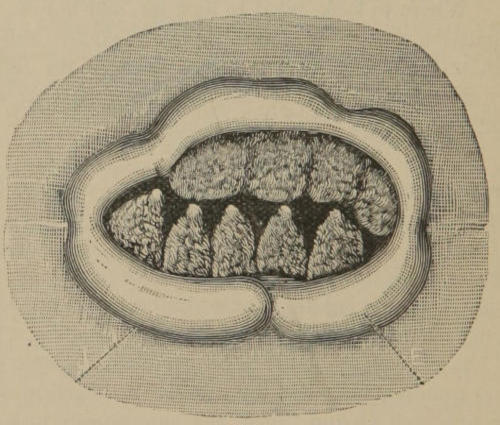
Fig. 1.—Internal hemorrhoids prolapsed and held out by the constriction of the sphincter. J. Junction of skin with mucous membrane. E. Everted bowel.
BY
W. P. Agnew, M. D.
SAN FRANCISCO, CAL.
R. R. Patterson, Printer, 429 Montgomery Street,
1890.
Entered according to Act of Congress, in the year 1890, by
W. P. Agnew, M.D., in the office of the Librarian of Congress at
Washington.
In preparing this hand-book, the object will be to give in plain and comprehensive language, as briefly as possible and with little discussion, a few general rules, which if even approximately observed, can but lead to success in the treatment of all non-malignant rectal diseases commonly known, and for which the general practitioner will not infrequently be called upon for relief.
Hemorrhoids, being by far the most common among this class of ailments, and the greatest bone of contention regarding the best manner of effecting a radical cure, will take precedence in our consideration, and receive the attention that their importance and dignity justly merits.
It is an indisputable fact that until within the past few years, an operation for the radical cure of hemorrhoids was considered so formidable an undertaking, that their treatment, outside of palliative measures, was almost entirely eschewed by the general practitioner.
“No fact is better known to the profession,” says Dr. S. S. Turner, U. S. Army, “than that nearly all men, doctors not excepted, will suffer more than the pain and inconvenience of a thousand operations, rather than undergo an operation for removal by any of the methods in vogue. The fame of some specialists who are distant enough to ‘lend enchantment to the view,’ will generally induce people of large means[4] when life has become something of a burden, to place themselves under their care and take what they offer.”
“But unfortunately, piles are by no means limited to people of large means. The greater number of sufferers must take what the general practitioner can give and will not take the cutting and crushing operations until compelled by dire necessity, and are only too glad of a less heroic alternative which offers them hope of relief. For this body of sufferers, the operation by carbolic acid injection offers a means of relief to which they will readily submit. In a sufficient number and variety of cases to justify me in having an opinion upon the question of its merits, I have never met with anything which I have regretted.”
With these stubborn and uncompromising facts confronting us on the one hand, and a full appreciation of the superiority, the simplicity, the safety and certainty of the operation by carbolic acid injection on the other, the writer has no alternative other than to espouse, and proclaim his honest conviction and hearty support in favor of the latter method of cure; and essays to point out in this little publication, in a plain, comprehensive and a practical way, what has been acquired by personal observations and experiences, and all in all, believed to be the best manner of applying this truly scientific and greatly superior method. A method, the discovery of which, I feel prepared to say, marks an epoch in the history of medicine, unrivaled in advancement by the treatment of any other disease or class of diseases to which the human family is subject.
“There is no organ that is so prone to become diseased as the rectum. There is no class of cases so little understood and treated as rectal diseases. There are no diseases so annoying and painful, and at the same time producing such dire results on the general system, directly and reflexly, as rectal diseases. For years Rectal Surgery has been principally in the hands of itinerants, whose remorseless greed for money has caused them to treat for revenue only, and to play the vampire on all that fall into their clutches. It is high time for the general practitioner to gather up all the information possible, in order to be able to treat all patients suffering from rectal disease, and thereby drive the itinerants back to their previous occupation of tilling the soil.”—(Yount.)
Nowhere in medical lore do we find suitable instructions whereby the beginner may knowingly and intelligently engage in a rectal examination—what to expect, where and how to find it, and how to pursue each succeeding step in applying the treatment. Writers either presume too much on the part of those who have not had experiences, or, are so habituated to the use of general anæsthesia in accomplishing the objects sought, that milder means have been seriously neglected. Finding many, otherwise well informed practitioners, at a great disadvantage in this respect, was a leading incentive to the hurried preparation of the following few pages.
The division of piles into internal and external, is naturally suggested by their observation and study, and clearly defined by designating all hemorrhoidal tumors originating above and within the grasp of the external sphincter as internal, while those situated external to or outside of the external sphincter, when the latter muscle is closed and the bowel not protruded, are external.
It matters not what form of tumor presents itself for treatment, whether of the capillary variety, distinguishable in being of small size, flat or sessile, made up of the terminable branches of the arteries, the beginning of the veins and the capillaries which join them, punctated, granular surface with thin covering and likely to bleed on the least provocation, or the arterial hemorrhoid with the arteries and veins freely anastomosing, larger, and presenting the glazed appearance of a very ripe strawberry, liable to inflammation, erosion, prolapse and hemorrhage; or the venous hemorrhoid, hard or soft, not very sensitive, blue and sluggish, which Kelsey says may result from the other two varieties or arise de novo and bleed per saltum; or any form of external hemorrhoid, cutaneous tag or like redundant tissue, they are all treated alike and with like good results, by the operation of injection and the use of the preparation herein recommended.
After obtaining something of a history of the case, you will have ascertained whether or not there is an inordinate protrusion at stool, its nature and if it has to be replaced. In the latter event the patient is directed to go to the closet or use a commode and make an effort to strain out the bowel. If not successful, use an injection of warm water, or select a time immediately after the usual hour for evacuation, which, if it occurs early in the day, may be deferred by the will power of the patient to a later hour.
This will bring to view any and all large hemorrhoids located on the upper margin of the internal sphincter, as well as those situated between the sphincters, their being caught in the grasp and button-holed like by the external muscle.
Should the prolapse not be sufficiently great or the piles sufficiently large to be thus caught and held out for inspection, let the patient lie on either side, with knees well drawn up, and instructed to strain down and extrude the parts as much as possible, assisting by gently pulling down and everting the mucous membrane at the verge of the anus with the thumbs. It is always better to precede by an injection of warm water, which may not only unload the rectum and give the patient greater confidence in the effort to extrude the parts, but washes away the mucous and retained feces in and about the sphincters. When the examination has been carried to this point and no satisfactory cause found to explain the trouble complained of, the finger and speculum will be required to complete the diagnosis.
The finger is of little use in diagnosing soft hemorrhoids[9] that form on the upper margin of the internal sphincter and lay back in the rectal pouch; being hindered by the pressure of the muscles and a like feel imparted by the bowel.
Bear in mind that you need not look for hemorrhoids higher up than the upper margin of the internal sphincter, a distance of not more than an inch from the verge of the anus, and if of any appreciable size, will always show at stool. Where to look, what to look for, and how to find it, is a question that often confronts the beginner, and it will not be out of place here to firmly impress the following rule: See all that can be seen and treat all that can be treated without the aid of a speculum.
There is not much probability of confounding hemorrhoidal tumors with any other abnormality in the vicinity of the rectum. The different varieties of internal hemorrhoids, a description of which is given on page 7, may confuse, but as stated before, no discrimination is necessary in applying the treatment for the purpose of effecting a radical cure, the one great object to be attained. Where several distinct tumors exist, they are usually arranged in rows on either side, not up and down, but antero-posteriorly, with the long diameter of each tumor at its base, parallel to the antero-posterior diameter, or, if the muscles were dilated, to the circumference of the rectum.
If situated on the upper margin of the internal sphincter there may be several isolated tumors thus arranged on one side, while they may have all coalesced, or originally have formed into one continuous hemorrhoidal mass on the opposite[10] side, Fig. 1. Or there may be one continuous hemorrhoidal mass on either side, separated only by an anterior and posterior commissure, Fig. 2. In some instances when the bowel is prolapsed and constricted by the external muscle, the branches of the middle hemorrhoidal veins that anastomose and encircle the upper part of the internal sphincter, may be so dilated and distended as to present an unsightly appearance, reminding the anatomist of the circle of Willis; at the same time a few capillary or sessile tumors may be seen studded around at different points.
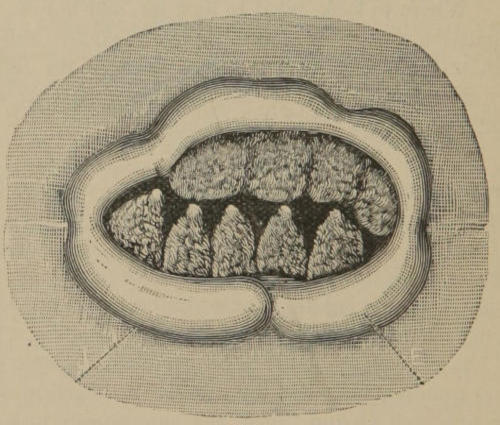
Fig. 1.—Internal hemorrhoids prolapsed and held out by the constriction of the sphincter. J. Junction of skin with mucous membrane. E. Everted bowel.
There can be no mistake in discriminating between a[11] large hemorrhoid and the bowel, but to distinguish a small, blanched hemorrhoid, located on the upper margin of the internal sphincter from an irritated and saggened portion of the bowel, when looking through a speculum, is more difficult. The bowel presents a more smooth and continuous surface, while the hemorrhoid is more uneven and irregular, and bleeds freely when scratched. Sometimes a victim of piles will call and speak of his piles having come down and are hanging out. On inspection a large fold of mucous membrane will be seen protruding on one side, which has been mistaken by physicians for a hemorrhoid, but the tumor will be found immediately above and possibly on the opposite side.
From polypi hemorrhoids may be distinguished by their spongy like texture, easy to bleed when scratched, more painful, history, shape, manner of arrangement, etc. Polypi are considered as a hypertrophy of the normal elements of the mucous membrane and the sub-mucous connective tissue. If originating from the former they are soft, if from the latter hard and fibrous, are often pediculated or club-shaped, sometimes grow rapidly, not painful unless within the grasp of the sphincter, may arise entirely above the sphincters, and are rarely of a glandular, villous or bleeding surface. Should a mistake be made and a polypus thoroughly injected, the result would be nothing more than a permanent removal of the offending growth.
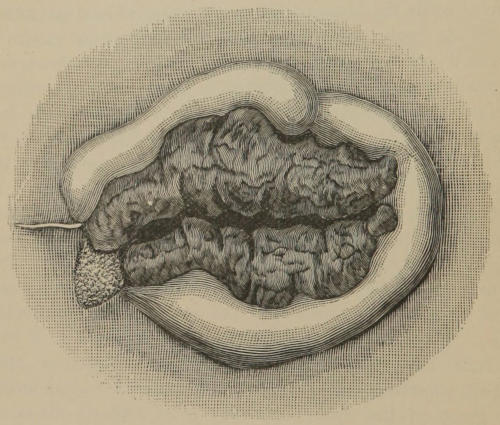
Fig. 2.—Prolapsed internal hemorrhoids, showing a continuous hemorrhoidal mass on either side, with an arterial pile on the left, all completely eradicated by two operations.
The external hemorrhoid does not elicit the thought or command the dignity of his neighbor, the internal pile, but usually makes himself known more forcibly in his incipient[12] stage of formation, caused by the rupture of a venule of the inferior hemorrhoidal vein, allowing extravasation and infiltration, which may lead on to inflammation and suppuration, or the clot absorb and result in an external cutaneous tag, subject to œdema, itching, induration, etc. On pulling down the mucous membrane at the verge of the anus, sometimes a slight fullness or bulbous-like expansion of an exposed part of a superficial vein will be seen, which should not be mistaken by the novice for an incipient hemorrhoid.
It is quite common for those afflicted with piles to call for treatment while suffering from an attack, sometimes called the hemorrhoidal state. This is not a favorable time to operate. Reduce all local congestion and inflammation first, by palliative measures, such as hot water douches, injections into the rectum of equal parts of Fl. Ext. Hamamelis and Pinus Canadensis (dark) in a little water, or water and glycerine if the latter is not repelled by an irritated bowel. At the same time open up the portal circulation by the use of equal parts of sulphur and cream of tartar, a teaspoonful in syrup or mixed with sugar, once or twice a day for a few days, or any other suitable means to put the bowel and piles at rest. Often patients will know what will relieve them of this condition better than the physician, as what relieves one will sometimes aggravate another.
In all cases of large growths, whether the patient is in a comparative state of ease or not, a similar preparatory treatment before operation will shrinken the tumors and lessen the tendency to local congestion and pain. Sulphur should not be taken within two or three days of operation since it continues its action about that length of time after dosage; but the bowels should be sufficiently evacuated previously to enable them to be held for four days afterwards, by any agreeable cathartic, or by flushing of the colon. This will be unnecessary in the treatment of small growths.
The same course should be pursued to expose the tumors for operation, as was named under the head of examination. In some instances, where the tumors are not very large but[14] exceedingly irritable (arterial), it might be quite difficult, even though the bowel be partially prolapsed, to expose them sufficiently for a good operation. In such event, paint the protrusion with a 5 per cent. solution of cocaine and allow the patient to sit, for a few moments, over a vessel containing a small quantity of steaming hot water. This will engorge the tumors, relax and materially aid in handling the parts.
As a precautionary measure in all operations by injection, to prevent the medicine from extending too deeply into the tissue of the gut by gravity, or the overflow from running down on the outside of the pile and over the bowel, let the patient lie on the side opposite to the tumor to be treated, so that the preparation will gravitate to the apex rather than its base of attachment.

Fig. 3.
Smear vaseline on the opposite side of the bowel and anus and over any piles that may show on that side, which, as the patient is now placed, are on the lower or under side and will catch any and all waste and overflow of medicine. As a further protection pack or hold absorbent cotton underneath the tumor being operated upon. If the tumor be small and partially obscured, the end of the finger may be held back of it to act as a counterforce while introducing the needle; or a double, slide tenaculum may be used to pull and hold it down for the same purpose, being careful not to remove the tenaculum when once applied until after the operation, as the least prick or scratch of a hemorrhoid will[15] cause a free flow of blood and greatly hinder the sight when it is desirable to watch the action of the injection compound.
Should any portion of the injection compound fall on the muco-cutaneous surface, unless the latter be heavily coated with vaseline, or protected with cotton, it will excoriate and probably cause a great deal more pain and soreness than the operation itself. In operating through a speculum such risk is avoided by the sides and floor of the instrument, which afford a protection to the surrounding parts; that is, if the precaution regarding position when operating is duly observed, to wit: always operate with the tumor pendent, or with its attachment on the upper side.
Make a glycerite of tannin in the proportion of 4 drachms (Squibb’s) tannic acid to 1 oz. (Price’s) glycerine. When the solution is complete, add 2 drachms each of (Squibb’s) salicylic acid and borax, putting in the salicylic acid first; stir over lamp, using a glass rod and porcelain dish, until dissolved, being careful not to burn. If any dirt or sediment be seen it had better be strained now through a piece of wet cheese cloth, while yet hot, into a two-ounce vial.
Select a No. 1 grade of carbolic acid, say Calvert’s, and barely liquify it by distilled water. Pour ½ ounce of the liquified carbolic acid in a clean graduate, and add ½ ounce of the glycerite of the salicylate of borax and tannin, previously made. Do not be sparing in giving the carbolic acid full measurement, if not a little in excess.
When the combination is effected with the acid, a floculent precipitate will occur, which should all clear up within[16] two or three days, otherwise something will be found wrong either in the purity of the chemicals used or the manner of effecting the combination.
Too much importance cannot be attached to the purity of the ingredients entering into this preparation, as anything unnecessarily irritating should be scrupulously avoided. I have tried synthetic carbolic acid and found the odor of tar decidedly stronger, and believe it much more acrid and irritating than the commoner preparations. Neither can I see that anything is gained in using vegetable glycerine.
Inject from 3 to 30 minims, or more, according to the size of the tumor. There is no rule to regulate the quantity by count. The object is to inject a sufficient quantity to permeate the entire substance of the tumor, its texture being much more spongy than the surrounding tissue, and not extend beyond its base of attachment.
Here is where many make a mistake in the injection of hemorrhoids. Some are prone to use too much, even though the solutions be weak, and apply it too deeply, reaching to and destroying the muscular coat of the bowel, causing prolonged pain, deep sloughing, etc. While others use too little, which may act as a foreign body or local irritant, producing a central slough and a slow breaking down of the disturbed growth.
A tumor, properly injected, cannot inflame, because there is nothing to inflame, the circulation is stopped and thus it is as effectually strangulated as by a ligature, with the advantages of the immediate local anæsthetic, antiphlogistic,[17] auterant and antiseptic properties of carbolic acid. The base of attachment heals, while the dead tissue, which is rendered non-inflammatory and antiseptic, disintegrates and is thrown off between the third and fourth day, a process that fortifies against secondary hemorrhage.
There is a medium ground to be taken, in regard to the quantity as well as the strength of carbolic acid to be used, with a little room for variation on either side; yet there must, in point of reasoning and fact, be a limit somewhere. If a little more should be used than is necessary to permeate the entire substance of the tumor, the result will not be disastrous, but may excite a little more local disturbance and pain. On the other hand, if a little less be used, the operation will be equally as effective and is probably the better side to err upon, provided the discrimination be not carried too far.
A similar dilemma confronts us respecting the strength. After trying the weaker solutions and watching their effects, I have concluded that the solution should contain not less than fifty per cent. of carbolic acid, combined with the glycerine of the salicylate of borax and tannin,[1] the latter in such proportions as to produce an immediate astringent effect. Tannic acid not only keeps the carbolic acid within limits by its non-irritating astringent effect, but of itself combines with a certain portion of the albumen of the blood and other tissue, forming an insoluble albumenoid. The salicylic acid and borax, original with Dr. Q. A. Shuford, of[18] Tyler, Texas, gives the preparation more consistency and seems to lessen the irritative properties of the carbolic acid.
[1] Original.
A weak, thin, watery solution, aside from doing poor work, is much more liable to diffuse itself and be carried into the circulation like a hypodermic of morphia, than a solution sufficiently strong to act as a cauterant, destroying the tissue, forming a compact and an insoluble coagulum and strangulating the circulation at once.
A solution, weak or strong, when deposited to any depth beneath the surface, with live tissue and the circulation passing on all around it, will of necessity excite pain, inflammation and a slough, the same as a splinter in the flesh. The properties of carbolic acid being non-inflammatory in their nature, will often, where a small quantity is used diluted, produce an adhesive inflammation, an induration and a contraction in a tumor, by destroying the capillaries where applied.
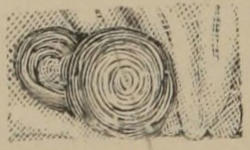
Fig. 4.—External hemorrhoid before operation.
Fig. 5.—Three days after operation, with coagulum still attached by pedicle.
It is always desirable, when operating on external hemorrhoids, to see that quite a goodly portion of the cutaneous surface, especially at the summit, is effected by the preparation applied inside the capsule; otherwise it will become inflamed in order to let out the interior coagulum, which I have often seen come out on the third day intact, and in[19] one unbroken cystic-looking mass, Fig. 5. The same rule obtains regarding internal hemorrhoids, having thick, unyielding coats.
Puncture the tumor at the most accessible point, preferably with the needle, nearly parallel with, or at an acute angle to its base, carrying the point of the needle to about the center of the tumor, if it be globe shaped, or equi-distant from base to apex, if it be elongated, with the face or opening of the needle toward the apex. Be sure the needle is inserted beyond the proximal end of its opening, which is not always observable in treating small growths; but may be tested by forcing the piston of the syringe a little, and if the end is not sufficiently buried the medicine will show around it on the outside.
Inject the first few drops the same as you would a hypodermic of morphia, then slowly, drop by drop, watching its action by change of color on the surface of the pile. This change of color on the surface is quite marked with hemorrhoids of delicate covering, less so with those possessed of more tough and fibrous coats. Hold the needle in position a moment and if the quantity injected does not appear sufficient, turn the nut on the piston with which you have previously gauged approximately the quantity to be injected, back a few rounds and throw in more. Puncture large elongated tumors in two, three, or four places. The compound diffuses itself slowly and no doubt extends some farther than is always apparent at the time of operation. Withdraw the needle carefully; it may be necessary to force out a few drops of the preparation at the point of entrance,[20] for the purpose of sealing up the puncture to prevent the escape of blood and medicine together, which, however, never amounts to much. If, after withdrawing the needle, some of the injection fluid runs out, unmixed with blood, take it up with absorbent cotton, since it indicates that the quantity at that particular part is superfluous. Now dry the surface of the tumor or tumors with absorbent cotton, smear with vaseline and return within the bowel.
A tumor properly injected immediately becomes hard. There are septa or compartments in elongated growths which do not permit the medicine to pass through readily, and if a soft section is noticed, it has not been penetrated, although will doubtless break down with the general mass. I have seen a liberal injection into the middle one of three tumors connected and arranged in a row, so cut into those on either side that a single reddened column like appeared afterwards on the extreme outside, (Figs. 6 and 7).
Fig. 6.—Three internal hemorrhoids before operation.

Fig. 7.—After a liberal injection into the middle tumor.
Large hemorrhoids must not be exposed too long after injection, since there is always more or less swelling produced around the tumor by the stoppage of circulation and the presence of a foreign body. Return the side not operated upon first, then the other, and if the tumor has considerable[21] length, let it go in endwise. The patient can often return the protrusion with least pain.
A little practice will enable any one to see the simplicity of the entire procedure. If you should make a mistake when operating through a speculum, and land the whole charge into a fold or saggened portion of the bowel do not be alarmed, as it will only be a little more painful and longer in healing. Injection into internal hemorrhoids is not painful to any degree, therefore if the patient complains much you might suspect that you are invading the tissue of the bowel. With some, the injection into external hemorrhoids is quite painful at the first contact of medicine, but immediately thereafter subsides. Where the tumor is very sensitive, external or internal, precede by a hypodermic of from three to five minims of a five per cent. solution of cocaine. Introduce the needle point barely underneath the covering of the growth and force out one drop. This will anæsthetize enough to allow further penetration, when another drop can be thrown in. By this time you can approach the interior to a sufficient depth to inject from three to five drops more, and anæsthesia will be immediate and complete. There need be no fears from cocaine absorption, since the carbolic acid compound will catch and hold the cocaine all within the body of the tumor before it can be absorbed and enter the general circulation.
From one to two hours after operation, the carbolic acid looses its local anæsthetic effect and what I have called the after pain commences, caused by the presence of a foreign body acting on the peripheral nerve at a point where the[22] line of demarkation forms. This pain varies in intensity with the sensibility of the patient and surface of attachment of the tumor or tumors. Some will not complain at all, saying the discomfort is not as great as the suffering from an attack of piles; while others will make considerable fuss, requiring an opium and belladonna suppository:
| ℞ | Opii Pulv. Optim. | gr. xii |
| Ext. Bellad. | gr. iv | |
| Ol. Theobrom. | ʒ iii | |
| M. et Ft. Sup. No. xii. | ||
The pain does not usually continue longer than from twelve to fourteen hours, unless aggravated by undue exercise, or other similar causes, being replaced by a feeling of soreness, which is sometimes reflected down the limb or up to the bladder.
The treatment after the operation should be markedly palliative: hot water sponge compresses, hot water sitz-baths, and hot poultices are great as long as pain and soreness are complained of, together with opium suppositories, pro re nata. If the extent of the operation requires constipation of the bowels, enemas should be dispensed with until after the expiration of four days. Then hot slippery elm water, flaxseed tea, or corn starch as prepared for stiffening clothes, may be used, as well as a soothing suppository:
| ℞ | Bism. Subnit. | ||
| Iodoformi | ā ā | ʒ i | |
| Opii Pulv. | gr. v-x | ||
| Ext. Bellad. | gr. v | ||
| Ol. Eucalypti | gtt. vi | ||
| Ol. Theobrom. | ʒ iiss | ||
| Ol. Olivæ | gtt. x | ||
| M. et Ft. Sup. No. xii. | |||
The oil of eucalyptus will almost completely disguise the odor of iodoform.
In old people who lack sufficient vitality to quickly heal a broken surface, coat with bismuth, bismuth and oxide of zinc ointment, oxide of zinc powder, reduced resin cerate, eucalyptol, etc.
Eucalyptol is a sovereign remedy to stimulate healthy granulatious, after a broken surface has lost its freshness or acquired some age, in the proportion of ½ dr. to 1 oz. oxide of zinc ointment, containing a small quantity of stramonium or opium and belladonna. Or, ½ dr. to 1 oz. vaseline with 1 dr. oxide of zinc.
Anything that excites and keeps up pain is hurtful. Severe, continuous and prolonged pain is an indication that the changes are not going on in a satisfactory manner. It should always be subdued as much as possible. Suppositories containing glycerine, castor oil, or anything productive of much pain, should be wholly discarded.
Temporary sympathetic paralysis of the bladder, or spasmodic stricture of the urethra may occur, being relieved by hip baths or the catheter; the latter is very seldom required. Enjoin as little straining as possible. Many of the worst cases, in otherwise healthy people, will speak of holding the bowels as being the greatest difficulty encountered[24] during the entire course of treatment. A little flatus will sometimes produce an annoying titilation of the muscles. It has been suggested that a small tube be introduced at such times for relief.
A certain amount of moisture begins to exude the second day after operation, particularly noticeable from external hemorrhoids, and a peculiar smell when the coagulum is thrown off. This should not be interpreted as suppuration.
It would not be reasonable to suppose that all cases will behave alike. The local and constitutional disturbance will, of course, depend upon the size or surface of attachment of the tumor or tumors and the nervous and physical condition of the patient. It is best to require patients to lay up for a few days after operation on large hemorrhoids, or when more than one of small size are taken, even though they do not complain.
In people enjoying average health, with internal hemorrhoids located on both sides, take one side at a time, making two operations of the treatment. In a case like Figure 1, not an uncommon form, it will be better to operate on all the five smaller tumors first, while they are exposed and kept out by the aid of the large one on the opposite side. Should the large growth be taken first, it may be impossible for the patient to hold down the bowel sufficiently afterwards to operate on any one of the five small fellows, and a speculum will be called into use; this will prolong the treatment, as few will submit to the operation on and the manipulation of all five tumors through the slot of a speculum at one sitting. Small isolated piles can be treated[25] singly, and the patients allowed to go about their business. It is these bad cases, where the patient knows the importance, prepares and lays up for treatment, that we should make as short work of as possible; those who have been great sufferers, and possibly the operation on one small tumor would so arouse the others that the suffering would be as much, if not more, than if all had been treated at the same time. Not unfrequently the piles on the opposite side, and left for a second operation, will set up the howl and cause more pain and suffering than the side treated; especially may you look for such alarm if you allow any of the injection compound to fall on their unprotected surface. A patient once observingly remarked that it must be a peculiar kind of medicine that caused pain when brought in contact with the outside of a pile, but none when applied to the interior.
As regards pain, it might be briefly stated that little can be done in the vicinity of the rectum, it matters not what strength of carbolic acid is used, or plan of treatment adopted, without causing more or less discomfort in all cases, amounting to actual pain and suffering for a brief period in others. Not at the time of operation, for that in itself is practically painless, but during the process of cure.
This cannot be wondered at, when considering the extreme sensibility of the parts and amount of tissue involved and actually removed by a radical operation. Yet it is no greater in the majority of instances and not as much in extremely irritable piles, as that caused by the periodical squirting in of a few drops of carbolic acid and water, extending over a[26] period of weeks, and even months, that is neither safe, certain, or otherwise satisfactory; and often brings discredit upon a process which, if properly understood and rationally applied, has no approach to comparison in any other method of cure.
Some physicians fear to use anything stronger than a little carbolized water and glycerine, lest they produce carbolic acid poison, embolism or a slough. This is a mistake, the dangers they seek to avoid are coupled with such uncertain and illogical practice.
Dr. E. H. Dorland, Chicago, Ill., says: “When a compact coagulum is formed, and the muscular layer of the bowel is not touched by the styptic it is impossible to do harm, all the learned theory to the contrary, notwithstanding. A weak solution forms little globules in a tumor, and we can imagine one so small as to be carried into the circulation.”
To effect a radical cure, it is desirable to get rid of the tumor bodily, not by shrinking or contraction into a hard knot, or by inflammatory destruction, but by a separation of the spongy and vascular growth from the normal tissue of the body, the same as if dissected off root and branch. This is obtained by putting a sufficient quantity of the preparation recommended just where you want it, and such results will invariably follow. I have seen internal hemorrhoids, about the third day after operation, become so friable that they could be crumbled off similar to a piece of cheese. The preparation can be relied upon to extend just as far as you put it and no farther, and will remove as much of the[27] tissue as permeated. It will extend farther, and permeate more readily the structure of a pile than the sound tissue, because the former is much more spongy and cellular, allowing the preparation to be easily forced and diffused throughout its integrity (Fig. 8). A pile, properly injected, should appear the next day after operation perfectly dead, as if boiled or cooked, and of a leaden color.
A gold or platinum pointed needle should be used, fitted with a screw to gauge the depth of insertion, and of sufficient caliber to allow the preparation to pass through freely. There are several makes admirably adapted to this purpose, Fig. 9. A common hypodermic would be utterly useless.
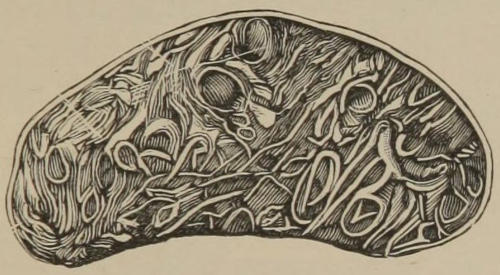
Fig. 8.—Section of hemorrhoid showing internal spongy structure (Esmarch).
A common glass barrel, metal bound, hypodermic syringe is all that is needed. It should be provided with side handles. Draw the medicine into the syringe before screwing on the needle, force out the air and gauge the nut on the piston for about as many minims as thought will be required.
When a syringe is not kept in constant use the piston will dry out and stick to the barrel. This is remedied by setting the nut on the piston when laying the syringe away, so that the piston will not quite go to the bottom of the barrel. When it is desired to use the syringe, screw back the nut, say sixteenth of an inch, and take up the syringe with thumb on the piston handle and finger on the cap at the other end, and press together, thus freeing the piston.
Fig. 9.—Syringe, needle and flexible silver canula.
A heavy, open face watch glass with a center facet is a good receptacle for the injection compound before drawing it up in the syringe.
Marginal swellings and abscesses, appearing the third or fourth day after operation, are produced by excessive irritation. I have never seen them occur except when the patient disobeyed instructions and exercised inordinately. One instance, in a case of long standing, where the piles occupied both sides of the rectum between the sphincters, I operated on both sides and injected every tumor at one sitting, enjoining rest and quiet. He afterwards rode a long distance and walked a half mile, which caused an unusual amount of pain and soreness; not content with this he took a dose of castor oil, when a very painful marginal swelling occurred. Being a strong man up to this time he had used no palliative measures whatever, and only then informed me of his suffering. Hot water and a sponge soon eased the pain and a superficial abscess developed; it was slit up and a good recovery followed.
According to my observation and belief, piles situated just above the verge and in proximity to the network or plexus of nerves surrounding the anus, are more prone to cause a marginal swelling than others, particularly if improperly or two deeply injected, and an irritating quality of carbolic acid be used. It might also be stated that pain varies in intensity as it approaches the verge, one of the most acutely sensitive surfaces of the body. A small sensitive pile not larger than a salmon egg, situated within the grasp of the external sphincter, will keep up a titilation and[30] contraction of the muscle sufficient to disturb and put ill at ease the entire animal economy.
A swelling or lump which often appears immediately after injection of piles of any considerable size just above the verge, is of no consequence and will subside within a few days. A similar swelling sometimes results from a severe attack of internal hemorrhoids, which some speak of as the developing of an external pile, but I do not see that such formations are anything more than marginal swellings, caused by the irritation above.
About the time the tumor is thrown off, between the third and fourth day, and sometimes later, before the healing surface becomes strong, or should the portal circulation become obstructed and the hemorrhoidal vessels congested, secondary hemorrhage may rarely occur. It is easily controlled by the use of Monsel’s Salt, to which a little morphia should be added, carried in a small piece of wet absorbent cotton, and held on the ruptured vessel by the end of the finger until the hemorrhage ceases. A few minutes will usually suffice. Knowing where you operated will be a guide to the place of application. The injection of a strong solution of tannic acid will be sufficient in mild cases. I have never known a secondary hemorrhage, following carbolic acid injection, amount to anything more than an easily controlled venous hemorrhage. Am inclined to think secondary hemorrhage is most likely to occur when a pile breaks down from a partial injection, leaving the vessels unprotected in places, or from an injection too deeply into[31] the substance of the bowel; yet, I have seen all these conditions time and again without the least tendency to hemorrhage.
With a fifty per cent. solution of carbolic acid and the combination given, carbolic acid poison and embolus are entirely out of the question. The only danger of embolus lies in the too sparing use of a weak solution of carbolic acid, injected slowly into the unobstructed calibre of a coursing vein. While a strong solution quickly and generously applied would destroy the tissue and obliterate the vessel as effectually as the hot iron.
The extensive sloughing that I have heard of so much I have never experienced, and am not able to conceive of such an occurrence, except it be in a very low state of vitality; but can imagine how a pile would slough if a few drops of carbolic acid were deposited in the center, or deeply into its base, leaving the apex and greater portion of the growth with a free circulation. A weak solution taking effect in the interstices of the most tender part of a hemorrhoid, but not sufficiently strong to attack the more fibrous portion, would doubtless result in inflammation and slough. A pile with a thin delicate covering and internal structure can be cured by an injection of water, while those of a more tough and fibrous character would only be exasperated by such annoying treatment and behave in a bad manner.
In looking over the comments of Kelsey, Andrews and others regarding the injection of hemorrhoids, it appears[32] quite evident that they have not given the subject scientific study. It would seem that representative men and authorities, after a knowledge of the brilliant results following the treatment in many cases, attended by accidents in others, would seek to know and try to obviate the cause or causes of these unexplained irregularities.
They never improved upon the method in its primitive and undeveloped state, but seemed willing to magnify and enlarge upon all the accidents and complications arising from and following the indiscriminate use of all sorts of injection compounds, in the hands of the ignorant and inexperienced, and in diverse and unfavorable conditions for treatment.
How about the old methods? Only a few months since my attention was attracted to a gentleman of prominence, in middle life, strong body and good habit, who had been operated upon for the removal of piles by ligature. He was seven months in recovering, during which time two fistulas developed. I do not mention this case as an isolated one, because we all know that excessive and prolonged pain, causing in some instances lock-jaw and death, retention of urine, sloughing and stricture by contraction of tissue, abscess, fissure, fistula, intractable ulceration, hemorrhage, immediate or secondary, great and lasting prostration and slow recoveries, saying nothing about the dangers of anæsthesia etc., are not uncommon when the old methods are practiced.
About the time that Kelsey, after having deposited five drops of a carbolic acid solution in the center of a large tumor, observed it looking dark, angry and inflamed from[33] the intrusion of a foreign substance, would have been a fitting moment for a full dose of carbolic acid, of suitable strength and in sufficient quantity to pervade the entire structure and form a compact coagulum; strangulating the circulation, cauterizing the tissue and thereby checking the inflammatory action at once; then followed up by the liberal application of hot water and a sponge.
The method that I adopt and recommend for the removal of piles, not only does the work neater and cleaner than the more heroic measures in vogue, but robs the patient of the terrors of etherization, as well as the dreaded consequences incumbent upon and more or less inseparable from operations of violence, in a peculiarly organized and sensitive locality; and, as Dr. E. F. Hoyt, of New York, says: “There is not a hemorrhoidal case possible but what can be obliterated by this means; and I am at a loss to explain why so many cling to methods that carry so much havoc and suffering. If every college in the land would have this subject demonstrated by men of experience and learning, all other means would soon lose recognition.”
I shall not take up time and space in enumerating cases but will briefly mention three of quite recent date, and of more than common interest on account of some of the associated history given.
Manuel L., aged 39, capitalist, had arranged his business affairs and prepared for the possible results of a ligature operation. All being in readiness, he was placed on the operating table by a prominent surgeon, who, upon examination,[34] found the hemorrhoids to look so formidable in appearance that he refused to proceed further, stating that the operation might prove fatal.
On his first visit to me, he was asked to use the commode and strain out the piles, which presented to view a large, continuous hemorrhoidal mass encircling nearly one-half the bowel on one side, with five distinct and typical tumors on the other, similar to Fig. 1. He was directed to lie on the operating chair with the large growth oil the upper side, and about 30 minims of the carbolic acid preparation was injected in three different places in the mass, the protrusion returned and the bowels constipated for four days; after which the bowels were moved by an enema of slippery elm water, when not a vestige of the growth could be seen, and no pain.
He put his hand back to push in the bowel, as he had been accustomed for the past eight years, and found it gone; whereupon he said if this had occurred in the day of miracles, he would think me Jesus Christ. One operation is all that is required for the remaining five tumors, and both piles and prolapsus are cured by two operations. In fact, the smaller tumors should have been taken first, when the opportunity to get at them was much better.
The only inconvenience suffered was from an effort to hold the bowels, and the after-pain, which lasted about 14 hours, but was not severe; during which time an opium suppository was introduced every two or three hours. He stated that he was just getting over an attack of La Grippe and had been purged pretty freely, consequently did not[35] evacuate the bowels previous to operation, but advised a liquid diet for the first three days.
George P., aged 37, druggist, had a continuous hemorrhoidal mass occupying both sides of the bowel when protruded, being separated only by an anterior and a posterior commissure. Glaring fibrous bands seemed to bind down the enlargements in places, presenting anything but an inviting case. He also had an arterial hemorrhoid attached just above the verge, constantly hanging out and exciting the external sphincter; looked like and was about as large as a medium sized strawberry, irritable and eroded.
The history of the case and the extreme ungainly appearance of the protrusion induced me to have it photographed. It is approximately represented in Fig. 2, but does not show the fibrous bands. The patient was placed on the side opposite the larger mass, which was injected at four different points. The bowels were constipated for four days by the occasional introduction of an opium suppository and then moved by enema, when the man shed tears of joy on having no pain at stool and finding no protrusion on that side. The next operation took the other side, together with the strawberry, and the case discharged, cured of piles and prolapsus.
Both of these gentlemen had been told time and again that the carbolic treatment was ineffectual and dangerous. One ex-army surgeon and college professor said he would not attempt any of the heroic operations in the second case, as there was too much tissue involved; that he would only agree to treat it by making local applications twice a week.
And further, he would not promise any results inside of ten months, asking twenty dollars per month. He would not swerve from his opinion, and could not say that a permanent cure would then be effected.
Mrs. Jane D., nearly 80, afflicted many years, had consulted fifteen different physicians, all of whom refused anything more than temporary relief because of extreme age; having always been considered delicate, with cataract now forming in both eyes. Would be satisfied if she could live not more than two years after a cure.
The tumors were “old bronzed veterans,” tough and unyielding. One side was taken at each operation and although confined to the bed mostly for the first seven or eight days after operation, could get out and in at any time without assistance. Had no constitutional disturbance, never missed a meal and was able to get up and down stairs inside of eight days unattended.
The dead piles embraced in the coagula were much longer in separating from the bowel, and base of attachment longer in healing than in the average case. Hot water sponge compresses were used frequently, together with opium suppositories for the first 24 hours, then occasionally for the next three days; after which hot water irrigation and iodoform suppositories. Later bismuth, eucalyptol and oxide of zinc ointment. An occasional dose of sulphur and pot. bitart. was given and the bowels moved by flushing of the colon; which was resorted to but twice.
In this case the edges of the thickened, calloused mucous membrane of the bowel where it joined the hemorrhoids,[37] appeared to be so cartilaginous in places, that I expected hard ridges would be left; but they all disappeared and softened down by the use of eucalyptol, buckthorn and stramonium ointment. At one point a small polypus sprang up, which withered from the injection of a few drops of pure carbolic acid, like a tender sprout, after being frozen, under a scorching sun.
The lady could not repress her feelings of emotion, in expressing gratitude for the services rendered, but gave way and freely cried. Although in rather poor circumstances, she did not think a charge of fifty dollars sufficient and afterwards returned, saying that she felt that she would not die happy unless I was better paid, and insisted upon my taking another “twenty.”
Do not operate during an attack of piles.
Operate with the tumor, or tumors, on the upper side.
Handle the parts with extreme gentleness and deliberation.
See all that can be seen and treat all that can be treated without the aid of a speculum.
Protect the under parts from excoriation by waste and overflow of medicine.
Evacuate the bowels previously and constipate for four days after operation on large growths, or when several small tumors are taken at one time.
Hot water sponge compresses, early, often and continuously, are indispensable and unequaled for the relief of a pain, swelling and soreness. To be effective it should be applied as hot as can be borne.
Wait until the soreness disappears before performing a second operation. This will require from one to two weeks, according to the extent of the first operation and the physical condition of the patient.
Take great pains and care to perform a neat operation. A certain amount of ingenuity and tact are required, which, unfortunately, all do not possess. If a bungling job be made, the bowel punctured, a pile injected on one side only and the surfaces excoriated, do not attribute an unnecessary amount of pain and suffering to the preparation used or the method employed.
As a general alterative and curative agent in many diseases, and particularly to relieve and prevent hemorrhoidal congestion in rectal troubles, sulphur in small doses, persisted in for some time, probably has no equal. The most convenient form for administration is a palatable tablet (Wyeth & Co.), containing 2½ grains, or 5 grains with 1 grain of cream of tartar. Reference to the learned articles on the physiological and therapeutical uses of sulphur, by Dr. John V. Shoemaker, published in the Dietetic Gazette, Sir Alfred B. Garrod in the Lancet, and in Ringer’s hand-book of therapeutics, will be amply repaid.
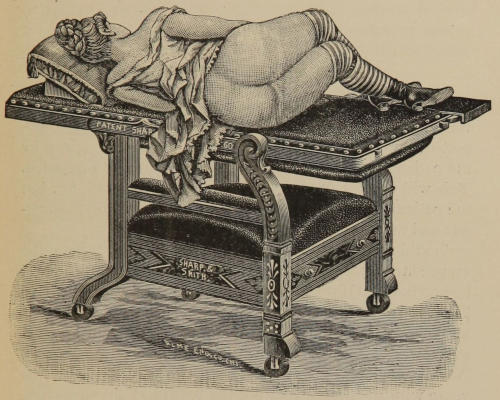
Fig. 10.—Position for operating, or making a rectal examination. Engraving kindly furnished by Sharp & Smith, who manufacture one of the best office and operating chairs combined, on the market. It works without “cranks,” “levers,” or “ratchets.” Upholstering is entirely protected during an operation.
It is unnecessary for a lady to disrobe herself for examination, or suffer immoderate exposure. A cloth cover should be used, when a lady patient is placed on the chair, the same as in gynæcological practice.
The first step to be taken in making an examination of the rectum, where disease of this organ is present or suspected, will be to obtain a history of the case as given by the patient, supplemented by questions naturally suggested. This will furnish an idea of what might be looked for, but the patient’s interpretation will often be found quite erroneous and misleading.
Should there be an undue protrusion at stool, pursue the same course recommended for the examination of internal hemorrhoids. If protrusion be absent, direct the patient to lie on the side with knees drawn up, separate the buttocks and inspect the anus; or, in other words, all that presents to view externally at the terminal orifice of the rectum. Now draw down and evert the mucous membrane at the verge with the thumbs, asking the patient at the same time to extrude the parts as much as possible. This will enable you to see all there is half an inch or more above the entrance.
Next, anoint the finger, pass in gently and examine all the surface limited by the sphincters, a distance upwards of not over an inch, being careful lest you be deceived by the mobility of the tissue, when introducing the finger, and a[41] small marginal growth be carried up and appear as one of internal origin.
Any one familiar with vaginal examinations can detect a rough or a broken mucous membrane, an indurated spot or prominence as soon as touched. Next, feel above the internal sphincter, keeping in mind the anatomy of the parts, turn the finger slowly, posteriorly you can hook it behind the muscle. Here is situated the bottom or floor of the rectum which forms a cul-de-sac (Fig. 11). By asking the patient to strain down moderately, its surface will be thrown up against the end of the finger and in this manner properly explored.
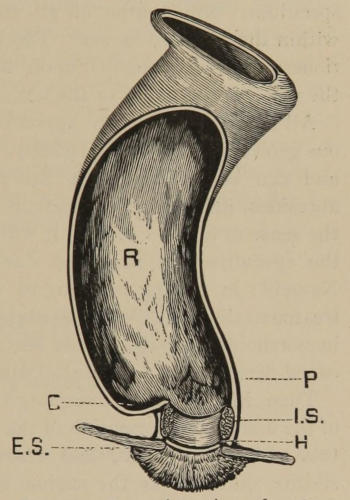
Fig. 11.—Lateral section of rectum; normal curve. R. Rectal pouch. C. cul-de-sac of the rectum. E. S. External sphincter. I. S. Internal sphincter. H. Hilton’s white line. P. Position of prostate gland.
A digital examination reveals, in the normal state, a soft, velvety, unbroken mucous membrane, the parts pliable and yielding, with no reflex excitability of the sphincters. The position and sensibility of the uterus should be[42] noted in the female, and size of the prostate gland in the male of advanced years.
The first three or three and a half inches of the rectum can be brought within reach of the finger. Explorations farther up will require a rectal sound and a long tubular speculum. Nine-tenths of all rectal ailments are found within the first two inches. Therefore, few general practitioners will ever be called upon to treat anything beyond the reach of the finger or the scope of a common speculum.
All hemorrhoids of any appreciable size, or other tumorous growths in the same vicinity, will show at defecation and can be treated while the parts are extruded. All abrasions, ulcerations, indurations, etc, are discoverable by the sense of touch. Hence, it will be seen that the uses of the speculum are narrowed down to a few in number. Namely: in that of bringing to view for observation and treatment diseased surfaces previously located; small, soft hemorrhoids and other minor affections which may have escaped detection by a careful digital examination.
Then, in view of the foregoing facts, and in consideration of the anatomical formation of the parts, being a collapsable tube, highly sensitive and extremely difficult of accessibility, quite unlike the vaginal canal, which is closed at one end, more capacious and dilatable, and designed by nature to be approached from the exterior, a speculum should be so constructed as to not only be easy of introduction and withdrawal, but to exclude all the surface except a limited portion, and permit the greatest amount of available light possible to fall on the exposed part shown in situ.
The greatest barrier to the successful use of a speculum is the unruly external sphincter and the excessive mobility of the mucous and muco-cutaneous surfaces. The upper margin of the external sphincter terminates beneath the junction or the skin with the mucous membrane, which place also marks the beginning of the internal sphincter and its junction with the external muscle by a more dense connective tissue, sometimes appearing as a white line at the muco-cutaneous junction called the white line of Hilton.
According to Dr. Andrews, Hilton has demonstrated that the locality where the two muscles join by the intervention of this fibrous ring forming the anal verge, the junction of the skin and mucous membrane, and the exit of the branches of the pudic nerve, is identical.
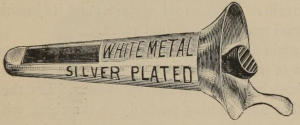
Fig. 12.—Author’s Rectal Speculum.
The internal sphincter is a collection of the circular fibres of the muscular coat of the bowel, about five-eighths of an inch in width, and constitutes in reality the terminus of the gut. For the external sphincter is a thin band of distinct and separate muscular fibres, elliptical in shape, between three and four inches from its anterior to its posterior extremity,[44] and expands out around the margin of the anus like the flaring end of a trumpet; with its superficial layer in close relation to the skin which it draws down in radiating folds.
With this understanding of the anatomical relations, it will be seen that the external muscle contributes so slightly to the length of the canal, that it might be considered wholly on the outside, where it guards closely the entrance, and is nowise concerned in an examination with a speculum except as a feature of incumbrance.
To correct an erroneous idea that there is any considerable depression or space intervening between the muscles, we mean, when we say between the sphincters, the distance bounded by the fibrous ring uniting the two muscles below, and the upper portion of the internal muscle above. More simplified, we mean all the surface included between the upper margin of the internal sphincter and its junction with the external muscle at the anal verge.
All examinations with a speculum should be preceded by an enema of warm water to wash away the mucous and retained feces in and about the sphincters. Let the patient lie on either side, turning partially on the chest, with knees drawn up, the one uppermost more firmly flexed on the abdomen, and hips so elevated that the speculum, when introduced points or inclines downward, and admits of strong natural light to fall in parallel rays to its axis.
Warm the speculum by dry heat over a single blast kerosene stove, where gas is not convenient. A suitable kerosene stove is an indispensible adjunct to an office for heating instruments, water, etc., causing no smell and leaving no[45] deposit of sut on the bottom of vessels as done by gas or alcohol. Use white vaseline as a lubricant; everything that tends to whiteness helps the sight. The vaseline may be squeezed from a tin-foil tube, and the finger not soiled in preparing the speculum for insertion.
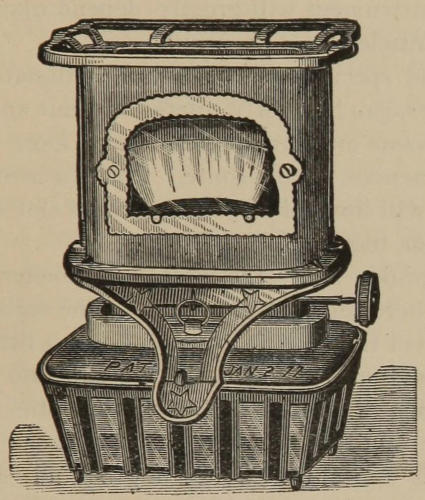
Fig. 13.—A suitable Kerosene Stove for office use. It is clean, safe, cheap, portable and has perfect combustion.
To prevent the loose tissue from rolling up and being pushed in with the speculum, the patient may assist by holding the upper buttock away, while the physician introduces the instrument with one hand and retracts the opposite buttock with the other.
Introduce slowly, giving time for the muscles to relax,[46] bearing in mind that all movements about the rectum and anus must be extremely easy and gentle. The proximal end of the slot must be carried and kept above the external sphincter during the entire course of the examination. It matters not what kind of a speculum is being used, the value of the instrument will greatly depend upon its power to hold this muscle out of the way.
A closed end speculum, with a proportionate slot and smooth corners, can be slowly rotated without any difficulty where the mucous membrane is not very loose and baggy and no prominences in the route. But if a hemorrhoid be in the way it will immediately drop in the slot and further progress is thus impeded.
When examining above the internal sphincter, especially posteriorly, where the bottom or floor of the rectum forms a cul-de-sac, direct the patient to strain down a little; this effort will throw the mucous membrane out into the speculum, at the same time spreads out and smooths its surface. In looking through a speculum this cul-de-sac of the rectum sometimes appears as a vacancy behind the internal sphincter, and has been mistaken and treated as an ulcer cavity. It often contains a liberal supply of mucous.
Fistula in the recto anal region so far exceeds that in any other locality, that its overwhelming predominence here almost entitles it to the exclusive right of the term; while, to those who have given this part of the physical organism special study, the word itself, calls to mind a local condition of disease that is anything but an easy one to manage.
In point of frequency fistula is next akin to hemorrhoids, but a much less desirable complaint to treat. Allingham states that the number of cases occurring in hospital practice is greater. That two-thirds of all the cases operated upon of the in patients at St. Mark’s Hospital, London, were fistula. The most frequent cause assigned being abscess. A failure of the abscess to heal, leaving a sinus or sinuses, is explained by the presence of loose areolar tissue and fat, excessive mobility of the parts by the action of the sphincters, respiration, coughing and sneezing, and a strumous diathesis.
In consequence of an occasional failure of the muscles to regain their power after division by the knife, elastic ligature or galvano-cautery wire in the treatment of fistula, leaving the subject in a pitiable state of incontinence of feces, which has resulted in several well authenticated cases in suicide, new and rational methods have been devised for the relief of this very troublesome and unpleasant affection.
Kelsey says: “A permanent incontinence of feces is always considered by the patient a very poor exchange for fistula, which was causing comparatively little suffering and annoyance.”
The fact that such a deplorable condition does sometimes follow complete section of the sphincters, and that we have no means of knowing previously when it may or may not occur, I submit the question to all thinking, conscientious and painstaking physicians: Should we not seek the adoption of any efficient means of treatment, whereby such risk is wholly avoided?
About the first of March, 1890, Daniel Mc., aged 35, who a few months before had been operated upon by a reputable surgeon for a simple, uncomplicated fistula, sought my acquaintance, exhibited his condition and related his experiences.
The fistula originated from a small abscess, with its internal opening between the sphincters, the external scarcely an inch outside the anus, and was not of long standing. The operation consisted in a division of the external muscle with the greater portion of the internal; he was put on a liquid diet, bowels confined for fifteen days and kept in a recumbent posture.
The incision was slow in healing, between three and four months; his health, which was formerly good, has been greatly impaired ever since the operation. The external sphincter has lost its power altogether and the internal muscle greatly weakened, which necessitate the wearing of a clout whenever the bowels become a trifle loose, and he lives[49] in constant fear of soiling himself by allowing the escapement of the least quantity of flatus. The time lost, the money expended, and the unfortunate condition in which he finds himself eight months after the operation, have so thoroughly embittered him against the cutting process, that he spares no pains and loses no opportunity to influence every one with whom he comes in contact, against all such heroic and uncertain measures.
For the purpose of obviating these very unsatisfactory and highly objectionable results, we have a choice of any one, or all of three different methods, viz: treatment by injection, treatment with the fistulatome, and treatment by the galvano-cautery as practiced by Dr. Shotwell; who, fully appreciating the dangers of muscular section, has hit upon a plan both new and commendable.
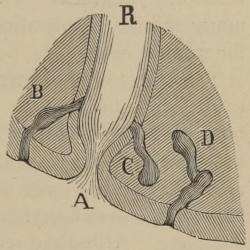
Fig. 14.—Varieties of Fistula. (Gosselin.)
The sub-cutaneous, or sub-mucous fistula can be cocainized and slit up with a pair of scissors, and the tract cleansed and cauterized with a solution of carbolic acid, a comparatively trivial affair; but the external blind, the internal blind, the complete, the complete with diverticula etc., are varieties which call forth a decidedly greater amount of ingenuity and thought in bringing them to a successful issue.
The treatment by injection, sometimes classified as a “non-operative method,” has been so successful in the hands of[50] many, that it is stoutly affirmed that any case curable by the usual heroic methods is equally curable by this method. Different preparations have been used, chief of all being carbolic acid, ranging in strength from 50 per cent. up.
In adopting the carbolic acid treatment, probably the better way after preparing the sinus, will be to use a 95 per cent. the first time and subsequently a 50 per cent. solution; protecting the parts from excoriation by any suitable unguent and absorbent cotton. Hot water compresses to relieve pain and reduce swelling. Iodoform, Eucalyptol, etc., in the interim. Judgment will be required in not making too many irritant applications and granulation thus hindered for want of rest.
The object is to destroy the pyogenic membrane by the cauterizing effects of the acid and get up a granulating carbolic acid sore. It may be necessary to evacuate the bowels and constipate for several days to give the muscles rest, or resort in extreme cases to divulsion. The sinus must have constant, free external drainage until the healing process is complete. Allingham recommends the introduction of the small end of a bone collar button to keep the orifice open, with a hole drilled through its centre for drainage.
As a preliminary step the external orifice should be dilated with a laminaria tent or other appropriate means. The fistulous tract explored with a common probe and thoroughly cleansed with hot water introduced through a flexible silver canula; which is also used for the injection of a 5 or 10 per cent. solution of cocaine to obtund the sensibility.

Fig. 15.—Bone Stud
Concerning the carbolic acid treatment Allingham says: “Since the publication of my last edition I have cured many patients by dilitation of the sphincters and the use of the bone stud and carbolic acid. One practical point I would mention. The further the external aperture is from the sphincter the more likelihood is there that the sinus will heal. This is shown as well in the cases of spontaneous cure as in my own successes. You must always enjoin rest after a strong application, and watch that not too much inflammation be set up.”
The fistulatome shown in fig. 16, is a contrivance which is perhaps destined to take the lead in the treatment of fistula generally. It is so constructed that the fine cutting blades close on themselves, while the instrument, which is probe pointed, is being introduced, but immediately open on withdrawal, and thus catch up and cut through the fistulous membrane.
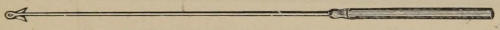
Fig. 16.—Fistulatome with blades extended.
Who the inventor of this clever device is, I have been unable to ascertain, having seen it claimed by three different physicians, one of whom speaks of curing 76 per cent. of all cases treated by one operation. That is by drawing the fistulatome through the tract once. Cases of long standing require that the instrument should be turned at right angles and drawn through the second time and possibly repeated later on, or a tenotome employed to scarify any remaining indolent sinus.
It will be readily seen, however, that a fistula with a side pocket, branch or diverticulum, would hardly be reached by this method; although the blades are so formed that they draw the membrane of a dilatable pouch to them from the sides. In such cases a little ingenuity would be required in finding these diverticula, for the purpose of scarifying them with a tenotome.
The preparation of the sinus and the after-treatment are the same as already mentioned. Also evacuation of the bowels and constipation by the use of an opium suppository, even to the dilitation of the sphincters, if thought necessary to bring about a cure. In rare instances, where divulsion has been practiced and while yet under the influence of anæsthesia, it might be advisable to lay open the cavity by cutting from the sphincters, pockets traced, scarified and partitions divided.
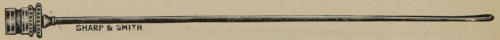
Fig. 17.—Flexible Silver Canula.
In relation to treatment, Andrews says: “The truth is, that anal fistulæ have a natural tendency to recovery, and are held back from it mainly by two things.
1. “The unfavorable effect of the undrained septic fluids within the sac.
2. “The tightness of the external opening, which prevents free drainage, and keeps the sac distended with this putrid pus.
“It is demonstrated by Dr. Mathews on the one hand and by the experiments of quacks on the other, that by controlling[53] these two conditions, many cases will heal spontaneously. It follows that among the thousands of patients subjected to cutting operations by surgeons for this disease, there are many who might be cured by much milder means.”
Shotwell’s operation consists in straitening out of the fistulous tract with a steel probe, having an eye at its distal end, which is carried entirely within the bowel whether the fistula is complete or not. He next pierces the solid structure about three-eighths of an inch farther from the anus with a lance-pointed probe also having an eye near its end, parallel with the first probe, until its end is seen penetrating the bowel a little beyond.
The eyes of the probes are then threaded with the opposite ends of a No. 24 platinum wire about ten inches in length, and both probes withdrawn, leaving the wire in situ forming a loop; both ends are now secured to an electrode, the current turned on and the loop drawn through the partition. Little, if any, dressing is required, but the bowels must be kept locked up for at least a week. This of course involves the use of general anæsthesia.
A word to the beginner, in the prevention and detection of fistula. Since abscess is the most prolific source, proper attention to the abscess by poulticing, early lancing, the sinus washed with hot, heavily carbolized water, allowed free drainage, the bowels evacuated, constipated and the muscles put at rest for a few days, will doubtless be successful in forestalling its almost certain fistulous sequence.
Dr. Hoyt strongly recommends divulsion of the sphincters, immediately after opening the abscess, as an unfailing remedy in preventing fistula.
Annoyance by itching, a slight discharge and soreness at times in a circumscribed spot, with previous history of abscess, might be considered a sure sign of fistula. But the patient may give the same symptoms with no knowledge of previous abscess, or other cause pointing to the formation of a fistula. Yet, on inspection, a small opening with pouty lips, or a closed cicatricial depression not much larger than a pin-head, will be found. This is the external ring or opening of a fistula, and if closed, may resist the introduction of a probe sufficiently to create the belief that no sinus exists.
A solution of continuity, varying from a slight abrasion of the mucous membrane to a marked degree of destruction of tissue, comes within the scope and meaning of rectal ulcer.
A deep-seated, non malignant type of rectal ulceration, complicated with stricture, fistula, etc., is not so very common, and seldom met with outside of hospital practice.
The less serious and more simple varieties, such as may be productive of considerable systematic disturbance through reflex excitability, without attracting much, if any attention locally, are the forms most frequently seen by the general practitioner.
With few exceptions, rectal ulcer is insidious in its nature; in some instances passing on to the stage of stricture, which alone may be the first symptom to cause alarm, as the following recent case will illustrate.
Mr. C⸺, aged thirty-three, married, applied for the treatment of hemorrhoids. He stated that the only inconvenience suffered was from constipation. That the piles did not come out and were never very sore but he had seen a little bloody mucous at times and had a constant desire[56] to go to stool. A free evacuation and relief being obtained only after the feces were made liquid by the injection of warm water.
On the introduction of the finger I found about one-inch and a half from the anus, an annular stricture which almost entirely occluded the bowel, with ulceration and gummata below. More close inquiry elicited the fact that the stools were not much larger in circumference than a lead pencil. He had noticed the trouble not more than two months before. There was a previous history of chancroid at the age of 19, with no constitutional symptoms.
It is claimed that organic stricture does occur without previous ulceration by interstitial deposit and thickening, and ulceration follow. But this must be considered exceptional. The ulcerative process usually precedes, and through efforts at repair, cicatricial bands are thrown out, producing a narrowing and contraction of the canal, either in places or throughout the circumference of the bowel.
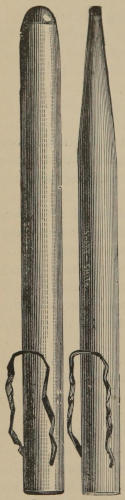
Fig. 18.—Rectal Bougies.
Electrolysis may be tried for the relief of stricture before resorting to the usual methods of breaking up by forced[57] dilitation. If divulsion be decided upon it should be complete at one operation. Should the fibrous bands be strong and unyielding, nicking the edges with a probe pointed bistoury is advantageous.
On account of severe hemorrhage and other untoward symptoms likely to follow a complete division of the stricture, the galvano-cautery is decidedly preferable to the common proctotomy knife. A duplicature of the peritoneum coming down to within about three and a half inches of the anus anteriorly, should not be lost sight of in operations on the rectum. The persistent use of bougies will be necessary for a long time after divulsion.
Stricture is mostly of syphilitic origin. Of the seventy cases, tabulated by Allingham, ten of the number were found in men and sixty in women, showing a great predominence in the latter; and none were more than three and a half inches above the rectal orifice.
It is not an easy matter to diagnose between the advanced stages of non-malignant rectal ulcer and cancer. Both may be accompanied by tender, condylomatous growths or flaps of skin outside the anus, bathed with an ichorous fluid. The characteristic, unremitting pain of cancer may be absent in its formative stage, and in this respect insidious in its approach, the same as the non-malignant ulcer.
Allingham speaks of a very rare species of rectal ulcer, which he terms rodent or lupoid, that is superficial, does not implicate the surrounding parts, devoid of hard edges or surface, very painful and only cured by complete extirpation.
I have intentionally omitted the early symptoms and course of rectal ulcer for the purpose of giving audience to Dr. A. C. Hall, who, in a communication to a medical journal, writes the following lucid description:
“Rectal ulcer is a more common disease than is generally supposed. Unfortunately the symptoms are generally obscure, and the patient suffers but very little, if any pain, and consequently consults his physician for some of the reflex symptoms, rather than for the initial disease itself; and very often these reflex symptoms are vainly treated till the patient and physician are both thoroughly disgusted and disheartened. There is one maxim which every physician should always bear in mind, and that is, always suspect rectal ulcer in every case of protracted or chronic diarrhœa. I have reports from eighty-six pension surgeons, in which they estimate that they have examined two thousand cases, where chronic diarrhœa was the alleged cause of disability in applicants for pensions. Of these two thousand cases of chronic diarrhœa, eighty-seven per cent. had rectal ulcers, and fully ninety per cent. of those who claimed chronic diarrhœa as their disability and who had no ulceration were rejected, because their proofs of the disease, aside from the ulceration were too meagre. Thus the strongest and most prominent symptom of rectal ulcer is chronic diarrhœa.
“The diarrhœa is generally more troublesome in the morning. The patient often on arising feels an urgent desire to go to stool. This act is often very unsatisfactory, for he passes very little feces and a great deal of wind. Occasionally these small stools are covered with a jelly-like, or white[59] of an egg substance, or the motion may be only a jelly-like mucous, with no feces. There is generally more or less tenesmus, or a disagreeable feeling, as if the rectum was imperfectly evacuated. Sometimes the patient will be compelled to go out two or three times before breakfast, and he may in the later attempts to have a stool, pass lumpy or scybalous feces, covered with mucous, and often streaked with blood. There sometimes exists, as a symptom of rectal ulcer, a desire to go to stool when cold drinks are taken. But generally the diarrhœa and tenesmus subside soon after breakfast, and the patient has no more trouble until the next morning. A great many, or I might say a majority of those suffering from rectal ulcer consult the physician for some symptom or other that suggests anything else but the rectum, but by close questioning, and following up the symptoms, one can soon tell whether they are reflex or otherwise.
“In cases of rectal ulcer of long standing, there is always more or less cachexia, or peculiar waxy, sallow, unhealthy complexion, which sometimes alone points significantly towards the disease.
“There is often more or less enlargement of the liver and spleen, especially the spleen.
“In advanced cases, the diarrhœa comes on at night as well as morning, and defecation is accompanied with pain and griping. Another almost characteristic sign of rectal ulceration, is alternating diarrhœa and constipation. The bowels remain constipated for a considerable while, then diarrhœa supervenes, and is accompanied by severe and excruciating colicky pains, and often nausea. Persons subject to chronic[60] diarrhœa always dread to take a physic to relieve a temporarily constipated state, for it will almost invariably put them to bed.
“In extreme cases, infiltration and thickening of the sub-mucous and muscular coats supervene, as a result of nature’s effort to repair the lost tissue. This thickening may be so extensive as to threaten and actually produce stricture. It will often convert the rectum into a passive tube, through which feces and fluids trickle, the patient having little or no control over the sphincters.
“The passage of hardened feces and the pressure of internal hemorrhoids and polypi are the most common causes of rectal ulceration. The lodgment of foreign bodies, such as fish bones, cherry stones and plum seeds that have been swallowed, and which act as irritants and produce ulceration.
“In women the pressure of the fœtal head on the rectum during childbirth is a frequent cause of ulceration, likewise the pressure of a misplaced uterus.
“On examination, by means of a speculum, the ulceration will be found about an inch or an inch and a half from the anus, generally on the posterior wall, but often on the anterior wall.
“When the ulcer is on the anterior wall, there is more or less irritability of the bladder, and seminal emissions or impotency. The ulcer itself may be round, oval or elongated, radiating or following the columns of Morgagni. The ulcer may present ragged, interrupted elevated edges, or they may be sharp cut and regular, as though cut with a sharp punch. The edges are sometimes hard and gristly, or may[61] be soft and with no elevation above the surrounding tissues. The surface of the ulcer is often clean, and healthy looking granulations may be seen, or the ulcerated surface may be loosely covered with a greyish, grumous scum, that is offensive, and decidedly unhealthy for the patient. Underneath this scum there is often found an ulcerated spot, that is apparently lifeless, and will require much attention, locally and constitutionally, to prevent its rapid extension. In this form of rectal ulcer there is always more or less marked cachexia. It is the indolent ulcer, occasioned by the gradual breaking down of the tissues, that produces the grave constitutional disturbances and death. It is the small, round, or oval ulcer, with elevated, hardened edges, that produces the many and various reflex nervous symptoms, which are misleading and troublesome.”
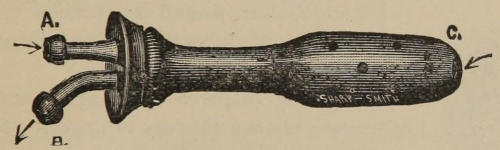
Fig. 19.—Rectal Irrigator.
In all cases of rectal ulcer of any considerable gravity, absolute rest, both of the parts and the body, is to be maintained. Hot water irrigations and a complete destruction of the diseased surface by carbolic acid, are the first things to be thought of, together with a liquid diet.
Convert the ulcer into a carbolic acid sore and use an iodoform suppository. In fact the treatment is very similar[62] to that recommended as an after treatment in a bad case of hemorrhoids, with such variations as the ingenuity will suggest. Bismuth, oxide of zinc, eucalyptus, mercury, resin cerates, etc.
Have found no use for iodine, nitrate of silver or acid preparation of iron, which corrode and destroy instruments in the treatment of rectal diseases.
Of all the diseases of the rectum, considering the apparent insignificance of the lesion, this heads the list as a pain producer. Fissure has characteristics peculiar to itself and I do not think, as is claimed, that its location, just above the muco-cutaneous junction or Hilton’s line, where the nerve supply is the greatest, explains these characteristics; neither do I think it of traumatic origin.
No other ulcer, wound or abrasion in the same locality produces the pain that identifies a fissure.
Fig. 20.—Fissure, complicated with polypi.
It might be compared to a rhagade or chap in the web between the toes or fingers. In its recent state it presents the appearance of a longitudinal tear of from three to five-eighths of an inch in length, looking raw and bloody, with ragged and somewhat everted edges; and may be complicated with polypi (Fig. 20), or a hemorrhoid occupy its base, called the “sentinel” pile.
It is aroused from its slumbers by a mechanical disturbance of the slightest nature, hence the name irritable. The act of defecation being followed by a dull, sickening, sometimes[63] lancinating pain lasting three hours or more, incapacitating the subject from labor. The mere introduction of the finger may produce a deathly pallor and possibly syncope.
Ask the patient to extrude the parts, then gently pull down the mucous membrane and apply a ten per cent. solution of cocaine to the tract with a camel’s hair brush or silver canula attached to a hypodermic syringe; carrying the solution fully to the top of the fissure, which may be out of sight. If any unguent has been used about the fissure it should be subjected to a hot water irrigation before using the cocaine, as cocaine will not take effect on a greasy surface.
When the tract is sufficiently anæsthetized to introduce a speculum, apply on the end of a probe wrapped with cotton, 95 per cent. carbolic acid, and prescribe the following ointment for daily use:
| ℞ | Acidi Salicyl. | ʒ ss |
| Vaselini | ℥ ss | |
| M. | ||
If unsuccessful after making two or three thorough applications of carbolic acid, inject into and beneath the bed of the fissure, in a sufficient number of places to encompass its length, possibly two, a few drops of the hemorrhoidal compound; and produce a slough. The object is to destroy the original ulcer and convert it into some other form that will heal. I have never seen a resulting sore from carbolic acid that was slow to heal.
A physician who had been a great sufferer from the effects of a fissure informed me that he had been etherized twice and the sphincters thoroughly stretched, and had submitted to incision three times, all of which had proved fruitless, and was finally permanently cured by the use of salicylic acid and vaseline.
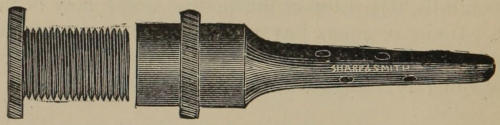
Fig. 21.—Ointment Applicator.
A prolapse of all the coats of the rectum, amounting in some instances to complete invagination, is of such rare form, occurring mostly during infancy, that it might be considered practically out of the list of rectal ailments.
Prolapse of the mucous coat of the bowel is not an uncommon affection, and is a frequent complication of internal hemorrhoids. When the hemorrhoids are cured the prolapsus usually disappears.
It is natural for the mucous membrane at the lower end of the rectum, by its loose attachment to the muscular coat through the cellular layer, to roll down and become somewhat everted during the act of defecation. It is only when this condition becomes excessive and the protrusion so great that it does not return of its own accord, that it is called prolapsus of the first degree and treatment required.
Should it occur independently or persist after the removal of piles, a cure may be easily effected by the injection of from eight to ten minims of a ten per cent. solution of carbolic acid, beneath the mucous membrane in the cellular structure, at points where it is desirable to take up a fold. The needle may be introduced in a line with the axis of the rectum, varying from one-fourth, one-half of an inch or more from the muco-cutaneous junction, and even as high up as the upper margin of the internal sphincter.
This can be done while the membrane is prolapsed, or through the slot of a speculum. The latter is preferable on account of the sides of the slot limiting the distribution of the medicine. Anything that will excite an adhesive inflammation or a change in the cellular coat will have a similar effect.
The following preparation is effective:
| ℞ | Acidi Salicyl. | ||
| Sod. Bibor. | ā ā | ʒ i | |
| Glycerinæ | ℥ i | ||
| M. | |||
Take six drachms of this preparation and add carbolic acid 40 minims.
If it be desirable to remove a thickened fold or bunch-like appearance of the mucous membrane, inject the same as you would piles, using the hemorrhoidal compound. It will slough off neatly and heal readily. It is peculiar of the injection of internal piles or of the same strength of medicine into or beneath the mucous membrane, that it tightens and takes up a slack of the membrane permanently, without apparent lessening of the calibre of the gut. It is also peculiar of the treatment and cure of internal hemorrhoids by injection, that no cicatrix, cicatricial tissue or contraction results, unless the operation has been extensive, involving both sides, and an active inflammation has been excited by extraneous causes.
Concerning the frequency of the diseased conditions to which the names rectal pockets and papillæ are applied, and their being such prolific sources of mischief as claimed by those who first caught up the craze and exaggerated the facts, a few brief comments may not be out of place.
That there are such morbid changes, and that they are more or less hurtful through reflex excitability can not be successfully disproved. That their appearance suggests the titles they have received is also undeniable. And the fact of their having been brought to notice in an irregular way, does not militate in the least against the existence of such affections, or the fitness of the terms used to designate them.
If it be true, as stated by enthusiasts on the subject of rectal pockets and papillæ, that they are frequently found in old, deep-seated, chronic diseases, where the presence of rectal trouble is never suspected by any local signs, we have, then, a sufficient reason to account for their having escaped the notice of specialists.
Andrews makes a labored effort, and with apparent success, to show that the so-called “pockets and papillæ” are normal structures. That the pockets are the sacculi Hornei (Fig. 22), which are little depressions situated just above and intimately connected with the verge of the anus, caused by the reticulated arrangement of bands of muscular and[68] connective tissue, beneath a delicate mucous membrane and deepened by the corrugating action of the sphincter ani. That the papillæ are little dot-like prominences frequently found between the lower ends of the sacculi Hornei, and when somewhat enlarged resemble in appearance the carunculœ myrtiformes of the vagina. That these little papillæ, with their adjacent “pockets,” constitute the so-called “pockets and papillæ” of the itinerant.
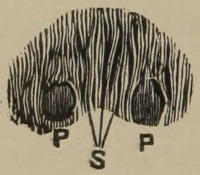
Fig. 22.—S. Sacculi Hornei. P.P. Papillæ, magnified three diameters. (Andrews.)
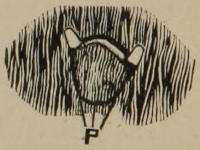
Fig. 23.—P. Bone fide rectal pocket with adjacent papillæ, not magnified at all.
I have seen just what Dr. Andrews very correctly describes, and will say, after carefully reading his explanation, I am fully convinced that he never saw what is meant by the discoverer of rectal pockets and papillæ. And further beg to say that the doctor must concede that there are others, who are not itinerants, capable of identifying a diseased surface when they see it, and pointing out its place of location.

Fig. 24.—Other varieties of papillæ and a simple form of rectal pocket.
It will be seen by a reference to the appended clipping, that Andrews has been making his microscopical dissections[69] nearly an inch below where true rectal pockets are found. And I can conscientiously attest that true papillæ bear no resemblance, in the least, to his papillæ or carunculœ myrtiformes at the anal verge.
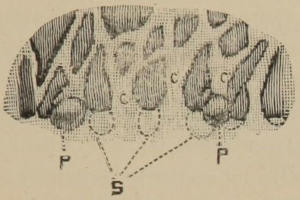
Fig. 25.—Represents figure 22, showing reticulated arrangement under post mortem relaxation. C.C.C. Columnæ recti. S. Sacculi Hornei. P.P. Papillæ. (Andrews).
Rectal pockets are doubtless a duplicature of the mucous membrane, forming cul-de-sacs with their mouths looking upwards. They are removed through a speculum by raising the outer wall with a blunt hook and excised with a pair of scissors, or slit through their center with a knife, and carbolic acid applied to the remaining flaps.

Fig. 26.—Author’s Knife-hook for slitting down pockets.
Papillæ may be seen in three different forms. One, a white, flat or sessile process, resembling the half of a split pea, but not quite so large. Another, a small, white, rather stiff projection on either side of a large pocket. The other, a slender, perfectly flexible, worm-like vegetation, possessed of a white or transparent top, Figs. 23 and 24. They appear to spring out of the mucous membrane similar to a polypus,[70] and can be snipped off at their base with little loss of blood and trifling pain.
“The usual location of pockets and papillæ is at a point about an inch from the anus, at the upper margin of the internal sphincter, where the large distended pouch of the middle portion of the rectum is abruptly puckered down to the narrow limits of its last inch.
“These pockets are curious formations, and have received very little attention from writers upon rectal disease, and they have been almost entirely overlooked by anatomists, as well as pathologists. Whether they belong to the anatomy or not, I am unable to state with any certainty, but I know for certain, however, that they are not always present. I know also that they can almost always be found in cases of old, deep-seated, chronic diseases, and that the removal of these pockets in this class of cases is followed by the most happy results.
“When these pockets are present, they always occasion a spasmodic contraction of the sphincter ani, a condition which is most frequently observed in those cases that are developing some deep seated constitutional disease. Their removal in this class of cases is invariably attended by more or less improvement of the patient’s general condition and circulation.
“In form and character these pockets may be long and narrow channels, and ulcerated at the bottoms; short (cul-de-sacs) or broad mouthed and pointed at the bottom. These pockets create a great amount of irritation to the nervous system. No matter what shape, condition or location they may be in, by reflex irritation they produce a long train of[71] nervous symptoms that cannot be remedied until they (the pockets) are removed.
“Papillæ are conical processes of mucous membrane, of variable size, shape and location. They have no relationship with rectal pockets, for they very frequently exist independently of them.

Fig. 27.—Pratt’s curved scissors.
“I look upon these conditions as being the most mischievous of rectal disorders, because they always occasion a tonic spasm of the internal sphincter, and this alone makes excessive demands upon the powers of the sympathetic nerve. They are common in all forms of chronic disease. I know of no reason why these conditions, which I have described should have been so long overlooked, and their importance have remained unappreciated.
Fig. 28.—Long blunt hook.
“Unless it be that their presence is unattended by local symptoms, and hence they have failed to attract the attention of either patient or the physician. But in view of the fact that they occur in so many chronic conditions, and the additional fact that marked benefit almost invariably follows their removal, I insist upon it that no obstinate case of[72] chronic disease has been properly examined until their presence or absence has been ascertained. The most happy and the most marvelous results that I have ever seen in the practice of medicine and surgery have followed the removal of pockets and papillæ, and in thus bringing them to your notice, I do so in the confident belief that a proper appreciation of their importance on your part will add materially to your resources in battling with disease, and in helping those who apply to you for relief.” (Pratt.)
Excluding all discoverable local causes whereby the presence of this obstinate affection may be explained, such as piles, ulcer, fistula, oxyuris vermicularis, eczema marginatum, etc., and take the disease unalloyed, or as it may exist in a state pure and simple, and assure a patient thus afflicted that he can be quickly and permanently cured, would not only be presuming too much, but would be stepping beyond the legitimate bounds of all past recorded experiences.
To furnish something of an idea to those who are not already familiar with this seemingly trivial yet rebellious complaint, I here quote the language of Dr. Hoyt, who uses words somewhat extravagantly in the beginning but palliates his feelings down later on with lotio niger.
“With what anguish its unhappy victims battle through innumerable sleepless nights fighting this demon of so-called[73] local epilepsy, with its long array of itching, burning, exuding, corroding, exhausting, and blaspheming characteristics, as though they had been brewed by the chemistry of hell. The whole organization becomes a chaotic discord, the disposition is cruelly warped, the countenance shows a sad picture of living woe, the carriage is nearly lost to all laws of equilibrium, and the complete being merges into a throbbing phantom of despair, trembling upon the very threshold of idolized suicide.
“Of course I speak of the most aggravated cases, instances that seldom occur within the experiences of general practitioners. Wherefore then these phenomena? What is the mighty influence that yields so much distress, as all these objective symptoms are but an appearance outflowered by some subtle and specific force. The meager literature upon this subject hobbles upon the crutches of hypothetical inferences, telling you perhaps it is capillary congestion or chronic proctitis, or neurotic hyperæsthesia or eczema, or malaria, suggesting a panoramic array of remedial agencies all unsatisfactory, thereby confessing to a sad condition of helpless empiricism.
“My comprehension of this subject compels me to endorse the parasitic theory, though it may excite your disapproval, and perhaps your ridicule, yet it can be easily verified by directing your management towards the destruction of the parasite, when all symptoms will disappear. Mercury is quoted as nearly a specific for the annihilation of these marauders, and the very best method of administration is by using Lotio Niger.
“Thrice daily the patient should relax, the respiration of the cutaneous surface by the free application of hot water, just as hot as it can be comfortably endured. Then immediately afterwards while the skin is made absorbent by the action of the liquid heat, it should be saturated with this medicine in the most thorough manner. Within three days time the itching will be reduced fifty per cent., but the complete result is attained only after a continued use of from four to eight weeks.
“In many cases there will remain points or patches where the agent does not seem to act, and to these I usually apply the regular unguentum hydrargyri. Avoid all soaps and ointments except as above stated, thereby preventing the obstruction to absorption of the remedy as it has to enter the pores of the skin in order to act upon these energetic enemies that hold their victims under such a terrible bondage.”
It is characteristic of pruritis for the paroxysms of itching to come on mostly after the patient gets warm in bed, at which time the annoyance may be further increased by a moisture or exudation about the anus.
In longstanding cases the skin becomes thickened, horny in texture, and loses its pigment and elasticity. Sometimes portions of the radiating folds will become so hypertrophied and elongated, from the effects of gouging and scratching, that they look like and are sometimes called external piles, which in reality are nothing of the sort, but properly speaking would come within the range and meaning of non-syphilitic condylomata.
I have successfully removed these formations by the same process adopted for the cure of piles. They go through similar changes after injection and open up a cavity surrounded by a ragged, thick, calloused skin, which, after first being cocainized, can be trimmed off with a pair of scissors. If there are several large tabs I do not operate on all at one sitting.
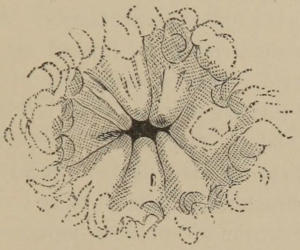
Fig. 29.—Thickened condition of the skin in pruritis (Esmarch).
In the treatment of pruritis ani, a thorough search for a local cause and its removal will find a lasting reward in the results obtained.
Of the obscure local causes, perhaps animal and vegetable parasites are the most difficult to find. The injection of a decoction of quassia bark or lime water and carbolic acid, will be efficacious in dislodging the oxyuris vermicularis, which may or may not be seen, like small pieces of white thread lodged between the anal folds.
For the vegetable parasites, tricophyton, etc., (microscopical) sulphurous acid ranging from 50 per cent. up is an old tried remedy. Immoderate eating, drinking coffee, and[76] smoking excites the itching with some. Whenever it be decided that no local or constitutional disease can be found as an assignable cause, and that it is purely neurotic in character, we commence to grope in the darkness for remedies. What relieves one will not another; and what relieves for a time will lose its effects altogether.
Hot water compresses, a little short of scalding, are good for relief and a good intercurrent remedy. Among the remedies highly recommended are linseed oil, thuja occidentalis, carbolic acid, citrine ointment, oil of cade, oxide of zinc, compound tincture of green soap, black wash, and galvanism. The anode is placed over the perineum and base of scrotum and the cathode against the anus or within the grasp of the sphincters. Claimed to be a specific. Nerve stretching by divulsion of sphincter muscles is also recommended.
Formulæ:
| ℞ | Ung. Citrini | ʒ ii |
| Balsam. Peru | ʒ iss | |
| Acid. Carbol. | gr. xx | |
| Sulphuris | ʒ iii | |
| Cerat. Simp. vel Lanolini | ℥ i | |
| M. | ||
| ℞ | Hyd. Chlor. Mit. | ℈ iv |
| Adipis | ℥ i | |
| M. Said to be specific for pruritis ani or vulvæ. | ||
| ℞ | Hyd. Chlor. Mit. | ʒ i |
| Balsam. Peru | ʒ iss | |
| Acid. Carbol. | gr. xx | |
| Lanolini | ℥ i | |
| M. et sig. Apply after hot sponging. | ||
| ℞ | Ol. Cadini | ʒ i |
| Acid. Salicyl. | gr. xv | |
| Ung. Zinci Oxidi q. s. ft. | ℥ i | |
| M. | ||
| ℞ | Saponi viridis | } | ā ā | ℥ i |
| Ol. Cadini | } | |||
| Alcohol. | } | |||
| M. (Kelsey). | ||||
| ℞ | Liq. Carbon. Detergentis (Wright’s). | |||
| Glycerinæ | ā ā | ℥ i | ||
| Zinci Oxidi | } | ā ā | ℥ ss | |
| Calamini Prep. | } | |||
| Sulphuris Precip. | } | |||
| Aquæ Puræ | ℥ vi | |||
| M. (Allingham). | ||||
Forced dilitation as a means of relief and cure for certain forms of rectal trouble, although a much abused and somewhat barbarous practice, has positive and undoubted merits. It is only justified, however, in peculiar and isolated cases.
The wholesale stretching of the sphincter ani muscles as a “cure all” is certainly to be deprecated as unscientific, illogical, and without the advantages or benefits claimed for it by rattling and noisy fanatics. Divulsion injudiciously employed may be followed by a long and tedious recovery, complicated with very undesirable sequelæ and thereby excites much adverse criticism.
The case of a lady recently came under my observation, who, although in average health, complained a little as many women do, and thought she was troubled with hemorrhoids. Through the advice of her physician, a college professor, she submitted to the operation of stretching on general principles. Irritability of the rectum followed, with soreness and continued pain. Finally two large sympathetic buboes developed, which suppurated, and were slow in healing. This happened a little over a year ago, I am reliably informed, and she has not yet fully recovered.
A number of cases have come to my notice where stretching was practiced for the cure of piles, imaginary spasmodic[79] stricture, etc., without the least benefit, except, possibly, that accruing to the physician.
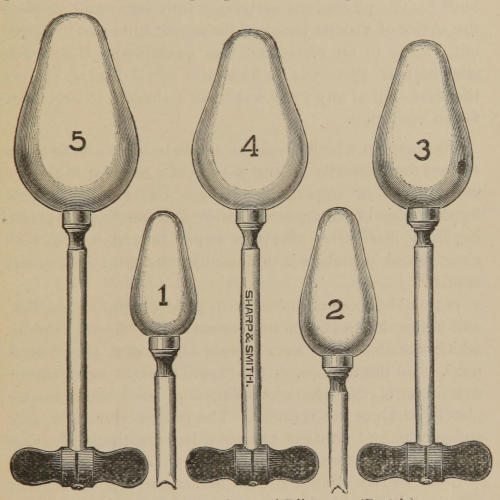
Fig. 30.—Graduated Rectal Dilators. (Pratt’s).
A young married man, foreman of a printing-office, complained at times of slight pain in the region of the liver. His physician, an editor of a medical journal, made an examination of the rectum with a speculum, and informed him[80] that it would be necessary, to preserve his health, to undergo the operation of stretching the sphincters.
The day was appointed and hour set for the operation, which, fortunately for the young man, was “nipped in the bud” by the physicians arriving a little late; and through the advice of a friend he seized the opportunity and “skipped out,” came to my office, and was examined. His bowels were regular, there was no history of rectal disease, and not the least sign of any; nor was there a shadow of an excuse for an operation.
The cases in which divulsion seems to be of greatest benefit are found mostly among women of a peculiar high nervous tension or organization, where the muscles become hypertrophied from repeated spasm, and constipation resulting from ineffectual efforts to expel the feces. In such cases forced dilitation is followed by the most satisfactory results.
It should be accomplished with patient lying on the side, and under the most profound anæsthesia. Rectal dilators, which distribute the force evenly all around, may first be used, then the thumbs, or the thumb of right hand and index finger of the left, or two fingers of each hand, to completely paralyze the muscles. The process should be slow and gentle, and caution exercised lest the tissue give way from the application of undue force.
Local causes should always be sought, and excluded if practical, before heroic measures are adopted for the relief of spasmodic sphincter. There are instances where tightness of the sphincters exist, superinducing constipation, etc.,[81] not traceable to any appreciable cause. These cases may be relieved without the aid of general anæsthesia, by graduated dilators or rectal bougies, accomplishing little at a time, daily or tri-weekly.
When constipation depends upon inertia, or a lack of expulsive power of the rectum, I think moderate dilitation advisable and decidedly beneficial.
These innocent growths can be successfully removed, when within reach and most of them are, without the loss of blood or the infliction of pain, by carbolic acid injection to act as a styptic and deaden the sensibility, while the scissors is used to sever their connection with the bowel.
Allusion is made, in speaking of the diagnosis of hemorrhoids, to the different forms and varieties of polypi, consequently no further description of them will be given here. Polypi, being more dense and fibrous than hemorrhoids, are not readily permeated by the injection compound. Neither can the hemorrhoidal needle be used with any advantage unless they be large and soft in structure. Therefore a small hypodermic needle is selected and 95 per cent. carbolic acid. This strength of carbolic acid is not only a powerful styptic and cauterant, but its fluidity permits it to be forced throughout the fibrous structure with ease.
The action of the acid should extend fully to the base of the polypus, which is then clipped off a little outside of the[82] line. The stump goes through similar changes to that of hemorrhoids after injection. In long or pediculated polypi, it will only be necessary to apply the acid at the base sufficiently to intercept the circulation before excision.
A little cocaine may be used first, if the parts are very sensitive, and the same precaution should be taken with regard to the protection of the adjacent and surrounding parts from the excoriating effects of the carbolic acid, as recommended when operating on hemorrhoids.
Inflammation of the rectum, like any other phlegmasia, may arise traumatically or idiopathically; by contiguity of structure or continuity of surface. The acute symptoms are very much like acute dysentery, which disease, in my opinion, nearly always extends to the rectum, causing the characteristic symptoms of weight, tenesmus and straining at stool.
Irritable rectum in the absence of diarrhœa is diagnostic of the complaint. The bladder and prostate may be affected through sympathy, and colicky pain reflected to the small intestines or stomach. In the more chronic forms, constipation, tenderness and the cul-de-sac partially filled with mucous are distinguishing features.
Carbolized hot water irrigation, prepared hot corn starch, slippery elm water, bismuth, etc, together with a suppository of iodoform, bismuth and opium, or bismuth, opium,[83] belladonna and calomel, will be found serviceable in the acute stage. About a half tumbler full of a saturated solution of chlorate of potash, injected slowly and retained for ten or fifteen minutes, is said to effect a cure by one or two injections.
Chronic proctitis, also called irritable rectum, and sometimes rectal catarrh, with symptoms that might be expected to emanate from a disease of the mucous membrane, rarely amounting to a diffuse thickening of the rectal walls, is treated similarly, except less palliative. Combinations of eucalyptol, iodoform and bismuth; or eucalyptol ½ dr., oxide of zinc 1 dr., vaseline 1 oz., are highly recommended after the rectal douche.
Some physicians hold that chronic inflammation of the rectum is a disease of more frequent occurrence than all other rectal diseases combined. And equally as pernicious, causing many functional and even organic troubles through reflex action.
I have always been loath to admit the value of a thing which did not come from an authoritative source. A little retrospective medicine, however, is sufficient to teach any of us that many important discoveries have been made without the free-will and full consent of “acknowledged authorities;” and that it is not positively necessary for progressive physicians to first obtain their permission before being allowed to think and act for themselves.
Flushing the colon is a discovery of intrinsic worth, brought to notice in an irregular way, and has its place as a remedial agent with which every physician should become familiar. If you doubt its efficacy, and want a free evacuation of the bowels without taking physic, lie on the back and inject into the rectum slowly with a bulb-syringe one-half gallon or more of hot water, and you will get it inside of fifteen minutes.
I do not see that Dr. A. W. Hall, who claims in his health pamphlet to be the father of the process, and whose name bears the titles of Ph.D. and LL.D., and consequently deserving of the respect of an educated man, makes out a clear case in defense of his “New Hygienic Treatment” as a life-giving principle, either in health or disease.
His argument is certainly unphysiological, and we are left to infer that nature has been derelict in the construction of man, which he has been instrumental in supplementing. If he were to confine himself to disease alone, his reasoning would appear more plausible; but he claims that people enjoying good health, with no physical ailment whatever, should wash out the colon.
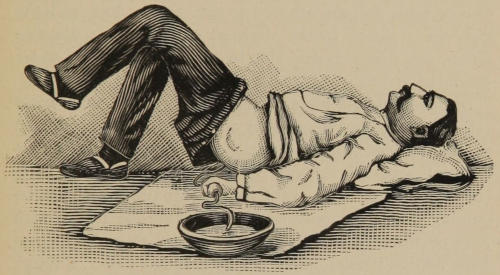
Fig. 31.—Flushing the Colon.
No doubt Dr. Hall has been greatly benefited by flushings of the colon, as also have many others, which offers some apology for the enthusiasm and interest he manifests in the “new revelation;” but we shall be compelled to look to others for the pathological conditions in which it will be found of greatest service.
Respecting the colon itself, there are two very diverse conditions, with their concomitant symptoms, in which[86] flushing will be found of great benefit. The one a diseased condition of the mucous membrane, of a chronic dysenteric or an ulcerative character. The other, a sluggishness or torpidity of the bowel belonging to a constipated habit.
The most easy, simple and efficient manner of practicing the flushings, according to my experience, is by assuming the position shown in the cut. A piece of oil-cloth, rubber-cloth, or a newspaper may be used to protect the carpet. One or both feet are allowed to rest on the floor, and the hips can be raised by the slightest exertion for a few moments, any time it is desirable to hold and hasten the water down the incline.
Beginners should use a common bulb syringe, with water rather hot, varying in quantity as they become accustomed to the process, from a quart to a gallon or more, and a bulb-full squeezed out slowly, with intervals between, giving it time to pass out of the rectum into the colon. On regaining the erect posture, if the rectum be loaded with feces or distended with water, the desire to expel its contents may be irresistible, especially if air has passed through the syringe; although a little practice will enable any one to exert great control over his or herself in this respect.
Dr. F. H. Etheridge (Trans. Chicago Med. Soc.) gives a number of cases of impacted colon, where daily flushings, extending over a period of from one to three months in each case, were followed by the most grateful results. This, too, after the persistent use of drugs had almost hopelessly failed to even afford temporary relief.
Without segregating the cases, some of the diseased conditions[87] mentioned in connection with his patients were dyspepsia, characterized by anorexia, acid and bitter eructations, bad taste in the mouth, gaseous distention, gastric weight and pain. Also cephalalgia, chills, vertigo, chloasmic spots, muddy sclerotics and complexion, insomnia, ennui, eczema, psoriasis, dysuria, etc.
He says: “Daily movements of the bowels are no sort of a sign that the colon is not impacted; in fact, the worst cases of costiveness that we ever see are those in which daily movements of the bowels occur. The diagnosis of fecal accumulations is facilitated by inquiring as to the color of the daily discharges. A black or a very dark green color almost always indicates that the feces are ancient. Prompt discharge of food refuse is indicated by more or less yellow color. It would be interesting to inquire why fresh feces are yellow and ancient feces are dark.
“Absorption of the feces from the colon leads to a great many different symptoms; amongst others, anæmia, with its results, sallow or yellow complexion, with its chloasmic spots, furred tongue, foul breath, and muddy sclerotics. Such patients have digestive fermentations to torment them, resulting in flatulent distention, which encroaches on the cavity of the chest, which in excessive cases may cause short and rapid breathing, irregular heart action, disturbed circulation in the brain, with vertigo and headache. An over-distended cæcum, or sigmoid flexure, from pressure, may produce dropsy, numbness or cramps in the right or left lower extremity.
“I have often questioned whether chloasmic spots were[88] not due to fecal absorption. These spots are pigmentary matter deposited under the skin. It is a physiological fact that all pigments originate in the liver. In a condition of health their abnormal deposit we never see. It is only when the patient is not well, in some way, that these spots are noticed. They are infinitely more common in women than in men. It is easy to see that their sedentary life is more apt to lead in them to the filling of the colon. Absorption from the colon produces a poisoned blood, which in turn deranges every organ of the body, among others the liver. It is possible that the action of light, as in photographs, contributes in some way to precipitate the deposits of these chloasmic spots, because we see them chiefly upon the parts of the body exposed to light....
“The use of a long rectal tube is unnecessary. The patient should be placed in a genu-pectoral position, the shoulders thus being lower than the hips. The water will be made to descend while anatomically ascending the intestines. Patients can be made to receive from one to six pints of water in this position without the slightest trouble. One of the effects of the water is to distend the colon, and in that way pressing away the walls of the loculi from the accumulations that fall into the current of water and are passed out while the water is leaving the intestine. The patient will oftentimes complain of severe tormina, checking the current of water for a few seconds, and will be followed by complete relief. The presence of such a strange foreign body in the intestine as hot water in many cases excites[89] prodigious peristaltic activity, thus producing the tormina. Plain hot water is all that is necessary to use; the water should be hot; cold water, or tepid water, will not do. It will produce great suffering. One patient took the flushings for a fortnight, returning vowed she would never use any more because they produced such terrific cramps. Upon inquiry it was found that she was using tepid water. The subsequent use of hot water by her was never followed by a cramp. Upon many patients this large amount of water acts as a vigorous diuretic. Where patients suffer as well from renal insufficiency, I am in the habit of telling them to use a pint or a pint and a half of hot water after the flushing has passed away, and to lie upon the back with hips elevated for half an hour. Thus retaining the water, it will act as a powerful diuretic. Some patients can administer this flushing with greatest ease, while others will develop a most phenomenal awkwardness. I am in the habit of telling patients to kneel in the bath-tub, who are at all awkward about using these flushings.”
The lower end of the rectum is richly supplied with both sensory and sympathetic nerves. The sensory greatly predominating at the verge, making it one of the most acutely sensitive surfaces of the body. In ascending upwards the sensory gradually give place to the sympathetic, until little sensibility is imparted by the touch three inches from the entrance in a normal condition.
This accounts for the hidden cause of so many reflexes, having their seat of origin from lesions an inch or more above the anus, where the sensibility is not always sufficiently great to attract attention.
It has been claimed that obscure rectal disorders may so undermine the nervous system by reflex irritation, allowing the inroad of general systemic disease, that many die yearly from this as the primary cause, without ever knowing the source and origin of the fatal malady.
That migratory pain, headaches, dyspepsia, sleeplessness, palpitations, sexual weakness, nervousness, despondency, irritability, and a general breaking down of the system, may all be caused by a small ulcer or other irritation of the rectum, which has passed unnoticed by either physician or patient.
Nearly every physician is familiar with the white ring around the mouth extending up the sides of the nose, produced by the presence of pin worms in the rectum, or a fatal lock-jaw caused by a broken off needle or rusty nail in the foot. Such illustrations alone, are sufficient to demonstrate conclusively the power of this dynamical disturbance called reflex action.
While there is doubtless unwarrantable exaggeration concerning rectal reflexes by some, there are many unpardonable oversights by others. A case was reported in the Medical Record where all preparations were made to operate for organic stricture of the urethra, which, perchance, proved to be a reflex from a small rectal fissure. When the fissure was cured the spasm ceased. A case of roaring in the right ear was relieved by the cure of a fistula, says Dr. Rorick, who also speaks of two other similar cases.
A very remarkable case occurred in my own practice, where the right testicle had been enlarged to the ordinary size of a well developed case of orchitis for some years, and had resisted all manner of treatment, completely disappeared after the removal of hemorrhoids. The case of hemorrhoids, which was one of the worst I ever saw, is represented in Fig. 2.
Another case was that of a merchant, who suffered frequently from a sensation of drawing and weight in the back of the head and neck. When these attacks came on, his memory became so badly impaired that he was rendered unfit for the transaction of business. He noticed during the attacks that there was a feeling of heaviness in the rectum,[92] swelling and tightness of the sphincters, and a lack of expulsive power at stool.
Examination revealed several pockets and papillæ of the variety shown in Fig. 23, which was taken from this case. Have not been apprised of any return of the trouble since an operation for the removal of these abnormalities.
As evidence that physicians should be a little more vigilant in the observation and study of rectal reflexes, the case of a very talented and influential lady of this State might be appropriately instanced. Her general health had been greatly impaired for a long time, with unexplained and repeated outbursts of sickness. Several prominent physicians were consulted, to whom she called attention to a little uneasiness, at times, in the rectum with an irritable bladder. They all examined the rectum, in their way, and ridiculed the idea of local disease, but went on treating the reflex symptoms, with nothing more than temporary relief.
The successes of a local specialist in the treatment of hemorrhoids by the Brinkerhoff system, whose ignorance of anatomy was such that he denominated the sphincters “dispenser” muscles, induced her to pay him a visit. He found a well defined superficial rectal ulcer, and exhibited it to one of the previously named doubting physicians. The ulcer was quickly healed and the lady restored to health.
She became so enthused over the result, that she took up the study of rectal diseases for the benefit of others, as a missionary, so to speak; and it is needless to say that the physicians who failed to detect the cause of her trouble did not reap any of the emoluments of her labors, but there[93] were several irregular practitioners who were ready listeners, took in some handsome fees as a reward. Her motto, true to a grateful nature, was to “praise the bridge that carries you over.”
Condyloma, from kondulos Gr., a “knot,” or “tubercle,” may be applied to any small, hard tumor, flaps, tabs of flesh or wart-like excrescence about the anus, whether of syphilitic or non-syphilitic origin.
They may take the form of one of the radiating folds, or flattened transversly by the pressure of the buttocks, and consist of a hypertrophy of the skin from localized inflammation or irritation, and sometimes continue to grow after the cause has been removed.
A cutaneous tag as a relic of an external hemorrhoid, after it has lost its identity and become dense in structure, is properly a condyloma; also a warty vegetation developed from the papillary layer of the derma. Certain forms of condylomata are pathognomonic of ulceration and other serious changes going on above. The discharge at the anus producing these fleshy tags.
Some writers prefer to limit the meaning of the word to certain varieties of growths about the anus. But it appears less liable to confuse, to use it in a literal and a generic sense; making the varieties associated with their causes,[94] qualifying terms: as syphilitic, non-syphilitic, warty, cancerous, innocent, etc.
The objection to cocainizing condylomatous growths of any size, and excising them, is the annoyance from the bleeding that sometimes follows, which will often break through a heavy crust of Monsels’ salt. The prettiest way to remove them is by galvano-cautery. When electricity is not at hand, carbolic acid injection is equally as effective. It may be necessary where the skin is thick and horny in texture, to afterwards trim off the remaining ragged edges with the scissors.
Neuralgia of the rectum as a clinical entity is rare indeed. Mention is made here simply in acknowledgment of the affection, having met with but one case, and that in a very nervous and delicate lady, who maintained that she was cursed with a rectal ulcer.
In obedience to this idea her physician had examined the rectum, under anæsthesia, and found what he called a rectal ulcer at a point where the uterine cervix rests on the rectum. His diagnosis was, no doubt, founded upon her belief, and as an apology for the examination and treatment resorted to, which put her to bed for six weeks.
There were no symptoms of rectal ulcer, other than pain, and no lesion found by a digital examination or seen through a speculum. She insisted on taking chloroform[95] and a more thorough examination made. This was done without revealing anything more than what had already been ascertained, and the diagnosis of neuralgia confirmed.
Pain continued, periodical or irregular, in the absence of mechanical pressure (uterine) or structural lesion, in the region of the sphincters, or higher up, is diagnostic. If in the sphincters alone, dilitation may be sufficient. When higher up, constitutional treatment with galvanism is advised.
Injection formula of:—
| ℞ | Sodæ Bibor. | ||
| Acidi Salicyl. | ā ā | ʒ i | |
| Glycerinæ | ℥ i | ||
| Acidi Carbolici | ℥ iii | ||
| Misce. | |||
(5 per cent. sol.)
| ℞ | Acidi Carbolici | gr. xxiv |
| Aquæ Destil. | ℥ i | |
| Misce. | ||
(3 per cent. sol.)
| ℞ | Acidi Carbolici | gr. xviss |
| Aquæ Destil. | ℥ i | |
| Misce. | ||
(A traveling pile doctor.)
| ℞ | Acidi Carbolici | ℥ i |
| Creosoti | gtt. x | |
| Acidi Hydrocyan. | gtt. i | |
| Olei Olivæ | ℥ i |
Mix and unite by heat in a water bath. Inject enough to turn the tumor an ashen grey color.
| ℞ | Acidi Carbolici | 40 | per cent. |
| Fl. Ext. Ergotæ | 15 | ” | |
| Glycerinæ | 15 | ” | |
| Aquæ Dest. | 30 | ” | |
| Misce. | |||
| ℞ | Acidi Carbolici | ℥ i |
| Olei Olivæ | ℥ v | |
| Zinci Chloridi | gr. viii | |
| Misce. | ||
| Largest piles, | 8 | minims. |
| Medium piles, | 4 to 8 | ” |
| Small piles, | 2 to 3 | ” |
| Page | 5, | 1st line, there in for there is. |
| ” | 17, | Weaker solution for Weaker solutions. |
| ” | 22, | Bism. Subuit. for Bism. Subnit. |
| ” | 22, | Iodoformis for Iodoformi. |
| ” | 23, | Resin Cirate for Resin Cerate. |
| ” | 52, | After the treatment for The after-treatment. |
| ” | 57, | Three inches for Three and a half inches. |
| ” | 64, | Incisions for Incision. |
Transcriber’s Note: The errata have been corrected.