courts have generally looked at the policy of the enactments, and have construed them so as to preserve inviolably the confidence existing between physician and patient, without narrowing their effect to a strict interpretation of their language.
In Indiana, under a former law which protected matters confided, it was said that the statute should be given a broader scope than the word confided in a strict sense imports, so as to cover matters learned by observation and examination.[230] But, though the statute in terms absolutely prohibits a disclosure, it has been said, in Indiana, that it gives no right to the physician to refuse to testify where the patient waives the privilege,[231][100] and that it creates no absolute incompetency, because to hold otherwise would result in obstructing justice without subserving the purpose of the statute.[232] In Missouri, there is a dictum that the privilege should be carefully limited to what the statute requires, not so much because it is in derogation of the common law as because it is in exclusion of the best evidence, on the ground of privilege;[233] but in this very case, the real question was whether the word oral should be construed into the statute so as to exclude from its protection information acquired by inspection and observation, and it was held that no such narrow interpretation was proper. In a later case the narrowing dicta of the foregoing opinion were disapproved,[234] and subsequently the disposition to make a liberal construction was shown by the highest court of the State, although a general rule of interpretation was not announced.[235] In New York, the rule that a statute in derogation of the common law is strictly construed does not apply to the Code of Civil Procedure.[236] But before the enactment of this statutory rule[237] there was a tendency to interpret liberally the law prohibiting disclosures.[238] In Arkansas the tendency seems to be to construe the law strictly.[239] The spirit of interpretation will be more fully illustrated in the discussion of particular cases which follows.
In New York it was claimed that the protection afforded by the statute is nullified by the provision for the examination of a party before trial,[240] but it was held that the statutes are consistent[101] and the physician cannot be made to disclose, though his patient may be.[241]
Classes of Actions.
Criminal Actions and Evidence of Crime in Civil Actions.—The statutes confining the restriction to civil actions have been cited above.[242] In Iowa, in an action for breach of promise to marry, it was said that the privilege does not extend to the protection of advice for the commission of a crime.[243] In New York the rule was at first embodied in the Revised Statutes of the State,[244] but upon the adoption of the Code of Civil Procedure it was included therein,[245] and subsequently the provision of the Revised Statutes was repealed.[246] In that State by law the rules of evidence in civil cases are applicable also to criminal cases, except as otherwise expressly provided;[247] and the statutes provide no different rule in criminal actions as to this class of evidence. Notwithstanding this fact, however, it has been said by the Court of Appeals, in a case where there was an attempt to screen a murderer by insisting that his victim’s physician was not a competent witness as to information acquired by him while attending his patient,[248] that the design of the law was to enable the patient to make known his condition to his physician without the danger of disclosing what would annoy his feelings, damage his character, or impair his standing while living, or disgrace his memory when dead, but that it was not intended to protect a murderer rather than to shield his victim; and quoting from the opinion of Talcott, J., in the court below,[249] the Court said: “The purpose for which the aid of the statute is invoked is so utterly foreign to the purpose and object of the act and so diametrically opposed to any intent[102] which the legislature can be supposed to have had in enacting it, so contrary to and inconsistent with its spirit, which most clearly intended to protect the patient and not to shield one who is charged with his murder; that in such a case the statute is not to be so construed as to be used as a weapon of defence to a party so charged instead of a protection to his victim.” Accordingly it was held that the evidence was not to be excluded under the statute. But the rule is still applicable to criminal actions. In a later case, where the accused was indicted for abortion, the same court held, that where the patient was living and the disclosure tended to convict her too of crime or to cast discredit and disgrace upon her, the evidence of her physician as to information acquired by him in attendance upon her was inadmissible in the trial of the man charged with the crime.[250] In a still later case,[251] the General Term of the Supreme Court held, where the accused was on trial for murder and he had confided to a physician what he had done, that the physician could not disclose the confidence. The rule deducible from these decisions seems to be that in New York the privilege extends to criminal actions, even though they be trials for murder, and even though the person accused be the patient, but that the statute will be applied only for the protection of the patient, and where it is apparent that no injury can possibly be done to the patient or his memory by the admission of the evidence, and the interests of justice demand the disclosure, for the punishment of a person for an injury done to the patient involving a violation of the criminal law, and the patient is not alive to waive the privilege, that the disclosure is not forbidden.
In New York efforts have been made to exclude from the operation of the statute other classes of actions, to which it has been urged that the reasons for the enactment do not apply, or in which the mischief alleged to be wrought by its enforcement has been suggested as ground for believing that the legislature could not have intended to include them. Of these, actions for divorce on the ground of adultery are one class; but it has been held that they constitute no exception.[252]
Testamentary Causes.—In New York it was long supposed that the policy of the law excepted probate proceedings; it was so held by the Surrogate of New York City;[253] and also by the General Term of the Supreme Court,[254] by which it was stated that the practice had prevailed for a half-century in will cases,[255] but the Court of Appeals,[256] has decided that testamentary cases constitute no exception to the rule, the judge who delivered the opinion stating that there is no more reason for allowing secret ailments of a patient to be brought to light in a contest over his will than in any other case, and that if mischief be wrought by the law the remedy lies with the legislature and not with the courts. The legislature has since afforded the remedy,[257] but not to the extent of adopting the rule of the earlier cases. In Indiana, in an action to set aside a will, the testimony of the testator’s physician has been excluded.[258] And in Michigan and Missouri it seems that testamentary cases are no exception to the general rule.[259]
Lunacy and Habitual Drunkenness.—It has been claimed in New York that inquisitions of lunacy are an exception, and recently it has been held that the alleged lunatic’s physician may testify as to his mental condition because no one is better qualified to testify,[260] but this decision seems to be at[104] variance with the principle of the decisions of the Court of Appeals with reference to testamentary cases, and presents no satisfactory reason for a distinction. In a similar case in the Supreme Court, Chambers, it was held that a medical attendant at an asylum could not testify.[261] It has also been held that a physician cannot make an affidavit as to the appearance and condition of his patient to support a petition for the appointment of a committee for him as an habitual drunkard.[262]
Fraud.—Still another class of actions in which contending principles have been invoked to make an exception in the law of privilege, is actions on life-insurance contracts. The contract of insurance is uberrimæ fidei, and the defence of fraud in the application is frequently interposed to defeat a claim under a policy. Medical testimony would often be the most satisfactory evidence to establish the fraud, and efforts have been made to introduce it under that excuse, but without avail. In the case of Dilleber vs. Home Life Insurance Company, in the Supreme Court of New York at General Term,[263] the question seems to have been directly before the court, and Davis, P. J., dissenting, insisted that the suppression of a physician’s testimony ought not to be permitted so as to cover up a fraud, but the majority of the court held otherwise; the case was subsequently overruled, but not on the ground urged by Justice Davis.[264] The number of insurance cases in which the rule has been enforced seems to leave it beyond question that it will not be relaxed for the purpose of establishing fraud,[265] although that announcement has not been specifically made. There seems no reason that the rule should be relaxed in that regard when it is not relaxed to establish the crime of the patient; though the mischief that may be done in such cases is apparent.[266]
The Witness.—The statutory provisions as to the professional status of the witness whose testimony is excluded have already been shown.[267] The facts which establish the relation of physician and patient will be treated later.[268] The witness is a member of a profession, but there is very little discussion in the cases as to what constitutes a physician or surgeon.[269] The language of the statutes as well as their policy and intent has been said to plainly embrace a physician who casually or in any way attends and prescribes for a patient, whether he be a family physician or the usual medical attendant or not.[270] The spirit of the acts would protect communications made to any person attending the patient in the accepted capacity of physician or surgeon wherever that might have happened, though the letter would confine it in some instances to duly authorized or duly licensed persons. It does not seem to have been established whether such authority or license must have been granted under the laws of the State where the trial is conducted, nor how the several statutes apply to communications made elsewhere, especially in States or countries where authority or license to practise is not required by law.
It has been said with reference to the New York law that it is absolutely necessary that the witness should be a duly qualified physician;[271] and it has been held that the words “duly authorized” mean those persons who are not prohibited by the penal code from practising, so that an unlicensed physician may be compelled to disclose confidential communications.[272] Whether the same rule would be applied with reference to information obtained in another State by a physician duly authorized to practise there although prohibited from practising in New York,[106] is a question that is suggested as a case within the reason of the law but outside of its letter, and one which does not seem to have been answered.
In New York, in an action by a physician for compensation for his services, it was held that a person who merely answered for a physician at his office in his absence, and was not himself a physician, is not a witness whose testimony is privileged.[273]
In Missouri it has been held that a drug and prescription clerk is not a privileged witness.[274] The question arose in the same State, whether a dental surgeon is forbidden to testify under the statute, but its determination was not essential to the judgment and it was left unanswered.[275]
To establish the privilege it is necessary that the person who insists upon it to exclude testimony should show by competent evidence that the witness belongs to the class privileged under the law.[276] But where the physician testified that he was a regular practising physician and attended in that capacity, and he was not examined further as to his due authority, it was held that a failure to produce his license could not be urged on appeal as reason for compelling him to testify.[277] The Court said that if the privilege were the physician’s he might, if the objection were taken, be required to prove by the best evidence that he was duly authorized, but as it is the patient’s privilege, in the absence of objection to the sufficiency of the proof, the patient is entitled to the benefit of the presumption that the physician had the license which the law requires to entitle him to practise.
Waiver of the Privilege.
Who may Waive.—Those States in which the law provides for a waiver have been enumerated;[278] in others the courts have determined that the privilege of waiving is implied in the reason for the law. In Indiana it has been held that although the statute contains in terms an absolute prohibition, it creates no absolute incompetency and the privilege may be waived by the person for whose benefit it is made or his legal representative.[279] Under the[107] Michigan law it was claimed that the physician is forbidden to reveal confidences even though he have his patient’s consent, but it has been held that the law only creates a privilege on the same footing with other privileged communications, which the public has no interest in suppressing when there is no desire for suppression on the part of the person concerned.[280] In Missouri too the patient may waive the privilege.[281]
The protection vouchsafed by the law is designed for the benefit of the patient, and therefore the physician himself cannot waive it.[282] The patient can disclose his own physical condition if he so desires.[283]
But the physician cannot refuse to testify if the patient waives the privilege.[284]
The patient can waive the privilege during his life.[285]
As it existed prior to 1891 the New York law provided that the prohibition should operate unless it was expressly waived upon the trial or examination by the patient.[286] This was interpreted to mean that the patient himself was the only person who could make a waiver; and that, therefore, the possibility of waiver ceased with the death of the patient, while the privilege of secrecy continued unabated, so that those claiming under the deceased patient could not waive the privilege, nor insist upon[108] the testimony of the physician, even though their interests were in jeopardy on account of his silence.[287] It seems, however, that a patient can during his lifetime waive the privilege, the waiver to take effect after his death.[288] The express waiver required by the statute may be given by the patient’s attorney, because of the nature of the attorney’s agency in conducting an action for the patient.[289]
None of the other statutes are in the exact terms of the New York statute, but those of California, Colorado, Idaho, Minnesota, Montana, Nevada, North Dakota, Ohio, Oregon, South Dakota, Utah, Washington, and Wyoming provide that the testimony shall not be given unless the patient consent; in Iowa, the waiver provided for is that of the person in whose favor the prohibition is made; and in Nebraska, of the party in whose favor the provision is enacted.
In Indiana, the privilege extends beyond the death of the patient, and it may be waived by the party who may be said to stand in the place of the deceased and whose interests may be affected by the disclosure.[290]
In Michigan, what the patient may do in his lifetime, those who represent him after his death may also do for the protection of the interests which they claim under him.[291] In Missouri the representatives of the patient may waive;[292] and where the dispute is between devisees and heirs at law all claiming under a deceased patient, either the devisees or heirs may call the attending physician of the testator as a witness regarding information acquired by him in his professional attendance.[293] In[109] Nevada it has been said that the parents of a seven-year-old infant, may waive for the infant.[294]
Objections to the Admission of Privileged Communications; When and by Whom Made.—Having considered who can waive the privilege, it is material to discuss also the question who may insist upon the enforcement of the law. If the protection were only enforced on the claim of privilege by the patient, the very object of the statutes would be defeated in the large majority of instances because of the absence of the patient and every one interested in his behalf to assert his right. It rests, therefore, with any party to raise the objection and assert the prohibition. But it seems that the physician himself, unless a party, cannot make the objection.[295] It seems to have been thought in some of the cases that the right to insist upon the enforcement of the law is coupled with an interest derived from the patient. This idea started from the language used in the early cases enforcing the privilege at the instance of those claiming under deceased patients;[296] and it led to some confusion where the right of representatives to waive the privilege was denied; but it seems to be clear that the right to object differs from the right to waive in that the latter is necessarily and logically dependent upon the relation between the patient and his representative, while the former is obviously suggested as the best method of enforcing the law. In Indiana it has been said that the statute gives to the representative of a deceased patient the right to object;[297] but that this is not by reason of the relationship appears from another case in the same State, where on an application for a new trial the Court voluntarily refused to grant one for newly discovered evidence disclosed to it by a physician’s affidavit, on the ground that if the patient should object in the new trial the evidence would be excluded.[298] In this State it has been held that the widow of the patient cannot object to the[110] disclosure, if his administrator with the will annexed waives the privilege.[299]
In Michigan it has been said that the physician cannot avail himself of the statute for his own benefit; but that was in a case where the communication was not really of the privileged class.[300] In New York, in proceedings to which a physician was a party an examination of his books of account before trial has been refused on the ground of privilege, and for the same reason a motion to direct a physician to turn his books of account over to a receiver has been denied.[301]
In Montana it has been said that when the patient consents no one else can object to the reception of the physician’s testimony.[302]
In New York it has been said that the benefits of the law are to be dispensed alike to those familiar with and those ignorant of its existence and applicability, and it is therefore no reason to refuse its enforcement, that the patient did not know that his communication was privileged.[303]
But, as in other cases of the receipt of improper evidence, it would seem that the objection should be made at the time it is offered, and if the objection is not then made, it will not avail to raise it later or on appeal.[304] It should not be prematurely made.[305] In New York where in pursuance of a special feature of practice in probate proceedings,[306] certain witnesses are regarded as the surrogate’s witnesses though produced at the instance of the contestant, and the contestant, after giving notice that the evidence of physicians as such witnesses was material, refused to examine them, and the surrogate required the proponent to suggest a line of examination, it was held that it did not lie with the contestant to object to the physicians’ testimony as privileged, because she had lost her right to object by giving notice that the evidence of those witnesses on these points was material.[307]
Objection cannot be raised in the progress of an examination[111] after the forbidden testimony has been in part received without objection; for that would unjustly enable a party to open the door and get in all he desired and then to close it to the disadvantage of his adversary; when the door is once properly opened the examination may be continued until it is complete, despite the objection of the party at whose instance it was begun.[308]
In Indiana, where there was no objection, it was held that the evidence should not be withdrawn from the consideration of the jury or its weight diminished by comments on its value as matter of law.[309]
But when such evidence has already been admitted in the face of objection, it is not necessary for the party to object again, as nothing is waived by conforming with a rule already laid down.[310] Where it is apparent that no harm is done to the objecting party by an improper ruling on the receipt of privileged communications, no weight will be given to an exception to such ruling.[311]
What Constitutes a Waiver of the Privilege.—The statutory provisions as to what constitutes a waiver have been set forth above.[312] In California it has been held that cross-examination of the physician by the patient, calling for privileged matter, is a waiver of privilege.[313] In Indiana it has been held that consent to disclosure cannot be inferred from the patient’s simply giving the name of his family physician in applying for a policy of insurance on his life, and that a waiver in such an application should be evidenced by a stipulation too plain to be misunderstood.[314] And a physician’s statements of the cause of his patient’s death, furnished to an insurance company, in pursuance of a stipulation of a policy that satisfactory proof of death shall be submitted to the company, are not rendered admissible by that stipulation.[315]
It has also been held that consent to the evidence of one physician is no consent that another physician may divulge confidential[112] communications;[316] and that the physician cannot testify that he found no evidence of injury on the examination of his patient, in order to contradict her;[317] the patient had already testified as to her condition and what the physician had done, but not as to anything said to her by her physician; she had expressly declined to testify concerning communications except as to his prescription for her injury, and without asking him to disprove her assertions the trial Court permitted him to say that he had found no evidence of injury; this was held to be error. It has also been held that the taking of a physician’s deposition and filing it, for the purpose of breaking the force of his testimony in a deposition taken by the opposite party, is no consent in itself to the reading of the other party’s deposition.[318] But when, in an action against a physician for malpractice, the patient testifies as to the manner of treatment, the physician is then at liberty to introduce the testimony of himself or another physician as to the facts thus put in issue by the patient.[319]
In Iowa it has been held that the testimony of a patient regarding the condition of his health is not a waiver of privilege, so as to allow his opponent to introduce the testimony of his physician to contradict him.[320]
In Michigan a physician has been allowed to contradict his patient as to the time when her trouble commenced, but on the ground that it had not been shown that the information was necessary to enable him to prescribe.[321] But it has been held that waiver as to one physician is not waiver as to another regarding a different time.[322]
In Missouri, the calling of a physician by the patient as a witness to testify as to information acquired while attending, is a waiver.[323] But offering one physician as a witness is not a waiver of the privilege with reference to another.[324] An applicant for insurance may, by an express waiver in his application,[113] make an efficient waiver, binding upon any one claiming under the contract of insurance.[325]
In Nevada a waiver has been implied from the testimony of the patient and her mother, where the patient was an infant seven years of age.[326] And it was said that the parents of such an infant may make the waiver.
In New York it has been held that reference to a family physician when answering questions on an application for insurance, is not a waiver;[327] nor is the presence of a third person, in aid of the patient;[328] nor is the bringing of an action for damages for an injury;[329] nor is the examination of the physician in a former trial by the opposing party;[330] but where the ban of secrecy is once removed in an action and the information once lawfully made public, at the instance of the patient, it cannot be restored, and the disclosure may then be compelled in any subsequent action;[331] it would seem, too, that a physician who becomes a witness to his patient’s last will and testament at the patient’s request is then subject to a thorough examination on all points involving the patient’s testamentary capacity.[332]
Where the patient testified herself and called an attending physician to prove her physical condition, this was not a consent to the examination of another attending physician, and it was said that the opposite party by tactics on cross-examination[114] could not compel the patient to abandon a privilege which she refused to waive.[333] Fish, J., in delivering the opinion of the Court in the last-mentioned case, said of the operation of the statute, that it allows the patient to use the testimony of the attending physician if he thinks his evidence will benefit his case, and to object and exclude it in case he thinks it will not benefit him; he may call to his aid the testimony of any one whose views he approves and exclude that of another whose testimony might tend to controvert that given with the consent of the patient; that in this case the excluded witness was the best witness and could tell nothing else than the patient had disclosed if she had told the truth and it would relate solely to what she and the other physician had described, but that the Court could not consider whether the statute tended to promote the cause of justice, and he distinguished McKinney v. Grand Street Railroad Company,[334] on the ground that there the consent had been that the same physician should disclose what he knew, while here the waiver of the excluded physician’s testimony had been constantly withheld.
A decision which seems to be at variance with Record v. Village of Saratoga Springs is Treanor v. Manhattan Railway Company,[335] where it was said that the patient cannot promulgate and uncover his maladies and infirmities in court and keep his physician under obligations to silence, and that he cannot, to mulct another in damages, inflame a jury with a false or exaggerated story of his injuries and sufferings and preclude the physician from making a truthful statement of the case.
But where the patient testifies as to what passed between him and his physician, the physician may testify on the same subject, as a waiver is inferred from the circumstances; for the reason, that the patient, having gone into the privileged domain to get evidence on his own behalf, cannot prevent the other party from assailing such evidence by the only testimony available, and the rule is no longer applicable when the patient himself pretends to give the circumstances of the privileged interview.[336][115] The requirement that a physician file with a board of health a certificate of the cause of death does not abrogate the privilege in a judicial proceeding.[337]
The Evidence Excluded.
“Information.”—In Arkansas, California, Colorado, Idaho, Michigan, Minnesota, Missouri, Montana, Nevada, New York, North Carolina, North Dakota, Oregon, South Dakota, Utah, Washington, and Wisconsin the privileged matter is characterized as information.[338]
In Arkansas it seems that the information must be a confidential communication;[339] but in the other States where it has been necessary to construe the word it has received a broader interpretation.
In Michigan information is not confined to confidential communications made by the patient, but includes whatever in order to enable a physician to prescribe was disclosed to any of his senses and which in any way was brought to his knowledge for that purpose;[340] it covers a letter written to a physician,[341] and matters observed by him;[342] but it does not include information acquired by a third person; for instance, the time when a physician saw his patient may be disclosed by her mother;[343] and the fact of treatment or non-treatment is not information;[344] nor are the facts that the physician was the patient’s family physician, and that he attended him professionally; nor are statements of the dates of such attendance and the number of such visits;[345] nor the facts that the physician has been called upon to examine and prescribe for a person and that his patient had told him that she would want him to testify for her in a lawsuit.[346]
In Missouri the statute protects information received from[116] the patient; but this is not confined to oral communications, and includes knowledge gained by inspection of the patient’s person.[347] In Lunz v. Massachusetts Mutual Life Insurance Company protection was said not to extend to information of this sort apparent on casual inspection, which any one might make, nor to symptoms which are obvious before the patient submits himself to any examination, such as an inflamed face, a bloodshot eye, alcoholic fumes, or delirium; nor to facts so superficial that in regard to them no confidence could have been reposed. But this distinction between hidden and patent facts is disapproved in Kling v. City of Kansas,[348] and the statement is made that the law does not rest on the confidence imposed. Knowledge or communications concerning the cause of a patient’s condition and the extent of his injuries have also been held to be included in the term information, because the disclosure of these matters involved the indirect disclosure of the condition;[349] but it was said that the physician may testify as to knowledge acquired independent of communications from the patient and of examination or inspection made by the witness for the purpose of treatment.[350] As divulging privileged information, a physician has not been allowed to answer what his patient’s hurts were, why he left a hospital, or whether he required longer treatment;[351] and it has also been held that a physician cannot give his opinion as to the mental condition of his patient based upon privileged knowledge.[352]
In New York information comprehends all knowledge acquired by the physician by communication, observation, or inspection;[353] it has been said to extend to all facts which necessarily come to the knowledge of the physician in a given professional case;[354] and it includes as well the opinion of the physician based upon his knowledge as the knowledge itself.[355]
The physician cannot disclose the nature of his patient’s disease, whether he learned it by observation or examination or from what his patient told him;[356] nor can he testify as to what he told his patient.[357] In Edington v. Ætna Life insurance Company[358] it was said by Judge Earl that the statute was aimed at confidential communications and secret ailments, and that it did not extend to matters superficially apparent, such as a fever, a fractured leg or skull, or raving mania apparent to all;[359] but this view was disapproved expressly in the later case of Renihan v. Dennin.[360]
The privileged information has been said to include knowledge acquired through the statements of others surrounding the patient.[361] But it would seem that the fact that a third person was present during a physician’s visit may be shown by the physician, as well as what passed between the patient and the third person, if it was such information as a layman would have gathered.[362] The information from the third person regarding the patient is protected even though the patient be absent;[363] but not if the third person does not employ the physician, and the information thus acquired is not necessary to enable the physician to act in a professional capacity.[364] It is suggested in one case, but not determined, that it would be improper for a physician to state the value of the services of a nurse in attendance upon his patient, as that would involve a consideration of the condition of his patient;[365] but it has been held that a physician can testify to the fact of a nurse’s services.[366]
But it is information regarding the patient that is privileged, and therefore a physician may disclose what his patient told him about another, even though the subject of inquiry be the attitude of the patient toward the other;[367] and likewise the physician may disclose what he told his patient about a third[118] person;[368] so also the physician may testify as to family events in no way connected with physical complaints.[369] It has been held, too, that admissions made by a patient to his physician, tending to show contributory negligence on the part of the patient, at a time when the communication could not well have been made to enable the physician to prescribe, namely, on the physician’s third and last visit, may be proven by the physician.[370]
The physician may properly testify that he did attend as physician,[371] and that the patient was sick, and he can state when and how often he attended him,[372] and whether his knowledge was acquired while in professional attendance,[373] but it is open to the Court to determine from the evidence whether it was so acquired.[374]
“Matter Committed.”—In Indiana the protection covers matter committed. It would seem that the use of the word committed implies confidence and that the protected matter is only confidential communications; but an earlier statute in that State applied to “matters confided,” and it was held to cover matters learned by observation or examination, or by communication from the patient, whether learned under an injunction of secrecy, express or implied, or not;[375] and it has been held that the present law forbids the disclosure of matters learned in a sick-room, no matter how the knowledge may have been acquired.[376]
“Confidential Communications.”—The laws of Iowa and Nebraska protect confidential communications properly intrusted. The construction put upon the word confided in Indiana has been shown. In Iowa it has been said that a confidential inquiry for advice to facilitate the commission of a crime or the infraction of law, is not properly intrusted and is not privileged;[377] but where the advice is sought for a purpose[119] which may or may not be lawful, the presumption is that it is lawful, and the communication is privileged.[378] It has been said that whether or not a physician treated a person for a particular disease, is not a confidential communication.[379]
The word confidential is not narrowly construed, for a physician has been prevented from disclosing whether his patient said that a car was in motion when he was injured, because the injury would be more severe if in motion;[380] and the fact that the physician’s partner was present does not remove the seal of secrecy, or permit the partner to testify.[381]
“Communications.”—In Ohio and Wyoming communications are privileged; and in Kansas and Oklahoma communications with reference to a physical or supposed physical disease and any knowledge obtained by a personal examination of a patient. It does not appear whether a narrower construction would be given to the term communications than to the term information; but it would seem not, if a person deprived of speech is to be protected,[382] or if the term communications is not to be construed as meaning oral communications.
“From the Patient; by the Patient.”—The former qualifying terms are used in the statutes of Arkansas, Indian Territory, and Missouri; the latter in the statutes of Kansas and Oklahoma. The liberal interpretation put upon this term in the Missouri law has already been shown.[383] The law of the Indian Territory is adopted from Arkansas.[384] The statute is strictly construed in Arkansas,[385] but this term does not seem to have received interpretation.
“Advice.”—The laws of Indiana, Ohio, and Wyoming expressly cover the physician’s advice. In New York it is incompetent for the physician to disclose what he told his patient;[386] but advice to a patient concerning a third person is not privileged.[387]
The Relation of Physician and Patient.—Under each of the[120] statutes, the relation of physician and patient must have existed at the time the information was acquired. In those cases where the relation is established by contract and is recognized by both physician and patient as existing, no difficulty arises in determining that it does exist. It is in those cases where some one of these elements is lacking that the difficulties are met. In California it has been held that the relation exists where a physician attends and prescribes for a person, notwithstanding he was employed by another, who seeks to disclose the evidence.[388] In Michigan, where the physician was employed by direction of the prosecuting attorney to examine the defendant in jail, and so notified the defendant at the outset of the examination, and he submitted voluntarily to a personal examination, and there was no intention to prescribe or to act as the defendant’s physician, it was held that the relation did not exist, and that the physician could testify as to the defendant’s physical condition.[389]
In one New York case it has been said that the relation is one of contract, and that the test is whether the physician would be chargeable with malpractice or negligence for failure to advise or prescribe in case the alleged patient were in urgent need of it at the time.[390] But the decisions of the Court of Appeals extend the privilege to cases where this test would lead to a different conclusion.[391]
Where the physician to a county jail was called in to attend a prisoner and examined him, though there was no prescription at the time, but it appeared that the doctor told the prisoner what he should prescribe, and subsequently two physicians came to see the prisoner at the instance of the coroner and examined him as they would have examined one of their patients, though they did not prescribe and had no conversation about a prescription, it was held that the prisoner had, under the circumstances, reason to suppose that the relation of physician and patient did exist between him and all three of the physicians, and that their testimony as to what they learned on such visits should have been excluded; and the rule is thus stated: whenever the patient has reason to suppose that the relation exists and does in fact and truth so suppose, in a case where the physician[121] attends under circumstances calculated to induce the opinion that his visit is of a professional nature, and the visit is so regarded and acted upon by the person attended, the relation of physician and patient contemplated by the statute may fairly be said to exist.[392]
But the fact that it is the duty of a physician to prescribe for a person in case of need, does not constitute the relation, though the position of the physician gives him the opportunity to observe such person; so, therefore, a jail physician was not precluded from testifying as to what he had observed of a prisoner, where it did not appear that he had ever attended the latter in a professional capacity or had ever been called on to attend him.[393]
It would seem, however, that where it is the duty of a physician to attend a person in a professional capacity or to acquire knowledge concerning him in such capacity, he cannot disclose information actually acquired in the performance of his duty. It has been said that a medical attendant at an insane asylum cannot testify as to the mental condition of an inmate;[394] and that a physician employed in a hospital to notice and enter in its records the arrival and condition of the patients coming in, cannot testify as to information so acquired.[395]
It is immaterial that another person employs the physician to examine the patient, and to report to the employer, and that the person examined does not appear to desire any knowledge as to his condition; if the examination is made as a professional act, the relation of physician and patient is established between the physician and the person examined, even though it be the only interview.[396]
And in a case where the public prosecutor sent a physician to a person for the purpose of making a professional examination, so as to obtain evidence against another person charged with crime, and the person examined accepted the services of[122] the physician in a professional character, it was held that he could not testify as to the results of his examination.[397]
But where the district attorney sent a physician to jail to make an examination of a prisoner’s mental and physical condition, and he made such examination, and it did not appear that he prescribed for or treated the prisoner or that the prisoner accepted his services, the opinion of the physician as to his mental condition was admitted.[398]
Where the defendant employed a physician to examine the plaintiff, and he went as coming from the defendant for that purpose, and examined the plaintiff in the presence of his attending physician, but not as the plaintiff’s physician and not for the purpose of prescribing, the relation of physician and patient was not established.[399] Where a physician examined the plaintiff at the instance of the plaintiff’s physician, but it was not shown that he was requested or expected to treat or prescribe or to advise in respect to either, or that he did either, it was held that the relation was not established;[400] but a physician consulted by the patient’s regular physician for the purpose of advice concerning his treatment is a physician contemplated by the statute;[401] as is also the partner of a physician who is present during a conference with the patient or who overhears such a conference.[402] Attendance at the patient’s house is not contemplated as essential by the law, and it makes no difference where the examination is conducted.[403] But where the physician was also a county clerk and the alleged patient was an attorney, and the consultation took place in the clerk’s office and consisted of an examination of an eruption on the skin, which was made gratuitously and without a prescription being made or asked for, the relation was held not to have been established, notwithstanding that the clerk made use of his knowledge and learning as a physician in forming his opinion, and that it was[123] in confidence that he possessed medical skill that the person requested the examination.[404]
It does not follow that the relation once established continues always; the secrecy growing out of the relationship, as to knowledge then acquired, always continues unless properly waived; and the physician will not be allowed to testify in regard to matter which is partly the result of such information, though another part may have been acquired independent of the relation;[405] but where it is clear that the matter desired is independent of the relation of physician and patient, such evidence is admissible if otherwise competent.[406]
“Professional Capacity.”—The States in which the statutes limit the privilege to information acquired in a professional capacity have been enumerated.[407] As to what constitutes a professional capacity, the discussion of the facts that establish the relation of physician and patient, and of the information necessary to enable a physician to prescribe or a surgeon to act, makes it unnecessary to discuss at length the meaning of this phrase. The decision in Lunz v. Massachusetts Mutual Life Insurance Company[408] would make it appear that in Missouri information apparent on a casual inspection which any one might make is not received in a professional capacity, but this idea is disapproved in the later case of Kling v. City of Kansas.[409] Information acquired by the physician by observing the patient on the street anterior to his employment as a physician is not received by him in a professional capacity.[410]
In New York, where the physician had not seen the patient before or since his interview for the purpose of treatment, and he was asked what his opinion was, based on a general sight of the man before the examination, it was held that the physician could not properly answer, as all the information upon which[124] the opinion would be based must have been acquired in a professional capacity;[411] but in another case a physician was permitted to express his opinion as to the mental condition of a patient whom he had seen at various times when not in attendance, excluding from his mind any knowledge or information obtained while acting as her medical attendant and confining his answer to such knowledge and information as he had obtained by seeing her when not his patient.[412] It has been said that where information is not such as is obtained on sight by any person, but by removing clothing and by percussion and listening to the action of the lungs, these are professional acts and the information may be considered as obtained professionally.[413] It has been said that information received in a professional capacity involves a decision, though it may be negative; and that signing as witness to a will is not a professional act.[414]
Matter Necessary to Enable a Physician to Prescribe or a Surgeon to Act.—A list of those States whose laws limit the privilege to matter necessary to enable the witness to prescribe or act for the patient is to be found in another place.[415]
In Arkansas, where six hours after delivery, the patient stated to her physician who attended at accouchement, that she had never been engaged to marry and never had promised to marry, the statements were held not to be necessary to enable the physician to act.[416]
In Iowa, a physician who had treated a patient for injuries was not allowed to testify whether his patient told him that the car on which he was injured was in motion at the time, because as the injury would be likely to be more severe if the car was in motion, that information was necessary to enable the physician to prescribe.[417]
In Michigan, a physician was allowed to contradict his patient as to when her trouble commenced, in the absence of evidence that such information was necessary to enable him to act.[418] Where a physician was asked whether he treated a person for[125] typhoid fever, and he answered that she was not so diseased, it was held that this information was not necessary to enable him to act.[419] And the same was held to be true where a physician examined a prisoner at the jail and testified that he was diseased, the prisoner having been notified at the time of the examination that it was made by direction of the prosecuting attorney and there being no intention to prescribe or act for the prisoner.[420] But it has been stated that all disclosures by a patient to a physician respecting ailments are privileged whether necessary to enable the physician to prescribe or not.[421]
In Minnesota, a physician was allowed to disclose statements as to suffering made by his patient, but not for the purpose of enabling him to prescribe or act.[422]
In Missouri, it has been said that information as to the way in which an injury was inflicted is of the greatest necessity for successful treatment; and that it is information which physicians universally demand and receive.[423] In another case, with reference to the cause of a patient’s condition, it was said that while knowledge of the cause may not be necessary, the disclosure of the cause cannot be made without a disclosure of the condition, and that as a medical person cannot tell indirectly what he is forbidden to tell directly, the physician’s evidence of the cause is inadmissible.[424] In another case it was said that any information, necessarily coming to a physician in order to treat his patient, is to be regarded as necessary information though unimportant, and that the test is how it was acquired, not whether it could have been acquired in a different way, and therefore it was incompetent for a physician to testify that his patient was drunk when he treated him.[425]
In New York, in an early case,[426] where a man consulted a physician with reference to committing an abortion and told him that a certain woman was pregnant by him, this admission was said not to be essential to enable him to prescribe, even if[126] the relation of physician and patient were considered established; but this seems to be at variance with the later case of People v. Brower,[427] where the accused consulted a physician with reference to the treatment of a woman on whom he had attempted to commit an abortion, and admitted that he had done so, and the physician was not permitted to disclose it. A broader view is now taken of the word necessary. It has been held by the Court of Appeals that a physician could not testify that his patient had a venereal disease while under his care as a physician, the presumption being that he learned it for the purpose of prescribing;[428] and again, that it is assumed from the relationship that the information would not have been imparted except for the purpose of aiding the physician to prescribe.[429] But this presumption does not attach to information regarding a patient, communicated by a third person.[430]
Where a person went to a physician to call for medicine, and it appeared that he was not consulting for himself and was not representing any one else who needed or desired medical assistance, the physician was allowed to testify as to a conversation which took place at that time.[431]
In the case of Edington v. Ætna Life Insurance Company,[432] it was said that before the exclusion, the facts on which it is justified must appear in some way, and the Court must know somewhat of the circumstances; from the opinion it is easy to infer that it is only confidential communications and information as to secret ailments which may be regarded as necessary within the statute; but this view was overruled in Grattan v. Metropolitan Life Insurance Company,[433] and there it was distinctly stated that it is enough that the witness acquired the information in his character as physician and in the due and proper exercise of his calling, and that it is not incumbent on the person objecting, to show by formal proof that the information was necessary to enable the witness to prescribe. In this case the examination of the witness was as to the cause of his[127] patient’s death, and the argument urged upon the attention of the Court was that information regarding the cause of death could not be necessary to enable the physician to prescribe, as the utility of the prescription ceased with the death and before the cause was determined; but the Court held that the privilege attached, because, although the death was the result of the cause, the facts constituting the cause were learned while the physician was attending the living patient in a professional capacity and from the symptoms manifested at that time.
In consonance with the decision in Grattan v. Metropolitan Life Insurance Company,[434] it has been held that a physician who amputated a patient’s leg could not testify as to its condition at the time it was amputated.[435]
The fact that the physician does not prescribe does not defeat the privilege; if the information is acquired in the course of professional employment the statute operates, for the decision that neither advice nor medicine is needed is a professional act within the spirit of the law.[436] Medicus optimus, medicamentum minimum, is the maxim used in another case to illustrate this point.[437]
But it cannot be predicated as matter of law that a physician cannot exclude from his consideration facts learned or opinions formed while attending as physician; therefore he can testify as to his opinion on hypothetical facts which might be deemed to relate to another person as well as the patient; and where the physician testified that he could so form an opinion, his opinion of such assumptions was held to be admissible in evidence as expert testimony.[438]
But it is not all information which will be presumed to have been necessary to enable the physician to act; it seems that where the knowledge is such that it is evidently immaterial to the physician’s decision, it will be admitted. Such a case is that of Hoyt v. Hoyt,[439] where the testimony of physicians was admitted to show the attitude of their patient toward his daughter[128] and their advice to him concerning her, the evidence being for the purpose of showing the testator’s opinion and not the physicians’. It has also been held that a statement made by a patient on the physician’s last visit as to what occurred at the time the patient was injured, tending to show contributory negligence, was not necessary information.[440] And a physician’s evidence of the declaration of his patient as to making a will and the doctor’s advice on that subject have been admitted.[441]
THE PROVINCE OF THE COURT IN DEALING WITH THE PRIVILEGE.
All questions of the competency of evidence are solved by the Court and not by the jury.[442] The facts establishing the privilege are presented to the Court for its consideration. In Iowa it has been held that a fair trial demands that it should not be made to appear to the jury in an action that the patient is reluctant to waive his privilege, and that therefore the subject-matter of waiver has no place in the taking of testimony except when introduced by the party permitted to make it, and the Court should not allow the patient to be asked to answer under oath whether he is willing to waive his privilege.[443]
Whether it is the duty of the Court to enforce the privilege where it is apparent and the patient is not present to object, is a question that seems to be variously regarded. In Indiana a court has refused a new trial for newly discovered evidence of the privileged sort, on the ground that if objection were madeon the new trial it would be rejected.[444] But where the evidence of a physician to contradict another physician, who was witness to a will, was received without objection, it was said that it should not be withdrawn by the Court from the consideration of the jury or its value commented on as matter of law.[445]
In Michigan, it has been said that a commissioner, whose ordinary duty is to take all evidence offered, should refuse to take this privileged evidence; and that it should be stricken out[129] without motion by the judge when returned by the commissioner, and that the physician should not be allowed to violate the privilege.[446] It has also been held that an order for the compulsory physical examination of a person by a physician for the purpose of testifying should not be granted, and that evidence so obtained should be stricken out, but on the ground that it was a violation of personal liberty, rather than of statutory privilege.[447]
But in New York it has been held that where a person voluntarily in an action exhibits an injured part as evidence, the adverse party is entitled to follow it up by a personal or professional inspection of the injured part.[448]
In Missouri, it has been said that the physician should be told that he is not at liberty to testify as to privileged information.[449]
In New York, in an early case in chancery, the chancellor said that a master was wrong in supposing there was legal evidence before him, where a physician had given evidence privileged under the statute;[450] but this decision was reversed on appeal, the Court of Errors saying that as no objection was made before the master by a party, the evidence was competent and legal.[451] This question seems to have been settled in New York by the decision in Hoyt v. Hoyt,[452] that the law does not prohibit the examination of a physician but it prohibits the evidence being received in the face of objection, so that if no objection is made by a party it is not the province of the Court to reject the evidence.
Where it appears that privileged information was improperly admitted, it is not ground for reversal on appeal if it is apparent that the appellant was not injured by its reception.[453]
Where the Court is not empowered to reject the evidence of[130] its own motion, the objection upon which it can reject is the objection of a party to the suit, and doubtless of the patient, but not of the physician.[454] But because of the privilege, it has been held that a physician will not be ordered to turn over his books of account to a receiver appointed in proceedings supplementary to an execution on a judgment against him.[455] Nor will examination of his books of account before trial be compelled.[456]
It is the province of the courts, however, to enforce the law and not to legislate by grafting exceptions upon it.[457] They have refused therefore to except, by judicial decision, from the operation of the law, criminal proceedings, testamentary causes, evidence of crime in civil actions, cases of lunacy and habitual drunkenness and fraud,[458] in all of which it was urged in argument without effect that the administration of justice was impeded by the privilege; but where the spirit of the law was violated by an enforcement of its letter and the privilege made a cloak to shield the murderer of the patient, it was held to be inapplicable.[459] The courts have also refused by mere judicial decision to limit the privilege to the life of the patient.[460]
THE EFFECT OF ENFORCING THE PRIVILEGE.
The courts are not warranted in admitting incompetent evidence in order to prevent the failure of justice by the exclusion of the privileged testimony. A letter written by a physician is inadmissible as evidence of the privileged facts which it states;[461] and a certificate of the cause of death, required by law to be signed by the physician and filed, is not admissible to prove the cause of death in an action in which the physician cannot testify.[462]
The making of the objection does not raise a presumption[131] against the person making it.[463] In Iowa it has been held that the patient should not be interrogated under oath as to whether or not he will waive his privilege, for the jury ought not to be prejudiced against him by any show of reluctance.[464] In Michigan, however, it has been held that a patient’s failure to produce his physician as a witness is a legitimate fact for the jury to consider.[465]
THE CHARACTER AND WEIGHT OF THE EVIDENCE TO SUSTAIN THE OBJECTION.
Where the objection is made, the burden of proof to establish the grounds of privilege is upon the person objecting.[466] In Missouri it has been said that the statement of the physician, that he cannot separate his impressions received in his relation of physician from those received at other times, is not in itself sufficient to justify the exclusion of his evidence; that the facts themselves must appear to the Court, and it might be developed on proper cross-examination that discrimination could be made.[467]
But it would seem that because of the necessarily delicate nature of the inquiry, to avoid disclosing what the statute forbids, the burden is overcome with slight evidence, and inferences and presumptions are freely indulged in aid of the privilege; for instance, where the physician was not permitted to answer whether he did converse with his patient about an injury, or whether he made an examination with reference to it, it was urged that the objection was prematurely made, but it was held that the fact that the patient consulted a physician on the occasion to which the inquiry related, when considered with the nature of the questions, justified the exclusion in the absence of other proof.[468] But the physician may testify that he did[132] attend his patient as physician;[469] and he may answer the question whether the information was necessary to enable him to act in his professional capacity;[470] for while his testimony on that point is not conclusive, and the Court uses its own judgment in reaching a determination, his testimony is competent evidence.[471] He may also testify that a person was ill and was his patient, that he attended as physician, and he can state when he attended and how many times.[472]
It has been said that where the evidence justifies the conclusion that information regarding the patient is acquired while attending in a professional capacity, it is not essential to show by formal proof that the information was necessary.[473]
THE RIGHTS AND DUTIES OF THE PHYSICIAN WITH REFERENCE TO THE PRIVILEGE.
The privilege established by law is a rule of evidence, and not a regulation of a physician’s general conduct outside of a proceeding in which rules of evidence are applicable.[474] The courts have, however, not hesitated to intimate that it is a physician’s duty to observe the same secrecy in his general walk and conversation.[475]
The physician may testify as an expert on hypothetical questions submitted to him regarding facts which might be equally true of any other person than his patient, and excluding from his consideration privileged knowledge.[476] And he may also testify as to matters which came to his knowledge before or after or independent of his employment as physician,[477] or which were immaterial to his acting in a professional capacity, and as[133] to which his patient could have had no reasonable ground for believing that they were necessarily disclosed in order that the physician might so act.[478] It is the patient’s privilege and not the physician’s; and, therefore, the physician is not absolutely incompetent as a witness, and has no right to refuse to testify.[479] But where he is a party he may object and then he will not be forced to disclose his patient’s confidence.[480]
In Indiana it has been held that where the patient testifies in an action against his physician for malpractice the physician is then at liberty to testify or to introduce any other witness to testify concerning the matters in controversy.[481]
In Michigan, a physician who was plaintiff in a libel suit was not permitted to insist upon the privilege to prevent the disclosure of his maltreatment of his patient or what other physicians had discovered with regard to it by visits to his patients.[482]
The measure of the physician’s exemption and liability in testifying is the language of the statute, and not his idea of his duty to his patient or the patient’s injunctions of confidence or secrecy.[483]
In some of the States there are statutory provisions entitling physicians to sue for compensation for their professional services.[484] The statutes regarding privileged communications are to be construed together with these. There seems to be no reason why a physician’s right of action for his services and medicines should not survive the prohibition of his evidence; but it would seem that he cannot as a witness in such an action testify regarding privileged matter. But he can prove it by other witnesses.[485]
THE RESULT OF THE LEGISLATION.
It is doubtless due to considerations of public policy that the statutes changing the common-law rule have been enacted;[486] but they have not proved an unalloyed benefit, and some of their features have brought about conditions which in some cases have embarrassed the administration of justice. The law in New York may be taken for illustration; it formerly cut off the safest means of ascertaining the mental condition and competency of a testator;[487] it now precludes a physician from disclosing the condition of his patient who is a lunatic or habitual drunkard,[488] though it be the most satisfactory evidence; it shuts out much testimony tending to show fraud in insurance cases;[489] it precludes a physician from stating the cause of his patient’s death,[490] though there is no longer any secrecy connected with it, for the law makes it the duty of the physician to make, for filing with the local board of health, a certificate of the probable cause of the death of a patient.[491] It has been the subject of much adverse criticism,[492] but all such considerations are properly to be addressed to the legislature and not to the courts. It seems to be the most far-reaching in its exclusion, and though it has been the longest in existence, was modified at the legislative sessions of 1891, 1892, and 1893, a fact which tends to show that there was sound reason in the criticisms.
A SYNOPSIS OF THE LAWS
OF THE
SEVERAL STATES AND TERRITORIES OF THE UNITED STATES OF
AMERICA, AND OF GREAT BRITAIN AND IRELAND, AND
OF THE NORTH AMERICAN PROVINCES OF GREAT
BRITAIN, REGULATING THE PRACTICE
OF MEDICINE AND SURGERY,
PREPARED FROM THE LATEST STATUTES.
BY
WILLIAM A. POSTE,
Late First Deputy Attorney-General of the State of New York,
AND
CHARLES A. BOSTON, Esq.,
of the New York City Bar.
SYNOPSIS OF THE EXISTING STATUTES
WHICH REGULATE
THE ACQUIREMENT OF THE RIGHT TO PRACTISE MEDICINE AND SURGERY IN THE UNITED STATES, GREAT BRITAIN AND IRELAND, AND THE CANADIAN PROVINCES.
[Note.—This synopsis is designed to contain especially those provisions of the statutes which regulate the right to practise medicine and surgery. It is not intended to include provisions regulating apothecaries, druggists, chemists, and dentists, or the sale of drugs, medicines, and poisons; nor provisions for the organization and procedure of boards of medical examiners, except so far as they regulate the requirements demanded from applicants for permission to practise; nor provisions with reference to the duties of clerks or registrars in the preparation and safe-keeping of records in their care; nor those defining the duties of members of boards, and punishing the misconduct of such members; nor those prescribing qualifications for appointment to the public medical service; nor former laws not now applicable to candidates; nor regulations of the form of certificates or licenses, where the issuing of them is committed to some public functionary or body; nor provisions with reference to the powers and disabilities of local institutions to confer diplomas or degrees, nor with reference to medical students except as candidates for admission to practise. In the synopsis words of the masculine gender are uniformly used except when the law by its terms makes a distinction between men and women, in which case the distinction is indicated.]
Alabama.
Qualification.—The board of censors of the Medical Association of the State of Alabama and the board of censors of the county medical societies in affiliation with the said association are boards of medical examiners (Code 1887, s. 1,301). In the absence of such board of medical examiners in any county, the[138] county commissioners may establish a board of from three to seven physicians of good standing, resident in the county, whose authority shall terminate whenever a board is organized in accordance with the constitution of and in affiliation with said association (ib., s. 1,296). Where the board of examiners is constituted as provided in sec. 1,296, it must issue a license to practise medicine in any one or more of its branches in the county, if on examination the applicant is found duly qualified, and is of good moral character (ib., s. 1,297).
In a county having only the medical board provided for in sec. 1,296, a regular graduate of a medical college in the United States, having a diploma, is entitled to practise medicine without a license, upon recording his diploma in the office of the judge of probate of the county (ib., s. 1,298).
A license issued by the last-mentioned board must be recorded in the office of the judge of probate of the county (ib., s. 1,299). The license or diploma, after record, is evidence of authority; if the original be lost, a certified copy of the record is sufficient evidence (ib., s. 1,300). Without a certificate of qualification from the board provided for in sec. 1,301, except as above provided, no person can lawfully practise medicine in any of its branches or departments as a profession or means of livelihood (ib., s. 1,302). The standard of qualification, method or system, and subjects of examination are prescribed by the medical association of the State (ib., s. 1,303).
The board of medical examiners, on application, must examine an applicant for a certificate of qualification as a practitioner of medicine, and if he be found qualified, and of good moral character must issue a certificate (ib., s. 1,304).
Physicians having a license as above before the organization in a county of a board, are on application thereto entitled to a certificate without examination and to be registered as licensed practitioners of medicine (ib., s. 1,305).
The certificate is a license throughout the State. It must be recorded in the office of the judge of probate of the county in which the person resides at the time of issue. Upon recording it, the judge must indorse a certificate of record and sign it and affix the seal of the court (ib., s. 1,306). Such certificate, or, if lost, a certified copy of the record, is evidence (ib., s. 1,307).
Penalty.—A contract for the services of a physician or surgeon is void unless he has authority to practise; proof of authority is not required at trial except on two days’ notice (ib., s. 1,318).
Practising medicine or surgery without a certificate is a misdemeanor under a penalty of a fine of from $25 to $100. This provision is not applicable to physicians practising medicine in Alabama in 1890, who are graduates of a respectable medical college and have complied with the law by having their diplomas recorded by the judge of probate in the county where they practise; nor to a physician who has practised in the State for the past five years (Act 1890-91, c. 376); nor to women practising midwifery (Code 1887, s. 1,308).
Fees.—The statutory fees are as follows:
To judge of probate, for record of diploma, or license or certificate, $1 (ib., s. 1,298, 1,299, 1,306).
To board of medical examiners, for examination, actual expenses (ib., s. 1,304).
Arizona.
Qualification.—It is unlawful for any person to practise medicine, surgery, or other obstetrics unless he have a diploma regularly issued by a medical college lawfully organized under the laws of the State wherein it is located, or a license issued and authorized by a board of medical examiners under and by virtue of the laws of any State or Territory. The diploma must state that the person named is qualified to practise medicine and surgery in all of its departments (Penal Code, 1887, s. 617, as amended Act of April 11th, 1893).
A diploma granted for moneyed consideration or other article of value alone, or revoked or cancelled by the college by which it was issued or by act of the legislature, is not a sufficient qualification (ib., s. 618).
Every practitioner of medicine, surgery, or obstetrics must register in the county recorder’s office his name, residence, and place of birth, and present his diploma or license, and the county recorder must make a copy of it under the record of his name, residence, and place of birth. The person registering must subscribe and verify an affidavit in writing, annexed to the copy[140] as transcribed, that he is the identical person named in the diploma (ib., s. 619, as amended by Act of April 11th, 1893).
Definition, Exception.—Any person is regarded as practising medicine who professes publicly to be a physician or habitually prescribes for the sick, or appends to his name “M. D.,” but the act does not prohibit gratuitous services in cases of emergency; nor apply to lawfully commissioned surgeons and assistant surgeons of the United States army and those who were commissioned and mustered into the United States service in the great rebellion, or physicians or surgeons who have been in active practice for ten years and at least three years in the Territory, nor prevent practice and receiving pay in localities fifteen miles or more from the residence or office of a regular physician (ib., s. 620).
Offence.—Violation of the act is a misdemeanor (ib., s. 621).
Fees.—To the county recorder, for registration, $5 (ib., s. 619).
Arkansas.
Qualification.—It is unlawful for any one to engage in the practice of medicine and surgery, or either, as a calling except as provided in the statute (Act April 14th, 1893, s. 1).
A person engaging in the practice of medicine or surgery must be of good moral character, twenty-one years of age, and a graduate of some reputable college of medicine and surgery that requires for graduation not less than two courses of lectures, each in a different year (ib., s. 2).
Before engaging in practice, such person must exhibit his diploma to some county clerk of the State and have it recorded. The clerk must give him a certificate of record, which may be attached to the diploma (ib., s. 3).
In all cases of doubt as to the reputability of a college, it is the duty of the clerk of the county court, when a diploma is offered for record, to make inquiry of the Secretary of the State where the said college exists as to its reputability and requirements for graduation, and if the said clerk shall find that the said college does not conform to the requirements of this article, he shall not receive the diploma and the holder shall not be allowed to practise in the State. The aggrieved applicant may[141] apply to the State board of medical examiners, whose decision shall govern the clerk in his action (ib., s. 4).
If after recording any diploma it shall come to the knowledge of the clerk making the record, or any other judicial or executive officer of the State, that the record was obtained by fraud or misrepresentation, it shall be his duty to institute before the said court of record proceedings to have such record reversed, and the holder of the diploma shall be judged guilty of a misdemeanor (ib., s. 5).
Exceptions.—The act does not affect the standing of any one practising at the time of its passage by virtue of a license under the then existing law, nor any one then legally engaged in the practice of medicine and surgery, nor does it prevent midwives from practising their calling or any one else from giving such simple domestic remedies as they are in the habit of using (ib., s. 6).
Examinations.—The constituted State board of medical examiners is authorized to examine persons having no diploma from a medical college, and if found qualified to practise medicine and surgery issue a certificate entitling the holder to practise in this State (ib., s. 7).
Systems, Definition.—No discrimination of schools of medicine is allowed. Any person who prescribes or administers medicine except as provided in sec. 6 is deemed a physician (ib., s. 8).
Penalty.—The violation of this act is a misdemeanor punishable with a fine of from $25 to $100. Each day of practice is a separate offence (ib., s. 9).
Date.—The act took effect ninety days after its passage (ib., s. 10).
Fees.—To the county clerk, for recording, $1.50.
For certificate of record the county clerk is not allowed to charge a fee (ib., s. 3).
California.
Qualification.—Every person practising medicine or surgery in any of its departments must present his diploma to the board of examiners with affidavits. If the board finds all facts required to be stated in the affidavit to be true, it issues a[142] certificate conclusive in any part of the State (Act 1877-78, c. 576; amending Act 1875-76, c. 518).
The secretary of the board receives applications. The board issues certificates to all who furnish satisfactory proof of having received diplomas or licenses from legally chartered medical institutions in good standing (Act 1875-76, c. 518, s. 3).
The medical society of the State, the eclectic medical society of the State, and the State homœopathic medical society each appoint annually a board of seven examiners who must be regular graduates (Act 1877-78, c. 576; amending Act 1875-76, c. 518).
The board examines diplomas as to genuineness. The affidavit accompanying the diploma must state that the applicant is its lawful possessor, and the person therein named; that the diploma was procured in the regular course of medical instruction and without fraud or misrepresentation of any kind, and that the medical institution granting it had, at the time of granting the same, a full corps of medical instructors, and was at said time a legally incorporated institution, actually and in good faith engaged in the business of medical education, and in good standing as a medical institution, and that the applicant had complied with all the requirements of said institution. The affidavit may be taken before any person authorized to administer oaths, and must be attested under the hand and official seal of the officer, if he have a seal. The board may hear such further testimony as they deem proper to hear as to the verification of the diploma or the identity of the person, or the manner in which the diploma was procured, and if it appears that any fact stated in the affidavit is untrue, the application is rejected. No board entertains an application rejected by another; a rejected application cannot be renewed for at least one year (ib., s. 4, as amended by Act 1877-78, c. 918); no certificates are granted except to persons presenting diplomas or licenses from legally chartered medical institutions in good standing (ib., s. 5).
Certificates must be recorded in the county of residence and the record indorsed thereon. A person removing to another county to practise must procure an indorsement to that effect on his certificate from the county clerk, and must record the certificate in the county to which he removes (ib., s. 6).
The board refuses certificates to individuals guilty of unprofessional conduct. The applicant is given an opportunity to be heard, by citation; the attendance of witnesses may be compelled by subpœna; witnesses may be examined at the hearing by either side, and either side may examine medical experts as to whether such conduct is unprofessional; if it appears to the satisfaction of the board that the applicant is guilty of the unprofessional conduct set out in the citation, no certificate can be granted. No application is refused for unprofessional conduct more than one year before the application. If the holder of a certificate is guilty of unprofessional conduct, the certificate must be revoked by board granting it; no revocation is valid without similar proceedings to the foregoing (ib., s. 10).
Definition.—Any person is regarded as practising medicine who professes publicly to be a physician, or habitually prescribes for the sick, or appends to his name “M.D.”
Exceptions.—The act does not prohibit gratuitous services in cases of emergency; nor apply to lawfully commissioned surgeons of the United States army or navy practising their profession (ib., s. 11, as amended 1877-78, c. 576).
Itinerant Venders.—A license of $100 a month is exacted from itinerant venders of drugs, nostrums, ointments, or appliances for treatment of disease, and from persons publicly professing to cure or treat disease, injury, or deformity by any medicine, drug, or drugs, nostrum, manipulation, or other expedient (Act 1877-78, c. 576, amending Act 1875-76, c. 518, s. 12).
Penalty.—The penalty for violation of the act is a fine of from $50 to $500, or imprisonment in the county jail from 30 to 365 days, or both, for each and every offence. Filing or attempting to file the diploma or certificate of another, or a forged affidavit of identification, is a felony, punishable the same as forgery (ib., s. 13; Act 1877-78, c. 918, s. 7).
Former Practitioners.—Holders of certificates theretofore granted by the board of examiners existing by the appointment of the California State Medical Society of Homœopathic Practitioners are excused by the Act 1877-78, c. 918, s. 7, from obtaining new certificates.
Rejected Applicant.—A certificate issued by one board[144] to an applicant rejected by another within a year is null and void (ib., s. 9).
Fees.—To secretary of board, for examining genuine diploma, $5.
If diploma fraudulent or property of another, $20 (Act 1877-78, c. 576, s. 3; amending Act 1875-76, c. 518, s. 4).
To county clerk, for recording certificate, usual recording fees (Act 1875-76, c. 518, s. 6).
Colorado.
Board of Examiners.—The State board of medical examiners is composed of nine practising physicians of known ability and integrity, graduates of medical schools of undoubted respectability, six of the regular school, two of the homœopathic, and one of the eclectic school or system, appointed by the governor (Mills’ “Annotated Statutes” 1891, s. 3,547).
Qualification.—Every person practising medicine must possess the required qualifications. If a graduate in medicine, he must present his diploma to the State board of medical examiners for verification, or furnish other evidence conclusive of his being a graduate of a legally chartered medical school in good standing. The board issues its certificate, and such diploma or evidence and certificate are conclusive. If not a graduate of a legally chartered medical school in good standing, the person must present himself before the board for examination. All persons who have made the practice of medicine and surgery their profession or business continuously for ten years, and can furnish satisfactory evidence thereof to the State medical examiners, shall receive a license to continue (ib., s. 3,550).
Examinations of persons not graduates are made by the State board, wholly or partly in writing, in anatomy, physiology, chemistry, pathology, surgery, obstetrics, and practice of medicine (exclusive of materia medica and therapeutics) (ib., s. 3,553).
The holder of a certificate should have it recorded in the office of the clerk of the county in which he resides, and the record indorsed thereon, and on removing to another county to practise should procure an indorsement to that effect on the certificate[145] from the county clerk, and record this certificate in the county to which he removes (ib., s. 3,554).
The board may refuse certificates to persons convicted of conduct of criminal nature; and may revoke certificates for like cause (ib., s. 3,356).
Definition.—Professing publicly to be a physician and prescribe for the sick, or attaching to name “M.D.,” or “surgeon” or “doctor” in a medical sense, is regarded as practising medicine. Gratuitous services in case of emergency are not prohibited (ib., s. 3,557).
Penalty.—The penalty for violation of the act is a fine of from $50 to $300, or imprisonment in the county jail from ten days to thirty days, or fine and imprisonment for each offence; filing or attempting to file the diploma or certificate of another, or false or forged evidence, is a felony punishable the same as forgery (ib., s. 3,558).
System of Medicine.—Certificates are issued without prejudice, partiality, or discrimination as to schools or systems of practice or medicine, including the electropathic school (ib., s. 3,561).
Fees.—To treasurer of board by graduates and practitioners of ten years’ standing, $5. By candidates for examination, $10 (ib., s. 3,552).
To county clerk, for recording certificate, $1 (ib., s. 3,554).
Connecticut.
Qualification, Exceptions.—After October 1st, 1893, no person shall for compensation, gain, or reward, received or expected, treat, operate, or prescribe for any injury, deformity, ailment, or disease, actual or imaginary, of another person, nor practise surgery or midwifery unless or until he has obtained a certificate of registration, and then only in the kind or branch of practice stated in the certificate, but the act does not apply to dentists practising dentistry only, nor to any person in the employ of the United States Government while acting in the scope of his employment, nor to medical or surgical assistance in cases of sudden emergency, nor to any person residing out of the State who shall be employed to come into the State to assist or consult with any physician or surgeon who has been[146] registered in conformity with the act, nor to any physician or surgeon then actually residing out of the State who shall be employed to come into the State to treat, operate, or prescribe for any injury, deformity, ailment, or disease from which any person is suffering at the time when such non-resident physician or surgeon is so employed, nor to any actual resident of this State recommending by advertisement or otherwise the use of proper remedies sold under trade-marks issued by the United States Government, nor to any chiropodist or clairvoyant not using in his practice any drugs, medicines, or poisons, nor to any person practising the massage method or Swedish movement cure, sun cure, mind cure, magnetic healing, or Christian science, nor to any other person who does not use or prescribe in his treatment of mankind drugs, poisons, medicine, chemicals, or nostrums (Act 1893, c. 148, s. 1).
Any resident of the State who, at the time of the passage of the act, was or previously had been actually engaged in the State in the practice of medicine, surgery, midwifery, or any alleged practice of healing, may, before October 1st, 1893, file with the State board of health duplicate statements subscribed and sworn to by him upon blanks furnished by said board, giving his name, age, and place of birth and present residence, stating whether he is a graduate of any medical college or not, and of what college, and the date of graduation, and if practising under a license from any of the medical societies of the State, which society and the date of such license and the length of time he has been engaged in practice in the State, and also elsewhere, and whether in general practice or in a special branch of medicine or surgery, and what branch. On receipt of such statements, the board shall issue a certificate of registration which shall state the kind or branch of practice in which he is engaged (ib., s. 2).
Any person who shall, subsequent to October 1st, 1893, file with said board such duplicated statements, showing that he is a graduate of a medical college recognized as reputable by any chartered medical society of the State, shall receive a certificate of registration which shall state the kind or branch of practice in which the person named therein is engaged or is to be engaged (ib., s. 3).
Any person residing in any town in another State which[147] town adjoins the boundary line of Connecticut, who was actually engaged in such town, at the time of the passage of the act, in the practice of medicine, surgery, or midwifery, or any branch of practice, may before October 1st, 1893, obtain from the said board a like certificate on filing such duplicated statements also showing that he is entitled to such certificate under this section (ib., s. 4).
Except as above provided, no person shall after October 1st, 1893, obtain a certificate of registration until he has passed a satisfactory examination before a committee appointed by said board, nor until he has filed with the said board duplicate certificates as aforesaid, signed by a majority of one of said examining commissioners, stating that they have found him qualified to practise either medicine, surgery, or midwifery, and any person filing said certificates shall receive from said board a certificate of registration (ib., s. 5).
The State board of health, in January, 1894, is to appoint three examining commissions, each of five physicians nominated respectively by the Connecticut Medical Society, the Connecticut Homœopathic Medical Society, and the Connecticut Eclectic Medical Association, and recommended by the said societies respectively as persons competent to serve upon the said examining commissions. Appointments are to be made thereafter from time to time by similar nominations (ib., s. 6 and 7).
The State board of health shall designate when and where the commissions shall hold examinations, but shall call a meeting of a commission within thirty days after the receipt of an application for examination. Applicants shall be examined in anatomy, physiology, medical chemistry, obstetrics, hygiene, surgery, pathology, diagnosis, and therapeutics, including practice and materia medica. Each commission shall frame its own questions and conduct its examinations in writing, and both questions and answers shall be placed on file with the board. Each applicant may choose by which of the commissions he will be examined.
After rejection by any examining commission, the applicant shall not be eligible to examination by another commission until after the expiration of twelve months (ib., s. 8).
On the receipt of duplicate statements, the board shall transmit[148] one of them with a duplicate certificate of registration to the town clerk of the town where the person filing the statement resides, and if he does not reside in the State to the town clerk of the town in the State nearest to his place of residence, and said clerk shall record the same and return them to the person who filed them with the board (ib., s. 9).
The secretary of each medical society shall file with the secretary of the State board of health a list of medical colleges or institutions recognized as legal and reputable by his society or all of such secretaries may agree upon a single list, and such list may be corrected from time to time (ib., s. 10).
Penalty.—The violation of sec. 10 shall be a misdemeanor, punishable with a fine of from $100 to $300 for the first offence, and for each subsequent offence by a fine of from $200 to $500 or imprisonment in the county jail for from thirty to ninety days, or both (ib., s. 11); swearing falsely to a statement is perjury (ib., s. 12).
Fees.—To the State board of health, on filing statements or certificates, $2 (ib., s. 2, 3, 4, 5).
To examining commission, before examination, their expenses not exceeding $10 (ib., s. 8).
To the town clerk, by State board of health out of the amount paid to it, for recording, 25 cents (ib., s. 9).
Delaware.
Qualification.—It is unlawful to practise medicine or surgery without a license (Laws 1887, vol. 18, c. 35, s. 1, as amended by Laws 1889, vol. 18, c. 518).
The medical board of examiners for the State must grant a license to any person applying therefor who shall produce a diploma from a respectable medical college, or shall, upon full and impartial examination, be found qualified for such practice (Rev. Stats., c. 47, s. 3). The board consists of as many fellows of the Medical Society of Delaware as the society deems proper (ib., s. 3).
The clerk of the peace of a county, on presentation of a license issued by the board of examiners of the Homœopathic Medical Society of Delaware State and Peninsula, under its corporate seal, signed by its president and countersigned by its[149] secretary, or of the license provided by sec. 3, c. 47, of the Revised Statutes, or on the affidavit of a person that he or she has practised medicine or surgery for eight years continuously in the State, and upon such person registering his name, the date of his graduation and college (if a graduate), and his place of intended residence, must issue a license (ib., s. 2).
A person opening a transient office or assigning a transient office by printed or written advertisement, must comply with the foregoing provisions and pay special license fee for a license good only for one year (Laws 1887, vol. 18, c. 35, s. 5).
Penalty.—The violation of this law is a misdemeanor punishable by a fine of from $100 to $300 (ib., s. 7).
Exceptions.—The present law exempts those who complied with the Act of April 19th, 1883, and also regular practitioners of another State in consultation with a lawful practitioner of medicine and surgery of this State (ib., s. 4, 6).
Fees.—To clerk of the peace, for issuing license to practise, $10.50 (Laws 1887, vol. 18, c. 35, s. 4). For issuing annual license for revenue of the State, $10.50 (Laws, vol. 13, c. 117, as amended, vol. 14, c. 16).
To secretary of board, for license, $10 (Rev. Stats., c. 47, s. 5).
A license fee to practise medicine, for the revenue of the State, is also required (ib., s. 8; vol. 13, c. 117, as amended, vol. 14, Laws, c. 16).
District of Columbia.
Registration.—It is the duty of every physician, accoucheur, and midwife practising medicine, or doing business, to register at the office of the board of health, giving full name, residence, and place of business, and in case of removal from one place to another in the District to make a change in the register (Regulation of Board of Health, August 28th, 1874, s. 8, legalized by resolution of Congress, No. 25, s. 2, April 24th, 1880).
Violation.—The violation of the foregoing provision is punishable by a fine of from $25 to $200 for every offence (ib., s. 9).
Qualification.—All physicians required to register must[150] do so upon a license from some chartered medical society or upon a diploma from some medical school or institution (ib., s. 11 [First]).
Florida.
Boards of Examiners.—The governor appoints a board of medical examiners for each judicial circuit, and a board of homœopathic examiners for the State (Rev. Stats., 1892, s. 801).
The circuit board is composed of three practising physicians of known ability, graduates in good standing of a medical college, recognized by the American Medical Association, residents of the circuit; the homœopathic board is composed of three practising homœopathic physicians of known ability, graduates in good standing of a medical college recognized by the American Institute of Homœopathy (ib., s. 802).
Qualification.—It is the duty of the board of examiners to examine thoroughly every applicant, upon the production of a medical diploma from a recognized college, upon anatomy, physiology, surgery, gynæcology, therapeutics, obstetrics, and chemistry, but no preference is given to any school of medicine; and it is the duty of the board of homœopathic medical examiners to examine thoroughly every applicant, upon the production of his diploma from a college recognized by the American Institute of Homœopathy, on anatomy, physiology, surgery, gynæcology, materia medica, therapeutics, obstetrics, and chemistry, but no preference is given to any school of medicine (Rev. Stats., 1892, s. 806).
When the board is satisfied as to the qualifications of the applicant, they grant a certificate which entitles him to practise medicine in any county, when recorded (ib., s. 807). Any two members of the board may grant a certificate. Any member may grant a temporary certificate, upon examination, until the next regular meeting, at which time the temporary certificate ceases to be of effect (ib., s. 808). Before he shall be entitled to practise, the certificate must be recorded in the office of the clerk of the circuit court of the county in which he may reside or sojourn; and the clerk must certify thereon, under official seal, the fact and date of the record, and return the certificate (ib., s. 809).
A practitioner engaged in the practice of medicine in any department prior to May 31st, 1889, upon the production of a diploma from a medical college recognized by the American Medical Association, is granted a certificate, without further examination and without charge (ib., s. 811).
Exceptions.—This act is not applicable to persons who have complied with prior laws, nor to females practising midwifery, strictly as such. No other person shall practise medicine in any of its branches or departments, without having obtained and recorded a certificate (ib., s. 812).
Penalty.—Practising as a physician without a certificate is punishable by imprisonment not exceeding six months, or a fine not exceeding $200 (ib., s. 2,669).
Fees.—To clerk, legal fee for recording (ib., s. 809).
To board, $10 from each applicant whether certificate granted or not (ib., s. 810).
Georgia.
The Code of 1882, s. 1,409 (a) as amended by chap. 413, Laws 1882-83, provides that—
Qualification.—No person is to practise medicine, unless he was theretofore legally authorized, or is hereafter authorized by a diploma from an incorporated medical college, medical school or university, or has after attending one or more full terms at a regularly chartered medical college, been in active practice of medicine since the year 1866, or was by law authorized to practise medicine in 1866, and by compliance with the statute.
Definition.—To “practise medicine” means to suggest, recommend, prescribe, or direct, for the use of any person, any drug, medicine, appliance, apparatus, or other agency, whether material or not material, for the cure, relief, or palliation of any ailment or disease of mind or body, or for the cure or relief of any wound, fracture, or other bodily injury, or any deformity, after having received or with the intent of receiving therefor, either directly or indirectly, any bonus, gift, or compensation (ib., s. 1,409 [b]).
Registration.—Every person now lawfully engaged in practice must register on or before December 1st, 1881; every[152] person hereafter duly qualified shall, before commencing to practise, register in the office of the clerk of the superior court of the county wherein he resides and is practising, or intends to practise, his name, residence, and place of birth, together with his authority; he shall subscribe or verify, by oath or affirmation, before a person duly qualified to administer oaths under the laws of this State, an affidavit containing such facts, and whether such authority is by diploma or license, and the date of the same, and by whom granted, which shall be exhibited to the county clerk, before the applicant is allowed to register, and which, if wilfully false, is punishable as false swearing (ib., s. 1,409 [c]).
Removal.—A registered physician changing his residence from county to county must register in the clerk’s office of the county to which he removes and wherein he intends to reside and to practise medicine (ib., s. 1,409 [d]).
Penalty.—The violation of this law or practising, or offering to practise, without lawful authority, or under cover of a diploma or license illegally obtained, is a misdemeanor, punishable by a fine of from $100 to $500, or imprisonment from thirty to ninety days, or both (ib., s. 1,409 [e]).
Exceptions.—Commissioned medical officers of the United States army or navy, or United States marine hospital service, and women practising only midwifery, are not affected (ib., s. 1,409 [f]).
Medical Boards.—All medical boards are abolished, and only the qualifications of practitioners of medicine set forth above are required (ib., s. 1,409 [g]).
Fees.—To county clerk, fifty cents for each registration (ib., s. 1,409 [c]).
Tax.—On practitioners of physic, $5 per annum (ib., s. 809).
Idaho.
Qualification.—No person can lawfully practise medicine or surgery who has not received a medical education, and a diploma from a regularly chartered medical school, having a bona fide existence when the diploma was granted (Rev. Stats., 1887, s. 1,298).
A physician or surgeon must file for record with the county[153] recorder of the county in which he is about to practise, or where he practises, a copy of his diploma, at the same time exhibiting the original, or a certificate from the dean of a medical school certifying to his graduation (ib., s. 1,298 [a]).
When filing the copy required, he must be identified as the person named in the papers, by the affidavit of two citizens of the county, or by his affidavit taken before a notary public or commissioner of deeds for this State; and the affidavit is filed in the office of the county recorder (ib., s. 1,298 [b]).
Penalty.—Practising without complying with the act is a misdemeanor, punishable by a fine of from $50 to $500, or imprisonment in a county jail from thirty days to six months, or both fine and imprisonment for each offence.
Filing or attempting to file as his own the diploma or certificate of graduation of another, or a forged affidavit of identification, is a felony; subject to fine and imprisonment (ib., s. 1,298 [c]; ib., s. 6,312).
Exceptions.—The act is not applicable to a person in an emergency prescribing or giving advice in medicine or surgery, in a township where no physician resides within convenient distance, nor to those who have practised medicine or surgery in this State for ten years preceding the passage of this act, nor to persons prescribing in their own families, nor to midwifery in places where no physician resides within convenient distance (ib., s. 1,298 [e]; as amended by Act of February 7th, 1889).
Fees.—No special fees are enumerated in the statute. The county recorder’s fees for services are prescribed in Rev. Stats., 1887, s. 2,128.
Illinois.
Qualification.—No person can lawfully practise medicine in any of its departments unless he possesses the qualifications required. If a graduate in medicine, he must present his diploma to the State Board of Health for verification as to its genuineness. If the diploma is found genuine, and from a legally chartered medical institution in good standing, and if the person named therein be the person claiming and presenting the same, the board must issue a certificate conclusive as to his right to practise medicine. If not a graduate, the person must present[154] himself before the said board and submit to examination, and if the examination is satisfactory the board must issue certificate (Laws 1887, p. 225, s. 1).
The verification of a diploma consists in the affidavit of the holder and applicant that he is the person therein named. The affidavit may be taken before any person authorized to administer oaths, and attested under the hand and official seal of such officer (if he have a seal). Swearing falsely is perjury. Graduates may present their diplomas and affidavits by letter or proxy (ib., s. 3).
All examinations of persons not graduates or licentiates are made by the board; and certificates authorize their possessor to practise medicine and,surgery (ib., s. 4).
The certificate must be recorded in the office of the clerk of the county in which the holder resides within three months from its date, and the date of recording indorsed. Until recorded, the holder cannot lawfully exercise the rights and privileges conferred. A person removing to another county to practise must record his certificate in the county to which he removes (ib., s. 5).
Examinations may be wholly or partly in writing and shall be of elementary and practical character, but sufficiently strict to test the qualifications of the candidate as a practitioner (ib., s. 8).
The board may refuse to issue a certificate to a person guilty of unprofessional or dishonorable conduct, and may revoke for like causes. The applicant in case of a refusal or revocation may appeal to the governor and his decision will be final (ib., s. 9).
Definition.—“Practising medicine” is defined as treating, operating on, or prescribing for any physical ailment of another. The act does not prohibit services in case of emergency, nor the domestic administration of family remedies, and does not apply to commissioned surgeons of the United States army, navy, or marine hospital service in the discharge of official duty (ib., s. 10).
Itinerant Vender.—An itinerant vender of drug, nostrum, ointment, or appliance intended for treatment of disease or injury, or professing by writing, printing, or other method to cure or treat disease or deformity by drug, nostrum, manipulation,[155] or other expedient, must pay a license fee of $100 per month into the treasury of the board. The board may issue such license. Selling without a license is punishable by fine of from $100 to $200 for each offence. The board may for cause refuse a license (ib., s. 11).
Penalty.—Practising medicine or surgery without a certificate is punishable by a forfeiture of $100 for the first offence, and $200 for each subsequent offence; filing or attempting to file as his own the certificate of another, or a forged affidavit of identification, is a felony, punishable as forgery.
Exceptions.—The act saves for six months after its passage the right of persons who have practised continuously for ten years in the State prior to its passage, to receive a certificate under former act. But all persons holding a certificate on account of ten years’ practice are subject to all requirements and discipline of this act in regard to their future conduct; all persons not having applied for or received certificates within said six months, and all persons whose applications have for the causes named been rejected, or their certificates revoked, shall, if they practise medicine, be deemed guilty of practising in violation of law (ib., s. 12).
Penalty.—On conviction of the offence mentioned in the act, the court must, as a part of the judgment, order the defendant to be committed to the county jail until the fine and costs are paid (ib., s. 13).
Fees.—To the secretary of the board, for each certificate to a graduate or licentiate, $5 (ib., s. 2).
For graduates or licentiates in midwifery, $2 (ib., s. 2).
To county clerk, usual fees for making record.
To treasury of board, for examination of non-graduates: $20, in medicine and surgery; $10, in midwifery only.
If the applicant fails to pass, the fees are returned. If he passes, a certificate issues without further charge (ib., s. 7).
Indiana.
Qualification.—It is unlawful to practise medicine, surgery, or obstetrics without a license (Act April 11th, 1885, s. 1).
The license is procured from the clerk of the circuit court of[156] the county where the person resides or desires to locate to practise; it authorizes him to practise anywhere within the State; the applicant must file with the clerk his affidavit stating that he has regularly graduated in some reputable medical college, and must exhibit to the clerk the diploma held by him, his affidavit, and the affidavit of two reputable freeholders or householders of the county stating that the applicant has resided and practised medicine, surgery, and obstetrics in the State continuously for ten years immediately preceding the date of taking effect of this act, stating particularly the locality or localities in which he has practised during the said period, and the date and length of time in each locality; or his affidavit and the affidavit of two reputable freeholders or householders of the county, stating that he has resided and practised medicine, surgery, and obstetrics in the State continuously for three years immediately preceding the taking effect of this act, and stating particularly the localities in which he practised during the said period, and the date and length of time in each locality, and that he, prior to said date, attended one full course of lectures in some reputable medical college. The clerk must record the license and the name of the college in which the applicant graduated, and the date of his diploma (ib., s. 2, as amended by Act March 9th, 1891).
A license issued to a person who has not complied with the requirements of sec. 2, or one procured by any false affidavit, is void (Act April 11, 1885, s. 3).
Penalty.—Practising medicine, surgery, or obstetrics without a license is a misdemeanor punishable with a fine of from $10 to $200 (ib., s. 4).
No cause of action lies in favor of any person as a physician, surgeon, or obstetrician who has not prior to the service procured a license; and money paid or property paid for such services to a person not so licensed, or the value thereof, may be recovered back (ib., s. 5).
Exemptions.—Women practising obstetrics are exempted from the provisions of the act (ib., s. 4).
Fees.—To clerk, for license, $1.50 (Act April 11th, 1885, as amended Act March 9th, 1891).
Registration.—It is the duty of all physicians and accoucheurs to register their name and post-office address with[157] the clerk of the circuit court of the county in which they reside (Act 1881, p. 37, s. 10).
Fees.—To the clerk, for registration, 10 cents (ib., s. 11).
Iowa.
Qualification.—Every person practising medicine, surgery, or obstetrics, in any of their departments, if a graduate in medicine, must present his diploma to the State board of examiners for verification as to its genuineness. If the diploma is found genuine, and is by a medical school legally organized and of good standing, which the board determines, and if the person presenting be the person to whom it was originally granted, then the board must issue a certificate signed by not less than five physicians thereof, representing one or more physicians of the schools on the board (sic), and such certificate is conclusive. If not a graduate, a person practising medicine or surgery, unless in continuous practice in this State for not less than five years, of which he must present to the board satisfactory evidence in the form of affidavits, must appear before the board for examination. All examinations are in writing; all examination papers with the reports and action of examiners are preserved as records of the board for five years. The subjects of examination are anatomy, physiology, general chemistry, pathology, therapeutics, and the principles and practice of medicine, surgery, and obstetrics. Each applicant, upon receiving from the secretary of the board an order for examination, receives also a confidential number, which he must place upon his examination papers so that, when the papers are passed upon, the examiners may not know by what applicant they were prepared. Upon each day of examination all candidates are given the same set or sets of questions. The examination papers are marked on a scale of 100. The applicant must attain an average determined by the board; if such examination is satisfactory to at least five physicians of the board, representing the different schools of medicine on the board, the board must issue a certificate, which entitles the lawful holder to all the rights and privileges in the act provided (Laws 1886, c. 104, s. 1).
The board receives applications through its secretary. Five[158] physicians of the board may act as an examining board in the absence of the full board; provided that one or more members of the different schools of medicine represented in the State board of health shall also be represented in the board of examiners (ib., s. 2).
The affidavit of the applicant and holder of a diploma that he is the person therein named, and is the lawful possessor thereof, is necessary to verify the same, with such other testimony as the board may require. Diplomas and accompanying affidavits may be presented in person or by proxy. If a diploma is found genuine and in possession of the person to whom it was issued, the board, on payment of the fee to its secretary, must issue a certificate. If a diploma is found fraudulent or not lawfully in possession of the holder or owner, the person presenting it, or holding or claiming possession, is guilty of a misdemeanor, punishable with a fine of from $20 to $100 (ib., s. 3).
The certificate must be recorded in the office of the county recorder in the county wherein the holder resides, within sixty days after its date. Should he remove from one county to another to practise medicine, surgery, or obstetrics, his certificate must be recorded in the county to which he removes. The recorder must indorse upon the certificate the date of record (ib., s. 4).
Any one failing to pass is entitled to a second examination within twelve months without a fee; any applicant for examination, by notice in writing to the secretary of the board, is entitled to examination within three months from the time of notice, and the failure to give such opportunity entitles such applicant to practise without a certificate until the next regular meeting of the board. The board may issue certificates to persons who, upon application, present a certificate of having passed a satisfactory examination before any other State board of medical examiners, upon the payment of the fee provided in sec. 3 (ib., s. 6, as amended c. 66, Laws 1888, 22 Gen. Assembly).
The board may refuse a certificate to a person who has been convicted of felony committed in the practice of his profession, or in connection therewith; or may revoke for like cause, or for palpable evidence of incompetency, and such refusal or[159] revocation prohibits such person from practising medicine, surgery, or obstetrics, and can only be made with the affirmative vote of at least five physicians of the State board, in which must be included one or more members of the different schools of medicine represented in the said board; the standing of a legally chartered medical college from which a diploma may be presented must not be questioned except by a like vote (ib., s. 7).
Definition, Exceptions.—Any person is deemed practising medicine, surgery, or obstetrics, or to be a physician, who publicly professes to be a physician, surgeon, or obstetrician, and assumes the duties, or who makes a practice of prescribing, or prescribing and furnishing medicine for the sick, or who publicly professes to cure or heal by any means whatsoever; but the act does not prohibit students of medicine, surgery, or obstetrics from prescribing under the supervision of preceptors or gratuitous services in case of emergency; nor does it apply to women at the time of its passage engaged in the practice of midwifery, nor does it prevent advertising, selling, or prescribing natural mineral waters flowing from wells or springs, nor does it apply to surgeons of the United States army, navy, or marine hospital service, nor to physicians defined therein who have been in practice in this State for five consecutive years, three years of which must have been in one locality, provided such physician shall furnish the State board with satisfactory evidence of such practice and shall procure a proper certificate, nor to registered pharmacists filling prescriptions, nor does it interfere with the sale of patent or proprietary medicines in the regular course of trade (ib., s. 8).
Penalty.—A person practising medicine or surgery without complying with the act, and not embraced in the exceptions, or after being prohibited as provided in sec. 7, is guilty of a misdemeanor punishable with a fine of from $50 to $100, or imprisonment in the county jail from ten to thirty days (ib., s. 9).
Filing or attempting to file as one’s own the diploma of another, or the certificate of another, or a diploma or certificate with the true name erased and the claimant’s name inserted, or a forged affidavit of identification, is forgery (ib., s. 10).
Fees.—To county recorder, 50 cents (ib., s. 4).
To State board, for certificate to holder of diploma, $2 (ib., s. 3).
To secretary of State board, in advance, by candidate for examination, $10 (ib., s. 6).
By practitioner for five years, $2 (ib., s. 8).
Kansas.
Qualification.—It is unlawful for a person who has not attended two full courses of instruction and graduated in some respectable school of medicine, either of the United States or of some foreign country, or who cannot produce a certificate of qualification from some State or county medical society, and is not a person of good moral character, to practise medicine in any of its departments for reward or compensation, for any sick person; provided in all cases when any person has been continuously engaged in practice of medicine for ten years or more, he shall be considered to have complied with the provisions of the act (Gen. Stats., 1889, s. 2,450).
Penalty.—Practising or attempting to practise medicine in any of its departments or performing or attempting to perform any surgical operation in violation of the foregoing is punishable with a fine of from $50 to $100; and a second violation, in addition to a fine, is punishable with imprisonment in the county jail for thirty days; and in no case wherein the act is violated shall the violator receive a compensation for services rendered (ib., s. 2,451).
Kentucky.
Qualification.—It is unlawful for any person to practise medicine in any of its branches who has not exhibited and registered in the county clerk’s office, in the county in which he resides, his authority to practise, with his age, address, place of birth, and the school or system of medicine to which he proposes to belong. The person registering must subscribe and verify by oath before such clerk an affidavit containing such facts, which, if wilfully false, subjects the affiant to punishment for perjury (Act 1893, April 10th, s. 2).
Authority to practise shall be a certificate from the State board of health issued to any reputable physician who is practising, or who desires to begin to practise, who possesses a diploma from a reputable medical college legally chartered under the laws of this State, or a diploma from a reputable and legally chartered medical college of some other State or country, indorsed as such by said board, or satisfactory evidence from the applicant that he was reputably and honorably engaged in the practice of medicine in the State prior to February 23d, 1864. Applicants may present their credentials by mail or proxy (ib., s. 3).
Nothing in the law authorizes any itinerant doctor to register or practise medicine (ib., s. 4).
The board may refuse a certificate to any individual guilty of grossly unprofessional conduct of a character likely to deceive or defraud the public, and may, after due notice and hearing, revoke such certificates for like cause. In cases of refusal or revocation the applicant may appeal to the governor, whose decision affirming or overruling the decision of the board shall be final (ib., s. 5).
Systems, Exceptions.—The law does not discriminate against any peculiar school or system of medicine, nor prohibit women from practising midwifery, nor prohibit gratuitous services in case of emergency, nor apply to commissioned surgeons in the United States army, navy, or marine hospital service, nor to a legally qualified physician of another State called to see a particular case or family, but who does not open an office or appoint a place in the State to meet patients or receive calls (ib., s. 6).
Penalty.—Any person living in this State or coming into this State who shall practise medicine or attempt to practise medicine in any of its branches, or perform or attempt to perform any surgical operation for or upon any person for reward or compensation in violation of this law, shall be punished with a fine of $50, and on each subsequent conviction by a fine of $100 and imprisonment for thirty days, or either, or both; and in no case where any provision of this law has been violated shall the violator be entitled to receive compensation for services rendered. To open an office for such purpose or to announce to the public in any other way a readiness to[162] practise medicine in any county shall be to engage in the practice of medicine (ib., s. 8).
Fees.—To the county clerk, for all services required, 50 cents (ib., s. 1).
Louisiana.
Constitutional Provision.—The general assembly must provide for the interest of State medicine in all its departments, and for the protection of the people from unqualified practitioners of medicine (Const. 1879, Art. 178).
Qualification.—No person is allowed to practise medicine or surgery as a means of livelihood in any of its departments without first making affidavit before a judge, justice of the peace, clerk of district court, or notary public in the parish wherein he resides, of his having received the degree of doctor of medicine from a regularly incorporated medical institution of respectable standing, in America or in Europe, and designating its name and locality, and the date of his diploma; the degree is manifested by the diploma, and the respectable standing of the institution is evidenced by the indorsement or certificate of the State board of health, written on the face of the diploma, and signed by its secretary; the affidavit must contain the full name of the person making the same, the date and place of his birth, and the names of the places where he may have previously practised medicine or surgery; a record of the diplomas certified must be presented by the State board of health, and copies thereof, certified by the secretary, are received in evidence. The State board of health is required to certify the diploma of any medical institution of credit and respectability without regard to its system of therapeutics and whether the same be regular, homœopathic, or eclectic (Act 1882, No. 31, s. 1).
The affidavit required by sec. 1 must be recorded in the office of the clerk of the district court of the parish; the clerk must certify the recordation by indorsement on the original affidavit, which the affiant must transmit to the State board of health; a copy of the original affidavit, duly certified by the clerk of the court, is admissible in evidence (ib., s. 2).
Exceptions.—The provisions of the act do not apply to female practitioners of midwifery as such, nor to persons who had been practising medicine or surgery in the State without[163] diplomas for five years prior to the passage of the act, nor to persons who had been practising medicine or surgery from a regularly incorporated medical institution of reputable standing in America or in Europe, for ten years prior to the passage of the act, provided such a practitioner make affidavit before a judge, justice of the peace, notary public, or the clerk of the court of the parish wherein he resides, setting forth the full name of the affiant, the date and place of his birth, the date of his diploma, if he have any, the name and locality of the institution by which it was made, the date and place where he began the practice of medicine in Louisiana, and the names of the places where he may have previously practised medicine or surgery such affidavit must be transmitted or delivered to the State board of health, and entitles the affiant to be placed on the list of registered physicians or surgeons. The State board of health must preserve said affidavits, and a copy signed by the secretary is received in evidence by the courts. To make a false affidavit is perjury (ib., s. 3).
Evidence.—A copy of the affidavit recorded by the clerk of the district court, certified by him, is prima facie evidence that the person making the affidavit is a duly registered physician or surgeon, and a certified copy of the original affidavit filed with the State board of health, or a certificate emanating from the said board, that the name of the person mentioned in the certificate is on the list of registered physicians and surgeons, is conclusive evidence (ib., s. 4).
It is the duty of the State board of health to publish annually in the official journal of the State, and if there is none, in one of the daily newspapers published in New Orleans, a list of the registered physicians and surgeons, and their places of residence, and such published list is evidence in the courts that the person is duly registered. The board is required to strike from said list the names of persons convicted of any infamous crimes by any court of this State or of the United States, or of any State of the United States, whether prior or posterior to registration; and is empowered to strike from the list persons who die after registration (ib., s. 5).
Civil Penalty.—A practitioner of medicine or surgery failing to comply with this act shall not be exempt from military or jury duty, nor be permitted to collect fees for services rendered,[164] nor be allowed to testify as a medical or surgical expert in legal or State medicine, in any court, nor to execute any certificate as surgeon or physician, nor to hold any medical office, nor to be recognized by the State, or any parish, or municipal corporation, as a physician or surgeon, nor entitled to enjoy any of the privileges, rights, or exemptions granted to physicians and surgeons by the laws of this State; and shall forfeit $100 for each violation, to be recovered in a civil action in the name of and for the benefit of the Charity Hospital at New Orleans, and in addition shall be subject to criminal prosecution (ib., s. 6).
Exceptions.—The act is not applicable to practitioners of medicine or surgery residing and practising in other States, who may be summoned in special instances to attend patients in the State of Louisiana by any registered physician (ib., s. 7).
Penalty.—Whoever shall practise or offer to practise medicine or surgery, for pay, without complying with the foregoing act, is guilty of a misdemeanor, punishable by a fine of not less than $50 or imprisonment for not more than three months, or both, at the discretion of the court (Act 1886, No. 55, s. 1).
No criminal prosecution shall bar the imposition of a fine by civil process, nor shall the imposition of such fine bar criminal prosecution (ib., s. 2).
Exceptions.—This act is not applicable to practitioners of medicine or surgery residing and practising in other States, who may be summoned in special instances to attend patients in the State by any registered physician (ib., s. 3).
Fees.—To board of health, for every diploma certified, 50 cents (ib., s. 1).
To officer before whom affidavit is made, 50 cents (ib., s. 2, 3).
Recording same, $1 (ib., s. 2).
To clerk of court, for copy of original affidavit, 50 cents (ib., s. 2).
To State board of health, for copy of original affidavit, 50 cents (ib., s. 3).
Maine.
Qualification, Penalty.—No person who has not received a medical degree at a public medical institution in the United States, or a license from the Maine Medical Association, shall[165] recover compensation for medical or surgical services, unless previous to such service he had obtained a certificate of good moral character from the municipal officers of the town where he then resided (Rev. Stats., 1883, c. 13, s. 9).
Maryland.
Qualification.—By the Act of 1892, c. 296, s. 1, 39, it is provided that every person not now practising medicine and surgery, who shall hereafter begin to practise medicine and surgery in any of its departments, shall possess the qualifications required by the act.
There are two boards of examiners, representing the medical and chirurgical faculty of the State and the State Homœopathic Medical Society respectively; each consists of seven members, appointed respectively by those societies, physicians actually engaged in the practice of medicine, and of recognized ability and honor; but no physician having a pecuniary interest in the trade of pharmacy can be appointed (ib., s. 2).
Suitable provisions must be made by each examining board to prepare a schedule of written examination upon anatomy, physiology, chemistry, surgery, practice of medicine, materia medica and therapeutics, obstetrics, gynæcology, pathology, medical jurisprudence and hygiene; the same standard of excellence is required from all candidates; in therapeutics and practice, the questions must be in harmony with the tenets of the school selected by the candidate; and the standard of acquirements therein is established by each board itself. The examination must be fundamental in character and such as can be answered in common by all schools of practice (ib., s. 1, 42).
Application for license is made in writing to the president of either board of medical examiners which the applicant may elect, with satisfactory proof that the applicant is more than twenty-one years of age, is of good moral character, has obtained a competent common-school education, and has either received a diploma conferring the degree of Doctor of Medicine from some legally incorporated medical college in the United States, or a diploma or license conferring the full right to practise all the branches of medicine and surgery in some foreign country, and has also both studied medicine three years and[166] attended three courses of lectures in different years in some legally incorporated medical college or colleges prior to the granting of the diploma or foreign license; two courses of medical lectures both begun or completed within the same calendar year do not satisfy the requirement; this condition is not applicable to students who shall be in their second year in a medical college, nor to physicians practising at the time of the passage of the act. Such proof is made, if required, upon affidavit, upon making the application and proof and payment of the fee. The president of the board, if satisfied, must direct the secretary to issue an order for examination, and when the applicant shall have passed an examination as to proficiency satisfactory to the board, the president must grant a license to practise medicine and surgery (ib., s. 1, 43).
All of the examinations are conducted so that the name, school of graduation, and preparatory training of the applicant shall not be made known to the board till his examination papers have been graded. An applicant receiving a majority of the votes of the board is considered to have passed a satisfactory examination and is entitled to a license (ib., s. 1, 44).
The board must refuse a license to an applicant radically deficient in any essential branch. In case of a failure, the candidate must have the privilege, after the expiration of one year from his rejection, of another examination by the board to which his application was first made (ib., s. 1, 46).
A license, or a certified copy, must be filed with the clerk of the circuit court of the county or city in which the licensee may practise; the number of the book and page containing the recorded copy must be noted in the body of license.
Evidence.—The records have the same weight as evidence that is given to the record of conveyances of land (ib., s. 1, 48).
Exceptions.—The act does not apply to commissioned surgeons of the United States army, navy, or marine hospital service, to physicians or surgeons in actual consultation from other States, nor to persons temporarily practising under the supervision of an actual medical preceptor, nor to a midwife or person who may render gratuitous services in case of emergency (ib., s. 1, 49, 51).
Penalty.—Practising, or attempting to practise, without a license is a misdemeanor punishable with a fine of from $50[167] to $200 for each offence, with confinement in jail, in default of payment, till fine and costs are paid; a person so practising is debarred from recovering compensation (ib., s. 1, 50).
Fees.—To secretary of board, before examination, $10 (ib., s. 1, 45).
To clerk of court, for registration, $1 (ib., s. 1, 48).
Massachusetts.
In Massachusetts there is no statute upon this subject.
Michigan.
Qualification.—It is unlawful to practise medicine or surgery or any branch except dentistry, without the prescribed qualifications and registration in the office of the county clerk (Laws 1883, c. 167, s. 1).
A person who was practising when the law took effect, and had been practising continuously for at least five years prior thereto in the State, is deemed qualified to practise medicine after registration (ib., s. 2, as amended 1887, c. 268).
A graduate of a legally authorized medical college in the State, or any of the United States, or any other country, is deemed qualified to practise medicine and surgery in all departments after registration. A student or undergraduate is not prohibited from practising with and under the immediate supervision of a person legally qualified to practise medicine and surgery (ib.).
A person qualified registers by filing with the county clerk of the county where he practises, or intends to practise, a sworn statement setting forth, if actually engaged in practice, the length of time he has been engaged in such continuous practice; if a graduate of a medical college, the name and location of the same, when he graduated and how long he attended the same, and the school of medicine to which he belongs; if a student or undergraduate, how long he has been engaged in the study of medicine and where, and if he has attended a medical college, its name and location and the length of his attendance, and when, and the name and residence of the physician under whose instruction he is practising, or intends to practise. The statement is to be recorded by the clerk (ib.).
Penalty.—No person practising medicine, surgery, or midwifery can collect pay for professional services unless at the time of rendering such services he was duly qualified and registered (ib., s. 4).
Advertising, or holding out to the public, as authorized to practise medicine or surgery, when not authorized, is a misdemeanor punishable with a fine of from $5 to $50 for each offence (ib., s. 7).
Fees.—To county clerk, for recording statement, 50 cents (ib., s. 2).
Minnesota.
Board of Examiners.—The governor appoints a board of medical examiners of nine members, no one of whom can be a member of a college or university having a medical department, and two of whom must be homœopathic physicians (Act 1887, c. 9, s. 1).
Qualification.—Persons commencing the practice of medicine and surgery in any of its branches must apply to the board for a license, and at the time and place designated by the board, or at a regular meeting, submit to an examination in anatomy, physiology, chemistry, histology, materia medica, therapeutics, preventive medicines, practice of medicine, surgery, obstetrics, diseases of women and children, of the nervous system, of the eye and ear, medical jurisprudence, and such other branches as the board deems advisable, and present evidence of having attended three courses of lectures of at least six months each; the examination must be scientific and practical, but of sufficient severity to test the candidate’s fitness to practise medicine and surgery. When desired, the examination may be conducted in the presence of the dean of any medical school or the president of any medical society of this State. After examination, the board must grant, with the consent of at least seven members, a license to practise medicine and surgery, which may be refused or revoked for unprofessional, dishonorable, or immoral conduct; and in case of refusal or revocation, the applicant may appeal to the governor (ib., s. 3).
The license must be recorded with the clerk of the district court in the county in which the licensee resides; if he moves into another county he must procure a certified copy of his[169] license from the said clerk and file it with the clerk of the district court in the latter county (ib., s. 4).
Penalty.—To practise without a license is a misdemeanor, punishable by a fine of from $50 to $100, or imprisonment in county jail from ten to ninety days, or both. Appending “M.D.” or “M.B.” to name, or prescribing, directing, or recommending for use any drug or medicine or other agency for the treatment, care, or relief of any wound, fracture, or bodily injury, infirmity, or disease, is regarded as practising medicine.
Exceptions.—The act is not applicable to dentists (ib., s. 6), nor to commissioned surgeons of the United States army or navy, nor to physicians or surgeons in actual consultation from other States or Territories, nor to actual medical students practising medicine under the direct supervision of a preceptor (ib., s. 5).
All persons licensed under the Act of 1883, c. 125, are regarded as licensed under this act (ib., s. 7).
Fees.—To treasurer of board, for examination, $10.
Mississippi.
Qualification.—A practitioner of medicine must obtain a license from the State board of health (Code 1892, s. 3,243).
Application is made in writing; and an examination is made in anatomy, chemistry, obstetrics, materia medica, physiology, pathology, surgery, and hygiene, and if the applicant is found by the board to possess sufficient learning in those branches, and of good moral character, the board issues a license to practise medicine, signed by each member who approves (ib., s. 3,244).
The application must state the applicant’s full name, place of residence, and post-office address, nativity and age, time spent in medical studies, name and post-office address of the preceptor under whom his medical studies were pursued, the courses of medical lectures attended, the name of medical schools attended; if a graduate of a medical college, the name thereof; the time spent in a hospital, the time spent in the practice of medicine, if any, the school or system of practice chosen, and references as to his personal character (ib., s. 3,245).
Examinations are to be conducted at the capital on the first Tuesday in April and October annually, and continue until all applicants are examined and the examinations are approved or disapproved; they are upon written questions and answers, and no distinction can be made between applicants because of different systems or schools of practice.
The license must be filed in the office of the clerk of the circuit court of the county in which the licensee resides, within sixty days from the date of its issue; otherwise it becomes void. The clerk must record the same with his certificate of filing and deliver the original to the licensee. When the licensee changes the county of his residence and usual practice, he must file the original or a certified copy of license, or record, in the office of said clerk in the county into which he shall move and practise within sixty days of the time of his removal, to be there recorded (ib., s. 3,249).
The board may issue a duplicate in place of a lost license (ib., s. 3,250).
The secretary of the board may issue a temporary license which shall be valid until the next succeeding meeting of board, such license to show its date of issue, otherwise to be void; it must be recorded as a permanent license is required to be; only one temporary license shall ever be issued to the same person, and it shall always be made to an individual and not to a partnership (ib., s. 3,251).
Physicians practising by virtue of a license under prior laws are not required to obtain a license under this law and may continue in practice under their licenses, but they must comply with the requirements of this law with reference to recording (ib., s. 3,252).
Penalty.—To practise without an examination and a license is punishable with a fine of from $20 to $200, or to imprisonment in the county jail not to exceed thirty days (ib., s. 1,258).
Exceptions.—Females engaged in the practice of midwifery need no license for that employment (ib., s. 3,253).
Non-Residents.—Licensed physicians residing without the State, and whose practice extends into it, may obtain a license without examination by presenting an application in the form prescribed; whereupon the secretary of the board must issue a license in the name of the board and the license must be recorded[171] as hereinbefore provided, in each county in which the licensee shall practise (ib., s. 3,254).
Fees.—To board, before examination, $10.
To secretary, before examination, 25 cents (ib., s. 3,247).
To secretary, for temporary license, 25 cents (ib., s. 3,251).
To secretary, for license to non-resident, 25 cents (ib., s. 3,245).
To the clerk of the court, for recording, his legal fees (ib., s. 3,249).
Missouri.
Qualification.—Every person practising medicine and surgery, in any of their departments, must possess the qualifications required. If a graduate of medicine, he must present his diploma to the State board of health for verification as to its genuineness. If the diploma is found to be genuine, and the person named therein to be the person claiming and presenting the same, the board must issue a certificate which is conclusive of the right to practise. If not a graduate, he must submit to such examination as the board shall require, and if the examination is satisfactory to the examiners the board must issue its certificate in accordance with the facts, and the holder shall be entitled to all the rights and privileges herein mentioned (Rev. Stats., 1889, s. 6,871).
The board must issue certificates to all who furnish satisfactory proof of having received a diploma or license from a legally chartered medical institution in good standing, of whatever school or system of medicine, and shall not make any discrimination against the holders of genuine licenses or diplomas under any school or system of medicine (ib., s. 6,872).
The verification of a diploma consists in the affidavit of the holder and applicant that he is the lawful possessor of the same, and the person therein named; the affidavit may be taken before any person authorized to administer oaths, and shall be attested under the hand and official seal of such officer, if he have a seal. Graduates may present their diplomas and affidavits by letter or proxy (ib., s. 6,873).
All examinations are made directly by the board, and the certificates authorize the possessor to practise medicine and surgery in the State (ib., s. 6,874).
The certificate must be recorded in the office of the county clerk of the county in which the holder resides and the record must be indorsed thereon; a person moving to another county to practise must procure an indorsement to that effect on the certificate from the said clerk, and have the certificate recorded in the office of the clerk of the county to which he removes (Ib., s. 6,875).
Examinations may be made wholly or partly in writing and must be of an elementary and practical character, but sufficiently strict to test the qualifications of the candidate as a practitioner (Ib., s. 6,877).
The board may refuse a certificate to an individual guilty of unprofessional or dishonorable conduct, and may revoke a certificate for like causes after giving the accused an opportunity to be heard (Ib., s. 6,878).
Definition, Exception.—A person is regarded as practising medicine who professes publicly to be a physician and to prescribe for the sick, or who appends to his name “M.D.,” but students are not prohibited from prescribing under the supervision of a preceptor, and gratuitous services may be rendered in case of emergency, and the act does not apply to commissioned surgeons of the United States army or navy or marine hospital service (ib., s. 6,879).
Itinerant Venders.—Every itinerant vender of any drug, nostrum, ointment, or appliance intended for the treatment of disease or injury, or who publicly professes to cure or treat disease, injury, or deformity by any drug, nostrum, manipulation, or other expedient, must pay a license fee of $100 per month; the violation of this section is a misdemeanor, punishable with a fine not exceeding $500 or imprisonment in the county jail not to exceed six months, or both (ib., s. 6,880).
Penalty.—The violation of the provisions of this act is a misdemeanor punishable with a fine of from $50 to $500, or imprisonment in the county jail for from thirty to three hundred and sixty-five days, or both, for each offence; filing or attempting to file the certificate of another, or a forged affidavit or identification, is a felony punishable as forgery in the second degree, but the provisions of this article do not apply to persons who had been practising five years in the State prior to 1883 (ib., s. 6,881).
Fees.—To the secretary of the board, for examining a genuine diploma, $1.
If fraudulent or not owned by the possessor, $20 (ib., s. 6,873).
To the clerk, for recording, the usual fees (ib., s. 6,875).
Montana.
Board of Examiners.—The governor, with the advice and consent of the council, appoints seven learned, skilled, and capable physicians who have been residents for not less than two years, no more than two from the same county, to constitute the board of examiners (Act of February 28th, 1889, s. 1).
Meetings of the board for examination are required to be held at the capital and such other central points as the board may select, on the first Tuesday of April and October in each year, and at other times as the board may determine. The board must keep a record of all applicants for a certificate, with their age, time spent in the study of medicine, name, and the location of all institutions granting to applicants degrees or certificates of lectures in medicine or surgery, and whether the applicant was rejected or received a certificate, and the register is prima facie evidence of matters therein recorded (ib., s. 2).
Qualification.—Every person wishing to practise medicine or surgery in any of their departments shall do so only upon complying with the requisites of this act. If a graduate in medicine, he must present his diploma to the board for verification as to its genuineness. If it be found genuine and issued by a medical school legally organized and in good standing, whose teachers are graduates of a legally organized school, which fact the board determines, and if the person presenting and claiming the diploma be the person to whom it was originally granted, the board must issue its certificate, which shall be conclusive of the holder’s right to practise. Any person coming to the State may present his diploma to any member of the board, who may issue a certificate good till the board’s next regular meeting. If not a graduate, the person must present himself to the board for such examination as may be required, unless he shall have been in continuous practice[174] in the State for not less than ten years, of which fact he must present satisfactory evidence in the form of affidavits to the board (ib., s. 3).
All persons entitled to practise under the ten-year provision and all persons commencing the practice of medicine and surgery in any of its branches shall apply to the board for a certificate, and at the time and place designated by the board, or at the regular meeting, be examined in anatomy, physiology, chemistry, histology, materia medica, therapeutics, preventive medicines, practice of medicine, surgery, obstetrics, diseases of women and children, diseases of the nervous system, diseases of the eye and ear, medical jurisprudence, and such other branches as the board may deem advisable, and present evidence of having practised the required term of ten years, or of having attended three courses of lectures of at least four months each; the examination must be both scientific and practical, and of sufficient thoroughness and severity to test the candidate’s fitness to practise medicine and surgery. The examination may be held in the presence of the dean of any medical school or of the president of any medical society of the State. After the examination, the board must grant to a candidate who is found qualified, a certificate to practise medicine and surgery. The board may refuse or revoke a certificate for unprofessional, dishonorable, or immoral conduct, or may refuse a certificate to any one who may publicly profess to cure or treat diseases, injuries, or deformities in such manner as to deceive the public. In cases of refusal or revocation, the aggrieved applicant may appeal to the district court of the county of his application (ib., s. 4).
Certificates must be recorded within sixty days after their date in the office of the county recorder in the county where the holder resides; or in case of removal certificates must be recorded in the county to which the holder removes. The county recorder must indorse on the certificate the date of its record (ib., s. 5).
Exceptions.—The act does not apply to midwives of skill and experience attending cases of confinement, nor to commissioned surgeons of the United States army or navy in the discharge of their official duties, nor to physicians or surgeons in actual consultation from other States and Territories, nor to[175] students practising medicine under the direct supervision of a preceptor, nor to gratuitous services in cases of emergency (ib., s. 6).
Penalty.—Violation of the act is a misdemeanor, punishable with a fine of from $100 to $500, or imprisonment in the county jail from thirty to ninety days, or both.
Definition.—Any person is regarded as practising within the meaning of the act who appends “M.D.” or “M.B.” to his name, for a fee prescribes medicine, operates in surgery, attends in obstetrics, or recommends for the use of any sick person the use of any drug or medicine or other agency of treatment, cure, or relief of any wound, fracture, or bodily injury or disease, as a physician or surgeon (ib., s. 7).
Re-examination.—Any one failing to pass the examination is entitled to a second examination within six months without fee (ib., s. 8).
Fees.—To the treasurer of the board, for examination, $15 (ib., s. 4).
To the secretary of the board, for examination, in advance, $15 (ib., s. 8).
To the county recorder, for recording, the usual fee (ib., s. 5).
To the county attorney, for prosecuting a violation, to be charged as costs, $5 (ib., s. 7).
Nebraska.
Qualification.—It is unlawful for any person to practise medicine, surgery, or obstetrics, or any of their branches, without having obtained and registered a certificate. No person is entitled to a certificate unless he be a graduate of a legally chartered medical school or college in good standing. The qualifications are determined by the State board of health. The act does not prevent physicians residing in other States from visiting patients in consultation with resident physicians who have complied. (Act of 1891, c. 35, s. 7).
A medical school is defined as a medical school or college which requires a previous examination for admission to its courses of study, and which requires for granting the degree of “M.D.” attendance on at least three courses of lectures of six[176] months each, no two of said courses to be held within one year, and having a full faculty of professors in anatomy, physiology, chemistry, toxicology, pathology, hygiene, materia medica, therapeutics, obstetrics, gynæcology, principle (sic) and practice of medicine and surgery, and clinical instruction in the last two named. But the three-year clause does not apply to degrees granted prior to July, 1891 (ib., s. 8).
A person intending to practise medicine, surgery, or obstetrics must present his diploma to the said board, with his affidavit that he is the lawful possessor of the same and has attended the full course of study required for the degree of “M.D.,” and that he is the person therein named. Such affidavit may be taken before any person authorized to administer oaths, and it shall be attested under the hand and official seal of the official, if he have a seal. False swearing is perjury (ib., s. 9).
If investigation of the diploma and affidavit proves the applicant entitled to practise, the board issues its certificate, which must be filed in the office of the county clerk of the county where he resides, or intends to practise (ib., s. 10).
The act gave physicians entitled to practise at the time of its enactment six months in which to comply with its provisions with reference to them (ib., s. 11).
The secretaries of the board may issue certificates, without a vote of the board, when the proof upon which certificates are granted may have been on file in its office for ten days without a vote of the board, when no protest has been filed, and if, in their opinion, the proof complies with the act (ib., s. 12).
When the holder of a certificate removes to another county, he must file and record it in the office of the county clerk in the county to which he removes (ib., s. 13).
The board may refuse certificates to persons guilty of unprofessional or dishonorable conduct, and may revoke for like causes provided they give the person an opportunity to be heard (ib., s. 14).
Penalty.—No person is entitled to receive any sum of money for medical, surgical, or obstetrical service unless he shall have complied with the act (ib., s. 15).
Violation of the act is a misdemeanor, punishable with a fine of from $50 to $300 and costs of prosecution, and a person[177] convicted shall stand committed till the fine and costs are paid (ib., s. 16).
Definition, Exceptions.—To operate on, profess to heal, prescribe for, or otherwise treat any physical or mental ailment of another, is to practise medicine under this act. But it does not prohibit gratuitous services in cases of emergency, nor apply to commissioned surgeons in the United States army or navy, nor to nurses in their legal occupation, nor to the administration of ordinary household remedies (ib., s. 17).
Itinerant Vender.—To be an itinerant vender of any drug, nostrum, ointment, or appliance for the treatment of disease or injury, or for such an one to publicly profess to cure or to treat disease or injury or deformity by any drug, nostrum, manipulation, or other expedient, is a misdemeanor punishable with a fine of from $50 to $100, or imprisonment in the county jail from thirty days to three months, or both, for each offence (ib., s. 18).
Fees.—To the secretaries of the board of health, for certificate at time of application, $5.
To the secretaries of the board of health, for taking testimony, same fees as a notary public is allowed for same service (ib., s. 19).
To county clerk, for recording, usual register’s fees for recording (ib., s. 10).
Nevada.
Qualification.—No person can lawfully practise medicine or surgery who has not received a medical education and a diploma from some regularly chartered medical school having a bona fide existence when the diploma was granted (Act of 1875, c. 46, s. 1).
A copy of the diploma must be filed for record with the county recorder of the county in which the person practises, and at the same time the original, or a certificate from the dean of the medical school of which he is a graduate, certifying to his graduation, must be exhibited (ib., s. 2).
The person filing a copy of a diploma or a certificate of graduation must be identified as the person named therein, by the affidavit of two citizens of the county, or his affidavit taken before a notary public or commissioner of deeds for this State,[178] which affidavit must be filed in the office of the county recorder (ib., s. 3).
Penalty.—Practising without complying with this act is a misdemeanor punishable with a fine of from $50 to $500, or imprisonment in the county jail from thirty days to six months, or both, for each offence. Filing a diploma or a certificate of another or a forged affidavit of identification is a felony (ib., s. 4).
Exceptions.—The act does not apply to a person who in an emergency may prescribe or give advice in medicine or surgery in a township where no physician resides, or when no physician or surgeon resides within convenient distance, nor to those who had practised medicine or surgery in the State for ten years next preceding the passage of the act, nor to persons prescribing in their own family (ib., s. 6).
New Jersey.
Board of Examiners.—The State board of medical examiners, appointed by the governor, consists of nine members, persons of recognized professional ability and honor, five of the old school, three of the homœopathic, and one of the eclectic, among whom can be no member of any college or university having a medical department (Act 1890, c. 190, s. 1).
The board must hold meetings for examination at the capital on the second Thursday of January, April, July, and October of each year and at such other times as they deem expedient; they shall keep a register of all applicants for examination, showing the name, age, and last place of residence of each candidate, the time he has spent in medical study in or out of a medical school, the names and locations of all medical schools which have granted the said applicant any degree or certificate of attendance upon lectures in medicine, and whether the applicant has been rejected or licensed, and it shall be prima facie evidence of all matters contained therein (ib., s. 2).
Qualification.—All persons commencing the practice of medicine or surgery in any of its branches must apply to the board for a license. Applicants are divided into three classes:
1. Persons graduated from a legally chartered medical school not less than five years before the application.
2. All other persons graduated from legally chartered medical schools.
3. Medical students taking a regular course of medical instruction.
Applicants of the first class are examined in materia medica, therapeutics, obstetrics, gynæcology, practice of medicine, surgery, and surgical anatomy; those of the second and third classes are examined in anatomy, physiology, chemistry, materia medica, therapeutics, histology, pathology, hygiene, practice of medicine, surgery, obstetrics, gynæcology, diseases of the eye and ear, medical jurisprudence, and such other branches as the board may deem advisable; questions for applicants of the first and second classes are the same in the branches common to both. The board after January 1st, 1892, cannot license applicants of the second or third classes without satisfactory proof that the applicant has studied medicine and surgery three years, is of good moral character, and over twenty-one years of age; applicants of the third class, after they shall have studied medicine and surgery at least two years, can be examined in anatomy, physiology, chemistry, histology, pathology, materia medica, and therapeutics; if the examination is satisfactory to all the members of the board, it may issue a certificate that the applicant has passed a final examination in these branches, and such certificate, if presented by the applicant when he shall make application for a license to practise, shall be accepted by the said board in lieu of examination in those branches. All examinations shall be both scientific and practical, but of sufficient severity to test the candidate’s fitness to practise medicine and surgery (ib., s. 3).
All examinations shall be in writing; the questions and answers, except in materia medica and therapeutics, must be such as can be answered in common by all schools of practice, and if the applicant intends to practise homœopathy or eclecticism, the member or members of the said board of those schools shall examine the said applicant in materia medica and therapeutics; if the examination is satisfactory, the board shall issue a license entitling the applicant to practise medicine. A license shall not be issued unless the applicant passes an examination satisfactory to all members of the board; the examination papers kept on file by the secretary of the board are prima[180] facie evidence of all matters therein contained; on refusal of the board to issue a license for failure on examination, the applicant may appeal to the governor, who may appoint a medical commission of review of three members, one from each school of medicine, who shall examine the examination papers of the applicant and from them determine whether a license should be issued, and their decision shall be final; if the said committee by unanimous vote reverse the determination of the board, the board shall issue a license; the expenses of the appeal are borne by the applicant (ib., s. 4).
The board may, by unanimous vote, refuse or revoke a license for chronic and permanent inebriety, the practice of criminal abortion, conviction of a crime involving moral turpitude, or for publicly advertising special ability to treat or cure disease which, in the opinion of the said board, it is impossible to cure.
In complaints for violating this section, the accused shall be furnished with a copy of the complaint and given a hearing before the said board in person or by attorney (ib., s. 5).
A person receiving a license must file it, or a certified copy thereof, with the clerk of the county in which he resides; and in case of removal into another county he must procure from the said clerk a certified copy of the said license, and file it with the clerk in the county to which he shall remove (ib., s. 6).
Exceptions.—The act does not apply to commissioned surgeons of the United States army, navy, or marine hospital service, or to regularly licensed physicians or surgeons in actual consultation from other States or Territories, or to regularly licensed physicians or surgeons actually called from other States or Territories to attend cases in this State, or to any one while actually serving as a member of the resident medical staff of any legally incorporated hospital or asylum in this State, or to any person claiming the right to practise in this State who has been practising therein since before July 4th, 1890, provided the said right or title was obtained upon a diploma of which the holder and applicant was lawfully possessed and it was issued by a legally chartered medical institution in good standing (ib., s. 7, as amended Act 1892, c. 212).
Definition.—Any person is regarded as practising medicine or surgery who appends “M.D.” or “M.B.” to his name, or prescribes[181] for the use of any person any drug or medicine or other agency for the treatment, cure, or relief of any bodily injury, infirmity, or disease (ib., s. 8).
Penalty.—Commencing the practice of medicine or surgery without a license or contrary to the act is a misdemeanor punishable by a fine of from $50 to $100, or imprisonment in the county jail from ten to ninety days, or both (ib., s. 9).
Fees.—To the treasurer of the board, for examination, for applicant of first and second class, $15.
To the treasurer of the board, for examination, for applicant of third class, $20 (ib., s. 4).
To the county clerk, for registering license, 50 cents (ib., s. 6).
New Hampshire.
In New Hampshire there is no statute on this subject.
New Mexico.
Board of Examiners.—The board of medical examiners is composed of seven practising physicians of known ability and integrity, graduates of some medical school, college, or university duly established under and by virtue of the laws of the country in which it is situated, four allopathic members, three homœopathic members, and one eclectic member (Compiled Laws 1884, s. 2,553).
Qualification.—Applications for certificates and examinations are made to the board through their secretary (ib., s. 2,555).
The board must examine diplomas as to their genuineness; the verification consists in an affidavit of the holder and applicant that he is the lawful possessor of the diploma and the person therein named; the affidavit may be taken before any person authorized to administer oaths, and shall be attested under his hand and official seal if he have a seal. Graduates may present their diplomas and affidavits by letter or by proxy (ib., s. 2,556).
Examinations of persons not graduates or licentiates must be made by the board, and certificates by a majority of the board[182] authorize the possessor to practise medicine and surgery (ib., s. 2,557).
The certificate must be recorded in the county clerk’s office in every county in which the holder practises or attempts to practise medicine or surgery (ib., s. 2,558).
When a certificate is filed, the clerk must record it and attach his certificate thereto, showing the date of filing and recording and the number of the book and the page of the record (ib., s. 2,559).
Examinations of persons not graduates must be made by the board and may be wholly or partly in writing, in anatomy, physiology, chemistry, pathology, surgery, obstetrics, and the practice of medicine (exclusive of materia medica and therapeutics) (ib., s. 2,561).
The board may refuse or revoke a certificate to an individual guilty of unprofessional or dishonorable conduct (ib., s. 2,562).
Definition, Exceptions.—Practising medicine is defined as professing publicly to be a physician and prescribing for the sick or appending to a name the letters “M.D.” The act does not prohibit students from prescribing under the supervision of a preceptor, nor prevent women from practising midwifery, nor prohibit gratuitous services in cases of emergency, nor apply to commissioned surgeons or acting surgeons of the United States army or navy (ib., s. 2,563).
Penalty.—Practising medicine or surgery without complying with the act is punishable with a fine of from $50 to $500 for each offence; and filing a diploma or a certificate of another, or a forged affidavit of identification, is a felony punishable the same as forgery.
Exception.—The provisions of the act do not apply to those who have been practising medicine ten years in the Territory (ib., s. 2,564, Act passed 1882).
Professional Conduct.—The code of ethics of the United States Medical Association is the standard, and the rule of decision, concerning professional conduct (ib., s. 2,565).
Penalty.—Persons unlawfully collecting or receiving fees or compensation for services as physicians or surgeons in violation of this act, are liable to the party paying it for double the amount thereof (ib., s. 2,568).
Fees.—To the secretary of the board, from each graduate or licentiate if the diploma is genuine, $5.
To the secretary of the board, from each graduate or licentiate if the diploma is fraudulent or not owned by the possessor, $20 (ib., s. 2,556).
To clerk of the county, for filing and recording certificate, the usual fees (ib., s. 2,559).
To the secretary of the board, for examination, in advance, $10 (ib., s. 2,561).
New York.
Prohibition.—No person can lawfully practise medicine unless registered and legally authorized prior to September 1st, 1891, or unless licensed by the regents of the University of the State of New York and registered as required by the present law; nor can any person lawfully practise medicine who has ever been convicted of a felony by any court, or whose authority to practise is suspended or revoked by the regents on the recommendation of a State board (Laws of 1893, c. 661, s. 140).
Boards of Examiners.—There are three separate State boards of medical examiners of seven members each, representing respectively the Medical Society of the State, the Homœopathic Medical Society of the State, and the Eclectic Medical Society of the State.
The regents appoint examiners from lists of nominees furnished by the said societies. Each nominee before his appointment is required to furnish to the regents proof that he has received the degree of doctor of medicine from some registered medical school, and has legally practised medicine in this State for at least five years. If no nominees are legally before them, the regents may appoint from the members in good standing of such societies without restriction (ib., s. 141).
At any meeting of the boards of examiners a majority constitute a quorum, but questions prepared by the boards may be grouped and edited, or answer papers of candidates may be examined and marked, by committees duly authorized by the boards and by the regents (ib., s. 144).
Qualification.—The regents are required to admit to examination[184] any candidate who pays a fee of $25, and submits satisfactory evidence, verified by oath, if required, that he—
(1) Is more than twenty-one years of age; (2) is of good moral character; (3) has the general education required in all cases after August 1st, 1895, preliminary to receiving the degree of bachelor or doctor of medicine in this State; (4) has studied medicine not less than three full years, including three satisfactory courses in three different academic years in a medical school registered as maintaining at the time a satisfactory standard; (5) has either received the degree of bachelor or doctor of medicine from some registered medical school or a diploma or license conferring the full right to practise medicine in some foreign country.
The degree of bachelor or doctor of medicine shall not be conferred in the State before the candidate has filed with the institution conferring it the certificates of the regents that three years before the date of his degree, or before or during his first year of medical studies in the State, he had either graduated from a registered college or satisfactorily completed not less than a three years’ academic course in a registered academy or high school; or had a preliminary education considered and accepted by the regents as fully equivalent; or had passed a regents’ examination in arithmetic, elementary English, geography, spelling, United States history, English composition, and physics. Students who had matriculated in a New York medical school before June 5th, 1890, are exempt from this preliminary education requirement provided that the degree be conferred before August 1st, 1895.
The regents may in their discretion accept as equivalent for any part of the third and fourth requirements evidence of five or more years’ reputable practice of medicine, provided such substitution be specified in the license (ib., s. 145).
Each board is required to submit to the regents as required lists of suitable questions for a thorough examination in anatomy, physiology, and hygiene, chemistry, surgery, obstetrics, pathology and diagnosis and therapeutics, including practice and materia medica. From these lists the regents are required to prepare question papers for all these subjects, which at any examination are required to be the same for all candidates, except that in therapeutics, practice, and materia medica all[185] questions submitted to any candidate shall be chosen from those prepared by the board selected by that candidate, and shall be in harmony with the tenets of that school as determined by its State board of medical examiners (ib., s. 146).
Examinations for a license are required to be given in at least four convenient places in this State at least four times annually in accordance with the regents’ rules, and exclusively in writing and in English. Each examination is conducted by a regents’ examiner who shall not be one of the medical examiners. At the close of each examination the regents’ examiner in charge is required to deliver the question and answer papers to the board selected by each candidate, or its duly authorized committee, and such board, without unnecessary delay, is required to examine and mark the answers and transmit to the regents an official report stating the standing of each candidate in each branch, his general average, and whether the board recommends that a license be granted. Such report must include the questions and answers and is filed in the public records of the university. If the candidate fails on a first examination, he may, after not less than six months’ further study, have a second examination without fee. If the failure is from illness or other cause satisfactory to the regents they may waive the requirement of six months’ study (ib., s. 147).
On receiving from a State board an official report that the applicant has successfully passed the examinations and is recommended for license, the regents are required to issue to him, if in their judgment he is duly qualified therefor, a license to practise medicine. The contents and execution of the license are regulated in detail by the act.
Applicants examined and licensed by other State examining boards registered by the regents as maintaining standards not lower than those provided by this article, and applicants who matriculated in a New York State medical school before June 5th, 1890, and who shall have received the degree of “M.D.” from a registered medical school before August 1st, 1895, may, without further examination, on the payment of ten dollars to the regents, and on submitting such evidence as they may require, receive from them an indorsement of their license or diploma conferring all the rights and privileges of a regents’ license issued after an examination.
If any person whose registration is not legal because of some error, misunderstanding, or unintentional omission shall submit satisfactory proof that he had all the requirements provided by law at the time of his imperfect registration, and was entitled to be legally registered, he may, on the unanimous recommendation of a State board of medical examiners, receive from the regents under seal a certificate of the facts, which may be registered by any county clerk and shall make valid the previous imperfect registration.
Before any license is issued, it must be numbered and recorded in a book in the regents’ office, and its number noted in the license. This record in all legal proceedings has the same weight as evidence that is given to a record of conveyances of land (ib., s. 148).
Every license to practise medicine is required, before the licensee begins to practise, to be registered in the county clerk’s office, where such practice is to be carried on, with his name, residence, place and date of birth, and the source, number, and date of his license. Before registering, each licensee is required to file an affidavit of the above facts, and that he is the person named in the license, and had, before receiving the same, complied with all the requisites as to attendance, terms, and amount of study and examinations required by law and the rules of the university as preliminary to the conferment thereof; that no money was paid for such license except the regular fees paid by all applicants therefor; that no fraud, misrepresentation, or mistake in any material regard was employed by any one or occurred in order that such license should be conferred.
Every license, or if lost a copy, legally certified so as to be admitted as evidence, or a duly attested transcript of the record of its conferment, shall before registration be exhibited to the county clerk, who, only in case it was issued or indorsed as a license under seal by the regents, shall indorse or stamp on it the date and his name preceded by the words, “Registered as authority to practise medicine in the clerk’s office,—— County.” The clerk is required thereupon to give to every physician so registered a transcript of the entries in the register with a certificate under seal that he has filed the prescribed affidavit (ib., s. 149).
A practising physician having registered a lawful authority[187] to practise medicine in one county and removing such practice, or a part thereof, to another county, or regularly engaged in practice or opening an office in another county, must show or send by registered mail to the clerk of such other county his certificate of registration. If such certificate clearly shows that the original registration was of an authority issued under seal by the regents, or if the certificate itself is indorsed by the regents as entitled to registration, the clerk is required thereupon to register the applicant in the latter county, and to stamp or indorse on such certificate the date, and his name preceded by the words, “Registered also in—— County,” and return the certificate to the applicant (ib., s. 150).
Every unrevoked certificate and indorsement of registration is presumptive evidence that the person named is legally registered. No person can register any authority to practise medicine unless issued or indorsed as a license by the regents. No such registration is valid unless the authority registered constituted at the time of registration a license under the laws of the State then in force. No diploma or license conferred on a person not actually in attendance at the lectures, institution, and examinations of the school conferring the same, or not possessed, at the time of its conferment, of the requirements then demanded of medical students in this State as a condition of their being licensed, and no registration not in accordance with this article, shall be lawful authority to practise, nor shall the degree of doctor of medicine be conferred causa honoris or ad eundum, nor if previously conferred shall it be a qualification for practice (ib., s. 151).
Exceptions.—The law does not affect commissioned medical officers serving in the United States army, navy, or marine hospital service while so commissioned; or any one while actually serving on the resident medical staff of any legally incorporated hospital; or any legally registered dentist exclusively engaged in the practice of dentistry; or any manufacturer of artificial eyes, limbs, or orthopædic instruments or trusses in fitting such instruments on persons in need thereof; or any lawfully qualified physician in other States or countries meeting legally registered physicians in this State in consultation; or any physician residing on a border of a neighboring State and duly authorized under the laws thereof to practise medicine therein whose practice[188] extends into this State, and who does not open an office or appoint a place to meet patients or receive calls within this State; or any physician duly registered in one county called to attend isolated cases in another county, but not residing or habitually practising therein (ib., s. 152).
Penalty.—A person practising without lawful registration or in violation of this article forfeits to the county $50, for each violation and for every day of unlawful practice. To practise under a false or assumed name or falsely personate another practitioner of like or different name is a felony. The violation of the other provisions of the act, or buying, selling, or fraudulently obtaining a medical diploma, license, record, or registration, or aiding or abetting such buying, selling, or fraudulently obtaining, or practising medicine under cover of a diploma or license illegally obtained, or signed and issued unlawfully or under fraudulent representation or misstatement of fact in a material regard, or after conviction of a felony attempting to practise medicine, or appending “M.D.” to the name or assuming to advertise the title of doctor in such manner as to convey the impression that one is a legal practitioner of medicine or any of its branches without having legally received the medical degree, is a misdemeanor punishable with a fine of not less than $250, or imprisonment for six months for the first offence, and for subsequent offences with a fine of not less than $500 or imprisonment for not less than one year, or both fine and imprisonment (ib., s. 159).
Definitions.—As used in the article, university means the University of the State of New York. Medical school means any medical school, college, or department of a university registered by the regents as maintaining a proper medical standard and as legally incorporated. Medicine means medicine and surgery; physician means physician and surgeon (ib., definitions).
Fees.—To regents, for examination, $25 (ib., s. 145).
To regents, for license without examination under sec. 148, $10 (ib., s. 148).
To county clerk, for registering affidavit and certificate, $1 (ib., s. 149).
To county clerk, for registration in an additional county, 25 cents (ib., s. 150).
North Carolina.
Qualification.—No person can lawfully practise medicine or surgery, or any of the branches thereof, nor in any case prescribe for the cure of disease for a fee or reward unless he shall have been first licensed (Code 1883, s. 3,122, as amended Act of 1885, c. 117, s. 1).
The board of medical examiners of the State consists of regularly graduated physicians appointed by the medical society of the State (ib., s. 3,123, 3,126).
The board must examine all applicants for a license to practise medicine or surgery, or any of the branches thereof, on anatomy, physiology, surgery, pathology, medical hygiene, chemistry, pharmacy, materia medica, therapeutics, obstetrics, and the practice of medicine, and grant to a competent applicant a license or diploma authorizing him to practise medicine and surgery or any of the branches thereof (ib., s. 3,124).
Where he has not been refused a license by the board, two members of the board may grant a temporary license to any applicant to continue in force no longer than the next regular meeting of the board (ib., s. 3,125, as amended Act of 1889, c. 181, s. 3).
The board of examiners must assemble when and where the medical society assembles, which society must assemble at least once a year; the board must remain in session from day to day till all applicants during the first five days after its meeting have been examined and disposed of (ib., s. 3,127).
Penalty, Exceptions.—A person practising without obtaining a license from the board shall not be entitled to sue for or recover any medical bill for services; and a person who has begun the practice of medicine or surgery in the State for a fee or reward since February 23d, 1885, without first obtaining such a license, shall in addition be guilty of a misdemeanor and punishable with a fine of from $25 to $100, or imprisonment at the discretion of the court for each offence; but the act does not apply to women pursuing the avocation of midwife, nor to any reputable physician or surgeon residing in a neighboring State, coming into this State for consultation with a registered physician resident therein, except a physician residing in a neighboring[190] State regularly practising in this State, nor does it apply to physicians who have a diploma from a regular medical college prior to January 1st, 1880 (ib., s. 3,132, as amended Act of 1885, c. 117, s. 2; Act of 1885, c. 261, s. 1; Act of 1889, c. 181, s. 1).
The board may rescind a license upon satisfactory proof that a licensee has been guilty of grossly immoral conduct (ib., s. 3,133).
Qualification.—Every person practising medicine or surgery in the State was required before January 1st, 1892, to appear personally before the clerk of the superior court of the county where he resided or practised, for registration, and all persons beginning to practise are likewise to appear and register within thirty days after obtaining a license (Act of 1889, c. 181, s. 3, as amended Act of 1891, c. 90).
Any person applying for registration must produce and exhibit before the clerk a license from the board of medical examiners, or make oath that he was practising medicine or surgery in this State prior to March 7th, 1885, and thereupon the clerk shall register the date, with the name and residence of the applicant, and shall issue a certificate of registration. The certificate entitles the recipient to practise in any county in the State, but if he removes his residence to another county he must exhibit his certificate to the clerk of such county and be registered. Persons having a temporary license are not entitled to register but may practise so long as the license is in force (Act of 1889, c. 181, s. 4, as amended Act of 1891, c. 420).
Penalty, Exceptions.—To practise without registration and a certificate is a misdemeanor punishable with a fine of from $25 to $100 or imprisonment for each offence, but this act does not apply to women pursuing the avocation of midwife nor to reputable physicians or surgeons residing in a neighboring State coming into the State for consultation with a registered physician of this State (Act of 1889, c. 181, s. 5).
License Fee.—A license of $10 for each county in which he carries on business is exacted from every (itinerant?) medical practitioner, one-half for the use of the county and one-half for the use of the State; but a State license may be obtained from the State treasurer for $30 good for twelve months, and he is then exempt from the portion of above tax due the State (Act 1891, c. 323).
Fees.—To the secretary of the board, before issuing a license or diploma, $10.
To the secretary of the board, for temporary license, $5 (Code, 3,130).
To clerk of the court, for registration and certificate, 25 cents.
To clerk of the county, for registration on removal, no fee (Act 1889, c. 181, s. 4).
North Dakota.
Board of Examiners.—The governor appoints a State board of examiners of nine members, eight of whom are practising physicians in good standing; no member of any college or university having a medical department shall be appointed. Two members shall be homœopathic physicians and one a lawyer (Act 1890, c. 93, s. 1).
The board must hold meetings for examination at such place or places as it may designate on the first Tuesday of January, April, July, and October of each year, and such other meetings as it may appoint and must keep a record of its proceedings with a register of every applicant for a license with his or her age, the time spent in the study of medicine, and the name and location of all institutions granting to such applicant a degree or a certificate of lectures in medicine or surgery, and whether the applicant was rejected or licensed; and said books and register shall be prima facie evidence of all matters therein recorded (ib., s. 2).
Qualification.—All persons hereafter commencing the practice of medicine, surgery, and obstetrics in any of its branches shall apply to the board for a license, and at the time and place designated by the board, or at its regular meeting, be examined in anatomy, physiology, chemistry, histology, materia medica, therapeutics, preventive medicines, practice of medicine, surgery, obstetrics, diseases of women and children, of the nervous system, of the eye and ear, medical jurisprudence, and such other branches as the board shall deem advisable, and produce evidence of having attended three courses of lectures of at least six months each; the examination must be both practical and scientific, but of sufficient severity to test the candidate’s[192] fitness to practise medicine, surgery, and obstetrics. When desired, the said examination may be conducted in the presence of the dean of any medical school or the president of any medical society of the State. After examination the board must grant a license to practise medicine, surgery, and obstetrics; seven members must consent. The board may revoke or refuse a license for unprofessional, dishonorable, or immoral conduct, chronic or persistent inebriety, the practice of criminal abortion, or for publicly advertising special ability to treat or cure diseases which, in the opinion of the board, it is impossible to cure. In complaints for violating the provisions of this section, the accused shall be furnished with a copy of the complaint, and given a hearing before the board in person or by attorney. Appeal lies from refusal or revocation to the appointing power (ib., s. 3).
The person receiving a license must file it, or a certified copy, with the register of deeds where he resides. On removal into another county he must procure from said register a certified copy of his license and file it with the register of deeds in the county to which he shall remove (ib., s. 4).
Exceptions.—The act does not apply to commissioned surgeons of the United States army or navy, to physicians or surgeons in actual consultation from other States or Territories, or to actual medical students practising medicine under the direct supervision of a preceptor (ib., s. 5).
Penalty.—Practising without a license or contrary to the act is a misdemeanor punishable with a fine of from $50 to $200, or imprisonment in a county jail from ten to sixty days, or both.
Definition.—Any person is regarded as practising who appends the letters “M.D.” or “M.B.” to his name, or who for a fee prescribes, directs, or recommends for the use of any person any drug or medicine or other agency for the treatment, cure, or relief of any wound, fracture or bodily injury, infirmity, or disease (ib., s. 6).
Former Law.—The former law is repealed only so far as it is inconsistent with the foregoing act (ib., s. 7).
The former law prohibited persons from practising medicine in any of its branches unless graduates of a medical college or unless they were shown by examination to be qualified and had[193] been actually engaged in practising for at least ten years (Compiled Laws of Dakota, s. 205).
Fee.—To the treasurer of the board, for examination, $20 (Act 1890, c. 93, s. 3).
Ohio.
Qualification.—No person who is not a graduate of a reputable school of medicine in the United States or a foreign country, or who cannot produce a certificate of qualification from a State or county medical society and is not a person of good moral character, can lawfully practise or attempt to practise medicine in any of its departments or prescribe medicine for reward or compensation; except a person who has been continuously engaged in the practice of medicine for ten years or more. The law allowed persons in continuous practice for five years or more, two years to comply with its provisions. In case a person is a graduate of a school of medicine in any State or foreign country in which any condition or restriction is imposed by law upon the practice of medicine by graduates of medical schools in Ohio, he is subject to the same restrictions or conditions. A person violating this section is not entitled to any compensation for services (Smith & Benedict’s Revised Statutes of 1890, s. 4,403).
Penalty.—Whoever prescribes or practises or attempts to practise medicine in any of its departments, or performs or attempts to perform a surgical operation without having attended two full courses of instruction and graduated at a school of medicine either in this or a foreign country, or who cannot produce a certificate of qualification from a State or county medical society, except a person who has been continuously engaged in the practice of medicine for ten years or more, is punishable with a fine of from $50 to $100 and for a subsequent offence with imprisonment for thirty days. Persons in continuous practice for five years or more were allowed two years to comply with this act (ib., s. 6,992).
Oklahoma.
Qualification.—No person can lawfully practise medicine in any department unless he be a graduate of a medical college, or unless upon examination before a board composed of the[194] superintendent of public health and two other physicians to be selected by the territorial board of health, he be found proficient in the practice of medicine and surgery, and shall be found upon proof to have been actually engaged in the practice of medicine not less than five years. No person shall practise medicine unless he be of good moral character, and is not an habitual drunkard.
A person possessing these qualifications shall, on presentation of his diploma, or proof thereof by affidavit if it be lost or destroyed, and the affidavit of two reputable citizens from the county where he resides that the applicant possesses the qualifications of a physician, as prescribed herein, to the superintendent of public health, receive from him a license, which shall be recorded in the office of the register of deeds in the county where such physician resides.
Offence.—To practise without complying with this law, or to violate any of its provisions, is a misdemeanor.
Definition.—A person is regarded as practising medicine who professes publicly to be a physician and to prescribe for the sick, or who appends to his name M.D.
Exceptions.—The law does not prohibit students from prescribing under the supervision of preceptors, nor prohibit gratuitous services in case of emergency, nor apply to commissioned surgeons in the United States army and navy.
Cancellation of License.—The district court has power on complaint of a member of the territorial board of health, or the county board of health where he resides, to cancel any license issued to a person to practise medicine, where such license was fraudulently obtained, or where the person to whom it was issued has been guilty of violating any provision of this act.
Fee.—To superintendent of board of health, for license, $2 (Comp. Stats., 1893, s. 352).
Oregon.
Qualification.—Every person practising medicine and surgery in any of their departments must possess the qualifications required by the act. If a graduate of medicine he must present his diploma to the board of examiners for verification as to its genuineness. If found genuine and the person named[195] therein be the person claiming and presenting the same, the board issues its certificate, which is conclusive. If not a graduate, he must submit to an examination as the board shall require, and if the examination be satisfactory the board issues its certificate, and the lawful holder is entitled to all the rights and privileges mentioned in the act (Act February 28th, 1889, s. 1).
The governor appoints three persons from among the most competent physicians of the State, residents of the State for seven years and of at least five years’ practical experience in their profession, to be the board of examiners (ib., s. 2).
The board must issue certificates to all who furnish satisfactory proof of having received a diploma or license from a legally chartered medical institution in good standing of whatever school of medicine, and they are not permitted to make discrimination against holders of a general license or diploma under any school or system of medicine in good standing (ib., s. 3, as amended February 21st, 1891).
The verification of a diploma consists in an affidavit of the holder and applicant that he is the person therein named, taken before any person authorized to administer oaths, attested under the hand and official seal of the official, if he have a seal; graduates may present their diplomas and affidavits by letter or proxy. The act allows persons taking advantage of section 13 ninety days after its passage in which to procure a certificate (ib., s. 4, as amended February 21st, 1891).
All examinations of persons not graduates or licentiates must be made directly by the board, and certificates authorize the person named to practise medicine and surgery (ib., s. 5).
The holder of a certificate must have it recorded in the office of the county clerk of the county in which he resides, and the record must be indorsed thereon. On removal to another county to practise he must procure an indorsement to that effect on the certificate from the clerk, and have the certificate recorded in the office of the clerk of the county to which he removes (ib., s. 6).
The examinations may be wholly or partly in writing and must be of an elementary and practical character, but sufficiently strict to test the qualifications of the candidate as a practitioner (ib., s. 8).
The board may refuse a certificate to an individual guilty of unprofessional or dishonorable conduct, and may revoke for like causes, after giving the accused an opportunity to be heard in his defence before the board (ib., s. 9).
Definition, Exceptions.—Any person is regarded as practising medicine who professes publicly to be a physician and to prescribe for the sick, or appends to his name the letters “M.D.;” but the act does not prohibit students from prescribing under the supervision of a preceptor, nor gratuitous services in cases of emergency, nor does it apply to commissioned surgeons of the United States army, navy, and marine hospital service (ib., s. 10).
Itinerant Vender.—Any itinerant vender of any drug, nostrum, medicine, ointment, or appliance of any kind intended for the treatment of disease or injury, who shall publicly profess to cure or treat diseases, injuries, deformities, or ailments by any drug, nostrum, medicine, or other appliance, shall pay a license to the Secretary of the State of $100 per month.
Violation of this section is a misdemeanor punishable by a fine of not more than $500 or imprisonment in a county jail for not more than six months, or both. Such licenses to any firm or company do not permit the transaction of business in different places at the same time (ib., s. 11, as amended February 21st, 1891).
Penalty.—Practising medicine or surgery without complying with the act is a misdemeanor punishable with a fine of from $50 to $500 or imprisonment in a county jail from thirty days to three hundred and sixty-five days, or both, for each offence. Filing or attempting to file as his own the certificate of another, or a forged affidavit or identification, is a felony punishable the same as forgery in the second degree (ib., s. 12).
Former Practitioners.—Persons practising in the State at the time of the passage of the act were allowed sixty days afterward to register (ib., s. 13).
Fees.—To the secretary of the board, for examining a genuine diploma, $1.
To the secretary of the board, for examining a fraudulent diploma, or a diploma not owned by the possessor, $20 (ib., s. 4).
To the county clerk, for recording certificate, usual fee (ib., s. 6).
To board of examiners, for examination, $10 (ib., s. 8).
To the Secretary of the State, from itinerant vender, for license, $100 per month (ib., s. 11, as amended February 21st, 1891).
Pennsylvania.
[Present Law.—The following is the law at present in effect; for the new law which goes into effect hereafter, see below.]
Qualification.—The standard of a practitioner of medicine, surgery, or obstetrics consists of a good moral character, a thorough elementary education, a comprehensive knowledge of human anatomy, human physiology, pathology, chemistry, materia medica, obstetrics, and practice of medicine and surgery and public hygiene (Act March 24th, 1877, s. 1).
It is unlawful for any person to announce himself as a practitioner of medicine, surgery, or obstetrics, or to practise as such, who has not received in a regular manner a diploma from a chartered medical school, duly authorized to confer upon its alumni the degree of doctor of medicine. The act does not apply to a resident practitioner who has been in continuous practice in the commonwealth for not less than five years prior to its passage (ib., s. 2).
Before any person can lawfully engage in the practice of medicine, surgery, or obstetrics, or who has not a diploma as provided in sec. 2, he must make an affidavit under oath, or affirm before the prothonotary of the county in which he intends to practise, setting forth the time of continuous practice and the place or places where such practice was pursued in the commonwealth, and it shall be entered of record (ib., s. 3).
Transient Practitioner.—Any person attempting to practise medicine or surgery for a valuable consideration by opening a transient office within the commonwealth, or by handbill or other form of written or printed advertisement, assigning such transient office or other place to persons seeking medical or surgical advice, or prescribing or itinerating from place to place or from house to house and proposing to cure any person sick or afflicted, by the use of any medicine, means, or agency whatsoever, for a valuable consideration, shall before being allowed to practise in this manner appear before the clerk[198] of the court of quarter sessions of the county where he desires to practise and furnish satisfactory evidence to such clerk that this act has been complied with, and shall take out a license for one year and pay $50 therefor (ib., s. 4).
Penalty.—To violate this act is a misdemeanor punishable with a fine of from $200 to $400 for each offence (ib., s. 5).
Qualification.—Every person who shall practise medicine or surgery, or any of their branches, for gain, or shall receive or accept for his services any fee or reward directly or indirectly, shall be a graduate of a legally chartered medical college or university having authority to confer the degree of doctor of medicine (except as provided in sec. 5), and shall present to the prothonotary of the county in which he resides or sojourns his medical diploma as well as a true copy of the same, including any indorsements thereon, and make affidavit before him that the diploma and indorsements are genuine; thereupon the prothonotary shall enter in the register the name in full of the practitioner, his place of nativity, place of residence, the name of the college or university that has conferred the degree of doctor of medicine, the year when it was conferred, and in like manner any other degree or degrees that the practitioner may desire to place on record; to all of which the practitioner shall make affidavit before the prothonotary and the prothonotary shall place the copy of the diploma and indorsements on file (Act June 8th, 1881, s. 2).
Any person whose medical diploma has been destroyed or lost shall present to the prothonotary of the county in which he resides or sojourns a duly certified copy of his diploma, but if the same is not obtainable a statement of this fact, with the names of the professors whose lectures he attended and the branches of study upon which each professor lectured, to all of which the practitioner shall make affidavit before the prothonotary; after which the practitioner shall be allowed to register and the prothonotary shall place such certificate or statement on file (ib., s. 3).
Any person desiring to commence the practice of medicine or surgery, having a medical diploma issued by any college, university, society, or association in another State or foreign country, shall lay the same before the faculty of one of the medical colleges or universities of this commonwealth for inspection,[199] and the faculty being satisfied as to the qualifications of the applicant and the genuineness of the diploma shall direct the dean of the faculty to indorse the same, after which such person shall be allowed to register as required by sec. 2 (ib., s. 4).
The act extends the privilege of continuing to practise to those who have been in the continuous practice of medicine or surgery in the commonwealth since 1871, but such a person must make affidavit to a written statement of the facts before the prothonotary of the county in which he resides; and the prothonotary shall enter in the register the name in full of the practitioner, his place of nativity, place of residence, the time of continuous practice in the commonwealth, and the place or places where such practice was pursued, to all of which the practitioner shall make affidavit, and the prothonotary shall place the certificate or statement on file in his office (ib., s. 5).
Penalty.—Presenting to the faculty of an institution for indorsement or to the prothonotary a diploma which has been obtained by fraud, or in whole or in part a forgery, or making an affidavit to a false statement, or practising without conforming with the act, or otherwise violating or neglecting to comply with the act, is a misdemeanor punishable with a fine of $100 or imprisonment in the county jail for not more than one year, or both, for each offence (ib., s. 7).
Exception.—The act does not prevent any physician or surgeon, legally qualified to practise medicine or surgery in the State where he resides, from practising in the commonwealth, but a person opening an office or appointing a place to meet patients or receive calls is a sojourner and must conform to its requirements (ib., s. 8).
Fees.—To the prothonotary, for affidavit of continuous practice, $2 (Act March 24th, 1877, s. 3).
To county treasurer, for transient license, $50.
To clerk of the court of quarter sessions, for issuing transient license, $5 (ib., s. 4).
To the prothonotary, for registration, $1 (Act June 8th, 1881, s. 6).
[New Law.—The following law has been enacted whose practical application does not begin until March 1st, 1894:]
Medical Council.—The law provides for a medical council of the State (Act of May 18th, 1893, s. 1).
The council is to supervise the examinations conducted by the State boards of medical examiners for licenses to practise medicine and surgery, and issue licenses to applicants who shall have presented satisfactory and properly certified copies of licenses from the State boards of medical examiners or State boards of health of other States, or who shall have successfully passed the examination of one of the State boards established by this act (ib., s. 5).
Medical Boards.—From and after March 1st, 1894, there are to be three separate boards of medical examiners, one representing the medical society of the State, one representing the homœopathic medical society of the State, and one representing the eclectic medical society of the State. Each board is to consist of seven members appointed by the governor from the full lists of the members of the said medical societies, and is to be composed exclusively of members of the same medical society. Each appointee must be a registered physician in good standing, and shall have practised medicine or surgery under the laws of the State for not less than ten years prior to his appointment.
The governor is to fill vacancies and may remove a member for continual neglect of duties or on the recommendation of the medical society with which he may be in affiliation, for unprofessional or dishonorable conduct (ib., s. 6).
Examinations.—For the purpose of examining applicants each board is to hold two or more stated or special meetings in each year after due public notice. A majority constitutes a quorum, but the examination may be conducted by a committee of one or more members authorized by the board (ib., s. 9).
The boards not less than one week prior to each examination must submit to the council questions for thorough examination in anatomy, physiology, hygiene, chemistry, surgery, obstetrics, pathology, diagnosis, therapeutics, practice of medicine, and materia medica; and the council must select therefrom the questions for each examination, and such questions for each examination shall be the same for all candidates, except that in the departments of therapeutics, practice of medicine, and materia medica the questions shall be in harmony with the teachings of the school selected by the candidate (ib., s. 10).
The examinations are to be in writing under rules prescribed by the council. After an examination the board must[201] act on it without unnecessary delay and transmit to the council an official report of its action stating the examination average of each candidate in each branch, the general average, and the result, and whether successful or unsuccessful. The report must embrace all the examination papers, questions, and answers, which shall be kept for reference and inspection for not less than five years (ib., s. 11).
Qualification.—The council must forthwith issue to each applicant returned as having successfully passed said examination, and adjudged by the council to be duly qualified, a license to practise medicine and surgery. The council must require the same standard of qualifications from all candidates except in therapeutics, practice of medicine, and materia medica, in which the standard shall be determined by the boards respectively. Before the license is issued, it must be recorded in a book in the office of the council, and the number of the book and page containing the record noted on the face of the license; the records shall have the same weight as evidence as that given to conveyance of land (ib., s. 12).
On and after July 1st, 1894, any person not theretofore authorized to practise medicine and surgery in the State may deliver to the secretary of the council a written application for a license with satisfactory proof that the applicant is more than twenty-one years of age, is of good moral character, has obtained a competent common-school education, and has received a diploma conferring the degree of medicine from some legally incorporated medical college of the United States, or a diploma or license conferring the full right to practise all the branches of medicine and surgery in some foreign country. Applicants who have received their degree in medicine after July 1st, 1894, must have pursued the study of medicine for at least three years, including three regular courses of lectures in different years in some legally incorporated medical college or colleges prior to the granting of said diploma or foreign license. Such proof shall be made, if required, upon affidavit, and if the council is satisfied with the same it shall issue to the applicant an order for examination before such one of the boards of examiners as the applicant may select. In case of failure at the examination the candidate, after the expiration of six months and within two years, shall have the privilege of a second examination[202] by the same board without additional fee. Applicants examined and licensed by State boards of medical examiners or State boards of health of other States, on filing in the office of the medical council a copy of said license certified by the affidavit of the president and secretary of such board, showing also that the standard of acquirements adopted by said board is substantially the same as is provided by secs. 11, 12, and 13 of this act, shall without further examination receive a license conferring on the holder all the rights and privileges provided by secs. 14 and 15 (ib., s. 13).
From and after March 1st, 1894, no person shall enter upon the practice of medicine or surgery unless he has complied with this act and shall have exhibited to the prothonotary of the court of common pleas of the county in which he desires to practise a license duly granted, which shall entitle him to be duly registered in the office of such prothonotary.
Penalty.—Violating the provisions of this act shall be a misdemeanor punishable with a fine of not more than $500 for each offence (ib., s. 14).
Exceptions.—The act does not interfere with or punish commissioned medical officers serving in the army or navy of the United States, or its marine hospital service, while so commissioned, or medical examiners of relief departments of railroad companies, while so employed, or any one while actually serving as a member of the resident medical staff of any legally incorporated hospital, or any legally qualified and registered dentist exclusively engaged in the practice of dentistry, nor interfere with or prevent the dispensing and sale of medicine or medical appliances by apothecaries [or] pharmacists, nor interfere with the manufacture of artificial eyes, limbs, or orthopædical instruments or trusses of any kind for (sic) fitting such instruments on persons in need thereof, or any lawfully qualified physicians and surgeons residing in other States or countries meeting registered physicians of this State in consultation, or any physician or surgeon residing on the border of a neighboring State and duly authorized under the laws thereof to practise medicine and surgery therein, whose practice extends into the limits of this State, provided such practitioner shall not open an office or appoint a place to meet patients or receive calls within the limits of Pennsylvania, or physicians duly registered[203] in one county of this State called to attend cases in another, but not residing or opening an office therein.
The act does not prohibit the practice of medicine and surgery by any practitioner who shall have been duly registered before March 1st, 1894, according to the Act of June 8th, 1881, and one such registration shall be sufficient warrant to practise medicine and surgery in any county (ib., s. 15).
Former Laws.—All acts or parts of acts inconsistent with this are repealed (ib., s. 17).
Fees.—To the secretary of the council, upon application for a license, $25.
To the secretary of the county, upon application for a license by licensees in other States, $15 (ib., s. 13).
To the prothonotary, upon exhibition of a license, for registry, $1 (ib., s. 14).
Rhode Island.
Registration.—Every physician must cause his name and residence to be recorded in the town clerk’s office of the town where he resides (Public Statutes, 1882, c. 85, s. 12).
Penalty.—Wilful neglect or refusal to perform this duty is punishable with a fine not exceeding $20 (ib., s. 11).
South Carolina.
Qualification.—All physicians engaging in the practice of medicine or surgery, before doing so, must submit their diplomas to a board consisting of three reputable physicians in each county. The board is appointed by the governor on the recommendation of the medical societies of the counties, and where no medical society exists, upon the recommendation of the senator and members of the House of Representatives for such counties (Act of 1890, c. 454, s. 1).
The said board must examine said diploma, when submitted, and if the holder is a bona fide holder, and if the college issuing said diploma is a reputable medical college, and if he also submits a certificate of good moral character, the board must certify to the fact, and upon such certificate the diploma shall be registered by the clerk of the court of the county in which the applicant resides (ib., s. 2).
Exception.—The act does not apply to physicians and surgeons already registered under former laws (ib., s. 4).
South Dakota.
Prohibition.—It is unlawful for any person to practise medicine, surgery, or obstetrics in any of their departments without having received a license to practise medicine from the board of health, and having it recorded in the office of the register of deeds in the county where such person resides (Act February 16th, 1893, s. 1).
Exceptions.—The act does not affect those in the lawful practice of medicine, surgery, or obstetrics in this State at the time of its passage (ib., s. 2).
Nor does it prohibit students from prescribing under the supervision of a preceptor, nor prohibit gratuitous services in case of emergency, nor apply to commissioned surgeons in the United States army and navy (ib., s. 3).
Penalty.—Violation of the act or practising without the license is a misdemeanor punishable with a fine of from $25 to $100 or imprisonment in the county jail not more than thirty days or both (ib., s. 4).
Qualification.—The State board of health is constituted a board of public examiners ex-officio to examine and license physicians to practise medicine. Any person who is a graduate of a lawful medical college, who has attended three full courses of medical lectures of six months each, no two full courses within the same year, and who is of good moral character, and is not an habitual drunkard, shall, upon proof of such facts to the superintendent of the State board of health, as the board shall require, receive from said superintendent a license; which shall be recorded as above. The requirement of three courses of lectures does not apply to those who had graduated prior to the passage of the act (ib., s. 5).
Cancellation of License.—The State board of health, upon complaint made to it on oath by one responsible person, has power to cancel any license that may have been fraudulently obtained or when the person to whom such license was issued is an habitual drunkard, or is guilty of immoral practices or gross unprofessional conduct. Such license shall not be cancelled[205] except after a hearing before such board of health, at which a majority of such board shall be present, and of which the person holding the license to be cancelled shall have had at least ten days’ notice, and only upon due proof of the facts stated in the complaint. An appeal may be taken to the circuit court of the county in which the person whose license is cancelled lives by any person aggrieved, in the same manner as now provided by law in case of appeal from the decisions of the county commissioners (ib., s. 6).
Fee.—To the superintendent of the State board of health, for a license, $5 (ib., s. 5).
Tennessee.
Qualification.—No person can lawfully practise medicine in any of its departments, except dentistry, unless he possesses the qualifications required by the act. If a graduate in medicine, he must present his diploma to the State board of medical examiners for verification as to its genuineness. If found genuine and from a legally chartered allopathic, homœopathic, or eclectic medical college in good standing with the school of medicine in which said college is classed, of which the State board of medical examiners shall be the judge, and the person named therein be the person claiming and presenting it, the board must issue a certificate to that effect, conclusive as to the rights of the lawful holder to practise medicine (Act of 1889, c. 178, s. 1).
Persons in actual practice at the time of the passage of the act were allowed till July 1st, 1891, to comply with the provisions of the act respecting them (ib., s. 2, as amended Act 1891, c. 109, s. 1).
A person wishing to enter upon the practice of medicine must present to the board of medical examiners a diploma from some medical college in good standing as provided by sec. 1, or shall present himself to the said board for examination upon anatomy, physiology, chemistry, pathology, surgery, obstetrics, and therapeutics. If the diploma be found genuine, or if the applicant for examination be found worthy and competent, the board shall issue a certificate which shall entitle the lawful holder to all the privileges of this act (ib., s. 3, as amended Act 1891, c. 109, s. 2).
The governor appoints six graduate physicians as a State board of medical examiners; the three schools allopathic, homœopathic, and eclectic must be represented on the board; five constitute a quorum and a majority of those present are necessary to reject an applicant, but such rejection shall not bar a re-examination after the lapse of three months; provided the members representing each school shall have the right to examine all applicants of that school, and the board shall issue the certificate to applicants who are recommended by the member or members of the board who belong to said school after such examination (ib., s. 4).
To prevent delay and inconvenience two members of the board may grant a temporary license to any applicant if the applicant has not been refused a license by the board within six months, which shall be in force till the next regular meeting of the board (ib., s. 5).
The members of the board shall not be members of the State board of health, nor any medical faculty (ib., s. 6).
The regular meeting of the board shall be once in each year at such time and place as the board may decide, but the president of the board may call a special meeting when demanded by public necessity (ib., s. 7).
Every person holding a certificate must have it recorded in the office of the county court clerk where he resides, and the date of record must be indorsed thereon. Until such record is made the holder shall not exercise any of the rights and privileges conferred. A person removing to another county to practise shall record his certificate in like manner in the county to which he removes. Practitioners may go from one county to another on professional business, without being required to register, if they have done so in the county in which they reside (ib., s. 9).
Itinerant Physician or Vender.—It is unlawful for an itinerant physician or vender of any drug, nostrum, ointment, or appliance of any kind intended for the treatment of disease or injury to sell or apply the same, or by writing, printing, or other method to profess to cure or treat disease or deformity by any drug, nostrum, manipulation, or other expedient.
A violation of this section is punishable with a fine of $100 to $400, but this section does not apply to merchants[207] and druggists, and this act does not apply to veterinary surgeons and stock doctors (ib., s. 13, as amended Act 1891, c. 109, s. 3).
Penalty, Exception.—To practise medicine or surgery without a certificate is a misdemeanor punishable with a fine of from $10 to $25.
To file or attempt to file as his own the diploma or certificate of another or a forged affidavit of identification is a felony punishable same as forgery. The act does not apply to women who pursue the avocation of midwife (ib., s. 14, as amended Act 1891, c. 109, s. 4).
Fees.—To the county court clerk, for recording certificate, the usual fee (ib., s. 9).
To the board of examiners, for issuing a certificate, $1.
To the board of examiners, for examination of non-graduate, $10.
If applicant fails to pass a satisfactory examination, and no certificate or license is issued to him, $5 only is retained.
For a certificate of temporary license, $1, which is to be credited to the applicant when he applies for a permanent license (ib., s. 12, as amended Act 1891, c. 109, s. 2).
Texas.
Constitutional Provision.—The legislature may pass laws prescribing the qualifications of practitioners of medicine, but no preference shall ever be given by law to any schools of medicine (Const. 1876, art. xiv., s. 31 in part).
Boards of Examiners.—A board of medical examiners for each judicial district is appointed by the judge of the district court (R. S., art. 3,625).
Each board is composed of not less than three practising physicians of known ability, graduates of some medical college recognized by the American Medical Association, residents of the district from which they are appointed (ib., art. 3,626).
The boards are required to meet regularly semi-annually at some central point in their districts to conduct examinations and grant certificates, and after at least one month’s public notice of the time and place of meeting by publication in at least one newspaper published in the district (ib., art. 3,629).
Qualification.—The board is required to examine thoroughly all applicants for a certificate of qualification to practise medicine in any of its branches or departments, whether furnished with medical diplomas or not, upon anatomy, physiology, pathological anatomy and pathology, surgery, obstetrics, and chemistry; but no preference shall be given to any school of medicine (ib., art. 3,632).
When the board is satisfied as to the qualifications of an applicant, they are required to grant a certificate, which entitles him to practise medicine in any county when it has been recorded (ib., art. 3,633).
Any two members of the board may grant a certificate, and any member may grant a temporary certificate upon examination, which shall be in force until the next regular meeting of the board (ib., art. 3,634).
The certificate must, before the person to whom it was granted is entitled to practise, be recorded in the office of the clerk of the district court of the county in which such practitioner resides or sojourns, and when recorded the clerk shall certify thereon under his official seal the fact and date of record, and shall return the certificate to its owner (ib., art. 3,635).
Exceptions.—This title does not apply to those who have already qualified under the act of May 16th, 1873, nor to those regularly engaged in the general practice of medicine in the State in any branch or department for five consecutive years prior to January 1st, 1875, nor to females who follow the practice of midwifery strictly as such (ib., art. 3,637).
Penalty.—No person except those named in art. 3,637 can lawfully practise medicine in any of its branches or departments without having first obtained and recorded a certificate of qualification as above provided. A person so offending shall be punished as provided in the Penal Code (ib., art. 3,638).
If any person shall practise for pay or as a regular practitioner medicine in any of its branches or departments, or offer or attempt to practise medicine without first having obtained a certificate of professional qualification from some authorized board of medical examiners, or without having a diploma from some actual medical college chartered by the legislature of the State, or its authority, in which the same is situated, he shall[209] be punished by a fine of not less than $50, nor more than $500 (Penal Code, art. 396).
Each patient visited or prescribed for, or each day’s offer to practise constitutes a separate offence (ib., art. 397).
If any person shall engage in the practice of medicine in any of its branches or departments for pay or as a registered practitioner, without having first filed for record, with the clerk of the district court of the county in which he resides or sojourns, a certificate from some authorized board of medical examiners or a diploma from some actual medical college, he shall be punished as prescribed in art. 396 (ib., art. 398).
Fees.—To the clerk of the district court, for recording certificate, $1 (R. S., art. 3,635).
To the board of examiners, for examination, $15, whether certificate is granted or not (R. S., art. 3,636).
Utah.
Board of Examiners.—The governor appoints by and with the advice and consent of the council a board of seven medical examiners from the various recognized schools of medicine; appointees are required to be graduates of a legally chartered medical college in good standing (Act 1892, c. 72, s. 1).
Qualification.—The board has power to issue certificates to all who furnish satisfactory proof of having received degrees or licenses from a chartered medical college in good and legal standing, and pass examinations before said board (ib., s. 2).
Graduates of respectable medical colleges at the time of the passage of the act engaged in actual practice in the Territory shall be licensed on presenting their degree to the board, and producing satisfactory evidence of identity (ib., s. 4).
Every person holding a certificate from said board must have it recorded in the office of the recorder of the county in which he resides within three months from its date, and the date of record must be indorsed thereon. Until the certificate is recorded, the holder shall not exercise any of the privileges conferred. A person removing to another county to practise must record his certificate in like manner in the county to which he removes (ib., s. 5).
Examinations shall be wholly or partly in writing (ib., s. 7).
The board may refuse to issue certificates to individuals guilty of unprofessional or dishonorable conduct, the nature of which shall be stated in writing, and it may revoke certificates for like causes to be stated in writing (ib., s. 8).
Definition.—Any person is regarded as practising medicine who treats, operates upon, or prescribes for any physical ailment of another for a fee, or who holds himself out by means of signs, cards, advertisements, or otherwise as a physician or surgeon.
Exceptions.—The act does not prohibit service in case of emergency or the administration of family remedies, and does not apply to commissioned surgeons of the United States army in discharge of their official duties, or to visiting physicians in actual consultation (ib., s. 9).
Offence.—Practising medicine or surgery without a certificate or contrary to this act is a misdemeanor (ib., s. 10).
Persons not graduates who had practised continuously for ten years in the Territory prior to the taking effect of the act were allowed six months in which to comply with its provisions concerning them. Practising without complying with these provisions, and practising after rejection of an application or the revocation of certificate, is a violation of the law (ib., s. 11).
Obstetricians.—Persons practising obstetrics were required within three months after the passage of the act to apply to the board for a certificate, and after passing a proper examination were entitled to one.
Practising obstetrics without first obtaining a license or contrary to this act is a misdemeanor; provided all persons who furnish to said board satisfactory evidence by affidavit or otherwise of having practised obstetrics previous to the passage of the act, shall receive a license without an examination. This section does not apply to physicians holding certificates nor prohibit services in cases of emergency, nor apply to persons practising obstetrics in communities where there are no licensed practitioners (ib., s. 12).
Board Meetings.—The board is required to meet at the territorial capital on the first Monday of January, March, June, and September of each year at 10 A.M., and such other times as the president of the board shall deem necessary (ib., s. 13).
Colleges.—“Respectable medical colleges” include colleges[211] in legal standing of any recognized school of medicine (ib., s. 15).
Fees.—To the treasurer of the board of examiners, for examination and certificate, $25 (ib., s. 3).
To the treasurer of the board of examiners, for license to a graduate, $5 (ib., s. 4).
The secretary of the board is required to enter without fee, on the register to be kept by him, the names of all persons to whom licenses are issued as physicians and surgeons (ib., s. 4).
To the county recorder, for recording, his usual fees (ib., s. 5).
To the treasurer of the board of examiners, upon examination for license to practise obstetrics, $10.
To the treasurer of the board of examiners, upon license to practise obstetrics without examination, $1 (ib., s. 12).
Vermont.
Qualification.—The medical societies organized under a charter from the General Assembly at each annual session elect a board of censors of three members, who may examine and license practitioners of medicine, surgery, and midwifery (Revised Laws, 1880, s. 3,908).
A practitioner of medicine, surgery, or midwifery who by sign or advertisement offers his services to the public as a practitioner of medicine, surgery, or midwifery, or who by such sign or advertisement assumes the title of doctor, shall obtain a certificate from one of such medical societies, either from a county, district, or State society (ib., s. 3,909).
A person not a resident of the State who has not received a diploma from a chartered medical college must obtain a certificate from a board of censors before he shall be permitted to practise the medical art in the State (ib., s. 3,910).
Each board of censors must issue certificates without fee to physicians and surgeons who furnish evidence by diploma from a medical college or university, or by a certificate of examination by an authorized board, which satisfies said censors that the person presenting such credentials has been, after due examination, deemed qualified to practise the branch mentioned in such diploma or certificate (ib., s. 3,911).
The censors in their discretion shall notify the practitioner of medicine, surgery, or midwifery of this chapter, and require such persons to comply therewith within thirty days after notification or such further time as is allowed by the censors not exceeding ninety days (ib., s. 3,912).
The certificate must set forth the branches of the medical art in which the person is qualified to practise (ib., s. 3,913).
The certificate must be recorded in the clerk’s office of the county in which the holder resides, or, if not a resident of the State, in the county in which he obtained his certificate (ib., s. 3,914).
A certificate issued by a board of censors is valid throughout the State after being duly recorded. The censors may revoke or annul a certificate if in their judgment the holder has obtained it fraudulently or has forfeited his right to public confidence by the conviction of crime (ib., s. 3,915).
Penalty.—To practise medicine, surgery, or midwifery in the State, or sign a certificate of death for burial or removal unless authorized by a certificate issued and recorded, is punishable with a fine of from $50 to $200 for the first offence, and for subsequent offences with a fine of from $200 to $500, recoverable by an action of debt for the use of any person who sues or by indictment (ib., s. 3,916).
No person practising either of the branches of medicine, surgery, or midwifery is permitted to enforce in the courts the collection of a fee or compensation for services rendered or medicine or material furnished in the practice of any of the branches for which he has not a certificate (ib., s. 3,917).
Exceptions.—The law does not apply to the practice of dentistry, nor to the practice of midwifery by women in the town or locality in which they reside, nor to practitioners of medicine who resided and practised medicine in the State for five years previous to November 28th, 1876 (ib., s. 3,918).
Virginia.
Board of Examiners.—There is a State board of medical examiners consisting of three members from each congressional district and two from the State at large, and five homœopathic physicians from the State at large (Code 1887, s. 1,744).
The board is composed of men learned in medicine and surgery appointed by the governor from a list of names recommended by the Medical Society of Virginia, together with five homœopathic physicians nominated to him by the Hahnemann Medical Society of the Old Dominion. The recommendations are required to be by votes of a majority present at some meeting of such society; but if the governor considers any person so recommended unsuitable he may decline to appoint him, in which case such society shall within ninety days after notification make another recommendation, and if the society fail to make a recommendation the governor is required to appoint such board in whole or in part without regard to such recommendation. If any examiner cease to reside in the district for which he was appointed his office is deemed vacant (ib., s. 1,745).
The regular meetings of the board are required to be held at least once a year, and at such times and places as the board may prescribe, and special meetings may be held on the call of the president and any five members (ib., s. 1,746).
Qualification.—The board at any of its meetings must examine all persons making application to them who desire to practise medicine or surgery; when an applicant shall have passed an examination satisfactory as to proficiency before the board in session the president must grant a certificate to that effect. If any applicant fail to pass a satisfactory examination before the board he shall not be permitted to stand a further examination within the next three months, nor shall he be required again to pay the fees prescribed, but no applicant shall be rejected on his examination on account of his adherence to any particular school of medicine or system of practice, nor on account of his views as to the method of treatment and the cure of disease.
When, in the opinion of the president of the board, the applicant has been prevented by good cause from appearing before the board, he shall appoint a committee of three members who shall examine the applicant and may grant a certificate having the same effect as though granted by a full board, until the applicant have an opportunity to appear before the board, when, if he fail to appear for examination, the president shall have the authority to revoke said certificate; or in any[214] case the president shall have authority, at his discretion, to grant a special permit to any applicant to practise medicine until he shall have an opportunity to appear before the board in session for examination, revokable at the discretion of the president. The board has in its discretion authority to accept in lieu of examination a certificate from a medical board of any other State, showing that the applicant has passed a satisfactory examination as to his proficiency, and obtained a license from said board to practise medicine and surgery in said State (ib., s. 1,747, as amended Act 1892, c. 70).
A person obtaining a certificate from the president of the board must cause it to be recorded in the clerk’s office of the county or the corporation court, of the county or corporation in which he resides, or, if he resides in the city of Richmond, in the clerk’s office of the chancery court of the said city (ib., s. 1,749).
No person who shall have commenced the practice of medicine or surgery since January 1st, 1885, or who shall hereafter commence the practice of the same, shall practise as a physician or surgeon for compensation without having obtained a certificate and caused it to be recorded.
Penalty.—The violation of this act is punishable with a fine of from $50 to $500 for each offence, and the violator is debarred from receiving compensation for services rendered as a physician or surgeon; a person assessed with a license tax as a physician or surgeon by any commissioner of revenue prior to July 1st, 1892, shall be taken as having commenced the practice of medicine or surgery prior to that date; but any person who shall not have been so assessed shall be taken as not having commenced such practice prior to that date (ib., s. 1,750, as amended Act 1892, c. 70).
Non-Residents.—A physician or surgeon residing in an adjoining State within ten miles of the boundary line of this State, is entitled to stand the examination and receive a certificate, and the certificate must be recorded in that county in the State nearest to his place of residence, and such certificate and recordation shall make it lawful for him to practise medicine and surgery in this State (ib., s. 1,751).
Exceptions.—This chapter does not affect practitioners of dentistry, nor include physicians or surgeons residing in other[215] States called into consultation in a special case with a physician or surgeon residing in this State, nor does it affect in any way the laws in reference to the license tax (ib., s. 1,752) nor does it apply to midwives (ib., s. 1,753).
Fees.—To the board of examiners, before examination, $5 (ib., s. 1,747, as amended Act 1892, c. 70).
To the clerk of the court, for recording, same fee as for recording a deed (ib., s. 1,749).
Washington.
Examining Board.—The governor is required to appoint a State medical examining board of nine members, learned and skilled in the practice and theory of medicine and surgery (Act March 28th, 1890, s. 1).
The said board is required to hold meetings for examination on the first Tuesday of January and July in each year, alternately in western and eastern Washington at such places as the board may designate. The board may call special meetings when, in the opinion of a majority of the board, they are necessary. The board is required to keep a record of all applicants for a license, with their ages, the time spent in the study and practice of medicine and surgery, and the name and location of all institutions granting to such applicants degrees or certificates of lectures in medicine or surgery, and whether such applicant was rejected or licensed; and said register is prima facie evidence of all matters therein recorded (ib., s. 2).
Qualification.—Every person desiring to commence the practice of medicine or surgery, or either of them, in any of their or its branches, must make a written application to the board for a license, supported by an affidavit of the applicant, setting forth the actual time spent in the study of medicine and surgery, and when; whether such study was in an institution of learning and, if so, its name and location; if not in such institution, where and under whose tutorship such study was prosecuted, the time engaged in the actual practice, if at all, of medicine and surgery or either, and where, and the age of the applicant at the time of the application, such application and affidavit to be filed and preserved of record in the office of the secretary of the board. At the time and place designated[216] by the board or at a regular meeting of the board, applicants must be examined in anatomy, physiology, chemistry, histology, materia medica, therapeutics, preventive medicines, the practice of medicine, surgery, obstetrics, diseases of women and children, of the nervous system, of the eye and ear, medical jurisprudence, and such other branches as the board deem advisable. The examination must be both scientific and practical, and of sufficient severity to test the candidate’s fitness to practise medicine and surgery, by written or printed, or partly written and partly printed, questions and answers, and the same are required to be filed and preserved of record in the said secretary’s office. After the examination, if it be satisfactory, the board shall grant a license, by the consent of not less than five members, except as hereinafter provided.
Refusal or Revocation.—The board may refuse or revoke a license for unprofessional or dishonorable conduct, subject to the right of appeal (ib., s. 3).
“Unprofessional or dishonorable conduct” means: procuring or aiding or abetting in procuring a criminal abortion; or employing what are popularly known as cappers or steerers; or obtaining any fee on the assurance that a manifestly incurable disease can be permanently cured; or wilfully betraying a professional secret; or advertisements of medical business in which untruthful and improbable statements are made; or advertising any medicine or means whereby the monthly periods of women can be regulated, or the menses re-established if suppressed; or the conviction of any offence involving moral turpitude; or habitual intemperance (ib., s. 4).
In case of a refusal or a revocation of a license, the board is required to file a brief and concise statement of the grounds and reasons thereof in the office of its secretary, which, with the decision of the board in writing, shall remain of record in said office. Before a license can be revoked for unprofessional or dishonorable conduct, a complaint of some person under oath must be filed in the office of the secretary of the board, charging the acts of unprofessional or dishonorable conduct and the facts complained against the accused in ordinary and concise language, and at least ten days prior to the hearing the board shall cause to be served upon the accused a written notice and a copy of such complaint containing a statement of the time and place[217] of the hearing. The accused may appear at the hearing and defend in person or by counsel, and may have the sworn testimony of witnesses taken and present other evidence in his behalf, and the board may receive arguments of counsel (ib., s. 5).
In case of refusal or revocation of a license by the board, there is a right of appeal within thirty days after the filing of the decree in the office of the secretary, to the superior court in and for the county in which was held the last general meeting of the board prior to the refusal of the license, in case of refusal; and to the superior court in and for the county in which the hearing was had upon which such license was revoked, in case of revocation. The person desiring to appeal must serve or cause to be served on the said secretary a written notice of appeal containing a statement of its grounds, and must file in the said secretary’s office an appeal bond with a good and sufficient surety to be approved by the Secretary of the State of Washington, conditioned for the speedy prosecution of such appeal and the payment of such costs as may be adjudicated against him upon such appeal. Said secretary must within ten days after service of said notice and filing, and the approval of the said appeal bond, transmit to the clerk of the court to which the appeal is taken a certified copy, under the seal of the board, of the decision and the grounds, in case of refusal, and in addition a certified copy under said seal of the complaint, in the case of revocation, with the bond and notice of appeal. The clerk must thereupon docket such appeal causes and they stand for trial in all respects as ordinary civil actions, and like proceedings are had thereon. On appeal the cause is tried de novo. Either party may appeal from a judgment of the superior court to the supreme court in like manner as in civil actions within sixty days after the rendition and entry of such judgment. If the judgment be in favor of the party appealing from the decision of the board, and the examining board does not appeal within sixty days, in that case at the end of sixty days the board shall immediately issue to the successful party the usual license, and in addition reinstate upon its records the name of such successful applicant, in case of revocation. In case of appeal to the supreme court by the board, no such license shall be issued nor re-instatement required until the final determination of the cause. In case[218] the final decision of the supreme court be against the board, then the said court shall make such order as may be necessary and the board shall act accordingly. No appeal bond can be required of the board, nor any costs adjudged or taxed against the same (ib., s. 6).
Filing Authority.—The person receiving a license must file it, or a copy, with the county clerk of the county where he resides, and the county clerk is required to file said certificate or copy and enter a memorandum thereof, giving its date and the name of the person to whom it was issued, and the date of filing, and on notice to him of a change of location or the death of a person licensed or of revocation, the county clerk is required to enter a memorandum of said fact at the appropriate place in the record. In case of removal into another county, the person licensed must procure from the county clerk a certified copy of the said license, and file it with the county clerk of the county to which he shall remove, with like effect as an original license (ib., s. 7).
Penalty, Definition.—To practise medicine or surgery without a license or contrary to this chapter is a misdemeanor punishable with a fine of from $50 to $100, or imprisonment in a county jail from ten to ninety days, or both. Any person is regarded as practising who appends the letters “M.D.” or “M.B.” to his name, or for a fee prescribes, directs, or recommends for the use of any person any drug or medicine or agency for the treatment, care, or relief of any wound, fracture, or bodily injury, infirmity, or disease; but the chapter does not apply to dentists.
Regulations.—The board has authority to prescribe and establish all needful rules and regulations to carry this chapter into effect (ib., s. 9).
Former Practitioner.—All persons licensed under sec. 2,289 of the laws of Washington Territory, 1881, or having complied with its provisions, are to be taken and considered as licensed under this act, and the secretary of the board is required to enter the names of such persons upon the register kept by him, as licensed physicians and surgeons on their written application (ib., s. 10).
Fee.—To the treasurer of the board, for examination, $10 (ib., s. 3).
West Virginia.
Qualification.—The following persons and no others are permitted to practise medicine:
1. Graduates of a reputable medical college in the school of medicine to which the person desiring to practise belongs. Such person must present his diploma to the State board of health, or the two members thereof in his congressional district, and if it be found to be genuine and was issued by such medical college as hereinafter mentioned, and the person presenting it be the graduate therein named, the board or said two members, as the case may be, must issue and deliver to him a certificate to that effect, and such diploma and certificate shall entitle the person named in the diploma to practise medicine in all its departments.
2. Persons not graduates in medicine who had practised medicine in this State under a certificate issued by the State board of health prior to the passage of the act are authorized to practise medicine in all its departments.
3. A person not a graduate of medicine and who has not practised medicine in this State under a certificate must be examined by the State board of health, or the two members thereof in the congressional district where he resides, or if he resides out of the State by the two members in the congressional district nearest to his place of residence, who, together with a member of the local board of health who is a physician, if there be such a member of the local board of health of the county in which the examination is held, shall examine him and if upon a full examination they find him qualified to practise medicine in all its departments, they, or a majority of them, shall grant him a certificate to that effect, and thereafter he shall have the right to practise medicine in the State to the same extent as if he had the diploma and certificate above mentioned. The members of the State board of health in each congressional district must, by publication in some newspaper printed in the county in which their meeting is to be held, or if no such paper is printed therein, in some newspaper of general circulation in such district, give at least twenty-one days’ notice of the time and place of their meeting for the examination[220] of applicants for permission to practise medicine, published at least once a week for three consecutive weeks before the day of such meeting.
This section does not apply to a physician or surgeon called from another State to treat a particular case or to perform a particular surgical operation in the State, or who does not otherwise practise in the State (Code of W. Va., 1891, c. 150, s. 9).
Every person holding a certificate must have it recorded in the office of the secretary of the State board of health, and the secretary is required to indorse on said certificate the fact of such recordation and deliver the same to the person named therein or his order.
The State board of health may refuse certificates to individuals guilty of malpractice or dishonorable conduct, and may revoke certificates for like causes; such revocation being after due notice and trial by the said board, with right of appeal to the circuit court of the county in which such individual resides; but no such refusal or revocation shall be made by reason of his belonging to or practising in any particular school or system of medicine (ib., s. 10).
The examination fee is not retained if a certificate is refused, but the applicant may again, at any time within a year after refusal, be examined without an additional fee, and if a certificate be again refused he may, as often as he sees fit, on payment of the fee, be examined until he obtains a certificate (ib., s. 11).
Examinations may be wholly or partly in writing, and shall be of an elementary and practical character, embracing the general subjects of anatomy, physiology, chemistry, materia medica, pathology, pathological anatomy, surgery, and obstetrics, but sufficiently strict to test the qualifications of the candidate as a practitioner of medicine, surgery, and obstetrics. The chapter does not apply to females practising midwifery (ib., s. 12).
Definition, Exceptions.—Any person is regarded as practising medicine who professes publicly to be a physician, and to prescribe for the sick, or who appends to his name “M.D.” This act also applies to apothecaries and pharmacists who prescribe for the sick. It does not apply to commissioned[221] officers of the United States army and navy and marine hospital service (ib., s. 13).
Itinerant Physician or Vender.—Any itinerant physician or itinerant vender of any drug, nostrum, ointment, or appliance of any kind intended for the treatment of disease or injury, or who shall by writing or printing or in any other method publicly profess to cure or treat diseases, injuries, or deformities by any drug, nostrum, manipulation, or other expedient, shall before doing so pay to the sheriff of every county in which he desires to practise a special tax of $50 for each month or fraction of a month he shall so practise in such county, and take his receipt in duplicate therefor. He shall present said receipts to the clerk of the county court of such county, who shall file and preserve one of them in his office and indorse on the other, “A duplicate of this receipt has been filed in my office,” and sign the same. For such a person to practise or attempt to practise in any county without having paid such tax and filed such receipt and obtained such indorsement, or to practise or attempt to practise for a longer time than that for which he has paid a tax, is a misdemeanor punishable with a fine of from $100 to $500. Any person who shall travel from place to place and by writing, printing, or otherwise publicly profess to cure or treat diseases, injuries, or deformities is deemed an itinerant physician subject to the taxes, fines, and penalties of this section (ib., s. 14).
Penalty.—To practise or attempt to practise medicine, surgery, or obstetrics without complying with sec. 9 is a misdemeanor punishable, for every offence, with a fine of from $50 to $500 or imprisonment in a county jail from one month to twelve months, or both. To file or attempt to file as his own a diploma or certificate of another, or a false or forged affidavit of identity, or wilfully swear falsely to any question propounded to him on examination or to any affidavit required to be made and filed, is punishable with confinement in the penitentiary from one to three years or imprisonment in a county jail from six to twelve months, and a fine of from $100 to $500 (ib., s. 15).
Fee.—To the State board of health, or its examining members, for examination, $10 (ib., s. 11).
Wisconsin.
Prohibition.—No person practising physic or surgery, or both, shall have the right to collect in any action in any court fees or compensation for the performance of any medical or surgical service, or to testify in a professional capacity as a physician or surgeon, unless he shall have received a diploma from some incorporated medical society or college or shall be a member of the State or some county medical society legally organized in this State; provided that in all criminal actions the court may in its discretion and in the furtherance of justice receive the testimony of any physician or surgeon without requiring proof of the incorporation of the medical society or college from which he graduated (R. S., 1878, s. 1,436, as amended c. 131, 1887).
No person practising physic or surgery, or both, prohibited by the above section from testifying in a professional capacity as a physician or surgeon, shall assume the title of doctor, physician, or surgeon by means of any abbreviation or by the use of any other word or words, letters of the alphabet of the English or any other language, or any device of whatsoever kind, printed, written, or painted, or exhibited in any advertisement, circular, handbill, letter, or other instrument, nor on any card, sign, door, or place whatsoever.
Penalty, Exceptions.—A violation of this act is a misdemeanor punishable with a fine of from $25 to $100, or imprisonment in a county jail from ten days to sixty days for each offence (s. 1, c. 256, 1881, as amended c. 40, 1882).
On complaint in writing under oath before any magistrate or justice of the peace charging the commission of an offence against the provisions of this act in his county, it is the duty of the district attorney to prosecute the offender, and in all such prosecutions the burden of proof shall be upon the defendant to establish his right to use such title under the provisions of this act (ib., s. 2).
Any person prohibited by sec. 1 from assuming the title of doctor, physician, or surgeon who shall practise or pretend to practise physic or surgery, or both, is not exempted from any, but is liable to all, of the legal penalties and liabilities of malpractice,[223] and ignorance shall be no excuse for a failure to perform or for neglect or unskilfully performing or attempting to perform any of the duties required by law of practising physicians or surgeons. The act does not prevent students from practising under the direction of a qualified preceptor, nor women from practising midwifery, nor veterinarians from practising in their special department (ib., s. 3).
Wyoming.
Qualification.—No person can lawfully practise medicine, surgery, or obstetrics who has not received a medical education and diploma from some regularly chartered medical school having a bona fide existence when the diploma was granted (R. S., 1887, s. 1,925).
Every physician, surgeon, or obstetrician must file for record with the register of deeds of the county in which he is about to practise or where he practises, a copy of his diploma, exhibiting the original, or a certificate from the dean of the medical school of which he is a graduate certifying to his graduation (ib., s. 1,926).
When filing a copy of his diploma or certificate of graduation, he must be identified as the person named in the paper about to be filed by the affidavit of two citizens of the county, or his affidavit taken before a notary public or commissioner of deeds for the State, which affidavit must be filed in the office of the register of deeds (ib., s. 1,927).
Penalty.—To practise without complying with this chapter is a misdemeanor punishable with a fine of from $50 to $500 or imprisonment in a county jail from thirty days to six months, or both, for each offence. To file or attempt to file as his own a diploma or certificate of another, or a forged affidavit of identification, is a felony subject to a fine and imprisonment in the penitentiary (ib., s. 1,928).
It is the duty of the police, sheriff, or constable to arrest all persons practising medicine, surgery, or obstetrics without complying with these provisions (ib., s. 1,929).
Exceptions.—This chapter does not apply to persons in emergency prescribing or giving advice in medicine, surgery, or obstetrics in a section of country where no physician, surgeon,[224] or obstetrician resides, or where no physician, surgeon, or obstetrician resides within a convenient distance, nor to persons prescribing in their own families, nor to persons claiming to practise medicine, surgery, or obstetrics in any section of the State where no physician or surgeon having a diploma or a certificate resides (ib., s. 1,930).
Evidence.—On the trial of persons charged with the violation of this chapter it shall be sufficient for the prosecution to show that defendant has practised medicine, surgery, or obstetrics within the county where the indictment is found at any time since the passage of the act (1876), and the defendant shall not after proof be entitled to acquittal until he shows by the testimony of some competent witness upon oath that the defendant has received a medical education, and a genuine diploma from some regularly chartered medical school; provided that the defendant may show such facts by depositions taken in the same manner as depositions in civil cases (ib., s. 1,931).
The United Kingdom of Great Britain and Ireland.
Medical Acts.—The Act 21 and 22 Victoria, c. 90, and the amendments thereof and additions thereto, are generally spoken of as the Medical Acts.
Medical Councils.—There is a general council of medical education and registration of the United Kingdom, with branch councils for England, Scotland, and Ireland (21 and 22 Vict., 1858, c. 90, s. 3, 6).
Members of the general council are chosen as provided in 49 and 50 Vict., c. 48, s. 7; those representing the medical corporations must be qualified to register under this act (21 and 22 Vict., c. 90, s. 7).
The general council appoints a registrar for England, and the branch councils for Scotland and Ireland appoint respectively a registrar for Scotland and Ireland (ib., s. 10, 11).
Registrar.—It is the duty of the registrars to keep their registers correct, and to erase the names of all registered persons who shall have died, and from time to time to make the necessary alterations in the addresses or qualifications of persons registered. It is lawful for the registrar to write a letter to any registered[225] person, addressed to him according to his address on the register, to inquire whether he has ceased to practise or has changed his residence, and if no answer be returned within six months from the time of sending the letter, it is lawful to erase the name of such person from the register, but it may be restored by direction of the general council (ib., s. 14).
Qualification.—Persons possessed of one or more of the qualifications described in Schedule A, on the payment of a fee not exceeding £5, are entitled to register on the production to the registrar of the branch council for England, Scotland, or Ireland the document conferring or evidencing the qualification in respect whereof he seeks to be registered, or upon transmitting by post to such registrar information of his name and address, and evidence of his qualifications and of the time or times at which they were obtained. The several colleges and bodies mentioned in Schedule A may transmit from time to time to the registrar, under their respective seals, lists of the persons who by grant of such colleges and bodies respectively, are for the time being entitled to register, stating the qualifications and residences of such persons, and it shall be lawful for the registrar on the payment of the said fee to enter in the register the persons mentioned in such lists with their qualifications and places of residences as therein stated without other application (ib., s. 15).
The general council is required to make orders for regulating the registers from time to time (ib., s. 16).
Persons actually practising medicine in England before August 1st, 1815, were entitled to register under the act (ib., s. 17).
Any two or more of the colleges and bodies in the United Kingdom mentioned in Schedule A may, with the sanction and under the direction of the general council, unite or co-operate in conducting the examinations required for qualifications to be registered (ib., s. 19, 37 and 38 Vict., c. 34).
The privy council may suspend the right of registration in respect of qualifications granted by any college or body (ib., s. 21).
After such revocation, no person shall be entitled to register in respect to any qualification granted by such college before revocation (ib., s. 22).
The privy council may issue an injunction directing any[226] body entitled to grant qualifications to desist from imposing upon any candidate for examination an obligation to adopt or refrain from adopting the practice of any particular theory of medicine or surgery as a test or condition of admitting him to examination or granting him a certificate; and in the event of their not complying, may order that such body cease to have the power of conferring a right to be registered so long as they shall continue such practice (ib., s. 23).
Where any person entitled to be registered applies to the registrar of any branch council for that purpose, such registrar is required forthwith to enter in a local register the name and place of residence, and the qualifications in respect of which the person is so entitled and the date of registration; and in case of the branch council for Scotland or Ireland, to send to the registrar of the general council a copy of the entry, and the registrar of the general council is required to cause the same to be entered in the general register; and such registrar is required to cause all entries made in the local register for England to be entered in the general register (ib., s. 25).
No qualification is entered on the register, on the first registration or by way of addition to a regular name, unless the registrar be satisfied by proper evidence that the person claiming it is entitled to it. Any appeal from the decision of the registrar may be decided by the general council or by the council for England, Scotland, or Ireland, as the case may be. Any entry proved to the satisfaction of such general council or branch council to have been fraudulently or incorrectly made may be erased from the register by an order in writing of such general council or branch council (ib., s. 26).
Medical Register.—The registrar of the general council is required to cause to be printed, published, and sold under the direction of such council, every year, a correct register of the names with the respective residences and medical titles, diplomas, and qualifications conferred by any corporation or university or by a doctorate of the Archbishop of Canterbury, with the dates thereof, of all persons appearing on the general register as existing on January 1st in every year. Such register is called the Medical Register, and a copy of the Medical Register for the time being is evidence that the persons therein specified are registered according to the act, and the absence of[227] the name of any person from such copy is evidence, until the contrary be made to appear, that such person is not so registered; provided, that in the case of any person whose name does not appear in such copy, a certified copy under the hand of the registrar of the general council or a branch council of the entry of the name of such person on the general or local register shall be evidence that such person is so registered (ib., s. 27).
If any college or body exercise any power it possess of striking off from its list the name of any one of its members, it shall signify his name to the general council and the said council may, if they see fit, direct the registrar to erase from the register the qualification derived from such college or body in respect of which such member was registered, and the registrar shall note the same therein, but the name of no person shall be erased from the register on the ground of his having adopted any theory of medicine or surgery (ib., s. 28).
If any registered medical practitioner shall be convicted in England or Ireland of any felony or misdemeanor, or in Scotland of any crime or offence, or shall be after due inquiry judged by the general council to have been guilty of infamous conduct in any professional respect, the general council may, if they see fit, direct the registrar to erase the name of such medical practitioner from the register (ib., s. 29).
Every person registered who may have obtained any higher degree or other qualification is entitled to have it inserted in the register in substitution for or in addition to his qualification previously registered, on the payment of such fee as the council may appoint (ib., s. 30).
Compensation.—No person is entitled to receive for any medical or surgical advice, or attendance, or for the performance of any operation or for any medicine which he shall have both prescribed and supplied, unless he prove upon the trial that he is registered under this act (ib., s. 32, as amended 23 and 24 Vict., c. 7, s. 3).
Definition.—The words “legally qualified medical practitioner” or “duly qualified medical practitioner,” or any words implying a person recognized by law as a medical practitioner or member of the medical profession in any act of Parliament, mean a person registered under this act (ib., s. 34, as amended 23 and 24 Vict., c. 7, s. 3).
Exemptions.—If they so desire, registered persons are exempt from serving on juries, and in all corporation, parish, ward, hundred, and town offices, and in the militia (ib., s. 35).
Disqualifications.—No unregistered person is permitted to hold any appointment as a physician, surgeon, or other medical officer in the military or naval service, or in emigrant or other vessels, or in any hospital, infirmary, dispensary, or lying-in hospital, not supported wholly by voluntary contributions, or in any lunatic asylum, jail, penitentiary, house of correction or of industry, parochial or union workhouse or poor-house, parish union, or other public established body or institution, or to any friendly or other society for affording mutual relief in sickness, infirmity, or old age, or as a medical officer of health (ib., s. 36, as amended 23 and 24 Vict., c. 7, s. 3).
No certificate required by any act from any physician or surgeon licentiate in medicine and surgery, or other medical practitioner, is valid unless the signer be registered under this act (ib., s. 37, as amended 23 and 24 Vict., c. 7, s. 3).
Penalty.—Wilfully procuring or attempting to procure one’s self to be registered by making or producing or causing to be made or produced any false or fraudulent representation or declaration, or aiding or abetting therein, is a misdemeanor in England and Ireland, and in Scotland a crime or offence, punishable by fine or imprisonment. The imprisonment cannot exceed twelve months (ib., s. 39).
Wilfully and falsely pretending to be or taking or using the name or title of physician, doctor of medicine, licentiate in medicine and surgery, bachelor of medicine, surgeon, general practitioner, or apothecary, or any name, title, addition, or description implying registration under this act, or recognition by law as a physician or surgeon or licentiate in medicine and surgery, or practitioner in medicine, or apothecary, is punishable on summary conviction by a penalty not exceeding £20 (ib., s. 40, 41).
Deceased Physicians.—Every registrar of deaths in the United Kingdom, on receiving notice of the death of any medical practitioner, is required to transmit to the registrar of the general council and the registrar of the branch council a certificate of such death with the time and place, and on the receipt[229] of such certificate the medical registrar is required to erase the name of the deceased from the register (ib., s. 45).
Exceptions.—The general council was by the act empowered by special order to dispense with such provisions of this act or such part of any regulations made by its authority as to them should seem fit, in favor of persons at the time of its passage practising medicine or surgery in any part of Her Majesty’s dominions other than Great Britain and Ireland by virtue of any of the qualifications in Schedule A, and in favor of persons practising medicine or surgery within the United Kingdom on foreign or colonial diplomas or degrees before the passage of this act, and in favor of any persons who had held appointments as surgeons or assistant surgeons in the army, navy, or militia, or in the service of the East India Company, or who were acting as surgeons in the public service, or in the service of any charitable institution, and in favor of medical students who commenced their professional studies before its passage (ib., s. 46).
The qualifications specified in Schedule A are as follows:
1. Fellow, member (inserted 22 Vict., c. 21, s. 4), licentiate, or extra licentiate of the Royal College of Physicians of London (this is declared by 23 and 24 Vict., c. 66, s. 1, to denote the corporation of “The President and College or Commonalty of the Faculty of Physics in London”). (The act makes provision for a new charter with change of name to “The Royal College of Physicians of England,” or retention of old name: ib., s. 47, as amended 23 and 24 Vict., c. 66, s. 2.)
2. Fellow, member (inserted 22 Vict., c. 21, s. 4), or licentiate of the Royal College of Physicians of Edinburgh. (The act makes provision for the granting of a new charter to the Royal College of Physicians of Edinburgh, whereby its name is to be changed to “The Royal College of Physicians of Scotland,” or its old name may be retained: ib., s. 49, as amended 23 and 24 Vict., c. 66, s. 2.)
3. Fellow or licentiate of the King’s and Queen’s College of Physicians of Ireland. (The act makes provision for the granting of a new charter to this college, whereby its name is to be changed to “The Royal College of Physicians of Ireland,” or its old name may be retained: ib., s. 51, as amended 23 and 24 Vict., c. 66, s. 2.)
4. Fellow or member or licentiate in midwifery of the Royal College of Surgeons of England.
5. Fellow or licentiate of the Royal College of Surgeons of Edinburgh (see 6, below).
6. Fellow or licentiate of the Faculty of Physicians and Surgeons of Glasgow. (The act makes provision for the possible amalgamation of the Royal College of Surgeons of Edinburgh with the Faculty of Physicians and Surgeons of Glasgow, in which case the united corporation is to be named “The Royal College of Surgeons of Scotland:” ib., s. 50.)
7. Fellow or licentiate of the Royal College of Surgeons in Ireland.
8. Licentiate of the Society of Apothecaries, London.
9. Licentiate of the Apothecaries’ Hall, Dublin.
10. Doctor or bachelor or licentiate of medicine, or master in surgery of any university of the United Kingdom; or doctor of medicine, by doctorate granted prior to the passage of the act by the Archbishop of Canterbury.
11. Doctor of medicine of any foreign or colonial university or college, practising as a physician in the United Kingdom before October 1st, 1858, who shall produce certificates to the satisfaction of the council, of his having taken his degree of doctor of medicine after a regular examination, or who shall satisfy the council under sec. 46 (amended 22 Vict., c. 21, s. 5) of this act, that there is sufficient reason for admitting him to be registered.
Nothing in the above act shall prevent any person, not a British subject, who shall have obtained from any foreign university a degree or diploma of doctor in medicine, and who shall have passed the regular examinations entitling him to practise medicine in his own country, from being and acting as the resident physician or medical officer of any hospital established exclusively for the relief of foreigners in sickness; provided always such person is engaged in no medical practice except as such resident physician or medical officer (22 Vict., c. 21, s. 6).
The following qualification was added by 23 and 24 Vict., c. 7, s. 1:
A diploma or license in surgery granted by any university in Ireland legally authorized to grant the same.
The act 39 and 40 Vict., c. 40, in sec. 3, provides that all persons who have obtained from any university of the United Kingdom legally authorized to confer the same, the degree of bachelor in surgery, shall be permitted to register the same as a qualification under 21 and 22 Vict., c. 90.
The diploma of a member of the King’s and Queen’s College of Physicians in Ireland, and the degree of Master in Obstetrics of any university in the United Kingdom are added to the qualifications in Schedule A of the Medical Act of 1858 (49 and 50 Vict., c. 48, s. 20).
The change of name of any of the corporations named in 21 and 22 Vict., c. 90, is not to alter or affect the qualifications constituted by the act (23 and 24 Vict., c. 66, s. 3).
Revocation of License.—The Society of Apothecaries may strike off from the list of licentiates of said society the name of any person who shall be convicted in England or Ireland of any felony or misdemeanor, or in Scotland of any crime or offence, or who shall, after due inquiry, be judged by the general council to have been guilty of infamous conduct in any professional respect, and the said society shall forthwith signify to the general council the name of the licentiate so stricken off (37 and 38 Vict., c. 34, s. 4).
Women.—The Society of Apothecaries is not relieved from any existing obligation, nor deprived of any right, to admit women to the examinations required for certificates to practise as apothecaries, or to enter the lists of licentiates of said society, any women who shall have satisfactorily passed such examinations, and fulfilled the other general conditions imposed upon persons seeking to obtain from the said society a qualification to be registered under 21 and 22 Vict., c. 90 (ib., s. 5).
The act 39 and 40 Vict., c. 41, extends the powers of every body entitled under 21 and 22 Vict., c. 90, to grant qualifications for registration so that it may grant any qualification for registration granted by such body without distinction of sex—but nothing in this act is compulsory.
The Medical Act of 1886 (49 and 50 Vict., c. 48) modified the foregoing acts as follows:
Examination.—A person cannot lawfully be registered under the medical acts in respect of any qualification referred to in any of those acts unless he has passed such qualifying examination[232] in medicine, surgery, and midwifery as is in this act mentioned (49 and 50 Vict., c. 48, s. 2).
A qualifying examination shall be an examination in medicine, surgery, and midwifery held for the purpose of granting a diploma or diplomas conferring the right of registration under the medical acts, by any of the following bodies:
(a) Any university in the United Kingdom, or any medical corporation legally qualified at the time of the passage of this act to grant such diploma or diplomas in respect of medicine or surgery; or
(b) Any combination of two or more medical corporations in the same part of the United Kingdom, who may agree to hold a joint examination in medicine, surgery, and midwifery, and of whom one at least is capable of granting such diploma as aforesaid in respect of medicine, and one at least is capable of granting such diploma in respect of surgery; or
(c) Any combination of any such university as aforesaid with any other such university or universities, or of any such university or universities with a medical corporation or corporations; the bodies forming such combination being in the same part of the United Kingdom (ib., s. 3 [1]).
The standard of proficiency at said examinations shall be such as suffices to guarantee the possession of knowledge and skill requisite for the efficient practice of medicine, surgery, and midwifery. It is the duty of the general council to secure the maintenance of such standard of proficiency, and it may appoint such number of inspectors as it may determine who shall attend at all or any of the said examinations (ib., s. 3 [2]).
The inspectors are not to interfere with the conduct of any examination, but to report to the general council their opinion as to the sufficiency or insufficiency of every examination which they attend, and such other matters in relation thereto as the general council may require (ib., s. 3 [3]).
If it appears to the general council that the standard of proficiency in medicine, surgery, and midwifery, or in any of those subjects or any branch thereof required at such examinations by any such body, is insufficient, the privy council, on a report from the general council after considering such report, and any objection thereto by any body to which it relates, may by order declare that the examination of such body or bodies shall not[233] be deemed a qualifying examination for registration, and Her Majesty, with the advice of the privy council, may revoke such order if upon further report from the general council, or any body to which it relates, it seems to her expedient (ib., s. 4 [1]).
During the continuance of such order, the examinations held by the body or bodies to which it relates shall not be deemed qualifying examinations, and a diploma granted to a person passing such examinations shall not entitle such person to registration (ib., s. 4 [2]).
If a medical corporation represent to the general council that it is unable to enter into a combination for holding a qualifying examination, and the general council is satisfied that the said corporation has used its best endeavor to do so on reasonable terms, the general council may on the application of such corporation appoint any number of examiners to assist at the examinations for granting a diploma conferring on the holder the right of registration (ib., s. 5 [1]).
It is the duty of the said assistant examiners to secure at the said examinations the maintenance of such standard of proficiency in medicine, surgery, and midwifery as is required from candidates at qualifying examinations, and any examination held subject to this section shall be deemed a qualifying examination (ib., s. 5 [2]).
Practitioner’s Rights.—A registered medical practitioner shall be entitled to practise medicine, surgery, and midwifery in the United Kingdom, and subject to any local law, in any other part of Her Majesty’s dominions, and to recover in due course of law in respect of such practice, any expenses or charges in respect of medicaments or other appliances, or any fees to which he may be entitled, unless he is a fellow of a college of physicians, the fellows of which are prohibited by by-law from recovering at law their expenses, charges or fees, in which case such prohibitory by-law, so long as it is in force, may be pleaded in bar of any legal proceeding instituted by such fellow for recovery of expenses, charges, or fees (ib., s. 6).
Members of General Council.—The constituent members of the general council are designated by this act in sec. 7.
Members of the general council representing the registered medical profession must themselves be registered medical practitioners,[234] and members of the branch council for the part of the United Kingdom in which they are elected (ib., s. 8).
Colonial and Foreign Practitioners.—When a person shows to the satisfaction of the registrar of the general council that he holds some recognized colonial medical diploma or diplomas granted to him in a British possession to which this act applies, and that he is of good character, and is by law entitled to practise medicine, surgery, and midwifery in such British possession, he shall on application to the said registrar, and on the payment of such fee not exceeding £5, as the general council may determine, be entitled without examination in the United Kingdom to be registered as a colonial practitioner in the medical register; provided he proves to the satisfaction of the registrar:
(1) That the said diploma or diplomas was or were granted to him at a time when he was not domiciled in the United Kingdom, or in the course of a period of not less than five years during the whole of which he resided outside of the United Kingdom; or
(2) That he was practising medicine or surgery or a branch of medicine or surgery in the United Kingdom on the prescribed day, and that he has continued practising the same either in the United Kingdom or elsewhere for not less than ten years immediately preceding the prescribed day (ib., s. 11).
When a person shows to the satisfaction of the registrar of the general council that he holds some recognized foreign medical diploma or diplomas granted in a foreign country, to which this act applies, and that he is of good character, and is by law entitled to practise medicine, surgery, and midwifery in such foreign country, he shall on application to said registrar, and on payment of such fee, not exceeding £5, as the general council may determine, be entitled without examination in the United Kingdom to be registered as a foreign practitioner in the medical register; provided he proves to the satisfaction of the registrar:
(1) That he is not a British subject; or
(2) That, being a British subject, the said diploma or diplomas was or were granted to him at a time when he was not domiciled in the United Kingdom or in the course of a[235] period of not less than five years, during the whole of which he resided out of the United Kingdom; or
(3) That, being a British subject, he was practising medicine or surgery, or a branch of medicine or surgery in the United Kingdom on the prescribed day, and that he has continued practising the same in the United Kingdom or elsewhere, for not less than ten years immediately preceding the said prescribed day (ib., s. 12).
The medical diploma granted in a British possession or foreign country to which this act applies, which is to be deemed requisite, shall be such a diploma as may be recognized by the general council as furnishing a sufficient guarantee of the possession of the requisite knowledge and skill for the efficient practice of medicine, surgery, and midwifery.
When the general council have refused to recognize any such diploma, the privy council may, on appeal, after communicating with the general council, order the general council to recognize such diploma.
If the refusal of the registration of a colonial or foreign practitioner be on any other ground, the registrar of the general council shall, if required, state in writing the reason for the refusal, and the person refused may appeal to the privy council, which, after communicating with the general council, may dismiss the appeal or order the general council to enter the name of the applicant on the register.
A person may be registered both as a colonial and foreign practitioner (ib., s. 13).
The medical register shall contain separate lists of the names and addresses of colonial and foreign practitioners, and the provisions of 21 and 22 Vict., c. 90, relating to persons registered and to the medical register, and to offences, shall apply in the case of colonial and foreign practitioners registered under this act so far as may be (ib., s. 14).
Any registered practitioner on the list of colonial or foreign practitioners who is in possession of or obtains any recognized colonial or foreign medical diploma granted in a British possession or foreign country to which this act applies may cause a description of such diploma to be added to his name in the medical register (ib., s. 15).
Any registered medical practitioner on the medical register[236] by virtue of English, Scotch, or Irish qualifications, and in possession of a foreign degree in medicine, may cause a description of such foreign degree to be added to his name as an additional title in the medical register, provided he satisfy the general council that he obtained such degree after a proper examination and prior to the passage of this act (ib., s. 16).
Her Majesty may from time to time, by order in the council, declare that this act be deemed to apply to any British possession or foreign country which in the opinion of Her Majesty affords the registered medical practitioners of the United Kingdom such privileges of practice in the said British possessions or foreign countries as to Her Majesty may seem just; and on and after the day named in such order such British possession or foreign country shall be deemed to be a British possession or foreign country to which this act applies. Her Majesty may also renew or revoke any such order, and upon such revocation such possession or foreign country shall cease to be a possession or country to which this act applies without prejudice to the right of any person whose name has already been entered on the register (ib., s. 17).
Nothing in the Medical Act of 1858 shall prevent a person holding a medical diploma, entitling him to practise medicine or surgery in a British possession to which this act applies, from holding an appointment as a medical officer in any vessel registered in that possession (ib., s. 18).
Default of General Council.—In default of the general council to perform any duty, the privy council may notify their opinion to the general council, and on the failure of the general council to comply with any direction of the privy council, the privy council may themselves give effect to such direction, and for that purpose exercise any power vested in the general council, and of their own motion do anything which they are authorized to do in pursuance of a report or suggestion from the general council (ib., s. 19).
Sanitary Science.—Every registered medical practitioner to whom a diploma for proficiency in sanitary science, public health or state medicine has after special examination been granted, by any college or faculty of physicians or surgeons or university in the United Kingdom, or by any such bodies acting in combination, shall, if such diploma appear to the privy[237] council or general council to deserve recognition in the medical register, be entitled on the payment of such fee as the general council may appoint, to have such diploma entered in the said register in addition to any other diploma or diplomas in respect of which he is registered (ib., s. 21).
Evidence.—Any act of the privy council shall be sufficiently signified by an instrument signed by the clerk of the council, and every order and act signified by an instrument purporting to be signed by the clerk of the council shall be deemed to have been duly made and done by the privy council, and every instrument so signed shall be received in evidence without proof of the authority or signature of the clerk of the council or other proof (ib., s. 22).
The following copies of any orders made in pursuance of medical acts or this act shall be evidence:
(1) Any copy purporting to be printed by the Queen’s printer, or by any other printer in pursuance of an authority given by the general council.
(2) Any copy of an order certified to be a true copy by the registrar of the general council, or by any other person appointed by the general council, either in addition to or in exclusion of the registrar, to certify such orders (ib., s. 23).
Rights Unaffected.—This act does not vary the rights of persons practising as registered medical practitioners on the day preceding the day when it goes into effect (ib., s. 24).
In consequence of the repeal of any enactment repealed by this act, no person legally entitled to practise as a medical practitioner in any colony or part of Her Majesty’s dominions other than the United Kingdom shall cease to be so entitled if he would have been entitled if no such repeal had taken place (ib., s. 25).
Definitions.—In the act the word diploma means any diploma, degree, fellowship, membership, license, authority to practise, letters, testimonial, certificate or other status or document granted by any university, corporation, college, or other body or by any departments of or person acting under the authority of the government of any country or place within or without Her Majesty’s dominion (ib., s. 27).
Fees.—The fees are to be determined by the general council within the limits set by the various sections authorizing fees.
British Columbia.
Medical Council.—There is a body styled “The Medical Council of British Columbia,” composed of seven members who are registered medical practitioners elected by the votes of registered medical practitioners (Cons. Acts 1888, c. 81, s. 2, 3, 4, 5).
No person can lawfully vote at such election unless his fees to the council have been paid; and no person is eligible to election unless qualified to vote at such election (ib., s. 14).
A register of such qualified voters is required to be prepared by the registrar of the council and no person is entitled to vote whose name is not on the register; it is the duty of the registrar to examine into the written complaint of any medical practitioner as to the improper omission or insertion of any name in the list; and appeal from his decision lies to a judge of the supreme court in a summary way, whose decision shall be final, and no unregistered person may vote (ib., s. 16, 17).
Register.—The council is required to appoint a registrar and to cause a register to be kept by him of the names of all persons who have complied with this act and with the rules and regulations made by the council respecting the qualifications of practitioners of medicine or surgery, and those persons only whose names are inscribed in the said register, are deemed qualified and licensed to practise medicine or surgery except as hereinafter provided (ib., s. 26).
The registrar is required to keep his register correct, and to make the necessary alterations in the addresses and qualifications of registered persons (ib., s. 27).
Qualification.—Every person at the passage of the act (1886) registered under the medical ordinance of 1867 is entitled to be registered under this act (ib., s. 28).
The council is required to admit upon the register any person who shall procure from any college or school of medicine and surgery requiring a three-years’ course of study, a diploma of qualification, provided he furnish to the council satisfactory evidence of identity and pass before the members thereof a satisfactory examination touching his fitness and capability to practise as a physician and surgeon (ib., s. 29).
The council is required to admit upon the register every person mentioned in 49 and 50 Vict., c. 48, of the Acts of Parliament of the United Kingdom, duly registered under the imperial Medical Act, prior to and inclusive of June 30th, 1887, upon complying with the orders, regulations or by-laws of the council and giving due proof of such registration, and that the person applying for registration has not lost the benefit of same by reason of misconduct or otherwise, and upon payment of the fees fixed by the council, not to exceed one hundred dollars (Act 1893, c. 27, s. 2).
Duties of Council.—The council is required to make orders, regulations, or by-laws for regulating the register and the fees to be paid for registration, and to make rules and regulations for the guidance of examiners, and may prescribe the subjects and modes of examination, and make all such rules and regulations in respect of examinations not contrary to this act as they deem expedient and necessary (Cons. Acts 1888, c. 81, s. 31).
Forfeiture of Right.—Any registered practitioner convicted of any felony thereby forfeits his right to registration and by direction of the council his name is required to be erased from the register, or in case a person known to have been convicted of felony presents himself for registration, the registrar has power to refuse such registration (ib., s. 32).
Rights of Registered Practitioner.—Every person registered under the act is entitled to practise medicine and surgery, including midwifery, or any of them as the case may be, in British Columbia, and to demand and receive in any court of the province, with full costs of the suit, reasonable charges for professional aid, advice, and visits, and the costs of any medical or surgical appliances rendered or supplied by him to his patient (ib., s. 33).
Evidence.—The registrar of the council, under the direction of the council, is required to publish a correct register of the names and residences with the medical titles, diplomas, and qualifications conferred by any college or body, of all persons appearing on the register at the date of publication. Said register is called “The British Columbia Medical Register.” A copy of such register for the time being, purporting to be so printed and published, shall be prima facie evidence that the persons[240] therein specified are registered according to the provisions of this act; and, subject to sub. sec. 2 of this section, the absence of the name of any person from such copy shall be prima facie evidence that such person is not registered according to this act (ib., s. 34).
In the case of a person whose name does not appear in such copy, a certified copy under the hand of the registrar of the entry of the name of such person on the register shall be evidence that such person is registered under this act (ib., s. 34, sub. s. 2).
Homœopathic Physicians.—Any homœopathic physician holding a diploma of qualification from any authorized school or college requiring a three-years’ course of study may be registered, and shall not be bound to pass the examination required by sec. 29, but in lieu thereof, shall pass before the council, or such of them as may be appointed for that purpose, a satisfactory examination in anatomy, physiology, pathology, chemistry, obstetrics, and surgery (ib., s. 35, as amended, Act 1890, c. 30, s. 2).
Neglect to Register.—Those entitled to register and neglecting to do so are not entitled to any of the rights and privileges conferred by registration and are liable to all penalties against unqualified or unregistered practitioners (ib., s. 37).
Fraudulent Registration.—If a person procures or causes to be procured his registration by means of any false or fraudulent representation or declaration, the registrar may, on receipt of sufficient evidence to that effect, report the matter to the council and, on the written order of the president, attested by the seal of the council, erase the name of such person from the register and make known the fact and the cause thereof in the British Columbia Gazette, and after such notice has appeared such person shall cease to be a registered practitioner, and to enjoy any of the privileges conferred by registration, without the express sanction of the council (ib., s. 39).
To wilfully procure or attempt to procure registration by false representations or declarations is punishable by a penalty not exceeding $100. To knowingly aid or assist therein is punishable with a penalty of from $20 to $50 for each offence (ib., s. 40).
Unlawful Practices.—It is not lawful for any person not registered to practise medicine or surgery for hire, gain,[241] or hope of reward. To so practise or profess to practise, or advertise to give advice in medicine or surgery, is punishable with a penalty of from $25 to $100 (ib., s. 41).
For a person to wilfully or falsely pretend to be a physician, doctor, or medical, surgical, or general practitioner, or assume any title, address, or description other than he actually possesses and is legally entitled to, is punishable by a penalty of from $10 to $50 (ib., s. 42).
A person not registered who takes or uses any name, title, addition, or description implying or calculated to lead people to infer that he is registered or recognized by law as a physician, surgeon, or licentiate in medicine or surgery is punishable with a penalty of from $25 to $100 (ib., s. 43).
Costs may be awarded in addition to the penalty against an offender, and on default of payment he may be committed to the common jail for one month unless the costs are sooner paid (ib., s. 47).
Unregistered Persons.—No one but a person registered under this act is entitled to receive any charge for any medical or surgical advice or attendance or the performance of any operation or for any medicine that he may have prescribed (ib., s. 44).
Appointments as medical officers, physicians, or surgeons in any branch of the public service, or in a hospital or a charitable institution not supported wholly by voluntary contribution, are conferred on registered persons only (ib., s. 45).
No certificate required from any physician or surgeon or medical practitioner is valid unless the signer is registered (ib., s. 46).
Evidence.—In a prosecution, the burden of proving registration is upon the person charged (ib., s. 48).
Registration may be proved by the production of a printed or other copy of the register certified under the hand of the registrar of the council for the time being, and any certificate on such copy purporting to be signed by any person as registrar is prima facie evidence that he is registrar without further proof (ib., s. 49).
Limitations.—Prosecutions under the act must be commenced within six months from the date of the offence (ib., s. 50).
Stay.—The council may stay proceedings in prosecutions (ib., s. 51).
Prosecutor.—Any person may be prosecutor or complainant under the act (ib., s. 52).
Fees.—To the registrar, for registration under this act, such sum as may from time to time be fixed by the council by resolutions or by-law, but not exceeding $100 (ib., s. 36, as amended, Act 1893, c. 27, s. 1).
To the medical council, on or before March 1st, annually, $10, or such other sum as may from time to time be fixed by the council (ib., s. 53, as amended, Act 1890, c. 30, s. 3).
For registration, by persons registered under Act 1893, c. 27, s. 2, a fee fixed by the council not to exceed $100 (Act 1893, c. 27, s. 2).
Manitoba.
College of Physicians and Surgeons.—The medical profession is incorporated as “The College of Physicians and Surgeons of Manitoba” (Rev. Stat. of Man., 1891, c. 98, s. 2).
All persons lawfully registered under previous acts or the present act are members of the said college (ib., s. 3, 4).
Council.—There is constituted by law a council of the said college composed of representatives selected as provided in the act, each of whom must be a practitioner licensed under this act (ib., s. 5 to 8).
No member of the college who is in arrears for his annual fees or any part thereof is entitled to vote at the election for members of the council or be eligible for election as a member thereof (ib., s. 15).
Register.—The council is required to appoint a registrar and to cause a register to be kept in which shall be entered the name of every person registered under this act or under the Consolidated Statutes of Manitoba, chap. 9, and the acts amending the same, and of all persons who comply with this act, and the rules and regulations made by the council respecting the qualifications of practitioners of medicine, surgery, and midwifery. Only those whose names are inscribed in the book are deemed qualified and licensed to practise medicine, surgery, or midwifery (ib., s. 17, 24, 25).
Qualification.—All persons duly registered under existing laws when the revised statutes took effect are deemed registered under the present law (ib., s. 27).
The registrar was required immediately upon his appointment to register the name of every person registered under previous acts (ib., s. 28).
Every person who possesses one or more of the following qualifications shall, upon the payment of the fee, to be fixed for each particular class by by-law of the council, be entitled to be registered on the production to the registrar of the document proving such qualification:
1. Persons entitled to be registered at the time of the coming into force of the revised statutes.
2. Any member of any incorporated college of physicians and surgeons of any province of the Dominion of Canada, or any member of any other incorporated body of medical men in Canada, exercising powers similar to those conferred by this act on the College of Physicians and Surgeons of Manitoba, where, by the laws of the province under which the said incorporated body exists, similar rights to register and to practise medicine are granted to the persons incorporated under this act.
3. Every person mentioned in chap. 48 of Act 49 and 50 Vict. of the Parliament of the United Kingdom.
4. Every graduate in medicine upon examination of the University of Manitoba.
5. Every person who produces to the registrar the certificate under the corporate seal of the University of Manitoba hereinafter provided for (ib., s. 29).
The registrar is required to keep his register correct, and to make from time to time the necessary alterations in the addresses or qualifications of the persons registered (ib., s. 30).
Every person registered who obtains a higher degree or other qualification is entitled to have it inserted in the register in substitution of or in addition to the qualification previously registered, on the payment of such fees as the council may appoint (ib., s. 34).
No qualification is entitled to be entered on the register unless the registrar be satisfied by proper evidence that the person claiming it is entitled thereto. Appeal lies from the registrar’s decision to the council (ib., s. 35).
The registrar, if dissatisfied with the evidence adduced, may, subject to appeal to the council, refuse registration until[244] proper evidence is furnished, duly attested by oath or affirmation before a judge of any county court (ib., s. 36).
Fraudulent Registration.—Any entry proved to the satisfaction of the council to have been fraudulently or incorrectly made may be erased from the register by order in writing of the council (ib., s. 38).
If a person procures or causes to be procured his registration by false or fraudulent representations or declarations, the registrar may, on the receipt of sufficient evidence of the falsity or fraudulent character, represent the matter to the council, and may on the written order of the president, attested by the seal of the college, erase his name from the register, and cause notice of the fact and cause to be published in the Manitoba Gazette, and after such notice has appeared such person shall cease to be a member of the College of Physicians and Surgeons, and to enjoy any privilege enjoyed or conferred by registration at any further time without the express sanction of the council (ib., s. 39).
Forfeiture of Rights.—Any registered medical practitioner convicted of felony or misdemeanor before or after the passage of the act or his registration forfeits his right to registration, and by direction of the council his name shall be erased. If a person known to have been convicted of felony or misdemeanor presents himself for registration, the registrar may refuse registration. If any person registered be judged, after due inquiry by the council, to have been guilty of infamous or unprofessional conduct in any respect, the council may direct the registrar to erase his name (ib., s. 40).
The council may, and upon the application of any three registered medical practitioners shall, cause inquiry to be made into the case of a person liable to have his name erased from the register, and on proof of such conviction or such infamous or unprofessional conduct shall cause his name to be erased; but no erasure shall be made on account of his adopting or refraining from adopting the practice of any particular theory of medicine or surgery, nor on account of conviction for a political offence out of Her Majesty’s dominions, nor on account of the conviction which ought not in the opinion of the council or committee disqualify him from the practice of medicine or surgery (ib., s. 41).
The council may order to be paid, out of funds at their disposal, such costs as to them may seem just, to any person against whom any complaint has been made which, when fully determined, is found to have been frivolous and vexatious (ib., s. 42).
An entry erased by order of the council shall not be again entered except by order of the council or a judge or court of competent jurisdiction (ib., s. 43).
If the council think fit, they may direct the registrar to restore any entry erased, without a fee, or on payment of a fee not exceeding the registration fee, as the council may fix (ib., s. 44).
The council is authorized to ascertain the facts of any case for the exercise of its powers of erasing and restoring by committee (ib., s. 45).
The act provides in detail for proceedings before such committee (ib., s. 46 to 50).
No action shall be brought against the council or committee for anything done bona fide under the act. Appeal from the decision to erase lies to any judge of the court of Queen’s Bench for Manitoba, and such judge may make such order as to restoration or confirmation of erasure or for further inquiry, and as to costs, as to him may seem right (ib., s. 51).
Evidence.—In a trial under this act the burden of proof as to registration is on the person charged (ib., s. 53).
The production of a certificate that the person named is duly registered, certified under the hand of the registrar, is sufficient evidence of registration, and his signature in the capacity of registrar is prima facie evidence that he is registrar without proof of signature or that he is registrar (ib., s. 54).
The registrar is required to print and publish from time to time under the direction of the council a correct register of the names and residences, with medical titles, diplomas, and qualifications conferred by any college or body, with the date thereof, of all persons appearing on the register as existing on the day of publication (ib., s. 55). The register is called “The Manitoba Medical Register;” a copy thereof for the time being purporting to be so printed and published is prima facie evidence that the persons specified are registered (ib., s. 56).
In the case of any person whose name does not appear in such copy, a certified copy under the hand of the registrar of the council of the entry of the name of such person on the register[246] is evidence that such person is registered (ib., s. 57). The absence of the name of any person from such copy is prima facie evidence that he is not registered (ib., s. 58).
Practitioner’s Rights.—Every person registered is entitled according to his qualifications to practise medicine, surgery, or midwifery, or any of them as the case may be, and to demand and recover full costs of suit, reasonable charges for professional aid, advice, and visits, and the cost of any medicine or other medical appliances rendered or supplied by him to his patient (ib., s. 59).
Neglect to Register.—A person neglecting to register is not entitled to the rights and privileges conferred, and is liable to all penalties against unqualified or unregistered practitioners (ib., s. 60).
Unregistered Persons.—It is not lawful for any person not registered to practise medicine, surgery, or midwifery for hire, gain, or hope of reward (ib., s. 61).
No person is entitled to receive any charge for medical or surgical advice or attendance, or the performance of any operation, or for any medicine which he may have prescribed or supplied, unless he be registered, but this provision does not extend to the sale of any drug or medicine by a licensed chemist or druggist (ib., s. 62).
No person can be appointed as a medical officer, physician, or surgeon in the public service, or in any hospital or other charitable institution not supported wholly by voluntary contribution, unless he be registered (ib., s. 63).
No certificate required from any physician or surgeon or medical practitioner is valid unless the signer be registered (ib., s. 64).
Definition.—The expression “legally qualified medical practitioner,” or any other words importing legal recognition as a medical practitioner or member of the medical profession, in any law, is construed to mean a person registered under this act (ib., s. 65).
Immunities.—A person registered under this act is exempt from jury and inquest duty if he desire it (ib., s. 66).
Limitations.—No duly registered member of the College of Physicians and Surgeons is liable in an action for negligence or malpractice by reason of professional services requested or[247] rendered, unless it be commenced within one year from the termination of such service (ib., s. 67).
Examinations.—The University of Manitoba is the sole examining body in medicine, and the council of the university may grant to any person a certificate under the seal of the university that the council of the university have been satisfied that the person mentioned in the certificate is, by way of medical education and otherwise, a proper person to be registered under this act; but such certificate shall not be granted until the person making such application shall have given evidence of qualification by undergoing an examination or otherwise, as the statutes of the university require, and the applicant shall in all other respects first comply with the rules and regulations of the university in that behalf (ib., s. 68).
Homœopathists.—Until a homœopathic medical college for teaching purposes is established in Manitoba, in the case of candidates wishing to be registered as homœopathists, the full time of attendance upon lectures and hospitals required by the university statutes may be spent in such homœopathic medical colleges in the United States or Europe as may be recognized by the University of Manitoba (ib., s. 69).
Every candidate who at the time of his examination signifies his wish to be registered as a homœopathic practitioner shall not be required to pass an examination in materia medica or therapeutics, or theory or practice of physic, or in surgery or midwifery, except the operative practical parts thereof, before any examiners other than those homœopathic examiners who shall be appointed by the University of Manitoba (ib., s. 70).
Unlawful Practices.—To wilfully procure or attempt to procure registration by false or fraudulent representation or declaration, is punishable by a penalty not exceeding $100. To knowingly aid or assist therein, is punishable by a penalty of from $20 to $50 for each offence (ib., s. 73).
Persons not registered, for hire, gain, or the hope of reward, practising or professing to practise medicine, surgery, or midwifery, or advertising to give advice in medicine, surgery, or midwifery, are liable to a penalty of from $25 to $100 (ib., s. 74).
A person wilfully or falsely pretending to be a physician, doctor of medicine, surgeon, or general practitioner, or assuming a title, addition, or description other than he actually possesses[248] and is legally entitled to, is liable to a penalty of from $10 to $50 (ib., s. 75).
For a person to assume a title calculated to lead people to infer that he is registered, or is recognized by law as a physician, surgeon, or accoucheur or a licentiate in medicine, surgery, or midwifery, is punishable with a penalty of from $25 to $100 (ib., s. 76).
On prosecution, costs may be awarded in addition to the penalty, and the offender may be committed to the common jail for one month, unless the penalty and costs are sooner paid (ib., s. 78).
Prosecutor.—Any person may be prosecutor or complainant under the act (ib., s. 80).
Limitations.—Prosecutions are limited to commence within six months after the date of the offence (ib., s. 81).
Appeal.—A person convicted under this act, giving notice of appeal, must before being released give satisfactory security for the penalty and costs of conviction and appeal (ib., s. 82).
Stay.—The council may stay proceedings in prosecutions (ib., s. 84).
Fees.—The council is authorized to determine by by-law an annual fee, which is required to be paid by each member of the college—the fee can be not less than $2, nor more than $5, is payable on January 1st, and may be recovered as a debt by the college (ib., s. 32).
The fee for registration is subject to regulation by the council (ib., s. 33).
New Brunswick.
Medical Society.—All persons registered under the act constitute the New Brunswick Medical Society (Act 1881, c. 19, s. 2).
Council.—There is a medical council called the Council of Physicians and Surgeons of New Brunswick, of nine legally qualified medical practitioners, of not less than seven years’ standing; four are nominated and appointed by the governor in council, and five by the New Brunswick Medical Society (ib., s. 3, 5).
The secretary of the council is the registrar (ib., s. 7).
Register, Evidence.—The registrar is required before May 1st annually to print and publish in the Royal Gazette of the province, and such other manner as the council shall appoint,[249] a correct register of the names and residences and medical titles, diplomas, and qualifications conferred by any college or body, with the dates thereof, of all persons appearing on the register on the 1st of January. The register is called the Medical Register; a copy for the time being purporting to be so printed and published, or a certificate signed by the president of the council, and attested by the registrar with the corporate seal of the council, is prima facie evidence that the persons therein specified are registered and qualified; the absence of a name from such copy or the want of such certificate is prima facie evidence that such person is not registered. If a name does not appear on the copy, a certified copy, under the hand of the registrar of the council, of the entry of a name on the register is evidence of registration (ib., s. 8).
Entrance upon Study.—A person beginning or entering on the study of physic, surgery, or midwifery, for the purpose of qualifying to practise in the province, must have obtained from the council a certificate that he has satisfactorily passed a matriculation or preliminary examination in the subjects enumerated in the act, unless he has passed a matriculation examination for the medical course in arts and science at some college in Great Britain, Ireland, Canada, the United States of America, or the Continent of Europe (ib., s. 10).
The act prescribes formalities for admission to such preliminary examination (ib., s. 10).
Qualification.—Subject to the exceptions hereinafter, no person can lawfully practise physic, surgery, or midwifery unless he be registered, or unless he shall have received from the council a license to practise (ib., s. 11).
No person is entitled to registration or license unless he shall satisfy the council that he has passed a matriculation or preliminary examination; that after passing such examination he has followed his studies for not less than four years, one of which may be under the direction of one or more general practitioners duly licensed; that during such four years he has attended at some university, college, or incorporated school of medicine in good standing, courses of lectures amounting together to not less than twelve months on general anatomy, on practical anatomy, on surgery, on practice of medicine, on midwifery, on chemistry, on materia medica and pharmacy, and on the institutes[250] of medicine or physic, and one three-months’ course of medical jurisprudence; that he has attended the general practice of an hospital in which are not less than fifty beds under the charge of not less than two physicians or surgeons, for not less than one year or two periods of not less than six months each; that he has also attended two three-months’ courses or one six-months’ course of clinical medicine, the same of clinical surgery; that he has, after an examination in the subjects of the course, obtained a degree or diploma from such university, college, or incorporated medical school if such institution require a four-years’ course for its diploma, or for the want of such degree or diploma that he has satisfactorily passed an examination in the various branches hereinbefore specified before the examiners appointed by the council; that he is not less than twenty-one years of age; that he has paid to the registrar of the council a fee of ten dollars. The council has power, subject to the approval of the governor in council, to make alterations as may be required in the foregoing curriculum. If any person apply for registration as a practitioner of any system of medicine, the registered practitioners of that system have the right to appoint an examiner or examiners on the subjects peculiar to that system, viz., materia medica, pharmacy, and therapeutics, and if they neglect so to do the council has the power to appoint such examiner or examiners (ib., s. 12).
The last preceding section does not apply to persons in actual practice entitled to register under sec. 38. Any person producing to the council conclusive evidence that he has passed a matriculation or a preliminary examination, as required by this act for persons beginning medical studies in New Brunswick, that he has before graduating or taking a diploma studied at least four years as provided in sec. 12, or pursued what the council deem an equivalent course of study and has passed a final examination in the subjects of such course, or, for the want of such requirement, shall have fulfilled such conditions as the council may determine, and shall pay a fee of ten dollars, shall be entitled to registration and to receive a license to practise (ib., s. 13).
The act makes special provision for residents of the province who began study before January 1st, 1881 (ib., s. 14, as amended 1882, c. 30, s. 1).
Duties of Council.—The council is empowered and required to regulate the study of medicine, surgery, and midwifery, with regard to preliminary qualifications, course of study, final examination, and the evidence to be produced before the council; to appoint a registration committee; to examine all degrees, diplomas, licenses, and other credentials presented or given in evidence under the act to enable the owner to practise in New Brunswick, and to oblige the owner to attest on oath or affirmation that he is the person whose name is mentioned therein, and that he became possessed thereof properly and honestly; to cause every member of the profession practising in New Brunswick to register his name, age, place of residence, place of nativity, date of license or diploma, and the place where he obtained it; to appoint medical examiners, who may be members of the council, to hold final examinations, who shall be regularly qualified practitioners of not less than five years’ professional standing and three years’ residence in the province (ib., s. 15, as amended 1882, c. 30, s. 2, 3).
Correction of Register.—The registrar is required to erase the names of all registered persons who shall have died, left the province without the intention of returning, or ceased to practise for five years; and from time to time to make the necessary alterations in the addresses or qualifications of registered persons. Any name erased shall be restored by the order of the council on sufficient cause duly shown (ib., s. 18).
Neglect to Register.—Persons entitled to registration, neglecting or omitting to register, are not entitled to any rights or privileges conferred by the act (ib., s. 19).
System of Practice.—No person otherwise qualified shall be refused registration or license on account of the adoption or the refusal to adopt the practice of any particular theory of medicine or surgery. In case of refusal the aggrieved party may appeal to the governor in council, who is required, on due cause shown, to issue an order to the council to register his name and grant him a license to practise, and thereupon the council shall forthwith register his name and grant him a license to practise (ib., s. 20).
Evidence of Qualification, Fraudulent Registration.—No qualification can be entered unless the registrar be satisfied by proper evidence that the person claiming it is entitled[252] to it. An appeal may be made from the registrar’s decision to the council. Any entry proved to the satisfaction of the council to have been fraudulently or incorrectly made may be erased by the order in writing of the council, and the name of such person fraudulently registering, or attempting to register, may, at the discretion of the council, be published in the next issue of the Royal Gazette (ib., s. 21).
Forfeiture of Right.—A registered medical practitioner convicted of felony, or after due inquiry judged by the council to have been guilty of infamous conduct in any professional respect thereby, subject to appeal to the governor in council, forfeits his right to registration, and by the direction of the council his name shall be erased from the register (ib., s. 22).
The time and place of inquiry under the preceding section must be fixed by the council, and at least fourteen days’ notice given to the party against whom inquiry is ordered (Act 1886, c. 82, s. 6).
The Act of 1886, c. 82, regulates the procedure on such inquiry.
Additional Qualifications.—Every person registered who may obtain a higher degree or other qualification is entitled to have it registered in substitution for, or in addition to, the qualifications previously registered, on the payment of such fee as the council may demand (Act 1881, c. 19, s. 23).
Practitioner’s Rights.—Every person registered under the act is entitled according to his qualifications to practise medicine, surgery, midwifery, or dentistry, or either or any of them as the case may be, and to demand and recover reasonable and customary charges for professional aid, advice, and visits, and the cost of any medicine or other medical or surgical appliances rendered or supplied by him to his patients (ib., s. 24).
No person is entitled to recover any such charge unless he shall prove upon the trial that he is registered under this act (ib., s. 25).
Definition.—The words “legally qualified medical practitioner,” or “duly qualified medical practitioner,” or other words implying that a person is recognized by law as a medical practitioner or member of the medical profession, when used in a legislative act or a legal or public document mean a person registered under this act (ib., s. 26).
Unregistered Persons.—No person shall be appointed a medical officer, physician, or surgeon in the public service or in any hospital or other charitable institution unless registered (ib., s. 27).
No certificate required from any physician or surgeon or medical practitioner is valid unless the signer be duly registered (ib., s. 28).
A person not registered or licensed, and not actually employed as a physician or surgeon in Her Majesty’s naval or military service, practising physic, surgery, or midwifery for hire, gain, or hope of reward, forfeits twenty dollars for each day of such practice (ib., s. 29).
The sum forfeited is recoverable with costs. The procedure in reference to all penalties is regulated by Act of 1886, c. 82.
Persons liable as provided in secs. 29 and 30 are not entitled to or subject to the provisions of any act for the relief of debtors (Act 1882, c. 30, s. 4).
On the trial of such cause, the burden of proof as to license or right to practise is upon the defendant (Act 1881, c. 19, s. 31; Act 1886, c. 82, s. 3).
Fraudulent Registration.—Wilfully procuring or attempting to procure registration by making or producing, or causing to be made or produced, a false or fraudulent representation or declaration, or aiding or assisting therein, is punishable with a forfeiture of not less than $100 (Act 1881, c. 19, s. 33).
Wilfully or falsely pretending to be or using any name or description implying registration is punishable with a forfeiture of from $50 to $100 (ib., s. 34).
Limitations.—No prosecution can be commenced under the act after one year from the date of the offence (Act 1886, c. 82, s. 4).
Exceptions.—The act does not prevent persons from giving the necessary medical or surgical aid or attendance to any one in urgent need of it, provided it be without gain, and the giving of it be not made a business or way of gaining a livelihood; nor does it prevent any woman from giving the necessary aid in cases of confinement as heretofore accustomed (Act 1881, c. 19, s. 36).
Examination.—All persons who subsequent to the passage of the act pass the examination prescribed by the council of[254] physicians and surgeons, or presenting approved credentials, certificates, or diplomas equivalent to such examination, are entitled to register and receive a license to practise (ib., s. 38).
Physicians in Army or Navy.—A person while employed in actual service in Her Majesty’s naval or military service as a physician or surgeon, may practise physic, surgery, or midwifery with registry or license (ib., s. 39).
Non-Residents.—Non-resident registered practitioners of medicine residing in the State of Maine or in the Province of Quebec or Nova Scotia near the boundary line of this province whose regular practice extends into any town, parish, or county in New Brunswick may register under the act (ib., s. 44).
No other non-resident practitioner of medicine is entitled to register (Act 1884, c. 17, s. 1).
Exceptions.—The act does not extend to clairvoyant physicians practising at the time of its passage in the province, nor to midwives (Act 1881, c. 19, s. 45).
Students.—The act establishes a uniform standard of matriculation or preliminary examinations (ib., Sched. B).
Oaths.—Any oath or affidavit required by the medical act may be taken before any justice of the peace or person by law authorized to take any oath or affidavit (Act 1882, c. 30, s. 6).
Fees.—To the registrar, for registration under secs. 12 and 13, $10 (Act 1881, c. 19, s. 12 and 13).
To the registrar, for the registration of an additional qualification, such fee as the council may demand (Act 1881, c. 19, s. 23).
To the registrar, or his deputy, annual fee from each practitioner, to be fixed by the council, not more than $2 nor less than $1 (Act 1882, c. 30, s. 5).
Each registered medical practitioner must, if required by the council, pay to the registrar, or a person deputed by him, an annual fee determined by the council, not less than $1 nor more than $2, payable January 1st each year, and recoverable as a debt with costs in the name of the council (Act 1882, c. 30, s. 5).
If any practitioner omit to pay the registration fee before the registrar causes the register to be printed in the Royal Gazette, the registrar shall not cause the name of such practitioner to be printed, and he shall thereupon cease to be deemed[255] a registered practitioner; but afterward, on paying such fee, he shall be entitled to all his rights and privileges as a registered practitioner from the time of payment (Act 1884, c. 17, s. 2).
Newfoundland.
Medical Board.—There is a board composed of seven regularly qualified medical practitioners of not less than five years’ standing, appointed as provided in the act, and known as the “Newfoundland Medical Board,” whose duties relate, among other things, to the making and enforcing of measures necessary for the regulation and the practice of medicine (Act 1893, c. 12, s. 2, 3, 19).
The board is authorized to appoint examiners and fix times of examinations (ib., s. 5).
The secretary of the board is the registrar (ib., s. 7).
Register, Evidence.—It is the duty of the registrar on or before January 1st in each year to cause to be published in the Royal Gazette of Newfoundland a list of the names of all persons appearing on the register at that date, with their places of residence, titles, diplomas, and qualifications as conferred by any college or body, with the date (ib., s. 8).
Such register is called the Medical Register, and a copy thereof is prima facie evidence that the persons therein specified are registered according to the act; and the absence of a name therefrom is prima facie evidence that such person is not so registered (ib., s. 9).
Qualification.—The members of the board form a body of medical examiners of diplomas and degrees, whose certificate shall be the only license permitting the practice of medicine, surgery, or midwifery, except as hereinafter provided, provided the applicant for such license shall previously have obtained a medical diploma from a recognized college or university, or as hereinafter provided (ib., s. 10.)
Every person is entitled to have his name entered on the register on satisfying the board that he holds a degree or diploma from some regular university or school of medicine in good standing, and he shall then receive from the board a license bearing its seal, on the payment to the registrar of $5, and shall have his name entered on the register (ib., s. 11).
No such licensed practitioner shall be entitled to practise in any year without taking out from the board, before the 1st of January in every year, a certificate of practice for which he shall pay $1 (ib., s. 12).
Students.—The act provides the requirements for entering on the study of medicine, surgery, or midwifery in the colony (ib., s. 13, 14, 17).
Duties of Board.—The board is required to examine all degrees and other credentials produced or given in evidence under the act for the purpose of enabling the owners to practise, and, if it be deemed necessary, to oblige the owner to attest on oath or affidavit that he is the person whose name is mentioned therein, and that he has become possessed of the same by lawful means (ib., s. 16).
The board is required to cause every member of the profession practising in Newfoundland to enter his name, age, place of residence, date of license or diploma and where it was obtained, on the register (ib., s. 18).
Neglect to Register.—A person entitled to be registered, who neglects or omits to apply, is not entitled to any of the rights or privileges conferred by the act so long as the neglect or omission continues (ib., s. 25).
Additional Qualification.—A person registered who obtains a higher degree or diploma is entitled to have it inserted in the register in addition to or in substitution for those previously registered (ib., s. 26).
Rights of Registered Persons.—A person properly registered under the act is entitled to practise medicine, surgery, and midwifery in any part of the colony, and to demand and recover reasonable charges for professional aid or advice with the cost of medicine or other medical and surgical appliance supplied by him (ib., s. 27).
Unregistered Persons.—No person whose name is not registered under the act is entitled to recover any fees for any medical or surgical advice, or for any services whatsoever rendered in the capacity of a medical man, nor to recover the payment of charges for any medicine or medical or surgical appliance which may have been both prescribed and supplied by him. This clause is not intended to interfere with the practice of midwifery by competent females as hereinafter provided (ib., s. 28).
Offences and Penalties.—Except as hereinafter provided, if a person not registered or licensed under the act practises medicine, surgery, or midwifery for hire, gain, help [sic] or reward, or wilfully and falsely pretends to be a physician, doctor of medicine, surgeon, or general practitioner, or takes or uses any name, title, addition [or] description, implying or calculating [sic] to deceive or lead the public to infer that he is registered under this act, or who proposes by public advertisement, card, circular, or otherwise, to practise medicine, surgery, or midwifery, or give advice therein, or in anywise lead people to infer that he is qualified to practise medicine, surgery, or midwifery, he shall forfeit $20 for each day that he so practises or leads people to infer that he is a practitioner, or shall suffer imprisonment not exceeding twelve months (ib., s. 29).
Persons violating the above regulations are subject to the penalties of the act, and in all cases the burden of proof as to qualification is upon the defendant or practitioner (ib., s. 30).
Expulsion of Member.—The Newfoundland Medical Board may try and expel any member of the profession for acts of malpractice, misconduct, or immoral habits, provided five-sevenths of the whole number record their signatures to such a measure (ib., s. 32).
Exceptions.—The act does not prevent private persons from giving the necessary medical or surgical aid in times of urgent need, provided such aid or attention is not given for gain or hire, nor the giving of it made a business or a way of gaining a livelihood (ib., s. 34).
Every person residing in the colony and who shall have practised medicine, surgery, and midwifery for five years consecutively in one locality previous to the passage of the act, on the proof of the same, shall have his name registered and receive a license to practise under the act; provided, the board may grant a license to any person who may have practised for a shorter period, on being satisfied by examination, or inquiry, that such person is reasonably competent and fit; and further provided, that the board may, after examination and inquiry, license persons with a reasonable amount of competence to practise in specified localities, in which no qualified practitioners reside (ib., s. 37).
Any person while employed in actual service in any naval[258] or military service as physician or surgeon may practise medicine, surgery, and midwifery after having been registered (ib., s. 38).
Definition.—The words “legally qualified medical practitioner” or “duly qualified medical practitioner,” or any other words importing a person recognized by law as a medical practitioner or a member of the medical profession, when used in any act of the legislature or legal or public document, mean a person registered under this chapter, unless as otherwise provided (ib., s. 39).
Medical Appointments.—No person shall be appointed as a medical officer, physician, or surgeon in any branch of the public service or any hospital or other charitable institution unless he be registered under the provisions of this chapter (ib., s. 40).
Theories of Medicine or Surgery.—No person otherwise fully qualified shall be refused registration, or a license to practise, on account of his adopting or refusing to adopt the practice of any particular theory of medicine or surgery. In case of such refusal by the board, the party aggrieved may appeal to the governor in council, who, on due cause shown, shall issue an order to the board to register the name of such person and grant him a license (ib., s. 41).
Midwives.—The act does not prevent competent females from practising midwifery (ib., s. 42).
Fees.—To the registrar, for license, $5 (ib., s. 11).
To the board, each year, for a certificate of practice, $1 (ib., s. 12).
Northwest Territories.
College of Physicians and Surgeons.—The members of the medical profession are a body corporate under the name of “The College of Physicians and Surgeons of the Northwest Territories” (Ord. 5 of 1888, s. 2).
Every person registered according to Ordinance 11 of 1885 is a member of the said college and shall be held to be registered under this ordinance from the date of its passage (ib., s. 3, as amended Ord. 9 of 1891-92).
Every person registered under this law is a member of the college (ib., s. 4).
Council.—There is a council of said college elected by the members from the members registered in pursuance of this ordinance (ib., s. 5, 6, 7).
The council appoints among other officers a registrar (ib., s. 26).
Register, Qualification.—Persons registered under Ordinance 11 of 1885 are entitled to register under this ordinance (ib., s. 31).
The council is required to cause the registrar to keep a register of the names of all persons who have complied with this ordinance, and the rules and regulations of the council respecting the qualifications required from practitioners of medicine or surgery. Only those persons whose names are inscribed in the register are deemed qualified and licensed to practise medicine or surgery, except as hereinafter provided (ib., s. 32).
The registrar is required to keep his register correct and to make the necessary alterations in the addresses or qualifications of persons registered (ib., s. 33).
The council is required to admit on the register:
(a) Any person possessing a diploma from any college in Great Britain and Ireland (having power to grant such diploma) entitling him to practise medicine and surgery, and who shall produce such diploma and furnish satisfactory evidence of identification;
(b) any member of the College of Physicians and Surgeons of the Provinces of Manitoba, Ontario and Quebec upon producing satisfactory evidence of the same and of identification;
(c) any person who shall produce from any college or school of medicine and surgery in the Dominion of Canada requiring a four-years’ course of study and (sic) a diploma of qualification; provided he furnish to the council satisfactory evidence of identification, and pass if deemed necessary, before the members thereof, or such examiners as may be appointed for the purpose, a satisfactory examination touching his fitness and capacity to practise as a physician and surgeon, upon payment to the registrar of fifty dollars (ib., s. 34, as substituted by Ord. 14, 1890, amended by Ord. 9, 1891-92).
Powers of Council.—The members of the council are required to make orders, regulations, or by-laws for the regulation of the register and the guidance of examiners, and may[260] prescribe subjects and modes of examination, and may make all regulations in respect of examinations, not contrary to the ordinance, that they may deem expedient and necessary (ib., s. 36).
The council may by by-law delegate to the registrar power to admit to practice and to register any person having the necessary qualifications entitling him to be registered by the council (Ord. 24, 1892, s. 4).
The council may direct the name of any person improperly registered to be erased from the register and such name shall be erased by the registrar (Ord. 24, 1892, s. 5).
Forfeiture of Rights.—If a medical practitioner be convicted of any felony or misdemeanor or after due inquiry be judged by the council to have been guilty of infamous conduct in any professional respect, the council may, if it sees fit, direct the registrar to erase the name of such practitioner from the register, and the name shall be erased (Ord. 5, 1888, s. 37, as substituted by Ord. 24, 1892, s. 1).
Rights of Registered Persons.—Every person registered under the ordinance is entitled to practise medicine and surgery, including midwifery, or any one of them, as the case may be, and to demand and recover with costs his reasonable charges for professional aid, advice, and visits, and the cost of medical or surgical appliances rendered or supplied by him to his patients (ib., s. 38).
Limitation.—A period of one year after the term of professional service is established as a limitation to actions for negligence or malpractice against members of the college (ib., s. 39).
Register, Evidence.—The registrar, under the direction of the council, is required to publish a register of the names and residences and the medical titles, diplomas, and qualifications conferred by any college or body, of all persons appearing on the register on the day of publication. The register is called “Northwest Territories’ Medical Register,” and a copy for the time being, purporting to be so printed and published, is prima facie evidence that the persons therein specified are registered according to the act. The absence of a name from such copy is prima facie evidence that such person is not so registered.
In case a person’s name does not appear on such copy, a certified[261] copy under the hand of the registrar of the entry of the name of such person on the register is evidence that such person is registered (ib., s. 40).
Neglect to Register.—A person neglecting to register is not entitled to the rights or privileges conferred and is liable to all penalties against unqualified or unregistered practitioners (ib., s. 4).
Offences and Penalties.—To practise or profess to practise without registration, for hire or reward, is punishable with a penalty of $100 (ib., s. 42).
To wilfully or falsely pretend to be a physician, doctor of medicine, surgeon, or general practitioner, or assume any title or description not actually possessed and to which the person is not legally entitled under this ordinance, is punishable with a penalty of from $10 to $50 (ib., s. 43, as amended by Ord. 24, 1892, s. 2).
To take or use a name or description implying or calculated to lead people to infer registration or recognition by law as a physician, surgeon, or licentiate in medicine or surgery is punishable with a penalty of from $25 to $100 (ib., s. 44).
Unregistered Persons.—No person is entitled to recover for any medical or surgical advice or attendance or the performance of any operation or medicine which he may have prescribed (ib., s. 45); nor to be appointed as medical officer, physician, or surgeon in any branch of the public service or in any hospital or other charitable institution not supported wholly by voluntary contributions, unless registered (ib., s. 46).
No certificate required from a physician or surgeon or medical practitioner is valid unless the signer is registered (ib., s. 47).
Costs.—In prosecutions, payment of costs may be awarded in addition to the penalty, and in default of payment the offender may be committed to the common jail for not more than one month (ib., s. 48).
Burden of Proof.—In prosecutions, the burden of proof as to registration is upon the person charged (ib., s. 49).
Proof.—The production of a printed or other copy of the register, certified under the hand of the registrar, for the time being is sufficient evidence of all persons [registered]; a certificate on such copy purporting to be signed by any person in the[262] capacity of registrar of the council under this ordinance is prima facie evidence that he is registered without proof of his signature or of his being in fact registrar (ib., s. 50).
Limitation of Prosecutions.—Prosecutions must be commenced within six months from the date of the offence (ib., s. 51).
Stay.—The council may stay proceedings in prosecutions where deemed expedient (ib., s. 52).
Prosecutor.—Any person may be prosecutor or complainant (ib., s. 53).
Definition.—“Legally qualified medical practitioner” or “duly qualified medical practitioner,” or any other words implying legal recognition as a medical practitioner or member of the medical profession, when used in any law or ordinance, mean a person registered under this ordinance (ib., s. 55).
Homœopathists.—Homœopathic physicians may be registered under this ordinance on complying with the terms of sec. 34 (ib., s. 58).
Fees.—To the council from each member annually as the council may determine, not more than $2 and not less than $1 (ib., s. 35).
To the registrar, for registration, $50 (ib., s. 56, as substituted by Ord. 24, 1892, s. 3).
Nova Scotia.
Medical Board.—There is a provincial medical board consisting of thirteen regular qualified medical practitioners of not less than seven years’ standing, seven nominated and appointed by the governor in council, and six by the Nova Scotia Medical Society (R. S., 5th ser., c. 24, s. 1).
The board appoints a secretary who is the registrar of the board (ib., s. 3, 4).
Register, Evidence.—The registrar is required before the 1st of August each year to cause to be printed and published in the Royal Gazette of the province, and in such other manner as the board shall appoint, a correct register of the names and residences and medical titles, diplomas, and qualifications conferred by any college or body, with the dates thereof of all persons appearing on the register as existing on June[263] 30th. Such register is called “The Medical Register,” and a copy thereof for the time being, purporting to be so printed and published, is prima facie evidence that the persons specified are registered according to this chapter. The absence of a name from such copy is prima facie evidence that such person is not so registered. In the case of a person whose name does not appear in such copy, a certified copy, under the hand of the registrar, of the entry of his name on the register is evidence that such person is registered under the provisions of this chapter (ib., s. 5).
Students.—No person can begin or enter on the study of physic, surgery, or midwifery, for the purpose of qualifying himself to practise in the province, unless he shall have obtained from the provincial medical board a certificate that he has satisfactorily passed a matriculation examination in the subjects specified in the chapter (ib., s. 6).
The chapter prescribes the prerequisites to admission to preliminary examinations (ib., s. 7, 12).
Qualification.—Subject to the exceptions hereinafter, no person can lawfully practise physic, surgery, or midwifery unless his name be registered and unless he shall have received from the provincial medical board a license to practise (ib., s. 8).
No person is entitled to be registered or to receive a license to practise unless he satisfy the board that he has passed the matriculation or preliminary examination; that after passing such examination he has followed his studies during a period not less than four years (one of which may be under the direction of one or more general practitioners duly licensed); that during such four years he has attended at some university, college, or incorporated school of medicine in good standing, courses of lectures amounting together to not less than twelve months on general anatomy, on practical anatomy, on surgery, on the practice of medicine, on midwifery, on chemistry, on materia medica and pharmacy, and on the institutes of medicine or physiology, and one three-months’ course of medical jurisprudence; that he has attended the general practice of a hospital in which are not less than fifty beds under the charge of not less than two physicians or surgeons, for a period of not less than one year or two periods of not less than six months each; that he has also attended two three-months’ courses or[264] one six-months’ course of clinical medicine, and the same of clinical surgery; that he has, after an examination in the subjects of the course, obtained a degree or diploma from such university, college, or incorporated medical school, or, for want of such degree or diploma, that he has satisfactorily passed an examination in the various branches hereinbefore specified before examiners to be appointed by the provincial medical board; that he is not less than twenty-one years of age; and that he has paid the registrar twenty dollars.
The provincial medical board has power, subject to the approval of the governor in council, to make such alterations in the foregoing curriculum as may from time to time be required (ib., s. 9).
The last preceding section does not apply to any person in actual practice duly registered under chap. 56 of Revised Statutes, 3d series; such persons are entitled to be registered and receive a license to practise under this chapter without fee. Notwithstanding such section, any person on producing to the said board conclusive evidence that he has passed a matriculation or preliminary examination such as is required for persons beginning their medical studies in Nova Scotia; that he has, before graduating or taking a diploma, studied for at least four years in the manner provided in sec. 9 or pursued what the board deem an equivalent course of study, and has passed a final examination in the subjects of such course; or, for the want of any of such requirements, shall have fulfilled such conditions as the board may determine and shall pay a fee of twenty dollars, shall be entitled to be registered and to receive a license to practise (ib., s. 10).
Powers of Board.—The said board among other powers has the power to examine all degrees, diplomas, licenses, and other credentials presented or given in evidence for the purpose of entitling the owner to practise in Nova Scotia; and to oblige the owner to attest on oath, or by affidavit, that he is the person whose name is mentioned therein, and that he became possessed thereof honestly; to cause every member of the profession practising in Nova Scotia to enregister his name, age, place of residence, place of nativity, date of license or diploma, and the place where he obtained it, in the register of the board; to appoint medical examiners to hold final examinations,[265] such examiners to be regular qualified practitioners of not less than five years’ professional standing, and three years’ residence in the province (ib., s. 12).
Register.—The registrar is required to keep his register correct, and to erase the names of all registered persons who shall have died, left the province without any intention of returning, or ceased to practise for five years, and to make from time to time the necessary alterations in the addresses or qualifications of persons registered. A name erased is required to be restored by the order of the board upon sufficient cause duly shown (ib., s. 15).
Neglect to Register.—Persons entitled to register and neglecting or omitting to register are not entitled to any of the rights or privileges conferred so long as the neglect or omission shall continue (ib., s. 16).
Theories of Medicine or Surgery.—No person shall be refused registration or a license on account of the adoption or the refusal to adopt the practice of any particular theory of medicine or surgery. In case of such refusal the party aggrieved has the right to appeal to the governor in council, who, on due cause shown, is required to issue an order to the board to register the name of such person and to grant him a license (ib., s. 17).
Powers of Registrar.—No qualification is entered unless the registrar is satisfied by proper evidence that the person claiming is entitled to it, and any appeal from the decision of the registrar may be decided by the board, and any entry proving to the satisfaction of the board to have been fraudulently or incorrectly made may be erased from the register by order in writing of the board (ib., s. 18).
Forfeiture of Rights.—A medical practitioner convicted of felony or, after due inquiry, judged by the board to have been guilty of infamous conduct in any professional respect, thereby forfeits his right to registration, and if registered his name shall, by the direction of the board, be erased from the register (ib., s. 19).
Additional Qualifications.—A registered person may have a higher degree or an additional qualification obtained by him, inserted in the register in substitution for or in addition to a qualification previously registered, on the payment of such fee as the board may appoint (ib., s. 20).
Rights of Registered Persons.—Every registered person is entitled according to his qualifications to practise medicine, surgery, or midwifery, or either or any of them as the case may be, and to demand and receive reasonable charges for professional aid, advice, and visits and the cost of any medicine or any medical or surgical appliances rendered or supplied by him to his patients (ib., s. 21).
No person is entitled to recover such charge unless he shall prove on the trial that he is registered under this chapter. This does not interfere with the sale by qualified druggists or chemists of articles properly belonging to their business (ib., s. 22).
Definition.—The words “legally qualified medical practitioner” or “duly qualified medical practitioner,” or any other words importing a person recognized by law as a medical practitioner or a member of the medical profession, when used in any act of the legislature or legal or public document mean a person registered under this chapter (ib., s. 23).
Unregistered Persons.—No person shall be appointed as a medical officer, physician, or surgeon, in any branch of the public service, or in any hospital or other charitable institution, unless he be registered under the provisions of this chapter (ib., s. 24).
No certificate required from any physician or surgeon or medical practitioner is valid unless the signer be registered (ib., s. 25).
Offences and Penalties.—For a person without registration or license to practise physic, surgery, or midwifery for hire, gain, or hope of reward, or wilfully or falsely pretend to be a physician, doctor of medicine, surgeon, or general practitioner, or to take or use any name or description implying or calculated to lead people to infer that he is registered, or to profess by public advertisement, card, circular, sign, or otherwise to practise physic, surgery, or midwifery, or to give advice therein or in anywise to lead people to infer that he is qualified to practise physic, surgery, or midwifery, is punishable with a forfeiture of $20 for each day that he so practises or leads people to infer that he is practising (ib., s. 26).
On trial of such cause the burden of proof as to the license or right of the defendant to practise physic, surgery, or midwifery is on the defendant (ib., s. 28).
If a person wilfully procures or attempts to procure registration by making or producing, or causing to be made or produced, a false or fraudulent representation or declaration, he, and all persons knowingly aiding or assisting therein, are each punishable with a forfeiture of not less than $100 (ib., s. 30).
To wilfully and falsely pretend to be or take or use any name or description implying registration, is punishable with a forfeiture not exceeding $100 (ib., s. 31).
Suits under this chapter are not to be begun after one year from the date of the offence or cause of action (ib., s. 32).
Exceptions.—This chapter does not prevent a competent female from practising midwifery in Nova Scotia, except that she must satisfy the board of her competency, and obtain a certificate from the registrar before she can lawfully practise in the city of Halifax (ib., s. 33).
Nothing in the chapter prevents any person from giving necessary medical or surgical aid or attendance to any one in urgent need of it, provided such aid or attendance is not given for hire or gain, nor the giving of it made a business or way of gaining a livelihood (ib., s. 34).
Every person residing in the province and who shall have practised therein prior to January 1st, 1850, is entitled on proof thereof to have his name registered and receive a license to practise under this chapter (ib., s. 36).
A person while employed in active service in Her Majesty’s naval or military service as a physician or surgeon may practise physic, surgery, or midwifery with (sic) registration or license (ib., s. 37).
Schedule B of the chapter prescribes the subjects for a matriculation or preliminary examination of those commencing the study of medicine.
Fees.—To the registrar, for registration under secs. 9 and 10, $20.
To the registrar, for a preliminary examination under sec. 7, $10.
For registering additional qualifications, such fee as the board may appoint (ib., s. 20).
Ontario.
College of Physicians, etc.—There is a corporation styled “The College of Physicians and Surgeons of Ontario” (Rev, St., 1887, c. 148, s. 2).
All persons registered according to the provincial acts 29 Victoria, c. 34, and 37 Victoria, c. 45, and amendatory acts, are members of said corporation (ib., s. 3); as well as all persons registered under this act (ib., s. 4).
Council.—There is a council of said college composed of representatives chosen from every university, college, or body in the province authorized to grant degrees in medicine and surgery, and which establish and maintain to the satisfaction of the College of Physicians and Surgeons of Ontario a medical faculty in connection therewith, with five members elected by the registered licensed practitioners in homœopathy, and twelve members elected from among and by the other registered members of the profession (ib., s. 6).
No teacher, professor, or lecturer of any such college or body shall hold a seat in said council except as a representative of the college or body to which he belongs (ib., s. 6, subd. 2, as amended Act 1893, c. 27, s. 2).
All members of the council representing the colleges of bodies aforesaid must be practitioners duly registered (ib., s. 6, subd. 3, as amended Act 1893, c. 27, s. 2).
All duly registered practitioners are entitled to vote at any election for members of the council (ib., s. 8).
Any member of the college may have his name transferred from one class of voters to any other on presenting to the registrar a certificate duly signed by the member or members of the board of examiners to examine candidates on subjects specified as peculiar to each school of medicine, testifying that the member so applying has shown a sufficient knowledge of the system of medicine he desires to connect himself with, to entitle him to be admitted to the class he desires, and being so admitted he is entitled to vote in that class only (ib., s. 9 [1]).
No member is entitled to return to the class from which he has been transferred without the sanction of the council (ib., s. 9 [2]).
The council appoints officers including a registrar (ib., s. 13).
The council must appoint an executive committee to take cognizance of and action upon all matters delegated to it by the council or which may require immediate attention or interference between the adjournment of the council and its next meeting, and all such acts shall be valid only till the next ensuing meeting of the council (ib., s. 4).
Division Association.—In each territorial division established by the act there may be established a Division Association, of which every member of the said college residing within the said territorial division shall be a member (ib., s. 15).
Professional Fees.—The division association may submit to the council a tariff of professional fees suitable to their division, and on the said tariff receiving the approval of the council, signed by the seal of the college and the signature of the president, such tariff shall be held to be a scale of reasonable charges for the division or section of a division where the members of the association making it reside (ib., s. 16).
Registration.—In a register kept by the registrar the council is required to cause to be entered the name of every person duly registered and all persons who have complied with the act and the rules and regulations made by the council respecting the qualifications of practitioners of medicine, surgery, and midwifery; and those persons only whose names are inscribed in the register shall be deemed to be qualified and licensed to practise medicine, surgery, or midwifery, except as hereinafter provided (ib., s. 21).
The registrar is required to keep his register correct and to make the necessary alterations in the addresses or qualifications of persons registered. And he may write to any registered person at his address on the register, to inquire whether he has ceased to practise or has changed his residence, and if no answer be returned within six months, may erase the name of such person; the name shall be restored on compliance with the other provisions of the act (ib., s. 22, as amended Act 1891, c. 26, s. 9).
It is optional for the council to admit to registration all such persons as are duly registered in the medical register of Great Britain, or otherwise authorized to practise medicine, surgery,[270] and midwifery in the United Kingdom of Great Britain and Ireland, upon such terms as the council may deem expedient (ib., s. 23 [1]).
Any person actually practising medicine, surgery, or midwifery, or any of them, in Ontario prior to January 1st, 1850, and who has attended one course of lectures at any recognized medical school, on such proof as the council may require, is entitled to register (ib., s. 23 [2]).
Any person actually practising medicine, surgery, or midwifery according to the principles of homœopathy before January 1st, 1850, and for the six years preceding March 24th, 1874, in Ontario, may in the discretion of the representatives of the homœopathic system of medicine be registered (ib., s. 23 [3]).
Any person who possesses any of the qualifications described in Schedule B, dated prior to July 23d, 1870, on the payment of the fee, is entitled to register on producing to the registrar the document conferring or evidencing his qualification or qualifications, or on transmitting by post to the registrar information of his name and address and evidence of the qualification or qualifications in respect whereof he wishes to be registered and of the time or times at which the same was or were attained. No one registered under the acts mentioned in sec. 3 is liable to pay for registration (ib., s. 24).
Every person wishing to be registered, and not possessed before July 23d, 1870, of one of the qualifications in Schedule B, must present himself for examination as to his knowledge and skill for the efficient practice of his profession before the board of examiners mentioned in sec. 28, and upon passing the examination required and proving to the satisfaction of the board of examiners that he has complied with the rules and regulations of the council, and on payment of such fees as the council may establish, he shall be entitled to register and in virtue of his registration to practise medicine, surgery, and midwifery (ib., s. 25).
When it appears that there has been established a central examining board similar to that constituted by this act, or an institution duly recognized by the legislature of any of the provinces of the Dominion of Canada as the sole examining body for the purpose of granting certificates of qualification,[271] and wherein the curriculum is equal to that established in Ontario, the holder of such certificate shall, upon due proof, be entitled to registration by the council of Ontario if the same privilege is accorded by such examining board or institution to those holding certificates of Ontario (ib., s. 26).
Board of Examiners.—The council is required at its annual meeting to elect a board of examiners whose duty it is to examine at least once in each year all candidates for registration in accordance with the by-laws, rules, and regulations of the council; such examinations are to be held at Toronto or Kingston at such times and in such manner as the council may by by-laws direct (ib., s. 28).
The board of examiners is composed of one member from each existing teaching body enumerated in sec. 6 and one from every other school of medicine organized in connection with any university or college empowered by law to grant medical or surgical diplomas and not less than six members chosen from the members of the College of Physicians and Surgeons of Ontario unconnected with any such teaching body (ib., s. 29, as amended Act 1893, c. 27, s. 5).
Homœpathists.—Every candidate who, at the time of the examination, signifies his wish to be registered as a homœopathic practitioner shall not be required to pass an examination in materia medica or therapeutics, or the theory or practice of physic or surgery or midwifery except the operative parts thereof, before any examiners other than those approved of by the representatives in the council of the homœopathic system (ib., s. 30).
Duties of Council.—The council is required to make orders, regulations, or by-laws for regulating the register and fees for registration and for the guidance of the board of examiners, and may prescribe the subjects and modes of examination and the time and place of holding the same, and may make all such rules and regulations for examination not contrary to the act as they deem expedient and necessary (ib., s. 31).
Additional Qualification.—Every person registered who obtains a higher degree or other qualification is, on the payment of the fee, entitled to have it inscribed in the register in substitution for or in addition to the qualifications previously registered (ib., s. 32).
Powers of Registrar.—No qualification is to be entered on the register unless the registrar be satisfied by proper evidence that the person claiming it is entitled to it. Appeal from the decision of the registrar may be decided by the council; any entry proved to the satisfaction of the council to have been fraudulently or incorrectly made may be erased from the register by order of the council in writing (ib., s. 33 [1]).
If the registrar be dissatisfied with the evidence adduced by a person claiming to be registered, he has power, subject to appeal to the council, to refuse registration until such evidence is furnished, duly attested by oath or affidavit before a judge of the county court of any county (ib., s. 33 [2]).
Erasure and Restoration of Name.—A practitioner is liable to have his name erased from the register where he has been convicted before or after registration of an offence which, if committed in Canada, would be a felony or misdemeanor, or where he has been guilty of any infamous or disgraceful conduct in a professional respect (ib., s. 34 [1]).
The council may, and on the application of any four registered medical practitioners must, cause inquiry to be made into the case of a person alleged to be liable to have his name erased under this section, and on proof of such conviction or conduct shall cause his name to be erased from the register. The name of a person shall not be erased on account of his adopting or refraining from the practice of any particular theory of medicine or surgery; nor on account of a conviction for a political offence out of Her Majesty’s dominions, nor of conviction for an offence which ought not either from its trivial nature or its circumstances to disqualify a person from practising medicine or surgery (ib., s. 34 [2]).
The council may order to be paid out of any funds at their disposal such costs as they may deem just to any person against whom any complaint has been made, which, when finally determined, is found to have been frivolous and vexatious (ib., s. 34 [3]).
When the council direct the erasure of any name or entry, it shall not be again entered except by direction of the council or any of the divisions of the high court of justice (ib., s. 35 [1], as amended Act 1891, c. 26, s. 3).
If the council think fit, they may direct the registrar to[273] restore any name or entry erased, without fee, or on payment of such fee not exceeding the regular fee as the council may fix (ib., s. 35 [2]).
The council is required to ascertain facts, in the exercise of its powers of erasing and restoring, by a committee of their own body of not more than five, and a written report of the committee may be acted on by the council (ib., s. 36 [1], as amended Act 1891, c. 26, s. 4).
At least two weeks’ notice of the first meeting of the committee for ascertaining the facts of any case must be served on a person whose conduct is subject to inquiry, and such notice must embody a copy of the charges or a statement of the subject-matter of the inquiry, and specify the time and place of meeting. The testimony is under oath, and subject to cross-examination and the full right to call evidence in defence and reply. In the event of the non-attendance of such person the committee, on the proof of personal service of the notice, may proceed with the inquiry in his absence and without further notice (ib., s. 36 [5]).
No action can be brought against the council or committee for anything done bona fide under this act notwithstanding want of form in the proceedings. Any person whose name has been ordered erased may appeal from the decision of the council to any division of the high court at any time within six months from the date of the order of erasure, and the judge may make such order as to restoration, confirmation, or further inquiries by the committee or council and as to costs, as to him shall seem right (ib., s. 37, as amended Act 1891, c. 26, s. 5).
The appeal may be by a summons served on the registrar to show cause, and is founded upon a copy of the proceedings before the committee, the evidence taken, the committee’s report, and the order of the council certified by the registrar. The registrar is required to furnish to any person desiring to appeal a certified copy of all proceedings, reports, orders, and papers on which the committee acted, on payment of five cents a folio (ib., s. 38, as amended Act 1891, c. 26, s. 6).
The Act of 1891, c. 26, s. 7, provides for procuring the attendance of witnesses before the committee, and for payment of costs by the person whose name has been directed to be erased.
Rights of Registered Persons.—Every person registered is entitled according to his qualifications to practise medicine, surgery, or midwifery, or any of them, as the case may be, and to demand and recover with full costs reasonable charges for professional aid, advice, and visits and the cost of any medicine or other medical or surgical appliances rendered or supplied by him to his patient (ib., s. 39).
Limitations.—One year after the termination of professional services is established as a period of limitations to an action for negligence or malpractice by reason thereof against duly registered members of said college (ib., s. 40).
Evidence.—The register is required to be printed and published, and a copy thereof purporting to be so printed and published is prima facie evidence that the persons specified are registered; and, subject to the provisions of subsection 2 of this section, the absence of the name of any person from such copy shall be prima facie evidence that such person is not registered (ib., s. 41 [1]).
In case of the name of a person not appearing in such copy, a certified copy, under the hand of the registrar, of the entry of the name on the register is evidence that such person is registered (ib., s. 41 [2]).
Annual Certificate of Registration.—Every registered medical practitioner is required to obtain from the registrar annually, before December 31st, a certificate under seal of the college that he is a duly registered medical practitioner (Act 1891, c. 26, s. 8).
On payment of all fees and dues payable by such practitioner to the college, the registrar is required to write his name and the date on the margin of the certificate, and the certificate is deemed to be issued only from such date; any fees properly charged during the time in which a name was erased from the register are legally recoverable on production of the certificate of registration at time of suit (ib.).
No certificate is issued to any practitioner indebted to the college, nor until the annual fee for the certificate prescribed by the statute and the by-laws of the college is paid (ib.).
If a practitioner omits to take out such certificate, he shall not be entitled thereto until he pays the certificate fee, and any other fees or dues which he owes the college (ib.).
After twelve months’ default in taking out such certificate, and two months’ notice of default by registered letter to the registered address of the defaulter, if payment is not made, the registrar is required to erase his name and the provisions as to unregistered practitioners forthwith apply (ib.).
Such practitioner may, unless otherwise disqualified, obtain re-registration and re-instatement to full privileges by applying to the registrar and paying up the fees and dues and taking out his certificate (ib.).
Neglect to Register.—Those entitled to register and neglecting so to do are not entitled to any rights or privileges conferred by registration, and are liable to all the penalties against unqualified or unregistered practitioners (Rev. St., 1887, c. 148, s. 42).
Fraudulent Registration.—If a person procures registration by means of false or fraudulent representations it is lawful for the registrar, on a receipt of sufficient evidence of such falsity or fraud, to represent the matter to the council, and on the written order of the president, attested by the seal of the college, to erase his name from the register and publish the fact and cause of erasure in the Ontario Gazette; and after such notice such person ceases to be a member of said college and to enjoy the privileges conferred by registration without the express sanction of the council (ib., s. 44 [1]).
Offences and Penalties.—Wilfully procuring or attempting to procure registration by false or fraudulent representations is punishable with a penalty not exceeding $100. Knowingly aiding and assisting therein is punishable with a penalty of from $20 to $50 for each offence (ib., s. 44 [2]).
Practising without registration for hire, gain, or hope of reward is punishable with a penalty of from $25 to $100 (ib., s. 45).
A person wilfully or falsely pretending to be a physician, doctor of medicine, surgeon or general practitioner, or assuming any title, addition, or description other than that he actually possesses and is legally entitled to, is punishable with a penalty of from $10 to $50 (ib., s. 46).
A person taking or using a name, title, addition, or description implying or calculated to lead people to infer that he is recognized by law as a physician, surgeon, accoucheur, or licentiate[276] in medicine, surgery, or midwifery is punishable by a penalty of from $25 to $100 (ib., s. 47).
Unregistered Persons.—No person is entitled to recover a charge for medical or surgical advice or attendance or the performance of any operation or any medicine prescribed or supplied unless he produces to the court a certificate that he is registered; but this section does not extend to the sale of drugs or medicines by a licensed chemist or druggist (ib., s. 48, as amended Act 1891, c. 26, s. 2).
No person shall be appointed as a medical officer, physician, or surgeon in any branch of the public service, or in any hospital or other charitable institution not supported wholly by voluntary contribution, unless he be registered (ib., s. 49).
No certificate required from any physician, surgeon, or medical practitioner is valid unless the signer be registered (ib., s. 50).
Costs.—The justice of the peace having jurisdiction of a prosecution may award payment of costs in addition to the penalty, and in default of payment may commit to the common jail for a period not exceeding one month unless the penalty and costs are sooner paid (ib., s. 51).
Appeal.—Any person convicted who gives notice of appeal must give satisfactory security for the amount of the penalty and the costs of conviction and appeal (ib., s. 52).
Proof.—In any trial under the act, the burden of proof as to registration is on the person charged (ib., s. 53).
Where proof of registration is required, the production of a printed or other copy of the register certified under the hand of the registrar for the time being is sufficient evidence of all persons who are registered practitioners, and any certificate upon such copy purporting to be signed by any person in his capacity of registrar is prima facie evidence that such person is registrar without proof of his signature or of his being registrar (ib., s. 54).
Limitations of Prosecutions.—Prosecutions are limited to commence within one year from the date of the offence (ib., s. 55)
Stay.—The council may, by order signed by its president having the seal of the college appended, stay proceedings in any prosecution when deemed expedient (ib., s. 56).
Prosecutor.—Any person may be prosecutor or complainant (ib., s. 57 [2]).
Qualification.—Schedule B referred to in the act is as follows:
1. A license to practise physic, surgery, and midwifery, or either, within Upper Canada under the acts of Upper Canada, 59 G., III., c. 13, and 8 G., IV., c. 3, respectively.
2. A license or diploma granted under 2 Vict., c. 38, or under the Consolidated Statutes for Upper Canada, c. 40, or any act amending the same.
3. A license or authorization to practise physic, surgery, and midwifery, or either, within Lower Canada, whether granted under ordinance 28 G., III., c. 8, or act 10 and 11 Vict., c. 26, and acts amending the same, or under c. 71 of the Consolidated Statutes for Upper Canada, or any act amending the same.
4. A certificate of qualification to practise medicine, surgery, and midwifery, or either, hereafter granted by any colleges or bodies named or referred to in sec. 6.
5. A medical or surgical degree or diploma of any university or college in Her Majesty’s dominions or of such other universities or colleges as the council may determine.
6. A certificate of registration under the Imperial Act 21 and 22 Vict., c. 90, known as “The Medical Act,” or any act amending the same.
7. A commission or warrant as physician or surgeon in Her Majesty’s military service.
8. Certificates of qualification to practise medicine under any of the acts relating to homœopathy or the eclectic system of medicine.
Fees.—To registrar, for transfer under sec. 9 (2), $2.
To registrar, for registration under sec. 24, not more than $10, to be fixed by the by-laws of council.
To registrar, for registration under sec. 25, such fees as the council may by general by-law establish.
To registrar, for copies under sec. 38, 5 cents a folio.
Members are required to pay an annual fee to the college; the amount and means of enforcing which are in the discretion of the elected members of the council (Act 1893, c. 27, s. 6).
Prince Edward Island.
Medical Society.—The members of the medical profession constitute a body corporate under the name of the “Medical Society of Prince Edward Island” (Act 1892, c. 42, s. 1).
Persons registered under the act 34 Vict., c. 25, or 37 Vict., or the Prince Edward Island Medical Act of 1890, are members of the society and entitled to register under this act without a fee (ib., s. 2).
All persons registered under this act are members of the said society (ib., s. 3).
Registration.—There is a council of said society, composed of seven members of the society elected by the society (ib., s. 4), which is required to appoint a registrar among other officers (ib., s. 6); and to cause him to keep a register of the name of every person registered under this act, or the acts mentioned in sec. 2, and from time to time of the names of all persons who have complied with this act and the rules and regulations made by the council respecting the qualifications of practitioners of medicine, surgery, or midwifery, which is called the Prince Edward Island Medical Register; and only those persons whose names are inscribed therein are qualified and licensed to practise medicine, surgery, or midwifery, except as hereinafter provided (ib., s. 8).
The registrar is required to keep his register correct, and to make the necessary alterations in the addresses and qualifications of persons registered (ib., s. 9).
The council is required to admit to registration, on the payment of the registration fee, all persons duly registered by the medical council of Great Britain or otherwise authorized to practise medicine, surgery, or midwifery in the United Kingdom of Great Britain and Ireland (ib., s. 10).
Every person who holds a medical or surgical degree or diploma dated prior to January 1st, 1880, from any university, college, or school of medicine in Great Britain, Ireland, or Canada, or any of the universities or colleges in the United States mentioned in Schedule A, is entitled to register on producing to the registrar such diploma or satisfactory evidence of the qualification in respect whereof he seeks to be registered (ib., s. 11).
Every person desirous of being registered, not registered under the acts mentioned in sec. 2, and who had not become possessed of a diploma as provided in sec. 11, must, before being entitled to register, be examined as to his knowledge and skill for the efficient practice of his profession before the medical council, and on passing the examination required and producing proof of study in medicine, surgery, and midwifery four years, one of which may be with a registered medical practitioner, shall, subject to the next section, be entitled to register and by virtue of such registration to practise medicine, surgery, and midwifery; provided, the council may, if it see fit, dispense with the examination in any case (ib., s. 12).
No person commencing the study of medicine on or after September 1st, 1892, shall be entitled to register unless he has passed a matriculation examination equivalent to that of the College of Surgeons of London, or shall hold a license as a first-class teacher in this province, or shall have obtained from the council a certificate that he has satisfactorily passed a matriculation examination in the subjects specified in Schedule B.
Any graduate or student matriculated in the arts in any university in Her Majesty’s dominions shall not be required to pass the matriculation examination (ib., s. 13).
The council may grant a license to practise medicine, surgery, or midwifery to an applicant at the time of the passage of this act practising medicine, surgery, or midwifery, or any of them, in Prince Edward Island, on a preliminary examination as the council may think necessary for the public safety, provided such person shall have practised five years in the province, but such person is not thereby entitled to registration (ib., s. 15).
When there has been established an authorized examining body or an institution recognized by the legislature of any other province of the Dominion of Canada as the sole examining body for granting certificates of qualification, and where the curriculum is equal to that appointed by the medical council of Prince Edward Island, the holder of such certificate shall, upon due proof, be entitled to registration by the council of Prince Edward Island, if the same privilege is accorded in such other province to those registered in Prince Edward Island (ib., s. 16).
The council is required to hold examinations at least every three months, if required, for candidates for registration, at such places and times and in the same manner as the council may direct (ib., s. 18).
Every person registered who obtains a higher degree or other qualification shall, on the payment of such fees as the council shall appoint, be entitled to have it registered in substitution for or in addition to the qualification previously registered (ib., s. 19).
No qualification is entered unless the registrar be satisfied, by proper evidence, that the person claiming is entitled to register it. There is an appeal to the council; any name proved to the council to have been fraudulently or incorrectly entered may be erased by an order in writing of the council (ib., s. 20).
If the registrar is dissatisfied with the evidence he may, subject to appeal to the council, refuse registration until the person claiming it has furnished evidence to the satisfaction of the registrar, duly attested by oath or affidavit before a notary public or justice of the peace (ib., s. 21).
A medical practitioner guilty of infamous or disgraceful conduct in a professional respect is liable to have his name erased, and if he apply for registration the council may refuse it (ib., s. 22).
The registrar may publish in a newspaper or newspapers of Prince Edward Island the fact that the name of such person has been erased, and the cause of the erasure, but not until the appeal, if any has been taken within the time allowed, has been disposed of (ib., s. 23).
Where the council refuse to register, or direct an erasure, the entry shall not be again made except by direction of the council or the order of the supreme court or a judge thereof (ib., s. 24).
Five days’ notice of the meeting of the council for the hearing of an appeal under sec. 2 must be served on the person charged, embodying a copy of the charges or a statement of the inquiry and the time and place of meeting (ib., s. 25).
Rights of Registered Persons.—Every person licensed or registered under the act is entitled according to his qualifications to practise medicine, surgery, and midwifery, or any of[281] them, as the case may be, and recover with costs his reasonable charges for professional aid, advice, and visits, and the cost of medicines or medical and surgical appliances rendered or supplied by him to his patient (ib., s. 26).
Limitations.—Twelve months is established as the period of limitations for an action from negligence or malpractice against a person registered (ib., s. 27).
Evidence.—The registrar is required, under the direction of the council, to print and publish once in two years a register of the names of all persons registered, with the residence and medical title, diploma, and qualification conferred by any college or body, with the dates thereof, as existing on the day of the publication. A copy of such register, for the time being, purporting to be so printed and published, is prima facie evidence that the persons specified are registered. The absence of a name from such copy is prima facie evidence that such person is not registered.
In case a name does not appear in the copy, a certified copy, under the hand of the registrar of the council, of the entry of a name is evidence that such person is registered (ib., s. 28).
Fraudulent Registration.—If a person be registered by false or fraudulent representations the registrar may, on the receipt of sufficient evidence thereof, report the matter to the council, and on the order of the council erase his name from the register and make known the fact and cause by a notice in the newspaper or newspapers on Prince Edward Island (ib., s. 29 [1]).
Offences and Penalties.—Wilfully procuring or attempting to procure registration by false or fraudulent representation is punishable with a penalty not exceeding $50. Knowingly aiding and assisting therein is punishable with a penalty of from $10 to $25 for each offence (ib., s. 29 [2]).
Without registration or license, practising for hire or hope of reward or advertising to give advice in medicine, surgery, or midwifery is punishable with a penalty not exceeding $25 (ib., s. 30).
Wilfully or falsely pretending to be a physician, doctor of medicine, surgeon, or general practitioner, or assuming a title, addition, or description not actually possessed, or pretending to be recognized by law as a physician, accoucheur, or a licentiate[282] in medicine, surgery, or midwifery, is punishable with a penalty not exceeding $25 (ib., s. 31).
Unregistered Persons.—No person is entitled to recover a charge for medical or surgical advice or attendance or for the performance of a surgical operation unless registered, licensed, or otherwise authorized under this act (ib., s. 32).
No person is to be appointed as a medical officer, physician, or surgeon in any branch of the public service, or any hospital or other charitable institution unless registered (ib., s. 33).
Costs.—On prosecution, costs may be awarded and the offender may be committed to a common jail in default of paying the penalty and costs, for not exceeding one month (ib., s. 34).
Appeal from Conviction.—A person appealing from conviction is required to give satisfactory security for the penalty, costs of conviction, and appeal before released from custody (ib., s. 35).
Limitation of Prosecutions.—Prosecutions are required to be commenced within six months from the date of the offence (ib., s. 36).
Prosecutor.—Any person may be prosecutor or complainant (ib., s. 37).
Appeal from Registrar’s Decision.—A person aggrieved by the decision of the registrar may appeal to the council, and persons aggrieved by the decision of the council may appeal to the supreme court of the province, which decision shall be final. The act prescribes the procedure on appeal (ib., s. 38, 39).
Powers of Council.—The council may make by-laws for carrying out the act, to be approved by the lieutenant-governor in council, but nothing shall prevent any registered medical practitioner from giving medical treatment or advice to any person by reason of such person having previously engaged the services of any other physician (ib., s. 40).
The council is authorized to make regulations regarding the holding of examinations and the subjects of examinations (ib., s. 41)
Exceptions.—The act does not prevent any person from giving necessary medical or surgical aid or attendance to any one in urgent need of it provided it be not for hire or gain, nor the giving of it be made a business or means of livelihood; nor[283] does it prevent women from practising midwifery, or any person from practising dentistry or treating cases of cancer by external application, and charging for such service and suing for and recovering reasonable charges; nor does it prevent a druggist, apothecary, or storekeeper from suing for and recovering the price of drugs or chemicals supplied or sold by him (ib., s. 42).
The act does not prevent a person not holding a medical degree, license, or diploma from a university or college from practising medicine, surgery, or midwifery provided he was engaged in such practice in the province for five years immediately before the passage of the act, nor from recovering with costs his reasonable charges for professional aid, advice, and visits and the cost of medicine or other medical or surgical appliances rendered or supplied by him to his patients (ib., s. 43).
Appeal on Prosecution.—Appeal from the decision on prosecution may be taken to the supreme court (ib., s. 44).
Schedule A:
University of Pennsylvania, Philadelphia, Pa.
Jefferson Medical College, Philadelphia, Pa.
Bellevue Medical College, New York, N. Y.
University of New York, New York, N. Y.
College of Physicians and Surgeons, New York, N. Y.
Harvard University.
University of Michigan.
Schedule B specifies at length the requirements for the examination mentioned in sec. 13.
Fees.—Persons registered under sec. 2 are not required to pay a fee.
For registration under secs. 11 and 12, not exceeding $20, to be fixed by the society.
To the council, for a license under sec. 15, $5.
An annual fee is required to be paid by members of the society, not more than $5 annually, as levied by the council (ib., s. 17).
For registration under sec. 19, such fees as the council may appoint.
Quebec.
College of Physicians, etc.—All persons residing in the province authorized to practise medicine, surgery, or midwifery therein, and registered under this law, are constituted a corporation by the name of “The College of Physicians and Surgeons of the Province of Quebec” (R. S., 1888, art. 3,969).
The affairs of the college are conducted by a board of governors, forty in number, chosen as provided in the act and known as the “Provincial Medical Board” (ib., art. 3,972 to 3,975).
Qualification.—No person can lawfully practise medicine, surgery, or midwifery unless he has obtained a license from the said board and unless he be registered (ib., art. 3,976).
Every person who obtains a medical degree or diploma in any university or college mentioned in art. 3,972 is entitled to such license without examination as to his medical knowledge or skill, provided such diploma has only been given after four years of medical study from the date of admission to study and according to the requirements of the act; provided, the said board has power to grant the same privileges to holders of degrees or diplomas of medicine and surgery from other British colonial or French universities or colleges (ib., art. 3,977).
The colleges referred to in art. 3,792 are: Laval University at Quebec, Laval University at Montreal, University of McGill College, University of Bishops College, The Incorporated School of Medicine and Surgery of Montreal affiliated with the University of Victoria College or with any other British university. The privilege above conferred on holders of degrees or diplomas from British colleges and universities is extended to every person whose name is entered upon the medical register under the Imperial Medical Act of 1886 (49-50 Vict., c. 48) or of any act amending the same (ib., art. 3,977 a, as added by Act 1889, c. 39).
The law prescribes the preliminary qualifications for admission to study medicine, surgery, or midwifery to be ascertained by examination. No one is entitled to the license of the college on presentation of a diploma unless previously admitted to study in accordance with these conditions, or unless he has passed an equivalent preliminary examination before a college, school or[285] board authorized by law to require and cause such preliminary examinations to be passed in Her British Majesty’s other possessions (ib., arts. 3,978, 3,979).
A candidate for a license to practise desiring to be registered, and who has not obtained a degree or diploma in medicine from any institution mentioned in art. 3,972 (supra) must, before being entitled to such license and to register, pass an examination before the board as to his knowledge and skill for the efficient practice of medicine, surgery, and midwifery. Upon passing the examination and proving to the satisfaction of the examiners that he has, in an institution for the teaching of medicine in Her Majesty’s possessions, complied with the rules and regulations made by the provincial board, and on payment of such fees as the board may by general by-law establish, such person shall be entitled to a license (ib., art. 3,980).
All persons coming from any recognized college outside of Her Majesty’s possessions desirous of obtaining a license from the College of Physicians and Surgeons of the province must previously pass a preliminary examination before the examiners appointed by the board or establish to the satisfaction of the board that they have already passed equivalent examinations, and they must moreover follow in one of the schools of medicine in the province a complete course (for six months) of lectures, and such other course or courses as shall be necessary to complete the curriculum required by the board. They may pass their professional examination immediately after their preliminary examination (ib., art. 3,981).
Powers of Medical Board.—The board of governors of the College of Physicians and Surgeons has among other powers the power to examine all credentials and documents purporting to entitle the bearer to a license to practise and all diplomas, degrees, or other qualifications sought to be registered, and to require the bearer to attest on oath, to be administered by the chairman, that he is the person whose name is mentioned therein, and that he became legally possessed thereof; and to register in the books of the college the name, age, place of residence and birth of every member of the profession practising in the province, the date of his license and the place where he obtained it (ib., art. 3,982).
The provincial medical board, among other powers, has[286] the power to make regulations respecting the tariffs or rates to be charged in towns and counties for medical, obstetrical, or surgical advice, or for attendance or for the performance of any operation or for any medicines prescribed or supplied. The tariff must be approved by the lieutenant-governor in council, and can only come into force six months after its publication once in the Quebec Official Gazette, and that of the order in council approving the same. The tariff does not, in case of suit, obviate the necessity of proof of giving the advice, care, prescriptions, medicines, and other things therein mentioned (ib., art. 3,983).
The said board has power to fix the fees for license and registration (ib., art. 3,984).
Qualifications of Candidate.—The qualifications of a candidate for a license are:
1. That he holds a certificate of study from a licensed physician for the period intervening between the courses of lectures which he has followed.
2. That he has reached the age of twenty-one years.
3. That he has followed his studies during a period of not less than four years, commencing from the date of his admission by the board to study medicine.
4. That during said four years he attended at some university, college, or incorporated school of medicine within Her Majesty’s possessions not less than two six-months’ courses of general or descriptive anatomy, of practical anatomy, of surgery, of the practice of medicine, of midwifery, of chemistry, of materia medica and general therapeutics, of the institutions of medicine or physiology and general pathology, of clinical medicine, and of clinical surgery; one six-months’ course or two three-months’ courses of medical jurisprudence, one three-months’ course of botany, one three-months’ course of hygiene, and a course of not less than twenty-five demonstrations upon microscopic anatomy, physiology, and pathology.
5. That he attended the general practice of a hospital in which are contained not less than fifty beds under the charge of not less than two physicians or surgeons, for not less than one and one-half years or three periods of not less than six months each.
6. That he has attended six cases of labor and compounded medicines for six months.
Each six-months’ course shall have consisted of one hundred and twenty lectures except in the case of clinical medicine, clinical surgery, and medical jurisprudence.
Of four years’ study required by this section, three six-months’ sessions, at least, must be passed in attending upon lectures at a university, college, or incorporated school of medicine recognized by the board.
The first of such courses must have been attended during the session immediately succeeding the preliminary examination, and the last during the fourth year of study, and the candidates must undergo an examination on the final subjects of the curriculum at the end of the session in the fourth year of study (ib., art. 3,985).
Members of College.—All persons obtaining a license to practise from the College of Physicians and Surgeons of the province are members of the college, but are not eligible for governors within four years from the date of their admission as members (ib., art. 3,986).
Women.—The provincial medical board has power to make regulations respecting the admission of women to the study and practice of midwifery. Women who were legally qualified on the 31st of October, 1879, to practise as midwives in the province, while required to conform to the rules of said college, retain their right. Nothing in the act or the regulations shall prevent women in the country from practising midwifery or assisting at accouchements without being admitted to the study or practice of midwifery; but they must obtain a certificate from a duly licensed physician certifying that they have the necessary knowledge (ib., art. 3,987).
Register.—The medical board is required to cause to be kept by the registrar a register of persons duly licensed and registered, and who have complied with the law and the regulations of the board, and those persons only whose names are inscribed therein are deemed to be qualified and licensed (ib., art. 3,988).
The registrar is required from time to time to make the necessary alterations in the register (ib., art. 3,989).
Evidence.—The registrar, under the direction of the board of governors, causes to be printed, published, and distributed to the members, from time to time, a copy, called The Quebec Medical[288] Register, of the register, containing names, surnames, residences, medical titles, diplomas, and qualifications conferred by a college or other medical body, with the dates of the same. A printed copy, certified under the hand of the registrar as such, is prima facie evidence that the persons named and entered have been registered in accordance with this law. The absence of the name of any person from such copy is prima facie proof that such person has not been lawfully registered; provided always in case a person’s name does not appear on such printed copy, a copy or extract from the register certified by the registrar of the college of the entry of such person’s name on the register is proof that such person is duly registered (ib., art. 3,990).
A certificate under the hand of the registrar of the payment of the annual contribution of members of the college is prima facie evidence that such payments have been made (ib., art. 3,991).
Neglect to Register.—A person entitled to register who neglects to register is not entitled to practise medicine, surgery, or midwifery, or to claim any of the rights and privileges conferred, and is liable for all penalties imposed for practising without registration, saving the right of certain members holding a license from the College of Physicians and Surgeons of Lower Canada (ib., art. 3,992).
Established Practitioner.—A person who has attended medical lectures during three sessions of a medical school in the British possessions, and who has actually been engaged in the practice of medicine for over thirty years in the province, may, on proof of these facts to the satisfaction of the provincial medical board, and producing a certificate signed by two resident medical practitioners in the neighborhood where he has practised that he has succeeded in his profession, and is entitled to the consideration of the board, be entitled to a license and to registration without an examination (ib., art. 3,993).
Unregistered Persons.—No person unless otherwise authorized is entitled to recover any charge for medical or surgical advice, or professional service, or for the performance of any operation, or for any medicines prescribed or supplied, nor is he entitled to any of the rights or privileges conferred, unless he has registered according to law and paid his annual contribution to the college (ib., art. 3,994).
No certificate required from any physician or surgeon or medical practitioner is valid unless the signer is registered (ib., art. 3,995).
Persons Guilty of Felony.—Any registered member of the medical profession convicted of felony forfeits his right to registration, and the medical board causes his name to be erased from the register (ib., art. 3,996).
If a person known to have been convicted of felony presents himself for registration, the registrar is required to refuse him registration (ib., art. 3,997).
Offences and Penalties.—A person not entitled to register convicted of having practised in contravention of this law, for reward or the hope of reward, is liable to a penalty of $50.
A like penalty is incurred by every person assuming the title of doctor, physician, or surgeon, or any other name implying that he is legally authorized to practise, if unable to establish the fact by legal proof, and by every person who in an advertisement in a newspaper or in a written or printed circular, or on business cards or on signs, assumes a designation so as to lead the public to believe that he is duly registered or qualified; and by every person who offers or gives his services as a physician, surgeon, or accoucheur for gain or hope of reward, if he be not duly authorized and registered.
Burden of Proof.—In every prosecution, proof of registration is incumbent on the party prosecuted.
Witnesses.—Members of the college are not incompetent witnesses by reason of their membership.
Costs.—The court imposing a penalty adds costs, and, in default of payment within a delay which it fixes, condemns the defendant to imprisonment in a common jail of the district for sixty days (ib., art. 3,998).
Evidence.—In cases where proof of registration is required, the production of a printed or other copy or extract from the register, certified under the hand of the registrar of the college, is sufficient evidence that all persons named therein are registered practitioners and any certificate upon such proof, or other copy of the register or extract from such register, purporting to be signed by any person in his capacity of registrar of the college, is prima facie evidence that such person is[290] registrar without proof of the signature or of his being in fact such registrar (ib., art. 3,999).
Homœopathists.—The rights of homœopathists are not affected by the foregoing sections (ib., art. 4,002).
The homœopathic physicians and surgeons of the province form a corporation under the name of the Montreal Homœopathic Association (ib., art. 4,003).
The corporation has power to appoint three medical graduates of a British or provincial university or medical licentiates of a British or provincial college or board legally incorporated to be a board of examiners, to examine all persons who may desire to obtain a license to practise homœopathic medicine (ib., art. 4,008).
A person desiring to be examined touching his qualifications to practise according to the doctrines and teaching of homœopathy shall give notice in writing of at least one month to the secretary or treasurer of the association, and show that he is not less than twenty-one years of age; has followed medical studies for not less than four years under the care of one or more duly qualified medical practitioners; has attended at some recognized university or incorporated school of medicine not less than two six-months’ courses of anatomy, physiology, surgery, theory and practice of medicine, midwifery, chemistry, materia medica, and therapeutics respectively, and not less than one six-months’ course of clinical medicine and medical jurisprudence respectively, or their equivalents in time; and shall have complied with the regulations of such university or incorporated school of medicine with regard to such courses, and shall have followed such other course or courses as may hereafter be considered by the board of examiners requisite for the advancement of a medical education.
All such persons shall, at a regularly appointed time and place, be examined on all the aforesaid branches by the board of examiners (ib., art. 4,009).
If the board be satisfied by examination that a person is duly qualified to practise either or all of said branches of medicine, as taught and practised by homœopathists, they shall certify the same under the hands and seals of two or all of such board.
The lieutenant-governor, on receipt of such certificate, may,[291] if satisfied of the loyalty, integrity, and good morals of the applicant, grant to him a license to practise medicine, surgery, and midwifery, or either of them, conformably to the certificate, and all such licensees are entitled to all the privileges enjoyed by licentiates of medicine (ib., art. 4,010).
The corporation appoints a secretary who keeps a register of names of all persons duly licensed to practise medicine, surgery, and midwifery, or either of them, according to the doctrines and teachings of homœopathy.
Only those whose names are inscribed in said register are qualified and licensed to practise according to the doctrines and teachings of homœopathy (ib., art. 4,015).
The said secretary is required to make the necessary alterations in the addresses or qualifications of the persons registered (ib., art. 4,016).
Offences and Penalties.—A person practising according to the homœopathic doctrines for reward in contravention of this act, or assuming a title implying that a person is legally authorized to practise according to homœopathic doctrines, if unable legally to establish such authorization; or by advertisement published in a newspaper or in a written or printed circular, or on business cards or signs, assuming a designation to lead the public to believe that he is duly registered and qualified to practise according to the doctrines of homœopathy; or offering or giving his services as physician, surgeon, or accoucheur for gain or hope of reward, if not duly authorized or registered, is punishable with a penalty of $50.
Burden of Proof.—In every prosecution, the proof of registration is incumbent on the party prosecuted.
Costs.—The court may condemn the defendant to pay $50 in addition to costs within a delay which it determines, and to imprisonment of sixty days in a common jail of the district on default of payment within the delay (ib., art. 4,017).
Witnesses.—A member of the corporation is not an incompetent witness on account of his membership (ib., art. 4,018).
Fees.—The provincial board of medical examiners may establish examination fees (ib., art. 3,981).
Members of the College of Physicians and Surgeons of the Province of Quebec are required to pay an annual fee of $2 (ib., art. 3,986).
FORENSIC MEDICINE.
THANATOLOGICAL.
THE
LEGAL STATUS OF THE DEAD BODY;
THE DISPOSAL AND OBLIGATION TO DISPOSE OF THE SAME; HOW
AND BY WHOM IT MAY BE EXHUMED OR REMOVED;
AUTOPSIES, BY WHOM ORDERED; THE RIGHTS
OF RELATIVES AND ACCUSED PERSONS.
INCLUDING
AN APPENDIX CONTAINING A SYNOPSIS OF THE STATUTES OF THE
DIFFERENT UNITED STATES AND TERRITORIES
CONCERNING SAME.
BY
TRACY C. BECKER, A.B., LL.B., ETC.,
Counsellor at Law, etc.; Professor of Civil Law and Medical Jurisprudence, Law Department, University of Buffalo.
LEGAL STATUS OF THE DEAD BODY.
Disposal and Obligations to Dispose of the Same.—There is no right of property, in the ordinary sense of the word, in a dead human body; but for the health and protection of society it is a rule of the common law, and which has been confirmed by statutes in civilized states and countries, that public duties are imposed upon public officers, and private duties upon the husband or wife and the next of kin of the deceased, to protect the body from violation and see that it is properly interred, and to protect it after it is interred. A parent is bound to provide Christian burial for a deceased child, if he has the means, but if he has not the means, though the body remains unburied so long as to become a nuisance, he is not indictable for the nuisance although he could obtain money for the burial expenses by borrowing it of the poor-law authorities of the parish, for he is not bound to incur a debt. (Reg. v. Vann, 2 Div. C. C., 325; 15 Jur., 1,090.) On the other hand it has been held in England, that every householder in whose house a dead body lies is bound by the common law, if he has the means to do so, to inter the body decently, and this principle applies where a person dies in the house of a parish or a union. (Reg. v. Stewart, 12 A. & D., 1,272.) And the expense may be paid out of the effects of the deceased. (Tugwell v. Hayman, 3 Camp., 298, and note.)
In Pierce v. The Proprietors Swan Point Cemetery, 10 R. I., 227, s. c., 14 Am. Rep., 667, the Court said: “That there is no right of property in a dead body, using this word in its ordinary sense, may be well admitted, yet the burial of the dead is a subject which interests the feelings of mankind to a much greater degree than many matters of actual property. There is a duty imposed by the universal feelings of mankind to be discharged by some one toward the dead; a duty, and we may also say a right, to protect from violation; it may, therefore, be considered as a sort of quasi property, and it would be discreditable[298] to any system of law not to provide a remedy in such a case; ... but the person having charge of it cannot be considered as the owner of it in any sense whatever, he holds it only as a sacred trust for the benefit of all who may from family or friendship have an interest in it.” See also Wyncoop v. Wyncoop, 42 Pa. St., 293; 4 Albany Law Jour., 56; Snyder v. Snyder, 60 How. Prac., 368; Weld v. Walker, 130 Mass., 422; Guthrie v. Weaver, 1 Mo. Apps., 136; Johnson v. Marinus, 18 Abb. N. C., 72, and note.[493]
The law casts the duty of burial of the wife upon the husband, and of the husband upon the wife. In Secord v. Secord (cited in note 1 above), the Court said: “There are cogent reasons connected with public policy and the peace of families, where in the absence of testamentary disposition the possession of a corpse and the right to determine its burial should follow the administration of the estate.” Inasmuch as the husband has the first right to administer upon the estate of the wife, and the wife upon the estate of the husband, the law imposes the correlative duty of burial upon the person having such right; and so it has been held that the husband is liable for the necessary expense of the decent interment of his wife from whom he has been separated, whether the party incurring the expense is an undertaker or mere volunteer.[494]
Where the deceased leaves a will appointing executors, the executors have a right to the possession of the body, and the duty of burial is imposed upon them, but it has been doubted whether at common law a direction by will concerning the disposal of the body could be enforced, and therefore the right to make such direction has been conferred by statute in several States.[495]
And where a widow ordered a funeral of her husband, it was held that she was liable for the expense, although she was an infant at the time, the Court holding that the expense fell under the head of necessaries, for which infants’ estates are liable.[496]
If there be no husband or wife of the deceased, the nearest of kin in the order of right to administration is charged with the duty of burial.[497]
Such acts as casting a dead human body into a river without the rites of sepulture (Kanavans Case, 1 Me., 226); stealing a corpse (2 East, PC., 652) or stealing for dissection a dead body of one executed when the death sentence did not direct dissection (Rex v. Cundick, D. & R., n. p., 13), were indictable offences at common law.[498]
In the works of the early dramatists, and by some writers of fiction, it has been stated, or implied, that the body of a deceased person could be seized and detained to compel the payment of his debts. This was never the law. In Jones v. Ashburnham, 4 East, 460, it was held that to seize a dead body on pretence of arresting for debt would be contra bonos mores, and an extortion on the relatives, and that case distinctly overrules any authority to be derived from the case of Quick v. Coppleton, 1 Vent., 161, to the effect that forbearance to seize or hold a body upon such a pretence would afford any consideration for a promise to pay a debt. So, also, where a jailer refused to give up a body of a person who had died while a prisoner in execution in his custody, to the executors of the deceased, unless they would satisfy certain claims against the deceased due the jailer, the Court issued a peremptory mandamus in the first instance, commanding that the body should be delivered up to the executors (Rex v. Fox, 2 Q. B., 247). And in R. v. Scott, 2 Q. B., 248, it was said, that a jailer who should[300] attempt to do so would be guilty of misconduct in his public character, for which he would be liable to prosecution.[499]
How and by Whom the Dead Human Body may be Removed or Exhumed.—Where the right of burial has been exercised, and the body interred in its final resting-place, no person has any right to interfere with it without the consent of the owner of the grave, or of the properly constituted public authorities. In Foster v. Dodd, 8 D. & E., 842-854, it was held, that a dead body belongs to no one, and is, therefore, under the protection of the public. If it lies in consecrated ground, ecclesiastical authorities will interpose for its protection; but whether in ground consecrated or unconsecrated, indignities offered to the remains or the act of indecently disinterring them, are the ground of an indictment.[500]
Even the purchaser of land upon which is located a burial-ground may be enjoined from removing bodies therefrom, if he attempts to do so against the wishes of the relatives or next of kin of the deceased. Every interment is a concession of the privilege which cannot afterward be repudiated, and the purchaser’s title to the ground is fettered with the right of burial.[501]
On the other hand, the right of the municipal or state authorities, with the consent of the owner of the burial lot or in the execution of the right of eminent domain, to remove dead bodies from cemeteries is well settled.[502]
After the right of burial has once been exercised by the person charged with the duty of burial, or where such person has consented to the burial by another person, no right to the corpse remains except to protect it from unlawful interference.[503]
On the other hand, where a husband did not freely consent to the burial of his wife in a lot owned by another person, it was held that a court of equity might permit him, after such burial, to remove her body, coffin, and tombstones to his own lot, and restrain any person from interfering with such removal.[504]
In Rhodes v. Brandt, 21 Hun, N. Y., 1, the defendant brought an action against one Beelard to recover for services rendered by him, as a physician, in treating a child of Beelard’s for a fracture of the thigh-bone, in which action Beelard set up malpractice on the part of the defendant as a defence. During the pendency of the action the child died and was buried. Subsequently Beelard, the father, acting under the advice of his counsel, directed and allowed the plaintiff, a physician, to cause the body of the child to be exhumed, and a portion of the thigh-bone to be removed, in order that it might be used in evidence on the trial of the question of malpractice. After the bone was removed, the body was returned to the grave. The defendant thereupon caused the plaintiff to be arrested for unlawfully removing the body from the grave contrary to the provisions of the statute, and the plaintiff sued the defendant for malicious prosecution. The Court held that the plaintiff had not removed the body from the grave “for the purpose of dissection or from mere wantonness,” as these terms were used in the statute (3 R. S., 6th ed., 965), for violation of which he had been arrested, nor had he committed any offence against public decency or the spirit of the statute.[505]
Autopsies, by Whom Ordered; the Rights of Relatives and Accused Persons.—As shown in a previous article in this volume, on the Powers and Duties of Coroners and Medical Examiners, in cases of sudden or suspicious death, it has been[302] the law for nearly a thousand years that an inquisition or inquest super visum corporis must be held by an officer known as a coroner, and that this office and its powers and duties were inherited by this country as part of the English common-law system in force at the time of the formation of the republic of the United States. When a body has been buried, and the coroner believes that an inquest is necessary, he has power to disinter the body and hold an inquest, and he may direct a post-mortem examination to be made, but after having done so he must cause the body to be reinterred. It is now well settled that in holding such an inquest, and making such an autopsy or post-mortem examination required by his official duty, the coroner has authority to employ, and it is his duty to employ, professional skill and aid, and his contract will bind the county to pay a reasonable compensation for the same.[506]
As will be seen below from a synopsis of the statutes relating to this matter, many of the States have enacted statutes defining and prescribing the duties of the coroner and other public officers in such cases. At an early period in England (see 2 and 3 Will. IV., chap. 75, sec. 7) it was enacted by the English Parliament that any executor or other person having lawful possession of the body of a deceased person, and not being an undertaker or other party entrusted with the body for the purpose only of interment, might lawfully permit the body of such deceased person to undergo an anatomical examination, unless to the knowledge of such executor or other party such person should have expressed his desire during his life in writing, or verbally in the presence of two or more witnesses during his illness whereof he died, that his body after death might not undergo such examination, or unless the surviving husband or wife or known relative of the deceased shall require the body to be interred without such examination. By another section of this statute (sec. 10), professors of anatomy and other persons duly licensed were declared not liable to punishment for having[303] in their possession human bodies when having such possession according to the provisions of the act.
Section 308 of the New York Penal Code, subdivision 3, as amended by chapter 500, Laws 1889, enacts that whenever and so far as the husband, wife, or next of kin of the deceased, being charged by law with the duty of burial, may authorize dissection for the purpose of ascertaining the cause of death and no further, the right exists to dissect the dead human body. The same statute also provides that whenever any district attorney of that State, in the discharge of his official duties, shall deem it necessary, he may exhume, take possession of, and remove the body of a deceased person, or any portion thereof, and submit the same to a proper physical or chemical examination or analysis, to ascertain the cause of death, which examination or analysis will be made on the order of a justice of the Supreme Court of the State, or the county judge of the county in which the dead bodies shall be, granted on the application of the district attorney, with or without notice to the relatives of the deceased person, or to any person or corporation having the legal charge of such body, as the court may direct. The district attorney shall also have power to direct the sheriff, constable, or other peace officer, and employ such person or persons as he may deem necessary to assist him, in exhuming, removing, obtaining possession of, and examining physically or chemically such dead body, or any portion thereof; the expense thereof to be a county charge paid by the county treasurer on the certificate of the district attorney.
The matter of ordering autopsies and dissections of dead bodies, or exhuming the same for that purpose or other purposes, is a matter of so much public importance that it has been regulated in nearly all of the United States by statutory enactments, which together with the other statutes relating to the subject-matter of this article are hereunto appended.
The author of this article is greatly indebted for assistance in preparing the same, and in compiling these statutes, to Mr. Amasa J. Parker, Jr., of the Albany, N.Y., bar.
APPENDIX.
Statutory Regulations Concerning Dead Bodies.
The coroner has power to hold inquest and direct autopsy,
Ala., Code, sec. 4,801 et seq.
Ariz., Pen. Code, sec. 2,309 et seq.
Ark., R. S., sec. 692.
Cal., Pen. Code; sec. 1,510.
Col., Mill’s Stat., sec. 870.
Conn., Gen. Stat., secs. 2,005, 2,008.
Del., R. S., ch. 33.
Fla., R. S., secs. 3,011, 3,019.
Ga., Code, secs. 590, 591, 4,101 et seq.
Idaho, R. S., sec. 8,377.
Ill., S. & C. Am. Stat., v. 1, 606.
Ind., R. S., secs. 5,878, 5,879.
Iowa, McCl. Am. Code, sec. 487.
Kan., Gen. Stat., secs. 1,780, 1,784.
Ky., Gen. Stat., ch. 25, secs. 3, 11.
La., Voorh. Rev. L., sec. 653.
Me., R. S., ch. 139, sec. 1.
Md., Code, art. 22, secs. 3, 4.
Minn., Gen. Stat., sec. 1,011 et seq.
Miss., Am. Code, sec. 816.
Mo., R. L., sec. 2,438 et seq.
Mont., Crim. L., secs. 869, 883.
Neb., Consol. Stat., sec. 3,144.
N. H., Pub. Stat., ch. 262, sec. 1 et seq.
N. J., Rev. Stat., p. 170 et seq.
N. C., Code, sec. 657.
N. Dak., Comp. Laws, sec. 664 et seq.
Ohio, R. L., sec. 1,221 et seq.
Oklahoma, Stat., sec. 1,745 et seq.
Ore., Crim. Code, sec. 453 et seq.
Pa., Bright Pen. Digest, 1536, sec. 37.
R. I., Pub. Laws, 1884, ch. 420, sec. 17.
S. C., R. S., secs. 711, 2,664 et seq.
Tenn., Code, sec. 6,139 et seq.
Va., Code, sec. 2,928 et seq.
[305]Wash., Hill’s Am. Stat., v. 1, sec. 245 et seq.
W. Va., Code, ch. 154.
Wis., S. & B. Am. Stat., ch. 200.
Wyo., R. S., sec. 1,879 et seq.
Medical examiner shall hold inquest and direct autopsy.
Mass., Pub. Stat., ch. 26, secs. 10, 11.
R. I., Pub. Laws, 1884, ch. 420.
Justice of the peace shall hold inquest and direct autopsy.
Mich., How. Am. Stat., v. 2, sec. 9,583 et seq.
Nev., Gen. Stat., sec. 225 et seq.
N. M., Comp. L., sec. 443 et seq.
Texas, Code Crim. P., art. 988 et seq.
Vt., Rev. L., sec. 3,934 et seq.
Wis., S. & B. Am. Stat., ch. 200.
And may order a body to be disinterred for the purpose of holding such inquisition.
Ark., R. L., sec. 718.
Cal., Pen. Code, sec. 1,510.
Del., R. L., ch. 33.
Ga., Code, secs. 590, 591, 410 et seq.
Idaho, R. L., sec. 8,377.
S. C., R. S., sec. 2,687.
Texas, Code Crim. P., art. 989.
And when not claimed by friends and relatives, to bury the body decently, and when the property of deceased is not sufficient to defray expenses, this may be done at public expense.
Cal., Pen. Code, sec. 3,094.
Col., Mill’s Stat., sec. 882.
Conn., Gen. Stat., sec. 2,015.
Idaho, R. L., sec. 2,081.
Ill., S. & C. Am. Stat., v. 1, 606.
Iowa, McCl. Am. Code, sec. 501.
Kan., Gen. Stat., sec. 1,792.
Ky., Gen. Stat., ch. 25, sec. 6.
La., Voorh. Rev. L., sec. 660.
Me., R. S., ch. 139, sec. 11.
Md., Code, art. 22, sec. 7.
Mass., Laws, 1887, ch. 310.
Mich., How. Am. Stat., v. 3, sec. 9,593.
Minn., Gen. Stat., sec. 1,021.
[306]Miss., Am. Code, secs. 3,145, 3,146.
Mo., R. L., sec. 2,456.
Mont., Gen. Laws, sec. 881.
Neb., Consol. Stat., sec. 3,144.
Nev., Gen. Stat., sec. 2,269.
N. H., Pub. Stat., ch. 262, sec. 16.
N. J., Rev. Stat., p. 170, sec. 5.
N. M., Comp. Laws, sec. 447.
N. Dak., Comp. Laws, sec. 676.
Ohio, R. L., sec. 1,227.
Oklahoma, Stat., sec. 1,759.
Ore., Crim. Code, sec. 462.
R. I., Pub. Laws, 1884, ch. 420, sec. 24.
Tenn., Code, sec. 6,150.
Va., Code, sec. 3,946.
Wash., Hill’s Am. Stat., v. 1, sec. 257.
W. Va., Code, ch. 154, sec. 8.
Wis., S. & B. Am. Stat., ch. 200.
Wyo., R. S., sec. 1,886.
Removal or disinterment of a dead body without authority of law or consent of relatives, for the purpose of selling such body or for dissection or for mere wantonness, is—
(a) A felony.
Cal., Pen. Code, sec. 290.
Ga., Laws, 1882, v. 2, p. 87.
Ill., S. & C. Am. Stat., v. 1, p. 794.
Ind., R. S., sec. 2,166.
Mo., R. S., secs. 3,842, 3,845.
Mont., Laws, 1889, p. 114.
N. C., Laws, 1885, ch. 90.
(b) A misdemeanor.
Ark., R. S., secs. 1,902, 1,903.
Del., Laws, 1883, ch. 234.
Kan., Gen. Stat., sec. 2,372 et seq.
Md., Code, art. 27, secs. 133, 134.
Pa., Bright Pen. Digest, 229, sec. 11.
Tenn., Code, secs. 5,659, 5,660.
(c) Is punishable by various sentences.
Ala., Code, secs. 4,023, 4,028.
Ariz., Pen. Code, sec. 491.
[307]Col., Mill’s Stat., sec. 1,367.
Conn., Gen. Stat., sec. 1,880.
Fla., R. L., sec. 2,625.
Iowa, McCl. Am. Code, sec. 5,328.
Ky., Gen. Stat., ch. 29, art. 17, sec. 16.
Me., R. S., ch. 124, sec. 27.
Mass., Pub. Stat., ch. 207, secs. 47, 48.
Mich., How. Stat., v. 2, sec. 9,297.
Miss., Am. Code, secs. 1,023, 1,024.
Neb., Consol. Stat., sec. 5,847.
N. H., Pub. Stat., ch. 266, sec. 7.
N Dak., Comp. Laws, sec. 6,559.
Ohio, R. L., sec. 7,034.
Oklahoma, Stat., sec. 2,198.
Ore., Crim. Code, sec. 656.
Texas, Pen. Code, art. 345.
Vt., Rev. L., secs. 4,194, 4,196.
Va., Code, sec. 208.
W. Va., Code, ch. 149, sec. 13.
Wis., S. & B. Am. Stat., sec. 4,592.
Wyo., R. L., sec. 1,029.
(d) A high misdemeanor.
N. J., Rev. Stat., p. 249, sec. 122.
Bodies of criminals executed under sentence, and those dying in jail, poor-house, etc., when to be delivered over for dissection.
Ark., R. S., sec. 2,552.
Cal., Pen. Code, sec. 3,094.
Col., Mill’s Stat., secs. 1,547, 1,548, 1,204.
Conn., Gen. Stat., secs. 1,729, 1,732.
Ga., Laws, 1887, v. 2, p. 87.
Ill., S. & C. Am. Stat., v. 1, 869.
Ill., Crim. Code, sec. 503.
Ill., S. & C. Am. Stat., v. 3, p. 867.
Ind., R. L., sec. 4,258 et seq.
Iowa, McCl. Am Code, sec. 5,329.
Kan., Gen. Stat., sec. 3,758.
Me., R. S., ch. 13, sec. 2.
Me., Laws, 1893, ch. 254.
Mass., Laws, 1891, ch. 185.
[308]Mass., Pub. Stat., ch. 202, sec. 8.
Mich., How. Stat., v. 3, sec. 2,284.
Minn., Gen. Stat., sec. 678.
Mo., R. S., sec. 6,883.
Neb., Consol. Stat., secs. 3,299, 3,301, 5,848.
N. H., Pub. Stat., ch. 136.
N. J., Rev. Stat., p. 239, sec. 69.
N. C., Laws, 1891, ch. 129.
N. Dak., Laws, 1890, ch. 92.
Ohio, R. S., sec. 3,763.
Ore., Hill’s Am. Laws, sec. 3,730 et seq.
Pa., Bright Pen. Dig., p. 94, sec. 1 et seq.
Vt., Laws, 1884, ch. 85.
Va., Code, ch. 80.
Wash., Hill’s Am. Stat., v. 1, sec. 2,428 et seq.
Wash., S. & B. Am. Stat., sec. 1,437.
Duty of burial, etc.
Ariz., Pen. Code, sec. 493.
Cal., Pen. Code, sec. 292.
Minn., Gen. Stat., sec. 6,221.
N. Dak., Comp. Laws, secs. 6,550, 6,556.
Oklahoma, Stat., sec. 2,189.
Concealing birth of child which, if born alive, would be a bastard, is punishable.
Col., Mill’s Stat., sec. 1,195.
Fla., R. L., sec. 2,393.
Mass., Pub. Stat., ch. 207, sec. 11.
Mich., How. Am. Stat., sec. 9,284.
Mont., Crim. L., sec. 41.
Neb., Consol. Stat., sec. 5,582.
Nev., Gen. Stat., sec. 4,597.
N. H., Pub. Stat., ch. 278, sec. 14.
N. Dak., Comp. L., sec. 6,947.
Oklahoma, Stat., sec. 2,179.
Ore., Crim. Code, sec. 649.
Pa., Bright Pen. Digest, 431, sec. 158.
R. I., Pub. Stat., ch. 244, sec. 8.
Wis., S. & B. Am. Stat., sec. 4,585.
Is a misdemeanor.
Minn., Gen. Stat., sec. 6,210.
N. J., Rev. Stat., p. 241, sec. 83.
Is a felony.
Mo., R. S., sec. 3,479 (whether born dead or alive)
Alabama.
Removal of body wantonly for dissection or sale, purchase of a body unlawfully disinterred, violating grave with intent to steal body, etc., or wantonly mutilating body, is punishable by fine or imprisonment (Code, secs. 4,023, 4,028).
Coroner, or in his absence justice of the peace, to hold inquest and direct examination of body by surgeon, etc. (Code, sec. 4,801 et seq.).
Arizona.
Mutilation, etc., of dead body is a felony (Pen. Code, sec. 491).
Removal of a part of body unlawfully is punishable (Pen. Code, sec. 492).
Duty of burying body is, if a married woman, on husband; if not a married woman, on nearest of kin who is an adult possessed of sufficient means. If deceased has no relatives, on coroner holding inquest or overseers, etc., of poor (Pen. Code, sec. 493).
Refusal of one on whom duty of burial is imposed by law, is punishable (Pen. Code, sec. 494).
Arrest or attachment of a dead body is a misdemeanor (Pen. Code, sec. 496 et seq.).
Coroner to hold inquest and direct autopsy (Pen. Code, sec. 2,309 et seq.).
Person whose duty it is to bury is entitled to custody except where coroner holds it until inquest is completed (Pen. Code, sec. 495).
Arkansas.
Bodies of persons dying in alms-house, prison, house of correction, or jail shall be surrendered to a physician for dissection, etc., unless the deceased request to be buried or the body is claimed by relatives, or unless deceased died suddenly and unknown; and after such use for dissection it shall be decently buried (R. S., sec. 2,552).
Removal of dead body for the purpose of dissection, or stealing, or from wantonness, or receiving same knowing it to have[310] been unlawfully disinterred, is a misdemeanor (R. S., secs. 1,902, 1,903).
Dead body can be transported out of county in which death occurred on permit of State board of health (R. S., sec. 480).
Coroner to hold inquest and direct autopsy, etc. (R. S., sec. 692).
And may order a body to be disinterred for inquisition (R. S., sec. 718).
California.
Removal, mutilation, or disinterment of dead body without authority of law is a felony (Pen. Code, sec. 290).
Removal of part of body for sale, dissection maliciously or wantonly is punishable (Pen. Code, sec. 291).
Duty of Burial.—Of married woman, on husband; not a married woman, nearest of kin who is an adult with sufficient means; where no relatives, on coroner who held the inquest or overseers, etc., of poor (Pen. Code, sec. 292).
Refusal to bury by person on whom duty rests by law to bury, is a misdemeanor and he is liable for treble the expenses (Pen. Code, sec. 293).
Custody of body is on him on whom duty to bury is imposed by law, except where coroner detains remains for inquest (Pen. Code, sec. 294).
Arrest or attachment of dead body for any debt or demand is a misdemeanor (Pen. Code, sec. 295).
One who disinters or exhumes a body without permit of board of health, health officer, or mayor, or transports such exhumed remains through streets of town, city, etc., except in a sealed coffin, guilty of a misdemeanor (Laws, 1878, ch. 673).
A sheriff, coroner, or keeper of county poor-house, public hospital, county jail, or State prison, etc., must surrender bodies of those who are to be buried at public expense, to any physician or surgeon for dissection, etc., unless deceased during his last sickness requested to be buried or body is claimed by relatives, etc., or deceased was a stranger or traveller, died suddenly (Pen. Code, sec. 3,094).
Coroner to bury body when no other person takes charge of same (Pen. Code, sec. 4,286).
Coroner to hold inquest, direct autopsy, and may exhume (Pen. Code, see. 1,510).
Colorado.
Concealment of death of issue which, if born alive, would be a bastard, is punishable (Mill’s Stat., sec. 1,195).
Body of criminal executed for capital offence shall be delivered to a physician or surgeon unless claimed by relative or friend (Mill’s Stat., sec. 1,204).
Board of health, mayor, etc., or officer, etc., having control of any alms-house, prison, hospital, jail, etc., shall surrender bodies to be buried at public expense to any physician or surgeon for dissection, etc., unless deceased during last illness requested to be buried, or body is claimed by relatives or friends, or deceased was a stranger or traveller who died unknown (Mill’s Stat., secs. 1,547, 1,548).
Non-resident poor person to be decently buried (Mill’s Stat., sec. 3,391).
Coroner to hold inquest, etc., or, if none, bury it decently at expense of county (Mill’s Stat., secs. 870-882).
Removal of body unlawfully for sale, dissection, etc., punishable (Mill’s Stat., sec. 1,367).
Board of health may direct removal of dead bodies from cemetery within a city (Laws, 1893, ch. 113, sec. 54).
Connecticut.
No body shall be buried or disinterred or removed beyond limits of any town unless a permit is obtained, and where deceased died of an infectious disease body shall be in a hermetically sealed case (Gen. Stat., secs. 106, 108, 113).
Custody of remains is in husband or wife or next of kin (Gen. Stat., sec. 536).
Coroner to hold inquest, etc. (Gen. Stat., secs. 2,005, 2,008). And deliver body to friends or, if none, to town authorities for burial (Gen. Stat., sec. 2,015).
Mayor, etc., may deliver bodies of those not buried within twenty-four hours after death to medical college for dissection, etc., unless relatives or friends do not consent, or deceased requested to be buried, or was a stranger or traveller (Gen. Stat., sec. 1,729).
Bodies of convicts dying in State prison and not having any[312] known relatives, shall be delivered to medical institution of Yale College (Gen. Stat., sec. 1,732).
Body of one dying in a hospital shall not be examined unless father, etc., consent, or if none, within forty-eight hours after death (Gen. Stat., sec. 1,735).
Removal of body from grave unlawfully, or receiving, secreting, or dissecting same, is punishable (Gen. Stat., 1880).
Body of executed criminal shall be buried by sheriff (Gen. Stat., sec. 1,640).
Delaware.
Coroner to hold inquest, etc., or may cause body to be disinterred (R. L., ch. 33).
Removal of body from grave unlawfully, a misdemeanor (Laws, 1883, ch. 204).
Florida.
Buying, selling, or having possession for purpose of buying or selling, a dead body is punishable (R. L., sec. 2,625).
Concealing birth of issue which, if born alive, would be a bastard, is punishable (R. L., sec. 2,393).
Coroner to hold inquest, etc. (R. L., secs. 3,011, 3,019).
Georgia.
Coroner to hold inquest or to disinter same for inquisition (Code, secs. 590, 591, 410 et seq.).
Public officers and their assistants, and their deputies of every county, city, town, or other municipality, or of every prison, chain gang, penitentiary, county morgue, public hospital, having control of dead body to be buried at public expense (not dying of infectious disease) shall deliver same to medical college for dissection, etc., unless claimed by friends or relatives or such friends or relatives request same to be buried, or unless deceased was a stranger or traveller (Laws, 1887, vol. 2, p. 77).
Removal of body from grave, etc., unlawfully for dissection or sale is felony, or receiving or purchasing it knowing it to have been so taken, or trafficking in dead bodies, or having them conveyed without the State for sale, etc., is a felony (Laws, 1882, vol. 2, p. 87).
Idaho.
Coroner to hold inquest, etc., and may exhume it for that purpose (R. L., sec. 8,377).
Coroner to bury body decently when not claimed by relatives, etc., and if necessary, at expense of county (R. L., sec. 2,081).
Illinois.
Removal of body unlawfully or aiding in such removal is punishable as a felony—one to ten years (S. & C. Am. Stat., vol. 1, p. 794).
Coroner to hold inquest, etc. (S. & C. Am. Stat., vol. 1, p. 606).
And to deliver body to friends or bury decently if no friends claim it, if necessary at county expense (S. & C. Am. Stat., vol. 1, p. 606).
Body of executed criminals may be delivered to any physician or surgeon for dissection unless friends object (S. & C. Am. Stat., vol. 1, p. 869; Crim. Code, sec. 503).
In cities and counties where population exceeds one hundred thousand, superintendents of penitentiaries, wardens of poor-houses, coroner, city undertaker, having body required to be buried at public expense, may deliver remains to medical college or any physician or surgeon for dissection, unless claimed by relatives (S. & C. Am. Stat., vol. 3, p. 867).
Indiana.
Removal of dead body or part of same unlawfully is a felony (R. L., sec. 2,165).
Concealment of body or part thereof, which has been unlawfully used for dissection, is a felony (R. L., sec. 2,167).
Receiving or buying a body knowing it to have been unlawfully disinterred is a felony (R. L., sec. 2,168).
Dead body of one dying in a State, city, or county prison or jail, or county asylum or infirmary or public hospital, or dead body of an executed criminal, or dead body of a vagrant, or one killed while committing a felony or escaping from prison or officers, may be delivered to the faculty of a medical college in State for dissection, etc., unless deceased requested to be buried or body is claimed by next of kin (R. L., sec. 4,258 et seq.).
Dissecting or possessing body for dissection except as prescribed by law is a felony (R. L., sec. 4,271).
Coroner to hold inquest, etc. (R. L, secs., 5,878, 5,879).
Iowa.
Coroner to hold inquest, etc. (McCl. Am. Code, sec. 487).
To bury body decently at expense of county, if necessary, or deliver it to relatives (McCl. Am. Code, sec. 501).
Removal, etc., of dead body unlawfully, or aiding such removal or knowingly receiving body so removed, etc., is punishable (McCl. Am. Code, sec. 5,328).
Coroner, undertaker, superintendent of public asylum, hospital, poor-house, or penitentiary, may deliver body to medical college or physician for dissection, etc., unless relatives, etc., refuse or deceased desired to be buried (McCl. Am. Code, sec. 5,329).
Bodies of those executed, or dying in hospitals or prisons under sentence for crime, shall be delivered to medical college or association or any physician or surgeon for dissection, etc., unless relatives or friends do not consent, or body shall have been interred, or is not claimed by relatives, or deceased expressed a wish to be buried, and after such use the remains shall be interred (Gen. Stat., sec. 3,758).
State board of health shall issue permits for transportation of bodies beyond county where death occurred (Gen. Stat., sec. 6,030).
Kansas.
Coroner to hold inquest, etc. (Gen. Stat., secs. 1,780, 1,794).
To bury body if not claimed by friends, etc., and at public expense, if necessary (Gen. Stat., sec. 1,792).
Removal of a body unlawfully for dissection or wantonly, or receiving body knowing it to have been so removed, is a misdemeanor (Gen. Stat., sec. 2,372 et seq.).
Kentucky.
Coroner to hold inquest, etc. (Gen. Stat., ch. 25, secs. 3, 11).
To bury the body or deliver to friends (Gen. Stat., ch. 25, sec. 6).
Body of one dying on a steamboat, or other craft, if not[315] claimed by friends, shall be buried by master or officer in command on shore, at least four feet deep (Gen. Stat., ch. 29, art. 17, sec. 15).
Removal of body unlawfully from grave is punishable (Gen. Stat., ch. 29, art. 17, sec. 16).
Louisiana.
Coroner shall hold inquest, etc., and bury body when not claimed by friends (Voorh. Rev. L., secs. 653, 660).
Maine.
Coroner to hold inquest, etc. (R. L., ch. 139, sec. 1).
To bury the body at State or town expense (R. L., ch. 139, sec. 11).
Seizure of body on execution, punishable (R. L., ch. 124, sec. 26).
Removal, etc., of body unlawfully, or receiving it knowingly, or exposing, etc., body, is punishable (R. L., ch. 124, sec. 27).
Bodies may be buried and the expense recovered from the town (R. L., ch. 24, sec. 34).
If any resident request or consent that his body be delivered to a physician or surgeon for dissection, it may be so delivered, unless kindred or family connection objects (R. L., ch. 13, sec. 1).
Body of criminal dying in State prison or jail, or who was executed, may be delivered to medical college or physician, etc., for dissection, unless deceased or kindred request to be buried (R. L., ch. 13, sec. 2).
Body of person dying in the State, which is not claimed by relatives, notice having been given, shall be delivered to medical school unless ten voters of the town object to such disposition in writing (Laws, 1893, ch. 254).
Maryland.
Coroner to hold inquest, etc. (Md. Code, art. 22, secs. 3, 4).
Shall bury the body when necessary at public expense (Md. Code, art. 22, sec. 7).
Removal, etc., from graveyard, etc. (except potter’s field), of a body is a misdemeanor (Md. Code, art. 27, secs. 133, 134).
Massachusetts.
Medical examiners shall hold inquest, etc. (Pub. Stat., ch. 26, secs. 10, 11).
And shall deliver it to relatives or friends, or if no one claims it, to overseer of poor etc., for burial (Laws, 1887, ch. 310).
Body shall not be buried in city or town or removed therefrom without a permit (Laws, 1888, ch. 306).
Body of one dying of infectious disease shall not be transported without permit, and only in a sealed case (Laws, 1883, ch. 124, sec. 2).
Body shall not be cremated without permit and inquest by medical examiner, or within forty-eight hours after death, unless death was occasioned by contagious disease (Laws, 1885, ch. 265, sec. 4).
Overseers of poor, mayor and alderman of city, or superintendent of State alms-house, may deliver body of person required to be buried at public expense, to any physician or surgeon or medical college unless deceased requested to be buried, or relative request burial or claim it, or deceased was a stranger or traveller (Laws, 1891, ch. 185).
Body of criminal executed shall be delivered for dissection to a medical college if requested; if not, to friends or relatives, or, if none, to any physician or surgeon (Pub. Stat., ch. 202, sec. 8).
Removal of body unlawfully from grave is punishable, or buying, selling, or possessing for such purpose, is punishable (Pub. Stat., ch. 207, secs. 47, 48).
Concealing birth of child which, if born alive, would be a bastard, is punishable (Pub. Stat., ch. 207, sec. 11).
Seizing dead body on execution is punishable (Pub. Stat., ch. 207, sec. 46).
Body of a prisoner shall be buried by sheriff at town expense if not claimed by relatives or friends (Pub. Stat., ch. 220, sec. 31).
Michigan.
Justice of the peace to hold inquest, etc. (How. Am. Stat., vol. 2, sec. 9,583 et seq.).
And shall bury the body at the State or town expense (How. Am. Stat., vol. 3, sec. 9,593).
Woman concealing death of issue which, if born alive, would be a bastard, is punishable (How. Am. Stat., vol. 3, sec. 9,284).
Board of health, officers, sheriff, etc., of any prison, etc., poor-house, alms-house, having body required to be buried at public expense, shall, if not claimed by relatives, or if it have died of any infectious disease, deliver it to University of Michigan, etc., for dissection, etc. (How. Am. Stat., vol. 3, sec. 2,284).
Body shall not be shipped out of State nor used in State for any purpose but anatomical study (How. Am. Stat., vol. 3, sec. 2,286).
Removal of body unlawfully is punishable (How. Stat., vol. 2, sec. 9,297).
Minnesota.
Gen. Stat., secs. 6,220, 6,230, same as N. Y. P. C., secs. 305-315.
Concealing birth of child which died before or after birth is a misdemeanor (Gen. Stat., sec. 6,210).
Coroner to hold inquest, etc. (Gen. Stat., sec. 1,011 et seq.).
And cause body to be buried at expense of county (Gen. Stat., sec. 1,021).
Section 6,216, same as 303, N. Y. P. C.
Body must be buried within four days, and if death was from contagious disease, within twenty-four hours and in a tightly sealed coffin which must not be reopened (Gen. Stat., sec. 607).
Wardens, superintendents of poor, and other persons having control of bodies shall deliver same to medical college committee, for dissection, unless claimed by relatives or friends, or relatives or friends do not consent, or one detained as a witness or on suspicion of having committed a crime, or deceased requested to be buried (Gen. Stat., sec. 678).
Mississippi.
Body of paupers and strangers to be buried (Am. Code, secs. 3,145, 3,146).
Coroner to hold inquest, etc. (Am. Code, sec. 816).
Removal of body unlawfully and wantonly, for sale or receiving same, is punishable (Am. Code, secs. 1,023, 1,024).
Missouri.
Coroner to hold inquest, etc. (R. L., sec. 2,438 et seq.).
And shall bury the body, if not claimed by friends, at public expense (R. L., sec. 2,456).
And may direct a chemical analysis and microscopical examination of body (R. L., sec. 2,469).
Superintendents or wardens of penitentiary, houses of correction, insane asylums, poor-houses, and coroners, sheriffs, city and county undertakers, having charge of a body required to be buried at public expense, shall deliver the same to medical college for dissection unless claimed by relatives or friends, and trafficking in such bodies is a misdemeanor (R. L., sec. 6,883 et seq.).
Concealing birth of child, so that it may not be known whether it was born alive or dead, is a felony (R. L., sec. 3,479).
Removal of dead body from grave without authority (except that of criminal executed for crime), for purpose of sale, etc., or receiving such body knowingly, is a felony (R. L., secs. 3,842, 3,845).
Montana.
Concealing birth of child which, if born alive, would be a bastard, is punishable (Crim. Laws, sec. 41).
Coroner to hold inquest, etc. (Gen. Laws, secs. 869, 883).
And bury body at public expense if not claimed by relatives, etc. (Gen. Laws, sec. 881).
Removal, etc., of dead body from grave without authority, and for the purpose of sale or dissection, or from wantonness, is a felony (Laws, 1889, p. 114).
Nebraska.
Coroner to hold inquest, etc. (Consol. Stat., sec. 3,130 et seq.).
To bury body if not claimed by friends (Consol. Stat., sec. 3,144).
Removal of body from grave without authority for sale, dissection, etc., is punishable (Consol. Stat., sec. 5,847).
Fœticide is punishable (Consol. Stat., sec. 5,582).
Bodies of paupers or criminals unclaimed by friends or relatives may be delivered to medical college or physician for dissection, etc., and such body shall not be transported out of State (Consol. Stat., secs. 3,299, 3,301, 5,848).
Nevada.
Justice of peace to hold inquest, etc. (Gen. Stat., sec. 2,256 et seq.).
And cause the body to be buried at public expense (Gen. Stat., sec. 2,269).
Body shall not be buried without certificate of physician or coroner (Gen. Stat., sec. 4,872 et seq.).
Body shall not be transported out of State without a permit (Gen. Stat., secs. 4,870, 4,871).
Concealing birth of child which, if born alive, would be a bastard, is punishable (Gen. Stat., sec. 4,597).
Non-resident, et al., to be buried at public expense (Gen. Stat., sec. 1,986).
New Hampshire.
Coroner to hold inquest, etc. (Pub. Stat., ch. 262, sec. 1 et seq.).
And bury body if a stranger, at public expense (Pub. Stat., ch. 262, sec. 16).
Concealing birth of child which, if born alive, would be a bastard, is punishable (Pub. Stat., ch. 278, sec. 14).
Body of person dying in a county, city, or town, or State prison or jail, required to be buried at public expense, shall be delivered to any physician or medical college for dissection, etc., unless deceased requested to be buried, or friends claimed it or request burial, or deceased was a stranger or traveller who died suddenly (Pub. Stat., ch. 136).
Body not to be buried without permit or disinterred (Pub. Stat., ch. 173, sec. 6).
Removal of dead body without authority, or concealing it, knowing it to have been so dug up, is punishable (Pub. Stat., ch. 266, sec. 7).
New Jersey.
Coroner to hold inquest, etc. (Rev. Stat., p. 170 et seq.).
And bury body if not claimed by friends (Rev. Stat., p. 170, sec. 5).
Concealing birth of child which, if born alive, would be a bastard, is a misdemeanor (Rev. Stat., p. 241, sec. 83).
Body of executed criminal may be delivered to physician, etc., for dissection unless claimed by relatives (Rev. Stat., p. 239, sec. 69).
Removal of a body without authority for sale, dissection, etc., is a high misdemeanor (Rev. Stat., p. 249, sec. 122).
Exposing body of an executed murderer is a misdemeanor (Supp. Rev. Stat., p. 194, sec. 19).
Body must not be buried without a permit; nor body brought into the State without permit; nor taken out of State without permit (Laws, 1888, ch. 39, secs. 5-8).
New Mexico.
Justice of the peace to hold inquest, etc. (Comp. Laws, sec. 443 et seq.).
And bury the body (Comp. Laws, sec. 447).
Body of one dying of a contagious disease shall not be carried in an open coffin, or be exposed (Laws, 1889, ch. 79, sec. 8).
Body shall not be buried within fifty yards of running stream (Laws, 1891, ch. 93).
New York.
Duty of burial, etc. (Pen. Code, sec. 305 et seq.).
Attempt at sexual intercourse with dead body is a crime against nature (Pen. Code, sec. 303).
Transfer of body of one who died of a contagious or infectious disease shall be in hermetically sealed casket (Laws, 1893, ch. 661, sec. 23).
Bodies of those dying in, or in custody of managers, etc., of any prison, asylum, morgue, hospital, or in possession of undertakers, shall be delivered to medical college of this State, etc., for purpose of medical study, unless claimed by relatives or friends, or friends or relatives do not assent to such disposal, or[321] deceased requested during last illness to be buried (Laws, 1893, ch. 661, sec. 207).
In certain cases bodies of convicts, unless claimed, shall be delivered to certain medical colleges (R. S., pt. 4, ch. 3, secs. 132, 133).
District attorney may cause body to be exhumed, examined, etc. (Pen. Code, sec. 308).
North Carolina.
Coroner to hold inquest, etc. (Code, sec. 657).
Concealing birth of child, by burying dead body, is a misdemeanor. Opening grave without authority for purpose of taking body is a felony (Laws, 1885, ch. 90).
Coroner may order a chemical analysis of remains (Laws, 1887, ch. 269).
Dead body of convict, unclaimed by friends, shall be delivered to medical college except such dying of contagious disease (Laws, 1891, ch. 129).
Body of one dying of contagious disease must not be transported by common carrier until disinfected, nor shall permit for removal be issued until such disinfection (Laws, 1893, ch. 214, sec. 16).
North Dakota.
Coroner to hold inquest, etc. (Comp. Laws, sec. 664 et seq.).
And bury the body if not claimed by friends, etc. (Comp. Laws, sec. 676).
Concealing birth of child which, if born alive, would be a bastard, or of child dying within two years after birth, is punishable (Comp. Laws, sec. 6,947).
| Comp. Laws. | |||||
| Sec. | 6,549 | same as | 305 | N. Y. P. C. | |
| ” | 6,550 | ” | 306 | ” | |
| ” | 6,551 | ” | 307 | ” | |
| ” | 6,552 | ” | 308 | (1-3) | ” |
| ” | 6,553 | ” | 309 | ” | |
| ” | 6,554 | ” | 310 | ” | |
| ” | 6,559 | ” | 311 | ” | |
| ” | 6,560 | ” | 312 | ” | |
| ” | 6,563 | ” | 314 | ” | |
Duty of burial of married woman, on husband. If not married woman, on nearest of kin who is an adult or has means sufficient (Comp. Laws, sec. 6,556).
Refusal to bury by one on whom duty is imposed by law, a misdemeanor (Comp. Laws, sec. 6,557).
Custody of body pertains to one whose duty it is to bury (Comp. Laws, sec. 6,558).
When cemetery is by law changed to other place, duty is on relative to move body (Comp. Laws, sec. 6,562).
Body of executed criminal, and those dying in State penitentiary or county jail under sentence, shall be delivered to medical college or any physician for dissection, unless deceased requested to be buried, or friends ask to have it buried, or deceased was a stranger or traveller (Laws, 1890, ch. 92).
Ohio.
Coroner to hold inquest, etc. (R. L., sec. 1,221 et seq.).
And bury body, etc. (R. L., sec. 1,227).
Body of pauper or unknown, not an inmate of any penal, charitable, or reformatory institution, and not claimed by relative or delivered for dissection according to law, shall be buried at public expense (Laws, 1890, p. 283).
Corpse shall not be conveyed to or from a city without a permit (R. L., sec. 2,119).
Bodies of those dying in city hospitals, city or county infirmaries, work-houses, asylums, charitable institutions, penitentiaries, or jails, which are required to be buried at public expense, shall be delivered to medical college or society for study, etc., unless claimed by relative, or deceased was a stranger or traveller (except tramps) (R. L., sec. 3,763).
Removing body from grave without authority for dissection or receiving such body is punishable (R. L., sec. 7,034).
Body of executed criminal, if not claimed by relative or friends, may be delivered for dissection, etc. (R. L., sec. 7,343, 1).
Oklahoma.
Coroner to hold inquest, etc. (Stat., sec. 1,745 et seq.).
And bury the body at public expense if not claimed by relatives (Stat., sec. 1,759).
Concealing birth of issue which, if born alive, etc., or dying within two years after birth, is punishable (Stat., sec. 2,179).
| 2,188-2,190 | same as | 305-307 | N. Y. P. C. | |
| 2,191 | ” | 308 | ” | (except subd. 4) |
| 2,192-2,193 | ” | 309-310 | ” | |
| 2,198 | ” | 311 | ” | (ex. punishment) |
| 2,199 | ” | 312 | ” | |
| 2,202 | ” | 314 | ” |
Custody is in him whose duty it is to bury (Stat., secs. 21, 97).
Duty of burial of married woman, on husband; if not married woman, on nearest of kin who is an adult and has sufficient means (Stat., sec. 2,195).
Refusal to bury by one on whom duty rests, is a misdemeanor (Stat., sec. 2,196).
Oregon.
Coroner to hold inquest, etc. (Crim. Code, sec. 453 et seq.).
And bury body if not claimed by friends (Crim. Code, sec. 462).
Unmarried woman concealing birth of child so that it may not be known whether it was born alive or not, is punishable (Crim. Code, sec. 649).
Bodies of criminals executed, those dying in hospitals, insane asylums, alms-houses, or penitentiaries, may be delivered to medical college or physician for dissection, etc., unless they shall have been interred, or claimed by relatives, or relatives and friends do not consent, or deceased expressed a wish to be buried; and they shall be used for such purpose only and in this State (Hill’s Am. Laws, sec. 3,730 et seq.).
Removal of body without authority, etc., is punishable (Crim. Code, sec. 656).
Pennsylvania.
Coroner to hold inquest in Philadelphia County only in case of a violent death (Bright Pen. Dig., 1536, sec. 37).
And may in Berks and Lancaster Counties order a post mortem (Bright Pen. Dig., 1536, sec. 38).
Concealing death of child which, if born alive, would be a bastard, is punishable (Bright Pen. Dig., 431, sec. 158).
Removal of body from grave without authority is a misdemeanor (Bright Pen. Dig., 229, sec. 11).
Bodies of those dying in alms-house, hospital, prison, or public institution, or those in morgue, which are required to be buried at public expense, shall be delivered to medical college, physician, etc., to be used for scientific purposes only, unless claimed by relatives or deceased was a traveller, and trafficking in such bodies is a misdemeanor (Bright Pen. Dig., p. 9, sec. 1 et seq.).
Rhode Island.
Concealing death of child which, if born alive, would be a bastard, so that it may not be known, etc., is punishable (Pub. Stat., ch. 244, sec. 8).
Seizing dead body under execution is punishable (Pub. Stat., ch. 223, sec. 2).
Bodies of those dying in jail shall, if not claimed by relatives, be buried at public expense (Pub. Stat., ch. 201, sec. 30).
Medical examiner to make autopsy (Pub. Stat., 1884, ch. 420).
And bury body of stranger at State expense if necessary (Pub. Laws, 1884, ch. 420, sec. 24).
Coroner to hold inquest if, in opinion of medical examiner, death was caused by act of some one other than deceased (Pub. Laws, 1884, ch. 420, sec. 17).
South Carolina.
Coroner to hold inquest, etc. (R. L., secs. 711, 2,664 et seq.).
And may have body disinterred for inquisition (R. L., sec. 2,687).
Tennessee.
Coroner to hold inquest, etc. (Code, sec. 6,139 et seq.).
And may order a chemical analysis of remains, etc. (Code, sec. 6,150).
Body to be buried, if not claimed by relatives, etc., at public expense if necessary (Code, sec. 6,160).
Wilfully and improperly exposing or abandoning a dead body is a misdemeanor (Code, sec. 5,658).
Removing or purchasing dead bodies without authority is a misdemeanor (Code, secs. 5,659, 5,660).
Body of deceased convict to be buried unless claimed by friends (Code, sec. 6,402).
Texas.
Justice of the peace to hold inquest, etc. (Code Crim. P., art. 988 et seq.).
And may disinter the body for such inquisition (Code Crim. P., art. 989).
Removal, etc., of dead body from grave without authority is punishable (Code, art. 345).
Bodies of convicts to be buried (Rev. C. Stat., art. 3,561).
Vermont.
Justice of the peace to hold inquest, etc. (Rev. Laws, sec. 3,934 et seq.).
Removal, etc., of dead body without authority, is punishable (Rev. Laws, secs. 4,194, 4,196).
Bodies of those dying in poor-house or other public institution, which are required to be buried at public expense, may be delivered to any physician for dissection, etc., unless deceased requested to be buried, or friends or relations request burial, or deceased was a stranger or traveller. Such body shall not be removed from State, and shall be used for scientific purposes only (Laws, 1884, ch. 85).
Virginia.
Coroner to hold inquest, etc. (Code, sec. 3,938 et seq.).
And to bury the body at public expense (Code, sec. 3,946).
Removal, etc., of dead body from grave without authority, is punishable (Code, sec. 3,794).
Bodies of those dying on vessels in State, shall be buried by master on the shore above high-water mark (Code, sec. 2,002).
Bodies of those dying in alms-house, prison, morgue, hospital, jail, or other public institution, which are required to be buried at public expense, and bodies of criminals executed for[326] crime shall be delivered to medical college, etc., and physician or surgeon for anatomical study, unless (except criminals) relatives and friends claim the body or deceased was a stranger or traveller; and such bodies shall not be sent out of the State (Code, ch. 80).
Washington.
Coroner to hold inquest, etc. (Hill’s Am. Stat., vol. 1, sec. 245 et seq.).
And bury body, if not claimed by friends, at public expense (Hill’s Am. Stat., vol. 1, sec. 257).
Bodies of those dying in poor-house, public hospital, county jail, State prison, etc., which are required to be buried at public expense, shall be delivered to medical college, physician, surgeon, etc., for study, unless deceased requested to be buried, or it is claimed by friends or relatives, or deceased was a stranger or traveller; and such body shall be used only in the State (Hill’s Am. Stat., vol. 1, sec. 2,428 et seq.).
Removal, etc., of body from the grave without authority is punishable (Pen. Code, sec. 208).
West Virginia.
Coroner to hold inquest, etc. (Code, ch. 154).
And bury the body at public expense, or if of a stranger, may forward it to its destination or bury it (Code, ch. 154, sec. 8).
Removal, etc., of a body from grave is punishable (Code, ch. 149, sec. 13).
Wisconsin.
Justice of the peace or coroner to hold inquest, etc. (S. & B. Am. Stat., ch. 200).
And shall cause the body to be buried at public expense (S. & B. Am. Stat., ch. 200, sec. 4,877).
Dead body of convict shall, if not claimed by relatives or friends, be buried (S. & B. Am. Stat., sec. 4,926).
Removal, etc., of body from grave without authority is punishable (S. & B. Am. Stat., sec. 4,592).
Concealing death of child which, if born alive, would be a bastard, is punishable (S. & B. Am. Stat., sec. 4,585).
A public officer having in his charge a body required to be buried at public expense, shall deliver same to member of State or county medical society, etc., for anatomical study, unless claimed by relatives, or they consent to such disposal, or deceased requested to be buried, or was a stranger or traveller (S. & B. Am. Stat., sec. 1,437).
THE POWERS AND DUTIES
OF
CORONERS AND MEDICAL EXAMINERS.
BY
AUGUST BECKER,
Of the Buffalo (N. Y.) Bar.
THE POWERS AND DUTIES
OF
CORONERS AND MEDICAL EXAMINERS.
BY
AUGUST BECKER,
Of the Buffalo (N. Y.) Bar.
POWERS AND DUTIES OF CORONERS AND MEDICAL EXAMINERS.
I. The Coroner and his Court.
Coroner an Ancient Officer.—The office of coroner is one of the most important and ancient known to the common law. A coroner, or coronator, was so called because he had principally to do with the pleas of the crown, or suit wherein the king was immediately concerned.[507] The office is first mentioned in a charter granted in the year 925 by King Athelstan, to the authorities of Beverley. The office as at present constituted was not clearly established until after the Norman conquest.
Under this head come the lord chief justice and puisne justices of the King’s Bench, who are supreme and sovereign coroners respectively.[508] The duties of the office of coroner involve questions of the greatest interest to society, to government, and to the rights and privileges of the individual citizen. The office has lost much of the honor and respect which formerly appertained to it. Its character and importance have been much diminished in latter times, making striking contrast with the high estimation it was held in by our ancestors in days when none but the gentry and knights of the shire were deemed eligible.
In fact so great was the dignity of this office in ancient times, that it was never presumed that coroners would condescend to be paid for their services.[509] They were chosen by all the freeholders of the county court for life or good behavior, and were liable to be removed for cause by the writ de coronatore exonerando. There were three kinds of coroners at common law: Virtute officii; virtute cartæ sive commissionis; and virtute electionis.[510] The office of coroner was[332] brought to America by the colonists along with the institutions of the common law, and may be said to exist in the several States with all the common-law incidents, except so far as they may have been modified by statute. The present defined powers of coroners in Great Britain and the United States, unless modified by British statutes and American acts, are derived from the English Stat. de Officio Coronatoris, 4 Edward I., s. 2. Coroners virtute officii and virtute cartæ sive commissionis are unknown to our institutions. Here the office of coroner may be classed under the head of coroners virtute electionis. Generally speaking the coroner is a county officer.
Coroner’s Duties both Judicial and Ministerial.
By the common law his powers and duties are both judicial and ministerial. In his ministerial capacity he is merely a substitute for the sheriff, as when the sheriff is a party.[511] His powers and duties thereunder it is not the present purpose to state and define. His judicial authority relates to inquiries into cases of sudden death, by a jury of inquest, super visum corporis, or, as it is more commonly defined, an inquisition, with the assistance of a jury, over the body of any person who may have come to a sudden or violent death, or who may have died in prison.[512] It is not necessary that the death should be both violent and sudden, and that both these circumstances must concur to give the coroner jurisdiction. It is sufficient to give the coroner jurisdiction if the death occurs from any violence done to a person by another, although such violence may not have terminated the life of a party suddenly, and it is still the duty of the coroner to hold an inquest.[513] Indeed the presumption is that he has acted in good faith and on sufficient cause.[514] And so when[333] several persons have been suddenly killed by the same violent cause, under circumstances proper to be inquired of by a coroner’s inquest, it is proper and necessary for the coroner, acting in good faith, to hold a separate inquest over each body.[515] A coroner’s inquest is a judicial investigation. The coroner cannot delegate his authority to any one. Neither can he appoint a deputy under the common law. He must act in person as any other judicial officer; and it may safely be said that a coroner has no power to appoint a deputy coroner, except where special provision is made therefor by statute.[516] In England, a coroner’s court is a court of record, and it has accordingly been held that trespass cannot be maintained for turning a person out of a room where the coroner is about to take an inquisition.[517] But in this country, it may safely be said that a coroner’s court is not one of record, but of inferior jurisdiction.[518] The performance of the functions of a coroner are judicial in their character; so judicial that he is protected under the principles which protect judicial officers from responsibility in a civil action brought by a private person. His proceedings amount to entries concerning[334] matters of public interest, made under the sanction of an official oath, and in compliance or presumed compliance of the law.[519]
Of his Authority to Hold an Inquest.—His authority to hold an inquest is not confined to the body of a person who may have died within his territorial jurisdiction, but extends to all bodies brought within his jurisdiction, no matter where death may have taken place.[520] So in any case where, after burial, an inquest becomes necessary to determine the manner of the death of a person who, dying in one, is buried in another county, the coroner of the latter county is the proper officer to hold the inquest.[521] A coroner cannot hold a second inquest while the first is existing. As we have seen, in holding an inquest the coroner performs a judicial duty, and he is functus officio as soon as the verdict has been returned. He can hold no second inquest in the same case unless the first has been quashed by a court of competent jurisdiction, and a new inquiry ordered. He cannot set aside or quash his own inquest. If he were allowed to hold two inquests, not only might the greatest inconvenience arise from the inconsistent findings of the respective juries, but such a practice would be liable to great abuse, and as the object of the proceeding is merely preliminary, the main purpose being to ascertain whether it is probable that a crime has been committed, and to examine the facts and circumstances and preserve the evidence, all the ends of this inquiry are answered by one inquisition, super visum corporis. We believe no reported case is to be found in this country where a second inquisition has been held, the first remaining undischarged, nor is any such practice known to or recognized by our laws.[522]
The Inquest must be Held upon View of the Body.
The coroner can in no case hold an inquest except upon view of the body. This is jurisdictional and cannot be waived by any one. He is not bound to hold an inquest before burial of the body takes place. When it has been buried, and he believes an inquest necessary, he is vested with authority to have the body disinterred and hold his inquest, and if necessary direct a post-mortem examination to be made, but after having done so, he must cause it to be reburied.[523] Deep interests are involved in the proper discharge of the duties of coroners; the character, liberty, and perhaps the life of a citizen accused of crime on the one hand, and on the other the aiding of public justice in establishing the guilt and securing the punishment of the actual criminal. Many of the questions which fall within the scope of a coroner’s inquisition are of an intricate and most perplexing character, a correct solution of which can only be arrived at by minds the best instructed and habituated to their investigation. In many cases some of these questions can be satisfactorily settled by the evidence of persons having cognizance more or less direct of the facts; in others, however, they can only be solved by the facts deduced from pathological anatomy, and other circumstances connected with the dead body, the cause of the extinction of life in which is the subject of the inquest.
In Massachusetts Office of Coroner Abolished.—Indeed, in Massachusetts the office of coroner was abolished in 1877, and the governor was invested with power, and it is his duty, to appoint, by and with the advice and consent of the council, able and discreet men, learned in the science of medicine, to be medical examiners, whose duties are to make examinations as provided in the statute upon the view of the dead bodies of such persons only as are supposed to have come to their death by violence.[524]
Coroner may Employ Professional Skill.—A thorough examination aided by professional skill is in general absolutely necessary to the proper administration of justice. It would no doubt be strange if a coroner had no authority to pledge the[336] responsibility of the county for the compensation of all auxiliary services which are necessary to the proper execution of his office, and which he can by no other means command; for instance, when his duty requires him to disinter a body, he cannot be expected to do it with his own hands, or by hands paid for with his means. Indeed it has been said that, in this enlightened age, a coroner who would consign to the grave the body over which he had held an inquest, without availing himself of the lights which the medical science has placed within his reach, would in most cases fall short of what his official duty requires.[525] It is the generally accepted view of the law now that it is the duty of a coroner holding an inquest super visum corporis to avail himself of professional skill and aid, and his contract will bind the county to the payment of a reasonable compensation for making a post-mortem examination.[526]
Post-Mortem Examination.
Whether such examination should take place before the coroner has empanelled a jury seems to be an open question. We would venture the opinion that it should not, inasmuch as the jury ought to see and view the body in the same condition, as near as may be, as it was when found, and not after it has been mutilated, as it must need be by a post-mortem examination.[337] It is, however, settled that the post mortem should not be in the presence of the jury, and that they are to be instructed by the testimony of the physicians who are designated by the coroner to make the examination.[527] The coroner’s right to dissect the dead body of a human being does not extend to all cases. Such a power could be wielded with the most injurious effects upon a community. His power to dissect is confined to those cases where he is authorized by law to hold an inquest upon the body. But a post-mortem examination, conducted by surgeons employed by a coroner holding an inquest, is not a part of the inquest in such a sense as that every citizen has a right freely to attend it. At common law it was essential to the validity of a coroner’s inquisition that the jury should view the body. And so is our law. But it was never required that the body should be dissected in any case. It is discretionary with the coroner to cause a dissection to be made, and to select the surgeons. He has also a discretion to determine whether any person, and what persons, may be present besides the surgeons. Not even the jurors have a right to witness the examination. They are to be informed of what it discloses by the testimony of the surgeons. Indeed, no person has a right to be present at the post-mortem examination upon the ground that he is suspected of having caused the death. He loses no legal right by being excluded. He has no right to dissect the body. If the coroner’s jury pronounce him guilty, the inquest, like the indictment of a grand jury, simply makes him liable to arrest.[528]
Massachusetts Statutory Provisions.
The statute law of Massachusetts has already been referred to. It has abolished the office of coroner and in its place put medical examiners, so called, who are presumed to be learned in the science of medicine. Their powers, however, are not co-extensive with those of coroners. A medical examiner cannot hold an inquest. He cannot hold an autopsy without being thereto authorized in writing by the district attorney, mayor, or selectmen of the district, city, or town where a dead body lies. He can only upon receiving notice that there has been found, or is lying within the county, the dead body of a person who is supposed to have come to his death by violence, repair to the place where such body lies, view and take charge of the same. If he deems a further examination necessary and is authorized so to do, he must make an autopsy in the presence of two or more discreet persons, whose attendance he may compel by subpœna if necessary, and he must then carefully reduce or cause to be reduced to writing every fact and circumstance tending to show the condition of the body and the cause and manner of death, together with the names and addresses of the witnesses. If he deems it necessary, he may employ a chemist to aid in the examination of the body or of substances supposed to have caused or contributed to the death,[529] the record of which he must subscribe.[530] Such an autopsy does not, however, upon the trial of an accused render other competent evidence, as to the condition and appearance of the dead body at the time of the autopsy, inadmissible.[531] The autopsy may be followed by an inquest held, not by the examiner, but by a justice of the district, police, or municipal court for the district or city in which the body lies, or a trial justice. One of these functionaries must hold an inquest upon being notified by a medical examiner that in his opinion a death was caused by violence, and after hearing the testimony draw up and sign a report and issue process for apprehension of a person charged by the report with[339] the commission of an offence, if he is not in custody.[532] Even though a medical examiner reports that a death was not caused by violence, and the district attorney or the attorney-general is of a contrary opinion, either one may, notwithstanding such report, direct an inquest to be held in accordance with the provisions of the statute.[533]
New York’s Statutory Provisions.
In New York the powers and duties of coroners are defined by statute. Coroners in the city of New York are governed by a special act relating to that city exclusively. For the State at large it is provided that whenever a coroner is informed that a person has been killed or dangerously wounded by another, or has suddenly died under such circumstances as to afford a reasonable ground to suspect that his death has been occasioned by the act of another by criminal means, or has committed suicide, he must go to the place where the person is, and forthwith inquire into the cause of the death or wounding, and summon not less than nine nor more than fifteen persons, qualified by law to serve as jurors, if such death or wounding be of a criminal nature, to appear before him forthwith at a specified place, to inquire into the cause of death or wound, and if it appears from the evidence taken or during the inquisition, that any person or persons are chargeable with the killing or wounding, or that there is probable cause to believe that any person or persons are chargeable therewith, and if they are not in custody the coroner must forthwith issue a warrant for the arrest of the person or persons charged with such killing or wounding, who must be arraigned before the coroner for examination, and the coroner has power to commit the person or persons so arrested to await the result of the inquisition. A coroner is disqualified from acting as such in any case where the person killed or dangerously wounded is a co-employee with the coroner of any person or persons, association or corporation, or where it appears that the killing or wounding has been occasioned, directly or indirectly, by the employer of the coroner.[534] It is further provided that whenever a convict shall die in any State prison, it shall be the duty of the inspector having charge of the prison[340] and of the warden, physician, and chaplain of the prison, if they or either of them shall have reason to believe that the death of the convict arose from any other than ordinary sickness, to call upon the coroner having jurisdiction to hold an inquest upon the body of such deceased convict.[535] The New York Criminal Code further provides that when six or more of the jurors appear, they must be sworn by the coroner to inquire who the person was, and when, where, and by what means he came to his death or was wounded as the case may be, and into the circumstances attending the death or wounding, and to render a true verdict thereon according to the evidence offered to them or arising from the inspection of the body.[536] The coroner may issue subpœnas for and summon and examine as witnesses every person who in his opinion, or that of any of the jury, has any knowledge of the facts; and he must summon as a witness a surgeon or physician, who must, in the presence of the jury, inspect the body, and give a professional opinion as to the cause of the death or wounding.[537] The jury, after inspecting the body and hearing the testimony, must render their verdict, and certify it by an inquisition in writing, signed by them, and setting forth who the person killed or wounded is, and when, where, and by what means he came to his death or was wounded, and if he were killed or wounded, or his death were occasioned by the act of another by criminal means, who is guilty thereof, in so far as by such inquisition they have been able to ascertain.[538] The testimony of the witnesses examined before the coroner’s jury must be reduced to writing by the coroner, or under his direction, and must be forthwith filed by him, with the inquisition, in the office of the clerk of the court of sessions of the county, or of a city court having power to inquire into the offence by the intervention of a grand jury.[539]
If, however, the defendant be arrested before the inquisition can be filed, the coroner must deliver it with the testimony to the magistrate before whom the defendant is brought.[540] If the jury find that the person was killed or wounded by another under circumstances not excusable or justifiable by law, or that his death was occasioned by the act of another by criminal[341] means, and the party committing the act be ascertained by the inquisition and is not in custody, the coroner must issue a warrant signed by him with his name of office, for the arrest of the person charged.[541] The coroner has power to compel the attendance of a witness and testify, and he may punish a witness for disobedience, as upon a subpœna issued by a magistrate.[542] The coroner’s warrant may be served in any county; and the officer serving it must proceed thereon, in all respects, as upon a warrant of arrest on an information, except that when served in another county it need not be indorsed by a magistrate of that county.[543] When the defendant is brought before the coroner, he must proceed to examine the charge contained in the inquisition or information, and hold the defendant to answer, or discharge him therefrom, in all respects as upon a warrant of arrest on an information.[544]
II. The Jury and Inquest.
Jurors Must be Sworn by Coroner.—The jurors summoned by a coroner to attend an inquest must be from the county or jurisdiction wherein the coroner is empowered to act. He cannot proceed with the inquest until he has summoned and sworn the jury. The jurors are not challengeable, and therefore they should be carefully selected and sworn by the coroner himself. His duties are judicial and he can only take an inquest super visum corporis, and an inquest in which the jury is not sworn by himself is absolutely void and of no effect.[545]
They Must Investigate and Determine the Facts.—After being sworn by the coroner they must investigate and determine and are the sole arbiters of the facts; the coroner’s duty being to instruct them in the law. They must go, view, and examine the body together, and not separately. It is essential to the validity of the inquest that the jury should view the body.[546]
Coroner may Compel Attendance of Witnesses.—When the coroner sits to hold an inquest, he sits as a judicial officer, armed with all the ordinary powers possessed by judicial officers. He may compel the attendance of jurors whose qualifications[342] are usually such as are required of jurors in a court of record. It is his duty to present before the jury all the material testimony within his power, touching the death as to the manner whereof the jury are to certify, and that which makes for as well as against the party accused. It is his duty to summon before his inquest every person whom he has any reason to believe possesses any knowledge relative to the death which he is investigating. He is to summon such persons to attend before him for examination. He has full authority to compel obedience to his subpœnas. He has this power by the common law.[547] If a post-mortem examination is made, the examining surgeons should testify before the jury as to the matters disclosed by the examination.[548] The witnesses produced must be sworn by the coroner, and their testimony reduced to writing by him or under his direction.
Rights of Accused Party.
The coroner is not required to take the testimony of the witnesses who are examined before the jury in the presence of the party accused. The accused has not the right to be represented by counsel, or to cross-examine the witnesses.[549] He is not permitted to produce witnesses before the coroner to show himself innocent of the crime. The coroner is not required to examine any witnesses to establish the guilt of such party when brought before him by virtue of process issued after the finding of the inquisition.[550]
Deliberation by Jury and Return of an Inquisition.—After the evidence has been taken, and the jury instructed in the law by the coroner, the jury should retire to deliberate upon their verdict. During such deliberation and until they have arrived at their verdict the coroner should not be present in the room where the jury is deliberating. After they have agreed on their verdict it should be reduced to writing, and the coroner[343] is bound to accept it as final in his court. The inquisition should then be signed by the coroner and jury.[551] If the inquest is signed by the coroner and duly certified by him, the jurors having signed by making their cross marks, and the whole being certified by the coroner, his certificate of the signatures of the jurors is sufficient and the inquisition is properly made.[552] If several jurors on the inquest have the same christian and surname, it is not necessary in the caption of the inquisition to distinguish them by abode or otherwise.[553] The law requiring the coroner to make a return of the testimony with the inquisition cannot be satisfied short of some official certificate indicating that the witnesses named were sworn before him, to the matter insisted on as evidence against a prisoner. At least if there be no formal authentication, there should be proof aliunde that the memorandum presents the testimony of the witness truly.[554]
III. The Effect of the Evidence and Verdict.
Under the common law formerly, a coroner’s inquisition was equivalent to an indictment by a grand jury upon which the accused might be tried. But in this country no person can be tried upon a coroner’s inquisition, yet the inquisition of a coroner’s jury finding a person guilty of murder has about the same force against him, until the grand jury passes upon his case, that an indictment found by them has thereafter, prior to his trial.
Coroner has Power to Issue Process of Apprehension.—If a person is charged with the crime in the inquisition, the coroner has power and he issues his process for the apprehension of the accused when not in custody solely upon the inquisition. The inquisition, though taken in the absence of the prisoner, and upon the testimony of witnesses he could not cross-examine, settles the question of his guilt until the grand jury passes upon the case. It justifies the commitment of the prisoner to jail, in the same manner that the testimony of witnesses does taken before a justice of the peace. The coroner can only examine the prisoner in the same manner as upon a[344] warrant of arrest or on information, and is not authorized to examine witnesses either against the prisoner or for him, when he is apprehended by virtue of process issued subsequent to the finding of the inquisition by the jury, or in custody of the coroner without process at the time the same is found.
Privilege of Prisoner upon Arrest.—The prisoner has the privilege of telling his own story before the coroner, which is to be returned with the inquisition, and that is all. He cannot be discharged on it, however plausible it may be; and he has not the privilege of proving it true before the coroner. He should, therefore, not be discharged, and he cannot have the case investigated again before it is passed upon by the grand jury.[555]
Under the provisions of the New York Criminal Code the defendant against whom an inquisition has been found by a coroner’s jury is entitled to a hearing before a magistrate, whether he has been arrested before the inquisition has been filed or is arrested after such filing. Under the provisions of sec. 779, in the case of a defendant who has been arrested before the inquisition can be filed, the prisoner is entitled to be examined before the magistrate, before whom he may be brought, as provided in sec. 781, and in the case of a prisoner who has not been arrested until after the inquisition was filed, under secs. 781 and 783 the defendant is entitled to be heard before a magistrate in all respects as upon a warrant of arrest on an information. The magistrate must proceed to examine the charge contained in the inquisition, and hold the defendant to answer or discharge him therefrom.[556] The information is the allegation made to a magistrate that a person has been guilty of some designated crime.[557]
When Evidence taken before Coroner of a Party Charged with Crime Admissible in Evidence upon His Trial Subsequently.
There is nothing which distinguishes between the proceedings of a coroner’s inquest and any other official proceedings[345] taken and returned in the discharge of official duty as to their admissibility in evidence. A witness, therefore, may be contradicted by the production of a deposition thus given by him before a coroner.[558] But the line is sharply drawn in what cases the testimony of a witness examined before a coroner’s inquest can be used on his subsequent trial, and in what cases it cannot. When a coroner’s inquest is held before it has been ascertained that a crime has been committed, or before any person has been arrested charged with the crime, and a witness is called and sworn before the coroner’s jury, the testimony of that witness, should he afterward be charged with the crime, may be used against him on his trial, and the mere fact that at the time of his examination he was aware that a crime was suspected, and that he was suspected of being the criminal, will not prevent his being regarded as a mere witness, whose testimony may be afterward given in evidence against himself. If he desires to protect himself he must claim his privilege. But if, at the time of his examination, it appears that a crime has been committed, and that he is in custody as the supposed criminal, he is not regarded merely as a witness, but as a party accused, called before a tribunal vested with power to investigate preliminarily the question of his guilt, and he is to be treated in the same manner as if brought before a committing magistrate, and an examination not taken in conformity with the statute cannot be used against him on his trial for the offence.[559] So the doctrine as to silence being taken as an implied admission of the truth of allegations spoken or uttered in the presence of a person, does not apply to silence at a judicial proceeding or hearing, and since the proceedings at a coroner’s inquest are of a judicial character, what there transpired must be considered as a part of the proceedings.[560] The leading cases[346] which have been before the New York Court of Appeals upon this important question, and from which that court has finally deduced that rule, may be here referred to.
Hendrickson Case.—In the first case the wife of the defendant died suddenly in the morning, and in the evening of the same day a coroner’s inquest was held. The defendant was called and sworn as a witness upon the inquest. At that time it did not appear that any crime had been committed, or that the defendant had been charged with any crime, or even suspected, except so far as the nature of some of the questions asked of him might indicate such a suspicion. On his subsequent trial on an indictment for the murder of his wife, the statements made by him at the coroner’s inquest were held admissible, on the ground that he was not examined as a party charged with the crime, that it had not appeared even that a crime had been committed, and that he had simply testified as a witness on the inquiry as to the cause of the death.[561]
McMahon Case.—Following this came the McMahon Case, in which it appeared that the defendant was arrested by a constable, without warrant, on a charge of having murdered his wife. The constable took him before the coroner, who was holding an inquest on the body, by whom he was sworn and examined as a witness. It was held that the evidence thus given was not admissible on the prisoner’s trial for the murder, and his conviction was reversed upon that ground.[562]
Teachout Case.—The doctrine of this case was more clearly defined and somewhat limited in a later case, the Teachout Case. In that case the defendant appeared at the coroner’s inquest in pursuance of a sub-pœna to testify, and voluntarily attended; he was not under arrest, but was informed by some one that it was charged that his wife had been poisoned and that he would be arrested for the crime. Before he was[347] sworn he was informed by the coroner that there were rumors that his wife came to her death by foul means and that some of those rumors implicated him, and that he was not obliged to testify unless he chose. He said he had no objection to telling all he knew. The Court in delivering its opinion preludes it by a reference to these facts as showing that the statements made were voluntary in every legal sense, and held that a mere consciousness of being suspected of a crime did not so disqualify him that his testimony, in other respects freely and voluntarily given before the coroner, could not be used against him on his trial on a charge subsequently made of such crime. On that ground it held the evidence properly admitted, at the same time referring with approval to the McMahon Case, and distinctly limiting the rule of exclusion to cases within its bounds.[563]
Mondon Case.—Then followed the Mondon Case, where on the finding of the body of the deceased, the defendant was arrested without warrant as the suspected murderer. While he was thus in custody the coroner empanelled a jury and held an inquest, and the defendant was called as a witness before the inquest and was examined by the district attorney and by the coroner. The prisoner was an ignorant Italian laborer unfamiliar with the English language. He was unattended by counsel, and it did not appear that he was in any manner informed of his rights, or that he was not bound to answer questions tending to criminate him He was twice examined; on the first occasion the examination was taken by questions put either by the district attorney or by the coroner, and the result written down by the coroner, who then read the evidence over to him, line by line, and asked him if he understood it and if it was the truth, and he said it was, and the coroner then reswore him to the deposition. The coroner, after taking the defendant’s testimony on the first day, came to the conclusion that the defendant did not understand English well enough to be examined, and that it ought to be taken through an interpreter, which was done, in order that they might get it a little better and a little fuller. It was held that the defendant’s testimony was not admissible upon his trial on the indictment.[564] It will be seen that this latter case follows in direct line with the rule announced in the McMahon Case and clearly distinguishes another case, the McGloin Case, upon the authority of which the trial court held the testimony of the prisoner in the Mondon Case admissible.
McGloin Case.—The case of McGloin was not that of the examination of a prisoner on oath before a magistrate before whom he was taken involuntarily, while in custody, and interrogated by the magistrate, who to all appearance had power to require him to answer, but while under arrest the prisoner said to the inspector of police who had him in charge that he would make a statement. The inspector then said[348] that he would send for a coroner to take it. The coroner was then sent for and came to police headquarters and took down in writing the confession dictated by the prisoner, the coroner asking no questions and not acting in any official capacity, but as a mere amanuensis to take down the confession and prove the contents. It was held that the confession of the prisoner was admissible in evidence upon his trial for murder.[565]
Rule in Pennsylvania.—The rule in Pennsylvania is substantially that when the testimony given by the prisoner under oath before a coroner’s inquest, previous to him being charged or suspected of the murder of the individual upon whose body the inquest was sitting, may afterward be given in evidence against him, on his trial for the murder of such person.[566]
Rule in Nebraska.—The statements of a prisoner to be competent evidence must have been voluntarily made. In cases of declaration made on an examination before a coroner’s inquest by a person under arrest or charged with the crime and also under oath, they are not admissible. But when the person, although he be subsequently charged with the offence, appears voluntarily, and gives testimony, before any accusation has been made against him, his statements are admissible in evidence against him on the trial of an indictment for the crime.[567]
MEDICO-LEGAL AUTOPSIES.
BY
H. P. LOOMIS, A.M., M.D.,
Professor of Pathology in the University of the City of New York; Visiting Physician
and Curator to Bellevue Hospital, New York; Pathologist to the
Board of Health, New York City; President New
York Pathological Society, etc., etc.
AUTOPSIES.
A medical examiner before proceeding with an autopsy, especially if called before the body has been removed from the place where it was found, should carefully note certain facts. These should be entered by himself or an assistant with great care, in a note-book, as this book can be introduced as evidence in any trial. A satisfactory way is to dictate to the assistant as the examination proceeds, and at the conclusion the assistant reads the notes taken, and the examiner verifies them.
SURROUNDING OBJECTS—POSITION OF THE BODY.
These should be first noted. The character of the soil; the condition of the ground, and whether it shows footprints; if so, their direction; the evidence of any struggle; the presence of any weapon; and finally, the exact position in which the body lies, especially the position of the hands and feet. This is important, for the body may be found in a position which the deceased could not have assumed on the supposition of the wound or injury having been accidental or homicidal. If possible a photograph should be taken of the body in the exact position in which it is found. If it is absolutely necessary to remove the body, it should be done with great care, keeping the body in as horizontal a position as possible.
The character of the surrounding soil should be noted. This is of special importance when the body to be examined has been exhumed: for the question of preservation of the body and the ability to recognize pathological changes may be brought up at a trial. This was an important point raised in the Buchanan case (New York, 1893).
If a body be found in the water, examine the character of the water and the temperature, and if found near the shore, the character of shore and bottom.
Blood.—The situation of blood-stains, and their number and extent, on clothing or surrounding objects should be noted.[352] This will often show whether a struggle has taken place after receiving the fatal wound, and is also of medico-legal importance if made at the time the body is found, for it may be so situated as to show that the body has been interfered with after death.
Again, spots of blood found upon articles of clothing or upon surrounding objects should be noted as to their form and direction, for they may serve to furnish an indication of the position of the person with respect to them when the wound was inflicted. For example, if the spot was oval, the presumption is that the person was placed obliquely with respect to the stain while the hemorrhage was occurring. The force with which the blood was thrown out will in some measure be indicated by the obliquity or length of the spot. The amount of blood will also often indicate whether the person has died suddenly, the exact spot where death occurred, whether a struggle took place, and will also preclude the possibility of a person moving after receiving the fatal injury. When we examine a body, especially when found in a room, care must be taken not to be misled by the accidental diffusion of blood by persons going in and out, or touching the body (see Blood-Stains, Vol. II.)
Clothing.—The examination of the clothing should be thorough. A description of each article should be noted, and the order in which it is removed; for often it is important to prove that the garments were worn by or belonged to the deceased. If any blood is on the clothing, note whether the blood is in large patches, or whether it is sprinkled over the garment: the amount of the blood and what garments are stained by it. Note and examine whether the blood has flowed down the front of the clothing, whether it has soaked the inner garments, or again, whether it has collected along the back; for these appearances will sometimes demonstrate whether a wound was inflicted while the person was sitting, standing, or lying down. For example, if the throat is cut while the person is lying down, the blood will be found on each side of the neck along the back and not down the front of the body. Few suicides cut their throats in a recumbent position, and this distribution of the blood may serve to distinguish a suicidal from a homicidal wound.
The condition of the clothing may also serve to show whether there has been any struggle, and the presence of dry spots or mud on it may sometimes serve to connect an accused person with an act of murder. This is well illustrated in the case of Reg. v. Snipe, reported in Beck’s “Medical Jurisprudence,” where evidence was adduced to show that some spots of mud on the boots and clothing of the prisoner, when examined microscopically, contained infusoria, shells, and some rare aquatic vegetables. The mud of the ditch close to where the body was found, as also the mud on the clothing of the dead body, presented the same microscopical appearances. The medical expert who gave this evidence swore that in his opinion the mud spots on the body and on the prisoner’s boots were derived from the same ditch, for the mud of all the other ditches in the locality was found, on microscopical examination, to be different. The well-known case which occurred in New York a few years ago, known as the “Shakespeare case,” furnishes an example of the importance of carefully examining all stains on the clothing found on bodies.
If there are several stabs or cuts on the body involving the dress, it should be noted whether they are blood-stained, and if so, whether the stain is on the inside or outside of the garments, for sometimes in simulated personal injury a stain of blood may be inadvertently applied to the outside of the dress, as in wiping a weapon.
Weapons.—If a weapon is found, the character of the weapon and its exact position should be noted. This is frequently of importance in telling whether a person has died from an accidental or self-inflicted wound. In a case where death occurs immediately or within a few minutes, the weapon is found near the body, or often so tightly grasped in the hand that it can be with difficulty removed. If the weapon is found near the body it should be noted on which side and at what distance, and it must be questioned whether it could have fallen on the spot or been thrown there by the deceased. It is compatible with suicide that the weapon should be found at some distance from the body. An instance has been recorded where an individual was discovered in bed with his throat cut, and the bloody razor was found closed and in the pocket of the deceased. If a weapon cannot be discovered, or is concealed,[354] it is strong presumptive evidence of homicide; especially when the wound is such as to produce speedy death.
Note whether the weapon is sharp or blunt, straight or curved. If a knife, the handle and inner portion should be examined, for the blade may have been washed.
If the wound has involved any large vessels, it is improbable that the weapon can have been thrown any distance from the body, and when it is, there are always fair grounds to expect interference with the original position of the body. One circumstance which always strongly points to suicide is the finding of the weapon firmly grasped in the hand of the cadaver. The hand of a dead person cannot be made to grasp or retain a weapon as does the hand which has grasped it at the last moments of life. The amount of blood on the weapon should be noted, but it must be remembered that a knife may have produced a fatal stab wound and still no blood be found on it. This is explained by the fact that in a rapid plunge the vessels were compressed, and only after the drawing of the knife and relieving of the pressure blood began to flow, or possibly the blood may have been wiped off the knife by the elasticity of the skin.
When a person has died of a gunshot wound, especially at close range, it is important to look for any wadding or paper found in the wound, as in a number of instances the finding of such has led to the detection of the criminal. For example, handwriting has been found on the paper, or it has formed part of a printed page the rest of which has been found in possession of the accused. When a gun is discharged near the body, a portion of the wadding is almost always found in the irregular wound produced.
POST-MORTEM EXAMINATION.
Having completed the examination of the surroundings, one next proceeds with the post-mortem examination, which should be conducted according to a well-defined plan, following which the results obtained will always be satisfactory.
If possible the body should be removed to a large, well-ventilated, and especially well-lighted room. No artificial light, if it can possibly be avoided, should be used when performing[355] the autopsy; artificial light is especially bad on account of its yellowness and its power to modify natural color. Many diseased conditions cannot be satisfactorily determined by artificial light. The body should be placed on a high table, and the facility with which the autopsy is made will often depend on having the table high enough to render stooping unnecessary. Never make an autopsy, if it can possibly be avoided, on a body while in a coffin, as the examination is always unsatisfactory. The size and surroundings of the room, and how it is lighted, should be entered in the note-book.
Instruments.—If possible the following instruments should be at hand before proceeding with an examination, although some of them may be dispensed with:
(1) Large section knife; (2) scalpels; (3) enterotome (for opening intestines and stomach); (4) costotome, or large bone forceps (for cutting ribs); (5) scissors, large and small (one blade blunt); (6) saw; (7) chisel; (8) dissecting forceps; (9) probe; (10) blowpipe; (11) curved needles and strong twine; (12) measuring and graduated glass; (13) small scales.
Besides the above instruments, some basins containing water; sponges, bottle of flexible collodion, Lugol’s solution of iodine for the amyloid test, will be needed.
Post-Mortem Wounds.—Various plans have been proposed to protect the operator’s hands from the post-mortem wounds which are often so dangerous, such as wearing rubber gloves, smearing the hands with carbolized vaselin, both of which have their disadvantages: the gloves being too clumsy, and the vaselin rendering it almost impossible to hold the knife steady. Gloves should always be worn, however, where the body has undergone much decomposition, or where the person may have died from any septic disease. A method which I have found satisfactory is to cover all cuts and hangnails with flexible collodion, and then to have a basin of clean water at hand, and from time to time to rinse one’s hands in the water. It is from bathing the hands in the cadaveric fluids and not from cuts that most of the danger comes. If possible an absolutely new board, large enough upon which to examine the organs, should be at hand, for it may be claimed at a trial that the organs and tissues, if placed and examined on surrounding objects, have become contaminated.
Toxicological.—If a chemical analysis of the various organs and tissues is to be made, and it is impossible to have the chemist present, the medical examiner should obtain some new glass jars of suitable size, with close-fitting glass covers. These jars should be rinsed with distilled water, and in them the various organs are to be placed; if possible with no preserving fluid on them. But if it is found impossible to deliver the jars to the chemist at once, alcohol may be poured over the organs in the jars, but it is specially important that a sample of this alcohol should be retained, that a chemist may at a future date test the same for any impurities. After the organs and tissues have been placed in the jars, the mouths should be closed and sealed, and the seal remain in the custody of the examiner until the jars are delivered to the chemist.
Parts to be Preserved for the Chemist.—In cases of suspected poisoning, it is not sufficient that the stomach and intestines alone should be preserved for the chemist as has been indicated, each part by itself; for it should be remembered that the portion of poison remaining in the alimentary tract is but the residue of the dose which had been sufficient to destroy life, and if the processes of elimination have been rapid no trace of the poison will be found in the alimentary canal but can readily be detected in other organs. Again, the poison may not have been introduced by the mouth, in which case none may be found in the digestive tract.
The chemist should receive, besides the stomach and entire intestinal canal, the liver, one or both kidneys, the spleen, a piece of muscle from the leg, the brain, and any urine found in the bladder.
When it is impossible for any reason to obtain the whole of any organ, the part removed should be carefully weighed and its proportion to the rest of the organ noted.
It is also of extreme importance to preserve in sealed and labelled jars those parts of a body which may show the evidence of disease, or on the appearance of which one’s evidence is founded.
ORDER OF AUTOPSY.
In making the autopsy, the operator should stand on the right side of the body and make the incision by grasping the[357] knife firmly in the hand, and cutting with the whole of the blade and not with the point. The knife should be swept along from the shoulder rather than from the wrist, thus making a long, smooth, deep cut; never a jagged one.
The method of examining the human body after death will vary somewhat according to the objects in view. These objects may be threefold: (1) To ascertain whether a person has died from violence or poison; (2) to establish the cause of death, especially if it has been sudden; and (3) to ascertain the lesion of a disease, or to confirm a diagnosis.
The only difference between a medico-legal and pathological autopsy is that in the former case everything which might subserve the ends of justice should be carefully noted, and the changes found most accurately described; especially any abnormalities found on the external examination of the body. A photograph should be taken of the body.
The head should be opened and the brain examined first, and not last, as is often done in the ordinary autopsy.
Careful notes should be taken during each step of the examination, to be reread, verified, and signed at the completion of the autopsy.
It must be remembered that most of the lesions of disease which are found, indicate the disease rather than the cause of death; that often the lesion found will seem hardly extensive enough to cause death, and that from accidents and injuries apparently trivial, death may result. It must often be acknowledged that no sufficient cause of death can be found, but the more accurate and careful the examinations (especially when a microscopical examination of the organs is made) the fewer will be the number of such cases. If no apparent lesion is found, it must not be forgotten that many poisons destroy life and leave no trace that the pathologist can discover.
Care should always be exercised not to mistake the ordinary post-mortem appearance which we find at autopsies for the lesions of disease.
The examination of the human body, whether it be made from a medico-legal or pathological standpoint, is divided into two main divisions:
(1) The external examination, and
(2) The internal examination.
EXTERNAL EXAMINATION.
Its minuteness will depend on the character of the case, as when the person is unknown, or when suspected to have died from unnatural causes. In such cases the external examination is very important.
The following are the steps to be followed:
(1) Give a general description of the body; apparent age, height, and weight of the individual; color of the hair and eyes; condition of the teeth; and the evidence of any personal peculiarities or abnormalities.
(2) Note the color of the skin and observe whether there are any spots of CADAVERIC LIVIDITY, and if present where situated.
(3) Contusions.—Note whether there are any contusions, and, if present, their character, situation, length, breadth, and depth should be described, and whether they are accompanied by inflammation or by the evidences of gangrene.
It is often important to determine whether a contusion has been inflicted before or after death. This is to be done by cutting into the ecchymoses and if the extravasated blood or the coloring matter of the blood is found free in the tissues, one can be almost certain that it is an ante-mortem injury. In post-mortem discolorations the blood is found in the congested vessels. The situation of ante-mortem contusions will not generally correspond to the discolorations produced by decomposition; the latter being confined to the most dependent parts. It should be remembered that the contusions produced by blows on a body dead only a few hours cannot be distinguished from those which were received during life; and also that putrefactive changes make it well-nigh impossible to distinguish between ante-mortem and post-mortem injuries. It should also be borne in mind that blows or falls sufficient to fracture bones or rupture organs may leave no mark on the skin (see Wounds, Vol. I., pp. 467, 474, et seq.).
(4) Wounds.—The situation, depth, extent, and direction of any wound should be recorded, as also the condition of its edges; the changes in the surrounding tissues, and whether inflicted by a cutting, pointed, or rounded instrument; or by a bullet. In the latter case the course and direction of the ball should be[359] ascertained by dissection rather than by the use of the probe, and the character of foreign bodies, if any are found in the wound, should be noted. What nerves or blood-vessels, particularly arteries, have been injured, should be ascertained. It is often important to determine whether a wound was made before or after death. The following may serve as a differential point: In all wounds made after death there is slight bleeding, non-contraction of the edges, and absence of blood in the tissues. This is the opposite of ante-mortem wounds. Again, wounds inflicted within two hours after death cannot be differentiated from those made during life (see Gunshot Wounds, Vol. I., p. 610 et seq.; Wounds, Vol. I., p. 476 et seq.).
(5) Fractures.—If there are any evidences of fractures, the situation of the bones involved should be noted, and whether they are accompanied by contusions of the soft parts. Fractures which are inflicted during life are always accompanied by much more extravasation of blood, more injury to the soft parts, and more evidences of reaction than those occurring after death. It is a well-known fact that it is much more difficult to produce a fracture in a dead than a living body (see Wounds, Vol. II., p. 482 et seq.).
(6) The temperature of the body should be taken.
(7) The rigidity and flexibility of the extremities should be ascertained.
(8) The state of the eyes should be noticed, and the relative size of the pupils.
(9) Attention should be paid to the condition of the cavities of the mouth and nose. The neck should be specially examined for marks of external injury, or signs of ecchymosis or compression.
(10) Genitals.—The external genitals should be very carefully examined for evidence of injury, the presence of syphilitic lesions, and in the female the condition of the vagina should be particularly ascertained.
(11) Œdema of the Feet.—If there is evidence of œdema in any part of the body, especially about the ankles, its situation and extent should be noted.
(12) Ulcers and Abscesses.—The situation and extent of any ulcer found on the body should be recorded, as also the presence and situation of any abscess.
(13) Burns.—The extent of a burn, as also the state of the parts involved, should be noted. For example, whether they are inflamed or show blisters, etc. (see Heat and Cold, Vol. I., p. 647 et seq.).
(14) Hands.—In medico-legal cases the hands of a dead person should always be examined for the presence of cuts, excoriations, or foreign substances found upon them; especially should the dorsal extremities be examined. This examination will often indicate that there has been a mortal struggle before death. The impression of a hand or of some of the fingers is often found on the skin of a dead body. The exact situation where found should be noted. This may be of importance, as when it occurs where it would have been impossible or improbable for the deceased to have caused it.
For appearances in death from lightning or electricity, see Vol. I., p. 701 et seq., and in death from hanging, strangulation, and garroting, see Vol. I., pp. 713, 746, 781, et seq.
INTERNAL EXAMINATION.
Having completed the examination of the external parts of the body, the next proceeding is to open the body and make an internal examination.
This should be done by following a regular method, so as to examine the relations of parts and not to injure one organ while removing another.
In opening the various organs an incision should be made which will expose the greatest amount of surface at one cut. Never make a number of small and always unsatisfactory incisions in an organ. In opening certain organs like the brain and heart, the incisions are so planned that the parts of the organ may be folded together, and, if necessary, their relations to one another and the whole organ studied. Such organs are opened as one would open a book to examine its pages.
It is important to remember that after death the blood leaves the arteries and left side of the heart, and collects in the veins and the right cavities of the heart. Especially does it collect in the vessels of the most dependent portions of the body and of the various organs, so that local congestions may often disappear after death; and again, they may be found at an[361] autopsy where they were not present during life. Especially is this true of the mucous membranes such as those of the trachea and bronchi, and also of the blood in the sinuses of the dura mater.
In making autopsies it is a cardinal rule that all the cavities of the body should be examined, and not alone the one where one might expect to find a lesion. At medico-legal autopsies, the great cavities—the head, the thorax, and the abdomen—should be examined in their successive order from above downward. The reason for beginning with the head is that the amount of blood in the brain and its membranes may be determined accurately; for, if the heart and great vessels of the neck are opened first, the blood will drain away from the brain and local congestions disappear. In pathological autopsies, the opening of the head first is not so important, and often the vertebral column need not be opened at all, for it is a complicated process and takes time; but in medico-legal cases, especially where a question as to the cause of death may arise, and has not satisfactorily been determined, after all the other cavities are examined the vertebral column should always be opened and the cord removed.
The Head.
Make an incision across the vertex of the skull from ear to ear. Dissect the anterior flap forward until within about three inches of the bridge of the nose, and the posterior flap backward to the external occipital protuberance. Examine the internal surface of the scalp for ecchymosis and evidences of injury. A circular incision is then made with a saw through the cranium as far backward and forward as the flaps have been reflected. An incision through the temporal muscle is necessary so that the teeth of the saw may not become clogged by the muscle fibres. When the cranium has been sawed through, a stout hook is inserted under its upper edge and it is removed with a quick jerk. If the dura mater is very adherent to the calvaria, it may be necessary to remove it with the bone, by cutting through it at the level of the cranial incision. Examine the calvaria as also the other bones of the skull after the brain has been removed and the dura stripped off, for evidence of fracture.
Note the symmetry, thickness, and density of the cranial bone, and remember that depressions along the sagittal suture are for the Pacchionian bodies, and are not pathological.
Dura Mater.—The dura mater may be slightly adherent to the bone of the cranium. This is especially seen in old people and does not indicate disease. The Pacchionian bodies are seen along the longitudinal sinus. Examine the internal surface of the dura mater for the presence of clots, tumors, or inflammatory lesions. Open the longitudinal sinus and examine for thrombi. Remove the dura mater by an incision following the cranial incision, the falx cerebri between the anterior lobes being drawn back and divided. Note whether the dura mater is adherent to the pia mater, and the condition of its internal surface.
Pia Mater.—The brain, covered by the pia mater, is now exposed. Note the degree of congestion of the membrane, its adherence, and the existence of pus, blood, or serum on its surface or in its meshes. Remember that a considerable amount of serum may be present within normal limits, especially in cachectic subjects, without indicating disease, but when the serum is so extensive as to raise the pia mater and to depress the convolutions, we have a pathological amount which may be a simple dropsy due to some general cause, or the result of a chronic meningitis. Enough serous effusion in the pia mater to produce a condition which has been called by some writers “serous apoplexy,” I believe never occurs as a primary condition.
Loss of transparency and thickening of the pia mater, especially along the longitudinal fissure, is often seen in old people and does not indicate disease.
Brain.—Remove the brain by raising the anterior lobes with the fingers of the left hand and cutting through the nerves, vessels, and the tentorium as they appear. The medulla is cut as low down as possible, and the brain as it rolls out is caught in the left hand.
After being placed on a clean board or in a large clean dish, it is minutely examined. The average weight of an adult male brain is forty-nine and one-half ounces; of the female, forty-four ounces. Its proportional weight to that of the rest of the body is as 1 to 45.
Lay the brain first upon its convex surface and examine the arteries at the base for atheroma, thrombi, emboli, and aneurisms. Examine the pia mater of the base, especially for the evidences of hemorrhage, tumors, tubercles, and inflammatory lesions. Next turn the brain over on its base, and proceed to open its various cavities and examine its internal structure. Separate the two halves of the cerebrum, until the corpus callosum is exposed. Make an incision downward and outward at the junction of the corpus callosum with the cerebrum, and the roof of the lateral ventricles will be cut through and their cavities exposed. Prolong the incision forward and backward so as to expose the cornua. The size and contents of the ventricles should be noted, as also the condition of the ependyma. The floor of the lateral ventricles being the most frequent spot of hemorrhage, if one is found its extent and the parts involved by it should be noted; especially its relation to the internal capsule.
Transverse incisions (about one-sixteenth of an inch apart) are made through the ganglia seen on the floor of the lateral ventricles. Thus any lesions in the substance of the ganglia will be disclosed. Three or four longitudinal incisions are now made outward into the hemispheres nearly to the pia mater. These will divide the hemispheres into long, prism-shaped pieces held together by the pia mater and a little of the cortex, thus enabling the brain afterward to be folded together, and the relations of lesions to the brain as a whole studied. The third ventricle is now examined by cutting through the fornix and corpus callosum at the foramen of Monroe. Next, the fourth ventricle is opened by a longitudinal incision through the lower portion of the vermiform process; its contents, the condition of its vessels and ependyma noted. Then the floor of the fourth ventricle is divided by transverse incisions one-sixteenth of an inch apart, and careful examination made for the presence of minute hemorrhages: for here is a place in the body where almost a microscopical lesion (hemorrhage) may cause sudden death. Each hemisphere of the cerebellum is now opened by a number of incisions starting from the fourth ventricle and passing outward into its substance. The presence of any tumors or hemorrhage in the cerebellum will now be recognized.
In opening the brain, when clots, areas of softening, tumors,[364] etc., are discovered, their exact location in relation to surrounding parts should be noted and the blood-vessels examined for areas of degeneration or aneurism. This examination can be facilitated by allowing a stream of water to flow over the affected part. This will wash out the affected area and allow the vessels to appear.
Eye.—In rare cases it may be necessary to remove the eye. This can be done by breaking through the roof of the orbit with a saw or chisel and dissecting away the muscles so as to expose the optic nerve and the posterior portion of the organ.
Thorax and Abdomen.
The body being placed on its back, and the operator standing on the right side, an incision is made through the skin, fascia, and muscles from the top of the sternum to the pubic bone, passing to the left of the umbilicus and dividing everything down to the sternum and the subperitoneal tissue. A small incision is now made through the peritoneum below the ensiform cartilage. Into this opening two fingers of the left hand are inserted, and by spreading the fingers and holding the knife horizontally the peritoneum can be divided to the pubes without injuring the intestines. The skin and muscles are now dissected from the chest as far back as the false ribs. This dissection may be facilitated by keeping the skin and muscles on the stretch and cutting with the flat part of the knife. In order to better expose the abdominal cavity, the recti muscles are divided beneath the skin at their insertion in the pubic bone. Examine the cut surface of the chest and abdominal muscles, and note their color, amount, and consistency. Observe whether the chest muscles show the evidence of any parasitic disease such as trichinosis. The mammary glands are now examined from behind and opened if necessary.
Superficial Examination of Abdominal Cavity.—This should be done before opening the chest cavity, because the position of organs may become modified, and blood and other fluids are liable to find their way from one cavity into another; and again, the blood in the presenting portion of the abdominal organs will change its color after exposure to the air.
Note the Following Points: (a) The relative position and general condition of the abdominal organs.
(b) The color and amount of blood in the presenting parts.
(c) Whether there are any signs of inflammation or the evidence of foreign bodies or tumors.
(d) Examine the vermiform appendix.
(e) The amount of fluid in the abdominal cavity. Normally a small quantity of reddish serum will be found, particularly in warm weather, at the most dependent portion of the abdominal cavity. If the quantity is small it can only be ascertained by raising the intestines from the pelvis. When the fluid is considerable, the exact amount should be ascertained and its character noted.
(f) Perforation, invagination, and hernia of the intestines should be looked for.
(g) Determine the height of the diaphragm. Normally, on the right side, it is at the junction of the fifth rib with the sternum, and on the left it reaches as high as the sixth. A variety of pathological conditions change its position. For instance, it may be raised when the contents of the abdomen are greatly increased in volume, and in new-born children who have never breathed. It may be depressed by enlargement of the lungs, disease of the heart, or fluid in the pleural or pericardial cavities. The presence of air or gas in the pleural cavity can be determined either by filling the abdomen with water and puncturing the diaphragm beneath the fluid so that the air will bubble up, or a puncture may be made through the thorax between the ribs, and the flame of a match will be deflected by the escaping air.
Thorax.
The thorax is opened by cutting the sterno-costal cartilages as close to the end of the ribs as possible, the cut being made downward, outward, and backward, and the knife held obliquely so as not to injure the underlying parts. Quite often the cartilages will be found ossified and it will be necessary to divide them by a costotome. Next, separate the clavicles by a semi-lunar incision at their attachment to the sternum.
Raise the sternum with the left hand and separate it from the underlying parts. If there is any adherence of the sternum a slight twist will be sufficient to remove it.
Superficial Examination of Thorax.—Observe the position, color, and degree of distention of the lungs. It should be remembered that healthy lungs, as soon as the chest is opened, owing to their inherent elasticity, will collapse, and when this normal collapse is not seen it is generally due to a loss of elasticity as occurs in emphysema, to inflammatory diseases binding the lung to the chest wall, or to the alveoli being filled with solid or fluid substances or pent-up air. Most complete distention is seen when death is due to drowning or suffocation.
The area of the heart uncovered will vary according to the degree of collapse of the lungs and to the abnormal size of the heart. Normally the cardiac area exposed is quadrangular in shape, and about three and a half inches in its longest diameter. Examine the pleural cavities for the presence of adhesions, foreign bodies, or fluid. If fluid is found it should be removed, measured, and its character noted. It is to be remembered that in warm weather, or when putrefaction has commenced, a moderate amount of reddish serum is found in the pleural cavities which has no pathological significance. Lastly, examine the mediastinum as to the condition of the thymus gland and great vessels outside the pericardium.
Pericardium.—Open the pericardium by an oblique incision along the anterior wall, and prolong this incision downward and outward toward the diaphragm and upward to its reflection from the great vessels. Normally, about a drachm of clear serum, sometimes, however, blood-stained from decomposition, will be found in the pericardial sac. The amount is best ascertained by raising the heart. Note next the contents of the pericardium and whether there is any serous, fibrous, or purulent exudation. If an abnormal amount of fluid is present, remove, measure, and note its character. Observe whether there are any adhesions between the two surfaces of the pericardium. White patches are often seen on the visceral surface of the pericardium, especially over the ventricles. These have no pathological significance and are due to slight thickenings of the pericardium.
The Heart.—Having passed the hand over the arch of the aorta and noticed whether there is any evidence of aneurism or dilatation, we grasp the heart firmly by the apex, raising and drawing it forward. We remove it by cutting through the[367] vessels at its base. Test the sufficiency of the aortic and pulmonary valves by allowing a stream of water to flow into these vessels, the heart being held in a horizontal position and care being taken not to pull the valves open.
To apply the water test to the mitral and tricuspid valves, the auricles are first opened so as to expose the upper surface of these valves, and by allowing a stream of water to flow through the aortic and pulmonary valves into the cavities of the ventricles, the degree of sufficiency of these valves can readily be ascertained.
Another rough test is what is known as the “finger test.” The mitral valve will normally allow two fingers, held flat and in contact, to pass through its opening. The tricuspid in the same way allows, normally, three fingers to pass; or if a more accurate test of the degree of insufficiency is desired, the valvular orifices should be measured. Normally, the aortic orifice is one inch across; the mitral, one and eight-tenths inches; pulmonary, one and two-tenths inches; and the tricuspid about two inches.
We open first the cavity of the right ventricle by making an incision over its anterior border close to the septum. Prolonging the incision downward to the apex and upward through the pulmonary artery, the cavity of the ventricle will be fully exposed. The left ventricle is similarly opened by an incision through its anterior wall which is prolonged upward through the aortic valve. The cavities of the auricle and ventricle, especially those of the right side, will often contain blood-clots. These clots are usually post-mortem clots formed during the last hours of life or after death. It may sometimes be necessary to distinguish these post-mortem clots from what are known as ante-mortem clots. The latter are usually of firm consistency, dry, of a whitish color, and closely entangled in the trabeculæ, while the former are succulent, moist, of a reddish-yellow color, and are easily detached from the walls of the heart cavities. Ante-mortem clots are rarely seen, and the medical examiner should be careful not to attribute the cause of death to the post-mortem clots which are so often seen. After the heart is opened we can with more care and greater accuracy examine the condition of the valves and recognize the extent of valvular lesions.
The condition of the endocardium should now be examined and any abnormality noted. Often it will be seen stained a deep red color. This is not due to disease, but is caused by the absorption of the coloring matter of the blood which has been set free by decomposition. The size of the heart cavity and the thickness of the heart walls should be noted, as also their consistency and color. It should be remembered that the heart walls may appear unusually flabby as the result of decomposition, or apparently thickened when death occurs in extreme systole. The interior of the heart can be further examined by passing the enterotome into each auricle, carrying the incision through the mitral and tricuspid valves to join at the apex with the previous incision, which has been prolonged through the ventricles to the apex. Thus the auriculo-ventricular valves are completely exposed.
Having removed the blood from the heart it is next weighed. The average normal weight of the human heart is about twelve ounces in the male, and a little less in the female: its size roughly corresponding to the closed hand of the individual. Normally, the thickness of the walls of the left ventricle about its middle is five-eighths to two-thirds of an inch, and of the right ventricle one-eighth to one-quarter of an inch.
Note the condition of the aorta above the heart, whether it is dilated, atheromatous, or shows calcareous deposits. Examine the coronary arteries by opening them with a blunt-pointed scissors. Disease of these vessels with thrombosis is one of the causes of sudden death which is often overlooked.
The Lungs.—The lungs are removed by lifting them from the pleural cavity and cutting through the vessels and bronchi at their base. If a lung is very adherent it is sometimes better to remove the organ with the costal pleura attached so as not to tear the lung substance. Examine the external surface of the lung as to its shape, color, and consistency. Next open the large bronchi with a blunt-pointed scissors, and prolong the incision into the pulmonary substance along the minute bronchi. Observe the contents of the bronchial tubes, the appearance of the mucous membrane, and their relative thickness. Remember that it is very difficult to tell the condition in which the mucous membrane was during life on account of the early post-mortem changes which affect it, and also because the contents of the[369] stomach may have been forced after death up the œsophagus and down the bronchi, giving the tubes a peculiar reddish and gangrenous appearance.
Having examined the bronchi, the lung is turned over and its base grasped firmly in the left hand. An incision is made from apex to base, which will expose at a single cut the greatest extent of pulmonary surface. Note the color of the lung substance, and whether the alveoli contain blood, serum, or inflammatory products. Blood and serum can easily be forced from the lungs by pressure between the fingers, while inflammatory exudations cannot. Examine carefully for the presence of miliary tubercles.
If a question should arise whether a portion of a lung is consolidated, this part can be removed, placed in water, and if the air cells are consolidated the portion will sink; if there is only congestion it will float. By squeezing the lung between the fingers an inflammation of the smaller bronchi (bronchitis) can be recognized by the purulent fluid which will exude at different points. It should be remembered that in normal condition the lower lobes and posterior aspect of the lungs will apparently be very much congested as a result of gravity.
Neck, Larynx, and Œsophagus.—Throw the head well backward, and place a block beneath the neck. Make an incision from the chin to the upper part of the sternum. Dissect the soft parts away on each side from the larynx and thyroid body, then cut along the internal surface of the lower jaw from the symphisis to its angle. Through this incision introduce the fingers into the mouth, and grasp and draw down the tongue. By dividing the posterior wall of the pharynx and pulling downward these parts, the trachea and œsophagus can readily be removed together, a ligature having been first placed around the lower portion of the œsophagus. Open now the pharynx and œsophagus along their posterior border. Examine the mucous membrane carefully for the evidences of inflammation, caustic poison, tumors, foreign bodies, or strictures. With an enterotome open the larynx and trachea along their posterior wall. Observe if there is any evidence of œdema of the glottis, and note the condition of the mucous membrane. Remember that redness of the larynx is very commonly the result of post-mortem changes and is also seen in bodies which have been kept cold. Dissect off and examine the thyroid gland.
Abdomen.
Having completed the examination of the organs of the thorax, we next proceed to examine those contained in the abdominal cavity. We first raise and,dissect off the omentum, noting if it is abnormally adherent.
The first organs to be removed are:
The Kidneys.—Drawing the intestines aside we cut through the peritoneum over the kidneys, and introducing our left hand we grasp the organs with their suprarenal capsules attached. Raising first one kidney and then the other, we easily divide the vessels and the ureters as close to the bladder as possible. The kidneys are often found imbedded in a mass of fat which must first be removed. Their surface is sometimes of a greenish color owing to the beginning of putrefaction. We note the size of the organ, its color and weight. A normal kidney weighs from four and one-half to five ounces. Grasping the kidney firmly in the left hand, we make an incision in its capsule along its convex border, and with a forceps strip off the capsule and note its degree of adherence and the condition of the surface of the organ; whether it is smooth or granular. Prolonging our incision already made through the cortex of the organ, inward toward the pelvis, we divide the organ into two halves and now closely examine the internal structure. The average thickness of the cortex, which should be about one-third of an inch, is noted; as also its degree of congestion, and whether the normal light (tubes) and reddish (vessels and tufts) lines are seen running through it. If these alternate light and dark markings are lost and the organ has not undergone decomposition, the presence of some of the forms of Bright’s disease may be suspected. If the cut surface of the organ presents a waxy appearance, the amyloid test should be applied by first washing the cut surface of the organ and dropping upon it a few drops of Lugol’s solution of iodine, when the amyloid areas will appear as dark mahogany spots on a yellow background.
The pelvis of the kidneys should be examined for calculi and the evidence of inflammatory lesions. The suprarenal capsules readily decompose, but if the autopsy is not made too late[371] hypertrophy, tuberculosis, tumors, and degeneration in them may be recognized.
The Spleen.—This organ will be found in an oblique position at the left side of the stomach. Grasping it firmly in the left hand and drawing it forward, it can easily be detached. Normally in the adult it is about five inches in length by three inches in breadth by one inch in thickness, and weighs about seven ounces. The size, color, and consistency of the organ should be noted, as well as abnormal thickenings of its capsule and the presence of any tubercles or tumors in its substance. The spleen softens very early as the result of decomposition, and this decomposition should not be mistaken for a pathological condition.
The Intestines.—In cases of suspected poisoning the greatest care should be taken in the removal of the intestines and the stomach. Double ligatures should be placed in the following situations so as to preserve the contents of the organs intact: (1) at the end of the duodenum; (2) at the end of the ilium; and (3) at the lower portion of the rectum; and an incision should be made with a pair of scissors between these ligatures. The jejunum and ilium should first be removed together by seizing the gut with the left hand, keeping it on the stretch, and cutting with a pair of scissors through the mesentery close to its intestinal attachment. The cæcum, colon, and rectum should then be removed in a similar manner.
The intestines being placed in large absolutely clean dishes, which have previously been rinsed with distilled water, are opened; great care being taken that none of the intestinal contents are lost. The small intestines should be opened in one dish and the large intestine in another. A portion of the intestines where morbid appearances are most likely to be seen in cases of poisoning are the duodenum, the lower part of the ilium, and the rectum. The comparative intensity of the appearances of irritation should be especially noted. For example, if the stomach appears normal and the intestines are found inflamed the possibility of poison from an irritant may be denied.
The intestines are opened along their detached border by the enterotome. Care should be taken to distinguish the post-mortem discolorations which are usually seen along the intestines[372] from those produced by disease. The former are most marked in the dependent portions. They are apt to occur in patches which can be readily recognized by stretching the wall of the gut. The darkish brown or purple discolorations which are sometimes seen as the result of decomposition are due to the imbibition from the vessels of decomposed hæmoglobin. Much care and experience are necessary to tell the amount of congestion which is within normal limits and to recognize changes of color produced by decomposition.
The pathological lesions ordinarily looked for in the examination of the intestines are ulcers, perforation, hemorrhages, strictures, tumors, and the evidences of various inflammations. To obtain an accurate idea of the various portions of the mucous membrane of the intestines, it is sometimes necessary to remove their contents. When very adherent this should be done by allowing as small a portion of distilled water as possible to flow over their surface. If any abnormalities are noticed along the intestinal tract, an accurate description should be given of their situation and extent; as also the amount of congestion seen in different portions of the intestinal tract.
If possible the different portions of the intestines, as well as the stomach, should be examined immediately after being exposed to view, as under the influence of the air those parts which are pale may become red, and slight redness may become very pronounced. In this way only can we estimate the degree of vascularity of the various parts after death. However, in cases of suspected poisoning, when it is impossible for the chemist to be present at the autopsy, the medical examiner should not open the stomach and intestines, but place them in sealed jars. As soon as possible afterward, the chemist being present, they should then be examined in the manner indicated. What may be lost by waiting, in changes of color which have taken place, will be more than counterbalanced by the data which the chemist will obtain from observing the contents and mucous membrane of the stomach and intestines when they are first exposed. The characteristic odors of certain poisons are so evanescent that they quickly disappear after opening of the stomach and intestines.
After a thorough examination of the intestines, they are to be put with their contents into wide-mouthed vessels, each[373] part by itself, and the basins in which they were opened washed with distilled water and the washings put into the same bottle. As soon as the intestines are transferred to the jars they should be sealed.
The Stomach.—The stomach and duodenum are removed together. They are opened by passing the enterotome into the duodenum and dividing it along its convex border, the incision being continued along the greater curvature of the stomach as far as the œsophageal opening. They should be opened in a large glass dish which has been carefully washed with distilled water. The chemist and medical examiner will carefully note the quantity, odor, color, and reaction of the stomach contents; also whether luminous or not in the dark; the presence or absence of crystalline matter, foreign substances, undigested food or alcohol.
Portions of the contents should be placed in a small glass bottle and sealed, so that at a future time they may be examined microscopically. Only in this way can an absolute knowledge of the character of the stomach contents be obtained. In certain medico-legal cases the ability to decide the character of the stomach contents is of the utmost importance. The mucous membranes of the stomach and duodenum must be next carefully examined for evidences of hemorrhages, erosions, tumors, and of acute or chronic inflammations. The appearance of the rugæ and their interspaces, principally in the region of the greater curvature, should be noted; because here traces of poison and its effects are most frequently seen. If the stomach is inflamed, the seat of the inflammation should be exactly specified, as also that of any unusual coloration.
The condition of the blood-vessels are also noted. Vascularity or redness of the stomach after death should not be confounded with the effects of poison or the marks of disease. It may occur in every variety of degree or character and still be within normal limits. Vascularities which we might call normal are seen in the posterior part of the greater end and in the lesser curvature, and may cover spaces of various extent. Rigot and Trosseau have proven by experiment that various kinds of pseudo-morbid redness may be formed which cannot be distinguished from the varieties caused by inflammation; that these appearances are produced after death and often not[374] until five or eight hours afterward, and that they may be made to shift their place and appear where the organ was previously healthy, merely by altering the position of the stomach. Ulcers, or perforations of the stomach as the results of disease, as also the digestion of the stomach after death, have been mistaken for the effects of irritant poisons.
When perforation of the stomach is the result of caustic poisons, the edges of the opening are very irregular, and are of the same thickness as the rest of the organ. The parts not perforated are more or less inflamed, and traces of the action of the caustic are found in the mouth, pharynx, and œsophagus. This is the opposite condition to that seen in spontaneous perforation.
In considering perforation of the stomach the following points given by Taylor are well to remember:
(1) A person may have died from perforation of the stomach and not from poisoning.
(2) A person laboring under disease may be the subject of poison.
(3) A person laboring under disease may have received blows or injuries on the abdomen, and it will be necessary to state whether the perforation did or did not result from the violence.
(4) The perforation of the stomach from post-mortem changes may be mistaken for perforations from poison.
Corrosives, if they do not produce perforation of stomach, will generally cause intense inflammation accompanied by softening of the inner coat, sometimes ending in gangrene. The inflammation varies as to its extent and intensity, sometimes affecting principally the mouth and œsophagus, but generally the changes are more pronounced in the stomach and duodenum, while in rare cases the inflammatory process may extend through the whole alimentary canal. The mucous membranes are sometimes bright red with longitudinal or transverse patches of a blackish color, formed by extravasated blood between the coats. Carbolic acid often produces in the stomach and œsophagus white patches—when these patches are carefully examined, an ulcerated surface beneath them is generally seen.
Narcotic Poisons.—It is a common but mistaken idea that these poisons produce some mark or characteristic effect upon the stomach walls; that they induce a rapid tendency to putrefaction;[375] that the blood is in a fluid state; that hemorrhages are seen in various parts; that the stomach and intestines show sloughing without any inflammation. Some of these conditions may and probably do occur, but they are far from being invariable in their appearance. Experiments made by Orfila on animals with narcotic poisons prove the above statement. In conclusion, I would emphasize the fact that the narcotic poisons produce no characteristic changes in the stomach that can be detected.
The Liver.—The liver should be removed from the body and no attempt made to examine the organ in situ. After raising first one lobe and then the other, the diaphragm should be cut on either side and the suspensory and lateral ligaments divided, then the organ can easily be removed. The weight of the organ is ascertained, as also the measurements of its size recorded. The normal weight is from fifty to sixty ounces. The organ is normally about twelve inches in length by seven inches in depth by three and one-half inches in thickness.
The gall bladder is first examined to determine the character and amount of the bile and the presence or absence of gall stones, inflammatory lesions, and tumors.
At autopsies the surface of the liver, especially along the free border, is generally seen to be of a greenish or dark-brown color. This discoloration is due to the action of the gases developed by decomposition on the coloring matter of the blood, and has no pathological significance. The character of the surface of the liver is now noted, whether smooth or rough. The organ is opened by deep incisions in various directions, and the color, consistency, and blood supply of the liver tissue carefully recorded. The presence of new connective tissue, amyloid degeneration, abscesses, or tumors should not be overlooked. It should be remembered that, of all the poisons, phosphorus alone leaves characteristic appearances in the liver.
The Pancreas.—The pancreas is now easily removed, and its size and weight recorded. Normally it should weigh three ounces and measure eight inches in length by one and one-half inches in breadth by one inch in thickness. The organ should be opened by a longitudinal cut and examined for evidences of acute or chronic inflammation, fat-necrosis, tumors, calculi, and amyloid degeneration.
Genito-Urinary Organs.—It is very important in medico-legal cases that all the urine should be preserved and obtained uncontaminated; therefore before the bladder is opened a catheter should be introduced and the urine drawn off into a clean bottle which has previously been rinsed with distilled water. If more convenient the bladder itself can be punctured at its upper portion, a pipette introduced, and the urine drawn off in this manner.
The genito-urinary organs are removed together. This is done in the following manner. The body of the penis is pushed backward within the skin and cut off just behind the glans penis; the remaining portion of the rectum is raised. This with the prostate gland, bladder, and penis attached is removed by carrying the knife around the pelvis close to the bone and separating the pubic attachments. The organs are then laid on a clean board and the urethra is opened on a grooved director passed into the bladder, and the incision prolonged so that the internal surface of the bladder itself will be completely exposed. Examine the urethra for strictures, inflammatory lesions, and ulcers. Examine the bladder for congestion, hemorrhages, inflammation, and ulcers of its mucous surface, and note the thickness of its walls. Open the rectum and examine for ulcers, strictures, tumors, and the evidence of hemorrhage. The prostate gland is opened by a number of incisions into its substance. Examine for hypertrophies, tumors, and inflammatory lesions. Force the testicles through the inguinal canal, and cut them off. Weigh, open, and examine them for evidence of inflammation, tuberculosis, and tumors.
Female Organs.—Before removing these organs, any abnormalities such as adhesions, malpositions, and tumors should be noted. Dissect the organs away from the pelvic bones by carrying the point of the knife around the pelvis close to the bone. Cut through the vagina at its lower third, and the rectum just above the anus. The organs can now readily be removed. Examine the vulva for ulcers, hypertrophies, and tumors. Open and examine the bladder. Open the vagina along its anterior border and carefully examine its mucous surface for evidences of inflammation.
The Uterus.—Before opening the uterus, its size and shape should be recorded. The average normal weight of the organ[377] is about one and one-quarter ounces; its length three inches, breadth two inches, and thickness one inch. Open the organ along its anterior surface by a blunt-pointed scissors passed through the cervix, and the incision carried as far as the fundus. Note the thickness of its walls and any abnormalities of its mucous membrane. During menstruation, the mucous membrane of the body is thickened, softened, and covered with blood and detritus. Retention cysts are found in the mucous membrane of the cervix and are not generally of pathological significance.
Remove, measure, and weigh the ovaries. Their normal weight is about one drachm each; their size, one and one-half, by three-quarters, by one-half inch. Open the organs by a single incision and examine for the evidences of acute and chronic inflammations, tumors, and cysts. The corpora lutea in various stages can be easily recognized in the substance of the organ. Open the Fallopian tubes and examine their contents and the condition of their membranes (see Disputed Pregnancy and Delivery, Vol. II.).
The Spinal Cord.
To remove the cord, the body should be placed on its face with a block beneath the thorax. An incision is made through the skin and muscles along the entire length of the vertebral column and the soft parts dissected away so as to expose the transverse process of the vertebræ. The lamina are divided with a saw through the articulate process (a double-bladed saw specially adapted for this work can be obtained). After the lamina have been completely severed, these together with the spinous process can now be readily torn away with a stout hook and the cord exposed. A long chisel with a wooden mallet will often greatly facilitate this work. Great care should be exercised not to injure the cord. The roots of the spinal nerves are now severed, and the cord removed within its membrane. It should be remembered that serous fluid within the membranes of the cord, as also intense congestion, especially along its posterior aspect, is often seen as the result of post-mortem change. The cord is laid on a clean board and the dura mater opened with a blunt-pointed scissors along its anterior aspect, and an examination made for the presence of hemorrhage, inflammatory[378] lesions, and tumors. Softening of the cord can generally be detected by the finger passed along it. This, however, is not a perfectly accurate test, especially if the body has been dead some time. The cord is now cut by transverse incisions about half an inch apart throughout its entire length, and the cut surface examined for the evidences of disease such as hemorrhages, softening, and inflammatory lesions.
After the cord has been removed, examine the vertebral column for the evidences of fractures and displacements.
LATE AUTOPSIES.
Late autopsies are those performed after partial or complete destruction of the soft parts of the body, through the natural processes of decomposition, or the examination of bones exhumed long after interment. The term may be employed also to mean the inspection of an embalmed body, dead for some time.
The object of late autopsies is to determine identity, or to establish the guilt or innocence of suspected persons. An examination of the skeleton even many years after death may give important information as to the manner in which the deceased came to his end. This cannot better be illustrated than by the citation of one or two cases.
In the celebrated case of “Eugene Aram,” the bones of his victim were discovered thirteen years after the crime had been committed. A man who afterward proved to be Aram’s accomplice was arrested on suspicion. He confessed the crime, and the opinion formed by the medical witnesses was confirmed by his statements. The skull presented evidence of fracture and indentation of a temporal bone. Aram argued the case in his own behalf, but the testimony was too strong against him: he was convicted and executed.
Taylor records the case of a man, Guerin, who was convicted of the murder of his brother from evidence obtained from an examination of the skeleton three years after interment. Here, again, blows upon the head were the cause of death, and the fractures were plainly perceptible upon the exhumed skull.
An autopsy upon a body before the soft parts have been[379] entirely destroyed, or upon an embalmed body, should be conducted in much the same manner as ordinary autopsies. In these cases the method of burial should be noted. If it be a case of murder, and the body has been hurriedly put into the ground, it is not likely that the custom of Christian nations has been observed—that of laying the body full length, with the head to the west.
In the case of partially destroyed bodies, the remaining soft parts will give little evidence of the mode of death unless the violence has been very extensive, and even then it may be impossible to determine whether a wound was inflicted prior to or after death. Recourse must be had to the skeleton, and the only evidence it can furnish is of fractures, unless, as happened in one case, a rope be found about the cervical vertebræ.
When the skeleton only is found, Taylor lays stress upon the following points:
(1) Whether the bones belong to a human being or one of the lower animals.
(2) If a human being, whether male or female.
(3) The length of time they have probably remained in the ground.
(4) The probable age of the individual to whom they belonged. If the maxillary bones be found, much information may be obtained from an examination of the teeth.
(5) The probable stature of the individual during life.
(6) The race to which he belonged. The conformation of the skull and thickness of the bones will give important information on this point.
(7) It should be determined whether solitary bones belong to the right or left side, and whether they form parts of one or more than one skeleton.
(8) Whether they have been fractured, and if so, whether it occurred during life, or by accident at the time of the exhumation. If it occurred during life, whether it be recent or of long standing.
(9) The presence or absence of personal deformities, of supernumerary fingers or toes, of curvature of the spine, of ankylosis of one or more joints.
(10) Whether they have been calcined, as murderers sometimes try to make away with the bodies of their victims by[380] burning. Especially is this the case in infanticides (see Identity, Vol. I., p. 408 et seq.; Time of Death, Vol. I., p. 452 et seq.).
AUTOPSIES OF FRAGMENTS.
These cases are usually cases of murder in the perpetration of which the criminal has mutilated the body with a view to destroying all traces of identity.
The importance which attaches to autopsies of fragments rests upon the fact that parts of a body may be found widely separated, and that one portion may be found before the others. In such cases it will be necessary to determine if they belong to one and the same body. The examination is conducted chiefly with a view to establishing this.
The examiner must note the manner in which the fragment has been separated; whether it is clean cut, as by one who understood something of anatomy, or, whether it has been separated roughly and by one ignorant of the body structure. The determination of this point will be one link in the chain of evidence which may lead to the detection of the criminal, or the acquittal of one accused. An anatomist or a butcher would be likely to cut through at a joint, and to do it neatly. The exact point at which the severance has taken place should be noted. The place of finding, the circumstances under which found, the condition and general appearance of the fragment should all be carefully recorded. The color of the skin will indicate with some accuracy the race to which the individual belonged. The probable sex may be determined by the presence or absence of hair, and the general conformation. This, however, will not apply in the case of children. The probable age may be fixed upon from the size and degree of development of the fragment. The cut surface should be carefully described, and if possible a drawing should be made of it.
There are special considerations which apply to certain parts of the body.
The Head.—The exact point of severance should be recorded. The number of vertebræ which remain attached to the head should be counted, and if the section pass through a vertebra, its number and the amount of it missing should be stated. The sex will be apparent in all instances; the race may[381] be determined both by the color of the skin and by the shape of the head; the age may be approximated, though care must be had in expressing an opinion, for the manner of living is well known to affect the appearance of age. Evidence of violence prior to death should be noted, and the presence or absence of fractures ascertained; also observe the color of the hair and whether it be thin or abundant; the presence or absence of beard or mustache, and if present the color; and the color of the eyes.
The Arm.—The following points should be determined: the color of the skin as indication of race; the probable sex from its shape and general conformation; the probable age from its size and degree of development; marks of any kind, such as tattooing; and deformities, such as signs of old or recent fracture, or dislocation; and supernumerary fingers.
The Leg.—The examination of the leg should be conducted in much the same manner as that of the arm.
The Trunk.—An examination of the trunk will reveal the race, sex, and probable age, and may give evidence as regards the manner in which the deceased came to his or her death. Any marks or deformities should be recorded, and in all cases the viscera should be examined.
MEDICO-LEGAL REPORTS.[568]
After making a medico-legal autopsy, it will be necessary for the medical examiner to draw up a report of his findings, and the conclusions based thereon. The report should be clear and concise, and the language such as a coroner’s jury can understand. Technical terms should be avoided, and when their employment is necessary they should be explained in the margin or in parentheses.
The report should be drawn up in somewhat the following manner:
1. When and under what circumstances the body was first seen; stating hour of day, day of week and month.
2. When deceased was last seen living, or known to be alive.
3. Any circumstances that would lead to a suspicion of suicide or murder.
4. Time after death at which the examination was made, if it can be ascertained.
5. The external appearance of the body: whether the surface is livid or pallid.
6. State of countenance.
7. Any marks of violence on the person, disarrangement of the dress, blood-stains, etc.
8. Presence or absence of warmth in the legs, abdomen, arms, armpits, or mouth.
9. Presence or absence of rigor mortis.
To give any value to this point it is necessary for the witness to observe the nature of the substance upon which the body is lying; whether the body be clothed or naked, young or old, fat or emaciated. These conditions materially influence the rapidity of cooling and the onset of rigor mortis.
10. Upon first opening the body the color of the muscles should be noted. Carbon monoxide poisoning causes them to be of a cherry-red color.
11. The condition of the blood and its color.
12. The state of the abdominal viscera, describing each one in the order in which it is removed (see p. 370). If the stomach and intestines are inflamed the seat of the inflammation should be exactly specified; also all evidences of softening, ulceration, effusion of blood, corrosion, or perforation. The presence of hardened fæces in the rectum will bear evidence that no purging occurred immediately before death.
13. The state of the heart and lungs. (For special consideration of the lungs in cases of suspected infanticide, see Vol. II.; and of persons drowned, see Vol. I., p. 805 et seq.).
14. The state of the brain and spinal cord.
After a thorough consideration of the results of the examination, conclusions must be drawn from this examination; never from the statements of others. The conclusions commonly relate to whether death was due to natural or unnatural causes; if to unnatural causes, what are the facts which lead the examiner to this opinion. As the conclusions are intended to form a summary of the whole report, they must be brief and tersely stated.
PERSONAL IDENTITY,
INCLUDING
THE METHODS USED FOR ITS DETERMINATION IN THE DEAD AND LIVING.
BY
IRVING C. ROSSE, A.M., M.D., F.R.G.S. (Eng.),
Professor of Nervous Diseases, Georgetown University; Membre du
Congrès International d’Anthropologie Criminelle, etc.
PERSONAL IDENTITY.
GENERAL CONSIDERATIONS.
Identity is the determination of the individuality of a person. In jurisprudence the term is applied to the recognition of a person who is the object of a judicial action. The establishment of the individuality of a person is known as absolute identity; while the relations of a person with some particular act is known as relative identity.
The great number and variety of facts concerned in the investigation of questions of identity are of considerable gravity and importance in their juridical bearing, and at the same time they are among the most interesting and most useful of the applications of modern medicine to the purposes of the law.[569]
Among the varied researches of legal medicine looking to an interpretation of facts, no other question occurs in which the solution depends more upon morphological and anatomical knowledge, and none is more dependent upon purely objective, visible, tangible facts.
Personal identity often constitutes the entire subject-matter of dispute in a civil case. Upon it may depend the question of absence or of marriage, of kinship or of filiation involving the possession of an estate, in which case the court often requires the most subtle of scientific evidence to assist in its decision. Many anthropological and medical facts, now appropriated by criminology and penal science, are useful in proving not only the present but in attesting future identity, thereby preventing in great measure the dissimulation of prisoners, deserters, false claimants to life insurance, fraudulent pensioners, and the like.
Such matters are of daily occurrence. The special agents of the U. S. Pension Office detect and cause the punishment of[386] many fraudulent claimants. Stratagems and conspiracies to defraud life-insurance companies go much further than mere substitution. Instead of a “fraudulent” a positive death may come up for investigation, and in order to defraud an insurance company of a large amount, a body may even be procured by homicide to consummate the deception, as was done in the Goss-Udderzook tragedy near Baltimore in 1872.
A celebrated case now before the Supreme Court of the United States and involving the question of personal identity is that of the Mutual Life Insurance Company of New York, the New York Life Insurance Company, and the Connecticut Mutual Life Insurance Company of Hartford, Connecticut (Consolidated), plaintiffs in error, vs. Sallie E. Hillmon.
It is pre-eminently in criminal trials that the personal identity of the victim often constitutes an essential connecting link. Before it can move, the law requires, at the outset, proof of the individuality of both the author of a crime and of the victim. I shall, therefore, not touch upon such elusive individuals as Charlie Ross and Jack the Ripper, but limit my remarks to a synthetical exposition of the best-known facts regarding identification of the dead body and the interpretation of its organic remains.
The identity of a living person, or even our own identity, is often a difficult point to establish. It may also require medical evidence, oftentimes of a most involved character, to establish the fact of death. Hence the medico-legal process of connecting a dead body, or the remains or traces of the same, with a human being once known to have lived and moved on earth, is beset with difficulties that may give rise to still greater antagonisms of evidence. The question of personal identity is one of the hardest that could possibly come before a court. Celebrated cases and judicial errors have given it great notoriety. There are consequently few questions in forensic medicine that require more attention and sagacity, and none upon which the medical legist should pronounce with more reserve and circumspection. Medical men are absolutely the only persons qualified to assist in resolving the really delicate question of personal identity; yet the physician and the lawyer pursue the same line of logic and of inquiry. As the former must have a subject to dissect or to operate upon, so must the[387] lawyer in pursuing a criminal investigation first prove a visible material substance known in legal phraseology as the corpus delicti, which he must connect with some personality, with some human being once known to have lived. In this important process the physician’s testimony being the indispensable guide of the court’s inference, he should limit himself to purely anatomical and material knowledge. The medical expert has absolutely nothing to do with guilt or innocence, as that is a question for the jury. He should, above all things, be absolutely free from prejudice, suspicion, or undue suggestion, and should remember that in thus sinking his personality his sole function as a skilled witness in cases of identity is to furnish testimony which, when taken in connection with other evidence in the case, may establish such a corpus delicti as would justify the inference of a crime.
A nice point may arise as to dispensing with the proof from the body itself, when the substantial general fact of a homicide is proved aliunde, as in the case of a criminal causing the disappearance of his victim’s body by means of its decomposition in lime or other chemical menstrua, or by submerging it in an unfathomable spot in the sea. Under circumstances such as the following: a person is seen to enter a building and is not seen to leave it, although all means of egress therefrom are watched; another person is seen to ignite the building, which thereupon burns down, and the charred remains of a human body are found in the ruins; the proof of identity from the body itself might be dispensed with in view of the substantial general fact of a homicide having been committed. In a delicate case where the man of art hesitates and finds no corpus delicti, the investigation of imprints and stains may give a clew of great value to the expert. Yet it is only upon absolute evidence, and in the strongest possible case, that the fundamental principle of the corpus delicti is disregarded.
In the case of Ruloff, the child’s body was not produced and no trace of it could be alleged to have been found; nevertheless the prisoner was found guilty of murder. This case was speedily overruled (18 N. Y., 179), on the ground that a dangerous precedent had been pronounced.
So indispensable is the showing of the corpus delicti in cases of recognition that lawyers have come to regard even the[388] judicial confession of an accused as often the flimsiest and most unsatisfactory kind of evidence. Numerous cases of demonstrated fallibility of confessions are cited in the books, where the statement was utterly lacking in anything except motive or hallucination. In the Proceedings of the New York Medico-Legal Society, December 6th, 1876, Mr. James Appleton Morgan mentions the case of a German servant-girl who assured her mistress, whose little boy, a child of seven, had just died and been buried, that she (the servant) had poisoned the boy. The servant swore to her crime and was taken into custody, and it was only when no poison was discovered upon exhuming the child’s body and examining its stomach that against her own protest she was acquitted of the possibility of the crime. Another case of the kind that has had medico-legal notoriety was tried a few years ago before a court in Brittany. The accused declared that he had killed his servant and thrown the body in a pond. His guilt seemed certain, when the alleged victim put in an appearance, thus reducing the evidence to the strange hallucination that had prompted the confession.
But the most wonderful of these is the celebrated case of Boorn, in which medico-legal evidence took no part. In view of the seeming hopelessness of his case, the accused confessed to murder in expectation of mercy from the court, but was finally acquitted on the alleged victim walking into court and confronting the man who had sworn to having killed him.
Although wisdom and experience point to the necessity of showing something corporal and material in cases involving questions of life and death, yet very small traces or minute remains of a human body may, in certain circumstances, constitute a corpus delicti that may lead to trial if not to conviction. In 1868 the Lambert case, for murder on the high seas, was tried before Judge Benedict in the United States Court, the only corpus delicti alleged being a large pool of blood and brains found on the forecastle of a ship at sea, out of sight of land or other vessel. Circumstances, acts, and words pointed strongly to the murder of one of the crew, who was believed to have been brained with an axe and thrown overboard. Notwithstanding the fact that animosity was known to exist between the accused and the missing man, it further appeared that the accused, in a state of great excitement, had followed[389] the missing man forward and returned alone with a hatchet in his hand, yet the jury in this instance were not satisfied as to the establishment of a corpus delicti beyond a reasonable doubt and accordingly failed to convict.
Two classical cases, that of Gardelle and of Dr. Webster, mentioned in many of the books, stand forth as instances of conviction where fragments of the human body were recognized after attempts to destroy them by intense heat. The conviction of Dr. Webster rested almost entirely upon medico-legal evidence; but it is probable that upon the same circumstantial evidence the increased industry of counsel would have so rung the changes in regard to its uncertain and unsafe nature, and would have so used the knowledge gained from advanced discoveries in the regions of the probabilities of science, as to have secured the acquittal of the prisoner had the trial taken place at the present time.
A similar affair of great medico-legal interest is the Goss-Udderzook tragedy, already referred to, an account of which is given by Drs. Lewis and Bombaugh among the “Remarkable Stratagems and Conspiracies for Defrauding Life Insurance Companies,” New York and London, 1878.
IDENTITY OF BURNT REMAINS.
The medical jurist will no doubt find cremation a formidable barrier in elucidating the question of identity, although the entire destruction of a dead body is a matter of extreme difficulty.
In the case of calcination chemical analysis of the ash would detect the phosphate of lime, but this would throw no light upon the subject, since the ash of human bones and that of the lower animals is identical. If the burnt bone is entire, the state of the epiphyses may enlighten the question of the determination of age. The following two cases, in which fragments or portions of bone had been submitted to the action of fire, show how medical training and some knowledge of comparative anatomy may contribute to the establishment of guilt or may attest innocence.
In the case of The Queen vs. John Henry Wilson, for murder, the accused burnt his step-father in a lime-kiln for[390] over a week, and on strewing ashes from the kiln fine fragments of bone picked up were afterward identified as human. At the trial identity rested on the fact of finding two buttons and a buckle, which were recognized as part of the deceased’s wearing apparel when last seen.
In the second case, that of a young woman supposed to be in the family way who should not have been, it was thought that she had been confined and made away with the infant. Under this supposition the premises where she lived were searched by the chief constable, who found in the stove some bones and fragments of bones that had been burnt. On examination by a qualified medical man, the fragments turned out to be not human bones, but those of some other animal, presumably those of a pig and of a chicken, which the family, who lived in a tenement-house without a back yard, had put in the stove to get rid of the refuse.[570]
IDENTIFICATION OF HUMAN BONES.
In deciding whether certain bones are human or not, the medical jurist should exercise great caution in venturing an opinion as to the precise animal of which he may believe they formed a part. There is no great difficulty in detecting the smallest fragments of bone by means of the microscope, but we cannot say with safety whether the fragments belonged to a mouse, a man, or an elephant. A real difficulty occurs in recognizing the nature and origin of the bony remains when only a small fragment or a single bone is submitted for report. If a sufficient portion of the skeleton be submitted it can be easily recognized as human, as in the imbedded remains of the troglodyte found in the limestone deposit of Luray Cave, Virginia, and only in the exceptional case of the bones of one of the manlike apes could a difficulty of distinction arise. The characteristic signs that distinguish a gorilla skeleton, for instance, are the smaller thumb; notable length of tibia and of radius, although this relative length of extremities has been remarked in negroes; small facial angle, 30° to 40° in the monkey, 70° to 80° in man; very inferior cranial capacity, the maximum in a gorilla being 550 cubic centimetres, while the[391] minimum in the human species is from 970 with a maximum of 1,500 to 1,900 centimetres; a low index of the foramen magnum; convexity of the squamo-parietal suture, and larger and more salient canines and incisors. The volume of the endocranium in the female gorilla, like that of the human species, is smaller than that of the male; this difference being almost 80 c.c. for the anthropoid female.
In studying the osseous system it should be remembered that certain modifying elements, as artificial compression, pathological deformities, posthumous distortions, and hygrometric conditions, may affect particularly the skull, and if due allowance be not made for these the study may lead to glaring absurdities. Not longer ago than 1725 there was found in a quarry at Œningen the skull of a fossil batrachian compressed into rude resemblance to the human cranium, which was announced to the world as Scheuchzer’s “Homo diluvii testis et theoscopos,” and as the remains of one of the sinful antediluvians who perished in the Noachic deluge.
Are the Bones Old or Recent?
An important point may arise in questions of identification of bones as to the oldness: whether they are old or recent. The first indication is furnished by the presence or by the absence of the soft parts. The existence of the periosteum and of the spinal marrow is the most persistent proof of a recent state; but these alone with the soft parts are usually destroyed in two or three years. In ordinary circumstances a body becomes skeletonized in about ten years, although in exceptional cases the cadaver may resist decomposition after many years.[571]
This summer in transferring an old cemetery in Georgetown, D. C., the remains of the grandmother of one of the writer’s patients were found in such a state of preservation as to be easily recognized after fifty years of burial. More recently, in unearthing the remains of an old graveyard in East Washington, a striking peculiarity was noticed in the fact that many bodies of young people buried in recent years when taken up consisted of a few blackened bones and shreds of grave-clothes.[392] while the remains of many older people buried long before the Civil War were found in an excellent state of preservation. One of these was a Mr. Fullin, who died from the effects of a sunstroke forty years ago and was buried in a metallic case. An old lady who attended his funeral was present when his remains were unearthed and said they looked as natural as when he was laid away in 1852. The features were well preserved and even the white linen of the shroud was unsoiled.
Alterations in the texture of the bone, such as that caused by dryness and by diminution in the proportion of organic matter, may be ascertained by histological examination, and one of the characters of age may be furnished by taking into consideration the specific weight. Placing the skull at an average density of 1,649, that of an infant would be 1,515, an adult 1,726, and that of old age 1,636.
Ascertaining the proportion of organic and inorganic matter, the phosphates and carbonates, by chemical means may furnish an additional help in the interpretation of the remains.
With all these diagnostic methods it may still be impossible to establish identity either absolute or relative, even where a whole skeleton is in question. The evidence may, however, be of great juridical use to the accused, as in the case of Van Solen, tried for the murder of Dr. Henry Harcourt, where the collective facts pointed to the identification of a body dead two years. The jury, however, after a second trial, were instructed to acquit unless they were certain that the remains were Harcourt’s. They acquitted, as no one decided and apparent feature was known to have existed by which the remains could be identified beyond a doubt.[572]
Identity in Case of Entire Skeleton or in Case of Isolated Bones.
Where an entire human skeleton has been discovered, the objects of inquiry here, as in the case of fragments or remains, are to establish the identity of the victim and that of the author of the act, and to collect all available information relative to the nature of the death and to the diverse circumstances attending the commission of the deed.
In gathering evidence from the examination of the skeleton or of isolated bones, with a view to find out the probable cause of death of the person of whom they form a part, a great variety of questions will arise for consideration, such as those relating to race, stature, age, sex, and trade or occupation; the exterior signs furnished by dentition; the traces of congenital peculiarity or of injury, and the signs of disease either hereditary or acquired.
Determination of Race.
The question of race in connection with the subject of identification is of more than usual importance in the United States, owing to our motley population, composed as it is of aboriginal Americans, Chinamen, negroes, and of Europeans and their descendants. I well remember the first human bones that I saw exhumed. They were discovered in digging the foundation of a building near a kitchen-midden on one of the tributaries of the Chesapeake Bay. The apparent oldness of the bones and the finding of stone arrow-heads, tomahawks, and fragments of aboriginal pottery in the immediate vicinity were additional accessory facts that strengthened the presumption of the bones being those of a Choptank Indian.
Roughly speaking, there is not much trouble in recognizing the platycnemic tibiæ of the mound-builder, the skull of a Flathead Indian, an Inca skull, a negro skull, or even the skull peculiar to the lower order of Irish.
In many very old skulls a considerable portion of hair is often found attached. This of course may lend assistance in the matter of race identity. A few years since I undertook at the Smithsonian Institution a series of micro-photographs of the structure and arrangement of hair, with a view to race classification as suggested by Professor Huxley. Various specimens of hair from the yellow races were compared with that of fair and of blue-eyed persons, with the hair of negroes, with reindeer hair, and with the hair-like appendage found on the fringy extremity of the baleen plates in the mouth of a “bowhead” whale. The experiments, though far from satisfactory, were sufficiently conclusive to enable one to recognize approximately the horse-like hair of some of the yellow races, that of the negro, and that of a blond Caucasian.
Beyond the forementioned characteristics, the task of race recognition from observation of the skull is one of great difficulty and perplexity with illusory results. A considerable experience of several years with the large collection of skulls in the Army Medical Museum enables me to speak advisedly on this point.[573]
Although the technical procedures of craniometry require special measurements and employ an arsenal of special instruments, the results are far from conclusive as regards the determination of human types. Time and space do not permit the mention even in epitome of the various methods most relied upon by trained craniologists. Among the oldest operations of cephalometry, as well as the most incomplete, is the measurement of the so-called facial angle, which is employed to distinguish the skull of a lower order of animal from that of the negro and the white man. This angle, acute in the skulls of the lower animals, approaches a right angle as we ascend the zoological scale; being from 30° to 65° in the various apes; 75° in the Mongolian; about 70° in the negro, and between 80° and 90° for whites. The prognathous (projecting) jaws of the negro cranium are distinctive, as well as the shape of the nasal opening, which in the black is an equilateral triangle, while it is isosceles in the white. The books usually speak of the Eskimo skull as pyramidal, which in point of fact is not true. Inspection and examination of a large collection of Eskimo crania has changed and greatly modified some of the previous notions of the conventional Eskimo skull. From more than one hundred, collected in the vicinity of Bering Strait,[574] I find that the skulls present very considerable variations among themselves; some being brachycephalic, others dolichocephalic. In many the facial angle is 80°, and in one instance 84°, which exceeds that observed by me in many German skulls. Nor is the prominence of the zygomatic arches such a constant difference in the configuration as to justify one in speaking of the skull as pyramidal. On the contrary, in many of the specimens lines drawn from the most projecting part of the zygomatic arch and touching the sides of the frontal bone, instead of forming a triangle[395] on being elongated, might, like the asymptotes of a parabola, be extended to infinity and never meet. The index of the foramen magnum in these skulls is about the same as that of European crania. The internal capacity shows marked difference, the cubic contents of the endocranium averaging that of the French or Germans.
As some modern writers lay great stress on the measurement of the cranial capacity, not only as an aid to race identification, but as an adjunct in the study of the criminal and insane classes, it may not be amiss to give the salient facts relative thereto.
It is admitted that the cranial capacity may vary with the intellectual state, hydrocephalic skulls, of course, being excluded. Microcephalic adults give a figure inferior to that of gorillas, some being as low as 419 c.c. Andaman Islanders and autochthonous Australians appear, in respect to cranial capacity, to be most badly off. The capacity of an Andaman has been found as low as 1,094 c.c.; while that of Australians (autochthonous) and of some American tribes show an average capacity of 1,224 c.c. in the normal as well as in their deformed crania. The cranial capacity increases in the yellow races and attains its maximum in the white races. In the middle European race 1,500 c.c. may be accepted as the average; 1,750 c.c. is the maximum, and anything above is macrocephalic; while the minimum is 1,206 c.c., which is rather too low than too high. According to Topinard’s nomenclature of the cranial capacity, macrocephalic in the adult European male are those having a capacity of 1,950 c.c. and above; a large skull is one of 1,950 to 1,650 c.c.; average or ordinary, 1,650 to 1,450 c.c.; small, 1,450 to 1,150 c.c.; microcephalic 1,150 c.c. and below. It would seem that the skulls of the insane are below the type, a measurement of sixteen male skulls giving an average of only 1,449 c.c. Scotchmen head the list with the most voluminous skulls, and according to a tabular statement made up from Welcker, Aitken, Broca, and Meigs, the English come next, with a capacity of 1,572 c.c. Then follow Eskimo, 1,483 c.c.; Germans, 1,448 c.c.; French, 1,403 to 1,461 c.c.; South African negroes, 1,372 c.c.; Ancient Peruvians, 1,361 c.c.; Malay, 1,328 c.c.; Mexican, 1,290 c.c.; Hottentot and Polynesian, each 1,230 c.c.; Australians, 1,364 c.c.; and Nubians, 1,313 c.c. The cranial[396] capacity in man, like that of the anthropoid apes, varies according to sex, the difference being so great that it is necessary to measure separately.
In the troglodyte skulls of prehistoric times the variation is not more than 99.5 c.c.; but in the contemporaneous races the difference varies from 143 to 220 c.c. French craniologists usually speak of the Auvernats as possessing the highest cerebral capacity (1,523 c.c.), and mention the skull of a Parisian of 1,900 c.c. as the highest known. Some Eskimo skulls, however, measure from 1,650 to 1,715 c.c., and two eurycephalic Indian skulls in the anatomical section of the Army Medical Museum measure respectively 1,785 and 1,920 c.c.
Mr. Havelock Ellis, speaking of the psychic characteristics of criminals, says that the lower human races present a far larger proportion of anatomical abnormities than the ordinary European population; and Sir William Turner writes of the skulls collected during the Challenger expedition that although their number is certainly too limited to base any broad generalization on, as to the relative frequency of occurrence of particular variations in the different races, there is obviously a larger proportion of important variations than would occur in a corresponding number of skulls of the white races. Thus, for example, the squamo-frontal articulation is found in less than two per cent of European skulls, while it is found in twenty per cent of negroes, according to Ecker, and 16.9 in Australian skulls, according to Virchow. Again, the spheno-pterygoid foramen is found in 4.8 per cent of European skulls and in 20 per cent of American Indians; 30 per cent in Africans; 32 per cent in Asiatics, and 50 per cent in Australians. The wormian bones are also more common among the lower races; as a rule, the cranial sutures coalesce much earlier and the teeth are more precocious.
Photography, though of undoubted service in craniometry, has been applied as a crucial test in the matter of identity and found wanting. It is objected to on the ground that it has no character of precision, and that photographs of the skull have the common defect of being central, not orthogonal projections, such as anthropometry requires. Besides, the lenses of cameras are not uniformly perfect. Anatomists know, moreover, that salient differences in any collection of crania prevent[397] methodical enumeration and constitute the stumbling-block of ethnic craniology. Cephalometry shows, further, that dolichocephalic, mesaticephalic, and brachycephalic skulls do not belong exclusively to the white, the yellow, or the black race, but exist among the three as a result of evolution.
On this subject Professor Lombroso, among the foremost contemporaneous medico-legal writers, cites the cranial asymmetry of Pericles, of Romagnosi, of Bichat, of Kant, of Chenevix, and of Dante, who presented an abnormal development of the left parietal bone and two osteomata on the frontal bone. Besides, there is the Neanderthaloid skull of Robert Bruce and the ultra-dolichocephaly noticeable in the skull of O’Connell, which contrasts with the mesocephaly of the Irish. The median occipital fossa is noticeable in the skull of Scarpa, while Volta’s skull shows several characteristics which anthropologists consider to belong to the lower races, such as prominence of the styloid apophyses, simplicity of the coronal suture, traces of the median frontal suture, obtuse facial angle (73°), and moreover the remarkable cranial sclerosis, which at places attains a thickness of 16 mm. (five-eighths of an inch). Further mention is made of the submicrocephaly in Descartes, Tissot, Hoffman, Schumann, and others.
De Quatrefages noted the greatest degree of macrocephaly in a lunatic, the next in a man of genius. Cranial capacity in men of genius is usually above the average, having been found as high as 1,660 c.c. in Thackeray, 1,830 c.c. in Cuvier, and 2,012 c.c. in Tourgueneff. The capacity is often found above the average in insanity, but numerous exceptions occur in which it drops below the ordinary average, as in the submicrocephalic skulls of Liebig, Döllinger, Hausmann, Gambetta, Dante, and Shelley.
From what has just been said, it follows that skull measurements for medico-legal purposes have no more significance than the fact that some men are taller and some shorter than others. The medical jurist should, therefore, not be too dogmatic in drawing conclusions as to race from the skull alone. To complete the diagnosis in the matter of skeletal race peculiarity, the splay foot of the negro with the unusual backward projection of the heel-bone, as well as the greater relative length of the tibia and of the radius, may be taken into consideration. There are[398] other characteristics of the lower jaw and of the facial bones generally, the study of which leads up to the realm of transcendental anatomy; so their further consideration would hardly appeal to the “dispassionate, sympathetic, contemplative jury” of our enlightened countrymen.
Determination of Height or Stature.
When we have the entire skeleton to deal with, the height or stature may be determined with a reasonable degree of certainty by allowing from one to two inches for the soft parts. Most of the proportions given in works on artistic anatomy approach mathematical exactness. For instance, if both upper and lower extremities are extended after the manner of spokes in a wheel, and a point corresponding to the umbilicus be taken as a centre, the circumference of a circle described therefrom should touch the bottom of the feet and the tips of the middle fingers. When the arms are extended horizontally the line included in the middle-finger tips equals the height in the generality of men, although in exceptional cases it may vary. The negro giant, Nelson Pickett, is reported to have been eight feet four inches high, while his outstretched arms measured nine feet from tip to tip. Ordinarily the upper part of the symphysis pubis is the centre of the body. Some anatomists contend that this important point is really below the symphysis in the average man. The length of the foot about equals that of the head. According to Quetelet, its length is just one-ninth of the body in women, a little more than one-ninth in men. The conventional representation of the human foot with a second longer toe is, according to Professor Flower (see “Fashion in Deformity”), of negro origin and does not represent what is most usual in our race and time. Statistics of measurements made in England by several observers on hundreds of barefooted children fail to show one instance in which the second toe is the longer.[575]
Taken singly the bones may enable an approximate estimate of the height of the person when alive; but it should be remembered in connection with this subject that the height is not a[399] fixed quantity, since it differs according to upright or recumbent position, also before and after a night’s rest. Moreover, the alleged height of the deceased may have been taken in boots and is probably incorrect.
Many tables of measurements have been constructed for the purpose of determining the height from the dimensions of the bones; but the relation that exists between the total height and the dimensions of different bones varies according to age, sex, asymmetry, and individual peculiarities, hence the tables will not bear the critical examination that warrants their use with assured correctness, even in a majority of cases. The femur is the bone that gives the best results in these measurements. Isolated fragments have been included in the enumeration; the nose and the middle finger multiplied by 32 and by 19 or 20 giving the approximate height. While the foregoing calculations will not bear scientific scrutiny, they are of sufficient importance to be taken in connection with other facts in determining the probable length of the skeleton. Among the most trustworthy of these tables are those of Dr. Dwight, of Harvard University.
Determination of Age.
The age is a still more difficult matter to state precisely. Even during life one may be as much as ten years out in guessing the age of an adult, while the error may be from fifteen to twenty years in the case of a corpse. Dr. Tourdes mentions a case where the age was guessed as sixty and sixty-five in a deceased person aged eighty-five.
The state of the osseous system and the condition and number of the teeth, which strictly speaking are not bone, are among the surest guides in the determination of age. The signs furnished thereby may vary according to the periods of increase, maturity, and decline.
During fœtal life and even at the epoch of birth the bone centres are few. The distal end of the femur, the proximal end of the tibia, and the astragalus are ossified at birth. Points of ossification appear in successive order of development. The exact period at which the bones begin to ossify and the progress of bony union being detailed in standard works on anatomy, it would be superfluous to repeat them here. These[400] changes are, however, not absolutely certain as to time and order, as the tip of the acromion process of the scapula sometimes remains ununited throughout life; the ossification of the sternum and of the costal cartilages is very uncertain, while the teeth, like certain railway trains, are only due when they arrive.
From the character of the progress of consolidation of the skeleton the age may be estimated with a reasonable approach to accuracy up to twenty-five or thirty years, which is the stationary period as regards alteration in the osseous system. Above this period it is difficult to arrive at the age. About forty the cranial sutures[576] begin to disappear, although the time of the closure of the sutures varies within large limits; the coccyx becomes consolidated; ossification begins in the thyroid cartilage and in that of the first rib (although this state of the rib is regarded by many as pathological); the lower jaw, which in the fœtus and in infancy formed an obtuse angle, now assumes nearly a right angle. As senility progresses toward decrepitude, the bones become lighter and more brittle, owing to fatty atrophy, and their medullary canal larger; the jaw returns to its infantile shape from loss of teeth and atrophy of the alveolar processes; the bodies of the vertebræ (according to some authorities) bevel off in front; osteophytes are formed, and the neck of the femur approaches the horizontal. (See Abortion and Infanticide.)
Determination of Sex.
In the matter of sex there should be no difficulty, after noting the proof furnished by the aggregate characteristics of both male and female skeletons. The points of contrast between the two skeletons are not so striking before the age of puberty. Generally speaking the cranial capacity of an adult woman is less, although it is contended that since the great majority of males of the human species are taller, heavier, and larger than the females, it follows that if due allowance be made for these variations, it will appear that the brain capacity of woman is relatively very little, if at all, inferior to that of man. The mastoid processes of the female skull are smaller; the lower[401] jaw-bone is relatively smaller and lighter; the ribs are lighter and compressed; the spine is relatively longer; the collar and shoulder bones and the sternum[577] are smaller and lighter; there is a less pronounced angle in the femur, the neck of which approaches a right angle, while smallness of the patella in front and narrowness of the articulating surfaces of the tibia and femur, which in man form the lateral prominences, are said to make the knee-joint in women a sexual characteristic. But it is the striking contrast in the pelvis that furnishes a sexual significance that is of greater value than all the rest of the skeleton together. From a glance at the text-book account of the pelvis, it does not appear that much anatomical knowledge is necessary to identify the important points that give shape to the female pelvis. Its greater diameter (except the vertical), larger and more curved sacrum and coccyx, and great spread of the arch of the pubes are well-nigh incontestible signs. The differences as detailed in the books can be objected to only on the possibility of a so-called hermaphrodite pelvis in one of the other sex. We sometimes see a very large pelvis in a subject who by a teratological freak became a man. Masculine characteristics are, however, oftener found in women than feminine characteristics in men; hence the conclusion that the presence of feminine characteristics leaves but little doubt as to the sex, but that certain masculine indications, while giving a great probability for the male sex, are not absolutely decisive. (See Hermaphroditism.)
The finding of fœtal bones around or about the supposed female skeleton is suggestive. It could not be inferred from this fact alone that the woman was or was not pregnant at the time of death, since the absence of fœtal remains on the one hand might imply their entire decomposition in advance of those of the adult; on the other hand, the indiscriminate habit of undertakers, who often bury still-borns with adults, may account for their presence.
Accidental Signs and Evolution of the Teeth.
The trade or occupation leaves but few marks on the bones that are useful in the matter of identification. It is in the[402] recent and well-preserved cadaver, or, better still, in the living subject, that the professional signs are of importance. As a rule, the relatively larger scapulæ point to the fact of a day-laborer; necrosis of the lower jaw suggests a worker in phosphorus; worn and discolored teeth a user of tobacco, and aurification of the teeth might suggest the previous social condition. Gold crowns and fillings and dental prosthesis generally are among the most common and, at the same time, among the most useful signs of identification. By this means the bones of persons killed by Indians on the Western plains have been recognized years afterward. The traveller Powell, massacred in Abyssinia, was recognized in this way. From the presence of artificial teeth and the mechanical appliances for fixing them, dentists may recognize their own work beyond a doubt. One of the most common-hackneyed of these cases is that of Professor Webster.[578] Later cases, in which this kind of proof established convincing and conclusive identification, are those of Dr. Cronin, assassinated in Chicago in 1889, and of the bomb-thrower, Norcross. Every now and then accounts appear in the daily press of corpses having been recognized by inspection of the teeth. In Washington, only a short time since, the remains of an unknown man were exhumed from the Potter’s Field for judicial reasons. The unrecognized body had been found in the Potomac in an advanced stage of decomposition. From the signs furnished by the teeth the remains were identified as those of a person who had disappeared mysteriously and under circumstances that pointed to his having been murdered at a Virginian gambling den, and his body thrown into the river. In connection with this subject the Goss-Udderzook tragedy is of instructive interest.
In every important case a cast of the mouth should be taken, in order to set at rest any question that may subsequently arise as to the condition of the jaw, the absence of teeth, their irregularity or other dental peculiarities. A cast of the mouth of the deceased in the Hillmon case showed all the teeth to be regular and perfect, while it is alleged that Hillmon’s teeth were just the opposite. External signs furnished by dentition may assist greatly in fixing both age and identity. The evolution of the human dental system has been so well studied[403] from intra-uterine life to old age that we may approximately tell the age, especially of children, from the teeth alone. This sign, so valuable in childhood, loses its value as the dentition progresses. Elaborate tables and dental formulæ to be found elsewhere deal with the two periods of dentition, the relative position and number of the teeth, and the like.
At birth the jaws show points of ossification only; but children are sometimes born with central incisors, as the writer has, in common with others, noted in several instances. The first dentition takes place from the seventh to the thirtieth month; the second between four and five years. In rachitic children these periods are later; but a syphilitic taint may hasten their development. The twenty-eight teeth characterize early youth. Wisdom teeth appear between eighteen and twenty-five, sometimes as late as thirty years. The presence of thirty-two teeth indicates maturity. This number is sometimes exceeded. Dr. Tidy, in his work on “Legal Medicine,” reports having seen several children between six and seven years with forty-eight teeth. Instances are recorded of cutting the teeth at advanced age, seventy and one hundred and eighteen years; of adults who have never had teeth; of supernumerary teeth, and of a third dentition. What purported to be a third dentition came under my notice some years ago, in the person of an old negro “voodoo doctor.” A more recent case, said to have occurred in an old man of seventy-four, at Seymour, Ind., is reported in the Weekly Medical Review, St. Louis, Mo., April 16th, 1892, p. 314.
The pathological signs furnished by the teeth should, of course, be looked upon as a personal characteristic that may lend additional light in the question of identity.
Congenital Peculiarities, Deformities, and Injuries.
But congenital peculiarities or injuries of other parts of the skeleton are studied to greater advantage in determining proof or disproof of identity. We may recognize cranial asymmetry; the peculiar conformation of the idiot skull; the prognathous skull of the negro; the pyramidal skull of some of the yellow races, and the oval head of the white man; besides the ethnic artificial deformities already touched upon in considering the[404] question of race. A metopic cranium, a cleft palate, a deformed spine or pelvis, a larger left scapula—indicative of left-handedness; a shortened extremity; bowed legs, club foot, the presence of extra fingers or toes, and the relative length of the fingers are each and all valuable facts in judiciary anthropology. In women of Spanish extraction the fifth finger is almost as long as the fourth—a fact so well known that glove-makers take advantage of it in sending gloves to Mexico, the Antilles, or to South America.
An estimate of the length of the hand seems to be a matter of difficulty, notwithstanding the extensive observation of high authority. In the majority of cases the ring-finger is longer than the index.
Important evidence is furnished from the existence of injuries such as fractures, whether old or recent; the marks of gunshot wounds, of trephining, amputation, excision, or other surgical operation on the bones. The remains of an old, ununited fracture in his left humerus enabled Sir William Fergusson to verify and settle all doubt as to the identity of the body of the great missionary and explorer, Dr. Livingston.[579] The existence of an injury may constitute evidence of great importance to the accused, as happened in the case of an English gentleman charged with murder, where the trial turned on the deposit of callus in a broken rib, the only bone produced in court. From the state of this callus there could be no doubt that the fracture must have been produced about eight or ten days before death, and could not have belonged to the deceased. There was, therefore, complete failure of the identity, and the accused was discharged.[580]
On the other hand, circumstances may arise in which the existence or not of an injury is a fact of great importance to the prosecution. Among other specimens in the Army Medical Museum at Washington, the bones of the forearm of Wirtz, executed for inhuman treatment of prisoners during the Civil War, show no remains or trace of fracture; yet it was claimed in defence at the trial that he could not have been guilty of the atrocities attributed to him, for the reason that this arm was disabled from a fracture.
Disease of the bones, whether hereditary or acquired, is an essential descriptive element in reconstituting individuality. Caries and necrosis, rickets, spinal disease, ankylosis, and other external manifestations of bone lesion may furnish pointers of such value as often to be incontestible. They are so evident as not to require detailed mention; but much care in such cases is necessary to distinguish between disease, decay, and violence, and artefacta. The last may have resulted from the axe or spade of the grave-digger or from post-mortem lesions made at the necropsy, as in the remains of the notorious Beau Hickman of Washington, whose body on being exhumed showed that sundry amputations and reamputations had been made on the principal limbs. Having died in a public hospital, the cadaver had been utilized in rehearsal of these operations previous to its burial in the Potter’s Field.
Injuries of the phalanges, known as “baseball fingers,” are valuable indications. This was one of the facts of identification in the celebrated Cronin case.
Duration of Burial.
The condition of the exhumed bones may throw some light on the question as to the probable length of time they have been under ground, as well as the probable cause of death. If the bones were entirely denuded of soft parts we should hardly expect them to be those of a corpse buried only three or four months previously. The noting of such an injury as a fracture inflicted by some sharp instrument on a skull found in a cesspool was sufficient, with other evidence of a general character, to convict a prisoner tried at the Derby Lent Assizes in 1847.
In all cases of the kind under consideration, special attention should be paid to the surroundings, every little detail of which should be noted with the utmost accuracy; for such articles as clothes, jewelry, buttons, and in fact anything that may furnish an inference,[581] may not only throw light on the identity of the person, but otherwise assist justice. Cases are recorded in which the identity has been established principally by the clothing found with the skeleton. In Taylor’s “Medical[406] Jurisprudence” a case is mentioned where the skeleton, portions of clothes, buttons, and boots of a Cornish miner were identified after twenty-six years’ submersion in water. Somewhat similar circumstances, a few years ago, enabled the arctic explorer, Lieutenant Schwatka, and others to identify the remains of Lieutenant Irving, of the ill-fated Franklin party.
In exceptional circumstances, as that of great cold, for instance, organic remains may be preserved indefinitely. Visitors to the Junior United Service Club in London may remember the mammoth bones discovered in digging the foundation of the club-house. Accounts of remarkable preservation of bodies discovered a long time after the occurrence of Alpine accidents, and the finding of well-preserved mammoth remains in the Siberian ice, are matters of common knowledge. A few years since, in assisting to take the remains of a mammoth from an ice cliff in Escholtz Bay, Alaska, I came across the skull of a musk-ox and the rib of a reindeer which showed the deformity and callus of a united fracture, yet there are geological reasons for believing that thousands of years must have elapsed since these remains were entombed in the ice.
A precaution to be taken in judicial investigation of bones is to ascertain whether they belong to more than one body, as they may have been put together with a view to deceive. Each bone should be examined separately, to ascertain whether it is a right or left bone or belongs to the same skeleton. They should be put together with intelligence and care, and if incomplete parts of a skeleton they may be laid in sand or putty and photographed, or the medical man may go further and, Agassiz-like, reconstruct the skeleton from the fragments. In the case of a fracture the bones should be sawn longitudinally in order to study the callus.
THE HAIR AND NAILS.
Since the hair and nails resist decomposition an unusually long time, and are even believed to grow after somatic death, they may be considered as accessories of such value in the question that occupies us as to make it possible to verify certain characteristics regarding the remains of the cadaver even after years of inhumation. For instance, hypertrophy of the great[407] toe-nail, the length and color of the hair, baldness, or a long beard might furnish evidence of the best kind. Both hair and nails may, however, change after death. A case is mentioned[582] in which the hair changed from a dark brown to red after twenty years of burial. Accredited cases of the growth of hair after death are also on record. Dr. Caldwell, of Iowa, states that he was present in 1862 at the exhumation of a body which had been buried for four years. He found that the coffin had given at the joints and that the hair protruded through the openings. He had evidence to show that the deceased was shaved before burial, nevertheless the hair of the head measured eighteen inches, the whiskers eight inches, and the hair of the breast four to six inches.[583] Quite recently in unearthing the remains of an old cemetery in Washington, D. C., a number of persons noticed that when the body of a young girl, supposed to be about twelve or thirteen years of age, was taken up it was found that her hair had grown until it extended from her crown to her feet. Many careful observations seem to prove the molecular life of the hair and nails after somatic death. It suffices to quote the well-known case mentioned in Ogston’s “Medical Jurisprudence,” of several medical students who were brought to trial for having in custody the dead body of an idiot boy. When found on the dissecting-table the body was so disfigured that there was only one means left of proving its identity. The boy had a whim during life of permitting his nails to grow, and had not allowed them to be cut for many years previous to his death. They had completely curled round the tips of his fingers and toes till they had thus come to extend along the palmar and plantar surfaces in a strange way. The counsel for the prosecution availed himself of the knowledge of this fact, and his proof seemed to be complete, when a medical man came forward and gave in evidence that it was not an unusual circumstance for the nails to grow for several inches after death. This astounding statement so nonplussed the judge that the case was allowed to drop as not proven.
In exceptional cases the hair may be green. I saw a case some years since, for which no cause could be assigned, and only a few days ago I saw another in a man who worked in a[408] brass-foundry. At the Cronin trial a barber, who had counted the victim among his customers, recognized the shape of the head and texture of the hair. Subsequent evidence of medical experts was conclusive as to the identity of hair found clinging to a trunk, the hair cut from the head of the murdered man, and that of a single hair discovered on a cake of soap. This single strand, being lighter in color in some portions than in others, seemed to indicate that it could not have come from the head of the deceased, whose hair was brown. But it was shown that hair placed on soap or other alkaline substances becomes bleached in a manner similar to the color of a single thread. This evidence of vital importance linked the hair found in the trunk with that cut from Dr. Cronin’s head, and went far toward proving that one of the murderers had washed his hands with the soap after the deed had been done.
Reviewing the signs furnished by the osseous system, it will be seen that the study of the skeleton alone is beyond contradiction more satisfactory and more important in establishing identity than that of all the other organs. Consequently a correct interpretation of the facts observed and judicious application of the rules deducible therefrom may in the matter of a human skeleton put its identity beyond a reasonable doubt. But the expert should remember that as no two cases are just alike, unexpected questions and unforeseen features may present themselves, giving to each case merits of its own. At best the medical man’s conclusions will be probabilities, not certainties; therefore his expressions of opinion should be the more guarded, as upon it may hang the life of an innocent man.
IDENTIFICATION OF MUTILATED REMAINS.
Many of the foregoing remarks on the identity of the skeleton apply in cases where mutilated remains or a portion only of the body has been recovered. Circumstances often occur in which bodies may require identification after having been drowned and partly eaten by fishes or crabs, or after having been partly eaten by buzzards, or torn into fragments by animals, as has happened in the remains of a dead infant partly devoured by a dog, and in the case of a farmer who died in the woods and was subsequently eaten by his own hogs. After[409] accidents and fires where many persons perish; after a railway disaster where bodies have been mangled, drowned, burnt, and frozen, all in the same accident; or after an explosion from steam or gas or in a mine, or from gunpowder, dynamite, or other substance, the human remains are generally in such a state as to defy all attempts at recognition.
To dispose of a dead body in order to avoid detection, criminals will mutilate, disfigure, and chop into fragments the remains, which they afterward place in a trunk, a wardrobe, or throw into a sewer or other hiding-place. Scarcely a year passes that judiciary medicine is not concerned with cases of the kind. The frequency of such crimes has been attributed by some to the so-called contagion of murder; others offer the simple law of the series in explanation; others still believe that imitation is the principal cause. While there is no doubt a grain of truth in each of these, less philosophic minds will look upon such a beastly proceeding as a mark of the complete satisfaction sought by the destructive instinct.
Why such things should be is of less concern than the fact that criminal mutilation of the dead body is not confined to any age or country. Though more frequent in the last fifteen years, it takes up quite a space in the history of human cruelty. The violent passion, wrath, and vengeance that caused the prophet Isaiah to be sawn in two at the age of one hundred years by order of Manasses and Agag cut into pieces by Samuel have not materially changed in the days of Jack the Ripper; and we find such crimes in antipodal parts of the world, among varied sociological conditions, no matter whether it be the North American Indian, who scalps and mutilates his enemy and places the severed penis in the mouth, or the civilized European, who cuts up the body of his victim and serves it in a curry at a feast of assembled friends.[584]
This new point of judiciary medicine has lately been elaborated by European writers under the title of Dépeçage Criminel, a term which applies to the operation resorted to by an assassin having for its end the getting rid of the body of the victim and to render more difficult the establishment of its identity.
The cleverness of experts scarcely keeps pace nowadays[410] with the more complicated proceedings adopted by criminals. In fact, at a trial of this kind truth and science are often the under dogs in a fight, than which none in forensic medicine is longer and more embarrassing. To cause a rapid disappearance of the proofs of a homicide, with a view to escape the investigations of justice, murderers have been known literally to make hash of the victim which was subsequently eaten by themselves and others. Gruner relates the case of a man who, having killed and cut into pieces his victim, boiled and roasted the fragments and ate them with his wife. Such examples, however, suggest morbid rather than passional phenomena, which manifestly call for rigid scrutiny into the mental state of the culprit, who may be more of a lunatic than a malefactor.
In cases of infanticide new-born children are sometimes cut into pieces and the fragments burnt in order to facilitate the disappearance of the cadaver. There does not appear to be, however, any well-authenticated instance of the operation having been done on a living child. Generally the dismemberment is done in order to cause more ready disappearance of the remains.
The medico-legal problem to be solved in cases of criminal mutilation is to establish the identity of the victim and that of the author of the crime.
Many apparently trivial circumstances may assist in the formation of an opinion as to the identity of the culprit. If the victim be an adult, a man is the author of the deed; if an infant, a woman, the mother, is almost always the guilty one. The London Lancet (May 30th, 1863, p. 617) reports a case in which the body of a child, of apparently four to six months, was found in the sewage of a water-closet, minus an arm cut off below the shoulder, presumably that a vaccination-mark might not be adduced as evidence. A young woman was suspected. Several women deposed having seen a dusky-brown mother’s mark near the child’s navel. After steeping in pure water a portion of the skin said to include the mark, and after washing, the mark gradually reappeared at the end of three days, perfectly distinct. It was recognized by witnesses and produced at the trial as corroborative evidence. The accused was found guilty.
In a case of infanticide at Tarare, in 1884, the upper extremity[411] of a fœtus was found to have been disarticulated after the manner of carving the wing of a fowl. This having suggested to Dr. Lacassagne a cook as the author of the crime, she was speedily discovered and convicted. A few years later an analogous case occurred in Florence and was reported by Dr. A. Montalti.
The instrument used for mutilating the body may furnish a suggestion of identity, to be dispelled or affirmed upon further investigation. The mode of section observed in various instances has led to the recognition of a butcher as the culprit. An expert would have but little trouble in distinguishing the hacking and mangling of a body from the careful cutting and preservation of muscles and blood-vessels in dissections made by medical students, whom the public, by the way, invariably suspect in cases of mutilation. If it can be ascertained that the instrument used was operated either by a left-handed person or by an ambidexter, such a fact may prove of importance. Sometimes the fragments are tied or sewn up in a package. The manner in which the knot is tied may indicate the occupation of the culprit. In one case the regularity of the sewing revealed that it was the work of a woman. Examination of the remains of clothing and of neighboring objects where the crime was committed may result in the identification of the victim or of the murderer. Indeed, it is the careful noting of trivial facts and their combination that is so valuable in all investigations of this class. A compound fact made up of minor facts, which considered severally would possess but little value, may sometimes solve the puzzle in a case where no single fact of conclusive value is obtainable.
Having collected as much of the mutilated remains as possible, the first step toward identification is to replace the pieces in anatomical order, to note carefully their correspondence or otherwise, and to ascertain whether the fragments belong to the same body or to two or several individuals. This is often a delicate and difficult matter, especially where decomposition is advanced or where the horror has been pushed to its utmost limits, as in the case of a fratricide committed in France by several persons, who fragmented the cadaver with a saw and hatchet; boiled the remains and fed them to hogs; and, after crushing the bones with a hammer, threw the fragments[412] into a deep gorge. Again, the body may be divided into numerous pieces, a hundred or more, and disposed of in widely different localities, as in a pond, a manure-heap, a river, or a cesspool. The chopped-up remains of infants have been boiled in lye and afterward thrown into a privy or put in a barrel of vinegar. A mother has also been known to cook with cabbage the dismembered remains of her six-months’ child and serve it at a meal of which both she and her husband partook.
Numerous counterparts of such cases happening in late years could be cited where the object was to favor the disappearance of the cadaver, and in which the establishment of the identity turned on the examination of some small part of the organism; the uterus, the spermatic cord, the lobe of the ear, the hair, or the teeth furnishing a positive demonstration that led to judiciary results.
Putrefaction goes on very fast in a corpse that has been mutilated; but it is slower in parts which, on being separated just after death, have become bloodless in consequence of the hemorrhage. After submersion the outward signs of putrefaction put a notable obstacle in the way of identification, and after drowning the body becomes rapidly unrecognizable.
Supposing it impossible to reconstitute the cadaver in all its essential parts, it is always possible, by following the instructions already given for examining the skeleton, to infer from one or several parts of the cadaver the sex, age, height, and sometimes pathological peculiarities of the victim. Examination of the skeleton and teeth is of capital importance in an investigation of this class. The indications furnished thereby having already been touched upon, and being about all that we are justified in saying, it is only necessary to repeat that many of the details relative to these special indications are so confusing as to suggest caution in using the statistical tables of even high authority, as the observations they rest on are not of sufficient extent to deserve confidence.
A survey of the head, limbs, trunk, and genital parts will give the most useful indications. The HEAD, in fact, is the surest index for justice, and one that lends promptness in the discovery of the assassin. Typical illustrations of this occur in the Goss-Udderzook case and in the recent example of the bomb-thrower, Norcross. In the case of a woman murdered by[413] her husband at Antwerp in 1877 and cut into one hundred and fifty-three pieces and her remains thrown into a privy, the color of the hair, the lobule of a torn ear, and the uterus of a woman having had children furnished special signs that led to identity and condemnation. Examination of the brain and its membranes, though furnishing no very notable characteristics in the matter of identification, may nevertheless be regarded as a natural corollary to that of the skull. Brain weight, which is greatest between thirty and forty years, 1,200 to 1,450 grams in man, 1,100 to 1,500 in woman, diminishes toward the sixtieth year. It is said that the diminution takes place a few years sooner in the opposite sex. The estimated loss of weight in a person of eighty years is admitted to be from 90 to 150 grams. Another sign of age is the tendency to degeneration found in the pineal gland, the cortical substance, the optic and striate thalami, and in the brain capillaries.
The state of the eyes, if not too decomposed, may still become a sign of identity. For instance, the color of the iris, an arcus senilis, a pterygium, a cataract or an operation for the same, an iridectomy, etc., are signs that occasion may utilize.
The TRUNK may show, as it has in several instances, incised wounds that caused death before the mutilation. Besides, the organs therein contained may by their weight, dimension, and tissue alteration indicate the progress of age and of degeneration. Modifications of the circulatory and respiratory apparatus are obviously characteristic. As age advances the only organ whose weight increases with the number of years, the heart, may become hypertrophied or dilated; its coronary arteries may undergo an alteration; the pericardium thickens, and in fact arterial atheroma and degeneration generally may begin between thirty-five and forty years. It should, however, be borne in mind that these signs of senility may come much later or even not at all. In a man of eighty-four years Tourdes found no notable tissue lesion; in another of one hundred and four Lobstein found no trace of ossification of the arteries of the trunk and upper extremities, and in Thomas Parr, aged one hundred and fifty-two years, Harvey found absolutely no lesion of this kind. Although toward eighty years the heart increases in weight in both sexes, the opposite has been observed in exceptional cases. Placing the average weight of this organ[414] in the adult at 266 grams for men, 220 for women, it will be found that progress in weight gives toward the eightieth year an increase of 90 grams for men and 60 for women. Yet a case of cardiac atrophy is reported in a woman of eighty whose heart weighed but 170 grams.
Diminished weight of the lungs becomes accentuated with years. Especially is this the case after pseudo-melanosis and senile emphysema. The state of the lungs of stone-cutters and miners and various thoracic and abdominal diseases may likewise become signs of identity. A cirrhosed liver, an enlarged spleen, a senile kidney, and the like, are sufficiently obvious in their bearings on this question.
Like the trunk, the ARMS AND LEGS, in cases of the class under consideration, show but few traces of disfigurement other than the fact of their having been disjointed. The manner in which the sections were made and the proceedings employed for the disarticulation would equally affirm an experienced hand or the reverse. Such facts have of late years assisted in the discovery and condemnation both of a farmer and of a medical student, and also in the case of the cook already mentioned, who cut off her child’s arm after the manner of carving the wing of a fowl. The existence of deformity, injury, and disease in the limbs should, of course, claim attention, but their relativity in an investigation of the kind is too apparent to require further comment.
Mutilation of the GENITAL ORGANS is not so common. Persons familiar with border warfare have observed the savage custom of cutting off the victim’s penis and placing it in his mouth. In more civilized communities the culprits are generally women in whom hatred and ferocity prompt an act that marks the evident satisfaction sought by the destructive instinct. Sometimes, however, the genital organs have been cut from the cadaver of a woman, presumably for the purpose of concealing traces of rape that may have preceded the murder. The signs furnished by the female genital organs as to virginity, maternity, and the menopause are so easily demonstrated at the necropsy as to become positive proofs of identity. The uterus loses both in size and weight with age. This along with hard, atrophied, and germless ovaries attests the stoppage of menstruation. The question of identity may turn on the age[415] at which menstruation ceases, as happened in an action of ejectment in the case of Doe on the demise of Clark vs. Tatom. The period known as change of life, when the uterus and ovaries lose their function, though placed at forty-five and fifty years, is quite uncertain. In spite of averages, menstruation is occasionally continued to seventy and upward.[585]
The signs furnished by the genital organs of the male are of less importance. Atrophy and diminished weight of the testicles and rarity or absence of the spermatozoids are indications of senility; although spermatozoids have been observed at ninety-four years. The structure of the spermatic cord at different periods of life from the last of intra-uterine to the first of extra-uterine life, in puberty, and in old age, is accompanied by characteristic modifications of development and regression, which are of interest on the question of medico-forensic diagnosis of identity, as shown by Dr. Pellacani.[586]
Congenital deformity of the genital parts, as epispadias or hypospadias; marks of circumcision, useful in India to identify Mussulmans above eleven years; traces of disease that may have left extensive cicatrices, as phagadenic chancre, suppurating buboes, etc., may also furnish characteristics of evidential value.
ENTIRE CADAVER DEAD BUT A SHORT TIME.
In the case of a body that has been dead a short time only, recognition from the features, even by the nearest relatives, is often a matter of the greatest difficulty. The change produced in the color and form of the body, especially after drowning, is a formidable obstacle to identification by likeness and general type of face. Pages could be filled with the mere mention of the multiplied instances of mistaken identity of the living, many of whom have been punished because they had the misfortune to resemble some one else. How much more careful, then, should be the medical examination of the remains in the progress of decay, with the distortion and discoloration of the features, and the consequent change or destruction of the peculiar expression of the countenance by which human features are usually distinguished and identified.
Among the innumerable instances of mistaken personal identity and cases of resemblance mentioned in history and fable, from the time of Ulysses down to the days of Rip Van Winkle’s dog Schneider, it appears that this animal is credited with more sagacity than man in the matter of recognizing his master even after years of absence. Indeed, recognition by animals may be considered a proof of identity. Many persons can recall instances of the kind, though perhaps not so dramatic as the one of the dog in the Odyssey, who recognized his master after twenty years of absence and died immediately thereafter.
As a matter of fact, time and circumstances will so alter resemblance as to account for some of these most striking proofs of the fallibility of human testimony that we see illustrated in chapters on mistaken identity. We easily forget the true image of persons and things, and time promptly modifies them. The evidence of the senses may be so little trusted in this regard that father, mother, husband, and nurse may attest a false identity in the case of their own children. A nurse has been known to testify to the identity of the severed head of a woman whom thirteen other persons were sure they recognized from characteristic signs, when the supposed victim put in an appearance and thus attested her own existence. The head of the unrecognized victim of this strange controversy is preserved in the museum of the Strassburg Faculty.
In another case of historical notoriety in France, forty witnesses on each side swore to the personality; while in the celebrated Tichbourne trial no less than eighty-five witnesses maintained positively, under the most rigid and scrutinizing cross-examination, that a certain person was Sir Roger Charles Doughty Tichbourne, a baronet; at the same time a corresponding number were equally unshaken in their conviction that he was a Wapping butcher, Arthur Orton.
Resemblances often bring about remarkable coincidences. A case is said to have occurred in Covington, Ky., where two men met, each the double of the other in form, stature, and feature, each having lost a right leg, amputated at the knee, and each being blind in the left eye from accident.
Puzzle and perplexity are not confined to remarkable cases and judicial errors; for so many people are unskilled in correct[417] observation that it is a matter of common occurrence for two individuals to be mistaken the one for the other. The writer for some years has frequently been mistaken for a certain naval officer he is said to resemble, while the officer in question has become so accustomed to being called “Doctor” that he answers to the title without protest.
A case that has of late been much quoted in the journals is that of Tiggs. What was supposed to be his mangled body was identified by his wife, and further identification was forthcoming from one of his children and the employer of the deceased. The coroner had granted a certificate for burial, and as the hearse neared the door, to the surprise of all parties the real Tiggs entered the house and gave a satisfactory account of his absence.
Most mistakes of this kind are the result of existing imperfections in the average human mind or in its use. So few people are skilled in minute observation that Lord Mansfield’s dictum regarding the “likeness as an argument of a child being the son of a parent” should be received with a certain degree of reserve, especially in the question of identity from likeness after death. In Ogston’s “Medical Jurisprudence” a case is related of a father who could not recognize the body of his son drowned at sea ten days previously. The mother, however, identified her boy from the existence of two pimple-looking projections on the front of the chest, which proved to be supplementary mammæ.
As a rule, the changes in the face and countenance two weeks after death are such that it is well-nigh impossible to establish identity from the features alone. Yet in exceptional cases the external results of putrefactive decomposition have been so delayed or modified as to produce very small changes in the features even after many years of burial. Bodies have been known to retain a remarkable state of preservation for long periods in such circumstances as burial in a peat bog, in the sand of the desert, and in the frozen ground of cold countries.
Even photography in the matter of identity is not to be trusted. Though an important accessory to other evidence, it is often, and very properly, objected to by lawyers on the ground of being incompetent, irrelevant, and immaterial. The[418] picture presented for comparison may not be an original one or it may have been taken years previously. The difficulty in recognizing one’s own most intimate friends from pictures taken only a few years back is a matter of common knowledge. Besides, the negative from which the picture was taken may have been retouched or altered, consequently it would not be the same as produced by the camera, and is, therefore, valueless as evidence. It is held to be incompetent to prove a photograph by merely asking a witness whether or not he recognizes the picture in question as that of a certain person.
In all cases where photographic pictures are required in a court of law the authorities are that the artist who took the picture must be produced and show that he took the picture, and that it is a correct representation of the original of which it claims to be a picture. If possible the negatives themselves should be called for and reproduced. Dr. Tidy states that he has known a volume of smoke appear in a print as issuing from a chimney, and used as evidence of the existence of a nuisance, when no smoke existed in the original negative. Only slight familiarity with the method of taking photographic pictures and the chemistry involved in the process suffices to show that many little details of sensitizing, exposing, developing, and printing greatly change the general appearance of the face. Some of the tricks that may be played with photography, illustrating its comparative incompetency as evidence in the matter of personal identification, I have seen in a series of pictures at the Department of Justice in Washington. All were photographs of the same person taken in such varying circumstances that no two are alike or recognizable as the same person, until scrutiny is brought to bear on the profile of the nose.[587] In considering photography in its bearing on this branch of medicine, it must also be borne in mind that a certain degree of imperfection arises from want of uniformity in the lenses of cameras. I have already mentioned the want of precision in photographing the skull, the common defect being central not orthogonal projection such as anthropometry requires.
SURFACE SIGNS OF IDENTITY.
Examination of the surface of the skin and of its appendages may in certain cases take decisive importance. Valuable medical proof is often furnished by scars, nævi, growths on the skin, pock-marks, traces of skin disease or of scrofula, and by the so-called professional stigmata which would suggest the trade, character of work, or occupation of the deceased. Thus cigarette-stains on the fingers of smokers, or silver-stains on the hands of photographers, the horny palm of the laborer, or the soft, delicate hand of one not accustomed to work, would be indicative. The alterations in the hand make it, so to speak, the seat of election; for in the majority of trades that may be mentioned it is the hand alone that bears the principal marks of daily work that indicate the calling. A case is recorded of a person who previously to his assassination was lame and walked with a crutch. Although the body was cut into fragments, an examination revealed in the palm of the hands characteristic callosities, showing prolonged use of support of this kind. In another instance of criminal mutilation a tattoo-mark found on the arm proved an overwhelming charge against the assassin and drew forth his confession. An accused was also convicted of murder after establishing the only missing link, the question of identity, which turned on the finding of cupping-marks and a tattoo on the body of the murdered man. Personal identity of the bodies of infants has, moreover, been proved by means of a small blister; by a patch of downy hair; by the similarity existing between two pieces of thread used to tie the umbilical cord; and by the severed end of that part of the funis attached to the infant fitting precisely to the corresponding portion attached to the after-birth. In addition to these a methodical examination may put in evidence other facts that may be derived from diverse influences that leave characteristic traces.
SIGNS FURNISHED BY MARKS, SCARS, STAINS, ETC., ON THE SKIN.
But of all the surface signs, whether congenital or acquired, that may throw light on the antecedents of the decedent, birth-marks, freckles, cicatrices, tattooes, and the professional signs[420] furnish the best indications. Birth-marks (nævi materni), from their supposed indelibility, have given rise to discussion at many celebrated trials. As a rule, these marks are permanent and seldom lose their distinctness, though in exceptional cases they may undergo atrophy in the first years of life. Hence testimony as to the existence of birth-marks may often be uncertain when it has reference to a period a long way back. In a recorded case of supposed recognition of a person having a mark of this kind on her face, the alleged victim turned up and established her identity as well as the fact that she did not have the birth-mark attributed to her.
Before the introduction of the electrolytic method it was customary to resort to cauterization, excision, vaccination, and tattooing the pigmentary spot in order to modify or remove these congenital marks. Such proceedings usually left more or less of an indelible scar which occasion might utilize in the matter of medico-legal diagnosis. The traces of nævi may, however, be entirely removed by electrolysis. I have recently seen a nævus of large dimension on the face of a young woman so completely destroyed as to leave no trace of the operation.
The possibility of the disappearance of a scar in such circumstances depends here, as it does in other instances, on the depth of the wound. A cicatrix being the result of a solution of continuity in the derma, the question arises whether a wound that has divided the derma without loss of substance and healed by first intention leaves any perceptible scar. Some are of the opinion that a cicatricial line persists, but grows fainter with time. Histological examination in a question of this kind might prove conclusive by showing the structure of the fibrocellular tissue that constitutes the cicatrix. In the case of very superficial burns or wounds, the scar may completely disappear if the epidermis alone or the superficial part of the derma is attacked; on the other hand, if there has been long suppuration or loss of substance from ulcers, chancres, or buboes, especially on the neck, groins, legs, or genital parts, traces of their lesion will be found. It may, therefore, be asserted as a general rule that all scars resulting from wounds and from skin diseases which involve any loss of substance are indelible. A scar on the face is one of the points at issue in the celebrated Hillmon case already mentioned.
As the matter of cicatrices is treated in the section on Wounds, further mention here would be superfluous.
Tattooing.
Of all the scars that speak, none in judiciary medicine affords better signs of identity by their permanency and durable character and the difficulty of causing their disappearance than those furnished by tattoo-marks.
The custom of tattooing having existed from the earliest historical epochs is of interest not only from an ethnological but from a medical and pathological point of view, while it is of great importance in its relation to medical jurisprudence in cases of contested personal identification which may be either established or refuted by this sign. So trustworthy is it in many instances as to become a veritable ideograph that may indicate the personal antecedents, vocation, social state, certain events of one’s life, and even their date.
Without going into the history of a subject mentioned by Hippocrates, Plato, Cæsar, and Cicero, it may be pertinent to say that tattooing is prohibited by the Bible (Leviticus xix., 28) and is condemned by the Fathers of the Church, Tertullian among others, who gives the following rather singular reason for interdicting its use among women: “Certum sumus Spiritum Sanctum magis masculis tale aliquid subscribere potuisse si feminis subscripsisset.” (De Virginibus velandis. Lutetiæ Parisorum, 1675, fº, p. 178.)
In addition to much that has been written by French, German,[588] and Italian authors, who have put tattooing in an important place in legal medicine, the matter of tattoo-marks a few years since claimed the attention of the law courts of England, the Chief Justice, Cockburn, in the Tichbourne case, having described this species of evidence as of “vital importance,” and in itself final and conclusive. This celebrated trial has brought to light about all the knowledge that can be used in the investigation of this sign as a mark of identity. Absence of the tattoo-marks in this case justified the jury in their finding that the defendant was not and could not be Roger[422] Tichbourne, whereupon the alleged claimant was proved to be an impostor, found guilty of perjury, and sentenced to penal servitude.[589]
The practice of tattooing is found pretty much over the world, notably in the Polynesian Islands and in some parts of Japan. It is, however, not found in Russia, being contrary to the superstitions of the people, who regard a mark of this kind as an alliance or contract with evil spirits. Its use appears to be penal only, and is limited to Siberian convicts. The degrading habit, confined to a low order of development, exists at the present time as a survival of a superstitious practice of paganism, probably owing to perversion of the sexual instinct, and is still common among school-boys, sailors, soldiers, criminals, and the lowest order of prostitutes living in so-called civilized communities. Indeed, unanimity of opinion among medical and anthropological writers assigns erotic passion as the most frequent cause of tattooing, and shows the constant connection between tattoo-marks and crime. Penal statistics show the greater number of tattooed criminals among the lowest order, as those who have committed crimes against the person; while the fewest are found among swindlers and forgers, the most intelligent class of criminals. Even amid intellectual advancement and æsthetic sensibility far in advance of the primitive man, such as exists in London and New York, for instance, are to be found persons who make good incomes by catering to this depraved taste for savage ornamentation. Persons who have been to Jerusalem may remember the tattooers, who try to induce travellers to have a cross tattooed on the arm as a souvenir of the pilgrimage. If a writer in the Revue des Deux Mondes, 15th June, 1881, is to be believed, it appears that the Prince of Wales on his journey to the Holy Land had a Jerusalem Cross tattooed on his arm, April 2d, 1862. The “Cruise of the Bacchante” also tells how the Duke of York was tattooed while in Japan.
The process is now rapidly done, an Edison electric pen being utilized for the purpose, and some of the wretched martyrs[423] have the hardihood to be tattooed from head to foot with grotesque designs in several colors. I know of several instances: one of a man in Providence, R. I.; another of a Portuguese barber, who has striped poles, razors, brushes, and other emblems of his calling over the entire body. Another man has likenesses of Abe Lincoln and of Kaiser Wilhelm of Germany on his respective shins. A Nova Scotian, tattooed from head to foot, has among other designs that of “St. George and the Dragon” on his back; while a Texas ranchman, six feet two inches tall, underwent the torture of eight weeks’ profanation of his body in order to appear in blue, brown, and red, with an irreverent image on his back of the Immaculate Conception and thirty-one angels.[590]
A singular mixture of erotic and religious emblems is often found among the varied and fantastic signs used in tattooing. I recall the case of a man who had represented on his back a fox-hunt, in which riders followed the hounds in full pursuit of a fox about to take cover in the anus. In another case of a man accused of criminal attempt on two little girls, examination of the sexual organs revealed a tattoo on the back of the penis representing the devil with horns and red cheeks and lips. When the little girls were asked if the accused had shown them his virile member, they answered, “This man unbuttoned himself and said to us: ‘I am going to make you see the devil.’” In the face of such affirmations, the accused confessed his crime and was condemned. Other tattoo signs of the grossest emblems of unnatural passion have been found among low prostitutes, pederasts, and tribades.
Statistics founded on numerous facts show many cases of tattooing of the penis and even of the labia majora in the lowest order of prostitutes, but these unclean images and revelations of lustful instinct do not occur in the same order of frequency as those noted on the forearm, the deltoid, or the inferior extremities. So valuable are these marks in their bearing on the class, vocation, character, and tastes of a person that the finding of anchors and ships would indicate a sailor; while flags, sabres, cannon, and other warlike signs would indicate a[424] soldier, etc. It is also noticeable that in the tattooing practised by lunatics the image relates in some way to the nature of the peculiar form of mental disease from which they suffer, and it is chiefly among the more severe and incurable cases of mental degeneration that these signs are found. (See Dr. Riva’s article, “Il tatuaggio nel Manicomio d’Ancona,” Cronica del Manicomio d’Ancona, November, 1888.)
Almost always the motive that prompts these disfigurements of the skin is the result of impulse, of thoughtlessness, or of orgy, and almost all the tattooed come to repent of their folly. The subject of détatouage has of late taken a polemic turn in some of the Continental journals. There are besides many cases on record of severe accidents and complications following the operation, such as severe inflammation, erysipelas, abscess, and gangrene. Dr. Beuchon gives statistics of forty-seven cases, in which four were followed by mutilation and eight by death either directly or in consequence of an amputation. A certain proportion of what is known as syphilis insontium is to be found among the reported statistics of tattooing. Dr. Bispham, of Philadelphia, informs me that while at Blockley Hospital he saw thirty cases of syphilis that had been communicated by the same tattooer.
Tattooing may sometimes be accidental. I have seen a departmental clerk with an elongated tattoo on the back of his hand caused by accidental wounding with an inked pen. A bursting shell during a naval engagement has caused a characteristic tattoo on the face of a well-known officer to be seen any day in Washington. Two cases of the bluish-black discoloration of the skin from taking nitrate of silver have also come under my observation. Both occurred in medical men, one of whom lives in Florida, the other in the District of Columbia. Silver discolorations of this kind are indelible, but I learn from one of these gentlemen that large doses of iodide of potassium cause temporary fading of the discoloration, which returns on stopping the medicine.[591]
The indelibility of tattoo-marks is such that their traces may be easily recognized in the cadaver, though in a somewhat[425] advanced stage of putrefaction. They have even been recognized on a gangrenous limb. Sometimes, however, it is impossible to recognize at first sight whether there has or has not been a tattoo. A strong light and a magnifying glass and a microscopic examination of the neighboring ganglia to detect the presence of coloring matter may assist in removing doubt. It has been found on the bodies of tattooed cadavers that the ganglia are filled with grains of coloring matter of the same nature as that employed in making the tattoo. Attempts to remove tattoo-marks generally leave a vicious scar that is equally indelible. An efficacious method is to tattoo the mark with a solution of tannin, which is followed by brushing over with nitrate of silver. A red cicatrix follows, and when the epidermis separates the tattoo disappears. A better method, however, is by means of the electric needle already mentioned in speaking of the electrolysis of nævi.
That a tattoo-mark may disappear by the effects of time and leave no trace is a matter that Cooper reports after examining the mutilated remains of a cadaver, and the statistics of Caspar, Tardieu, and Hutin place it as high as nine in the hundred. An officer of the United States Revenue Marine lately called my attention to several superficial tattooes on the back of his hand which had disappeared. The deeper ones, however, remained. The spontaneous disappearance of a tattoo seems to be possible when the operation has been done in such a superficial way as not to have passed the rete Malpighii, or when the tattooing has been done with some substance not very tenacious, as vermilion, which appears to be easily eliminated. But when the particles of coloring matter penetrate into the fibro-elastic tissue of the derma, the disappearance of the tattoo is rare.
In seventy-eight individuals tattooed with vermilion alone, Hutin found eleven upon whom the tattoo had disappeared. Out of one hundred and four tattooes made with a single color, India-ink, writing ink, blue or back, not a single one had completely disappeared. The results are identical if the tattooes are made with two colors. Thus in 153 tattooes with vermilion and India-ink, one instance showed a fading of the black, in another it had completely disappeared, the red being well marked; twenty times the red was partly effaced, the black[426] being well marked; and in sixteen cases the red had completely disappeared, the black remaining visible.[592]
A tattoo-mark may sometimes be altered, in which case it proves deceptive as an index. A workman changing his trade seeks to transform the insignia of his first calling into those of the second, or a criminal in order to avoid identity will make a change. In the former instance the transformation is not difficult to detect, but in the latter so much care is required to recognize the change that penal science has relegated the sign to a secondary place.
As to the length of time since a tattoo-mark has been executed, authorities are that it is impossible to tell after two or three weeks. Whether a tattoo-mark is real or feigned is easily settled by simply washing the part. This question, as well as that of the judicial consequences of such marks, is hardly pertinent to the matter in hand.
Value of Professional Stigmata.
The so-called professional signs are of undoubted value in the surface examination for establishing identity, but it does not seem that their importance warrants the extreme prolixity given to them by some Continental writers, and even by one in the city of Mexico, Dr. Jose Ramos.[593] For instance, it is pretended that cataract is more common among jewellers because of the fineness of their work; yet out of 952 cataracts, of which a record has been kept, only two cases occurred in jewellers. Besides, there is not one special sign or physical trace left on the body by which a prostitute may be known, notwithstanding the fact that in life the collective appearance would seldom deceive an experienced man.
Only in the case of sodomy, where anal coitus has been frequent, would characteristic signs be found. On anal examination of 446 prostitutes, Dr. Coutagne[594] found the signs of post-perineal coitus in 180. He cites the case of a young prostitute presenting the astonishing contrast of a gaping anus surrounded by characteristic rhagades, with the genital parts of an extreme freshness, a very narrow vagina, and non-retracted[427] hymen, constituting by their reunion a still firm ring. A fact yet more curious is shown by a specimen in the collection of the museum of the laboratory of legal medicine at Lyons. The genital organs of the cadaver of a woman of twenty-eight or thirty years showed a hymen intact and firm, but on examining the anal region it was surprising to find an infundibuliform deformity with all the signs of sodomitical habits, which of course rectified the opinion that had been made regarding the chastity of this woman.
Many of the signs enumerated as peculiar to different callings have no special anatomical characteristic that is easy to distinguish with precision, consequently they do not present a degree of certainty or constancy sufficient to be invoked as strong medico-legal proof of identity. Moreover, the effects of time or treatment may have caused alteration or disappearance of many of the signs in question, which would at best be of negative rather than of absolute value.
To arrive at an impartial appreciation of the relative value of the professional stigmata as signs of identity, a certain number of the signs should be thrown aside as illusory. Others, on the contrary, are durable, special, and constant, and assist in establishing the identity accordingly as the lesions or alterations are complete or evident; but it should be borne in mind that the physical alterations and chemical modifications resulting from the exercise of certain trades are not in our country so important from a medico-legal point of view as they are in Europe, where class distinctions are more defined.
VALUE OF STAINS AND DIFFERENT IMPRINTS.
In the same manner that a very small portion or fragment of the human body may suffice to establish the corpus delicti, so will minute remains or traces, as finger-marks, footprints, and other material surroundings, even smells or traces of perfume, be of great assistance to justice in determining the identity of both culprit and victim, and at the same time throw light on the attendant circumstances of the deed. The traces of a bloody hand or foot, smears of tar or paint, the various spots or stains found on fabrics, instruments, etc., may involve questions of great nicety the relativity of which is apparent,[428] especially in criminal trials. Newspapers have familiarized the public with many cases of the kind, in which medical experts have demonstrated blood and other stains with sufficient accuracy and positiveness to satisfy a jury. The Cronin case is a notable instance.
Imprints made by finger-tips are known to be singularly persistent. In four specimens of inked digit marks of Sir William Herschel, made in the years 1860, 1874, 1885, and 1888 respectively, though there was a difference of twenty-eight years between the first and last, no difference could be perceived between the impressions. The forms of the spirals remained the same, not only in general character, but in minute and measurable details, as in the distances from the centre of the spiral and in the direction at which each new ridge took its rise. Sir William Herschel has made great use of digit-marks for the purposes of legal attestation among natives of India.[595] The extraordinary persistence of the papillary ridges on the inner surface of the hands throughout life has been a theme of discussion by the Royal Society,[596] and Mr. Galton has devised a method of indexing finger-marks.[597]
The IMPRESS OF A NAKED FOOT covered with blood may serve to direct the investigations of justice. In a criminal affair in France, where eight individuals were implicated, comparative experiments upon the identity of the foot, made with a view to determine to which of the individuals ought to be attributed the bloody footprints found near a wardrobe, it was shown that a degree of recognition could be established on reproducing the footprints with defibrinated blood. From the eight imprints of the left foot of each individual, impregnated with blood, measures and comparisons could be made, thus helping to establish the difference or the resemblance with those found near the wardrobe.
Imprints thus obtained may be looked upon as a kind of documentary evidence, but too much importance should not be attached to them as articles tending to prove criminality. The futility of such evidence is shown in the varying sizes of different impressions of the foot of the same person—first in rapid[429] progression, secondly by standing, and third by slow advance. The results appear less sure in the case of footprints made in mud, sand, dust, or snow. Nevertheless many facts relating thereto may be noted with great certainty. The question has been mooted as to whether or not the impress left upon the soil gives always the exact dimensions of the foot that has made them. One side has contended that the footprints are a little smaller, while the other refutes this opinion and thinks that they are a little larger. The consistency of the soil, which does not seem to have entered into the discussion, doubtless accounts for the small differences that have given rise to this discrepancy of opinion. The outline of the sole of the foot and the relative position of the toes are more or less neatly designed as the ground is more or less wet or soft. The means employed for taking impressions of foot or other tracks in mud, etc., show considerable ingenuity on the part of those who have elaborated the subject. To discover foot-marks in mud, powdered stearic acid is spread over the imprint and a heat of at least 212° is applied from above. By this means a solid mould may be taken of the imprint. These researches have been extended to the exact reproduction of imprints left upon snow by pouring melted gelatine upon the imprint previously sprinkled with a little common table salt, which rapidly lowers the temperature of the snow about fifteen degrees and permits the mould to be taken without too much hurry. The study has been extended to the configuration of the plantar imprints in tabetics, but it does not appear so far to be of much medico-legal value.
The question may arise as to the length of time since the imprints were made. This would, of course, depend upon many circumstances, as weather, temperature, and the like. It is a fact that in Greenland footsteps in snow have been recognized many months after they were made. A few summers ago, on an arctic expedition, I climbed Cape Lisbourne, Alaska, in company with another person. The ground being thawed in many places, our feet left very decided imprints in the mud. A year afterward I visited the same spot, and on again making the ascent was astonished to recognize the footsteps made the year before.
Circumstances sometimes direct expert attention to vestiges[430] of other animals. The tracks of a dog or of a horse may become the object of a medico-legal inquest. The books record a case in which it was necessary to ascertain whether a bite had been made by a large or a small dog. This question was settled by producing the dogs and comparing their teeth with the scars. Persons familiar with border life know the importance of trails and the minute observation that is brought to bear on them by the experienced frontiersman. In following cattle-thieves and murderers, while with the Fourth United States Cavalry on the Rio Grande frontier, I have known the peculiarity of a horse’s footprint in the prairie to tell a tale of great significance.
Observation in this respect may extend to such apparently trivial objects as the tracks of wheels, as those of a wagon, a wheelbarrow, or a bicycle, or to the singular imprints left by crutches or a walking-stick. The imprint left in the ground by a cane usually occurs in the remarkable order of every two and a half or every four and a half steps. Investigation of such circumstances may result in material facts that may be of great assistance in establishing the relation of one or several persons with some particular act.
DEFORMITIES AND PATHOLOGICAL PECULIARITIES.
The existence of deformities or injuries is so apparent in serving to establish identity that it seems almost superfluous to mention them, except for the purpose of deciding whether the wounds were made during life or after death. In the matter of gunshot wounds on persons who took part in the late Civil War, many of whom unfortunately belong to the vagrant class and are often found dead, their wounds sometimes afford excellent means of identification. In many instances the multiple character of these wounds is almost incredible. When on duty at the Army Medical Museum, in connection with the preparation of the “Medical and Surgical History of the War of the Rebellion,” I saw a man who was literally wounded from the crown of his head to the sole of his foot, the scars being fifty-two in number.
Wounds made during life might show the suggillation peculiar to bruises or traces of inflammation. Besides, the gaping nature of the lips of the wound, the fact of hemorrhage[431] having taken place and the coagulation of the blood, the infiltration of blood into the cellular tissue, etc., are surgical facts that would leave but little doubt as to the infliction of the wounds during life.
The cause of death is often a difficult matter to determine, as it may have been accidental, suicidal, or the result of homicide. The causes relating thereto are, moreover, so many and varied that space and time compel a reference to other headings of this work. In forming an opinion as to the probable date of death the extent of putrefaction is the chief guide. If death is quite recent, we may be guided by the post-mortem rigidity or the extent to which the body has cooled. The march of putrefactive decomposition would, of course, be regulated by circumstances. It takes place very rapidly in persons who have succumbed to excessive fatigue or to any disassimilative excesses or derangement resulting in ante-mortem change of the tissues, such as those occurring in virulent or infectious diseases. The body of an infant decays more rapidly that that of an adult. The course of putrefactive phenomena is also influenced by the seasons, the extent of the exposure to air, and to other mesological causes. There is a manifest difference in the special putrefactive change accordingly as a body is buried in the earth, submerged in a fluid, thrown into a cesspool, or buried in a dung-heap.
In certain cases, especially where the body has been much mutilated, it may be desirable to know whether there was one or several murderers. While no definite rule can be laid down on this point, we are justified in supposing that there were two or more assassins when the body of the victim shows both gunshot and knife wounds, or that two persons were concerned in the dismemberment and mutilation of a body which shows the simultaneous presence of parts skilfully cut, while others show evident awkwardness.
Where there is more than one mortal wound on the same dead body, a question of medico-legal significance may arise. This occurred in the Burton murder case at Newport, R. I., in 1885, which gave rise to discussion of the following abstract question: “Whether it is possible for an individual, with suicidal intent, and in quick succession, to inflict a perforating shot of the head and another of the chest implicating the heart.[432] Or, reversing the proposition, is it incredible that a person bent on self-destruction can, with his own hand, shoot himself in the heart and in the head?”
After consideration of the case referred to and reversal of the previous decision of the coroner, the supposed suicide proved to be a homicide. Yet if the abstract question of possibilities is alone regarded, there is no doubt of the fact that a suicide could shoot himself in such manner, both in the head and the heart, or, changing the order, of shots in the heart and in the head. The number of cases recorded establishes beyond a doubt the feasibility of the self-infliction of two such wounds, and make it clear that the theory of suicide may be maintained in such circumstances.[598]
JUDICIAL ANTHROPOMETRY.
Of late years the subject of anthropometric identification has taken such a place before justice that it cannot be ignored by the medical legist. The facts of scientific anthropology have here been applied in such a way as to establish with great certainty both the present and future identity of individuals who attempt dissimulation of their name and antecedents. The method used principally in the identification of criminals and deserters from the army has been adopted in the public service[599] and by most municipalities, with the exception of New York, where the subsequent identification of persons connected with municipal affairs has been and may be a source of no little embarrassment.
The system is based on three recognitory elements: photography, anthropometric measurements, and personal markings, from which a descriptive list is made that gives absolute certainty as to individual identity.
Owing to the illusory nature of photography and the difficulty in finding the portrait of any given individual in the large and constantly increasing collection of a “rogues’ gallery,” the matter has been simplified and facilitated by grouping the photographic collection according to the six anthropological[433] coefficients of sex, stature, age, and color of the eyes. Each of these primordial groups is again subdivided in such a way as to reduce the last group to a small number, when the portrait is easily found and verified on comparing the measurements of the head, of the extended arms, the length of the left foot, and that of the left middle finger.
The photographic proof for each individual consists of two portraits side by side, one of which is taken full face, the other in profile of the right side. On the back of the photographic card is recorded with rigorous precision all personal markings or peculiarities.
The measurements, which can be made by any person of average intelligence in three or four minutes, are extremely simple. The right ear is always measured, for the reason that this organ is always reproduced in the traditional photograph which represents the right face. Other special measurements are taken on the left side. The height sitting, dimensions and character of the nose, color of eyes, etc., are also noted.
It is contended that by these measurements alone the identity of an individual whose face is not even known may be established in another country by telegraph. The application of the system has proved of great service in the apprehension of deserters from the United States army (when the authorities have been able to find the card), while it is claimed to have caused the disappearance of numerous dissimulators of identity in the prisons of Paris. The police authorities of that city report that out of more than five hundred annual recognitions by the foregoing means, not one mistake has yet occurred.[600]
To avoid a possible source of error mensuration of the organs and the ascertainment of their form may be resorted to in the case of a cadaver that is much decayed, or in one that has been purposely mutilated or burned by the assassin in order to prevent recognition. A sufficient number of cases may be cited in which the measurement of a limb or a bone of a deceased person known to have been lame or deformed during life has resulted in the establishment of identity or the reverse.
A mistake may be prevented in the case of supposed mutilation of a drowned body, which may have been caused by the[434] screw of a passing steamer. Other errors may result from carelessness, incorrect observation of signs, and neglect to follow the ordinary precautions that should obtain in all researches on identity of the dead body.
Certain circumstances indicative of the mental state of the culprit may throw light on the identity. A person of unsound mind would certainly be suggested as the perpetrator of such a deed as that of the woman already mentioned, who after killing and cutting up her infant, cooked portions of the remains with cabbage and served them at a meal of which she herself partook. Equally conclusive should be the inference in the case cited by Maudsley of a person who, for no ascertainable motive, kills a little girl, mutilates her remains, and carefully records the fact in his note-book, with the remark that the body was hot and good.
The handwriting left by the assassin might also furnish a strong presumption as to the existence of a mental lesion, since the writing of the insane is often characteristic, especially in the initial stage of dementia. I recall the case of a former patient, an aphasic, imprisoned for having stabbed a man in the abdomen and for having wounded his wife in such a way that her arm had to be amputated. Having lost the power to express himself phonetically, this man used a book and pencil, but his writing showed a degree of agraphia which alone would establish his identity beyond a doubt.
While it is quite possible that dishonest transactions, and even theft, may take place by telephone and the voices of the perpetrators may be unmistakable between distant cities, it is more likely that the phonographic registration of speech or other sound by means of a gramophone should become a matter of medico-legal investigation and a possible means that may lend great assistance in establishing personal identity. Although no precedent may be cited, it is not going into the domain of theoretical hypothesis to mention a discovery of such real scientific certainty that for years after death, and thousands of miles away, gives an indefinite number of reproductions that cannot possibly be mistaken by any one familiar with the voice before it had become “Edisonized.” Some gramophone disks lately shown me from Germany registered greetings and messages to relatives in Washington, who were[435] delighted to recognize the exact reproduction of familiar tones and accents of the Fatherland.
So limitless is the field of research in this direction that there is scarcely an anthropological, biological, or medical discovery that may not sooner or later be applied with profit in the investigations of personal identity where the combined efforts of an attorney and an expert are required.
After the most rigid and scrutinizing anatomical and material examination is made and the closest inquisition entered on, it may often be impossible to give a reasonable explanation for the cause of the physical facts observed. The medical man should remember that his is the one great exception to the rule that rigidly excludes opinions, and that scientific men called as witnesses may not give their opinion as to the general merits of the case, but only as to the facts already proved. This qualifying rule being altogether reversed in investigations into personal identity, and the physician’s opinion as to identity being indispensable, it becomes a matter of most serious import that this opinion should be grounded upon absolute and well-attested facts.
MEDICO-LEGAL DETERMINATION
OF
THE TIME OF DEATH.
BY
H. P. LOOMIS, A.M., M.D.,
Professor of Pathology in the University of the City of New York; Visiting Physician
and Curator to Bellevue Hospital, New York; Pathologist to the
Board of Health, New York City; President New
York Pathological Society, etc., etc.
MEDICO-LEGAL DETERMINATION OF THE TIME OF DEATH.
SIGNS OF DEATH.
The cessation of respiration and the absence of audible heart-beats are signs generally regarded as sufficient in themselves to determine the reality of death. But persons have been resuscitated from a state of asphyxia or have recovered from a state of catalepsy or lethargy in whom, to all appearances, the respiratory and circulatory processes have been arrested.
So it is advisable that we should be acquainted with some absolute tests of death which are not connected with the heart-sounds or the respiration.
It is well known that these important functions, although apparently held in abeyance, must be speedily re-established so as to be recognized, or death will rapidly follow. This condition of apparently suspended animation is seen among hibernating animals; the bear, for instance, will remain for four or five months without food or drink in a state of lethargy—the heart-action and respiration hardly appreciable. Yet it will be sufficiently rapid to sustain life during the slow metabolic processes. A number of well-authenticated cases are reported in which persons could slacken their heart-action, so that no movement of the organ could be appreciated. The case of Colonel Townsend, reported by Cheyne, is an example. He possessed the power of apparently dying, by slowing his heart so that there was no pulse or heart-action discernible. The longest period he could remain in this inanimate state was half an hour.
Instances have occurred in the new-born child where without question there have been no heart-beats or respiratory movements for a number of minutes, the limit being set at five.
These are exceptional cases, and it is setting at defiance[440] all physiological experience to suppose that the heart-action and respiration can be suspended entirely when once they are established, for a period as long. So, then, if no motion of the heart occurs during a period of five minutes—a period five times as great as observation warrants—death may be regarded as certain.
The respiratory movements of the chest are sometimes very difficult to observe. They can always be better appreciated if the abdomen and chest are observed together. There are two methods to determine whether respiration is absolutely suspended or not. First, by holding a mirror in front of the open mouth, observing whether any moisture collects on its surface. Second, by placing on the chest a looking-glass or basin of water, and reflecting from it an image by artificial or sun light. The slightest movement would be registered by a change in position of the image. While the writer considers the absence of heart-beats and of respiratory movement an absolute test of death, still some cases may occur in which the establishment of this test is very difficult, and the following additional tests may be employed:
1. Temperature of the body same as surrounding air.
2. Intermittent shocks of electricity at different tensions passed into various muscles, giving no indication whatever of irritability.
3. Careful movements of the joints of the extremities and of the lower jaw, showing that rigor mortis is found in several parts.
4. A bright needle plunged into the body of the biceps muscle (Cloquet’s needle test) and left there, showing on withdrawal no signs of oxidation.
5. The opening of a vein, showing that the blood has undergone coagulation.
6. The subcutaneous injection of ammonia (Monte Verde’s test), causing a dirty-brown stain indicative of dissolution.
7. A fillet applied to the veins of the arm (Richardson’s test), causing no filling of the veins on the distal side of the fillet.
8. “Diaphanous test:” after death there is an absence of the translucence seen in living people when the hand is held before a strong light with the fingers extended and in contact.
9. “Eye test:” after death there is a loss of sensibility of the[441] eye to light, loss of corneal transparency, and the pupil is not responsive to mydriatics.
POST-MORTEM CHANGES.
The human body after death undergoes certain changes which will be discussed under the following heads:
1. Cooling of the body.
2. Flaccidity of the body.
3. Rigor mortis.
4. Changes in color due to
(a) Cadaveric ecchymoses.
(b) Putrefaction.
Cooling of the Body.
Immediately after death there is a slight rise of temperature, supposed to be due to the fact that the metabolic changes in the tissues still continue, while the blood is no longer cooled by passing through the peripheral capillaries and lungs.
The body gradually cools and reaches the temperature of the surrounding air in from fifteen to twenty hours; this is the ordinary course, but the time may be influenced by a variety of causes, such as the condition of the body at the time of death, manner of death, and circumstances under which the body has been placed.
In certain diseases, as yellow fever, rheumatism, chorea, and tetanus, the temperature of the body has been known to rise as high as 104° F. and remain so for a time. Again, it has been observed that when death has taken place suddenly, as from accident, apoplexy, or acute disease, the body retains its heat for a long time. The bodies of persons dying from hanging, electrocution, suffocation, or poisoning by carbon dioxide, do not generally cool for from twenty-four to forty-eight hours, and cases are recorded where three days have elapsed before the body was completely cold. On the other hand, bodies dead from chronic wasting diseases or severe hemorrhage cool very rapidly, even in four or five hours.
In determining the temperature of a dead body the hand is not a reliable guide: the thermometer should always be used.
Flaccidity.
The first effect of death from any cause is general relaxation of the entire muscular system. The lower jaw drops, the eyelids lose their tension, the limbs are flabby and soft, and the joints become flexible.
In from five to six hours after death, and generally while the body is in the act of cooling, the muscles of the limbs are observed to become hard and contracted, the joints stiff, and the body unyielding. Muscles which are contracted in the death-agony do not necessarily become relaxed at any time.
The muscular tissues in the dead body can be considered as passing through three stages: (1) flaccid but contractile, (2) rigid and incapable of contraction, (3) relaxed and incapable of further contractility.
Rigor Mortis.
This is sometimes called cadaveric rigidity and occurs generally within six hours after death and disappears within sixteen to twenty-four hours. Many theories have been advanced to account for it, but the most probable one is that the rigidity is due to the coagulation of the myosin in the muscles by the weak acids which are no longer removed from the system; the muscles always give an acid reaction and are opaque instead of transparent; after putrefaction has set in ammonia is developed, the myosin dissolved, and so flaccidity results.
Rigor mortis occurs first in the muscles of the eyelid, next the muscles of the lower jaw and neck are affected, then the chest and upper extremities; afterward it gradually progresses from above downward, affecting the muscles of the abdomen and lower limbs. The rigidity disappears in the same sequence. The period after death when rigor mortis manifests itself, together with its duration, is chiefly dependent upon the previous degree of muscular exhaustion. Brown-Séquard has demonstrated that the greater the degree of muscular irritability at the time of death, the later the cadaveric rigidity sets in and the longer it lasts. He has also shown that the later putrefaction sets in, the more slowly it progresses.
The more robust the individual and the shorter the disease, the more marked and persistent is this muscular rigidity. It has been noticed that the bodies of soldiers killed in the beginning of an engagement become rigid slowly, and those killed late quickly. This explains the reason why bodies are sometimes found on the battle-field in a kneeling or sitting posture with weapons in hand.
If the rigidity of rigor mortis after it is once complete is overcome, as in bending an arm, it never returns; but if incomplete it may return. This will serve at times to distinguish real death from catalepsy and its allied conditions. While the average duration of rigor mortis has been given as sixteen to twenty-four hours, it must be remembered that in some cases it has been known to last only a few hours, as in death by lightning or by electrocution. In other cases it has persisted for seven and fourteen days.
This long continuance of rigor mortis has been noted in death from strychnine and other spinal poisons, in suffocation, and in poisoning by veratrum viride.
Atmospheric conditions modify to a large extent the duration of rigor mortis. Dry, cold air causes it to last for a long time, while warm, moist air shortens its duration. Also immersion in cold water brings on rigor mortis quickly and lengthens its duration.
Cadaveric Ecchymosis—Cadaveric Lividity or Hypostasis.
Within a few hours after death the skin of the body, which is of a pale, ashy-gray color, becomes covered by extensive patches of a bluish or purple color, which are most pronounced and are first seen on the back part of the trunk, head extremities, ears, face, and neck, and are due to the blood, before coagulating, settling in the most dependent parts of the body, producing a mottling of the surface with irregular livid patches. There is also a stagnation of blood in the capillary vessels, especially in those in the upper layer of the true skin or in the space between the cuticle and cutis. The discoloration continues to increase until the body is cold, when it is entirely arrested. Later on, just before putrefaction begins, the color[444] deepens, and the change appears to proceed from an infiltration of blood pigment into the dependent parts of the body.
At the same time the discolorations are appearing on the surface of the body, internal hypostasis is also taking place, most marked in the dependent portions of the brain, lungs, intestines, kidneys, and spinal cord.
This condition in the brain may be mistaken for so-called congestive apoplexy; in the lungs, for pulmonary apoplexy or the first stage of lobar pneumonia; in the intestines and spinal meninges, for the beginning of inflammatory changes.
The position of these hypostases will afford the best correction for this possible error. The appearances presented by cadaveric ecchymoses have often been mistaken for the effects of violence applied during life. Innocent persons have been accused and tried for murder or manslaughter on charges afterward proved to be groundless. Therefore it is of the utmost importance that the medical jurist should be able to distinguish between ante-mortem and post-mortem ecchymoses.
The following are the points of difference:
1. Situation. Post-mortem ecchymoses are seen on that portion of the body which has been most dependent, generally the posterior aspect, and they involve principally the superficial layers of the true skin; ante-mortem ecchymoses may occur anywhere, and generally the deeper tissues are discolored.
2. In cadaveric lividity there is no elevation of the skin and the discoloration terminates abruptly.
3. After cutting into the tissues where an ecchymosis has been produced by violence, the blood without the vessels is free in the tissue; this is not so in cadaveric ecchymosis.
4. Post-mortem ecchymoses are very extensive, ante-mortem generally limited in area.
A peculiar appearance of cadaveric lividity is observed in bodies which have been wrapped in a sheet and allowed to cool or that have cooled in their clothing. It occurs in the form of bands or stripes over the whole surface, and often gives an appearance as of a person flogged. The explanation of this appearance is that the congestion of the vessels takes place in the interstices of the folds, while the parts compressed remain whole. The unbroken condition of the cuticle, together with the other characteristics just mentioned, are sufficient to distinguish[445] these ecchymoses from those produced by violence. While cadaveric lividity is seen in all bodies after death, it is especially pronounced in those persons who have died suddenly in full health or by violence, as from apoplexy, hanging, drowning, or suffocation. It is very slight in the bodies of those who have died from hemorrhage or anæmia.
The time at which cadaveric lividity appears varies greatly. Casper, who has investigated the subject thoroughly, sets the time at from twelve to fifteen hours after death.
Putrefaction.
At a period varying from a few hours to three days after death, certain changes are seen in the human body which show that putrefaction has commenced. A change of color appears first upon the middle of the abdomen and gradually spreads over the rest of the body; it is first pale green, which gradually deepens, and finally becomes purplish or brown. This change in color is due to the action on the hæmoglobin of the gases developed by decomposition. Similar discoloration makes its appearance on the chest, between the ribs, on the face, the neck, the legs, and lastly on the arms, where it is more marked along the large venous trunks, and has sometimes been mistaken for marks of violence. The eyeballs become flaccid, and if exposed to the air the conjunctiva and cornea become dry and brown. Gases are formed, not only in the hollow organs of the abdomen but also in the skin. Those developed in the cavities of the head and face force frothy, reddish fluid or mucus from the mouth and nostrils, and may cause swelling of the features and protrusion of the eyes and tongue. It must be remembered that the gases while producing distention of the abdomen may also cause changes in the position of the blood and slight displacement of the organs; they may also force undigested food into the mouth and into the larynx, and so lead to suspicion of death from suffocation.
As putrefaction advances, after a period of five or six days the entire surface of the body becomes green or brown, the cuticle becomes loose and easily detached; the tissues flaccid and often bathed in a reddish serum in such situations as the neck, the groin, and the back part of the scalp. The thorax and[446] abdomen become enormously distended, the features distorted and scarcely recognizable, and the hair and nails loosened. Beyond this, it is impossible to follow the changes leading to disintegration with any degree of certainty. The changes which I have just described as produced by putrefaction are the ordinary ones seen in a body exposed to the air at a moderate temperature, but it must be remembered that the time and rapidity of the development of these changes may be influenced by a large number of factors, and that they are of very little importance in estimating the time of death. I have seen bodies buried two months that have shown fewer of the changes produced by putrefaction than others dead but a week.
The appearance of a body buried in a coffin will be as follows after a period varying from a few months to one or two years. The soft tissues will have become dry and brown and the face and limbs covered with a soft white fungus. Hard white crystalline deposits of calcium phosphate will be found on the surface of the soft organs, and when found on the surface of the stomach care should be taken not to confound them with the effects of poison. In time the viscera become so mixed together that it is difficult to distinguish them. For the most part the changes that take place in a body buried in a coffin are similar, but much slower, to those that occur if the body is exposed to the air or buried in soil. Even under apparently identical circumstances the most varied results have been observed, so it is not possible for a medical jurist to fix a definite period of death or the time of burial from the appearance of an exhumed body. For example, Taylor records a case where after thirty-four years’ interment an entire and perfect skeleton was discovered, surrounded by traces of shroud and coffin, while in an adjoining grave all that remained of a body that had been dead twenty-five years were the long bones and base of the skull, In one case a body was found well preserved after six years’ burial and in another after even thirty years’ interment.
This brings us next to a consideration of those factors that favor or retard decomposition.
Circumstances Favoring Putrefaction.
1. Temperature.—Putrefaction advances most rapidly at a temperature between 70° and 100° F. It may commence at any temperature above 50° F., but it is wholly arrested at 32° F. So one day’s exposure of a body in summer may effect greater changes than one week in winter. After freezing, putrefaction takes place with unusual rapidity upon the thawing out of the body. A temperature of 212° F. stops all putrefactive changes.
2. Moisture.—Putrefaction takes place only in the presence of moisture. An excess of moisture, however, seems to retard the process, possibly by cutting off the excess of air. The viscera according to the amount of water they contain decompose at different times after death—for instance, the brain and eye rapidly, the bones and hair slowly.
3. Air.—Exposure to air favors decomposition by carrying to the body the micro-organisms which bring about putrefaction; absence of air soon arrests the changes: this is seen in bodies hermetically sealed in lead coffins, which remain unchanged for a long period of time. Moist rather than dry air favors putrefaction by lessening evaporation. Air in motion retards while still air favors the change.
It is to be remembered that a body decomposes more rapidly in air than in water or after burial. Given similar temperatures, the amount of putrefaction observed in a body dead one week and exposed to the air will about correspond to one submerged in water for two weeks or buried in a deep grave for eight weeks.
4. Age.—The bodies of children decompose much more rapidly than those of adults; fœtuses still more rapidly. Aged bodies decompose slowly, probably on account of a deficiency of moisture. Fat and flabby bodies decompose quickly for the same reason.
5. Cause of Death.—In cases of sudden death, as from accident or violence, the body decomposes more rapidly than when death results from disease. Putrefaction sets in early in death from the infectious fevers, such as typhus, pyæmia, and typhoid fever, also in death from suffocation by smoke or coal gas, by strangulation or after narcotic poisoning. Those parts[448] of a body which are the seat of bruises, wounds, or fractures, decompose rapidly; this is especially seen in parts after a surgical operation.
6. Manner of Burial.—When a body is buried in low ground in a damp, swampy, clay soil, decomposition advances rapidly, as also when the grave is shallow so the body can be exposed to constant variations of temperature. A porous soil impregnated with animal and vegetable matter favors putrefaction, as also burying a body without clothes or coffin; this is especially seen where infants have been thrown into the ground and loosely covered with earth.
Circumstances Retarding Putrefaction.
1. The Temperature.—Below 32° F. and above 212° F. putrefaction is entirely arrested. The rapidity of the change considerably lessens as the temperature advances above 100° F. A remarkable instance of the preservative power of cold is given by Adolph Erman, who states that the body of Prince Menschikoff, a favorite of Peter the Great, exhumed after ninety-two years’ burial in frozen soil, had undergone hardly any change. Buried in hot sand as is seen in the desert, a body putrefies very slowly and generally becomes mummified.
2. Moisture.—Absence of moisture retards decomposition. In the dry air of the desert bodies have been preserved for a long period of time.
3. Air.—If access of air to a body be prevented in any way by its inclosure in a coffin, by closely fitting clothes, or by complete immersion in water, putrefaction is retarded.
4. Age.—Adults and old people decompose more slowly than children. Males are said to change less rapidly than females, lean people than fleshy ones.
5. Cause of Death.—Putrefaction is delayed after death from chronic diseases unless they are associated with dropsy. Poisoning by alcohol, chloroform, strychnine, and arsenic retard putrefaction. In the latter case the putrefactive changes seem to stop after they have once commenced, and often a result very similar to mummification is seen. Death from the mineral acids, especially sulphuric, appears to delay putrefaction.
6. Manner of Burial.—Putrefaction is retarded by burial[449] a short time after death; by interment on high ground, in dry, sandy, or gravelly soil; by having the grave deep, over six feet in depth if possible by the body being well wrapped and secured in a tight coffin, a lead one being the best in this respect. Lime or charcoal applied freely about a body will retard decomposition, as will also injection of the body through the arteries with such substances as arsenic, chloride of zinc, or antimony. The ultimate effect of putrefaction is to reduce all bodies to inorganic compounds, chiefly water, ammonia, and carbon dioxide. Three conditions are necessary for its establishment, (1) a given temperature, (2) moisture, (3) free access of air.
The order in which the various organs and tissues undergo decomposition, as given by Casper, who has investigated the subject carefully, is as follows: Trachea and larynx, brain of infants, stomach and intestines, spleen, omentum and mesentery, liver, brain of adults, heart and lungs, kidney, bladder and œsophagus, pancreas, large vessels, and last of all the uterus.
As the result of putrefaction, fluids, generally blood-stained, collect in the serous cavities of the body, and should not be confounded with serous effusions occurring during life. So also the softening of the organs and tissue resulting from decomposition should be carefully distinguished from those resulting from inflammation. These cadaveric softenings are most frequently found in the brain, spleen, and gastro-intestinal mucous membrane. Inflammatory softenings are differentiated by being rarely general but almost always limited, by the substance of the inflamed part being infiltrated with serum or pus and showing traces of vascular injection. In doubtful cases the pathologist should have recourse to the microscope.
As the result of putrefaction, various changes take place in the mucous membrane of the stomach and intestines which simulate the effects of poisons. The color of the stomach varies from red, which becomes brighter on exposure to the air, to a brown, slate, or livid purple. We can only presume that these color-changes are the result of irritant poisons when they are found in non-dependent parts and parts not in contact with organs engorged with blood, when they are seen soon after death, and when the membrane is covered with coagulated blood, mucus, or flakes of membrane.
Effects on Putrefaction of Submersion in Water.
There are certain modifications of the putrefactive changes when bodies have been submerged in water. In the first place, the changes are much less rapid; they often do not show themselves until about the twelfth day, and then as discolorations appearing generally first about the ears and temples, then on the face, from which they spread to the neck, shoulders, chest, abdomen, and finally to the legs. This is almost the inverse order of the putrefactive changes in bodies exposed to the air. As a result of the formation of gases, the body in a short time becomes buoyant; after floating on the surface of the water for a time, the gases escape and the body sinks, rising a second time when fresh gas has formed.
The rapidity of decomposition in water varies, being most rapid when the temperature is from 64° to 68° F. Stagnant as well as shallow water favors putrefaction. If a body becomes coated with mud the change is delayed. Submersion in a cesspool also retards it, and the conditions are such as to favor the formation of adipocere.
After a body has been removed from the water an exposure of a very few hours to the air causes rapid decomposition, so that in twenty-four hours more marked changes may occur than would have resulted from a fortnight’s longer submersion. The face soon becomes bloated and black, so that identification is well-nigh impossible. It is quite important in medico-legal cases to estimate the time which has elapsed since death in bodies found submersed in water. The following are the various changes ordinarily seen at different periods of time, as estimated by Devergie, who has especially investigated the subject:
First Four or Five Days.—Little change: rigor mortis may persist, particularly if the water is cold.
Fourth or Fifth Day.—Skin of the ball of the thumb and little finger, also the lateral surface of the fingers, begins to whiten. This whitening gradually extends to the palms of the hands and soles of the feet. The skin of the face will appear softened and of a more faded white than the rest of the body.
Fifteenth Day.—Face slightly swollen and red; a greenish[451] spot begins to form on the neck and skin of the mid-sternum. The skin of the hands and feet is quite white and wrinkled. The subcutaneous cellular tissue of the thorax is reddish and the upper part of the cortical substance of the brain of a greenish tint.
At One Month.—The face is reddish-brown, the eyelids and lips green and swollen, and the neck slightly green. A greenish discoloration is also seen over the upper and middle part of the sternum. The skin is wrinkled. The hair and nails still remain intact. The scrotum and penis are distended by gas. The lungs become very emphysematous and overlap the heart.
Saponification.
When the bodies were removed from the Cimetière des Innocents in Paris, in 1786, Fourcray observed that many of them had been converted into a substance which he termed ADIPOCERE. He gave it this name because it resembles both fat (adeps) and wax (cera). Under certain circumstances which will be considered later, it is known to be a late product of the putrefactive processes. Adipocere is a substance of a cheese-like consistency, yellow or yellowish-brown in color, and composed chiefly of a mixture of the fatty acids. Chevreul has shown by analysis that it is a true ammoniacal soap, but that when formed in water impregnated with lime a calcareous may be substituted for an ammoniacal base. This may take place either in a body exposed to river-water or buried in a grave wet by water containing calcium carbonate or sulphate. Saponification can only take place when animal fat is in contact with nitrogenous matter. Neither fat nor fibrin when kept separate will saponify. Skin deprived of all its fat will not be transformed into adipocere.
Saponification commences in the fat of the female breast, of the cheeks and other parts of the body where large accumulations of fat are found, such as around the kidneys and in the omentum. As fat is distributed extensively throughout the body, nearly all parts may undergo this transformation. Taylor gives the following conditions as favorable to the change:
1. Bodies of young persons, because the fat is abundant and chiefly external.
2. Bodies of corpulent adults.
3. Exposure of bodies to the soil of water-closets.
4. The immersion of bodies in water, the change taking place more rapidly in running than in stagnant water.
5. Humid soil, especially when bodies are placed in it one upon the other. In this case the lowest of them is first changed.
When a body has been completely saponified it may remain in this state for years. In one instance, after seventeen years’ burial many of the organs could still be recognized.
The time required for saponification to take place is sometimes of medico-legal importance. Three years are usually necessary for bodies buried in the earth. The change occurs more rapidly in water. Cases are recorded where the body of a new-born child was completely saponified in six weeks, and again, the change had commenced in a body which had been in the water about four months; but these are unusual cases.
DATA UPON WHICH OPINION AS TO TIME OF DEATH IS FORMED.
The changes which take place in a body before putrefaction sets in may enable a medical jurist to form an opinion as to the probable time which has elapsed since death; yet it must be remembered, to pronounce the time which has elapsed can only be done approximately, for very many conditions will have to be considered, which will vary in each individual case. The importance of considering the minutest detail is well illustrated by the death of Prince de Condé, Duke of Bourbon, who was found dead in his bedroom in the chateau of St. Cyr. When discovered at 8 o’clock in the morning, the deceased was found partly undressed, hanging by his cravat to one of the window shutters. The body was cold and the lower extremities rigid. As in asphyxia from hanging the warmth of the body is usually preserved longer than under common circumstances, viz., from twelve to fifteen hours, before which period rigidity is seldom complete, the medical examiner inferred that the deceased must have died very soon after he retired to his bedroom on the previous night. As this was proven to have been 10 P.M., it followed that only ten hours had elapsed—a short time for cooling and rigidity to have taken place. It was thus rendered probable[453] that the hanging took place soon after deceased reached his bedroom. It was alleged that the duke had been murdered, and that his body had been afterward suspended to create a suspicion of suicide. The condition of the body was, among other things, adverse to this opinion. From 10 to 12 o’clock it was proved there were numerous attendants moving about near the duke’s apartments. They would have heard any unusual noise the duke must have made in resisting his assailant. But no noise was heard in the room at that or any other time, and the presumption of this being a homicide was thus strongly rebutted.
Cadaveric rigidity, while often it will aid to, is not a reliable guide. When once it is established it may remain two, three, or four days, according to the season of the year and other circumstances, and when it exists there is no rule by which it can be determined whether a body has been in this state three hours or three days.
Putrefaction, while appearing on an average, under a mean temperature, in from three to six days, is yet influenced by many circumstances. The heat and moisture of the surroundings, the age, sex, amount of flesh on the body, mode of death, position and coverings of body, all must be considered.
The temperature of the body aids us, yet the retention of warmth by the abdominal viscera may be met with in a marked degree twenty hours after death; in one case, personally known to me, the thermometer registered 76° F. seventeen hours after death.
The temperature of the body, its rigidity, and the evidences of putrefaction all furnish data from which we can estimate the probable time which has elapsed since death. It must be remembered that no one of them furnishes any positive proof.
Some medical jurists have attempted to give a more definite character to these changes in the recently dead body by dividing the interval between the stopping of the heart’s action and the beginning of putrefaction into three periods. In the first, the warmth, pliability, and muscular irritability remain. In the second, these conditions are lost and the body is cold and rigid. In the third, the body is cold and pliant, the muscles are relaxed, and the joints are flexible, the cadaveric rigidity having entirely ceased.
There can be no doubt about the existence of these stages, but when we come to define the precise time at which one begins and the other ends, we find it impossible. For example, the first stage embraces a period which cannot be more closely defined than by stating that the person may have been dead from a few minutes to twenty hours—a statement too vague to be upheld by a counsel who defends a prisoner.
The changes which take place in these periods and the average time they last have been given as follows by Devergie:
First Period, Few Minutes to Twenty Hours.—Characterized by warmth of the body and general or partial relaxation of the voluntary muscles. To what portion of this period the special case belongs must be estimated according to the degree of heat in the trunk and extremities and the degree of rigidity in the muscles, the neck and the jaws commonly showing this condition first, the legs last. Warmth of the body rarely remains as long as twenty hours; in general it is sensibly cold in from ten to twelve hours. During this period the muscles are susceptible of contraction under the galvanic current, and in the early stage under the stimulus of blows.
Second Period, Ten Hours to Three Days.—The body is perfectly cold throughout and rigidity is well marked. The muscles no longer respond to stimuli. The duration of this period seems long, yet in one instance the body will be found cold and rigid nine hours after death. Again, cooling and rigidity may not come on for three or four days.
Third Period, Three to Eight Days.—The body is perfectly cold. The limbs and trunk pliant and free from cadaveric rigidity. The muscles are not capable of contracting. In summer this period is much shorter; often it will come on before three days.
Putrefaction commences when a body is kept under the most favorable conditions, in from six to twelve days, as a slight greenish discoloration of the abdomen which gradually spreads throughout the body. The time at which putrefaction shows itself and the rapidity with which it advances is dependent upon so many factors, many of which it is impossible often for the medical examiner to ascertain, that too much reliance must not be placed upon it. Casper estimates the following to be the average changes generally found in the periods of time given:
Twenty-four to seventy-two hours after death a slight green color is visible over the centre of the abdomen. The eyeballs are soft and yield to external pressure.
Three to five days after death the green color of the abdomen becomes intensified and general, spreading if the body be exposed to the air or buried in the ground in the following order: genitals, breast, face, neck, upper and lastly lower extremities.
Eight to ten days after death the discoloration becomes more intense, the face and neck presenting a shade of reddish-green. The ramifications of the superficial veins on the neck, breast, and limbs become very apparent. Finally the patches congregate. Gases begin to be developed and distend the abdomen and hollow organs and to form under the skin in the subcutaneous and intermuscular tissue. The cornea falls in and becomes concave. The sphincter ani relaxes.
Fourteen to twenty-one days after death the discoloration over the whole body becomes intensely green, with brownish-red or brownish-black patches. The body is bloated and appears greatly increased in size from the development of gases within the abdomen, thorax, and scrotum, and also in the cellular tissue of the body generally. The swollen condition of the eyelids, lips, nose, and cheeks is usually of such extent as to obliterate the features and to destroy the identity of the body. The epidermis peels off in patches, while in certain parts, more particularly the feet, it will be raised in blisters filled with red or greenish liquid, the cuticle underneath frequently appearing blanched. The color of the iris is lost. The nails easily separate and the hair becomes loosened.
Fourth to sixth month after death the thorax and abdomen burst and the sutures of the skull give way from the development of gases within the head. The viscera appear pulpy, or perhaps disappear, leaving the bones exposed. The bones of the extremities separate at the joints. At an advanced stage the soft parts gradually disappear.
In giving an opinion as to how long a time has elapsed since death when a body has undergone marked putrefactive changes, we must consider carefully not only the conditions of the organs, but the mode of death and the “surroundings.” By these I mean the quantity of clothing worn, the depth of the[456] grave in which the body has been interred, the season of the year, the heat and moisture of the atmosphere. The question sometimes presents itself to the medical examiner, Of two persons found dead, which died first? The importance of this point was well illustrated in the “Lizzie Borden case.” By a careful consideration of all the conditions presented by each body in the ways I have indicated, the question will not ordinarily be a difficult one to decide.
THE
MEDICO-LEGAL CONSIDERATION
OF
WOUNDS,
INCLUDING
PUNCTURED AND INCISED WOUNDS, AND WOUNDS
MADE BY BLUNT INSTRUMENTS OTHER
THAN GUNSHOT WOUNDS.
BY
GEORGE WOOLSEY, A.B., M.D.,
Professor of Anatomy and Clinical Surgery in the Medical Department of the University
of the City of New York; Surgeon to Bellevue Hospital; Member
Medical Society of the County of New York, New York Academy
of Medicine, New York Surgical Society, etc., etc.
WOUNDS.
GENERAL CONSIDERATIONS. THE DIFFERENT KINDS OF WOUNDS.
The surgical and medico-legal ideas of wounds are quite different, the latter including the former as well as other varieties of injuries.
Definitions.—Surgically a wound means a solution of continuity and refers to every such lesion produced by external violence or developing spontaneously. The medico-legal acceptation of the term is much broader and includes any injury or lesion caused by mechanical or chemical means. Vibert[601] quotes Foderé as defining a wound medico-legally as, “Every lesion of the human body by a violent cause of which the results are, singly or combined, concussion, contusion, puncture, incision, tear, burn, twist, fracture, luxation, etc.; whether the cause is directed against the body or the body against the cause.” The same author quotes another definition of a wound as, “Every lesion however slight, resulting in concerning or affecting the body or health of an individual.” Taylor[602] defines a wound in a medico-legal sense as “a breach of continuity in the structures of the body whether external or internal, suddenly occasioned by mechanical violence.” Thus, the term wound in its medico-legal acceptation includes not only surgical wounds but contusions, fractures, burns, concussion, etc. In France at least the voluntary inoculation of syphilis has been considered as coming under the category of wounds.[603]
Medico-legally, the severity of a wound is much more important than the kind of wound. Thus we may consider wounds according to their comparative gravity, as mortal, severe, or slight.
A mortal wound is one which is directly fatal to life in a comparatively short time, usually from hemorrhage, shock, or the injury of a vital part. A wound may result fatally without being a mortal wound, as when a slight wound causes death on account of some wound infection.
Severe wounds, or “wounds causing grievous bodily harm,” as they have long been called, do not put life in imminent danger, though they may be inconvenient or detrimental to health. Pollock, C. B., says that a wound causing grievous bodily harm is “any wound requiring treatment.”
A medical opinion or certificate may be required as to the danger of a given wound, and on this opinion may depend the question of bail for the prisoner. By the danger of a wound in such a case is usually meant imminent danger, as any wound may be remotely dangerous to life.
Slight wounds, as already stated, may result fatally under certain conditions. Under the French practice a slight wound is one which does not incapacitate one from work for more than twenty days. Looked at in another way, slight or severe wounds may be classified according as they are completely curable, leaving no infirmity or disturbance of function, or not completely curable. The latter are such as are necessarily followed by permanent or temporary infirmity.
The question as to the severity of any given wound may sometimes be left to the jury to decide from the description of the wound, or a medical opinion may be required.
Although the intent of the assailant is often of equal or greater importance than the severity or kind of wound, yet this can only occasionally be inferred from the surgical aspects of the wound.
The classes of wounds to be treated in the following pages are incised and punctured wounds and wounds with blunt instruments, some of the characteristics of which we will now consider.
Incised wounds are such as are produced by a cutting instrument, and they are distinguished by the following characteristics: They measure more in length than in the other dimensions. They are usually straight in direction, though not infrequently curved, and they may even be zig-zag, especially where the skin lies in folds. The edges of an incised[461] wound are linear, and show no signs of contusion. They are either inverted or everted and the edges and sides of the wound are retracted. The eversion of the skin is due to its elasticity, but in some regions of the body, e.g., in the scrotum, etc., the skin is inverted owing to the contraction of the muscle fibres immediately beneath. The gaping of the wound is due to the retraction of the divided muscles and fibrous structures. It varies according as the muscles are cut directly across or more lengthwise, and in proportion to the distance of the wound from the points of attachment of the muscles.
The fibrous tissues, fasciæ, and aponeuroses retract less, and so give a somewhat irregular surface to a large wound.
Ogston[604] divides incised wounds into three parts, the commencement, centre, and end, of which the end often has two or more serrations differing from the commencement, which has but a single point. There are often one or more slight, superficial, tentative incisions situated almost always, though not invariably, near the commencement.[605] The deepest part of the wound is more often near the commencement. If there are angular flaps on the edges their free angles point to the commencement of the wound.
Coagula and clots of blood are to be found in the wound, more or less filling it up if it has not been interfered with. On examination the ends of the divided vessels are found plugged with clots which may protrude somewhat from their openings.
If the wound is seen very shortly after its infliction, hemorrhage is in progress, and the divided arteries show their position by their individual, intermittent jets of blood. The severity of incised wounds depends upon the amount of hemorrhage, which is greater the deeper and larger the wound, and the more vascular the tissues in which it occurs, especially if large and important vessels are concerned. In the latter case an incised wound may be very rapidly fatal.
Incised wounds present the least favorable conditions for the spontaneous arrest of hemorrhage of any form of wounds. The edges of an incised wound may be quite rough and even dentated or lacerated if the edge of the weapon be rough and irregular.
The kind and condition of a weapon which has produced a[462] given incised wound may often be learned by an examination of the characteristics of the wound.
Weapons cutting by their weight as well as by the sharpness of their edges, such as axes, etc., may cause a certain amount of contusion about a wound; they crush the soft parts to a certain extent, and the bones may be indented or even fractured.
Wounds caused by fragments of bottles, pieces of china, earthenware, or glass, though strictly speaking incised wounds, are often curved, angular, and irregular, and their edges jagged and contused.
Wounds caused by scissors may sometimes be of the nature of incised wounds. When they present a double wound of triangular shape, with the apex of the triangle blunt, they are more of the nature of punctured wounds. In general a “tail” or long angle in the skin at one end of an incised wound indicates the end of the wound last inflicted, and some light may thus be thrown upon the inflicter of the wound.
Incised wounds present very favorable conditions for healing by primary union, but often fail in this and heal by secondary union. When an incised wound fails to unite by primary union, bleeding continues for several hours or even as long as a day, the blood being mixed more or less with a serous discharge. The latter continues until the third day or so. By the fourth or fifth day the surface has begun to granulate, and there may be a more or less profuse purulent discharge from the surface. The granulating surfaces do not necessarily discharge pus, however. For some days, therefore, after the infliction of an incised wound, or until the surface is covered with granulations, the characteristics of the wound permit of a diagnosis as to the nature of the wound.
The diagnosis of an incised wound is generally without difficulty. Some wounds by blunt instruments, however, in certain regions of the body, resemble incised wounds very closely. Such instances are found where a firm, thin layer of skin and subjacent tissue lies directly over a bony surface or a sharp ridge of bone. These are seen most often in the scalp or in wounds of the eyebrow where the sharp supra-orbital ridge cuts through the skin from beneath. The diagnosis of an incised wound can often be made with great probability from the[463] cicatrix. This is especially the case if the wound has healed by primary union and the cicatrix is linear.
The prognosis in incised wounds is good as to life unless a large vessel has been divided or unless an important viscus has been penetrated. The prognosis as to function varies with the position and extent of the wound, and the circumstance of the healing of the wound.
Punctured Wounds, Stabs, etc.—These are characterized by narrowness as compared to depth, though the depth is not necessarily great. They are more varied in character than incised wounds owing to the great variety of form of the weapons by which they may be made. From the form, etc., of a particular wound we may often infer the variety of weapon by which it was produced. According to the weapon used, punctured wounds have been divided into several classes, of which M. Tourdes distinguishes four: 1st. Punctured wounds by cylindrical or conical instruments like a needle. If the instrument be very fine like a fine needle, it penetrates by separating the anatomical elements of the skin, etc., without leaving a bloody tract. Such wounds are generally inoffensive, even when penetrating, if the needle is aseptic, and they are difficult to appreciate. On the cadaver it is almost impossible to find the tract of such a wound. If the instrument be a little larger it leaves a bloody tract, but it is difficult to follow this in soft tissues, more easy in more resistant structures, such as tendon, aponeurosis, cartilage, or serous membrane.
If the instrument be of any size this variety of punctured wounds presents a form quite different from that of the weapon. Instead of a round wound it is generally a longitudinal wound with two very acute angles and two elongated borders of equal length, showing but little retraction. This is the shape of the wound even when the instrument producing it is so large that the resulting wound resembles that made by a knife (see Fig. 2). The direction of the long axis of these wounds varies in different parts of the body and is uniform in the same part. Their shape and direction are explained by the tension of the skin or still more clearly by the direction of the fibres of the skin, just as with the same round instrument in a piece of wood a longitudinal opening or split would be made parallel to the grain (see Fig. 1). In some regions, as near the vertebræ, the fibres[464] may run in different directions, and the resulting wound is stellate or triangular in shape as if a many-sided instrument had caused it. As the direction of the fibres of the various tissue layers, such as aponeuroses, serous and mucous membranes, etc., may be different, a deep wound involving several such layers would have a different direction for each layer. In illustration of this, examine the figure of a wound through the wall of the stomach (see Fig. 3).
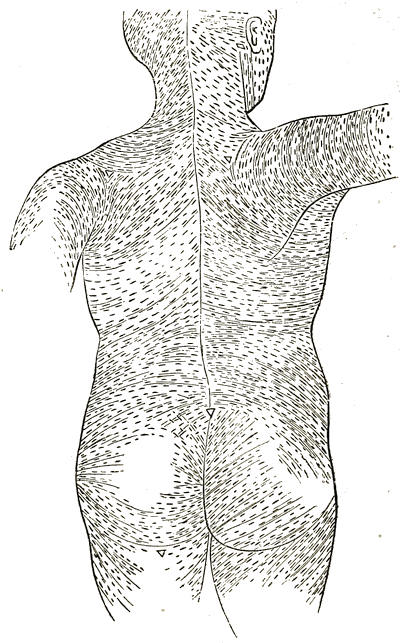
Fig. 1.—Direction of the Long Axis of Wounds of the Back caused by Conical Instruments.
(After Langer.)
The wounds above described when large are smaller than[465] the weapon, as the splitting of the skin has certain limits and also owing to the elasticity of the skin, which is put on the stretch by the weapon and relaxed on its withdrawal. When such wounds are small they are larger as a rule than the instrument causing them.
Fig. 2.—Slit-like Wound caused by a Pointed Conical Instrument 2.5 cm. in Diameter. Natural size.
Fig 3.—Wounds of Stomach Wall by a Conical Instrument, showing the Different Direction of the Long Axis of the Wounds in Different Layers.
Fig. 4.—Stab-Wound of the Skin with a Knife a Few Minutes before Death.
—————————
2d. Punctured wounds by instruments both sharp pointed and cutting, like a knife or dagger. If these wounds are perpendicular to the surface, they have more or less the form of the weapon used. The angles may show whether the knife, etc., had one or two cutting edges, but even though the back of the knife is broad the wound may resemble one caused by a double-edged weapon. Thus stab-wounds from a common pocket-knife show only exceptionally a wedge-shape, but regularly a slit, the edges of which are slightly curved to one another and end in two acute angles. The reason of this lies in the fact that the wound is only caused by the cutting edge of the knife, so that we cannot tell as a rule which angle was occupied by the back of such a knife (Figs. 4 and 5). The depth of these wounds may equal the length of the weapon or be almost any degree less, but the depth may[466] even be greater than the length of the weapon by reason of a depression of the parts at the time of the blow. The wound is often shorter and broader than the weapon causing it, though more often it is larger than the weapon from the obliquity of the wound and the movement of the weapon on being withdrawn. The wound is smaller than the instrument where the parts are on the stretch at the time the wound is inflicted.
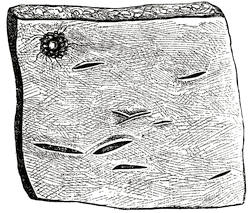
Fig. 5.—Nine Suicidal Stab-Wounds in the Region of the Heart made by a Knife used for Cutting Rubber.
This variety of punctured wounds may resemble the former class in the direction of its long axis, if the cutting edge of the instrument is blunt. The regularity and smoothness of the edges distinguish them from certain contused wounds.
3d. Wounds made by instruments with ridges or edges, files, foils, etc. If the edges are cutting the wound presents more or less the shape of the weapon (Fig. 6). But this is not always so, probably from the instrument puncturing obliquely or from the tissues being unequally stretched (Fig.7). If the edges are not cutting the wound resembles those of the first class, though the edge often presents little tears, and the wound may thus be more or less elliptical with two unequal angles. The wound of entrance and exit may be different.
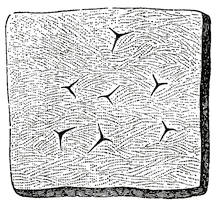
Fig. 6.—Stab-Wounds caused by a Three-Sided Sharp-Edged Pointed Instrument.
4th. Irregular perforating instruments, the wounds from which resemble contused wounds.
Contusions and Contused Wounds.—A contusion is a wound of living tissues by a blow of a hard body, not sharp-edged or pointed, or by a fall, crushing, or compression, and without solution of continuity of the skin. A contusion usually involves a moderately large surface in comparison to the two other classes of wounds. Contusions are of all degrees of severity. If the blow or injury is slight, there is only slight redness and swelling of the skin with pain, disappearing in a few hours, and leaving no traces. If the blow be harder it produces more or less crushing of the tissues, accompanied by ecchymosis with or without a wound or excoriations of the skin, etc. The contusion may have the shape of the contusing body, such as a whip, the fingers, etc.
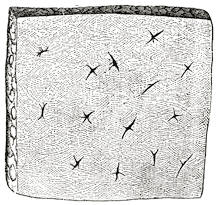
Fig. 7.—Stab-Wounds caused by an Eight-Sided Sharp-Edged Instrument. Some show a transition stage to wounds made by a conical instrument.
Ecchymosis.—This is characteristic, as a rule, of contused wounds. It consists in the infiltration of blood into the tissues, especially the cellular tissues. The source of the blood is from the rupture of blood-vessels, and the size of the ecchymosis varies partly with the number and size of the blood-vessels, or with the vascularity of the part. The size of the ecchymosis also varies with the looseness of the tissues into which it is infiltrated. This looseness of the tissues may be natural as in the scrotum and eyelids, or it may be due to the attrition of the tissues caused by the blow. An ecchymosis is larger when the contused parts cover a bony or resisting surface, and there may be no ecchymosis whatever, even from a severe blow, where the underlying parts are soft and yielding, as is the case with the abdominal parietes. Here we may have rupture of the viscera without any signs of ecchymosis superficially. An ecchymosis may be infiltrative or it may mostly occupy a cavity usually[468] formed by a traumatic separation of the tissues; this is especially the case in the scalp and extremities when the injury is severe. These tumors, which are called hematomata, may be rapidly absorbed or they may remain a long time and occasionally suppurate. Sometimes the anatomical conditions, especially of the connective-tissue spaces, allow the extension or migration of the ecchymosis under the action of gravity, even to a considerable distance. When it meets an obstacle it accumulates above it, as in the inguinal region for abdominal ecchymosis and at the knee for those of the thigh. The course along which the ecchymosis travels is indicated externally by a yellowish stain, soon disappearing, so that soon no sign persists at the site of injury, but only below where the blood is arrested.
An ecchymosis becomes visible at varying times after the injury according to the depth of the ecchymosis and the thinness of the skin, for the ecchymosis is mostly beneath, not in the skin. If the ecchymosis is superficial it shows in one or two hours or even in less time where the skin is very thin, as in the eyelids and scrotum. In such cases it increases for thirty or forty hours and disappears in a week, but may last longer, i.e., as long as fifteen to twenty-five days.
An ecchymosis may not show at the point struck, at least not until several days have elapsed, or it may only show on the under surface of the subcutaneous fat until it has imbibed its way, as it were, to the surface. This may explain the discrepancy in the description of an injury examined by two medical experts at different times.
If an ecchymosis is extensive and deep, especially if it occupies a cavity, there may be nothing to see in the skin for four or five days, and then often only a yellowish discoloration instead of a dark blue color. In such cases, too, the appearance in the skin may be more or less remote from the injury, having followed the course of the least anatomical resistance. Between these two extremes, an ecchymosis may become visible at almost any time. Rarely an ecchymosis occurs only deeply between muscles (pectorals, etc.) and not superficially at all.
The extravasation of blood which forms an ecchymosis has sometimes been given different names, according to its extent or position, for instance, parenchymatous or interstitial hemorrhages or apoplexies, suffusions, ecchymoses, petechiæ or vibices.[469] All such may, however, be called ecchymoses or hematomata. When blood is effused into the serous cavities of the body, special names are sometimes applied according to the position, such as hemothorax, hematocele, etc.
The color of an ecchymosis is at first a blue-black, brown, or livid red. This color changes first on the edges, later in the darker centre, and becomes in time violet, greenish, yellow, and then fades entirely. This change in color is owing to a gradual decomposition of the hæmoglobin of the blood. We can tell the age of an ecchymosis from its coloration only within rather wide limits, for the rapidity of change of color varies widely according to a large number of circumstances, especially according to whether the ecchymosis is superficial or deep. We can only say that the first change, i.e., that to violet, in a superficial ecchymosis, occurs in two or three days.
As an exception to the above color change, we may mention subconjunctival ecchymosis, which always remains a bright red, as the conjunctiva is so thin and superficial that the coloring matter of the blood is constantly oxidized.
The form of an ecchymosis often reproduces well enough that of the instrument, except if the latter be large it cannot all be equally applied to the surface, and its form is not distinctly shown by that of the ecchymosis. After its first appearance an ecchymosis spreads radially, the edges becoming less clear. This change occurs more rapidly the looser the surrounding tissues, and at the end of a few days the first form of an ecchymosis may be changed, so that an examination to determine the nature of the weapon should be made as early as possible.
Ecchymoses are more easily produced in the young, the aged, and in females, also in the case of such general diseases as scurvy, purpura, hemophilia, etc. In fact, in the last three classes they may occur spontaneously. This fact should never be lost sight of, as the attempt may be made to explain a traumatic ecchymosis in this way. The diagnosis between the traumatic variety and such cases of spontaneous ecchymoses is, in general, easy, for in the latter case their number, form, size, and occurrence on parts little exposed to injury and on the mucous membranes, as well as the general symptoms of the disease, leave little or no room for doubt.
From an oblique or glancing blow a considerable area of[470] skin may be stripped up from its deep attachments forming a cavity which may be filled by a clear serous fluid alone, or with some admixture of blood. These cases have been studied especially by Morel Lavallée and Leser, and the fluid has been thought to be lymphatic in origin, hence the name “lymphorrhagia.” Carriage accidents, especially where the wheels do not pass directly but obliquely across or merely graze the body, are especially liable to show this form of extravasation, which is thought to be more common than is generally supposed, being often obscured by a small quantity of blood.
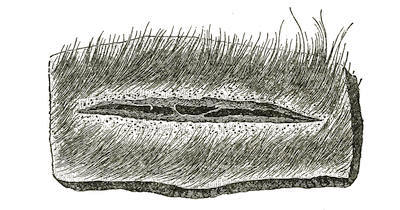
Fig. 8.—Linear Wound with Nearly Clean-Cut Edges, with Strands of Tissue bridging across at the Bottom and caused by a Fall on the Head on a Smooth Surface.
Contused Wounds.—If with the contusion we have a solution of continuity of the skin, then we have a contused wound. This may sometimes resemble an incised wound if the weapon has marked angles or edges, as a hammer, or, as we have already seen, in wounds of the scalp or eyebrow (Fig. 8). Careful examination, however, by a small lens if necessary, is sufficient to distinguish them if they are fresh. If they are four or five days old and have begun to granulate, it may be impossible to distinguish them. Contused wounds present on examination small tears on the edges which are widely separated and more or less extensively ecchymosed. Contused wounds are often irregular, and have thickened or swollen and ragged borders. They may, like simple contusions, show by their shape the form of the instrument which caused them. In contused wounds, unless they be perfectly aseptic, we usually find sloughing of the contused, necrotic tissues. This leaves a cavity to be filled up by granulation[471] like wounds with loss of substance. They therefore often present large cicatrices which may be mistaken for those of ulcers. In contused wounds the bone may sometimes show the impression of the instrument causing the wound.
A variety of contused wounds is that where the wound of the skin consists merely of an erosion or excoriation with an ecchymosis beneath. The wound may reproduce the shape of the weapon, i.e., finger-nails, etc. After death the skin becomes brownish-yellow, hard, and dry, and then they are called by the French “plaques parcheminées.” They are distinguished, as a rule, from those produced after death, by the ecchymosis beneath.
Lacerated wounds resemble contused wounds very closely, but are not ecchymosed to any considerable extent. The solution of continuity is sometimes very extensive and irregular, and may present several flaps. The bone or bones are often fractured at the same time. They seldom bleed much. The course of repair resembles that of contused wounds as a rule. The prognosis is variable, for there may be slow and extensive cicatrization and impairment of function, etc. These wounds usually result from machinery accidents and accidental tears, etc. They are therefore seldom the occasion of criminal proceedings but more often of a civil suit, and thus require medical examination.
The injury which causes a contusion or contused wound may not infrequently produce effects far more serious and more or less remote from the contusion. Some of these effects it may be well to particularize. Blows on the abdomen are sometimes quickly followed by death without visible lesion to account for it. That authentic examples of this exist has been denied by Lutaud, except for cases of rapid death following contusions of the abdomen which had caused extensive rupture of the viscera and abundant hemorrhage. But Vibert gives two cases from his own experience, which are as follows:
A young man, twenty years old, received a kick in the stomach at a public ball. Numerous witnesses of the scene testified that he only received this one blow. The man collapsed immediately and died in a few minutes. On autopsy nothing was found but two small ecchymotic spots in the peritoneum covering the intestine, the largest not the size of a bean.
In the second case, the injury was also a kick in the stomach and the man died almost immediately. Absolutely no lesion was found on autopsy. Both were in full digestion.
König[606] says: “A number of severe contusions of the belly run a rapidly fatal course without the autopsy showing any definite anatomical lesion of the viscera.” He also adds that the less severe cases at first often show very profound shock, which is out of proportion to the force of the injury. The cause of death has been explained, like that of sudden death from a blow on the larynx, by the theory of inhibition. These cases are often illustrated experimentally on frogs, where the same result is obtained under similar conditions. Such cases are the more remarkable from the fact that the fatal blow may cause no ecchymosis or other mark of injury to appear on the abdominal walls.
Blows on the head may produce a variety of results besides that of the contusion itself. In fact, death itself may result though the marks of contusion are very slight or even imperceptible. Intracranial hemorrhage, laceration with ecchymosis of the brain, on the same or opposite side to the injury, and concussion of the brain may result. Of these only concussion will be considered now.
Concussion has been defined as a shock communicated to an organ by a blow or fall on another part of the body, which may or may not be remote, and without producing a material or appreciable lesion. According to Lutaud,[607] English pathologists understand by it a temporary or permanent nervous exhaustion resulting from a sudden or excessive expense of nervous energy. Its effect is observed in the function of an organ and especially in the brain. Concussion of the brain causes stupidity, loss of consciousness, amnesia, coma. The intracranial lesion most often associated with concussion is ecchymosis and laceration on the surface of the brain, but there may be no lesion visible even if the case is a fatal one. Fatal concussion has been observed where the marks of external violence were very slight or even failed entirely, as illustrated by the two following cases cited by Vibert:[608]
Vibert made an autopsy on a man who had been struck by a[473] pitchfork, one of the teeth of which struck behind the ear, the other two in the face, only producing slight skin wounds. The man immediately lost consciousness and died in two days in coma. No lesion whatever was found within the skull, and only three slight ones externally.
He observed another case where the man fell three or four metres into an excavation, landing on his feet, and died in a short time. On autopsy only slight erosions and no intracranial or extracranial lesions were found.
This case belongs to a rare class where the blow is transmitted through the spinal column without sign of injury externally or internally to the head.
The following case cited by Vibert is even more remarkable in the production of the severe though not fatal concussion: An officer was riding at full speed on horseback, when his horse suddenly stopped short. By great exertion the officer clung to the horse, but immediately lost consciousness. His fall from the horse was broken by those about him, and the concussion he received was not due to the fall, but to the shock of stopping suddenly when his momentum was great.
As a rule, however, the diagnosis of concussion, especially if it is severe enough to be fatal, is easily made by the marks of external violence with or without intracranial lesions. The effects of concussion may be transient and leave no trace, but, on the other hand, they may be prolonged and severe, i.e., paralysis, aphasia, loss of memory, imbecility, etc. The medical examiner should be on his guard against simulation in respect to these prolonged effects of concussions. One of the most frequent consequences of concussion is temporary amnesia, which ordinarily succeeds immediately after the injury, but sometimes develops more slowly. The following curious case is quoted from Lutaud as cited by Brouardel:
A woman in getting out of a train at Versailles, where she had gone to attend the funeral of a relative, was struck by the door of the compartment. She fell, but did not lose consciousness, and picked herself up, but forgot what she had come for.
Another result of an injury which has caused a contusion or contused wound may be a fracture or dislocation. Fractures and dislocations of special parts will be referred to later, in considering injuries of the several regions of the body, but[474] it seems appropriate here to refer to some of those general considerations relating to these injuries which may especially demand the attention of the medical expert.
Fractures may be produced by blows or falls, or from muscular action. The medical witness may be questioned as to the cause of the fracture or, if it was produced by a blow, whether a weapon was used or not, as the defence is likely to assert that it was caused by an accidental fall. The nature of the associated wounds and contusions, if any exist, may, as we have seen, indicate the weapon used. If anything exists to indicate that a fall which caused the fracture was not accidental, this should be noted, as the assailant is responsible for the effects of the fall.
A number of conditions influence the ease with which a fracture is produced and account for a fracture being due to a slight injury, and so are mitigatory circumstances in the case.
Fractures are more easily produced in the old and young, especially the former, than in the adult from the same force. This is due to brittleness of the bones in the old and their small size in the young. Certain diseases like syphilis, arthritis, scurvy, carcinoma, and rickets make the bones more frangible, and there is a peculiar brittle condition of the bones known as fragilitas ossium, more or less hereditary, in which the bones become fractured from very slight violence. Mercer is quoted by Taylor as stating, but on how good authority it does not appear, that in general paralysis of the insane the bones are particularly liable to fracture. Certain it is that not uncommonly insane patients are found dead with single or multiple fractures, but the attendants are generally convicted.
In some parts, like the orbital plate of the frontal bone, the bone is very thin and brittle, but brittleness from any cause only mitigates, it does not excuse.
Taylor[609] reports a case in point where it was proved that the bones of the skull were thin and brittle, and the fractured skull proved fatal from inflammation of the brain. The punishment was mitigated owing to the circumstance of the brittleness of the bones.
Spontaneous fractures may occur from only a moderate degree of muscular action, and even where there is no disease[475] of the bones, but the above-mentioned condition of fragilitas ossium, rendering the bones more brittle, aids in the production of such fractures. The olecranon, patella, and os calcis are particularly liable to such fractures, but the long bones of the ribs and extremities are sometimes so fractured, as instanced in the following cases cited by Taylor:[610]
The humerus of a healthy man has been broken by muscular exertion simply by throwing a cricket ball.[611] In 1858 a gentleman forty years old, during the act of bowling at cricket, heard a distinct crack like the breaking of a piece of wood. He fell immediately to the ground, and it was found that his femur was fractured.
Again, in 1846, a healthy man, æt. 33, was brought to Gray’s Hospital with the following history: He was in the act of crossing one leg over the other to look at the sole of his foot, when something was heard to give way; his right leg hung down and he was found to have received a transverse fracture of the femur at the junction of the middle and lower thirds.
The writer had a case in Bellevue Hospital during the past winter (1892-93) of a man who stated that he had been well and active until some weeks previously, when, from muscular force alone, he sustained a fracture of the neck of the femur. Something abnormal in the bone may be present in such cases.
In cases of spontaneous fractures there are no marks of external violence which, if present, would remove the idea of spontaneity.
Fractures of the extremities are not dangerous per se, unless they are compound or occur in old, debilitated, or diseased persons, and they are more severe the nearer they are to a joint. The healing of fractures is more rapid in the young than in the old and in the upper than in the lower extremity. It is not proven that adiposity of itself impedes union.
The question may be asked, how long before examination a given bone was fractured. As a rule, we can only say as to whether the injured person has lived a long or short period since the injury, as the process of repair varies according to age and constitution. No changes occur until eighteen to twenty-four hours, when lymph is exuded. According to Villermé[476] the callus is cartilaginous anywhere between the sixteenth and twenty-fifth days, it becomes ossified between three weeks and three months, and it takes six to eight months to become like normal bone.
The question may also be asked: Has a bone ever been fractured? The existence and situation of a fracture can often be recognized long after the accident, by the callus or slight unevenness due to projection of the edges or ends of the fragments. Where the bone lies deeply covered by soft parts, it is difficult and often impossible to tell, long after union has taken place, whether or where a fracture has occurred.
The answering of this question may sometimes be of importance in identifying the dead, especially in the case of skeletons. In the latter instance by sawing the bone longitudinally we can tell by the thickness, irregularity, or structure of the bone tissue whether a fracture existed, and if it were recent or old at the time of death.
Dislocations call for a medico-legal investigation less often than fractures. They are less common in the old and where the bones are brittle, when fracture occurs more readily. They are seldom fatal per se, unless between the vertebræ or when compound. They may occur from disease in the affected joint or even spontaneously. The diagnosis of a dislocation is easy until it has been reduced, and then it may leave no trace except pain in and limitation of the motion of a joint besides swelling and ecchymosis. These effects are transient, and after they have disappeared it may be impossible to say whether a dislocation has existed on a living body, unless, as sometimes occurs, especially in the shoulder joint, there may be a temporary or permanent paralysis of a nerve and muscular atrophy. After death, the existence of an old dislocation may often be recognized on dissection by scar tissue in and about the capsule.
EXAMINATION AND DESCRIPTION.
The examination of wounds or injuries in a case which is or may become the subject of a medico-legal investigation should be made with particular care and exactness.
As the examination of the wounded person is to give most, and in some cases all, the information to the medical expert on[477] which he is to base his testimony, it should be made with reference to all the possibilities of the case.
The particular variety of wound as described in the foregoing section should be noted, and any peculiarities as to its situation, shape, extent, length, breadth, depth, direction, and the parts involved. Besides these points, the condition of the edges of the wound, whether swollen and ecchymotic, smooth and straight or dentated and irregular, and whether inverted or everted and gaping, are matters of importance. The presence or absence of coagula and clots, the staining of the tissues with blood, the presence of ecchymosis and its comparative age, as shown by its color, should also be noted.
Many of the above points help us in solving another problem, namely, the form of the instrument used. This question will be discussed in a subsequent section, but the basis for our opinion is founded, of course, on an examination of the particulars of the wound. The solution of still another question which often arises and which will be discussed in the next section, namely, whether a wound was produced before or after death, is based upon particular features of the wound such as the fluid or clotted condition of the blood on the surface, or ecchymosed in the tissues, also the amount of the hemorrhage as compared to the vascularity of the part as well as the greater or less staining of the tissues with blood, and the conditions of the edges, whether inverted or everted and whether or not retracted. The question as to whether a wound was directly, secondary or necessarily the cause of death, is determined, in part at least, by examination of the wound. In this connection we take note as to whether a wound has opened or divided a large vein or artery or is situated in such a vascular part as to be fatal from hemorrhage. We also note whether death could have been due to shock from the situation of the wound, or whether an inflammation which was directly responsible for death was necessarily due to the wound, as in case of a penetrating wound of the viscera, etc. Further, we note whether one of the many forms of wound diseases from infection of the wound has complicated the case and caused death in the case of a wound not otherwise necessarily fatal. It may be added that often the necropsy aids us in the solution of the question as to whether the wound was the necessary and direct cause[478] of death, by showing a healthy or diseased condition of the viscera.
The question as to which of a number of injuries was first inflicted, also as to the relative position of the victim and assailant, can be answered, if at all, only by an accurate and close examination of the wounds.
Finally, the most important question of all, from a medico-legal standpoint, namely, the distinction between homicidal, suicidal, and accidental wounds, is decided or inferred from the characteristics of the wound after careful examination.
All the foregoing questions contribute to the solution of this the most important one. The various questions referred to above will be considered at greater length in the subsequent sections. They have been merely referred to in brief above, to show the various lines of thought a medical examiner must have in mind in making an examination.
As to the act of examination itself, the physician should conduct it in such a way as not to harm the wounded person. Often simple inspection is the most that can be done, or the examination may have to be deferred altogether until the physician in charge informs the court that an examination may be safely made. It is often necessary for the expert to get information as to the original lesion from the physician in charge. If the wound has been a fatal one and if we are called in after death, we may examine the wound on the dead body with much more freedom. Here we may examine the depth, direction, etc., of a punctured wound by cutting down on a probe or director. After careful inspection of the wound we may examine it by palpation, and go on to the dissection of the wound and the surrounding parts, tracing and noting the various vessels, muscles, etc., involved in the wound, and looking for the presence of any foreign body in the wound.
Furthermore, if the cause of death be at all obscure, we should examine not only the wound itself and the parts about the wound, but also, by an autopsy, all the cavities and organs of the body. For death may have been due to natural causes in an organ not examined, if the examination has not included all, and the physician has to disprove it.
In examining at an autopsy the depth of a wound in reference to the instrument which caused it, it should be borne in[479] mind that the wound may be deeper than the weapon owing to a depression of the surface by the handle of the weapon. This may appear especially marked in the case of the movable viscera, as at the time of the accident the viscus may have been as near as possible to the surface, and at the examination as far as possible from the surface, as in the case of a given coil of the intestines. Also the thorax when opened at autopsy enlarges or expands a little, so that the measured depth of a wound may be greater than the weapon which caused it. Vibert[612] mentions a case of a penetrating wound of the thorax involving the heart, where the measured depth of the wound was 0ᵐ.035 greater than the length of the instrument. This may also be accounted for by a depression or flattening of the thorax by the blow, as in the case of soft parts. It is often difficult in an examination to measure accurately the depth of a wound, for one may find it hard to determine the precise end of a wound. Also, for exact measurement it is necessary to have the parts in the same position as at the time of the accident, and these parts are more or less displaced by the necessary dissection.
Besides the examination of the wound there are other points the examination of which may aid us in solving the problems presented by a case. Among these, the examination of the clothing or dress is perhaps the most important. This may indicate the weapon used in an incised or punctured wound. Contused and lacerated wounds or fractures, etc., may be produced without injuring the clothing. Blood, dirt, or grease on the clothing may throw light on the case. In self-inflicted wounds the wound in the clothing and that on the body may not and often do not correspond, as an intending suicide often (a murderer rarely) opens the clothing to select the spot for the wound. The wound in the dress is then added by a second blow not corresponding to the first. In this way we may sometimes distinguish between a homicidal and suicidal wound, and thus remove a false suspicion of murder or show that a wound was self-inflicted to conceal other crimes or to falsely impute it to another. The suspicion of homicide in accidental wounds may be cleared up by an examination of the dress, as in the following instance related by Taylor:[613]
A woman was found dead in bed with two indentations about the middle of the right parietal bone, a large superficial clot here and three ounces of clotted blood between the dura mater and skull, which latter was fractured over an area of four inches. No other cause of death was found. The evidence brought out the facts that she had been knocked down the evening before, about 7:30 o’clock, by a man accidentally running into her. She fell on the back of the head, was stunned, raised up, and stimulated; she then walked home, ate her supper, and was last seen at 9 o’clock by a fellow-lodger who let her in and noticed nothing unusual. The next morning she had evidently been dead some time. Suspicion fell upon the lodger, who had often quarrelled with her, and the two claws of a hammer found in his room corresponded more or less closely with the two indentations found in the skull. At the adjourned inquest, however, the bonnet worn by the deceased at the time of the accident was found to have two indentations on the back of it corresponding to those on the woman’s skull and containing dust and dirt, and rendering probable what from the history seemed unlikely, that the fall in the road caused the fatal injury. The examination of the dress thus avoided an unjust accusation of murder.
Contused and lacerated wounds and fractures or dislocations may be produced without injury to the dress, especially if the latter be elastic or yielding. The comparison of the wound in the clothes with that on the body may indicate the position of the body at the time of the blow. The examination of the clothes of the injured person may indicate a struggle which would support the idea of homicide. A blunt instrument may indirectly cause an injury by striking something in or on a person’s clothes. Instances have been reported where a wound has been caused by an article in the pocket, or worn outside the clothing, without any trace of an injury to the clothes or pocket lining.[614]
The examination of the dress may further show which of several cuts or stabs was first inflicted. This is shown by the staining of the edges of the cuts in the clothing, the edges of the first cut or stab showing no blood-stain or only on the inner[481] surface, as the knife is clean of blood on entering and all that is removed by the clothing on its withdrawal is found on the inner edges. If the edges of the cuts in the outer layers of clothing are bloody, it is evident that the knife was already bloody when used, and the corresponding wound was not the first inflicted.
The imprint of the bloody hand of the assailant may sometimes be found on the clothing of the one injured, and is especially important as evidence, when the hands of the assaulted are not bloody. In the case of a severe wound, especially if it is likely to become the object of a criminal investigation, the physician should always require to see the dress of the wounded. The examination of the clothing which the accused wore at the time the assault took place may give important evidence by showing evidences of a struggle or blood-stains. Absence of the latter would not prove the innocence of the accused, as the clothes actually worn may be destroyed and others substituted, or the marks and stains may be removed. In the latter case, the eye of a medical man may detect traces of blood which otherwise would go unnoticed, and a microscopical and chemical examination would reveal the real character of the stain.
Besides the examination of the clothing of the accused, the examination of his person may furnish evidence of his being engaged in a more or less desperate struggle by the scratches, marks of nails, contusions, bites, etc., on the face, neck, front of chest, forearms, and hands. If the accused should attempt to explain these wounds and spots, the latter may or may not verify the explanation, and thus additional evidence may be obtained as to the guilt or innocence of the accused.
It is well for the medical expert, as well as for others, to collect the statements of the wounded person relative to the circumstances of the injury. Also, if the accused will vouchsafe any such statements we may compare these with one another and with the facts indicated by the wound, etc.
Other points to examine, especially in cases of suspected suicide, may be briefly mentioned. The presence of the weapon in the hand of the victim and firmly grasped in general indicates suicide, if it corresponds to the weapon causing the wounds, for otherwise it may have been used for defence. If not in the hand, note the spot where the weapon was found.[482] In the case of a suicide, the hand as well as the weapon held by it is likely to be bloody, also in case of murder the generally empty hand is apt to be bloody, as the hand is naturally carried to the wound.
We cannot further describe the many points which the medical examiner should bear in mind in making an examination in a medico-legal case, without repeating too fully what will be given at greater length in subsequent sections, reference to which should be made for further particulars. Tardieu proposed as a basis for examining and studying wounds, (1) to visit the wounded person and see what state he is in, and to determine (2) the nature, (3) the cause, (4) the consequences of the wound. Also if the wounded person is dead (5) to examine the body for the cause of death in order to see if the latter is due to the wound. Also (6) to determine the circumstances of the affray.
The description of a wound should be given in plain language, avoiding the use of scientific terms or expressions, so as to be readily understood by judge and jurors. Otherwise the usefulness of the medical expert is very much decreased. The description should also be precise and sufficient to justify the conclusions arrived at as to the cause of a wound, its gravity and results, and the weapon used. With a view to exact statement in description, it is well to take notes as to the result of the examination and not depend merely on memory. The object of the witness should be to be understood and not to be thought thoroughly scientific.
WAS THE INJURY INFLICTED BEFORE OR AFTER DEATH?
This is a question which may often be asked in cases of fatal injuries, and it is one which must be answered as definitely as we are able, for the defence may rest on the assertion that the wound or injury was post mortem and not ante mortem. What are the means we have to enable us to answer the above question? The most important factor is the condition of the blood and the changes that it undergoes after death. For some hours after death the body retains its animal heat. As long as this is retained rigor mortis does not set in and the blood is more or less fluid. This period varies, but on the average it does not[483] last longer than eight or ten hours. Before this time, however, the blood has begun to undergo certain changes. These changes result in the inability of the blood from a post-mortem wound to coagulate completely. At first the greater part may coagulate, but after a time coagulation is less and less complete, and the coagula are not as firm as those from the blood of a living person. The period at which these changes occur also varies, but they may generally be clearly noticed in from three to four hours after death, or even sooner. In the first two to four hours after death, therefore, as far as the condition of the blood is concerned, it may be difficult or impossible to say whether a wound was made before or soon after death. In other words, this difficulty exists as long as the tissues of the body live after the body as a whole is dead.
There are certain general pathological or occasional conditions of the body in which the blood during life does not coagulate at all or only imperfectly, as in scurvy and in the case of the menstrual blood. Also blood in a serous cavity, especially if it be abundant or there exists inflammation, is found not to coagulate or only imperfectly. Post mortem the blood remains liquid long after death in cases of death by drowning, asphyxia, etc., and in such cases hemorrhage may be free in a wound made some time after death. Furthermore, after putrefaction has set in the blood again becomes more or less liquid, and may flow away from a wound like a hemorrhage, but it no longer coagulates.
The principal signs of a wound inflicted during life are (1) hemorrhage, (2) coagulation of the blood, (3) eversion of the lips of the wound, and (4) retraction of its sides.
1. Hemorrhage varies in amount with the size of the wound, the vascularity of the part, and the number and size of the large vessels involved. In incised or punctured wounds the amount, as a rule, is quite considerable. If there is a free exit most of the blood runs off; the rest stays in the wound, where it soon coagulates with the exceptions mentioned above. But besides partly filling the wound in the form of a clot, the edges of the wound are deeply stained with the coloring matter of the blood, and this stain cannot be removed by washing. This staining involves especially the muscular and cellular tissues.
Further, a hemorrhage during life is an active and not a[484] passive one; the blood is forced into the interspaces of the tissues in the vicinity of the wound, and is found infiltrated in the cellular tissue, the muscles, the sheaths of the vessels, etc. It is here incorporated, as it were, with the tissues so that it cannot be washed away. In an ante-mortem wound the arterial nature of the hemorrhage may show by the marks of the jets of blood about the wound or on the clothes or surrounding objects. When a large vessel has been divided and the exit for the blood is free, this may run off without infiltrating the tissues or even staining the edges to any considerable extent, and there may remain but little in the wound. In the case of lacerated and contused wounds the amount of hemorrhage is less, but rarely fails entirely, and if the wound is in a vascular part it is liable to cause death from hemorrhage, though a whole limb may possibly be torn off without much hemorrhage. In the latter case, however, there are usually found clots of blood adhering to the edges of the lacerated wound and the ends of the vessels. In contusions where there is no wound of the skin the blood is prevented from flowing externally, and its accumulation and distribution form an ecchymosis. Here again we see the active power of the hemorrhage which infiltrates between the tissues, stains them deeply, and appears either as a mere stain or in fine clots incorporated, as it were, with the tissues or partly occupying a cavity formed by an extensive displacement of the surrounding parts. The amount of blood varies under the same conditions as in incised wounds, and also according to the greater or less disintegration of the tissues by the blow, allowing a larger or smaller central cavity to be formed. In “bleeders” the amount of the hemorrhage does not vary under the normal conditions, but a fatal hemorrhage may occur from a very insignificant wound. After hemorrhage from a wound made during life the veins are empty about the wound, especially those situated centripetally, while normally after death the blood is mostly aggregated in the veins. They are the source of post-mortem hemorrhage, but do not empty themselves to any great extent.
The hemorrhage from a wound made after death may be extensive if the blood remains fluid as in the cases mentioned above, i.e., after death from drowning or asphyxia or after the commencement of putrefaction. Otherwise the amount of[485] hemorrhage decreases with the length of time after death, until the blood loses its fluidity and hemorrhage no longer occurs. In general, it is slight unless a large vein is opened, for the veins are the source of the hemorrhage. There is usually scarcely any hemorrhage after the first two to four hours. This applies also to subcutaneous hemorrhages or ecchymoses. These post-mortem hemorrhages are passive and not active, consequently there is less infiltration of blood into the surrounding tissues, which merely imbibe it, and the stain is less deep and may be washed off the edges of the wound, in contrast to the stain of ante-mortem wounds. After putrefaction has set in the hemorrhage may be more abundant, as the blood is driven to the surface by the formation of gas in the abdomen and thorax. At the same time, the coloring matter of the blood transudes through the walls of the veins and is imbibed by and stains the tissues, so that it may be impossible to distinguish it from a true ecchymosis. Fortunately these conditions are of small moment, as an examination is seldom deferred so long.
Cadaveric ecchymoses show almost invariably while the body is still warm and the blood more or less liquid, i.e., during the first eight or ten hours after death. They are not due to injury or violence before or after death, but they may closely resemble ecchymoses produced on the living body and be mistaken for them. This is the more important as they are quite constant on the cadaver.
In this connection, it may be said that an ecchymosis due to a blow before death may not show till after death, as it requires some time for a deep ecchymosis or even an ecchymosis covered by a thick layer of skin to show superficially. Thus a man kicked in the abdomen died thirty-five hours after the injury from peritonitis, due to a rupture of the bladder. No ecchymosis appeared at the site of the injuries until after death. It is not uncommon in cases of hanging to observe an ecchymosis along the course of the cord appearing only after death. Huize met with a case of this description. Devergie remarked that on the bodies of those drowned ecchymoses are often hidden for a time on account of the sodden state of the skin, and they appear only after the water has evaporated, which may require some days. Furthermore, it is not necessary to survive long[486] after an injury in order that an ecchymosis may show post mortem. If the blood is fluid at the time of the blow and any capillaries or larger blood-vessels are torn, then we may have an ecchymosis though death be almost instant. Casper thought that it required some time before death for an ecchymosis to develop, and that if the person injured by a contusion died soon after the injury, an ecchymosis would not appear after death. There are many well-authenticated cases to prove that Casper’s opinion is wrong. Among the most famous of these is that of the Duchesse de Praslin.[615] She was attacked and killed by her husband while she was asleep in bed. The thirty or so wounds showed a mortal conflict, and she could not have survived more than one-half hour, and yet after death there were numerous ecchymoses from the contusions.
Another case is also mentioned by Taylor.[616] A young man died suddenly after a blow from a companion, having been struck in the side a fortnight before by a heavy box, which knocked him senseless and nearly killed him. The post mortem revealed an ecchymosis on the side which on the authority of Casper’s opinion was attributed to the old injury. The color of the ecchymosis would be sufficient to settle all such doubts, as the changes of color would have fully developed or the color even disappeared in part in fourteen days’ time.
An ecchymosis made post mortem does not undergo the color changes seen in ecchymoses during life, unless the tissues are œdematous in which the ecchymosis occurs. These changes in color have already been described, the deep blue changing to violet in eighteen to twenty-four hours at the earliest. In support of the foregoing and disproving Casper’s views, Christison found that within two hours after death severe blows on a dead body are followed by a livid discoloration, similar to those produced by a blow shortly before death. This livid discoloration is due to the effusion of a very thin layer of blood external or superficial to the true skin, sometimes in a stratum of the true skin or more rarely into the cellular tissue, staining deeply the partition walls of the fat-cells. Of course, a more or less recent contusion or ecchymosis on a dead body was not necessarily produced at the same time as the cause of death. It should[487] be borne in mind in this connection that ecchymosis is not a necessary result of a blow or contusion.
According to Devergie, ecchymosis does not appear when a blow inflicted post mortem is received by skin directly covering a bony surface beneath, and rarely appears where there is a large amount of fat and no solid point of resistance beneath the site of the blow.
We have already referred to the fact which Portal long ago remarked, namely, that the spleen has been ruptured without ecchymosis or abrasion of the skin. The same absence of ecchymosis has been noticed in cases where the liver, stomach, intestines, bladder, etc., have been ruptured as the result of contusing blows.
The following case cited by Taylor[617] illustrates this point. Henke reported the case of a man who died of peritonitis a few hours after fighting with another man. There was no mark on the skin or ecchymosis, though there existed peritonitis from rupture of the small intestine. The blow was proven by direct evidence, and though some medical witnesses on account of the absence of external signs thought that no blow could have been struck, others of more experience admitted that it could have been the cause of the rupture.
Watson[618] reports a similar case of a girl nine years old who received a blow from a shoe on the abdomen. This was followed by great pain, collapse and death in twenty-one hours. No marks of injury were visible externally, but peritonitis existed from rupture of the ileum.
A similar case is reported by Williamson,[619] where peritonitis resulted from complete rupture of the ileum without any trace of injury externally, though the blow was struck by the hoof of a horse.
Another case was brought into Guy’s Hospital[620] who had been run over by an omnibus. No injury was discoverable, though the wheel had passed over the chest and abdomen. He died of peritonitis, however, which set in on the second day, and on post-mortem examination the liver and small intestines were found ruptured.
Christison thought as the result of his experiments and experience that the most reliable signs of an ecchymosis made during life, and distinguishing it from one caused by a blow after death, were as follows: The skin of the ecchymosed area is generally much darkened and discolored from blood infiltrated through its entire thickness; the skin is also much firmer and more elastic from swelling of the part if the contusion is received some hours before death. But we may have an effusion beneath and not in the substance of the skin, and the above signs might possibly be due to an injury inflicted only a few minutes after death. The above signs may therefore be absent, and when present are not absolutely indicative of an injury received during life. In general, the effects of severe contusions inflicted soon after death may closely resemble those of slight contusions received during life.
There is little danger of contusion if the blow be inflicted on a dead body after the loss of body heat and the beginning of rigor mortis.
2. Coagulation of Blood.—As stated at the beginning of this section, blood from a wound inflicted during life coagulates with the exception of that from those suffering from certain pathological or occasional conditions or in certain locations, already mentioned. This coagulation is not immediate, but is complete in about five minutes. The entire amount of blood lost is thus coagulated and the coagula are firm. These coagula (if the wound is not interfered with) occur in the opening of a wound and on its edges, especially at the mouths of the blood-vessels, which are thus plugged. The blood which infiltrates the interspaces of the tissues is coagulated in the form of these interspaces. The same is true of the blood of an ecchymosis whether there be a hematoma or only an infiltration between the tissues, or both. These clots represent more or less the form of the space occupied by the blood. In the case of the scalp a subcutaneous clot may be mistaken for a depressed fracture of the skull from the fact that the edges of the clot become very hard while the centre is still quite soft. A wound in which a large artery has been divided may present very little clotting in the wound if the opening is free and the blood has mostly escaped in a jet.
In a wound produced soon after death there may be some[489] clotting, but less in amount, firstly, because there is less hemorrhage, and, secondly, because not all the blood clots. These conditions increase with the length of time after death, so that after a time a wound made on a cadaver would show very little if any clotting owing to very slight hemorrhage, and little or no clotting of the blood extravasated. When the body has lost its animal heat and rigor mortis has begun to set in, then there is no more coagulation of the blood and no more hemorrhage, under normal conditions, for the blood has mostly become clotted in the vessels of the body. Consequently, with the exception of wounds inflicted very soon after death, we can distinguish an ante-mortem from a post-mortem wound by the condition in which the blood is clotted. If there is any hemorrhage, the wound being inflicted before the loss of animal heat and the blood remains entirely fluid on the surface or in an ecchymosis, we know that the wound was produced after death and some hours after death unless any of those conditions exist in which the blood does not normally coagulate. If the hemorrhage is slight or quite moderate in amount and venous in character, if the blood is only clotted in part and the clots are rather soft and do not form a plug at the mouth of each artery, and especially if the staining of the walls of the wound can be washed off, then the wound was probably produced post mortem, but not so long after death as in the first case supposed. If the characters of the hemorrhage and the clotting are still more like those normal to a wound inflicted during life, then, as a rule, it is impossible to say from these two features of the wound, hemorrhage and clotting, whether the wound was inflicted during life or a very short time after death.
3. Eversion of the Lips of the Wound.—The edges or lips of a wound inflicted during life may be inverted, instead of everted, if a thin layer of muscular fibres is attached directly to the deep surface of the skin, as is the case in the scrotum. The eversion of the edges of the skin is due to their elasticity, and ceases to occur as soon as the skin loses its vitality. Consequently eversion ceases to occur soon after death, within a very few hours. A wound in which the edges are neither inverted or everted was therefore inflicted after death. If this sign is present and marked, the wound was inflicted during life or within two or three hours or less after death. If this sign is[490] present but very slightly marked, the wound may have been made even somewhat longer after death.
4. Retraction of the sides of the wound is also dependent on their vitality and ceases to occur when this is lost a few hours after death. In the retraction of the edges of the wound we have all the parts involved, but unequally. The muscles, arteries, skin, and layers of connective tissue all retract, varying in the degree of retraction according to the order in which they are named. In different parts of the body this comparative order of retraction is liable to more or less variation. Every surgeon is familiar with this retraction of the tissues, which necessitates certain rules in the technique of operations, especially of amputations. Muscles retract the more the longer they are and the farther the incision is made from their attachment. Without specifying a definite time, we may say that, as a rule, this retraction lasts no longer than about two hours after death, consequently when it is absent we may infer that the wound was inflicted two hours or more after death. The amount of retraction grows less and less after death for about two hours, after which it is very slight if it occurs at all, owing to the loss of elasticity of the tissues. This sign is especially useful in the case of a mutilated body where, by examining the degree of retraction of the muscles, we may infer whether the mutilation was done before or after death. The sides of a cut made on the cadaver are comparatively smooth and even, owing to the absence of the unequal retraction of the various elements, which makes the surfaces of a gaping ante-mortem wound uneven and irregular. Relying on these circumstances in the “affaire Ramus,” cited by Vibert,[621] one was able to recognize the order in which the body had been mutilated.
Other minor signs of a wound inflicted during life may be briefly mentioned. If the edges of the wound are swollen, or show signs of inflammation or gangrene, or if pus or adhesive material is present on the edges of the wound, we may infer that the wound was inflicted some little time before death. Of course, if cicatrization has commenced, some days must have elapsed before death after the wound was received. If the blow causing a contusion was inflicted some time before death, there will be more or less of a general swelling of the[491] region, partly due to the blood effused, but also partly due to œdema.
It is not always easy to say whether a fracture was produced while the body was living or dead. If the body was still warm when a post-mortem fracture was produced there is little difference from an ante-mortem fracture, except that there may be a little less blood effused. In a fracture produced after rigor mortis has set in there is little or no blood effused. In the case of fractures the presence of callus, indicating the process of repair, shows that the accident occurred during life, and, as we have already seen, we may form some idea of the length of time elapsed between the injury and the time of death. On the cadaver it is said to be harder to cause fractures and lesions of the skin than on the living body. Casper says that fractures of the hyoid bone and the larynx are impossible after death, and he also was not able to rupture the liver or spleen.
In distinction to the characteristic signs of a wound inflicted during life, we may mention briefly some of the signs of post-mortem wounds when the wound has been inflicted from two to ten or twelve hours or more after death:
(1) The hemorrhage is slight in amount and may fail altogether.
(2) The character of the hemorrhage is venous, corresponding to the source of the hemorrhage from the veins, the arteries being nearly empty after death.
(3) The edges of the wound are not deeply stained, and this staining may be removed by washing. The spaces between the tissues are not infiltrated with blood.
(4) The blood remains either entirely fluid or, if there are clots, these are softer than those in an ante-mortem wound, and only a portion of the blood is thus clotted. There are no clots plugging the open mouths of the arteries on the surface of the wound; the veins may or may not be closed by an imperfect clot.
(5) The skin of the edges is not everted or inverted.
(6) The sides of the wound do not gape and their surfaces are smooth and even, as the tissues are not unevenly retracted.
Résumé.—It is very easy from the foregoing to distinguish between a wound inflicted before death and one ten or twelve hours after death.
If the hemorrhage has been abundant and arterial, if it has infiltrated between and deeply stained the tissues and the stain cannot readily be washed off; if the blood coagulates completely and the coagula are firm and are found lying in the wound, plugging the vessels, and incorporated with the tissues between which they lie; if the edges of the skin are everted and the sides of the wound are retracted and uneven—under these circumstances, we may be sure that the wound was inflicted during life or a very short time after death. If, on the contrary, the hemorrhage is slight in amount or almost fails altogether; if it is venous in character; if the edges of the wound are only stained by imbibition of the blood, which is not infiltrated between the tissues, and the stain may be washed off; if the blood is not at all or only slightly clotted and the clots are soft; if the skin is not everted and the sides of the wound are smooth and lie nearly in contact; if there are no clots plugging the divided arteries on the surface—then we need have little hesitancy in saying that the wound was produced after death, but probably not later than ten or twelve hours after death. If the wound was inflicted still longer after death and before putrefaction, then we would have a lack of the signs due to hemorrhage, clots, staining, etc. If we find the conditions more or less midway between the first two, we may be left in some doubt as to the date of the injury. Thus if the hemorrhage is moderate, the blood mostly but not altogether clotted and the clots moderately firm, the skin slightly everted, and the sides slightly separated and not altogether smooth on their surface; if the surfaces are fairly deeply stained and the stain cannot be easily washed off—then we can only say that the wound was inflicted during life or within two hours or so after death, and this fact is often enough for the purposes of the medico-legal inquiry.
The same is the case with contusions where there is no bleeding externally. If we have a bluish, violet, green, or yellow tumor with or without more or less superficial œdema; if this tumor fluctuates or is hard, but in either case is elastic; if on incision the skin and the tissue spaces are infiltrated with blood which is coagulated, or if there is a cavity filled with clotted blood, the coagulum being firm and the entire amount of blood coagulated—then the wound was inflicted during life. If, however,[493] the surface shows a bluish or violet color, little or no swelling of the skin, which is of natural thickness, and the ecchymosed area is not tense and elastic to the touch; if further the blood is found on incision to be fluid or if coagulated only partly so, and the blood is not infiltrated into the tissue spaces, but merely imbibed by the tissues—then the blow was inflicted after death, and probably more than two or three hours after.
In contusions especially we may have difficulty, as the sign of fluidity of the blood may fail and putrefaction may modify the conditions of the wound unless parts deep beneath the surface be examined.
We see, then, that in some cases it is very easy to say that a wound was inflicted post mortem. If a wound was not inflicted until ten or twelve hours after death or even sooner, we cannot easily mistake it. But in many cases it may be hard or impossible to say whether a wound was inflicted during life or within an hour or two after death. Here we must be cautious in expressing an opinion which should be guarded. But we should remember that it is important to be able to state that a wound was inflicted before or immediately after death, as no one but a murderer would think of inflicting a fatal injury on a body immediately after death. In such cases a well-guarded medical opinion may often meet all the requirements of the case.
Granted that a given wound was produced before death. There are, then, one or two questions which may arise, and which depend for their answer on the length of time the wounded person could have lived and the physiological or muscular acts which he could have performed after receiving the injury and before death. The first of these questions may be expressed as follows:
Could the Victim have Performed Certain Acts after having Received his Fatal Injury? The term “certain acts” here refers to almost any thing or things which would require time and strength—in other words, the continuance of life with bodily and mental powers for a certain time after receiving a mortal injury.
This question may be raised in relation to an attempted alibi of the accused, who may have been proved to be in the presence of the victim a moment before death. If after this[494] moment the victim has moved from the spot or performed certain acts before death, the attempted alibi may depend upon the answer to the question as to whether the given acts of the victim were compatible with the fatal character of the wound. An alibi can aid in the acquittal of the accused only when the nature of the injury was such that death would be supposed to be immediate or nearly so. Great care should be taken on the part of the medical witness in answering this question, for after very grave wounds, proving speedily fatal, the victim sometimes can do certain acts requiring more or less prolonged effort, as shown by numerous examples. Wounds of the brain are especially noticeable in allowing a survival of several hours, days, or even weeks, during which time the injured person may pursue his occupations. Where the survival has lasted days or weeks, the alibi has no importance, but not if the survival is of shorter duration. The following case is cited by Vibert[1] and may be mentioned in this connection, though the wound was caused by a bullet which traversed from behind forward the entire left lobe of the brain. After the injury the victim was seen by several witnesses to climb a ladder, though with difficulty, for he had right-sided hemiplegia. He was found insensible more than half a mile away, and did not die until six or eight hours after the injury. Severe injury of important organs is sometimes not incompatible with an unexpectedly long survival. Devergie cites two illustrations of this which are quoted by Vibert.[622] A man received several extensive fractures of the skull, with abundant subdural hemorrhage, and rupture of the diaphragm with hernia of the stomach. The stomach was ruptured, and nearly a litre of its contents was contained in the left pleural cavity. Notwithstanding all this, he was able to walk about for an hour or so and answer several questions. He died only after several hours. Another man, crushed by a carriage, received a large rupture of the diaphragm, complete rupture of the jejunum, and rupture and crushing of one kidney. Yet he walked nearly five miles, and did not die until the next day.
More rarely wounds of the great vessels are not immediately fatal. M. Tourdes is quoted by Vibert[623] as citing the case of a man who descended a flight of stairs and took several steps[495] after division of the carotid artery; also of one who lived ten minutes after a bullet-wound of the inferior vena-cava.
Even wounds of the heart are not as speedily fatal as is commonly supposed, and often permit of a comparatively long survival.
Fischer[624] found only 104 cases of immediate death among 452 cases of wounds of the heart, and healing occurred in 50 cases among 401. Vibert[625] mentions two striking cases of long survival after wounds of the heart. A woman received a stab-wound which perforated the right ventricle, causing a wound one centimetre long. She did not die until twelve days later, when on autopsy there was found an enormous extravasation of blood in the left pleural cavity and pericardium. The second case, though one of bullet-wound, is equally applicable and instructive in this connection. A man received a bullet-wound which perforated the left ventricle, the bullet being found later in the pericardium. After being wounded he threw a lamp at his assassin which set fire to the room. He then went into the court-yard, drew some water, carried it back in a bucket, extinguished the fire, and then lay down on his bed and died.
In studying the wounds of different regions of the body, we may find many other mortal wounds which, though speedily fatal, leave the possibility of more or less activity before death. We see, therefore, that even in those wounds which are commonly supposed to be immediately fatal, even by many medical men where attention has not been called to the exceptions, such exceptional cases are not uncommon in which death is not immediate. Time and even strength may thus be allowed for more or less complicated activity. An alibi cannot, therefore, be allowed without question on the part of the medical expert, who must exercise great caution in expressing an opinion. The second question which may sometimes arise in connection with the last, but having little to do with the subject of this section, is the following:
How Long before Death had the Deceased Accomplished Certain Physiological Acts? For instance, how[496] long after a meal did he die? This is hard to answer with precision, as digestion varies with the individual, and digestion begun during life may go on to a certain extent after death. We may be able to say if digestion has just commenced, is well advanced, or has terminated. What was eaten at the last meal may be learned by the naked eye, the microscope, the color of stomach contents and their odor. The state of the bladder and rectum is sometimes called in question. All the above facts have less bearing on the case than those in relation to the former question.
THE CAUSE OF DEATH FROM WOUNDS.
The cause of death should be certain and definite. In reality, there is only one real cause, though one or many circumstances may be accessory causes. In most cases of death from the class of wounds which we have been considering, there is no difficulty in determining the cause of death so as to be able to state it definitely. But if the deceased had recovered from the first effects of the wound and then died, or if death seems as much due to disease as to injury, then the real cause of death may be obscure. If the medical witness is in doubt as to which of two causes was the primary cause of death the doubt should be stated at once, as it may weaken the testimony if brought out later.
Wounds may be directly or indirectly fatal. They are directly fatal if the victim dies at once or very soon after the wound, with no other cause internally in his body or externally from his environment. Wounds are indirectly or secondarily fatal if the injured person dies from a wound disease or complication, the direct consequence of the wound, or from a surgical operation necessary in the treatment of the case. Wounds may also be necessarily fatal either directly or secondarily, or not necessarily fatal. In the latter case death may be due as much, if not more, to other causes than the wound, and sometimes not at all to the wound itself. Thus death may be due to natural causes, latent disease, an unhealthy state of the body, imprudence or neglect of treatment, or improper treatment, etc. These various degrees of responsibility of a wound as the cause of death we will now consider more at length.
I. Was the Wound the Cause of Death Directly?
If so, it must have caused death in one of the following ways:
1. Hemorrhage.—This may act by producing syncope. But the amount of the hemorrhage may not be sufficient for this result, and still cause death by disturbing the function of the organ into which it is effused, as in the brain or in the pleural or pericardial cavities. The blood here acts mechanically. Blood in the trachea may also kill mechanically by causing asphyxia.
The amount of hemorrhage required to produce syncope varies under a variety of circumstances. Less is required in the very young, the aged, and the diseased, also less in women than in men. Young infants may die from hemorrhage from very slight wounds, even from the application of a leech or the lancing of the gums. A sudden loss of blood is much more serious than an equal amount lost slowly. This is the reason that the wound of an artery is more serious and more rapidly fatal than a similar loss of blood from other sources. It is hard to specify the absolute quantity which must be lost in order to cause death by syncope. The total blood in the body is about one-thirteenth of the weight of the body, making the total amount of blood weigh about twelve pounds. Of this, about one-fourth is in the heart, lungs, and large blood-vessels. According to Watson, the loss of an amount varying from five to eight pounds is enough to be fatal to an adult. But less is enough to prove fatal in many cases, as the rapidity of the loss of blood and the age, sex, and bodily condition of the wounded person affect the amount necessary. Though death from a small artery is slower than that from a large one, yet it may occur in time, as shown in the instance quoted by Taylor,[626] where a man bled to death in thirty-eight hours from the wound of an intercostal artery. Thus, too, a wound of the branches of the external carotid artery is often enough to cause death, and a wound in a vascular part may cause death from hemorrhage, though no vessel of any size be divided.
Internal hemorrhage may be fatal from mechanical interference[498] with the function of an organ, as well as from syncope. Thus we may have death from syncope due to hemorrhage into the peritoneal cavity or, after contusions, into the intercellular spaces and the cavity due to the blow, into which several pounds of blood may be extravasated. Internal hemorrhage is most fatal when due to the rupture of a viscus such as the heart, lungs, liver, kidney. Taylor[627] cites a case of a man run over and brought to Guy’s Hospital in November, 1864. He had pain in the back, but there were no symptoms or marks of severe injury. He left the hospital and walked home, where he was found dead in bed a few hours later. His abdomen contained a large amount of blood from the rupture of a kidney. After severe flagellation blood may be effused in large quantity beneath the skin and between the muscles, which is just as fatal as if it had flowed externally from a wound. In fact, if the injuries are numerous the loss of much less blood is enough to prove fatal, the element of shock here assisting that of hemorrhage.
How are we to ascertain whether a person has died from hemorrhage? This may be more difficult in the case of an open wound, for the body may have been moved from the spot where it lay after the wound was received, and the blood on the body, clothes, and surrounding objects may have been removed. Then the case may be presumptive only, but we may arrive at a definite conclusion by attention to the following points: If the wound was in a very vascular part and of some size, or if a large vessel or many moderately large vessels were divided and the vessels, especially the veins in the neighborhood, are empty, then we may be quite sure of death from hemorrhage. If there is no disease found which could be rapidly fatal the case is still stronger. The body should be pallid after fatal hemorrhage, but the same may be the case from death from other causes. In case the body and surrounding objects have not been disturbed, then the amount of clotted blood in the wound, on the body and clothes, and about the body, taken in connection with the foregoing points, can leave no doubt. We should remember, however, that not all the blood about the body was necessarily effused during life, but a little hemorrhage may have occurred after death while the[499] body was still warm and the blood fluid, i.e., during the first four, eight, or ten hours. But the amount thus lost is small. In cases of death from internal hemorrhage we do not have so much difficulty in pronouncing an opinion, as by post-mortem examination we can determine the amount of the hemorrhage. We can judge, too, from its position, whether it has acted mechanically to interfere with a vital function, and has thus caused death, or whether the latter was due to syncope from the quantity lost.
2. Severe mechanical injury of a vital organ, such as crushing of the heart, lungs, brain, etc. This crushing may be accompanied by hemorrhage, but death may be more immediate than the hemorrhage would account for. The mechanical injury done to the vital centres in the medulla by the act of pithing is the direct cause of the sudden death which follows it. Exceptionally slight violence to a vital organ is fatal, but this may be better explained by attributing it to shock.
3. Shock.—An injury is often apparently not enough to account for the fatal result so speedily. The marks of external injury may fail entirely or be very trifling. Thus more than once persons have died in railway collisions with no external marks of violence. So, too, a blow on the upper abdomen, on the “pit of the stomach,” has been rapidly fatal without any visible injury to the viscera. Death is attributed to the effect on the cardiac plexus, and there may be no marks externally or only very superficial ones. In Reg. v. Slane and Others (Durham Wint. Ass., 1872), quoted by Taylor,[628] the deceased was proved to have sustained severe injuries to the abdomen by kicks, etc., but there were no marks of bruises. All organs were found healthy on post-mortem examination, but the injured man died in twenty minutes. Death was attributed to shock and the prisoners were convicted of murder.
Death from concussion of the brain is another example of death from shock. This may occur with only a bruise on the scalp and with no intracranial hemorrhage or laceration of the brain. The medical witness should be cautious in the above classes of cases in giving evidence, as the defence may rely upon the absence of any visible signs of mortal injury to prove that no injury was done, a principle fundamentally wrong.
Also a number of injuries, no one of which alone could be the direct cause of death, may cause death on the spot or very soon afterward. Death in such cases, where there is no large effusion under the skin, is referred to exhaustion, which, however, is merely another term for shock. Such cases are exemplified by prize-fighters who, during or after the fight, become collapsed and die of exhaustion. Having sustained numerous blows on the body during the many rounds, the body presents the marks of various bruises, but there may be nothing else to explain the sudden death. No one injury or bruise is mortal, and yet, when the deceased was previously sound and in good health, death must be referred directly to the multiple injuries received in the fight. We have already stated above that if the injuries are numerous, the loss of a smaller amount of blood may be fatal. We see, therefore, that there is not always a specific and visible “mortal” injury to account for death. This is a well-known medical fact, but it does not accord with the erroneous popular prejudice that no one can die from violence without some one visible wound which is mortal. In other words, the non-professional mind leaves out of account the idea of shock, only regarding material injury and not functional disturbance. If the circumstances accompanying death are unknown, it is well to be cautious. But if the deceased was in ordinary health and vigor and there was no morbid cause to account for the sudden death, we need not hesitate to refer death to the multiple injuries.
II. Was the Wound the Cause of Death Necessarily?
This brings up a number of interesting questions to be considered. In medical jurisprudence there is probably no condition so common as that the injury is admitted, but death is attributed to some other cause. Thus if there are several wounds it may be hard to decide on the relative degree of mortality of any particular one, so as to be able to say that death was directly or necessarily due to this or that one. The defence may plead that death was not necessarily due to the particular wound attributed to the prisoner. This brings up the question—
Which of two or more Wounds was the Cause of Death? No general rule can be laid down for all cases, but[501] each case must be judged by itself. Another way of putting the question is: “Which of two or more wounds was mortal?” The questions are not quite synonymous, for two or more of the wounds might be “mortal” but not equally the cause of death. In fact, as we have already seen, no one of the wounds if they are multiple may be of itself mortal, but taken together they are so. Consequently we will suppose that there are but two wounds, and not multiple ones, and the question remains which of these wounds was the cause of death. A wound may be said to be of itself mortal when it is the cause of death directly or indirectly in spite of the best medical assistance. In some continental states mortal wounds are divided into two classes, those absolutely and those conditionally mortal, the former including those in which the best medical assistance is at hand, sent for or timely rendered without everting the result. The mortal result in the second class is conditional on want of treatment, improper treatment, or accidental circumstances. As Taylor says, it is better to look at the effect of the wound and the intent of the assailant, as is done in English law, rather than at accidental relations of the wound.
To return to the question, we can readily imagine that a man may receive two wounds at different times or from different persons, and die after the second wound. Taylor[629] mentions the following case in which the question arose as to which of two injuries caused death: In Reg. v. Foreman (C.C.C. February, 1873) the prisoner had struck the deceased some severe blows on the head. A fortnight later, having partially recovered, another man gave him some severe blows on the head. A fortnight later still he had left hemiplegia, and died a few days later of a large abscess in the brain. The question arose which set of blows had been the cause of the abscess. The prisoner, the first assailant, was acquitted, as the deceased had had no serious symptoms until the second assault, and there was no satisfactory medical evidence as to the relation of the two assaults to the abscess formation. The same author also supposes the following case: A man having received a gunshot wound of the shoulder is doing well, when in another quarrel he receives a penetrating stab-wound of the thorax and abdomen.[502] He dies after lingering for a time, under the effects of these wounds. If the wound of the shoulder could be proven to be the cause of death, the second assailant could not be convicted of manslaughter, and so too with the first assailant if it could be shown that the victim died of the stab-wound. It might be possible for a surgeon to decide the question definitely at once if death occurred soon after the stab, which was found to have penetrated the heart, a large blood-vessel, or one of the viscera; or, on the other hand, if the stab-wound was found to be superficial and not penetrating, and the wound in the shoulder had suppurated and caused septicæmia.
In either or any case, everything would depend upon the evidence furnished by the medical witness. His knowledge and judgment are required to distinguish the guilty from the innocent.
Again, sometimes death may appear to be equally the result of either or both wounds, in which case, as far as the medical evidence goes, both assailants would be liable to the charge of manslaughter. Or the second wound may be accidental or suicidal, and again the question would arise as to the cause of death. A case illustrating this is told by Taylor[630] substantially as follows: A grocer’s assistant pursued a thief, who had stolen from a cart, into a coal-shed, where he was stabbed twice in the abdomen. The larger wound suppurated, the smaller wound healed up, and the man died of peritonitis. On post-mortem examination the suppurating wound was found not to involve a vital part, while the small healed wound had wounded the liver and gall bladder and had set up the fatal peritonitis. The large suppurating wound had apparently been inflicted purposely; the fatal wound, directed upward and backward, might have been accidental by the deceased rushing upon the knife held more or less in self-defence. The case never came to trial, as the assailant was never found, but it can be readily imagined what complications might have arisen.
Furthermore, the wounded person may have taken poison or been subsequently ill-treated, and he may have died from these causes rather than the injury. But the question arises as to whether the wound was necessarily the cause of death. Here, in order to exculpate the assailant, the supervening disease or[503] maltreatment must be such as to account for sudden or rapid death under the symptoms which actually preceded death.
Was Death Due to Natural Causes? Again, the injury may be admitted, but it may be claimed that death is due to natural causes. It is not unusual for wounded persons to die from natural causes, though the case may appear otherwise to laymen. This is often seen with suicidal wounds, especially those inflicted during the delirium of a disease, or the disease may supervene later and cause death without relation to the wound. Where the wound was inflicted by another, accurate discrimination is especially important in order to save the accused from imprisonment under false accusation and consequent loss of character. A careful examination is the only way to determine such cases, which depend therefore on the medical testimony.
Again, the question may arise as between DEATH FROM WOUNDS OR LATENT DISEASE, the wound perhaps being admitted, but death being attributed to latent disease. Here a close attention to symptoms and a careful post-mortem examination can alone decide. A man may die from the rupture of an aneurism, from an apoplexy or some other morbid condition after receiving a severe wound. Or a man with a hernia may receive a blow upon it causing a rupture of the contained intestine followed by peritonitis and death, or the recipient of a blow may have a calculus in the kidney which may perforate a blood-vessel or the kidney tissue and set up a fatal hemorrhage as the result of a blow.
Thus, medically speaking, the result of the injury is unusual and unexpected, and due to an abnormal or unhealthy state of body of the wounded person.
If it can be clearly shown by the medical testimony that death was due to the above or any other latent diseases, the responsibility of the assailant may be lessened or removed. The law looks to this point and is lenient in its punishment in the absence of malice on the part of the assailant. The crime is still manslaughter and may even be murder if the assailant was actuated by malice and the abnormal or unhealthy state of the body of the victim was taken advantage of. Generally there is no intention of murder, but the nature of the wound and the means of infliction will help to show this, which is for the jury rather than the medical witness to decide.[504] There is less ground for mitigation of the punishment if the assailant was aware of the peculiar condition of the wounded person, especially in the case of those notoriously ill or of pregnant women.
Closely allied with this subject are those rare cases where ABNORMAL ANATOMICAL CONDITIONS, such as a thin skull or brittle bones, cause a slight injury to be followed by unexpected and untoward results, not to be looked for in the average individual. In such cases the evidence of the abnormal condition furnished by the medical witness may diminish the responsibility and mitigate the punishment.
Furthermore, the responsibility of the assailant may not be altogether removed, for the question naturally arises, Was death accelerated by the wound? This depends upon the circumstances in each case upon which the medical witness must base his opinion. Maliciously accelerating the death of another is regarded as criminal on the principle that that which accelerates causes. The following cases are quoted from Taylor[631] to illustrate the above distinctions. In Reg. v. Timms (Oxford Lent Ass., 1870) the deceased had been struck on the head by the accused with a hatchet, from which injury he had partly recovered under treatment in twelve days. But six weeks later he was seized with inflammation of the brain, with convulsions, and died. At the autopsy disease of the kidneys was found, and death was referred to this and the inflammation of the brain due to the blows. The prisoner was convicted after the judge had charged the jury that it was manslaughter if they believed that the blows conduced in part to the death of the deceased.
In the following cases there was no connection between the violence and the cause of death. A man struck his father on the head with a hammer and was sentenced to two months’ imprisonment, as the injury did not appear serious. The father thought the punishment too little, became much excited, and was hemiplegic six days after the wound was inflicted and died three days later. No injury of the brain was found under a fracture of the inner table at the site of the blow, but a large clot was found in the lateral ventricle which, in the opinion of the medical witnesses, was not dependent on the blow, and the[505] prisoner was acquitted (see Reg. v. Saxon, Lancashire Sum. Ass., 1884). Also in Reg. v. Hodgson (Leeds Sum. Ass., 1876) the prisoner had struck his wife with a belt, a short time after which she fell back and died suddenly. The cause of death was found to be heart disease, and the blow not being causative in producing the fatal result, the prisoner was acquitted. Or again in Reg. v. Thompson (Liverpool Sum. Ass., 1876): The prisoner had stabbed his wife in the cheek. The wound was severe but not mortal. Two days later she was delivered of a child in the infirmary to which she was taken. She died nine days later of puerperal fever. The prisoner was acquitted on the charge of murder, as there was no necessary connection between the wound and the puerperal fever. Acquittals have taken place in cases of death occasioned by terror or dread of impending danger produced by acts of violence, as in the case of Reg. v. Heany (Gloucester Lent Ass., 1875). Here the prisoner in an altercation with his wife, who was suffering from cancer, held up a knife in a threatening manner, but did not touch her. This gave her a shock; she died two days later from fright. As there was no distinct proof that death was accelerated by this act, the prisoner was acquitted of the charge of murder. Taylor[632] found among a large number of cases occurring in England during twenty years that the latent causes of death, as registered in wounded persons, were chiefly inflammation of the thoracic or abdominal viscera, apoplexy, diseases of the heart and large blood-vessels, phthisis, ruptures of the stomach and bowels from disease, internal strangulation, and the rupture of deep-seated abscesses. Sometimes the person was in good health up to the time of injury, while in other cases there was merely a slight indisposition. It was only by carefulness on the part of the medical experts that the true cause of death was ascertained.
Again, it may be claimed that DEATH was not necessarily the result of the wound and was AVOIDABLE BY GOOD MEDICAL TREATMENT. There are many cases of wounds not mortal with proper and skilled treatment which might become so by improper treatment. They may thus become directly mortal by interfering with a source of hemorrhage which had been arrested, or secondarily mortal by infection of the wound by meddlesome[506] treatment. It would depend on the medical witnesses to determine whether and how far the treatment had been responsible for the fatal result. If the wound is not of itself mortal and it has only become so from improper treatment, this should be a mitigating circumstance in favor of the accused. Medically speaking, we can seldom make the sharp distinction which Lord Hale did legally between a wound becoming mortal from improper treatment and one in which improper treatment causes death irrespective of the wound. In case of a slight wound this distinction might be possible, but not so in case of severe wounds. Also there would probably be no conviction, as far as the medical evidence is concerned, if the wound was only mortal in consequence of improper treatment and not mortal as its usual and probable result. This may naturally introduce the question of the COMPARATIVE SKILL IN TREATMENT. If death is entirely or partly due to a wound the responsibility of an assailant is not altered by unskilful treatment. The entire question of the relation of the wound to the fatal result and the effect on this result of the treatment employed is left to be determined by the medical experts, and in its solution great care and judgment must be used. Although a given fatal wound might not have caused death under the best possible treatment and surroundings, yet, according to the above rule, the assailant is held responsible as long as the fatal result is due partly, at least, to the wound. Therefore we see the responsibility of the surgeon not only for the life of his patient, but also for that of the prisoner. He should, therefore, not deviate from the ordinary and most accepted practice in such cases, as any such deviation is taken hold of by the counsel for the defence. In fact, every point of the treatment is subjected to criticism.
In a lacerated wound of the foot, if death occurs from tetanus, it may be claimed that death would not have occurred if the foot had been amputated, or, if the foot were amputated and death followed, it may be claimed that amputation was unnecessary and was the cause of death. The surgeon should, therefore, be able to give the best reasons for every step of treatment.
Again, it may be claimed that DEATH was not a necessary result of the wound and WAS AVOIDABLE BUT FOR IMPRUDENCE[507] OR NEGLECT on the part of the wounded person. A man after being wounded may refuse to receive medical assistance, or, after receiving it, may disobey instructions or refuse to submit to an operation proposed. Thus with a compound depressed fracture of the skull the patient may either refuse to see a surgeon, or he may refuse to submit to an operation proposed, or he may with or without operation disobey the instructions as to diet and quiet, and eat or drink heavily and refuse to go to bed. Such a case we can readily imagine might die of meningitis, etc.
If the symptoms of a wound are unfavorable from the start, or if the wound of itself is likely to prove mortal, the responsibility of the assailant is unmitigated by imprudence or neglect of medical assistance by the wounded person. This is not allowed as mitigatory, as a sane man is a free agent and is not obliged to call in or submit to medical treatment. Moreover, a medical witness in many cases could not swear that an operation or other plan of treatment would certainly save life. Thus an amputation of the leg for wound of the foot causing tetanus is by no means a certain means of cure. But we can readily imagine a case where the refusal to submit to the treatment proposed might be an important element in causing death. Thus in a compound depressed fracture of the skull with compression, the medical witnesses would agree that the operation would in all probability save life. This fact would probably be only mitigatory in diminishing the penalty, and, as stated above, would not secure acquittal. But it is none the less important for the medical witness to bear these facts in mind and bring out the facts and conclusions clearly in his testimony.
Death Following Slight Personal Injuries.—Here again the claim might apparently be justified that death was not necessarily due to the trifling injury. And in reality there is commonly some unhealthy state of the body to explain such an unexpected result. When the disease accounting for this unhealthy state of the body is in some other part than the injury, an examination with ordinary care will explain the case. But if the disease and injury are located in the same part, especially in the head, the case is more perplexing, but may be cleared up by careful and thorough examination. Also the usual results of such an injury should be considered, and whether the disease[508] would be a usual result of the injury, or whether the sum total of the pathological conditions found would be accounted for by the violence. It should be remembered that the presence of chronic disease is no excuse. Thus Taylor[633] cites the case of Reg. v. Hapley (Lewes Aut. Ass., 1860), where a boy with chronic disease of the brain suffered from no unusual symptom until he received a severe flogging, which was followed by death in less than three hours. The same author mentions also the following case to show that fatal results may follow very slight and trivial blows. Annan[634] tells of a healthy four-year-old girl who received a slight blow from the shaft of a wheelbarrow on the skin about three inches below the knee. There was even no external mark of violence, and the injury was thought to be so slight as not to require treatment. There was pain, however, which increased on the following day, marked constitutional symptoms appeared, and the child died on the fourth day. Even to the punishment inflicted by schoolmasters death has been imputed.
When DEATH occurs FROM WOUNDS AFTER LONG PERIODS the injury may be admitted, but it may be claimed that death was not necessarily due to the wound. Medically speaking, death is just as much the result of the injury as if it occurred on the spot. Of course, death must be clearly traceable to the usual and probable results of the injury, and not be dependent on any other cause. An examination of the wounded part and of the whole body will enable the medical witness to determine the cause of death and whether it is clearly traceable to the injury. A doubt on this point may lead to acquittal. Certain forms of wounds or wounds in certain localities are especially liable to end fatally after a long delay, but as the direct result of the wound. These are wounds of the head and of the spine. As to the first class, the injured person may apparently recover and be doing well, when he may suddenly die from a cerebral abscess, for instance. This is the result of the injury, but remains a longer or shorter time latent. In wounds of the spine the patient is generally paralyzed below the point of fracture, but is apparently in good health. In a longer or shorter time he may die of a pneumonia, cystitis, or bedsores, which are the[509] known and regular consequences of the injury or injured condition. Astley Cooper cites the case of a man who was injured on the head and died two years later from the effects of the injury, as was clearly made out by the continuance of brain symptoms during the entire period. An interval of eleven years occurred in another head injury between the injury and the fatal result. The first result of the injury was concussion of the brain, and the case is mentioned by Hoffbauer.[635] This long interval is unusual. There is a rule in English law by which the assailant cannot be indicted for murder if the victim of the assault lives a year and a day. Practically this makes little difference, as nearly all cases would die within that time; but the principle is wrong as looked at from the medical standpoint. The protracted cases concern, as above stated, mostly injuries of the head, spine, and chest, among which there are some cases, like the examples cited, where, according to English law, justice would fail to be done.
III. Was a Wound the Cause of Death Secondarily?
A wound is secondarily the cause of death when the victim, having recovered from the first ill effects, dies from some wound disease or accident or from a surgical operation rendered necessary in the proper treatment of the wound. There may be much difficulty in establishing the proof of death from a wound by means of secondary causes, for, 1st, the secondary cause must be in the natural course of things; and, 2d, there must be no other accidental circumstances to occasion the secondary cause.
The secondary cause may be partly due to the constitution of the deceased from habits of dissipation, which fact would serve as an expiatory circumstance in the case. Among the secondary causes of death may be mentioned septicæmia, pyæmia, erysipelas, tetanus, gangrene, that is, wound diseases, also the wound accident—as we may call delirium tremens, and surgical operations rendered necessary to the treatment of the case. We may add, besides the regular wound diseases, inflammation in and about the wound, septic in character, perhaps not justifying the title of septicæmia, but which, with its accompanying fever, may be the “last straw” in a case which might otherwise[510] recover. Some of these secondary causes will now be considered more at length.
Septicæmia is a general febrile disease due to the absorption into the system from a wound of the products of bacteria or due to the introduction into the blood and tissues of the bacteria themselves. Depending on the two sources of origin, we have two forms of septicæmia: 1. Septic intoxication or sapremia, due to the absorption of a chemical poison, ptomaïnes, and often readily influenced and cured by the removal of the source of these ptomaïnes in decomposing blood-clots, secretions, etc. 2. Septic infection comes on less rapidly but is more serious than the former is, if properly and quickly treated, because the source of the trouble cannot be removed, but is in the blood and the tissues. The latter form is the more common one in wounds, though the former may occur in abdominal wounds, especially when a blood-clot is present. The first form begins acutely, the second form more gradually. The infection in septicæmia takes place through a wound and may be due to the weapon which caused the wound, the unclean condition of the parts wounded, or to the subsequent treatment or want of treatment. It may even take place through the intestinal mucous membrane as in cases of tyrotoxicon poisoning. It is most likely to occur during the first four or five days before the surfaces of the wound granulate, and it consists in the introduction of bacteria, especially staphylococci and streptococci. The disease is characterized by severe constitutional symptoms, acute continuous fever, inflammation of certain viscera and of the wound, and nervous disorders. A pronounced chill ushering in the fever is generally absent. Prostration is especially marked, the patient finally passing into a typhoid condition indifferent to surroundings. Anorexia and headache are usually present; diarrhœa is common, vomiting is not. The skin is pale and dusky, but not commonly icteric; at first it is hot and dry, later moist and finally cold and clammy. The spleen is often enlarged. The pulse becomes weak and rapid and delirium is followed by coma. The prognosis is grave. Antiseptic treatment generally prevents and often cures the disease, as is the case with many other of the wound diseases; hence the failure to employ it may be alleged by the defence in mitigation of the responsibility of the assailant for the fatal result.
Pyæmia is closely allied to septicæmia. It is due to the setting free of bacterial emboli or septic emboli from a broken-down, septic thrombus in the neighborhood of the wound, and the circulation of these emboli in the blood until they are arrested and form the characteristic metastatic abscesses, especially in the lungs, joints, abdominal viscera, and parotid gland. Almost always the source of infection is an infected wound. Granulation does not prevent the occurrence of pyæmia, which, as a rule, commences at a later stage than septicæmia. It is most important, however, for our purpose to remember that there is such a thing as spontaneous pyæmia. An injury not causing a wound may here be the exciting cause, but the resulting pyæmia is an unexpected consequence. A bruise of a bone, for instance, by allowing bacteria, which in certain conditions may be circulating in the blood, to find an exit from the vessels into the bruised part, may develop an acute osteo-myelitis, which may be a starting-point of a pyæmia. It is but proper to state, however, that spontaneous pyæmia is a rare occurrence. In fact, it is so rare that if pyæmia occurs and we find ever so trifling an infected wound, we can safely attribute the pyæmia to the wound and not to a spontaneous origin.
Pyæmia begins, as a rule, in the second week of the healing process or even later. It usually begins with a chill, which may be frequently repeated. The fever is very irregular and exacerbations occur with each metastatic abscess. The skin is icteric, the icterus being hematogenous. The pulse is rapid and becomes weaker. Infective endocarditis may develop, which increases the danger of metastatic abscesses, which may then occur in the brain. Otherwise the mind is clear and unaffected until the final delirium and coma. The disease may become chronic, but usually lasts a week or ten days. The prognosis is very grave.
Erysipelas is a still more frequent complication of medico-legal wounds, and though not so fatal as the two preceding, it is probably more often the secondary cause of death on account of its far greater frequence. It too is an acute infective inflammation due to the presence of a micro-organism, streptococcus erysipelatis. This occurs mostly in the lymphatics of the skin, and effects an entrance through some wound or abrasion of the skin or mucous membrane, which may be almost[512] microscopic in size. Probably there is no such thing as true spontaneous erysipelas, though the wound may be often overlooked and only visible on the closest examination. If a wound has been inflicted, the size and severity of it cannot be alleged as a reason why it was not the starting-point of an erysipelas. The erysipelas must be clearly traced to the injury. That is, it must occur before recovery from the wound or not later than a week after it has healed, for the incubation is probably not longer than this. It is difficult to connect an erysipelas with a wound if it occurs some time after it has healed or if it occurs at a different place and not about the wound. Wounds of certain regions, as, for instance, scalp wounds, are especially liable to develop erysipelas, but this is probably owing to the imperfect antiseptic treatment or delay in applying it. Certain individuals are more prone to it than others; thus it has been stated that blondes and those suffering from Bright’s disease are more susceptible, though how true this is it is hard to say. It is also probably more prevalent at certain times of the year, particularly in the spring. A wound after it has scabbed over or has begun to granulate, that is, after the first four or five days, is very much less apt to serve as the avenue for infection. Erysipelas usually begins with a chill, or a convulsion in children. Nausea and vomiting are the rule. The fever is remittent and ranges from 102° to 104° F., and the temperature may be subnormal when the inflammation is subsiding. Prostration is marked and the pulse more or less weak. There may be delirium while the fever is high. Locally there is rarely anything characteristic until twenty-four hours or so after the chill. Then we have a reddish blush with some tension, burning and itching of the skin. At first the redness is most marked about the wound, later at the edge of the advancing, serpentine margin. It spreads widely and rapidly, and after three or four days the part first attacked begins to improve. Desquamation follows. The duration may be a week or ten days or as long as a month. The inflammation may be much more severe, involving the subcutaneous connective tissue in phlegmonous erysipelas.
Facial erysipelas is a common variety and was once regarded as idiopathic, but a wound on the skin or mucous membrane is probably always present. The prognosis of erysipelas[513] is usually favorable. Since the use of antiseptics it is far less common than formerly, though still the most common of the infective wound diseases.
If a man wounded in an assault is taken to a hospital where erysipelas prevails, the question of responsibility arises, for, medically speaking, he is subjected to great and avoidable risks.
Tetanus is an infective bacterial disease affecting chiefly the central nervous system and almost always, if not always, originating from a wound. Tetanus, like erysipelas, is probably always traumatic and never strictly idiopathic. The wound may be so slight as to escape notice. When it follows such injuries as simple fracture internal infection probably occurs, though such cases are extremely rare. It is said that the weather influences the development of tetanus, and that it is more common in the tropics. There are also certain sections where tetanus is much more common than elsewhere and where it may be said to be almost endemic. Punctured wounds are most likely to be followed by tetanus, for they offer the best opportunity for the development of the bacteria, which are anaërobic. Wounds in dirty parts of the body, like the hands and feet, are more apt to be followed by tetanus than those elsewhere. Tetanus usually appears about the end of the first week after a wound has been received, but it may not appear for a longer period, even three or four weeks, so that the wound may have been some time healed. To connect tetanus with a particular wound, note (1) if there were any symptoms of it before the wound or injury, (2) whether any other cause intervened after the wound or injury which would be likely to produce it, and (3) whether the deceased ever rallied from the effects of the injury. Tetanus comes on suddenly without warning. The injured person first notices that he cannot fully open the mouth, he has lock-jaw, and the back of the neck is stiff. The muscles of the abdomen and back are next involved so that the back is arched in the position known as opisthotonos, and the abdomen presents a board-like hardness. The muscles of the fauces, pharynx, and diaphragm may next become involved, causing difficulty in swallowing and breathing. The thighs may or may not be involved, but the arms and legs almost never. Owing to the spasm of the abdominal muscles,[514] micturition and defecation are difficult and respiration is hindered. The muscles are in the condition of tonic spasm which permits the patient no rest, the face bears the “risus sardonicus,” and the suffering is extreme. If the patient lives more than two or three days the tonic spasm partly gives way to increased reflex irritability, in which a noise, jar, or draught of air may give rise to clonic and tonic spasms in the muscles affected. The patient may die at such times from tonic spasm of the respiratory muscles, or he may die of prostration from want of food and sleep, worn out by the suffering and muscular spasm. The mind is usually clear to the last. Fever is not characteristic of the disease. Tetanus may be rapidly fatal; in two or three days, or it may be or become more chronic. The prognosis of acute tetanus is almost invariably fatal; that of chronic tetanus is grave, but a certain proportion of cases recover.
Diagnosis.—This is easy. It differs from a true neuritis in the peripheral nerves in that no matter where the wound is situated the first symptom is in the muscles of the jaw and the back of the neck, and not at the site of the injury and distally from this point. Trismus is applied to a milder form of the disease in which only the face and neck muscles are involved and “lock-jaw” is a prominent symptom. Some cases of tetany may be mistaken for so-called spontaneous tetanus. Tetany may follow child-bed, fevers, mental shocks, exposure to cold and wet, extirpation of goitre, intestinal irritation, etc. It consists of painful tonic spasms of the muscles of the arms and feet. The attacks last one-half to two hours or more, and may be preceded by a dragging pain. They may be brought on by pressure on the nerve leading to the muscles affected. Striking the facial nerve often causes contraction of the face muscles. There is no trismus but there may be opisthotonos. The patient seems well between the attacks and most cases recover without treatment.
Delirium tremens may occur as a secondary consequence of injuries, or necessary surgical operations in the case of those who are habitually intemperate. Those who habitually use opium, tobacco, cannabis indica, or even tea or coffee to excess are said to be subject to it. It may, therefore, be justly alleged that death is avoidable in very many cases, but for an abnormal[515] and unhealthy state of the body. The disease is characterized by delirium, a peculiar tremor of the muscles, insomnia, and anorexia. Pneumonia may complicate the case. The patients die in fatal cases from exhaustion due to insomnia, lack of nourishment, and their constant activity of body and mind. The prognosis is usually favorable, taking all cases together, but in delirium tremens secondary to surgical injuries or operations the prognosis is serious.
Death from surgical operations performed for the treatment of wounds. The operation is a part of the treatment, and if it is done with ordinary care and skill the accused is responsible for the result. The necessity and mode of operation must be left to the operator’s judgment. As the defence may turn on the necessity for and the skilful performance of the operation, it is well to wait for the advice and assistance of others if practicable, for death is not unusual from severe operations. The patient may die on the operating-table after losing little blood, from fear, pain, or shock. Or he may die from secondary hemorrhage or any of the secondary causes of death from wounds enumerated above. The evidence of the necessity of the operation must, therefore, be presented by the operator. If an operation is necessary and not performed, the defence might allege that death was due to the neglect of the surgeon. Another question for the medical witnesses to determine is whether the operation was rendered necessary because of improper previous treatment, for if it was the responsibility of the assailant may be influenced. The meaning of the term “necessity” is here a matter of importance. Unless an operation is necessary to the preservation of life, if death occurs there is some doubt whether the assailant is responsible. But, medically speaking, we would not hesitate to urge an operation on a wounded man in order to preserve function, or even to save deformity as well as to save life. In the case of operations done under a mistaken opinion, neither necessary to save life nor, as the result proves, to save function or guard against deformity, if death follows the assailant may be relieved from responsibility. Thus an aneurism following an injury might be mistaken for an abscess and opened with skill but with a fatal result. It is also for the medical experts to determine whether an operation was unnecessary or unskilfully performed, for if it were and death resulted[516] from it, the responsibility of the prisoner is affected unless the original wound would be likely to be fatal without operation. According to Lord Hale, if death results from an unskilful operation and not from the wound, the prisoner is not responsible. But yet death may occur as the result of the most skilful operation necessary to the treatment of a wound, and not be dependent at all on the wound itself. If the operation is skilfully performed, and yet the patient dies from secondary causes, such as those above enumerated or any others, the prisoner is still responsible, and the medical testimony is concerned with the performance of the operation and the secondary causes of death. The relative skill of the operator or surgeon is probably not a question for the jury in criminal cases, on the ground that the man who inflicts the injury must take all the consequences, good or bad. In a civil suit, for instance an action for malpractice, the case is otherwise, and all the medical facts and opinions are submitted to the jury. The law regards three circumstances in death after surgical operations: (1) The necessity of the operation, (2) the competence of the operator, and (3) whether the wound would be fatal without operation.
Death may occur from anæsthetics used in an operation without any recognizable contributing disease of the patient, or carelessness or lack of skill in the administration of the anæsthetic. Of course, the question of absence of contributing disease on the part of the patient and of its proper administration must be satisfactorily answered in cases of death from the anæsthetic in an operation rendered necessary in the treatment of a wound. Death from an anæsthetic may occur before, during, or after an operation itself. Medically speaking, the necessity of the use of an anæsthetic in operations cannot be questioned, and in emergencies where an operation becomes necessary, and not a matter of choice, its use, with special care, is justifiable even with existing organic disease, which usually contraindicates it. As death may be alleged to be due to the use of a particular anæsthetic, it is always best in operating on account of an injury which may require a medico-legal investigation, to use that anæsthetic which is most generally used and indorsed in the particular section of country in question. Of course, it is not lawful to operate against the will of a person[517] who preserves consciousness and will. It may be added in this connection that if a medical man be guilty of misconduct, arising either from gross ignorance or criminal inattention, whereby the patient dies, he is guilty of manslaughter, according to Lord Ellenborough. Omissions or errors in judgment, to which all are liable, are not criminal.
IV. Was the Wound made by the Instrument Described?
It is not often necessary to prove that a weapon was used, though it may affect the punishment. For the use of a weapon implies malice and intention and a greater desire to do injury. The prisoner may swear that no weapon was used when the nature of the wound clearly proves that one was used. The explanation of the prisoner of the origin of the wound may thus be discredited. We cannot often swear that a particular weapon was used, but only that the wound was made by one similar to it in shape and size. Thus Schwörer tells of the case of a man stabbed in the face by another. The medical witness testified that the wound was caused by a knife shown at the trial which had a whole blade, but a year later the point of the knife which had really caused the wound was discharged from an abscess in the cheek at the site of the wound. The surgeon thus made a too definite statement in regard to the knife shown.
It is often very difficult to answer the above question. We base our opinion chiefly on two sources: 1st, and most important, by an examination of the wound, and, 2d, by an examination of the instrument said to have been used. Certain particulars of the wound may furnish indications as to the weight, form, and sharpness of the instrument used. There are certain wounds which must have been made by an instrument, namely, incised and punctured wounds. The above question is determined more or less by what has been said in a former section on wounds, but we will now consider what special features of these and other classes of wounds indicate the nature, shape, size, etc., of the weapon used.
Incised wounds must be made by a cutting instrument. We would here exclude those contused wounds of the scalp and eyebrows which closely resemble incised wounds, but we have already seen that we can diagnose between these wounds and[518] incised wounds by careful inspection. But the locality should put us on our guard, so that in case of wounds of these two regions we should be especially careful in making the examination.
In the case of incised wounds we cannot often tell the shape or size of the weapon, but we are able to tell certain characteristics about it. The sharpness of the instrument may be inferred from the clean and regular edges. The depth of the wound may also indicate the sharpness of the weapon. A long “tail” in the wound indicates that the weapon was sharp as well as that this was the part of the wound last made. If the edges of the wound are rough, we may infer that the edges of the weapon were rough and irregular. Wounds caused by bits of china or glass or fragments of bottles, besides having rough and lacerated edges, are characterized by an irregular or angular course in the skin.
Some cutting weapons, like an axe, act as much by means of their weight as by their cutting edges. Wounds caused by such weapons we can often distinguish by the following signs: The edges are not as smooth as is the case with a cutting instrument, and they may be more or less lacerated and show signs of contusion. The wound is often deep in comparison with its length, and the ends of the wound abrupt instead of slanting up from the bottom to the surface. The section of resisting organs and the impression of the edge of the weapon on the bone are further signs of the use of such a weapon.
The form and direction of a wound may possibly give some indication of the form of the instrument—for instance, whether it be straight or curved like a pruning-knife, as in the case cited by Vibert[636] of a wound of the neck which suddenly became deeper toward its extremity and changed its direction; the whole being explained on the supposition that it was made by a pruning-knife.
But it is in punctured wounds especially that we are enabled most often and most accurately to determine the kind of a weapon used. Here from the form of the wound we may judge of the form and size of the weapon. In speaking of punctured wounds in a former section we divided them into four groups, reference to which may here be made. In the first[519] group, or those caused by cylindrical or conical weapons, when the weapon is very fine it may leave no track at all; if a little larger, we may infer from a linear bloody track that the weapon was needle-like in shape. The length of the instrument or the depth to which it penetrated may be found, as a rule, only by dissection. If the weapon were larger and conical, we have seen that the wounds would be linear with two angles, the length of the wound being parallel to the direction of the fibres in the skin.
Here we may judge of the form of the weapon from the following circumstances: From a comparison of the depth with the size of the opening, we know that it was a punctured wound. The edges and angles are not smooth and even enough for a stab-wound with a knife, for the edges are torn and not cut, and a stab-wound would be the only form of wound with which we would be likely to confuse it. Furthermore, the direction of the long axis of the wound parallel to that of the skin fibres in the region in which it occurs and the very slight retraction of the edges distinguish it from a stab-wound. By these signs we can almost always distinguish such wounds from stab-wounds, and thus tell the form of the weapon used. As to the size of weapon used, these wounds if of any size are generally smaller than the weapon, for the skin is put on the stretch by the weapon and yields to a certain extent. The actual wound, therefore, is smaller in circumference than the weapon. The size of the wound is smaller than that part of the weapon occupying the wound when the weapon was arrested; it may be very much smaller than the weapon at its largest point. Small wounds of this kind are generally larger than the instrument producing them.
The second group of punctured wounds, or stab-wounds, are by far the most common and, therefore, the most important variety of punctured wounds. If the stab-wound is perpendicular to the surface the form of the wound may represent pretty closely that of the weapon at the point where the latter was arrested, whether it has a single or double cutting edge. But even here there are exceptions. Frequently a weapon with a broad back and only one cutting edge may produce a wound resembling that of an instrument with two cutting edges, the second angle tearing as in the former class. Here[520] on close examination we can sometimes distinguish the difference between the two angles, and judge correctly of the shape of the weapon. In fact, wounds made by common pocket-knives are regularly slit-like and not wedge-shaped, as the wound is caused only by the cutting edge of the knife. Again, if the single cutting edge is blunt, in rare cases the wound is produced in the same manner as those of the first group, or conical and cylindrical instruments. We would be led to suppose that the wound was produced by such an instrument, as both angles are torn, unless the direction of the wound might not follow that of the fibres of the skin, in which case we would be left in doubt. Stab-wounds are sometimes angular from the knife being withdrawn in a slightly different direction from that in which it was introduced or from an unequal retraction of the skin (see Fig. 9). If the stab-wound is obliquely directed, we can still judge of the general shape of the weapon, with exception of the cases above mentioned. The dimensions and size of the weapon are here much harder to determine. The dimensions of a stab-wound in the skin may be the same as those of the weapon, or of that part of the weapon which is arrested in the wound, but often they are not so. To measure the size of a wound exactly so as to get at the exact size of the instrument, we should place the region of the wound in the same position, etc., that it was when the wound was inflicted, and this we cannot often do. As the skin was tense or relaxed at the time the wound was inflicted, so the wound in the skin appears smaller or larger, just as with a sheet of rubber under similar conditions. If the instrument is very blunt, the wound in the skin may be smaller than the weapon whether the skin near the wound is tense or not. Thus Hofmann saw the wound from a blunt bayonet one centimetre shorter than the weapon.
The wound of the skin may be shorter and broader than the weapon used on account of retraction of the edges of the wound, and this is especially marked when the wound lies transversely to the direction of the skin fibres. On the other hand, the length of the external wound is more often greater than that of the weapon, because the wound is elongated by making pressure toward the cutting edge on withdrawal of the weapon, and an oblique wound measures longer than the weapon. If the[521] blow is from above downward and the cutting edge of the weapon is uppermost, the length of the wound is not so likely to be increased much beyond the measurement of the weapon as when the cutting edge is directed downward. There is but one condition in which a stab-wound is at all likely to correspond in dimensions with that of the weapon, and that is when the wound is perpendicular to the surface. Even here the wound may be lengthened on withdrawal of the weapon, and we have to allow for retraction of the edges and try to put the parts in the same condition of tension or laxity as at the time of wounding. Even in the most favorable case, therefore, we cannot with certainty tell the exact size of the weapon. If a stab-wound be directed obliquely to the surface, then the length of the wound is greater than that of the weapon, unless this increase be exactly counterbalanced by the lateral retraction of the wound. The size of the weapon in such oblique wounds is further obscured by the changes of size due to withdrawal of the weapon, retraction of the edges, and the condition of the tension of the skin at the time the wound was inflicted.
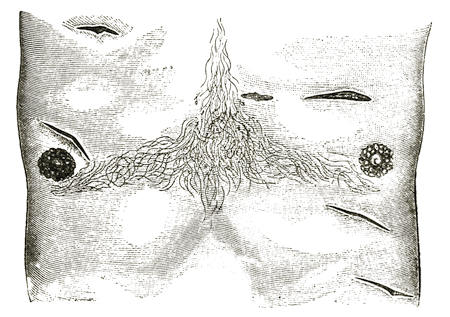
Fig. 9.—Angular Stab-Wounds of the Anterior Chest Wall caused by a Strong Pocket-Knife.
Dupuytren remarks that stab-wounds are smaller than the weapon owing to the elasticity of the skin, but a lateral motion of the weapon may cause considerable enlargement of the[522] wound. If a stab-wound has traversed a part of the body, the wound of exit is smaller than that of entrance.
The depth of a punctured wound may be any part of the length of the weapon, or it may even be deeper than the length of the weapon owing to a depression of the surface by the force of the blow, or the pressure of the handle of the weapon or the hand holding it. We have already seen that this may occur in a marked degree in penetrating wounds of the abdomen involving one of the movable viscera, also in wounds of the thorax, partly from depression of the surface and partly from an expansion of the thorax when opened at the autopsy, thus increasing the measured depth of the wound. Punctured wounds of the third class made by instruments with ridges or edges, like foils, files, etc., present more or less the shape of the weapon if the edges are cutting, but not always so if the direction of the wound be oblique or the parts unevenly stretched. If the edges are not cutting they cause wounds more or less like the first class of punctured wounds, but we can often distinguish them from the latter by little tears in the edges. The entrance and exit wounds may not be alike.
Wounds made by bits of glass and earthenware have irregular and uneven edges. Taylor[637] relates a case, Reg. v. Ankers (Warwick Lent Ass., 1845), where the wound was attributed to a fall on some broken crockery, but the wound was cleanly incised and the prisoner was convicted. As it may be alleged in defence that a given wound was caused by a fall on broken crockery or other substances capable of producing a punctured wound, it is important to notice whether the edges are lacerated and irregular or smooth and clean. The author quoted above cites another case which occurred to Watson, where the prisoner alleged that a deep, clean-cut wound of the genitals of a woman which had caused her death was due to a fall on some broken glass. The character of the wound disproved this defence. Another feature of such wounds, especially if they be deep in comparison to their length, is that they are very apt to contain small particles of the glass or earthenware which caused them. In fact, in all wounds it is well to search for any small fragments which will throw light upon the weapon used.
Wounds caused by scissors are often of characteristic shape. If the scissors were open we find two symmetrical, punctured diverging wounds, presenting more or less clearly the form of the blades of the scissors. If the blades have been approximated there is a triangular interval between the punctures, the apex of which is truncated if any skin remains between the punctures.
Lacerated wounds may not indicate the weapon used as clearly as punctured wounds, but the agent which produced them is often indicated by the appearance of the wound. They are generally accidental. But where they occur, as they not infrequently do, on the bodies of new-born children, they may give rise to the charge of infanticide. In some cases the weapon which caused the wound fits the wound produced, and thus important evidence may be furnished the prosecution. Taylor[638] cites the case of Montgomery (Omagh Sum. Ass., 1873), where a bill-hook which fitted the injuries on the skull of the deceased was found buried in a spot to which the prisoner was seen to go. These facts connected the prisoner with the weapon and the weapon with the murder. In other cases the wounds may be so lacerated or contused that the indications of the weapon are obscured.
Contusions and Contused Wounds.—The shape of a contusing body is sometimes reproduced by the contusion and the ecchymosis. Thus we are enabled to distinguish the marks of a whip, the fingers, the fist, etc. This is best seen when the ecchymosis is fresh, for soon the edges extend and the outline is less clearly marked. Plaques parcheminées, which we have already described as the marks of contused erosions, may show the form of finger-nails, etc. Contused wounds like simple contusions may show the shape of the weapon.
If the contusing body has a large area, the whole of this area cannot often strike the body at once, so that the outline of the contusion does not represent that of the weapon. But in general, severe contusions present greater difficulties than the preceding classes of wounds. We must generally be content if we can determine whether the wound was caused by a weapon, including the fist, or by a fall, and we are often unable to say even this. A fall is often alleged by the defence as the cause[524] of the injury, but of course if the prisoner was responsible for the fall he is responsible for the results of the fall. If there are contusions or contused wounds on several parts of the head, or if the wounds are on the vertex of the head, it is presumptive of the use of weapons. We cannot often swear that each and every wound on the head was due to the use of a weapon. On the other hand, the presence of grass, sand, gravel, etc., in a wound is presumptive of a fall and of the origin of the wound in this manner. In case of a fall from a height the wound or wounds might be in almost any part of the body, on the vertex or elsewhere. Such a fall may be the result of accident, suicide, or murder. It is not unusual for female complainants to ascribe their wounds to a fall to exculpate the prisoner, especially if this happens to be her husband. We should remember that in the scalp or over the eyebrows a contused wound caused by a blunt instrument may resemble an incised wound. As already stated, however, if the wound is fresh careful examination will lead to a correct opinion, and the use of a sharp instrument may be disproved. If the wound is not recent there is great difficulty in judging of the cause. It is well to caution against accepting the interested statements of others in regard to the use of a weapon, unless the character of the wound bears them out very strongly. There may be a bad motive for imputing the use of a certain weapon to the assailant. It is far better to rely solely upon the evidence furnished by the wound in such cases.
It would be useful if we could lay down some general rules to discriminate between wounds caused by the blow of a weapon and those caused by falls, but this we are unable to do so as to cover all cases. Each case must be judged by itself.
If the question is asked which of two weapons caused certain contusions or contused wounds, we are still less likely to be able to answer it. In such a case we must make an accurate examination of the form of the wound and compare it closely with that of the weapon. In such cases also the second source of information on which we base our opinion as to the relation of a weapon to the wound may be of use, namely, the examination of the weapon. The presence of blood, hair, cotton or woollen fibres on one of two weapons indicates that this was the weapon used. The presence of blood is particularly to[525] be looked for, and in those parts of the weapon from which it could be washed off least easily. We should further note the condition of the point and edge of the weapon, and if the edge is broken or nicked at all, whether this condition is old or recent. The sharpness of the edge should further be noted, and if the edge is sharp note whether it has recently been sharpened. All these points have a certain bearing on the case. Also the location, shape, depth, etc., of the wound should be carefully noted to see if an accidental fall would be likely to account for it. For these features of the wound may be such that no fall could cause it.
We see, therefore, that in incised and punctured wounds the use of a weapon may not be hard to make out, but that in general the question whether a particular instrument caused the wound is often difficult or impossible to answer. Often the best we can do is to say that the wound could have been produced by the weapon.
V. Was a Wound Self-Inflicted or was it Inflicted by Another?
In other words, was it suicidal or homicidal? Speaking of suicide in general, its most common cause is alcoholism. It is not infrequent in youth. Lutaud[639] states that in fifteen years, presumably in France, there were 1,065 cases of suicide between the ages of ten and fifteen years. This seems to be only explicable on the ground of heredity or of cerebral affections. Among 27,737 cases of suicide, observed in France, the same author gives the following commonest causes in the order of greatest frequence: Drowning, strangulation, pistol-wounds, incised and punctured wounds, poison. The age, sex, and social conditions influence the choice of means. Thus among males drowning is preferred by the young, pistol-wounds by the adult, and hanging by the aged, while among females asphyxia is the favorite method, as there is no pain and no disfigurement.
While many pathologists consider suicide an act of mental alienation, and though such may be the case in a large number or even in a majority of cases, yet in a considerable number it is[526] a voluntary and rationally planned act. The question, Is it suicide or homicide? may be put in all cases of death by cutting instruments, and in many from other kinds of wounds. It is often, if not generally, impossible to answer it with absolute certainty. It is hardly suitable for the medical witness to try to reconstruct the scene of the crime from the medical facts, for he should abstain from everything not medical and should distinguish that which is positively proven from that which is merely probable.
Suicides often leave a letter or some such indication to show that the wound was self-inflicted. If such is not the case, the question as to the cause of the wound may or may not be medical. If the question is a medical one, there are certain points to notice as to the wound, such as its nature, situation, direction, and the number and extent of the wounds, from which we are to form an opinion. There are also other circumstances which furnish evidence and thus assist us in answering the question. This evidence is furnished by the weapon, the signs of struggle, the examination of the clothes and body of the deceased and the accused, the position and attitude of the body, and any organic lesions, etc., predisposing to suicide.
The nature of the wound bears upon the question of the homicidal or suicidal origin in the following way: Most suicidal wounds are incised or punctured wounds. Incised wounds of the throat are generally presumptive of suicide, but a homicidal wound may be inflicted here to conceal the source of infliction of the wound. Such a wound if homicidal would imply malice, on account of the attempt at deception and concealment, and would convict the assailant of murder. Unless the deceased was asleep or drunk or was otherwise incapable of resistance, such a homicidal wound can often be distinguished from a similar suicidal wound by the form and direction of the wound, by its irregularity, and by other wounds on the hands or person of the deceased. Taylor[640] mentions a case in which the peculiar form of the wound, like that made by butchers in killing sheep, led to the suspicion that homicide had been committed by a butcher, who was subsequently arrested, tried, and convicted of murder. The regularity of the wound has been[527] taken to indicate suicide rather than homicide. That it does so is not questioned, but it is more or less fallacious if resistance is impossible, in which case a murderer may easily make a regular, clean, incised wound here. Contused wounds are seldom suicidal, for they are not sufficiently speedily or certainly fatal. They are also more painful and disfiguring. Contused wounds usually indicate murder or accident, though there are not wanting cases of suicide by such weapons as a hatchet or a hammer. There is more difficulty in the case of a contused wound from a fall instead of from a weapon; for here we have to decide whether the fall was accidental, suicidal, or homicidal. The nature of the wound is of little assistance in the case of insane or delirious patients, who may commit suicide in the most unusual and curious manner.
Taylor[641] relates the case of a delirious patient in Guy’s Hospital, in 1850, who tore away the whole of the abdominal muscles from the lower part of the anterior abdominal wall. If the case had not occurred in the hospital or where there were witnesses of the deed, the nature of the wound would have indicated homicide except for the delirium. The following case, quoted by the same author, illustrates a wound of very unusual nature and situation, which might have been taken for a homicidal wound with intent to conceal as far as the situation of the wound was concerned. The wound was accidental and occurred in the following way. A girl fifteen years old jumped on to her uncle’s knee while he was holding a stick between his legs which she did not notice. The Stick passed up her anus, but she withdrew it and went on playing, though she complained of pain. On the following night acute symptoms of peritonitis set in, and she died of it in forty-eight hours. On post-mortem examination a rent was found in the anterior part of the rectum penetrating the peritoneal cavity.
The Situation or Position of the Wound.—A suicidal wound must be in such a position that the deceased could have inflicted it himself. Such wounds are, therefore, generally anteriorly or laterally situated. The “site of election” for suicidal wounds is the neck for incised wounds and the chest, especially in the region of the heart, for punctured wounds. The situation of suicidal wounds, of lunatics, etc., shows all[528] kinds of fantasies. The mere situation does not suffice to distinguish suicidal wounds, as a murderer may simulate a suicidal wound for purposes of concealment. Some regard a wound in the back as proof against suicidal origin, but it is not so much the situation of a wound as the situation taken in connection with the direction which furnishes the proof against suicide in such wounds.
As a rule, a suicidal wound, besides being in an accessible part of the body, is also in a part commonly known to be rapidly mortal, as the neck and heart. But suicidal wounds are not always in the situation which is anatomically best for being rapidly fatal. Concealed wounds or wounds in inaccessible parts presumptive of murder may be suicidal and so placed to impute them to another and give rise to the suspicion of murder. The blood-vessels of the arms and legs may be selected as the site of a suicidal wound. This situation is often regarded as uncommon, though the writer has met with it in one or more cases of attempted suicide. It is illustrated in the famous case of Abdul Aziz, the Sultan of Turkey. He was found dead under suspicious circumstances with two oblique, ragged wounds at the bend of each elbow, directed from above downward and from within outward. The joint on the left side was penetrated, while only the skin and veins were involved on the right side. Death was due to bleeding from the ulnar artery and the veins. The clothing was soaked with blood and scissors stained with blood were found on the sofa. These wounds were consistent with suicide, though not what would be expected. Nineteen physicians who examined the body agreed in reporting it as suicidal, though one reason given for this opinion, namely, “that the direction and nature of the wounds, as well as the instrument which might have effected them, lead to the conclusion of suicide,” was hardly a valid one, for the wounds were not typical of suicide in nature, direction, or position. Such wounds are rarely homicidal, though at least one such case is mentioned.
Suicidal incised wounds, as has been said, are usually in the neck, where they may sometimes be arrested by the larynx, especially if it be ossified, though the incision often divides the larynx. The situation of the wounds is often between the larynx and the hyoid bone, and then meeting no bony resistance,[529] they may divide the great vessels and even nick the vertebræ. But it is rare to be so deep, at least on both sides at once. As a rule, it is deepest on the side on which it is begun and ends more superficially. As far as the situation of a wound is concerned, there is no wound which a suicide can inflict but what may also be inflicted by a murderer. The reverse, however, is not true. We cannot always certainly distinguish between suicidal and homicidal wounds from their situation.
The direction of the wound is one of the most important points to notice. It is considered by some to furnish presumptive evidence for the medical jurist, and taken in connection with the nature and situation of the wound may often lead us to a positive opinion as to the question of the suicidal or homicidal nature of a wound. The evidence from the direction of wounds is only furnished by incised and punctured wounds, rarely by contused wounds. Suicidal incised wounds of the throat are almost always directed from above downward and from left to right if the suicide be right-handed, and in the same direction from right to left if the person be left-handed. Transverse wounds in this situation without obliquity are also compatible with suicide, though perhaps more common in homicide, while obliquely transverse wounds from above downward and from right to left in a right-handed individual are indicative of their infliction by another. Homicidal incised wounds of the neck inflicted from behind or the right side, if the victim and assailant are right-handed, or from the left side if they are left-handed, may have the same direction as similar suicidal wounds. Such a wound may be inflicted by a murderer to deceive as to the cause of the wound by raising the suspicion of suicide. If an incised wound of the throat be inflicted by another from in front, then its direction is usually the reverse of a similar self-inflicted wound.
Homicidal incisions, especially in the throat, may extend at one or the other end beyond the skin wound. In similar suicidal wounds at both angles of the wound the skin is the first and the last part injured, and in such wounds the spine is seldom reached. It should be borne in mind in this connection that a given suicide may be ambidextrous and this fact may be unknown to the friends of the deceased. This is especially[530] the case in the use of the razor from practice in shaving, and the razor is the usual weapon used in such incised wounds of the throat. Neglect of this point may lead to an unwarranted suspicion of murder. The two following cases cited by Taylor[642] well illustrate this fact:
In the case of Sellis,[643] the man was generally supposed to be right-handed, though he was found dead in bed with his throat cut and the razor on the left side of the bed. In point of fact, he was ambidextrous in the use of the razor. The second case, which occurred in London in 1865, was still more remarkable.
A publican was found dead in bed with his throat cut in a left-handed manner. He was supposed to be right-handed and there was bloody water in a basin in the room. His wife, who gave the alarm, had marks of bruises on her, and though she said she had found her husband dead in bed after having left it for a short time, suspicion fell upon her, especially as they were in the habit of quarrelling. The suspicions were removed, however, by the explanation that he had been brought up as a wood-carver, which required him to use both hands equally, and that he had frequently threatened to kill himself, and further that the bloody water in the basin was due to a daughter washing her hands after having touched her father. It is even conceivable that an ambidextrous person, to avoid suspicion of suicide or to impute murder to another, might inflict a suicidal wound from right to left. Notwithstanding all this, the above cases are very rare exceptions, and the rules stated above as to incised wounds in the throat hold in almost every case.
In the case of stab-wounds of the chest, especially in the cardiac region, the same rule as to the direction holds good, and in these wounds we can often define the direction more accurately than in the case of incised wounds. If the suicide is right-handed the wound is regularly on the front or side of the body and directed obliquely from above downward and from right to left, while it is from left to right in case of a left-handed suicide. A murderer from behind, or from that side the hand of which the victim would use, may inflict a wound in the same situation and direction as a suicidal one. Here again this may be done with the motive of concealment of the nature[531] of the crime. Homicidal stab-wounds inflicted from in front, as they generally are, are usually directed from left to right, and they may be directed from above downward or in the opposite direction. Oblique wounds from above downward may be either suicidal or homicidal; those directed from below upward are almost always homicidal.
When a wound is caused by an instrument both cutting and puncturing, suicide cannot be admitted unless the direction of the wound is compatible with that which the weapon which inflicted the wound, held in the hand of the deceased, might cause. Taylor recommends to place the weapon in the hand of the deceased to see if the direction of the wound could possibly correspond with that which could be taken by the weapon in the hand of the deceased with any position possible for the arm and hand. Therefore certain wounds by position and direction exclude suicide, but if a wound is possibly suicidal it is also possibly homicidal.
Though suicidal wounds vary, the above points are sometimes of real assistance in distinguishing between suicide and homicide, especially if the body has not been moved.
Evidence Furnished by the Number and Extent of Wounds.—Multiplicity of wounds, as a rule, indicates homicide, and indeed the reverse is true in a majority of cases that a single wound points to suicide. There are many exceptions, however, to both statements. Multiple wounds are possible in suicide, and that, too, with different weapons; even drowning or hanging may be resorted to after self-inflicted wounds have failed. If several wounds are found, each one of which or more than one of which may be considered grave, it is usual to conclude that the wounds were not self-inflicted, but the medical expert should not judge too hastily from this fact alone, for most wounds do not kill instantly. With the presence of several wounds in a case of suicide only one of these, as a rule, is “mortal” in character. This being so, some have asserted that if two mortal wounds are present, especially if one of them is stupefying, such as a wound about the head, such wounds are incompatible with suicide. A definite statement of this kind cannot go unchallenged unless the two wounds are in different parts of the body, and both of such a nature as to be immediately or very rapidly fatal. For all cases of suicide or homicide[532] do not die immediately from wounds commonly called mortal; in fact, this may be said to be the exception rather than the rule. We may safely say, however, that if there are several distinct wounds on the throat, each involving the large vessels, the inference is plainly murder.
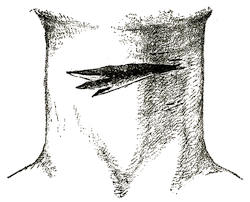
Fig. 10.—Suicidal Cut Throat from Left to Right, showing the Tentative Cuts at the Commencement and the Serrations at the Termination of the Wound.
Several wounds by the same or different weapons cannot, therefore, be proof of homicide. The case of a lunatic suicide is reported who inflicted thirty wounds upon his head. In a case of homicide with multiple wounds the situation or direction of some one or more of them may give evidence as to the origin of the wounds. Ogston, Sr.,[644] states that especially in the case of incised wounds of the throat a suicide may make a number of small or superficial tentative cuts besides the principal one, but these incisions are all usually parallel (see Fig. 10). In the case or multiple homicidal incised wounds of the throat, on the other hand, the wounds are not parallel, owing probably to the resistance of the victim in this case and his remaining passive in the former. The extent of the wound refers to the number and importance of the parts injured. In regard to incised wounds of the neck, this point has been thought by some to furnish presumptive evidence of suicide or homicide—of homicide if the wounds are deep, of suicide if they are not. While it is true that suicidal wounds of the neck are, as a rule, not very deep, and that they seldom reach the vertebræ and generally do not divide the vessels on more than one side, yet sometimes such wounds are as deep and extensive as homicidal ones. This may imply a determined purpose not to be foiled in the attempt at suicide. Thus Marc reports a case of suicide by an incised[533] wound of the neck, where the wound was so deep as to reach the vertebræ or their anterior ligaments and to divide the trachea and œsophagus, both carotids and jugular veins. The extent of this wound was greater than in most suicides, but still we can hardly lay down a hard-and-fast rule of much practical value according to which extensive wounds are evidence of murder. Such wounds are, however, presumptive of murder taken in connection with other signs pointing that way.
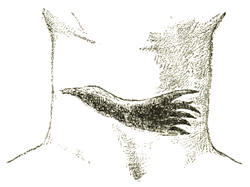
Fig. 11.—Homicidal Cut Throat from Right to Left, showing a Tentative Cut at the Commencement and the Serrations at the Termination of the Wound.
The question may arise in regard to a wound, whether the victim wounded himself by precipitating himself on the weapon. This may be alleged by the defence, but it is difficult to believe if the wound is deep, for the body would naturally repulse the weapon. If the wound is deep the weapon must at least have been strongly held, which may or may not be consistent with the theory of self-defence. If the direction of the wound is oblique from above downward, or if there is one external wound and two separate tracts internally, from a second use of the weapon on the part of the person holding it, then the above allegation is doubtful, if not impossible.
By comparing the relative positions of the deceased and accused, as indicated by the witnesses and accused, with the position and direction of the wound, we may often judge whether the allegation is possible or probable.
Besides the above points derived from the wound itself, there are several other factors which belong to the category of circumstantial evidence, but which come within the province of the medical expert. These latter points of evidence are sometimes almost as important as the former, while taken in connection with them they help to make the evidence far more conclusive.
Evidence furnished by the weapon as to the origin of wounds.
We have already seen in a former section that we can often tell, by various signs of the wound, with what kind of a weapon it was made. We may thus be able to say that a wound was made by a weapon similar to one exhibited. Also by examination of the weapon itself and from the circumstantial evidence of where and how it was found, we may sometimes say that the wound was inflicted almost certainly with a particular weapon. All this evidence may sometimes be made use of in judging between the suicidal and homicidal origin of a wound.
The POSITION of the weapon or the place where it is found is a matter of considerable importance. If it has not been touched, its position should be carefully examined, or inquired about if it has been moved. The presence of a weapon which might have caused the wounds in the hand of the victim is in general proof of suicide. The weapon must not merely lie in the hand, it must be gripped by the hand. One might suppose that the weapon placed and held in the hand until rigor mortis sets in would still be firmly held. Casper says that this is not so, but that the weapon falls from the grasp as soon as the hand is unbound. Also Hofmann’s[645] experiments proved the same point. By the use of ligatures and several artificial means he tried to confine a weapon in the hand of a recently dead body so that it would be as firmly held as by a contraction of the muscles during life. These experiments were entirely unsuccessful, for though the fingers remained closed, the object was simply held and not grasped, and fell from the hand on the release of pressure.
In suicide the weapon is sometimes held so firmly that force is required to dislodge it. It seems as if the muscular spasm or grip persists after death, as cadaveric spasm, until rigor mortis occurs and sets it, as it were. The murderer, therefore, cannot imitate this grip, and an unsuccessful attempt to do so would indicate murder. It should be borne in mind that the weapon in the hand of the deceased may have been for the purposes of defence; therefore it is necessary to note whether the wounds on the body correspond to those which could be made by the weapon. Indeed, this fact is most important to note in all cases of suspected suicide where the weapon is found. If the weapon is not in the hand of the deceased, note carefully[535] where it lies. If death is due to a suicidal or accidental wound which is immediately or very rapidly fatal, the weapon is generally found near the body. If so, it is well to note on which side it lies, and if it lies near, whether it has apparently fallen or been thrown or placed there. If the relation of the body and the weapon has been disturbed by moving either, the position of the weapon as found by the medical witness is of little value. In cases of suicide the weapon may possibly be found at some distance or even concealed, though this is exceptional. Thus Taylor[646] states that the razor in one instance was found shut at the side of the deceased, who had committed suicide by cutting his throat. In another instance the razor was found in the pocket of the deceased, bloody and closed. As a rule, the weapon is found lying at the side of a suicide if it is not grasped in the hand. If the weapon is far from the body and the wound was quickly fatal, especially if the weapon is hid or cannot be found, it is strongly presumptive of murder. If the weapon is found near the body it is well to note whether the edge is sharp or blunt, straight or bent, or notched, as these points may assist us in forming a judgment as to suicide or murder.
A weapon belonging to the victim may be substituted by the murderer for the one really used, and the former may be placed by the side of the body. Therefore the weapon found should correspond to the wounds as to length, depth, sharpness, etc., to be compatible with suicide.
Generally a suicide foiled in the attempt to take his life uses the same weapon over again if he persists in the attempt. But he may not do so; on the contrary, if the first attempt was made with a knife, the second may be made with a pistol, etc. Several wounds by the same or different weapons cannot therefore be an absolute proof of homicide.
The presence of blood, hair, and other substances on the weapon used, or probably used, is a matter of some importance. Blood is not necessarily found on the weapon used to inflict a mortal wound, especially in the case of blunt instruments. In stab-wounds, too, the vessels may be compressed by the blow or the weapon may be wiped as it were on withdrawal by the elasticity of the skin and by the clothing, except for a thin yellowish film. Thus it is that the first stab-wound shows[536] no blood on the outside of the clothes but only on the inside, but the outside of the second is usually bloody but may be but little so. To make sure whether or not there is blood on a knife or other weapon it is necessary to examine all the depressions on the instrument, as the blade itself may have been washed, and only those traces of blood remain which are less accessible to cleaning by washing. Blood coagulated on a blade indicates, as a rule, blood from a living animal, but it may not do so. Furthermore, it may be hard to distinguish between a thin layer or spots of dried blood not coagulated or coagulated and dried blood in a similar form.
If blood is not found on a weapon, hair and other substances which can be identified may be. This is especially the case with blunt weapons, on which, as we have seen, blood usually fails. A fragment of the weapon may break off in the wound, as in stab-wounds, and may be identified as belonging to one in the murderer’s possession.
The signs of a struggle furnish important evidence, as they are not likely to be found in the case of suicide. If the wounds were inflicted by a cutting instrument, the existence of a struggle may be indicated by incisions on the palm of the hand or fingers or on the dorsum (see Fig 12). Such wounds would not be self-inflicted and would indicate a struggle with the murderer. Or if contusions or ecchymoses indicating the form of the foot, fist, fingers, or finger-nails are found on the face, neck, chest, forearm, or hand of the deceased, this again indicates a struggle with the assailant, and goes far to prove murder. The same is true of the imprint of a bloody or dirty hand on the clothes of the victim when the victim’s hands were not bloody. Also such an imprint in a position where the deceased could not have reached with the particular hand indicated, as is the case if the impression of a right hand be found on the victim’s right arm; this indicates a struggle with a murderer, etc. In one case of murder, on the back of the left hand of the deceased there was found the bloody mark of a left hand evidently not that of the victim himself. The presence of marks of violence about the mouth of the deceased, done to close it to prevent the victim from giving an alarm, especially if surprised during sleep, is presumptive of murder. Sometimes hair or fragments of clothing belonging to the accused are found in the grasp of the deceased,[537] indicating a desperate struggle, and they are very suspicious of murder. Thus Taylor[647] cites the case of a murder trial in Ireland, in 1877, where hairs found firmly grasped in the hands of the deceased were found to correspond to the hair of the accused. The clothes of the deceased, as well as those of the accused, often indicate a struggle unless the accused can satisfactorily account for the condition of his own clothes in some other way.

Fig. 12.—Incised Wounds of Right Hand in the Struggle of Defence. Homicide.
The examination of the clothes and body of the deceased and the accused may furnish important evidence.
If suicide is accomplished by a weapon like a knife, it is rare for the hand not to be bloody. If it is not bloody we may well suspect a case of supposed suicide. The presence of blood on the hand does not prove suicide, though its absence may[538] disprove it, as the hand is generally bloody in case of murder by being carried to the wound.
The examination of the clothing of the deceased is of great importance. As we have noticed before, a suicide generally opens them, a murderer rarely. A suicide is often partly or even wholly undressed when he inflicts the wound, while murder is usually committed on those entirely dressed. The wound of the clothes should correspond to that of the body in case of murder. In suicide the wounds of the body and of the clothes may not correspond, especially if there exists a motive to falsely impute the crime. The clothes of the deceased as well as those of the accused may indicate a struggle, as we have already noticed. Of course, in regard to the clothes examined, it is necessary to clearly prove that they were worn at the time by the deceased or accused, otherwise serious mistakes may be and sometimes are made. In examining the blood-spots on the clothing, note whether the blood occurs in large patches or sprinkled as by a spurting vessel or by continued violence.
The body of the accused may present scratches, marks of nails, contusions, bites, or other wounds indicative of a struggle. It would be well to ask the accused how he received the wounds or scars, to see if his explanations tally with the injuries. It is hard to tell when wounds which have cicatrized were inflicted; we can only distinguish between old and recent ones, and thus control the statements of the accused. An examination of the finger-nails of the prisoner soon after the crime may reveal blood underneath when the rest of the hands and person are free from it. Note also the site and shape of the blood-spots, if they exist, and whether or not they came from an arterial jet. These spots may be on the body or clothes of the accused. The account of the accused as to these spots may or may not correspond to the facts as indicated by them. The above leads us to the more or less important question:
Could the Assailant have Escaped without Stains?
It is possible for the murderer to escape without being spotted with blood, but the probability of this occurrence depends on the nature of the wound and the relative positions of the deceased and the assailant at the time the wounds were inflicted. This latter fact is very largely, if not altogether, a matter of[539] speculation as far as the medical evidence goes. It is a popular, though false, idea that a murderer’s clothes must be bloody, and the police may be misled in expecting to find them so in every instance. Taylor[1] cites several cases in which either no blood was found on the murderer’s clothes, or only small spots wholly out of proportion to the amount of blood which must have spurted or flowed from the wound. Absence of blood on the prisoner’s clothes is often made use of by the defence to prove the prisoner’s innocence, whereas, besides the possibilities of having had no spots in the first place, the clothes may have been changed or washed before the examination was made. This has occurred in more than one murder trial. Taylor[648] mentions the following cases in illustration:
It was alleged that the absence of blood-stains on the prisoner’s clothing was a strong proof of his innocence in the trial of Sub-Inspector Montgomery for the murder of Mr. Glasse (Omagh Ass., July, 1873). In this case the weapon was a bill-hook which had produced contused wounds on the head. There was blood on the floor about the body, but the wounds were not likely to have been accompanied by much spurting. Yet it was assumed that the assailant in this case must have been covered with blood. Much stress was laid upon the absence of blood-stains. On the first two trials the jury could not agree, owing chiefly to the absence of blood-stains, but on the third trial he was convicted and afterward admitted that he had removed the blood-stains from the clothes with cold water. Also in the case of Reg. v. Courvoisier (C.C.C., 1840) the accused, who was tried for the murder of Lord William Russel, had no blood-stains on his clothes. All the vessels of the throat of the deceased had been cut to the vertebræ while he was asleep. It was contended most strongly that the accused could not possibly have committed the crime, as he had no blood-stains. But after conviction he confessed that he wore no clothes when he committed the murder, and he only had to wash his hands and the carving-knife he used. Again, in the case of Reg. v. Thompson (Durham Wint. Ass., 1863) the defence mainly relied on the absence of blood on the prisoner’s clothing. The wound in the throat of the wife of the accused was five inches long, directed from left to right, dividing all[540] the vessels and nerves of the neck. The medical witness stated justly that no such wound could be self-inflicted. It was rapidly fatal. No weapon was found near the body. The prisoner was convicted.
The same author cites the case of a prisoner on whose trousers worn soon after the murder no blood-marks were found, but the trousers actually worn by him were found with blood upon them. Juries have even acquitted the prisoner apparently only because no marks of blood were found, though the other circumstances were explicable only on the theory of murder.
It should be remembered in this connection that blood-stains may be found on the clothing of many, especially on the coarse clothing of working-people. This may be accounted for by the occupation, flea-bites, accidental circumstances, or it may occur without definite explanation. Such persons may be accused of murder and yet the blood-stains be consistent with innocence. Too much importance should not, therefore, be attached to them, even if the accused cannot satisfactorily explain them and if he does not attempt to do so in a suspicious way. That blood on the clothing even under suspicious circumstances may be consistent with innocence is illustrated by the case of a suicide by cutting the throat, in 1872, cited by Taylor.[649] In this case the son first found his father dead, and thought that he had broken a blood-vessel. He raised the body, staining his hands and clothes, then went for help. At the inquest he was closely questioned as to the presence of the blood-stains, but there could be no doubt that the case was one of suicide.
In general, we may say that a murderer is much more likely to escape without blood-stains in contused wounds, and more likely in the case of punctured wounds than in incised wounds, for in punctured wounds the bleeding is much less free and is less likely to spurt from the wound. In the case of incised wounds he is most apt to escape without stains if he is behind or to the side of the victim when he inflicts the wound—in other words, when a part of the body of the deceased was between the assailant and the wound inflicted. Furthermore, the assailant is more likely to escape without blood-stains if there is a single wound than if there are several, and each additional wound makes it more likely that he will be spotted with blood.
The examination of the ground or floor and the furniture, etc., may furnish some evidence as to the nature of the crime, and also help the witness to answer the questions which may sometimes be asked, i.e., At what spot was the victim wounded? and Where did he die? This question is sometimes settled by examination of the spot where the deceased lay and the furniture, etc., about. Sometimes the floor or ground and the furniture or surrounding objects at a distance give the requisite evidence. The examination of the cracks and corners of the floor and furniture should not be neglected, and Taylor instances a case where the hair of a dog helped to clear up the case. If the body has not been disturbed the most blood is usually found where the deceased died. If the victim succumbs at the spot where he was wounded, blood is found only in the immediate neighborhood, except for arterial jets, which may be as far distant as two metres. The separate blood-spots of an arterial jet are circular if the jet strikes the object perpendicularly, oval or wedge-shaped with the larger end away from the body if it strikes the object obliquely.
If the blood-stains are more diffused and are found in other places, careful notice should be taken as to whether the different places communicate with one another by traces of blood. If they do not communicate, it goes to show that the body was moved after active bleeding had ceased, that is, after death, but this indication is not absolutely positive. If traces of blood do connect the larger blood-spots, it is of interest and importance to know where the deceased was wounded and where he died, also whether he moved or if he was moved before or after death. This question is not always capable of solution. Some injuries exclude the possibility of active motion. Stupefying contused injuries of the head or an incised wound opening a great artery are both inflicted where there is the greatest hemorrhage, and the spot where the deceased was wounded and died should be identical. In such cases a second large spot of blood, connecting or not with the first wound, indicates that the body has been moved. But if the wound does not bleed much or rapidly, the wounded person may fall at a distance from the spot where he was injured, and death occurs, as a rule, where there is the greatest amount of blood; for a certain amount of bleeding occurs for a short time after the victim falls or even[542] after death. One can find in many places the signs of arterial jets marking the movement of the deceased from one blood-spot to another. This is quite different from the tracks caused by dragging a bleeding body. All this it is important to notice, for the dragging or passive moving of the body strongly indicates murder. Blood at a distance may indicate the occurrence of a struggle, or that the body was moved, or it may show the tracks of a murderer. As to the latter point, the imprints of the hands and feet, whether bloody or not, may indicate murder and establish the identity of the murderer. We have already seen how they may occur on the deceased and indicate a struggle, and thus be presumptive of murder. When the marks are made by the naked foot, it is well to examine it by lining it off in squares, and so to compare it with the imprint of the foot of the accused. Simple inspection can sometimes give the required evidence. We may even get an impression of such imprints in the snow. Imprints of the boots or shoes worn by the accused compared with those imprints found at and near the scene of the crime may sometimes help to clear up the case, but this may perhaps be considered outside of the sphere of the medical witness. Such and other signs of a struggle about one of the blood-spots would indicate that the wound was received there, though death may have occurred at another spot. In such a case it would be well to examine to see if there was much blood where the body was found, for if there was not it would indicate that the body had been moved there after death, and thus be strongly presumptive of murder.
As furnishing some evidence which may help to distinguish between suicide and homicide in the origin of wounds, the question may be asked, What was the position of the victim when injured or dying? and also, What were the relative positions of the victim and assailant?
The position of the victim at the moment of the injury is sometimes indicated by the position of the wound, the direction of its tract, and the direction from the wound of the blood on the body and clothes. On the neck or extremities the course and form of the wound may indicate the position of these parts when the wound was inflicted, for sometimes in flexions of these parts the skin lies in folds, and a wound inflicted when these parts were so flexed would be irregular, wavy, or zig-zag.[543] Further, the position and movement of these parts necessary to restore directness to the wound may indicate the position of the parts when the wound was inflicted. The examination of the relative positions of the wound in the clothes and the body may help to indicate the position of the body when wounded. The position of the blood on the body and the direction of the blood from the wound, whether below or at the sides, etc., tends to show the position of the body when bleeding. Thus if the body was at any time in the erect position, some of the blood-stains will be vertically below the wound, or if the victim was lying on the back then the stain would be at the sides only and not below the wound, except such stains as indicate that they were produced by arterial jets. Few suicides cut the throat in the recumbent position; therefore it may be considered in the light of an indication of homicide if the blood-stains show that the victim was not erect after the wound was inflicted. It is well also to note the form, direction, and obliquity of the blood-spot. This would indicate, by comparison with the wound, the relative position of the wounded person and the blood-spot, and thus show whether the body had been moved or not, as, for instance, by the murderer for the purpose of robbery. The force of the bleeding is also indicated by the form of the spot, and this would indicate how rapidly death probably ensued. This fact might thus help us to judge whether the victim probably died where he was wounded, and whether other and remote blood-spots would not be presumptive of murder. If the victim is found in night-clothes, this fact would help to show that he was lying down when wounded. The medical evidence as to the position of the victim when injured is, therefore, circumstantial and not very positive; that in regard to the relative position of the victim and assailant is even less positive. We presuppose in this question that the case is one of murder. We are not to prove murder or refute suicide. We can rarely be positive as to the relative position of the assailed and the assailant. A wound in the back may be caused by some one in front with an arm behind. The direction of the wound would indicate this, for if the assailant is right-handed and inflicts a wound on the back from in front, a stab-wound would almost always be directed from left to right, an incised wound from right to left, both from above[544] downward. With a left-handed murderer the direction would most likely be from right to left and from above downward for a stab-wound, and from left to right and from above downward for an incised wound. If the assailant were at the back of the victim and wounded him in front, the direction of these wounds would be the opposite of the above, i.e., from right to left for a stab-wound and from left to right and from above downward for an incised wound with a right-handed assailant and vice versa with a left-handed assailant. These wounds occur more commonly than those of the back, and are especially noticeable in incised wounds of the throat. In the case of these incised wounds of the throat inflicted from behind, the direction from left to right and from above downward resembles that of self-inflicted wounds in the same situation. As a general rule, wounds are on the same side of the victim that the assailant was; the facts given above help to show us the exceptions. Thus a wound on one side is presumptive that the murderer was on that side, or possibly at the front or back and only exceptionally on the opposite side. The presence of wounds on one side only may help to confirm the testimony of a witness that the victim was against a wall or some other obstacle which protected the other side. The question of the relative position of the combatants in duels and the nature of the weapons used as shown by the wounds has sometimes come up, especially in other countries, to determine whether the combat was regular and fair.
In all cases of suspected suicide, but where a doubt exists between suicide and murder, or even accident, hereditary disposition and organic affections of the body, such as alcoholism, incurable or painful diseases, chronic inflammation of the brain and meninges or of the genito-urinary organs—all such and hereditary predisposition may support the idea of suicide.
Imputed or Self-Inflicted Wounds.
Closely allied with the question of the suicidal or homicidal origin of wounds is the question whether a wound imputed to another is self-inflicted or inflicted by another. These wounds are seldom fatal. In discussing the question whether a wound is self-inflicted or inflicted by another, we have referred occasionally[545] to suicidal wounds where the circumstances were such as apparently purposely to imply murder and impute the cause of death to some one else. This happens more often in cases of unsuccessful suicide. Here we have recourse to the same evidence that we have gone over in the present section which helps to distinguish between a suicidal and a homicidal wound. The case may be somewhat more difficult, as the unsuccessful suicide may manufacture evidence against the accused and hide to some extent the evidence of suicide. These cases can usually be decided, however, in connection with the circumstantial and other evidence. The majority of cases of imputed but self-inflicted wounds are very superficial, often not below the true skin. Being self-inflicted they have many of the characters of suicidal wounds. Thus they are usually situated in front and on the left or right according as the wounded person is right or left handed, and the direction is usually similar to that in suicidal wounds. Such wounds are generally incised or punctured wounds, seldom contused wounds, and in this respect they resemble suicidal wounds. As exceptions to this rule, Bergeret[650] mentions some cases where females in attacks of hysteria have inflicted severe contusions on themselves, and have preferred charges of attempted murder against innocent persons. Like suicides also the hands are seldom injured, though they may be much so in resisting homicide.
In other respects, however, these wounds differ from suicidal wounds. Thus they are not usually situated over a “mortal” spot, and they are often numerous and scattered, sometimes parallel and sometimes not. The wounds in the dress do not correspond even as often as in suicide. In comparing cuts in clothing with those on the body, it is important to find what articles were worn at the time the assault was alleged to have taken place, and to make sure that the clothes examined were those worn or alleged to have been worn. It may not be necessary that the clothes examined should have been really worn, for if they were alleged to have been worn and were not, the examination of them will almost always show the deception or the self-inflicted nature of the wounds. Then take careful note of the position, direction, form, and size of the cut and the apparent sharpness of[546] the weapon in the several layers, and see if they correspond with one another and with the wounds on the body in those various particulars. In imputed wounds the clothes are generally cut when off the body and can seldom be done so as to deceive a careful examiner. Several wounds cannot exist in the same region of the body without some being bloody and showing the marks of it on the clothes. Even a single wound of the clothes generally shows blood on the inner surface if there is a corresponding wound of the body underneath. In simulated and imputed injuries the blood-stain may be on the outside of the clothing instead of on the inside, showing that it was artificial and not natural. An impostor may either do too much or too little, and the medical witness should be on guard against both alternatives. Taylor[651] mentions a case which occurred in London some time ago, in which there were two cuts in the shirt near together exactly alike in size, form, and direction, making it evident that the weapon had gone through a fold of the shirt. This proved that the shirt could not have been worn at the time it was cut, for if the shirt was folded while on the body the weapon must have gone through the fold and then through another layer of shirt, making three cuts instead of two, or five instead of four, before it could have reached the body. This and other facts made self-infliction of the slight wound on the chest probable. The same author cites another case showing the imperfect manner in which the cuts in the clothes are made in imputed wounds, the clothes being off the body at the time. The case occurred in Nottingham in 1872, the accused being charged with wounding the plaintiff on the highway by stabbing him in the arm, though there was no robbery or other motive for the act. The coat and shirt sleeve were found cut, but there was no corresponding cut in the lining of the coat sleeve. The charge was clearly false, and was trumped up by the youth who was the plaintiff because he wished to leave the place where he had been sent for private study.
In examining a case where the self-inflicted nature of imputed wounds is in question, the following are some of the many points to keep in mind in the examination and to be ascertained by the examination: (1) The relative position of the plaintiff and the assailant at the time of the alleged attack.[547] This can be compared with the position as stated by the plaintiff or other witnesses. (2) The situation, direction, depth, nature, and number of the wounds. (3) The situation and direction of blood-marks or wounds on the dress or person of either or both. (4) The marks of blood and the quantity of it at the spot of the alleged struggle. (5) The signs of a struggle and the various other points of circumstantial evidence gone over in considering suicidal and homicidal wounds.
Though a severe blow may cause a slight mark, it does not follow that a slight mark implies a severe injury, else the exception is made the rule. The inconsistency of the story of the plaintiff is generally so palpable that imposture is evident, but prejudice and unjust suspicion are often excited against those accused. Thus Taylor[652] states that “a strong suspicion was raised against the then Duke of Cumberland, in 1810, in reference to the death of Sellis, when a skilful examination of the wounds on the deceased would have shown that they might have been self-inflicted.” The same author also cites the case of M. Armand, a merchant of Montpelier, who at Aix in March, 1864, was tried for an alleged murderous assault on, or imputed murderous strangulation of, his servant. The excoriation on the back of the neck was so slight as to escape the observation of some medical men, and it was evidently self-inflicted, either accidentally or purposely, as the facts showed. The assertions of a number of medical men were taken by the court to support the servant’s story to the effect that his master had struck him a severe blow on the back of his neck, rendering him insensible for many hours from concussion of the brain. The evidence given chiefly by Tardieu for the defence showed the story of the complainant to be a fabrication, and the accused was justly acquitted.
Was a Wound Accidental?
In answering this question we must distinguish accidental wounds from those self-inflicted and those inflicted by another. These three classes comprise all wounds. In case of a trial for murder it may be alleged by the defence that the wound was caused by accident or that it was due to suicide from a fall,[548] falls being a common class of accidental wounds. So we have to judge between accident on the one hand and homicide and suicide on the other hand. The question arises especially in cases where the injury causing death is one commonly due to accident.
As to the QUESTION BETWEEN ACCIDENTAL AND SUICIDAL WOUNDS, they are often easily distinguished, especially if the body has not been disturbed. In suicide there is clear evidence of design, and the circumstantial evidence helps to make the case clear. It may not always be possible to decide, however, as an accidental wound may sometimes resemble a suicidal or homicidal one. Accident is often shown by the nature of the wound. Thus it is rare for an accidental mortal wound to be caused by a knife or similar weapon held in the hand and forced into the body by a fall, the blow of an opening door, etc. But such exceptional cases have been reported. Incised and punctured wounds are, therefore, very rarely accidental, and most accidental wounds are contused wounds or contusions.
Again, accident is often shown by the situation of the wound, which should be on an exposed part of the body unless the accident is due to a fall from a height, when the wound may be almost anywhere. But such injuries are easily shown to be due to falls. The fall, of course, may be accidental, suicidal, or homicidal. Some wounds in exposed parts forbid accident on account of their nature, i.e., deep incised wounds of the throat. If the deceased has a life insurance, suicide is less probable, as the insurance is not paid in case of suicide. In fine, accidental wounds are distinguished from suicidal by—(1) Their nature; accidental wounds are almost always contused, suicidal very rarely so, only in cases of lunatics and delirious persons and where suicide is accomplished by a fall. (2) The situation of the wound or wounds indicates their origin. We have already studied the situation of suicidal wounds and have also seen that accidental wounds are only on exposed parts, except when the injury clearly indicates a fall from a height. The evidence from the direction of wounds rarely applies, as this is valuable only in incised and punctured wounds, which are seldom accidental. Both kinds of wounds are usually few in number except in case of a fall from a height or a crush, though sometimes suicidal wounds are multiple.
The evidence from weapons, if there be any, points strongly to suicide. The signs of a struggle are hardly consistent with either suicide or accident. The only case in which they might occur would be where a struggle occurred to prevent a suicide from throwing himself off a height or before a vehicle or railway train. In such a case accident would be excluded by the signs of a struggle, and the question would lie between homicide and suicide. The examination of the clothes of the deceased would furnish no evidence unless some letter or paper were found stating the purpose of committing suicide. Little or no evidence would be furnished by the position of the body when found in cases which might otherwise be doubtful. Organic lesions or other facts predisposing to suicide would furnish presumptive evidence against the wounds being accidental. Of all these various points the first, as to the nature of the wounds, is by itself the most valuable and conclusive. But this gives us no assistance in clearing up a case where it is doubtful whether a fall from a height or a crush by a vehicle or railway train was accidental or suicidal. Some of the other points mentioned may aid us in such a case, and also the fact that such injuries are far more often accidental than suicidal. But in these cases, also, certain circumstances may show that the fall was not the result of accident.
Accidental wounds are generally caused by a fall or a crush, and the fact of their accidental character is generally established by the circumstances of the event. Certain accidental wounds present characteristics which allow the true nature of the wounds to be determined. But in some cases a suspicion may arise and the question may be asked as to WHETHER THE WOUND WAS ACCIDENTAL OR HOMICIDAL. For instance, if a person receives fatal homicidal injuries, and just before or after death the body is thrown from a height or is run over and crushed, it may be hard to determine the murderous element among the many wounds. This is the case if the homicidal wounds were contusions or were caused by blunt instruments, but rarely, if ever so, if they are incised or punctured wounds or both. But even in the former instance, a close examination of the lesions and of the locality of the injury can often clear up the case. Thus in a case mentioned by Vibert,[653] as cited by[550] Hofmann after Taylor, a woman was found dead at the foot of some stairs in a cave. She had died of a fracture of the skull and of the spine, produced by the fall. But about four or five feet above the level of the top step there was found on the wall the fresh marks of an arterial jet of blood. Examination showed a wound in the right temporal region which had opened the temporal artery, and it was therefore thought that the woman was wounded at the top of the stairway and then thrown down, which was afterward proved to be true. In another case, reported by M. Tourdes, a man knocked down and killed by an axe, which crushed his skull and caused the brain to exude, was placed in a road frequented at night by heavy wagons. The head was placed in the rut, but the coagulated blood and brain formed a puddle which did not appear on the wheels or their track, and no bloody furrow was caused by their passage. The same author mentions the case of a woman plainly strangulated by the hands and then thrown into the ditch of the fortifications of Paris.
It is especially with regard to fractures of the skull that the question often comes up as to the accidental or homicidal nature of the injury, as to whether it is due to a fall or a wound. Sometimes a depressed fracture may show the form of the instrument. An extensive comminuted fracture of the skull may indicate greater violence than would be received from a fall from the little height which the circumstances may allow. As to the slighter degrees of fracture, the disposition of the fracture itself often shows less than the form and site of the ecchymosis, the lesion of the scalp, and the place and position of the body when found. In such cases the traces of a struggle, the existence of other wounds, etc., may be of great importance. In distinguishing between homicide and accident, as in distinguishing between the latter and suicide, the most obscure and difficult cases are those where the injury has been caused by a fall from a height or by a crush.
This is illustrated by the case of Madame de Tourville, which is quoted by Taylor.[654] She was killed in July, 1876, by a fall from a precipice. Her husband, a lawyer, was accused of murder committed by pushing her over a precipice in the Stelvio Pass. The place where her dead body was found was at a considerable[551] depth below, and the injury was chiefly in the head, which had been crushed by the fall. The body showed no evidence of intentional violence. The prisoner’s guilt was established on the following points: (1) The false and inconsistent statements made as to the occurrence; (2) the marks of the body having been dragged some distance so that a part of the dress was found, in a bloody condition, some way from the body; (3) there were marks of blood on the prisoner’s hands and clothing. After a long trial he was convicted, though the sentence was afterward commuted to imprisonment for life. Of course, as we have already stated, if a person is responsible for a fall he is also responsible for the results of the fall. This applies to many of the contused injuries and deaths from falls in prize-fights and drunken brawls.
We may sum up the points of evidence which help us to distinguish between an accidental and a homicidal injury much as we did when the question lay between accident and suicide. (1) The evidence from the nature of the wound is not quite so conclusive as when the question lies between suicide and accident. For contusions and contused wounds are far more often homicidal than suicidal, and accidental wounds are almost always of this class. If, however, the wounds are incised or punctured, this fact points almost certainly to homicide. (2) As to situation, a homicidal wound may be situated almost anywhere; an accidental wound, except in falls from a height, only on an exposed place. (3) The direction of the wound can seldom help us in the case of contused wounds which, practically, are the only ones in question, though it may possibly be incompatible with accident. (4) As to the number of wounds, homicidal wounds are far more apt to be multiple either in a small area or scattered in such a way that an accident could hardly account for them all. (5) A weapon may give evidence more often here than when suicide is in question, for a weapon may be used to inflict contused wounds which may resemble those received in a fall. The evidence furnished by a weapon or blood, hair, etc., on the weapon, etc., is strongly in favor of murder. (6) The evidence from a struggle is also more important because it is more often found. A struggle may occur in homicide, and only in homicide, as a rule, so that signs of a struggle are strong evidence of murder and against the idea of accident.[552] (7) The examination of the clothes and body of the deceased may give valuable evidence, showing, as it may, signs of a struggle or other marks of an assailant and indicating murder. (8) Examination of the position and attitude of the body and of the spot where it lay and the ground around may furnish more or less proof of murder, as in the case quoted above. Thus the track of the murderer may be discovered or the body may have been interfered with and moved or robbed, all indicating homicide.
In any case, whether it is desired to distinguish accidental from suicidal or homicidal wounds, those cases present the most difficulty which result from falls from a height or crushes. But, as the case of Madame de Tourville shows, the above given and other circumstances may often show even then that the fall or the crush was not the result of accident.
Falls from a height may, therefore, be the result of suicide, homicide, or accident. The injuries are similar in all three cases. A fall of six to eight metres causes, as a rule, numerous lesions, and shows such a traumatism that the case usually excludes the possibility or, at least, the probability that the wounds resulted from blows. Sometimes, however, the gravity of the lesion is not proportional to the height of the fall. Thus Vibert[655] relates the case of a man, afterward employed for several years in the École de Médicine, who jumped from the top of the column of the Bastile, a height of fifty metres. He rebounded on to some canvas stretched at the foot of the monument, then fell to the ground, and was able to get up and walk away. Curiously enough, he killed himself later by jumping from the top of an omnibus in motion. In the case of falls from a height, it is especially true that with grave lesions internally the skin may be intact or only slightly ecchymosed or eroded, or the ecchymosis may be only deeply seated so as not to appear superficially. In the latter case, if life had continued the ecchymosis might have shown itself at some spot on the surface in a few days, but these falls from a height are fatal as a rule. In falls from a height, besides ecchymoses, which may occur where there are no other injuries or may fail where there are many injuries, the lesions consist of fractures of bones and ruptures of internal organs, with or without surface[553] wounds. The fractures may be of a number of bones, and especially of those which first touched the ground, though the skull may be fractured at some part whether or not it was struck in the fall. These fractures are often comminuted, especially fractures of the skull and pelvis, and when the fall is from a great height. Ruptures of muscles may occur with the fractures.
Ruptures of internal organs are not rare in such cases. According to Vibert,[656] the order of frequency of rupture of the various organs is as follows: liver, spleen, kidneys, lungs, heart, stomach, intestines, bladder, brain. Rupture of the liver occurs especially on the anterior and inferior surfaces and the bleeding is rather abundant. The healthy spleen does not rupture readily, except from a severe traumatism, but if it is hypertrophied it may rupture spontaneously from muscular violence. The lung may be ruptured internally without showing the rupture on the surface and with the ribs intact. Two such cases are mentioned by Vibert,[657] and he refers to others mentioned by Nelaton and Holmes. Rupture of the brain without fracture of the skull is very rare, though cases have been observed and reported, among others by Casper-Liman. In falls from a height the rupture of the aorta, mesentery, diaphragm, and larynx have been noted. It should be remembered in this connection that rupture of the liver, intestine, bladder, etc., may be caused by contusions without sign of violence externally, and such cases cannot, therefore, be attributed to falls unless there are other signs of the latter.
In crushes caused by a heavy vehicle, the lesions resemble in many respects those due to a fall from a height. Thus we find fractures and internal ruptures, but we more often and regularly find subcutaneous ecchymoses and ecchymoses between the muscles. The skin is often stripped up extensively and the injuries are generally limited to the region injured. It is rare to find that the cause of the injury leaves no trace on the skin, for it usually gives the form to the erosions or ecchymoses. Sometimes, for instance, the marks of a horseshoe are clearly visible. Ruptures of internal organs may occur here too when there are slight external marks of violence or even[554] none at all. Thus Vibert[658] relates the case of a man with the head crushed, but with no signs of injury to the trunk save a few erosions at the level of the sternum, who had not only rupture of the kidneys, the liver, and the spleen, but also of the lungs and of the heart. In the heart the apex was completely detached and floating in the pericardium, which was intact. There was no fracture of the ribs nor subcutaneous or sub-muscular ecchymoses. The age of the subject was thirty-two, so that the costal cartilages were not probably ossified, which may have accounted for the absence of fracture of the ribs.
Crushes by the fall of heavy weights resemble the latter class of crushes, and differ from falls from a height in the fact that the wounds are usually limited to one region. The lesions themselves are more or less similar. Similar internal lesions may be caused by the compression of the chest and body by the knee of a murderer, which may occasion rupture of the internal organs, fractures of ribs, etc. Thus, too, from the pressure of a crowd the ribs may be fractured and the lungs injured. It is particularly in these cases of injury from crushes or falls from a height that we may have most difficulty, as far as the medical evidence goes, of distinguishing between accident, suicide, and murder. But the various points and considerations mentioned above will sometimes enable the medical witness to clear up the case. In some cases the non-medical evidence, circumstantial and otherwise, may be sufficient of itself, or at least in conjunction with the medical evidence.
In falls from a less high place the difficulty is somewhat different, for here there may arise the question between a fall and a contusion or contused wound, and the question generally lies between accident and murder, or, very rarely, between accident and suicide. We have referred to both of these questions above, and from the facts mentioned the case can often be solved.
Of more than One Injury which was the First Inflicted?
We can sometimes tell the order in which wounds were received, but the question is rarely answerable with certainty.[555] If one wound is mortal and one or more are not, whether the wounds are suicidal or homicidal, it has sometimes been considered that the former must have been inflicted last. But we cannot admit that as a general rule the most grave wound was the last inflicted. For the murderer or suicide, especially the former, may go on wounding after the infliction of a mortal wound, especially as it is the exception, and not the rule, to die instantly after a mortal wound. Several assailants may have inflicted wounds at the same time, which would still further increase the difficulty. The question might then arise, Which assailant had inflicted the mortal wound or which had first inflicted a mortal wound? Under such circumstances, it would not be easy to give a specific answer. There are several signs which may indicate which wound was first inflicted in certain cases. An instrument may become duller or even bent or twisted after and on account of the first wound, and the subsequent wounds would vary accordingly. The wound of the clothes corresponding to the first stab-wound may be and often is only bloody internally, while the second and following wounds are bloody on both sides. The following case quoted by Taylor[659] from the Annales d’Hygiene, 1847, p. 461, illustrates this point. A man received three stabs from an assailant, one in the back at the level of the eighth rib, traversing the lung and heart and causing rapid death, and two on the left elbow, cutting the coat and shirt but only grazing the skin. The first one was evidently the first inflicted, for both the wounds in the clothing on the arm were bloody externally at the edges, although there was no blood effused here. The correctness of this opinion was confirmed at the trial.
The point of a knife arrested and broken off in a bone may show that this was the last wound. The amount of bleeding may show which was the first wound. Thus if several severe wounds have been inflicted, all or several of which would naturally cause profuse hemorrhage, and one showed signs of such hemorrhage while another did not, the former would be likely to be the first wound inflicted. Or if one showed slight hemorrhage where much would be expected, this fact would indicate that it was one of the last inflicted. The absence of the signs of spurting blood may tell which of two or more fatal wounds[556] were first inflicted, for this would indicate that this wound was inflicted when the heart action was weakened by loss of blood or even after death, and the other wound or wounds which did not present this sign would have been the first received. In fact, if any of the signs are present about a wound which we have seen to indicate that a wound was inflicted at any time after death, this would show that this wound was not the first received, and that the other or others were inflicted earlier.
Questions as to the CONSEQUENCES of WOUNDS NOT FATAL may often be brought up in civil actions for damages. In certain countries the question of the consequences as to incapacity may determine whether an injury shall be the ground of a criminal as well as of a civil action. Thus in France an injury which involves an incapacity of twenty days or more subjects the assailant to a criminal action. The term “incapacity” in this instance refers to general incapacity and not to incapacity for fine and professional work. The latter, however, comes in under the civil action which may be instituted against the assailant or those directly or indirectly responsible for the injury. The amount of the incapacity, its causes, whether due wholly or partly or not at all to the given injury, the probable duration of the incapacity, the treatment which it has and will necessitate, and many other such questions form part of the medical testimony required in such cases. Sometimes with slight wounds the results, accompaniments, and complications may prolong the incapacity very greatly, as also the state of health and the habits of the wounded person, the neglect of treatment, improper treatment, etc.
Any bodily or mental infirmity or ill-health which may result from an injury and its necessary treatment in the past and future, all these questions and many more unnecessary to mention may be required of the medical witness. No general rules can be laid down for all such cases. In giving his testimony the medical man must depend in any particular case upon his knowledge, judgment, and experience.
We can seldom give a precise solution of the question of survival to determine the succession or inheritance if several of a family die together in an accident. In case of death from inanition, cold or heat, or in drowning especially, if some have wounds more or less grave in themselves, we can sometimes[557] form an opinion. With wounds we cannot often do so, although in case of murder, the nature of the wounds, the position of the bodies, the examination of the spot of the accident or tragedy, may sometimes help us to form an opinion.
INCISED AND PUNCTURED WOUNDS AND WOUNDS OF BLUNT INSTRUMENTS REGIONALLY CONSIDERED.
The several varieties of wounds which we have been considering vary considerably in their nature, their effects, their danger, and in many other ways according to the region of the body in which they are situated. Some of these varieties are common in one situation and almost never occur in others. Although the nature of wounds found in the several regions of the body is not as important for a medical jurist as their danger and their influence in causing death, we will now consider the differences they exhibit on account of the region in which they occur.
WOUNDS OF THE HEAD.
These are often characterized by their apparent harmlessness and their real gravity sooner or later. We might almost make the opposite statement and say that those apparently grave are often virtually harmless, though this would be true only in a limited sense and in certain cases.
As to their nature, we find punctured wounds extremely rarely, incised and lacerated wounds often, while contusions and contused wounds are still more common. Incised and lacerated wounds of the head involve the scalp almost exclusively. These wounds heal remarkably well, even when the attachment is merely by a narrow pedicle, owing to the abundant blood-supply. Hemorrhage from the incised wounds is often free, for the vessels cannot retract, but it is seldom dangerous unless the wounds are very extensive. The only way in which they differ materially from similar wounds elsewhere is in the greater frequency of complicating erysipelas here than elsewhere. This is probably owing to the presence of septic conditions, as the head is generally dirtier than other parts of the body, and slight wounds especially are neglected. If the scalp is shaved over a wide margin and cleaned like other parts[558] of the body, erysipelas is found little or no oftener than with similar wounds elsewhere. The density of the scalp is so great that the redness and swelling accompanying inflammations is comparatively slight. If erysipelas follows slight wounds of the head, there is some reason to suspect constitutional predisposition or careless treatment. From infection of such wounds of the scalp abscess or diffuse cellulitis of the scalp may develop as well as erysipelas. The constitutional symptoms in such a case may be marked or even severe, but the prognosis is favorable. In very rare cases necrosis of the skull may result or the inflammation may even extend to the brain. These incised and lacerated wounds of the scalp are usually accidental or inflicted by another; they are rarely self-inflicted. Contusions and contused wounds are the most common forms of injury to the head. These two kinds of injuries are almost invariably inflicted by another or are accidental. We have already seen that contused wounds of the scalp or over the eyebrow may closely resemble incised wounds in these localities. This fact should be borne in mind, as careful examination can usually distinguish them if they are fresh and until they begin to granulate. These wounds are liable to the same complications as incised wounds, in fact more liable, as the contusion makes the wound more susceptible to inflammation and the edges are more apt to be infected at the time of the injury.
One of the results of contusions of the head is the extravasation of blood, most often between the aponeurosis of the occipito-frontalis muscle and the pericranium. These extravasations are usually in the form of a hematoma. Such hematomata often present a hard circular or oval rim with a softer centre, and may readily be mistaken for fracture of the skull with depression. The diagnosis between hematoma and depressed fracture is not usually difficult, however, for with hematoma the ridge is elevated above the level of the skull and is movable on the surface of the skull; also the wounded edges often pit on pressure. With depressed fracture, on the other hand, the edge is at or about the level of the rest of the skull; it is sharper, more irregular, and less evenly circular. Contusions and the resulting hematoma may occasionally end by suppurating, but this event is rare. Contusions and contused wounds may occasionally show the marks of a weapon, indicating[559] that they were inflicted by another. Also the position of the injury will indicate its origin, whether it is accidental or inflicted by another, for the former would not naturally occur on the vertex unless the fall was from a considerable height.
Another result of injuries to the head, especially of contusions and contused wounds, is FRACTURE OF THE SKULL. This may be simple or compound, depressed or not, etc. Fractures are serious inasmuch as they imply a degree of violence which may do damage to the brain. The fracture itself, especially if properly treated, affords a good prognosis, irrespective of any brain lesion. One variety of fracture of the skull offers an exception to this favorable prognosis, and that is fractures of the base of the skull. These may be fatal directly from injury of the vital centres at the base of the brain or soon fatal from hemorrhage in these parts. Or the fatal result may be secondary to an inflammation or meningitis which good treatment is often unable to prevent. It should not be considered that these fractures are uniformly fatal, for quite a considerable proportion recover. Fracture of the base usually occurs as the result of a fall. The injured person may land on the feet or buttocks, and yet receive a fracture of the base of the skull, the force of the fall being transmitted through the spine to the base of the skull. Fracture of the base of the skull usually occurs from an injury to the vault, not by contre coup, but by extension of a fissure found higher up in the skull. This extension takes place in the same meridian line of the skull with that of the force which produced the fracture, and in this way the base of the skull is fractured in different parts according to the point and direction of the application of the force. Thus in case the force compresses the skull antero-posteriorly the fracture will pass antero-posteriorly toward the base from the front or the back, whichever received the blow (see Fig. 13). Fractures of the vault of the skull occasionally occur opposite to the point struck; this may occur by contre coup, but not always so, as not infrequently in such rare cases a close examination may reveal an extension of a fissure from the point injured to the opposite pole of the skull. The shape and rarely the size of a fracture of the skull, especially if punctured in character, may show the shape and more rarely the size of the instrument or object which produced it. Apart from fracture of the base, the prognosis[560] in fracture of the skull is serious, mainly on account of the danger of inflammation, which is greater in compound fractures, and also on account of the more remote danger of irritation from depressed fragments causing epilepsy, insanity, etc., at a later period.
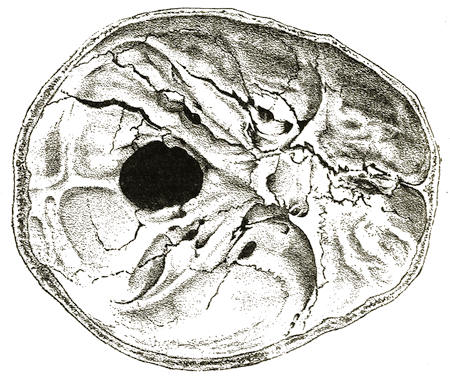
Fig. 13.—Several Fractures of the Left Half of the Base of the Skull, Running Parallel to One Another and Approaching One Another, also Separation of the Mastoid Suture. The injury was caused by a fall on the left side of the back of the head.
A circumstance that Taylor[660] says is connected with fracture of the skull with depression—namely, that the person, sensible as long as the object producing the fracture remained wedged in, became insensible and began to manifest other fatal symptoms as soon as it was removed—must be extremely exceptional. It may be explained, if it occurs, by the occurrence of hemorrhage after the object which occluded an open vessel by its presence or its pressure was removed. For it should be remembered that the symptoms of compression in a depressed fracture of the skull are very rarely due to the compressing effect of the depressed bone, but rather to an injury of the brain, intracranial[561] hemorrhage, or a local and temporary interference with the circulation.
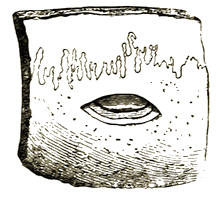
Fig. 14.—“Terraced” Fracture of the Left Parietal Bone near the Sagittal Suture, caused by the Lower Part of the Rim of a Round-Headed Hammer. The blow was struck from the right side. ½ natural size.
We may truly say that wounds of the head are dangerous in proportion as they affect the brain. The existence of affection of the brain may be hard to tell from the appearances, for an injured person may recover from the first effects of a comparatively slight wound and yet die suddenly later.
Concussion is the name applied to one of the effects on the brain of a more or less violent blow directly on the head or transmitted indirectly to the head. Though the term “concussion” implies a functional rather than an organic lesion, yet in the majority of cases it is equivalent to laceration of the brain. With laceration of the brain there is usually more or less effusion of blood which may be limited to a very thin layer. Concussion may exist without laceration of the brain. Even death has been known to occur from concussion of the brain without any visible signs of injury to the brain, so that the concussion must have been functional and the fatal result due to shock of the nervous system. Fatal concussion does not, therefore, necessitate the existence of compression or visible injury of the brain. Concussion may sometimes be due to a violent fall upon the feet, in which case the shock is transmitted through the[562] spinal column to the head with or without fracture of the base of the skull. It was in this way that the Duke of Orleans, the son of Louis Philippe, died.

Fig. 15.—Fractures of the Skull caused by a Four-sided Hammer. One caused by the Corner, the Other by the End of the Head of the Hammer. ¼ natural size.
Fig. 16.—Four-sided Fracture caused by a Hatchet-Shaped Instrument, the Edges Formed by Depression of the Broken Outer Table of the Skull.
—————————
The symptoms of concussion show all degrees of severity. Thus the injured person may become confused and giddy with or without falling, he may become pallid and nauseated and may vomit, but after a short period he recovers gradually.
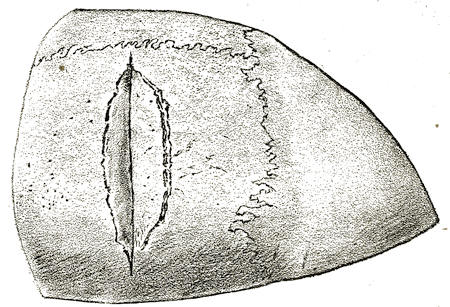
Fig. 17.—Fracture of Parietal Bone with Depression, caused by the Blow of an Axe.
With a more severe injury, with which there is generally some laceration of the brain, the injured person falls and lies quiet and relaxed, apparently unconscious, though often he can be partly roused. Paralysis and anæsthesia are absent. The heart is feeble and fluttering, the skin cold and clammy. The pupils, as a rule, react to light, but otherwise vary considerably. Urine and fæces may be passed involuntarily. As he begins to regain consciousness, vomiting usually occurs. Consciousness usually returns within twenty-four or forty-eight hours, when headache and indisposition to exertion are complained of, and this may last for a long time. Occasionally the symptoms instead of abating increase, and coma supervenes, often indicating meningitis, encephalitis, or intracranial hemorrhage. In other cases the person may die almost immediately on the spot where he fell, while in still others apparent recovery takes place and death occurs later either suddenly or after a reappearance[563] of symptoms. In such cases, abscess of the brain may occur and be the cause of the fatal result. These abscesses are the result of the injury, which may be almost anything from a compound fracture to a slight contusion not leaving any scar. The abscess may occur within a week[661] or not until after months or years. This interval of apparent recovery may lead to the false supposition that death was not due to the injury, but to some intervening cause. It is well to bear in mind that about half of the cases of abscess of the brain are not traumatic. A large majority of these are due to suppuration in the middle ear, a few to septic diseases or tuberculosis. The situation of the abscess often distinguishes between the traumatic and non-traumatic varieties. The traumatic variety is usually found beneath the injury or sometimes directly opposite, where the brain is injured by a kind of focussing of the radiated effects of the blow. The cases of abscess of the brain due to ear disease are usually found in the temporal lobe of the brain lying over the position of the ear or in the cerebellum behind it. The uncertainty of the nature and the extent of the cerebral injury in so-called contusion of the brain renders it necessary to be very careful in giving a prognosis. Any injury should be considered serious which has produced unconsciousness, for such an injury may produce enough laceration of the brain to render serious danger possible or even probable. We have seen that as a rule the symptoms of concussion come on immediately, but it is possible that symptoms at first so slight as to escape notice may become serious in a few hours or days. A gradual hemorrhage may sometimes account for this. The knowledge of certain acts performed or a conversation held at the last moment before the injury may be retained after recovery from concussion of the brain. This is not necessarily the case, for instead of remembering up to the moment of the injury, the injured person may remember only up to a certain time shortly before, or a part and not everything may be remembered.

Fig. 18.—Wounds of the Vault of the Cranium caused by Artillery Side-Arms, followed by Death shortly after.
The diagnosis of concussion of the brain from alcoholism is sometimes a matter of medico-legal interest or importance. Concussion may be so slight as to simulate intoxication. The history often clears the case up. The history of a blow or a fall or the presence of marks of violence on the head indicates concussion, though the blow or fall may not have caused the symptoms, which may be due to alcoholism. The odor of the breath may indicate alcoholism, but here too we may have both present and the concussion may be responsible for the symptoms. Or again the alcohol may have been given as a heart stimulant after the accident. This combination often occurs. If there is no odor in the breath, the presumption is in favor of concussion. As mistakes are still not infrequently made in diagnosis, those cases in which there is any ground for doubt should be carefully watched for developments. In general, the existence of concussion is more often overlooked than the coexisting alcoholism, so that if there is any doubt in a given case it should be treated as one of cerebral injury. The injury which causes the concussion in such cases is often due to the alcoholism. We may be able to verify this supposition if the injury is such as would be likely to be caused by a fall. There may be nothing found in the brain after death to distinguish between concussion and alcoholism. A bruise on the head only indicates a probability of concussion, for the bruise and alcoholism may both be present, the former perhaps due to the[565] latter. The presence of alcohol in the stomach would indicate the existence of alcoholism.
Another effect of an injury which has caused concussion of the brain is an extravasation or effusion of blood. Extravasation of blood in or on the brain is one of the commonest causes of death from injury to the head. It may occur with or without marks of external injury. A person suffering from such an extravasation of blood may recover from the first effects of the injury, and at a varying time afterward the symptoms may return and increase so as to result fatally. In such a case the opening of the bleeding vessel may have become plugged until some exertion, emotion, or excitement on the part of the injured person has loosened the plug. A hemorrhage may have ceased from partial syncope and return with a stronger heart action due perhaps to the administration of alcohol. This effusion may occur on the surface of the brain in connection with a superficial laceration of the brain or just beneath or outside the dura mater and not involving the brain directly. The latter cases are almost always due to the effects of violence, though there is at least one case of apparently spontaneous rupture of the middle meningeal artery. The violence which causes a rupture of the branches of this artery may be so slight as to leave no bruise or so severe as to cause fracture of the skull. The most important symptom of such extradural hemorrhage is a period of consciousness after recovery from the first effects of the injury, then stupor may appear and deepen into coma. A subdural hemorrhage may cause almost the same symptoms, though the injury is usually such as has produced a depressed fracture. This hemorrhage is most often due to the rupture of a number of small vessels under the fracture, though if one larger vessel is ruptured it is most often the middle cerebral. A thin layer of hemorrhage in connection with a superficial laceration of the brain is of frequent occurrence with or without the other two forms of intracranial hemorrhage. If the brain is lacerated we may have convulsions in addition to other symptoms. Death occurring during or soon after a prize-fight may occur from some of the above classes of intracranial extravasations. It may be questioned whether the blows or a fall caused the hemorrhage. It is generally due to a fall in such cases, but may be due to blows, but the guilt is[566] the same unless the fall was accidental. As the result of severe traumatism the vessels of the interior of the cerebrum may be ruptured or hemorrhage may occur into the ventricles of the brain. In such cases the symptoms will resemble those of ordinary apoplexy, only the cause is different from the latter and the injury is usually so severe as to leave no doubt as to the existence of a traumatism. The following question may arise in cases of intracranial hemorrhage and especially in the latter class of such cases, i.e., in cerebral hemorrhage:
Was the Extravasation of Blood due to Disease or Violence?—It may be alleged in defence that the hemorrhage was the natural result of disease. Where the hemorrhage is extradural or subdural or in connection with a superficial laceration of the brain, the cause is almost always traumatic. We have referred to one case of extradural hemorrhage from spontaneous rupture of the middle meningeal artery.[662] Subdural hemorrhage may occur from Pachymeningitis hæmorrhagica interna, but this condition is readily diagnosed on post-mortem examination and often with considerable certainty during life. A history of alcoholism, headache, impaired intellect, unsteady gait, occasional losses of consciousness, stupor increasing to coma, etc., indicates such a condition.
It is in cases of cerebral hemorrhage that there is the most difficulty in discriminating between that due to disease and that due to injury. It may be alleged that the hemorrhage was from diseased vessels, or that the effects of a blow, which cannot be denied, were aggravated by disease of the cerebral vessels or by excitement due to intoxication or passion. Cerebral hemorrhage from disease is rare before 40 years of age, except in alcoholics. When the hemorrhage is due to disease the blood-vessels are diseased. The most frequent site of such hemorrhages is the course of the lenticulo-striate artery in the ganglia of the base or the white substance of the centrum ovale.
When injury is the cause of the hemorrhage it is usually found beneath the point injured or directly opposite to this. External signs of the blow are generally visible if it be severe enough to cause a cerebral hemorrhage. The vessels may be[567] perfectly healthy and the victim quite young if the hemorrhage is due to an injury, also the ruptured vessels may be plainly torn. The most difficult cases are those where there is the history of an injury and at the same time such a condition of disease of the cerebral vessels, etc., as would account for spontaneous hemorrhage. Where the injury was slight in the case of alcoholics or aged people the medical witness should be especially careful in stating that a cerebral hemorrhage was due to the injury. Then, too, in the act of falling from the occurrence of a cerebral hemorrhage due to disease the head may be injured and show marks of violence. It should be borne in mind that an injury to the head may be inflicted when disease of the brain, vessels, or membranes already exists. In such a case a slight blow might cause extensive hemorrhage, but as that which accelerates causes, death, even though it might sooner or later have occurred in the same manner without injury, is due to the injury inflicted.
From the above considerations we see that spontaneous cerebral hemorrhage and that due to disease are not always easily distinguished from that due to violence. In severe injuries the structure of the brain is plainly bruised, etc., but the greatest difficulty exists in cases of slight violence where arteritis of the cerebral blood-vessels coexists. The spontaneous extravasation of blood in or upon the brain from excitement does not usually occur except with diseased vessels, old age, or alcoholism. It is rare, therefore, in the young and healthy. If there is any doubt as to the origin of the hemorrhage, the medical witness should state the cause most probable in his judgment. Taylor[663] supposes the case of a man excited by passion, alcohol, or both, who becomes insensible and dies after being struck a blow so slight that it would not have affected a healthy person. If examination reveals a quantity of blood effused into the substance of the brain, there can be little doubt in the mind of the medical man that the excitement was the principal cause of the effusion. On the other hand, if a severe blow or a violent fall on the head had been received in a personal conflict with another and it is found that death was due to an effusion of blood upon the surface, there can be little doubt in the mind of the medical examiner that death was due[568] to the blow, which would satisfactorily account for the conditions found without reference to coexisting excitement, etc. In fact, in all cases where a question is raised as to the cause of the hemorrhage, it is most important to consider whether the violence was not sufficient to account for the hemorrhage without the coexistence of disease or excitement. It is also most important to bear in mind that after severe injuries, as after a fall, causing extensive fracture of the skull, followed or not with extravasation of blood, the injured person may walk about and die some distance from the place of the accident and where no chance for a similar accident exists. In this way the suspicion of murder may be occasioned, as illustrated in the following case cited by Taylor:[664] A man was accused of the murder of his companion, who was found dead in a stable with fracture of the temporal bone which had caused rupture of the middle meningeal artery. The accused stated that the deceased had been injured by falling from his horse the day before. After the fall, however, the deceased had gone into a public-house, where he remained some time drinking before returning to the stable. The extravasation had here taken place gradually, as is characteristic of hemorrhage from the middle meningeal artery, and perhaps the excitement due to the drinking had influenced it.
The date of an effusion of blood may sometimes be a matter of importance in determining whether a given extravasation of blood in or on the brain was caused by a recent blow or had existed previously. The color and consistence of these effusions indicate whether they are old or recent; the precise date we cannot state, but the information we can give is often all that is required. The color of recent effusions is red, which changes after some days to a chocolate or brown, which generally turns to an ochre color (see Plate I.). This latter color may be met with from twelve to twenty-five days after the injury. The consistence of the coagula also becomes firmer with age, and as the coagula become firmer they are more or less laminated and the expressed lymph may lie between the laminæ or around the coagula.
MEDICAL JURISPRUDENCE—PLATE I.

Extravasations in several portions of the Arachnoid, with hemorrhages in neighboring portions of the brain. Death in four days.

Cerebral abscess. Epilepsy, Paresis. Death 3¼ years after the injury.
RECENT AND OLD CEREBRAL EFFUSIONS.
On account of the many layers of the brain coverings, a rough diagram of the coverings as given by Taylor[1] may be of much use to the medical expert in illustrating his evidence so as to make it clear to the court (see Fig. 19).
Wounds of the brain vary very widely in their immediate results according to the part of the brain injured. Thus sometimes a slight wound of the brain may be instantly fatal and often a severe wound in another part is not so. Extensive wounds may occur especially in the frontal lobes with remarkably slight disturbance. If a person with a wound of the brain survives the first effects of the injury the danger of inflammation remains. This danger may not be removed for a long time, for the inflammation may develop very slowly, not showing itself for from three to ten weeks or even later. Thus Taylor[665] cites the case of a child who was accidentally shot through the brain. The symptoms of inflammation did not appear until the twenty-sixth day and death occurred on the twenty-ninth day.
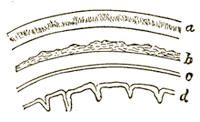
Fig. 19.—Diagramatic Representation of the Skull and Membranes of the Brain for Exhibition in Court. a, Skull with outer and inner tables and diploë; b, dura mater; c, arachnoid membrane; d, pia mater.
Wounds of the face heal remarkably well on account of its great vascularity. If severe they may leave great deformity or disfigurement, which may be the ground of a civil suit and thus require the testimony of a medical expert. If the wound involves the orbit or its contents it may be more serious, either from a fracture of the thin upper or inner wall of the orbit, separating it from the brain, or from extension of a secondary inflammation of the contents of the orbit to the brain. Wounds of the eyebrow may cause supra-orbital neuralgia or amaurosis from paralysis of the upper lid. Some fractures of the nose, especially those due to severe injury near the root of the nose, may be more serious than they appear. For in such cases, of which the writer has seen several, the fracture is not confined to the nose, but involves also the ethmoid bone and its cribriform plate forming part of the base of the skull. In such a case a fatal meningitis is a common result.
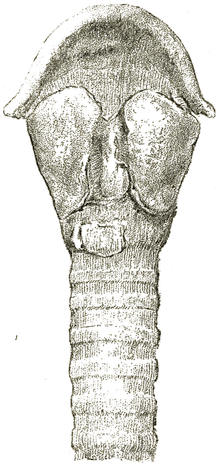
Fig. 20.—Double Fracture of the Thyroid and Cricoid Cartilages of the Larynx, from the Blow of a Flat-Iron.
Wounds of the neck are very rarely accidental, more often homicidal, but most often suicidal. In nature they are most often incised wounds. As we have already seen, the kind[570] and condition of the weapon used is often indicated by the character of the wound. We have also seen that in many cases a suicidal wound of the neck can be distinguished from a homicidal one with more or less probability or even certainty. Wounds of the neck are often dangerous, and they may be rapidly fatal if they divide the main vessels, especially the carotid arteries. Wounds of the larynx, trachea, and œsophagus are grave and often fatal from entrance of blood into the air-passages or from subsequent œdema or inflammation occluding the air-passages. Wounds of the sympathetic and pneumogastric nerves may be fatal, and those of the recurrent laryngeal nerves cause aphonia. The situation of the average suicidal or homicidal cut-throat wound is in front, generally across the thyro-hyoid membrane, sometimes dividing the cricoid-thyroid membrane, and not at the side of the neck where the great vessels lie and would be more easily divided. The force is expended, as a rule, before the great vessels are reached. The epiglottis may be cut or detached and the incision may even reach the posterior wall of the pharynx, but the majority of the suicidal cases recover with proper treatment. The homicidal cases are more often fatal from division of the great vessels, though, as already stated, in either class of cases a fatal result may occur if the air-passages are opened from the entrance of blood into them and the consequent asphyxia.
Contusions of the neck may be so severe as to cause unconsciousness or even death. The latter may be due to a reflex inhibitory action, as in cases of death from a blow upon the pit of the stomach. As a result of such contusions we may have a fracture of the larynx usually confined to the thyroid[571] and cricoid cartilages (see Fig. 20). This may be followed by hemorrhage from the larynx, some of which may pass down into the trachea and threaten death from asphyxia. Later emphysema often develops throughout the tissues of the neck, and there is great danger of œdema of the larynx. The prognosis is serious unless tracheotomy is performed early or the case is closely watched. It is most serious where the cricoid cartilage had been fractured, as this requires a greater degree of violence. Whereas incised wounds of the throat are most often suicidal, contusions are most often accidental or inflicted by another. Among the latter class of injuries may be included the so-called garroting, by which a person is seized violently around the throat, usually from behind, and generally with a view to strangle and rob. In such cases the larynx or trachea may be injured in the same way as by a contusing blow.
WOUNDS AND INJURIES OF THE SPINE AND SPINAL CORD.
Injuries of the spine resemble more or less closely those of the head. Fractures of the spine generally occur in combination with dislocation, as fracture-dislocation. Thus displacement is generally present and causes a fatal compression or crushing of the cord. When the cord has once been crushed at the site of the displacement of the fracture-dislocation there is no hope of its ever healing. Therefore the lower end of the cord is never again in functional connection with the brain. These injuries are more rapidly fatal the higher up they are. If the injury is above the fourth cervical vertebra death is nearly immediate, for then even diaphragmatic breathing is impossible, and the injured person dies of asphyxia. Fracture of the odontoid process of the axis, which regularly occurs in hanging, may occur from falls on the head, etc., and is not always immediately fatal. Thus in one case[666] the person lived fifteen months and in another case sixteen months. In the latter case the fracture was due to the patient turning in bed while his head was pressed on the pillow. In some cases it may be questioned how far this injury may result from disease of the bones or ligaments. Therefore a careful examination of these parts should be made after death, which will usually[572] enable us to answer this question, which may be brought up by the defence. It is hardly necessary for our purpose to enumerate the symptoms of fracture-dislocation of the spine. Of course the patients are almost always unable to walk and so are bed-ridden. A marked feature of fracture-dislocation of the spine is the length of time intervening between the injury and the fatal termination, and yet the injury is wholly responsible for the death of the injured person. This delay may last for months or even for years with careful treatment. But sooner or later the case generally ends fatally, though not necessarily so. Where the cord has been entirely crushed the result is almost always fatal; where the cord is not so injured recovery may and often does occur. According to Lutaud, fractures of the spine are sometimes followed by secondary paralysis coming on after healing of the fracture. At the outset we can seldom give a definite prognosis, which can only be given after watching the developments of the case. The prognosis is more favorable in fracture of the arches alone or when the injury is in the lower part of the spine and not very severe. The commonest cause of fracture-dislocation of the spine is forced flexion of the spinal column. Injuries to the spine are generally the result of falls or blows on the spine, especially in its lower part. Lutaud[667] states that after forced flexion of the spine without fracture paraplegia may sometimes occur, which is attributed to forced elongation of the cord. This paraplegia, which may seem to be grave, is completely recovered from as a rule.
Incised or punctured wounds of the spinal cord are rare, as it is so well protected except in the very highest part behind. Here between the occiput and the atlas and between the latter and the axis, and to a less extent between the axis and the third cervical vertebra, the cord is more exposed, owing to the narrowness of the laminæ. It is here that pithing is done, which is almost instantly fatal, as the medulla oblongata and upper part of the spinal cord are the parts injured, and they contain the respiratory and other vital centres. Pithing may be done with such a small needle-like instrument as to leave scarcely any trace. Only a slightly bloody streak may persist, which may appear superficial if the instrument is introduced[573] obliquely. Such a mark in this location with no other apparent cause of death should always lead to an examination of the upper part of the cord, which will always reveal the cause of death in such cases. Pithing is practised especially in infanticide.
As with the brain, so with the spinal cord, we may have CONCUSSION due to the shock of a contusing blow. Concussion of the spinal cord, as of the brain, may be fatal without showing scarcely a mark of violence externally or internally. As the cord is so well protected from injury, it must be extremely rare to have concussion of the cord without some actual lesion of its substance. As concussion of the cord is not often the result of the injuries of which we are treating, but rather of railroad injuries and the like, it will not be considered at length in this connection. As a result of a blow or fall on the spine or communicated to it, hemorrhage may occur in the substance of the cord or around it between or outside its membranes. In very rare cases such a hemorrhage may occur spontaneously as the result of disease, of which the writer has seen one case. It may be associated with concussion or laceration of the cord. It may destroy life directly by extension or indirectly by leading to a spreading inflammation. Hemorrhage in or about the cord causes a gradual compression of the cord, and in cases of fracture of the spine often adds to the compression due to the displacement of the bones. In hemorrhage into the substance of the cord paralysis comes on early or immediately and may be complete while symptoms of irritation fail. The latter symptoms are most marked in meningeal hemorrhage in which paralysis is delayed in appearance and generally incomplete. The products of an inflammation due to an injury may compress the spinal cord in the same way that hemorrhage does.
Wounds and injuries of the varieties we are considering, affecting the spine and spinal cord, are generally accidental, less often homicidal, and almost never suicidal.
WOUNDS OF THE THORAX AND THORACIC ORGANS.
Wounds of the thorax caused by incising, puncturing, or blunt instruments. These wounds are most often punctured wounds; contused wounds are common and incised wounds are not rare. They are perhaps most often homicidal[574] in origin or at least inflicted by another, and the accidental origin of these wounds is probably the least common.
Incised or punctured non-penetrating wounds of the thoracic wall are rarely grave. Bleeding, as a rule, is not serious, though it may be quite free. Such wounds may be accompanied by emphysema, though not penetrating, owing to the movements of the chest and a valve-like action of the edges of the wound. Contused wounds of the thorax are more dangerous, especially if the violence was great, owing to the complicating fracture of the ribs, rupture of the thoracic viscera, etc.
Fracture of the ribs is a common result of contusions of the chest. It is more dangerous when due to a direct blow or injury, as then the splintering occurs internally and may wound the lungs, heart, or large vessels, while with fracture from indirect violence, from compression of the chest, the splintering of the ribs occurs externally. Fracture of the upper ribs requires more force than that required to fracture the lower ones, and consequently the former is the more dangerous. The diagnosis of fracture of the ribs is generally quite easy by means of crepitus felt or heard, false motion, local tenderness, etc. Fracture of the sternum may be serious if depressed on account of the wounding of the viscera behind it. Devergie[668] cites such a case where the depressed portion of the sternum produced a transverse non-penetrating wound of the heart about an inch in length, which had caused death in thirteen days. Simple fracture of the sternum without displacement of the fragments is rarely serious unless injury of the thoracic viscera is produced by the same violence. Wounds or injuries of the thorax are grave or not according as they penetrate or injure the thoracic viscera or do not do so. A wound may just penetrate the thoracic wall without wounding the thoracic viscera, and is then serious as a rule only when followed by inflammation. In fact, many of the penetrating wounds of the thorax wounding the viscera are only grave on account of consecutive inflammation. We have already seen that various characteristics of wounds of the thorax, especially of stab-wounds, enable us to determine the kind of weapon used, its size, sharpness, etc., and sometimes to identify the weapon itself. In much the same way we can often determine whether[575] the wound was suicidally or homicidally inflicted. The cause of death in wounds of the thorax may be directly due to the wounding of one or more of the thoracic viscera, or it may be due to the inflammation occasioned by it. Wounds of the lower part of the thorax may involve at the same time the thoracic cavity proper and its contained viscera, the diaphragm and the abdomen and its viscera. This is the order in which the different parts would be met with in a wound from behind forward; the order might be the reverse of this in a wound from before backward. Penetrating wounds of the thorax may involve the lungs, heart, or great blood-vessels. Of these, the lungs are most often injured, which is easily accounted for by the greater size of the lungs. In wounds of the lungs the immediate danger is from hemorrhage. The hemorrhage appears externally through the wound and from the mouth, being coughed up. Where the lungs are injured by a blow, fall, or crush without external injury, blood appears in the mouth only. The blood coughed up from the lungs is bright red and frothy, and it may also be frothy at the external wound. Hemorrhage from the external wound may be slight, especially if the wound is oblique and acts as a valve. In wounds of the lungs most of the blood may collect in the pleura or in the lungs, and thus, by compression from without or by displacement by the blood within it, prevents air from entering the lungs and produces asphyxia, which may be fatal. More or less dyspnœa usually occurs at first. Emphysema is generally present in the cellular tissues, but this latter symptom may also occur at times with non-penetrating wounds of the chest. If death does not occur speedily from hemorrhage by compression of the lungs or heart, there are good hopes of saving the patient, but the prognosis should be reserved. For even when the first effects of the wound of the lung are survived, the patient may die from the effects of inflammation, recurring hemorrhage, or a too sudden relaxation of regimen. Thus, for instance, if too much food, talking, or exertion are indulged in the case may on this account terminate fatally, and such aggravating causes of death may mitigate the sentence.
Wounds of the heart are among the most fatal. Although it was once considered, and is usually thought now by laymen, that wounds of the heart must be necessarily and instantly[576] fatal, the facts are otherwise. If the wound is small and oblique life may be prolonged, and cases are recorded[669] in which wounds of the heart were not directly fatal, and in some of which recovery would have probably resulted if not for other diseases. Cases in which the heart wall was wounded but not penetrated, and in which healing took place, are not very rare.[670] Thus Callender removed a needle from the substance of the heart. But there is perhaps only one case[671] on record in which a wound penetrating the cavities of the heart was recovered from. It is the rule rather than the exception that wounds of the heart, penetrating or not, are not immediately fatal. Thus in a series of twenty-nine cases of penetrating wounds mentioned by Devergie,[672] as collected by Ollivier and Sanson, only two ended fatally within forty-eight hours, the rest in periods ranging from four to twenty-eight days. This delay in the fatal result has been attributed to the arrangement of the muscle fibres crossing one another and tending to close the wound, or at least to make it smaller. As to the various parts of the heart wounded, the right side, especially the ventricle, is most often wounded. Thus out of fifty-four cases of wounds of the heart, Taylor[673] states that the right ventricle was wounded in twenty-nine cases, both ventricles in nine, the right auricle in three, and the left auricle in one case. This greater frequency of wounds of the right side of the heart is easily accounted for by its more exposed position anteriorly, just beneath the chest wall in a part of its extent. The rapidity of death depends largely upon the site and extent of the wound. Lutaud[674] states that out of twenty-four cases of wounds of the right ventricle only two were fatal within forty-eight hours, and out of twelve cases of wounds of the left ventricle three were not immediately fatal. Wounds of the auricles are generally fatal immediately, especially if the cavity is extensively laid open. It is the general opinion that wounds of the auricles are most rapidly[577] fatal, next those of the right ventricle, and lastly those of the left ventricle. This difference is probably due to the comparative thickness of the walls of these parts. Thus the wall of the left ventricle is so thick as to tend to close a wound unless it be extensive. In wounds of the heart death rarely occurs from external hemorrhage, which may be quite slight or even altogether wanting where the wound is due to a crush or fracture of the ribs. Death is usually due to the compression of the heart by the blood in the pericardium. This usually causes syncope, or a slighter pressure may be fatal by causing cerebral or pulmonary anæmia or shock. Death may occur suddenly in this manner or not until after some time. Thus in penetrating stab-wounds little or no blood probably escapes at first, in most cases, but it may ooze or, later on, suddenly burst out into the pericardium. Therefore after a wound of the heart the patient does not, as a rule, die immediately, as formerly and often at the present time erroneously supposed. This fact is of little importance as a rule in surgery, for the patients generally die sooner or later, but it is of importance in medical jurisprudence, for upon it may hang the solution of questions of murder, suicide, or justifiable homicide. It also accounts for the fact that the injured person can exercise voluntary power after the injury. Thus Watson[675] met with a case where a man ran eighteen yards and died six hours after a stab-wound of the right ventricle. The coronary artery was divided and the pericardium was filled with blood. Also Boileau met with an accidental penetrating stab-wound through both ventricles in a soldier who ran two hundred yards, then fell and died in five minutes. A boy admitted to Guy’s Hospital in 1879 lived forty-two hours with a bayonet-wound transfixing the right auricle, the septum, the left ventricle, the mitral valve, and entering the left auricle.
Minute wounds of the chest are sometimes made by needles, etc., in the region of the heart with the intention of killing infants or children. Taylor[676] also mentions the case of a fatal wound of the heart from a needle, the result of accident. We have already cited the case of a needle lodged in the heart wall[578] and removed by Callender by operation. That the puncture of the heart by a small instrument is not necessarily serious is proved by the experiments of Senn,[677] by which he found that “the heart can be punctured with a perfectly aseptic, medium-sized aspirator needle without any great immediate or remote danger.”
In cases of RUPTURE OF THE HEART the question may come up as to whether it was the result of disease or violence. We have already seen that rupture of the heart may occur from falls or crushes without marks of violence to the chest. In general, we may say that in rupture of the heart from violence the right side and base are most often involved, while in rupture from disease the left ventricle is generally ruptured, especially near the apex. The exciting causes of rupture of a diseased heart are often violent emotions or exertion, which may both be present in a quarrel with another and cause rupture without direct violence. The cause need be but slight if the heart is diseased, whether the cause is a natural one or outward violence. Rupture from disease may therefore excite suspicions of murder, but those cases can usually be satisfactorily solved by examination of the organ post mortem. A slight degree of violence may cause rupture of a diseased heart about ready for rupture from natural causes. When a diseased heart ruptures during a quarrel, the symptoms of rupture of the heart may be observed to come on suddenly before and without the infliction of any violence.
Wounds of Arteries and Veins, especially within the thorax.—Wounds of large trunks are generally speedily mortal. In the chest we may occasionally meet with wounds of the intercostal or internal mammary vessels or the vena azygos veins. These wounds are often serious and may be fatal. We have already seen that blood in the large cavities of the body, like the chest, is commonly not coagulated, or at least the greater part of it. We have already seen, too, that after wounds of the carotid artery the victim may preserve the power of locomotion for a short time, but not the power of struggling. This fact may be important to help distinguish between murder and suicide. In such wounds of the carotid the voice may be lost, as the trachea is often divided. Death from wounds of large[579] vessels may be due to loss of blood, and if this danger is passed the case may still terminate fatally, as in a case where the brachial was tied for injury and death occurred in three days from gangrene. The wounds of comparatively small vessels may prove fatal from hemorrhage, etc.
In wounds of blood-vessels death may occur from the entrance of air into them. In some cases where this is supposed to have occurred it is quite probable that death was really due to hemorrhage. A considerable quantity of air may enter the circulation, especially the arterial circulation, without a fatal result. When death does occur it is owing (1) to “mechanical over-distention of the right ventricle of the heart and paralysis in the diastole,” or (2) to “asphyxia from obstruction to the pulmonary circulation consequent upon embolism of the pulmonary artery.”[678] Senn found that fatal air embolism could hardly occur spontaneously in a healthy jugular vein, as the walls collapse readily from atmospheric pressure.
Wounds and Ruptures of the Diaphragm.—These may be due to weapons, fracture of the ribs, falls or crushes, and disease. They also occur as the result of congenital malformation, though these cases seldom survive long. These injuries are generally homicidal or accidental in origin. As a rule, the viscera are wounded at the same time, or, if not wounded, at least herniated, and may thus become strangulated. It is therefore hard to estimate the danger in such cases, but the prognosis is at all times serious. The most serious cases of such injury to the diaphragm are due to violent contusions or falls when the stomach and intestines are full. The hemorrhage is usually slight, but hernia of one or more of the abdominal viscera usually occurs in such cases, and is said to be more readily produced during inspiration when the fibres are on the stretch. According to Devergie, rupture of the diaphragm with hernia is more common on the left side in the central tendon in front of the crura and at the junction of the left muscular leaflet. Also on either side of the ensiform cartilage and especially on the left side there occurs an area of the diaphragm which may be congenitally weak or even absent, and here too rupture and hernia are likely to occur. Phrenic or diaphragmatic hernia occurs especially after lacerated wounds, even[580] after the wounds have apparently healed. If hernia occurs long after the injury was inflicted, it may be asked whether the wound was the cause of the hernia, and so of death. This can only be determined by examination. Almost any or all of the movable abdominal viscera may be found in a diaphragmatic hernia. It was once supposed that this accident would be immediately fatal, but this is far from the truth. Devergie relates the case where a person lived nine months with the stomach and colon in the chest and died from another cause. Thus a person may have a phrenic hernia and die from another cause, or having had a rupture or wound of the diaphragm he may suddenly acquire a diaphragmatic hernia by reason of a blow or sudden exertion, or the latter may strangulate an existing hernia. A person with a diaphragmatic hernia may have the power of moving or walking, but is more or less incapacitated owing to the compression of the lungs which exists and the consequent dyspnœa, etc.
WOUNDS AND CONTUSED INJURIES OF THE ABDOMINAL WALL AND VISCERA.
Such wounds and injuries of the abdominal wall may be incised, punctured, or due to blunt instruments, etc. They are usually homicidal or accidental, seldom suicidal except in delirious patients or lunatics. The cause of death in such cases may be due to hemorrhage, shock, etc., or to secondary inflammation, which is especially likely to occur in penetrating wounds. The kind of weapon used may often be judged from the nature of the wound. Incised and non-penetrating punctured wounds are usually simple and not grave, but may be otherwise from hemorrhage from the deep epigastric artery, or from inflammation in or between the muscles, or in the subperitoneal connective tissue. In the latter case peritonitis may occur, but is rare. A ventral hernia may, however, result later on, as also from a cicatrix, especially if it is transverse. In such cases the question arises whether the natural results of the wound were aggravated by unskilful or improper treatment or even wilful neglect on the part of the patient or practitioner.
Contusions of the abdomen are more serious often than those of the chest, for there is less power of resistance. We[581] have already seen that death may occur from a contusion of the abdomen too slight to show a mark of ecchymosis or a serious injury internally. This has been attributed by some to an effect on the solar plexus or reflexly on the cardiac plexus causing a fatal inhibition. Lutaud and others have expressed the doubt whether the cases reported by Travers, Allison, Watson, Cooper, Vibert, and others were carefully examined, and have inferred that some visible organic change must have been present. Some such cases, however, have been examined with especial reference to this point, and no physical injuries and no other cause of death elsewhere has been found. There is no ground, therefore, for a jury to doubt that a contusion of the abdomen was the cause of death because there are no visible marks of injury.
Again, it is a well-known fact that the blows severe enough to cause rupture of the abdominal viscera may sometimes leave no trace of violence in or on the abdominal wall. On the other hand, it must be remembered that effusions of blood may be found post mortem in the sheaths of muscles without indicating violence, so that blood may be found effused in considerable quantity in and around the abdominal muscles without violence having been done. In such cases, therefore, we should note whether abrasions or ecchymoses of the skin are absent or not. If they are absent and there is no other evidence of a blow, the medical witness should hesitate to attribute such an effusion of blood between the muscles to an act of violence.
As in the case of the chest, so wounds of the abdomen are serious, as a rule, mainly as they involve the abdominal viscera. The viscera may be wounded by a penetrating wound or by rupture, and the fatal result is due sometimes to internal hemorrhage or to shock, but generally to secondary septic peritonitis, which may be fatal in a few hours or only after days or weeks. Occasionally wounds of the abdominal viscera undergo spontaneous cure without surgical interference and with or without medical treatment. But as a rule they are fatal unless they receive proper surgical treatment. A wound of the abdominal wall may be penetrating without wounding any of the viscera. Such wounds may be fatal if they are infected, otherwise they usually heal readily and without danger unless they are extensive and the abdominal contents are exposed to the air. The[582] gravity of penetrating wounds varies somewhat with the particular viscus or viscera injured. It is well not to examine wounds of the abdomen by the finger or probe too freely unless a laparotomy is anticipated; for a simple wound or penetrating wound without wounding of the viscera may thus be infected. Enough examination is necessary to diagnose between a simple and a penetrating wound of the abdominal wall.
RUPTURE OR WOUNDS OF THE ABDOMINAL VISCERA.
The Liver is most often wounded of any of the abdominal viscera, with the possible exception of the intestines, because of its size, and it is most often ruptured partly because of its size, but mostly owing to its friable consistence. Such injuries most often involve the right lobe, as it is much the larger of the two principal lobes. The anterior surface and inferior border is the most frequent site both of wounds and ruptures of the organ. Ruptures rarely pass entirely through the organ, but are generally not more than an inch or two in depth. They are usually directed antero-posteriorly or obliquely, rarely transversely, and the lacerated granular edges are not much separated as a rule (see Fig. 21). Rupture of the liver may be due to a blow, crush, or fall, or even to sudden muscular action if the organ is large and fatty. Thus Taylor[679] relates the case of a woman who died after child-birth of uræmic convulsions, and in whom there was quite an extensive hemorrhage into the liver beneath its capsule, and apparently due to violent muscular contraction. As we have already seen, the liver may be ruptured without the abdomen showing the marks of external violence. Rupture or wound of the liver is one of the causes of the fatality of wounds and injuries of the abdomen. The fatal result may be and often is due to hemorrhage; in other cases it is due to shock or the occurrence of peritonitis. Wounds of the liver heal readily and hemorrhage is arrested at once, as a rule, by the approximation of the edges. There may be little blood in and about the wound, but it collects in the right iliac region or in the pelvis and is not wholly coagulated. Unless the wound or rupture involves the vena cava, portal vein, or a large branch of either of these, the hemorrhage is apt to be slow and the[583] victim may survive hours or even days, except for active exertion or repeated violence. Two cases illustrating the slowness of the hemorrhage have occurred in Guy’s Hospital. In one[680] the man, showing no urgent symptoms at the time, was sent away, and died a few hours later in a police-station. In this case the liver was ruptured nearly through its thickness, and a basinful of blood had been effused, causing death. In the other case,[681] which occurred to Wilks, the patient survived the accident ten days, and Taylor[682] cites a case which was reported to have ended fatally eight years after the accident. As a rule the injury is fatal, without treatment, within forty-eight hours. Not being immediately fatal as a rule, the victim of a rupture or wound of the liver can walk about, and may be capable of more or less severe muscular exertion after the injury, though the fact of such exertion has sometimes been used by the defence to prove that the rupture was not due to the particular violence in question.
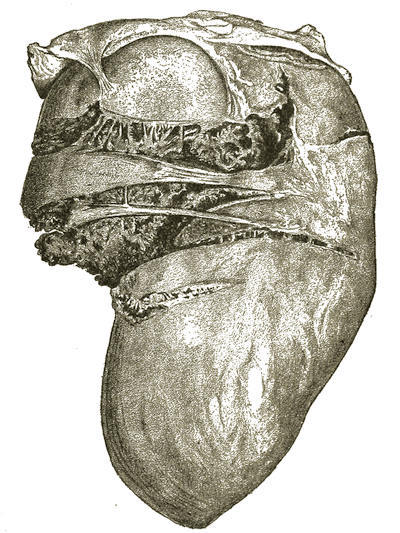
Fig. 21.—Ruptures of the Liver from a Fall from a Considerable Height, causing Immediate Death.
Wounds and ruptures of the gall-bladder result in the effusion of bile. While rupture of the liver is not necessarily followed by peritonitis, rupture of the gall-bladder with the effusion of bile generally causes peritonitis, and is fatal in this way and not from hemorrhage. Rupture of the gall-bladder may be favored by the presence of gall-stones, but the result is still attributable to the injury.
Spleen.—Ruptures of the spleen may be due to a bruising violence in this region, and here too the skin may not show the marks of the contusion, though this fact is still employed by the defence to try to disprove the connection between the injury and the result. It is important to remember, from a medico-legal point of view, that an enlarged and softened spleen may be ruptured from a comparatively slight muscular exertion. This might occur in a sudden movement to avoid a blow, and the charge of manslaughter might be affected by the mode of the production of the injury and the previous abnormal condition. Only direct violence is liable to rupture the healthy normal spleen. Rupture and wounds of the spleen may be and generally are fatal from hemorrhage, owing to the vascularity of the organ; more rarely are they fatal from shock. Peritonitis is not a result to be expected.
The hemorrhage accumulates in the lower and left side of the abdomen or in the pelvis, and coagulation is imperfect if present at all.
Kidneys.—These are occasionally ruptured from violence, but more often from accident. Wounds of the kidney are rare, owing to the depth from the surface at which they lie. They are more accessible from behind. A wound from behind is generally extra-peritoneal unless it perforates the organ; not so a wound from in front. Accidents in which the lumbar region is forcedly flexed are most apt to be followed by injury[585] to the kidney. The injury may cause no prominent symptoms, but usually lumbar pain and tenderness, frequent micturition and hematuria, and in severe cases the symptoms of hemorrhage and shock are present. The injury may be speedily fatal from hemorrhage or collapse, or more slowly fatal from peritonitis, when the peritoneum is involved, or from abscess and septic infection, or from uræmia if the other kidney is diseased. Slight injuries are generally recovered from. As is the case with the liver and spleen, so after injuries of the kidney the victim may walk about, etc., unless there is copious and immediate hemorrhage.
The bladder may be wounded directly through the hypogastrium, vagina, or rectum; it may be punctured by a broken fragment of the pelvis, especially the pubis, or it may frequently be ruptured from blows, crushes, or falls. The latter accident occurs especially where the bladder is distended. The bladder may also rupture spontaneously from over-distention, which may or may not be favored by disease of the bladder wall, in which case rupture occurs more easily. Medico-legally the question may arise whether the rupture was spontaneous or due to injury. In this connection it should be remembered that the injury may leave no external mark of violence, and a case is recorded in which the bladder was ruptured by a fall in wrestling; but the question can be determined only by an examination of the bladder. If the wall of the bladder is thinned by the pressure of a calculus or from other causes, or if it is weakened by tubercular, syphilitic, or carcinomatous deposits or ulcerations, it may be spontaneously ruptured from slight distention or a slight degree of violence may rupture it. If violence has been employed it is responsible for the rupture, though the diseased condition may act as a mitigating circumstance; not so a distended bladder, as the latter is not abnormal. In spontaneous rupture from over-distention without disease of the bladder wall, stricture, hypertrophied prostate, or some such condition must be present to account for the over-distention. Spontaneous rupture of the bladder can, therefore, only occur when either disease of the bladder wall or obstruction of the urethra is present. No condition excludes rupture from violence. If there is an injury followed by the symptoms of rupture of the bladder and death and the bladder and urethra are healthy,[586] there can be little doubt that death was due to the injury. Wounds or rupture of the bladder may be extra-peritoneal or intra-peritoneal. Rupture from disease of the bladder wall occurs at the site of the diseased and weakened spot, which is most often at the base of the bladder. Rupture of the bladder from violence occurs most often on the postero-superior wall, running downward from the urachus, in which case the peritoneum would be involved. A punctured wound of the bladder wall may be so minute that the leakage is very slow and the customary symptoms may be obscured, or the opening may be valvular in character, perhaps allowing escape of urine only when the bladder is not distended. The symptoms consist of pain, inability to micturate, and the presence of blood in the little fluid which can be drawn by a catheter. Fluid injected is not all returned and the bladder cannot be distended. After a time varying from a few hours to a few days, depending upon the size of the opening and the condition of the urine, peritonitis or peri-vesical cellulitis is set up, the former being generally fatal, the latter not necessarily so. Prompt surgical treatment may save the patient’s life by avoiding peritonitis. Extra-peritoneal ruptures are far less dangerous than intra-peritoneal, as in the former case cellulitis and abscess in the cellular tissue around the bladder, which may subsequently be treated by operation and drainage, take the place of peritonitis in the latter case, for which prevention is the only safe treatment. In extra-peritoneal rupture death, if it occurs, is generally due to septicæmia; in the intra-peritoneal variety it is due to peritonitis. These cases of injury to the bladder may die suddenly and speedily from shock or from peritonitis in three to seven days, or not until fifteen days or so. In punctured and incised wounds the urine escapes more slowly, peritonitis develops less early, and death is longer delayed. Hemorrhage in injury to the bladder is not usually serious; the blood is found partly in the bladder, partly in the pelvis, where the fluid extravasated by peritonitis is also found. The victim of a wound or rupture of the bladder may often walk about for some time after the injury.
Stomach and Intestines.—Punctured wounds, or, more rarely, incised wounds of the abdomen may involve these organs, or they may be ruptured by blows, crushes, and falls, or[587] from disease. Stab-wounds of these viscera may be multiple from a single stab, the instrument traversing one coil, perhaps, and then wounding others, though this is less often the case than with gunshot wounds. Ruptures too may be multiple, though less often so than wounds. The ileum is most liable to rupture, though several cases of rupture of the jejunum are on record. Like the bladder, the stomach and, to a less extent, the intestines are more liable to be ruptured when distended. Ruptures of the stomach or intestines are seldom attended with much hemorrhage, while wounds may occasionally cause a serious and fatal hemorrhage from the wounding of a large blood-vessel. The principal danger lies in the leakage of the contents of the stomach and intestines, which almost always sets up a septic peritonitis. This may sometimes become localized and go on to spontaneous cure, though as a rule it becomes general and is fatal. In such cases early operation may avoid the fatal peritonitis. A punctured wound may be so small as to be closed by the mucous membrane, avoiding the escape of the contents of the gut. Or a wound may not entirely penetrate the wall of the stomach or intestines, which only gives way some days, perhaps, after the injury, though the injury is entirely responsible for the delayed result. These injuries are sometimes fatal immediately or very speedily from shock, while in other cases of very extensive injury there may be almost no shock, and the victim is aware of no serious injury. It is an important point to remember medico-legally that spontaneous rupture of the stomach or intestines may occur owing to ulceration due to disease. This can be determined by a careful examination of the wall of the stomach or intestines at the site of the rupture. A slight injury may also cause rupture if the wall of the gut is weakened by disease, as the disease causes greater liability to rupture. Here too it is to be remembered that a severe injury causing rupture may leave no mark of violence on the abdominal wall. The power of walking or other muscular exertion after such injuries of the stomach or intestines is not infrequently preserved, as recorded in numerous cases.[683] The prognosis in such injuries of the stomach and intestines is always extremely grave.
Incised, Punctured, and Contused Wounds of the Genital Organs.
These are not common as medico-legal cases. Self-castration or mutilation is sometimes practised by lunatics, idiots, or even intoxicated persons. Thus a man who, while intoxicated, cut off his genital organs and died the next day from the effects of hemorrhage was seen by Demarquay.[684] Circumcision in infants is also sometimes fatal from phlegmonous inflammation.[685]
Incised, lacerated, or contused wounds of the female genitals may be fatal from hemorrhage from many small vessels. Deeply incised wounds of the female genitals proves wilful and deliberate malice; accident is out of the question and suicide is improbable in such cases. But we sometimes have to determine between accidental, self-inflicted, and homicidal wounds of these parts, as accidental wounds may occasionally resemble those made by design and so may furnish more or less difficulty, unless all the circumstances are known. Thus Taylor[686] relates the case of a child in whom a sharp-pointed stick entered and passed through the posterior wall of the vagina as she fell from a tree. The stick was removed by a woman, and the child died in a little over a day from peritonitis. Unless the circumstances were known, this case might have caused suspicion of homicide.
Lunatics, idiots, and drunkards sometimes inflict on themselves wounds unlike ordinary suicidal ones. In other cases the various points we have enumerated in a previous section to distinguish between suicide, homicide, and accident may be applied to solve the case.
Contused wounds, such as kicks, etc., of the female genitals may be fatal from hemorrhage due to the laceration of the parts.[687] Like the wounds of the eyebrows, contused wounds of the vulva may sometimes resemble incised wounds owing to the sharp bony surfaces beneath. Careful examination allows a discrimination to be made from incised wounds. If hemorrhage occurs[589] a long time after the alleged violence, it is probably due to natural causes, especially in cases of metrorrhagia, etc. It may be alleged in defence that contused wounds of the female genitals were inflicted post mortem, but besides the other features which we have already seen help to distinguish between ante-mortem and post-mortem wounds, we may add that kicks and other contusions of the vulva, if fatal, are so from hemorrhage or effusion of blood, and no post-mortem hemorrhage is enough to cause death.
INCISED, PUNCTURED, AND CONTUSED WOUNDS OF THE EXTREMITIES.
These may be fatal if a large blood vessel or vessels are opened, or sometimes if a compound fracture or wound of a joint becomes infected. They may also in some cases be fatal from shock, from the severity of the injury. As a rule they are the cause of civil suits, not of criminal ones. The various injuries may cause disability for a longer or shorter time, or even permanently, and more or less deformity may also remain. This may be the case with fractures, especially if they occur near the joints, in which case great caution should be exercised in giving an opinion or prognosis. It is a common mistaken idea of the laity that a fractured or dislocated limb can be made in every case as good as before the injury. On the contrary, they not infrequently leave a slight deformity and impairment of function, sometimes even under the best treatment. Dislocations may also leave a lasting disability or weakness, often owing to the carelessness of the injured person.
Wounds of an artery or vein, or both, may result in an aneurism or an arterio-venous aneurism. Wounds of nerves may cause paralysis and anæsthesia of the parts supplied. Wounds of muscles or tendons may cause weakness or complete loss of motion of particular joints. Wounds of the soft parts, if infected, may lead to cellulitis and phlegmonous inflammation, which may result in much injury. Wounds of joints, if penetrating, are serious, for without the proper treatment they may result in suppuration in the joint, disorganization of the joint, and final ankylosis. Before the use of antiseptic treatment such wounds were not uncommonly fatal. Fractures,[590] simple or compound, or contusions of bone especially in young subjects, may be followed by osteo-periostitis and its consequences, which may require a long time for recovery after the fracture is entirely recovered from, and a still longer time before the limb can be used. These and many other of the various results of wounds and injuries of the extremities, causing deformity or disability, or both, can often be cured or improved by surgical treatment or operation.
THE MEDICO-LEGAL CONSIDERATION
OF
GUNSHOT WOUNDS.
BY
ROSWELL PARK, A.M., M.D.,
Professor of Surgery in the University of Buffalo; Attending Surgeon to the Buffalo
General Hospital; Fellow of the German Congress of Surgeons; of the American
Orthopædic Association; of the American Genito-Urinary
Surgeons’ Association; of the New York Academy
of Medicine, etc., etc.
GUNSHOT WOUNDS.
GENERAL CONSIDERATIONS.
Few medical men there are who have long engaged in practice who have not been compelled to take part in some medico-legal controversy in cases of accidental or alleged homicidal gunshot wounds. So soon as death occurs the surgeon ceases to work as such, but may continue to work as a medical jurist, and in preparation for this event must be ready to answer any questions bearing upon the case which, though possibly ridiculous in surgery, are or may be necessary in law. He may be called upon to testify as to the precise nature of a wound inflicted upon the body of a man seen before or after death; as to the means by which it was inflicted; whether the purport was suicidal or homicidal; how much blood was lost; whether the weapon was near to or at a distance from the body when fired; whether it were possible that the deceased could have fired it himself; whether after the reception of the wound the person could have moved or performed any act—in other words, whether death was instantaneous. He may be asked also as to genuine or spurious blood-stains, whether genuine blood-stains were human or from some other animal; whether possibly they were from the body of the deceased. He will be expected to tell from what direction the bullet or missile was fired; which the wound of entrance and which of exit, and many other things possible concerning the circumstances under which death occurred. It is unnecessary to state that questions of this nature call not only for conventional surgical skill, but for the highest degree of shrewdness and general information, as well as sometimes for expert knowledge with regard to small-arms and their ballistics.
It has been well said that the first duty of a medical jurist is to cultivate a habit of minute observation. When this is combined with a knowledge of what the law requires and with the[594] results of a technical education, he will be able to meet all or nearly all of the scientific questions which may be asked of him. A learned judge once said that “a medical man when he sees a dead body should notice everything.” Certainly he should make a minute scrutiny of the body to note whether there are upon the dress or hands of the deceased marks of blood, or whether blood-stains are noted in different parts of the room; whether the body or any part of it is cold or warm; whether the limbs are cold or rigid or pliant, since by these means the accurate date of death may be more accurately determined.
EXAMINATION AND DESCRIPTION.
In determining facts attending a suspicious case of gunshot wound, there should be noted, if known, 1st, the exact time of death, as well as of infliction of the wound; 2d, location and attitude of the body; 3d, condition of clothing; 4th, anything of importance in its environment; 5th, external appearance of the body, as well as state of countenance; 6th, exact description of all marks of violence and of blood-stains; 7th, the presence of cadaveric rigidity and the surface upon which cadaver has been lying, as well as its age and condition of general nourishment; 8th, time when deceased was last seen alive or known to have been alive; 9th, time after death at which examination is made; 10th, all physical circumstances corroborating or arousing suspicions of suicide or homicide; 11th, account of an accurate internal post-mortem examination, in which direction of the bullet or missile is noted, along with a careful description of parts disturbed or injured in its course, large vessels or nerves cut across, effusions of blood, and in every way as accurate a description as possible of the exact damage done. To this also should be added a minute scrutiny of other parts, in order to establish clearly that death was due to the alleged injury, or on the other hand that it may have resulted from natural causes, and that the injury in question was only a consecutive and contributing cause. Especially should there be examined those organs in which occur the most common causes of death, namely, the brain, the heart and great blood-vessels, and the viscera. Moreover, if an operation has been performed the post-mortem examiner should be prepared to speak with reasonable[595] positiveness as to whether said operation was, in the first place, necessary if life were to be preserved, and, in the second place, whether death were due to the injury proper or to the attempt to save life thus made necessary. For the determination of all this, obviously the best time for the performance of the examination is the earliest possible moment after death. Nevertheless, bodies are sometimes exhumed for this purpose, and much information is obtainable even after a considerable interval of time.
If death has been caused by a bullet which has not passed through the body, but lodged, it should by all means be obtained, since evidence of the greatest value may inhere in it. Moreover, in first noting the position of the body, the direction of the wound, or the location of a blood-clot upon the floor or clothing or elsewhere, may indicate to the surgeon or other astute person the point at which the bullet may be found concealed or buried in some soft or hard object. This bullet should be recovered, if possible, at all events, although if taken from the body itself the evidence it conveys may possibly weigh more heavily than if removed from some object outside the body. The exact number of gunshot wounds with a minute description and location of each should be committed to paper at once, as well as any statement, if at all reliable, concerning the number of shots fired, since valuable deductions may be reached as to the number of bullets which have passed through or which have lodged within the body. It is well sometimes, also, before dissecting out the bullet-wound, to insert first a stiff and then a flexible probe or something which shall, if possible, follow the bullet-track, since occasionally a question comes up of the direction in which it was fired. Even though surgeons well know that such questions are impossible of satisfactory answer, owing to the manner in which a bullet is diverted in its course by the various tissues of the body, it will nevertheless create a good impression as to the thoroughness and exactness of an examination should it be brought out, in answer to questioning, that this had been done. Many an excellent surgeon has been surprised upon the stand by the question from one of the counsel as to whether he knew that some certain writer had stated that it was always well, in trying to determine the course and direction of a bullet, to put the patient or the body, as the case might[596] be, in the exact position in which it was when the shot was fired, providing this be known. The accomplished surgeon knows that this is a matter of very trifling import, but the witness’ status will be much better established with the jury if he can show himself familiar with this possible method of examination.
When a suspected person is brought before a magistrate, accused of homicidal attempt, it is very likely that the judge will require a written statement or opinion from the surgeon in attendance as to the extent and danger of the victim’s injuries, and especially as to whether these are of a character dangerous to life. The meaning of these words is left entirely to the sagacity of the surgeon. A mere naked declaration of this fact is insufficient. He must, if called upon by the court, give his grounds for his belief, and these may be rigorously examined by counsel. He will also probably be asked as to the presumable duration of life and possibly the effect of operation. Thus the prisoner’s immediate liberty or restraint may depend upon the surgeon’s words. Perhaps the only advice which can be offered here is to qualify between injuries directly dangerous to life and those in which life is endangered merely by possible complications, such as sepsis, gangrene, etc. Still, aside from wounds which are either fatal or may be nearly completely recovered from, there is another quite large class of those causing grievous bodily harm in which it is a question for the jury always to decide what was the intent of the accused. A medical witness may thus in such a case be of great assistance to the court by giving an account of the injury devoid of technicalities, and of its possible consequences. It should also always be stated, if known, whether the patient was under the influence of liquor or any narcotic at the moment of injury.
In the examination of wounds either of the living or dead body, it should always be determined for medico-legal purposes whether there is about them fluid or coagulated blood or ecchymosis, that is, livid discoloration of the skin from effused blood. The color of the ecchymotic spot will give a valuable clew as to the time between the infliction of the wound and death. Putrefaction of such a wound must not be mistaken for gangrene. In giving reports on such cases care should be taken to distinguish between facts and inferences. In fact,[597] the inferences had better be kept unreported or confined to a separate statement.
Should there be any possible suspicion of a combination of poisoning and gunshot wound, the stomach contents should be carefully preserved and sealed up in the presence of witnesses before turning over the same to the analytical chemist, whose receipt for the package, with a careful description of the same, will probably have to be placed in evidence. Any fact on the condition of the stomach with regard to digestion is always worth noting. In the case of Reg. v. Spicer (Berks Lent Assizes, 1846) a most important point hinged on the examination of the stomach. The body was found at the foot of a stairway. The prisoner stated that after he and his wife had had their dinner he heard a fall. The woman had died instantaneously and the death occurred about the dinner-hour. Upon examination the stomach was found empty, without a trace of food. It was, therefore, clear that a part at least of the prisoner’s story was untrue.
Evidence as to whether the wounds were superficial or deep may be of value. If the edges are swollen or large, or if granulation or cicatrization have commenced, it is evident that the person must have lived some hours or some days after their reception. The same is true of suppuration, adhesion, or gangrene. It must also be remembered in this connection that very few gunshot wounds will show much change in less than ten or twelve hours save that due to the extravasation of blood. Should the question come up as to whether a gunshot wound had been inflicted before or after death, we may remember the principal characteristics of a wound inflicted during life, which are more or less eversion, more or less hemorrhage with diffusion of blood into the tissues, and the presence of clots. In a wound made after death little or no blood is effused, unless it come from some vessel very near the surface, in which case it will be venous in character and will not coagulate as does that which is poured out of a wound in the living. The track of the bullet also will not be found filled with coagula. In these respects a little will depend upon whether the body has lost its animal heat or not. The gunshot puncture of a divided artery in a dead body will present a very different appearance from one inflicted before death, even though it be the cause of death.[598] Bleeding after death is exclusively venous, and there does not occur extravasation of blood in the cellular tissues, nor does it coagulate. Questions of this character come up sometimes in the case of multiple wounds or injuries, and it is, at times, of importance to be able to determine whether the assault or injury has been continued after death. Changes in color of an ecchymosed spot rarely begin until after the expiration of twenty-four hours, when its dark margins become lighter, and as time goes on the whole area passes through successive shades of violet, green, and yellow; its area may also increase sometimes to remarkable proportions, but the central portions are always darker than the periphery, the darkest spot corresponding to the centre of violence. Ecchymosis is longer in disappearing in the old than in the young. Its various features also will vary a little in accordance with the tissues bruised.
Gunshot wounds pertaining to spurious suicidal attempts are usually found not to involve vital parts, while they will have most of the characteristics of injuries inflicted from a weapon near at hand. The skin or the clothing will show powder-marks, and if a wad is a feature of the cartridge used, it may be found in one place or the other. In these cases there is also relatively more laceration and bruising, while sometimes the hand which held the weapon may be blackened or burnt by the discharge of the same. Self-inflicted wounds, in other words, must necessarily partake of the character of near wounds.
EVIDENCE FROM THE SITUATION OF THE WOUND.
It has been generally noted that suicidal wounds are for the most part confined to the front or lateral parts of the body; gunshot wounds of this character being found usually in the region of the heart, the face, and the temples. The presence of an injury to these parts is not necessarily indicative of suicide, but the existence of such injuries in other parts of the body is at least negative evidence of homicidal attempt. Moreover, Orfila has observed that it is not so much the situation as the direction of the wound which gives evidence for or against the presumption of suicide. The question has been raised whether it were possible to have a gunshot wound without external evidence. There has been recorded more than one case where a[599] bullet entering through the open mouth has penetrated the brain without passing through the vertex of the skull and has killed instantly without leaving any external mark.
It is very necessary to establish, if possible, the direction of such a wound, and this may be coupled with a knowledge of the right-handedness or the left-handedness of the person who inflicted it, or may shed light in this way upon some personal peculiarity which may lead to the detection of the guilty person. Thus it is said of Sir Astley Cooper that in one instance he remarked that a certain wound could not have been inflicted except by a left-handed person, and that his observation led to the detection of the murderer. It has been stated that for the detection of the weapon or instrument used it should be placed first in one hand of the deceased and then in the other, while the other extremities are so manipulated that it may be clearly determined whether suicidal attempt were possible or no. There is ordinarily little difficulty experienced in distinguishing suicidal from accidental wounds. In the former case extraneous signs and circumstances point more clearly to the intent of the deceased than do, perhaps, the peculiarities of the wound itself. This is to be settled mainly by the evidence of those who find the body; in other words, by circumstantial evidence.
In suicides ordinarily one wound only is met with. At any rate, probably one only that has destroyed life. Consequently the presence of several wounds, each of which was necessarily fatal, constitutes almost conclusive evidence of murder, the strength of the same depending upon the necessary fatality of more than one of these. Thus it is hardly conceivable that a suicide should shoot himself through the heart and through the brain; the coexistence of two such wounds would be almost conclusive of homicide. The existence of multiple wounds is a rather strong presumption of insanity or drunkenness of the person who inflicted them. Men who kill when under the influence of liquor not infrequently inflict injuries enough to be several times fatal.
The coexistence of wounds made by cutting weapons, as well as firearms, is not unknown. These are occasionally suicidal, ordinarily they betoken murderous attempt. If suicidal the deceased will ordinarily be found to have been a lunatic.
But evidence is to be obtained also from signs and circumstances[600] separable from the wound itself. Thus the position of the body may be such as to invalidate the theory of accident or suicide. The position of the weapon, too, is something to be noted with great care. Whether, for instance, this be firmly held within the hand of the corpse, or whether it had been simply placed there after his death; whether it be found where it would seem to have been most naturally dropped after its discharge, or found somewhere where it could scarcely have been placed or thrown by the deceased; whether it be found at such a point that it is clearly evident from other signs it could not have been dropped by the deceased, since death must have been caused too quickly for him to have traversed the intervening space.
EVIDENCE FROM THE WEAPON AND PROJECTILE.
Evidence of great value may be obtained often from the weapon itself. First of all, from the position in which it is found, as stated above; second, from a careful examination of itself. It should be noted whether there be any blood upon it, and whether this be so fresh as not to have caused any rust; whether it may possibly be so smeared with blood as to indicate a hand-to-hand conflict; or whether any part of the weapon may have been used as a club or bludgeon, as would be shown by the presence upon it of hair entangled in dry blood. When such blood is removed from the weapon it should be carefully examined with the microscope, since from the detection and identification of hair or fibres of fabric evidence of the greatest value may be adduced. Next it should be ascertained whether a weapon shows signs of having been recently discharged or whether it be evident that it could not have been so, and such determination of the time element as may be afforded by a study of this kind should be contrasted with that made after a study of the wound. If the weapon be a revolver or a repeating arm of any kind, it should be determined if possible how many cartridges or bullets have been fired, and whether at or about the same time, and this information should be compared with the evidences obtained from the body and from the room or locality in which the suicide or murder occurred. If, for instance, it be determined that three cartridges have been[601] fired and but two bullet-wounds are found in the body, an examination of the room may show where went the third bullet. Next the calibre of the weapon should be noted and the weight of the ball which it discharged and its dimensions should be compared with any which may be found in or about the body. The weight of the bullets attached to cartridges of various sizes and makes is usually stamped upon the packages in which they are sold, or can readily be obtained from the makers of the same. A bullet taken from a body weighing after its removal more than do the other bullets undischarged in the weapon by which an injury is alleged to have been inflicted is rather presumptive evidence against the injury from that source.
Can a Bullet Lose in Weight between the Time when it Leaves the Bore of a Gun and its Discovery in a Body?—Here springs up a question upon which some very interesting evidence has been adduced in different trials. To discuss this matter completely the question should be divided into two, the first being:
Does a Bullet Suffer Loss of Weight during its Course through the Piece and the Air before it comes in Contact with the Body?—A personal letter received from Captain Charles Shaler, of the Ordnance Department of the United States Army, in reply to certain questions, tends to fully settle that a lead bullet suffers a certain loss of weight in the barrel due to the friction between the bullet and the bore; this is known as “leading” and varies according to circumstances. “Patching” the bullet is often resorted to in order to reduce the leading; lubrication is also practised. The fusing of a bullet takes place especially with lead bullets. A ball which has been partly fused in the bore will lose the fused portions in the bore or in flight, and will move irregularly on account of the resulting irregularity of form. A .45-calibre, 500-grain service bullet, lead alloyed with tin, was weighed without lubricant and was found to weigh 500.5 grains. It was then lubricated in the cannelures and was fired into a butt composed of three barrels placed end to end and filled with sawdust. Tho bullet was recovered, no lubricant being found in the cannelures, and re-weighed, the weight obtained being 485.5. The loss of weight was, therefore, 15 grains or three per cent, some of which may have been due to the bullet penetrating the sawdust. A German-silver[602] “jacketed” .30-calibre bullet, weighing before firing 231 grains, fired without lubrication, when recovered and re-weighed was found to have suffered a loss of weight of one-half grain or one-quarter of one per cent. The other part of the main question is:
Does the Bullet Lose in Weight in its Course through the Body?—This is, of course, intended to pertain only to those instances in which there is no evidence of splitting or division of the bullet, and refers only to the effect of friction or attrition. June 5th, 1878, in Saratoga County, Mrs. Jesse Billings was accidentally killed by a bullet. Her husband was arrested and tried for murder. On the first trial he was acquitted. A second trial, however, was held, and some very interesting expert testimony was brought out on matters pertaining to these questions. The medical evidence is published in full by Dr. Lewis Balch, of Albany, in the Transactions of the Medical Society of the State of New York for 1881. The rifle from which the bullet was supposed to have been fired was found in a well, and was sworn to have belonged to Jesse Billings. In it was found a cartridge of the type known as the Commercial Long No. 44. This gun became an important factor in the case, and most of the evidence as to whether it was the weapon with which the murder had been committed was referred to the medical experts. The defence in the first trial claimed that all the lead fired was found in Mrs. Billings’ head. On the second trial the same claim was not made, but that it was a smaller bullet than a .44 and its weight less than 220 grains; that in consequence this rifle could not have been that from which the shot was fired, for it only called for a .44 ball, and that it would have thrown a bullet with such force that it must have gone entirely through the head. They further claimed that powder-marks and grains of powder were found in the window-sash, showing that the weapon was fired near the window, and that the hole in the glass was not large enough to admit a full-sized .44 ball. The verdict was mainly won upon these statements. A question for the medical experts to answer was, what would be the effect upon the skull of a .44-calibre ball fired from a Ballard rifle, the ball weighing 220 grains and the charge of powder being 28 grains? also what would be the effect upon the ball? Experts from the Ordnance Corps and[603] from the rifle factories were able to testify that the bullet found in Mrs. Billings’ head was originally a .44-calibre ball; also that its markings showed the peculiar left-handed twist used in rifling this particular arm. The defence maintained that it could not have been a .44, claiming that the hole in the window-pane showed that. The original window produced in court was no criterion, since from repeated handling the hole made by the bullet had become enlarged and changed in shape. Both of the experts for the defence believed that the ball could not make a hole smaller than itself when passing through glass. This necessarily supposes that the ball after being fired is the same calibre as before, which, as shown above, is not always the case. So Dr. Balch fired forty-five rounds from the Billings rifle with 220 grains of lead and 28 grains of powder. The shots were fired through glass set in sashes, the glass being 28×13¼, double thick and American make. The rifle was discharged at varying angles and at distances varying from two to seventy feet, and he obtained one shot where the hole made would not admit a full-sized ball. His summary was as follows:
| Balls unable to pass through | 1 |
| Balls partly passed | 3 |
| Balls passed | 18 |
| Cartridge passed | 21 |
| Glass broken out | 2 |
| —— | |
| Total | 45 |
Other rounds were fired from a Colt’s navy revolver, old style, .36 calibre, at distances varying from ten to twenty feet. The holes made were so large that the barrels and ramrods could be passed without touching. The examination of the one instance noted above where the aperture in the glass was smaller than the ball is explained by Balch as follows: “A ball conoidal in form, passing with great velocity, strikes glass, penetrates, but does not break the glass at the point of entrance. The point struck is instantly disintegrated, and so rapid is the stroke that it has not time to call upon the surrounding particles for support; hence the smallness of the hole. As glass is made it varies in elasticity; some parts which are to be cut into panes cool faster than others. A bullet striking the portion of the glass which has cooled quickly strikes an object which will[604] yield somewhat to the force; in doing this a hole will be made smaller than if that more brittle had been struck. Furthermore, all rifles taper more or less from breech to muzzle, that is, the muzzle will measure one or more thousandths or hundredths less than the breech. The bullet being forced through the narrow aperture yields to the pressure and becomes smaller. The gun under consideration was measured at the New York Armory, and found to be .44 at the breech or chamber and .423 at the muzzle. Considering these various facts, statements that a ball of known size will make a hole through glass smaller than the size of the ball when fired do not admit of doubt as to their verity. Some statements bearing on this same point contained in a recent letter from Captain Shaler, of the United States Army, deserve mention here. The following experiment was made in Washington by Captain Lyon in October, 1880:
“Noticing a statement in a newspaper to the effect that a ball fired from a rifle would, in passing through glass, make a round hole smaller than the diameter of the ball used, the following experiment was made:
“Service ammunition used, in a calibre .45 Springfield rifle to penetrate glass.
| Time Fired. | Size of Hole made in Glass, inches. |
Remarks. |
| 1 | 0.570 | The frame holding the glass was placed 25 yards from the muzzle of the gun. |
| 2 | 0.550 | |
| 3 | 0.600 | |
| 4 | 0.600 | |
| 5 | 0.575 | |
| 6 | 0.575 | |
| 7 | 0.590 | |
| 8 | 0.620 | |
| 9 | 0.600 | |
| Average size of hole | 0.586 | |
| Calibre of bullet | 0.458 | |
| ——— | ||
| Difference | 0.125 | |
“From the above it will be noted that there is no uniformity in the size of the holes and that they all exceed the diameter of the bullet.
“These experiments were supplemented by some made recently in which a sash containing six panes of ordinary window-glass[605] was placed at twenty-five yards from the firer and the glass was successively penetrated (a separate pane being used in each case) by bullets from a service .45-calibre Springfield rifle, a .30-calibre Springfield rifle, a .45-calibre Colt’s revolver and a .22-calibre revolver. In every case the hole made was much larger than the bullet making it.”
With reference also to the effect of a ball being smaller than its original diameter after it leaves the piece, Captain Shaler states: “All very compressible bullets forced by inertia lose a certain amount even though they also gain force by slugging. Forcing by inertia tends to shorten the bullet and increase the diameter, while slugging tends to lengthen the bullet and reduce its diameter. Whether the bullet is smaller after it leaves the piece depends upon the bullet used and the method of forcing employed.”
To return to the Billings case, it was claimed that the bullet was also too small. It weighed 165 grains, 55 less than when it was fired from the rifle. Balch found in firing at human skulls, the subjects in all the trials but two being placed in a sitting posture, sometimes with a sash like the Billings window in front of the subject, that the ball lost lead in accordance with the resistance it met with and the amount of bone ploughed in its passage. These experiments conclusively prove that the weight of a ball taken from a body after being fired, it having traversed a bone in its flight, is by no means evidence of its weight before firing; in other words, a ball always loses some lead when passing through bone. With the same rifle as that produced at the trial he made a series of experiments in the dissecting-room, endeavoring to make a bullet enter the skull at the same point and in nearly as possible the same direction as in the case of the murdered woman. In six such experiments there were varying losses of lead, all the bullets used being the same general weight. In two trials the distance was but ten feet from the muzzle, yet more lead was lost than in any of the other four. The least loss recorded took place at the longest distance, thirty-five feet. This in part accounts for the loss of lead, for at ten feet the bullet has not acquired its greatest penetrating power, for he showed by experiment that a 220-grain bullet fired at a human skull will lose more lead than was missing from the Billings bullet, thus disposing of[606] the question raised by the defence that a ball could not have weighed 220 grains before being fired.
Just how to account for the missing lead has never been clearly established. We have to remember that a few grains may be left in the bore of a rifle, especially if rusty; that in passing through glass another portion is lost, and finally it is scarcely conceivable that any bullet should penetrate an adult skull, especially in the neighborhood of the mastoid processes, without losing quite a perceptible percentage of its mass by friction.
It was also claimed by the defence that the ball taken from Mrs. Billings’ head had been fired from a weapon of low velocity, which was held to account for the fact that the ball failed to pass out of the skull. The rifle when tested at the Government Arsenal showed a mean velocity of 999 feet per second. Had it been as high as was supposed by the defence, namely, 1,300 or 1,400 feet, the argument that a bullet driven with this force would always go through the skull would have more weight, but with the velocity found by actual test the energy of the ball was lessened to nearly one-half of that supposed. The bullet which killed Mrs. Billings did not pass entirely through the skull. It ploughed into the opposite side and broke before it a triangular piece of bone which broke the skin externally. This shows the resistance of external fascia against perforation. A study of the lines of fracture in this particular case proved very interesting, but perhaps would be somewhat irrelevant here. A measurement of the skull and of the bullet-track through it shows the former to have been of more than ordinary thickness and density, and the channel ploughed in the bone by the bullet along the base of it to have been nearly two inches in length. Dr. Balch gives the following conclusions to his very interesting evidence: 1st. A leaden ball passing through bone loses lead in proportion to the amount of bone traversed. 2d. If the petrous portion of the temporal bone be the part struck by the ball and struck squarely at the base, that portion of the bone is crumbled or broken in such exceedingly fine pieces as to defy restoration. 3d. That if the ball struck any part of the skull the petrous portion will be broken, but can be usually recognized and generally put together again. 4th. That a ball of given calibre fired through glass may make[607] a hole enough smaller than the full size of the ball before firing to prevent an unfired ball of like calibre passing.
In all this kind of experimentation upon cadavers for the purpose of eliciting evidence by reproducing as nearly as possible ante-mortem injuries, we must not forget that Casper has strongly insisted that “it is extremely difficult to break up the organic cohesion of dead organs.... If we endeavor to fracture the skull of a dead adult we shall find that an amount of force which if applied in life would indubitably produce fissures if not fracture, or complete crushing of the skull, leaves the dead skull quite uninjured.... The most powerful blows struck down upon the body, laid down horizontally, were without result, and only after repeated violent blows were we able to produce perhaps one or a few fissures in the occipital or parietal bone, or in the temporal bone (squamous portion), and usually in the latter. We were unable to produce more considerable effects, such as complete smashing of the skull or fissures of its base, even in one single instance. The dead skull seems to have considerably more power of resistance, and after its removal fissures of the bone were more easily produced by similar blows” (Vol. I., p. 245). And again: “The result of my experiments on the dead body in regard to gunshot wounds could only be to make more complete the proof of the resistance of the dead corporeal tissues, in contradistinction to the tissues when alive. After I had already learned this peculiarity from my experiments with contused wounds, this peculiar resistent property was found to be confirmed in a most remarkable manner” (“Forensic Medicine,” Vol. I., p. 271).
If the number of bullets known to have been fired, or, more important still, which have been found exceeds the number which could have been discharged from the weapon in question, a very large element of doubt and uncertainty is introduced which must be quieted by other and more circumstantial evidence. Should two different weapons be in question, it is very necessary to establish from which of them the bullets have been discharged. This can be done mainly by weight and evident calibre of the bullets, or some other peculiarity; possibly in disputed cases even by analysis of the metal.
Wounds by Shot-Guns.—In most of what has been said it has been supposed that the injury has been inflicted by an[608] arm of the kind commonly described under the terms pistol, revolver, or rifle. Gunshot wounds are, however, occasionally inflicted with shot-guns and a charge of shot varying in size from small bird-shot up to that generally known as buck-shot. It is characteristic of such missiles that they separate after their discharge from the gun, and a determination of the degree of their separation is approximately a determination of the distance of the mark from the muzzle of the weapon. In suicide or accidental discharges of a shot-gun the muzzle is so near the body that the charge of shot acts very much as would a single bullet of the size of the bore of the gun, and near wounds thus inflicted, while necessarily large, have about them a minimum laceration and disturbance of tissue, so that perhaps only by their size could one say, viewing the wound alone, that the weapon used had been a shot-gun. On the other hand, at a distance of a few feet the shot begin to separate to such an extent that there is much more laceration of tissue, and after separation to an indeterminate, because variable, number of feet we get such marks as individual shot may make. This distance is indeterminate because it is predicated on the size of the gun, the dimensions of shot, and the weight of the charge of powder. The writer, for instance, has recently seen one case where the muzzle of the gun could not have been more than two feet away from the surface of the foot at which it was discharged, the consequence being a round and very slightly ragged hole through the mid-tarsal region from dorsum to sole.
It is possible for a single grain of shot to produce death. Such a case is related by Ollivier d’Angers: a thief scaling a wall received at a distance of fifteen paces a charge of shot from a fowling-piece; he fell dead immediately. The charge had struck him in the breast, centring over a space of three or four inches, but one shot had penetrated the aorta over the attachment of the sigmoid valves, and another had traversed the entire wall of this vessel.
Powder-Marks.—A very important part of evidence in case of near wounds of gunshot character pertains to the powder-marks upon the clothing and skin. Naturally every one knows that when a weapon is discharged near a given surface there will be more or less powder-marking upon that surface, the same being due to particles of gunpowder which are incompletely[609] or not at all consumed, and which are black because of the charcoal they contain; but the circumstances under which powder-marks of a given character can be inflicted are so extremely variable that no statistics or information of value in a general way can be given. Thus the fineness of the marks will depend upon the fineness of the powder, and the area covered and the depth of the marking upon the same, upon the distance of the muzzle from the surface; and the only way to make out the exact distance of the muzzle from the surface at the time of the infliction of a given wound is to use the same weapon, if possible, with cartridges or charges out of the same lot as that used at the time of injury. Distances could, perhaps, be stated in round numbers, but their value would only be remotely approximate, and in a given case the best evidence is to be obtained by experiment with the fire-arm in question.
Dimensions of Perforations.—At different times a great deal of weight has been attached to the dimension of the perforation through such objects as wood, glass, or even through the bones of the body, made by the bullet which is supposed or known to have destroyed life. Wrong inferences have been drawn sometimes from a study of undischarged bullets or cartridges similar, at least before firing, to that which has been taken from a given body. It has been stated, for instance, that such a bullet was too large to have passed through such an aperture or to have made such a hole, or that it was so much smaller than a certain hole that it was not the particular missile which made that perforation. Upon this matter has hinged a great deal of uncertainty and consequently a good deal of study. The size of opening which a bullet of given calibre will make through wood depends upon the distance of the weapon, the firing charge, the velocity of the bullet, the extent to which its shape has been altered by passing through the given barrier, by the heat of the explosion, by the impact of the air upon the heated and consequently softened metal, and by the density and thickness of the wood, as well as by the resistance which it may have offered mainly from its being fixed in place or movable. There is, however, ordinarily less question about the size of a similar hole through a piece of glass or bone. It is generally supposed that a bullet passing through a window-pane will shatter it. This depends, however, mainly upon the perfection[610] of fixation of the glass in its resting-place. If for purposes of experiment panes of glass be tacked into a shutter and bullets be fired at them from varying distances, they will be practically invariably shattered. It is, however, quite different if the pane of glass be firmly fixed in a frame by means of putty which has become old and hard, and especially if the window-frame itself be closely fitted in the casing. Under these circumstances a bullet will often make a clearly punched hole, or one with very few radiating lines of fracture. Experiment, therefore, to secure evidence should be made under circumstances exactly parallel to those which necessitate such evidence.
EVIDENCE FROM EXAMINATION OF THE DEAD BODY.
Fractures.—Considerable evidence of great interest with respect to the effect of a bullet-wound upon the skull and the possibility of fractures being produced at the base by contre coup will be found in the statement of the case of The People v. Elisha B. Fero, published by Dr. Charles T. Porter, of Albany, in the Journal of Psychological Medicine, April, 1870. Mrs. Fero was murdered while in her bed and was found to have been bruised about the head and body, her husband claiming that the deed was that of a robber who had attacked them both. He was found with slight bruises or scratches about the face and black marks as if from burnt powder between the middle fingers of his right hand. The first autopsy appears to have been carelessly made, but a flattened conical ball weighing twenty-six and one-half grains was found lodged in the middle of the right cerebral hemisphere. It had not gone completely through the brain. Its base fitted the shells of the metallic cartridges used in Fero’s revolver. Eight days after death a second examination was made, after which the head was removed and preserved in 95% alcohol. A theory of the prosecution was that Mrs. Fero was murdered by her husband; that he shot her, as well as struck her numerous blows upon both sides of the head and its front and back with some broad, heavy, and elastic body, making fractures found on autopsy. Not the least interesting part of the testimony is that referring to the condition of tissues alleged to have been bruised after long[611] preservation in alcohol. The expert testimony in this case appeared to show that such fractures as were found, without reference to the fact of external bruises, were due to the unskilful manner in which the skull-cap was removed. In this connection it is well right here to emphasize the fact that fresh fractures can be produced in the skull by too forcible or injudicious efforts to remove the calvarium when making autopsies, or that fractures previously existing can be extended or complicated in the same way. Shaw in his “Manual of Anatomy” says: “The question whether there has been a fracture of the cranium previous to death is sometimes more difficult to decide than a person not accustomed to make dissections might imagine. If the fracture has occurred immediately before the patient’s death, there will be found coagulated blood upon the bones and in the fissures. If the patient has survived for some time, there will be marks of inflammation and, perhaps, pus in contact with the skull, but if a fracture has been made in making the examination, which sometimes happens in even very careful dissectors’ hands, the blood in the fracture will not be coagulated, nor will there be any effusions around the portions. In Beck’s Medical Journal, Vol. XXII., p. 28, Mr. Alcock some time since stated in a public lecture in London that he had known a fracture of the base of the skull produced by the awkward and violent tearing of the upper portion by the saw in penetrating enough to divide the bones, and this to be mistaken by the inexperienced operator for fracture of the skull producing death. Being a medico-legal case, it might have led to melancholy consequences had not the error been detected by an observer.” That an extensive and often complicated fracture by contre coup can occur as the result of gunshot injuries of the skull is a fact well known to all surgeons of experience and laid down in all text-books and illustrated in all large museums.
In view of these well-known facts, it would always be well to insist in cases of this kind that the saw alone should be used and not the hammer nor the chisel. When a cranial bone is fractured blood is poured out from the ruptured vessels, as is always the case with any bone. Its amount varies indefinitely with the number and size of the ruptured vessels, the activity of circulation, the length of time a person lives, etc. The blood may collect in circumscribed masses or become infiltrated in[612] the surrounding tissues, although usually both phenomena are observed. The extent to which infiltration takes place depends upon the quantity of blood and the nature of the surrounding tissues. In loose tissues like those about the orbit infiltration is much more rapid and extensive.
Examination of the Weapon.—French medical jurists have tried to indicate how we may determine the time elapsed between the death of a person and the discharge of a weapon found near the body, but exact statements in this matter are utterly out of the question. Certain facts bearing on the subject are these: When recently discharged there will be found adhering to the barrel of the piece and consisting of the fouling of which sportsmen complain, a quantity of potassium sulfid mixed with charcoal. This is shown by its forming a strong alkaline solution with water, evolving an odor of hydrogen sulfid, and a dark precipitate with a solution of acetate of lead. Depending upon the degree of exposure to air and moisture, after some hours or days this sulfid becomes converted into potassium sulfate, which forms a neutral solution with water and gives a white precipitate with acetate of lead; but if a considerable time has elapsed since the discharge of the piece oxid of iron (iron rust) with traces of sulfate may be found (Ann. d’Hygiene, 1834, p. 458; 1837, p. 197; 1842, p. 368).
Was the Weapon Fired from a Distance or Near By?—A gunshot injury from a bullet implies at least one wound, namely, that of entrance, and perhaps another, that of exit. It does not always happen that the bullet passes through the body. The appearance of the wound of entrance is usually one of irregular circular puncture, its edges perhaps slightly torn or lacerated, with a purplish or dark areola, varying in width from a line or two to one-half inch. When the weapon is fired close to the body there are likely to be more or less powder-marks, and possibly actual burning from the heat and flame of the gunpowder. If the part of the body injured had been covered by clothing at the time, the marks of powder and of burning would probably be confined to the same. Bleeding is usually slight and occurs more commonly from the wound of entrance than from that of exit. Regularity of either of these wounds depends in large measure upon the angle at which the bullet has struck the surface. When striking very obliquely[613] the wound may be more oval or the bullet may have ploughed a furrow or a channel, by a study of which the relative position of the assailant and the assailed at the moment of injury may, perhaps, be determined. It is of importance to determine if possible the approximate distance at which the bullet was fired, since the question of self-defence, for instance, may hinge upon evidence of this character. The charge of powder and the weight of the bullet being known, one may sometimes estimate this distance by the depth of penetration or the appearance of the bullet. Still, the nature of the tissues must figure largely in such consideration. Many suicides who shoot themselves in the head show only one wound of entrance and none of exit.
Experiments Testing Powder-Marks.—Powder-marks and burns from weapons ordinarily used will scarcely appear when the distance has exceeded ten or twelve feet. LaChese, of Antwerp, found that in firing a gun even from a distance of only four feet the skin was only partially blackened.
As the result of experiments made with a Ballard rifle, old style, .44 calibre, with bullets of 220 grains and 28 grains of powder, Dr. Balch, of Albany, found that powder-marks were made at distances as follows:
At two feet, particles too numerous to count, with some of the lubricant blown upon the board;
At four feet the same;
At six feet the same;
At eight feet, nine grains of powder;
At ten feet, five grains of powder in one case and six in another.
That these were powder-grains were shown in court by picking some of them out, placing them on a glass, and igniting them with a galvano-caustic point. From those at ten feet no distinct flash could be elicited; from those obtained at eight feet distinct flashes were seen (Trans. New York State Med. Soc., 1881).
In the celebrated case of Peytle, brought in 1839 for the murder of his wife, who had been killed by two bullets entering near the nose, the eyebrows, lashes, and lids were completely burned, and a large number of powder grains were imbedded in the cheeks. Experiments being made in order to ascertain the distance necessary to produce these effects, it was found[614] that the weapon must have been held within a distance of twelve inches.
Wounds of Entrance and of Exit.—A great deal has been written in time past about the peculiarities of the wounds of entrance and of exit, much of which cannot be maintained under expert criticism. It is true that the wound of entrance will usually be well defined, the skin slightly depressed and appearing as above noted. It is true also that powder-marks will appear about this wound rather than that of exit. Usually, too, the orifice of exit is larger, less regular, its edges everted slightly, with more or less laceration of the skin, and quite free from any powder-marks or evidence of burning. The depression at the border of the wound of entrance differs after some days, by which time the contused margins slough away, and its appearance is daily changed by a process of granulation providing the individual recover or live long enough. According to Dupuytren, the hole in the clothing is smaller than that made by the same bullet in the skin. These are all points worth remembering when fitting bullets into wounds which they are supposed to have made; but the conditions under which gunshot punctures occur are constantly varying, and the significance of local markings is mainly the product of experience, care, observation, and reasoning. Thus the shape of either of these wounds will depend naturally upon the integrity of the bullet and its original shape and dimensions. Matthysen’s experiments give the following: A pistol fired at twelve paces distance, with a ball 15 mm. in diameter, made a wound in chest of 8¼ mm. diameter, and at its point of exit at the back one of 10 mm. In two experiments at the same distance as above, the entrance wound was 4 mm. larger in diameter than that of exit, and when a larger ball with a diameter of 17 mm. was used the same results were preserved, both wounds being less in size than the ball which made them. A spherical ball will usually cause more loss of substance than a conical, while the latter will cause usually more irregularity of outline and may even give the wound of entrance a slit-like appearance. Complications may also occur from other sources; a single wound of entrance may give rise to two or more wounds of exit due to splitting of the bullet, or if the bullet have been divided and the larger part lodged in the bone, only the smaller[615] portion passing out, the wound of exit may in reality be much smaller than that of entrance. Again, a bullet may split into fragments before striking the body, and of these one may enter the body, or one or more of them lodge. Multiple wounds are possible even from one bullet, as when it passes through two different parts of the body. Again, when two wounds, for instance, are discovered, one of them may be regarded as that of exit, when in reality they may be two wounds of entrance, neither bullet having left the body. So while it is possible in some cases to decide which is which, too much dependence should not be placed upon appearances of this kind, least of all until after a careful autopsy has been made.
Course of the Projectile.—When a bullet traverses a body the two apertures may be nearly opposite to each other, although the bullet may not have taken a direct course between them, having been deflected by tissues of varying density in its course. This leads to the mention of the effect of animal tissues upon the course of bullets, with which works on military surgery deal extensively.
The following is a remarkable illustration, yet authentic, of a devious path of a ball. In a duel with pistols between two students at Strasburg one fell, apparently mortally wounded in the neck, but recovered without feeling any inconvenience from his wound. It was found that the bullet had struck the larynx and had gone completely around the neck. It was taken out by simply making an incision over it. Other instances may be cited where bullets have made a circuit around the head, thorax, or abdomen. The ball may make a half circuit of the body and lodge or emerge at a point opposite that at which it entered, thus leading one to suppose that it must have passed directly through (Wharton and Stille).
As the writer of a chapter on the effect of projectiles of small-arms, in the Third Surgical Volume of the “Medical and Surgical History of the War of the Rebellion,” p. 709, says: “Such bullets attain great range and effectiveness as oppose least frontage of resistance to air; their velocity consequently is greater. Rotation upon their long axes tends to give them steadier flight and more direct course. By their pointed apices they pierce more easily the structures opposed to them. Such bullets, owing to the elasticity of the skin, make a wound of[616] entrance perhaps a trifle smaller in diameter than themselves, while spherical balls are more likely to carry a portion of the integument in with them.”
The differences of structure and density of the muscle tissues and their aponeuroses encountered by a bullet in its passage materially influence the directness of its course unless its velocity be very great, while round bullets are the more easily deflected from their course. The track of a small conical bullet passing swiftly through a muscle is more cleanly cut than that made by a round bullet, but in all gunshot wounds there is usually found a regular canal, with lacerated walls, with more or less destruction along the area of injury, shading off concentrically until lost in healthy tissue. There is always loss of substance dependent on muscle tension or direction of the bullet, whether transverse or obliquely to the direction of the muscle fibres; the more fibrous structures are torn and lacerated or simply perforated, mainly owing to their different tension at the instant; their openings seldom correspond to those of the muscle tissues or those upon the surface of the body, because of the constant change in the relation of the parts due to muscle action. This makes it often difficult to follow the course of a bullet with accuracy. The irregularity of a bullet-track due to these causes constitutes one of the great sources of danger, since cavities and pouches thus formed give lodgment to foreign matter driven in with the bullet, by retention of which a fertile source of sepsis is maintained. Gunshot injuries of bone may be classified as contusions, simple fractures, partial fractures, penetrations, perforations, and complete fractures with more or less comminution or loss of substance, all of these, of course, in the surgical sense compound. These are all manifestations of mechanical force acting in accordance with established laws. On autopsy these will be ascertained, while one or more portions or all of a bullet may be found imbedded in or attached to some bone. The best illustration of such accidents will be found in the “Medical and Surgical History of the War of the Rebellion.”
Such questions as pertain to the position of the wounded person when shot or that of his antagonist, and other similar inquiries, can only be settled by reference to particular circumstances of individual cases. Position of the wound may help a little. A bullet-wound directly in the centre of the top of the[617] head could scarcely be received by a person standing unless his assailant occupied an elevated position. If accompanied by evidence of severe blows by which the deceased might have been knocked down, it might show that he had been shot after falling.
Wounds by Small Shot.—Small shot rarely traverse the entire body unless discharged from such proximity as to make a clean, round opening. Paley relates the following instance: A boy was shot in the neck by the accidental explosion of his own gun, No. 8 shot. He died instantly. He was lying forward of the muzzle so that it was nearly in contact with the skin of the neck. A large round hole was produced, in diameter one and one-half inches, whose edges were slightly darkened by powder. The wound of exit at the back of the neck, at the third vertebra, was a mere slit in the skin scarcely an inch in length with the diameter placed vertically. The smallness of this aperture may have been owing to the greater part of the charge being lodged in the body. Dr. Lowe states that in some experiments it was found that a round aperture might be produced by a discharge of small shot at a much greater distance than that assigned by Dr. LaChese, namely, ten to twelve inches. Even admitting such exceptional instances, it will scarcely ever occur that a wound from a small shot can be mistaken for one produced by a leaden bullet.
De Vergie has shown that when the ball enters a portion of the body well covered with fat, this often protrudes between the edges of the wound and may alter its character. If clothing have been carried in some shreds of it may show upon the wound, and such fragments of texture will nearly always characterize the wound at once as that of entrance.
Wounds by Blank Charges.—Experience has shown that no matter with what the piece is charged, it is capable, when fired close by, of producing a wound which may prove fatal. Thus a gun loaded with wadding or gunpowder only may cause death. A portion of clothing may be carried into the wound and lead to death from hemorrhage, or death may occur from many secondary causes, such as tetanus or sepsis. Accidents so frequently occur from weapons discharged in sport, not loaded with ball or shot, that it is worth while to bear this in mind. It has been observed, for instance, that persons attempting[618] to commit suicide have forgotten to put a bullet in the pistol, nevertheless the discharge of the weapon into the mouth has sufficed, from the wadding alone, to produce a considerable laceration and hemorrhage (Taylor). Many fatal accidents have taken place by the discharge of wadding from cannon. LaChese has ascertained by experiment that a piece charged with gunpowder alone is capable of producing a penetrating wound somewhat resembling that produced by gunshot, when the piece is large and fired within six feet of the body (Ann. d’Hygiene, 1836, p. 368). This arises from unexploded grains of powder acting as pellets of small shot. Sweet has experimented with pistols loaded with gunpowder and wadding in order to determine the effect of their discharge at different distances. At twelve inches he found that the clothing was lacerated and the skin abraded, but the wadding did not penetrate; at six inches the clothes were lacerated and the wadding penetrated to the depth of one-half inch; at one and one-half inches from the chest the wadding passed into the thoracic cavity between the ribs, and at a second experiment carried away a portion of the ribs.
It is probable that an ordinary wadding such as loosely wrapped paper, rag, or similar material, especially as prepared by one not accustomed to military use of a weapon, would not produce a wound which would resemble that made by a bullet, and it is doubtful whether such a wound could be produced at a greater distance than six inches from the body.
It is on record that in Paris, in 1858, a circus cannon of four inches bore, loaded with three ounces of grain powder retained by a wad of old theatre bills loosely folded together and rammed home with only moderate force, was discharged in the direction of the boxes at a distance of about one hundred and fifty feet. A man seated in one of these boxes opposite the muzzle of the gun, leaning forward, his arms crossed upon the handle of his umbrella, had his arm broken above the elbow immediately upon its discharge. Several portions of wadding were found beneath the place where the man sat, but no marks existed upon his clothing nor upon the anterior part of the arm, which must have been inaccessible to any projectile that did not first strike the forearm. It was concluded that the fracture had been caused by the violent and sudden starting of the man backward,[619] which must have brought his arm against the hard part of the partition. An experiment tried with the cannon proved that any wadding that could be made with paper was dispersed in passing, or lost all power of mischief, at much less distance than one hundred and twenty feet (Annales d’Hygiene, 1859, p. 420, Wharton and Stille).
The Mannlicher Rifle.—It may be of interest here to note the effects of the rifle-bullets used in the most recently invented improved arms. The last new projectile used in the German army, 1892, with the Mannlicher rifle, has an inner core of lead inclosed in a casing of steel or firm metal, which prevents the lead, even when softened by heat, from becoming deformed and enlarged by contact. The weight of the bullet is much less than any of the old, but to its higher rate of velocity and its pointed shape, which is preserved, must be ascribed its greater perforating power. Owing to this immense velocity and the small surface of contact, it meets with little resistance on striking a person, has no time to stretch the various tissues it encounters, causes little or no commotion of the neighboring parts, and merely punches a hole, carrying the contused elements before it clear out of the wound without seriously damaging the surrounding wall of the bullet-track. This absence of contusion must lead to more frequent deaths from hemorrhage, while when this arm is used we shall hear very little of deflection or deviation of the bullet from its path, since it has sufficient power to pass directly through any part of the body which it may meet on its way. The result in battle will be a reduction of the list of wounded, but a terrible augmentation of that of the dead.
IDENTITY FROM A FLASH OF GUNPOWDER.
Taylor states the following: “Among the singular questions which have arisen out of this subject is the following: whether the person who fires a gun or pistol during a dark night can be identified by means of the light produced during the discharge. This question was first negatively answered by a class in physical science in France, whereas later a case tending to show that their decision was erroneous was subsequently reported by Fodere. A woman positively swore that she saw the face of the prisoner, who fired at another during the night, surrounded[620] by a kind of glory, and that she was thereby enabled to identify him. This statement was confirmed by the deposition of the wounded party. Desgranges, of Lyons, performed many experiments on this subject, and he concluded that away from every source of light the prisoner who fired the gun might be identified within a moderate distance; if the flash were very strong, the smoke very dense, and the distance great, the person firing the piece could not be identified. The question was raised in England in the case of Reg. v. White at the Croydon Autumn Assizes, 1839. A gentleman was shot at while driving home on a dark night, being wounded in the leg. When he saw the flash of the gun he saw that the piece was levelled toward him, and the light of the flash enabled him to recognize at once the features of the accused. In cross-examination he said he was quite sure he could see the prisoner and was not mistaken as to his identity; but the accused was skilfully defended and he was acquitted. A similar case was tried at the Lewes Lent Assizes, 1862, Reg. v. Stapley. The prisoner shot at the prosecutor on a dark December evening, and the latter swore that he distinctly saw the prisoner by the flash of the gun and could identify him by the light on his features. His evidence was corroborated and the man was convicted. A case is also quoted, Rex v. Haines, in which some police officials were shot at by a highwayman during a dark night. One of these stated that he could distinctly see from the flash of the pistol that the robber rode a dark-brown horse of remarkable shape, and that he had since identified the horse at a stable in London. He also was positive that the prisoner had on a rough brown great-coat.
There seems to be enough evidence in this direction to show that identification under these circumstances is occasionally possible.
GENERAL MEDICO-LEGAL CONSIDERATIONS.
The result of the wonderful advance in the practice of surgery made during the past fifteen years has been in a large measure to revolutionize the treatment of gunshot wounds, and inasmuch as the result of many homicidal attempts will depend in large measure upon what the surgeon can do for the victim of assault, it may not be amiss to very briefly epitomize in this place something of what modern surgeons believe with regard[621] to the best treatment of bullet-wounds, expressed in a general way. They have learned, among other things, that the harm which a bullet does is done by it during its flight, and that after it has come to a stop it is, per se, an almost invariably harmless foreign body. This is practically always the case unless it has carried in with it foreign material which may serve as a source of septic infection.
In time past there has always been a strong feeling, which had, however, nothing scientific to justify it, that every gunshot wound was a poisoned one. Of late, since bacteriology has attained the proportion of a science, it has been held that bullets were necessarily sterilized by the heat of the discharge of powder behind them. Very recently Dr. B. Von Beck, Medical Director of the 14th German Army Corps, has made experiments upon the amount of heat imparted to leaden and other bullets after firing. After making an allowance for specific heat and the conductivity of the different metals used, he found that even when the projectiles encountered resistance from three to four times greater than that offered by the human body the results were as follows: Temperature of leaden bullets of .45 calibre, when recovered, 69° C.; of .30 calibre, covered with steel, when recovered, 78° C.; of .30 calibre, covered with copper, when recovered, 101° C. He states that these experiments disprove the theory that certain lesions in wounds can be in any way attributed to the heat imparted by the bullet.
While these experiments prove that the bullets may be heated to the above degrees when recovered, they by no means prove that they are so heated at the time when they inflicted the wound. During the year 1892 some very interesting experiments were carried on by Dr. Lagarde, of the Army Medical Department (New York Medical Journal, Oct. 22d, 1892, p. 458). He experimented by deliberately infecting bullets and then firing them into cotton, and animals as well, studying the effect both on the bullets themselves and upon the animals. Some of these bullets were taken from the original packages, while others had been intentionally rolled in dirt. The experiments were carefully carried out and appear reliable, and the conclusions given by the author, which interest us here, are as follows:
(1) The vast majority of cartridges in original packages are sterile or free from septic germs because of the disinfection[622] and absolute cleanliness observed in the process of their manufacture.
(2) The majority of gunshot wounds are aseptic because the vast majority of the projectiles inflicting them are either sterile or free from septic germs.
(3) The heat developed by the act of firing is not sufficient to destroy all the organic matter of the projectile, the cherished notions of three centuries or more to the contrary notwithstanding.
The results as set forth justify the assumption that a septic bullet can infect a gunshot wound. The average bullet-wound, however, is sterile so far as infection from the bullet is concerned, and in accordance with this view of its usual innocence there need be no longer the clamor for removal of the missile which the fears of previous generations have nearly always called for; and the best practice among military surgeons of to-day is rather to let the bullet remain where lodged than to make a more serious wound for its removal. Exceptions to this rule occur only in cases where operation is called for on account of injury done by the bullet while still in motion. It is also held to be a violation of simple physiological and surgical rules to probe or carelessly search for a bullet whose location cannot be made out from a study of signs and symptoms in a given case. The act of probing breaks up blood-clot, often brings on fresh hemorrhage, is in a majority of cases unsatisfactory, frequently introduces specific elements from without, and really gives little, if any, more information than can be gathered from a study of the case without the use of the probe. If every ordinary bullet-wound which did not call for immediate operation because of injury to some essential or vital part—such as a large blood-vessel or nerve-trunk, or some of the viscera—were antiseptically and hermetically sealed at the very outset, there would be a much smaller percentage of death from gunshot wounds, either in civil or military practice, than now obtains. And it might be a matter upon which to go to the jury whether violation of such rules, to-day, does not mitigate the offence of the accused.
Recent discoveries in so-called cerebral localization have instigated numerous operations upon the skull and brain for the relief of pressure, as from blood-clot, or for removal of depressed[623] bone or a bullet which twenty years ago would have been impossible. The brain is no longer the terra incognita of the past generation of medical men, and it is now often possible for the surgeon to intervene in such a way as to save life in cases previously considered hopeless; in fact, such is now his duty when consent can be gained, and it should be held that he is culpable when deficient in general knowledge in this respect.
In wounds of the thoracic cavity it should now be held that so long as air has entered through a bullet-wound there are cases where free incision, even with removal of ribs, can scarcely increase the dangers, while permitting opportunity for much more accurate exploration and determination of life-saving methods. The experiments of numerous investigators, the writer included, have shown that bullet-wounds of the heart need not be always and invariably fatal, and have afforded an element of hope from the possible surgery of even this organ. The writer looks forward to the time when some accomplished yet daring surgeon, getting the right patient at the right time and in the right place, i.e., where conveniences are at hand, shall, in some case of perforating wound of the pericardium or of the heart itself, resect some portion of the anterior thoracic wall, lay open the pericardium, maintaining meanwhile artificial respiration if necessary, and suture a wound in the heart-substance, thereafter closing the pericardium and external wound, and save life which would otherwise be surely sacrificed. With others he has done this upon animals, hence why may it not be done in man?
In the mean time for, first, the recognition and, second, the surgical treatment of perforating wounds of the abdominal viscera, American surgeons have won for themselves the greatest credit, and an already long list of successful laparotomies after gunshot wounds of the intestines, with intestinal suture or resection, has shown the very great value of this procedure, even though it has kept some would-be murderers from the gallows.
These lines are inserted here because the time and effort which surgeons have devoted to this kind of surgery deserve only the highest encomiums and encouragement from the legal profession, although to our deep regret they have not always met with the same.
OF THE VARIOUS CONDITIONS WHICH COMPLICATE GUNSHOT WOUNDS AND MAKE THEIR RESULTS UNCERTAIN,
Delirium Tremens is one of the commonest and must always be regarded as one of the most serious. It is well known to surgeons that a slight injury even, and often a severe one, is enough to provoke manifestations of this character in intemperate persons. The medico-legal question under these circumstances is this: Would the same amount of injury have been likely to cause death in a person of ordinary health and vigor? The law as applied to these cases has been stated by Lord Hale: “It is sufficient to prove that the death of a person was accelerated by the malicious acts of the person, although the former labored under a mental disease at the time of the act. The intent of the accused may often be judged by the character of the wound and the means of its infliction. Drunkenness of the victim admits of no excuse when his assailant is aware, or ought to have been aware, of the condition of his victim. It is held that the assailant ought to have known that violence of any kind to such a person is likely to be attended by dangerous results. It is known also that a wound which accelerates death causes death.” The commissioners who were appointed to define criminal law on the subject of homicide have thus expressed themselves: “Art. 3. It is homicide although the effect of the injury be merely to accelerate the death of one laboring under some previous injury or infirmity, for although if timely remedies or skilful treatment had been applied, death might have been prevented” (Taylor, p. 327).
Death from Surgical Operations Necessitated by Gunshot Wound.—The modern treatment of serious or so-called penetrating gunshot wounds where the cranium, thoracic viscera, or the abdominal viscera, especially the intestines, have been perforated one or more times, calls for surgical procedures which are of severity and danger in proportion to the gravity of the wound which necessitates them, and which, while they often save life, must necessarily often fail. Indeed, such operations may prove fatal upon the operating-table, i.e., patients may die before the conclusion of the operation. The question may, therefore, arise whether the person who inflicted the wound should be held responsible for his act, or whether by[625] the intervention of the surgeon the responsibility may not at least be shifted from the shoulders of the accused. The law in this respect is explicit and regards such operation as the outcome of necessity and a legitimate part of treatment, so that if it be undertaken in good faith, with reasonable care and skill, the accused will be held responsible, be the result what it may. The question of necessity and the plan of operation are left to the judgment of the surgeon in charge. Considering the responsibility involved in such cases and the possibility of a suit being raised, we should always advise the operator to secure the counsel of other surgeons or practitioners in his vicinity. The verdict of such a counsel of talent will always stand. According to Lord Hale, when death takes place from an unskilful operation under such circumstances, and not from the wound, the responsibility of the prisoner naturally ceases, but the burden of proof that such has been unskilfully performed rests naturally with the defence. It is much better also in these cases that the primary responsibility be borne by one surgeon from the beginning of the case, though he may associate with himself as many others as he chooses, since the ends of justice have more than once been defeated by a division of such responsibilities. Should it be made to appear that the surgeon in charge has not availed himself of such means as are supposed to be in the hands of every competent practitioner and has neglected ordinary antiseptic precautions, it would not be difficult to show that the operation had been unskilfully performed, and the prisoner would naturally get the benefit of such defence. At the present date of writing there exists a large class of the profession who still continue to do surgery according to the views and practices of twenty or thirty years ago, and who, while perhaps carrying out some of the forms of antiseptic surgery, are still ignorant of its fundamental principles and consequently guilty of neglect, since there is now no reason why all should not practise them. The writer holds to the view that if it can be shown that these precautions were not adopted when others would have adopted them, it constitutes criminal neglect.
On the other hand, circumstances may arise where a simple or a more serious operation would have saved life, as, for instance, in cases of hemorrhage, and where a surgeon from[626] timidity or carelessness has failed to take the necessary steps. Such neglect as this should inure to the benefit of the accused, but when at any time it can be shown that the possible benefits of operation have been offered to the deceased before his death and have been declined, the surgeon at least is relieved of all further responsibility. Among the dangers of operations under these circumstances are of course to be reckoned those pertaining to the use of anæsthetics. The surgeon in charge, however, is responsible for the selection of his assistants, at least when assistants are at hand, and must be regarded as equally competent in this as in other features of the operation; and even though the patient die from collapse or the anæsthetic, the burden of proof must rest with the defence to show that it had been unskilfully administered.
Note.—The assistance which the microscope may afford in the procurement of evidence in cases of gunshot wound is beautifully illustrated in the expert testimony reported by Dr. James, of St. Louis, in the presidential address before the American Society of Microscopists, in Washington, August, 1891, printed in Vol. XIII. of its Transactions. It occurred in St. Louis, in the case of The People v. Vail, who had a pistol in his pocket at the instant when his wife fell from a wagon against him, knocking him, as he claimed, against the wheel of the wagon, the pistol being discharged by accident. By a minute study of the fibres of the various textures making up his overcoat and of the effect of the explosion of powder upon textile fabrics almost in contact with it, he was enabled to establish the accident and secure the acquittal of the accused.
DEATH
BY HEAT AND COLD,
INCLUDING
INSOLATION IN ITS MEDICO-LEGAL ASPECTS.
BY
ENOCH V. STODDARD, A.M., M.D.,
Emeritus Professor of Materia Medica and Hygiene in the University of Buffalo;
Member of the Medical Society of the State of New York and of the Central
New York Medical Association; Fellow of the New York Academy
of Medicine and of the American Academy of Medicine;
Late Surgeon 65th Regt. N. Y. Vols.; Late
Health Commissioner, Rochester,
N. Y.; etc., etc.
DEATH BY HEAT AND COLD.
TEMPERATURE OF THE BODY.
The production and regulation of heat in the body is a problem by no means elucidated. We consider heat production to be of internal origin, by a complex process involving tissue metamorphosis, chemical changes in nutrient elements, muscular movements, etc. Heat regulation is accomplished, not only by variation in the loss of heat by the body, but by what is more important, variations in the amount of heat generated. It is an accepted physiological conclusion that there exists in the body a thermotaxic nervous mechanism which controls its normal, as well as its abnormal, manifestations of heat.
The average temperature of the body in health is 37° C. (98.6° F.), in the axilla. Taken in the vagina or rectum, .9° C. (1.3° F.) higher is noted. The daily average range of variation is about 1° C. (1.8° F.).
In disease or injury considerable variations occur; very high, as well as very low, temperatures are met. In severe neuroses and some forms of malarial disease a temperature of 42.2° C. (115° F.) has been recorded, and after an injury 71° C. (122° F.).[688]
Very low temperatures are reported in several cases of acute alcoholism, accompanied by exposure to cold, where a temperature of 28.8° C. (75° F.) in the rectum was noted, recovery following.[689]
Such extreme temperatures, though authentic, are exceptional.
Very high temperatures in febrile conditions are borne because remitting; and low temperatures, subject to periods of elevation, are met in wasting and other conditions. Very high and very low temperatures are also noted, just before[630] death, in acute diseases and conditions specially involving the nervous system.
The degree to which the temperature may be raised without destroying life has been investigated by Berger, Bernard, Chossat, and others.[690]
Their experiments show that if an elevation of temperature of the body 7.20° C. (13° F.) be maintained for any length of time in warm-blooded animals, death ensues. Depression of the temperature of warm-blooded animals 12° C. (20° F.), or even less than these degrees below the normal, results fatally. Portions of the body may be frozen and yet, under appropriate treatment, recover. But freezing of the whole body must necessarily prove fatal.
Great differences in ability to endure extremes of heat and cold appear among different nations and in different individuals. The very young and the very old are unable to bear exposure to extreme cold. In both, the capacity for heat production is low and the vital powers are soon enfeebled to a critical degree. The healthy adult can, with proper precautions, safely endure great extremes of heat and cold. The experience of arctic explorers in the expeditions of Kane, Nares, Greely, and others has demonstrated the power of endurance, for a considerable period, of a temperature from 90° to 100° F. below the freezing-point. On the other hand, laborers employed in pottery and other establishments, using ovens raised to 148° to 315° C. (300° to 600° F.) or higher, are often exposed for some time without injury to temperatures approaching these intense figures.
EFFECTS OF EXTREME COLD.
Legal inquiry into the conditions of death from cold occurs almost entirely in cases of unintentional exposure. Cold has been employed, however, with homicidal intent. The depressing influence of continued low temperatures is observed in the death-rates of cities, in winters of protracted severity, where the proportionate mortality among infants, the aged and enfeebled shows marked increase. While age is a prominent predisposing and contributing factor, other causes exist. Exhaustion[631] from severe and prolonged exertion, deprivation of food, intoxication, former illness, and other conditions of depression lessen the powers of the body to resist cold. Thus an exposure which might be safely borne in perfect health might result fatally in the same person in conditions of depression just referred to (Case 1).
Investigation may be demanded in case of the death of
A. Young children.
B. The injured.
C. The insane.
A. In Young Children.—This may be in the new-born or older children.
In the new-born exposure to cold soon causes death, as warmth is essential to the life of the young being. The length of time necessary to a fatal issue is modified by several conditions. In the immature or prematurely born infant the resisting power is much less than in the child born at full term and otherwise healthy. In cases of suspected infanticide by exposure the question of the maturity of the child at birth is to be decided. Careful examination of the place in which the body was discovered should be made as to its lack of warmth; and the degree of external cold at the time of probable exposure should be recorded. The circumstances as to whether the exposure was inadvertent or accidental, as in cases of premature or unexpected delivery, or whether from intentional and deliberate purpose or from culpable neglect, should be carefully considered. The post-mortem examination should decide whether the appearances and conditions of the body are those peculiar to death from cold (Case 2).
Death may occur from culpably careless exposure to cold, as a contributory if not as a direct cause, in such conditions of enfeeblement. Criminal neglect to provide medical attendance, food, and other essentials has been proven in some cases of the so-called “faith cure” or “prayer cure.” Exposure may be resorted to with deliberate homicidal intent. It may, in some cases of death, become an important legal question to decide whether a studied and persistent neglect of this nature may not have been followed, with the purpose of getting rid of a troublesome care (Cases 2 and 3).
B. Exposure of the injured or wounded, thereby inducing[632] some grave condition or complication which under proper care would have been avoided, may raise an important question in injuries inflicted by another, with or without criminal intent. It is undeniable that serious or fatal results may follow a slight wound, otherwise trivial, where the injured person was subjected, accidentally or intentionally, to extreme cold for a considerable period. While such cases are comparatively rare, they may demand investigation.
C. Exposure of the Insane.—While it must be admitted that the insane subject is usually indifferent to matters of temperature, death from exposure to cold may call for special examination. Carelessness, incompetence, or wilful neglect on the part of nurses or keepers of insane hospitals, or deliberate criminal intent in such or others having the care of or an interest in the death of an insane person may lead to a judicial inquiry.
Sudden death has been reported as occurring, in several cases, after the ingestion of large quantities of cold water when the person was greatly heated. It is somewhat difficult to explain all such cases reported on a single line of causation. Some observers have attributed death to syncope or asthenia by the shock produced, in the sudden effect of the cold upon the sympathetic nervous system inducing heart failure. This seems the most natural explanation.
Others consider the causative factor to be the formation of thromboses in the capillaries of the brain, lungs, and other organs, inducing active and obstructive congestions causing death by apnœa or coma. Others regard these cases as similar to “heat apoplexy.”
Symptoms.
Under the influence of external cold, the vessels of the skin are contracted and the internal splanchnic areas dilated. Thus the surface of the body contains less blood and the internal organs a larger proportion. This vascular change is one of the important factors in maintaining the uniform temperature of the body. The thermometer, placed in the mouth, in such conditions frequently indicates a rise of temperature. This is probably due, not only to the increased volume of blood collected[633] in the internal organs, but also to an increased production of heat through a thermogenic action.
In exposure for a time to severe cold the nose, ears, cheeks, hands, feet, and other portions of the body, after the first appearance of dusky lividity, become bloodless and white, lose sensation, and become congealed; a condition known as “frost-bite.” From this, recovery without injury is possible under appropriate treatment, by which the temperature is gradually raised and the circulation restored. Where the latter result is not secured, the part becomes gangrenous and is ultimately removed by a process of inflammation and sloughing.
If the application of cold be protracted and the temperature extreme, the loss of heat becomes rapid and symptoms of depression of the heart’s action appear. Painful sensations of the surface and other portions of the body are experienced, succeeded by impaired sensation and anæsthesia. The skin acquires a dusky, reddish, and livid appearance, with the formation occasionally of vesicles or blisters. With the lessened sensation stiffness of the limbs appears, due to failing muscular contractility. The congestion of the central portions of the nervous system induces a condition of advancing stupor, resulting in complete coma with ultimate suspension of respiration and the heart’s action.
Death from exposure to cold may be rapid or slow. In cases of recovery the period of reaction is a critical one. The depression of the heart is apt to continue, and gangrene of parts of the body is likely to occur. Ulcers and sores healing with difficulty develop in some cases.
Treatment.
In the treatment of those who are suffering from the effects of extreme cold, the restoration of the congealed or “frost-bitten” portions of the body should be gradually accomplished. Raising the temperature rapidly is liable to induce the death and destruction of the affected parts. Ice or snow should, at first, be rubbed upon the frozen part, to be succeeded later by cold water. The patient should be placed in a cool room and distant from the fire or source of heat. As soon as warmth begins to return the part should be enveloped in wool, cotton,[634] or some substance of poor conducting powers. If the whole body be chilled, frictions of the surface with stimulating lotions are of benefit, wrapping the person in woollen or fur coverings or garments afterward.
Hot coffee or alcoholic stimulants are of value as restoratives, but the latter are to be avoided during an exposure to cold.
Post-Mortem Appearances.
The appearances indicative of death from cold are sufficiently marked to enable one to decide whether exposure to cold was the chief determining cause of death, provided that a careful consideration of the circumstances of season, temperature, place, and other conditions be also had.
In the examination of a body in a case of apparent death from cold, the limbs and internal organs may be found frozen. It must be remembered that this occurs after, not before, death; and the frozen condition must not be mistaken for “rigor mortis.”
In cases where a body is found, in freezing conditions of atmosphere, showing commencing putrefaction, the death must not be hastily attributed to cold, which prevents putrefaction. It is evident that if cold was the cause of death the temperature of the body had been raised since that event, or, more probably, death occurred from other causes and the body remained some time before becoming frozen.
The finding of a body in the snow or frozen in severe weather must not preclude the search for other causes of death, such as apoplexy, etc., which may have occurred anterior to the freezing.
Observers generally have agreed upon the presence of certain post-mortem conditions in cases of death from cold.
Externally.—Upon the skin are found dusky reddish patches, irregular in outline, which are in sharp contrast with the general pallor of the surface. Krajewskey,[691] Ogston,[692] Dieberg,[693] and others, in the several series of cases reported by them, all describe this condition. The skin otherwise is pale.
Internally.—The viscera, including the brain, are congested. The heart contains a large quantity of blood in the cavities of both sides, and the large vessels leading from it are also full. The color of the blood is a bright red, resembling its arterial hue. This condition has been generally noted and described; but some excellent observers have not referred to it.
EFFECTS OF EXTREME HEAT.
The application of moderate heat to the surface of the body causes dilatation of the cutaneous capillaries. In such application the exhalant and perspiratory function of the skin is increased, by which means a rise in general body temperature is prevented. If, however, severe physical exertion accompany the exposure, a more pronounced result is induced and a depressing effect upon the nervous system becomes manifest. If the degree of heat be raised and the exertion increased and prolonged, marked depression ensues. Under circumstances of quiet and rest a high degree of temperature is borne by man without depression or discomfort, but with continued and severe muscular effort the rise in animal temperature is productive of distress and depressing conditions. In the Turkish or Russian baths, in the healthy subject, a temperature of 48.8° to 54.4° C. (120° to 130° F.) produces profuse perspiration but no depression, and a plunge in or affusion of cold water is not only borne with impunity but is acceptable. In conditions of heat accompanied by physical exhaustion, such sudden exposure to cold would prove extremely dangerous.
In the condition of rest, exposed to external heat, the tendency to elevation of body temperature arises from the external causes alone, which in no way specially modify the nutritive functions. But in the second condition the internal processes of nutrition, which have been subject to great stimulation, are suddenly embarrassed by suppression of the compensating activity of the cutaneous surface, and severe organic and nervous derangements follow.
In the summer season the temperature rises to 32.3° C. (90° F.) and even much higher in certain localities. During the prevalence of such heat, the mortality among young children, the aged and enfeebled is very marked; these two periods[636] of life being very susceptible to the depressing effects of heat. A high temperature is easily borne if the air be pure and the atmosphere be not saturated with moisture. Telluric electric conditions also have a modifying influence, undoubted though obscure.
In certain occupations an intensely heated atmosphere is endured with impunity for a considerable time, provided the air be maintained in a condition of purity and water be supplied to the person exposed. The stokers upon ocean steam-ships, where a forced draught is employed, are subjected to extreme heat, sometimes reaching 60° C. (140° F.). Resort to forced and continuous ventilation of the stoke-rooms, with short hours of duty, renders tolerance of the high temperatures possible.
SUNSTROKE.
The terms “sunstroke,” “insolation,” “coup de soleil,” are applied to conditions induced, not alone by exposure to the rays of the sun, but rather by a combination of great heat with other exciting causes. They are used to designate attacks occurring in very hot weather after exposure to solar or other sources of extreme heat. The striking and usual phenomena are exhaustion, unconsciousness, stertorous respiration, and death, occurring by syncope, within a few moments or hours. In a number of cases the symptoms of cerebral apoplexy with death by coma are present.
In others, the condition seems one of complete exhaustion. The majority of cases seem to be a combination of these several conditions, with death resulting from syncope.
The ordinary phenomena of the attack are pain in the head, hurried respiration sometimes stertorous, violent beating of the heart with failing of its power, oppression within the chest and, occasionally, nausea and vomiting. The pupils are sometimes dilated and sometimes contracted, but in all cases exhibit lessened sensitiveness to light. The suddenness of the attack modifies the symptoms developed.
Pathological Conditions.
These are exhaustion with syncopic tendency and a rapid rise in the temperature of the body to a point destructive to[637] the activity of the nervous centres. This is accompanied by an abnormal condition of the blood, resulting from loss of its watery portions, with retention of effete products and impaired aeration. A tendency to general stasis, specially marked by congestions of the lungs and brain, is present. The change in the blood is a very important factor. In some cases, not fatal at the outset, this induces a septic condition.
The greatly elevated temperature of the body undoubtedly produces certain modifications which type it, in some respects, as a febrile disease; but this, with the septic tendency due to blood changes, is not sufficient to designate it as a purely “thermal fever,” as some have claimed. It is something more than this.
Sunstroke occurs more commonly in tropical than temperate climates;[694] and usually in the day-time, at the period of greatest solar activity, those attacked being engaged in labor involving considerable exertion. It occasionally, though rarely, occurs at night. The military service affords abundant opportunity for observation. Here the seizures are on the march, rarely in camp. Fatigue, prolonged and extreme exertion, ill-adjusted clothing and accoutrements, with the deprivation of cool water, are fully as active factors as the heat of the sun. The death-rate ranges between forty and fifty per cent, the mild cases being excluded. Death in some cases is marked by syncope, in others by apnœa, though the majority seem to die by a combination of both, as in most cases the pulmonary congestion is more or less pronounced. Undoubtedly the character of the symptoms and mode of death are influenced, in many cases, by individual tendencies leading to apoplectic conditions or to cardiac or other complications.
Treatment.
This must be adjusted to the pathological conditions of the patient. As already indicated, two classes of cases are met: one marked by exhaustion, with tendency to death by syncope; the other, a state of or tendency to cerebral congestion or apoplectic conditions. Exactly opposite methods of treatment are[638] demanded. In the first, frequency and feebleness of the heart’s action, with faintness of the heart sounds and embarrassment of respiration, indicate the tendency to death by nervous exhaustion, and must be met by placing the patient in a condition of absolute rest and quiet in a cool place. Stimulants must be promptly administered, though cautiously on account of the tendency to nausea and vomiting. Hypodermic injections of alcohol or ether, or rectal enemata of turpentine, alcohol, or other stimulants, afford means of securing speedy effects when the stomach is irritable. Carbonate of ammonia and other cardiac stimulants are recommended. Depleting agents, or such as prove depressing, are to be avoided. In some cases, hypodermic injections of small doses of morphine prove beneficial. Individual cases must modify therapeutic procedures.
In the second class of cases the tendency to cerebral congestion indicates sedative and depleting procedures. Blood-letting has been recommended by some authors, if employed with extreme judgment and discrimination.[695] Cold applied to the head and also to the whole body by rubbing with ice[696] or by effusion and the wet sheet, or other means, is indicated if the temperature is high (104° to 105° F.). Active catharsis, by promptly acting purgative enemata, is also to be resorted to in most cases. The convulsions occurring in some cases are successfully modified and controlled by inhalations of small quantities of chloroform.
Post-Mortem Appearances.
These, though not clearly characteristic, are pronounced. In some cases no distinct conditions are found.[697] Local congestions are present in nearly all cases. Upon the skin are found petechial and livid spots, pallor being occasionally noted. Ecchymoses and subserous hemorrhages are also common. These conditions have been described as resembling those of spotted typhus (Levick).
Rigor mortis is marked and occurs early, putrefaction beginning soon after death. The lungs are highly congested and[639] often œdematous, and effusions of serum are frequently found in the pleural cavities.[698]
The heart is usually changed in color and consistence, with the left ventricle contracted and the aorta empty, while the right ventricle and pulmonary arteries are dilated and engorged. The blood is fluid and dark.[699] The large vessels of the pia and dura are full of dark blood. Congestion of the cerebral mass is not always noted. The ventricles contain serum; and extravasations of blood into the cervical sympathetic ganglia and vagus are sometimes found. The kidneys are usually moist and œdematous; the liver and spleen congested and dry.
BURNS AND SCALDS.
For all purposes of practice it is unnecessary to draw any distinction between a burn and a scald, for in reality none exists, except as regards the nature of the causative agent. In some cases requiring investigation, this may prove to be a matter of much importance.
Definition.—A burn is an injury produced by the application to the body of a heated substance, flame or radiant heat.
A scald is an injury produced by the application of a liquid at or near its boiling-point.
Appearances as Indicating Origin.
A hot body may produce a burn of any intensity, ranging between reddening of the skin and complete charring of the tissues, according as its temperature is elevated and the period of contact prolonged: the shape of the object and its size being indicated by the form of the burn. Metallic substances heated to a temperature of 100° C. (212° F.) are capable of producing redness and vesication and other injurious effects. At this temperature the albuminous elements of the blood and other fluids undergo coagulation. Some bodies require to be heated to redness, or nearly so, in order to produce a defined burn.
Very hot and partially-fused solids cause burns of greater severity than where the heated body is of a character favoring[640] prompt removal. In such cases their adhesion to the skin involves the tearing away of the superficial portions of the derma in their removal, or they by their adherence prolong the contact of the heated body, thus intensifying their destructive action.
Metals in a state of fusion produce burns which cannot be easily distinguished from those caused by solid bodies. Such burns are classed as scalds. Their effects may vary in any degree between slight redness and complete destruction of the tissues with charring. Burns caused by melted solids are less regular in form and outline than those caused by heated solids. They are usually of greater severity on account of the high temperature to which they have been raised.[700]
Boiling Water.—Scalds by boiling water may be so slight as to produce redness only, or they may be so severe as to cause marked and characteristic symptoms. Those noted in severe cases are an ashy hue of the skin, accompanied by a soaked or sodden appearance and the production of blisters. Occasionally these features are not easily distinguished from those of burns from other sources. Blackening of the skin and charring of the tissues never result from burns by boiling water. As in all burns, a large surface involved renders an early fatal issue probable. In severe cases, not necessarily fatal, gangrene of the parts injured sometimes occurs. Most of those met with are accidental, yet cases of scalding by hot water with intent to injure are not uncommon, aside from injuries and death resulting from explosion of boilers, bursting of steam-pipes, etc. Occasional instances are recorded of death of children, the insane or feeble persons by inadvertent immersion in a bath of hot water (Case 21).
Severe and fatal burns of the mouth, fauces, and larynx in young children occur from inhaling steam or swallowing boiling water from a teapot or kettle in an attempt to drink (Case 5).
Burns by burning oil produce effects and appearances similar to those by melted metals.
Burns by flame are specially characterized by scorching of the surface. Hairs upon the part actually burned are scorched and usually also those in the vicinity of the burned[641] patches. Such conditions could not result from scalds by hot water, boiling oil, or from a hot body only.
Burns by petroleum or its derivatives resemble the burns from flame, except that the injured portions of the body are not only scorched but blackened and are usually burned more severely than by flame alone, as the clothing holds the burning substance in contact with the parts. The odor of the agent is also very noticeable.
Burns by Acids and Corrosive Agents.—The injury produced by a mineral acid, the caustic alkalies, etc., has frequently been the source of judicial inquiry. “Vitriol-throwing,” as it has been termed, has been and occasionally is resorted to with malicious intent to injure. No case of death resulting directly and solely from this cause is recorded, but grave injuries, involving loss of sight, etc., have resulted. A case is referred to by Taylor[701] where sulphuric acid was poured into the ear of a woman while asleep by her husband. Death ensued, after six weeks, from disease of the brain resulting indirectly from the use of the acid.
The appearances of a burn by a mineral acid are distinguished from heat burns with little difficulty. The eschar which results is not dry and leathery, as in a burn by heat, but soft and readily sloughing away. There is no redness around the site of the injury, the color of the burn being uniform, and no blisters are formed. There is no blackening of the skin and the hairs are not scorched. The color of the skin around the injured portion may afford valuable evidence of the nature of the agent employed. Nitric acid produces a yellow stain, sulphuric acid a dark brown, and chlorohydric acid a brownish-yellow stain.[702] The clothing also is capable of affording characteristic evidence by the discolorations produced; and the destructive agent employed may be determined by a chemical analysis of the fabric.[703]
It is not possible to distinguish a post-mortem from an ante-mortem burn by an acid when no vital reaction has taken place.
THE CLASSIFICATION OF BURNS.
A classification of burns according to the severity of the injury inflicted is the most practical course. Upon this plan, burns may be divided into four general classes:
I. Burns in which the skin or subcutaneous cellular tissues only are injured.
II. Burns which involve the muscles, nerves, and blood-vessels.
III. Burns involving the internal organs and bones.
IV. Burns in which the other three classes are variously mixed.
Class I.—The skin in cases such as may occur from a brief contact with a hot body or water near the boiling-point shows a slight redness or scorching with no enduring mark. Pain is considerable.
Class II.—In the mildest cases the cutis is destroyed in its whole thickness, and the parts injured are occupied by eschars of a yellowish-gray or brownish color. The surrounding skin is reddened, and the formation of blisters occurs either immediately or after an interval of a few hours. In these cases a shining cicatrix remains after the healing, without contraction of surrounding parts. In the severer cases the subcutaneous cellular tissue and underlying muscles and nerves are destroyed. The blackish eschars formed are insensible and separate by suppurative process, leaving a granulating surface below. Extensive redness of surrounding tissues, with more or less vesication, is usually noted. The resulting cicatrices, together with the skin and adjoining structures, are prone to contraction, resulting in considerable deformity, according to location and extent. So great is the deformity in injuries of the extremities, or even some parts of the head and trunk, that extensive surgical operations become necessary to relieve it.
Class III.—Burns of this class are so severe that an immediately fatal issue is usually the result. Such instances involve a prolonged exposure to flame or to a source of intense heat. The appearances described as belonging to the preceding class are in part found here with the addition of charring or carbonizing the parts destroyed.
EFFECTS OF BURNS.
The effects of burns may be considered as I., Local, and II., Constitutional.
Local Effects.—In different instances the effects vary in accordance with the extent and severity of the burn. Redness, blisters, destruction of the cuticle and of the subcutaneous cellular tissue, blackening of the skin, scorching of the hair, and roasting of portions of the body are met with in varying degrees. In some severe cases all these are found upon a single body. The redness produced varies in intensity and extent, according to the nature of the agent producing the burn, its form, and the length of time the part was exposed.
Very soon after the infliction of the burn a special line of redness appears between the burned parts and the uninjured skin. This red line of demarcation is formed by intensely injected vessels and becomes a very important medico-legal sign in some cases. The vesication may be single or multiple, consisting of one or two large and full blisters or a number of large and small ones, scattered over the portions burned, some unbroken and still holding their contents, others broken and denuded of cuticle or with breaks from which their serum has escaped upon the surrounding parts. In some cases of burning cracks or fissures in the skin occur, due to the effect of the heat, making it dry and brittle and causing it to rupture by the movements of the patient (Case 8). These fissures are most frequently noted in proximity to the joints.[704] They resemble wounds, and it occurs occasionally that it is important to accurately distinguish their character. In some cases the skin only is fissured; in others the subjacent tissues are also involved. This difference depends upon the depth of the burn. In the first condition the skin splits, leaving the subcutaneous fat exposed, which in some instances is partially melted by the heat and flows out over the edge of the crack upon the surrounding skin (Cases 8, 13). The blood-vessels in such cases usually are not burned and, owing to their elasticity, remain stretching across the fissure (Case 14). The smaller may be seen by careful examination with a lens: they should[644] always be looked for. In the second class of injuries the vessels are involved in the burn and break with the cracking of the skin. The importance of careful observation of these fissures is emphasized in cases of apparent wounds associated with burning. It may be necessary to decide whether the wounds are the result of the action of heat as above described or were caused by some sharp instrument or weapon. Careful inspection of the edges of the wounds will show whether they are ragged, as the result of fissure, or clean-cut by some sharp instrument. The absence of evidences indicating hemorrhage upon the surrounding parts and the detection of uncut blood-vessels extending across the fissure will establish the differential diagnosis. Wounds of the above character resulting from the action of fire may exist on the same body with wounds of actual violence. It is important, therefore, in all cases to examine each wound with special care and record its position, shape, depth, and other characteristics.
Constitutional Effects.—As in all sudden and violent injuries, the effect of a severe burn upon the nervous system is very marked. This is manifest in the symptoms of “shock,” with pallor and coldness of the surface of the body, a feeble pulse, chills or shivering, and a tendency to collapse. In other cases, proving immediately fatal, these symptoms are followed by obstructed respiration with death from coma succeeding. In other cases convulsions precede death, while in such as are not immediately fatal a reaction more or less imperfect ensues upon the first constitutional symptoms.
Death from cerebral congestion or effusion may result before any definite evidence of reaction appears. In some instances pulmonary congestion or œdema occurs, with or without pleural effusion, terminating in death before reaction. This period usually covers the first two days. In some cases immediate death results from the depression produced by the severity of the pain. During the subsequent two weeks a period of inflammatory reaction succeeds, when inflammations of the thoracic and abdominal viscera, with ulcerative processes in some organs, are developed and induce a fatal termination (Cases 10, 11, 16).
Causes of Death.
The causes of death are due to several conditions. This fact is explained in part by the relation which exists between the cerebro-spinal and sympathetic nervous systems, and of the nervous supply of the surface to that of the internal organs, which in cases of extensive injury proportionately modify the conditions of the visceral organs. As death in burning results from various causes, it is convenient to consider them under two classes:
1st. Those immediately fatal.
2d. Those fatal after an interval.
The FIRST DIVISION would include cases in which the deprivation of fresh air and the presence of asphyxiating products of combustion (carbon monoxide and carbon dioxide) were the immediate causes of death by suffocation or asphyxia (Cases 9, 18).
Accidents in endeavoring to escape or injuries by falling walls or timbers may cause death immediately, and burning the body occur subsequently.
Immediate death may result from syncope or collapse from the violence of the shock to the nervous system by the pain resulting from the burns.
The SECOND DIVISION includes those conditions where death may result early, from a series of causes less immediate than those just mentioned.
Cerebral congestion and effusion, resulting in death from coma, is not unusual (Case 15). In this connection Taylor[705] cites a case of alleged poisoning by opium, in the treatment of a burn, in a child dying comatose, and emphasizes the undesirability of administering opium or its preparations to children in cases of burns of any severity. The danger claimed to exist is hardly to be considered. In the case referred to, Abernethy, who was a witness in the case, ascribed death to coma induced by the effect of the burn. The powerfully depressing influence of the pain in sensitive organizations and liability to death from shock therefrom must be remembered.
Inflammatory conditions of the respiratory tract or organs[646] are common results; pneumonia, bronchitis, and sudden congestion or œdema of the lungs are frequent (Cases 11, 15, 16).
Inflammation of the intestines, inducing peritonitis and ulcerations of the intestines with or without resulting hemorrhage, occurs as a frequent lesion (Case 10).
Gangrene or septicæmia causes death in other instances.
Exhaustion, from extensive and prolonged suppuration or from severe and long-continued pain and other conditions, terminates other cases (Case 12).
Legally, burns and scalds are included among injuries endangering life, but are not described as wounds. They may be considered dangerous according to the extent of surface which they cover, rather than the depth to which they involve the tissues.
The extensive injury to the sensory nerve structures and the suspension of function or destruction of a considerable portion of the perspiratory tracts render large superficial burns far more fatal than those confined to a small part of a limb, for example, which may be deeply burned. From a medico-legal point it is desirable to establish the fact of how large a surface must be injured to prove fatal. The effort to reduce the subject to a statement of an exact minimum area of square inches seems very objectionable and liable to lead to erroneous conclusions.
It is possible to make a general statement, subject to some qualifications, which may serve as a basis of conclusion, as each individual case must be considered in its own circumstances.
A burn involving two-thirds of the body may be regarded as necessarily fatal; but the injury of a much less proportion, even one-fourth of the surface, has resulted in death. The qualifications to be made in burns of less extent are pronounced. The part affected is of much importance. Burns of the trunk are more fatal than those of the extremities; and those of the genital organs[706] and lower part of the abdomen are especially so (Case 7).
The character of the burn, whether single and continuous or multiple and scattered over various portions of the body, is a very important modifying circumstance, involving the questions[647] of excessive pain and the difficulty in insuring necessary treatment for all parts injured.
The physical condition of the patient and sensitiveness of the nervous system to pain exert a powerfully determining influence. Burns in children and sensitive, nervous females are specially serious and call for an unfavorable prognosis.
Spontaneous Combustion.—Spontaneous combustion of the human body has been seriously discussed in this connection, and explanations of popularly reported cases have been attempted. The writer refers to the subject here for the sole purpose of stating that no trustworthy evidence of the possibility of any such condition or result exists.
Treatment.
In cases of severe burns the constitutional as well as the local conditions demand attention. Locally, a great variety of applications has been employed: starch, gum, oxide of zinc, solution of caoutchou, collodion, cotton wadding, a mixture of linseed oil and lime-water on cotton or lint, and many other agents are used. The important consideration is to exclude the air from and to afford a protective covering for the injured surface. The constitutional treatment varies in different cases; but its main object is to relieve pain, induce reaction from the shock, and support the depressed nervous system.
For the first opium or its preparations in proper doses is indicated. Alcoholic stimulants in some cases are demanded in addition. After the stage of reaction has occurred the therapeutics must be governed by inflammatory conditions; or later by the exhaustion from continued pain, suppuration, etc.
Post-Mortem Appearances.
In the EXTERNAL post-mortem examination of a burned body careful note should be made of the sex, probable age, and every circumstance leading to the establishment of the identity of the individual. The parts burned should be specially examined as to their condition, whether exhibiting redness, vesication, or charring. The amount of surface covered by the burns should be computed; also the relation of the burned parts to[648] those uninjured, whether separated by a sharply marked line of redness or merging into the sound skin without a line of demarcation. The condition of the blisters should be examined as to whether they are full or empty and their contents as to whether consisting of clear or turbid serum.
Internally.—In some cases no lesions are found on examination. These are usually cases where death occurred from shock or severe pain (Case 12). Ordinarily the mucous membrane of the respiratory tracts is congested. In some instances, however, no redness has been discernible. Where death occurred by suffocation and asphyxia, the trachea and bronchial tubes have been found to contain a dark smoky or sooty mucus[707] (Case 9).
The serous membranes of the brain, thorax, and abdomen are in many cases found reddened with effusions, more or less considerable, into the ventricles of the brain and the pleural, pericardial, and peritoneal cavities from the sudden inflow of blood from the surface, caused by the local injuries.
When the body has been badly charred or incinerated the skeleton usually remains, and it is possible to determine the age from the size and development of the bones and the sex from the shape of the bones of the pelvis. Careful search should be made for special articles of identity. False teeth,[708] a watch and chain, buttons, etc., have alone been sufficient to identify the incinerated remains (Case 23). Where the whole body and even the bones have been reduced to ashes, some portions of bone, etc., may be found on careful search. Sifting the ashes will give some pieces of bone, etc., which may be sufficient to disclose the presence of human remains[709] (Case 24). A chemical analysis of the ashes also will aid in establishing this fact. In cases where cremation of the body has been resorted to to conceal crime, the length of time necessary to entirely consume the human body may become an important question. A period of less than ten hours has been proven sufficient.[710]
Period of the Occurrence of Death.
As already indicated, death may occur from direct causes during the first forty-eight hours after the infliction of the burn, or may take place during a period extending from the second day to the fifth or even the sixth week. In the great majority of cases the fatal result occurs during the first five or six days. In some instances it may be important to establish the fact as to how long after the infliction of the burn the person may have survived.
Inflammation and suppuration would not ordinarily begin until about the third day, hence the existence of this condition would indicate that the person had probably lived two days or more; and the state of advancement of these processes would afford some further evidence. The existence of intestinal inflammations and ulcerations, which require some days for their appearance and development, would also give some indication of the probable time elapsing.
WAS THE BURN ANTE MORTEM OR POST MORTEM?
In describing the anatomical characters of a burn occurring during life, vesication, the formation of blisters, is regarded as a marked symptom.
While it is not an invariable result in a burn of the living body, it is so constant as to become one of the most important factors in answering the question as to the ante-or post-mortem infliction of the burn. Where the burn has been caused by a scalding fluid, or by burning of the clothing, or the direct application of flame, blisters are more likely to occur than where contact with a highly heated body has taken place. In the formation of a blister the cuticle is raised from the derma or true skin by the effusion of a highly albuminous serum, and the surrounding skin is of a bright or coppery red color. The time of the appearance of such a blister is not fixed. It may occur almost immediately or may not do so for several hours, an interval sufficiently long for death to occur from shock. It must be remembered that a burn inflicted in a condition of great depression of the vital powers with insensibility may be[650] followed by no vesication or redness, but upon reaction and return of sensation both redness and blisters may appear (Case 17). In the absence of blisters, therefore, it cannot be decided that for this reason the burn was post mortem. If from a blister formed on the living body the cuticle be carefully removed, the site of the blister will present an intensely reddened base. In the dead body, if the cuticle be removed, no red base appears, but the surface of the blister becomes dry and of a grayish color.
On the other hand, if the presence of blisters is noted, can it be concluded that the burn was ante mortem? While their presence affords reason for an affirmative answer, careful examination of the blisters as to their character and contents must be made in order to decide; the presence of apparent blisters is not alone sufficient (Cases 20, 18; Plate II.).
Elaborate experiments have been made in order to decide the possibility of producing blisters post mortem.
Leuret,[711] in experiments upon dropsical subjects twenty-four hours after death, shows the possibility of raising a blister post-mortem, but one which can be distinguished from one of ante-mortem production, in that it contains a reddish serum very slightly albuminous. He urges extreme care in deciding this question.
Christison[712] found it impossible to produce a blister a few hours after death. In a patient unconscious from narcotic poison, heat applied four hours before death produced a blister and a red line was formed around the burns. In the burns produced half an hour after death, in the same patient, blisters formed in two places only, and these were covered by dry skin and contained air. No redness appeared around them.
Champouillon[713] agrees with Leuret in his conclusions, from experiments upon dropsical subjects.
Kosack[714] considers blisters with albuminous contents diagnostic of burns during life, but states the necessity for care in deciding in the absence of other signs of reaction.
Wright[715] was able to produce blisters three and a half hours[651] after death containing a small quantity of pale serum. On the same body, similar experiments fifteen hours after death produced blisters containing no serum.
Caspar[716] states, as a result of experiments, that blisters may be produced by flame after death; that they result from vaporization of the fluid beneath the cuticle by the heat employed; that they are not found to contain serum and no line of redness is found at their base. The presence after death of vesications containing serum and surrounded by a reddish base is an evidence that the burn was inflicted ante mortem. He distinctly says: “It is quite impossible to confound a burn inflicted during life with one inflicted after death.”
Woodman and Tidy,[717] in an extended series of experiments, conclude that while blisters can be produced post mortem, they are readily distinguished from those formed ante mortem in containing no serum; and even in dropsical subjects, where blisters containing some fluid were formed, the presence of but a mere trace of albumin was shown; and, in all, no redness about the base of the blisters was produced, nor any appearance of redness after removal of the cuticle.
Taylor[718] has never observed vesications in post-mortem experiments on infants. He cites a case of drowning where the person, “pulseless and apparently dead,” was imprudently placed in a hot bath. Blisters containing bloody serum were formed over several portions of the body. He concludes that hot water on the living and recently dead body, so far as vesication is concerned, produces similar effects.
In experiments on the dead body immediately after death the writer has failed to produce any blister containing serum or fluid. The so-called blisters are produced by the rapid expansion and evaporation of the fluid beneath the cuticle over the portion to which the heat was applied, and differ distinctly from blisters caused during life, in the absence of serum or any redness of adjacent or subjacent parts (Plate II.).
Chambert[719] concludes that in living bodies and in dead bodies within twenty-four hours after death blisters can be produced, and that less heat will develop them in the living.[652] He specially emphasizes the difference, in the albuminous character of the contents, of a blister formed ante mortem and of one formed post mortem.
Jastrowitz[720] emphasizes the difference between blisters formed during life and those occurring in œdematous conditions.
Blisters are to be distinguished from the bullæ arising from putrefaction. There is little danger of confounding such cases. In conditions of putrefaction no redness or line of demarcation exists, and the green discoloration and other conditions of the skin will suffice to establish the diagnosis.
Schjerning[721] considers blisters containing highly albuminous serum as diagnostic of burns produced during life. In some conditions of depression of nutrition blisters occasionally form, but are not liable to be confounded with those caused by burning.
A second anatomical feature of much importance, even more so than vesication, is the condition of the skin to which the heat was applied. It assumes a dusky red color and a dry and parchment-like condition (Case 8). Surrounding this is an area of grayish-white skin bounded by a sharply defined and deeply injected red line, which in turn shades into the color of the surrounding skin. These features are more or less pronounced according to the degree of heat applied and to the length of time of contact; or, in other words, to the depth and severity of the burn (Plate I.).
MEANS OF DISTINGUISHING ANTE-MORTEM FROM POST-MORTEM BURNS.
Differentially, a distinction is to be made between the surrounding redness and the line of redness. The redness due to capillary distention is transient, disappears under pressure during life, and fades after death. The line of redness is permanent, changing but little under pressure, and remains after death. It is a vital reactionary effort, a true line of separation between living and dead tissue, formed in the same manner as the line of demarcation in sphacelus or gangrene. This line of redness, developed only during life and permanent after[653] death, is of great significance in cases with a medico-legal bearing. It has been already stated that in persons in a condition of depressed vitality the appearance of redness and vesication is sometimes very tardy and imperfect, and that death from shock or pain may occur before their development at all. They are vital processes and require time for their appearance in proportion to the activity of the powers of reaction. Hence in cases of burning resulting fatally where vesication and redness do not appear, the circumstances must be carefully considered before deciding that the burns produced were post mortem. With these qualifications, it may be stated that the presence of the red line is almost uniform in burns inflicted during life and absent in those occurring after death.
If upon a body bearing evidences of exposure to heat there be found blisters containing highly albuminous serum, and such blisters, after the removal of the cuticle, present a bright red base surrounded by a bright and sharp line of demarcation, with redness of adjacent surface, we are justified in concluding that the burns were inflicted ante mortem or, at farthest, within a few moments of death. If, on the contrary, the red line is absent and the blisters contain a thin watery fluid, with a yellowish and dry condition of their base after removal of the cuticle, the presumption is that the burning occurred post mortem.
Where a number of burns are found upon a body, the question whether they were produced simultaneously may be raised. This can be answered by examination as to their condition. If some show signs of recent infliction, while others are in conditions of suppuration or other changes which only occur after an interval, a difference of time in production would be probable. But if all present mainly the same conditions, the probability of their occurring at the same time may be concluded (Plates I. and II.).
The Condition of the Blood.—Special examination of the blood of persons dying from the effect of burns has been made by competent observers. While it is not at present possible to define an exact and constant condition, specially characteristic, some features of interest have been recently recorded.
The color of the blood has been variously reported; in some[654] cases as being of a dark color and in others of a bright arterial hue. Death by asphyxia or suffocation, by the deprivation of oxygen, and by the products of combustion, would be accompanied by a dark or venous hue of the blood. An atmosphere containing an excess of carbon monoxide, resulting from combustion, would cause death by apnœa with an arterial hue to the blood.[722] But other influences must be considered. According to Schjerning,[723] it is difficult to deduce positive conclusions from the condition of the blood. The changes induced by the spleen and kidneys, as well as the varying intensity of the degree of heat to which the body may be subjected, tend to render positive and constant conclusions from this source difficult.
Falk[724] refers to the bright red color of the blood found in some cases, and explains this condition in part by the influence of chemical changes in the tissues surrounding the vessels.
Wertheim[725] describes certain conditions observed by him and mentions an increase in the number of the leucocytes, together with the presence of hæmoglobin and melanin.
Hoppe Seyler meets with similar results and arrives at the same conclusions in his observations.
Ponfik,[726] on the contrary, is doubtful of the constant presence of some of these conditions and also of their diagnostic value.
Seliger[727] confirms the conclusions of Wertheim, in that he describes the presence of crystalline bodies and of dark discolorations (melanin).
Some spectroscopic analyses have disclosed the presence of bands additional to those of normal blood. The lack of uniformity of conditions described and of conclusions reached leaves the subject in a position of uncertainty. Examination of the blood of those dying from burns has not been so extensively and minutely followed as to enable us to decide questions which may arise in any case.
EXPLANATION OF PLATE II.
————————
FIGURE 1.—ANTE-MORTEM BURN.
Scald by steam from a boiler bursting, July, 1892.
From a photograph taken sixty hours after the accident. The injury covered one-half of the surface of the body. The red line is sharply marked; the extensive blisters formed are broken and their contents have escaped; the serum drying has produced yellowish discolorations; the blush of redness on adjacent parts is well marked. Death resulted on the fifth day.
FIGURE 2.—POST-MORTEM BURN.
Exp. 1. (Appearances after application of a tin can containing boiling water.) The cuticle was raised by expansion. The blisters contained no serum and no red line is developed.
FIGURE 3.—POST-MORTEM BURN.
Exp. 2. (Appearances after the application of iron at a dull red heat.) No proper blister formed; the cuticle was raised, as in previous experiment. There was no serum and no red line or redness of adjacent parts. The cuticle is charred at one point, where the iron was brought into contact with it.
MEDICAL JURISPRUDENCE—PLATE II.

Burn, Two hours after death, by Iron at a dull red heat.

Burn, Two hours after death, by Tin Can containing boiling water.

Burn by Steam, Sixty Hours after injury.
POST-MORTEM AND ANTE-MORTEM BURNS.
WAS DEATH ACCIDENTAL, SUICIDAL, OR HOMICIDAL?
Nearly all deaths occurring from burning are accidental, very few homicidal, and hardly more than a few exceptional cases suicidal.
It is important in cases of legal investigation to note the position of the body when found and its relation to the apparent source of fire; the parts of the body and clothing burned, etc.; evidences of violence should be carefully observed, such as contusions, fractures of bones, wounds of the soft parts, evidences of strangling, etc. (Case 22). These should be specially sought in the site of the burned portions, as burning and cremation of the victim are sometimes a resort to conceal homicide. In considering the character of the apparent wounds, it must be remembered that extensive injuries, resembling wounds, may result from the effects of fire,[728] and these must be carefully distinguished.
Inability to detect special marks of violence need not preclude the possibility of its commission and of its being a possible cause of death (Case 19). The parts burned, the character and depth of the burns, and their relation to the apparent source of burning, with consideration of their probable simultaneous exposure, are all circumstances of weight in forming an opinion. The position of the body in relation to the fire should also be considered. In accidental burning, except in cases of intoxication, epileptic seizures, or other sources of helplessness, the victim is quite likely to be found at a distance from the fire, owing to his efforts to escape.
————————
CASES.
Case 1. Death from Cold. Accidental (Dr. Hilty in Caspar’s Vierteljahrschrift, II., 1865, p. 140).—Male, æt. 52; intoxicated. Severe winter weather; death from exposure. Post mortem: Blood crimson; both sides of heart full; internal organs congested.
Case 2. Criminal Exposure to Cold (Ann. d’Hygiene, 1868, Vol. II., p. 173).—Girl, unmarried; sudden delivery when at stool. She stated that she had fainted, and found the child dead when she recovered.[658] The child had breathed and the cord was cut. No marks of violence. Evidence of death being caused by wilful exposure. Imprisoned.
Case 3. Ill-Treatment and Criminal Exposure (Ann. d’ Hygiene, Vol. VI., p. 207, 1831).—Man and wife tried for manslaughter of a child, æt. 11. Wife the stepmother. Starvation and ill-treatment by mother, followed by forcing the child, in a cold December day, to get into a barrel of cold water and remain there. Though removed by a servant, she was again placed in the cold water by the mother, death resulting. The woman was sentenced to life imprisonment.
Case 4. Sunstroke, High Temperature, etc. (Dr. A. Flint, Jr., New York Med. Jour., 1872, p. 168; Dr. Katzenbach, New York Med. Jour., 1873, p. 93).
Case 5. Scald, Drinking from a Tea-kettle. Accidental (Mr. Sympson, Brit. Med. Jour., 1875, June 19th, p. 809).—Boy, æt. 2½ years, drank boiling water from spout of tea-kettle. Inflammation of pharynx and glottis. Tracheotomy; recovered.
Case 6. Fatal Scald of Insane Person in a Bath (Brit. Med. Jour., April, 1871, p. 456).—An insane patient fatally scalded in a bath, through carelessness of an attendant. The charge of manslaughter brought against the attendant.
Case 7. Fatal Burn of Genitals. Accidental (Caspar, “Forensic Med.,” Vol. I., p. 315).—Female child, 2½ years, fell on a hot flat-iron. Genitals burned; died in eleven days. Vagina gangrenous; blood fluid; lungs anæmic and pale; trachea bright red, etc.
Case 8. Red, Parchmenty Skin, Cracks, etc. (Caspar, “Forensic Med.,” Vol. I., p. 307).—While a chimney-sweep was cleaning a chimney a fire was lighted below. Death. The entire skin was of a coppery red color, with yellow patches. No carbonization. Skin parchmenty, with fissures upon the edges of which the fat had melted and flowed out.
Case 9. Asphyxia. Sooty Mucus, etc. (Caspar, “Forensic Med.,” Vol. I., p. 314).—Two children, æt. 3 and 7, burned; death from asphyxia. The youngest, the girl, burned externally; the boy was not. Post mortem in both showed the trachea to contain frothy and sooty mucus. Lungs and vessels of thorax and abdomen distended with dark and fluid blood. Brain congested, etc.
Case 10. Burn of Body. Inflammation of Stomach (Amer. Jour. Med. Sciences, Jan., 1861, p. 137).—Superficial burn of lower part of body. Death on the thirteenth day. Post-mortem examination showed the stomach inflamed and the intestines also.
Case 11. Accidental Scald. Pleurisy (Caspar, “Forensic Med.,” Vol. I., p. 312).—Female child, æt. 6; scalded with a pot of boiling coffee overturned upon the side of neck, right axilla, thorax, and right arm. Death on the eighth day. Post-mortem examination revealed inflammation of right pleura, pericardial effusion, etc. Body anæmic.
Case 12. No Internal Lesion Found (Guy’s Hospital Reports, 1860, Vol. VI., p. 146).—Female, æt. 9. Burn of upper part of chest and arms by clothing taking fire. Death on the ninth day. Post-mortem examination revealed no lesion of the internal organs.
Case 13. Cracks and Fissures of Skin (Caspar, “Forensic Med.,” Vol. I., p. 314).—Male, æt. 83. Clothing caught fire; death. Body carbonized. On right side were fissures opening into the abdomen; the viscera could be seen, etc.
Case 14. Fissures, Vessels Crossing, etc. (Taylor, “Med. Jurisprudence,” Vol. I., p. 696).—Boy, æt. 2; death in three-quarters of an hour. On legs were fissures and lacerations near each knee. On right thigh a laceration 2¾ inches long, 1/6 inch deep and 1/4 inch wide; fatty tissue seen beneath. No blood effused; small vessels could be seen stretching across the fissures.
Case 15. Brain Congested, etc. (Caspar, “Forensic Med.,” p. 316, Vol. I.).—Boy, æt. 1-1/2 years, set fire to his clothing. Death in 1½ days. Post-mortem examination showed congestion of the brain, inflammation of the trachea, engorgement of the lungs with hepatization of the lower part of the right lung.
Case 16. Burn of Lower Part of Body. Death (same reference).—Woman, æt. 81; burn of lower part of body, including the gluteal region, the perineum and genital organs (external). Death after several days. Post-mortem examination showed the upper lobe of left lung in a stage of red hepatization, etc.
Case 17. Tardy Appearance of Redness and Vesication (Tidy, “Legal Med.,” Vol. II., p. 124, Case 15).—Woman, insensible from cold, had hot water applied in tins to her sides and feet. The flannel coverings became displaced and the hot tins came in contact with the body. No redness or vesication could be detected two hours afterward. The next day, when consciousness had returned and recovery from insensibility had taken place, the parts had become reddened and vesicated.
Case 18. Were the Burns Ante Mortem or Post Mortem? (Caspar, “Forensic Med.,” Vol. I., p. 317).—Woman intoxicated; clothing caught fire; death due to asphyxia. Some burns apparently caused during life and some after death. The case was decided upon the character of the vesications and their contents. Lungs and other organs normal. Right side of heart engorged with dark blood.
Case 19. Murder. Body Burned (Dr. Duncan, Med. Gazette, Lond., Vol. VIII., p. 170).—Man charged with the murder of his wife and attempting to burn the body afterward. The body was so extensively burned as to remove all means of deciding the cause of death. The man claimed that her clothing took fire when she was intoxicated. Persons in the same house had heard sounds of a struggle before smelling smoke and fire. Furniture was not burned, nor the house. The prisoner was found guilty of murder.
Case 20. Blisters. Was the Scalding Ante Mortem? (Taylor, “Med. Jurisprudence,” 8th Am. Ed., p. 411).—The body of an infant found in a saucepan, boiled. The prisoner admitted that the child had breathed. The boiling water had destroyed the means of positively deciding whether the child had breathed. Blisters found upon it contained yellow serum. Was the child living when put in the water? The prisoner was acquitted.
Case 21. Scald of a Lunatic in a Bath (Taylor, “Med. Jurisprudence,” 8th Am. Ed., p. 411).—Insane patient placed in a hot bath. Temperature 123° F. Death in collapse next day (1879).
Case 22. Criminal Burning, Strangling (Report of Profs. Liebig and Bischoff, of Giessen, March, 1850).—The man Stauff was tried at Darmstadt for the murder of the Countess of Goerlitz, whom he had attacked and murdered in her chamber, and then fired the furniture in order to conceal the crime. It was uncertain whether she had died from injury to the head or from strangulation. The tongue protruded and was swollen, as in cases of strangling, and maintained this condition. He was convicted chiefly on circumstantial evidence. After conviction he confessed that he had strangled her and then set fire to the furniture, which he had piled up about her.
Case 23. Murder. Body Burned. Identified (“Report of the Trial of Prof. Webster,” etc., Boston, 1850).—Prof. Webster killed Dr. Parkman and then burned the body, in portions, in a furnace in his laboratory. Search among the cinders of the furnace disclosed pieces of human bones and a set of false teeth which the dentist who made them recognized as made by him for Dr. Parkman, etc.
Case 24. Murder. Body Entirely Burned. Identified (the “Druse Case,” Trans. New York State Med. Soc., 1887, p. 417).—Mrs. Druse, with the compulsory aid of her children, killed her husband with an axe. The body was burned in a wood stove, with pine shingles. The ashes were thrown into a swamp near by. They were found and carefully sifted. Pieces of bone of various sizes, identified as human, were found, as also a few porcelain buttons, etc. A few hairs found, with stains, completed the identity. Experiments in this case showed that the body could have been consumed within ten hours. The prisoner was convicted of murder.
THE MEDICO-LEGAL RELATIONS
OF
ELECTRICITY.
BY
WILLIAM N. BULLARD, M.D.
MEDICO-LEGAL RELATIONS OF ELECTRICITY.
As the frequency of accidents caused by electricity is rapidly increasing, we have of late years been enabled to generalize in a manner never before possible in regard to their results, and although our present conclusions must be recognized as provisional and perhaps temporary—to be changed or modified in accordance with future knowledge—yet we have obtained a basis of fact on which we can securely rely. The general laws of injury and accident through electricity have been fairly well determined, although many of the details are not yet thoroughly worked out or understood. The advances of knowledge in this direction are so rapid that an article on this subject, if it deals too closely with details, is liable to become out of date almost before it has left the press. Like all large subjects when first made objects of general interest and investigation, and in regard to which we are on the threshold only of knowledge, the facts discoverable may lead us at any time in unexpected directions and open out new fields of thought and inquiry. We shall try to limit ourselves here, as far as possible, to proved facts, and leave questions doubtful or in dispute to be settled later; contenting ourselves merely with pointing them out and, perhaps, in some cases giving the facts on either side.
Electrical accidents and injuries may be divided into those which are caused by the atmospheric electricity—lightning proper, globes of fire, St. Elmo’s fire—and those produced through the agency of mechanical or artificial electricity—electrical machines, batteries, dynamos, etc. The effects caused by these different agents probably vary only in degree: the atmospheric electricity in the form of lightning, etc., being so much more powerful than the charges usually produced artificially as to cause some difference in the results.
RESULTS OF ACCIDENTS AND INJURIES FROM ELECTRICAL MACHINES AND CONDUCTORS.
Medical Electricity.—In the ordinary use of the mild forms of electricity employed for medical purposes, certain phenomena may at times occur, which, although not of any serious import or of long duration, may yet cause considerable inconvenience, pain, or discomfort to the patient or others, and may even be of some importance from a medico-legal point of view. We shall not enter here into the discussion of the proper methods of application of medical electricity, nor do more than point out that if these be not followed with care the patient may be not only not benefited, but made worse, and may even suffer considerable injury. The increase of pain caused by the improper application of certain currents is usually temporary and of minor consequence. But serious and lasting inflammations may be caused by the careless, ignorant, or injudicious use of the stronger currents internally, and metritis and peri-uterine inflammations have been not infrequently reported from the unskilled practice of the methods of Apostoli. These subjects, however, scarcely come under the scope of this article.
In addition, however, to these troubles we may have external injuries produced. Even in cases where the current amounts to not more than a few milliamperes burns may be caused by the ordinary electrodes of the galvanic battery. The faradic current when medically used does not, as a rule, produce any external injuries. Such might be caused by a spark from a static machine, but it would be due to gross carelessness, and is very unusual. Burns, however, from the use of the galvanic current are not very uncommon. They usually occur under the electrode after it has been for a few moments stationary in contact with the skin. They occur in certain patients with extraordinary readiness, especially in those with organic spinal lesions, and where the sensation is somewhat diminished, and where also some trophic lesion might be supposed to exist. They are not confined, however, to this class of cases, but may occur in any one if the electrode be retained too long in any one place, and especially if it be allowed to become dry. These[665] burns are peculiar in appearance and can usually be recognized at once. They are circular, as if punched out, about the size of a common pencil or a little smaller, comparatively deep, gray with perhaps a dark ring at the circumference, and frequently surrounded by a reddened area. The edges are sharp. Their peculiarity consists (1) in their painlessness and (2) in their size, regular form, their depth in comparison to their extent, and the sharp limitation of the area of tissue destroyed. One or more may occur under a broad electrode, and they are probably produced at those points where the contact is imperfect or the conduction in some other way impeded. They heal without much difficulty and leave no serious results.
Other unpleasant symptoms produced by currents in medical use may be mentioned for the sake of completeness, and also as an introduction to the more serious symptoms caused by stronger currents. Dizziness, vertigo, tinnitus, nausea, vomiting, and syncope are readily caused by even slight currents. The sensation of light in the eyes and the metallic taste in the mouth are the results of medical currents of ordinary strength when applied to the head or in its neighborhood, and stronger currents applied at greater distances cause these sensations. All the above symptoms may be readily caused by even slight currents, whether galvanic or faradic, passed through the head. The syncope thus produced is to be carefully differentiated from the syncope caused psychically by excitement or fear of the application of electricity. Hysterical women, and even persons who show no special signs of nervous instability, may faint at the suggestion of the application of electricity. I have seen a large, strong, well-built Italian man, perfectly sound physically, so far as could be detected, except some slight local neuralgia, faint from pure fright when the electricity was to be applied. But even the application of moderately severe shocks from the ordinary medical battery are not likely to produce serious results. These shocks are ordinarily caused by the opening or closing of the galvanic current, and are most severe when the current passes through some portion of the head. A still more powerful shock may be given by reversing the current in a galvanic battery by means of the commutator.
Currents of High Tension—Strong Artificial Currents.
Passing on now to the consideration of the stronger currents, we come to those used for mechanical purposes, for electric lighting, electric railways, and other analogous objects. These currents start from dynamos or from storage batteries, and accidents are caused by them whenever they are diverted from their proper course and are caused to come in contact with or to pass through any portion of the human body in any considerable strength. Accidents not infrequently occur from direct contact with the batteries or dynamos, but still more frequently they are produced in their circuit along the wires or transmitters. They may also be caused, as some of the most fatal have been, by contact with metallic or other readily conducting objects which have themselves accidentally come in contact with some portion of an electric circuit (usually wires) and have diverted the whole, or more usually a portion, of the current to themselves. Thus was killed a young man in New York, the clerk in a store, who while lifting the metal-edged cover of a show-case brought it in contact with the charged wires of an electric light and received an immediately fatal shock. As a rule, those meeting with accidents from dynamos or electric machines directly are employees of electric companies, who are presumed to have more or less knowledge of the risk of carelessness, or they may be workers in institutions or factories in which such machines are in use. Many of the accidents due to wires also occur to linemen and other employees of electric, telephone, or telegraph companies or of electric railway companies in charge of wires or electric outfit. So long as the current transmitters and terminals (wires, etc.) are properly insulated and in their proper position in relation to other conductors, it is unusual for accidents to occur, except in cases of gross ignorance or carelessness. Unfortunately, however, proper insulation is not always accomplished, and frequently wires and other transmitters are removed from their proper positions by accidents and otherwise. So long as and wherever the system of overhead wires exists, if there be among these wires any which are the transmitters of strong electric[667] currents, there is always a risk, and often a very serious one, that at some time or other one of these current-bearing wires will come into contact with some other non-current-bearing and ordinarily harmless wire in such a manner that the current of the first should be diverted, in whole or in part, on to the ordinarily innocuous wire, which thereby becomes at once charged and dangerous. Such an accident may be due to the displacement of either wire or to any other cause which brings the two in contact, either direct or indirect, at a point where the current-bearing wire is not sufficiently insulated. The current having once passed out of its proper circuit will, of course, follow the paths of best conduction, and may hence suddenly appear in unexpected quarters and produce the most dangerous and even fatal effects. It is accidents of this character which most frequently occur among the people who are neither employees of electric companies nor engaged in factories or buildings where electrical machines are employed.
Insulation of Wires and Other Electrical Transmitters.—We cannot mention here the various methods employed to insulate wires, as the general principles of insulation are well known. Electric wires even with very strong currents can be insulated and can be kept insulated if sufficient pains be taken and sufficient money be expended. But this is very expensive and in many cases is not done. Only partial insulation is attempted, and even this is not always carried to the degree intended or stipulated. Hence so long as overhead wires of various kinds exist, accidents from the transmission of strong electric currents along ordinarily harmless wires are liable at any time to occur, as practically little or no attempt at keeping the current-bearing wires covered with a thoroughly insulating material is in most cases made. It is usually deemed sufficient that glass or other insulators should be so placed that under ordinary conditions the wire will not come into contact with any conductor which may cause any essential part of its current to diverge. In most cases a so-called insulating material is placed over the wire itself, but this usually is insufficient at the outset or becomes so before very long and is then not renewed.
It must not be supposed, however, that underground electric wires or transmitters cannot produce accidents. On the contrary,[668] the current may be diverted from them to the gas or water pipes or to any other conductors which come into contact with them or can attract to themselves a portion of their current. Severe shocks have been experienced by persons attempting to draw water at their faucet from causes of this character. At the same time, so far as mere safety is concerned and freedom from electrical accidents, it would seem that underground wires are preferable to overhead wires.
Electrical wires have not infrequently come in contact with telegraph and telephone wires causing unpleasant results. Telephone boxes have been set on fire, and also telegraph boards and tables, and in certain cases what might have been serious conflagrations have been started in this manner. By means of proper arrangements on the telegraph and telephone circuits these dangers can be at least partially avoided, but there is always the risk that the automatic alarms and other contrivances do not act, and the still greater one that persons or things may come into contact with these charged wires and receive dangerous or serious injuries.
Electric Cars.—The danger from the overhead wires in the trolley system of electric cars would not be great were these wires properly supported, properly insulated, and properly protected. Each of these terms must be explained. Wires which fall for any cause whatever short of being intentionally removed cannot be deemed properly supported in the sense in which we use the term. Any one of these electric wires which falls is liable to produce serious injury to persons or animals (many horses have been killed by them), or to set fire to objects with which it comes into immediate or indirect contact, the amount of injury being in part dependent upon the nature and the condition (wet or dry) of the object and its position in relation to other conductors. Wires as dangerous as these car wires should be so supported that no ordinary accident, no condition of the weather, strong winds, or heavy falls of snow should be capable of wrenching them from their supports, and they should be placed in such positions and with such protection as not to receive blows from passing or falling objects.
Secondly, these wires should be properly insulated. This is to be understood to mean that all the wires which carry the electric current, or are liable to carry it, should be attached to[669] their poles or other support in such a manner that no appreciable quantity of electricity is under any circumstances liable to be diverted to the poles or supports, and in this way cause destruction or injury. In addition to this the side wires should be so covered that if any accident occurs, it will be difficult or impossible for the current to pass away from them to other objects. The middle wire on which the trolley runs cannot be thus covered, but must be left bare, and hence, if knocked down or brought into contact with properly conducting objects, must be the most dangerous; but on the other hand from its position it is less liable to accidents.
When we say that these wires should be properly protected we mean that such arrangements and contrivances should be used as will prevent them while in their usual position from coming into contact with dangerous objects, particularly with other wires. This may be accomplished by guard wires or in other ways. It is plainly of great importance that this should be specially cared for, and particularly in a city where there are many overhead wires, and perhaps a considerable number of dead or non-used wires. If the electricity comes into contact with one of these no one can tell where it may be transmitted or what harm it may do.
The principles which apply to these overhead wires of course apply ceteris paribus to all other electric overhead wires, and in like manner the statements made in regard to the diffusion or spreading of currents in underground wires are applicable to all methods of transmitting electricity mechanically through the ground so far as the conditions are similar. An electric current will always follow the path of best conduction, and where several paths are opened it will follow them proportionally according to the excellence of their conduction or inversely to the amount of their electric resistance.
We shall not enter here into any questions in regard to the diffusion of electricity, its transmission through fluids, water, air or other gases, nor shall we discuss the relations of good or bad conductors to electricity except so far as this relates to certain portions of the human body. An elementary knowledge of physics and electricity must be presupposed.
We can now enter more directly upon the immediate subject of this article, that is, the effect upon the human body of[670] severe or moderately strong currents of electricity derived from artificial sources. The accidents produced by these currents may be divided into two classes, the direct and the indirect. Under the direct we place all those conditions which are apparently produced by the action of the electricity itself, such as the general shock, the loss of consciousness, the burns, etc. On the other hand, all those accidents are to be considered indirect which are not primarily due to the action of the electric current, but are only secondary results thereof. These are largely determined by the immediate surroundings and conditions at the time. Such, for example, are the surgical injuries due to falls caused by the loss of consciousness produced by the electric shock.
Indirect Accidents.
These will be considered first, as they do not demand so detailed a description as the direct. They are traumatic in character and are the result either of loss of consciousness, momentary or lasting, or of the involuntary muscular contraction which may be occasioned by the electric shock. They are among the most frequent effects of severe electric shocks. These accidents consist in contusions, fractures, dislocations, wounds, and any other injuries which may be produced from sudden loss of consciousness while in a dangerous position. Death may readily occur either immediately or as the more or less delayed result of such injuries. If the person shocked falls into the water he may be drowned, or if into the fire he will be burnt. The varieties of such accidents dependent on the sudden loss of consciousness produced by the electricity are, of course, innumerable, and their occurrence must largely depend upon the position of the victim at the moment of the shock. We see, perhaps, most of these accidents in linemen on the tops of poles or houses or in other exposed places, but persons who receive shocks when simply standing on the ground or when sitting are not exempt from severe surgical injuries other than burns. They are often cast to the ground with great violence, and not infrequently are thrown to a distance of several feet. This is caused by the violent muscular contraction produced by the electric shock, and it may occasion, like any[671] violent push or fall, severe injuries from contact with the various objects against which they may be forced. Although much rarer, it is also possible that the violence of these muscular contractions may be such as of themselves to cause injury, as rupture of a muscle or tendon. As practically all these indirect accidents are traumatic and surgical in character, they do not differ from other accidents similar in kind, but otherwise caused, and are to be treated on the same general principles as these.
Direct Accidents.
Quite different from the indirect are the direct accidents; those produced by the immediate (direct) action of the electricity. These are of various kinds, which we shall consider separately. They may be divided into immediate and late symptoms, and they vary much according to the severity of the shock and the constitution of the patient, and the part of the body through which the electricity passes. The character of the current which gives the shock, whether constant or interrupted, also naturally has an influence on the effect.
General Principles.—A shock may be given in three ways with an ordinary galvanic battery. If the current be sufficiently strong, a distinct shock will be produced when the circuit is closed and again when the circuit is opened, while with a current of the usual strength for medical purposes, the sensation while the current is passing through the body steadily is much less and is often limited to a sensation of burning at the seat of the electrode. A shock may also (thirdly) be produced by a reversal of the current, and the shock thus caused is stronger for the same current than that produced in either of the other ways.
The strength of these shocks is shown both by the sensation produced and by the amount of muscular contraction caused. When now a shock is caused by a continuous or constant current which starts from an ordinary dynamo or other electric generator or storer, it is practically always caused by the opening or closing of the circuit, or, what is essentially the same, the diversion of a part or the whole of the current from its proper path to and through some portion of the human body causes a shock at the time of the entrance of the body into the[672] circuit and another at the time of its exit therefrom. Shocks from reversal of current when such current arises from a constant machine might occur, but only through some peculiar accident. Hence the shocks (distinguished from any other effects of electricity) which are received by the person coming into contact with a constant current are felt only at the moment of entering the circuit (closure) and of leaving it (opening). If a person introduces himself between the two wires of an electric circuit in which a constant current is used, in such a manner as to cause the current to pass through his body, he will feel the shock only at the moment when he touches the second wire and completes the circuit, and at the moment when he lets go one of the wires and opens the circuit (unless the current be so strong or be so placed that he can divert to himself sufficient electricity to cause a shock, or, in other words, close a secondary circuit in some other way). While the current is passing through the body, although it may burn and cause tingling and other unpleasant symptoms, there is no proper shock. In other words, an electric shock is caused only by a change in the amount of electricity passing through the body or a portion thereof.
If we now consider the effects of alternating currents, we find that we have another factor to deal with. The general principles are exactly the same, but inasmuch as the reversal shock is stronger than the closure or opening shocks, other things being equal, we are likely to receive a stronger shock from a current of the same force, and in addition to this, as in alternating machines the reversals occur with considerable rapidity, the person who becomes connected with this circuit receives a number of strong shocks within a short space of time. This is a much more serious matter than to permit a current of equal strength to flow through the body without change.
—The effect of this form of electricity on the human body is first stimulating and then tetanizing to the muscles. It consists in a very rapidly interrupted current, the shocks being at times so frequent that they are not singly perceptible. There is probably also a distinct difference in the action of this current from that of the galvanic current aside from its rapid interruption. This is not, however, of so defined a character as to enable us at the present time to distinguish in[673] man the results of severe injuries and deaths caused by this form from those caused by other strong currents. Practically this form of current is but little used, except in medical batteries and for the purposes of experimentation in laboratories.
Static electricity has, so far as we know, rarely or never caused serious injuries or death. The sparks produced in this way have sometimes caused burns, and it is conceivable that a strong electric current produced in this way might be dangerous. The symptoms could not be distinguished from those caused by other forms of electricity.
Summary.—The greatest source of danger from electric currents is the shock produced by them. In ordinary constant or continuous currents this is produced only at the moment of the opening and the closure of the circuit. In alternating currents a shock is also produced at each reversal of the machine. Faradic and static currents are rarely or never used mechanically or in the arts.
Resistance.—The resistance of the human body to electric currents has been very variously estimated.
The reasons for these variations are: (1) that the different tissues present different resistances; (2) that the resistance in the same tissue varies greatly under different circumstances.
The tissue which offers the greatest resistance and also practically the greatest variation is the skin, or, more properly speaking, the epidermis. The resistance of this is many times as great as that of the rest of the body, and when perfectly dry it is impervious to currents of great strength. Witz states that in using a Ruhmkorf coil with an estimated force of 250,000 volts in Guinea-pigs and rabbits, it is advisable to cut through the skin in order to apply the electrodes directly to the flesh, or, at least, to wet the skin thoroughly, otherwise the shock caused by the full strength of the battery (six jars charged from the coil) would not cause death. Various animals offer rates of resistance which vary somewhat apparently according to the nature of the animal, but are probably largely dependent on the conducting power of its tissues, that is, of its skin. The variations between the resistance of similar animals, according to the condition of the skin at the time of the experiment, are much greater than those which are found between animals of different species under similar conditions, or which are referable[674] to specific susceptibility. Mr. Harold P. Brown testified in the Kemmler case (Court of Appeals, State of New York—State of New York ex rel. William Kemmler against Charles F. Durston, agent and warden) that he had in the course of his experiments seen a horse weighing 1,320 pounds, with a resistance of 11,000 ohms, killed by an alternating current at 700 volts.
The resistance of the different cutaneous surfaces of the human body as measured by Jolly in Siemens’ units was from 400,000 down to 15,000 in the male and to 8,000 in the female (Siemens’ unit is to the ohm as 1.06 to 1.00).
Tschirfew and Watteville made the resistance from 80,000 to 3,000 ohms.
Experiments made at the Edison Phonograph Factory and Edison Laboratory in July, 1889, on 259 males between the ages of eleven and fifty-one, showed a resistance, measured between the hands immersed to the wrists in a solution of caustic potash independent of polarization, averaging 986 ohms and varying from 1,970 to 550 ohms.
The resistance of 236 men employed at Messrs. Bergmann & Co.’s Electrical Works in New York appears to have averaged 1,184 ohms and to have varied from 1,870 to 610 ohms. These measurements were also taken between the hands, which were washed with soap and water and then dipped in jars containing a solution of caustic potash. The battery consisted of four chromic-acid cells each having an E. M. F. of 2 volts.
As shown in all the experiments on animals and more especially in the cases of electrocution, the continuance or duration of the current has much effect on the resistance. As the current continues the resistance diminishes. Thus in the case of McElvaine the resistance between the immersed hands was at the beginning 800 ohms and at the end of the contact of fifty seconds had decreased to 516 ohms. In this case, when the current of 1,500 volts was applied from the forehead to the leg, the resistance was practically steady at only 214 ohms. Of course the small resistance in these cases (electrocutions) depends largely on the perfect contact secured.
According to the amount of resistance offered do the effects of severe shocks of electricity differ. This is shown especially well in the action of lightning, but is also true of powerful currents produced mechanically. If the resistance of the skin[675] be slight at the moment of entering the circuit of a strong current, the current will pass through it with comparative ease and without causing much injury; but if on the other hand the resistance is great, the current will be, as it were, momentarily retarded or stored, heat will be developed, and there will ensue a burning and charring of the tissue of a special kind. These burns occur principally at the places where the current is specially resisted, that is, at the point of entrance of the current to the body and at its point of exit. This is the cause of the frequent burns in the heel or sole of the foot in the case of those struck by lightning while standing, as the electricity passes away from the body into the ground and finds a strong resistance at the point of leaving the body. This is also the cause of the burns where the current leaves the body from any other cause, as from the contact or proximity of a metallic object. The greater the resistance so long as the current passes, other things being equal, the more severe is the burn. It is for this reason that in medical electricity we usually use wet sponges on the skin or electrodes moistened with salt and water or with other fluids which will assist in rendering the passage of the electricity through the skin more easy. Solutions of chlorid of sodium and of certain other salts do this.
The mechanical effects of currents vary thus according to the resistance encountered. They also vary according to the intensity or concentration of the current. If a current of moderate force be applied through a small metallic point, it will burn, pain, and produce active irritative symptoms, while if the same amount be applied over a large surface simultaneously, it may have little or no irritating effect. We have, therefore, three factors in determining the mechanical effect of any electric current on the body: (1) the condition of the body, that is, the amount of resistance which the current will encounter at its entrance and exit; (2) the amount and intensity of the current; and (3) the character of the current. For practical purposes of the more severe currents we have only to deal with the continuous and alternating.
SYMPTOMS.
Direct Symptoms.
The direct symptoms produced by powerful mechanical currents of electricity may be divided into three classes: I. The mechanical; II. The essential or internal; III. The mental or psychical.
These classes are fairly distinct, but they are not absolute, and certain symptoms are on the borders.
The most important mechanical symptoms produced by these currents are burns. These occur at all points of strong resistance externally, hence especially at the points of entrance and departure of the current. They vary from all grades, from the lightest possible, where only the fine hairs on the skin are singed, to those of extraordinary depth and severity. The characteristic burn from powerful currents is, however, well distinguished. It consists in a deep hole of various shapes with clear-cut edges surrounded by an inflamed area and containing in its cavity a mass of blackened tissue which only separates from the portions below after several days, and causes a wound which, though not very painful, heals very slowly. The severity of electric burns is often at first sight underrated, and their duration, when severe, is unexpectedly long. It occasionally happens that after a burn of this character appears nearly healed, the surrounding and, in appearance, healthy tissue breaks down, perhaps under a healthy skin, and a destructive process occurs which much retards recovery. This is evidently due to tissue destruction from a strong electric current of such a character as to produce necrobiosis without the external appearances of a burn. These burns are, perhaps, oftenest seen on the hands, but this is only because these parts are more likely to come into contact with the current. They may occur in any portion of the body.
Eyes.—The injurious effect of electric light upon the eyes has been carefully studied by several competent observers. So far as known it has been caused solely by the arc light. The symptoms produced by exposure of the eyes for a considerable period to the electric light may be slight or severe. In the slighter cases we find merely an acute conjunctivitis with a[677] slight central scotoma which passes off within twenty-four to forty-eight hours. The symptoms are those usual in acute conjunctivitis—photophobia, lachrymation, sensation of a foreign body under the lids, discomfort in the eyes, and swelling of the lids. In the more severe cases all these symptoms are increased; the photophobia and lachrymation may be intense. There is sometimes severe pain in the supra-orbital nerve, and occasionally a tendency to somnolence. In these cases we find an intense conjunctivitis with chymosis, a central scotoma which may render the patient for the time practically blind, and on ophthalmoscopic examination a congestion of the vessels of the retina and choroid, a neuro-retinitis, and sometimes even hemorrhages into the retina. There is sometimes peripapillary œdema and infiltration around the optic nerve. The pupil of the eye in these cases is usually much contracted. There is sometimes loss of epithelium from the cornea.
In certain severe cases there is produced in addition to the eye symptoms an erythema of the face. Bresse states that this erythema can be produced on the face, arm, or hand by exposure to the voltaic arc at a distance of thirty to forty centimetres. The blush grows deeper for three or four hours, then remains stationary for a time, and ends in desquamation leaving a very durable pigmentation. The erythema is accompanied by a sensation of smarting.
The strength of the light and the length of time required to produce these effects probably vary somewhat according to the color of the light. Emrys Jones states that he is informed that either excess or defect of current gives a less injurious light than the normal current; the excess gives a more violet, the defect a more orange light. On the other hand, Charcot considered that the harmfulness of the electric light was due at any rate in considerable part to the chemical or violet rays, and Bresse found that when violet rays were added to an electric light as by aluminium it was more injurious than before to animals. What part the brilliancy of the light plays in determining the pathological results is not yet fully settled. The heat, however, does not, as a rule, seem to have much effect unless in extraordinary instances where the cornea is burned.
Muscular Contractions.—Another effect of electricity which is externally visible on the human system is muscular[678] contraction. Slight muscular contractions are produced purposely in many cases in medical treatment therapeutically or for the sake of diagnosis. When the stimuli are sufficiently strong and follow each other with great rapidity, or when a strong continuous current is passed through the muscles, they are brought into a state of continuous contraction or tetanus, and in this condition they will remain for a long period or until the electric stimulus is removed. In cases where a severe electric shock is received as from an electric wire, the muscles which come in contact with the wire immediately contract and remain contracted while the current continues to pass through them. As a result of this we often find that when a severe electric shock has been received through the hands by means of a wire or other conductor the sufferer’s hands are involuntarily closed upon the wire or conductor, and cannot be unclosed by any voluntary effort until the current is stopped. While thus holding the conductor the hands are often very severely burnt. Under these circumstances a strong force is required to remove a person from a charged wire if the current be not turned off, and it can only be done at a considerable risk unless by those expert and provided with special means.
Not only the muscles immediately in contact with the conductor, but nearly all the voluntary muscles of the body may be thus affected by a powerful current. Another effect of this involuntary muscular contraction is the forcible muscular movements produced by the shock. As previously stated, when a sufficiently strong shock occurs, the voluntary muscles of the trunk and limbs may be thrown into sudden contraction in such a manner as to throw the person violently and forcibly on to the ground, or against some object or objects in the neighborhood. In this way one may be propelled several feet, and many varieties of surgical injury may be caused. Rarely the force of the contraction is such as of itself to rupture muscles or tendons, and it might even fracture bones or dislocate joints already predisposed.
Essential or Internal Symptoms.
We pass now to what we may consider the internal or essential conditions of electric shock, leaving the mental or psychical results for examination later.
When a person receives a severe electric shock, the symptoms are usually as follows: In the first place there may be little or nothing except a burn or burns, though usually there is some sensation at the moment of the shock. This may be a simple dizziness, and is often accompanied by the sensation of a brilliant flash of light before the eyes, and sometimes by a sense of impending danger. Usually, however, there is a loss of consciousness more or less complete and more or less lasting according to the severity of the shock and the character and course of the current. In the less severe cases this gradually passes away, and in many cases the patient, although weak and feeling shaken and tired, suffers no further ill effects beyond those of the burns and mechanical injuries. Sometimes there follows a general tremor which may last a few hours or for days, and occasionally a clonic rhythmical spasm of one or more extremities. The loss of consciousness may, however, be accompanied or followed by a condition of collapse, in which the pale face, profuse perspiration, cold extremities, and feeble pulse all suggest the administration of stimulants and restoratives. As a rule, in the stage of unconsciousness the face is reddened and rather cyanotic. The pupils are dilated as a rule and the respiration stertorous or absent; the pulse may be full or feeble, sometimes imperceptible for a time. The unconsciousness sometimes lasts for hours, and all means of stimulation, electricity, artificial respiration, rubbing, have to be applied before the patient can be restored. Sometimes this condition is succeeded by delirium (Moyer). In a certain number of cases the shock is immediately fatal, and in others the patients cannot be recalled from their unconsciousness.
The secondary results of the shock, aside from the injuries, may be very slight or again may be serious and lasting. They are far more apt to be of the first class, and when long or continued motor or sensory changes unconnected with injuries follow, we are justified in suspecting mental or psychical phenomena. One class of secondary results is the motor. In addition to weakness, unsteadiness and tremor of the limbs and trunk, it is not uncommon for the patient to suffer from grand rhythmical movements, at first, perhaps, of all extremities, but soon limited to the extremity or extremities which were most exposed or injured by the current. We have personally seen these[680] movements, and feel convinced that they can be distinguished from most of the ordinary forms of convulsive motions and tremors. The whole limb is moved at once and not separate muscles, and the movement is a large, rhythmical one, slow and co-ordinated, not at all suggestive of tremor. Movements of this character are sometimes seen in so-called functional disease (hysteria and allied conditions). They more nearly resemble the movements seen in some forms of Jacksonian epilepsy than any others known to me as occurring in organic disease, but I believe them in these cases to be always strongly suggestive, if not absolutely significant, of functional affections. A case reported by Dr. Robert, of El Paso, well illustrates this condition. The patient, a male, twenty-eight years old, received a shock through a telephone wire. When seen first, reaction was slowly taking place, the entire muscular system was in clonic convulsions. Temperature 97°; pulse rapid and of low tension; respiration 50; no cerebral symptoms. An hour later the movements were limited to the left upper and the right lower extremities, and there was pain running from the region of the spine down the left arm. Twenty-four hours after the shock, temperature 99.5°; respiration 40; pulse 100. Had slept well, but the movements in the left arm had never ceased. The next day these motions were limited to the muscles of the forearm, and on the fourth day they had wholly ceased. These convulsions consisted in extensive motions of the whole extremity or of muscles or muscle-groups, and not of simple tremor. If the movements were forcibly controlled, severe pain ensued.
Next to the motor symptoms the sensory are the most important. Pain not infrequently occurs after the recovery of consciousness in the affected limb; it is apt to be sharp, severe, darting and neuralgic in character. This may last at intervals for some days, a dull ache occurring at first between the intermissions. It disappears of itself in time without lasting effects.
Hyperæsthesia may exist at first. Should this continue, or if anæsthesia not due to secondary traumatic conditions should appear later, we should be inclined to place these symptoms in the third class.
Of other symptoms occurring in accidents from currents of high potential, those which seem to be due to the direct action of the electricity are not serious. Buzzing in the ears and a[681] metallic taste in the mouth often occur at the very beginning before the consciousness is involved. Nausea and vomiting frequently occur later. There is often considerable dizziness and vertigo. Patients sometimes complain of sensations as of an electric shock running through the body which occur without cause some hours or even days after the real shock. Some of these sensations are certainly to be reckoned under the mental or psychical symptoms. Susceptibility to the effects of electricity, of lightning, and of thunder-storms, though undoubtedly in many cases psychical, has probably in some cases an actual foundation. This is certainly the case in lightning stroke. On the other hand, in the large majority of cases of electric accidents no such result follows, and in many we are expressly told that such a result was looked for but not found.
The temperature, as affected by the electricity alone and not as secondary result of injuries, is not always easy to determine. It seems to be in most cases lowered at first, being in that of Moyer 97.5° and in that of Robert 97°. Later it may rise to a certain extent, usually to not more than 101°, but here again the influence of traumata is difficult to separate.
The pulse may be full and soft or weak and compressible. It is frequently very feeble, sometimes almost imperceptible, and often rapid. It is apt to remain rapid and somewhat soft for days in severe cases.
The respiration is at first rapid in severe cases unless the shock be so great as to cause its cessation. This rapidity remains for a varying period and then disappears.
As a typical case of the results of shock from an electric wire, we will mention the one reported by Dr. F. W. Jackson. The patient, a man twenty-two years old, came in contact with a live electric-light wire, touching it with his hands. He was thrown a distance of about ten feet and then back again, “swinging back and forth two or three times.” His hands were in contact with the wire about three minutes, when the current broke and he fell to the ground unconscious. Was seen two hours later by physician. Temperature 100°; pulse 100, strong and bounding; pupils dilated; headache; nervous and irritable; reflexes increased. The headache was accompanied by insomnia which continued for three days, after which it disappeared, and he resumed work apparently none the worse[682] for his accident. The palmar surfaces of both hands and the anterior surfaces of the forearms were blackened from the tips of the fingers to a point midway between the wrists and the elbows, and these parts were exceedingly sensitive to the touch. The least irritation of the muscles would cause them to contract violently. This condition ceased on the second day. The current was from a fifty-light arc circuit of about 2,100 volts; 6.8 amperes. The accident took place out-of-doors on a very rainy night. The amount of electricity which the patient received was, as in all such cases, very uncertain.
FATAL CURRENT.
The amount of current which will produce a fatal effect varies with the character of the current and with the points of contact. Currents passing through the head or those which affect the pneumogastric nerves are much more dangerous than others of the same character and equal strength passing through one extremity, for example.
The same current will, of course, also produce different effects, according to the facility of its conduction into and through the body, and this depends again on the completeness of the contact and whether the body or the portion thereof concerned enters directly into the circuit or only forms, as it were, a partial conductor and diverts a certain portion only of the current to itself. Again, the condition of the epidermis, whether dry or wet, and the position of the person in relation to good conductors, metallic or otherwise, has much effect.
If the skin and clothes be wet, the resistance to the current is lessened and it passes more readily into the body. In the same way, if a person stands in close relation to a good conductor and places his hand on one wire of a high-tension electric circuit, he will receive a much more severe shock than if not connected with such conductor. Thus a person standing in a pool of water (water is a good conductor), and more strongly if standing on the metallic rail of a railway track, and touching one wire of an electric circuit with one hand, receives a much stronger shock than if he were standing on dry land, or if his boots were rubber or he was otherwise insulated.
The accidents most frequent in practice are those in which[683] the current has been partially diverted from its original course and the person has not entered fully into the circuit. In such cases it is not usually possible to estimate accurately or even approximately the amount of current which the person has received. No calculations can, therefore, be based on these accidents. Again, we find that a person may be seriously or even fatally injured by a current which another person seems to bear with impunity.
D’Arsonval in 1887, in France, advised 500 volts as the maximum for the continuous current and 60 volts as the maximum for the alternating current which might be employed without special permission.
Our only accurate knowledge in regard to fatal currents comes from the experience derived from electrocutions. From these it appears that an alternating current of 1,500 volts is deadly if it passes through the body for more than a few seconds and if the contact is perfect.
Death.—Death may ensue immediately as the result of an electric shock without any evident preliminary symptoms, or it may occur later, either as the direct result of the shock or as the consequence of the exhaustion produced by the burns and other injuries, or directly from the injuries themselves. If death does not occur immediately and if appropriate means of aid are at hand, the sufferer usually survives and the effect of the electric shock gradually passes away. The danger after this arises from the burns and other injuries, and almost all the deaths not immediate are the results of these.
ELECTROCUTION.
Electricity has been adopted in the State of New York as the agent for the execution of condemned criminals. This has given rise to much discussion as to what form of current were the best adapted for this purpose and as to what amount were required to produce death at once and painlessly. These questions may now be regarded as practically settled, at least so far as regards the purposes mentioned, and we shall only refer incidentally to the discussions and their results.
Early in 1890 a committee consisting of Dr. Carlos F. MacDonald, Dr. A. D. Rockwell, and Prof. L. H. Landy made[684] a report to the superintendent of prisons at Albany in regard to the efficiency of the electrical appliances and dynamos placed in the State prisons of Sing Sing, Auburn, and Clinton. This report gave details of various experiments made on animals to determine the amount of current and the time required to produce a fatal result.
On the 6th of August, 1890, occurred the first electrocution, that of William Kemmler, alias John Hart, at Auburn Prison. Dr. MacDonald in his official report to the governor in relation to this says: “It is confidently believed that when all the facts in the case are rightly understood the first execution by electricity will be regarded as a successful experiment. As might have been expected at the first execution by this method, there were certain defects of a minor character in the arrangement and operation of the apparatus. But in spite of these defects the important fact remains that unconsciousness was instantly effected and death was painless.”
The efficiency, rapidity, and painlessness of this form of execution have been confirmed by the later experiences. Up to the present date (May 26th, 1892) eight condemned criminals have been executed in the State of New York. Apparently all the officials who are intrusted with the care and inspection of this subject seem satisfied that this is, on the whole, the wisest, easiest, and most effective form of death thus far practised among civilized nations. The Medico-Legal Journal of New York, in printing the official report of the recent executions of four men made by Drs. C. F. MacDonald and S. B. Ward to the warden of Sing Sing Prison, states that it furnishes “indisputable evidence of the fact (1) that the deaths were painless and the victims unconscious from the instant of contact; (2) that they were certain and unattended with any of the revolting scenes so frequently witnessed at the scaffold; (3) that the method is humane so far as inflicting physical pain or suffering, and from all sides considered infinitely preferable to the death by hanging; and that so long as capital punishment for murder exists in New York, we need not desire to change the method of punishment.” These claims would seem to be thus far substantiated.
The value of this method of execution is now beyond doubt. When properly performed it is rapid, painless, and not repulsive.[685] The criminal has probably no physical sensation of pain or discomfort due to the mode of death from the moment the first shock occurs. Since the rapidity of the transmission of the electric current through the body is in these cases much greater than the rapidity of the transmission of sensation, it seems just to conclude that no sensation from the electricity reaches the consciousness. The only distress suffered by the criminal is the unavoidable mental suffering natural to his position.
The mechanical means employed in electrocution are practically the same at Sing Sing, Clinton, and Auburn prisons. A special room is provided for the purpose, which should be, if possible, in the basement with a concrete floor: this room must be of sufficient size to admit readily the criminal with the attendant officers, the warden and other officials in charge or on duty at the execution, and the witnesses for whom seats are usually provided at a little distance from the criminal’s chair, and also to allow of plenty of room for the management of the electrical apparatus, and a good space around the chair in which the criminal is placed. The electrical plant consists of an alternating-current dynamo and its accessories, placed wherever may be convenient, according to the arrangements of the buildings of the institution, but connected by means of wires with the switch-board in the execution-room. In the execution-room also should be the voltmeter, the ammeter, and such other instruments of measurement or precision as may be required. In charge of these and of the switch-board during the execution is the electrical expert, an official paid by the State of New York. Means of communication by electric bells or otherwise are, of course, arranged between the execution-room and the engineer in charge of the dynamo, so that the current can be produced as desired.
The chair in which the criminal is placed is made of stout beams of oak and is securely fastened to the floor and insulated. It is perfectly plain, with broad arms and an upright back, which latter can be tilted backward a little by means of a special arrangement and firmly fixed in the desired position. This is accomplished by means of a bar of wood which is firmly attached at one end to the lower portion of the back and runs forward thence parallel to the seat of the chair and alongside of[686] it; to the anterior end of this is fastened a perpendicular bar running downward, which can be raised or lowered at will, and securely fastened at any height. As this is raised or lowered, it raises or lowers the anterior end of the horizontal beam and correspondingly lowers or raises the opposite end to which the back of the chair is attached, thus moving the latter. When the anterior end of the horizontal bar is raised the posterior end is lowered and the back of the chair is straightened. Attached to the upper portion of the back of the chair is a head-rest, which can be raised or lowered as desired: it may, as in the case of Kemmler, have a horizontal arm which projects forward and from which the head-electrode may be suspended. The chair is also furnished with broad leather straps firmly attached, two of which pass around the body, one around each upper arm, one around each lower arm, and one around each leg. There is also a broad conjoined or compound strap which passes over the head, encircling the forehead and the chin and securing the head firmly to the head-rest. When these straps are properly adjusted and fastened, any marked degree of movement is impossible. The adjustment and fastening of these straps can be performed very rapidly, in practiced hands taking not more than forty seconds.
The electrodes used have varied slightly in different cases. In the case of Kemmler they each consisted of a bell-shaped rubber cup about four inches in diameter, with a wooden handle through which passed the wires into the bell to end in a metallic disk about three inches in diameter, faced with sponge. The upper electrode was so arranged as to rest firmly on the top of the head, where it was held closely by means of a spiral spring: it was attached to the horizontal arm of the head-rest, a sliding arrangement shaped like a figure 4. The lower electrode was in this case attached to the lower part of the back of the chair, and projected forward at a level with the hollow of the sacrum. There was also connected with it a sliding arrangement, and a spiral spring which in connection with a broad strap around the prisoner’s lower abdomen rendered contact secure.
In the later executions these electrodes have been somewhat modified and differently applied. The head-electrode is now so formed as to cover the forehead and temples, and can be easily fastened in this position without a spring. The lower electrodes[687] have been applied to the leg in each case, sometimes apparently to the calf and sometimes more to the outer side, where they are securely strapped. They are made of such a shape as to cover a considerable portion of the surface in this region. It is not a matter of importance to which leg the indifferent electrode is attached, but they have actually been applied in most cases to the right leg, though in some they were attached to the left. They are thoroughly moistened, usually with a solution of salt and water, and a drip may be arranged so as to keep them wet during the passage of the current or other means employed to this effect.
The electromotive pressure, as shown by readings of the voltmeter by Professor Laudy, in the cases of Slocum, Smiler, Hood, Jugigo, and Loppy, varied from 1,458 to 1,716 volts. The ammeter showed a variation of from two to seven amperes.
The alternating current in the case of McElvaine made roughly 150 periods per second.
The number of contacts made in each case and the duration of each contact were as follows:
| Number of Contacts. |
TIME, SECONDS. | ||||
| 1st. | 2d. | 3d. | 4th. | ||
| Kemmler | 2 | 17 | 70 | .. | .. |
| Slocum | 2 | 27 | 26 | .. | .. |
| Smiler | 4 | 10 | 10 | 10 | 19 |
| Hood | 3 | 20 | 20 | 20 | .. |
| Jugigo | 3 | 15 | 15 | 15 | .. |
| Loppy | 4 | 15 | 11 | 15½ | 10½ |
| McElvaine | 2 | 50 | 36 | .. | .. |
| Tice | 4 | Total time, 50 | |||
In the case of McElvaine, the first contact of fifty seconds was made through the hands, the second contact of thirty-six seconds from the head to the leg. The hands were immersed in cells containing tepid salt water, connected respectively with the opposite poles of the dynamo. Kennelly states that in this case, with the hands immersed and the electromotive force at 1,600 volts, the current began at 2.0 amperes, and in fifty seconds had increased to 3.1 amperes, indicating a resistance between the electrodes of from 800 ohms at the beginning to 516[688] ohms at the end. In the second application from the forehead to the leg with an electromotive force of 1,500 volts, the current amounted to 7.0 amperes during the thirty-six seconds contact, indicating a resistance practically steady at 214 ohms.
Alternating currents of from 1,600 to 1,700 volts and upward may be considered fatal currents, and as capable of producing death when contact is perfect. Dr. MacDonald goes so far as to say: No human being could survive the passage through his body of an alternating current of more than 1,500 volts for a period of even twenty seconds, contact being perfect.”
The physical phenomena caused in the body by electrocution as at present conducted are comparatively simple, and such as we should logically expect. The instant the body of the patient enters into the circuit of the current, all the voluntary muscles appear to be thrown into a condition of violent contraction which continues so long as the current lasts, and on cessation of the current is replaced by a condition of extreme muscular relaxation. All consciousness is apparently lost immediately on the application of the current. This probably has never returned in any case, but on the removal of the body from the circuit of the current the relaxation of the muscles causes movement, and sometimes, as in the case of Kemmler, slight spasmodic movements of the chest have occurred. The pupils in this case were dilated. The condition of contraction and rigidity is renewed at each new application of the current, to cease immediately when the current is removed.
In Kemmler chest movements and possibly heart-beat occurred after the first contact, the former perhaps half a minute after the cessation of the current.
In Slocum there were chest movements and radial pulsation after the first contact. In Smiler no movement of the chest, but radial pulsation after the third contact. In Jugigo a slight fluttering of the radial pulse when final contact was broken, which rapidly ceased. In Hood no movement or pulse-beat.
In some of the patients superficial burns have been caused by imperfect contact of the electrodes, either on the head or at the position of the lower electrode. In Kemmler’s case the cerebral cortex was somewhat affected under the head-electrode.
The practical effect of the application of the current to the criminal fastened in the death-chair, as seen by the bystander,[689] is that immediately on its reaching him the whole body is straightened and rendered rigid in extension, the extremities tend to straighten out, and the face may grow red and turgid. There is reported at times swelling and turgidity of the neck. The whole body remains in this tetanic, stiffened condition until the removal of the current, when all the muscles relax and the body sinks back into the chair in a state of complete muscular collapse.
MENTAL OR PSYCHICAL SYMPTOMS.
The third class of results which are found after electrical shocks from high-tension currents are the mental or psychical. By the use of these terms we do not wish to imply that they are voluntary. They are, however, so far as our present knowledge of pathology reaches, largely functional. This is precisely the class of cases which, when resulting from railway accidents, are placed under the head of railway-brain or railway-spine. They may be considered in the present state of our knowledge as traumatic functional neuroses, though it is probable that when our means of examination and investigation are more complete we may succeed in discovering a visible or perceptible lesion. The symptoms affecting motion and sensation in these cases are frequently accompanied by others of an emotional character, and in many cases there seem to be partially or wholly voluntary conditions and symptoms with the involuntary. There is in many cases a characteristic loss or diminution of the force and power of volition, but in others this is not perceptible.
These conditions are so well known when produced by other causes that we do not consider it proper to enter into a full consideration of them here, but we cannot leave this important subject without a few general remarks.
No form of affection or disease has caused more discussion among the medical profession or figured more prominently in the courts than this, and even now there are many questions in relation to these conditions still under dispute. Our own view, confirmed both by observation and experience, is that the tendency in New England, at least, has been on the whole to underrate the severity, the duration, and the amount of suffering caused by these conditions. That because there have been cases[690] of malingering, of deception, and of rapid cure after the receipt of damages, and because in addition to this a certain visible emotional and at times apparently controllable element exists, the profession, and above all the laity, are led to conclude that this forms the essential condition and basis of the disease. On the contrary, in a very large proportion of cases the symptoms are such as cannot possibly be voluntarily assumed; they produce extreme discomfort and often much suffering for the patient, and frequently last for years, rendering their victims incapable of carrying on their former occupations.
Fortunately in the patients suffering from electric shock the severer forms of these affections are not so common. In most of the cases reported recovery has been more or less rapid. Cases in which previous hysteria or neurasthenia have existed are more liable to these manifestations than persons of a previously equable nervous constitution, but these latter are by no means wholly exempt. To consider these conditions, as is sometimes done, as the fault of the patient seems to us both unwarrantable and unjust.
LIGHTNING.
We now come to the consideration of the action of electricity in another form, that of natural electricity or lightning. The effects of this are practically the same as those of the forms previously described, except such differences as seem to be fairly accounted for by the vastly greater force of the currents with which we have to deal. Injuries and deaths from lightning stroke have been recognized and described for many centuries, and we have now a large collection of careful observations on them. They occur in most temperate regions with comparative frequency. In France the number of deaths from 1835 to 1852 inclusive (eighteen years) was 1,308. In England, including Wales, there were in twenty years, 1865 to 1884 inclusive, 416 deaths. In 1846 Mr. Eben Merriam, of Brookline, wrote to Mr. Arago that in the three last years about 150 persons had been killed by lightning in the United States. In thirty years, from 1855 to 1884 inclusive, we find 101 deaths in Massachusetts from this cause.
Exposure.—Injuries and deaths from lightning may occur[691] in various places and under various conditions. The severe lightning strokes are popularly supposed to occur only during thunder-storms, and in this latitude this is undoubtedly, as a rule, true, but lightning strokes are reported to have occurred, particularly in the South, from a clear sky, and there seems no reason to doubt that this may happen. It is said also that dangerous discharges from the earth to the atmosphere may take place at a considerable distance from an atmospheric storm. As a rule, the lightning is more likely to strike some tall object, as a tree or a tower or steeple, and for this reason, and to avoid injury from falling branches, the shelter of trees should not be sought during thunder-storms if lightning stroke be dreaded. Ships at sea are frequently struck by lightning, partly perhaps on account of the height of the masts and partly on account of the metal in or on them.
Lightning obeys the same general laws as the other forms of electricity and naturally follows the paths of least resistance. Persons, therefore, who are in the neighborhood of or in contact with good conductors are in more danger of injury by lightning than when surrounded by or in contact with poor conductors. The proximity or contact of a large metallic object exposed in a thunder-storm is consequently more or less dangerous. On the other hand, the absence of tall objects or of specially good conductors of any kind does not insure safety. In many cases persons in fields are struck, and cases are related of persons struck on the prairies in the West. In Fredet’s case a shepherd was found dead in the midst of the barren moors (landes) in Southern France.
More accidents appear to occur directly to persons out-of-doors than to those in houses or other buildings. When inside buildings, persons struck are usually near an open door or window through which the lightning enters, and they are more exposed to danger from this source if there be some metal object or good conductor in the vicinity. Persons carrying or wearing metallic objects render themselves thereby more liable to be injured in this way.
Not only does the liability to injury from lightning vary somewhat according to the exposure or position of the person, both in relation to the free access of the atmospheric air and to the contact with or neighborhood of metallic objects or other[692] good conductors, but also the severity of the injuries may be largely dependent upon what they are wearing or carrying and the condition of their clothing at the time. If the clothing be wet it will act as a good conductor, as will also any metallic object about the person. We have already referred to the action of metallic objects upon the passage of the electricity to and from the body and to the condition of the skin in relation thereto. The laws of conduction and resistance are precisely the same for the electricity of lightning as for the other forms. Hence the greater the resistance to the electricity at the points where it enters or leaves the body, the deeper will be the burn. Thus we find not infrequently that the lightning, in its course from the head to the feet, meets with a chain or a truss, and almost invariably at least a portion of the current follows this, causing a deep burn where it again passes into the skin. All the external burns of the lightning, except the initial one, are determined by the position and conditions of the body, the clothing, and the conductors near. All electricity obeys the same law and, roughly speaking, follows the path or paths of least resistance.
The clothing worn by a person when struck by lightning may be acted upon in the most various ways. Sometimes it is wholly stripped off the unfortunate sufferer, who, as in a case reported by Cook and Boulting, may have to be protected with sacks or other hastily improvised coverings. In a case reported by Nason, a girl of thirteen was struck while in the street and most of her clothes stripped off and torn to shreds, and the top of her hat, which contained steel wires, was torn from the brim. In the case of Wilks the body was stripped entirely naked and absolutely nothing left on except a portion of the left arm of the man’s flannel shirt. The clothing is sometimes torn to the finest shreds, like those of a mouse’s nest, as described by Van Horn, and in another case (Claes), where the patient was struck while on board ship, his woollen jacket was torn into fine bits, which stuck to the ropes, and the deck was covered with fibres of wool as fine as those of cotton-wool. In this case the woof of the trousers was said to have been wholly destroyed, while the web was untouched.
The clothing is also often burnt. Not only are holes burnt in it as is usually the case at the point where the lightning[693] strikes and at the point where it leaves the body, but it may be set on fire. It may be found smoking or in flames.
Of all portions of the clothing injured, perhaps the coverings of the feet are the most frequently so, as the electricity is very apt to leave the body through the feet, and the resistance opposed is great. Hence the boot or shoe is frequently injured. Sometimes it is pierced as by a bullet, or a large hole is torn in it, or it may be torn to pieces or reduced almost to lint, while the foot remains uninjured. It may be torn, shrivelled, and burnt. In one case the soles of the shoes had disappeared; in another the leg of the boot was clearly divided from the sole and both straps were torn out; while again in another the shoe was carried wholly off.
The amount of injury to the clothing does not necessarily correspond to the amount done to the body. A person may be killed by lightning while the clothing is uninjured. On the other hand, the clothing may be torn to pieces, carried away, or even partially burnt, while the portion of the body underneath remains unhurt.
Symptomatology.—The symptoms of stroke by lightning resemble, in a general way, those due to high-tension currents of electricity. As in the case of the latter, they can be divided into the direct, produced immediately by the lightning itself, and the indirect, or secondary, produced through the medium of other factors.
In the milder cases the person struck feels dazed and benumbed and may or may not lose consciousness for a short time. At the moment struck they may have the sensation of a blow, and they often see a blinding flash. On recovery of their faculties there may be a temporary anæsthesia or weakness of one or more extremities, which rarely lasts more than twenty-four hours. There is a general shock to the system, sometimes slight loss of memory for a time, and occasionally nausea and vomiting. There are often discolorations of the skin of medium extent, and frequently burns and blisters. These persons have usually received the stroke on one extremity or have escaped the full force. In the more severe cases the patient loses consciousness immediately and may continue unconscious for some hours. He passes into a condition of collapse with rapid, feeble pulse and cold extremities, and the[694] pupils are dilated. On recovery of his senses the same symptoms as in the less severe cases, only more pronounced, are found. The loss of memory may be marked and the intellect temporarily weakened, while the weakness and anæsthesia of the extremities persist longer. The external injuries, burns, and wounds are liable to be more severe.
In the fatal cases where death is directly due to the electricity it is usually instantaneous or at least without recovery of consciousness. It may be caused by shock or by apoplexy, i.e., intracranial hemorrhage or by the direct effect of the electricity on the brain. Of course death is often due to burns or to indirect traumatic injuries.
The indirect traumatic injuries caused by lightning are due either to the loss of consciousness of the patient, which causes him to fall and thus sustain injury, or to the direct action of the electricity upon him, knocking him down or throwing him to some distance, sometimes with great violence, or lastly, and perhaps the most frequent cause, to the impact or pressure of objects which are torn or cast down by the electricity and by striking or falling on a person produce great injury. Thus persons have been killed by the fall of buildings, sheds, or trees which were struck by the lightning, or their branches. Of course all kinds of traumata may be produced thus.
The direct external injuries caused by lightning are burns, subcutaneous hemorrhages, discolorations and markings of the skin either dendritic or metallic, lacerations or wounds.
Burns occur in nearly all, perhaps all, severe cases of lightning stroke. They may be of any or all degrees, and may extend over very small points or over the whole or nearly the whole body. They may consist in a simple singeing of the hair, or they may be very deep and extend to the bone. As before stated, the deep burns are found at the points of resistance to the current, at its points of entrance and exit from the body, and, to a lesser degree, at all points where its course is impeded. This occurs wherever the clothes are fastened tightly or pressed against the body, hence especially at the neck, waist, knees, and sometimes at the ankles. The position of the burns is determined, therefore, by the point at which the lightning strikes the person, the position at the moment, and by the arrangement of the dress and the presence of metallic substances.[695] In the large majority of cases the upper portion of the body is the part first touched by the lightning, and thence it descends along the body to the ground. We are apt, therefore, to find a severe burn about the upper portion of the body, the head, neck, or shoulders; then a scorching, singeing, or burning, more or less severe, in the form of a stripe or stripes more or less broad down the body: the burns being deeper where the clothes are tighter or where metallic objects come into contact with or are near the body; and finally a deep burn at the nearest point of contact with the ground, usually the heel or some portion of the foot.
The burns, however, vary greatly. The eyes may be burnt and severely injured or destroyed. The lightning has been known to enter the mouth and burn the mucous membrane within. The deeper burns not infrequently assume the form of holes. In Heusner’s cases about twenty whitish-gray spots, varying from the size of a lentil to that of a pea, were found on the soles of the feet. The hair is usually singed and may be burnt off in large areas, or wholly as in a case reported by Bernard.
Wounds.—These may be direct or indirect. We shall speak here only of the first. Like burns they occur usually at the points of greatest resistance, that is, the places of entrance and exit, but they may be found in any part of the body. They may be clean-cut, as if made by a sharp knife, or they may be lacerated and ragged with the edges contused or burnt. They may consist of holes which look as if they had been punched out.
Contusions or ecchymoses. These may also be produced directly by the lightning, and like burns and wounds are most apt to occur where the resistance is greatest. They may be of considerable importance in a medico-legal sense, as in Fredet’s case, where there were ecchymoses on the neck similar to those produced by the fingers of a hand applied for strangulation. In the case related by Cook and Boulting the right side of the body appeared like an exaggerated example of post-mortem staining. There are sometimes found also dark-brown spots, small or large, which may be soft and, when cut, containing fluid blood, or they may be hard and like parchment, dry, and bloodless on section.
Closely connected with these are the so-called dendroid or dendritic marks, which are dark-colored reddish bands or stripes, often more or less dichotomously branched, not disappearing under pressure, found on the bodies of those struck by lightning. Though usually of the form mentioned, they may assume other shapes, as that of an irregular star with zig-zag rays. Balfour has figured an excellent example of these.
Metallic staining of the skin has been known to occur where metals were in contact with it at the time of the lightning stroke. These stains may be permanent and are due to the introduction of the finely divided metal. Richardson has succeeded in producing this artificially in animals. He found two conditions required, that the metallic conductor should be sufficiently fine to offer resistance to the current and that the current itself should be an electric discharge of low tension.
Loss of hair is said to have occurred from lightning, though the hair was not burnt. One case has been reported where after a severe stroke all the hair on the body is said to have fallen out.
Symptoms.
Under this heading we shall consider only such symptoms as are, so far as can be ascertained, the direct result of the electricity and not those secondary to injuries.
We will consider first those relating to the nervous system.
Loss of Consciousness.—This occurs to a greater or less extent in all but the very mildest cases. It varies throughout all degrees from a slight momentary benumbing of the faculties to the most profound stupor or coma. It may then last hours or even days. On recovery the patient is apt to have some loss of memory, to be dazed and confused for some time, and a certain obtuseness or blunting of the intellectual faculties may persist for a considerable period. This loss of consciousness is often accompanied by flushing of the face and dilatation of the pupils, or on the other hand the patient may present all the symptoms of collapse.
Loss of memory in regard to the lightning stroke after recovery of consciousness is not rare. It is frequently complete so far as any recollection of the lightning goes, and there may be no remembrance of the thunder-storm. Sometimes a defective[697] memory persists together with general mental impairment (James).
Mental Disease.—A condition of mental impairment lasting at least weeks or months may occur. Mania and the delirium of terror are said to have occurred.
Various symptoms of the disturbance of the nervous equilibrium are not uncommon. Among these we may mention tremor, insomnia, and nervous dread of thunder-storms and of electricity. There is no doubt that some persons who have been exposed to lightning stroke do, at least for a time, become unusually susceptible to the influences of atmospheric electricity.
Loss of Motion—Paralysis.—This is a very frequent result of a stroke from lightning. Hemiplegia is not uncommon. In Bonnet’s case the patient was struck on the head by the lightning, which caused a lacerated wound in the left temple, but did not injure the aponeurosis. On recovery of consciousness the patient was found to have a left hemiplegia involving the face and both extremities accompanied by a diminution of sensation over the left half of the body. The sensation became normal in two days, but a partial hemiplegia remained permanently. In the case of Durand there was a nearly complete right hemiplegia with accompanying hyperæsthesia and some affection of speech. Deglutition and mastication were difficult, and there was persistent hiccough. There was photophobia and hyperæsthesia. The patient improved in two weeks and finally recovered. There is often a temporary hemiplegia.
Nearly all forms of paralyses of the extremities may occur. We may have paralysis of all the extremities or of both arms or legs, or monoplegias. Paraplegia occurs not very rarely. It is usually of short duration. It may be accompanied by paralysis of the bladder. Single muscles or muscle groups only may be affected.
Ptosis may occur with paralysis of other branches of the third nerve, causing diplopia. Facial paralysis occurs also alone; in one case it lasted only twenty-four hours, in another one month.
Difficulty in mastication is sometimes found, but much more frequently difficulty in deglutition is reported.
Retention of urine, dysuria, or incontinentia urinæ may all[698] occur, and there is sometimes a paralysis of the rectum, usually temporary, and sometimes obstinate constipation, which in one case was combined with paralysis of the bladder and monoplegia.
Aphasia in various degrees and various forms of dysphasia or difficulty in speech are not uncommon. They are apt to be temporary.
Loss of co-ordination in the lower extremities with partial paralysis of bladder and rectum is reported.
Convulsions.—Epilepsy may be brought on by lightning: this would be more likely to occur in a person previously subject to epileptic attacks. Hysterical convulsions and spasms may also be produced, both immediately and as a more remote result, usually in persons predisposed. Tetany and catalepsy are said to occur.
Clonic spasms of the whole body and convulsive movements of the limbs are not very infrequent. In some cases a marked sensitiveness remains for a time in the limbs struck, so that if touched they are immediately thrown into clonic spasms.
Disturbances of Sensation.—Pain occurs in nearly all cases. It is most frequently a secondary result of the burns and other injuries. Not rarely, however, it exists as a direct symptom in the form of a burning or stinging neuralgia in the limb or limbs affected. Sometimes the first sensation on the recovery of consciousness seems to be pain all over the body or confined to some portions only, but the amount and character of the pain, aside from that produced by the injuries, varies much. One patient had a burning pain in the back and leg lasting only half an hour after recovery of consciousness. In another case there were pains all over at the end of the first week. On the whole, severe pain in some or all of the limbs, and less commonly in the head, without paralysis and lasting some days is not rare. In one case reported by Paige the patient had intense pain in the head, neck, arms, and chest; that in the head was constant, severe, and lasted seven days, elsewhere less constant.
Pain in the arms accompanied by paralysis and anæsthesia and lasting three months has been reported.
Headache is not rare as a later or secondary symptom.
Disturbances of sensation other than pain are not rare.
A certain amount of hyperæsthesia almost always exists in the portion affected immediately after the stroke. This is often so marked that it cannot be wholly due to the burns or other injuries. It is usually very temporary and ceases in a few hours. In some cases a permanent or lasting sensitiveness to the action of electricity is said to remain.
Anæsthesia, loss or diminution of sensation, occurs either with or without paralysis. In the cases reported by Balfour, one boy said he could not feel his legs and another that his arms were cut off. In a case reported by Free there was loss of sensation in the right upper extremity from the elbow to the fingers and in the left lower extremity from the knee to the toes. As a rule, the loss of sensation is temporary and quickly passes away, but it may last, in company with paralysis, for some time. In such cases either an organic lesion or a traumatic neurosis is to be suspected.
Paræsthesiæ are very common after lightning stroke. Most frequent, perhaps, is the subjective sensation of numbness. Tingling, formication, and the sense of “pins and needles” may occur.
Reflexes.—As a rule, the deep reflexes seem to remain normal. The superficial reflexes of the parts affected are at least temporarily increased.
Special Senses.—Sight.—Affections of the eye. The eye and the surrounding parts may be directly injured by burning. We also find many serious conditions caused by the lightning the pathology of which will be considered later. When a person is first struck he may perceive a flash of light or a ball of fire before losing consciousness. While unconscious the pupils are usually dilated, but react. Sight may be at once totally lost, but this is usually only temporary. There may be amblyopia; photophobia, lachrymation, and pain are not uncommon for a time. Cataract may be produced and other severe ocular affections may result.
Hearing.—Sudden and total deafness may be caused by lightning, as in the case of Cook, where perforation of both tympana was found. This may prove to be only temporary, as in the case of Nason, where the patient, though totally deaf at first, is reported as hearing fairly on the fifth day; on the seventeenth day, however, the hearing was still dull. The[700] deafness may be permanent. With deafness tinnitus is apt to occur. Hyperacustia, or extreme sensitiveness to noise, has also been reported in several cases.
Smell and Taste.—The person affected sometimes has noticed a smell resembling that of sulphur, and this has also been said to have been apparent to others. A metallic taste in the mouth is not rare.
General Symptoms.—When first struck by lightning and while still unconscious, the patient has usually a flushed and reddened face, with dilated pupils. Immediately following, or perhaps without this preliminary stage, appear the symptoms of collapse. Cyanosis may occur, and the patient may appear to be asphyxiated.
Fever, not caused by injuries, may sometimes occur, but certainly not to any extreme degree. In many cases the temperature when taken was normal, and even in cases of severe stroke without serious surgical injury the temperature has not risen above 101°. In these latter cases it is hard to say how far the temperature is affected by the burns which are always present.
The pulse is sometimes slow, sometimes rapid and feeble, or almost imperceptible; at times it is irregular.
The respiration is apt to be labored. In Paige’s case there was marked dyspnœa. It may be almost imperceptible. It is sometimes slow and sometimes rapid.
Nausea and vomiting occur often after recovery of consciousness. Vertigo and reeling may exist from various causes.
It is probable that seminal emissions may occur at the moment of shock.
Menstruation, when present, may be checked or may continue. Pregnant women do not necessarily abort.
Pathology and Pathological Anatomy.
A few words must be said in regard to the pathological conditions which may be directly produced by lightning and can be detected during life. The burns, wounds, ecchymoses, dendritic marks, and other external signs have already been fully considered.
Certain pathological changes, however, have been found in[701] the eyes which are capable of being verified during life. In addition to swelling and œdema of the lids, to the injuries from burns and to the various paralyses of the ocular muscles, changes in the tissues of the eye itself may occur. In the first place we may find corneal opacities and adhesive iritis. Iridocyclitis may occur. Cataract formation is not rare, and its causation has given rise to many theories. Optic neuritis and neuro-retinitis are sometimes found; and we have sometimes optic atrophy. Structural changes in the choroid may also be caused by lightning. Rupture of the choroid, hemorrhage from the choroid and retina, and partial detachment of the retina may occur from the shock without the patient being struck by the lightning and without rupture of the external tissues.
Ears.—Perforation of the tympanum is reported in more than one case.
Autopsies.
We shall consider here the pathological conditions found in deaths from electricity, whether due to artificial or to atmospheric sources. The results are or may be the same in either, so far as we now know, and it is probable that the action of the electricity is practically the same in either case, only varying as regards the strength and tension of the current.
Rigor Mortis.—This has generally been found in cases of death from artificial electricity. In the case of Jugigo, who was executed by electricity, it was present four and one-half hours after death. As regards its occurrence in death by lightning and the rapidity of its onset, there has been much discussion. It is certainly present in many cases, and the probability is there is nothing diagnostic in regard to it in deaths by lightning. When absent, its absence is probably due to the presence of some external factor and has no relation to the form of death. We have, on the other hand, no proof that the rapidity of its onset is increased.
Coagulation of the Blood.—It has been observed frequently that the blood of persons struck by lightning does not coagulate readily. Sullivan states that in certain cases of complete disorganization after lightning shock the blood is left fluid and incoagulable and its color changed to a deep black.[702] In one of the cases of death from artificial electricity reported by Grange, the heart was found sixty-two hours after death to be filled with liquid blood of a rosy vermilion color, which quickly became darker on contact with the air. A spectroscopic examination of the blood showed the normal lines of oxidized blood reducible by sulphydrate of ammonium. In a case reported by Matzinger the blood as submitted was black and perfectly fluid, the corpuscles, both red and white, were normal, and no fibrin was detected. In those executed by electricity the blood seems to have been fluid and not in any way remarkable.
There seems to be no evidence that the bodies of those dying from electricity in any form suffer unusually rapid decomposition.
The only absolute sign of death from electricity is decomposition of the tissues, but the usual signs are to be relied upon to the same extent as in ordinary cases of death.
Internal Organs.—In the cases of death from mechanical electricity no changes in the internal organs other than those due to accidental traumata have been found, except a considerable degree of congestion and sometimes minute hemorrhages in the heart substance beneath the pericardium and into the pulmonary air-vesicles and pleura. In one of Grange’s cases the heart was filled with liquid blood; in the other it was completely empty, the right ventricle collapsed, the walls of the left ventricle hard and contracted.
Careful autopsies were made in the cases of the criminals executed by electricity, but no important changes caused by the electric current have been detected either macroscopically or microscopically. A few petechial spots (Tardieu’s spots) are apt to be found underneath the pericardium in the heart tissue and sometimes beneath the pleura. The organs were not extremely congested. In the case of Jugigo the vessels of the spinal cord and its membranes contained if anything less blood than usual. In this case the amount of blood found in the brain seems to have been about normal, the vessels of the dura were moderately dilated and those of the pia “in a medium state of congestion.” In the case of Kemmler the portion of the intracranial contents underneath the head-electrode was somewhat affected directly by the heat, the meningeal vessels[703] in the dura were carbonized, and the brain cortex was sensibly hardened to one-sixth of its depth, “where there was a broken line of vascularity.” The post-mortem temperature in this case seems to have remained unusually high, being 97° F. in the fourth ventricle and 99° F. at the back of the neck three hours after death in a room where the temperature was only 83°.
In autopsies after death by lightning the results are in general analogous. The brain and its membranes may be anæmic or congested. Effusions of blood may be found beneath the dura or in the brain substance itself, due to the laceration or injury of vessels. Rupture of the brain is said to have occurred, and Phayre reports a case in which the left hemisphere was entirely destroyed and changed into a dark gray homogeneous fluid mass, only a small portion of the corpus callosum remaining. No extravasation of blood, laceration of the vessels or membranes, or injury of the bones was detected.
Ecchymotic spots are frequently found beneath the serous membranes, pericardium, pleura, and peritoneum.
Schmitz states that parenchymatous inflammation of the internal organs may occur, and Sullivan reports a case where the stomach was found to be gangrenous over a large surface, the patient having lived several days. Cases of rupture of the heart, the liver, and the spleen are reported.
THE MEDICO-LEGAL CONSIDERATION
OF
Death by Mechanical Suffocation
INCLUDING
HANGING AND STRANGULATION.
BY
DANIEL SMITH LAMB, A.M., M.D.,
Pathologist Army Medical Museum, Washington, D.C.; Professor of Anatomy Medical
Department Howard University, Washington; Secretary Association of American
Anatomists; Late Acting Assistant Surgeon United States Army;
President of Association of Acting Assistant Surgeons
U. S. A.; Member of Learned Societies.
MECHANICAL SUFFOCATION.
Suffocation is the name applied to both the act of and condition resulting from the deprivation of atmospheric air. If the deprivation is due to mechanical interference, the term MECHANICAL SUFFOCATION is used.
Mechanical interference may be by pressure upon or obstruction within some portion of the respiratory tract. Suffocation by pressure upon the neck is called hanging when the constricting force is the weight of the body itself; and strangulation in all other cases. German writers designate strangulation by cords, ropes, and the like as Erdrosselung, and by the hand as Erwürgung; French writers do not make this distinction. In English the word throttling is probably oftener applied to strangulation by the hand than by cords.
The term suffocation is also applied in a special sense to the act and result of pressure on the mouth, nose, or chest and abdomen, stopping the breathing; or of obstruction within the respiratory tract; or of pressure upon the tract from the œsophagus, etc.; or of breathing of irrespirable gases.
Strangulation is almost always homicidal, hanging almost always suicidal, and suffocation (limited) usually accidental, but also often homicidal.
Strangulation may be admitted, therefore, as including all cases of suffocation by pressure on the neck, whether by cords or the hand; but excluding hanging.
It will facilitate the study of the subject if we use the word ligature as a general term to cover the many forms of cords, ropes, etc., used in strangulation and hanging.
The word GARROTING is often used to indicate the forcible compression of the neck by the hands of thieves. The assault is usually made from behind, and the victim is robbed while the throttling proceeds. The brevity of the process explains why death is not more frequent. The word garroting comes from the Spanish; criminal execution in Spain and Italy is[708] usually by means of the GARROTE, a steel collar which is tightened on the neck of the condemned by a screw. The notorious thugs of the East Indies used sometimes a soft loin-cloth, at others a lasso or long thong with a running noose. In Turkey and some other Eastern countries the bowstring is a common mode of execution.
An examination of the reported cases of strangulation and hanging shows a great variety of forms of ligature: cords, ropes, thread, thongs, lassos, flexible twigs, bamboos, leather straps, girdles, turbans, fishing-nets, collars, cravats and other forms of neckwear, bonnet strings, handkerchiefs, sheets, etc. Women have even strangled themselves with their own hair (Case 34). Stones, sticks, coal, and other hard substances have sometimes been inserted in the ligature to increase the pressure (Cases 36, 38, 42, 43, 44). Drunken and otherwise helpless persons have been strangled by falling forward with the neck against a firm substance.
STRANGULATION.
Symptoms and Treatment.
The symptoms and post-mortem appearances in strangulation will vary, according as the deprivation of air is sudden or gradual, partial or complete; and whether there is coincident pressure on the great arteries, veins, and nerves of the neck.
The deprivation of air disposes to asphyxia; pressure on the great arteries by cutting off the supply of arterial blood to the brain disposes to anæmia of the brain and syncope; pressure on the great veins, by preventing the return of blood to the heart, to congestion of the brain and coma; pressure on the great nerves, the pneumogastrics, to syncope. Statistics of hanging show that in about seventy per cent of cases death is by a mixture of asphyxia and coma. While it is probable that the proportion is less in strangulation, yet it is also probable that a mixed result frequently occurs.
Asphyxia is from α priv. and σφίξις, pulse—absence of pulse. Apnœa from α priv. and πνέω, I breathe—absence of breathing. Syncope, συνκοπή, a faint; suspended animation from sudden failure of heart. Coma, κῶμα, deep sleep. Richardson[729] makes[709] the following distinction between asphyxia and apnœa: Asphyxia is difficulty of taking in breath; apnœa is breathlessness. There is asphyxia when the blood from the heart can go to the lungs, but there is no access of air; apnœa, when there is access of air, but the blood fails to reach the lungs. In asphyxia the lungs obstruct the circulation; in apnœa the obstruction is in the heart. In asphyxia the air cannot reach the blood; in apnœa the blood cannot reach the air.
Quinquaud[730] and Fredericq[731] conclude from experiments on animals that asphyxia is due to the deficiency of oxygen, not to the accumulation of carbon dioxide.
Page[732] divides the phenomena witnessed in an animal killed by simply depriving it of air, without interfering with the blood-vessels of the neck, into four stages:
First. A short stage. (In the human subject this stage could scarcely last longer than fifty seconds, which is said to be the extreme limit of the most expert divers. The breath can be held longest if a number of deep breaths have previously been taken, so as to surcharge the blood with oxygen.)
Second. The stage of “besoin de réspirer,” when the want of air begins to be felt; the animal makes vigorous and violent efforts to overcome the obstacle. This stage may continue for three to four minutes.
Third. Unconsciousness supervenes with irregular and spasmodic movements; efforts at respiration continue.
Fourth. Efforts at respiration cease, but the heart still beats. This stage may last from two to four minutes. Hofmann[733] says that it may last a half-hour. In new-born infants, asphyxiated, it may be quite long.
The post-mortem appearances in such an animal were as follows: the lungs were pale, reddish, not much distended; there were a few dilated air-cells toward the anterior border; hemorrhages irregularly dispersed over the surface of the lung, varying in number and size. The right cavities of the heart contained dark fluid blood, the left were empty. The pulmonary artery and systemic veins, even the smallest branches, were gorged with dark blood. Page adds that when the[710] great vessels of the neck are interfered with death may occur “by coma, syncope, and even asthenia.”
Colin[734] made twenty-five experiments on horses, and records three of them as follows: they were all strangled with a hempen cord at the middle of the neck. The first was quiet till the second or third minute, then there were violent movements and strong efforts to dilate the chest; at four minutes, spasms; four and one-half minutes, quiet; six minutes, pupils dilated, tongue hanging out, limbs flaccid; blood black. Second horse: Carotid artery denuded to observe its action. In fifteen seconds, blood nearly black; four and one-quarter minutes, no pulsation in carotids; five and one-half minutes, no respiratory movement; six minutes, heart-beat ceased, except feeble contraction of auricles, which continued till twenty-first minute. Third horse: In five minutes respiration ceased; tracheotomy performed, but there was no attempt to breathe; eight minutes, heart ceased to beat. Similar results were obtained in ruminants and in small animals, except that the larger animals lived longer than the smaller.
Faure[735] made the following experiment on a large dog. He tied a cord tightly round its neck; for fifty-five seconds it was quiet, then suddenly it became agitated, threw itself against the wall, rolled on the ground, twisted itself; bloody mucus escaped from the nose and mouth; the teeth were ground together; urine and fæces were passed. The efforts at respiration became very rapid. It fell dead at the end of three and one-half minutes.
The symptoms of strangulation in the human subject resemble closely those just described as occurring in the dog.
The FIRST or PRELIMINARY STAGE lasts a variable time, according to the suddenness and completeness with which the access of air is prevented; it lasts until there is a demand for the air. In a case of homicide, injuries may be inflicted on the victim in this stage which may have an important bearing on the cause of death. Blows on the head may cause unconsciousness, or even apoplexy; upon the stomach, may cause syncope; stab-wounds may tend to cause death from hemorrhage.
The SECOND STAGE begins with the demand for air and lasts till unconsciousness supervenes. It is characterized by frantic efforts to breathe, efforts in which the entire body takes part. If the subject is conscious, he is intensely so; the expression of the face is intense; the eyes may protrude, the hands be clinched; the memory is unusually active, and the events of a[711] lifetime may rapidly pass before the mind in a few minutes. The tongue may be thrust between the clinched teeth and bitten; and urine, fæces, and semen may be discharged.
The THIRD STAGE usually appears suddenly, and is characterized by unconsciousness and irregular involuntary movements, i.e., spasms; these may end in opisthotonos; the veins become turgid, and hemorrhages may occur from the eyes, nose, mouth, throat, ears, and into the connective tissues of the lungs, pleura, pericardium, etc. The circulation of venous blood in the arteries is shown by the general lividity, especially where the skin is thin, as the lips and tips of fingers. Hofmann[736] states that coincident with the oncoming of unconsciousness and convulsions the respiratory effort becomes expiratory, followed still later by inspiratory efforts.
The FOURTH STAGE begins with the cessation of spasms and of efforts to breathe. The subject is quiet, but the heart still beats. The stage ends with the cessation of the heart-beat.
Discharges of semen, urine, and fæces may occur in the first and second stages, from terror; in the second and third from the general agitation, and in the third and fourth from paralysis.
Strangulation according to Bernard[737] causes a rise in temperature, varying from one to two degrees (Cent.). He thinks that this is due to the changes from arterial to venous blood, especially in the muscles.
Lukomsky[738] concluded from experiments that in asphyxia both arterial and venous pressure is increased in the systemic circulation, but diminished in the pulmonary artery. The highest degree of blood pressure coincides with the strongest respiratory movements, especially expiration. He also concluded that the Tardieu spots (subpleural ecchymoses) directly depended on the efforts of breathing and blood pressure.
Some writers, as Taylor and Tidy, think that death occurs sooner in the human subject than in the lower animals; where the access of air is suddenly and completely prevented death may be immediate. Tardieu says that death follows pressure of the hand sooner than that of a ligature.
Fleischmann[739] placed cords round his own neck between hyoid bone and chin, tied them tightly, sometimes at the side, sometimes at the back, without respiration being interfered with, because there was no pressure on the air passages. But his face grew red, eyes protruded slightly, there was a feeling of great heat in the head, of weight, commencing dizziness, and suddenly a hissing and rustling in his ears. The experiment should stop at this point. The same symptoms occurred from applying the cord over the larynx. The first experiment lasted two minutes, the second a half-minute. The difference was due to the different situation of the cord.
Dr. G. M. Hammond[740] gives an account of a personal experiment in strangulation. He sat down; a towel was passed around his neck, and the ends twisted together, making forcible compression of the neck. At first he had a feeling of warmth and tingling, first in the feet, then passing over the entire body; vision partly lost; his head felt as if it would burst; there was confused roaring in ears, like the sound heard on placing the ear to a shell; he remained conscious. In one minute twenty seconds all sensibility was abolished. After a few minutes’ rest a second similar trial was made, with similar results, except that sensibility was lost in fifty-five seconds. A stab with a knife drawing the blood caused no sensation.
Should the subject recover from the immediate effects of the strangulation there may yet be serious secondary results. Among these are convulsions and paralysis; extreme swelling of face, neck, and chest; loss of voice; lesions of larynx and lungs; abscesses. Death may occur suddenly and remotely from one of the sequelæ.[741]
In the treatment of strangulation the first indication obviously is to remove the pressure from the neck. Artificial respiration will probably be required, and may be aided by ammonia applied to the nostrils, tickling of the fauces, and galvanism. Colin[742] states that artificial respiration is useless after cessation of heart-beat. (See the treatment by galvanism under “Suffocation.”) If the body is cold, artificial heat by means of hot bottles, etc. Venesection may be necessary. Colin strongly advises venesection to relieve the distention of the heart. Stimulants and light food are often required.
Limousin[743] recommends the use of oxygen. Cobos[744] experimented on animals by injecting oxygen hypodermically, as a means of artificial respiration. His conclusions are that the oxygen is absorbed and carbon dioxide eliminated in the same place. The oxygen thus introduced causes no trouble. Testevin[745] cures asphyxia by hypodermic injection of ether.
The after-treatment will depend on the after-conditions.
The prognosis is good if there is no serious injury to the neck and treatment is promptly applied.
Post-Mortem Appearances.
The post-mortem appearances in strangulation are external and internal.
The external appearances are of two kinds: those directly due to violence and accident and those due to asphyxia.
External Appearances Directly Due to Violence or Accident.—The MARKS on the neck. In some fatal cases there are either no marks at all or they are but slight; this is more likely to be the case in suicides than homicides, and is usually due to the ligature being soft and yielding. The victim of a homicide may, however, first be stunned and afterward strangled.
Marks are said to be plainer after the body has become cold and where subjects have recovered from attempts at suicide.
The marks of the ligature in strangulation usually encircle the neck more completely and more horizontally than in hanging. These conditions may, however, be reversed, because a body may be dragged by the neck after strangulation, and there have been suicides by hanging in whom the mark of the cord was horizontal. As a rule, however, a horizontal mark with the knot on the same level as the cord, especially if below the larynx, suggests strangulation rather than hanging; and if there are several marks the probability is even greater. In compression with the fingers the marks are not in a horizontal but oblique line.
The mark of the ligature is usually circular, well defined,[714] and corresponds closely to the breadth of the ligature; rather depressed, and usually below the larynx. As a rule this depression is not deep; the skin at the bottom of the groove is usually very pale, while the adjacent parts are red or livid. Sometimes the bottom of the groove shows ecchymoses. Neyding[746] says that suggillations in the groove made by the ligature on the neck are rare, but are oftener found in strangulation than hanging, because the conditions favoring their formation are oftener found in strangulation. In most cases the skin and connective tissue of the groove and of the parts in the vicinity show, microscopically, hyperæmias and hemorrhages. Liman[747] states that when we find suggillation in the groove or its vicinity, we may know that some other form of violence has been applied at the same time as that of the ligature or hand. He had not seen suggillation in the furrow either in strangulation or in hanging, except when the injured persons had lived some time, and in cases of twisting of the umbilical cord. The absence of suggillation and ecchymosis was due, he thought, to the pressure on the capillaries. Bremme[748] says that in the subcutaneous connective tissue of the mark of the ligature there is no hemorrhage either in strangulation or hanging, if death occurs at once and the cord is removed at once after death; but if the cord remains for some time after death there may be hemorrhage, or if death does not occur at once whether the ligature is removed or not. It is impossible to distinguish ante-mortem from post-mortem hemorrhage.
The parchment skin seen in hanging is seldom seen in strangulation. Neyding[749] says that the dryness and induration called parchment skin depend mainly on the amount of excoriation of the skin, and this is greater in hanging. Tardieu explains this frequency as being due to the fact that the constriction in hanging lasts a longer time. Liman has seen the parchment skin in those strangled.
The violence used may cause ecchymoses and abrasions of the skin of the neck adjacent to the mark of the ligature.
The marks of very different constricting ligatures may be[715] quite similar. Taylor[750] mentions a case in which a soft silk handkerchief was used, and the appearance was the same as that of a narrow cord, due to the tightness with which it was tied.
Where a hard substance like a piece of coal or stone is inserted into the ligature, usually then a soft cloth, and presses directly against some part of the neck, there is usually a corresponding bruise.
Marks of pressure by the thumb and fingers are usually on the front of the neck, and either just above or below the larynx. In many cases these marks are only those of the finger-tips with some scratches. These marks may show definitely the probable size of the assaulting hand, and whether right or left.
Marks of strangulation may disappear rapidly after the removal of the ligature. Assailants usually constrict the neck much more violently than is sufficient to cause death. Marks of violence on the neck are, therefore, greater in strangulation than in hanging.
A great variety of external injuries other than those on the neck have been found in the different cases reported where other forms of violence were used. With few exceptions such additional injuries indicate homicide.
External Appearances Due to Asphyxia.—A few of these have already been given under the caption “Symptoms.” If death occurs quickly there may not be any signs of asphyxia. The general LIVIDITY which comes on in the second stage usually remains after death. The face varies in color from violet to black and may be swollen. Casper[751] says that the face has the appearance of any other corpse. Liman[752] found the face livid in only one of fourteen cases. Hofmann[753] says that the cyanosis appears during the agony because of paralysis of the circulation and gravitation of blood. The cyanosis of the face, projection of the eyes, and congestion of the conjunctivæ are due to the expiratory effort. These signs are also seen in fat persons who do not die of strangulation. Tardieu[754] mentions a dotted redness or minute ecchymosis of the conjunctivæ and[716] skin of face, neck, and chest as constant; but this cannot be considered characteristic, because it has been seen, though not so well marked, in death from other causes. It has been found in suffocation from compression of the chest and belly; and also where there is respiratory interference in the prolonged efforts of tedious labor and in convulsions. Liman[755] found it in those who were hung. It is due, according to Hofmann,[756] to increased blood pressure and consequent hemorrhages. It is of importance as tending to show that there was stasis of blood in the head and face during life. Liman[757] found cyanosis in the conjunctivæ, lips, back of mouth, and in the muscles. Maschka[758] in 234 cases of asphyxia found capillary hemorrhages of the eyes and eyelids 87 times.
Dastre and Morat[759] claim that in asphyxia the cutaneous circulation becomes more active than in the normal state, while at the same time the vessels of the abdominal cavity are contracted. Laffont[760] considers the mechanism of this peripheral dilatation.
Post-mortem stainings (hypostases) are usually darker in strangulation than in other forms of death. They appear soon, as does also putrefaction, because of the quantity and fluidity of the blood.
Signs of HEMORRHAGE from the nose, eyes, and mouth may be visible; as also bloody froth from the mouth and nose. Chevers[761] never saw bleeding from the ears in strangulation. Taylor[762] states that Dr. Geoghegan informed him of a case of suicidal strangulation by a ribbon; the violence was great, there was bleeding from the ear, and the drum was found ruptured. In this case the mark on the neck, which was deep, nearly disappeared after the ligature was removed. Taylor also says Wilde, of Dublin, saw a case of rupture of drum and hemorrhage in strangulation. Pellier[763] says that Littré mentions a case of rupture of tympanic membrane in strangulation by a cord. Zoufal and Hofmann have offered explanations of the occurrence (Case 35).
The FACE usually shows pain and suffering; although sometimes the features are calm. In the latter case there may have been syncope.
The EYES are usually staring, prominent, and congested, and the pupils dilated. Casper[764] doubts their prominence. Budin and Coyne[765] state that in asphyxia the dilation of the pupil progresses to a maximum and then convulsions occur. Ophthalmoscopic examination during the dyspnœa of asphyxia shows a lessened fulness of the retinal vessels.
The TONGUE is often swollen, dark, protruding, and sometimes bitten. Maschka[766] states that if the ligature lies above the hyoid bone, the tongue will be drawn backward; if over or below the bone, the tip of the tongue may appear more or less between the jaws.
The HANDS are usually clinched and may have in their grasp articles which, under the circumstances, have a medico-legal value.
The EXTERNAL GENERATIVE ORGANS are sometimes congested; erection of the penis may have taken place and persisted. The vagina may be moist. Tardieu, Devergie, and Casper[767] deny that these appearances are usual.
Involuntary discharges of urine, fæces, and seminal fluid may have occurred. There is nothing characteristic in their appearance.
All the external appearances of asphyxia are usually more marked in strangulation than in hanging.
Internal Appearances.—The mark. Usually there is hemorrhage into the loose connective tissue under the mark and in the subjacent muscles; in most cases isolated and circumscribed, but sometimes extending beyond the line of the mark. Hemorrhage from compression by the fingers is more marked than that from ligature.[768] Sometimes there is only fulness of the subcutaneous veins.
The CAROTID ARTERIES may suffer rupture of their inner and middle coats, especially in atheromatous subjects and when the compression has been great. Friedberg[769] states that the[718] injury of the carotid, if there is hemorrhage into its middle and internal coats, is a proof that the strangulation occurred during life, and probably from pressure of the fingers on the neck, without any regard to any disease of the artery. He reports two cases. The examiner should be careful not to injure the artery with his forceps. The vessels may contain clots.
The NECK occasionally suffers extreme injury, and, owing to the violence used, this occurs oftener in strangulation than in hanging.[770] Occasionally the neck is broken.
The HYOID bone may be fractured (see Case 5). Maschka[771] saw one case in eighteen of Erdrosselung and five cases in fifteen of Erwürgen.
The TRACHEA is sometimes torn, or may be folded on itself.
The cartilages of the LARYNX, especially if calcareous, may be fractured. This is more likely to affect the thyroid than cricoid. The fracture would appear to occur only as the result of enormous force; especially in the young in whom the cartilages are so elastic. The experiments of Keiller[772] on cadavers led him to conclude that falls on the larynx, even from a height and with superadded force, are unlikely to fracture that organ; that severe pressure or violent blows against the larynx from before backward may cause fracture; but that severe lateral pressure, as in ordinary throttling, is more likely than other forms of violence to fracture the alæ of the thyroid or even the cricoid cartilages and also the hyoid bone. Taylor[773] states that Dr. Inman, of Liverpool, had informed him of a case of splitting of rings of windpipe from pressure (see Cases 5, 13). Maschka[774] in fifteen cases of choking found six fractures of the larynx.
Chailloux[775] has collected eight cases of fracture of larynx in strangulation. They were all made with the fingers. The experiments of Cavasse[776] seem to show that there is no great difficulty in fracturing the thyroid in strangulation.
Internal Appearances Due to Asphyxia.—The VEINS of the entire body are distended with very dark and very fluid blood, while the arteries, especially in the young, are mostly empty. Experiments on the lower animals have shown that[719] the pulmonary artery and systemic veins to the finest ramifications are distended with dark blood.[777]
The Heart.—The right side, especially the auricle, is usually full of dark fluid blood, due to the mechanical impediment to the passage of blood through the lungs. If the heart continues to beat after the respiration has ceased the right ventricle is commonly well contracted, like the left cavities, and nearly empty, the lungs being much congested. Sometimes the left cavities of the heart contain blood. This would be most likely to occur if the heart should stop in the diastole. Sometimes clots are found in the right ventricle. Maschka[778] found clots in the heart 25 times in 234 cases of asphyxia.
The LUNGS are usually much congested, resembling red hepatization, except that the blood is darker. Hemorrhages (apoplexies) into the substance of the lungs are common. Tardieu found patches of emphysema due to rupture of the surface air-vesicles, giving the surface of the lung the appearance of a layer of white false membrane. Ogston admits this occurrence in pure strangulation but to a less extent in mixed cases. Liman[779] found the lung surface uneven, bosselated, the prominences being of a clearer color and due to emphysema. The lungs were in the same condition of congestion and emphysema in strangulation, suffocation, and hanging. He failed to find the apoplexies described.
The lungs are sometimes anæmic. In healthy young subjects, especially children, the blood-vessels of the lungs often empty themselves after the heart stops. The lungs may, therefore, be bloodless, but emphysematous from the violent efforts to breathe. Page’s experiments on the lower animals showed the lungs of a pale reddish color and not much distended; a few dilated air-cells might be seen toward their anterior borders, and there might be small hemorrhages over the surface. His experiments appear to show that subpleural ecchymoses occur as a result of violent and repeated efforts to breathe. Among other experiments[780] he stopped the mouth and nostrils of a young calf long enough to excite violent efforts at respiration; it was then instantly killed by pithing. The lungs were found[720] pale red, not congested, but showed subpleural ecchymoses. Page believed these were due to the changed relation between the capacity of the thorax and volume of lungs. Liman found these ecchymoses in cases of strangulation, hanging, drowning, poisoning, hemorrhage, and œdema of brain, in the new-born, etc. He failed to find them in some cases of suffocation. He believes them due to blood pressure from stasis in the blood-vessels. Ssabinski[781] made many experiments on dogs and cats to ascertain the presence or absence of subpleural ecchymoses in strangulation, drowning, section of pneumogastrics, opening of pleural sac, compression of chest and abdomen, closure of mouth and nose, burial in pulverulent materials, etc. Similar hemorrhages may appear on the mucous and serous membranes, as the respiratory, digestive, and genito-urinary tracts, and pleuræ, pericardium, peritoneum, membranes of brain, and the ependyma. These are sometimes minute and stellate, at others irregular in shape; many are bright-colored. According to Tardieu the punctiform ecchymoses are rarely present except in suffocation. Maschka,[782] in 234 cases of asphyxia, found the lungs congested 135 times, anæmic 10, and œdematous 42. He thinks the subpleural ecchymoses valuable signs of asphyxia.
The BRONCHIAL TUBES are usually full of frothy, bloody mucus, and the mucous membrane is much congested and shows abundant ecchymoses.
The lining membrane of the LARYNX and TRACHEA is always congested and may be livid; the tube may contain bloody froth or blood alone.
Tidy comparing strangulation and hanging concludes that because strangulation is usually homicidal, and greater violence is used, therefore the external marks are more complete in strangulation and the congestion of the air passages is invariably much greater.
Maschka found the PHARYNX cyanotic in 216 of 234 cases of asphyxia.
The other MUCOUS MEMBRANES are generally much congested. Serum is found in the serous cavities.
Maschka[783] considers the rounded, pin-head ecchymoses of the[721] inner surface of the scalp and pericranium valuable evidence of asphyxia.
The BRAIN and membranes are sometimes congested; occasionally apoplectic. Maschka[784] found congestion of brain and membranes 48 times and anæmia 30 times in 234 cases of asphyxia.
The ABDOMINAL ORGANS are generally darkly congested, although Maschka denies this for the liver and spleen in asphyxia.
The congestion of the viscera generally is doubtless due largely to the prior congestion of lungs and engorgement of heart.
Page[785] experimented on six kittens, strangling three of them by the hand, the other three by ligature. The results of the post-mortem examinations were nearly similar: the veins were full of dark fluid blood; the right cavities of the heart were similarly gorged, the left empty; lungs pale red, not congested and not distended. Brain normal. The differences were in the lungs; in the first series there were many small, irregular, circumscribed, dark-red ecchymoses scattered over the general surface; in the second, a small number of bright-red ecchymoses, somewhat larger than a large pin-head.
Langreuter[786] made some experiments on a cadaver from which enough of the posterior part had been removed to enable him to view the throat. He saw that the lateral digital pressure on the larynx closed the glottis; stronger pressure made the vocal cords override each other. Similar pressure between the larynx and hyoid bone caused apposition of the ary-epiglottic folds and occlusion of the air-passages. He experimented on sixteen bodies to ascertain the effect of blows and pressure on the larynx, with the following results: In eight cases, women, the thyroid cartilage was injured three times, the cricoid four; in eight, men, the thyroid eight and cricoid five. Whence he concluded that the larynx is better protected in women. In the sixteen cases the hyoid bone was fractured ten times.
The Proof of Death by Strangulation.
Tidy[787] says that “nothing short of distinct external marks would justify the medical jurist in pronouncing death to be the result of strangulation.” On the other hand, Taylor[788] considers[722] the condition of the lungs described as characteristic. Liman[789] did not think there were any internal appearances which could distinguish suffocation, strangulation, and hanging from each other.
In estimating the value of testimony it will be well to consider the following facts:
A victim may be strangled without distinct marks being found. The practice of the thugs shows that this may be done with a soft cloth and carefully regulated pressure without making marks. Taylor,[790] while admitting the possibility, states that this admission “scarcely applies to those cases which require medico-legal investigation.”
The subject while intoxicated or in an epileptic or hysterical paroxysm may grasp his neck in gasping for air, and leave finger-marks.
Different constricting agents may make quite similar marks. Marks may be made on the neck within a limited time after death, similar to those made during life. Tidy’s experiments led him to fix this limit at three hours for ecchymoses and six hours for non-ecchymosed marks. Taylor,[791] however, doubts if such marks could be made one hour after death. He says that the period cannot be stated positively, and probably varies according to the rapidity with which the body cools.
It is, however, unlikely in such post-mortem attempts at deception that the other conditions usual in strangulation would be found—such as lividity and swelling of face; prominence and congestion of eyes; protrusion of tongue; rupture of surface air-vesicles and apoplexies in the lung; congestion of larynx and trachea, etc.
No conclusion can be drawn from the presence or absence of any single appearance.
A cord may be found near a body or even around its neck; there may even be a mark around the neck. These may be attempts at deception.
Marks much like those of violence may be made by tight collars and handkerchiefs remaining until the body is cold.
Cases are reported of bodies having been first strangled and[723] then burnt or hung to cover the crime; and of partial suffocation by gags, followed by or coincident with strangulation (see Cases 18, 20, 24).
In apoplectics with short and full neck we may find at the borders of the folds of skin in the neck one or more depressions, red or livid, that bear some resemblance to the marks of a ligature; but on section there are no ecchymoses.
Froth, tinged with blood, in the air-passages is considered by Tardieu[792] one of the most constant signs of strangulation.
The marks of topical medical applications, as plasters, sinapisms, etc., must not be confounded with marks of violence.
In strangulation by ligature the marks are usually horizontal; in hanging, oblique. In hanging too they are usually dry and parchmenty. Ecchymoses are more marked in strangulation.
The dotted markings of face, neck, and conjunctivæ described by Tardieu are more characteristic of strangulation.
The principal distinctions between strangulation and suffocation would be the absence in the latter of marks on the neck.
Taylor[793] quotes the case of Marguerite Dixblanc, in which the question was raised whether she had strangled her mistress, Madame Riel, or whether the body had been dragged by a rope around the neck. The question was left unsettled by the medical evidence.
The only motive for attempting to simulate strangulation on a corpse would seem to be to inculpate an innocent person.[794]
Both suicides and murderers are usually more violent than is necessary to destroy life; murderers more than suicides.
Putrefaction may cause external marks to disappear.
All marks on a body should be carefully noted; the cavities of the skull, thorax, and abdomen carefully examined; the possibility of death having occurred from other causes, even in strangulation, must be considered.
As Taylor well says, our judgment must not be swayed to the extent of abandoning what is probable for what is merely possible.
In all cases the cord or strangulating ligature should be carefully examined for marks of blood, for adherent hair or[724] other substances. The precise manner in which the cord has been tied should be noted.
Strangulation: Accidental, Suicidal, Homicidal, Simulated.
The question whether a case of strangulation is accidental, suicidal, or homicidal is very difficult to answer.
Accidental strangulation is rare. If the body has not been disturbed, there is usually no difficulty in arriving at a conclusion; but if disturbed a satisfactory conclusion may not be reached.
It is worthy of mention that the umbilical cord may be twisted around the neck of a new-born infant and may have caused strangulation; the mark may give the appearance of death by violence.
Suicidal strangulation is rare. The experiments of Fleischman (supra) suggest that one may commit suicide by compressing his throat with his fingers (see Case 48).
Where a ligature of any kind has been used it is important to notice the number and position of the knots. In a general way a single knot either in front or at the back of the neck might suggest suicide; more than one would suggest homicide. There are, however, exceptions.
Suicide has been committed by mere pressure of a cord fixed at both ends a short distance from the ground; by twisting a rope several times around the neck and then tying it (the coils may continue to compress even after death); by tightening the cord with a stick or other firm substance; by tightening the cords or knots by means of the hands or feet or some portion of the lower limbs; by the use of a woollen garter passed twice around the neck and secured in front by two simple knots, strongly tied one to another.
It is difficult to simulate suicide; requires great skill and premeditation on the part of a murderer. “The attitude of the body, the condition of the dress, the means of strangulation, the presence of marks of violence or of blood on the person of the deceased, on his clothes or the furniture of the room, or both, rope or ligature, are circumstances from which, if observed at the time, important medical inferences may be[725] drawn.” The assassin either does too little or too much. Taylor[795] cites a number of cases of simulation.
Strangulation is generally HOMICIDAL. The marks of fingers or of a ligature on the neck suggest homicide. This is true even if the mark is slight; because infants and weakly persons may be strangled by the pressure of the hands on the throat. Even a strong man, suddenly assaulted, may lose his presence of mind and, with that, his power of resistance; with approaching insensibility his strength still further diminishes. This is true even if his assailant is the less powerful. It requires more address to place a ligature on the neck than to strangle with the hand.
A victim may be made insensible by drugs or blows and then strangled by a small amount of compression; or suffocation by gags and strangulation may both be attempted.
The importance of considering the position and number of the knots in a cord is mentioned under suicidal strangulation.
In homicide, in addition to the marks on the neck, there is likely to be evidence of a struggle and marks of violence elsewhere on the body. It is important, therefore, to notice any evidence of such a struggle.
The nature of the cord may assist in identifying the assailant.
It must be remembered that homicidal strangulation may be committed without disturbing noise even when other persons are near.
Simulation.—False accusations of homicidal strangulation are on record. Tardieu[796] states that a distinguished young woman (for some political purpose) was found one evening at the door of her room apparently in great trouble and unable to speak. She first indicated by gestures and then by writing that she had been assaulted by a man who tried to strangle her with his hand, and also struck her twice in the breast with a dagger. She was absolutely mute—did not even attempt to speak—quite contrary to what is always observed in unfinished homicidal strangulation. On examination by Tardieu, no sign of attempt to strangle was found, and the so-called dagger-openings in her dress and corset did not correspond in position. She confessed that she had attempted deception.
The celebrated Roux-Armand[797] case was another instance of attempted[726] deception. A servant named Roux was found on the ground in the cellar of his employer Armand; his hands and legs were tied and there was a cord around his neck. He was partly asphyxiated, but after removal of the ligature from his neck he rapidly recovered, except that he was weak and voiceless. He stated by gestures that he had been struck by his employer on the back of the head with a stick and then bound as described. The next day he could speak. Armand was imprisoned. Tardieu examined carefully into the case and the results may be stated as follows: The asphyxia was incipient, else he could not have so rapidly recovered. The cord around his neck had not been tied—simply wound around several times; the mark was slight and there was no ecchymosis. Although the legs and hands were tied, the hands behind the back, there was no doubt but that Roux could and did tie them himself. He had stated that he had been eleven hours in the cellar, in the situation in which he was found. This could not be true, for a very much shorter time, an hour probably at the furthest, would have caused death, in view of the condition of asphyxia in which he was found. Again, if his limbs had been bound for so long, they would have been swollen and discolored; but they were not. Again, if the ligature had been around his neck so long as he said, the impression of it would have been more marked. Again, if his stertorous breathing had lasted long it would have been heard by neighbors. The injury on the back of the head, said to be due to a blow, was believed by Tardieu to be due to dragging him on the ground. He further had stated that when he received the blow on the head he became unconscious, and yet he also described how Armand bound him after knocking him down. Again, he had made no outcry; but if he had been strangled while partly unconscious and afterward recovered his senses, he would have been unable to give an account of the matter; if, however, he had been strangled while conscious, there was no reason why he should not have cried out. His inability to speak the first day was assumed, because what was a simulation of absolute mutism should have been simply a loss of voice. The innocence of Armand was ultimately established.
ILLUSTRATIVE CASES.
Homicide.
1. Cullingworth: Lancet, May 1st, 1875, p. 608.—Woman. Believed to have been intoxicated. Face, especially right side, swollen and livid; a little blood had oozed from mouth, nose, and inner angle of each eye. Immediately over (in front of?) larynx and on each side of middle line were marks of irregular outline such as might be caused by pressure of thumb and fingers. Several dark, bruise-like discolorations[727] on flexor surface of each forearm. Hands clinched. Elbows flexed. Discharge of fæces by rectum. Necroscopy: Brain and membranes normal. Hyoid bone and laryngeal cartilages uninjured. Mucous membrane of larynx and trachea congested and covered with frothy mucus. Lungs intensely congested. Several hemorrhages; masses of tissue of each lung, chiefly toward base, were solidified by effused blood. All the heart cavities empty. Stomach normal, empty. No congestion of abdominal viscera.
2. Taylor: “Med. Jur.,” Am. Ed., 1892, p. 412.—Man and woman. Strangled by cord, tied so tightly that there was hemorrhage from mouth and nose.
3. Harvey: Indian Med. Gaz., December 1st, 1875, p. 312.—Hindoo woman, age 45. Strangled with the right hand. Necroscopy: Two contusions and abrasions on temple. Neck discolored from right to left jugulars; marks of thumb on right side and three fingers on left, extending from jugulars to windpipe. Eyes half protruded. Tongue discolored. Blood-vessels full of clots. Brain congested (?) and showed external hemorrhages (?). Lungs normal. Heart empty. Liver ruptured to the extent of four inches, with adherent blood-clot. Spleen, stomach, and intestines normal. Muscles of chest, both sides, congested, discolored, and there were clots of blood over and under them. First six ribs of left side and first three of right fractured.
4. Harris: Ibid., p. 313.—Boy, age 10. Abrasions over front of neck, especially near left ear, probably from ligature; also abrasion on upper part of chest, probably from forcible pressure. Underneath these marks the veins were much distended. Trachea minutely congested; contained much frothy fluid. Lungs showed rupture of some of the air-vesicles; entire tissues distended with blood and frothy fluid. Dark fluid blood in both sides of heart. Large quantity of fluid in pericardium. Brain much congested. Eyes congested. Tip of tongue between teeth. Other organs normal.
5. Mackenzie: Ibid., February, 1889, p. 44.—Hindoo woman, age not given, strangled by another, stronger woman. Necroscopy: Abrasion on front and lower part of neck just above sternum and clavicles; four inches long, three broad; five superficial lacerated wounds on sides of neck, four on left, one on right, apparently nail scratches. Two contusions below and behind lower jaw. Also contusions on thighs. No spots of ecchymosis on neck. Contusion under skin of lower part of neck and upper part of chest, eight inches long, four broad. Left greater cornu of hyoid bone fractured. Both upper cornua of thyroid cartilage fractured; cricoid fractured on each side. Larynx, trachea, and bronchi contained pink frothy mucus; mucous membrane congested. Lungs much congested; pink frothy mucus in bronchi; no emphysema nor apoplexies. Right side of heart full of dark blood; left side empty. Liver, spleen, and kidneys congested. Stomach and[728] intestines normal. Bladder empty. Internal genitals normal. Brain congested.
6. Mackenzie: Ibid., August, 1888, p. 232.—Hindoo man, age about 30. Strangled by soft cloth cord. Necroscopy: Circular mark of cord, one-fourth inch diameter around lower part of neck; indistinct in front, but distinct at sides and back. Superficial abrasions of lips and right cheek as from a gag. Faint marks of blisters on temples. Fingers not clinched. Face livid, swollen. Eyes closed; conjunctivæ congested; corneæ hazy; pupils normal. Tongue protruding and bitten; not swollen. Fluid blood oozing from mouth and nose. Clotted blood under scalp of left temple. Skin beneath cord had the color and consistence of parchment. Muscles not torn. Hyoid, thyroid, and cricoid not injured. Larynx, trachea, and bronchi empty; congested. Lungs much congested. Some dark fluid blood in right side of heart; left side empty. Liver, spleen, and kidneys congested. Small patch of congestion in stomach. Intestines normal. Bladder normal, contained some urine. Brain congested.
7. Ibid., p. 234.—Hindoo woman, age about 40. Broad, circular, depressed “parchment” mark, one inch broad, around the neck, between hyoid bone and thyroid cartilage; made by two pieces of cloth, each three feet seven inches long and one inch broad, twisted into a single cord and tied tightly by three ordinary knots on right side of neck. Superficial wound on left side of head above ear. Face turgid, swollen. Eyes closed. Tongue between teeth and bitten; not swollen. Muscles of neck uninjured. Trachea uninjured. Lungs congested. Right side of heart full of dark fluid blood; left side empty. Liver and spleen congested. Other organs, including brain, normal.
8. Ibid., p. 235.—Hindoo woman, age about 25. Piece of cloth twisted tightly twice around mouth. Double cord made of two twists of thin coir rope tied tightly around middle of neck just below thyroid cartilage; beneath the cord the skin was “parchment” like. No injury to muscles of neck nor windpipe. Eyes closed. Face not flushed. Tongue not ruptured nor bitten. Hands not clinched. Larynx, trachea, and lungs congested. Right side of heart full of dark fluid blood; a little fluid blood in left. Liver, spleen, and kidneys congested. Other organs, including brain, normal. Dr. Mackenzie considered death to be due to “asphyxia or suffocation.”
9. Harvey: Ibid., January 1st, 1876, p. 2.—Hindoo woman, age 12 or 13. Faint mark on front of neck; none at back. Severe bruise on top of head, under which was much clotted blood, but no fracture. Lungs congested. Clots in right ventricle; left empty. Brain, larynx, and trachea congested. The examiner believed that she had been stunned and then suffocated by pressure of some soft substance against the neck.
10. Ibid.—Hindoo man, age 20. Dead seven days; much decomposition[729] and discoloration. Wrists and ankles were bound. The two corners at one end of a cotton lungi (turban) were passed one on each side of the neck and fastened in a knot under left angle of jaw. The lungi was then passed around the body under the arms, etc., so as to draw upon the neck and be buried deeply in the swollen flesh. Under the bands the skin was blanched; the tissues above the bands were black and much swollen. Lungs, larynx, and trachea much congested. Heart empty.
11. Ibid.—Cases of strangulation by sticks and other hard substances. Boy, age 7 or 8. No external marks of violence. There was hemorrhage from mouth and nose. Face swollen and crepitant. Congestion of subcutaneous tissues and bruising of muscles of right side of neck. Mucous membrane of larynx and trachea covered with blood. Lungs much congested; blood in both pleural cavities. Heart empty; bloody serum in pericardium. Brain congested; slight hemorrhage on surface. Abdominal organs normal. Dr. Harvey states that the boy was no doubt strangled by pressure of a lathi on his neck.
12. Ibid.—In another subject two sticks were tightly tied together, one pressing on the front, the other on the back of the neck, flattening larynx and other soft parts. In the following case some hard substance, like a brick, had been wrapped in a cloth and used for compression. Boy, age 15. Necroscopy: Large dark ecchymosis in subcutaneous tissue of front of neck and upper part of chest. Also marks of violence on chest and left side of face. Dissection of neck showed blood-clot and also laceration of muscles. Trachea folded on itself, showing that compression had lasted several minutes. Tongue protruding and bitten. Eyes closed. Features calm. Trachea much congested. Lungs congested. Great veins of heart and neck full of fluid blood. Heart, dark fluid blood in both sides, mostly in right. Brain and membranes much congested.
13. Pemberton: Lancet, May 22d, 1869, p. 707.—Woman, age 60. Found dead. Nose partly displaced and cartilages injured. Lips pale. Mouth closed. Lividity of front of neck from jaw to sternum. Cricoid cartilage ossified (cretified?) and broken on left side; hemorrhage in surrounding tissues. Lungs and heart as usual in suffocation.
14. Cullingworth: Med. Chron., Manchester, 1884-85, i., p. 577.—Woman, married, found dead. Bruise and ecchymosis beneath the ear; effusion of blood in underlying tissue. Other bruises on face, etc. Several bruises in mouth, on lips and tongue. Blood dark and fluid. Brain and membranes much congested. No marks of injury on throat. Lungs congested; surfaces emphysematous. Heart contained dark fluid blood. Urine and fæces had been discharged.
15. The Gouffé Case.—Murdered by Eyraud and Bompard in 1889. Archiv anthropologie criminelle, Paris, 1890, v., pp. 642-716; vi., 1891, pp. 17 and 179. Reports by Bernard, Lacassagne, and others.[730] Gouffé was decoyed into a room and strangled; afterward his body was tied up, placed in a trunk, and taken some distance away. The murderers fled to America; but eventually Bompard returned to France and Eyraud was captured; both confessed. When found, the body was well advanced in putrefaction; after a very careful examination was identified. He was strangled by the pressure of fingers; the head was afterward wrapped in a cloth which was held in place by five turns of a cord around the neck; traces of the furrows made by these cords were found. Heart empty; no blood in muscles of neck; hyoid bone intact but superior thyroid cornua fractured at base.
16. Horteloup: Ann. d’Hygiène, 1873, xxxix., pp. 408-416.—Man found dead on some leaves in a fountain at bottom of staircase; skull and spine fractured. The murderers stated that they had struck him on the head with a crutch; then, believing him to be dead, carried him and threw him into the fountain. When examined, his face was livid, tongue between teeth and bitten nearly in two; and three parallel abrasions on left side of neck and one on right; slight wounds about the face in addition to the fractures mentioned. No report of examination of lungs or larynx. Horteloup concluded that the man had been strangled to death, and that when thrown into the fountain, alighting on his head, the jaws were brought together and tongue bitten.
17. Laennec: Journ. de med. l’ouest, 1878, xii., pp. 68-71.—Woman, age 53; attempted strangulation by her husband. There were slight ecchymoses on each side of neck under angle of jaw, most marked on left side; when seen, she complained of lassitude and lively pain in hypochondria and region of lower ribs antero-laterally; no sign of lesion. She stated that she was awakened from sleep by pressure on neck and chest and feeling of suffocation; she soon lost consciousness and so remained for some hours. Her statements were corroborated by other testimony. Laennec considered the case one of prolonged syncope from pressure on carotids.
18. Lancet, ii., 1841-42, p. 129.—Woman, found dead, her clothing on fire and lower part of her body burnt. Necroscopy showed face and neck swollen as low as thyroid cartilage, and purple; eyes prominent and congested; mouth closed; tongue not noticed; front of neck below swollen part showed two dark-brown hard marks and slight marks also of pressure; on incision the vessels were engorged. Blood, fluid; brain, congested. There were no vesications from the burns and no sign of inflammation.
19. Alguie: “Étude méd. and exp. de l’homicide réel ou simulé par strangulation, relativement aux attentats dont Maurice Roux a été l’objet,” Montpellier, 1864, p. 121.—This essay contains the reports of many interesting experiments on animals and the cadaver. His conclusions in this case were that the victim had first been struck on the neck by a club; then a ligature was placed on the neck, with[731] many turns, tied tightly, but the knots did not remain tight. [The marks were visible four months afterward.] The assailant then tied the limbs. The victim recovered with temporary loss of voice, memory, etc.
20. Gatscher: Mittheil. d. Wien. med. Doct. Colleg., 1878, iv., p. 45.—A man found hanging. The examiner declared that he had hung himself. Eight years afterward, suspicion of violence. A commission appointed. The protocol had shown the blood fluid; a red-brown dry furrow around the neck; ecchymoses in connective tissues of same; the entire back and posterior parts of limbs showed post-mortem suggillation. The commission declared that the man had been strangled, had lain for at least three hours on his back, and then been hung up. The murderer confessed.
21. Ibid., p. 46.—Woman, age 50, found dead in bed. Blood fluid; two ecchymoses size of beans in crico-thyroid muscles of each side; patch of hepatization size of fist, in lung; injury of body. The examiner declared that she had been strangled by compression of larynx with two fingers, but he could not say how long the pressure had continued, that is, whether she had died of the strangulation or of the pneumonia. The assailant stated that he had choked her and when she seemed to be dead, had left her. The woman lived alone.
22. Waidele: Memorabilien, 1873, xviii., pp. 161-167.—Husband and wife quarrelled and fought; he stated that he choked her with her neck handkerchief, and as she turned round toward him, then choked her with his hand until she died. The examiner declared that she died of asphyxia; there was a brownish-red dry streak on each side of the neck in the laryngeal region corresponding to the handkerchief, and also two small abrasions of skin which might have been made by the hands; he concluded, however, that she had been choked to death by the handkerchief, because there were no ecchymoses.
23. Rehm: Friedreich’s Blätter f. ger. Med., 1883, xxxiv., pp. 325-332.—Woman, age 37. Choked by the hand on the neck, and at the same time assailant’s knee pressed against her abdomen, pressing her against a wall, causing hemorrhage around the pancreas. Death stated as due to asphyxia.
24. Schüppel: Vier. ger. öff. Med., xiii., 1870, pp. 140-156.—Woman, just delivered of child, and boy ten years old, were burnt to death in a fire which consumed their house. Examination of the bodies showed upon the neck of the boy a groove, and his tongue protruded. The husband was charged with murder, was imprisoned, and committed suicide.
25. Weiss: Ibid., xxvii., 1877, pp. 239-244.—Woman strangulated by the bands of her nightcap.
26. Isnard and Dieu: Rev. cas jud., Paris, 1841, p. 101.—Man, age 65. Marks of fingers on face and neck. Opinion that he had been assaulted by two men. The two murderers confessed.
27. Friedberg: Gericht. gutacht., 1875, pp. 211-224.—Woman[732] found hanging to branch of tree, but in half-lying position, feet on ground. Opinion given that she had been strangled and then hung.
26. Tardieu: “Pendaison,” p. 223.—New-born infant. Question whether its death was due to asphyxia from compression of neck by the mother with her hand to hasten delivery. He doubted the possibility of the mother thus assisting her child. But the direction of the seven excoriations on its face contradicted the mother’s statement. The traces of finger-nails were distinct. The lungs and alimentary canal showed that the child had lived. Opinion given, infanticide.
29. Ibid., p. 219.—Woman, advanced in years, habits dissipated; found strangled. Four excoriations on left side of larynx, one on right; blood in subcutaneous tissue. Marks of nails and long scratches on wrist. Injuries on face and left breast. She had been strangled by one hand on her neck while the other was over her mouth and nose. Face livid; eyes congested; frothy bloody liquid flowing from mouth and nose; tongue behind teeth; bloody froth in larynx and trachea; lungs large, much congested, splenized in places, surface emphysematous, looking like white spots; black fluid blood in heart; brain somewhat congested.
30. Ibid., p. 216.—Wife of the celebrated painter Gurneray; found dead in bed, where a fire had been placed and slowly burnt and charred her lower limbs, belly, chest, and right hand. A running noose around her neck. Injuries of head; face livid; tongue between teeth; brain normal; mark of cord slight; subcutaneous tissue infiltrated with blood. Marks of pressure on chest; bloody froth in trachea; lungs congested; heart contained fluid blood. Opinion given that she had been struck on head, causing unconsciousness; then partly stranded and partly suffocated by pressure on neck and chest. Body afterward burnt to cover up the crime.
31. Ibid., p. 211.—Three murders by one man. All women. All injured about the head and then strangled by both hand and ligature. Two died; one had an odor of alcohol and had apparently not resisted. The third was resuscitated. She was strong and stout, and resisted. Marks of fingers and nails on neck. Afterward she had headaches and giddiness for a long time.
Suicide.
32. Francis: Med. Times and Gaz., December 2d, 1876, p. 634.—Hindoo lunatic, a giant, strangled himself. He passed two or three coils of stout thread around his neck, attached the ends securely to his wrists, and then extended his arms to their utmost limit. This occurred during a ten-minute absence of his attendant, who, returning, found the man had fallen to one side from a kneeling position, with his back against a wall, quite dead. No reason to suspect homicide.
33. Badahur: Indian Med. Gaz., December, 1882, p. 330.—Hindoo woman, age about 17, strangled herself with the border of her saree. Necroscopy: Circular depressed mark caused by the border of a band of cloth, which she had passed in three coils around her neck, the coils tightly overlapping each other; the short ends had been knotted together with a “granny” knot at the back of the neck, like the native women tie up their hair. The coils were so tight that they had to be cut off. Face swollen, dark purple; conjunctivæ congested. Tongue between the shut teeth; bloody froth issuing from mouth and nostrils [the examination was in September, thirty hours after death]. Skin of neck reddened in nearly a continuous line all around, both above and below the band, about three-fourths inch wide, evidently caused by the pressure of the three folds. Considerable ecchymosis above and below the coils; the neck underneath the folds was swollen and red. Brain and membranes much congested. Trachea, pharynx, and œsophagus congested. Lungs congested. Right cavity (auricle?) of heart full, left empty. Liver, spleen, and kidneys congested. Intestinal peritoneum congested. Stomach contained half-digested food. Small intestines empty; fæces in large intestine. Bladder empty. Uterus and appendages congested; no evidence of catamenia.
34. Harris: Ibid.—Woman; made a loop of her hair around her neck, knelt down so as to put it on the stretch; when found, was nearly dead.
35. Geoghegan: Taylor’s “Med. Jur.,” Am. Ed., 1892, p. 413.—Informed Dr. Taylor of a suicidal strangulation by a ribbon. The mark on the neck nearly disappeared after removing the ligature. There was bleeding from one ear, from rupture of tympanic membrane. No froth from mouth or nostrils; but little lividity or swelling of face.
36. Taylor: “Med. Jur.,” Am. Ed., 1892, p. 418.—Boy: found dead with handle of pitchfork under necktie; marks of strangulation on larynx; eyes and tongue protruded; tongue livid and marked by teeth; brain congested. Also man found dead with handkerchief tied around neck and twisted by razor strop. Taylor considered both as suicides. Also a third case (Amer. edit., 1880, p. 465). A man of unsound mind twisted a fishing-net firmly around his neck several times; it remained secure without the aid of a knot.
37. Fargues: Rec. de mém. de méd., etc., Paris, 1869, xxii., pp. 443, 444.—Soldier, age 32, while drunk, strangled himself with his handkerchief, wrapping many folds around his neck, making a deep furrow without ecchymosis; face pale, eyes closed, lips partly closed.
38. Borchard: Jour. de méd. de Bordeaux, 1860, v., p. 349 et seq.—Collation of cases of suicide by strangulation: First, an officer who placed his sabre scabbard under his cravat. Second, a woman strangled herself with a silk cravat, tightly tied. Third, a man tied the sleeve of his jacket around his neck and fastened the end to a window, so that[734] the strangulation was partly due to suspension. Fourth, a woman strangled by a cord.
39. Hofmann: Wien med. Presse, 1879, xx., p. 16, et seq. Also Lehrbuch, p. 559.—Woman, age 20, found dead in bath-room, with a thick thread passed three times around the neck, and tied tightly in front at the second and third turns; so tightly that even after cutting the cords the pressure continued. No signs of violence. (Illustration.)
40. Zillner: Wien med. Woch., 1880, xxx., pp. 969, 999.—Woman, age 33; found dead on the floor; a neck-handkerchief tied in a firm knot in front of the neck; and underneath, a cord passed twice around the neck and knotted in front in the middle line between the larynx and hyoid bone. Blood was flowing from the ears. No sign of violence or struggle.
41. Bollinger: Friedreich’s Blätter f. ger. Med., 1889, xl., p. 3.—Man, age 48; melancholic; found dead. Had torn up part of a sheet, fastened it around his neck and the ends around a bed-post, then placed his feet against the farther post and pressed, tightening the ligature. (Illustration.)
42. Roth: Ibid., p. 9.—Man, age 68; melancholic; found dead in bed. Had made loose ligature of cravat, tied into it a piece of wood; the ligature lay in front of larynx. Had attempted suicide once before.
43. Ibid.—Son-in-law at 36 years of age had committed suicide in the same way.
44. Ibid.—Man, age 63; found dead in his bed; cord around neck inclosing piece of wood.
45. Maschka: Vier. ger. öff. Med., 1883, xxxviii., pp. 71-77.—Woman, age 45. A cloth was found wound tightly three times around her neck in front of larynx, and tied in a simple knot. There were also injuries of the head. At first it was thought that she had been murdered, but Maschka concluded that she had committed suicide.
46. Ibid.—Woman; supposed to have been murdered by her son. There were marks on the neck and other injuries, and hemorrhage into the brain. Maschka concluded that the marks on the neck were not due to strangulation.
47. Hackel: Dorpat Diss., 1891, p. 34.—Man, age 48; strangled himself with part of a mattress. Was found lying on his back, dead, holding the ends in his hand. There was a double mark of ligature.
48. Binner: Zeitsch. f. Med-beamte, 1888, i., pp. 364-368.—Woman; suicided by choking herself with her hands.
For other cases, see Tidy, “Med. Jur.,” Cases 20 to 65; Maschka, “Handbuch,” p. 625.
Accident.
49. Bédié: Rec. de mém. de Méd., etc., Paris, 1866, xvi., pp. 482-484.—Soldier, age 39, found dying, lying on his bed; had returned to[735] his room drunk and lay down in his uniform. Face much congested; lips cyanosed; eyes closed. Skin of neck below thyroid cartilage showed deep mark from pressure of collar of uniform where the collar was fastened; had passed urine into his clothing. When examined after death his face was pale yellow, lips cyanosed, eyes closed; large hypostatic patches; traces of pressure on neck still visible; lungs congested; larynx, above level of pressure, congested; below was normal. Fibrin clots in both ventricles of heart. Liver, spleen, stomach, and intestines congested. Brain somewhat congested. Bladder contained urine.
50. Liégey: Jour. de Méd. chir. et pharm., Brussels, 1868, xlvi., pp. 339-342.—Infant, age 8 months, accidentally strangled; it had been placed in its cradle; coverlet over it and held in place by a cord passed across. Some time afterward it was found dead beside the cradle, its head hanging with the right side pressing on the cord. Liégey had the mother replace everything as it had been and satisfied himself that the above statement was correct. When found, the face was pale, eyes and mouth closed; transverse furrow on right side of neck, level of larynx, 3.5 cm. long, one deep; muscles in vicinity congested. Lungs congested. Right side of heart contained clotted blood; left side nearly empty. He concluded that the case was one of accidental strangulation.
51. Friedberg: Gericht. gutacht., p. 240.—New-born child found dead in closet. Mother stated that she had taken the child by the neck and drew it into the world. Opinion given that the child had been accidentally choked to death by the hand.
For other cases, see Tidy, “Med. Jur.,” Cases 15 to 19, 59, and 62; Maschka, “Handbuch,” p. 623.
HANGING.
Hanging is a form of mechanical suffocation by ligature of the neck, in which the constricting force is the weight of the body itself. The French call it “Pendaison” or “Suspension,” preferably the former; the Germans, “Erhängen.” The expression “incomplete hanging” is applied to those cases in which the subject is partially supported; kneeling, sitting, or otherwise. The same expression has also been used for cases which did not prove fatal.
The pathological effects of hanging are partly those of strangulation, to which must be added the effects of the weight or fall of the body, sustained as it is only by some form of ligature around the neck. These additional injuries will, of course, be proportioned to the weight of the body, length of rope, and suddenness of the fall.
In some countries, as the United States, England, Germany, and Austria, hanging is a mode of capital punishment. It is desirable that for judicial purposes it should be divested, as far as possible, of unnecessarily cruel features; the victim should quickly be made insensible, and death be speedy. Many suggestions to this end have been made, among which is that of Haughton. He recommended that the drop be long, say ten feet, so that the cervical vertebræ may be dislocated. He also advised that the knot be placed under the chin. Others advise that it be placed under the left ear; and others yet, as Barker, of Melbourne,[798] near the spine. In any event the rope should be “freely elastic.” G. M. Hammond[799] thinks that the object in judicial hanging should be strangulation, and that the criminal should be pulled up and left to hang thirty minutes; the rope should be soft and flexible so as to closely fit the neck; a weight should be attached to the feet of persons under 150 pounds. Larimore[800] also advocates strangulation instead of attempting dislocation of the vertebræ. Porter[801] suggests that for dislocation the noose be drawn tightly around the neck at the last moment, the knot being either at one side or, still better, in front. Dislocation may be still further assured if a hollow wooden or leaden ball be placed over the knot close to the neck, thus forming a fulcrum to throw the spinal column out of the perpendicular line at the point of pressure.
Hanging is a common mode of suicide, especially in insane asylums and prisons. It is sometimes accidental, and rarely homicidal. It is said to have been attempted for erotic purposes.
The compression of the neck acts in line with the axis of the body; while in strangulation it acts perpendicularly to that axis.
The final cause of death will depend on: 1. The suddenness and completeness of interference with the access of air; asphyxia. 2. Pressure on the large veins of the neck, preventing the return of blood from the head, causing congestion of brain and coma. 3. Pressure on the large arteries of the neck, preventing access of blood to the brain; causing anæmia of the brain and syncope. 4. Injury to spinal cord or pneumogastric nerves or all of them; causing paralysis. A combination of numbers 1 and 2 is usually found in suicidal hanging; and probably all of them in homicidal and judicial[737] hanging. The more protected the air-passages are from pressure the greater part will coma or syncope have in the cause of death.
Mackenzie,[802] as the result of examination of 130 suicidal hangings, says that 119 died of asphyxia, 8 of asphyxia and apoplexy, 2 of syncope, and 1 of apoplexy alone. Coutagne[803] thinks œdema of the lungs, “œdema carminé,” has an important part in causing death.
The following conditions tend to produce asphyxia: a tight ligature, or a loose ligature above the hyoid bone. To produce coma, a loose ligature pressing against the hyoid bone or larynx, especially a cretified larynx. To both asphyxia and congestion of brain, a ligature just beneath the lower jaw, or around lower part of neck.
Hofmann[804] states that when the ligature is placed between the larynx and hyoid bone, the base of the tongue is pushed upward against the posterior wall of the pharynx, completely stopping respiration and causing asphyxia. Taylor[805] states that if the rope presses on or above the larynx, the air-passages are not so completely closed as when pressure is below the larynx. In the latter case death would be immediate; in the former a slight amount of respiration might continue. The instantaneous loss of consciousness is due, not to asphyxia alone, but to compression of the large vessels, especially the carotids, against the transverse processes of the vertebræ, causing rupture of the middle and inner coats, and at the same time compression of the jugular veins and pneumogastric nerves. Immediate unconsciousness will almost certainly follow compression of the pneumogastrics. He also believes that the loss of consciousness and of power of self-help occur at the moment that the noose is tightened around the neck. There is no record of any one who attempted suicide by hanging seeking to recover himself, although no doubt some would have done so if the speedy unconsciousness had not prevented. Hofmann mentions the case of a man who was found hanging, and with a loaded revolver in his hand, apparently having intended to shoot as well as hang himself, but lost consciousness before[738] he had time to discharge the revolver. According to him the causes of death are three: occlusion of the air-passages, interruption of passage of blood to brain, and compression of pneumogastric nerves.
Von Buhl[806] experimented on cadavers and concluded that in hanging, the epiglottis and arytenoids are pressed over the glottis, and the tongue and the œsophagus against the vertebræ, causing death by apnœa. When the trachea was isolated from the vessels and tied, the air-passages below became dilated and the lungs emphysematous and anæmic. The heart continued to beat and blood to circulate.
The vertebral arteries being much smaller than the carotids, the circulatory disturbance in the brain is not adjusted with sufficient promptness. Compression of the pneumogastrics, according to Waller,[807] has caused subjects to fall to the ground as if struck by lightning. He holds that the unconsciousness in hanging is the result of the compression of the pneumogastric nerves and not of the arteries. Thanhöfer[808] knew a student who had acquired a certain dexterity in compressing these nerves. One day he compressed the two nerves, his pulse stopped and he became unconscious. Thanhöfer[809] tried bilateral compression of pneumogastrics in a young man sentenced to be executed. The pulse fell at once and the heart soon stopped; the eyes were fixed and glassy. It was some time before he regained consciousness and for two days there was malaise.
Hofmann says that the compression irritates and, in a higher degree, paralyzes the pneumogastric nerves and causes disturbance of the action of the heart.
Faure[810] denies that the constriction of the vessels of the neck has any effect in the production of symptoms[811].
Coutagne believes that the pressure on the pneumogastric nerve is a factor in causing death. He hung two dogs; in one the pneumogastric nerves were dissected out and placed in front of the ligature; this dog (No. 1) lived a quarter of an hour and died of pure asphyxia with efforts at inspiration continued to the end. The other dog (No. 2), in[739] which the nerves were compressed, died in five minutes. In both, the abdominal organs were congested and the cavities of the heart were full. The lungs of the first were dry and uniformly red; of the second were resisting, crepitant, and quite œdematous. No subpleural ecchymoses in either. The experiments on animals by Corin[812] led him to conclude that pressure on the pneumogastrics caused increased frequency of the heart-beat and slowing of respiration. Pellier[813] considers the subject quite fully. It would appear that the pressure on the pneumogastrics disposes to stop the action of the heart and cause rapid, perhaps instant death. The pressure on the carotids causes cerebral anæmia and is then only a secondary cause. Levy[814] does not think the action of the pneumogastrics is sufficiently well known.
Tidy states that a dog lived for three hours suspended by a rope placed above an opening in the windpipe; and that Smith[815] mentions the case of a criminal who was hung; Chovet tried to save the man by making an opening in the trachea before the execution and introducing a small tube. The man was alive forty-five minutes after the drop, but could not be resuscitated, although the surgeon bled him.
In a small proportion of cases of hanging, homicidal and judicial, death occurs by dislocation of the spine. This is said to have been first noticed by the celebrated Louis, who states that the Paris executioner was in the habit of giving a violent rotary movement to the body of the convict as the trap was sprung, causing a dislocation of the odontoid process and compression of the cord and almost instant death. Taylor[816] says that for dislocation the body must be heavy and the fall long and sudden. Devergie[817] found this to occur in about two per cent of cases. It is said that the Paris hangman placed the slip-knot under the chin in front, which is as Dr. Haughton suggests.
Death may occur from secondary causes after apparent recovery; from congestion of brain and other lesions of the nervous system; these may prove fatal at remote periods.
Fracture of the odontoid process according to M. de Fosse is more common than dislocation, and the giving away of the intervertebral substance more likely than either of the others.[740] The phrenic and other respiratory nerves are likely to be paralyzed; the vertebral and carotid arteries may be ruptured. The medulla oblongata is also likely to be fatally injured. Death may also occur from hemorrhage upon the cord, causing pressure.
Besides the ropes used as ligatures in judicial hanging, almost every conceivable article that could be made into the semblance of a cord has been used by suicides; usually, however, some portion of the bedding or clothing. When one resolves on suicide, all the precautions of the managers of prisons and asylums fail to prevent.
The secondary effects in those who recover involve the respiratory organs—dyspnœa, cough, bloody sputa, bronchial râles, and fever; or the nervous system—aphonia, dysphagia, numbness, chilliness, spasms, pains in neck, face, or shoulder; sometimes paralysis of bladder and rectum, and loss of memory. The marks on the neck slowly disappear.[818] Verse[819] collated a number of cases in which the hanging was not completed and the subjects lived for varying periods afterward. Wagner and Möbius[820] discuss the spasmodic seizures and amnesia, which often appear after the restoration from hanging.
Symptoms in Hanging.
Obviously these will be in some respects identical with those of strangulation. In considering the latter, some of the similarities and dissimilarities of symptoms and post-mortem appearances of strangulation and hanging were mentioned.
Death may be immediate and without symptoms.
There is, of course, no preliminary or “waiting” stage, as in strangulation, except in those rare cases of suicide where the subject inclines his body forward with his neck against the ligature, his body being near the floor or ground. The absence of a drop makes this condition very similar to ordinary strangulation. The body of a victim of homicide might be similarly placed for the purpose of deception, and also that of a subject previously made unconscious; in these cases the symptoms and appearances would resemble those of strangulation.
In other words it is necessary that there should be a drop or fall, or at least the weight of the body, to produce the characteristics of hanging. The jerk of the fall or sudden dependence of the body upon the ligature causes a much greater constriction of the ligature on the neck, and in a different direction, than in strangulation; and also a much greater pressure on the blood-vessels and nerves of the neck.
Tidy divides hanging into three stages:
First stage: Partial stupor lasting thirty seconds to three minutes, according to the length of the drop, the weight of the body, and tightness of the constriction. The testimony seems to be uniform that there is no pain in this stage; indeed, that the feeling is rather one of pleasure.[821] The subjective symptoms described are an intense heat in the head, brilliant flashes of light in the eyes, deafening sounds in the ears, and a heavy numb feeling in the lungs. Sometimes there is a feeling of absence of weight. In many cases efforts to breathe are made for a time after the air-passages are closed. It is doubtful whether there are any voluptuous feelings, as has been suggested.
Chowne[822] reports the case of Hornshawor, “Monsieur Gouffé,” who was in the habit of hanging himself for exhibition. He fixed the noose with a knot that would not slip, sprang into it, the rope coming behind the lower jaw and the two sides passing up behind the ears. He would hang for ten to fifteen minutes, and in addition to his own weight would sustain one hundred and fifty pounds. Three times the rope slipped and he would have died but for the help of spectators. He described his sensations as follows: He lost his senses all at once. The instant the rope got in the wrong place he felt as if he could not get his breath, as if some great weight was at his feet; and could not move only to draw himself up; felt as if he wanted to loosen himself but never thought of his hands. He said: “You cannot move your arms or legs to save yourself; you cannot raise your arms; you cannot think.”
Taylor[823] mentions the case of Scott, the American diver, who was in the habit of making public exhibitions of hanging. The last time he hung for thirteen minutes, the spectators not suspecting that he had died. It is supposed that the ligature had slipped. Taylor also reports a case (from Dr. Elliott) of a boy, age 11, who, to frighten his parents, tied a knot in a handkerchief and put it around a knob and his neck in one continuous ligature. The pressure against the trachea was so effective[742] that he became unconscious and died before he could relieve himself.
Second stage: The subject is unconscious and convulsions usually occur. The convulsed face, however, is a part of the general agitation and does not indicate pain. In judicial cases the face is covered with a cap. Sometimes there are no spasms. Urine, fæces, and semen may be discharged in any stage. Jaquemin, however, in forty-one cases of hanging, noted discharge of urine and fæces only twice. Semen has, however, been found in the urethra where none was ejected externally.[824]
Third stage: All is quiet except the beating of the heart. As a rule, the pulse may be felt for ten minutes.
Blankenship[825] reports an execution of a man by hanging. After the rope was adjusted the pulse was 121; first minute after drop, pulse 54; second minute 52; third 39; fourth 20; fifth 0; sixth 70; seventh 73; eighth 0; ninth 34; not perceptible afterward. Died from strangulation; neck not dislocated. The heart beat once in the nineteenth minute; from the ninth to the nineteenth, only two or three times. No priapism.
In judicial executions, however, the right auricle is found in action when the subject is taken down at the end of the usual period of suspension (see Case 89). Tardieu mentions a case where the heart was beating 80 to the minute one and one-half hours after supposed death. It is probable that in these cases the deprivation of air and compression of the vessels has not been complete. In such cases life may sometimes be restored. Cases are reported where restoration has been possible within a period of a half-hour of suspension; although the fatal period is usually five to eight minutes at most. If, however, the tissues and especially the spinal cord are injured, or the ligature has compressed below the larynx, the chance of recovery is very small, even if the body is cut down at once. According to Faure, animals experimented upon die in twelve to twenty minutes.
Many cases of “incomplete” hanging have been reported; where the feet touch the floor, or would do so if the subject should choose to have it so. Tardieu[826] collected 261 cases, in[743] 168 of which the feet touched the ground, in 42 the subject was on his knees, in 29 the body was lying, in 29 sitting and in 3 squatting. Hackel,[827] in 67 cases of hanging, found it incomplete in 34 per cent.
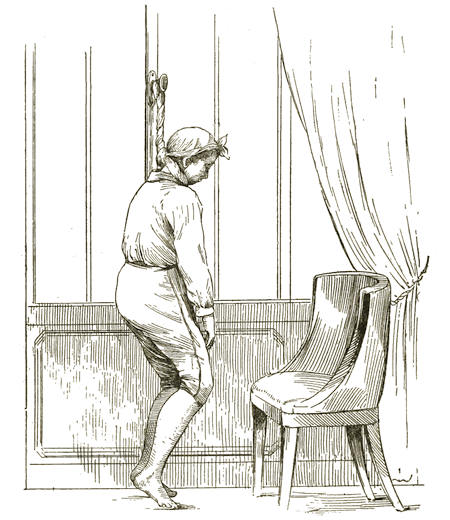
Fig. 22.—Suicide of Prince Condé. (See page 763.)
In one of the experiments of Faure[828] a large dog was hung, his feet touching the ground. For five minutes he was quiet, breathing without difficulty. He then tried to release himself, but instead tightened the knot; he made still greater efforts to release himself, became comatose and fell, apparently dead, at the end of ten minutes; was really dead in twenty-eight minutes.
In incomplete hanging the upper limbs may have any position; the lower limbs are disposed according to the position of the body (Cases 1, 10, 18, 19, 20, 22, 24, 26, 28, 37, 43, 50, 56).
Faure[829] made many observations on dogs which he killed by hanging. He describes the results as follows: The dog remains quiet usually twenty to thirty seconds, sometimes eight to ten minutes; then becomes violently agitated, the body being thrown forward and backward so powerfully that it bounds to a great height; the head is in motion; the jaws parted; the feet extended and flexed; sometimes brought up to the mouth and neck, trying to remove the obstruction; the inside of the mouth is violet-colored; tongue blackish, livid, may be bitten, often falls backward; the teeth are ground together; the eyes sometimes protrude; conjunctivæ congested; urine and fæces discharged. The agitation lasts two to five minutes, and then the dog gradually becomes quiet. Toward death, however, the agitation is renewed but in a different way; the fore feet are raised and put forward, the tongue often has a peculiar spasm, the chest is raised, the eyes drawn back into the orbits, pupils contracted; all of this is over within two seconds. Such paroxysms may be repeated half a dozen times. In dying, the eye oscillates from side to side and the pupil dilates. The heart beats some time longer.
Francis Bacon records that he knew a man who wanted to find out by experience if there was any suffering in hanging. He placed the cord around his neck and stepped off a bench, intending to step back again, but became immediately unconscious and would have died but for the opportune arrival of a friend. He said he saw a light before his eyes.
Treatment.
The first indications obviously are to let the subject down, and remove all constriction of neck and chest. Artificial respiration should then be used, and this may be assisted by the vapor of ammonia to the nose and tickling the fauces. If the body is warm, cold affusions may be applied to the head and chest, and galvanism may be used.
If the body is cold, apply warmth. Friction of the limbs aids in restoring warmth. If the subject can swallow give stimulants; these may also be used by rectum. Venesection may be required to relieve cerebral congestion or distention of the right heart and pulmonary circulation.
The following cases illustrate what may be done to resuscitate one who has been hanged: A man, age 35, in good health, weight one hundred and sixty pounds, was executed with a drop of over six feet; the rope slipped behind the mastoid process. After three minutes his struggles[745] ceased; the radial beat ceased at six and one-half minutes; all signs of life at ten and one-half minutes, and the body was blue. Fourteen and one-half minutes, body let down; mark about one-fourth inch deep on neck; swelling above and below; no fracture of vertebræ. Strong galvanism of the pneumogastrics after sixteen or seventeen minutes at intervals of four seconds caused marked respiratory efforts; sixty-six minutes, galvanism renewed; heart-beat and radial pulse recognized; epiglottis swollen, requiring the tongue to be drawn forward; a few ounces of blood removed; pupils contracted. One hundred and four minutes, galvanism renewed; subject swallowed a little brandy-and-water. One hundred and thirteen minutes, slight muscular action; cornea sensible. One hundred and eighty-six minutes, feet warm, carotid pulsation. Signs of life now increased till six hours after drop, when pupils began to dilate again. Twelve to fifteen ounces of blood were taken and pupils again contracted and pulse beat strong and steady; breathing easy, more regular; eyes followed movements of persons around the room. Died nine hours later, fifteen hours after drop. The experiments were repeatedly interrupted by the sheriff.[830] Taylor[831] reports a case of recovery. Woman, age 44; found hanging from a clothes-line, thrown over a door and fastened to a handle on the other side; her knees on the floor; white froth around the mouth; tongue protruding and swollen; face dusky and swollen; lips dark blue; brown parchment mark on neck; skin abraded over larynx; conjunctiva insensible; pupils dilated and fixed; fingers clinched; limbs flaccid; no reaction from tickling feet; no respiration; faint heart-beat and fine thready pulse. Sylvester’s artificial respiration method used at once and continued for four and one-half hours; tongue held forward by forceps. One hundred and fifteen minutes after body was first seen there was spontaneous movement of legs. One hundred and forty-five minutes, conjunctivæ sensible. One hundred and seventy-five minutes, retching. Two hundred and five minutes, free vomiting. She recovered but remembered nothing of the hanging. Keen[832] reports the results of experiments upon a criminal who was executed by hanging. He was cut down about half an hour after the drop. Faradization and galvanization of pneumogastric and recurrent laryngeal nerves caused movements of left vocal cord, but not the right; there was no reflex motion in the larynx. The left phrenic nerve made no response to stimulus. The internal intercostal nerves caused the raising of the cartilage below them (inspiratory), the external intercostals depressed the upper seven ribs (expiratory), and raised the eighth. The other four not examined. The muscles of the face retained their contractility.
Very few, comparatively, however, have been restored after hanging. For cases of recovery see Medical Times and[746] Gazette, London, 1871, Vol. I., p. 669 (Cases 12, 13, 42, 44, 47, 49, 66).
Post-Mortem Appearances.
The post-mortem appearances are external and internal.
The external appearances are those due to the action of the ligature on the neck and to other violence, if any has been done, and those due to asphyxia or syncope.
The MARKS of the ligature. If the suspension be very brief and the ligature soft and supple, and the body instantly cut down after death, there may be no mark. Allison[833] questions the value of the mark, contending that it is post mortem, and reports cases; says it is present only if the drop be considerable or the suspension continue after death. Tidy says that the mark is, in a measure, independent of the ligature and duration of suspension, and does not usually acquire its color for some hours after death; sometimes, however, it has occurred in a much shorter time. It may be slight because the ligature has been placed over the clothing. The longer a body hangs after death, the more the mark shows. It can be produced upon the cadaver.
Harvey[834] says: “The characteristic mark is sometimes found in non-fatal cases.... In eight instances in the present returns (of nearly 1,500 cases of hanging) there was a distinct mark.”
Coutagne,[835] in twenty-four necroscopies on subjects hung, found only slight or doubtful lesions in five cases; but of these, one was in a condition of advanced putrefaction, another was apparently weakened by loss of blood from wounds, and in the other three there were marks of violence. In seventeen cases the lesions of the neck were plain; hemorrhage in connective tissue or muscle.
The direction of the mark is usually oblique, following the line of the lower jaw upward and backward behind the mastoid processes; it may, however, be horizontal. If the ligature encircles the neck more than once, one mark may be circular, the other oblique. If a running noose is used the mark may be circular, and be seen all the way around the neck, looking like the mark of a strangulation. Taylor[836] states that if the noose[747] should be in front, the mark may be circular, the jaw preventing the ligature from rising upward in front as much as it does behind. If it encircles the neck but once, its continuity is apt to be broken by the prominence of the hyoid bone, thyroid cartilage, sterno-mastoid muscles, etc.
In four-fifths of the cases (117 out of 143, Tardieu) the mark is found between the chin and larynx; in nearly all the remaining fifth, over the larynx; in a very few below the larynx; the last position is due to the protection of the neck by a handkerchief or beard, or where there is some anatomical or pathological peculiarity which prevents the ligature from going higher.
Hofmann[837] had seen two cases of tumor of neck; one in a woman, where the cord was below the larynx; and in a man where it was over the larynx. He quotes[838] as follows: Remer, above larynx, 38; over larynx, 7; below larynx, 2. Devergie, above larynx, 20; over larynx, 7; below larynx, 1. Casper, above larynx, 59; over larynx, 9. Roth[839] in 49 cases found the ligature mark above the hyoid bone in 5; between the bone and the larynx, 31; over the larynx, 8; below the larynx, 1. Hackel found the ligature in forty per cent of cases between hyoid bone and larynx; in sixty per cent lower down. The ligature always appears lower after the body is laid down than it was in suspension. Maschka found the furrow 147 times in 153 cases above the larynx.
The mark will vary in character according to the kind of ligature used, its mode of application, the vitality of the tissues, and the period that has elapsed since death. The result is different according as the knot or loop is single or double, a running or slip knot.
The mark may differ in character in one part of the neck from another. The same furrow may be soft in one part and dry in another. The width of the mark does not necessarily correspond to the diameter of the ligature. A double mark usually means that the ligature has been twice passed around the neck, although the marks may not be continuous or parallel. Tardieu states that a large single leather thong pressing on the neck only by its borders may make a double mark. The mark is usually depressed. The depth of the depression, groove, or[748] furrow, as it is called, is greater the narrower and firmer the ligature, the longer the suspension, and the greater the weight of the body. The mark may be merely a slight depression, without color, or only a red blush, if the subject is young, tissues healthy, and suspension brief. Roth,[840] in 49 cases of hanging, found the furrow of the ligature was brown in 40, red-brown in 6, and 3 times bluish.
In about two-thirds of the cases the bottom of the furrow, the place of greatest pressure, is white, especially so where the knot is tied; while the edges of the furrow are usually slightly raised and red or livid. If the subject is very fat, there may be only a slight depression. Harvey[841] says that this hard, white, shining, translucent band from compression of the connective tissue is the first stage of the parchment or vellum skin, and is chiefly noticed in fresh bodies. The borders are swollen and œdematous, called by Lacassagne “bourrelet de sillon.”
The skin beyond the furrow is usually violet. Authors differ as to whether this is due to congestion or hemorrhage. Roth[842] in 49 cases found swelling below the furrow 27 times. Hackel found ecchymoses above the mark in thirty-five per cent of the cases of hanging. Hofmann thinks that the lividity of the upper border of the furrow is due to the stopping of the venous blood descending from the head.
The dry, hard, yellowish-brown, or reddish-brown “parchment” furrow, described by writers, is said to be common. Ogston[843] found it in one-third of his cases. It is found only when the body has remained suspended for several hours after death; indeed, may be produced by applying the ligature to the cadaver; is not at all, therefore, a proof of suspension during life. Liman states that constriction by a ligature even for some time does not necessarily cause a mummified or excoriated furrow. He saw cases in which the mark was soft, flat, scarcely colored, but little interrupted, and not parchmenty. The parchment skin seems to depend very much upon a previous excoriation of the skin. Its appearance can be prevented or delayed by examining a body soon after death or by rehanging it; and after it has appeared it will disappear on the application of some liquid. Taylor[844] compares this parchment mark[749] to the cutis from which the cuticle has been removed for two or three days.
Slight abrasions and ecchymoses are sometimes found in the furrow. Ecchymoses alone do not indicate whether suspension has been before or after death; but abrasions with hemorrhage strongly suggest suspension during life. Devergie regards ecchymoses of the neck as strongly suggestive of homicide. Neyding[845] says that suggillation in the groove is oftener found in strangulation than hanging. And Bremme[846] that there is no hemorrhage in the subcutaneous tissue of the mark if death occurs at once and the cord is removed at once after death; but if the cord remains for some time after death there may be hemorrhage, or if death does not occur at once, whether the ligature be removed or not.
Roth[847] found ecchymoses or small bladders at the lower margin of the furrow, 9 times in 49 cases. Riechke found only once in 30 cases a hemorrhage beneath and on both sides of the mark. Chevers did not find ecchymoses of the skin of the mark in cases of hanging. Casper found no ecchymoses in 50 of 71 cases. Maschka has seen two cases where burns on the neck resembled mark of ligature.
The furrow, when once distinct, remains constant for a long time after death, even in putrefaction. Marks from soft substances, however, disappear sooner than those from strong and uniform compression.
The NECK nearly always appears stretched. According to Roth the mobility of the head is increased by this stretching. The HEAD is always inclined to the opposite side to that of the knot. In suicides the head is usually bent forward on the chest. The HANDS are often clinched so tightly that the nails are driven into the palms. This occurs more especially when the hanging has been done with violence. When the feet touch the ground, as often occurs in suicide, the hands may be stretched out. Roth found the hands and feet flexed in 44 of 49 cases. Taylor says that we may expect to find the hands clinched when constriction of the neck is sudden and violent. The LEGS are usually livid.
The FACE varies with the duration of the suspension; at first it is pale, afterward livid; congested and swollen, if the[750] subject has been long suspended. Roth found the face pale in 43 of 49 cases. In about one-half the cases the features are calm and placid (syncope). Maschka found the lips bluish in 98 of 153 cases. The EYES are often prominent, staring, and congested, and usually the pupils are dilated. Lacassagne and Maschka[848] look upon ecchymoses of the eyelids and conjunctivæ, “piqueté scarlatin,” as important as favoring the idea of hanging or strangulation. Roth found in 49 cases the eyelids closed 28 times; half open, 12; congested in 6; ecchymosed in 2. Pupils dilated in 31; narrowed in 2. Dilated in 97½ per cent of Ogston’s cases (Cases 85, 86; rupture of crystalline lens). Harvey[849] says the blood was found flowing from the EAR in 6 cases of nearly 1,500, but no details were given. Ogston, one case. Hofmann saw a case in which there was bleeding from the ears. He says this is not due, as has been supposed, to rupture of the tympanic membrane, but to hemorrhage from subcutaneous vessels (Case 27).
The TONGUE is usually livid and swollen, especially at the base. According to Tidy, Dr. Guy looks on this as showing that suspension took place very probably during life. In about one-third of the cases the tongue is protruded and compressed between the teeth; sometimes bitten. Some observers found it protruded only as a result of putrefaction. The protrusion of the tongue is not believed to depend on the position of the ligature. Hackel in 67 cases found the tongue lying forward in all cases where the cord was between the larynx and the hyoid; in 55 per cent in front of the teeth, in 18 per cent between the teeth; where the ligature was lower down, the tongue was behind the teeth. He found by experiment that in the spasmodic expiratory effort the tongue was thrust forward; in the inspiratory movement, drawn backward. He concluded that the forward movement was the result of reflex action. Maschka[850] found the tongue between the teeth 58 times in 149 cases. Roth in 49 cases found the tongue projecting and bitten in 22, the teeth shut in 15 others; in 15 the mouth was open; the tongue was retracted in 30 cases.
Harvey, after examining reports of nearly fifteen hundred hangings, says: “In the majority of instances immediately after death[751] the features were placid, the face pale, the eyes not unduly prominent, the mouth closed or half open, the tongue pressed against the teeth but not protruding; the superficial veins full, but the head, neck, and trunk free from lividity. After a longer or shorter time, however, and apparently after a very few hours, in India, all this is changed. Livid patches appear about the chest, back, and shoulders; the face and head become bloated and puffy, the tongue and eyes protrude.”
Bloody froth is sometimes seen at the nose and mouth.
Saliva is invariably secreted and runs out of the mouth down on the chin and chest. Its presence is considered as evidence that suspension occurred during life. The URINE and FÆCES are sometimes found to have been expelled. These discharges occur in all kinds of violent death. Tardieu found them, however, but twice in 41 cases of hanging. Roth in 49 cases found discharges of fæces in 17 and urine in 4; in 15 cases not noticed.
Harvey mentions a case where internal piles had burst, and there were stains and clots of blood about the perineum and anus. In such cases without careful examination there would naturally be a suspicion of violence.
In about one-fourth of the cases the GENITAL ORGANS are congested. The penis is large and more or less erect; seminal fluid, generally prostatic, and sometimes mixed with blood, is often expelled. The fluid may pass only into the urethra and it may be necessary to press the urethra to secure it. The clitoris may be found erect, and there may be a sort of menstrual flow. Orfila showed by experiment that swelling of the sexual organs and emission of semen can be produced after death in those who had been suspended during life. The flow of semen is found in all kinds of death by violence. Roth in 39 cases of hanging of men found the penis enlarged 18 times and ejaculation in 19. Hackel found the penis swollen in 43 per cent of cases of asphyxia. Erection may come on soon or late, even days after death.
Internal Appearances.—The CONNECTIVE TISSUE UNDER THE MARK is usually white and condensed, the more so if the body has been long suspended. This dryness or condensation was found by Hackel in 52 per cent of hangings. Deeper-seated parts are injured only when the hanging has been violently done. The MUSCLES, especially the sterno-mastoid, are sometimes[752] ruptured. Hofmann[851] reports several cases. Lesser[852] in 50 hangings saw 11 ruptures of muscle. Maschka never saw the rupture in suicides. The sterno-mastoid was ruptured in the case of Wirtz (Case 96) and Guiteau (Case 95). Hackel in 67 cases failed to find the muscle ruptured. Hofmann[853] believes that the rupture of the muscle is sometimes post mortem. Coutagne[854] found the sterno-mastoid muscle ruptured once in 24 cases (Cases 29, 89, 95, 96).
The LARYNX may be fractured or dislocated. These lesions are very rare in suicide; more frequent in homicide and judicial hanging, and in the old where the cartilages are calcareous. Remer found the injury in but 1 case in 101 of suicidal hanging. Barker found the larynx lacerated in his judicial cases.[855] Harvey says that the TRACHEA was reported lacerated 11 times in nearly 1,500 cases; twice the laryngeal cartilages were separated from each other. In 5 these cartilages were fractured, but there was nothing to show under what conditions. Hemorrhage in vicinity of larynx, 43 times. Pellier[856] reports 1 case, and adds that the existence of the lesion easily escapes notice because of the mobility of the cornua. Roth in 49 cases failed to find any fracture. Pellier found the cricoid was injured oftener than the thyroid, which is the reverse of what is found in strangulation. Cavasse[857] was unable to cause fracture of larynx by hanging the cadaver. Chailloux[858] collected 6 cases of fracture of larynx in hanging. He concluded that the fracture could not be produced on the cadaver by hanging, and is, therefore, caused during life. Coutagne[859] in 24 cases found fracture of thyroid cartilage 8 times (Cases 9, 51, 82).
The HYOID BONE is rarely dislocated. Orfila mentions a case of fracture. Barker found the bone usually fractured in judicial cases. In the case of Wirtz (supra) the greater cornu was broken. Pellier reports 2 cases. Hofmann[860] says the hyoid cornua are often fractured, especially when the ligature is between the hyoid bone and thyroid cartilage. Coutagne[753] found fracture of hyoid bone 8 times in 24 cases. He attributed the fracture to pressure against the spine. Pellier speaks of fracture of STYLOID PROCESS (Cases 51, 84, 88, 89, 95, 96).
Dr. Barker, of Melbourne,[861] states that in 50 cases of hanging by the old method there was not one case of fracture or dislocation of vertebræ. After adopting his suggestion to place the knot near the spine, he found that dislocation occurred between the second and third cervical vertebræ with fracture of the third and pressure on the spinal cord. Death was sudden and complete. The drop in these cases was short, three to four feet. Coutagne thinks that the ordinary mobility of the head, axis, and atlas on each other have led reporters into the mistake of supposing a dislocation of vertebræ. Roth failed to find fracture of vertebræ in any of 49 cases. These injuries are especially rare in suicide; but in violent hanging, dislocation or fracture may occur and also rupture of the ligaments. Harvey gives 5 cases of dislocation of vertebra and 4 of fracture of vertebra in suicides. Three of the latter were doubtful. Tardieu says these fractures have no significance as to the hanging having occurred during life. They can be produced on the cadaver; but infiltration of clotted blood around injured vertebræ shows that suspension occurred during life (Cases 5, 7, 8, 68, 76 to 79, 83, 84, 91, 92, 94).[862]
The CAROTID ARTERIES may be injured; usually the inner and middle coats are torn; and hemorrhage may occur into the wall of the vessel. The common carotids are the ones usually affected, and just below the bifurcation, but the external is also occasionally injured. The injury is said to be due to the stretching and squeezing of the artery, stretching being the most effective since the rupture often occurs at a distance from the mark of the ligature. Such injury of the artery does not prove that hanging took place during life because it has been produced on the cadaver; but hemorrhage into the wall of the vessel or wound or rupture after death is very improbable. Maschka says the lesion is very rare. Tardieu says that the injury to the carotid is rare and therefore unimportant. Pellier reports 4 cases of rupture of carotid in a total of 23. Levy records the experiments of Hofmann, of Vienna, and Brouardel[754] and himself, of Paris, 5 in number. He concluded that compression of the carotid arteries, if it produces obliteration, can cause rapid loss of consciousness and death; and explains why in incomplete suicide the subject is unable to help himself. Coutagne found rupture of carotids 10 times in 24 cases. He insists on the importance of the lesion.
Hofmann[863] says the rupture is always transverse, may be simple or multiple and may occur in suicides; more apt to occur when the ligature is thin. Lesser[864] tabulated 50 fatal cases of suicidal hanging; in 29, he was satisfied that the hanging occurred during life. In 3 of these the skin of the neck alone showed any lesion; there was a double mark, the skin being otherwise bloodless. In 5 the deeper soft parts were the only ones affected. In 3 the skin showed lesions, the deeper soft parts none, but either the hyoid bone, larynx, or vertebræ were involved. In 12 the skin showed no mark, but the deeper soft parts and either the larynx or hyoid bone were involved; and in 6 the hyoid bone only or the bone and larynx were injured. In the remaining cases it was not possible to say that the hanging occurred during life. In 2 cases there were no marks at all; in 9 there were changes in the skin; in 4, changes in the skin and deeper parts; in 2, changes in the skin, deeper parts, and hyoid bone or larynx; in 3, changes in the skin and hyoid bone or larynx, or both. In 14 of the 50 cases the hyoid bone was fractured; in 20 the larynx; and in 1 the vertebræ. The common carotid arteries were injured in 6. The number and severity of the lesions bore no constant relation to the thickness of the ligature, nor to the force used, but rather to the position of the body.
Ecker[865] reported a case of suicidal hanging in a man, age 40, where the soft palate was swollen and filled up the passage so that the air evidently could not enter.
The LARYNX and the TRACHEA are usually deeply congested, of a red color; a violet color indicates putrefaction. Ogston reports mucus but not bloody froth 9 times in the pharynx, 6 in the trachea, and 4 in the lungs, in a total of 40 cases. In one case there was a quantity of blood in the larynx and pharynx. Taylor thinks that pinkish froth in the trachea indicates incomplete obstruction; and Chevers that it is due to spasmodic efforts to breathe when the obstruction is nearly complete. Chevers always found clear mucus in the larynx and upper part of trachea, each follicle being marked by a minute[755] globule of mucus. Harvey states that this was noted a few times in his reports. Baraban[866] discusses the condition of the epithelium of the air passages in hanging.
The condition of the lungs and heart varies according to whether death is due to syncope or asphyxia. Ogston found, in 22 cases, the lungs were expanded in 4 and collapsed in 2.
Harvey says the LUNGS are congested in over seven-eighths of the cases; emphysematous in a few; and subpleural ecchymoses present in a few. Patenko[867] experimented on dogs by hanging them. When the constriction occurred after expiration the lungs were congested; when after inspiration, not congested. In the first case (p. 223) the blood flows from the periphery to the heart and thence to the lungs, but cannot flow from the lungs because of the difficult circulation in the dilated pulmonary vessels and deficiency of intrathoracic pressure. There is in both cases cerebral congestion in the region of the bulb. Tardieu holds that punctiform ecchymoses and apoplexies do not occur in hanging unless suffocation has preceded. Pellier,[868] however, found these ecchymoses 14 times in 22 cases. He says that the lesion is not characteristic of suffocation, and quotes Lacassagne, Grosclaude, Dechoudans, Vicq, Chassaing, and Legroux to the same purpose. Hofmann[869] says that the ecchymoses are relatively rare in adults. Maschka[870] found them 18 times in 153 cases.
Harvey states that the presence of serum in the PERICARDIUM seems more a matter of time elapsed after death than anything else. Still the fact is that it is found much oftener in strangulation than in hanging. The difference is explained by the comparative slowness of death in strangulation. Harvey finds that in about one-half of the cases, if the body is fresh, the right side of the HEART, pulmonary artery, and venæ cavæ are full of dark fluid blood, the lungs being also much congested, and the signs of death by asphyxia well marked. When blood is found in both sides of the heart, it is probable that death is due to neuro-paralysis. When decomposition is advanced all the cavities are often empty. Taylor says that if the examination is delayed for several days, the distention may not be observed.
The STOMACH is often much congested, and this fact might sometimes suggest the possibility of poisoning. The LIVER, SPLEEN, and KIDNEYS are usually much congested. Hofmann[871] says that this occurs in the kidney only when the body has been hung a long time.
The BRAIN is rarely much congested. In 101 cases Remer found hemorrhage but once; and in 106 cases Casper failed to find it. Tardieu[872] says the brain is oftenest anæmic. If, however, the body is cut down and placed horizontally, the blood-vessels of the brain may fill up. Evidence may be found in the brain suggesting insanity and therefore an explanation of a probable suicide. Harvey says that hemorrhages in or about the brain are found in a much larger proportion of cases in India than in Europe in cases of hanging. “No common condition likely to cause extravasation is apparent, only one man being noted as plethoric, but in many the rope seems to have been very tight.” Champouillon[873] reports a case of suicide in a man, age fifty-two; the rope broke and the body fell. The physician who made the necroscopy reported a rupture of the pons Varolii. Champouillon believed that the rupture must have been made in removing the brain from the skull. Wilkie[874] reports a judicial hanging in which a man age about twenty-five, fell about three and one-half feet. A recent clot was found in the brain. The experiments of Brouardel of hanging rabbits showed the brain anæmic.
The conjunction of the following appearances would suggest that the hanging had been of some duration: lividity of face, congestion and prominence of eyes, dryness of skin under the ligature, deep furrow, congestion of sexual organs, swelling and lividity of lower limbs, hypostatic congestion of lungs.
Page experimented on a young cat and young dog; both were hung in the same way. Examination of the cat showed the veins generally engorged; sublingual veins much engorged; tongue protruded slightly and much swollen; no frothy mucus in bronchi. In the dog the tongue did not protrude and was not swollen; right cavities of heart contained blood, left empty; brain and other organs normal. In the cat, the lungs were uniformly congested, dark red; no ecchymoses. In the dog, the lungs were much distended, posterior borders mottled[757] violet; emphysematous patches on surface; no apoplectic effusions; subpleural ecchymoses bright red, irregular, clearly defined in outer surface, most numerous toward the roots and on the lower lobes.
Pellereau[875] gives an account of hanging as seen by him in warm climates. He had not seen the elongation of the neck described nor the erection of the penis, nor subconjunctival ecchymoses, nor fracture of larynx, nor rupture of walls of carotid artery, nor subpleural ecchymoses, nor fracture of vertebra. He always found a mark on the neck; the left cavities of the heart always empty, the right always full of black blood. Mackenzie says that in 130 cases of suicidal hanging, the protrusion of the tongue between the teeth, the open and protruding eyes, clinched hands, and blue nails were very frequent, the tongue was found bitten many times, there were urethral and rectal discharges and rupture of carotid artery. The penis was found erect several times. The hyoid bone fractured 24 times in 93 cases. In no case was the larynx or vertebra fractured. In 73 cases ropes were used; in 30, portions of clothing. The marks of ropes were always well defined, indented, and parchment-like; the marks of soft ligatures faint and reddish. In no case were the muscles of the neck, the larynx, trachea, or large bronchi injured, and in none was there subcutaneous hemorrhage or blister.
Proof of Death by Hanging.
As in strangulation, no single sign in any given case is sufficient of itself to prove that death was caused by hanging. But the sum total of the lesions found, viewed in the light of the surroundings of the body, will suffice to lead to a definite conclusion.
The fact that a body has been found suspended does not of itself prove that hanging caused the death, because the victim may have been killed in some other way, and the body afterward hung up to avert suspicion. Chevers records many cases of this kind.
The value of the presence or absence of marks on the neck and the characters of the marks has been questioned. Orfila, Casper, and Vrolik have shown by experiment that if a body is hanged within one or two hours after death the furrow, parchment skin, lividity, and the density of the connective tissue will appear just as is seen when suspension has occurred during life; but ecchymoses and infiltration, clotted blood in the[758] skin, connective tissue, and muscles of the neck suggest suspension during life.
If a cord is removed immediately after death, there may be scarcely any mark at all.
Tardieu collected 261 cases of suicide by hanging where the subject was not entirely off the ground. In 168 the feet rested on the ground; in 42 the subject was kneeling; in 29 lying down; in 19 sitting, and 3 were huddled up or squatting. Fatal hanging may, therefore, occur in almost any position of body. He shows incomplete hangings by thirteen plates. Taylor also collected reports of 11 cases in a few years; in 3 the subjects were nearly recumbent; in 4, in a kneeling position; in 4, sitting. Remer in 101 cases of suicidal hanging found in 14 that the body was either standing or kneeling; in 1, sitting. Duchesne published 58 cases of partial suspension, 26 of which were new. Some of these failures of complete suspension were due to soft and elastic cords.[876]
Taylor says that “that which is difficult to a conscientious medical jurist in confining himself to the medical facts is often easily decided by a jury from these as well as the general evidence afforded to them.”
The limbs may be secured by the suicide before hanging himself. Persons even with some disability of the hand have suicided by hanging. Blindness is no obstacle, nor age; a boy as young as nine and a man as old as ninety-seven.
Burger[877] fully discusses the question whether the hanging is before or after death.
Hanging—Suicidal, Homicidal, or Accidental?
Hanging is usually suicidal. Lesser[878] states that for three years, 1876-79, there were admitted to the Berlin morgue 274 bodies of “hanged,” of which 272 were suicidal; 2 infants of three and eighteen months, homicidal. One man had first tried to kill himself with sulphate of copper; another by cutting his throat; a woman by cutting her arm. The other cases were uncomplicated. Pellier states that the number of suicides in France[759] from 1876-1880 was 13,445, and nearly all were by hanging. Taylor[879] states that 2,570 persons committed suicide by hanging in England in five years, 1863-67; four-fifths of these were males. Harvey[880] reports for three years 1,412 cases of hanging in India, of which 2 were accidental, in 3 there was presumption of homicide, the rest probably all suicidal.
Feebleness of body does not preclude subjects taking their lives in this way. They sometimes also wound or poison themselves first and hang themselves afterward. A subject being found suspended in a room fastened on the inside, would be suggestive of suicide. The absence of signs of struggling or of any marks of injury also favors the idea of suicide.
The possibility of a suicide breaking a rope, being injured by the fall, and rehanging himself successfully, must be admitted (Cases 57, 58). The possibility of blood flowing after death must not be forgotten.
It is worthy of note that after beating or other violence children and women may commit suicide from shame. Again, as Tardieu says, many have hung themselves while partially intoxicated, and it is likely that some such have just previous to the suicide met with falls or other accidents which have left marks like those of violence. He also records the case of a woman who fastened a cord to a bed-post, put her head in a noose while kneeling on the bed, and made a deep wound in her arm with a razor. She closed the razor, laid it aside, and fainted from loss of blood. She must then have fallen forward and died from the pressure of the cord on her neck.[881]
Homicidal hanging is rare but does occur. Where the hands are tied together; where the injuries produced by the cord are severe; where there are contusions and well-marked ecchymoses; where the laryngeal cartilages and hyoid bone are fractured or the cervical vertebræ dislocated or fractured; or where the carotids are injured or there is hemorrhage into their walls; where there are severe wounds, the hemorrhage from which would be sufficient to threaten syncope; where there are many marks of violence on the body; where there is evidence of a severe struggle—in all these cases murder may be reasonably suspected. The number, situation, extent, and direction of[760] must be carefully noted and weighed. If these are out of proportion to the ligature, the suspension, etc., they strongly suggest homicide, although they may occur in suicide (see Cases 4, 11, 18, 20, 28, 29, 44, 52, 55, 59, 66).
Homicidal hanging may be committed by an assailant who is strong on a subject who is weak, on a child, a woman, an old person; on one stupefied by liquor or narcotic poison; or by many combined against one person.
Cases are reported where injuries were inflicted or poison given, and the subject was afterward hanged to avert suspicion. Most of these cases are those of murder either by strangulation or suffocation (Cases 64, 65, 67, 68, 69, 70, 74).
Sometimes hanging is accidental. Children and even older persons play at hanging successfully. Taylor mentions the case of a boy who witnessed a hanging and afterward tried the experiment himself to ascertain the sensation, and caused his own death.
Tardieu[882] relates the case of a man, T., age 37, of small stature, feeble constitution, very thin, of sinister face, eyes hollow but lively, cunning nose and mouth, who meeting a man aged 81, learned that he had some trouble with his leg and promised to cure him. The old man lived alone. T. told him to buy a strong cord as thick as his little finger and one and one-half yards long, and keep the whole thing a secret. T. would see him at his room at 7 P.M. The old man became suspicious and had T. arrested. The investigation showed that already T. had made away with three old men by hanging, who were known to be opposed to suicide. Their bodies showed no trace of violence. Two others had escaped when the cord was passed around their necks.
Tardieu gives a number of cases of suicidal hanging which were falsely attributed to criminal violence, in which the pressure of public opinion joined to circumstances improperly explained by inexpert physicians caused deplorable judicial errors.
ILLUSTRATIVE CASES.
Suicide.
1. Harvey: Indian Med. Gaz., 1876, xi., p. 2.—Man, age 30. Found hanging by turban to bars of cell door; slip-knot around neck; heart beating feebly; died in about a minute after being cut down. “The point of suspension was forty-seven inches from the ground, the position[761] of the noose twenty-eight inches, and the feet were forty-two inches away from the door supported on the toes.” Experiment showed that the turban could not have borne the full weight of the body. He died from strangulation.
2. Ibid., p. 3.—Insane man, age 60. Put his neck in a V-shaped fork of a tree and let his body swing. A broad abrasion found on each side of neck. Scalp, brain, and membranes much congested; reddish serum in lateral ventricles; two ounces clear fluid in pericardium. Lungs congested; all the heart cavities contained blood.
3. Ibid., p. 5.—Woman, age 28. Two marks of ligature on neck; one deep and circular passed up behind left ear; the other passed from the circular mark behind, crossed it on either side under lower jaw, thence up to chin. Appeared at first to be a case of strangulation following hanging; but the two marks were finally explained, that after the body was taken down it was ordered up again until the police should arrive.
4. Ibid., p. 5.—Man, age 45; first cut his throat and then hung himself. “He had probably only just had time to hang himself before dying.”
5. Ibid., p. 30.—Woman; hung herself with a twisted cloth. There was much ecchymosis about the neck and upper part of chest; lungs much congested; fibrin clot in left mitral orifice; liver, spleen, and stomach congested; transverse ligament of atlas ruptured.
6. Ibid.—Man, age 39. Distinct mark of cord around neck; no other mark of violence; laceration of larynx and dislocation of odontoid process; hands clinched; involuntary discharge of semen; thoracic and abdominal organs normal.
7. Ibid.—Man, age 70. Mark of cord around the neck, superficial in front, deep behind; second cervical vertebra dislocated; tongue slightly protruding; fingers clinched; meningeal vessels engorged; lungs tubercular, congested; right heart contained a little coagulated blood.
8. Ibid.—Sex and age not given. Found hanging on a tree; usual signs; odontoid process fractured; rope in a double noose without knot, a common dooree, such as is used for drawing water.
9. Ibid., p. 32.—Man, age 50. Face livid, eyes red and protruding; teeth clinched; lower jaw retracted; tongue behind the teeth; hands and feet contracted; anus covered with fæcal matter; circular depressed mark of cord around neck, hard as parchment, slightly ecchymosed along edges; some infiltration of blood in connective tissue beneath the cord; some tearing of soft parts; laryngeal cartilage displaced. Brain and membranes congested. Right cavities of heart distended with dark blood. Trachea congested.
10. Hurpy: Ann. d’ Hygiene, 1881, vi., pp. 359-367, with illustration.—Woman, age 77, suicided by hanging in the following way: a[762] short cord was fastened by one end to a table leg; the other end was around her neck; she lay on the floor, face downward, clothing not disordered. The brain was congested; lungs congested and emphysematous; left side of heart empty (see Fig. 23).
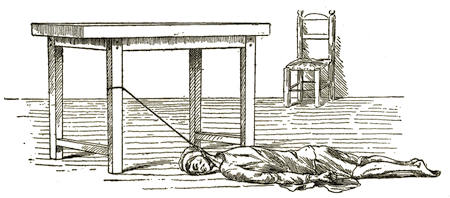
Fig. 23.—Suicide. The cord on the neck is 44 cent. from the cord on the table leg; vertex of head 30 cent. from table leg. Case reported by Hurpy (see p. 717, Case 10).
11. Champouillon: Same journal, 1876, xlvi., p. 129.—Man, age 62; first tried to suffocate himself with charcoal smoke and then hung himself, but the rope broke and the body fell. He lived two days.
12. Pellier: Lyon thesis, 1883, No. 188, p. 72.—Boy, age 16, hung himself; rope broke; he was resuscitated; reddish circular furrow on neck, not like parchment; he had erection and ejaculation; buzzing in his ears and flashes before his eyes.
13. Lacassagne: Pellier thesis (supra), p. 71.—Man; hung himself; was cut down and sent to hospital; was aphonic for four days; then a severe bronchitis set in, and at the end of a week a gangrenous expectoration. The mark of the cord lasted fifteen days.
14. Maschka: Archiv. de l’anthrop. crim., Paris, 1886, i., pp. 351-356.—Man, age about 60, found dead under a tree in the woods near Prague. No sign of violence. A cord thick as a sugar-loaf around the neck; another cord attached to a branch of the tree. There was at first a strong suspicion of violence, but the conclusion reached was that he had hung himself and that the body had fallen from breaking of the cord; that death was due to asphyxia was shown by the furrow on the neck, the dark liquid blood, and the congested lungs. There was no infiltration below the furrow in the neck, and no lesion of larynx. The man had shown signs of melancholy.
15. Friedberg: Virchow’s Archiv, 1878, lxxiv., p. 401.—Suicidal hanging. Examination twenty-eight weeks after death. The front of the neck showed a groove above the larynx, firm and of gray color; ecchymosis in subcutaneous tissue.
16. Bollinger: Friedreich’s Blätt. f. ger. Med., 1889, xl., p. 7.—Man, age 48; found dead. Had made a ligature out of a night-gown and tied it around his neck, the other end around top of a low bed-post; his neck hung by the ligature placed below the larynx. Illustrated.
17. Med. Times and Gaz., London, 1860, ii., p. 39.—Woman; had collected accounts of celebrated persons who had been hanged; finally hanged herself.
18. E. Hoffman: Mitt. d. Wien. Med. Doct. Colleg., 1878, iv., pp. 97-112.—1st. Woman, age about 25; found dead sitting in bed, a handkerchief around her neck fastened to the bed-curtain. The police thought she had been killed and then hung, but the physician concluded that she had committed suicide. An examination of the stomach showed that she had previously tried to poison herself with arsenic.
19. 2d. Woman, age 51; found hanging in half-lying position.
20. 3d. Man, age 50. First tried to kill himself with phosphorus, then sulphuric acid; finally hung himself in a half-kneeling position.
21. Müller-Beninga: Berlin. klin. Woch., 1877, xiv., p. 481.—Man, age 40; hung himself. There was no swelling of genitals and no soiling of clothing. Necroscopy showed death from asphyxia, and in urethra near meatus quite a quantity of seminal fluid, as shown by microscopical examination.
22. Tardieu: Op. cit., p. 18.—The Prince of Condé was found hanging in his room, August 27th, 1830. He was suspended by two handkerchiefs to a window fastening, his feet, however, touching the floor. The knot was at the back of the neck (as shown by the illustration), the face turned slightly to the left, the tongue protruding; face discolored; mucus at the mouth and nose; arms hanging and stiff; fists shut; heels raised; knees half bent. The text says that the knot was nearly under the right ear, but the illustration shows a different position (see Fig. 22, p. 743).
23. Allison: Lancet, 1869, i., p. 636.—Three cases of suicide by hanging, in which there was no mark: 1st. Woman, hung herself with a piece of sheep-net band; cut down before death. 2d. Man, hung with plough-string; cut down in about six minutes. 3d. A heavy man.
24. Tardieu: Op. cit., pp. 93-105.—Woman, died of coma and asphyxia from suicidal hanging, according to report of Drs. Costan and Facieu. Tardieu approved their report. It was at first thought a case of homicide with subsequent hanging, more especially because of the kind of knot used, nœud d’artificier. But Tardieu showed that it was also a nœud de batalier. Her feet touched a chair, and her knees were bent. There was a neckcloth in front of her mouth, but it did not seem to have interfered with respiration.
25. Ibid., pp. 67-72.—The famous case of Marc-Antoine Calas, who committed suicide by hanging (see Voltaire, “Traité sur le tolérance,” etc., in Nouv. Philos. Histor., 1772, xxxii., p. 30). He hung himself to a door. No sign of violence. The city hangman said it was impossible for a man to commit suicide in that way. The father was accused and convicted of homicide. Tardieu shows that the act was a suicide.
26. Ibid., p. 72.—Another famous case. A woman, age 30, hung herself to the key of her bedroom door. Her husband cut her down. He was accused and convicted of the crime and condemned to prison, where he died. Tardieu showed that the case was one of suicide.
27. Hofmann: Wien. med. Presse, 1880, xxi., p. 201.—Man, age 68, suicide by hanging. There was profuse hemorrhage from both ears.
28. Ibid.: 1878, xix., pp. 489-493.—Woman, found dead sitting in bed. She first tried to poison herself with arsenic, then hung herself.
29. Ibid.—Man, tried to poison himself with phosphorus and sulphuric acid, then hung himself. There was a transverse rupture of the sterno-cleido mastoid muscle and suffusion in its sheath.
30. Maschka: Wien. med. Woch., 1880, xxx., pp. 714, 747, 1075.—Man, age 63. It was at first a question of suicide by hanging or homicide by strangling. He concluded that it was the former.
31. Ibid.—Also man, age 58. Similar case. Same opinion.
32. Ibid. 1883, xxxiii., pp. 1118-1120.—Woman. age 23. Question whether she committed suicide by hanging or was strangled and then hung. Opinion, that it was a case of suicide.
33. Hofmann: Allg. Wien. med. Zeit., 1870, xv., pp. 192-214.—Man, age 60. Suicide by hanging or homicide; opinion, that it was the former.
34. Van Haumeder: Wien. med. Woch., 1882, xxxii., pp. 531-533.—Suicide by hanging or homicide. There were many wounds in the head; these occurred during the delirium of typhus.
35. Maschka: “Sammlung gericht. Gutacht.,” etc. (Prag), Leipzig, 1873, p. 137.—Boy, age 9; found dead in sitting position. Injuries on neck and elsewhere. Question, had he hung himself or been choked? Were the injuries inflicted before or after death? Opinion, suicide.
36. Ibid., p. 144.—Boy, age 13. Found hanging in sitting position. Question whether murder, suicide, or accident. Opinion, suicide.
37. Ibid., p. 149.—Woman, age 60; found hanging, sitting position. Suicide or homicide. Opinion, suicide.
38. Ibid., p. 156.—Woman, age 30; found hanging. Opinion, suicide.
39. Ibid., p. 165.—Man, age 63. Suicide by hanging, or homicide by strangling? Opinion, suicide.
40. Berliner: Viert. f. ger. Med. und öff. San., 1874, xx., pp. 245-253.—Woman, age 30; found hanging. Opinion, suicide.
41. Deininger: Friedreich’s Blät. ger. Med., 1884, xxxv., pp. 47-59.—Woman, age 61; found hanging. Opinion given, suicide.
42. Mader: Bericht d. k. k. Rud. Stift., Wien. (1875), 1876, p. 378.—Woman, age 43; tried to hang herself. She was at once cut down, bled, and taken to hospital unconscious. Next day, face red; pulse and temperature normal. Third day, conscious and could speak, but not aloud; tongue twisted and turned to right; paralysis of right hypoglossal nerve. Uvula drawn to left. Skin of right limb felt “furry.” Applied electricity and gave strychnine; phonation was more distinct during the use of the battery. Two months later she was still aphonic, but the vocal cords were in better action. The right hemiparesis was lessened.
43. Grant: Lancet, 1889, ii., p. 265.—Man, age 48; found sitting against a door, hung to the knob by a handkerchief.
44. White: Lancet, 1884, ii., p. 401.—Woman, age 53, insane. Made several attempts at suicide; once with a stocking around her neck, once with an apron; the last time by fastening a portion of her dress to a ladder. She was quickly cut down, cold affusion applied, and artificial respiration (Sylvester). The eyes were prominent and glassy, pupils widely dilated, no reaction to light; conjunctivæ insensitive; lips livid; tongue swollen and pale; face pale; oblique depressed mark on neck, most marked on left side; skin cold; no pulse; no heart-beat recognizable; no respiration; no reflex action. Galvanism failed to arouse any muscular action. The details are too numerous to give all of them. There was reduplication of heart-sounds for several days, due to interference with pulmonary circulation. She recovered both bodily and mental health.
45. Richards: Indian Med. Gaz., 1886, xxi., p. 78.—Man, age 20; suicide; was cut down and lived for four days.
46. Kite: Univ. Med. Mag., 1888-89, i., p. 475.—Man, age 69; suicide.
47. Terrier: Prog. Méd., 1887, vi., pp. 211-214.—Two men, age 29 and 25, insane. Attempted suicide by hanging. Both resuscitated.
48. Nobeling: Aertz. Intellig.-bl., 1884, xxxi., p. 213.—Two suicides by hanging; men, ages 24 and 40.
49. Ritter: Allg. Wien,. med. Zeit., 1886, xxxi., p. 375.—Soldier, found hanging. Cut down in ten minutes. Artificial respiration applied; fifteen minutes later, an effort at respiration; face changing from blue to white and then to red; pulse small, irregular; still unconscious; mark of ligature distinct; a few hours later had a maniacal seizure; gave morphia hypodermically and he slept; was also aphonic. Gradually recovered and returned to duty.
50. Strassmann: Viert. f. ger. Med., 1888, xlviii., pp. 379-381.—Three[766] cases of suicidal hanging in men, ages 27, 37, and 40. The last was found kneeling.
51. Balta: Pest. Med. Chir. Presse, 1892, xxviii., p. 1244.—Man, age 45-50; hanging; suicide. Thyroid cartilage and hyoid bone broken.
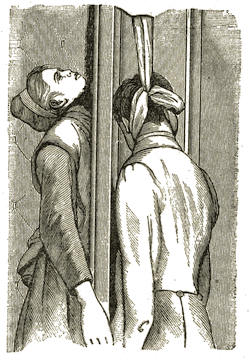
Fig. 24.—Double Suicide
(see Case 55).
52. Hackel: Op. cit., p. 35.—Man, found hanging to a beam by a sheet. Had previously tried to choke himself with his hands.
53. Ibid.—Two cases of suicidal hanging where the cord made no mark. In the first the body hung free; in the second the body was partly supported. In the first there was no rubbing of the skin; in the second the body was soon cut down.
54. Freund: Wien. klin. Woch., 1893, vi., pp. 118-121.—Man, found hanging; cut down, but could not be resuscitated. Ligature between hyoid bone and larynx, then crossed over itself about middle line of neck, passed up along each side of face, knotted above the head, then thrown over a beam, and on the other side the loop was caught between his legs.
55. Hoffman: Op. cit., p. 525, illustrated.—Case communicated by Dr. Rosen, of Odessa. Man, age 21, and woman, age 17, hung themselves by same ligature thrown over an open door, one of them on each side. They had previously tried other means of suicide without success (see Fig. 24).
56. Ibid., p. 530.—Man found hanging by handkerchief to branch of tree but sitting on the ground. Mark of handkerchief superficial and pale. When the necroscopy was made the mark had disappeared. Also a similar suicide where there was no mark at all.
57. Ibid., p. 541.—Man found hanging to a window. Another man cut the cord and the suspended one fell into a cellar, fracturing his skull.
58. Ibid.—Man found hanging; cut down; the fall caused rupture of liver.
59. Ibid., p. 539.—Drunkard hung himself; there was evidence that he had previously injured himself during his drunkenness.
60. Ibid.—Boy hung himself because he had been punished by the[767] schoolmaster. There were marks on his back and lower limbs from the punishment.
See also Taylor, “Medical Jurisprudence,” pp. 451-452; Tidy, “Medical Jurisprudence,” incomplete hanging, Cases 33 to 36 and 62; Hofmann, “Lehrbuch,” p. 538.
Homicide.
61. Harvey: Indian Med. Gaz., 1876, xi., p. 3.—Woman, age 20, feeble. Her mother-in-law had kicked her; she probably had fainted; supposing her to be dead, the husband hanged her to a tree within half an hour after the supposed death. Autopsy: No marks of injury; oblique mark of cord on right side of neck; tip of tongue between the teeth; face somewhat livid; right side of heart full of dark blood; lungs congested posteriorly.
62. Ibid., p. 4.—Woman, age 38. Rope close under the chin passed upward behind the ears. Head bent on chest. Large wound above clavicle. Under the rope was a depression (made after death) but no hemorrhage. Much blood in abdomen and a hole in the liver. Kidney bruised and blackened. Right lung torn through; blood in pleuræ. Wounds were supposed to be gunshot, but the husband confessed that he had thrust a sharp solid bamboo into her body and afterward hung it up. She died of hemorrhage.
63. Rehm: Friedreich’s Blät. f. ger. Med., 1883, xxxiv., pp. 332-362.—Man, age 73; first roughly maltreated; afterward hung.
64. Tardieu: Op. cit., p. 125.—Woman found hanging in her room. Circumstances indicated homicidal strangulation and that the hanging was done to avert suspicion. Post-mortem examination showed the base of the tongue ecchymosed, and ecchymosis extending up to the soft palate; mucous membrane of pharynx congested; connective tissue and mucous membrane between hyoid bone and larynx congested posteriorly; epiglottis showed slight ecchymosis, mucous membrane red. These ecchymoses were not caused by the cord, for the latter was placed below the hyoid bone and this bone was not broken. There were also marks on the collar-bone like the mark of two hands.
65. Ibid., p. 124.—Girl, 15 years old. Body found hanging. Post mortem showed beyond doubt that she had been violated, then strangled, then hung. Her head showed many ecchymoses from either the fist or the foot; blood flowing from left ear. Brain slightly congested. Tongue between teeth, bitten and bloody. On front of neck were two marks: the lower were impressions of fingers close together, nearly uninterrupted, and which had bruised, flattened, and tanned the skin, which here was dry, hard, and horny. This lesion was above the intraclavicular notch and extended toward the sides of the neck with regularity of curve and neatness of imprint, evidently made with[768] the right hand. Above the first furrow under the skin was a kind of track, less extended, more regular, a bruising of the same nature as the preceding, but continued, due to the pressure of the index finger and thumb of left hand. A little below the jaw was a livid place on the skin, which was otherwise unaffected by the ligature. There was nothing to indicate a circular action of the ligature. Froth in larynx and bronchi. Lungs apparently normal. Food had passed from stomach into œsophagus and air-passages.
66. Ibid., p. 122.—Woman found hanging in her room, and was resuscitated. She stated that the man who lived with her had tried to strangle her and then hung her. Tardieu saw her in hospital. Respiration short and embarrassed; pains in neck and jaw. Found narrow, circular, sinuous, horizontal, uninterrupted line around the neck below thyroid cartilage; line everywhere equal, deep, and three to four mm. wide; the skin excoriated and covered with thick crust. Below this were several superficial excoriations. There were many contusions on other parts of the body. Tardieu concluded that the mark on the neck was from attempt to strangle; the wounds elsewhere to prevent resistance. She had at the time pulmonary consumption. She died of this disease aggravated by the assault.
67. Ibid., p. 106.—The Duroulle affair. Woman found hanging. Presumption of homicide; arrest of husband; acquitted. She was found with her face to the floor, one end of a cord around her neck; another similar cord attached seven feet above to a rafter, over which it passed three times. Bidault and Boulard reported it a suicide. The results of the post mortem were as follows: Skin of a red-violet color; face swollen; eyes prominent and congested; conjunctivæ a vinous red; lips violet; tongue swollen, tip between teeth; froth in air-passages; lungs congested; brain congested; blood fluid. Circular depression around neck with congestion of skin above and below; ecchymosis in subcutaneous tissue on level of angle of jaw and about one centimetre in size, supposed to correspond to the knot. Tardieu reported that the marks rather resembled those of strangulation than hanging; the ecchymoses were more like those produced by the hand over the mouth. The marks on the face supposed to have been made by a supposed fall of the body were by him considered to have been caused by violence. He believed the woman had been strangled and then hung.
68. Ibid., p. 130.—The Daugats affair. Man found hanging, sitting on the ground, head and trunk somewhat inclined to the left; legs stretched out; clothing not disordered; the part of the cord which was around the neck was applied to the neck of the waistcoat and shirt; on his head a woollen cap. The ground had been recently swept. Necroscopy twenty-four hours afterward. Face pale; right eye open and prominent, left closed; mouth closed, contained food apparently from[769] the stomach; tongue retracted; slight mark on neck under which the tissue was normal: atlas dislocated on axis, but tissues around were normal; no lesion in spinal canal; penis not erect; moisture having the odor of urine on the shirt; large ecchymosis and infiltration of left cheek; extensive contusions on scrotum, with hemorrhagic infiltration, especially around right testicle. Veins of head engorged with black fluid blood. Brain normal. Some black fluid blood in right cavities of heart, left side empty. Lungs black. Other organs normal. Causse and Orfila concluded that the man had been suffocated and then hung. The wife and son confessed that they had injured the testicle through the pantaloons; he then fainted; they then suffocated him with the woollen cap placed over the mouth and nose; the son kneeled on the man’s belly, the body was then hung up and the head violently twisted.
69. Passauer: Viert. f. ger. Med. und öff. San., 1876, xxiv., pp. 26-49.—Woman found hanging in a kneeling position. The ligature on the neck was loose. The necroscopy showed the following: Tongue between the teeth; eyelids swollen and livid; livid spots on face and left ear; lower lip torn; a number of marks on neck; one red stripe not sharply limited; skin not parchmenty and no ecchymosis; ecchymoses of scalp; periosteum of skull reddened; hemorrhage in temporal muscle; brain and pia mater congested; much fluid in ventricle. Larynx and trachea dirty red-brown; right side of heart empty; a little dark fluid blood in left; great vessels, including aorta, containing much dark fluid blood. Lungs congested and œdematous. Liver, spleen, and kidneys congested. Opinion given that she died of asphyxia and was either choked or hanged. Reference to Royal College of Medicine, Königsberg, where the opinion was given that she died of injuries on head and neck and was afterward hanged.
70. Becker: Same journal, 1877, xxvii., pp. 463-473.—Woman, age 52; found hanging. Death caused by shock and incipient asphyxia from strangulation and probably the wounds on head and limbs.
71. Maschka: “Samm. gericht. Gutacht.,” etc. (Prag), Leipzig, 1873, published a number of interesting cases, in each of which there was a question raised as to the cause of death.
72. Ibid., p. 127.—Man found dead. Had he been strangled or hung, or had he died some other way? Opinion, death from paralysis of the brain.
73. Ibid., p. 133.—Woman, age 42; found hanging; a mark around her neck. Did she hang herself or die of other injuries? Opinion, died of other injuries.
74. Rehm: Friedreich’s Blätt., 1883, xxxiv., pp. 322-362.—Man, age 73; found hanging. Opinion, while weak, sick, and suffering from wounds inflicted by his own son, he was hanged by his daughter-in-law.
75. Hofmann: “Lehrbuch,” p. 538.—A father hung his five children, the eldest 9 years. Another man hung two children, the eldest 13 years.
See also Tidy, “Med. Juris.,” Cases 40, 48, 51, 57(?), 58(?); “Hanging after Death,” Case 50.
Judicial Hanging.
76. MacLaren: Indian Med. Gaz., 1873, viii., p. 234.—Three cases of judicial hanging; hung at the same time and cut down and necroscopy begun forty minutes afterward; drop twelve inches. In the first and third there were reflex movements for a few minutes after drop fell. First man, age 40; pupils slightly dilated; no protrusion of tongue or eyeballs; mark of cord above thyroid cartilage; no discharge of semen or fæces; ecchymosis under cord, left side; dislocation of atlas from axis; odontoid ligaments ruptured; transverse ligament uninjured. Brain and membranes much congested; clear fluid in lateral ventricles. Lungs collapsed, anæmic; one ounce straw-colored serum (measured) in pericardium; dark fluid blood in both ventricles of heart; liver much congested.
77. Second man, age 16; pupils widely dilated; eyeballs protruding. Marks of cord same as in preceding case. No discharge of fæces or semen. No ecchymosis under cord; dislocation and rupture of ligaments between axis and third vertebra. Brain did not show well-marked congestion. Lungs collapsed and anæmic. One and one-quarter ounces serum (measured) in pericardium. Heart normal; dark blood in both ventricles; liver normal.
78. Third man, age 20; pupils slightly dilated; eyeballs and tongue not protruded. Marks of cord as in preceding. No discharge of fæces or semen. Slight ecchymosis under cord; mark in front of neck. Dislocation of occipital bone from atlas. Brain and membranes much congested. Lungs collapsed and anæmic. Half ounce serum in pericardium. Heart normal; dark fluid blood in both ventricles; liver normal.
79. Cayley: Ibid., p. 122.—Man, age 35; executed by hanging. Scarcely any convulsive movements after drop fell. Necroscopy two hours afterward. No congestion or protrusion or swelling of the tongue; no muscular rigidity or contractions. About half-way around the neck was indentation of cord, obliquely directed; hardly perceptible in front; its surface appeared rubbed and compressed; no discoloration; no ecchymosis under skin. Cord lay across upper part of thyroid cartilage. Larynx and trachea not injured. Fracture and dislocation of upper cervical vertebræ. Lungs collapsed, not congested. Pericardium empty; heart distended, left side with red blood just beginning[771] to clot; right side with fluid black blood. Liver and other abdominal organs much congested. No discharge of fæces or semen.
80. Garden: Same journal, 1880, xv., p. 12.—Man, age 40, weight about one hundred and twenty pounds; drop two feet; was in a fainting condition, and had to be supported; was not probably fully conscious when platform fell. There were spasmodic retractions of arms and legs for about two minutes; forty seconds after the drop his jungeas fell off; his penis was in strong erection, and the ejaculatory movements were seen. Necroscopy one and one-quarter hours after drop fell. Head and limbs cold; eyes open, natural; tongue not protruding; fingers clinched; superficial veins contained fluid black blood. Mark of cord extended from just below left mastoid process, where the knot was applied, across the thyro-hyoid membranes to a place on right side about two inches below ear. There was scarcely a trace of it behind. Skin dark and ecchymosed, but no ecchymosis of subcutaneous connective tissues. No discoloration nor fracture in neck. Subarachnoidal fluid in excess; puncta vasculosa unusually numerous. Under surface of epiglottis reddened and showed two small dark red ecchymoses; mucous membrane of larynx and trachea pale. Lungs showed venous congestion; no infarctions or small ecchymoses; right lung emphysematous; the left showed old firm adhesions throughout. Heart large, flabby, pale, a very little blood in each ventricle; subpericardial ecchymosis one-fourth inch square anteriorly, another larger one posteriorly; extensive pericardial adhesions. Liver and kidneys congested.
81. See two cases of judicial hanging by Wilkie, same journal, 1881, xvi., p. 275.
82. Porter: Archiv. Laryngol., New York, 1880, i., p. 142.—Redemier hung. Drop five feet. Pulse beat rapidly a few minutes, then lessened in frequency and stopped beating in fifteen minutes. During this time there was violent spasm of muscles of thorax and upper limbs. Necroscopy, dark groove around neck crossing larynx just below pomum Adami. Brain congested. Lungs emphysematous. Cricoid cartilage fractured diagonally. Laryngeal mucous membrane showed ecchymosis and œdema. Vertebræ neither fractured nor dislocated.
83. Another criminal hung at the same time had dislocation of cervical vertebræ.
84. Fenwick: Canada Med. Jour., 1867, iii., p. 195.—Man executed; drop six feet; second cervical vertebra torn from attachment to third; medulla torn across; hyoid bone and tongue torn from thyroid cartilage; general congestion of viscera; lenses normal; eyes congested; clot between sclerotic and choroid coats left eye.
85. Dyer: Trans. Amer. Ophthal. Soc., 1866, p. 13.—Man, age 24; weight one hundred and seventy-four and a half pounds; drop three feet; knot under left ear; for two minutes at intervals, slight motion of abdomen, like effort at respiration, and at same time knees drawn[772] up a little. Death speedy and quiet. Cut down at end of thirty minutes. Necroscopy thirty-five minutes after drop. Body and head moist and warm; emission of semen; face livid; upper lid discolored; abrasion of skin under right ear; deep red mark around neck. Eyeballs not prominent; eyelids closed; corneæ dull; pupils a little dilated. Both lenses fractured. Brain normal; spinal cord normal. Heart empty.
86. Dyer: Same Trans., 1869, pp. 72-75.—Man hung. One eye showed fracture of lens, the other lens showed fine lines. A second case showed dislocation of a cataractous lens. A third showed fissure of lens.
87. Green: Same Trans., 1876, p. 354.—Man hung; drop seven or eight feet. Died quietly and without struggle. One-half to one hour after drop fell, eyes were examined. No lesion of capsule or lens.
88. Keen: Amer. Jour. Med. Sci., 1870, lix., p. 417.—Two criminals hung; drop five feet. Hyoid bone fractured in one; no fracture of vertebræ in other.
89. Clark: Boston Med. and Surg. Jour., 1858, lviii., p. 480.—Execution of Magee. Man, age 28; weight 130 pounds. Drop seven to eight feet. No struggle nor convulsion. Urine discharged at once. Seven minutes after drop fell, heart-beat one hundred; nine minutes, ninety-eight; twelve minutes, sixty and fainter; fourteen minutes, not audible; twenty-five minutes, body lowered. Face purple; pupils dilated; eyes and tongue did not protrude. Mark of cord just above thyroid cartilage, a deep oblique furrow except a small space under left ear; knot over mastoid process. Forty minutes, cord and strap removed; body, especially face, became paler. Necroscopy a little over an hour after drop fell. Body pale; skin mottled; small ecchymosis just above line of cord right side. Right sterno-mastoid muscle torn. Hyoid bone fractured; spine not injured. No seminal discharge. Ninety minutes, pulsation in right subclavian vein; heart-beat, eighty per minute; thorax opened, heart exposed; right auricle showed full and regular contractions and dilatations. The spinal cord was then divided. One hundred and twenty minutes, heart-beats forty per minute. These pulsations of right auricle continued at intervals for three and a half hours longer; readily excited by point of scalpel. Heart normal; left ventricle contracted; right ventricle not so; no coagulation. Brain normal; lungs collapsed; liver and spleen congested; mucous membrane of small intestine pinkish; other organs normal. In the discussion, Dr. Gay thought the absence of cerebral congestion was due to the circulation continuing in the left carotid.
90. Hofmann: Wien. med. Woch., 1880, xxx., pp. 477-480.—Man, a criminal, hung; after hanging ten minutes, the body was cut down. Examination half-hour after drop fell. He was resuscitated and partly regained consciousness, but died three days afterward of œdema of[773] lungs after repeated severe convulsions. He had tumors of the neck which probably interfered with the compression of the trachea. See also Allg. Wien. med. Zeit., 1880, xxv., p. 161, and Wien. med. Blät., 1880, i., pp. 423-430; translated in Ann. Mal. Oreill. and Larynx, Paris, 1880, vi., pp. 99-112.
91. Kinkhead: Lancet, and 701-703.—Cases of hanging. In one, the body of the third cervical vertebra was broken across and the two pieces separated; in another case dislocation of second and third cervical vertebræ.
92. Nelson: Southern Clinic, 1885, viii., pp. 198-202.—Two colored men hung; drop five feet. In one there was atlo-axoid dislocation.
93. Dercum: Phila. Med. Times, 1886-87, xvii., p. 368.—Description of the brain of a man executed by hanging.
94. Kirtikar: Trans. M. and P. Soc., Bombay, 1885, vi., pp. 104-107.—Man, age 25, and woman, age 35. Both hanged. Drop nine feet. Knot tied over cricoid cartilage, a little to left side. In falling, the knots slipped to below the ear. There was fracture of the body of third cervical vertebra and rupture of ligaments. The cord was ruptured in each; in the woman in two places—once at the third cervical, the other at the dorso-lumbar junction.
95. Lamb: Med. News, Philadelphia, 1882, xli., pp. 42-45.—Execution of Guiteau. Drop six feet; knot placed under left ear, but slipped to back of head. Yellowish furrow a few lines wide around the neck, directed downward and forward. Sterno-mastoid muscles torn transversely about midway of their length. Thyro-hyoid ligament ruptured; hyoid bone and thyroid cartilage widely separated. Large blood-vessels not injured. No fracture or dislocation of vertebræ.
96. Thomson and Allen: Catalog. Surg. Sec. Army Med. Mus.; specimens 298 to 302.—Execution of Wirtz. Rope one-half inch diameter; drop five feet; knot under left ear. Several slight shrugs of shoulders, after which body was quiet; let down in fifteen minutes. No involuntary evacuation. Face pale, placid. Eyes partly open; pupils dilated; slight injection of conjunctivæ. Mouth open; tongue not protruding. Just above thyroid cartilage extending on right side from median line in front to spinous process was a dirty brown deep furrow with congested walls; on left side a line of discoloration due to direct action of rope. Soft parts above and below the line much swollen, particularly on right side. Larynx and hyoid bone unnaturally mobile. Right trapezius muscle torn; sterno-mastoid divided transversely, leaving an interval of two inches. Slight ecchymoses between muscle and larynx. Ecchymoses on ligamentum nuchæ. Hyoid bone, both greater cornua fractured and dislocated from body; lesions more marked on right side. Several small ecchymoses in vicinity. Larynx not injured. Brain normal. No bloody or frothy mucus in[774] air-passages. Lungs not congested. One drachm of straw-colored serum in pericardium. Heart empty. Abdominal organs normal. Bladder somewhat distended with urine.
See also Tidy, “Med. Juris.,” Cases 1 to 4 and 60.
Accident.
97. Harvey: Indian Med. Gaz., 1876, xi., p. 3.—Boy, age 1½ years; was swinging by two ropes attached to two posts; the ropes became twisted around his neck. Necroscopy showed mark of very small rope in front of neck from ear to ear; mucous membrane of larynx dark; lungs much congested.
98. Hackel: Op. cit., p. 35.—Man, age 19, sitting on a load of wood, with the lines around his neck, fell and was hung by the lines.
99. Biggs and Jenkins: New York Med. Jour., 1890, lii., p. 30.—Case 16; child, 6 months old, sitting on a high chair, fell between the chair guard and seat and was asphyxiated by compression of neck.
See also Tidy (op. cit.), Cases 53 and 54.
SUFFOCATION.
The term suffocation is applied in a special sense to the act and condition of preventing access of air in other ways than by pressure on the neck, as by pressure on the chest, by obstruction at the mouth or nose, by obstruction in the air-passages or on them from neighboring organs, by irrespirable gases, etc.
This article will consider all of these except drowning and irrespirable gases, which are treated of elsewhere by other writers.
Smothering is generally understood to mean the act and effect of stopping the mouth and nose.
Causes.
External Causes.—Overlaying is a frequent cause of suffocation in infants, which in such cases have usually occupied the same bed with one or both parents. In some cases the parents have been drunk or otherwise unable to prevent the injury, and the infant may also be partly stupefied with the alcohol derived from its mother’s milk. Infants are also sometimes overlaid by domestic animals. Again, they have been suffocated by being pressed too closely to the mother’s breast, or[775] by covering with bedclothes, shawls, etc. Noble[883] attributes some cases of asphyxia in the new-born to anæmia of the brain from pressure on the skull by forceps, etc., and recommends as treatment for this condition hanging the child head downward, so that the blood may gravitate to the brain (Cases 12 and 30).
Infants are sometimes smothered for mercenary purposes.
Persons have been suffocated by the pressure of a crowd. Pressure on the chest combined with forcible closure of the mouth and nose was the method of Burke and Williams, in the notorious burking murders (Case 58). The close application of a hand, cloth, or plaster over nose and mouth is of itself sufficient to cause suffocation, especially in children and feeble persons. Pressure on the abdomen crowds up the diaphragm and interferes with breathing. It is very likely that no external mark will be found in cases of pressure on the chest and abdomen, but the lungs will be marbled and emphysematous.
Taking plaster casts of the face and neck without inserting tubes in the nostrils has caused death in some cases. Suffocation often follows the falling of walls, houses, banks of earth, piles of coal or corn or wheat. One may fall into and be imbedded in some mobile substance as coal, wheat, corn, quicksand, or nightsoil, and be suffocated. Infants have been destroyed[884] by burying them in manure, ashes, bran, etc. In these cases there is not only the entrance of the foreign body into the air-passages, but the pressure of the mass against the chest and abdomen.
Internal Causes.—The air-passages may be closed up by foreign bodies within them, or within adjoining organs, especially the œsophagus. A great variety of substances in one of these two ways has caused suffocation: mud, cotton, rags, corn, meat, beans, pepper, potato skins, the fang of a tooth, artificial teeth, buckles, shells, flint, buttons, screws, crusts of bread, bones, fruit, stones, heads of grass, coins, slate pencils, nuts, nut-shells, shot, penholders, worms, fish, etc. (see Cases 6 and 55). Taylor[885] states that there were eighty-one deaths in one year in England and Wales from food in the air-passages.
Should an inspiration occur in the act of vomiting, the[776] vomitus may pass into the air-passages; a similar accident may occur in a person who attempts to swallow and speak at the same time. Infants have been suffocated by inspiring vomited milk. Fitz[886] states that food may pass from the digestive tube to the air-passages after death.
A case of suffocation in an infant by retraction of the base of the tongue is recorded. It has been stated that negroes have committed suicide by doubling back the tongue into the throat, or, as it is called, swallowing the tongue.[887] In giving anæsthetics, the subject being supine, and the head and neck somewhat flexed, the tongue, epiglottis, and soft palate may fall backward and suffocation may follow. Howard[888] states that pulling the tongue forward under such circumstances may reopen the pharynx, but will not lift the epiglottis. The thorax should be raised and head and neck extended backward. He believes that in giving anæsthetics the head should be lower than the shoulders. In order to avoid vomiting no food should be taken for some hours before the anæsthetic.
Cases are recorded of artificial teeth having fallen from the mouth into the air-passages during anæsthesia and sleep, and in epileptic and puerperal convulsions. It would appear advisable that these teeth should be worn only while eating (Case 13).
Hemorrhage from the lungs, from rupture of an aneurism or from injury of the mouth or throat, may make its way into the air-passages and cause suffocation. So also the bursting of an abscess of the tonsils or other part near the air-passages (Case 7).
Œdema of the glottis from scalding or other irritation of the fauces or glottis, or from disease of the kidneys; tumors pressing on some portion of the air-passages; rapid, profuse bronchial secretion in infants; acute double pleuritic effusion; cheesy glands ulcerating into trachea; simultaneous œdema of both lungs—all of these may cause suffocation (Cases 18 and 49). [For cases of enlarged thymus gland, see Hofmann, op. cit., pp. 587, 588.]
Paralysis of the muscles of swallowing, from diphtheria or[777] other cause, predisposes to suffocation. Progressive asthenia in which the muscles are exhausted; injury of spinal cord or pneumogastrics; paralysis of muscles of respiration from the use of curare; the spasms of tetanus and strychnia poisoning; the entrance of air into the pleural cavities with collapse of the lungs—all tend to cause mechanical suffocation either by pressure or by paralysis (for deaths in epileptics, see Cases 1, 10, 11, 33, and 40).
It is not necessary that the air-passages should be absolutely closed to cause suffocation.
The cause of death is more likely to be pure asphyxia, because of the absence of the complicating pressure of the hand or ligature on the vessels and nerves of the neck, and of fracture of larynx or vertebræ.
Symptoms.—Foreign bodies[889] entering the trachea naturally fall toward the right bronchial tube instead of the left because of the size and position of the entrance of the right tube. If then but one tube is involved, the signs will usually be on the right side; whereas if the foreign body stop in the larynx or trachea, both sides will be affected. The latter condition is much more dangerous. The symptoms would be resonance over the lung with the respiratory murmur partly or wholly absent; less mobility; puerile breathing on the unaffected side. In either case there may at first be little disturbance, especially if the shape of the foreign body is such as not to greatly interfere with the access of air; otherwise there may be at once, and almost always will be after a time, more or less urgent dyspnœa. Diminution of the necessary oxygen may cause convulsions, apoplexy, and other brain symptoms. Acute emphysema of the portion of lung not obstructed may follow its forcible distention. The local effect of the foreign body is an irritation which causes spasm and cough. It may be carried upward by the expirations and downward again by each inspiration. Inflammation is likely to appear eventually and may involve the lung. If the obstruction is not complete there may follow periods of alternation of good and bad health, ending perhaps in recovery. The foreign body may be expelled after a greater or lesser interval. On the other hand death may result from secondary causes. In the absence of correct history[778] the symptoms may lead to a wrong diagnosis and inappropriate treatment; as where a patient whose symptoms resulted from the presence of a piece of bone in the larynx, was treated for syphilis. A foreign body may be coughed up from the lung into the trachea and fall backward into the opposite lung.
Partial closure of the larynx, most likely caused by a flat or irregular substance, rather than globular, may cause gradual asphyxia with symptoms of apoplexy, making the diagnosis difficult.
When a foreign body remains a long time in the larynx, spasmodic cough and croupy breathing usually ensue, expectoration tinged with blood, hoarseness, or complete aphonia, pain, dyspnœa, possibly crepitation and dulness over the lungs. The case may end suddenly in death from closure of the glottis, or the foreign body may pass into the trachea and set up a new train of symptoms, or it may be expelled.
The frequency with which foreign bodies in the pharynx or œsophagus obstruct respiration, and the facility with which they may usually be removed, suggest a careful examination. Otherwise the patient may be treated indefinitely for supposed obstruction in the air-passages. Foreign bodies in the œsophagus have perforated into the trachea, and even the lungs, heart, and aorta.
In complete suffocation death will occur in from two to five minutes (see remarks under Strangulation). Death may also occur instantaneously.
The experiments of the Committee on Suspended Animation[890] showed that when the trachea of a dog was exposed, incised, and a tube tied in, the average time covered by the respiratory efforts after stopping up the tube with a cork was four minutes five seconds; the heart-beat stopping at seven minutes eleven seconds on the average. After four minutes ten seconds it seemed to be impossible for the dog, unaided, to recover. Faure[891] made the following experiment upon a large dog: He fixed a cork in the trachea. At first the dog was quiet; it then extended its neck, parted its jaws, and made efforts as if to vomit; then tried to walk, but its gait was uncertain; fell down and rose up. Its eyes became dull, and finally it fell down on its side, and became convulsed; then after several seconds stretched itself out. The thoracic movements were at first tumultuous, then became rapidly[779] feeble; the heart beating very slowly. At the necroscopy the lungs filled the thorax, were full of thick dark blood and emphysematous. The blood was black and fluid in the left ventricle and arteries, and in the right cavities and veins resembled molasses. Liver darkly congested. There was no mucus in the trachea and no ecchymosis in the lungs. He also (p. 306) tried the experiment upon a large dog of fastening boards against its thorax and tightening them by means of cords. For some minutes it was quiet, but suddenly it became much agitated, stood upon its hind legs, threw itself against the wall, rolled on the ground, and uttered frightful cries; finally fell on its side. There was no movement of the thorax, but the muscles of the neck and belly were in full and rapid action, dry and sonorous râles were heard, and a large quantity of mucus appeared at the nose and mouth. The movements grew feebler, the respirations infrequent, and at the end of thirty-four minutes it was dead. The necroscopy showed the blood black and thick; heart relaxed; lungs red, a little emphysematous, containing but little blood, and on their surface were blackish points and small red spots.
The death of Desdemona (Shakespeare’s “Othello”) has been much criticised. The declaration that she was strangled (or suffocated) does not consist with the symptoms described (see Med. News, Philadelphia, May 1st, 1886, p. 489).
Treatment.
The obvious indication is to search for and remove the obstruction. The means and methods of treatment are fully treated of in surgical works, but may be briefly mentioned here.
Laryngoscopical examination may be necessary. A curved forceps is usually the best instrument for removing the foreign body. A tallow candle may serve to push it into the stomach if there is no bougie at hand. Suction may be used. Sneezing may be brought on by tickling the nostrils; coughing by tickling the glottis; vomiting by irritating the fauces, or by emetic; the body of the subject may be inverted and in this position the fauces may be tickled, or fingers may be passed back into the pharynx. Johnson[892] says that at the moment of inversion the patient should try to take a deep inspiration; this opens the glottis and facilitates the expulsion of the foreign body. The inspiratory current has no appreciable effect in retarding the movement of the foreign body in the direction of gravity.
Noble recommends inversion of the body in new-born infants[780] in which asphyxia may be supposed to be due to anæmia of the brain. Tracheotomy or laryngotomy may be necessary. It may be necessary to administer oxygen. Foreign bodies like beards of grass and fish-heads can be withdrawn only with difficulty because of their sharp projections. Intense suffering and dyspnœa in a robust subject may necessitate venesection. Generally speaking it is better to bring up the foreign body than to push it down into the stomach. Beveridge suggests to blow into the ear, to induce a reflex action and cause expulsion of the foreign body. Cold affusions, artificial respiration, galvanism, frictions of the limbs, artificial heat, stimulants by mouth and rectum, may one or all be needed.
Hamilton[893] says that it is useless to expect good results from electricity if five minutes have elapsed since life appeared to be extinct; Althaus,[894] that three hours after death the muscles will cease to respond to faradization; and Richardson,[895] that a low temperature prolongs the sensitiveness of the muscle.
With regard to insufflation, Le Bon[896] objects to it in asphyxia as being hurtful and not useful. Colin[897] tamponed the trachea of a horse; in four minutes fifty seconds it was apparently dead; the tampon was removed and insufflation practised for fifteen to twenty minutes without effect. He claims that artificial respiration is useless after the circulation ceases.
Fell[898] and O’Dwyer[899] recommend forced inspiration. McEwen[900] uses a tracheal tube by the mouth.
Dew[901] offers a new method of artificial respiration in asphyxia of the new-born; Lusk[902] considers the subject of life-saving in still-births; Forest,[903] artificial respiration in the same; Read[904] discusses Schultze’s method with approval; Duke[905] plunges the infant into hot water;[781] Richardson[906] recommends artificial circulation by injection of vessels, or electric excitation; Jennings[907] recommends the same; Richardson[908] also considers fully the subject of artificial respiration and electrical excitation; Woillez[909] has described and recommended what he calls a spirophore.
After the removal of a foreign body the irritation remaining may cause a sensation as if the body was still lodged.
Death may occur from hemorrhage after its removal.
Post-Mortem Appearances.
These are mainly those of asphyxia. There may also be evidences of external violence, homicidal or accidental, as of pressure on the chest. Persistent deformity, flattening of the nose and lips, and excoriation of these parts may result from forcible closure of mouth and nose.
The SKIN AND CONJUNCTIVA usually show patches of lividity and punctiform ecchymoses; especially lividity on the lips and limbs. The face may be pale or violet; it is often placid, especially if the suffocation is accidental. Tardieu[910] admits that infiltration of the conjunctiva and punctiform ecchymoses of the face, neck, and chest may also be found sometimes in women after severe labor, and in epileptics. He records the result of the examination of those who died from suffocation at the Pont de la Concorde, 1866. The face and upper parts of the trunk were generally light red to a deep violet or black color, with punctated blackish ecchymoses on the face, neck, and upper part of chest.
The EYES are usually congested. Mucus and sometimes bloody froth are found about the NOSE and MOUTH. The TONGUE may or may not protrude.
The BLOOD is usually dark and very fluid. Wounds after death may bleed. According to Tardieu[911] fluidity of the blood is most constant in compression of the chest and abdomen, as also its accumulation in the vessels and right side of heart. Its color varies from red to black.
The BRAIN and pia mater are generally congested. This is said to be invariable if the eyes are congested. Mackenzie in thirteen cases found the brain congested in all.
The HEART varies much in appearance and condition. The right side is often full of blood; occasionally empty. Sometimes subpericardial ecchymoses are found, usually along the coronary vessels. The blood in the heart may be partly coagulated if the agony has been prolonged and there has been a partial access of air, which is gradually diminished. Mackenzie[912] found the right cavities full and the left empty in nine out of thirteen cases. Johnson[913] as a result of experiment on animals claims that when access of air is prevented there is a rise in pressure in the arteries, the right side of the heart fills, the pulmonary capillaries become empty, and therefore the left side of the heart becomes empty. As a result of further experiments[914] he verified his former conclusion, and added that in the last stage of asphyxia there is increased pressure on the pulmonary artery and lessened pressure in the systemic vessels. He thinks[915] that when both sides of the heart contain blood, there is paralysis of vaso-motor nerves and the arteries.
The TRACHEA is usually bright red and often contains bloody froth. The LARYNX or trachea as well as PHARYNX or ŒSOPHAGUS may contain a foreign body. If the latter has been removed the resulting irritation may be seen. The LUNGS are sometimes congested, at others normal; color red or pale. Sometimes one lung only is affected. They may be emphysematous. Mackenzie found them congested in all of thirteen cases examined by him. The lungs of young persons may be found comparatively small, almost bloodless, and emphysematous. Tardieu, Albi, and others believed that the punctiform subpleural ecchymoses indicated suffocation, and were due to small hemorrhages from engorged vessels which ruptured in the efforts at expiration. These spots are usually round, dark, from the size of a pin-head to a small lentil, and well defined. They are not like the petechiæ in the lungs and heart after purpura, cholera, eruptive fevers, etc., nor like the hemorrhages under the scalp after tedious labor, all of which are variable in[783] size. These punctiform spots are usually seen at the root, base, and lower margin of the lungs. Hofmann states (“Lehrbuch”) that they are found in the posterior part of the lungs and in the fissures between the lobes. They are indisputably frequent after death from suffocation, and if well marked either in adults or infants that have breathed, they indicate suffocation, unless some other cause of death is clear. Simon, Ogston, and Tidy, however, have shown that they are sometimes absent in fatal suffocation, and are sometimes present in the absence of suffocation, as after hanging and drowning; in fœtuses before labor has begun; often in still-births, although some of these are probably due to suffocation from inhaling fluid or from pressure. Also in death from scarlet fever, heart disease, apoplexy, pneumonia, and pulmonary œdema. Grosclaude[916] quotes from Pinard, who declares that these ecchymoses are found in fœtuses which die from arrest of circulation. Grosclaude himself made a large number of experiments on animals by drowning, hanging, and strangling, and fracturing the skull. The ecchymoses were found in nearly all the cases.
The ecchymoses are partly the result of venous stasis, which overcomes the resistance of some capillaries; and the latter rupture, partly from the aspirating action of the thoracic wall, the lung being unable to fill itself with air, but mainly[917] from vaso-motor contraction and lateral pressure at the maximum of the asphyxia, the time of tetanic expiration. If the asphyxia is interrupted before this stage, the spots do not appear. Similar ecchymoses may be found under the scalp, in the tympanum, retina, nose, epiglottis, larynx, trachea, thymus, pericardium, in the parietal pleura, along the intercostal vessels, rarely the peritoneum, in the stomach, and sometimes the intestines; and in other parts of the body, especially the face, base of neck, and front of chest; in convulsive affections, as eclampsia and epilepsy, and in the convulsions of strychnia and prussic acid poisoning there may be suffusion and congestion of the lungs though not the punctated spots.
Mackenzie, in thirteen cases of suffocation from various causes, failed to find the Tardieu spots either externally or internally. Briand and Chaudé[918] state that they are less constant[784] and characteristic in those who have been buried in pulverulent substances.
Ogston[919] holds that in infants that are smothered the ecchymoses are found in greater number in the thymus gland; while in adults dying from other forms of asphyxia they were found only once in that gland. The spots are found in clusters in infants that are smothered, but only single and scattered in adults who die from drowning, hanging or disease. They were wanting in the lungs of but one infant.
They may be recognized as long as the lung tissue is unchanged. The apoplectic spots in the lungs seen in strangulation are not found in suffocation.
Tardieu[920] from experiments on animals and examination of twenty-three new-born infants who showed traces of violence around the mouth, found the lungs rather pale and anæmic, subpleural ecchymoses well marked. All the deaths were rapid. In cases of compression of chest and abdomen[921] the congestion of the lungs was extensive, and pulmonary apoplexy frequent; more so than in other forms of suffocation. He gave strychnia to animals which died in convulsions, and found very irregular and partial congestions, generally not marked because death was so prompt; blood always fluid; no subpleural ecchymoses.
The LIVER, SPLEEN, and KIDNEYS are generally congested; the kidney more than the other organs named. The spleen is said to be often anæmic. Semen has sometimes been found, unexpelled, in the urethra.
Page[922] experimented on three kittens, suffocating them in cinders. The post-mortem examinations showed the veins engorged, left side of heart empty, right side full of dark, half-clotted blood. Lungs distended, much congested, color violet; many small fluid hemorrhages in substance; no subpleural ecchymoses. Frothy mucus tinged with blood in trachea and bronchi; bronchi congested. Brain and abdominal organs normal.
Proof of Death by Suffocation.
It is sometimes difficult in a given case to state WHETHER DEATH IS DUE TO SUFFOCATION. There is no lesion which of itself could be accepted as proof. But a collation of the lesions[785] found taken in connection with the surroundings of the body will in many if not in most cases lead to a definite conclusion.
Infants have been found alive four and five hours after having been buried in the earth.[923] If the pulverulent material has penetrated into the œsophagus and stomach, the burial has occurred during life. Exceptionally when burial has occurred after death and traces of the material are found in the air-passages, they are not found in the œsophagus or stomach.
The committee on “Suffocation,” of the New York Med. Leg. Soc., reported[924] the following group of appearances as evidences of death by suffocation: The general venous character of the blood, the turgidity of the larger veins, the congestion of the parenchymatous organs, especially at the base of the brain, the lungs congested in a variable degree and œdematous, frothy mucus in the bronchi, the right side of the heart always fuller than the left. Fitz[925] holds that suffocation is a condition composed of a group of symptoms and appearances due most probably to accumulation of carbon dioxide in the blood and a deficiency of oxygen. The appearances are: The blood dark and fluid (though in gradual suffocation there may be clots in the right side of the heart), the right side of the heart full, venous congestion of the lungs (not constant), interstitial emphysema of the lungs, and venous congestion of the liver, kidneys, and brain. He prefers the word engorgement to congestion in this connection.
Tardieu[926] holds that when in infants buried in pulverulent substances we find emphysema of the lungs in high degree, bloody froth in the air-passages, abundant subpleural and subpericardial ecchymoses and the blood fluid, the burial has occurred during life. The same lesions are found in small animals similarly treated.
It must not be forgotten that an intoxicated person or one in an epileptic spasm is practically helpless, and can, therefore, be suffocated, accidentally or otherwise, under circumstances in which one in possession of his senses would be able to escape.
Accidental, Homicidal, and Suicidal Suffocation.
Accidental suffocation is frequent, as has already appeared. Suicidal suffocation is very rare. Homicidal suffocation occurs. Foreign bodies have been forced into the[786] air-passages. Smothering has been done by holding the face in various materials to prevent access of air; by pressure on the chest; by forcible closure of the mouth and nose as in burking; by laying compresses over the face, as in the case of King Benhadad,[927] whom Hazael killed. “And it came to pass on the morrow that he took a thick cloth and dipped it in water, and spread it over his face so that he died; and Hazael reigned in his stead.” Benhadad was already quite ill and not expected to live.
Death by suffocation[928] may be considered as presumptive of homicide unless the facts are already referable to accident.
In infants, suffocation is, of course, either accidental or homicidal; in adults usually accidental. The absence of signs of a struggle in adults suggests accident; unless there is cause of suspicion of previous stupefying with narcotics.
Taylor[929] calls attention to a dangerous practice among some attendants upon infants, of putting into the mouth of the child to quiet it a bag containing sugar; and instances a case in which the child would have died of suffocation but for the fortunate discovery of a part of the bag protruding from the mouth.
In ten years, 3,612 deaths were reported in the city of London, of infants smothered by being overlaid.[930]
Infants may be born into a mass of blood and fæces, from which the unattended mother in her weakness may be unable to remove them.
Page[931] shows by experiment that the inspiratory effort when violently exerted is sufficient to convey small objects into the air-passages. Cinders passed thus into the trachea and œsophagus of kittens and rabbits. Berenguier[932] experimented on new-born pups, placing them in ashes, plaster, and starch. In ashes they lived fifteen hours; these found their way into the middle of the œsophagus, but were stopped at the glottis. Plaster and starch formed a paste with the oral mucus and the movement of the mass was not so great as the ashes. In no case did either of the materials pass beyond the glottis. Tardieu[933] examined three infants which had been buried during life. One was in ashes: the nose was obstructed, mouth full: ashes also in the œsophagus[787] and stomach, but none in larynx or bronchi. The second infant was in manure; a greenish stuff was found in the mouth and stomach. The third in bran (confessed to by the mother); the nose and mouth were full, but there was none in the throat; a few grains in the trachea. Tardieu experimented on rabbits and Guinea pigs by burying them in bran, sand, and gravel, some of them being alive and the others dead. In those buried alive he found the substance filling the mouth and nose to the base of the tongue; in most of the cases the œsophagus and trachea were not penetrated. In the animals first killed and then buried, the substance had not passed into the mouth or nose. In one case only he found ashes in the larynx and trachea of a rabbit which had been buried many hours after death in a box of ashes. Matthyssen[934] held a Guinea pig, head downward, with its nose under mercury; the lungs were full of globules of mercury (which has a specific gravity of 13.5). A dog was plunged head first into liquid plaster-of-Paris; the plaster was found in the bronchial tubes.
ILLUSTRATIVE CASES.
Accidental.
1. Huppert: Vier. ger. Med. und öff. San., 1876, xxiv., pp. 237-252.—Two cases. A man choked by piece of bread in pharynx. Second, an epileptic, suffocated by flexion of chin on larynx. In both cases seminal fluid was found in urethra near meatus, unexpelled; determined by microscope.
2. Johnson: Lancet, 1878, ii., p. 501.—Boy swallowed penny, became black in face; eyeballs protruded; symptoms soon subsided. Some hours afterward it was found that he could not swallow solids, and liquids only with difficulty and coughing. Throat much irritated; discharge of mucus sometimes tinged with blood, from mouth; moist rattling noise in throat in respiration; frequent cough; could not sleep. Laryngoscope showed penny in upper part of œsophagus, just below laryngeal opening. Removed by long curved forceps.
3. Ibid.—Man suddenly fell while at dinner; face blue; breathing stertorous. Died. Piece of tendon found under epiglottis.
4. Ibid.—Boy, age 5 years. Button in larynx. Aphonia, dyspnœa, stridulous breathing. Distress gradually subsided. Many years afterward found mucous membrane of larynx thickened; vocal cords red and uneven.
5. Ibid.—Man, drunk, swallowed a half-sovereign. Urgent dyspnœa; pain in throat; aphonia; stridulous breathing; dysphagia; cough; copious mucous expectoration. Laryngoscopic examination showed coin in œsophagus. The crico-thyroid membrane was incised and coin pushed upward and ejected.
6. Med. Times and Gaz., 1874, i., p. 486.—Man, age 20, had severe dyspnœa. In taking a living fish in his teeth (it was about four inches long and had large dorsal fin), the fish passed into the pharynx and lay doubled up. Impossible to remove it because of spines. Tracheotomy at once. Twenty-four hours afterward the fish had decomposed enough to be partly removed. Patient died of exhaustion.
7. Littlejohn: Edin. Med. Jour., 1875, xx., p. 780.—Woman found dead in bed. Suffocated by pus from abscess of tonsil which burst during sleep. Found pus in air-passages down to smallest bronchi; lungs congested; right side of heart distended with dark fluid blood; left side contracted and nearly empty. Blood everywhere fluid. Some lividity of face. The woman had died quietly lying beside her husband, who was not awakened.
8. Sayre: New York Med. Jour., 1874, xix., p. 420.—Girl, age 7, swallowed a bead. Had continuous cough; much pain under middle of sternum. The bead moved upward and downward in respiration. Tracheotomy. Four days afterward she coughed the bead out, inspired once, and apparently died. Artificial respiration used; alcohol injected into rectum; galvanization of phrenic nerves. She finally coughed up a piece of thick mucus and recovered.
9. Duffy: Trans. Med. Soc. No. Car., 1874, p. 126.—Boy, age 8, swallowed a cow-pea. It lodged in the trachea. Some months afterward, laryngotomy performed. The boy seemed to die at once. Artificial respiration used. After a while he expelled first some mucus, then the pea. Recovered.
10. Tardieu: Op. cit., p. 290.—Man, age 50, found dead on the floor. At base of neck and front of chest were many punctated ecchymoses. Brain and lungs much congested; the latter showed subpleural spots. Tongue and lips bitten. Death was due to cerebral and pulmonary congestion from an epileptic seizure.
11. Oesterlen: Vier. f. ger. Med. und öff. San., 1876, xxiv., p. 10.—Woman, age 30, epileptic. Found dead. Examination showed signs of asphyxia; blood-vessels engorged, marked œdema of lungs, etc. Opinion given that she died in epileptic paroxysm, and certain injuries observed were caused by a fall.
12. Tardieu: Op. cit., p. 322.—Two children, one 2 months old, the other 18 months old; in bed together. The older overlay the younger, which died. Necroscopy: lungs voluminous, in places congested, in others pale; abundant subpleural ecchymoses; quite emphysematous. Fluid blood in heart.
13. Blum: New York Med. Jour., 1885, xlii., p. 207.—Woman, found dead. Vulcanite plate of usual size, with four teeth attached, found wedged in trachea about two inches below larynx.
14. Wyeth: Same journal, 1884, xl., p. 487.—Boy, age 12, inspired a pin-dart in trying to blow it through a blowgun. Violent cough,[789] gasping for breath, lividity of face for a few minutes; symptoms subsided leaving slight cough. The dart had lodged in right bronchus beyond first bifurcation, as shown by hissing, fluttering sound in both inspiration and expiration. Tracheotomy. The dart could not be reached. At a later date the dart was brought up into the mouth by a strong expiration.
15. Partridge: Same journal, 1890, li., p. 303.—Child, 4 months old, found dead; fluid, partly digested milk in air-passages.
16-41. Biggs and Jenkins: Same journal, 1890, lii., p. 30.—Report of many cases of fatal suffocation from foreign bodies, etc. Boy, age 15—collar-button in larynx. Boy, age 10—mass of butter in larynx. Boy, age 5—bronchial gland discharged into trachea at bifurcation. Boy, age 3—screw in larynx. Boy, age 5—rubber balloon with whistle attached; it was partly inflated with each expiration. Girl, age 10—a “jack” in larynx. Man, age 45—had been drinking freely; piece of meat in larynx. Man, age 40—piece of meat in larynx and pharynx. Man, age 40—ditto. Insane patient—piece of meat in trachea. Man—piece of meat in larynx. Man, age 40—crackers and cheese in larynx. Child—rubber nipple in larynx. During administration of ether, patient vomited; vomitus entered larynx. Two children in bed asleep; one, 3 years old, overlay the face of the younger, age 5 months. Woman, age 25, epileptic—fell on a child and smothered it. Two children found dead, covered with bedclothing. Man, age 21, epileptic—found lying on his face in bed. Girl, age 12, epileptic—ditto. Woman, age 21—ditto. Girl, age 18—ditto. Woman, age 35, epileptic—fell on the floor. Woman, age 28—ditto. Man, age 35, epileptic; vomited while in spasm; vomitus entered larynx. From Dr Janeway: Man, epileptic, fell on his face in pile of manure, which entered larynx. Man, drunk, lying on his face.
42. Roy. Indian Med. Gaz., 1880, xv., p. 71.—Man, believed to be drunk, had vomited in bed; vomitus entered trachea and bronchi.
43-47. Mackenzie: Same journal, 1890, xxv., p. 257.—Reports fatal cases: Boy—bone button in larynx. Sailor—meat in larynx. Boy—vomited matter in larynx. Infant—while taking the breast, a rush of milk suddenly filled the air-passages. Also three cases of crushing under walls; two buried in loose earth; two crushed in a crowd; one by bags of grain.
48. Feulard: Bull. Soc. Anat., 1883, viii., pp. 384-386.—Woman, age 79. Piece of beef in larynx. Necroscopy showed hematoma in dura mater.
49. Poupon: Bull. Soc. Clin., Paris (1882), 1883, vi., pp. 236-238.—Boy, age 5½ years. Death from cheesy gland in trachea.
50. Pons: Jour. Méd., Bordeaux, 1889-1890, xix., pp. 57-61.—Woman, age 24. Death from œdema of larynx from presence of particles of food.
51. Kemény: Wien. med. Blat., 1890, xiii., p. 37.—Man, age 45. Suffocated by curdled milk in air-passages.
52. Maschka: Vier. ger. Med., 1885, xliii., pp. 11-14.—Man, age 65. Accidental compression of chest.
53. Heidenhain: Same journal, 1886, xliv., pp. 96-101.—Vomited matter passed into air-passages while subject was drunk.
54. Langstein: Wien. med. Woch., 1880, xxx., pp. 624-626.—Child found dead in bed; had vomited food while asleep and breathed it into air-passages.
55. Ward: Catalog. Army Med. Mus., Med. Sec., p. 33.—Soldier, age 17; choked to death by lumbricoid worm passing from pharynx into right bronchus. Specimen 7,737.
Suicide.
56. Sankey: Brit. Med. Jour., 1883, i., p. 88.—Epileptic; found dead in bed, lying on his back. A round pebble in each nostril; strip of flannel rolled up and stuffed in throat.
57. Macleod: Ibid., 1882, ii., p. 1246.—Suicidal maniac. Had to be fed because he refused food. Was seen to be blue in the face and breathing hard. His mouth was forced open; roll of flannel found in throat. Macleod refers to another case, a woman in dissecting-room, with similar roll of flannel in throat.
See Tidy, “Med. Jur.,” Cases 15 to 17.
Homicide.
58. Christison: Edin. Med. Jour., 1829, xxxi., pp. 236-250.—The famous Burking case. A woman was struck down to a sitting posture. Burke then threw himself on her, kept her down by the weight of his body, covered her mouth and nose with one hand and placed his other hand under the chin for ten to fifteen minutes, till she died. Necroscopy showed a severing of the posterior ligamentous connections of the third and fourth cervical vertebræ, with blood in spinal canal but not under the dura mater; cord not injured. Christison made experiments to ascertain if the injury to spine had been made during life.
59. Hackel: Dorpat Diss., 1891, p. 35.—Case of choking with pressure on breast and belly. Woman found lying on floor, with many injuries.
60. Tardieu: Op. cit., p. 315.—New-born infant; found buried in earth. Mother stated that the child had not breathed. Putrefaction had begun. There was a brownish tint of skin of upper front part of neck below jaw; drops of sanious fluid flowing from nose; umbilical cord had not been tied; subcutaneous hemorrhage in right temporal region; brown bruised surface and contused wounds of pharynx, where[791] particles like ashes and vomited matter were found. Lungs filled the pleural cavities, were rose-colored and showed abundant punctated subpleural ecchymoses; bloody, frothy mucus in trachea and bronchi; some serum in pericardium; respiration had been complete. Opinion given, that the infant had been suffocated by obstruction of pharynx, probably by fingers.
61. Tardieu: Op. cit., p. 323.—New-born infant found under a cask, partly eaten by a dog. The head showed transverse flattening and subcutaneous hemorrhage. Lungs voluminous, rosy; abundant subpleural ecchymoses; hemorrhage in left lung. Heart filled with fluid blood. Coagulated blood in abdomen. Opinion given, suffocation by pressure on head, chest, and abdomen. The mother confessed that she had placed the child under the cask.
62. Ibid., p. 325.—New-born infant found buried in the earth; gravel and earth in pharynx and œsophagus down nearly to stomach, and in trachea and right bronchus. Lungs congested, crepitant. Opinion given, that the child had been buried while living.
63. Ibid., p. 326.—New-born infant found in ashes; nose and lips obstructed, mouth filled; ashes in œsophagus and stomach; none in larynx or trachea. Lungs distended with air, emphysematous; subpleural ecchymoses; fluid blood in heart.
64. Ibid., p. 327.—New-born infant, buried in bran; nose and mouth filled; some in trachea; none in œsophagus or stomach. Lungs distended with air, emphysematous; subpleural ecchymoses; heart empty.
65. Devergie and Raynaud: Ann. d’Hyg., 1852, xlviii., pp. 187-206.—Man found dead on a pile of grain; mouth, nose, and eyes contained some of the grain; some also in stomach, larynx, trachea, and bronchi. Some marks of injury on face and other parts of body. Internal signs of asphyxia. Opinion given, that the case was homicide. The defence offered was that the man had fallen into the grain.
66. Rauscher: Friedreich’s Blat., 1886, xxxvii., pp. 324-330.—Woman, age 71, suffocated by a cloth over nose and mouth.
See Tidy, “Med. Jur.,” Cases 1 to 11.
DEATH FROM SUBMERSION
IN ITS
MEDICO-LEGAL RELATIONS.
BY
IRVING C. ROSSE, A.M., M.D., F.R.G.S. (Eng.),
Professor of Nervous Diseases, Georgetown University; Membre du Congrès International
d’Anthropologie Criminelle, etc.
DEATH BY SUBMERSION OR DROWNING.
GENERAL CONSIDERATIONS.
The frequence and importance of drowning having arrested attention from the days of Noah’s Ark and those of Hippocrates down to the present time, it is quite possible to array in chronological order the fictitious, transitory, and positive periods that mark the sequence of ideas touching the subject.
Mooted questions relative to drowning have been debated since the fourteenth century; and modern statistics show the great development of this class of emergency, than which none is of more startling character. In France between four and five thousand cases of this kind of accident are officially recognized each year, which is about one-third of all the accidental deaths, and the number appears to increase yearly. Nearly the same figures apply to the inland waters of England and Wales, not including the coast. The Board of Trade Return shows that out of 86,695 seamen who died in English ships abroad, 53,673 were drowned, and a late report of the Fisherman’s Federation places the number drowned in the inland waters and upon the immediate coasts of the United Kingdom and its adjacent islands as 6,268 annually. The many hundreds drowned in the late Victoria disaster and in the great storm that swept the British Isles are matters of current knowledge. In our own country accounts of drowning are of daily occurrence, and help to the drowning forms the greater part of the work done by that noble governmental branch, the Life Saving Service. Not only does the sea claim its numerous victims, but the great floods and cyclones have destroyed thousands, while on the lakes and rivers drowning accidents are lamentably frequent. If the statistics of such accidents were as available as those of the late war, for instance, the exhibit would doubtless be surprising. Where the aggregation of killed in action is shown to be 67,058, there were drowned 106 officers and 4,838 men.[796] The small regular army lost 5 officers and 89 men from this cause; the negro troops, 6 officers and 289 men; and the volunteers furnished a large contingent, the State of Ohio alone having lost 14 officers and 770 men from drowning.[935]
Aside from the point of view of public hygiene and that of pathology, further evidence is not wanting to show the medico-legal value of the phenomena of drowning, and the frequency and importance of the judicial questions that may arise in this class of accidents.
DEFINITION AND PHENOMENA OF DROWNING.
Late studies as to the cause and mechanism of asphyxia by submersion or drowning warrant our speaking of submersion as immersion complete enough to menace or to extinguish life.
When an animated body or a part only of the body is immersed a sufficient time in water or any liquid medium whatever in such a way as to exclude fresh air from the respiratory orifices, suffocation follows, and death by submersion or drowning takes place.
The phenomena occurring in such instances are mostly those common to imperfect aeration or non-aeration of the blood, and for this reason the majority of medical writers describe asphyxia or apnœa, that is, death beginning at the lungs, as the determining cause of death by drowning. It must not be thought that asphyxia is always the mode of death in those submerged, although it is commonly present in a certain number of cases. Other causes may often modify the circumstances of the death or directly produce it, as congestion of the brain and syncope, or the cause of death may be a mixed one. Occasionally one reads accounts of persons resuscitated from drowning who, on recovering from the primary effects of the asphyxia, die suddenly without apparent cause after a lapse of a few minutes or several days. Such cases are explained as the secondary results of the arrested interstitial nutrition that took place during the period while breathing was temporarily arrested. Another secondary cause is physical injury to the lungs from water penetration, which may result in a fatal pneumonia. A case[797] related in England last summer is that of a drowning boy who, on being resuscitated after submersion in contaminated water, suddenly died of cholera.
MODE OF DEATH IN DROWNING.
Since various lesions may be found, accordingly as the death from drowning has taken place from one or more of the foregoing modes, it is necessary to have a clear notion of asphyxia and to study in detail the mechanism of arrest of the thoracic movements and of the hindrance to hæmatosis.
Broadly speaking, there will be asphyxia when any obstacle hinders air from entering the pulmonary vesicles, or when the fluid that penetrates them is of any other nature than the medium in which the animal is destined to live. Consequently the name asphyxia is applied generically to all accidental conditions in which life is threatened by any intervention whatever of the respiration. (See Mechanical Suffocation, Vol. I., p. 705 et seq., and Asphyxiating Gases, Vol. IV.)
Submersion in any liquid medium causes asphyxia. This condition may be caused on being surrounded by a medium devoid of oxygen and improper to support sufficient hæmatosis, as hydrogen, nitrogen, and the protoxide of nitrogen, gases not toxic properly speaking, but considered irrespirable. Diminished respiration from deficiency of oxygen is the true cause of asphyxia. No animal can maintain the respiratory process in an atmosphere devoid of oxygen or in one that does not contain at least ten per cent of this gas, and such quadrupeds as whales, hippopotami, and seals or the pygopodous birds would drown in the same manner as a dog if kept submerged long enough. The suppression of the gaseous exchange by submersion is also fatal to such aquatic insects as hydrophiles, dytiscidæ, and the like, which drown in the same manner as the hymenoptera, coleoptera, diptera, or other terrestrial insects. Ants drown in less than a minute when the body is wet, and the disappearance of apparent vitality is accompanied by convulsive movements indicating functional trouble of the nervous apparatus. Sir John Lubbock found that after eight hours of immersion they could be restored to life, and several ants after two days and five days were restored to momentary life with[798] feeble motions, followed by death in two hours. Even a terrestrial plant when submerged drowns like a terrestrial animal, the mechanism of asphyxia by submersion being the same in plants and aerian animals, and due to closure of the principal way of gaseous exchange.
Notwithstanding the interruption of the gaseous exchange necessary to support life, there is long persistence of vitality after submersion of some creatures in which an intra-molecular respiration or gaseous dialysis with aerated water takes place, as in ants who have not been wetted before submersion.
The resistance of new-born animals to this mode of asphyxiation is especially noted in the greater time required to drown a pup than an adult dog. One minute and a half usually suffices to drown a dog, while a new-born pup often requires as much as fifty minutes. This great difference is owing to the less active change of tissue and the smaller consumption of oxygen in the young animal. The more active the vital combustion and the greater the demand upon the general store of oxygen in the blood, the quicker the young animal perishes when the respiration is obstructed.
It is observed in a general way that all kinds of death caused by the privation of respirable air have between themselves the greatest resemblance. Whatever be the obstacle that intercepts the connection of the lungs with the atmosphere, the apparent differences are only secondary and the essential symptoms are identical, because all act in suppressing the functions of the blood and hæmatosis. In fact, the phenomena of asphyxia are constant and related to disturbances in the respiration, innervation, and circulation, which vary according as the asphyxia is the result of submersion or of the absence of oxygen in the surrounding medium, according as asphyxia is immediate or slow. The fatal result of asphyxia is owing to the introductory arrest of the pulmonary circulation, the capillaries of the lungs being incapable of conveying venous blood. The stagnation of the blood in the lungs is followed by paresis of the respiratory centre and stoppage of the heart.
STAGES AND SYMPTOMS OF DEATH BY DROWNING.
The authorities are that an individual who dies asphyxiated by submersion passes through three stages. At first he experiences[799] a violent shock, followed by an inspiration of surprise, which results from the contact of water with the lungs causing a reflex cough. Then for some seconds there is a voluntary suspension of respiration, giving rise to other forcible involuntary expirations. In this dyspnœic second period the face and brain become congested, owing to slowing of the encephalic circulation. Loss of consciousness soon follows, when the drowning person enters the third stage, which is that of asphyxia. In this period the individual gasps deeply, the pupils are dilated, the sphincters paralyzed, and the limbs are agitated by clonic convulsions. This is followed by complete insensibility and speedy death.
When a fatal termination in drowning results from that form of neuro-paralysis known as syncope, in which death begins at the heart, we infer from experiments that the sudden loss of consciousness arises from the violent impressions that the sensitive nerves convey to the bulb. Such a result is more likely to occur in persons with weak heart and languid circulation, who are more susceptible to fright and shock or to the sudden collapse from intense cold. It is also shown that stammerers, who have a defective innervation of the phrenic and of the pneumogastric, succumb more rapidly than others.
The importance of syncope as a cause of death in drowning is much restricted when we consider the fact that the circulation is the last of the functions extinguished in an animal that for purposes of experiment has been subjected to submersion. This has been shown in a sensuous way by experiment, aided by the resources of the graphic method, which registers the respiratory modifications as shown by the pneumograph and also the condition of the femoral artery in connection with a kymographion. The heart continues to beat as much as three minutes after the animal has succumbed, and recent autopsy gives almost constant proof of asphyxia. In fact, it is held that syncope takes but small part in this form of death, the general agreement of opinion being that nothing short of a syncope that would be fatal either in or out of the liquid medium can account for the entire absence of some of the signs of death from asphyxia.
Among the symptoms often present in drowning persons, many relate to nervous phenomena and the mental state, which[800] may vary with individual presence of mind and moral force. Persons who have escaped this kind of death have observed auditory and visual hallucinations, as flashes of light, the ringing of distant bells, and the like. Just before the outset of the asphyxiation a rather curious functioning of the brain known as hypermnesia[936] takes place, in which the revivescence of ideas, of objects, or of facts relates to anterior impressions long past that seem to have been forgotten. According to the narratives of many drowning persons who have escaped the last consequences of asphyxia, this condition was attended by general exaltation of the memory of such a nature that their whole previous conscious existence seemed, in an incredibly short period and with great clearness and precision, to pass before them in panoramic review. In Admiral Beaufort’s letter to Dr. Wollaston, the memory impressions are said to have occurred in retrograde succession. A medical man resuscitated from drowning reports that just before losing consciousness this particular cerebral activity, in his case, took on a most realizing sense of the situation and of the consequences to his family. This cerebral superexcitement is not, however, a constant thing, nor do all subjects experience the ineffable agony of drowning. Persons have been taken from the water apparently dead who, on regaining consciousness, declared that they experienced neither oppression nor suffering and had no recollection of what had passed. A very intelligent woman of my acquaintance, having such an experience a few years since at Newport, quotes herself as and really believes that she is an instance of a person once dead and afterward restored to life.
This peculiar vividness of mind has been observed in other kinds of death than drowning, notably in chronic insanity. A priest with extended experience at the Government Hospital for the Insane tells me that he has often noticed the vaticinatio morientium in the form of so-called lucid interval of the insane when called on to administer the last rites of the Church. The condition is explainable from the stoppage of the pulmonary artery and the stimulus caused by circulation of non-oxygenated blood in the brain.
The condition known as asynesia, or amnesia, sometimes[801] follows the return to consciousness in persons asphyxiated and apparently dead from drowning. Dr. F. A. Burrell reports the case of a boy of eighteen, submerged for six minutes and resuscitated after four and three-quarter hours, in whom the memory of everything that had occurred from half an hour previous to the accident up to return of consciousness had been entirely obliterated. When last heard from the lapse of memory still remained.[937]
The statement that death from submersion results from true asphyxia or from asphyxia in a more or less modified form rests on the authority of a large number of facts. Indeed, recent investigators make the proportion so much greater than formerly as to warrant the statement that asphyxia is the generic cause of death by drowning. Dr. S. Coull Mackenzie[938] reports 305 cases of drowning, in which 297, or 93.37 per cent, died from asphyxiation; 1, or .32 per cent, from syncope; 1, or .32 per cent, from apoplexy and asphyxia; and in 6, or 1.96 per cent, the mode of death could not be determined because of advanced putrefaction.
As the post-mortem signs of drowning are known to vary according to a number of circumstances, it is difficult to deal with the subject unless certain fundamental points be kept in mind. These relate more particularly to the external signs and to the different lesions that follow the mode of death, although they are not constant. Surgeon-Major E. G. Russell[939] illustrates how widely the post-mortem appearances may vary in cases of drowning, even when the outward circumstances of the period of death are identical and the bodies have been subjected to precisely similar conditions as regards duration of immersion, subsequent exposure to air, and times of necropsy. He relates that five persons were drowned while proceeding to a ship in the Hooghley River. Three died the same death; and at the same time the bodies were recovered together after the same period of immersion, and were examined together; thus from beginning to end they had been under exactly similar conditions, yet there were very marked differences in the state of preservation of the bodies and in the post-mortem appearances. After[802] five hours’ exposure in air at 88° F., one body, in which the tissues were extremely fatty, showed beginning decomposition; in the other two there were no signs. Decomposition in the scalp, face, and neck indicative of drowning had begun under water, although in ordinary cases it first invades the abdomen, genitals, breasts, etc. Rigor mortis present in one case was absent in the other. The penis was semi-erect in one case, flaccid in the other, retracted and shrunken in the third. Emission of semen and expulsion of fæces were also noted. Tongue not swollen or protruded in any case, and cutis anserina absent in all three, which may have been owing to the high temperature. Water was inspired into the lungs in two cases. The larynx, trachea, and bronchi had regular congestion and scarlet ecchymoses in one case characteristic of asphyxia, and there was muddy water in the stomach.
The first question likely to arise when a drowned body has been found is the one of identity. All the circumstances in which the body was observed before its removal to the place where it lies for examination should therefore be minutely detailed, and all lethal injuries and the like should be noted with care, since the smallest accessories often lead to identification. The locality in which a drowned body is found may be a fact of considerable importance that may help to complete the chain of evidence in which the matter of crime or of accident turns upon the question of identity. It must be remembered that bodies often drift many miles away from the spot where the drowning occurred, owing to tides or currents. Such a circumstance I noted a few years ago at Brownsville, Texas, where it was a common sight to see bloated cadavers going down the Rio Grande. Time and putrefactive changes are also elements that enter into the matter of recognizing the drowned cadaver. To resolve this question with desirable precision, the reader is referred to more detailed instruction in the chapter on Identity.
TREATMENT OF THE APPARENTLY DROWNED.
Help to the drowned does not properly come within the province of judiciary medicine, being rather a humane question that belongs to public hygiene. Systematic writers, however, treat the subject at considerable length, and the statistics of[803] institutions for helping the drowned give such marvellous results that it would manifestly not be out of place to cite briefly some of the means employed for restoring life to persons taken from the water asphyxiated and apparently dead.
The prime object in resuscitating the drowned is the introduction of air into the pulmonary vesicles, which is best accomplished by artificial respiration, and the employment of such means as excite the nervous system with a view to reanimate sensibility and develop the reflex movements that contribute to the re-establishment of the respiratory function.
The exigencies of drowning also call for special means to restore the animal heat and the circulation, as well as the precaution of removing mucus and fluids from the obstructed air-passages.
As the knowledge of securing patency of the air-passages by artificial respiration is generally diffused among medical students and is taught in some schools, it would be superfluous to repeat in detail the procedures of Hall, Sylvester, and others.
Laborde’s method of resuscitating those apparently dead has lately gained some notoriety. It consists in stimulating the respiratory reflex by regular rhythmical traction of the tongue, which should be vigorously pulled forward fifteen or eighteen times a minute, to correspond in frequency to the normal respiration.
Another method, alleged to have marvellous effects over the respiration, is that of anal dilatation. Its advocates claim that irritation of the anus is a much more effective measure in resuscitating the drowning or narcotized.[940]
Respiration may be further promoted by alternate dashes of hot and cold water on the face and chest, by smelling-salts, tickling the throat and nares with a feather, and by electrization of the diaphragm and inspiratory muscles. Protracted galvanism may, however, prove dangerous.
When signs of life appear, a warm tonic stimulating drink should be given. A hypodermic injection of caffeine is also recommended.
Whatever means are employed should be used on the spot in the open air and without a moment’s delay.
Restorative efforts may be kept up for two or three hours,[804] although in the majority of cases life is extinct in the human subject after two minutes’ submersion or even less, and the chance of restoration after five minutes’ complete submersion is doubtful. To be sure, trained tank performers remain under water longer than two minutes, and exceptional instances occur of recovery after twenty minutes’ submersion in individuals in a state of syncope or with catalepsy.
CADAVERIC SIGNS IN CASES OF DROWNING.
The signs alleged to be common to death by drowning and characteristic of it are difficult to deal with, for the reason that there are no sure signs of drowning and the lesions furnished by necropsy are of feeble importance. There is consequently a divergence of opinion on this subject.
External Signs.
Among the external diagnostic signs consistent with the supposition of death by drowning, the presence of froth at the mouth and nostrils is of first importance. Cadaveric rigidity, pallor, goose-skin, rosy or violet discolorations on various parts of the body, retraction of the penis and scrotum, fish-like expression of the eye, peculiar position of the tongue, maceration of the palmar and plantar epidermis, and convulsive contraction of the limbs, particularly of the hands, which may be clinched after the manner that marks death by asphyxia, are all signs which when united form strong presumption in favor of submersion.
These typical and classic signs may, however, be varied by many circumstances. Hence the dissidence of authors. Dr. F. W. Draper states that after inspecting 149 drowned bodies, he has never observed that important sign of death, the presence of substances grasped in the hands.[941] Sand or mud in the hollow of the nails and excoriations of the fingers are also regarded as probable, not certain, signs, since each of these might have occurred either before or after death. The peculiar clinched condition of the hand is not pathognomonic, though strongly suggestive of drowning, as it may appear in asphyxiation from other causes. I have lately noticed this among the[805] external appearances of the bodies taken from the Pompeiian excavations. The further index of drowning known as washer-woman’s or cholera hand, with non-adherent tendency of the epidermis, is an effect that may be produced upon the living after a prolonged bath, notably in the aged and habitually unclean. Nor is the position of the tongue a special and distinctive characteristic of drowning. Only a few months ago I observed its presence in some of the victims of mechanical suffocation in the Ford’s Theatre disaster in Washington.
The shrunken state of the genital organs is apparently of little positive value as a thanatological sign, since the negative and opposite state of erection has been often observed, and Dr. Ogston states that he met semi-erection in twenty-two cases.
The value of “goose-flesh” as a link in the chain of evidence is also weakened when we consider that it frequently occurs after other violent modes of death. Anserine skin is often met with during life, and cases of drowning are recorded where this appearance has been absent.
The aspect of the face and the general position of a drowned cadaver may likewise vary according to the mode of death. Immobility of the body in the attitude of agony, the horrible grimaces of asphyxia, the pale, calm features of syncope, and putrefactive changes are further circumstances of medico-legal detail that may complicate the problem and render an autopsy necessary in order to invalidate or confirm the uncertain conclusions furnished by the external signs.
Internal Lesions.
Autopsies on the drowned are remarkable owing to their negative signs. But as an extension of diagnostic means, the autopsy may show the vertical (though not invariable) position of the epiglottis; the presence of water and foreign matter in the bronchi; swelling and emphysema of the lungs; hydræmic engorgement of the liver; fulness of the right heart and emptiness of the left; fluidity of the blood; water in the stomach and middle ear; and a characteristic frothy mucus or lather more or less bloody, which most observers and writers consider the only constant post-mortem appearance of drowning.
Examination of the respiratory apparatus is of extreme importance[806] in a question of this kind, for it is contended that the presence of foreign bodies is a proof of submersion.[942]
This opinion is in part erroneous, since it has been observed that when a body is submerged after death water will penetrate the larynx, trachea, and remote bronchi, as well as the stomach and middle ear. Moreover, Dr. Ogston states that in 48.7 per cent of cases of drowning no water was found in the lungs.
The emphysematous condition of the lungs, which are said to force their way out of the chest on removing the sternum, is difficult to distinguish from the result of putrefaction. Dr. Gilberti shows that in the drowned the lungs disintegrate rapidly, while the heart, in which putrefaction begins chronologically, is relatively in a good state of preservation.[943]
Since many cases have been observed in which both sides of the heart may be partly filled or both be empty and flaccid, or the left side distended more than the right, we are obliged to regard the exceptions concerning this post-mortem sign of drowning as co-extensive with the rule.
Excessive fluidity of the blood depends upon the rapidity with which the drowning took place. Slight hydræmia occurs in rapid submersion, but when the drowning has taken place slowly a large amount of water passes into the blood. In certain poisonings by opium this fluidity also exists; but it is claimed that analysis and the spectroscope may clear up the diagnosis.
Hydræmic engorgement of the liver is regarded as a characteristic fact by Lacassagne, who claims to be able to diagnosticate drowning from a single examination of this organ.[944]
It is now generally admitted that the presence in the stomach of a certain quantity of liquid in which the body was found immersed may be considered as a sign almost certain of asphyxia by submersion.
Dr. Fagerlund concludes from his experiments that liquids do not penetrate after death either the stomach or anus unless strong pressure be made. But when asphyxia occurs in water the liquid is found in the stomach and the intestines, where it[807] is helped on by peristaltic movements. The pylorus is an obstacle to the passage of this water, the movement of which is easier when the stomach is empty and the submersion prolonged.[945]
The quantity and quality of the water may constitute important evidence; but to be of full value the water or other fluid found in the stomach ought to be the same as that in which the immersion has taken place.
The liquid, which may have been taken just before drowning, should not be noticed unless it exceeds half a pint; but anything peculiar in the fluids, either of the lungs or stomach, should be subjected to microscopic or other examination.
Presence of water in the middle ear is regarded as a thanatological sign of great value. Dr. Bourgier claims as the result of his examination that 23 cases out of 27 had water in the middle ear. Several German observers pretend to have found amniotic liquid in cases of fœtal asphyxia. The fluid may be aspired by a small pipette.
Many of the foregoing signs and lesions disappear or undergo variable alterations after sojourn in water, putrefaction, etc. They may, as they have done in the past, give rise to many controversies, so that presumptions only can be established. Hence the necessity for careful and detailed necropsy in such cases, with a view not only to minimize conjecture and uncertainty, but to prevent opposing counsel from entering the plea of negligence and incompleteness.
WAS THE DROWNING ACCIDENTAL, SUICIDAL, OR CRIMINAL?
Assuming the probabilities to be in favor of death by submersion, the question next turns upon the character of the event.
In the absence of lesions it is almost impossible to say whether the individual fell in, jumped in, or was pushed in the submerging fluid. The person’s antecedents should be inquired into—whether subject to epilepsy, vertigo, intemperance, or mental aberration. Alcoholism is an important factor in accidental[808] drowning, and a person intoxicated may be drowned in very shallow water. A few years ago a young man over six feet tall, while bathing in a tributary of the Potomac River, near Washington, was drowned in only three feet of water. On considering all these circumstances, it may not be possible, even after careful inspection of the body and minute exploration of all the organs, to declare the drowning the consequence of an accident. The existence of traces of violence or of injury which may have occasioned death or disability, of such a nature as to render the person unable to defend himself, would seem to merit particular attention. But their presence leads to further consideration—were the marks of injury caused by the water itself, by some object in the water, or were they self-inflicted? Dislocations, fractures, and other injuries have been caused by jumping or falling into the water from a great height. I know an instance of a professional who, on jumping from a height of ninety feet, split his upper lip on striking the water with his mouth open. The autopsy in the case of Odlum, the Brooklyn Bridge jumper, is said to have shown rupture of the liver. On the other hand, many persons jump from great heights into water with perfect impunity. For many weeks at the London Aquarium a performer has nightly jumped into a tank from an elevation of 127 feet, and several persons have successfully jumped from bridges much higher.
Objects in the water that may account for cadaveric lesions are numerous. I have known a soldier, a good swimmer, to break his neck on diving from a river bank.[946] Other traumatic lesions may occur in a rapid current, from the breaking up of ice, from the screw or paddle-wheel of a passing steamer, or from aquatic animals.
A matter much discussed in connection with this subject—that of shark-bites—may enter into the question of survivorship where it is alleged that several persons during shipwreck or other disasters at sea have been devoured by sharks. Though an occasional accident, such bites are more a figment of the mind than a reality, as the concurrent testimony of disinterested observers will show. After years of investigation among nautical people and much experience as a swimmer in widely[809] different parts of the world, I have no personal knowledge of such injuries, and have met but two persons that had any actual personal knowledge of shark-bites.
Documentary evidence as to shark-bites is also very scanty. During the last fifty years soldiers by the tens of thousands have swum at Fort Monroe, Virginia, yet there is no record of one having been bitten by a shark; nor have I been able to ascertain that any accident of the kind has occurred at Malta or at Gibraltar. There does not appear to be a record of any one ever having been bitten off the British Isles. I have been unable to ascertain that a single bite of the kind is reported among the medical records of our War or Navy Department or those of the Marine Hospital. In the West Indies but few facts are reported indicating danger from sharks, and these are not well authenticated. The same may be said as to newspaper accounts, which deserve about as much credence as the reports concerning sea-serpents. A few years ago a public journal gave an account of a boy who was bitten while swimming near New York and afterward died in a hospital.
But medical literature has a few reports of shark-bites. After ten years’ diligent search I have found seven references, the earliest in the London Medical Gazette, 1823, and the latest in the London Lancet, 1886. The bites occurred in Australia, South Africa, and India. The Hooghley and Ganges Rivers are the worst place in the world for sharks and alligators. A particular kind of shark, the Carcharras Gangeticus, which is very fierce and bold, sometimes dashes among the crowds at the bathing ghâts, and has been known to bite a boy in two feet of water. All persons bitten at these places generally die from the bite, for the reason that the shark, living on carrion, portions of which stick between the teeth, carries infection to those whom it may afterward bite. The former habit of throwing the dead in the river is supposed to account for the boldness of these particular sharks in attacking the human species.
Self-inflicted wounds rather suggest suicide, as numerous instances attest, where one or two kinds of death were intended to make assurance doubly sure. I once saw an Eskimo stab himself and then jump overboard from a ship off the Siberian coast. But as a rule suicidal drowning is unaccompanied by[810] traumatic lesions, unless it be those produced by falls. Hence the absence of lesions leads to the presumption that the individual while living fell into the water or other fluid accidentally or voluntarily.
Exception may be made in the case of infanticide and homicidal submersion as the result of surprise, where a person taken unawares is suddenly and unexpectedly pushed or thrown into the water. A case in point is that of a man suddenly robbed and seized by three persons, who threw him into the river. Another is that of a man who, wishing to get rid of his wife, gave her arsenic. The effects of the poison being slow he induced her to take a walk along the river, and when her back was turned he pushed her rapidly off the bank into the stream, where she drowned. Death by submersion is rarely the result of murderous intent, and in the case of adults it is suddenly resorted to in order to paralyze resistance and facilitate the success of crime.
Submersion is oftener intended to hide a crime. A body may be taken from the water after murder or rape. Whether the cadaver is recent or one that has lain in the water a long time, the expert is confronted with a question of the differences that he may expect to find in a body drowned and one thrown into the water after death. This difficulty can only be resolved by considering all the signs and lesions furnished by the autopsy. No single sign or post-mortem appearance is characteristic of drowning, and none enables us surely to diagnosticate death by submersion either in putrid or fresh cadavers. Nor do we have any significant infallible signs that may serve as a parallel between the immerged post mortem and the submerged. The exterior signs being nearly the same in the two, the diagnosis must necessarily depend upon assembled circumstances, and these are liable to vary.
CIRCUMSTANCES THAT MAY AFFECT THE TIME OF SUBMERSION.
Putrid decomposition is the chief obstacle to diagnosis in a body that has been drowned. This presents great differences. The death happening in winter or summer, in a temperate or intertropical country, and sojourn of the cadaver in salt or fresh[811] water, are each and all important details to be considered in studying the submergence of a body.[947]
It is only by studying the events in this order, along with the immediate signs of death, that the duration of the submergence may be conjectured. With anatomical appearances as the only guide it is impossible to fix the time of immersion. Many elements combined may affect even the gaseous putrefaction that takes place in submerged bodies. Summer heat and shallow or stagnant water hasten the development of putrid gas and subcutaneous emphysema which bring the cadaver to the surface, and that, too, sometimes in spite of precautions taken to insure the submersion. A case in point is the body of the Italian admiral, Caraccioli, mentioned in Southey’s “Life of Nelson.” Bodies weighted with lead or other heavy substance for the purpose of hiding crime have also been known to float in consequence of the putrefactive phenomena.
At Evansville, Ind., unsuccessful efforts were made to raise a sunken steamer with thirty head of cattle between decks. A few days after the attempt was abandoned the steamer was suddenly seen to float. The carcasses of the putrefying animals, swollen by gas, had sufficed to bring the wreck to the surface.
A great development of gas is very noticeable in what is known as a “blasted” whale, the stomach of which assumes balloon-like proportions. A few summers ago, at Provincetown, Mass., it was my rare fortune to be within a few feet of an enormously distended putrid whale, which suddenly exploded.
In cold countries drowned bodies are longer in coming to the surface. In Russia, for instance, in spring after the rivers and lakes have thawed, the bodies of numerous victims of alcoholism and accidental drowning of the previous winter are taken from the water. Last summer, at Quebec, I was present when the body of a man drowned the winter before came to the surface of the St. Lawrence River. On a visit to the northern lakes many persons connected with the navigation of Lake Superior told me that bodies drowned in its waters seldom or never came to the surface.
Specific gravity of the water itself may be an additional[812] cause for the body coming to the surface. Dr. Tidy says that every structure of the human body floats in the water of the Dead Sea. The same cannot be said about the buoyancy of the water of Great Salt Lake, the accounts of which have been greatly exaggerated. It does not “support a bather as if he were sitting in an arm-chair and float him like a fresh egg.” Experience shows that there is no difficulty either in swimming or in sinking in its waters, the solid constituents of which are estimated to be about six and a half times more than that of sea-water. Analysis of Dead Sea water places the solid constituents at 24.580, while that of Salt Lake is 22.282. Another strong natural brine in the United States is said to be that of Syracuse Saline, New York, which contains 17.35 per cent of sodium chloride.
It is evident from what has been stated that no positive assertion can be made as to how soon a drowned body will rise to the surface, and at best any conclusion as to the date of submersion is so unsatisfactory that it may be said to be an unscrupulous use of guessing privileges. Errors in legal medicine are sadder in their consequences than those of medical diagnosis. The medical legist would therefore do well to preserve the frame of mind that often doubts and rarely affirms, and he should be circumspect enough to avoid dogmatic assertions about matters of uncertainty.
DEATH FROM STARVATION.
IN ITS MEDICO-LEGAL ASPECT.
BY
ENOCH V. STODDARD, A.M., M.D.,
Emeritus Professor of Materia Medica and Hygiene in the University of Buffalo;
Member of the Medical Society of the State of New York and of the Central
New York Medical Association; Fellow of the New York Academy
of Medicine and of the American Academy of Medicine;
Late Surgeon 65th Regt. N. Y. Vols.; Late
Health Commissioner, Rochester,
N. Y.; etc., etc.
STARVATION.
GENERAL CONSIDERATIONS.
Physiology teaches that life can only be maintained in the living organism by a constant equilibrium between its waste and repair. Nutrition is a term by which we describe this double movement of renewal of the molecular structure of the body, and in this general sense only, that nutrition is synonymous with the maintenance of the organism in a stable condition, is it employed here.
This condition of equilibrium is maintained by a regular and constant supply of food.
A food may be defined to be a substance which, after introduction into the body, supplies material for the renewal of its tissues or sustains some of its vital processes. Foods vary greatly in their properties as restorative or constructive agencies, some containing but few essential properties, while others combine almost all of the elements required. As some foods contribute elements for tissue restoration, others are specially concerned in the calorifacient activities of the organism,[948] while others are marked in their tendency to take part, almost exclusively, in special chemical processes.[949]
The various articles used as foods contain nutritive elements combined with innutritious substances. They have been variously classified, but are conveniently divided into
| I. Organic foods, | { | a. Nitrogenous (C.H.O.N.). |
| b. Non-nitrogenous (C.H.O.), | { | Oleaginous Carbohydrates. |
| II. Inorganic foods, | { | a. Water, H2O. b. Saline substances. |
Nitrogen enters largely into the composition of the body, and hence must be abundantly supplied and in combination.
Of the non-nitrogenous elements the most important are fat, sugar, and starch.
The inorganic principles are essential to the process of nutrition. Water, constituting 87 per cent of the bulk of the body, is demanded in constant supply; while the saline substances are necessary for the perfect performance of many of its chemical processes.
It is apparent that no single element can alone carry on the nutrition of the body, and hence variety in the supply of food, as well as sufficiency in its quantity, is essential to normal nutrition. Nor are these the only factors in this complex problem. Proper preparation of food, its supply at necessary temperatures,[950] and other requirements enter into the question of normal or sufficient alimentation.[951]
Alimentation is sufficient when it is so regulated that all the functions of the body are performed in a complete and regular manner. Insufficient alimentation induces a series of phenomena and a result which have been designated “inanition,” or “starvation.”
The exact amount of aliment required by each individual can only be stated in a general way. In the circumstances in which he is placed, the supply must be of such character and quantity as shall be proportionate to the constructive and reparative needs of his body. It is possible, however, to state a mean for the various ages and occupations of life.
Physiologists generally agree that in ordinary conditions of exercise the following represents the amounts of the several food elements necessary for the adult individual daily:
| Albuminous substances | 120 | gms. | = | 4 | oz. |
| Fatty substances | 60 | ” | = | 2 | ” |
| Carbohydrates | 360 | ” | = | 12 | ” |
Taking the fatty matters as the unit, the daily allowance would bear the following proportions:
Fats, 1; albuminoids, 2; carbohydrates, 6.
These quantities and especially the fats and carbohydrates, in conditions of hard muscular labor, must be increased; and the proportion would then stand:
Fats, 1; albuminoids, 1.7; carbohydrates, 7.
The division of this amount of food elements into proper portions during twenty-four hours is important. This must be regulated by the habits and other circumstances of the individual.[952]
The occurrence of death solely from privation of food is comparatively rare; yet it is sufficiently frequent to be considered as one of the causes of violent death and to demand investigation, since circumstances may be such as to constitute a homicide from criminal neglect or a suicide from intentional abstinence from food.
“Starvation,” or “inanition,” may be considered as being acute or chronic according as the requisite food has been suddenly and completely or gradually withheld.
ACUTE STARVATION.
The complete deprivation of food induces a series of modifications of the functions of the body, differing somewhat from those developed by a partial and prolonged deprivation. The length of time during which complete absence of food can be endured varies with circumstances. In absolute stoppage of the food supply the acute sensations of hunger pass away after the first one or two days, and are succeeded by profound functional disturbances with weakness and depressing sensations over the epigastric region, accompanied by distressing thirst.[953] The mouth is dry and the tongue heavily coated; the breath is fetid; the skin is harsh, dry, and exhales a disagreeable odor; the feces become more and more scanty until the latter days of life, when diarrhœa usually supervenes; the face and extremities become rapidly emaciated; the person walks with a weak and tottering gait;[954] the urine is small in quantity and very acid; muscular feebleness gradually reaches complete inability to move; ringing in the ears, insomnia and, in some cases,[818] hallucinations[955] with delirium and convulsions precede death, though these latter symptoms are not uniformly observed.[956]
“CHRONIC STARVATION,” “CHRONIC INANITION.”
This form of starvation, met with most extensively during the prevalence of famine, also occurs in conditions demanding legal investigation.
The symptoms are sufficiently constant and characteristic. Emaciation becomes extreme, the skin dry and rough, exhaling a disagreeable odor and often covered with a coating not entirely attributable to filth; the breath is fetid and offensive. With some exceptions, the victim retains his consciousness and ability to move about, muscular efforts becoming more and more feeble; the voice becomes faint; the evacuations infrequent, dry and dark; the urine scanty and high-colored, death occurring suddenly at the end, with delirium in some cases.
The length of time during which these symptoms are developed and their intensity depend mainly upon the amount and character of the aliment actually supplied during the period before death.
Upon the PULSE and CIRCULATION the effects of starvation are manifest in increased frequency and feebleness of the cardiac contractions and lessened force of the cardiac impulse; this is more and more marked as the anæmic condition becomes profound. In some cases the pulse is greatly reduced in frequency, as well as in force, dropping as low as thirty-seven beats in the minute,[957] and auscultation reveals the existence of cardiac bruits.
In connection with enfeeblement of the circulation, a tendency to hemorrhagic conditions is common, with purpuric and petechial eruptions in some cases.
Temperature.—A subnormal temperature is frequently noted in the progress of chronic wasting disease. In inanition, which in some respects induces a similarly profound disturbance of the functions of nutrition, an analogous lowering of the[819] body temperature occurs. Chossat clearly shows in his experiments the influence of starvation in depressing the body temperature. This abasement of temperature does not remain constant, but daily oscillations appear, differing from those occurring in conditions of normal alimentation.
While the normal diurnal variation in the fully nourished is about 0.3° to 1.0° C. (0.5° to 1.7° F.), in the starving this variation reaches 3.28° C. (5.4° F.). This rises to nearly double this amount during the latter days of life, and is greatly increased above this figure during the day preceding death. The temperature at the close falls to a mean of 24.9° C. (76° F.), and at the moment of death has been noted at 18.5° C. (66° F.).
Emaciation.—Loss of weight is the most striking and constant symptom of starvation. The rapidity of its production and its extent are modified by circumstances. A very considerable loss of weight can be sustained by the ordinary individual without a fatal result.
Chossat[958] fully demonstrated the effects of inanition upon the various functions and organs of the body in animals, and has drawn the conclusion that a loss of weight exceeding four-tenths of the entire weight of the body is productive of a fatal result. These deductions may be adopted as applicable to the human species. This statement must be accepted as a mean, as it is capable of variation by circumstances, such as age, obesity, etc.
Death may occur before so great a loss has been reached in some cases, and in the obese the fat may disappear entirely and cause a loss reaching five per cent of the entire weight of the body, in a very fat animal, without a fatal result.
Bouchardat[959] considers that the important question is the extent to which the blood and organs of the body contribute to this loss of weight. Impoverishment of the blood by inanition, which at the time of death has been found to amount to six-tenths of its solid constituents, is one of the most vitally serious elements of this loss; and a relative increase of its watery portion appears, without regard to the employment of water as a beverage.
It must be remembered that in wasting diseases extreme emaciation may occur under a liberal diet, and may continue for a considerable time before death.[960]
The muscular system becomes greatly enfeebled, atrophied, and unable to perform its functions; the loss sustained by the muscles least used being most marked. The extent of muscular power possible in starvation varies in different individuals and in various circumstances.
The vigorous and healthy adult, as a rule, retains muscular power to a greater extent and for a longer period than the child or aged person, under similar circumstances.
Exposure to a rigorous climate, prolonged fatigue, etc., rapidly reduce capacity for muscular effort in conditions of inanition.
The Period at which Death Occurs.
This is influenced by many circumstances. It is difficult to fix an exact period for the duration of life in complete deprivation of food, or acute starvation, and it is certainly more so in chronic inanition, when the modifying circumstances are increased in number and complexity.
A large number of cases of prolongation of life during a period of absolute deprivation of food which has been stated to extend over weeks and even months, cannot be accepted as free from error, and hence are not considered here.
A sufficient number, accurately observed and well attested by unimpeachable authorities, have led to the conclusion that the healthy adult, in a total deprivation of food, can exist for a period not exceeding ten to twelve days. On one of the Inman line of steamers, a young man, aged twenty years, endured absolute deprivation of all food and water during eleven days, recovery following.[961]
Sarah Jacobs, a child of thirteen years (“the Welsh fasting girl”), had been exhibited by her parents as a miraculous being under the pretence that she had eaten nothing during two years.
The child being placed under complete surveillance by four[821] nurses from Guy’s Hospital for eight days, during which period no food was taken, died on the ninth day.
The post-mortem examination showed all organs of the body to be in a healthy condition. The stomach was empty, with the exception of three teaspoonfuls of a thin acid fluid. The intestines were also empty and their walls were not thinned. A layer of fat, half an inch or more in thickness, was found under the skin of the chest and abdomen. The liver was in a healthy condition, as also the kidneys and spleen. The bladder was empty.
The parents were tried on a charge of manslaughter and were convicted of causing death by criminal negligence.[962]
Caspar gives the details of a case observed by him of a man aged thirty-six years, who endured total abstinence from all food for eleven days, recovery following.[963]
Cases are reported of miners who have been imprisoned by accidents in mines for eight, nine, and nine and one-half days, with recovery following rescue at the end of this time.[964]
While the period stated may serve as a maximum limit to which life may be extended in acute starvation, there are circumstances which must be considered as modifying this.
Body Condition.—It need hardly be stated that the individual in perfect health can sustain complete inanition longer than the enfeebled or diseased. The presence or absence of fat modifies considerably the power of endurance.
Age.—Infants bear starvation badly and succumb more quickly than the adult. The aged, while they bear a moderate amount of food better than the young adult, do not endure a complete deprivation for so long a time.
Cold.—The depressing influence of cold upon the vital functions, especially in the young and feeble, renders it a powerful factor in shortening the duration of life in starvation.
The Supply of Water.—When all food is withheld, free use of water as a drink tends to increase the length of the interval before death. In several cases of protracted fasting, the use of water in moderate amount has been resorted to with[822] the apparent result of amelioration of some of the distressing symptoms and lengthening the period of endurance.
Dr. Tanner, a physician, attempted in July and August, 1880, at New York, a complete fast of forty days’ duration, with the exception of the free use of water. In this case absolute abstinence from all nourishment is questioned, as no strict medical surveillance was maintained.
The Italian Succi, at New York, in 1890, undertook a voluntary abstinence from food for forty days, under surveillance, with the use of simple liquids and of some narcotic substance. He completed the fast, but beyond this fact the case is without scientific value.
Catalepsy.—Certain abnormal conditions of the nervous system are met where the activity of the vital functions is very considerably lowered and the various processes of the economy are in a condition of semi-suspension. Cases of this character have been observed where the supply of food has been almost entirely suspended for a period of several days, with but little emaciation and other symptoms characteristic of inanition.
WAS STARVATION ACCOMPANIED BY OTHER ILL TREATMENT?
This question may arise where evidences of starvation are apparent.
Such cases are met among young children neglected or abused by parents or those in whose care they may have been placed, or among the alienated or sick in the care of cruel or unsympathetic attendants.
Infants placed with “wet-nurses” or found in the so-called “baby farms” also furnish cases which fall under this head.
A careful examination into the collateral circumstances of the case, together with the results of a careful post-mortem examination, usually render a positive answer to this question possible.
POST-MORTEM EXAMINATION.
The dead body exhibits appearances quite characteristic.
Emaciation is very marked and sometimes reaches an extraordinary degree, surpassing that of prolonged and wasting diseases.
In extreme cases the fat entirely disappears throughout the body; the omentum and mesentery are entirely devoid of it, as well as the subcutaneous and intermuscular cellular tissue. The muscles are atrophied and the heart is sometimes considerably reduced in size; the liver and kidneys in some cases show great reduction of volume. The spleen also is small and often softened.
The stomach and intestines usually display an extensive thinning of their walls, so much so that their contents may be distinguished through them; their calibre also is frequently found to be diminished, though occasionally they may be distended with gas. Usually they are empty, or contain only a small quantity of bile and fecal matter. In some cases various foreign substances which have been swallowed by the victims to appease hunger have been found in them.
The thinning of the walls, so constantly noted, has been considered as a specially characteristic symptom of starvation.[965]
The congestion, softening, and ulcerations which have been observed in some cases cannot be considered as evidences of starvation or as its results, but rather as being due to an enteritis induced by the ingestion of improper substances.
The gall bladder is usually found filled with dark and inspissated bile. In death by starvation the entire organs of the body exhibit no specific form of disease. Evidences of the existence of an organic affection observed in the post-mortem examination at once raise the question:
WAS DEATH CAUSED BY STARVATION OR DISEASE?
Was the original disease aggravated by a failure to supply the patient with food, or are the lesions observed the result of starvation? A positive conclusion can be reached in such cases by carefully considering the results of a post-mortem examination together with other facts elicited by the inquiry.
Harriet Staunton,[966] a young girl, had been kept in close confinement by four interested persons, and removed in great[824] haste, when in a condition of extreme prostration, to Penge, where she died, on the day succeeding her removal, in a state of extreme exhaustion and emaciation. Fat was absent from every part of the body; the stomach and intestines were empty, contracted, and their walls were greatly thinned.
A small deposit of tubercle was found at the summit of the left lung and a recent deposit of miliary tubercle beneath the arachnoid, upon the surface of one of the cerebral hemispheres. No other tuberculous deposits were found. The opinion given by the physicians making the post-mortem examination was that death resulted from starvation. This opinion was shared by Professor Virchow, of Berlin, who stated that the tuberculous deposits found could not explain the cause of death.
In this case the extreme emaciation, entire absence of fat, thinning of the intestinal walls, etc., were the determining conditions. While extreme emaciation alone is not sufficient to decide the case to be one of starvation, its existence, taken in connection with some of the conditions found constantly in persons known to have died of starvation, is a strongly corroborative fact. Nor can its absence be taken as conclusive evidence that death occurred from other cause than starvation, since in some cases of death from inanition emaciation has not been extreme and in a few cases not at all marked.[967] Instances of this character are reported by Taylor and others.
DISEASES PRODUCED BY STARVATION.
The effect of insufficient alimentation in the production of disease has long been recognized. It is understood that this result follows the deficiency in either quality or quantity. The so-called “famine fever,” prevalent in times of dearth, has afforded extensive opportunity for observation of the effects produced. The symptoms developed are those directly referable to impoverishment of the blood. Pallor, emaciation, nervous depression, derangement of the digestive organs, and muscular enfeeblement appear in every case.
The development of strumous, herpetic, and cutaneous diseases generally is marked.
Of the secondary effects, the cachectic condition induced expresses[825] itself in pulmonary phthisis largely, while in infants and very young children intestinal disorders are specially frequent. Organic diseases already existing are seriously aggravated; wounds fail to heal, become ulcerative and sometimes gangrenous; while all degenerative processes are rapidly hastened to a fatal issue.[968]
INDEX.
————
Abdomen, contusions of, 580
post-mortem examination of, 370
wounds of, 580
Abdominal viscera, rupture of, 582
wounds of, 582
Abscess of brain, 563
Actions to recover for services (see Privileged Communications), 26
amount of recovery in, 45
elements to be proved in, 47
evidence in, 22-48
Actions for malpractice, 73-87
Adipocere, 451
Age, determination of, 399
Alcoholism, 564
Anthropometry, 432
Arteries, wounds of, 578
Asphyxia, 708
external appearances due to, 715
internal appearances due to, 718
in cases of poisoning, 356, 371
late, 378
of fragments, 380
order of, 356
Bills for services, effect of, 43
Bladder, rupture of, 585
wounds of, 585
Blank charges, wounds by, 617
Blood, coagulation of, 488, 701
condition of, after burns, 653
extravasation of, in brain, 565
on weapons, 535
stains, 350
Body (see Dead Body), examination of, 537
temperature of, 629
Bones, identification of, 390
old or recent? 391
Books, medical, when and where used in court, 64
of original entry, when admissible as evidence, 48
of physician, see Privileged Communications
Brain, abscess of, 563
concussion of, 561
congestion of, in drowning, 796
extravasation of blood in, 565
post-mortem examination of, 362
wounds of, 569
Bullets, 595
loss of weight of, 601
track of, 595
Burking, 775
by acids, 641
burning oil, 640
corrosives, 641
flame, 640
fused metals, 640
lightning, 694
petroleum, 641
cases of, 657
causes of death by, 645
classification of, 642
constitutional effects of, 644
local effects of, 643
period of death from, 649
post-mortem appearances of, 647
whether ante- or post-mortem, 649
Cadaveric changes (see Post-mortem), 441
Cadaveric saponification, 451
Cases of burns, 657
of hanging, 760
of strangulation, 726
of suffocation, 787
Catalepsy, 822
Cause of death, see Coroners
from burns, 645
severe mechanical injury, 499
submersion, 797
Cause of Death,
hemorrhage as, 497
latent disease as, 503
shock as, 499
was it natural? 503
wounds as secondary, 509
Clothing, examination of, 352, 537
Cold, effects of extreme, 630
Combustion, spontaneous, 647
Communications, privileged (see Privileged Communications), 33
Compensation, see Physician and Patient; Expert Witness; Coroners; Medical Examiners
Concussion, 472
of brain, 561
spinal cord, 573
Congenital peculiarities, identity from, 403
Constitutionality of statutes regulating practice of medicine and surgery, 7-11
Contracts between physician and patient (see Physician and Patient), 25
Contusions, 358, 467, 470, 523
by lightning, 695
of abdomen, 580
of head, 558
of neck, 570
Coroner (see Post-mortem Examinations), 331
is virtute electionis in America, 332
duties of, are both judicial and ministerial, 332
judicial authority of, relates to inquiries into cases of death, 332
jurisdiction of, 332
kinds of, at common law, 331
presumption that he has acted in good faith, 332
protected under same principles which protect judicial officers, 333
Effect of evidence and verdict, 343
at common law was equivalent to indictment by grand jury, 343
not so now, yet inquisition has same power until grand jury passes upon the case, 343
Evidence before, when admissible upon a subsequent trial, 344
Inquest, all evidence must be presented to jury, 342
coroner cannot hold a second inquest while the first is undischarged, 334
coroner has power to hold, 332, 334
is a judicial investigation, 333
must be held in view of the body, 335
separate inquests must be held over each of several bodies, 333
Jury and inquest, coroner may compel attendance of witnesses, 341
Jury and inquest, jurors must be from jurisdiction wherein coroner is empowered to act, 341
jurors must be sworn by coroner, 341
jurors must investigate and determine the facts, 341
jurors must view the body, 341
jurors not challengeable, 341
witnesses must be sworn by the coroner, 342
Massachusetts, see Medical Examiners
office abolished by statute in, 338
statutory provisions in, 338
who may hold an inquest, 338
New York, coroner may issue warrant of arrest of person charged with the death, 341
must, after examination of charges, hold defendant to answer or discharge him, 341
must proceed to examine charges against accused upon his arrest, 341
inquisition and testimony must be filed, 340
jurors must inspect the body and hear the testimony, 340
jury must render verdict and certify it by an inquisition, 340
six or more jurors must be sworn, 340
statutory provisions, 339
testimony must be reduced to writing, 340
when inquest may be held, 339
Powers of,
cannot delegate authority or appoint deputy, 333
contract will bind county for payment of reasonable compensation, 336
may employ professional skill to aid him, 335
may have body disinterred, 335
may issue process of apprehension, 343
Return of inquisition, 342
inquisition should be signed by the coroner and jury, 343
should certify that witnesses before the coroner were sworn, 343
verdict of the jury is final, 342
Rights of accused party before, 342
has not the right to be represented by counsel or to cross-examine witnesses, 342
is not permitted to produce witnesses to show himself innocent, 342
privilege of prisoner upon arrest, 344
testimony may be taken by the coroner in his absence, 342
under New York criminal code defendant is entitled to a hearing before a magistrate, 344
Craniometry, 394
Cremation, 389
Custom of physicians to serve each other gratuitously, 52
changes in, 441
chemical examination of, 303
cooling of, 441
coroners’ duties concerning (see Legal Status of, Appendix), 301
crimes against (see Legal Status of, Appendix), 299
disposal of, 298
dissection, when permitted (see Legal Status of, Appendix), 302
district attorney’s powers concerning, 303
duty of burial, 298
examination of gunshot wounds, 610
exhumation of, 300
external examination of, 358
flaccidity of, 442
internal examination of, 360
legal status of, 297
Appendix, giving statutes concerning, 304
physical examination of (see Autopsies), 302
post-mortem examination of (see Autopsies; Post-mortem Examiners), 303
putrefaction of, 445
right of burial or removal, 301
saponification of, 451
seizure for debt forbidden, 299
statutes regulating interment or exhumation, etc., generally, 304
Alabama, 309
Arizona, 309
Arkansas, 309
California, 310
Colorado, 311
Connecticut, 311
Delaware, 312
Florida, 312
Georgia, 312
Idaho, 313
Illinois, 313
Indiana, 313
Iowa, 314
Kansas, 314
Kentucky, 314
Louisiana, 315
Maine, 315
Maryland, 315
Massachusetts, 316
Michigan, 316
Minnesota, 317
Mississippi, 317
Missouri, 318
Montana, 318
Nebraska, 318
Nevada, 319
New Hampshire, 319
New Jersey, 320
New Mexico, 320
New York, 320
North Carolina, 321
North Dakota, 321
Ohio, 322
Oklahoma, 322
Oregon, 323
Pennsylvania, 323
Rhode Island, 324
South Carolina, 324
Tennessee, 324
Texas, 325
Vermont, 325
Virginia, 325
Washington, 326
West Virginia, 326
Wisconsin, 326
Death, apparent, 439
from anæsthetics, 516
burns, causes of, 645
period of, 649
whether accidental, suicidal, or homicidal? 657
cold, 633
post-mortem appearances in, 634
electrical currents, 683
hanging, proof of, 757
latent disease, 503
natural causes, 503
slight injuries, 507
starvation, 813
strangulation, proof of, 721
suffocation, proof of, 784
signs of, 440
time of, 437
Deformities, identity from, 403
Diaphragm, rupture of, 579
wounds of, 579
Diploma or license, how proved in court, 20
Dislocations, 476
Drowning (see Submersion), 793
Ecchymoses, 467
ante-mortem, 444
Electric cars, 668
Electric light, effects of, on eyes, 676
Electrical apparatus, injuries from, 664
Electrical currents, burns from, 664, 676
direct injuries from, 671
direct symptoms of injury from, 676
fatal, 682
high tension, 666
indirect injuries from, 670
injury from, 664
internal symptoms caused by, 678
mechanical effects of, 675
mental symptoms from, 689
muscular contraction from, 677
Electrical resistance, 673
Electricity, 661
medical, 664
static, 673
Electrocution, 683
Erosion, 471
Erysipelas, 511
Examination of body, 537
of clothing, 537
of surroundings, 541
Excoriation, 471
Experiments, testing powder-marks, 613
with cadavers, 607
Expert witness (see Privileged Communications), 49-72
compensation of, 60
competency of, 61
conduct of, in court, 65
definition of, 53
examination of, scope of, 65, 68
impeachment of, 64
in civil and criminal cases, 61
medical books, how may be used in examining, 64
practical suggestions, 70
summons of court must be obeyed, 60
system in Germany and France compared with that in United States, 54
Exposure, effects of, 630
Extremities, wounds of, 589
Face, wounds of, 569
Falls, 549
Faradism, 672
Firearms, evidence from, 600
examination of, 612
Flash, identity by, 619
Footprints, 427
by gunshot wounds, 610
of ribs, 574
skull, 559
spine, 571
spontaneous, 474
Gall-bladder, wounds and rupture of, 584
Genital organs, post-mortem examination of, 376
wounds of, 588
Gunshot wounds, see Wounds, Gunshot
Hæmatomata, 468
Hair, identity from, 406
on weapons, 535
Handwriting, 434
accidental, cases of, 774
cases of, 760
homicidal, 759
cases of, 767
judicial, cases of, 770
post-mortem appearances, 746
proof of death by, 757
suicidal, 758
cases of, 760
symptoms in, 740
treatment in, 744
Health, Boards of, see Practice of Medicine and Surgery
physicians reporting contagious diseases to, not liable for mistaken reports, 23
Head, post-mortem examination of, 361
wounds of, 557
Heart, in strangulation, 719
post-mortem examination of, 366
rupture of, 578
wounds of, 575
Heat, effects of extreme, 635
internal, 444
Identification, 383
by flash of gunpowder, 619
from congenital peculiarities, 403
entire skeleton, 392
imprints, 427
injuries, 403
scars, 419
stigmata, 426
tattooings, 421
teeth, 401
in death from submersion, 802
of burnt remains, 389
human bones, 390
mutilated remains, 408
recently dead, entire cadaver, 415
surface signs for, 419
Incised wounds, see Wounds
Infants, liability of, for medical services, 37
Information, duty of patient as to (see Physician and Patient), 33
Injuries, coagulation of blood in, 488
fatal, acts performed after, 493
identification from, 403
medical inspection of, 101
of abdominal walls, 580
viscera, 580
spinal cord, 571
spine, 571
slight, death from, 507
whether ante- or post-mortem, 482
Inquest, see Coroners
Insane persons, liability of, for medical services, 39
Insolation, 636
Insulation of electrical conductors, 667
Intestines, post-mortem examination of, 371
wounds of, 586
Kidneys, post-mortem examination of, 370
rupture of, 584
wounds of, 584
Larynx, in death from hanging, 754
strangulation, 718
post-mortem examination of, 369
License (see Practice of Medicine and Surgery), 7
(or diploma), how proved in court, 20
licensed physician presumed competent as an expert witness, 58
licensed practitioner, pretending to be, when not a misdemeanor, 22
statutes requiring, constitutional, 7
suits cannot be maintained by persons without, 18
unlicensed practitioner not presumed competent as expert witness, 62
when may be compelled by courts, 14
when presumed, 19
Lightning, 690
burns from, 694
contusions by, 695
effects on internal organs, 702
loss of consciousness from, 696
memory from, 696
paralysis from, 697
pathology of, stroke of, 700
staining of skin by, 696
symptoms produced by, 693, 696
wounds by, 695
Liver, post-mortem examination of, 375
wounds of, 582
Lungs, in death from strangulation, 719
submersion, 805
post-mortem examination of, 368
wounds of, 575
Lymphorrhagia, 470
Malpractice, 73-87
abortion is, 74
civil cases concerning, 80
contributory negligence in, 87
criminal cases concerning, 73
damages for, 83
definition of, 73
degree of care and skill in, 80
evidence in, 84
inspection before trial in, 85
partners liable for, 84
Mannlicher rifle, effects of, 619
Marks of powder, 608
Married women, liability of, for medical services, 37
Master, liability of, for services rendered servant, 39
Massage, not practising medicine or surgery, 28
Medical examiners, see Coroners
contract of coroner with, binds county to payment of reasonable compensation, 336
coroners may employ, 335
In Massachusetts:
cannot hold autopsy unless authorized, 338
cannot hold an inquest, 338
in place of coroners, 338
Medical societies, by-laws of, 15
fee bill, 22
Medicine and surgery, see Physician and Patient; and Practice of Medicine and Surgery
Muscular contraction, from electrical current, 677
Mutilated remains, identification of, 408
Nails, identification from, 406
Neck, contusions of, 570
wounds of, 569
Œsophagus, post-mortem examination of, 369
Overlying, 774
Pancreas, post-mortem examination of, 375
Patient, rights of, concerning confidential communications, 96
Physician, action for professional services, 133
his books containing confidential entries, 110
his rights and duties concerning confidential communications, 132
receiver not entitled to his books of account, 110
what is a professional capacity? 123
contracts between, compensation for services, 37
conditional and unconditional, 34
consulting physicians, 44
physician, 28
employment, how terminated, 26, 28, 30
may be declined, 24
estates of deceased persons, when liable for, 43
express or implied, 26
express, 27
implied, elements of, 28
infants, liability of, 43
insane persons, when liable, 45
married women, generally not liable, 43
masters, liable for services rendered servants, 45
measure of recovery for, 45
patient presumed liable, 37
person calling in physician not presumed liable, 36, 41
physicians treating each other, when they may recover, 47
railway company, when liable for, in case of accident, 42
railway physicians, authority of, 42
relation of physician and patient, 119
compensation for services, right to sue for in United States, 26
how lost, 19
students’ services, 44
skill and care required of (see Malpractice), 28, 31, 32, 33
schools of medicine not recognized by courts, 15
standard of school professed must be attained, 31
stranger may not be called in without patient’s consent, 29
Pithing, 572
Poisoning, 597
Post-mortem appearances, in death from burns, 647
cold, 634
hanging, 746
starvation, 822
strangulation, 713
sunstroke, 638
Post-mortem changes, 441
hypostasis, 443
lividity, 443
Post-mortem examinations (see Autopsies, Coroners), 354
when and ow made by coroner, 337
Post-mortem wounds, 355
Practice of medicine and surgery (see Physician and Patient), 7-25
acquirement of right, regulated by statutes, 7
constitutionality of, statutes regulating, 8
criminal cases, proof of, 19, 22
license for, may be compelled, 14
how proved, 20
medical societies and by-laws of, 14
fee bills, 15
massage not, 22
patent medicines, 14
statutory regulations concerning, in:
Alabama, 137
Arizona, 139
Arkansas, 140
California, 141
Colorado, 144
Connecticut, 145
Delaware, 148
Dist. of Columbia, 149
Florida, 150
Georgia, 151
Idaho, 152
Illinois, 153
Indiana, 155
Iowa, 157
Kansas, 160
Kentucky, 160
Louisiana, 162
Maine, 164
Maryland, 165
Massachusetts, 167
Michigan, 167
Minnesota, 168
Mississippi, 169
Missouri, 171
Montana, 173
Nebraska, 175
Nevada, 177
New Jersey, 178
New Hampshire, 181
New Mexico, 181
New York, 183
North Carolina, 189
North Dakota, 191
Ohio, 193
Oklahoma, 193
Oregon, 194
Pennsylvania, 197
Rhode Island, 203
South Carolina, 203
South Dakota, 204
Tennessee, 205
Texas, 207
Utah, 209
Vermont, 211
Virginia, 212
Washington, 215
West Virginia, 219
Wisconsin, 222
Wyoming, 223
Great Britain, 224
Scotland, 224
England, 224
Ireland, 224
Brit. Columbia, 238
Manitoba, 242
N. Brunswick, 248
Newfoundland, 255
N. W. Terr., 258
Nova Scotia, 262
Ontario, 268
Prince Edw. Is., 278
Quebec, 284
Privileged communications, 91
cause of death, 111
communications to physician not privileged at common law, 91
“confidential communications,” 115, 118
between physician and patient, when privileged, 94
dependent upon professional capacity, 98
effect of excluding privileged evidence, 130
evidence admitted not to be commented on, 111
in criminal actions, 101
in lunacy proceedings, 103
of abortion, 102
of adultery, 102
of crime in civil actions, 101
of criminal intimacy, 102
of habitual drunkenness, 103
of value of physician’s services, 133
to establish privilege, 106
function of the court, 128
ground of privilege, 91
harmless admission no ground for exception, 111
how evidence of physician taken in New York, 97
how privilege established, 131
in actions for divorce, 102
in criminal actions, 101
“matters confided,” 99
“matter necessary to enable a physician to prescribe or a surgeon to act,” 124
mental condition of patient, 103
necessity, 98
objections to evidence, 109
when made, 110
objection once made need not be repeated, 111
partner of physician, as privileged witness, 122
patient’s ignorance immaterial, 110
rights concerning confidential communications, 96
physician defined, 105
“duly authorized,” 105
as witness to establish privilege, 131
physician’s advice, 98
books, 110
cannot refuse to disclose when patient waives privilege, 99
knowledge, 98
presumption from failure to give privileged evidence, 130
privilege is patient’s, not physician’s, 107
“professional capacity,” 123
purpose of statutes prohibiting disclosures, 96
relation of physician and patient, 119, 122
result of legislation, 134
rights and duties of physician, 132
statutory privileges concerning confidential communications, 93
statutory privileges for waiver of privilege, 96
surgeon defined, 105
testamentary causes, 103
waiver after death of patient, in New York, 98
waiver of privilege after patient’s death, 108
by application for insurance, 111
by proof of death to insurance company, 111
by contract, 112
by infant, 108
by patient’s attorney, 107
by representative of deceased patient, 103
by requesting physician to witness will, 113
certificate of death, 115
infant’s, 113
taking physician’s deposition, 112
testimony of patient, 111
what constitutes, 111
what evidence is excluded, 97
what is privileged, 115
when patient may be contradicted by physician, 112
who may waive, 106
whose testimony is privileged, 105
witness, 97
Projectile, course of, 615
evidence from, 600
Punctured wounds, see Wounds
circumstances favoring, 447
retarding, 448
Pyæmia, 511
Race, determination of, from hair, 393
skeleton, 393
Railway companies, when liable for medical services, 41
Railway physicians, authority as to employing nurses, 42
Reports, medico-legal, 381
Resistance, electrical, 673
Respiration, suspended, 439
Ribs, fracture of, 574
Rifle, Mannlicher, 619
Rupture of abdominal organs, 582
bladder, 585
gall-bladder, 584
of heart, 578
internal organs, 553
kidneys, 584
spleen, 584
stomach, 586
Saponification, 451
Scalds, 639
Scars, in relation to identity, 419
Schools of medicine not recognized by courts, 15
Septicæmia, 510
Sex, determination of, 400
Sharks, bites of, 808
Shock, 499
Shot-guns, wounds by, 607
Signs of death, 440
Skin, marks on, 419
Skull, fracture of, 559
measurements of, 394
Small shot, wounds by, 617
Smothering, 774
Spinal cord, concussion of, 573
post-mortem examination of, 377
wounds of, 571
Spine, dislocation of, 572
fracture of, 571
wounds of, 571
Spleen, post-mortem examination of, 371
rupture of, 584
wounds of, 584
Spontaneous combustion, 647
Stabs, 463
Stains, could assailant have escaped without? 538
Starvation, acute, 817
chronic, 818
death from, 813
diseases produced by, 824
or disease, which was cause of death? 823
period of death from, 820
post-mortem appearances in, 822
whether accompanied by other ill-treatment, 822
Stature, determination of, 398
Sternum, fracture of, 574
Stigmata, 426
Stomach, post-mortem examination of, 373
rupture of, 586
wounds of, 586
accidental, 724
cases of, 734
cases of, 726
external appearances due to, 713
homicidal, 725
cases of, 726
internal appearances due to, 727
post-mortem appearances, 713
proof of death by, 721
simulated, 725
stages of, 710
suicidal, 724
cases of, 732
symptoms of, 708
treatment of, 712
Struggle, signs of, 536
Submersion, 793
asphyxia by, 796
cadaveric signs in death by, 804
circumstances modifying time of, 810
definition of, 796
mode of death by, 797
post-mortem appearances, 801
stages and symptoms of death by, 798
treatment of apparently drowned, 802
whether accidental, suicidal, or homicidal, 807
accidental, 785
cases of, 787
by submersion, 796
cases of, 787
external causes of, 774
homicidal, 785
cases of, 790
internal causes of, 775
mechanical, 705
post-mortem appearances, 781
proof of death by, 784
suicidal, 785
cases of, 790
symptoms of, 777
treatment, 779
Sunstroke, 636
Surgeon, definition of term, 56
duties of, see Physician and Patient
Surgical operations, death from, 515
Survival, 556
Tattooing, 421
Teeth, determination of identity from, 401
Temperature of body, 629
Tetanus, 513
Thorax, post-mortem examination of, 365
wounds of, 573
Time of death, 437
how determined, 452
Veins, air in, 579
wounds of, 578
evidence from, 600
as to origin of wounds, 533, 549
examination of, 612
presence of blood and hair on, 535
was it fired from a distance or near? 612
Witness, see Expert Witness; Privileged Communications
physician as expert and ordinary witness, 50
when must testify as, 60
as directly cause of death, 497
as secondary cause of death, 509
by what instrument made? 517, 524
coagulation of blood in, 488
consequences of non-fatal, 556
death from, after long periods, 508
definitions of, 459
description of, 482
direction of, 529
eversion of lips of, 489
evidence from weapon, 533, 549, 600
examination of, 476
from crushing, 553
falling, 549
lightning, 695
gunshot, 593
by blank charges, 617
by shot-guns, 607
gunshot, by small shot, 617
complications of, 624
course of projectile, 615
death from surgical operations in, 624
description of, 594
dimensions of perforations, 609
direction of, 599
examination of, 594
of body in, 610
of entrance, 614
of exit, 614
situation of, 598
treatment of, 620
imputed, 544
diagnosis of, 462
kinds of, 459
mortal, 460
nature of, 548
number and extent of, 531
of abdominal viscera, 580
walls, 580
arteries and veins, 578
bladder, 585
brain, 569
diaphragm, 579
extremities, 589
face, 569
gall-bladder, 584
genital organs, 588
heart, 575
intestines, 586
kidneys, 584
liver, 582
lungs, 575
neck, 569
spinal cord, 571
spine, 571
spleen, 584
stomach, 586
thoracic viscera, 573
thorax, 573
throat, incised, 526
origin of, evidence from weapons, 533, 549
regionally considered, 557
retraction of sides of, 490
severe, 460
situation and position of, 527, 548
slight, 460
whether accidental, 547
ante-mortem or post-mortem, 482
necessarily the cause of death, 500
self-inflicted or by another, 525, 544, 548
which of several was first inflicted? 544
two was cause of death? 500
FOOTNOTES:
[1] The distinction made in the text and in the title of this work is not new. It was recognized by the father of medico-legal science, Zacchias, in his two prefaces, one to the “lector medicus,” the other to the “lector legumperitus” (“Quæst. Med. Leg.,” Ed. Venet., 1727, fol.). In a note to the introduction of the “Medical Jurisprudence” of Dr. Paris and Mr. Fonblanque (the first work produced by joint authorship of a physician and a lawyer, in 1823) is the following (p. i.): “Some authors have objected to the term Medical Jurisprudence as implying a knowledge of the laws relating to medical topics, rather than an acquaintance with the medical science necessary for the elucidation of legal subjects. As it is our peculiar object to unite the sciences and to show their mutual relevance, the title becomes most applicable to this, although it may have been improperly affixed to former works.” The title of one of two existing French works in whose authorship a lawyer is associated is: “Traité de Médecine légale, de Jurisprudence médicale et de Toxicologie,” par Le Grand du Saulle, Geo. Berryer et Gab. Pouchet, 2d ed., 8vo, Paris, 1886.
[2] “Bibl. Hist.,” I., ii., 77; Miot’s transl., Paris, 1834, i., 157.
[3] L. c., I., ii., 82; transl., i., 165.
[4] L. c., I., ii., 75, 76; transl., i., 152.
[5] The “Papyros Ebers,” in the University of Leipzig, the most ancient medical text known, was written about 1550 B.C., and is probably one of the books referred to by Diodorus. It contains no statement bearing upon our subject. It is, however, simply a collection of descriptions of remedies, and their uses, including the incantations to be used with them. (See “Papyros Ebers,” H. Joachim, Berlin. 1890.) The same is true of the Berlin and Leyden papyri. The Bibl. Nat. (Tf. 2) possesses a Chinese manuscript on legal medicine. The catalogue does not, however, state to what period it belongs.
[6] For an account of early Indian medicine, see Th. A. Wise, “Review of the Hist. of Med.,” Lond., 1867, i., 272 et passim; “Hindu System of Medicine,” 1845, by the same author; Haeser, “Lehrb. d. Gesch. d. Med.,” 3. ed., i., 5-40.
[7] Hippocr.: “De Superfœtatione,” ed. Littré, viii., 472.
[8] Hippocr.: “De Septimestri partu;” ibid., “De Octimestri partu,” ed. Littré, viii., 432, 436, 452.
[9] “Aphorismi,” vi., 18, 24; “De Morbis,” ed. Littré, vi., 144.
[10] Petit, S.: “Leges Atticæ,” Lugd. Bat., 1742, lib. iii., tit. 8.
[11] “Od.,” iv., 229; xvii., 384.
[12] For an excellent account of Attic criminal procedure, see Kennedy, C. R.: “Demosthenes’ Orations,” ed. Bohn, iii., 326-372.
[13] “Var. Hist.,” iii., 38.
[14] Kennedy’s transl., ed. Bohn, v., 95.
[15] What the contents of these depositions were and by whom made is unknown, as the papers referred to by the orator are not given. In the Attic courts the testimony was taken at a preliminary trial, and referred to at the trial by the orator.
[16] “Oratores Attici,” C. Müller, Paris, 1877, i., 20.
[17] “Oratores Attici,” C. Müller, ed. Didot, Paris, 1877, i., 200-203.
[18] In a doubtful fragment of Lysias the expression “as physicians andmidwives declare” (ὡσπερ οὶ ἰατροὶ καὶ αὶ μαῑαι ἁπερηναντο) is used in connection with the question whether a fœtus has life and may be murdered. Cf. “Orat. Attici,” Müller and Hunziker, Paris, Didot, 1858, ii., 257.
[19] “Jul. Cæs.,” 82.
[20] “Hist. Nat.,” xi., 71.
[21] “Hist. Nat.,” vii., 4.
[22] A. Gellius: “Noct. Att.,” 1. 3, c. 16: “requisitis veterum philosophorum et medicorum sententiis.” The word “veterum” seems to indicate that the emperor consulted books, not living physicians.
[23] “Medici non sunt proprie testes, sed majis est judicium quam testimonium.”
[24] For accounts of the medico-legal provisions of the Justinian enactments, see: G. A. v. d. Pfordten, “Beiträge z. Gesch. d. ger. Med. aus d. Justin. Rechtssam.,” Würzburg, 1838: M. F. Eller, Bull. Med. Leg. Soc. N. Y., 1879, i., 226-237; and Friedreich, Blt. f. ger. Anthr., Nürnberg, 1850, I., iii., 1-64; 1862, xiii., 188-215.
[25] See Mende: “Handb. d. ger. Med.,” Leipzig. 1819, i., 83-87.
[26] “Etablissements et Coûtumes, Assises et Arrêts de l’Echiquier de Normandie au xiii. Siècle,” A. J. Marnier, Par., 1839: “veue d’homme en langueur, veue de méfaits, veue d’homme occis et veue de femme despucelée.”
[27] “Ut peritorum judicio medicorum talis percussio asseveretur non fuisse letalis,” Mende, “Handb. d. ger. Med.,” i., 91.
[28] Hensschel, in “Janus,” Breslau, 1847, ii., 135.
[29] Assises de Jérusalem,” Beugnot, Paris, 1841-43, quoted by Ortolan, l.c., infra.
[30] Ortolan: “Débuts d. l. Méd. lég.,” Ann. d’Hyg., Par., 1872, 2 s., xxxviii., 361.
[31] “Registre Criminel du Châtelet de Paris,” Par., 1861, i., 255.
[32] Ibid., i., 313.
[33] Ibid., i., 375, 409.
[34] “Quæst. Medico-legales,” t. ii., lib. vi., tit. ii.: vol. ii., pp. 33-49, ed. Venet., fol., 1737.
[35] See also “Reg. Crim. Chât. de Paris.,” i., 204, ii., 429; Desmaze: “Hist. Méd. Lég.,” 11-20, 33-41.
[36] Isensee: “Gesch. d. Med.,” i., 216.
[37] “Constitutio criminalis Carolina.” The first edition was printed at Mayence, 1533, fol., by J. Schöffer. See also Kopp, “Jahrb. d. Staatsarznk.,” Frankf., 1808, i., 183.
[38] “Con. cr. Car.,” art. 147.
[39] Ibid., art. 149.
[40] Ibid., arts. 35, 36, 131, 133; “Bambergische Halssgerichts-Ordenung.” Bamb., 1507, art. 44.
[41] “Con. cr. Car.,” art. 37.
[42] Ibid., art. 134.
[43] Ibid., arts. 135, 179, 219.
[44] “Non per quoslibet, nec per insipidos et imperitos, sed tantum per peritos ac doctos medicos aut chirurgos,” p. 245.
[45] “Praxis Rerum Criminalium,” Antw., 1554 (the dedicatory epistle is dated 1551), pp. 245-252, 223-228.
[46] Wildberg, “Bibl. Med.-for.,” Berl., 1819, Nos. 553, 554, 1,124, 1,125, 1,126, 1,304, 1,835, 1,836, 2,342, cites nine works earlier than 1575. These are, however, monographs on the period of gestation, witchcraft, fasting girls, drunkenness, and wounds of the head.
Works on toxicology were written at a much earlier date: the Θηριακά and Αλεξιφάρμᾶκα, of Nicander, ca. B.C. 135; θeπερὶ δηλητηρίων φαρμάκων, of Dioscorides, ca. A.D. 50; the treatises, “De Venenis,” of Petrus de Abbano (ca. A.D. 1250), first printed Mantua, 1472; of Arnoldus da Villanova (ca. A.D. 1300), first printed (sine loc. et an.) ca. 1470; of Santes de Ardoynis, Venice, 1492, and of F. Ponzetti, Venice, 1492, are among the earliest. Works on toxicology are not considered in this Introduction, the historical sketch of that science being reserved for a later volume.
[47] Ed. Malgaigne, 1840, t. iii., l. xxvii., pp. 651-658; ed. princ., Paris, 1575, fol., pp. 931-944. On the title-page of an earlier work, printed in 1562, Paré is referred to as “chirurgien ordinaire du Roi, et Juré à Paris.” Ploucquet, “Lib. Med. dig.,” Tüb., 1809, iv., 349, mentions a monograph by “Tygeon, Th.,” printed at Lyons, 1575.
[48] S. Pineau: “De notis Integritatis et Corruptionis Virginum,” Paris, 1598; A. Hotman: “De la Dissolution du Mariage par l’Impuissance,” etc., Paris, 1581; de la Corde, “Ergo Virgo ... lac in mammis habere potest,” Paris, 1580. Wildberg, l. c., Nos. 555, 1,308, 1,309, are not properly medico-legal.
[49] In his “De Vitiis Vocis,” etc., Frankf., 1597. He had previously published a treatise, “De morbis veneficis ac veneficiis,” Venet., 1595.
[50] “De relationibus medicorum ... in quibus ea omnia quæ in forensibus ac publicis causis medici referre solent,” etc., Panormi, 1602. Mongitore, “Bibl. Sic.,” Panormi, 1707-14. i., 199, mentions an edition of 1598, Pan., under the title: “Bissus [Birrus?], sive medicorum patrocinium,” etc.
[51] “Quæstiones Medico-legales,” Rome, 1612-35, 3 t., fol. See also Kerschensteiner: Friedr. Bl. f. ger. Med., etc., Nürnb., 1884, xxxv., 401-410.
[52] Wildberg, “Bibl. Med.-for.,” gives the titles of thirty-four treatises on legitimacy, impotence, sterility, signs of virginity, etc., published in France during this period.
[53] On reports: Réné Gendri, 1650; Nicolas de Blegny, 1684; J. Devaux, 1693; Prevot, 1753; H. M. Maret, 1757. On signs of death: P. E. Dionis, 1718; J. B. Winslow, 1740; S. J. Bruhier, 1745.
[54] On the signs of death, 1752; on the distinction between suicide and murder by hanging, 1763; on the duration of pregnancy, 1764, etc. These and other articles on drowning, etc., are collected in his “Œuvres diverses de Chirurgie,” 2 vols., Par., 1788.
[55] Cases of Monbailly, Syrven, Calas, Cassaigneux, Baronet, etc.
[56] “Recueil de pièces relatives à la question des naissances tardives,” Amst. and Par., 1766, 2 vols.
[57] “Consult. Méd.-lég. s. u. Accus. d’Infanticide,” 1785; “Obs. Chir.-lég.,” 1790; “Méd.-lég.,” 1809; “Consult. et Rapp. sur diverses obj. d. Méd.-lég.,” 1824; “Mém. méd.-lég. s. l. Viabilité,” 1826; “Consult. Méd.-lég. s. u. cas d’amp. d. l. Cuisse,” 1828.
[58] “Les Lois éclairées par les Sciences physiques,” Par., 1798, 3 vols., 8vo; “Traité de Méd.-lég. et d’Hyg. publ.,” Par., 1813, 6 vols., 8vo.
[59] “Méd.-lég.,” etc., Rouen, 1801; Paris, 1807, 1811.
[60] “Cours. de Méd.-lég.,” Paris, 1809, 1811, 1819.
[61] “Aperçu et obs. s. l. Méd.-lég.,” Lyon, 1811; “Secours aux Asphyxies,” Lyon, 1818; “Man. d. Méd.-lég.,” Lyon, 1821.
[62] In the later editions Chaudé took the place of Brosson, and a chemist, J. Bouis, was added.
[63] Devergie, “Méd.-lég.,” 1836, contains a legal chapter by de Robécourt. Paris and Fonblanque, “Med. Jurispr.,” Lond., 1823; Wharton and Stillé, “Med. Jur.,” Phila., 1855; Le Grand du Saule, Berryer et Pouchet, “Tr. de Méd.-lég. de Jur. méd. et de Tox.,” 2d ed., Par., 1881.
[64] “Sur les Attentats aux Mœurs,” 1st ed., 1857; 7th ed., 1878; “Sur l’Avortement,” 1856, 1861, 1868; “Sur la Pendaison,” etc., 1865, 1870, 1879; “Sur l’Empoisonnement” (with Z. Roussin), 1867, 1875; “Sur l’Infanticide,” 1868; “Sur la Folie,” 1872; “Sur les Blessures,” 1879; “Sur les Maladies, etc.,” 1879.
[65] Lib. iv., cap. ix.: Qua ratione morbum simulantes deprehendi queant; cap. x.: testificandi methodus circa eos, quibus venenum fuit exhibitum; cap. xi.: testificandi ratio in vulneribus capitis; et in iis qui aquâ fuerunt suffocati; cap. xii.: Quomodo amissa virginitas: et alterius utrius conjugis sterilitas deprehendatur.
[66] “De renunciatione vulnerum,” etc., Lips., 1689, 8vo (“Egregium opus,” Haller).
[67] “De officio medici duplici, clinico nimirum et forensi,” Lips., 1704, 4to (“Eximius liber,” Haller).
[68] “Pandectæ Medico-legales,” etc., Francof., 1701, 4to; “Novellæ Medico-legales,” etc., Francof., 1711, 4to; “Corpus Juris Medico-legale,” etc., Francof., 1722, fol.
[69] “Medicina forensis, hoc est responsa facultatis medicæ Lipsiensis ad quæstiones et casus medicinales, ab anno 1650 usque 1700,” Francof., 1706, 2 vols., 4to.
[70] “Der medicinische Richter, oder Acta physico-medico forensia Collegii medici Onoldini,” Onolzbach, 1755, 4to.
[71] “Systema Jurisprudentiæ Medicæ,” etc., 6 vols., 4to, Halle, Leipzig, and Görlitz, 1725-47.
[72] “Institutiones Medicinæ legalis et forensis,” Jena, 1723, 1731, 1740, 1762.
[73] “Medicina forensis demonstrativa,” etc., Frankf., ad Viadr., 1723; “Introductio in historiam litterariam scriptorum qui medicinam forensem commentarius suis illustraverunt,” Frankf., 1723, 1735.
[74] “Elementa Medicinæ forensis,” Jena, 1767, published posthumously.
[75] Hebenstreit: “Anthropologia forensis,” Lips., 1753; Ludwig: “Institutiones Medicinæ forensis,” ed. 2, Lips., 1774.
[76] “Beiträge zur medicinischen Gelehrsamkeit,” etc., Halle. 1748-54; “Sammlung medicinischen ... Zeugnissen,” etc., Leipz., 1776; “Institutionum Medicinæ publicæ,” etc., Lips., 1778.
[77] “Kurzgefasstes System der gerichtlichen Arzneywissenschaft,” Königsb. u. Leipz., 1793.
[78] “Entwurf der gerichtlichen Arzneiwissenschaft,” etc., Frankf., 1796-1801, 4 vols.
[79] “Collectio Opusculorum selectorum ad Medicinam forensem spectantium.” Lips., 1785-90, 6 vols.
[80] “Conspectus Medicinæ legalis,” etc., Prague, 1780.
[81] “Elementa Medicinæ et Chirurgiæ forensis,” Viennæ, 1781; “Toxicologia,” etc., Viennæ, 1785.
[82] Magazin für die gerichtliche Arzneikunde und medicinische Polizei, Stendal, 1782-87, 6 vols. Pyl also published “Aufsätze und Beobachtungen aus der gerichtlichen Arzneiwissenschaft,” Berlin, 1783-93, 8 vols. Uden was the first to edit a medical journal in Russia.
[83] “Vollständiges System der gerichtlichen Arzneikunde,” Stendal, 1795-1800; “Beiträge zur praktischen und gerichtlichen Arzneikunde,” Stendal, 1799.
[84] Jahrb. der gesam. Staatsarzneikunde, Leipzig, 1835-40, 7 vols.; Bibliotheca Medicinæ publicæ,” Berol., 1819, 2 vols. Between 1804 and 1849 Wildberg published fifteen books and treatises on medico-legal subjects.
[85] Kritische Jahrb. f. d. Staatsarznk. f. d. xix. Jahrb., 1806-09. Jahrb. d. Staatsarznk., 1808-19.
[86] Zeitschrift für die Staatsarzneikunde, Erlangen, 1821-64, 118 vols.; “Lehrbuch der ger. Med.,” 1te Aufl., Berlin, 1812, 13te Aufl., Berlin, 1859.
[87] “Visa Reperta,” Wien, 1827-45, 3 vols.; “Systematisches Handb. d. ger. Med.,” Wien, 1te Aufl., 1813, 5te Aufl., 1846.
[88] “Ausfürl. Handb. d. ger. Med.,” Leipzig, 1819-32, 6 vols.
[89] “Handb. d. ger. Med.,” Berlin, 1841.
[90] “Enzyklop. Handb. d. ger. Arzneyk.,” Leipzig. 1838-40, 2 vols.; Magazin f. die Staatsarzneykunde.
[91] Centralarch. f. d. ges. Staatsarznk., Ansbach, 1844-49; Blätter f. d. gerichtliche Anthropologie, Erlangen, 1850, now published at Erlangen under the title Friedreich’s Blätter f. ger. Med. u. Sanitätspolizei.
[92] “Gutachten u. Aufsätze,” etc., Leipzig, 1847; “Auswahl von Gutachten,” etc., Dresden, 1853.
[93] “Beiträge z. medicin. Statistik,” etc., Berl., 1825-35, 2 vols.; “Denkwürdigkeiten z. medicin. Statistik,” etc., Berl., 1846; “Gerichtl. Leichen-Oeffnungen,” Berl., 1851-53, 1850-52; “Klinische Novellen,” etc., Berl., 1863.
[94] “Pract. Handb. d. ger. Med.,” Berl., 1te Aufl., 1857-58; 8te Aufl., Berl., 1889, also translation of Geo. Balfour, New Sydenham Soc., London. 1861-65. The fourth and succeeding editions, published after Casper’s death (1864), were edited by Karl Liman, his successor in the chair of medical jurisprudence (d. 1892).
[95] Vierteljahresschr. f. ger. u. öffentl. Med., Berl., 1852, edited after Casper’s death by Horn, 1865-70, Eulenberg, 1871-90, Wernich, 1891.
[96] “Handb. d. ger. Med.,” Tübingen, 1881-82, 4 vols.
[97] Daniel: “Bibl. d. Staatsarznk.,” Halle, 1784, No. 107, mentions: “E. Prat, Rationarium chirurgicum, oder nothwendiges Handbuch des Wundarztes, wie er Bericht an die Obrigkeit thun soll u. s. w., aus dem Engl.,” Hamb., 1684. 4, 690. 8. The same title is reproduced by Wildberg (No. 239) in 1819, and the edition of 1684 is mentioned by Ploucquet, “Initia” (1803), Suppl. iv., 36, and “Litt. med. dig.” (1809), iii., 54, the name of the author being given as “Pratt (Elias).” This may be an early work by Ellis Pratt, but we can find no mention of it elsewhere. In the years 1734, 1761, and 1787 dissertations on abortion were defended at Edinburgh by Arnot, Harris, and Murray. Three treatises on death from suffocation by Goodwyn, Frank, and Coleman appeared in 1788-91. In 1788 S. Farr published at London his “Elements of Medical Jurisprudence,” to which Percival (“Med. Ethics,” Oxford, 1849, p. 102) justly refers as “a valuable epitome of S. F. Faselii’s “Elementa Medicinæ Forensis [Regiom., 4to, 1787], in English by Dr. Farr.”
[98] “Med. Jur.,” iii., p. 226 seq. Report that Joseph Lane died of poison (1623). Report that Sir James Standsfield was strangled and not drowned, with account of autopsy (1687). Also extracts from the medical evidence in the cases of Spencer Cowper (from 13 Howell’s “State Trials”); Mary Blandy (Oxford, 1752); John Donellan (Warwick, 1781); and R. S. Donnall (Launceston, 1817).
[99] “Heads of Lectures on Medical Jurisprudence, or the Institutiones Medicinæ legalis,” vi., 24 pp., 8vo, Edinb., 1792.
[100] See Beck “Med. Jur.,” 7th ed., xvi., and note.
[101] In the preface Dr. Percival says: “This work was originally entitled ‘Medical Jurisprudence,’ but some friends having objected to the term Jurisprudence it has been changed to Ethics.” An unfinished and unpublished edition, written prior to 1794 and containing Chapter IV., was printed about 1800 (see Editor’s Preface, p. 2, and note, Author’s Preface, pp. 25, 26, ed. Oxford, 1849).
[102] “An Epitome of Juridical or Forensic Medicine,” etc., viii., 199 pp., 8vo, London, 1816, also in Th. Cooper’s “Tracts on Med. Jur.,” Phila., 1819. In the preface the author refers to the lectures of Prof. Duncan.
[103] This excellent work (“The Principles of Forensic Medicine”) went through three editions in six years. Dr. Smith, who was a teacher of medical jurisprudence in the Royal Institution, Westminster Hospital, and University of London, and also published a number of papers in the Edinb. M. and S. Jour., and “Hints for the Examination of Medical Witnesses,” Lond., 1829, died at the age of forty-one in 1833, after fifteen months’ imprisonment in a debtors’ prison.
[104] “Med. Jur.,” 3 vols., 8vo, London, 1823. See note 1, p. v.
[105] “A Manual of Med. Jur.,” London, 1831, 2d ed., 1836, Amer. ed., with notes by R. E. Griffith, Phila., 1832.
[106] “Outlines of a Course of Lectures on Med. Jur.,” Edinb., 1836, 2d ed., 1840, Amer. ed., Phila., 1841.
[107] A. Amos, Lond. M. Gaz., 1830, vii.; 1831, viii. A. T. Thomson, Lond. M. and S. J., 1834-35, vi.; 1835, vii.; also Lond. Lancet, 1836-37, i., ii. (Thomson’s lectures were printed in German in book form, Leipzig, 1840.) H. Graham, Lond. M. and S. J., 1835, vi., vii. W. Cummin, Lond. M. Gaz., 1836-37, xix. T. S. Smith, Lond. M. Gaz., 1837-38, xxi.; 1838, xxii.
[108] Dease: “Med. Jur.,” and Haslam: “Med. Jur. Insanity,” along with the treatises of Farr and of Male, are reprinted in Cooper’s “Tracts on Med. Jur.,” Phila., 1819.
[109] Synop. Mod. Med. Jur.,” Lond., 1829.
[110] “Treatise on Med. Jur.,” Lond., 1834; Phila., 1836.
[111] “Homicide by External Violence,” Lond., 1837.
[112] “Med. Jur.,” Dublin, 1839.
[113] “Cases in Leg. Med.,” Edinb., 1840.
[114] “Med. Jur. of Insanity,” Lond., 1840.
[115] “Criminal Jurisprudence in relation to Mental Organization,” London, 1841.
[116] “Principles and Practice of Med. Jur.,” 1st ed., Lond., 1865; 3d ed., Lond., and Phila., 1883. “On Poisons,” 1st ed., Lond., 1848; 3d ed., Lond., 1875. “Lectures on Med. Jur.,” Lond. M. Gaz., 1846, n. s., ii., iii.; 1847, n. s., iv. Articles on arsenic, antimony, strychnine, and other toxicological subjects, strangulation, blood-stains, etc., in Guy’s Hosp. Repts.
[117] “Principles of Forensic Medicine,” Lond., 1844. The work is now in its sixth edition. Prof. D. Ferrier, Dr. Guy’s successor in King’s College, having been associated in the authorship of the 4th ed. in 1875 and subsequently.
[118] “Lectures on Med. Jur.,” edited by Fr. Ogston, Jr., Lond., 1878.
[119] Woodman and Tidy: “A Handy-book of Forensic Medicine and Toxicology,” Lond. and Phila., 1877. Tidy, “Legal Medicine.” 2 vols., Lond., 1882-83; also, Phila., 3 vols., 1882-84; New York, 3 vols., 1882-84.
[120] “Cirurgia Forense,” etc., 3 vols., 12mo, Madrid, 1796-97. Wildberg mentions two earlier monographs: “De partu Septimestri,” Antw., 1568, by F. Mena, physician in ordinary to Philip II.; and “Diez privilegios para mugeres prennantes,” Complut., 1606, by J. A. de Fontechia, professor at Alcala de Hénares.
[121] “Elementos de Medicina y Cirurgia legal,” etc., Madrid, 1834; 4th ed., Zaragossa, 1844.
[122] “Tratado de Medicina y Cirurgia legal,” etc., Madrid, 1844; 5th ed., 4 vols., 8vo, Madrid, 1874-75.
[123] “Instituições de Medicina forense,” Paris, 1832; 2d ed., Lisbon, 1840.
[124] “Vorlesungen über die gerichtliche Arzneiwissenschaft,” 3 vols., 12mo, Bern, 1728-84.
[125] “Utkast til Medicinal-Lagfarenheten,” etc. (Project of medical jurisprudence, etc.) Stockh., 1776.
[126] “Forelaesninger over den legale Medicin,” Christiania, 1838.
[127] “Haandbog i den legale Medicin,” Kjøbenhavn, 1843.
[128] “Versuch eines Umrisses der philosophisch.-medizinischen Jurisprudenz.” u. s. w., Dorpat, 1803.
[129] See Wildberg: “Bibl. med. leg.,” Nos. 1,198, 1,142, 1,215.
[130] Lugd. Bat., 1610, etc.
[131] Amstel., 1615.
[132] Rotterd., 1767.
[133] Lugd. Bat., 1768.
[134] S. Gravenh., 1815.
[135] “Traité de Médecine légale et de Jurisprudence de la Médecine,” 2 vols. in 1, Gand., 1859-60; 2d ed., Paris, 1878; 3d ed., Bruxelles, 1885. (See Toxicology.)
[136] “Yei sei honron” (Lectures on medical jurisprudence, translated by Gento Oye), 3d ed., 2 vols., Tokio, 1880.
[137] “Saiban igaku teiko” (Medical Juris.), 3 vols., Tokio, 1882-84.
[138] “Sixteen Introductory Lectures,” etc., Phila., 1811, pp. 363-395.
[139] Amer. Med. and Phil. Reg., N. Y., 1814, iv., 614. It is to be regretted that instruction in medical jurisprudence is not now given at this school (1893).
[140] Beck, “Med. Jur.,” 7th ed., xix. The Index Catalogue contains the titles of forty-nine works by Caldwell, none of which are medico-legal.
[141] Beck, loc. cit.
[142] “Tracts on Medical Jurisprudence,” etc., Phila., 1819.
[143] “Elements of Medical Jurisprudence,” 2 vols., 8vo, Albany, 1823; 12th ed., 2 vols., 8vo, Phila., 1863. A chapter on Infanticide by John B. Beck was added to the third edition. This and later editions are “by T. R. and J. B. Beck.”
[144] N. Y. Med. and Phys. Jour., 1823, ii., 9-30.
[145] “An Essay on Medical Jurisprudence,” Phila., 1824.
[146] Phila. J. M. and Phys. Sc., 1825, x., 36-46.
[147] “Syllabus of Lectures.” etc., Univ. of Va., 1827.
[148] “An Introductory Address,” etc., Phila., 1829, and “Syllabus of a Course of Lectures on ... Medical Jurisprudence in the Philadelphia Medical Institute” [n. p., n. d.].
[149] “A Catechism of Medical Jurisprudence.” etc., Northampton, 1835.
[150] Dean (A.): “Manual of Medical Jurisprudence,” Albany, 1840; Dean (A.): “Principles of Medical Jurisprudence,” Albany, 1854: Elwell (J. J.): “Medico-legal Treatise on Malpractice and Evidence,” New York, 1860; 4th ed., New York, 1881.
[151] “Medical Jurisprudence.” Phila., 1855. 4th ed., edited by R. Amory and E. S. Wood, 3 vols., Phila., 1884.
[152] “A Medico-legal Treatise on Malpractice and Medical Evidence,” N. Y., 1860; 4th ed., N. Y., 1881.
[153] “The Jurisprudence of Medicine,” etc., Phila., 1869.
[154] In that case (Bailey v. Mogg), the Court says of that statute (Laws of 1844, p. 406): “The triumph was now complete, for the legislature had made every man a doctor, and nostrums of every description and admixture could now be safely prescribed, and payments therefor exacted by authority of law.”
[155] Notwithstanding these statutory enactments, it has been held that one who undertakes to cure disease by rubbing, kneading, pressing, and otherwise manipulating the body (massage) is not liable for having violated the provisions of the statute against practising medicine or surgery without a license. Smith v. Lane, 24 Hun (New York Supreme Court), 32.
[156] Analysis of this decision shows that the main ground, upon which the court of last resort sustained the right of the applicant for admission to be admitted as a member of the society, was, that the provisions of the by-law in question were not specifically made applicable to a person applying for membership. The Court observed, pp. 192 et seq.: “The regulations embodied in the so-called code are admirably framed, and commend themselves to every reader, as tending to raise to a still higher elevation the character of the learned and honorable profession to which they were submitted for approval and adoption. They are not limited in their scope to the range of moral obligation, but embrace express rules of conduct, in personal, professional, and public relations. They are regulations in the various departments of morals and manners, of courtesy and etiquette, of delicacy and honor. They bind those who pledge themselves to their observance, but cannot be recognized in law, as conditions precedent to the exercise of an honorable profession, by learned, able, and upright men, who have not agreed to abide by them. The non-observance of such regulations may be made cause for exclusion or disfranchisement; but it must be either by the agreement of parties or by the exercise of the law-making power.
“The applicant was not a member either of the American Medical Association or of the Erie County Medical Society, at the time of his alleged deviation from the formulas prescribed by these conventional rules. He was under no legal obligation to observe them, and had neither actual nor constructive notice of their existence. Those who were members of the society could not lawfully be expelled for antecedent deviation from the code (Fawcett v. Charles, 13 Wend., 477). Much less could such deviation be alleged, as cause for exclusion, against one who had never agreed to be bound by it, and as to whom it was not merely an inoperative but an unknown law.
“As the relator demanded admission to the enjoyment of a franchise to which he was presumptively entitled, his exclusion could be justified only by facts repelling the presumption that he was duly qualified for admission, or by extraneous facts, showing that, if his application was granted, there were then subsisting causes, making ‘a clear case’ for immediate expulsion (Ex parte Paine, 1 Hill, 665).
“The burden was upon the appellant to establish affirmatively the existence of such present cause for expulsion. The society waived the right of making a return and taking a formal issue on the claim of the relator, to be determined as matter of fact by a jury, under the direction of the court; but submitted its objections in the form of affidavits, which failed to establish cause either for exclusion or expulsion.
“The only specific fact alleged in the opposing affidavits, as ground of objection, was the publication by the relator of a professional advertisement, which was inserted in one or more of the Buffalo journals in May, 1855, and discontinued in January, 1857, more than two years before his application was presented. It is charged that the printing of this notice was an empiricism, and in conflict with the code of ethics adopted by the Erie County Medical Society.
“There is nothing in the terms of the advertisement from which any inference can justly be drawn against the relator, in respect either to his personal character or his professional skill. There is no suggestion, in the affidavits, that any of the statements of fact contained in the notice are untrue, and there is nothing in its contents inconsistent with perfect good faith on the part of the relator. It refers to the treatment of bronchitis, asthma, and consumption, as a special department of the profession to which he had directed his particular attention; and it alludes to his use of the method recently introduced, of medicated inhalation, through an instrument appropriate to that purpose, in aid of such general treatment as experience had proved to be beneficial in that class of diseases. It is not denied that the relator possessed peculiar skill in this department of the profession; and the case discloses the fact that the method of auxiliary treatment, introduced by him in the county of Erie, was not only successful in his own practice, but was adopted, with beneficial results, by members of the county society of high professional standing, and that it was accepted by a large proportion of the physicians of Western New York. If, at the time this remedy was introduced, he had been a member of the County Society or of the American Medical Association, he would not have been at liberty to direct attention, through the medium of the public journals, to the benefits resulting from its use. This would, perhaps, have been unfortunate for those who were suffering, in that vicinity, from this particular class of diseases; but it is undoubtedly true that the suppression of such an advertisement would have been more considerate toward his professional brethren, and more in accordance with the rules of delicacy and good taste. But an error, in this respect, by one who had no notice of the society regulation is not cause for disfranchisement. The act of the relator was neither immoral nor illegal. It was no violation of the by-laws; for, as to him, they were wholly inoperative. It was no present cause for exclusion; for the publication of the objectionable notice had been discontinued for more than two years. When he applied for admission, he proposed to become bound by the by-laws; and this the society refused to permit, for the sole cause that he had not observed them before they became rules of conduct for him. ‘Where there is no law, there is no transgression.’ The relator, therefore, had been guilty of no legal wrong which could bar his claim to the franchise.”
[157] In Macpherson v. Cheadell (24 Wend., N. Y., 15) the Court said, p. 24:
“In the first place I doubt much whether the defendant below, after retaining the plaintiff as a physician and accepting his services as such, could call upon him in the first instance to prove a regular license. In other like cases, the presumption is against the defendant. It is so as between attorney and client, in a suit for services performed under a retainer. Pearce v. Whale, 7 Donl. & Ryl., 512, 515, per Bayley, Judge; 5 Barn. v. Cress., 38, S. C. There, if the objection sound in the fact that the plaintiff was never admitted, or that his admission has become inoperative, it lies with the defendant to show it. Id., and see Berryman v. Wise, 44 T. R., 566. and other cases; 1 Phil. Ev., 227, Cowen v. Hill’s ed. Besides, the contrary would be doing great violence to the presumption that no man will transgress the command of a positive law.” See also Thompson v. Sayre (1 Denio, N. Y., 75), where this principle seems to have been assumed as correct without question upon the strength of the decision quoted above. A similar doctrine appears to have been enunciated in the State of Illinois in Chicago v. Wood, 24 Ill. App., 42; and Williams v. People, 20 Ill. App., 92. It may be sound, and undoubtedly the English cases cited in Macpherson v. Cheadell, supra, tend to support it. But in a case in which the physician’s right to practise is denied, the safe course will be for him to have a duly authenticated copy of his license ready to be offered in evidence. The general rule is that the burden is on the plaintiff to show all the facts which make up his right of recovery. See Bliss v. Brainard, 41 N. H., 256; Salomon v. Dreschler, 4 Minn., 278; Kane v. Johnston, 9 Bosw., N. Y. Superior Ct., 154.
[158] That is, the burden devolves upon the defendant, and this notwithstanding the presumption of innocence, of showing what must be peculiarly within his own knowledge, namely, that he has been duly licensed. People v. Nyce, 34 Hun, N. Y., 298, and cases cited; 1 Greenleaf on Ev., § 79, and cases cited. See, contra, State v. Evans, 5 Jones. N. C., 250.
[159] In Finch v. Gridley’s Executors (25 Wend., N. Y., 469-471), Nelson, Ch. J., said: “I am also inclined to think the evidence which was given competent to prove the diploma from Fairfield College. The witness identified the corporate seal, and had himself received a diploma from that institution subscribed by the same president and secretary. Though he did not actually see them subscribe the paper, he had every means of becoming acquainted with their signatures; the delivery of it to him was an acknowledgment they had signed it. Besides, he was familiar with diplomas from the institution under their signature,” etc.
And see, also, Raynor v. State, 62 Wis., 289; Wendel v. State, id., 300.
[160] In some of the States, persons who simply administered roots and herbs in treating disease, have been excepted from that portion of the statute which forbids the practice of medicine and surgery without a license. The proper construction of such an exception is, that it is a question of fact for the jury, whether the person accused who claims the benefit of the exception, simply administered a concoction of roots and herbs within the meaning of the statute, or whether, under the guise of so doing, he really held himself out as and acted as a regular practitioner. All such penal statutes are to be construed, like all other penal statutes, with due regard to the rights of the individual, and at the same time with such degree of liberality as will tend to preserve the public safety.
[161] It has been held that the act of a physician in reporting to a health-board in good faith that his patient is suffering from small-pox, is not actionable. Brown v. Purdy, 8 N. Y. St. Rep., 143. The Court said (per Sedgwick, J.): “In order to give the public the protection due to it, according to the intention of the statute, any physician that possesses in fact an opinion that a patient has a contagious disease, is bound to report the case, whether he has or has not used ordinary professional skill and knowledge. A physician of skill in everything but cases of small-pox, which happily are not numerous, may, unexpectedly to himself, be called to a case which presents to him the appearance of small-pox. It may be said that he may call in counsel. It cannot, however, be said that private counsel should be called in rather than such as the law has appointed. Certainly, if he really thinks the case to be one of small-pox, it is his duty to communicate his opinion to the public authorities, who furnish skilled physicians peculiarly competent to pass upon the case. They are the experts the law points out for the physician. The attendance of these experts upon a patient can cause no injury, and thereafter the responsibility rests solely upon the public officer.”
As to how far the decision of an inspector appointed by a board of health is regarded by the law as quasi-judicial, and therefore conclusive, see Underwood v. Green, 42 N. Y., 140; Raymond v. Fish, 51 Conn., 80. Health officers who were guilty of gross negligence in removing infected persons from a city in stormy weather, and putting them in an unprotected and unsafe structure, so that such persons died from the exposure, have been held liable. Aaron v. Broiles, 64 Tex., 316.
The latest and most complete statute laws creating or regulating health boards are: England, 38 and 39 Victoria, chap. 55; United States (National Board of Health), 20 Stat. L., 484, suppl. to U. S. Rev. Stats., chap. 202, passed March 3d, 1889; Mass., chap. 79, Mass. Rev. Stats.; Pa., Laws of 1885, chap. 56; New York (State Board of Health), 2 N. Y. Rev. Stats., 1195; Local Boards, id., 1191-1193, chap. 270, Laws of 1885. The statutes of New Jersey are considered in Lozier v. Newark, 19 Vr., 453. In Missouri the power to license physicians is conferred upon the State Board of Health, and the Supreme Court of that State has held that the act of that board in granting or refusing a license is discretionary and its action in such a matter will not be enforced by a writ of mandamus (State v. Gregory, 83 Mo., 123); and a similar doctrine prevails in Minnesota, State v. State Med. Board, 32 Minn., 324. The latest and best work on the general subject of the organization and powers of boards of health is Parker & Worthington’s “Public Health and Safety,” M. Bender, publisher, Albany, N. Y., 1892.
[162] Consult, as to this, Parsons on “Contracts,” vol. ii., p. 56.
[163] Of course in those States or countries in which statutes of fraud render void, contracts for personal services for a longer period than one year (or any period named in the statute), unless such contracts are in writing and duly signed, contracts should be drawn and entered into with regard to those statutes.
[164] See also “Field’s Medico-Legal Guide,” 208-210, where the following cases are cited as sustaining this doctrine: New York, Carpenter v. Blake, 60 Barb., 488; same case on appeal, 75 N. Y. Court of Appeals, 12. Connecticut, Landon v. Humphrey, 9 Conn., 209. Iowa, Smothers v. Hawks, 34 Ia., 286. Indiana, Long v. Morrison, 14 Ind., 595. Maine, Leighton v. Sargeant, 27 Me. (7 Fost.), 468; Howard v. Grover, 28 Me., 97. Illinois, MacNevins v. Lowe, 40 Ill., 209. Kansas, Teft v. Wilcox, 6 Kan., 46. Massachusetts, Com. v. Thompson, 6 Mass., 134; Small v. Howard, 128 Mass., 131, 35 Am. Rep., 363. Pennsylvania, Potter v. Warner, 91 Pa. St., 362, 36 Am. Rep., 668. Wisconsin, Reynolds v. Graves, 3 Wis., 416. Vermont, Briggs v. Taylor, 28 Vt., 180.
[165] See Shear. & Redf. on Negligence, 440; Elwell on Malpractice, 55; Carpenter v. Blake, supra; Rex v. Long, 4 C. & P., 422; Slater v. Baker, 2 Willes (Eng.), 259; Ordronaux on Jurisp. of Med., pp. 29 et pass.; 20 Am. Law Rev., 82.
[166] On the points here suggested cf. Edington v. Life Ins. Co., 67 N. Y., 185, same case, 77 N. Y., 564; Grattan v. Life Ins. Co., 80 N. Y., 281; Dilleber v. Life Ins. Co., 87 N. Y., 79; Westover v. Life Ins. Co., 99 N. Y., 56; People v. Murphy, 23 N. Y. Weekly Digest, 42; same case, 101 N. Y., 126; Hunn v. Hunn, 1 T. & C., 499; Pierson v. The People, 79 N. Y., 432-435; People v. Carlyle Harris, 136 N. Y., 424.
[167] Patten v. Wiggin, 51 Me., 594.
[168] See on this question also Bigelow’s “Leading Cases,” on Torts, 295-303.
[169] Stevenson v. The New York, etc., Railroad Co., 2 Duer, 341; same case, 1 Am. & Eng. R. R. Cases, 343; Cincinnati, etc., R. R. Co. v. Davis, 43 Am. & Eng. R. R. Cases, 459.
[170] Bronson v. Hoffman, 7 Hun, 674; Williams v. Glenny, 16 N. Y., 389, and see Ordronaux on “Juris. of Med.,” supra, p. 46; but see also Danzinger v. Hoyt, 46 Hun, 270.
[171] And it has been held that a decedent’s estate is liable for fees of expert, who by direction of probate court examined widow and testified as to her pregnancy. This notice was put upon the ground that his testimony was necessary for the information of the court in a matter before it affecting the disposition of the estate. Rollwager v. Powell, 8 Hun, 10.
[172] Crain v. Baudouin, supra; Shelton v. Johnson, 40 Iowa, 84; Garry v. Stadlen, 67 Wis., 512.
[173] And a physician may recover the value of services rendered by his students. People v. Monroe, 4 Wend. (N. Y.), 200; Jay Co. v. Brewington, 74 Ind., 7. And the physician in attendance is not liable to the physician thus called. Guerard v. Jenkins, 1 Strobh., 171.
[174] Deway v. Roberts, 46 Michigan, 160.
[175] MacPherson v. Chedell, 24 Wend., 15; Adams v. Stevens, 26 Wend., 451; Story on Bailments, § 37.
[176] Duly licensed physicians are presumed to be experts as to the value of other physicians’ services. Beekman v. Platner, 15 Barb., 550.
[177] Bellinger v. Craigue, 31 Barb., 534; Gates v. Preston, 41 N. Y., 113; Blair v. Bartlett, 75 N. Y., 15. The general rule is that in an action arising on contract damages arising for a tort cannot be set up as a counter-claim. It follows from this that in an action of a physician for services, damages for malpractice could not be recouped or counter-claimed ordinarily. The way in which that rule is avoided, and the safer method, is for the defendant to plead that it was part of the contract of the physician (which it undoubtedly is), to perform his services in a faithful and skilful manner, and that he committed a breach of it, thus charging the damages which flowed from his acts as a breach of contract, not as a cause of action in tort for malpractice or negligence. If that is done the counter-claim arising in malpractice can probably be pleaded in an action for services, and possibly a counter-claim in excess of the amount claimed by the physician recovered as an affirmative judgment against him. On the other hand, in an action for malpractice brought by the patient against a physician, which is generally in form an action for a tortious act, or neglect, the physician cannot plead the performance of services and the non-payment of his bill as a counter-claim or recoupment, because that arises on a contract. If there is any exception to this rule it will be found to grow out of the language of sections 549 and 550 of the Code of Civil Procedure of the State of New York, and of similar enactments in other States, which permit counter-claims arising out of the same subject-matter as the cause of action, to be pleaded in that action. In New York State, however, any effect of that kind is negatived by the general provision that the actions must not only arise out of the same subject-matter but be of the same kind and class.
[178] The degree of care and skill required to be shown to entitle the physician or surgeon to recover compensation for his services has already been stated to be simply such care and skill as are possessed by the majority of other professional men of the same school of practice at the time, or what is known as ordinary care and skill.
[179] Foster v. Coleman, 1 E. D. Smith, 85; Larue v. Rowland, 7 Barb., 107; Clarke v. Smith, 46 Barb., 30; Knight v. Cunningham, 6 Hun, 100; Bay v. Cook, 22 N. J. L., 343.
[180] The writer is indebted for many valuable suggestions concerning this subject to Ansley Wilcox, Esq., of the Buffalo, N. Y., Bar, and his admirable lectures on Medical Jurisprudence before the Medical Department of the University of Buffalo.
[181] The conservatism of lawyers is proverbial. It is hard to convince them that forms that have been long in use and have been found to serve a useful purpose in the past, are not applicable to new conditions as they arise; for instance, that the methods of procuring the attendance and of examining ordinary witnesses do not fit the necessities of expert testimony. But the question as to the defects of the system as it now exists has been brought to public attention in the journals of the day, in papers read before medical societies and bar associations, and in arguments in legislative bodies, and it is hoped and believed that ere long a reform, something of the character indicated, may be brought about in this very important matter.
[182] It has been a matter of great discussion whether an expert is compellable to testify on matters of opinion, without compensation, the weight of the decisions being that he is not bound to do so. 1 Greenleaf on Evidence, § 310; 1 Warwick Law Assizes, 158; Parkinson v. Atkinson, 31 L. J. (n. s.) C. P., 199; Webb v. Page, 1 E. & K., 25; People v. Montgomery, 13 Abb. Pr., n. s., 207; Ex parte Roelker, 1 Sprague, 276; Buchanan v. The State, 59 Ind., 1; Dills v. The State, Id., 15; U. S. v. Howe, 12 Cent. L. J., 193; contra, 6 Central Law Journal, 11; Ex parte Dement, 53 Ala., 389; Sumner v. The State, 5 Tex., 21; 6 Southern Law Review, 706.; and see generally Wharton on Evidence, sec. 380, note 66, sec. 456; Lawson on Expert and Opinion Evidence; Rogers on Expert Testimony. As to the compensation being paid before the testimony is given, see Wharton on Evidence, secs. 456, 380; People v. Montgomery, 13 Abb. Pr., n. s., 207.
It is proper, although not necessary, that upon cross-examination the witness should be asked as to his fee; that is, as to whether he expects to receive any additional fee besides that of an ordinary witness, and it has been held that where the expert witness testified that he was to receive a fee which was contingent upon the case, he was disqualified from testifying. Pollock v. Gregory, 9 Bosworth, N. Y. Superior Ct. Rep., 121-124.
[183] This latter case holds that a second expert may be called to testify after the first has been thus challenged, to support his capacity and skill. The contrary rule, however, obtains in Alabama (Tellis v. Kidd., 12 Ala., 643; Pugh v. State, 44 Ala., 33). Neither can an expert be contradicted by books of science; that is, by books of science introduced in evidence as such (Wharton on Evidence, 666, 721). This is so because the rule is well established that books, although of great authority in themselves, may not, even if proven to be such, be placed in evidence. They may, however, be read to the witness, and so be placed upon the record, passage by passage, and the witness may be asked whether he agrees with that doctrine, not, however, as part of his direct examination, but as part of his cross-examination.
A medical expert is sometimes confronted upon the witness-stand by long quotations from well known medical text-books, and he is asked whether the doctrines, opinions, etc., there laid down are sound. Especially is this done when such doctrines and opinions are in apparent discord with his evidence as he gives it. In such cases as this, however honest, however intelligent and non-partisan the witness may be (except as any opinion on one side or the other of a disputed question may be considered partisan), he is placed in a very difficult position. If the citations and questions are from well-known authors, and he is a modest man, as most men of learning are, it will be difficult for him to deny that such authorities as these have great weight, even more weight than his experience, skill, and knowledge entitle him to claim. On the other hand, if he takes the bold course and sticks to his opinion, he is cried down the winds by counsel in summing him up, as a man of gall, boldness, audacity and egotism. His course is difficult whichever way he turns, but modesty as well as honesty is usually the best policy. Perhaps the best thing for such a witness to do under such circumstances is to do as once did the great mental alienist Dr. John P. Gray, when, having given an opinion on a question of insanity, he was cross-examined as to the different theories from time to time prevalent as to what insanity was, and having stated what theories were then the accepted ones, he was confronted by counsel on his cross-examination with the question: “What do you think of Dr. John P. Gray as an authority on that question?” and then with his own writings, quite extensive, of many years before, in which he had advocated theories apparently different from those which he had professed upon the witness-stand. Placed in this position, the distinguished gentleman simply replied: “It is true I cherished those theories at that time, but I lived to learn better,” thus substantially disarming any criticism that could be made of him in his capacity as a witness in that case.
[184] For general rules for the conduct of expert witnesses see infra.
[185] The principal classes of such subjects may, however, be briefly stated as follows:
1. Causes of death; especially in cases of homicide, suicide, accident, etc., including poisoning.
2. Causes, nature, and extent of personal injuries, by violence, accidents, explosions, railway disasters, collision between vessels, etc.
3. Birth of infants; was infant born dead or alive; if dead, was death the result of natural causes or of internal violence; age of infant at the time of birth or death. Also causes of alleged sterility or pregnancy; time pregnancy has existed; also cases of alleged impotency.
4. Rape, abortion, bastardy, pederasty, onanism, masochism, and many other matters relating to the sexual organs.
5. Malpractice cases, involving the degree of care and skill usual, and that used in the case under investigation, and involving delicate questions as to the propriety of the treatment adopted, etc.
[186] See also 1 Bishop Crim. Law, sec. 36; Rex v. Romiski, 1 Moody, 19; Reg. v. Ellis, 2 Car. & K., 470.
[187] In such cases as these the patient would have a right of action in the civil courts for damages against the physician or surgeon, because he had taken wilful and wicked advantage of his professional relation to her, to do her a grievous wrong.
[188] The Pennsylvania courts at an early period refused to follow this common-law doctrine, and held that the moment the womb is instinct with life in embryo and the process of gestation has begun the crime may be perpetrated. Mills v. Com., 13 Pa. St., 631.
[189] 1 Bishop Crim. Law, sec. 217, citing Rex v. Williamson, 3 Car. & P., 635.
[190] The same learned and philosophical text-writer (2 Bishop Crim. Law, sec. 664) compares the English and American cases and declares that the difference between them is more apparent than real.
[191] See Rice v. The State, 8 Mo., 561; Fairlee v. People, 11 Ill., 1; Holmes v. State, 23 Ala., 17; Rex v. Spilling, 2 M. & Rob., 107; Ferguson’s Case, 1 Lew., 181; Thomas v. Winchester, 2 Selden, N. Y. Court of App., 397; Com. v. Pierce, 138 Mass., 165, and cases cited; State v. Hahn, 38 Ark., 605; Wharton’s Crim. Law, sec. 1015; Elwell on Malpractice, etc., 238, 239.
[192] 1 Bishop Crim. Law, sec. 558, citing Groenvelt’s case, 1 Lord Raymond, 213; Rex v. Long, 4 C. & P., 398.
[193] See also Kelsey v. Hay, 84 Ind., 189; Small v. Howard, 128 Mass., 131; Gates v. Fleisher, 67 Wis., 286; Smothers v. Hanks, 34 Iowa, 286; Almond v. Nugent, 34 Iowa, 300; Haire v. Reese, 7 Phila. (Pa.), 138; Nelson v. Harrington, 72 Wis., 591.
[194] Ruddock v. Low, 4 F. & F., 519; Musser v. Chase, 29 Ohio St., 577.
[195] See particularly Gieselman v. Scott, 25 Ohio St., 86; Lanphier v. Phipos, 8 C. & P., 475; Pym v. Roper, 2 F. & F., 783; Carpenter v. Blake, 60 Barb., 485, 50 N. Y., 696, 10 Hun, 358, 75 N. Y., 12; Leighton v. Sargent, 7 N. H., 460.
[196] Synonymous terms with “reasonable care” are “fair knowledge and skill,” Jones v. Angell, 95 Ind., 376; “ordinary care and skill,” Heath v. Glisan, 3 Oregon, 64.
[197] See Corsi v. Maretzek, 4 E. D. Smith, 1, quoted at p. 362 of this volume.
[198] Small v. Howard, 128 Mass., 131, and cases cited.
[199] Clairvoyancy of course is not recognized in the courts as medical or surgical practice. And any one professing to treat patients as a clairvoyant must be held to the standard of regular practising physicians in the neighborhood where the clairvoyant operates. Nelson v. Harrington, 72 Wis., 591; Bibber v. Simpson, 59 Me., 181; Musser v. Chase, 29 Ohio St., 577.
[200] McCandless v. McWha, 22 Pa. St., 261; Carpenter v. Blake, supra; Leighton v. Sargent, supra.
[201] Kelley v. Hay, 84 Ind., 189; Stone v. Evans, 32 Minn., 243; Teft v. Wilcox, 6 Kans., 646; Brooke v. Clark, 57 Tex., 105; Graunis v. Branden, 5 Day (Conn.), 260, s. c., 5 Am. Dec., 143; Wenger v. Calder, 78 Ill., 275; Carpenter v. Blake, supra.
[202] Hyrne v. Irwin, 23 S. Car., 226, s.c., 55 Am. Rep., 15; Whittaker v. Collins, 34 Minn., 209.
[203] Boor v. Lowrey, 103 Ind., 468.
[204] Hitchcock v. Burgett, 38 Mich., 501.
[205] See U. P. R. R. Co. v. Botsford, 141 U. S., 250; McQuiggan v. D., L. & W. R. R. Co., 129 N. Y., 50; Roberts v. O. & L. C. R. Co., 29 Hun, 154, and cases cited.
[206] Olmstead v. Gere, 100 Pa. St., 127; Carpenter v. Blake, supra.
[207] Greenleaf Ev., s. 236; Taylor Ev., s. 908; Bouvier’s Law Dictionary, p. 363; Am. and Eng. Enc. of Law, vol. 19, p. 122; Code Civ. Pro. Cal., s. 1,881; Mills’ Ann. Stats. of Col., 1891, s. 4,824; Rev. Stats. Idaho, 1887, s. 5,958; Gen. Stats. Minn., 1891, s. 5,094; Comp. Stats. Mont., 1887, s. 650; Gen. Laws Ore., 1892, s. 712; Comp. Laws Utah, 1888, s. 3,877.
[208] Taylor Ev., s. 911; Stephen, Dig. of Ev., art. 115; Greenleaf Ev., s. 237.
[209] The successive efforts made to extend protection by judicial ruling to communications between physician and patient will appear from a consideration of the cases that are usually cited as authority for the English rule: Annesley v. Earl of Anglesea (1743), 18 How. St. Tr., 1,139; Duchess of Kingston’s case (1776), 20 How. St. Tr., 355 (cf. p. 572, p. 585, p. 586, p. 613); Wilson v. Rastall (1791)., 4 Term R. (Durnford & East), 753; Rex v. Gibbons (1823), 1 C. & P., 97; Broad v. Pitt (1828), 3 C. & P., 518; Greenough v. Gaskell (1832), 1 My. & K., 98. See also Wheeler v. Le Marchant, 50 L. J. Ch., 795 (1880).
1 Phillips Ev., p. 136; Starkie Ev., p. 40; Wharton Ev., s. 606; Greenleaf Ev., secs. 248, 237, 239; Taylor Ev., s. 916; Stephen, Dig. of Ev., art. 115; Rogers’ Expert Testimony, s. 45; Reynolds’ Theory of Evidence, s. 86.
It is to be noted that none of the cases which are cited as authority for the common-law rule as usually stated are really precedents to that extent. The cases of the Duchess of Kingston (supra); Lord William Russel (9 How. St. Tr., 602); Dr. Ratcliff (9 How. St. Tr., 582); Earl Ferrers (19 How. St. Tr., 886), and Rex v. Gibbons (supra), were all criminal prosecutions; and in Annesley v. Anglesea, Wilson v. Rastall, Broad v. Pitt, and Greenough v. Gaskell (supra), which were civil causes, the question of the privilege of a medical man was not really in dispute. It is well settled that communications between attorney and client are privileged, and yet Judge Pitt Taylor expresses some doubt whether the protection cannot be removed without the client’s consent in cases where the interests of criminal justice require the production of the evidence (Taylor Ev., s. 929). This intimation of a distinction between criminal and civil actions, even in the case of attorneys, suggests the possibility of a difference between those two classes of actions in the case of medical men. The cases cited establish authoritatively that in criminal prosecutions, at common law, confidential communications between medical man and patient are not privileged; but in civil causes, the opinions of the eminent judges seem to be obiter dicta. It is, however, established by other decisions that mere confidential relations do not prevent the disclosure of communications. (For the case of bankers, see Loyd v. Freshfield, 2 C. & P., 325; managers, Anderson v. British Bank of Columbia. 45 L. J. Ch., 449; clerks, Lee v. Burrell, 3 Camp., 337; Webb v. Smith, 1 C. & P., 337; stewards, Vaillant v. Dodemead, 2 Atk., 524; Earl of Falmouth v. Moss, 11 Price, 455; Pursuivant of Herald’s College, Slade v. Tucker, 49 L. J. Ch., 644.)
The opinions of so many eminent men, though strictly speaking obiter dicta, together with the uniform statements of text-writers based upon them, leave no room for reasonable doubt that independent of statute, in civil as well as criminal causes, communications between medical adviser and patient are not entitled to protection from disclosure in evidence.
[210] See Duchess of Kingston’s case (supra, p. 91, note 3) (cf. ib., pp. 572, 585, 586, 613).
[211] Greenleaf Ev., secs. 249, 252, 252a.
[212] Greenleaf Ev. s. 249.
[213] See Barnes v. Harris, 7 Cush., 576; Hatton v. Robinson, 4 Pick, 422. See also historical review of the attorney’s privilege and the reasons for it, by Judge Seldon, at Special Term, in Rochester City Bank v. Suydam, 5 How. Pr. (N.Y.), 254.
[214] Wilson v. Rastall, 4 Term R., 753.
[215] Best, Prin. of Ev., s. 582.
[216] The revisers of the New York Statutes in 1828 in their report (5 N. Y. Stats. at Large, edited by John W. Edmonds, 2d ed., p. 726) stated as their reason for suggesting a statutory privilege for communications between physician and patient, that “in 4 Term Rep., 580, Buller, J. (to whom no one will attribute a disposition to relax the rules of evidence), said it was ‘much to be lamented’ that the information specified in this section (2 R. S., p. 406, s. 73) was not privileged. Mr. Phillips expressed the same sentiments in his treatise on Evidence, p. 104. The ground on which communications to counsel are privileged is the supposed necessity of a full knowledge of the facts, to advise correctly, and to prepare for the proper defence or prosecution of a suit. But surely the necessity of consulting a medical adviser, when life itself may be in jeopardy, is still stronger. And unless such consultations are privileged, men will be incidentally punished by being obliged to suffer the consequences of injuries without relief from the medical art, and without conviction of any offence. Besides, in such cases, during the struggle between legal duty on the one hand and professional honor on the other, the latter, aided by a strong sense of the injustice and inhumanity of the rule, will in most cases furnish a temptation to the perversion or concealment of truth, too strong for human resistance. In every view that may be taken of the policy, justice or humanity of the rule as it exists, its relaxation seems highly expedient.”
These or similar reasons have prevailed in many States and Territories to bring about a statutory restriction on disclosures.
[217] The following cases show or tend to show that the English rule is in operation in Connecticut, Maine, Maryland, Massachusetts, New Jersey, Texas, and West Virginia: Wilson v. Town of Granby, 47 Conn., 59; Fayette v. Chesterville, 77 Me., 28; Weems v. Weems, 19 Md., 334; Morrissey v. Ingham, 111 Mass., 63; Barber v. Merriam, 11 Allen, 322; Castner v. Sliker, 4 Vr., 95; Steagald v. State, 3 S. W. Rep., 771; Jarrett v. Jarrett, 11 W. Va., 584. For the common-law rule in the States where statutes are now in force, see Campau v. North, 39 Mich., 606; Territory v. Corbett, 3 Mont., 50; Pierson v. People, 79 N. Y., 424; Edington v. Ætna L. I. Co., 77 N. Y., 564; Buffalo Loan Tr. & S. D. Co. v. Knights Templar, etc., 126 N. Y., 450.
[218] Dig. Stats. Ark., 1884, s. 2,862; Code Civ. Pro. Cal., s. 1,881 as amended Law 1893, c. 217; Mills’ Ann. Stats. Col., 1891, secs. 4,824, 4,825; R. S. Ida., 1887, s. 5,958; Myers’ Ann. R. S. Ind., 1888, s. 497; Act of May 2d, 1890, U. S. Stats. at Large, c. 182, making the laws of evidence of Arkansas applicable to Indian Territory; McClain’s Ann. Code Iowa, 1888, s. 4,893; Code Civ. Pro. Kan., s. 323; Gen. Stats. Kan., 1889, s. 4,418; Howell’s Ann. Stats. Mich., 1882, s. 7,516; Kelley’s Gen. Stats. Minn., 1891, s. 5,094; R. S. Mo., 1889, s. 8,925; Comp. Stats. Mont., 1887, s. 650; Code of Civ. Pro. Neb., secs. 333, 334; Bailey & Hammond’s Gen. Stats. Nev., 1885, s. 3,406; Code Civ. Pro. N. Y., secs. 834, 836, as amended by Laws 1893, c. 295; Laws of N. C., Act of 1885, c. 159; Code Civ. Pro. Dak., 1883, s. 499; Smith & Benedict’s R. S. Ohio, 1890, s. 5,241; Stats. of Okl., 1893, s. 4,213; Hill’s Gen. Laws Ore., 1892, secs. 712, 713; Code Civ. Pro. Dak., 1883, s. 499; Code Civ. Pro. Utah, s. 1,156; Comp. Laws of Utah, s. 3,877; 2 Hill’s Ann. Stats. Wash., 1891, s. 1,649: Sanborn & Berryman’s Ann. Stats. Wis., 1889, s. 4,075; R. S. Wyo., 1887. s. 2,589. For the chronological order and the date of the passage of the earlier of these laws, see note to Gartside v. Connecticut Mutual L. I. Co., 76 Mo., 446.
[219] Rev. Stats. U. S., s. 721.
[220] Conn. Mut. Life Ins. Co. v. Union Trust Co., 112 U. S., 250. See also Dreier v. Continental L. I. Co., 24 Fed. Rep., 670; Adrereno v. Mutual Res. Fund L. I. Co., 34 Fed. Rep., 870.
[221] Logan v. United States, 144 U. S., 263; United States v. Reid, 12 How., 361.
[222] See references to the several statutes in note 2 on p. 94.
[223] See Freel v. Market St. Cable Ry. Co., 31 Pac. Rep., 730 (Supr. Ct. Cal.).
[224] This seems to be the proper construction of the Kansas and Oklahoma statutes, though what seem to be typographical errors in the published laws render it doubtful.
[225] For laws regulating practice in the several States and Territories, see infra, p. 137 et seq.
[226] Laws N. Y., Act 1893, c. 295.
[227] N. Y. Code Civ. Pro., s. 836, as amended Act 1893, c. 295. A similar exception was introduced by Act 1891, c. 381, and modified by Act 1892, c. 514.
[228] Supra, p. 94, note 1.
[229] Bishop, Written Laws, secs. 119, 155; Potter’s Dwarris, Statutes, p. 185; 1 Bouvier’s Law Dictionary, “Construction,” p. 386.
[230] Masonic Mut. Ben. Assn. v. Beck, 77 Ind., 203. For the construction of particular words and phrases, see infra, p. 115 et seq.
[231] For waiver of the privilege, see infra, p. 106.
[232] Penn Mut. L. I. Co. v. Wiler, 100 Ind., 92.
[233] Lunz v. Mass. Mut. L. I. Co., 8 Mo. App., 363.
[234] Kling v. City of Kansas, 27 Mo. App., 231.
[235] Gartside v. Conn. Mut. L. I. Co., 76 Mo., 446; said to be overruled by Groll v. Tower, 85 Mo., 249, in Squires v. City of Chillicothe, 89 Mo., 226; but followed in Thompson v. Ish, 99 Mo., 160.
[236] N. Y. Code Civ. Pro., s. 3,345. Disclosures by physicians are restricted by secs. 834, 836 of said Code.
[237] Code Civ. Pro., secs. 834, 836, as new existing are re-enactments with modifications of 2 R. S., p. 406, s. 73.
[238] People v. Stout, 3 Park Cr. Rep., 670; Edington v. Mut. L. I. Co., 67 N. Y., 185. Cf. Kendall v. Grey, 2 Hilt., 300; Pearsall v. Elmer, 5 Redf., 181. A disposition to construe the statute strictly was disclosed in the opinion of Earl, J., in Edington. v. Ætna L. I. Co., 77 N. Y., 564, but his personal views were disapproved in subsequent cases; see Grattan v. Metro. L. I. Co., 80 N. Y., 281; Renihan v. Dennin, 103 N. Y., 573; Buffalo Loan, etc., Co. v. Knights Templar, etc., 126 N. Y., 450. See also Jones v. Brooklyn, etc., Ry. Co., 3 N. Y. Supp., 253; in matter of Darragh, 52 Hun, 591; Marx v. Manhattan Ry. Co., 56 Hun, 575; Treanor v. Manhattan Ry. Co., 28 Abb. N. C., 47.
[239] See Collins v. Mack, 31 Ark., 684.
[240] N. Y. Code of Pro., s. 390; N. Y. Code of Civ. Pro., s. 870.
[241] Edington v. Mut. L. I. Co., 5 Hun, 1; s. c., 67 N. Y., 185.
Under sec. 873, Code Civ. Pro., as amended by Law 1893, c. 721, the plaintiff in an action for personal injuries may be compelled to submit to a physician’s inspection. Cf. Page v. Page, 51 Mich., 88.
[242] Supra, p. 96.
[243] Guptill v. Verback, 58 Iowa, 98. In this case, however, it was determined that it did not appear that a crime was intended.
[244] 2 R. S., 406, s. 73.
[245] Act 1876, c. 448, Code Civ. Pro., secs. 834, 836.
[246] Act 1877, c. 417, s. 1.
[247] 3 R. S., 1029, s. 19. Superseded by Code Crim. Pro., s. 392, as amended by Act 1892, c. 279, s. 7. People v. Murphy, 101 N. Y., 126. People v. Brower, 53 Hun, 217.
[248] Pierson v. People, 79 N. Y., 424; People v. Harris, 136 N. Y., 423.
[249] Pierson v. People, 18 Hun, 239.
[250] People v. Murphy, 101 N. Y., 126 (1886).
[251] People v. Brower, 53 Hun, 217 (1889). See also People v. Stout, 3 Park Cr. Rep., 670.
[252] Johnson v. Johnson, 4 Paige, 460; s. p., 14 Wend., 636; Hanford v. Hanford, 3 Edw. Ch., 468; Hunn v. Hunn, 1 T. & C., 499.
In Indiana, information as to abortion and criminal intimacy is protected in an action for criminal conversation. Harris v. Rupel, 14 Ind., 209. In Hewitt v. Prime, 21 Wend., 77 N. Y. (1839), in an action for seduction the testimony of a physician that he was asked for medicine to produce an abortion was admitted. It was stated that such testimony is not privileged, but there were other reasons for the judgment, and the case seems to be at variance with later decisions on that principle.
See also Briggs v. Briggs, 20 Mich., 34.
[253] Allen v. Pub. Adm., 1 Bradf., 221 (1850).
[254] Staunton v. Parker, 19 Hun, 55 (1879).
[255] Citing the fact that no objection was raised in the noted case of Delafield v. Parish, 25 N. Y., 1.
[256] Renihan v. Dennin, 103 N. Y., 573 (1886), followed in Loder v. Whelpley, 111 N. Y., 239 (1888). In re Hannah, 11 N. Y. St. Rep., 807 (Supr. Ct., G. T., 1887). In matter of Connor (Sup. Ct., G. T.), 27 N. Y. St. Rep., 905 (1889); Mason v. Williams (Sup. Ct., G. T., 1889), 6 N. Y. Supp., 479; Van Orman v. Van Orman (Sup. Ct., G. T., 1890), 34 N. Y. St. Rep., 824. See also In matter of Halsey (N. Y. Surr.), 29 N. Y. St. Rep., 533 (1890). Allen v. Pub. Adm., 1 Bradf., 221, had been overruled in part by Edington v. Mut. L. I. Co., 67 N. Y., 185 (1876), but not on this point.
[257] Supra, p. 98.
[258] Heuston v. Simpson, 115 Ind., 62.
[259] Fraser v. Jennison, 42 Mich., 206. In this case the testimony was admitted on the ground that the representative could waive the privilege. See Thompson v. Ish, 99 Mo., 160.
[260] In re Benson (Monroe County Court), 16 N. Y. Supp., 111 (1891). Some States have statutory provisions for the qualification of physicians as examiners in lunacy, e.g., Laws of Col., 1893, c. 119, s. 5; Laws of N. Y., 1874, c. 446, t. 1, art. 1, s. 1. The bearing of these provisions upon the statutory privilege has not been made clear.
[261] In matter of Baird, 11 N. Y. State Rep., 263 (1887).
[262] In matter of Hoyt, 20 Abb. N. C. (Sup. Ct., G. T., 1887).
[263] 13 N. Y. W. D., 505 (1880).
[264] Dilleber v. Home L. I. Co., 13 N. Y. W. D., 505 (1881).
[265] The following cases in which the rule has been enforced have arisen out of contracts of life insurance: Masonic Mut. Ben. Assn. v. Beck, 77 Ind., 203; Excelsior Mut. Aid Assn. v. Riddle, 91 Ind., 84; Penn Mut. L. I. Co. v. Wiler, 100 Ind., 92; Ætna L. I. Co. v. Denning, 123 Ind., 390; Lunz v. Mass. Mut. L. I. Co., 8 Mo. App., 363; Edington v. Mut. L. I. Co., 67 N. Y., 185; Grattan v. Metrop. L. I. Co., 80 N. Y., 281; s. p., 92 N. Y., 274; Conn. Mut. L. I. Co. v. Union Tr. Co., 112 U. S., 250.
[266] See Renihan v. Dennin. 103 N. Y., 573, dictum to same effect.
As to whether a physician may contradict his patient to prevent fraud, see infra, p. 111 et seq.
[267] Supra, p. 97.
[268] Infra, p. 119.
[269] “Physician: A person who has received the degree of doctor of medicine from an incorporated institution; one lawfully engaged in the practice of medicine.”—Bouvier’s Law Dict., vol. ii., p. 412.
“Surgeon: One who applies the principles of the healing art to external diseases or injuries, or to internal injuries or malformations, requiring manual or instrumental intervention. One who practises surgery.”—Bouvier’s Law Dict., vol. ii., p. 698, q. v.
[270] Edington v. Mutual L. I. Co., 5 Hun, 1.
[271] People v. Stout, 3. Park Cr. Rep., 670 (1858). In this case the witness was undoubtedly a duly qualified physician under the State law.
[272] Wiel v. Cowles, 45 Hun, 307 (1887) (Supreme Ct., Gen. T.). Sec. 356, N. Y. Penal Code, which was in operation at that time, was repealed by Act 1887, c. 647, s. 9, but the prohibition of unauthorized practice is now to be found in Act 1893, c. 661, s. 140.
[273] Kendall v. Gray, 2 Hilt., 300 (N. Y. Com. Pl., Gen. T., 1859).
[274] Brown v. Hannibal & St. J. R. R. Co., 66 Mo., 588.
[275] Carrington v. St. Louis, 89 Mo., 208.
[276] Infra, p. 128.
[277] Record v. Village of Saratoga Springs, 46 Hun, 448 (N. Y. Supr. Ct., Gen. T.).
[278] Supra, p. 96.
[279] Penn Mut. L. I. Co. v. Wiler. 100 Ind., 92; Morris v. Morris, 119 Ind., 341.
[280] Grand Rapids & Ind. R. R. Co. v. Martin, 41 Mich., 667; Fraser v. Jennison, 42 Mich., 206.
[281] Carrington v. St. Louis, 89 Mo., 208; Squires v. City of Chillicothe, 89 Mo., 226; Blair v. C. & A. R. R. Co., 89 Mo., 334; s. p., 89 Mo., 383; Adrereno v. Mut. Res. F. L. I. Co., 34 Fed. Rep., 870; Davenport v. City of Hannibal, 18 S. W. Rep., 1122.
[282] The most of the cases in which the rule has been enforced are those in which the physician has actually testified without raising the objection himself, and in which, therefore, the rule could not be enforced if the physician’s waiver were valid, but the following cases particularly are in point: Harris v. Rupel, 14 Ind., 209; Barton v. Allbright, 29 Ind., 488; Storrs v. Scougale, 48 Mich., 387; Lunz v. Mass. Mut. L. I. Co., 8 Mo. App., 363; Johnson v. Johnson, 14 Wend., 636; Hanford v. Hanford, 3 Edw. Ch., 468; People v. Stout, 3 Park Cr. Rep., 670.
[283] Mulhado v. Brooklyn City R. R. Co., 30 N. Y., 370; Heller v. Sharon Springs, 28 Hun, 344; Winner v. Lathrop, 67 Hun, 511.
[284] See Penn Mut. L. I. Co. v. Wiler, 100 Ind., 92; Territory v. Corbett, 3 Mont., 50; Johnson v. Johnson, 14 Wend., 636; Babcock v. People, 15 Hun, 347.
[285] Barton v. Allbright, 29 Ind., 488; Campau v. North, 39 Mich., 606; Territory v. Corbett, 3 Mont., 50; Blair v. Chic. & Alton R. R. Co., 89 Mo., 334; Johnson v. Johnson, 14 Wend. (N. Y.), 636.
[286] N. Y. Code Civ. Pro., s. 836 (Act 1876, c. 448), as amended Act 1877, c. 416, s. 185. Previous to the Code of Civil Procedure the provision for waiver was not in the statute, 2 R. S., 406, s. 73.
The amendment of 1891 allowed an express waiver of information, except confidential communications and such facts as would tend to disgrace the memory of the patient, by his personal representatives, or if the validity of the last will and testament of the patient is in question, by the executor or executors named in said will. Law 1891, c. 381.
The amendment of 1892 added the surviving husband, widow, heir at law, any of the next of kin or any other party in interest, in case the validity of the last will and testament of the patient is in question. Law 1892, c. 514. The present law contains the same provisions. Act 1893, c. 295.
[287] Westover v. Ætna L. I. Co., 99 N. Y., 56; Loder v. Whelpley, 111 N. Y., 239; Alberti v. N. Y., L. E. & W. R. R. Co., 118 N. Y., 77. Staunton v. Parker, 19 Hun, 55, is thus overruled.
[288] See In matter of Freeman, 46 Hun, 548 (N. Y. Supr. Ct., G. T.,1887).
See Adrereno v. Mut. Res. F. L. I. Co. (U. S. C. C. Mich.), 34 Fed. Rep., 870.
[289] Alberti v. N. Y., L. E. & W. R. R. Co., 118 N. Y., 77.
[290] Masonic Mut. Ben. Assn. v. Beck, 77 Ind., 203.
[291] Fraser v. Jennison, 42 Mich., 206.
[292] Groll v. Tower, 85 Mo., 249.
[293] Thompson v. Ish, 99 Mo., 160, distinguishes the New York statute from the Missouri statute; but seems to misinterpret Heuston v. Simpson, 115 Ind., 62, which does not hold that representatives cannot waive, but that they can invoke protection.
[294] State v. Depoister, 25 Pac. Rep., 1000.
[295] Johnson v. Johnson, 14 Wend., 636; Babcock v. People, 15 Hun, 347; Valensin v. Valensin, 14 Pac. Rep., 87 (Supr. Ct. Cal., 1887); cf. In re Hannah, 11 N. Y. St. Rep., 807.
[296] Penn Mut. L. I. Co. v. Wiler, 100 Ind., 92; Allen v. Pub. Adm., 1 Bradf., 221; Edington v. Mut. L. I. Co., 67 N. Y., 185; see Westover v. Ætna L. I. Co., 99 N. Y., 56. Breisenmeister v. Supr. Lodge, etc., 45 N. W. Rep., 977 (Supr. Ct. Mich., 1890).
[297] Penn Mut. L. I. Co. v. Wiler, 100 Ind., 92.
[298] Harris v. Rupel, 14 Ind., 209. See also Carthage T. Co. v. Andrews. 1 N. E. Rep., 364.
[299] Morris v. Morris, 119 Ind., 341.
[300] Scripps v. Foster, 41 Mich., 742.
[301] Mason v. Libbey, 2 Abb. N. C., 137; Mott v. Consumers’ Ice Co., 2 Abb. N. C., 143.
[302] Territory v. Corbett, 3 Mont., 50.
[303] People v. Stout, 3 Park Cr. Rep., 670 (N. Y., Oy. and Ter., 1858).
[304] Johnson v. Johnson, 14 Wend., 636 (overruling s. c., 4 Paige, 460); Breisenmeister v. Supreme Lodge, etc., 45 N. W. Rep., 977 (Supr. Ct. Mich., 1890).
[305] Valensin v. Valensin, 14 Pac. Rep., 87 (Supr. Ct. Cal., 1887).
[306] N. Y. Code Civ. Pro., s. 2, 618.
[307] Hoyt v. Hoyt, 9 N. Y. St. Rep., 731 (N. Y. Supr. Ct., G. T.), affirmed 112 N. Y., 493.
[308] Hoyt v. Hoyt, 9 N. Y. St. Rep., 731 (N. Y. Supr. Ct., G. T.).
[309] Van Valkenburg v. Van Valkenburg, 90 Ind., 433.
[310] Dilleber v. Home L. I. Co., 69 N. Y., 256.
[311] Loder v. Whelpley, 111 N. Y., 29.
[312] Supra, p. 96.
[313] Valensin v. Valensin, 14 Pac. Rep., 87 (Supr. Ct. Cal., 1887).
[314] Masonic Mut. Ben. Assn. v. Beck, 77 Ind., 203.
[315] Dreier v. Continental L. I. Co., 24 Fed. Rep., 670; cf. Breisenmeister v. Supr. Lodge, etc., 45 N. W. Rep., 977 (Supr. Ct. Mich., 1890).
[316] Penn Mut. L. I. Co. v. Wiler, 100 Ind., 92.
[317] Williams v. Johnson, 112 Ind., 273.
[318] Ætna L. I. Co. v. Denning, 123 Ind., 390.
[319] Lane v. Boicourt, 27 N. E. Rep., 1111.
[320] McConnell v. City of Osage, 45 N. W. Rep., 550.
[321] Campau v. North, 39 Mich., 606.
[322] Dolton v. Albion, 24 N. W. Rep., 786.
[323] Carrington v. St. Louis, 89 Mo., 208; Squires v. Chillicothe, 89 Mo., 226; Thompson v. Ish, 99 Mo., 160.
[324] Mellor v. Mo. Pac. Ry. Co., 14 S. W. Rep., 758; 16 S. W. Rep., 849.
[325] Adrereno v. Mut. Res. F. L. I. Co., 34 Fed. Rep., 870.
[326] State v. Depoister, 25 Pac. Rep., 1000; but see dissenting opinion of Bigelow, J.; see also McKinney v. Grand St. R. R. Co., 104 N. Y., 352.
[327] Edington v. Mut. L. I. Co., 5 Hun, 1 (reversed in part by Edington v. Mut. L. I. Co., 67 N. Y., 185, but affirmed on this point).
[328] Cahen v. Continental L. I. Co., 41 N. Y. Super., 296 (overruled on another point but affirmed on this in 69 N. Y., 300).
[329] Jones v. Brooklyn, B. & W. E. Ry. Co., 3 N. Y. Supp., 253.
[330] Grattan v. Metrop. L. I. Co., 92 N. Y., 274.
[331] McKinney v. Grand St. R. R. Co., 104 N. Y., 352; see criticism of this case in Breisenmeister v. Supr. Lodge, 45 N. W. Rep., 977 (Supr. Ct. of Mich., 1890). See also Mason v. Libbey, 2 Abb. N. C., 137; see unanswered queries on similar points in People v. Schuyler, 106 N. Y., 298.
[332] See In re Freeman, 46 Hun, 458, in which a will was admitted to probate on the concurrence of Learned, J., who held that the relation of physician and surgeon was not established, and Landon, J., who held that the request to sign constituted a waiver; Williams, J., dissenting, on the ground that the relation was established in the case, and the waiver could not be assumed without proof of the patient’s mental capacity to comprehend the waiver; that it was not proper to assume testator’s competency to waive in order to enable the witness to testify that the patient was competent to make a will.
On the analogous case of an attorney as witness to a will, see Matter of Coleman. 111 N. Y., 220; and N. Y. Code Civ. Pro., s. 836, as amended Act 1893, c. 295.
[333] Record v. Village of Saratoga Springs, 46 Hun, 448 (Supr. Ct., Gen. T., N. Y.). See also Hope v. Troy and Lansingburg R. R. Co., 40 Hun, 438; Jones v. B., B. & W. E. R. R. Co., 3 N. Y. Supp., 253.
[334] Supra, p. 113, note 7.
[335] 28 Abb. N. C., 37 (N. Y. Com. Pl., Gen. T., 1891).
[336] Marx v. Manhattan Ry. Co., 56 Hun, 575 (N. Y. Supr. Ct., Gen. T.).
[337] Buffalo L. & T. Co. v. Masonic Mut. Aid Assn., 126 N. Y., 450.
[338] Supra, p. 98.
[339] Collins v. Mack, 31 Ark., 684. The main point of this decision was that the information was not necessary; see infra. p. 124.
[340] v. Briggs, 20 Mich., 34.
[341] Ibid.
[342] Fraser v. Jennison, 42 Mich., 206; Breisenmeister v. Supr. Lodge, etc., 45 N. W. Rep., 977 (Supr. Ct. Mich., 1890).
[343] Dalman v. Koning, 54 Mich., 321.
[344] Brown v. Mut. L. I. Co., 65 Mich., 306.
[345] Breisenmeister v. Supr. Lodge, etc., 45 N. W. Rep., 977.
[346] Cooley v. Foltz, 48 N. W. Rep., 176.
[347] Lunz v. Mass. Mut. L. I. Co., 8 Mo. App., 363; Gartside v. Conn. Mut. L. I. Co., 76 Mo., 446 (said to be overruled by 85 Mo., 249; see 89 Mo., 226, but followed in Thompson v. Ish, 99 Mo., 160). For an argument on the distinction between information and communications, see brief of respondent’s counsel in Gartside v. Conn. Mut. L. I. Co.
[348] 27 Mo. App., 231 (1887).
[349] Streeter v. City of Breckenridge, 23 Mo. App., 244.
[350] Ibid.
[351] Corbett v. St. L., I. M. & S. Ry. Co., 26 Mo. App., 621.
[352] Thompson v. Ish, 99 Mo., 160.
[353] People v. Stout, 3 Park Cr. Rep., 670.
[354] Edington v. Mut. L. I. Co., 5 Hun, 1; s. p., 67 N. Y., 185; Grattan v. Met. L. I. Co., 80 N. Y., 281.
[355] Grattan v. Met. L. I. Co., 80 N. Y., 281; Van Orman v. Van Orman, 34 N. Y. St. Rep., 824 (Supr. Ct., G. T.); Wilcox v. Wilcox, 46 Hun, 32.
[356] Sloan v. N. Y. C. R. R. Co., 45 N. Y., 125; Dilleber v. Home L. I. Co., 69 N. Y., 256.
[357] Cahen v. Continental L. I. Co., 69 N. Y., 300.
[358] 77 N. Y., 564.
[359] See also Staunton v. Parker, 19 Hun, 55.
[360] 103 N. Y., 573; see also Grattan v. Met. L. I. Co., 80 N. Y., 281.
[361] Grattan v. Nat. L. I. Co. of U. S., 15 Hun, 74; Edington v. Mut. L. I. Co., 5 Hun, 1; see s. c., 67 N. Y., 185.
[362] Per Smith, J., in Steele v. Ward, 30 Hun, 555.
[363] People v. Brower, 53 Hun, 217.
[364] People v. Harris, 136 N. Y., 423.
[365] Burley v. Barnhard, 9 N. Y. St. Rep., 587 (Supr. Ct., G. T., 1887).
[366] Pandjiris v. McQuillen, 37 N. Y. St. Rep., 602 (Supr. Ct., G. T., 1891).
[367] Hoyt v. Hoyt, 9 N. Y. St. Rep., 731 (Supr. Ct., G. T., 1887).
[368] Hoyt v. Hoyt, ibid.
[369] In matter of Boury, 8 N. Y. St. Rep., 809 (Supr. Ct., G. T., 1889).
[370] Brown v. R. W. & O. R. R. Co., 45 Hun, 439.
[371] Numirich v. Supr. Lodge K. & L. of H., 3 N. Y. Supp., 552 (Trial Term, City Ct. of N. Y., 1889); Patten v. U. L. & A. Ins. Assn., 133 N. Y., 450.
[372] Patten v. United L. & A. Ins. Assn., 133 N. Y., 450.
[373] In matter of Darragh, 15 N. Y. St. Rep., 452 (N. Y. Surr.).
[374] In matter of Darragh, 52 Hun, 591 (Supr. Ct., G. T.), see infra, p. 128.
[375] Masonic Mut. Ben. Assn. v. Beck, 77 Ind., 203.
[376] Heuston v. Simpson, 115 Ind., 62; Penna. Co. v. Marion, 23 N. E. Rep., 973.
[377] Guptill v. Verback, 58 Iowa, 98.
[378] Guptill v. Verback, 58 Iowa, 98.
[379] McConnell v. City of Osage, 45 N. W. Rep., 550.
[380] Raymond v. Burlington, C. R. & N. Ry. Co., 65 Iowa, 152.
[381] Ibid.
[382] See argument in Edington v. Mut. L. I. Co., 67 N. Y., 185. See argument for difference between information and communications in brief for respondent, Gartside v. Conn. Mut. L. I. Co., 76 Mo., 446.
[383] Supra, p. 115.
[384] Act of Congress, May 2d, 1890, c. 182.
[385] Collins v. Mack, 31 Ark., 684.
[386] Cahen v. Continental L. I. Co., 69 N. Y., 300; see Grattan v. Met. L. I. Co., 24 Hun, 43.
[387] Hoyt v. Hoyt, 112 N. Y., 493.
[388] Freel v. Market St. Cable Ry. Co., 31 Pac. Rep., 730.
[389] People v. Glover, 71 Mich., 303.
[390] Per Learned, J., In matter of Freeman, 46 Hun, 458 (Supr. Ct., Gen. T., 1887).
[391] Renihan v. Dennin, 103 N. Y., 573; and cases in notes following.
[392] People v. Stout, 3 Park Cr. Rep., 670 (N. Y. Oy. and Ter., 1858); see Grossman v. Supreme Lodge, etc., 6 N. Y. Supp., 821 (Gen. T. Supr. Ct., 1889), visiting physician at a hospital attending out of curiosity with regular physician.
[393] People v. Schuyler. 106 N. Y., 298, affirming 43 Hun, 88.
[394] In matter of Baird, 11 N. Y. St. Rep., 263 (N. Y. Supr. Ct., Chambers, 1887, per Donohue, J.).
[395] See 28 Abb. N. C., 55. note.
[396] Grattan v. Met. L. I. Co., 24 Hun, 43 (Supr. Ct., Gen. T., 1881); 92 N. Y., 274.
[397] People v. Murphy, 101 N. Y., 126.
[398] People v. Kemmler, 119 N. Y., 580; People v. Sliney, 137 N. Y., 570.
[399] Heath v. Broadway & S. A. Ry. Co., 8 N. Y. Supp., 863 (Super. Ct., Gen. T., 1890).
[400] Henry v. N. Y., L. E. & W. R. R. Co., 57 Hun, 76 (Supr. Ct., Gen. T., 1890).
[401] Renihan v. Dennin, 103 N. Y., 573; Jones v. B., B. & W. E. Ry. Co., 3 N. Y. Supp., 253.
[402] Ætna L. I. Co. v. Deming, 123 Ind., 390; Raymond v. B., C. R. & N. Ry. Co., 65 Iowa, 152.
[403] Grattan v. Metr. L. I. Co., 24 Hun, 43 (Supr. Ct., Gen. T., 1881).
[404] Edington v. Ætna L. I. Co., 13 Hun, 543 (Supr. Ct., Gen. T., 1878), affirmed 77 N. Y., 564. The broad expressions of this latter case were disapproved in Renihan v. Dennin, 103 N. Y., 573, but it does not appear that this point was not properly decided.
[405] In matter of Darragh, 52 Hun, 591 (Supr. Ct., Gen. T., 1889), 15 N. Y. St. Rep., 452 (N. Y. Surr.) Brigham v. Gott, 3 N. Y. Supp., 518 (Supr. Ct., Gen. T., 1889).
[406] Stowell v. American Co-op. Assn., 23 N. Y. St. Rep., 706 (Supr. Ct., Gen. T., 1889).
[407] Supra, p. 98.
[408] 8 Mo. App., 363.
[409] 27 Mo. App., 231.
[410] Gartside v. Conn. Mut. L. I. Co., 76 Mo., 446; see also Burley v. Barnhard, 9 N. Y. St. Rep., 587 (N. Y. Supr. Ct., Gen. T.).
[411] Grattan v. Metr. L. I. Co., 92 N. Y., 274.
[412] Fisher v. Fisher, 129 N. Y., 654.
[413] Grattan v. Metr. L. I. Co., 24 Hun, 43 (Supr. Ct., Gen. T., 1881).
[414] Per Learned, J., In matter of Freeman, 46 Hun, 458.
[415] Supra, p. 98.
[416] Collins v. Mack, 31 Ark., 684.
[417] Raymond v. B., C. R. & Nor. Ry. Co., 65 Iowa, 152.
[418] Campau v. North, 39 Mich., 606.
[419] Brown v. Metr. L. I. Co., 65 Mich., 306.
[420] People v. Glover, 71 Mich., 303.
[421] Breisenmeister v. Supr. Lodge, etc., 45 N. W. Rep., 977 (Supr. Ct. Mich., 1890).
[422] Jacobs v. Cross, 19 Minn., 523.
[423] Norton v. City of Moberly, 18 Mo. App., 457.
[424] Streeter v. City of Breckenridge, 23 Mo. App., 244.
[425] Kling v. City of Kansas, 27 Mo. App., 231.
[426] Hewitt v. Prime, 21 Wend., 77 (N. Y. Supr. Ct. of Judic., 1839). See Edington v. Mut. L. I. Co., 67 N.Y., 185.
[427] 53 Hun, 217 (Supr. Ct., Gen. T., 1889).
[428] Sloan v. N. Y. C. R. R. Co., 45 N. Y., 125.
[429] Edington v. Mut. L. I. Co., 67 N. Y., 185. See also People v. Stout, 3 Park Cr. Rep., 670 (N. Y. Oy. and Ter., 1858).
[430] People v. Harris, 136 N. Y., 423.
[431] Babcock v. People, 15 Hun, 347; see also People v. Harris, supra.
[432] 77 N. Y., 564; see also s. p., 17 W. D., 566.
[433] 80 N. Y., 281.
[434] 80 N. Y., 281.
[435] Jones v. Brooklyn, Bath and West End Ry. Co., 3 N.Y. Supp., 253 (City Ct. of Brooklyn, Gen. T., 1888).
[436] Grattan v. Metr. L. I. Co., 24 Hun, 43 (Supr. Ct., Gen. T., 1881).
[437] In matter of Freeman, 46 Hun, 458.
[438] People v. Schuyler, 43 Hun, 88, affirmed 106 N. Y., 298.
[439] 9 N. Y. St. Rep., 31 (Supr. Ct., Gen. T.), affirmed 112 N. Y., 493. Although this point was discussed, the case was really decided on the ground that the objector had lost her right to object if she ever had it.
[440] Brown v. R. W. & O. R. R. Co., 45 Hun, 439 (Supr. Ct., Gen. T.).
[441] In matter of O’Neil, 26 N. Y. St. Rep., 242 (N. Y. Surr., 1889).
[442] Taylor, Ev., s. 2; Greenleaf, Ev., s. 2.
[443] McConnell v. City of Osage, 45 N. W. Rep., 550.
[444] Harris v. Rupel, 14 Ind., 209.
[445] Van Valkenberg v. Van Valkenberg, 90 Ind., 433.
[446] Storrs v. Scougale, 48 Mich., 387; see also Dolton v. Albion, 24 N. W. Rep., 786.
[447] Page v. Page, 41 Mich., 88; see also McQuigan v. D. & L. R. R. Co., 129 N. Y., 50; Roberts v. Ogdensburgh, etc., Ry. Co., 29 Hun, 158; McSwyny v. Broadway & S. A. Ry. Co., 7 N. Y. Supp., 459; and cf. N. Y. Code Civ. Pro., s. 873, as amended Act 1893, c. 722.
[448] Winner v. Lathrop, 67 Hun, 511.
[449] Lunz v. Mass. Mut. L. I. Co., 8 Mo. App., 363.
[450] Johnson v. Johnson, 4 Paige, 460 (Chancery, 1834); see also Hanford v. Hanford, 3 Edw. Ch., 468 (Vice Chan., 1841).
[451] 14 Wend., 636 (Ct. of Errors, 1835).
[452] 112 N. Y., 493.
[453] Edington v. Ætna L. I. Co., 17 W. D., 1883 (N. Y. Supr. Ct., Gen. T.); Hoyt v. Hoyt, 9 N. Y. St. Rep., 731 (Supr. Ct., Gen. T.), affirmed 112 N. Y., 493.
[454] Johnson v. Johnson, 14 Wend., 636; Babcock v. People, 15 Hun, 347; Valensin v. Valensin, 14 Pac. Rep., 87 (Supr. Ct. Cal., 1887).
[455] Kelly v. Levy, 8 N. Y. Supp., 849 (G. T. N. Y. City Ct., 1890).
[456] Mott v. Consumers’ Ice Co., 2 Abb. N. C., 143 (N. Y. Com. Pl., Sp. T., 1877).
[457] Edington v. Mut. L. I. Co., 5 Hun, 1; Renihan v. Dennin, 103 N. Y., 573; Record v. Village of Saratoga Springs, 46 Hun, 448; Loder v. Whelpley, 111 N. Y., 239.
[458] Supra, p. 101 et seq.
[459] Supra, p. 101 et seq.
[460] Supra, p. 107.
[461] Grattan v. Nat. L. I. Co. of U. S., 15 Hun, 74.
[462] Buffalo L. T. & S. D. Co. v. Knights T. & M. M. Aid Assn., 126 N. Y., 450.
[463] Edington v. Ætna L. I. Co., 13 Hun, 543; see Grattan v. Nat. L. I. Co. of U. S., 15 Hun, 74.
[464] McConnell v. City of Osage, 45 N. W. Rep., 550.
[465] Cooley v. Foltz, 48 N. W. Rep., 176.
[466] People v. Schuyler, 43 Hun, 88 (N. Y. Supr. Ct., Gen. T.), affirmed 106 N. Y., 298; Stowell v. American Co-operative Assn., 23 N. Y. St. Rep., 706 (N. Y. Supr. Ct., Gen. T.); Henry v. N. Y., L. E. & W. R. R. Co., 57 Hun, 76 (N. Y. Supr. Ct., Gen. T.); Edington v. Ætna L. I. Co., 77 N. Y., 564; Gartside v. Conn. Mut. L. I. Co., 8 Mo. App., 592.
[467] Gartside v. Conn. Mut. L. I. Co., 8 Mo. App., 592.
[468] Feeny v. Long Island R. R. Co., 116 N. Y., 375.
[469] Numirich v. Supr. Lodge K. & L. of H., 3 N. Y. Supp., 552 (Trial Term, City Ct. of N. Y., 1889); see also supra, p. 115.
[470] Herrington v. Winn, 60 Hun, 235 (Supr. Ct., Gen. T., 1891).
[471] In matter of Halsey, 29 N. Y. St. Rep., 533 (N. Y. Surr., 1890); cf. Matter of Darragh, 52 Hun, 591.
[472] Patten v. United L. & A. Ins. Assn., 133 N. Y., 450.
[473] Brigham v. Gott, 3 N. Y. Supp., 518 (Supr. Ct., Gen. T., 1889); supra, p. 124.
[474] Buffalo L. T. & S. D. Co. v. K. T. & Mas. Mut. Aid Assn., 126 N. Y., 450.
[475] Harris v. Rupel, 14 Ind., 209; Sullings v. Shakespeare, 46 Mich., 408; Storrs v. Scougale, 48 Mich., 387; Buffalo, etc., Co. v. Knights T. & Mas. Mut. Aid Assn., 126 N. Y., 450.
[476] Coryell v. Stone, 62 Ind., 307; People v. Schuyler, 43 Hun, 88, affirmed 106 N. Y., 298.
[477] Supra, p. 123.
[478] Supra, p. 119.
[479] Penn Mut. L. I. Co. v. Wiler, 100 Ind., 92. Valensin v. Valensin, 14 Pac. Rep., 87 (Supr. Ct. Cal., 1887); cf. In re Hannah, 11 N. Y. St. Rep., 807.
[480] Mason v. Libbey, 2 Abb. N. C., 137; Mott v. Consumers’ Ice Co., 2 Abb. N. C., 143.
[481] Lane v. Boicourt, 27 N. E. Rep., 1111; see also Winner v. Lathrop, 67 Hun, 511 (N. Y. Supr. Ct., G. T.).
[482] Scripps v. Foster, 41 Mich., 742.
[483] Grattan v. Metr. L. I. Co., 80 N. Y., 281.
[484] See p. 137, this volume, for the medical laws of the several States and Territories; for history of physician’s right of action for services, see Graham v. Gautier, 21 Tex., 117; see Wood v. Munson, 70 Hun, 468. In Georgia and Alabama a physician’s books are evidence in such actions. Code Ala., 1886, s. 2,777; Code Ga., 1882, s. 3,777.
[485] Kendall v. Grey, 2 Hilt., 300.
[486] Kling v. City of Kansas, 27 Mo. App., 231; Pierson v. People, 79 N. Y., 424.
[487] Supra, p. 103. Matter of Coleman, 111 N. Y., 220.
[488] Supra, p. 103.
[489] Supra, p. 104.
[490] Supra, p. 127.
[491] Laws of N. Y., Act 1893, c. 661, secs. 23, 31. In New York physicians are also required to attest certificates of the fact of birth for registration (Act 1893, c. 661, secs. 22, 31), and to certify the existence of contagious and infectious diseases (ib., s. 24).
[492] See suggestions on the policy of the New York law in Conn. Mut. L. I. Co. v. Union Tr. Co., 112 U. S., 250; Pearsall v. Elmer, 5 Redf., 181; and contra, Edington v. Mut. L. I. Co., 5 Hun, 1.
[493] A valuable note is appended to this last case, citing the law literature of burial-grounds, burials, etc., and also giving in full the opinion of the Special Term of the New York Supreme Court, in the case of Secord v. Secord, not elsewhere reported. And see also The Law of Burial, 4 Bradf., 503. (Matter of Beekman St.)
[494] Ambrose v. Kerreson, 10 C. B., 776; Bradshaw v. Beard, 12 Com. B., n. s., 344; Johnson v. Marinus, 18 Abb. N. C., 72; Hewitt v. Bronson, 5 Daily, 1; Cunningham v. Reardon, 98 Mass., 538.
[495] In New York State, section 305 of the Penal Code provides: “A person has the right to direct the manner in which his body shall be disposed of after his death; and also to direct the manner in which any part of his body, which had become separated therefrom during his lifetime, shall be disposed of; and the provisions of this chapter do not apply to any case where a person has given directions for the disposal of his body or any part thereof inconsistent with those provisions.” See also Patterson v. Patterson, 59 N.Y., 583; Me. R. S., ch. 13, sec. 1; Minn. Gen. Stats., sec. 6,220; N. D. Comp. Laws. sec. 6,549; Oklahoma Stats., sec. 2,188. See also Williams v. Williams, Law Rpts., 20 Ch. D., 659; 2 Wms. on Exrs., p. 968; Secord v. Secord, supra.
[496] Chappel v. Cooper, 13 M. & W., 252.
[497] Secord v. Secord, supra; Wyncoop v. Wyncoop, 42 Pa. St., 293; Bogert v. Indianapolis, 13 Ind., 135; Snyder v. Snyder, 60 How. Prac., 368; Law of Burial, 4 Bradf., 503.
[498] 1 Bishop Crim. Law, sec. 506; see also Roscoe’s Cr. Ev., 445, 446; Stephens’ Dig. Crim. L., sec. 292; Reg. v. Clark, 15 Cox C. C., 171.
[499] Some of the United States have enacted statutes declaring it to be a misdemeanor to attach or seize under execution a dead body. Arizona Pen. Code, 491, etc.; Cal. Pen. Code, sec. 295; Me. R. S., chap. 124, sec. 26; Mass. Pub. Stat., chap. 207, sec. 46; N. Dak. Comp. Laws, sec. 6,563; Oklahoma Stat., sec. 2,202; R. I. Pub. Stat., sec. 3,222.
[500] So in Meagher v. Driscoll, 96 Am. Dec., 759, it was held that a dead body is not the subject of property, and after burial it becomes a part of the ground to which it has been committed; “Earth to earth, ashes to ashes, dust to dust.”
[501] 1st Pres. Ch. v. 2d Pres. Ch., 2 Brewster, 372; and see also Pierce v. Proprietors Swan Point Cem., supra.
[502] Craig. v. 1st Pres. Ch., 88 Pa. St., 42; Charleston v. Wentworth Cem., 4 Strob. (S. Car.), 306; Coates v. New York City, 7 Cow., 585; Hamilton v. New Albany, 30 Ind., 482; Paige v. Symonds, 63 N. H., 17.
[503] Peters v. Peters, 43 N. J. Eq., 140; Lowry v. Plitt, 11 Phila., 303; Weld v. Walker, supra; In re Downs, 14 N. Y. St. Rep., 189; Morland v. Richardson, 22 Beav., 596; s.c. 24 id., 33; Guthrie v. Weaver, 1 Mo. App., 136; 4 Step. Com., 371; Reg. v. Theiss, 10 B. & S., 298.
[504] Weld v. Walker, supra; see also Johnson v. Marinus, supra.
[505] See also Com. v. Slack, 19 Pick., 304; People v. Fitzgerald, 105 N. Y., 146; People v. Richards, 138 N. Y., 137. In this last case it was held that a tomb, although constructed in the form of an elaborate mausoleum and built above the surface of the ground, was not a “building, erection or enclosure,” within the meaning of the criminal statutes defining the crime of burglary in entering a “building, erection or enclosure;” and hence that entering such a tomb and taking therefrom a dead body with its grave-clothes and cerements would not amount to the crime of burglary.
[506] County of Northampton v. Innes, 2 Carey (Pa.), 156; Com. v. Hannan, 4 Barr. (Pa.), 269; Alleg. Co. v. Watts, 3 Barr. (Pa.), 468; Van Hovenbergh v. Hasbrouck, 45 Barb. (N. Y.), 197; Cosford v. Board Supervisors, 38 N. Y. St. Rep., 964; Co. of Alleg. v. Shaw, 34 Pa. St., 301; Board of Com. v. Jameson, 86 Ind., 154; Mo. Rev. Laws, sec. 2,469; No. Car. Laws, 1887, chap. 269; Tenn. Code, sec. 6,150; N. Y. Laws of 1874, chap. 535, sec. 2; N. Y. Laws, 1889, chap. 500, amending sec. 308 of The Pen. Code.
[507] Am. & Eng. Enc. of Law, vol. 4, p. 171.
[508] 4 Co., 57; 3 Com. Dig., 242.
[509] 1 Black. Com., 347.
[510] Am. & Eng. Enc. of Law, vol. 4, p. 173.
[511] Giles v. Brown, 1 Mill (S. C.) Const., 230; People v. Devine, 44 Cal., 452.
[512] Bouvier’s Law Dict., vol. 1, p. 405.
[513] Lancaster County v. Dern, 2 Grant (Pa.), 262. In this case a concussion or collision took place in a street between the sleighs of two parties, whereby a woman sustained an injury by the shaft, or some other part of one of the parties’ sleigh, striking her immediately above the eye, and penetrating the brain. Surgical aid was immediately called in, and the woman received all the care and attention that the exigencies of the case required till five days afterward, when she died in consequence of the wound received. On the sixth day the coroner held an inquest, and in this, an action to recover for his services against the county, it was held he could recover.
[514] County of Lancaster v. Mishler, 100 Pa. St., 624. In this, a suit by the coroner against the county to recover his fees, it was held that this presumption was not conclusive, and evidence was admissible to show that he acted in bad faith and knowingly without sufficient cause or reason. The Court said: “The duty of a coroner to hold an inquest rests on sound reason, on that reason which is the life of the law. It is not a power to be exercised capriciously and arbitrarily against all reason. The object of an inquest is to seek information, and obtain and secure evidence, in case of death by violence or other undue means. If there be reasonable ground to suspect it was so caused, it becomes the duty of the coroner to act. If he has no grounds for suspecting that the death was not a natural one, it is a perversion of the whole spirit of the law to compel the county to pay for such services.”
[515] County of Fayette v. Batton, 108 Pa. St., 591. It appeared in this case, that nineteen persons came to their death suddenly and almost simultaneously by an explosion of fire-damp in a coal-mine. The coroner held a separate inquest over each body at the respective homes of the deceased, qualifying the same jury separately over each body, and the inquest returned a separate finding in each case. It was held that this was the necessary and proper course to pursue under the circumstances, and that the coroner was entitled to the legal fees in each case. In Boislinieu v. Board of Co. Commissioners, 32 Mo., 375, it was held that the coroner is the sole judge as to the propriety or necessity of holding the inquest, and his action in that respect is not subject to revision by the county commissioners, and he is entitled to fees under the statute notwithstanding the verdict of the coroner’s jury discloses that the deceased died of a natural death, and not by casualty or violence.
[516] Am. & Eng. Enc. of Law, vol. 4, p. 175.
[517] Garnett v. Ferrand, 6 Barn. & Cress., 611.
[518] People v. Fitzgerald, 43 Hun (N. Y.), 46.
[519] People v. Devine, 44 Cal., 452; Commonwealth v. Hawkins, 3 Gray (Mass.), 463.
[520] People v. Fitzgerald, 105 N. Y., 146.
[521] Jameson v. Board of Comrs., 64 Ind., 524.
[522] Regina v. White, 3 Ellis & Ellis (Eng.), 137. In this case a second inquisition found by a coroner’s jury was quashed by the court upon application of the defendants who were charged therein with wilful murder. In People v. Budge, 4 Park Crim. Rep. (N.Y.), 519, a coroner’s jury found that the death was caused by suicide, and nearly four months afterward the coroner summoned another jury and held a second inquest, at which the jury found that the deceased was killed by another, whereupon the coroner issued a warrant of commitment under which the accused was imprisoned, but on habeas corpus he was discharged from imprisonment on the ground that the second inquisition was unauthorized.
[523] The King v. Ferrand, 3 Barn. & Ald. (Eng.), 260; 2 Hawk P. C., 77.
[524] Mass. Pub. Stat., chap. 26, §§ 1 and 10.
[525] County of Northampton v. Innes, 2 Casey (Pa.), 156; Commonwealth v. Hannan, 4 Barr (Pa.), 269.
[526] Allegany County v. Watts, 3 Barr (Pa.), 462; Van Hoevenbergh v. Hasbrouck, 45 Barb. (N. Y.), 197. The New York legislature has made provision making the physician’s services in such a case a charge against the county and the physician must look to the county for his pay. Cosford v. Board of Supervisors, 38 N. Y. St. Rep., 964; 15 N. Y. Supp., 680. In Pennsylvania a physician or surgeon, employed by the coroner to make a post-mortem examination, may recover from the county a reasonable compensation for his services; and the county commissioners have no power to appoint a surgeon to perform such services, so as to preclude the coroner from selecting a proper person, in the exercise of his discretion. County of Allegany v. Shaw, 34 Pa. St., 301. It has been held that the authority of a coroner to employ a chemist to discover whether poison caused the death of one on whose body he holds an inquest does not restrict him to the employment of a resident of the county, and that the analysis of the chemist must not be made in the county of the coroner, and that even though the latter was, by corrupt appliances of others, induced to employ a chemist, it is no defence to a suit by the chemist to recover compensation for his services. Board of Commissioners v. Jameson, 86 Ind., 154.
In New York he is empowered by statute to employ not more than two competent surgeons to make post-mortem examinations and dissections and to testify to the same. N. Y. Laws of 1874, chap. 535, § 2.
[527] People v. Fitzgerald, 105 N. Y., 146. In this case, upon application of the defendant and upon affidavits showing sufficient reasons therefor, a coroner of Chemung County, N. Y., directed the exhumation of the body of a man, who died in California about one year previous and was buried in Chemung County; for the purpose of a post-mortem examination to determine whether the deceased was murdered, and the body was accordingly exhumed, and an examination had without empanelling a jury. An indictment was found against the defendant charging her with body-stealing under section 311 of the New York Penal Code, against body-stealing. It was held that conceding the proceeding to have been irregular, a conviction under that provision of the Penal Code could not be sustained, and this, without regard to the motives which actuated the defendant; that if she had committed any offence it was not that of body-stealing.
[528] Crisfield v. Perine, 15 Hun, 200, affirmed 81 N. Y., 622. This was an action of assault and battery and it appeared that the defendant was a coroner, and that he held an inquest on the dead body of a man who died after receiving personal injuries in an affray which he had with his nephew. A post-mortem examination was about to be made by two surgeons employed by the coroner for that purpose. The plaintiff, who was also a physician and surgeon, was in the room when the examination was about to be entered upon and said that he wished to remain and witness it, but the coroner asked him to leave, and on his refusing caused him to be put out of the room. For this act this suit was brought. It was held that the suit could not be maintained.
[529] Mass. Pub. Stat., chap 26, § 19.
[530] Ib., chap. 26, § 11.
[531] Commonwealth v. Dunan, 128 Mass., 422.
[532] Mass. Pub. Stat., chap. 26, §§ 12, 13, 17.
[533] Mass. Pub. Stat., chap. 26. § 18.
[534] N. Y. Criminal Code, § 773.
[535] N. Y. Revised Statutes, part iv., chap. iii., § 102.
[536] N. Y. Criminal Code, § 774.
[537] Ib., § 775.
[538] Ib., § 777.
[539] Ib., § 778.
[540] Ib., § 779.
[541] N. Y. Crim. Code, § 780.
[542] Ib., § 776.
[543] Ib., § 782.
[544] Ib., § 783.
[545] 2 Hawk P. C., 77; King v. Ferrand, 3 Barn. & A. (Eng.), 260.
[546] Rex v. Ferrand, 3 B. & Ald., 260.
[547] In re Coroners, 11 Phila. (Pa.), 387.
[548] Crisfield v. Perine, 15 Hun, 200, affirmed 81 N. Y., 622.
[549] 2 Hawk P. C., 77.
[550] Matter of Collins, 11 Abb. Pr. (N. Y.), 406; 20 How. Pr., 111. In this case it was held that a commitment issued by a coroner against a person charged with murder is not void for the omission of the allegation that he caused the death “feloniously,” if it is such that the fact that he caused the death feloniously may be collected on its face. And see People v. Beigler, 3 Park Crim. Rep. (N. Y.), 316.
[551] Rex v. Bowen, 6 Car. & P., 602; Rex v. Bennett, 6 Car. & P., 179.
[552] State v. Evans, 27 La. An., 297.
[553] Rex v. Nicholas, 7 Carr & Payne (Eng.), 538.
[554] People v. White, 22 Wend. (N. Y.), 167.
[555] Matter of Collins, 11 Abb. Pr. (N. Y.), 406; 20 How. Pr., 111.
[556] Matter of Ramscar, 10 Abb. N. C. (N. Y.), 442. The prisoner in this case was detained on a commitment issued by a coroner, he not having had an examination, and the Court directed an examination before a magistrate.
[557] N. Y. Code Crim. Pro., § 145.
[558] People v. Devine, 44 Cal., 452; Commonwealth v. Hawkins, 3 Gray (Mass.), 463.
[559] People v. Monden, 103 N. Y., 211.
[560] People v. Willett, 92 N. Y., 29. In this case upon the trial of an indictment for murder, evidence was received on the part of the prosecution, under objection and exception, to the effect that upon the coroner’s inquest a witness testified that shortly after the murder a stranger called at her house and asked the way to Sandy Hill, and also for a drink of water; that the prisoner with a number of others was placed around a room, and the witness pointed out the prisoner as the one who so called; also that a number of persons, including the prisoner passed behind her, each one repeating the question asked her by the stranger, and she identified the prisoner by his voice, and that the prisoner on that occasion did not Footnote: deny that he was such stranger. It was held that the prisoner was not bound to speak and his silence could not be regarded as an evidence of guilt, and that the evidence was improperly received. The Court said: “The question whether the defendant was bound to speak, and understood that he was at liberty to speak, if he chose, was submitted to the jury by the Court in his charge, and an exception taken thereto. The doctrine as to silence being taken as an implied admission of the truth of allegations spoken or uttered in the presence of a person, does not apply to silence at a judicial proceeding or hearing. And if the proceedings before the coroner were of a judicial character the evidence was erroneously received. It is very apparent that the examination before the coroner partook of a judicial character, and what then transpired must be considered as a part of the proceedings; the coroner was there, a jury had been empanelled, and witnesses were examined whose testimony was returned as a portion of the coroner’s proceedings. It is difficult to see upon what ground it can be claimed that the experiments which were made were not in connection with the proceedings before the coroner and a part thereof.”
[561] Hendrickson v. People, 10 N. Y., 13.
[562] People v. McMahon, 15 N. Y., 384.
[563] Teachout v. People, 41 N. Y., 7.
[564] People v. Mondon, 103 N. Y., 211.
[565] People v. McGloin, 91 N. Y., 241.
[566] Williams v. Commonwealth, 29 Pa. St., 102. In this case the prosecution was permitted to prove upon the trial that a justice of the peace had held an inquest on the body of a dead person, and appointed another person foreman of the inquest, and directed him to swear witnesses; and while the inquest was still sitting, the foreman called upon and requested the defendant to be sworn and give evidence as a witness, and he was duly sworn and was examined by the foreman, in presence of the inquest. It was held on appeal that his evidence was admissible. On this point the Court said: “If the defendant had been awakened out of sleep, charged with crime, and then, in the necessary confusion of his faculties sworn to testify, I should have steadfastly resisted the subsequent introduction of the testimony against him. The common law, which justifies an accused man in entire silence, appears in beautiful contrast to the continental systems, which permit the criminal to be racked by inquisitorial skill, until something be wrung from him which may be patched up into proof of guilt. This case shows nothing of the kind. The phrase ‘called up’ commented on by the counsel, does not appear in the record, and if employed by the witnesses related doubtless to the ordinary case of calling forth a witness, and not awakening him from slumber. When the defendant was sworn before the inquest, he had neither been charged with nor suspected of crime. He might have declined to testify, and this would have pointed suspicion directly to him. He took the risk of a statement, and cannot complain that he met the legitimate consequences of the act. In the eye of all the authorities, it was a voluntary statement.”
[567] Clough v. The State, 7 Neb., 320.
[568] The facts upon which the following statements are based have been largely drawn from Taylor. See Stevenson’s Taylor, vol. i., p. 204 et seq.
[569] Recent attention to such subjects by Italian writers places them in the foremost rank. Although their system of judicature differs from our own, this fact does not lessen the value of their medico-forensic literature.
[570] Canada Med. and Surg. Journal, 1875, vol. iii., pp. 56-60.
[571] Some interesting facts by Dr. W. H. Holmes regarding “The Condition of Bodies Long Buried” may be found in the Boston Med. and Surg. Journal, July 23d, 1891.
[572] Quar. Journal of Psychological Medicine, N. Y., 1869, vol. iii., p. 691.
[573] See writer’s article, “Cephalometry, Craniometry,” in “Reference Handbook of the Medical Sciences.”
[574] See writer’s “Cruise of the Corwin” to Alaska and the Northwest Arctic Ocean, Washington, 1883.
[575] See writer’s article, “Feet,” in “Reference Handbook of the Medical Sciences;” also, Ellis, T.S., “On the Human Foot,” London, 1889.
[576] See Dwight: “The Closure of the Cranial Sutures as a Sign of Age,” Boston Med. and Surg. Journal, April 29th, 1890.
[577] See Dwight: “The Sternum as an Index of Sex, Height, and Age,” Journal of Anatomy and Physiology, vol. xxiv.
[578] Boston Med. and Surg. Journal, March, 1850, vol. xii., p. 162.
[579] The British Medical Journal, April 18th, 1874, p. 527.
[580] Taylor’s “Med. Jurisprudence,” vol. i., p. 157.
[581] Theatre-goers are familiar with the establishment of personal identity by means of traces of a perfume in the play of “Diplomacy.”
[582] New York Med. Journal, vol. x., p. 412.
[583] New York Med. Record, August 18th, 1877.
[584] Annales d’Hygiene Publique, 1883.
[585] Med. Gazette, vol. xli., p. 650.
[586] In a series of papers to Riv. Sper. di freniat, Reggio-Emilia, 1883.
[587] See Mr. Galton’s paper in Nature, June 21st, 1888, p. 173; also in his recent work on Finger Prints.
[588] For a few classical citations that are more erudite than profitable see Zeitschrift für Ethnologie, Berlin., 1888, xx., p. 412.
[589] See “Guy’s Hospital Report,” xix., 1874; also “Histoire Médicale de Tatouage” in Archiv. de Médecine Navale, tom. 11, 12, Paris, 1869. A later study on the medico-legal importance of tattooing may be found in Lo Spallanzani, Roma, 1891, 2s, xx., 169, 208.
[590] According to Lombroso, all who are tattooed on the back or the sexual organs have without exception either been among the Pacific Islands or sojourned in a prison.
[591] A paper by Dr. J. N. Hall on “The Medico-Legal Value of Powder-Stains in Gunshot Wounds,” with a report of cases, may be found in the Transactions of the Colorado Medical Society, 1890, xx., 94.
[592] Bulletin de l’Acad. de Méd., 17 janvier, 1853, t. xviii., p. 348.
[593] La Escula de Medicina, Mexico, 1880-81.
[594] Lyon Medical, 1880.
[595] Med. Press and Circular, May 30th, 1888, p. 576.
[596] Phil. Trans., B., 1891.
[597] See Proc. Royal Soc., London, May 28th, 1891. A medico-legal study of imprints may also be found in Archiv d’Anthropologie Criminel, 15th July, 1891.
[598] See Annual of the Universal Medical Sciences, 1888, vol. v., pp. 143-147.
[599] See paragraph II., General Orders No. 33, Adjutant-General’s Office, April 1st, 1889.
[600] In 1892 only three failures are recorded.
[601] “Précis de Méd. Lég.,” 2d Ed., 1890.
[602] “Med. Jurisprud.,” 11th Amer. Ed., 1892.
[603] Arrêt du tribunal de Lyon, 8 et 15 décembre, 1859.
[604] “Lectures on Med. Jurisprud.,” 1878, pp. 422, 423.
[605] See Figs. 10 and 11.
[606] “Lehrbuch der Speciellen Chirurgie.”
[607] “Manuel de Leg.,” 5th Ed., 1892.
[608] “Précis de Med. Leg.,” 2d Ed., 1890.
[609] Taylor: “Medical Jurisprudence,” 11th American Edition (1892).
[610] Taylor: “Medical Jurisprudence,” 11th American Edition (1892).
[611] London Med. Gaz., vol. xvi., p. 596.
[612] Ch. Vibert: “Précis de Médecine Légale,” 2d Ed., p. 205.
[613] Taylor’s “Medical Jurisprudence,” 11th Amer. Ed., 1892.
[614] London Lancet, Jan. 21st, 1893, and N. Y. Med. Journal, March 11th, 1893, and May 13th, 1893.
[615] Ann. d’Hyg., 1847, t. 2, p. 377.
[616] Taylor: “Medical Jurisprudence,” 11th Amer. Ed., 1892.
[617] “Med. Jurisprud.,” 11th Amer. Ed., 1892.
[618] “On Homicide,” p. 187.
[619] Med. Gaz., May, 1840.
[620] Guy’s Hosp. Gaz., 1873.
[621] Vibert: “Précis de Médecine Légale,” 2d Ed., 1890.
[622] Vibert: “Précis de Médecine Légale,” 2d Ed., 1890.
[623] Vibert: “Précis de Médecine Légale,” 2d Ed., 1890.
[624] Vibert: “Précis de Médecine Légale,” 2d Ed., 1890.
[625] Quoted by Vibert from the “Traite de pathologie externe” of Follin and Duplay.
[626] “Med. Jurisprud.,” 11th Amer. Ed., 1892.
[627] “Med. Jurisprud.,” 11th Amer. Ed., 1892.
[628] “Med. Jurisprud.,” 11th Amer. Ed., 1892.
[629] Taylor: “Medical Jurisprudence,” 11th Amer. Ed., 1892.
[630] Taylor: “Medical Jurisprudence,” 11th Amer. Ed., 1892.
[631] Taylor: “Medical Jurisprudence,” 11th Amer. Ed., 1892.
[632] Taylor: “Medical Jurisprudence,” 11th Amer. Ed., 1892.
[633] Taylor: “Medical Jurisprudence,” 11th Amer. Ed., 1892.
[634] Med. Times, 1854, ii., p. 238.
[635] “Ueber die Kopf-Verletzungen,” 1842, p. 57.
[636] “Précis de Médecine Légale,” 2d Ed., 1890, p. 203.
[637] “Med. Jurisprud.,” 11th Amer. Ed., 1892.
[638] Taylor, “Med. Jurisprud.,” 11th Amer. Ed., 1892.
[639] Lutaud: “Man. d. Méd. Lég.,” 5th Ed., 1892.
[640] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[641] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[642] Taylor: “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[643] Willis: “Circumstantial Evidence,” p. 97.
[644] “Lectures on Med. Jurisprudence,” p. 424.
[645] See “Med. Leg.,” trad. par Brouardel, p. 601.
[646] “Med. Jurisprudence.” 11th Amer. Ed., 1892.
[647] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[648] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[649] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[650] Ann. d’Hyg., 1863, t. 1. p. 463.
[651] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[652] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[653] Vibert: “Précis de Méd. Lég.,” 2d Ed., 1890.
[654] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[655] “Précis de Méd. Lég.,” 2d Ed., 1890, p. 264.
[656] “Précis de Méd. Lég.,” 2d Ed., 1890.
[657] “Précis de Méd. Lég.,” 2d Ed., 1890, p. 246.
[658] “Précis de Méd. Lég.,” 2d Ed., 1890.
[659] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[660] “Med. Jurisprudence,” 11th Amer Ed., 1892, p. 334.
[661] London Lancet, 1873, i., p. 697.
[662] “An American Text-Book of Surgery,” p. 496.
[663] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[664] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[665] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[666] Edin. Med. and Surg. Jour., Oct., 1845, p. 527.
[667] “Manuel de Méd. Lég.,” 5th Ed., 1892.
[668] “Méd. Lég.,” t. 2, p. 243.
[669] Beck, vol. ii., pp. 329, 333; Wharton and Stillé, 2d Ed., p. 580; N. A. Med. and Chir. Review, March, 1859, p. 299; N. Y. Med. Times, Apr. and May, 1855; Amer. Jour. Med. Sciences, July, 1861, p. 292, and Aug., 1829, p. 307.
[670] Amer. Jour. Med. Sci., July, 1861, p. 292. Case of bullet in heart wall for twenty years.
[671] Edin. Med. and Surg. Jour., Oct., 1844, p. 557.
[672] “Méd. Lég.,” t. 2, p. 253.
[673] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[674] “Manuel Méd. Lég.,” 5th Ed., 1892.
[675] Quoted by Taylor, “Med. Jurisprudence,” 11th Amer. Ed., 1892, p. 340.
[676] “Med. Jurisprudence,” 11th Amer. Ed., 1892, p. 351.
[677] Senn, “Experimental Surgery,” 1889.
[678] Senn, “Experimental Surgery,” 1889.
[679] “Med. Jurisprudence,” 11th Amer. Ed., 1892.
[680] Med. Times and Gazette, 1864, ii., 527.
[681] Med.-Chir. Rev., 1836, p. 296.
[682] “Med Jurisprudence,” 11th Amer. Ed., 1892, p. 347.
[683] Lancet, 1872, ii., p. 10.
[684] Lancet, 1870, ii., p. 471.
[685] See Taylor, “Med. Jurisprudence,” 11th Amer. Ed., 1892, p. 348.
[686] “Med. Jurisprud.,” 11th Amer. Ed., 1892.
[687] See Taylor, “Med. Jurisprud.,” 11th Amer. Ed., 1892, p. 351.
[688] Reported by Teale, Lon. Clin. Society, Feb. 26th, 1875.
[689] Reineke, Brit. and For. Med. and Surg. Rev., April, 1876.
[690] “Experiences sur les effets de chaleur, etc.,” Jour. de Physique, lxiii., p. 77. Paris, 1805.
[691] Henke’s “Zeitschrift,” 1860.
[692] Brit. and For. Med.-Chir. Rev., 1855.
[693] Caspar’s “Vierteljahrschrift,” 1864.
[694] Flint, “Practice of Medicine,” p. 685; Aitken, “Practice of Medicine,” vol. ii., p. 388.
[695] Flint, “Practice of Medicine,” p. 685; Aitken, “Practice of Medicine,” vol. ii., p. 391.
[696] Levick, Amer. Jour. Med. Sciences, Oct., 1866.
[697] Katzenbach, New York Med. Jour., vol. xvii., p. 91.
[698] Wood, Phil. Med. Times, Aug. 5th, 1876.
[699] Hanfield Jones, Brit. Med. Jour., July, 1870, p. 35.
[700] Pouillet, Comptes Rendus, 1836, p. 782.
[701] Taylor, “Med. Jurisprudence,” 8th Amer. Ed., p. 444; also the Med. Gazette, vol. xviii., p. 89.
[702] Chambert, Annales d’Hygiene. 1859.
[703] Buchner, Prager Vierteljahr., i., p. 129.
[704] Tidy, “Legal Medicine,” vol. ii., p. 124.
[705] Taylor, “Med. Jurisprudence,” 8th Amer. Ed., p. 407.
[706] Tidy, “Legal Medicine,” vol. ii., p. 99.
[707] Caspar, “Forensic Medicine,” vol. i., p. 314; Schjerning, Vierteljahr. für gericht. Med., xli., 1884.
[708] The “Parkman Case,” Boston, 1850.
[709] Report of the “Druse Case,” Trans. New York State Med. Society, 1887, p. 417.
[710] See the Druse Case above.
[711] Annales d’Hygiene, 1835, ii., p. 387.
[712] Edinb. Med. and Surg. Journal, vol. xxxv., p. 320, April, 1831.
[713] Ann. d’Hygiene, 1846, i., p. 320.
[714] Friedrich’s Blatter f. gericht. Med., 1877, Heft iii., p. 210.
[715] “Path. Research, on Vital and Post-Mortem Burning,” 1850.
[716] “Forensic Medicine,” vol. iv., p. 299.
[717] “Forensic Medicine,” Ed. 1877, p. 886.
[718] “Med. Jurisprudence,” Amer. Ed., 1880. p. 408.
[719] Annales d’Hygiene, 1859, 2d ser., xi., 342, 379.
[720] Vierteljahr. f. gericht. Med., Bd. xxxvi., Heft i., 1880.
[721] Eulenb., Vierteljahr. f. gericht. Med., xli., 1885, xlii., 1887.
[722] Tidy, “Legal Med.,” vol. i., p. 108; also Buzzard, London Lancet, vol. i., p. 60, 1863.
[723] Eulenberg’s Vierteljahr. f. gericht. Med., xli., p. 44 et seq.
[724] “Die Verbrennungen und Verbrühungen.”
[725] Wien. med. Presse, 1868, pp. 309, 605.
[726] Berliner klinische Wochenschrift, 1876, No. 17; 1877, No. 46.
[727] Eulenberg’s Vierteljahr. f. gericht. Med., xlii., p. 47.
[728] See page 643 of this section
[729] Asclepiad, 1890, vii., pp. 102-117.
[730] Compt. Rendu Soc. Biol., 1890, ii., pp. 383-387.
[731] Archiv. Biol. de Gand., 1887, vii., pp. 217-227.
[732] “On the Value of Certain Signs,” etc., Edinburgh, 1873.
[733] “Lehrbuch gericht. Med.,” 1891, p. 502.
[734] Bull. Acad. Méd., 1876, v., p. 763.
[735] Archiv. gén. de Méd., 1856, p. 302.
[736] “Lehrb. d. ger. Med.,” 1891. p. 500.
[737] “Leçons sur les anæsthésiques,” Paris, 1875, p. 471.
[738] Viert. f. ger. Med., etc., 1871, xv., pp. 58-96.
[739] Translation in Ann. d’Hyg., 1832, viii., p. 432.
[740] Med. Record, N. Y., 1882, xxii., p. 427.
[741] See Maier (Friedreich’s Blat., 1882, p. 460); Moreaud (Virchow’s Archiv, 1880, i., p. 648); Petrina (Prag. med. Woch., 1880, No. 39); Wagner (Jahr. f. Psych., 1889, viii.). [Hofmann, “Lehrbuch,” pp. 570-572]. See Cases 17, 19, 31.
[742] Bull. Ac. Méd., 1876, v., p. 761.
[743] Ass. Franç. Av. Sci. (1883), 1884, xii., pp. 1042-1045.
[744] Rev. d’Hyg. thér., 1890, ii., pp. 67-72 and 131-137.
[745] Alger. Méd., 1887, xv., pp. 78-90.
[746] Viert. ger. and öff. Med., 1870, xii., pp. 340-369.
[747] Ann. d’Hyg., 1867, xxviii., pp. 388-402.
[748] Viert. f. ger. Med., etc., 1870, xiii., pp. 247-260.
[749] Loc. cit.
[750] “Med. Jur.,” Amer. ed., 1892, p. 411.
[751] Tidy, “Med. Jur.,” Amer. ed., 1884, iii., p. 263.
[752] Ann. d’Hyg., 1867, xxviii., p. 393.
[753] “Lehrb. d. ger. Med.,” 1891, p. 504.
[754] “Pendaison,” etc., 1870, p. 169.
[755] Op. cit., p. 393.
[756] Op. cit., p. 504.
[757] Op. cit., p. 394.
[758] “Handb. ger. Med.,” i., 1881, p. 569.
[759] Compt. rend. Soc. Biol. (1879), 1880, i., p. 310.
[760] Compt. rend. Soc. Biol. (1881), 1882, iii., pp. 159-161 and 165-168.
[761] Tidy, op. cit.
[762] “Med. Jur.,” Am. ed., 1892, p. 413.
[763] Lyon thesis, 1883, No. 188, p. 85.
[764] Tidy, op. cit.
[765] Gaz. Méd. de Par., 1875, xlvi., pp. 90-92.
[766] “Handb. ger. Med.,” i., p. 571.
[767] Tidy, op. cit.
[768] Tardieu, “Pendaison,” etc., p. 174.
[769] Virchow’s Archiv, 1880, lxxix., p. 409, and 1878, lxxiv., p. 401.
[770] Tidy, “Leg. Med.,” Am. ed., iii., p. 265.
[771] “Ger. Med.,” i., p. 623 and 632.
[772] Edinb. Med. Jour., 1856, ii., p. 824.
[773] “Med. Jur.,” Am. ed., 1892, p. 414.
[774] “Ger. Med.,” i., p. 632.
[775] Paris thesis, 1874, No. 291.
[776] Paris thesis, 1859, No. 9.
[777] Page, “On the Value of Certain Signs,” etc., Edinburgh, 1873.
[778] “Ger. Med.,” i., 573.
[779] Tardieu, “Pendaison,” etc., p. 178.
[780] Op. cit., p. 29.
[781] Vier. f. ger. Med., etc., 1867, vii., pp. 140-174.
[782] “Ger. Med.,” i., p. 576.
[783] Ib., p. 572.
[784] “Ger. Med.,” i., p. 575.
[785] “On the Value of Certain Signs,” etc., Edinburgh, 1873, p. 24.
[786] “Vier. f. ger. Med., etc., 1886, xlv., p. 295.
[787] “Leg. Med.,” Am. ed., iii., p. 267.
[788] “Med. Jur.,” Am. ed., 1892, p. 415.
[789] Ann. d’Hyg., 1867, xxviii., pp. 388-402.
[790] “Med. Jur.,” Am. ed., 1892, p. 416.
[791] Ib., p. 415.
[792] “Pend.,” p. 186.
[793] “Med. Jur.,” Am. ed., 1892, p. 415.
[794] Op. cit., p. 415.
[795] “Med. Jur.,” Am. ed., 1892. p. 419.
[796] “Pend.,” p. 208.
[797] Ib., p. 242.
[798] Med. Times and Gaz., 1871, i., p. 671, and 1876, i., p. 93.
[799] Med. Record, N. Y., 1882, xxii., p. 428.
[800] Ohio Med. Record, 1878, ii., pp. 350-352.
[801] Arch. Laryngol., N. Y., 1880, i., p. 144.
[802] Indian Med. Gaz., 1888, xxiii., p. 299.
[803] Archiv. anthrop. crim., Paris, 1886, i., p. 229.
[804] “Lehrbuch f. ger. Med.,” 5th ed., 1890-91.
[805] “Med. Jur.,” Am. Ed., 1892, p. 394.
[806] Aertz. Intel. Bl., 1876, xxiii., p. 324.
[807] Practitioner, 1870, iv., p. 193.
[808] Mitt. d. Wien med. Doct. Colleg., 1878, iv., pp. 97-112.
[809] Centralb. f. med. Wiss., 1875, xiii., p. 403.
[810] Arch. gen. de Med., 1856, vii., p. 310.
[811] Archiv. anthrop. crim., Paris, 1886, i., p. 229.
[812] Bull. Acad. Roy. Med., 1893, vii., pp. 331-342.
[813] Lyon thesis, 1883, No. 188.
[814] Paris thesis, 1879, No. 172. p. 39.
[815] “Forensic Med.,” Appendix, p. 561.
[816] “Med. Jur.,” Am. Ed., 1892, p. 394.
[817] Tidy, op. cit., p. 240.
[818] Tardieu, “Pendaison,” 1870, p. 16.
[819] Lyon thesis, 1891, No. 647.
[820] Münch. med. Woch., 1893, xl., pp. 87-91, 127-129, 194.
[821] Tracy, Pop. Sci. Mo., 1878, xiii., pp. 349-354.
[822] Lancet, 1847, i., p. 403.
[823] “Med. Jur.,” Am. Ed., 1892, p. 396.
[824] See articles of Huppert, Vier. ger. Med., etc., xxiv., pp. 237-252, and Müller-Beninga, Berlin. klin. Woch., 1877, xiv., p. 481.
[825] Jour. Amer. Med. Assn., 1885, i., p. 658.
[826] “Pend.,” etc., p. 22.
[827] Dorpat Diss., 1891.
[828] Arch. gén. de Méd., 1856, vii., p. 315.
[829] Op. cit., p. 308.
[830] Lancet, 1871, ii., p. 98.
[831] Glasgow Med. Jour., 1880, xiv., p. 387.
[832] Philadelphia Medical Times, 1875.
[833] Lancet, 1869, i., p. 636.
[834] Indian Med. Gaz., 1876, xi., p. 29.
[835] Op. cit., p. 245.
[836] “Med. Jur.,” Am. ed., 1892, p. 398.
[837] Op. cit., p. 523.
[838] Op. cit., Levy’s translation, 1881, p. 363.
[839] Deutsch. Archiv f. Staats, 1870, xxviii., p. 313.
[840] Op. cit., p. 281.
[841] Indian Med. Gaz., 1876, xi., p. 29.
[842] Op. cit., p. 287.
[843] “Med. Jur.,” p. 527.
[844] “Med. Jur.,” Am. ed., 1892, p. 399.
[845] Vier. f. ger. Med., 1870, xii., pp. 340-369.
[846] Ib., 1870, xiii., pp. 247-260.
[847] Op. cit., p. 281.
[848] Pellier, op. cit., p. 83.
[849] Ind. Med. Gaz., 1876, xi., p. 30.
[850] “Handbuch,” p. 571.
[851] Wien. med. Presse, 1881-1882, xxii., p. 1533.
[852] Vier. f. ger. Med., 1881, xxxv., p. 201.
[853] Lehrbuch, p. 532.
[854] Op. cit., p. 245.
[855] See Brit. and For. Med. Rev., ii., p. 214.
[856] Op. cit., p. 98.
[857] Paris thesis, 1859, No. 9.
[858] Paris thesis, 1874, No. 291.
[859] Op. cit., p. 245.
[860] Op. cit., p. 533.
[861] Med. Times and Gaz., 1871, i., p. 671.
[862] Lyon Méd., 1883, xliv., p. 11.
[863] Lehrbuch, p. 535.
[864] Vier. f. ger. Med. and öff. San., 1881, xxxv., pp. 201-248.
[865] Virchow’s Archiv, 1870, xlix., p. 290.
[866] Rev. Méd. de l’Est, 1890, xxii., pp. 545-554.
[867] Ann. d’Hyg., 1885, xiii., pp. 209-228.
[868] Op. cit., p. 105.
[869] Lehrbuch, p. 537.
[870] Op. cit., p. 607.
[871] Op. cit., p. 597.
[872] Op. cit., pp. 44, 54.
[873] Bull. Soc. Méd. Lég., Paris, 1875-76, iv., p. 373.
[874] Indian Med. Gaz., 1881, xvi., p. 275.
[875] Ann. d’Hyg., 1886, xvi., pp. 108-125.
[876] “Med. Jur.,” Am. ed., 1892, p. 408.
[877] Freidreich’s Bl. f. ger. Med., 1890, xxi., pp. 149-171.
[878] Vier. f. ger. Med., etc., 1880, xxxii., p. 232, foot-note.
[879] “Med. Jur.,” Am. ed., 1880, p. 448.
[880] Indian Med. Gaz., 1876, xi., p. 3.
[881] Op. cit., p. 132.
[882] Op. cit., p. 66.
[883] Amer. Jour. Obstet., 1886, xix., pp. 349-352.
[884] Tardieu., op. cit., p. 291.
[885] “Med. Jur.,” Am. ed., 1892, p. 428.
[886] Trans. Mass. Leg. Soc., 1878, i., pp. 14-24.
[887] See Ogston, p. 550.
[888] Med. Times and Gaz., 1878, i., p. 603.
[889] Johnson, Lancet, 1878, ii., p. 501.
[890] Med. chir. Trans., 1862, xlv., p. 449.
[891] Archiv. gén. de Méd., 1856, vii., p. 300.
[892] Op. cit., p. 539.
[893] “Amer. Pract.,” 1872, vi., pp. 193-206.
[894] Brit. Med. Jour., 1879, i., p. 970.
[895] “Nature,” 1879, xx., p. 108.
[896] Gaz. hebd. Méd., Paris, 1872, ix., p. 806.
[897] Bull. Acad. Méd., Paris, 1876, v., p. 764.
[898] Jour. Amer. Med. Ass., 1891, xvi., p. 805.
[899] Trans. Amer. Pæd. Soc., 1891, iii., pp. 128-132.
[900] Brit. Med. Jour., 1880, ii., pp. 122-124 and 163-165.
[901] Med. Rec., N. Y., 1893, xliii., p. 289.
[902] Amer. Jour. Med. Sci., 1891, ci., pp. 109-116.
[903] Coll. and Clin. Record, 1892, xiii., pp. 170-172.
[904] Glasgow Med. Jour., 1885, xxiv., pp. 344-354.
[905] Med. Press and Circ., 1889, xlviii., p. 433.
[906] Asclepiad, 1885, ii., pp. 171-187.
[907] Lancet, 1885, i., pp. 245-247, 289-292.
[908] Asclepiad, 1890, vii., p. 201.
[909] Bull. Acad. Méd., Paris, 1876, v., pp. 611, 754, 904; and 1881, x., pp. 847-852.
[910] Op. cit., p. 279.
[911] Op. cit., p. 288.
[912] Indian Med. Gaz., 1890, xxv., p. 257.
[913] Brit. Med. Jour., 1877, i., p. 444.
[914] Ib., 1891, p. 399.
[915] Lancet, 1889, ii., p. 255.
[916] Paris thesis, 1877, No. 327.
[917] Hofmann, “Lehrbuch,” p. 514.
[918] “Méd. Lég.,” 1874, p. 406.
[919] Op. cit., p. 554.
[920] Op. cit., p. 275.
[921] Op. cit., p. 288.
[922] Op. cit., p. 23.3
[923] Tardieu, op. cit., pp. 296, 298.
[924] Physician, etc., New York, 1880, xiii., p. 181.
[925] Trans. Mass. Med. Leg. Soc., 1878, i., pp. 14-24.
[926] Op. cit., p. 291.
[927] Second Kings, viii., 15.
[928] Taylor, op. cit., p. 482.
[929] Op. cit., p. 434.
[930] Taylor, “Med. Jur.,” Am. ed., 1880, p. 485.
[931] Op. cit., p. 31.
[932] Jour. de Méd. de Toulouse, 1851, iii., p. 237.
[933] Op. cit., p. 295.
[934] Ann. d’Hyg., 1843, xxx., p. 225.
[935] See writer’s “Bathing and Boating Accidents,” Jour. American Medical Association, April 19th, 1890.
[936] See writer’s article, “Memory, Diseases of,” in “Reference Handbook of the Medical Sciences.”
[937] Medical Record, August 22d, 1891.
[938] “Medico-Legal Experience in Calcutta,” Edinburgh, 1891.
[939] Indian Medical Gazette, December, 1888.
[940] Jour. of Orificial Surgery, April 1st, 1893, p. 709.
[941] Trans. of the Massachusetts Medico-Legal Society, vol. i., No. 8, 1885.
[942] Lesser, Dr. Adolph: “Ueber die wichtigsten Sectionsbefunde bei dem Tode durch Ertrinken in dünnflüssigen Medien,” Berlin, 1884.
[943] Gilberti, Dr. A.: “I Segni dell’ Annegamento nel Cadavere in Putrefazione,” 1889.
[944] Barlerin, Paul, le Dr.: “Etude Médico-légale sur la Submersion,” Tarare, 1891.
[945] Fagerlund, L. W.: Ueber das Eindringen von Ertränkungsflüssigkeit in die Gedärme.” Vierteljahrschrift für gerichtl. Med. und off. Sanitätswesen,” Berlin, 1890.
[946] Circular No. 3, War Department, Surgeon-General’s Office, Washington, 1871, pp. 129-131.
[947] The subject has been well studied by Dr. A. Carré, Archiv. de l’Anthropologie Criminelle et des Sciences Pénales, 15 Janv., 1892.
[948] Flint’s “Text-Book of Physiology,” Ed. 1877, p. 517; I. Forster, “Zeitschrift für Biologie,” tome ix., 1872.
[949] Foster, “Handbook of Physiology,” Ed. 1880, p. 457; Kirke’s “Handbook of Physiology,” 11th Ed., vol. i., p. 311.
[950] F. Spaeth, “Archiv für Hygiene,” 1886, pp. 68-81.
[951] Rochard, “Encyclopæd. d’Hygiene,” vol. ii., p. 796.
[952] For elaborate statements consult Edward Smith, “Foods,” Int. Sci. Ser., N. Y. Ed., 1878; Pavy, “On Food,” 2d Ed., 1881, N. Y., p. 467; Buck, “Hygiene,” Ed. 1879, vol. i., p. 190; Parkes, “Hygiene,” Ed. 1873, p. 179; Levy, “Traïté de Hygiene,” vol. i., p. 739.
[953] Corrigan, “On Famine and Fever,” etc., Dublin, 1849.
[954] Donnivan, “On Famine,” Dublin Med. Press, 1848, p. 67.
[955] Folet, Ann. de Hygiene et de Méd. Legal, 2d ser., vol. xlviii.
[956] Sloan, London Med. Gazette, vol. xvii., p. 265; Martin, Med. Times and Gazette, 1861, vol. i., p. 344.
[957] Chossat, “Récherches experimentales sur inanition,” Paris, 1843, p. 45.
[958] “Récherches experimentales sur inanition,” 1845.
[959] Bouchardat, “De l’Alimentation insuffissant,” Paris, 1852, p. 10.
[960] Greenfield, Brit. Med. Jour., Oct. 20th, 1877.
[961] Dr. McLoughlin, London Lancet, Nov. 2d, 1878.
[962] Reg. v. Jacobs and wife, Carmarthen Summer Assizes, 1890; also London Lancet, 1890, vol. ii., p. 132.
[963] Caspar, “Forensic Medicine,” Syd. Soc. Pub., vol. ii., p. 29; London Lancet, April 11th, 1877, pp. 580-620.
[964] Thornhill, Med. Gazette, Nov. 28th, 1835, p. 390.
[965] Caspar, “Forensic Medicine,” Syd. Soc. Pub., vol. ii., p. 36; Martin, Med. Times and Gazette, March 30th, 1861 (Case 132).
[966] “The Penge Case;” Reg. v. Staunton, Central Crim. Court, 1877.
[967] The case of Reg. v. Jacobs and wife.
[968] Holland, “On Morbid Effects of Deficiency of Food,” London, 1839.